Abstract
Background
Atrial arrhythmias are commonly noted in patients with alcohol withdrawal syndrome (AWS), requiring inpatient admission.
Objective
The burden of arrhythmias and the association with in-hospital outcomes are incompletely defined in patients hospitalized with AWS.
Methods
The nationwide inpatient sample database was accessed from September 2015 to December 2018 to identify hospitalizations for AWS. We studied a cohort of patients with arrhythmias noted during hospitalization using the appropriate International Classification of Diseases, Tenth Revision billing codes. We compared patient characteristics, outcomes, and hospitalization costs between alcohol withdrawal hospitalizations with and without documented arrhythmias. Propensity score matching (PSM) and multivariate regression were performed to control confounders and develop odds ratios (OR), respectively.
Results
Among 1,511,155 hospitalization with AWS, 146,825 (9.72%) had concurrent arrhythmias. After PSM, we identified 135,540 cases in each group. Hospitalizations with AWS and concurrent arrhythmias had higher in-hospital mortality (4.19% vs 1.95%, OR 1.76, confidence interval [CI] 1.67–1.85, P < .0001). The most common arrhythmia was atrial fibrillation (66.7%). Arrhythmias in AWS were also associated with poorer in-hospital outcomes, including a higher risk of acute heart failure (8.40% vs 4.58%, OR 1.97, CI 1.90–2.05, P < .0001), acute kidney injury (21.32% vs 15.27%, OR 1.39, CI 1.36–1.43, P < .0001), and acute respiratory failure (9.19% vs 5.49%, OR 1.70, CI 1.64–1.76, P < .0001) requiring intubation. The length of hospital stay (6 days vs 4 days P < .0001) and cost of hospital care ($12,615 [$6683–$27,330] vs $7860 [$4482–$15,868], P < .0001) were higher in AWS with arrhythmias.
Conclusion
Arrhythmia in AWS is associated with higher in-hospital mortality and poorer in-hospital outcomes.
Keywords: Alcohol withdrawal syndrome, Arrhythmia, Atrial fibrillation, Acute heart failure, Mortality, Acute kidney injury, Acute respiratory failure
Key Findings.
-
▪
Atrial fibrillation is the most common arrhythmia associated with alcohol withdrawal syndrome (AWS).
-
▪
AWS complicated by arrhythmias is associated with higher all-cause in-hospital mortality.
-
▪
AWS complicated by arrhythmia leads to poor in-hospital outcomes, extended hospital stay, and higher costs.
Introduction
Alcohol use disorder (AUD) is a serious disease among the adult population in the United States, with an estimated prevalence of 15 million.1,2 In 2016, AUD accounted for approximately 3 million deaths worldwide.3 It is well known that alcohol consumption increases the risk of arrhythmias.4 Prior data revealed that even 1 glass of any alcoholic beverage could increase the odds of having an episode of atrial fibrillation (AF) by 2-fold.5
One of the frequent consequences of AUD is alcohol withdrawal syndrome (AWS), affecting one-fifth of patients during emergency department encounters, intensive care unit admissions, and the perioperative period.2,6,7 AWS occurs after cessation of persistent drinking and, given the absence of drinking during hospitalization, can manifest during time as an inpatient.
However, real-world data regarding mortality and in-hospital outcomes in AWS complicated by arrhythmia are limited. Therefore we sought to perform a nationwide study from the National Inpatient Sample (NIS) to address this question.
Methods
Data sources
A retrospective analysis of 1,511,155 alcohol withdrawal–related hospitalizations in patients aged >18 years with or without arrhythmias was conducted from September 2015 to December 2018 using the NIS database. The NIS is an administrative database inclusive of all the insured and uninsured hospitalized patients in the United States generated by the Healthcare Cost and Utilization Project (HCUP) sponsored by the Agency for Healthcare Research and Quality (AHRQ) from the 46 participating US states.8 It incorporates a stratified sample of 20% nonfederal US community hospitals. NIS includes all patients covered by Medicare, Medicaid, and private payers, as well as those who are uninsured. Weighted, it represents more than 95% of the US population, providing nationwide estimates of over 35 million hospitalizations annually, and consists of patient-level data points, up to 25 discharge diagnoses, and up to 15 procedural diagnoses. Its large sample size is ideal for developing national and regional estimates and enables analyses of rare conditions, uncommon treatments, and special populations. The NIS database has been used effectively recently to study arrhythmia risk in various conditions.9 Since NIS uses de-identified hospital discharges as samples with prior ethical committee approval, no additional ethical committee approval was required for the present analysis. The Reporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement, a checklist of items, is provided as Supplemental Table 1.
Study cohort
We used International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) codes to identify hospitalizations in patients aged 18 years or older with AWS and divided patients into 2 groups—those with and those without arrhythmias. Demographic information, including age, sex, race, insurance status, comorbidities, types of arrhythmias, hospital characteristics, location/teaching status, and regions, was evaluated. The prevalence of different arrhythmias was analyzed using appropriate ICD-10-CM codes (Supplemental Tables 2 and 3). The primary outcome was all-cause in-hospital mortality. Secondary outcomes included acute heart failure (AHF), acute kidney injury (AKI), acute respiratory failure requiring intubation, length of stay, and total hospital charges. We also performed subgroup analysis looking at the in-hospital mortality and outcomes independently for some of the most common arrhythmias.
Statistical analysis
We compared hospitalizations for baseline demographics, hospital characteristics, comorbidities, and outcomes. Most hospital-level characteristics were directly extracted as provided in the NIS, whereas the Elixhauser Comorbidity Index was used to identify comorbid disorders. To obtain the cost of hospitalization, hospital charges were multiplied with the cost-to-charge ratios for each hospital for a given year and indexing to the year 2018 to adjust for inflation.10
Categorical variables are presented as numbers and percentages and were obtained using the χ2 test. Numerical variables are presented as the median and interquartile range and were obtained using the Wilcoxon test. A 2-tailed P value of <.05 was used to determine the statistical significance. As recommended, discharge weights were used to generate national estimates.11 Next, we examined whether concomitant arrhythmia in AWS was associated with a higher risk of our study endpoints. Since patients in the arrhythmia group may differ from those without arrhythmias, we used a matched propensity score analysis to account for confounding. The propensity score was estimated using a nonparsimonious logistic regression model, which included all comorbidities to balance the differences between the 2 groups. Propensity matching was performed with a 1-to-1 scheme without replacement, using the nearest-neighbor matching and a caliper width of 0.05 on the probability scale. Hospitalizations that could not match per the above-mentioned caliper width were excluded to mitigate bias as best as possible because their comorbidities were out of proportion to the rest of the cohort. We have followed the methodology for data analysis as recommended by the NIS-HCUP and included in Supplemental Table 4. Finally, logistic regression was performed to calculate the adjusted odds ratio (OR) with confidence intervals (CI). We utilized SAS 9.4 (SAS Institute, Inc, Cary, NC) software for statistical analyses.
Results
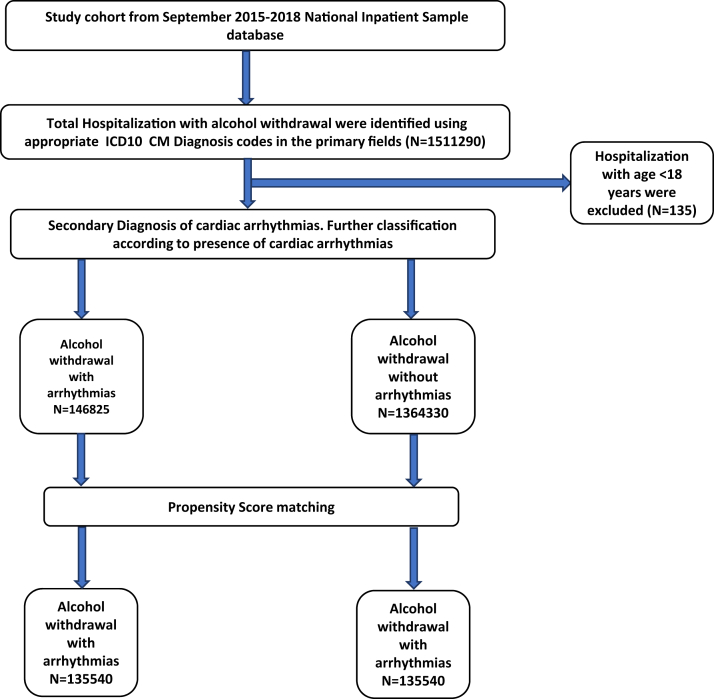
Out of 1,511,155 AWS hospitalizations with >18 years of age, 146,825 (9.7%) had associated arrhythmias and 1,364,330 were without arrhythmia (90.2%). After propensity score–matched analysis, each group had 135,540 hospitalizations (Figure 1). AWS hospitalizations with arrhythmia were more frequent in white (81.13%) males (81.95% male vs 18.05% female, P < .0001) and between 55 and 65 years of age (34.02%, P < .0001). Similar results were found after propensity-matched analysis (Table 1).
Figure 1.
Patient selection and study design.
Table 1.
Demographics and baseline characteristics of alcohol withdrawal hospitalizations
| Alcohol withdrawal without arrhythmias N = 1,364,330 |
Alcohol withdrawal with arrhythmias N = 146,825 |
P value | Alcohol withdrawal without arrhythmias (propensity matched) N = 135,540 |
Alcohol withdrawal with arrhythmias (propensity matched) N = 135,540 |
P value | |
|---|---|---|---|---|---|---|
| Age (mean) | 49.20 ± 12.59 | 59.332 ± 12.38 | <.00001 | 52.72 ± 12.64 | 59.00 ± 12.44 | <.0001 |
| Age groups | <.0001 | <.0001 | ||||
| ≥18 to <45 | 34.50% | 11.49% | 25.75% | 12.01% | ||
| ≥45 to <55 | 30.05% | 20.82% | 28.96% | 21.02% | ||
| ≥55 to <65 | 24.97% | 34.02% | 28.95% | 34.13% | ||
| ≥65 to ≤75 | 8.49% | 23.08% | 12.79% | 22.59% | ||
| >75 | 1.99% | 10.60% | 3.55% | 10.25% | ||
| Sex | <.0001 | <.0001 | ||||
| Male | 73.70% | 81.95% | 74.41% | 81.63% | ||
| Female | 26.30% | 18.05% | 25.59% | 18.37% | ||
| Types of admission | <.0001 | .09 | ||||
| Elective | 7.87% | 6.12% | 6.19% | 6.03% | ||
| Nonelective | 92.13% | 93.88% | 93.81% | 93.97% | ||
| Race | <.0001 | <.0001 | ||||
| White | 72.64% | 81.13% | 73.71% | 80.99% | ||
| Black | 11.84% | 9.59% | 12.63% | 9.64% | ||
| Hispanic | 10.19% | 6.02% | 8.93% | 6.09% | ||
| Asian/PI | 0.85% | 0.58% | 0.79% | 0.56% | ||
| Native American | 1.62% | 1.06% | 1.37% | 1.08% | ||
| Other | 2.86% | 1.63% | 2.57% | 1.64% | ||
| Primary payer | <.0001 | <.0001 | ||||
| Medicare | 20.41% | 42.22% | 27.39% | 41.31% | ||
| Medicaid | 39.07% | 26.38% | 35.27% | 27.00% | ||
| Private | 23.60% | 20.48% | 22.86% | 20.41% | ||
| Others | 16.91% | 10.92% | 14.47% | 11.28% | ||
| Income quartile | <.0001 | <.0001 | ||||
| 0–25 | 30.65% | 28.34% | 30.88% | 28.43% | ||
| 26–50 | 25.23% | 25.00% | 25.92% | 24.94% | ||
| 51–70 | 23.83% | 24.82% | 23.90% | 24.85% | ||
| 76–100 | 20.30% | 21.84% | 19.30% | 21.78% | ||
| Comorbidities | ||||||
| Obesity | 6.03% | 10.29% | <.0001 | 8.76% | 8.77% | .97 |
| OSA | 2.31% | 6.47% | <.0001 | 4.89% | 4.88% | .92 |
| HTN | 47.10% | 59.37% | <.0001 | 59.63% | 59.60% | .87 |
| HLD | 14.29% | 27.76% | <.0001 | 26.16% | 26.14% | .93 |
| DM | 5.85% | 7.05% | <.0001 | 6.36% | 6.36% | .96 |
| Hypothyroidism | 4.40% | 5.57% | <.0001 | 4.82% | 4.83% | .92 |
| CHF | 3.39% | 18.70% | <.0001 | 15.64% | 15.63% | .95 |
| Cardiogenic shock | 0.17% | 2.11% | <.0001 | 0.81% | 0.83% | .67 |
| COPD | 17.38% | 26.45% | <.0001 | 25.31% | 25.30% | .96 |
| CKD | 2.31% | 6.25% | <.0001 | 4.87% | 4.86% | .85 |
| Pulmonary HTN | 0.42% | 1.19% | <.0001 | 0.69% | 0.69% | .99 |
| Smoking (tobacco use disorder) | 50.05% | 42.23% | <.0001 | 42.52% | 42.53% | .96 |
| Drug abuse | 8.07% | 6.65% | <.0001 | 6.17% | 6.17% | .99 |
| Valvular heart disease | 0.94% | 4.08% | <.0001 | 2.76% | 2.76% | .90 |
| Electrolyte imbalance | 44.93% | 56.92% | <.0001 | 56.94% | 56.93% | .95 |
| Coagulopathy | 18.36% | 22.71% | <.0001 | 22.11% | 22.13% | .88 |
| Prior MI | 2.51% | 6.00% | <.0001 | 4.83% | 4.82% | .96 |
| PVD | 1.82% | 4.97% | <.0001 | 3.90% | 3.90% | .99 |
| Liver diseases | 19.07% | 19.56% | <.0001 | 19.09% | 19.08% | .98 |
| Hospital characteristics | ||||||
| Hospital bed size | <.0001 | |||||
| Small | 22.68% | 19.95% | 22.69% | 20.13% | <.0001 | |
| Medium | 29.62% | 29.77% | 29.70% | 29.77% | ||
| Large | 47.70% | 50.28% | 47.61% | 50.10% | ||
| Hospital region | <.0001 | <.0001 | ||||
| Northeast | 25.91% | 22.82% | 23.03% | 23.12% | ||
| Midwest | 22.82% | 22.54% | 27.00% | 22.19% | ||
| South | 30.29% | 31.59% | 31.41% | 31.65% | ||
| West | 20.98% | 23.06% | 18.57% | 23.04% | ||
| Hospital location | <.0001 | <.0001 | ||||
| Rural | 7.93% | 6.98% | 7.75% | 6.96% | ||
| Urban non-teaching | 22.29% | 22.80% | 21.60% | 22.81% | ||
| Urban teaching | 69.78% | 70.22% | 70.65% | 70.23% |
CHF = congestive heart failure; CKD = chronic kidney disease; COPD = chronic obstructive pulmonary disease; DM = diabetes mellitus; HLD = hyperlipidemia; HTN = hypertension; MI = myocardial infarction; OSA = obstructive sleep apnea; PI = Pacific Islander; PVD = peripheral vascular disease.
Comorbid conditions such as hypertension (59.37% vs 47.10%, P < .0001), obstructive sleep apnea (6.47% vs 2.31%, P < .0001), congestive heart failure (HF) (18.70% vs 3.39%, P < .0001), obesity (10.29% vs 6.03%, P < .0001), chronic obstructive pulmonary disease (26.45% vs 17.38%, P < .0001), chronic kidney disease (6.25% vs 2.31%, P < .0001), etc, occurred more frequently among AWS patients with arrhythmias. However, after propensity-matched analysis, there was no difference in the comorbidities between the 2 groups (Table 1).
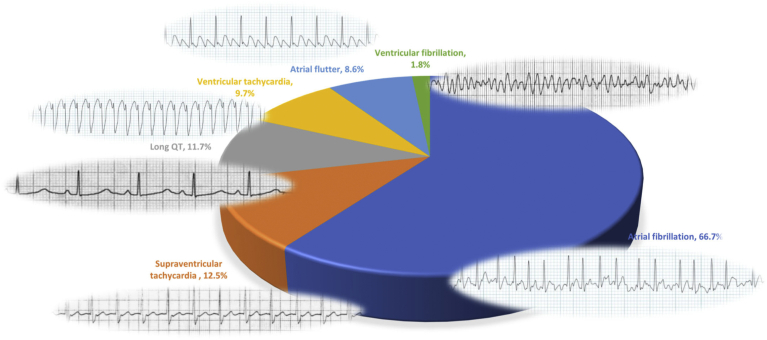
Among all the arrhythmias identified in AWS, AF was the most common (66.70%), followed by supraventricular tachycardia (SVT) (12.54%), long QT (11.67%), ventricular tachycardia (VT) (9.69%), and atrial flutter (8.61%) (Figure 2).
Figure 2.
Spectrum of arrhythmias in alcohol withdrawal. This figure illustrates the frequency of different arrhythmias in hospitalizations with alcohol withdrawal.
In-hospital outcomes
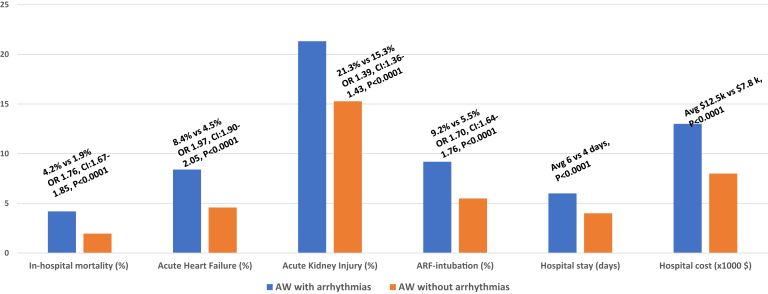
All-cause-in-hospital mortality was higher in AWS with arrhythmias (4.19% vs 1.95%, OR 1.76, CI 1.67–1.85, P < .0001). In addition, patients with AWS and arrhythmias were significantly associated to have an increased risk of HF (8.40% vs 4.58%, OR 1.97, CI 1.90–2.05, P < .0001), AKI (21.32% vs 15.27%, OR 1.39, CI 1.36–1.43, P < .0001), and acute respiratory failure requiring intubation (9.19% vs 5.49%, OR 1.70, CI 1.64–1.76, P < .0001) (Tables 2 and 3, Figure 3).
Table 2.
Outcomes in alcohol withdrawal hospitalizations with and without arrhythmias
| Outcomes | Without arrhythmias N = 135,540 |
With arrhythmias N = 135,540 |
P value |
|---|---|---|---|
| All cause in-hospital mortality (%) | 1.95% | 4.19% | <.0001 |
| Length of stay median (days) | 4 | 6 | <.0001 |
| Total hospital charges, median (range), $ | 7860 (4482-15,868) | 12,615 (6683-27,330) | <.0001 |
| Acute kidney injury | 15.27% | 21.32% | <.0001 |
| Acute heart failure | 4.58% | 8.40% | <.0001 |
| Acute respiratory failure requiring intubation | 5.49% | 9.19% | <.0001 |
P value <.05 indicates clinical significance.
Table 3.
Odds ratio for outcomes in alcohol withdrawal hospitalizations with and without arrhythmias
| Outcomes | aOR | LL | UL | P value |
|---|---|---|---|---|
| All-cause in-hospital mortality | 1.76 | 1.67 | 1.85 | <.0001 |
| Acute kidney injury | 1.39 | 1.36 | 1.43 | <.0001 |
| Acute heart failure | 1.97 | 1.90 | 2.05 | <.0001 |
| Acute respiratory failure requiring intubation | 1.70 | 1.64 | 1.76 | <.0001 |
Significant P < .05 at 95% confidence interval. Logistic regression model was adjusted for age, sex, race, admission type, hospital characteristics, and relevant comorbidities.
aOR = adjusted odds ratio; LL = lower level; UL = upper level.
Figure 3.
Impact of arrhythmias in outcomes of alcohol withdrawal (AW).
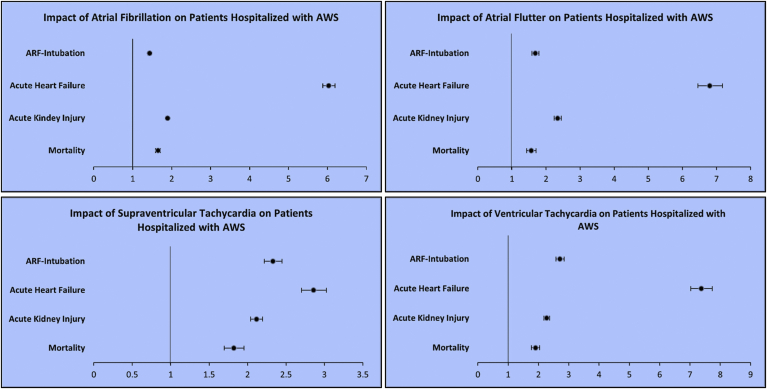
The median length of hospital stay (6 days vs 4 days, P < .0001) and cost of hospitalization ($12,615 [$6683–$27,330] vs $7860 ($4482–$15,868), P < .0001) were significantly greater among AWS hospitalizations with arrhythmias compared to those without. The in-hospital mortality after matching for secondary outcomes including AHF, AKI, and respiratory failure requiring intubation remained higher (2.95% vs 2.09%, OR 1.39, CI 1.31–1.48, P < .0001) in AWS patients with arrhythmias as opposed to those without arrhythmias. Additionally, we found similar results describing higher mortality and secondary outcomes for individual arrhythmia, including AF, atrial flutter, SVT, and VT (Figure 4).
Figure 4.
In-hospital outcomes in patients hospitalized with alcohol withdrawal based on types of arrhythmias. A: Odds ratio of outcomes in alcohol withdrawal hospitalizations with atrial fibrillation. B: Odds ratio of outcomes in alcohol withdrawal hospitalizations with atrial flutter. C: Odds ratio of outcomes in alcohol withdrawal hospitalizations with supraventricular tachycardia. D: odds ratio of outcomes in alcohol withdrawal hospitalizations with ventricular tachycardia. ARF-Intubation = acute respiratory failure requiring intubation; AWS = alcohol withdrawal syndrome.
Discussion
In this study, we performed an analysis of 1,511,155 hospitalizations for AWS and found 146,825 had associated arrhythmias (9.72%).
The main findings of our study were that patients with AWS complicated with arrhythmias had the following: (1) an increased all-cause in-hospital mortality; (2) increased risk of AHF, kidney injury, and respiratory failure requiring intubation; and (3) a longer length of stay and higher cost of care; and the most common arrhythmia was AF.
Alcohol use and arrhythmias
Data regarding arrhythmias associated with AWS are scarce. In a study by Bär and colleagues,12 in some of the electrocardiogram findings in AWS patients, most importantly alternating QT intervals were revealed. Another study by Cuculi and colleagues13 reported several tachyarrhythmias, including SVT, AF, sustained VT, and torsades de pointes in AWS patients. Of all alcohol-induced supraventricular arrhythmias, prior data suggest that AF is the most common.14 A recent meta-analysis15 showed an association between alcohol consumption and the risk of AF. Alcohol consumption causes direct alcohol cardiotoxicity.16 Alcohol intoxication and withdrawal are associated with hyperadrenergic drive and impaired vagal tone, which in turn increases the intra-atrial conduction time.16 These factors promote the development of re-entries that correspond to the development of AF.14,17 A case-control study by Rich and colleagues18 described that AWS is associated with diffuse beta-adrenergic discharge from the brain stem, causing agitation, hyperthermia, and tremulousness, which increases the risk of arrhythmia, including AF. In addition, a meta-analysis of 53,969 patients concluded that HF in AF is independently associated with higher all-cause mortality compared to HF in sinus rhythm,19 which is again reflected in our study showing a higher risk of AHF and AF being the most common arrhythmia.
Prolonged QT has been reported in studies of patients with alcohol abuse. Ethanol significantly affects the inward L-type calcium currents and outward K currents responsible for repolarization, resulting in QT prolongation.20 Additionally, there is a potential contribution from the high incidence of concomitant polysubstance abuse, psychiatric comorbidities on QT-prolonging medications such as tricyclic depressants and selective serotonin reuptake inhibitors, and underlying electrolyte disturbances due to renal/hepatic dysfunction.14 Campbell and colleagues20 reported long QT as a poor prognostic marker and associated with sudden cardiac death in those with chronic alcoholism. Some of the possible mechanisms contributing to this are polymorphic VT and early afterdepolarizations triggered by the hyperadrenergic state.21
Alcohol withdrawal syndrome and in-hospital outcomes
Alcohol cardiomyopathy is found in individuals with a history of long-term heavy alcohol consumption.22,23 The incidence of alcohol cardiomyopathy ranges from 1% to 2%.24 We have already established that AF can occur owing to alcohol consumption, but the presence of AF or HF increases the likelihood of the other, with acute HF being the strongest risk factor for the development of AF.24 Similarly, AF precipitates and exacerbates left ventricular dysfunction, giving rise to AF-induced cardiomyopathy.24 These theories may explain the increased risk of HF in the arrhythmia group. Interestingly, Lazarević and colleagues22 described that even a moderate amount of alcohol over a long period increases the risk of HF with preserved ejection fraction.
Our study showed an increased risk (21.32%) of AKI in the arrhythmia group, comparable to the development of AKI in 1 in 5 hospitalizations globally.25 The difference in AKI between the cohorts may be explained by the increased incidence of AHF in the arrhythmia group, but this is speculative. HF leads to low cardiac output or congestive status (cardiorenal syndrome) combined with drugs such as diuretics and renin-angiotensin blockade that can cause AKI.26
Admission to the intensive care unit is common in AWS owing to respiratory failure requiring intubation. This occurs in the setting of respiratory collapse (hypoxemia, hypercapnia, and pneumonia), cardiovascular complications (HF, arrhythmias), and the need for frequent high doses of intravenous sedatives.27 The higher occurrence of HF in the arrhythmia group may explain the increased incidence of respiratory distress and intubation need.
AWS and mortality
The in-hospital mortality related to AWS is reported to be between 5% and 10%30, 29, 28 compared to our analysis, where the mortality was about 2% in the cohort without arrhythmias and 4% in the cohort with arrhythmias. Higher mortality in the arrhythmia group may be related to increased sudden death due to malignant VT, which may be a consequence of long QT syndrome in the setting of multiple factors during AWS hospitalization, though this is speculative. We do note that about 10% of the arrhythmia cohort had VT.
Limitations
The present study has several limitations. First, the retrospective nature of the study does not allow for the inference of causality. Second, the documentation of diagnoses using ICD codes may not be completely accurate, adding some uncertainty to the findings. However, the authors used validated codes from literature laid out by HCUP/AHRQ to identify the ICD-10-CM codes for a particular diagnosis or procedure. Third, the order of AWS and arrhythmia occurrence cannot be determined owing to the cross-sectional nature of the database. Fourth, NIS does not allow to differentiate the prior history of arrhythmia vs new-onset arrhythmia. Nonetheless, we took AWS as our primary diagnosis for hospitalization and arrhythmia as secondary diagnosis code while performing analysis. Our study conveys that arrhythmia is associated with worse clinical outcomes irrespective of previous or new onset. Fifth, the NIS database does not allow to follow patients longitudinally; therefore, long-term outcomes could not be assessed. Finally, the present analysis did not account for diagnostic and management strategies, given the database's limitation. However, the strength of our study includes the use of a national database with large population size and propensity score matching to balance out confounders.
Conclusion
Arrhythmias occurring in patients hospitalized with AWS is associated with higher in-hospital mortality and poorer in-hospital outcomes such as AHF, kidney injury, and respiratory failure. These data require future study with prospective analysis to verify such magnitude is clinically actionable.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosures
The authors have no conflicts to disclose.
Authorship
All authors attest they meet the current ICMJE criteria for authorship.
Patient Consent
De-identified information from the National Inpatient Sample (NIS) was used for this analysis; thus, consent was not applicable.
Ethics Statement
Since the NIS uses de-identified hospital discharges as samples with prior ethical committee approval, no additional ethical committee approval was required for the present analysis.
Footnotes
Supplementary data associated with this article can be found in the online version at https://doi.org/10.1016/j.hroo.2021.09.014.
Appendix. Supplementary data
References
- 1.Understanding Alcohol Use Disorder | National Institute on Alcohol Abuse and Alcoholism (NIAAA) https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-alcohol-use-disorder
- 2.Alcohol Facts and Statistics | National Institute on Alcohol Abuse and Alcoholism (NIAAA) https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-facts-and-statistics
- 3.Alcohol. https://www.who.int/news-room/fact-sheets/detail/alcohol
- 4.Voskoboinik A., Kalman J.M., Silva A. De, et al. Alcohol abstinence in drinkers with atrial fibrillation. N Engl J Med. 2020;382:20–28. doi: 10.1056/NEJMoa1817591. [DOI] [PubMed] [Google Scholar]
- 5.American College of Cardiology Alcohol May Have Immediate Effect on Atrial Fibrillation Risk, Events. https://www.acc.org/about-acc/press-releases/2021/05/17/04/43/alcohol-may-have-immediate-effect-on-atrial-fibrillation-risk
- 6.Jones C.M., Paulozzi L.J., Mack K.A. Alcohol involvement in opioid pain reliever and benzodiazepine drug abuse–related emergency department visits and drug-related deaths — United States, 2010. MMWR Morb Mortal Wkly Rep. 2014;63:881. [PMC free article] [PubMed] [Google Scholar]
- 7.Makdissi R., Stewart S.H. Care for hospitalized patients with unhealthy alcohol use: a narrative review. Addict Sci Clin Pract. 2013;8:1–10. doi: 10.1186/1940-0640-8-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thakkar S., Patel H.P., Chowdhury M., et al. Impact of arrhythmias on hospitalizations in patients with cardiac amyloidosis. Am J Cardiol. 2021;143:125–130. doi: 10.1016/j.amjcard.2020.12.024. [DOI] [PubMed] [Google Scholar]
- 9.CPI Inflation Calculator. https://www.bls.gov/data/inflation_calculator.htm
- 10.George A., Figueredo V.M. Alcohol and arrhythmias: a comprehensive review. J Cardiovasc Med (Hagerstown) 2010;11:221–228. doi: 10.2459/JCM.0b013e328334b42d. [DOI] [PubMed] [Google Scholar]
- 11.Samokhvalov A.V., Irving H.M., Rehm J. Alcohol consumption as a risk factor for atrial fibrillation: a systematic review and meta-analysis. Eur J Cardiovasc Prev Rehabil. 2010;17:706–712. doi: 10.1097/HJR.0b013e32833a1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bär K.J., Boettger M.K., Neubauer R., et al. Heart rate variability and sympathetic skin response in male patients suffering from acute alcohol withdrawal syndrome. Alcohol Clin Exp Res. 2006;30:1592–1598. doi: 10.1111/j.1530-0277.2006.00191.x. [DOI] [PubMed] [Google Scholar]
- 13.Cuculi F., Kobza R., Ehmann T., Erne P. ECG changes amongst patients with alcohol withdrawal seizures and delirium tremens. Swiss Medical Weekly. https://smw.ch/ [DOI] [PubMed]
- 14.Barnett A.G., Dobson A.J. Excess in cardiovascular events on Mondays: a meta-analysis and prospective study. J Epidemiol Community Health. 2005;59:109–114. doi: 10.1136/jech.2003.019489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Balbão C.E.B., de Paola A.A.V., Fenelon G. Effects of alcohol on atrial fibrillation: myths and truths. Ther Adv Cardiovasc Dis. 2009;3:53–63. doi: 10.1177/1753944708096380. [DOI] [PubMed] [Google Scholar]
- 16.Voskoboinik A., Prabhu S., Ling L.H., Kalman J.M., Kistler P.M. Alcohol and atrial fibrillation: a sobering review. J Am Coll Cardiol. 2016;68:2567–2576. doi: 10.1016/j.jacc.2016.08.074. [DOI] [PubMed] [Google Scholar]
- 17.Rich E.C. Alcohol-related acute atrial fibrillation. A case-control study and review of 40 patients. Arch Intern Med. 1985;145:830–833. doi: 10.1001/archinte.145.5.830. [DOI] [PubMed] [Google Scholar]
- 18.Li Z., Guo X., Liu Y., et al. Relation of heavy alcohol consumption to QTc interval prolongation. Am J Cardiol. 2016;118:1201–1206. doi: 10.1016/j.amjcard.2016.07.033. [DOI] [PubMed] [Google Scholar]
- 19.Mamas M.A., Caldwell J.C., Chacko S., Garratt C.J., Fath-Ordoubadi F., Neyses L. A meta-analysis of the prognostic significance of atrial fibrillation in chronic heart failure. Eur J Heart Fail. 2009;11:676–683. doi: 10.1093/eurjhf/hfp085. [DOI] [PubMed] [Google Scholar]
- 20.Campbell R.W.F., Day C.P., James O.F.W., Butler T.J. QT prolongation and sudden cardiac death in patients with alcoholic liver disease. Lancet. 1993;341:1423–1428. doi: 10.1016/0140-6736(93)90879-l. [DOI] [PubMed] [Google Scholar]
- 21.Lazarević A.M., Nakatani S., Nešković A.N., et al. Early changes in left ventricular function in chronic asymptomatic alcoholics: relation to the duration of heavy drinking. J Am Coll Cardiol. 2000;35:1599–1606. doi: 10.1016/s0735-1097(00)00565-9. [DOI] [PubMed] [Google Scholar]
- 22.Mirijello A., Tarli C., Vassallo G.A., et al. Alcoholic cardiomyopathy: what is known and what is not known. Eur J Intern Med. 2017;43:1–5. doi: 10.1016/j.ejim.2017.06.014. [DOI] [PubMed] [Google Scholar]
- 23.Shaaban A., Gangwani M.K., Pendela V.S., Vindhyal M.R. Alcoholic cardiomyopathy. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK513322/ [PubMed]
- 24.Gorenek B., Halvorsen S., Kudaiberdieva G., et al. Atrial fibrillation in acute heart failure: a position statement from the Acute Cardiovascular Care Association and European Heart Rhythm Association of the European Society of Cardiology. Eur Hear J Acute Cardiovasc Care. 2020;9:348–357. doi: 10.1177/2048872619894255. [DOI] [PubMed] [Google Scholar]
- 25.Susantitaphong P., Cruz D.N., Cerda J., et al. World incidence of AKI: a meta-analysis. Clin J Am Soc Nephrol. 2013;8:1482–1493. doi: 10.2215/CJN.00710113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Holgado J.L., Lopez C., Fernandez A., et al. Acute kidney injury in heart failure: a population study. ESC Heart Fail. 2020;7:415–422. doi: 10.1002/ehf2.12595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Long D., Long B., Koyfman A. The emergency medicine management of severe alcohol withdrawal. Am J Emerg Med. 2017;35:1005–1011. doi: 10.1016/j.ajem.2017.02.002. [DOI] [PubMed] [Google Scholar]
- 28.Cushman P. Delirium tremens. Update on an old disorder. Postgrad Med. 1987;82:117–122. doi: 10.1080/00325481.1987.11699999. [DOI] [PubMed] [Google Scholar]
- 29.Foy A., Kay J., Taylor A. The course of alcohol withdrawal in a general hospital. QJM. 1997;90:253–261. doi: 10.1093/qjmed/90.4.253. [DOI] [PubMed] [Google Scholar]
- 30.Horstmann E., Conrad E., Daweke H. [Severe course of delirium tremens. Results of treatment and late prognosis]. Medizinische Klinik. https://pubmed.ncbi.nlm.nih.gov/2622419/ [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.