Summary
Background
There is minimal experience in continuous glucose monitoring (CGM) among underserved racial/ethnic minority populations with or at risk of type 2 diabetes (T2D), and therefore a lack of CGM-driven insight for these individuals. We analyzed breakfast-related CGM profiles of free-living, predominantly Hispanic/Latino individuals at-risk of T2D, with pre-T2D, or with non-insulin treated T2D.
Methods
Starting February 2019, 119 participants in Santa Barbara, CA, USA, (93 female, 87% Hispanic/Latino [predominantly Mexican-American], age 54·4 [±12·1] years), stratified by HbA1c levels into (i) at-risk of T2D, (ii) with pre-T2D, and (iii) with non-insulin treated T2D, wore blinded CGMs for two weeks. We compared valid CGM profiles from 106 of these participants representing glucose response to breakfast using four parameters.
Findings
A “northeast drift” was observed in breakfast glucose responses comparing at-risk to pre-T2D to T2D participants. T2D participants had a significantly higher pre-breakfast glucose level, glucose rise, glucose incremental area under the curve (all p < 0·0001), and time to glucose peak (p < 0·05) compared to pre-T2D and at-risk participants. After adjusting for demographic and clinical covariates, pre-breakfast glucose and time to peak (p < 0·0001) were significantly associated with HbA1c. The model predicted HbA1c within (0·550·67)% of true laboratory HbA1c values.
Interpretation
For predominantly Hispanic/Latino adults, the average two-week breakfast glucose response shows a progression of dysglycemia from at-risk of T2D to pre-T2D to T2D. CGM-based breakfast metrics have the potential to predict HbA1c levels and monitor diabetes progression.
Funding
US Department of Agriculture (Grant #2018–33800–28404), a seed grant from the industry board fees of the NSF Engineering Research Center for Precise Advanced Technologies and Health Systems for Underserved Populations (PATHS-UP) (Award #1648451), and the Elsevier foundation.
Keywords: Continuous glucose monitoring, Dysglycemia, Breakfast glucose response, Hispanic/Latino adults, Non-insulin treated T2D, Multiple regression
Research in context.
Evidence before this study
There is very limited experience in continuous glucose monitoring (CGM) among underserved racial/ethnic minority populations with or at risk of type 2 diabetes (T2D). However, previous research has suggested that glycemic responses related to breakfast can influence subsequent glycemia.
Added value of this study
This study analyzed CGM profiles in predominantly Hispanic/Latino adults living with or at risk of developing non-insulin treated T2D. Participants were stratified by HbA1c levels. We observed that the peaks of the breakfast glucose response shifted in a northeast direction, comparing participants who were at-risk of T2D, with pre-T2D, or with T2D, indicating a progression in dysglycemia. Participants with T2D had significantly higher starting glucose, glucose rise, time to glucose peak, and overall glucose response than at-risk and pre-T2D participants.
Implications of all the available evidence
These findings may offer new opportunities for non-pharmacologic and pharmacologic interventions for underserved communities facing a disproportionate burden of diabetes.
Alt-text: Unlabelled box
Introduction
One main advantage of continuous glucose monitoring (CGM) is the ability to observe glycemic excursions that cannot be captured using HbA1c levels alone. Data obtained from CGM profiles can be used to set glycemic targets and guide therapeutic decision-making for people with established diabetes.1 For adults developing type 2 diabetes (T2D), there appears to be a progression from normal glucose tolerance to T2D due to progressive loss of adequate β-cell insulin secretion in the setting of insulin resistance.2 However, the natural history of progression from normal glucose tolerance to T2D has not been well defined using CGM. There are also no national or international guidelines that include CGM-derived data from racial and/or ethnic minority groups, which in the United States (U.S.) are populations disproportionately impacted by T2D.3 Further, access to diabetes technology in the U.S. is also influenced significantly by race and ethnicity as well as social deprivation status.4
To understand data derived from CGM profiles, a variety of metrics have been suggested. Average glucose and glucose variability measured over two weeks of CGM use provide an overall picture of glycemia in individuals.1 These metrics also include the time in range, which correlates with both HbA1c levels and risk of complications. Additional recommended metrics include time below (<70 and <54 mg/dL) and time above (>180 mg/dL) target ranges as useful parameters for re-evaluation of a treatment regimen.5 A recent study showed that the standard metrics differ comparing overnight and daytime CGM data in adults at risk of as well as with non-insulin treated T2D.6 Furthermore, in that study, the time spent in the 70–140 mg/dL range during the day but not overnight was closely associated with HbA1c.
Current CGM-based metrics provide a clinically meaningful macroscopic perspective on an individual's glycemia. However, these metrics average out the effect of distinct and potentially prognostic glycemic patterns occurring at different times of the day, e.g., due to meals. This study aimed to gain data-driven insights from the postprandial glucose response to breakfast in a cohort of participants at risk of or with established T2D, most of whom were underserved Hispanic/Latino adults. We chose to analyze post-breakfast glycemia as the start of breakfast is relatively easier to detect compared to meals later in the day since it is the first major meal after several hours of sleep. Breakfast-related glycemia has also been the target of several diet-focused interventions for diabetes and obesity.7, 8, 9, 10 We observed that the breakfast glucose response shows a distinct progression of dysglycemia from individuals at-risk of T2D, to pre-T2D, to those with T2D. We quantified the breakfast response using four parameters that were found to be significantly associated with the HbA1c levels of the participants independently of known clinical and demographic covariates. These CGM-based breakfast metrics therefore have the potential to enable novel monitoring and therapeutic approaches in underserved populations facing a disproportionate burden of T2D.
Methods
Participant cohort
This study was approved by an Independent Review Board (Advarra IRB Study 2018–01793, Protocol 00036476). Following IRB approval, and prior to participation in any activities, participants provided written informed consent to be enrolled in an observational cohort study called Farming for Life (ClinicalTrials.gov number: NCT 03940300).11 Farming for Life began in February 2019 with participants recruited via bilingual (Spanish and English) outreach materials and with help from bilingual community health workers through community outreach, from existing programs, Hispanic/Latino-focused community organizations, and local health and social services. Eligible and consented participants provided baseline demographic and clinical information on age, gender, self-reported race and ethnicity, health insurance status, and whether participants had been informed of a diagnosis of T2D by a qualified medical provider. The following inclusion criteria were used: adults ≥ 18 years of age, with T2D for at least 6 months, or self-reported as at risk for developing T2D using the American Diabetes Association diabetes risk assessment tool.12 Exclusion criteria included current or previous use of insulin, pregnancy, or any active clinically significant disease or disorder which in the investigator's opinion could interfere with participation in the study. Height, weight, and waist circumference were measured following the National Health and Nutrition Examination Survey Anthropometry Procedure Manual, January 2016.13 Body mass index (BMI) was then calculated using the Quetelet Index (body weight (kilograms) divided by height squared (meters).14 Baseline measurements were also taken of fingerstick HbA1c (Siemens DCA Vantage, Siemens Healthcare, Norwood, Massachusetts, USA). Participants were stratified using HbA1c into at-risk (HbA1c < 5·7%), pre-T2D (5·7% ≤ HbA1c ≤ 6·4%), and T2D (HbA1c> 6·4%). The complete protocol details have been published previously.6,11
Continuous glucose monitoring
Participants were trained to wear a blinded CGM (Abbott Freestyle Libre Pro) sensors using manufacturer educational materials under the supervision of research staff. Participants were asked to wear the CGM for 14 days after enrollment. Normal activities continued during this time and the participants returned to the research site for sensor removal at 2 weeks. On return, the CGM reader was connected to https://www.libreview.com/ to create an individual participant report.
Quantifying breakfast CGM response
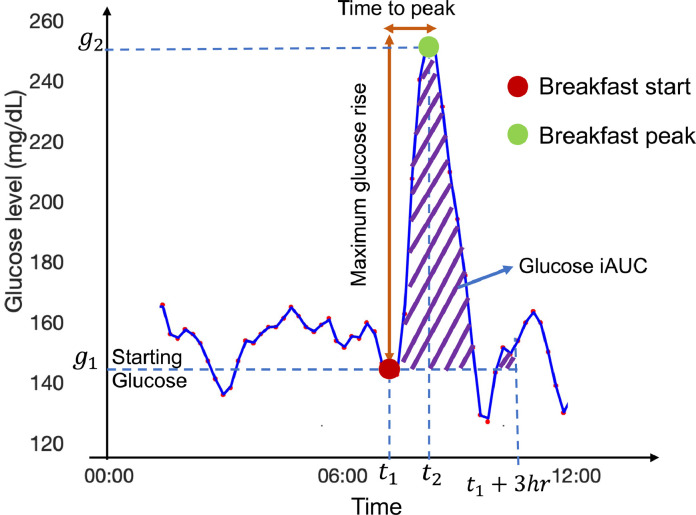
For each day of CGM, we manually annotated the start of breakfast response and the peak of the breakfast response based on visual inspection as shown by the two large dots (red for start and green for peak) in Fig. 1. The following rules were followed to annotate breakfast: (i) the start time of breakfast should lie between 5 and 11am, (ii) the rise in glucose from start to peak should be more than a pre-defined threshold of + 40 mg/dl, and (iii) if multiple segments of the glucose curve satisfied (i) and (ii), we chose the earlier segment to be the breakfast. The glucose rise threshold of 40 mg/dL was chosen based on previous post-breakfast glucose response studies in healthy, pre-T2D, and T2D participants.15, 16, 17 Four parameters were then computed for each breakfast segment:
-
•
Starting glucose (SG): The glucose value at the start of the breakfast.
-
•
Time to peak (TTP): The time difference between the start of breakfast response and the breakfast response peak in minutes.
-
•
Maximum glucose rise (Max GR): The difference between the glucose levels at the start of breakfast and post-breakfast peak in mg/dL.
-
•
Glucose incremental area under curve (Glucose iAUC): The positive area under the post-breakfast glucose curve after subtracting the glucose value at the start.
Fig. 1.
Proposed breakfast CGM measures. Annotated breakfast start and peak shown with a red and green circle respectively in a participant with T2D. g1: starting glucose (SG) value, t1: start time of breakfast response, g2: glucose value at breakfast response peak, t2: time at breakfast response peak. (g2- g1) represents the maximum glucose rise (Max GR) and (t2- t1) represents the time to glucose peak (TTP). The purple hatched region represents the incremental area under the glucose curve (Glucose iAUC).
We subsequently used these parameters to compare post-breakfast glycemia across diabetes subgroups stratified by HbA1c levels (at-risk, pre-T2D, and T2D). We also computed median values for the parameters over two weeks of breakfasts for each participant to represent their overall breakfast glucose response.
Statistical analysis
Since this analysis is part of a larger study, no a priori sample size calculation was performed specifically for the CGM-based T2D risk stratification task. Statistical analyses were performed using MATLAB software (https://www.mathworks.com/, V.R2019b). Between-group comparisons were made using a Kruskal-Wallis test, followed by multiple comparison testing using the Tukey's honest significance difference criterion. Correlation values were computed via the Spearman rank correlation method. Multiple linear regression analyses were performed using the ‘fitlm’ function in MATLAB. The regression models adjusted for potential confounders such as participant's age, self-reported gender, waist circumference, whether they were of Hispanic/Latino ethnicity, and whether they were born in Mexico or not. Statistical significance was expressed at the 5% level.
Role of the funding souce
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript. The corresponding author (DK) had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Participant cohort
From the start of February 2019 until June 2021, 221 participants have been enrolled in Farming for Life. Overall, 119 predominantly Hispanic/Latino participants wore a blinded CGM for up to two weeks upon enrollment and before any study-related intervention. Demographic and clinical details of the cohort are presented in Table 1. Participants were stratified by baseline HbA1c levels into at-risk (HbA1c < 5·7%, n = 35), pre-T2D (5·7% ≤ HbA1c ≤ 6·4%, n = 49), and T2D (HbA1c> 6·4%, n = 35) as per the American Diabetes Association guidelines.2
Table 1.
Demographic and clinical measurements for the participant cohort.
| Variable | All | By baseline HbA1c |
||
|---|---|---|---|---|
| HbA1c < 5·7% | 5·7% ≤ HbA1c ≤ 6·4% | HbA1c > 6·4% | ||
| Number of participants | 119 | 35 | 49 | 35 |
| Age | 54·4 ± 12·1 | 49.7 ± 12.9 | 55.9 ± 9.8 | 57.1 ± 13.1 |
| Gender | 93 Female 26 Male |
25 Female 10 Male |
44 Female 5 Male |
24 Female 11 Male |
| BMI (kg/m2) | 31·2 ± 5·5 | 30.6 ± 5·0 | 30.2 ± 5·4 | 33.1 ± 5·9 |
| Waist circumference (cm) | 100·4 ± 12·5 | 99.7 ± 11.1 | 97.8 ± 13.2 | 104.8 ± 11.8 |
| Hispanic/Latino ethnicity |
104 (87.4%) | 33 (94.3%) | 43 (87.8%) | 28 (80%) |
| Born in Mexico | 99 (83.2%) | 32 (91.4%) | 41 (83.7%) | 26 (74.3%) |
| HbA1c (%) | 6.3 ± 1.1 | 5·4 ± 0.2 | 6.0 ± 0.2 | 7.6 ± 1.3 |
| On medication* | 29 | 2 - 2 Metformin |
4 - 4 Metformin - 1 DPP-4 |
23 - 19 Metformin - 5 Sulphonylurea - 4 SGLT2 - 1 DPP-4 - 1 GLP1-RA |
Values for age, BMI, waist circumference, and HbA1c reported as mean ± SD.
T2D: Type 2 diabetes, BMI: Body mass index, SGLT2: Sodium-glucose co-transporter-2, DPP-4: Dipeptidyl peptidase 4, GLP1-RA: Glucagon-like peptide-1 receptor agonists.
*Some participants are on only one type of medication while others are on multiple types of medication.
Breakfast analysis
We manually annotated a dataset comprised of a total of 1666 days of CGM data, with an average of 14·0 [±3·3] days of data per participant. We extracted 786 valid breakfast response CGM profiles for the two-week period before the study intervention started based on the three criteria outlined above. The breakfast CGM segments consisted of glucose values from the start time of breakfast for the next 3 h. Since the CGM records glucose every 15 min, this provides 13 CGM readings for each breakfast response profile. 164 of the breakfast profiles were generated from the at-risk participants, 300 from the pre-T2D participants, and 322 from the T2D participants. The at-risk participants typically had fewer annotated breakfasts compared to their pre-T2D and T2D counterparts, due to fewer glucose peaks within 5–11am that passed the 40 mg/dL height threshold. In all, 106 of the 119 participants had at least one breakfast profile that passed our listed criteria. The details of the annotated breakfast dataset are presented in Supplementary Table 1.
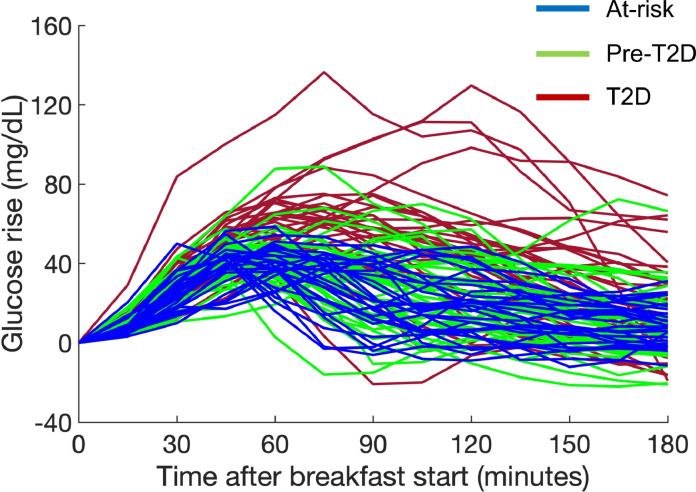
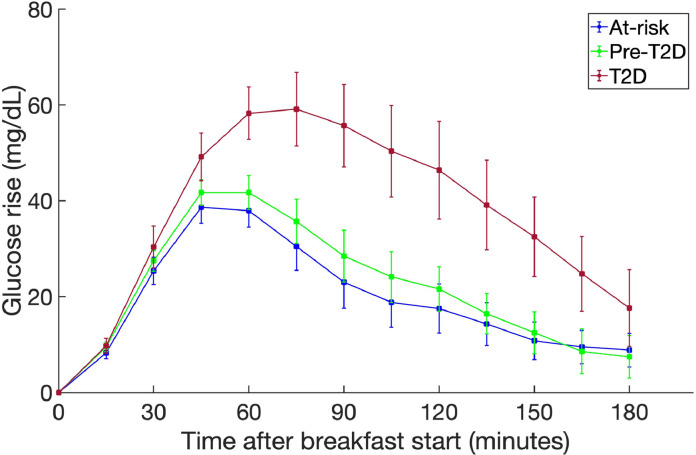
The northeast drift
To investigate if the breakfast glucose response has distinct signatures across different categories of T2D progression, we calculated a timepoint-wise median of the CGM breakfast profiles to create a median breakfast response for each participant (Fig. 2). Subsequently, we averaged the breakfast responses across participants in each of the three HbA1c stratified categories. There was a shift in breakfast peaks in a northeast direction comparing the sub-groups, indicating a progression in dysglycemia (Fig. 3). We also examined if this phenomenon is sensitive to the glucose rise threshold of 40 mg/dL that we use as a criterion to annotate breakfast segments. For this, we first generated valid breakfast profiles over glucose thresholds 20, 30, and 50 mg/dL. As expected, we extracted more valid breakfast profiles when the threshold was more relaxed (<40 mg/dL) and fewer profiles when the threshold was more stringent (>40 mg/dL). (Supplementary Table 2) Then, we recomputed the average breakfast CGM responses for the three sub-groups for each choice of the threshold. We observed the northeast drift to be a stable phenomenon over a wide range of glucose thresholds ranging from 20 mg/dL to 50 mg/dL (Supplementary Fig. 1). Notably, while the glucose peak increases in height with the threshold value, the relative dysglycemia between diabetes sub-groups remains consistent.
Fig. 2.
Median breakfast response for each participant (n = 106). Participants at-risk of T2D in blue, those with pre-T2D in green, and those with T2D in red.
Fig. 3.
The northeast drift phenomenon in breakfast glucose responses, showing the timepoint-wise average breakfast profile over all participants in each group; at-risk of T2D in blue (n = 28), with pre-T2D in green (n = 45), and with T2D in red (n = 33). Error bars represent the standard error around the mean value.
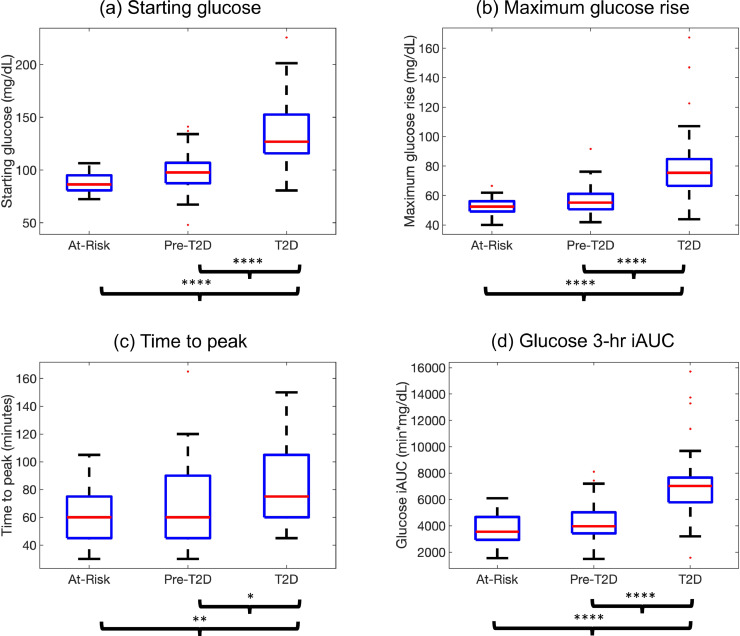
Analysis of breakfast response CGM measures
We also compared the different breakfast response CGM measures across the groups (Fig. 4). The T2D participants had significantly higher starting glucose, maximum glucose rise, and glucose iAUC than the at-risk and pre-T2D participants (all p < 0·0001). The T2D group also had higher time to peak values than the at-risk group (p < 0·01) and the pre-T2D group (p < 0·05). The detailed statistical analysis is reported in Supplementary Table 3.
Fig. 4.
Statistical comparison of various CGM measures across at-risk, pre-T2D, and T2D groups, (a) starting glucose, (b) maximum glucose rise, (c) time to peak, and (d) glucose 3-hr iAUC. Boxplots shown as median (red), interquartile range (blue edges) and total range (black tails). Outliers shown as red dots. *p < 0·05, **p < 0·01, ***p < 0·001, ****p < 0·0001.
Association of breakfast response CGM measures with HBA1c
Subsequently, we used multiple linear regression to examine the association between breakfast response CGM metrics and HbA1c, after adjusting for demographic and clinical covariates (Table 2). The covariates were age, gender, waist circumference, whether Hispanic/Latino or not, and whether born in Mexico or not. The BMI was highly correlated with waist circumference (rho = 0.83, p < 0.0001) and therefore only the latter was included to avoid multicollinearity issues. None of the 106 participants with at least one breakfast profile had any missing information for any of the CGM-based, demographic, or clinical predictors. The glucose iAUC had a high correlation with both the time to peak (rho = 0·65, p < 0·0001) and the maximum glucose rise (rho = 0·75, p < 0·0001), so we exclude the glucose iAUC to minimize multicollinearity in the model. The other CGM measures had a correlation of lower than 0·5 with each other (Supplementary Fig. 2). The linear regression analysis showed that starting glucose and time to the post-breakfast peak were significantly associated with HbA1c (p < 0·0001). None of the other covariates showed any association with the HbA1c.
Table 2.
Multiple linear regression using CGM-based breakfast measures with clinical and demographic variables to predict HbA1c.
| Predictor | Regression coefficient | Standard error | T-statistic | p-value |
|---|---|---|---|---|
| (Intercept) | 1·598 | 0·738 | 2·165 | 0·03 |
| Starting glucose | 0·035 | 0·002 | 14·679 | <0·0001⁎⁎⁎⁎ |
| Time to glucose peak | 0·012 | 0·002 | 4·721 | <0·0001⁎⁎⁎⁎ |
| Maximum glucose rise | 0·002 | 0·004 | 0·412 | 0·68 |
| Age | −0·006 | 0·006 | −1·122 | 0·26 |
| Gender (male) | 0·178 | 0·144 | 1·227 | 0·22 |
| Waist circumference | 0·004 | 0·005 | 0·796 | 0·43 |
| Hispanic/Latino (HL) | −0·100 | 0·295 | −0·339 | 0·74 |
| Mexican-born (MEX) | 0·164 | 0·256 | 0·642 | 0·52 |
****p < 0·0001, ***p < 0·001, **p < 0·01, *p < 0·05.
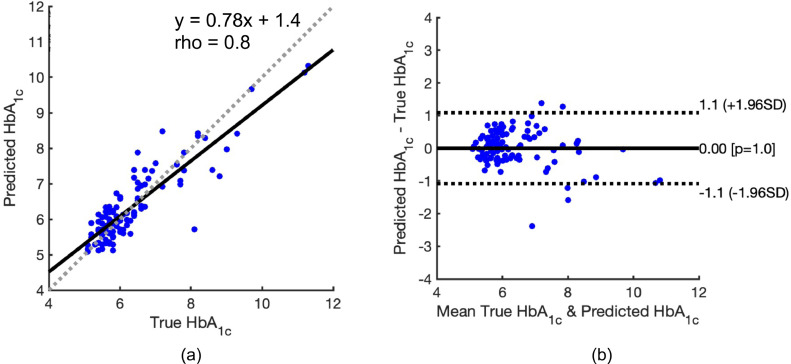
We also calculated the accuracy of the model in predicting HbA1c via a Bland-Altman analysis18 (Fig. 5). The model was found to predict HbA1c within (0·550·67)% (meanSD) of the true HbA1c value. In addition, there was a significant correlation between the true and predicted HbA1c (rho = 0·80, p < 0·0001) (Fig. 5(a)). Bland-Altman analysis shows that there was no overall systematic bias in the predicted HbA1c, with the mean difference between true and predicted values being 0·0 (95% CI [−1·1,1·1]; p = 1·0) (Fig. 5(b)).
Fig. 5.
Bland-Altman analysis comparing the true HbA1c measured in the laboratory and the HbA1c predicted by a multiple linear regression model built on our breakfast CGM measures and demographic/clinical covariates. (a) Scatterplot of the true and predicted HbA1c values. The equation representing the best-fit line (solid black line) and the correlation value rho are reported. The dotted line is a 45-degree diagonal line representing equal values for the true and predicted HbA1c values. (b) Plot of the mean of the true and predicted HbA1c values (x-axis) against their difference (y-axis). The horizontal bold line shows the mean difference of the true and predicted HbA1c and the p-value of the difference. The dotted lines represent the upper 95% and lower 95% confidence interval of the differences. Each dot in the plot represents a participant.
Diabetes risk stratification using breakfast CGM measures
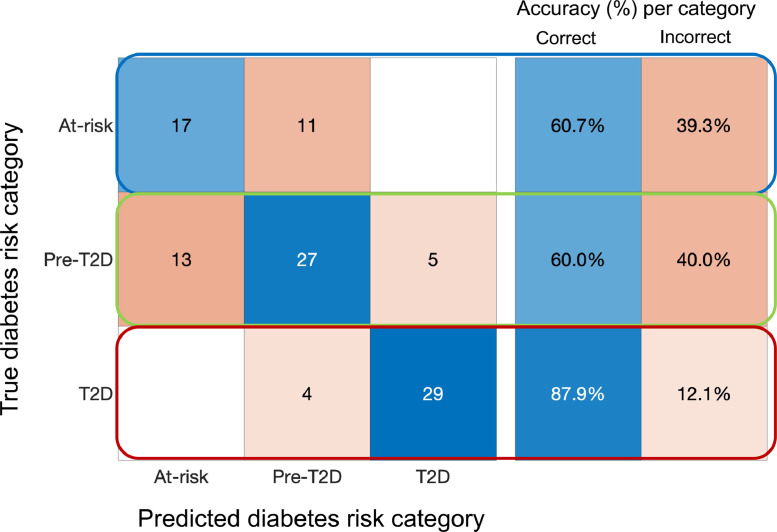
We further investigated how accurately the breakfast CGM measures predict the diabetes risk category (At-risk, pre-T2D, and T2D) using the above linear regression model.19 For this, we first converted the predicted HbA1c to the corresponding diabetes risk group using the HbA1c thresholds defined in the Methods section. Next, we computed a confusion matrix to examine the model's accuracy for each of the three groups. (Fig. 6) We observed that our model predicts T2D with a high accuracy of 87.9%. The model tends to confuse at-risk and pre-T2D participants (60.7% and 60.1% accuracy, respectively), which follows intuitively given the closeness of their breakfast profiles we observed in Figs. 2 and 3.
Fig. 6.
Confusion matrix depicting the accuracy of the linear regression model built using breakfast CGM measures in predicting the three diabetes risk categories: at-risk of T2D, pre-T2D, and T2D. Each row of the 3 × 3 matrix corresponds to the true category, with the entries adding up to the number of participants in each category. Each column represents which of the three categories the model predicted. The 3 × 2 matrix on the right reports the model's prediction accuracy for each of the three categories.
Association of breakfast response CGM measures with GMI
A CGM-based measure increasingly used by physicians in lieu of HbA1c is the Glucose Management Indicator (GMI).20,21 The GMI is defined mathematically as GMI (%) = 3.31 + 0.02392 [average CGM glucose in mg/dL], where the average glucose is calculated over the duration of CGM wear. We first examined the relationship between GMI and HbA1c for our participant cohort. We observed a correlation of 0.77 between GMI and HbA1c; however, we do note that the GMI underestimates the HbA1c at higher values (Supplementary Fig. 3(a)). We then computed a multiple linear regression with the same set of predictors as above to predict GMI instead of HbA1c. We again found that starting glucose (p < 0.0001) and time to glucose peak (p < 0.0001) are significantly associated with the GMI. (Supplementary Table 4). The maximum glucose rise was close to but did not achieve statistical significance (p = 0.06). The model predicted GMI to be within (0·190·07)% (meanSD) of the true GMI value. (Supplementary Fig. 3(b)) Bland-Altman analysis demonstrated no systematic bias in the GMI predictions with a mean difference between true and predicted values being 0.0 (95% CI [−0.38, 0.38]; p = 1.0). (Supplementary Fig. 3(c)).
Discussion
Based on evidence from clinical trials and real-world experiences, clinical guidelines have been established for using continuous glucose monitoring (CGM) data for people living with diabetes. CGM use is likely to expand given recent evidence that CGM-derived measures, such as time in range (TIR), correlate with long-term complications.22 However, very few studies have been published on CGM in people with non-insulin treated T2D, with pre-T2D, or from minority communities. Guidance from the American Diabetes Association suggests that CGM may be helpful for the 70% of adults with diabetes who are not treated with insulin.23,24
In this study involving predominantly Hispanic/Latino adults, we explored the potential of using the breakfast CGM response as an indicator of the progression of dysglycemia by comparing individuals at-risk for T2D, with those with pre-T2D, or T2D. Participants were stratified into these groups using HbA1c values. After a manual annotation of CGM-derived breakfast glucose responses, we computed pre-breakfast glucose levels, the rise in glucose after breakfast, time to the peak glucose level, and the incremental area under the glucose curve for 3 h (3 h glucose iAUC) after breakfast. Using this approach, we observed that the average breakfast glucose response over two weeks shows a distinct “northeast drift” comparing at-risk to pre-T2D to T2D individuals. The northeast drift refers to an increase in the maximum glucose rise and the time to the post-breakfast glucose peak with increasing disease severity. Notably, we consistently observed this phenomenon across several glucose threshold values used to determine breakfast peaks. It is also important to note that we observed the northeast drift in participants consuming free-choice meals that they would normally consume, as opposed to laboratory-prepared test meals. Thus, the robustness of the northeast drift makes it a potential candidate for monitoring diabetes progression using CGMs. For individuals with established T2D, there was a considerably higher starting glucose, maximum glucose rise, and 3-hr glucose iAUC versus at-risk and pre-T2D individuals. The T2D group also had a higher time to postprandial glucose peak than the at-risk and the pre-T2D groups.
These findings suggest that CGM-based breakfast-focused profiles may have value for underserved and other communities with or at risk of developing T2D by offering potential new targets for therapeutic intervention at an early stage of the disease. Our analysis was based on two weeks of CGM data, and participants were allowed free choice breakfasts prior to the intervention phase of the Farming for Life study. In this study, the focus was on changes in glycemia with breakfast. We chose this meal for two reasons. First, based on visual observation of CGM profiles, we found that breakfast was the meal that was the least challenging to identify. Second, previous research has suggested that glucose profiles associated with breakfast impact overall glycemia and may be amenable to nutrition-based therapeutic interventions. For example, nutritional interventions targeting breakfast using food low in carbohydrates have reported improved glycemic responses in individuals with T2D.10,16 The timing and macronutrient content of breakfast also appear to influence the risk of progression of T2D.25 Previous studies have suggested an association between consuming a regular breakfast with a decreased risk of T2D progression compared with breakfast skipping or infrequent breakfast consumption.26,27 The macronutrient content of breakfast can also influence subsequent glucose and insulin responses.28
A recent study reported progressively higher average glucose levels, more glycemic variability, and less time spent in the ranges between 70 and 140 and 70 and 180 mg/dL comparing individuals with established T2D with those at-risk or with pre-T2D.6 Taken together with findings here, the ability of CGM profiles to stratify individuals into sub-groups with differentiating glycemic profiles during the day, at night, and around breakfast potentially offers novel approaches for non-pharmacological and pharmacological interventions to attenuate the progression of T2D. This may have economic as well as health benefits for underserved populations experiencing a disproportionate burden of T2D.11
While the northeast shift was less marked comparing at-risk to pre-T2D participants, the effect was more profound comparing pre-T2D to T2D individuals. This may be a consequence of differences in insulin sensitivity between pre-T2D and T2D individuals or a failure of timely and appropriate insulin secretion in the latter group.29,30 We also found that, after adjusting for demographic and clinical covariates using a multiple linear regression model, the pre-breakfast glucose level and the time to peak were significantly associated with HbA1c values. Via a Bland-Altman analysis, we found that the HbA1c values predicted by the model were highly correlated with the true values (rho = 0·8, p < 0·0001), and furthermore there was no systematic bias in the predictions with a mean difference [95% CI] of 0·0 [−1·1,1·1] (p = 1·0). Although regular HbA1c testing is invariably recommended in authoritative guidelines, many studies have reported that undertesting is very common.31 In type 1 diabetes (T1D) and insulin treated T2D, CGM provides various glycemic metrics that can be used to set glycemic targets and guide therapeutic decision-making.1 We demonstrated that our breakfast CGM measures can also predict the CGM-based glucose management indicator (GMI) with a high accuracy, which can be of additional value in this cohort. Others have also shown that glycemic variability measured by CGM is present to an increasing degree comparing adults with normal glucose tolerance and impaired fasting glucose or impaired glucose tolerance with newly diagnosed T2D.32 Notably, data from the National Health and Nutrition Examination Survey (NHANES) showed that HbA1c detected only 30% of undiagnosed diabetes in a sample cohort, while 2-h plasma glucose after an oral glucose tolerance test detected 90% of undiagnosed diabetes.33 In this study, participants were not provided with real-time CGM profiles. Evidence shows that having access to real-time profiles is associated with improved glycemic control for adults with pre-T2D and T2D.34 In the U.S. and elsewhere, the use of CGM has been recently included in guidance for selected patients with T2D, including those not on insulin.35 These findings, supported by our observations in this study, suggest the potential of monitoring breakfast glucose response for early detection of T2D.
Several limitations need to be addressed in subsequent studies. A major limitation of the study is the cross-sectional design of participants, and therefore determining the value of CGM in predicting the risk of progression from at-risk to T2D will require longitudinal analyses. The computed measures need to be validated on a larger cohort of participants and potentially across multiple CGM periods. We recognize that dietary choices can differ across populations due to cultural factors.36, 37, 38 Therefore, our breakfast response metrics likely will need to be recomputed in CGM data from other underserved minority communities before use.39 We had a broad spectrum of ages in our participant cohort, which aligns with data showing that Hispanic/Latino (and specifically Mexican-American) adults develop T2D across the age spectrum, including younger ages.40,41 This suggests that with a larger cohort additional analyses stratified by age may provide other insights related to age. We chose a fixed threshold of 40 mg/dL post-breakfast glucose rise to select valid breakfast responses; however, a separate threshold for each sub-group may help select breakfast more accurately. As an example, seven of the 35 at-risk participants did not contribute a single breakfast profile for the threshold of 40 mg/dL glucose rise, which may mean that the breakfast threshold was too high for a portion of the at-risk sub-group. A future study quantifying the glucose response to known meals in this population may yield more optimal threshold criteria for each sub-group. An ongoing study (ClinicalTrials.gov number: NCT 03940300) using CGM, activity monitors, and self-recorded food diaries in the same population is underway. Further, this study did not account for the breakfast macronutrient content and other lifestyle factors. Knowing the specific associations between nutrient content, lifestyle factors, etc., and CGM profiles may help design more personalized interventions. Previous studies have demonstrated links between the timing of food intake with insulin sensitivity.42 Timing, duration, and intensity of physical activity can also influence postprandial glucose levels up to 24 h after the activity.43 In this study, we focused on the rise in glucose after breakfast and the time to post-breakfast peak. These parameters do not capture any information about the fall in the glucose curves after the peak, which can impact appetite and subsequent energy intake.44 We aggregated per-day breakfast CGM measures over the duration (∼14 days) of CGM wear by a median computation. Aggregation has the advantage in that it smooths out inter-day variations caused by difference in food choices (type of food, quantity, etc.) and therefore captures the underlying physiology better. Potentially beneficial information such as the shapes of the curves and inter-day variations is, however, lost in aggregation. This limitation can be addressed in future studies through algorithms such as multivariate functional principal component analysis (MFPCA).45,46 MFPCA preserves shape properties while accounting for inter-day variability, and has previously been used to model multi-day time series data similar to ours for applications such as remote sensing,47 stock market forecasting,48 and cancer risk prediction.49,50 We also did not examine the same parameters related to other meals. While the breakfast peak is typically easier to identify, the accuracy of the annotated start point of breakfast may be affected by the dawn phenomenon.51,52 An appropriate correction strategy for the dawn phenomenon can increase the accuracy of the proposed breakfast metrics.53 For real-world deployment, an important next step would be to reduce the possibility of human error in manual annotation by instead using an accurate automated annotation software. Several automated meal detection algorithms have been proposed in the literature primarily in the T1D and artificial pancreas setting,54, 55, 56 which need to be adjusted for meal detection in populations at-risk for or with T2D. Thus, a complete T2D detection solution would involve three components: a CGM recording glucose continuously, a breakfast response detection software, and a diabetes risk scoring tool based on our breakfast metrics.
In conclusion, in a predominantly Hispanic/Latino cohort at-risk for or with non-insulin treated T2D, CGM-derived profiles associated with breakfast showed a distinct northeast drift with increasing diabetes progression. In addition, new CGM-based metrics based on these profiles related to breakfast glucose increments also appear to have a significant relationship with HbA1c. These findings may offer new opportunities for non-pharmacologic and pharmacologic interventions in underserved communities facing a disproportionate burden of diabetes.
Contributors
SB conceptualized the novel breakfast-based CGM measures, wrote software for computing the measures, performed statistical analyses, created visualizations, and led the writing of the manuscript. AS conceptualized the analysis framework, supervised SB in design of the analysis pipeline, and contributed to review and editing of the manuscript. NG was involved in development and execution of the protocol design and IRB approval, data collection and analyses, manuscript generation and editing. CC, WB and AL were involved in execution of the study protocol including participant recruitment and retention, data capture and analyses and manuscript editing. DK came up with the original idea for Farming for Life and developed the protocol with NG. DK also contributed to data analyses, drafting, and editing the manuscript and is guarantor of the study. All authors contributed to writing of the manuscript. SB, AS, and DK have verified the underlying data.
Data sharing statement
Data are available upon reasonable request. The investigators agree to share de-identified individual participant data that underlie the results reported in this article, the computational and statistical analysis tools, and the study protocol with academic researchers beginning three months after publication and ending five years following article publication. Proposals should be directed to dkerr@sansum.org. To gain access, data requestors will need to sign a data access agreement.
Funding
Funding for the study was provided by the U.S. Department of Agriculture (Grant No: 2018–33800–28404), a seed grant from the industry board fees of the NSF Engineering Research Center for Precise Advanced Technologies and Health Systems for Underserved Populations (PATHS-UP) (#1648451), and the Elsevier Foundation.
Declaration of Competing Interest
DK reports non-financial support from Abbott Diabetes Care, during the conduct of the study; grants from Lilly, personal fees from Sanofi, personal fees from NovoNordisk, personal fees from Glooko, outside the submitted work. NG, CC, AL, and WB report non-financial support from Abbott Diabetes Care, grants from US Dept of Agriculture, during the conduct of the study; grants from Lilly, outside the submitted work. SB and AS declare no competing interest(s).
Acknowledgements
The authors thank Abbott Diabetes Care for supplying the Freestyle Libre sensors and readers that provided continuous glucose monitoring for this study.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2021.101241.
Appendix. Supplementary materials
References
- 1.Battelino T., Danne T., Bergenstal R.M., et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019;42:1593–1603. doi: 10.2337/dci19-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Association AD. 2 Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care. 2021;44:S15–S33. doi: 10.2337/dc21-S002. [DOI] [PubMed] [Google Scholar]
- 3.Cheng Y.J., Kanaya A.M., Araneta M.R.G., et al. Prevalence of diabetes by race and ethnicity in the United States, 2011–2016. JAMA. 2019;322:2389–2398. doi: 10.1001/jama.2019.19365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kerr D., Warshaw H. Clouds and silver linings: COVID-19 pandemic is an opportune moment to democratize diabetes care through telehealth. J Diabetes Sci Technol. 2020;14:1107–1110. doi: 10.1177/1932296820963630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Association ADs 6. Glycemic targets: standards of medical care in diabetes-2021. Diabetes Care. 2021;44:S73–S84. doi: 10.2337/dc21-S006. [DOI] [PubMed] [Google Scholar]
- 6.Barua S., Sabharwal A., Glantz N., et al. Dysglycemia in adults at risk for or living with non-insulin treated type 2 diabetes: insights from continuous glucose monitoring. EClinicalMedicine. 2021;35 doi: 10.1016/j.eclinm.2021.100853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jakubowicz D., Wainstein J., Landau Z., et al. High-energy breakfast based on whey protein reduces body weight, postprandial glycemia and HbA1C in type 2 diabetes. J Nutr Biochem. 2017;49:1–7. doi: 10.1016/j.jnutbio.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 8.King D.G., Walker M., Campbell M.D., Breen L., Stevenson E.J., West D.J. A small dose of whey protein co-ingested with mixed-macronutrient breakfast and lunch meals improves postprandial glycemia and suppresses appetite in men with type 2 diabetes: a randomized controlled trial. Am J Clin Nutr. 2018;107:550–557. doi: 10.1093/ajcn/nqy019. [DOI] [PubMed] [Google Scholar]
- 9.Jakubowicz D., Barnea M., Wainstein J., Froy O. High caloric intake at breakfast vs. dinner differentially influences weight loss of overweight and obese women. Obesity. 2013;21:2504–2512. doi: 10.1002/oby.20460. Silver Spring. [DOI] [PubMed] [Google Scholar]
- 10.Chang C.R., Francois M.E., Little J.P. Restricting carbohydrates at breakfast is sufficient to reduce 24h exposure to postprandial hyperglycemia and improve glycemic variability. Am J Clin Nutr. 2019;109:1302–1309. doi: 10.1093/ajcn/nqy261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kerr D., Barua S., Glantz N., et al. Farming for life: impact of medical prescriptions for fresh vegetables on cardiometabolic health for adults with or at risk of type 2 diabetes in a predominantly Mexican-American population. BMJ Nutr Prev Health. 2020;3:239–246. doi: 10.1136/bmjnph-2020-000133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bang H., Edwards A.M., Bomback A.S., et al. Development and validation of a patient self-assessment score for diabetes risk. Ann Intern Med. 2009;151:775–783. doi: 10.1059/0003-4819-151-11-200912010-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention 2007.National health and nutrition examination survey (NHANES): Anthropometry procedures manual. Atlanta Centers for Disease Control and Prevention.
- 14.WHO Expert Committee on Physical Status : the Use and Interpretation of Anthropometry . World Health Organization; 1995. (1993 : Geneva S, organization WH. physical status : the use of and interpretation of anthropometry, report of a who expert committee.https://apps.who.int/iris/handle/10665/37003 accessed Dec 23, 2020. [PubMed] [Google Scholar]
- 15.Kanamori K., Ihana-Sugiyama N., Yamamoto-Honda R., et al. Postprandial glucose surges after extremely low carbohydrate diet in healthy adults. Tohoku J Exp Med. 2017;243:35–39. doi: 10.1620/tjem.243.35. [DOI] [PubMed] [Google Scholar]
- 16.Mustad V.A., Hegazi R.A., Hustead D.S., et al. Use of a diabetes-specific nutritional shake to replace a daily breakfast and afternoon snack improves glycemic responses assessed by continuous glucose monitoring in people with type 2 diabetes: a randomized clinical pilot study. BMJ Open Diabetes Res Care. 2020;8 doi: 10.1136/bmjdrc-2020-001258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bittel A.J., Bittel D.C., Mittendorfer B., et al. A single bout of premeal resistance exercise improves postprandial glucose metabolism in obese men with prediabetes. Med Sci Sports Exerc. 2021;53:694–703. doi: 10.1249/MSS.0000000000002538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martin Bland J., DouglasG A. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327:307–310. North Am Ed. [PubMed] [Google Scholar]
- 19.Breiman L. Random forests. Mach Learn Dordr. 2001;45:5–32. [Google Scholar]
- 20.Bergenstal R.M., Beck R.W., Close K.L., et al. Glucose management indicator (GMI): a new term for estimating A1C from continuous glucose monitoring. Diabetes Care. 2018;41:2275–2280. doi: 10.2337/dc18-1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leelarathna L., Thabit H., Hovorka R., Evans M. Estimated HbA1c and glucose management indicator (GMI): are they the same? Diabet Med. 2021;38:e14423. doi: 10.1111/dme.14423. [DOI] [PubMed] [Google Scholar]
- 22.Beck R.W., Bergenstal R.M., Riddlesworth T.D., et al. Validation of time in range as an outcome measure for diabetes clinical trials. Diabetes Care. 2019;42:400–405. doi: 10.2337/dc18-1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Association AD 7. Diabetes technology: standards of medical care in diabetes-2021. Diabetes Care. 2021;44:S85–S99. doi: 10.2337/dc21-S007. [DOI] [PubMed] [Google Scholar]
- 24.Selvin E., Parrinello C.M., Daya N., Bergenstal R.M. Trends in insulin use and diabetes control in the U.S.: 1988–1994 and 1999–2012. Diabetes Care. 2016;39:e33–e35. doi: 10.2337/dc15-2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ren X., Gao J., Han T., Sun C. Association between risk of type 2 diabetes and changes in energy intake at breakfast and dinner over 14 years: a latent class trajectory analysis from the China health and nutrition Survey, 1997–2011. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-046183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Odegaard A.O., Jacobs D.R., Steffen L.M., Horn L.V., Ludwig D.S., Pereira M.A. Breakfast frequency and development of metabolic risk. Diabetes Care. 2013;36:3100–3106. doi: 10.2337/dc13-0316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jakubowicz D., Wainstein J., Landau Z., et al. Influences of breakfast on clock gene expression and postprandial glycemia in healthy individuals and individuals with diabetes: a randomized clinical trial. Diabetes Care. 2017;40:1573–1579. doi: 10.2337/dc16-2753. [DOI] [PubMed] [Google Scholar]
- 28.Maki K.C., Phillips-Eakley A.K., Smith K.N. The effects of breakfast consumption and composition on metabolic wellness with a focus on carbohydrate metabolism. Adv Nutr. 2016;7:613S–621S. doi: 10.3945/an.115.010314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abdul-Ghani M.A., Jenkinson C.P., Richardson D.K., Tripathy D., DeFronzo R.A. Insulin secretion and action in subjects with impaired fasting glucose and impaired glucose tolerance: results from the veterans administration genetic epidemiology study. Diabetes. 2006;55:1430–1435. doi: 10.2337/db05-1200. [DOI] [PubMed] [Google Scholar]
- 30.Hanefeld M., Koehler C., Fuecker K., Henkel E., Schaper F., Temelkova-Kurktschiev T. Insulin secretion and insulin sensitivity pattern is different in isolated impaired glucose tolerance and impaired fasting glucose: the risk factor in impaired glucose tolerance for atherosclerosis and diabetes study. Diabetes Care. 2003;26:868–874. doi: 10.2337/diacare.26.3.868. [DOI] [PubMed] [Google Scholar]
- 31.Lyon A.W., Higgins T., Wesenberg J.C., Tran D.V., Cembrowski G.S. Variation in the frequency of hemoglobin A1c (HbA1c) testing: population studies used to assess compliance with clinical practice guidelines and use of HbA1c to screen for diabetes. J Diabetes Sci Technol. 2009;3:411–417. doi: 10.1177/193229680900300302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wang C., Lv L., Yang Y., et al. Glucose fluctuations in subjects with normal glucose tolerance, impaired glucose regulation and newly diagnosed type 2 diabetes mellitus. Clin Endocrinol. 2012;76:810–815. doi: 10.1111/j.1365-2265.2011.04205.x. Oxf. [DOI] [PubMed] [Google Scholar]
- 33.Cowie C.C., Rust K.F., Byrd-Holt D.D., et al. Prevalence of diabetes and high risk for diabetes using A1C criteria in the U.S. Population in 1988–2006. Diabetes Care. 2010;33:562–568. doi: 10.2337/dc09-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ehrhardt N., Al Zaghal E. Behavior modification in prediabetes and diabetes: potential use of real-time continuous glucose monitoring. J Diabetes Sci Technol. 2019;13:271–275. doi: 10.1177/1932296818790994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jackson M.A., Ahmann A., Shah V.N. Type 2 diabetes and the use of real-time continuous glucose monitoring. Diabetes Technol Ther. 2021;23:27. doi: 10.1089/dia.2021.0007. S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kulkarni K.D. Food, culture, and diabetes in the United States. Clin Diabetes. 2004;22:190–192. [Google Scholar]
- 37.Mora N., Golden S.H. Understanding cultural influences on dietary habits in asian, middle eastern, and latino patients with type 2 diabetes: a review of current literature and future directions. Curr Diabetes Rep. 2017;17:126. doi: 10.1007/s11892-017-0952-6. [DOI] [PubMed] [Google Scholar]
- 38.Sumlin L.L., Brown S.A. Culture and food practices of african American women with type 2 diabetes. Diabetes Educ. 2017;43:565–575. doi: 10.1177/0145721717730646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marwaha J.S., Kvedar J.C. Cultural adaptation: a framework for addressing an often-overlooked dimension of digital health accessibility. npj Digit Med. 2021;4:1–2. doi: 10.1038/s41746-021-00516-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Centers for Disease Control and Prevention. Hispanic/Latino americans and type 2 diabetes. 2021; published online April 6th. https://www.cdc.gov/diabetes/library/features/hispanic-diabetes.html (accessed Oct 14, 2021).
- 41.Wang M.C., Shah N.S., Carnethon M.R., O'Brien M.J., Khan S.S. Age at diagnosis of diabetes by race and ethnicity in the United States from 2011 to 2018. JAMA Intern Med. 2021 doi: 10.1001/jamainternmed.2021.4945. published online Sept 7DOI. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pizinger T., Kovtun K., RoyChoudhury A., Laferrère B., Shechter A., St-Onge M.P. Pilot study of sleep and meal timing effects, independent of sleep duration and food intake, on insulin sensitivity in healthy individuals. Sleep Health. 2018;4:33–39. doi: 10.1016/j.sleh.2017.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.MacLeod S.F., Terada T., Chahal B.S., Boulé N.G. Exercise lowers postprandial glucose but not fasting glucose in type 2 diabetes: a meta-analysis of studies using continuous glucose monitoring. Diabetes Metab Res Rev. 2013;29:593–603. doi: 10.1002/dmrr.2461. [DOI] [PubMed] [Google Scholar]
- 44.Wyatt P., Berry S.E., Finlayson G., et al. Postprandial glycaemic dips predict appetite and energy intake in healthy individuals. Nat Metab. 2021;3:523–529. doi: 10.1038/s42255-021-00383-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chiou J.M., Yang Y.F., Chen Y.T. Multivariate functional principal component analysis: a normalization approach. Stat Sin. 2014 doi: 10.5705/ss.2013.305. DOI. [DOI] [Google Scholar]
- 46.Happ C., Greven S. Multivariate functional principal component analysis for data observed on different (Dimensional) domains. J Am Stat Assoc. 2018;113:649–659. [Google Scholar]
- 47.Cardot H., Faivre R., Goulard M. Functional approaches for predicting land use with the temporal evolution of coarse resolution remote sensing data. J Appl Stat. 2003;30:1185–1199. [Google Scholar]
- 48.Foutz N.Z., Jank W. Research note-prerelease demand forecasting for motion pictures using functional shape analysis of virtual stock markets. Mark Sci. 2010;29:568–579. [Google Scholar]
- 49.Barua S., Solis L., Parra E.R., et al. A functional spatial analysis platform for discovery of immunological interactions predictive of low-grade to high-grade transition of pancreatic intraductal papillary mucinous neoplasms. Cancer Inform. 2018;17 doi: 10.1177/1176935118782880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barua S., Elhalawani H., Volpe S., et al. Computed tomography radiomics kinetics as early imaging correlates of osteoradionecrosis in oropharyngeal cancer patients. Front Artif Intell. 2021;4 doi: 10.3389/frai.2021.618469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schmidt M.I., Hadji-Georgopoulos A., Rendell M., Margolis S., Kowarski A. The dawn phenomenon, an early morning glucose rise: implications for diabetic intraday blood glucose variation. Diabetes Care. 1981;4:579–585. doi: 10.2337/diacare.4.6.579. [DOI] [PubMed] [Google Scholar]
- 52.King A.B., Clark D., Wolfe G.S. Contribution of the dawn phenomenon to the fasting and postbreakfast hyperglycemia in type 1 diabetes treated with once-nightly insulin glargine. Endocr Pract. 2012;18:558–562. doi: 10.4158/EP12042.OR. [DOI] [PubMed] [Google Scholar]
- 53.Monnier L., Colette C., Dejager S., Owens D. The dawn phenomenon in type 2 diabetes: how to assess it in clinical practice? Diabetes Metab. 2015;41:132–137. doi: 10.1016/j.diabet.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 54.Harvey R.A., Dassau E., Zisser H., Seborg D.E., Doyle F.J. Design of the glucose rate increase detector: a meal detection module for the health monitoring system. J Diabetes Sci Technol. 2014;8:307–320. doi: 10.1177/1932296814523881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xie J., Wang Q. A variable state dimension approach to meal detection and meal size estimation: in silico evaluation through basal-bolus insulin therapy for type 1 diabetes. IEEE Trans Biomed Eng. 2017;64:1249–1260. doi: 10.1109/TBME.2016.2599073. [DOI] [PubMed] [Google Scholar]
- 56.Zheng M., Ni B., Kleinberg S. Automated meal detection from continuous glucose monitor data through simulation and explanation. J Am Med Inform Assoc. 2019;26:1592–1599. doi: 10.1093/jamia/ocz159. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.