Abstract
Significant progress has been made on the molecular biology of the severe fever with thrombopenia virus (SFTSV); however, many parts of the pathophysiological mechanisms of mortality in SFTS remain unclear. In this study, we investigated virologic and immunologic factors for fatal outcomes of patients with SFTS. We prospectively enrolled SFTS patients admitted from July 2015 to October 2020. Plasma samples were subjected to SFTSV RNA RT-PCR, multiplex microbead immunoassay for 17 cytokines, and IFA assay. A total of 44 SFTS patients were enrolled, including 37 (84.1%) survivors and 7 (15.9%) non-survivors. Non-survivors had a 2.5 times higher plasma SFTSV load than survivors at admission (p < 0.001), and the viral load in non-survivors increased progressively during hospitalization. In addition, non-survivors did not develop adequate anti-SFTSV IgG, whereas survivors exhibited anti-SFTSV IgG during hospitalization. IFN-α, IL-10, IP-10, IFN-γ, IL-6, IL-8, MCP-1, MIP-1α, and G-CSF were significantly elevated in non-survivors compared to survivors and did not revert to normal ranges during hospitalization (p < 0.05). Severe signs of inflammation such as a high plasma concentration of IFN-α, IL-10, IP-10, IFN-γ, IL-6, IL-8, MCP-1, MIP-1α, and G-CSF, poor viral control, and inadequate antibody response during the disease course were associated with mortality in SFTS patients.
Keywords: SFTS phlebovirus, fatal outcome, cytokines, chemokines, humoral immunity
1. Introduction
Severe fever with thrombocytopenia syndrome (SFTS) is an emerging tick-borne disease in East Asia, primarily in China, Korea, and Japan. SFTS virus (SFTSV), now renamed Dabie bandavirus, has been identified as the causative agent. This virus is a novel phlebovirus of the family Phenuiviridae, order Bunyavirales, and is usually transmitted by a tick such as Haemaphysalis longicornis [1]. The disease is characterized by thrombocytopenia and leukopenia following the onset of fever, as well as respiratory or gastrointestinal symptoms, and multiple organ failure can develop in severe cases. Since its first description, the incidence of SFTS has increased in China, Japan, and South Korea, and the case fatality ratio has been reported to be 16.2–32.6% [2,3]. There has been significant progress in our understanding of the molecular biology of SFTSV. Recent research findings have indicated that SFTSV can enter various cell types via pH-dependent endocytosis and interfere with the signaling pathways of the innate and adaptive immunity [4,5,6,7,8,9]. However, many aspects of the pathophysiological mechanisms that lead to fatal outcomes in SFTS patients have remained unclear.
A cytokine storm was reported to be one of the major pathophysiological features underlying the high mortality rate for SFTS [10,11]. This dysregulation of the immune system via hypercytokinemia can cause leukopenia and thrombocytopenia due to peripheral destruction of platelets and/or bone marrow suppression. Recent studies have reported that some cytokines are elevated in severe cases and in the acute phase of this disease [10,12,13,14,15]. Our previous study also found an initial hypercytokinemia in a small number of SFTS patients (n = 11) [16]. However, limited data are available on the detailed kinetics of the cytokine profiles in SFTS patients with fatal outcomes, compared to those who survive this infection [10,12,13]. In the present study, we analyzed the cytokine profiles, viral load, and antibody responses to SFTSV during the disease course and identified some of the factors that can lead to fatal outcomes of patients with SFTS.
2. Materials and Methods
2.1. Patients and Clinical Samples
We prospectively enrolled 44 confirmed cases of SFTS admitted to 5 university-affiliated hospitals in South Korea from June 2015 to October 2020: Asan Medical Center, Gyeongsang National University Hospital, Soonchunhyang University Seoul Hospital, Chung-Ang University Hospital, and Dongguk University Ilsan Hospital. SFTSV infection was confirmed by detection of viral RNA with real-time reverse transcription polymerase chain reaction (RT-PCR). During the hospitalization period, plasma samples were obtained from each patient and collected in an EDTA-treated vacutainer. The plasma was immediately separated from the whole blood and frozen at −80 °C until further analysis. The study protocol was approved by the respective institutional review boards of participating hospitals (Asan Medical Center IRB no. 2016-0748 (15 July 2016); Gyeongsang National University Hospital IRB no. 2019-10-019 (28 November 2019); Soonchunhyang University Seoul Hospital IRB no. 2016-09-001 (30 November 2016); Chung-Ang University Hospital IRB no. 1970-002-376 (18 November 2019); Dongguk University Ilsan Hospital IRB no. 2016-01-088 (25 August 2016)).
2.2. Quantification of Viral RNA
The viral load of patients with SFTS was measured by using one-step multiplex real-time RT-PCR. Viral RNA was extracted from plasma samples using the Qiagen RNeasy Mini Kit (Qiagen, Hilden, Germany). Segment S and M genes were detected to quantify the viral load, and the human β-actin gene was used as an internal control. The sequences of the primers and probes used in this study were as follows: Seg S Forward 5′-CGAGAGAGCTGGCCTATGAA-3′, Reverse 5′-TTCCCTGATGCCTTGACGAT-3′, and Probe 5′-FAM-TGTCTTTGCCCTGACTCGAGGCA-BHQ1-3′; Seg M Forward 5′-ATGCTTGTCGTGAAGAAGGC-3′, Reverse 5′-CTAGACTTCCCACTGCCACA-3′, and Probe 5′-Cy5-ACTTTTGATGGATACGTAGGCTGGGGC-BHQ2-3′; β-actin Forward 5′-ACTAACACTGGCTCGTGTGA-3′, Reverse 5′-CTTGGGATGGGGAGTCTGTT-3′, and Probe 5′-HEX-AGGCTGGTGTAAAGCGGCCTTGG-BHQ1-3′. The reaction mixture was prepared with LightCycler Multiplex RNA Virus Master (Roche Diagnostics, Indianapolis, IN, USA), and RT-PCR was conducted using a LightCycler 96 system (Roche Diagnostics) in accordance with the manufacturer’s instructions. The SFTSV RNA copy number was determined on the basis of a standard curve generated from the Ct values of in vitro transcript RNA. The detection limit of the RT-PCR was 4.3 copies/μL of plasma sample. The method is described in detail in our previous study [17].
2.3. Measurement of Plasma Cytokines
We simultaneously measured the levels of 17 selected cytokines in the plasma samples of the SFTS subjects using a cytometric bead array (BD biosciences, San Jose, CA, USA), as described in our previous study [16]. In brief, capture beads for the following cytokines were incubated with the plasma samples: granulocyte colony-stimulating factor (G-CSF), granulocyte macrophage colony stimulating factor (GM-CSF), interferon (IFN)-α, IFN-γ, tumor necrosis factor (TNF)-α, interleukin (IL)-1β, IL-6, IL-8, IL-10, IL-12p40, IL-13, IL-17A, monocyte chemotactic protein (MCP)-1, macrophage inflammatory protein (MIP)-1α, regulated on activation and normally T cell expressed and secreted (RANTES), IFNγ-induced protein (IP)-10, and vascular endothelial growth factor (VEGF). PE-conjugated antibodies were used to detect the proteins on the capture beads following washing out of the reagents and unbound antibodies. Data were acquired using a FACS CANTO II flow cytometer, FACS Diva software (ver 8.0, BD Biosciences, San Jose, CA, USA), and FlowJo software (ver 10.7.1, FlowJo LLC, Ashland, OR, USA).
2.4. Measurement of Anti-SFTSV IgG
Serological testing for the presence of anti-SFTSV IgG was performed using an immunofluorescence antibody (IFA) assay as previously described [18]. For IFA, Vero E6 cells infected with SFTSV were grown in a 5% CO2 incubator at 37 °C for 5 days. For preparation of IFA antigens, cells were harvested, coated onto Teflon-coated well slides, and then fixed with acetone. IFA assay was carried out using the patient’s serum as the primary antibody and fluorescein-labeled antihuman IgG secondary antibodies (Thermo Fisher Scientific, Waltham, MA, USA). A monoclonal anti-SFTSV N antibody, manufactured in our laboratory, was used as the positive control.
2.5. Statistical Analysis
For statistical analyses, categorical variables were compared using Fisher’s exact test or the χ2 test, and continuous variables were compared with the Mann–Whitney U test. The Spearman test was used to calculate the correlation coefficient between cytokine/chemokine levels and viral RNA load. Principal component analysis (PCA) was used to assess the relationship between multiple cytokines/chemokines and the outcome of SFTS. All tests of significance were two-tailed, and p values less than 0.05 were considered statistically significant. Statistical analyses were performed using GraphPad Prism 9.1.2 (GraphPad Software, Inc., La Jolla, CA, USA).
3. Results
3.1. Clinical Characteristics of the Patients
Forty-four patients with SFTS confirmed by an SFTSV-specific RT-PCR result from plasma specimens were enrolled, including 37 (84.1%) survivors and 7 (15.9%) non-survivors. Among these patients, 27 (61.4%) were men, and the mean age (±standard deviation) was 63.8 (±10.5) years. Twenty-five (56.8%) patients had no underlying diseases, but the others had a broad range of underlying diseases including diabetes mellitus (n = 12, 27.3%), a solid tumor (n = 3, 6.8%), chronic liver disease (n = 3, 6.8%), chronic lung disease (n = 4, 9.1%), and autoimmune disease (n = 1, 2.3%). Detailed baseline characteristics of these patients are provided in Table 1.
Table 1.
Baseline characteristics of the study patients with SFTS.
| Total (n = 44) |
Survivor (n = 37) |
Non-Survivor (n = 7) |
p Value | |
|---|---|---|---|---|
| Age (years), mean ± SD | 63.8 ± 10.5 | 62.4 ± 10.0 | 71.0 ± 10.9 | 0.031 |
| Male gender | 27 (61.4) | 21 (56.8) | 6 (85.7) | 0.220 |
| Season (months) | ||||
| Spring–Summer (3–8) | 21 (47.7) | 15 (40.5) | 6 (85.7) | 0.042 |
| Fall (9–11) | 23 (52.3) | 22 (59.5) | 1 (14.3) | |
| Eschar | 11 (25.0) | 9 (24.3) | 2 (28.6) | 1.000 |
| Clinical characteristics | ||||
| Fever | 43 (97.7) | 36 (97.3) | 7 (100.0) | 1.000 |
| Skin rash | 6 (13.6) | 5 (13.5) | 1 (14.3) | 1.000 |
| Bleeding | 6 (13.6) | 5 (13.5) | 1 (14.3) | 1.000 |
| Myalgia | 25 (56.8) | 22 (59.5) | 3 (42.9) | 0.443 |
| Anorexia/General weakness | 34 (77.3) | 29 (78.4) | 5 (71.4) | 0.649 |
| Nausea/Vomiting | 21 (47.7) | 18 (48.6) | 3 (42.9) | 1.000 |
| Diarrhea | 19 (43.2) | 16 (43.2) | 3 (42.9) | 1.000 |
| Stomachache | 13 (29.5) | 10 (27.0) | 3 (42.9) | 0.404 |
| Dyspnea | 13 (29.5) | 10 (27.0) | 3 (42.9) | 0.404 |
| Altered mental status | 24 (54.5) | 17 (45.9) | 7 (100.0) | 0.011 |
| Concomitant infection | 12 (27.3) | 9 (24.3) | 3 (42.9) | 0.369 |
| Underlying diseases | ||||
| Previously healthy | 25 (56.8) | 19 (51.4) | 6 (85.7) | 0.119 |
| Diabetes mellitus | 12 (27.3) | 9 (24.3) | 3 (42.9) | 0.369 |
| Solid tumor | 3 (6.8) | 2 (5.4) | 1 (14.3) | 0.413 |
| Chronic liver disease | 3 (6.8) | 1 (2.7) | 2 (28.6) | 0.061 |
| Chronic kidney disease | 0 | 0 | 0 | |
| Chronic lung disease | 4 (9.1) | 2 (5.4) | 2 (28.6) | 0.113 |
| Autoimmune disease | 1 (2.3) | 0 | 1 (14.3) | 0.159 |
| Immunosuppressive condition | 0 | 0 | 0 | |
| Laboratory findings | ||||
| WBC (/μL), median (IQR) | 1800 (1070–2823) | 1800 (1080–3065) | 1800 (1000–2500) | 0.712 |
| Hemoglobin (g/dL), median (IQR) | 14.0 (12.9–15.1) | 14.0 (12.2–15.1) | 15.0 (17.7–15.2) | 0.051 |
| Platelets × 103(/μL), median (IQR) | 57.5 (42.0–77.5) | 59.0 (42.0–80.0) | 53.0 (33.0–66.0) | 0.577 |
| BUN (mg/dL), median (IQR) | 17.0 (12.0–23.8) | 14.0 (10.5–21.5) | 26.0 (20.0–28.0) | 0.013 |
| Creatinine (mg/dL), median (IQR) | 0.84 (0.66–1.13) | 0.80 (0.64–1.08) | 1.33 (0.89–1.72) | 0.017 |
| AST (IU/L), median (IQR) | 214.0 (121.8–429.3) | 213.0 (127.5–355.5) | 484.0 (51.0–2005.0) | 0.466 |
| ALT (IU/L), median (IQR) | 103.0 (69.0–184.5) | 101.0 (59.5–138.5) | 197.0 (69.0–535.0) | 0.286 |
| CRP (mg/dL), median (IQR) | 0.46 (0.10–0.98) | 0.30 (0.10–0.80) | 1.30 (0.42–5.70) | 0.070 |
| Time from symptom onset to admission (days), median (IQR) | 6.0 (4.3–7.0) | 7.0 (4.0–7.0) | 5.0 (5.0–6.0) | 0.476 |
| Time from hospital admission to defervescence (days), median (IQR) † | 3.0 (2.0–5.8) | 3.5 (1.8–6.3) | 3.0 (1.8–5.0) | 0.715 |
| Time from hospital admission to hospital discharge or death (days), median (IQR) | 10.0 (7.3–14.5) | 11.0 (9.0–15.0) | 5.0 (3.0–7.0) | <0.0001 |
| Clinical course | ||||
| ICU admission | 17 (38.6) | 10 (27.0) | 7 (100.0) | 0.0005 |
| Treatment | ||||
| Doxycycline | 37 (84.1) | 32 (86.5) | 5 (71.4) | 0.307 |
| Ribavirin | 18 (40.9) | 15 (40.5) | 3 (42.9) | 1.000 |
| Plasma exchange | 29 (65.9) | 23 (62.2) | 6 (85.7) | 0.393 |
| Convalescent plasma therapy | 3 (6.8) | 2 (5.4) | 1 (14.3) | 0.413 |
† Data missing for 5 survivors and 1 non-survivor. Abbreviations: WBC, white blood cells; BUN, blood urea nitrogen; AST, aspartate transaminase; ALT, alanine transaminase; CRP, C-reactive protein; ICU, intensive care unit; SD, standard deviation; IQR, interquartile range.
3.2. Viral and Immunological Factors Associated with Mortality
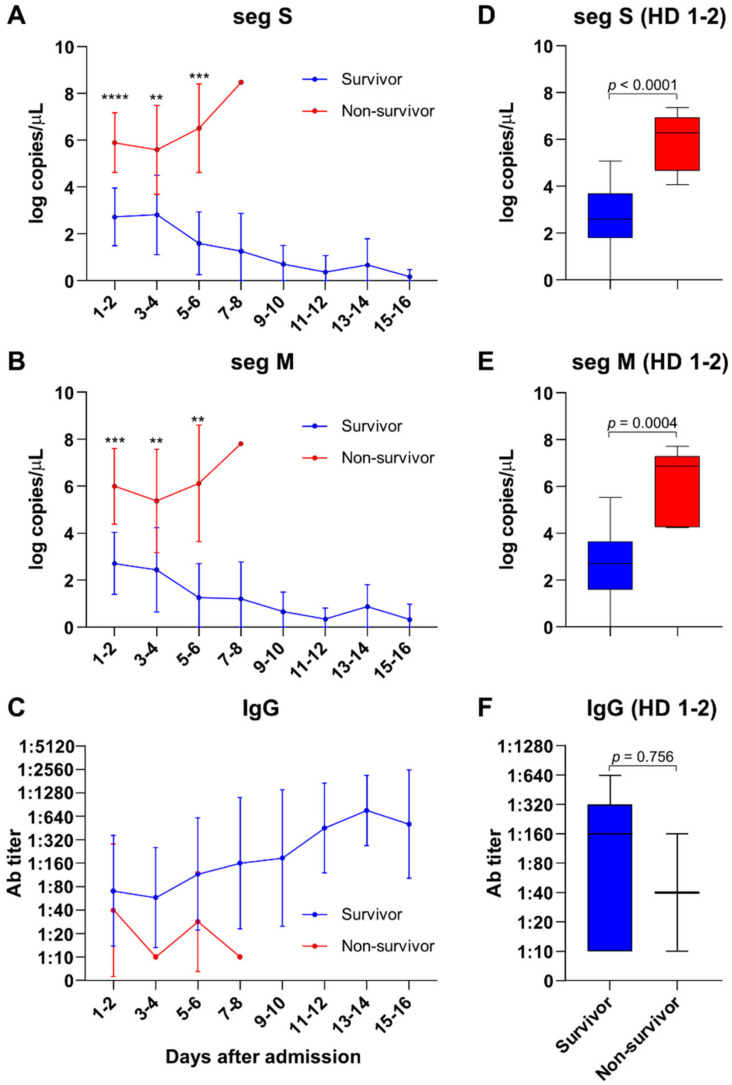
The detailed kinetics of viral load and antibody response in the SFTS patients after admission are shown in Figure 1. The non-survivors had median viral loads that were about 2.5 times higher than those of the survivors, and these loads continuously increased during the hospitalization period (Figure 1A,B). The peak viral load in the survivors was observed at hospital days 1–2, and the amount of viral RNA decreased over time in these cases. The initial viral loads were also significantly higher in patients who died compared with those who recovered (p < 0.0001 for seg S, p = 0.0004 for seg M, Figure 1D,E). The median initial viral load in the survivors was 2.59 log copies/µL (IQR, 1.78–3.68) for segment S, and 2.70 log copies/µL (IQR, 1.59–3.64) for segment M. In the patients who died, however, the initial titer for segment S was 6.28 log copies/µL (IQR, 4.67–6.94), and that for segment M was 6.86 log copies/µL (IQR, 7.29). An anti-SFTSV IgG response developed in survivors but was found to be impaired in the non-survivors (Figure 1C,F).
Figure 1.
Plasma SFTS viral load and antibody titer in patients with SFTS. Both segment S (seg S) and M (seg M) titers were significantly higher in non-survivors than in survivors and increased during hospitalization (A,B). The SFTS viral load (hospital days 1–2) was significantly higher in non-survivors (D,E). The plasma antibody titer against SFTSV increased in survivors during hospitalization but decreased in non-survivors (C). There were no differences between the initial (hospital days 1–2) anti-SFTSV-IgG titers of the survivors and non-survivors (F). Blue, survivor; red, non-survivor. ** p < 0.01, *** p < 0.001, **** p < 0.0001.
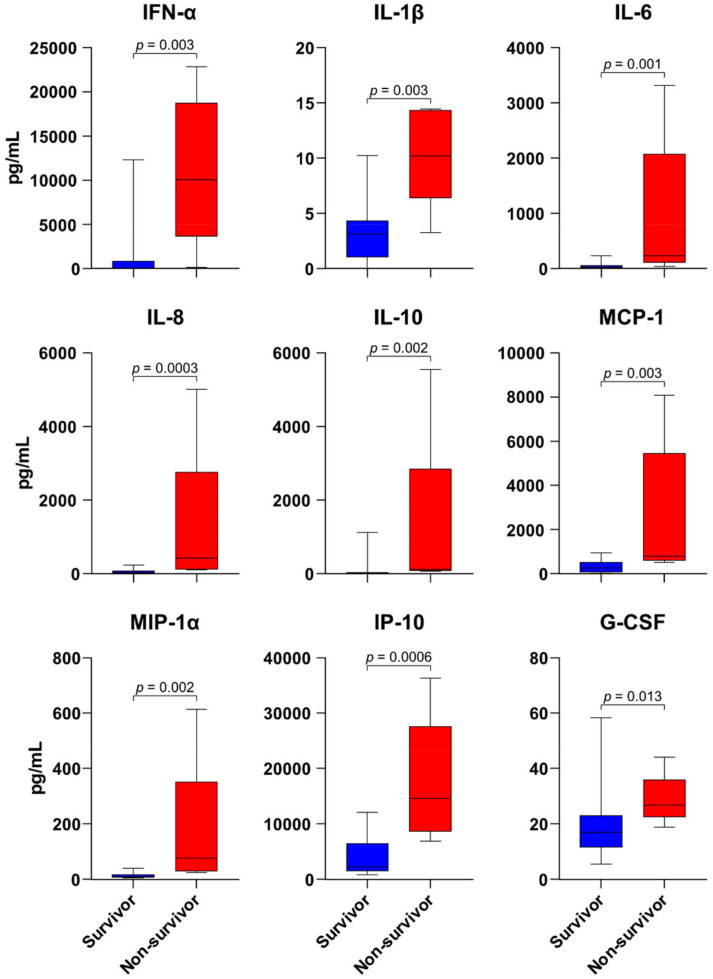
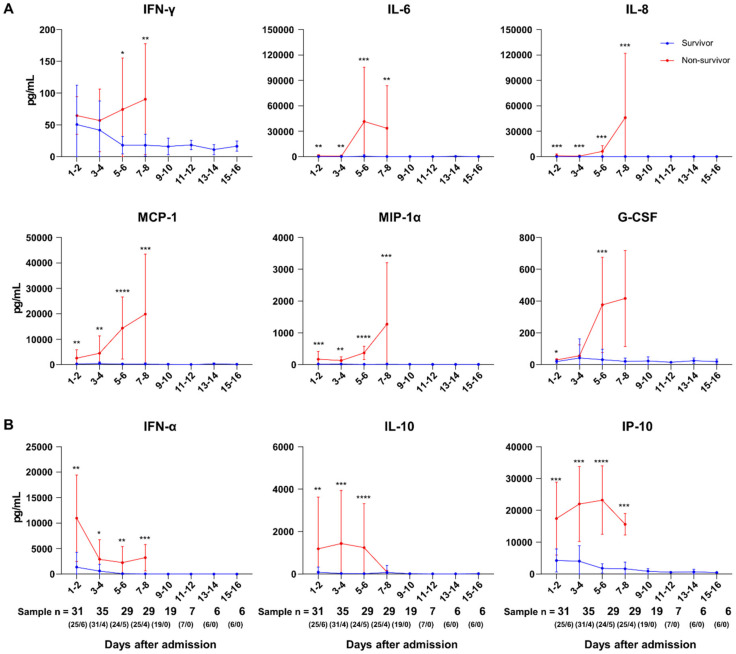
A total of 162 plasma specimens from the SFTS subjects were available for multiplex cytokine bead array analysis. Among the 17 cytokines measured in these assays, the plasma concentrations of IFN-α, IL-1β, IL-6, IL-8, IL-10, MCP-1, MIP-1α, IP-10, and G-CSF were found to be significantly higher in the non-survivors at admission (Figure 2). In addition, the plasma concentrations of these cytokines were markedly higher in non-survivors throughout the disease course. During the disease course, IFN-γ, IL-6, IL-8, MCP-1, MIP-1α, and G-CSF were elevated and reached a maximal level in non-survivors after day 5 of hospitalization (Figure 3A). On the other hand, IFN-α was at its highest level on the day of admission and decreased throughout the disease in all patients. The plasma concentrations of IL-10 and IP-10 did not show significant changes during hospitalization (Figure 3B). The levels of these cytokines did not return to within a normal range in either survivors or non-survivors. The RANTES level in non-survivors decreased below its normal range during the disease course and was significantly lower in non-survivors compared with survivors, at hospital days 7–8 (p = 0.001). As shown in Supplementary Table S1, IFN-α, IFN-γ, IL-10, MCP-1, IL-8, IP-10, IL-6, MIP-1α, and G-CSF were significantly correlated with the initial viral load, while RANTES and VEGF showed inverse correlations with the initial viral load. In addition, when the cytokines were compared on the basis of intensive care unit (ICU) admission, the plasma concentrations of IL-6, IL-8, IL-10, and MIP-1a were significantly higher in ICU-admitted patients than in others (Supplementary Table S2). Moreover, the plasma concentrations of IL-6 and IL-8 were significantly higher in patients with CNS involvement than in others (Supplementary Table S3). Therefore, proinflammatory cytokines IL-6 and IL-8 may contribute to severity in survivors.
Figure 2.
Initial plasma concentrations of cytokines and chemokines in patients with SFTS. The plasma concentrations of IFN-α, IL-1β, IL-6, IL-8, IL-10, MCP-1, MIP-1α, IP-10, and G-CSF on hospital days 1–2 in non-survivors were significantly higher than those in the survivors. Blue, survivor; red, non-survivor.
Figure 3.
Plasma concentrations of cytokines and chemokines in patients with SFTS. IFN-γ, IL-6, IL-8, MCP-1, MIP-1α, and G-CSF levels gradually increased during hospitalization (A), whereas IFN-α, IL-10, and IP-10 levels decreased or did not change (B). The numbers of analyzed samples were as follows: HD 1–2, n = 31 (survivor/non-survivor, 25/6); HD 3–4, n = 35 (31/4); HD 5–6, n = 29 (24/5); HD 7–8, n = 29 (25/4); HD 9–10, n = 19 (19/0); HD 11–12, n = 7 (7/0); HD 13–14, n = 6 (6/0); HD 15–16, n = 6 (6/0). * p < 0.05, ** p < 0.01, *** p < 0.001, **** p < 0.0001.
In addition, principal component analysis (PCA) was performed to identify the prognostic marker for SFTS (Supplementary Figure S1). The data of non-survivors and survivors had different distributions on the plot. Most cytokines and chemokines had a positive relation with the first principal component (PC1); therefore, PC1 was associated with SFTSV infection. The second principal component (PC2) had a positive relation with the data of non-survivors, and thus PC2 was associated with the fatality of SFTS. The cytokines most related to PC1 were identified in the order of MCP-1, MIP-1α, IL-1β, and IL-8. In addition, IP-10, MCP-1, IL-10, IFN-α, and IFN-γ were identified to be related to PC2 in that order. Therefore, these cytokines might be useful as prognostic markers for SFTS.
4. Discussion
It is well known that an excessive release of cytokines and chemokines by activated immune cells and infected cells is involved in immunopathology and the development of organ dysfunction. Our findings in this study, namely, that there are high plasma concentrations of IFN-α, IL-10, IP-10, IFN-γ, IL-6, IL-8, MCP-1, MIP-1α, G-CSF, and viral RNA in non-surviving cases of SFTS, suggest that excessive cytokine release and uncontrolled viremia were critical determinants of these fatal outcomes.
IL-10 plays immunoregulatory roles during a variety of infections [19]. IL-10 is expressed by almost all subsets of leukocytes and protects the host from tissue damage resulting from excessive proinflammatory responses during infection. In certain types of infection, however, the cytokine may interfere with pathogen clearance and contribute to pathogenesis. Polymorphisms in the IL-10 gene or increased IL-10 production can increase host susceptibility to a wide variety of infections in humans and in animal models [20]. In addition, the cytokine is critical to the establishment of T cell exhaustion and viral persistence [21]. In terms of SFTSV infection, our present results are comparable with those of several studies that have consistently reported that IL-10 is higher in severe and fatal cases than in mild cases [10,12,13,14]. Choi et al. suggested that a local immunosuppressive environment created by the upregulation of IL-10 following TPL2 activation by the non-structural (NS) protein of SFTSV enables vigorous viral replication, leading to viral pathogenesis [22]. Although IL-10 is commonly known to promote B cell survival and plasma cell differentiation, its upregulation does not seem to affect the increase in humoral immune response in non-surviving SFTS patients. In a previous study, Song et al. suggested that IL-10 contributes to disrupted B cell immunity by suppressing germinal center formation and inhibiting the differentiation of dendritic cells [8]. It is worth noting that there was a decrease in IL-10 in non-surviving SFTS patients (Figure 1 and Figure 3), despite a high viral load. The initial increase in immunosuppressive IL-10 production induced by an SFTS non-structural protein may be considered as a key immune evasive mechanism of SFTS [23]. It is thus unclear why IL-10 decreases in the late course of fatal SFTS. However, a limited number of patients were included in this non-survivor late course (HD# 7-8), and thus further studies are needed on whether there is a decrease in IL-10 in the late course of fatal SFTS. Taken together, the evidence to date suggests that elevated IL-10 may play an important role in the pathophysiology leading to fatal outcomes in patients with SFTS.
IFN-α, a member of the type I IFNs, is a cytokine produced by virus-infected cells and activated immune cells. Exposure of cells to IFNs induces an antiviral state and prevention of productive viral infection. Type I IFN is thought to play a protective role during phlebovirus infection, and these viruses have counterstrategies to delay or prevent type I IFN responses. It has been reported that the NS proteins of SFTSV and other phleboviruses disrupt type I IFN by various mechanisms [24]. Chaudhary et al. and Ning et al. observed that the SFTSV NS protein suppresses type I IFN signaling by reducing STAT1 and STAT2 activity, leading to an inhibition of downstream interferon-stimulated gene responses [5,6,7,25]. Hence, an initial elevation in IFN-α in patients with a high SFTSV load would seem to be counterintuitive. However, an early appropriate type I IFN response may be important to control viral replication, but delayed type I IFN with an excessive response due to extensive tissue damage may be detrimental for tissue inflammation, as shown in our non-surviving patients who initially presented as having multi-organ failure. Further research on the role of type I IFN in SFTSV infection is needed [15,16].
Significant roles of MIP-1α, MCP-1, and IP-10 and their receptors in viral infection have been reported [26]. Elevated chemokine levels in fatal and severe SFTS were also described previously [10,12,27]. In addition, we found in our present analysis that increased chemokine levels returned to a normal range in patients who survived SFTS, but not in non-survivors. The consistent finding of high chemokine levels in fatal and severe SFTS cases may indicate the importance of the innate immune response in this disease.
There were several noteworthy limitations to the present study. First, we analyzed a relatively small number of patients (n = 44) and thus could not perform multivariate analysis to identify any confounding factors. Second, we did not examine the adaptive cellular immune response that may well contribute to a resolution of this viral infection. More in-depth investigations on cellular and humoral immune responses against SFTSV are needed, as they may assist with the development of vaccines and therapeutic agents. Finally, our findings suggest that uncontrolled viremia or high cytokine/chemokine releases may be associated with pathophysiologic mechanisms resulting in a fatal outcome. However, the pathophysiologic mechanism of SFTS is largely unknown. The patients with fatal SFTS merely had a more severe disease course with more upregulated immunologic parameters. Thus, uncontrolled viremia or high cytokine/chemokine releases might be intermediate variables in the causal pathway, as with septic shock in bacteremia patients [28]. Further studies are needed in this area.
5. Conclusions
In conclusion, the current study shows that severe inflammation reflected in a high plasma concentration of cytokines, poorly controlled viral replication, and an impaired humoral response is associated with fatal outcomes in SFTS patients.
Supplementary Materials
The following are available at https://www.mdpi.com/article/10.3390/v13122351/s1, Figure S1: Principal component analysis (PCA) biplot of the entire dataset from 44 SFTS patients, plotted along PC1 and PC2. Table S1: Correlation of cytokine and chemokine levels with levels of initial viral RNA from blood in patients with SFTS., Table S2: Comparison of initial cytokine and chemokine levels of survivor SFTS patients upon ICU admission., Table S3: Comparison of initial cytokine and chemokine levels of survivor SFTS patients with CNS involvement.
Author Contributions
Conceptualization, S.-H.K. (Sung-Han Kim) and S.-H.K. (Sun-Ho Kee); data curation, J.-S.K., J.-Y.K., D.K. and H.-H.C.; formal analysis, J.-S.K., J.-Y.K., S.-H.R., T.K., S.-Y.P. (Se-Yoon Park), M.-C.K., S.-Y.P. (Seong-Yeon Park), D.K. and H.-H.C.; funding acquisition, S.-H.K. (Sung-Han Kim); investigation, J.-S.K., J.-Y.K., S.-H.R., T.K., S.-Y.P. (Se-Yoon Park), M.-C.K., S.-Y.P. (Seong-Yeon Park), D.K., H.-H.C., H.-J.L. and S.J.; methodology, J.-S.K., J.-Y.K., D.K., S.-H.K. (Sung-Han Kim) and S.-H.K. (Sun-Ho Kee); project administration, K.-H.L., S.-H.K. (Sung-Han Kim) and S.-H.K. (Sun-Ho Kee); resources, T.K., S.-Y.P. (Se-Yoon Park), M.-C.K., S.-Y.P. (Seong-Yeon Park), M.-J.K., Y.-P.C., S.-O.L., S.-H.C., Y.-S.K., K.-H.L., S.-H.K. (Sung-Han Kim) and S.-H.K. (Sun-Ho Kee); validation, J.-S.K., J.-Y.K., D.K. and H.-H.C.; visualization, J.-S.K., S.-H.K. (Sung-Han Kim) and S.-H.K. (Sun-Ho Kee); writing—original draft, J.-S.K. and S.-H.K. (Sung-Han Kim); writing—review and editing, J.-S.K., S.-H.K. (Sung-Han Kim) and S.-H.K. (Sun-Ho Kee). All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by a grant from the Korea National Institute of Health (Grant No. 2021-ER5304-01).
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the institutional review board of Asan Medical Center (IRB no. 2016-0748), Gyeongsang National University Hospital (IRB no. 2019-10-019), Soonchunhyang University Seoul Hospital (IRB no. 2016-09-001), Chung-Ang University Hospital (IRB no. 1970-002-376), and Dongguk University Ilsan Hospital (IRB no. 2016-01-088).
Informed Consent Statements
Written informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data sharing is not applicable.
Conflicts of Interest
There are no conflicts of interest for any of the authors.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yu X.J., Liang M.F., Zhang S.Y., Liu Y., Li J.D., Sun Y.L., Zhang L., Zhang Q.F., Popov V.L., Li C., et al. Fever with Thrombocytopenia Associated with a Novel Bunyavirus in China. N. Engl. J. Med. 2011;364:1523–1532. doi: 10.1056/NEJMoa1010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li H., Lu Q.-B., Xing B., Zhang S.-F., Liu K., Du J., Li X.-K., Cui N., Yang Z.-D., Wang L.-Y., et al. Epidemiological and clinical features of laboratory-diagnosed severe fever with thrombocytopenia syndrome in China, 2011–2017: A prospective observational study. Lancet Infect. Dis. 2018;18:1127–1137. doi: 10.1016/S1473-3099(18)30293-7. [DOI] [PubMed] [Google Scholar]
- 3.Choi S.J., Park S.-W., Bae I.-G., Kim S.-H., Ryu S.Y., Kim H.A., Jang H.-C., Hur J., Jun J.-B., Jung Y., et al. Severe Fever with Thrombocytopenia Syndrome in South Korea, 2013–2015. PLoS Negl. Trop. Dis. 2016;10:e0005264. doi: 10.1371/journal.pntd.0005264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hofmann H., Li X., Zhang X., Liu W., Kühl A., Kaup F., Soldan S.S., González-Scarano F., Weber F., He Y., et al. Severe fever with thrombocytopenia virus glycoproteins are targeted by neutralizing antibodies and can use DC-SIGN as a receptor for pH-dependent entry into human and animal cell lines. J. Virol. 2013;87:4384–4394. doi: 10.1128/JVI.02628-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chaudhary V., Zhang S., Yuen K.-S., Li C., Lui P.-Y., Fung S.-Y., Wang P.-H., Chan C.-P., Li D., Kok K.-H., et al. Suppression of type I and type III IFN signalling by NSs protein of severe fever with thrombocytopenia syndrome virus through inhibition of STAT1 phosphorylation and activation. J. Gen. Virol. 2015;96:3204–3211. doi: 10.1099/jgv.0.000280. [DOI] [PubMed] [Google Scholar]
- 6.Ning Y.-J., Feng K., Min Y.-Q., Cao W.-C., Wang M., Deng F., Hu Z., Wang H. Disruption of Type I Interferon Signaling by the Nonstructural Protein of Severe Fever with Thrombocytopenia Syndrome Virus via the Hijacking of STAT2 and STAT1 into Inclusion Bodies. J. Virol. 2015;89:4227–4236. doi: 10.1128/JVI.00154-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamada S., Shimojima M., Narita R., Tsukamoto Y., Kato H., Saijo M., Fujita T. RIG-I-Like Receptor and Toll-Like Receptor Signaling Pathways Cause Aberrant Production of Inflammatory Cytokines/Chemokines in a Severe Fever with Thrombocytopenia Syndrome Virus Infection Mouse Model. J. Virol. 2018;92:e02246-17. doi: 10.1128/JVI.02246-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Song P., Zheng N., Liu Y., Tian C., Wu X., Ma X., Chen D., Zou X., Wang G., Wang H., et al. Deficient humoral responses and disrupted B-cell immunity are associated with fatal SFTSV infection. Nat. Commun. 2018;9:3328. doi: 10.1038/s41467-018-05746-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li M.-M., Zhang W.-J., Weng X.-F., Li M.-Y., Liu J., Xiong Y., Xiong S.-E., Zou C.-C., Wang H., Lu M.-J., et al. CD4 T cell loss and Th2 and Th17 bias are associated with the severity of severe fever with thrombocytopenia syndrome (SFTS) Clin. Immunol. 2018;195:8–17. doi: 10.1016/j.clim.2018.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun Y., Jin C., Zhan F., Wang X., Liang M., Zhang Q., Ding S., Guan X., Huo X., Li C., et al. Host Cytokine Storm Is Associated With Disease Severity of Severe Fever With Thrombocytopenia Syndrome. J. Infect. Dis. 2012;206:1085–1094. doi: 10.1093/infdis/jis452. [DOI] [PubMed] [Google Scholar]
- 11.Saijo M. Pathophysiology of severe fever with thrombocytopenia syndrome and development of specific antiviral therapy. J. Infect. Chemother. 2018;24:773–781. doi: 10.1016/j.jiac.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Hu L.-F., Wu T., Wang B., Wei Y.-Y., Kong Q.-X., Ye Y., Yin H.-F., Li J.-B. The Regulation of Seventeen Inflammatory Mediators are Associated with Patient Outcomes in Severe Fever with Thrombocytopenia Syndrome. Sci. Rep. 2018;8:159. doi: 10.1038/s41598-017-18616-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li J., Han Y., Xing Y., Li S., Kong L., Zhang Y., Zhang L., Liu N., Wang Q., Wang S., et al. Concurrent Measurement of Dynamic Changes in Viral Load, Serum Enzymes, T Cell Subsets, and Cytokines in Patients with Severe Fever with Thrombocytopenia Syndrome. PLoS ONE. 2014;9:e91679. doi: 10.1371/journal.pone.0091679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ding Y.-P., Liang M.-F., Ye J.-B., Liu Q.-H., Xiong C.-H., Long B., Lin W.-B., Cui N., Zou Z.-Q., Song Y.-L., et al. Prognostic value of clinical and immunological markers in acute phase of SFTS virus infection. Clin. Microbiol. Infect. 2014;20:O870–O878. doi: 10.1111/1469-0691.12636. [DOI] [PubMed] [Google Scholar]
- 15.Liu M.-M., Lei X.-Y., Yu H., Zhang J.-Z., Yu X.-J. Correlation of cytokine level with the severity of severe fever with thrombocytopenia syndrome. Virol. J. 2017;14:6. doi: 10.1186/s12985-016-0677-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kwon J.-S., Kim M.-C., Kim J.Y., Jeon N.-Y., Ryu B.-H., Hong J., Chong Y.P., Lee S.-O., Choi S.-H., Kim Y.S., et al. Kinetics of viral load and cytokines in severe fever with thrombocytopenia syndrome. J. Clin. Virol. 2018;101:57–62. doi: 10.1016/j.jcv.2018.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim J.Y., Koo B., Jin C.E., Kim M.C., Chong Y.P., Lee S.-O., Choi S.-H., Kim Y.S., Woo J.H., Shin Y., et al. Rapid Diagnosis of Tick-Borne Illnesses by Use of One-Step Isothermal Nucleic Acid Amplification and Bio-Optical Sensor Detection. Clin. Chem. 2018;64:556–565. doi: 10.1373/clinchem.2017.280230. [DOI] [PubMed] [Google Scholar]
- 18.Kim W.Y., Choi W., Park S.-W., Wang E.B., Lee W.-J., Jee Y., Lim K.S., Lee H.-J., Kim S.-M., Lee S.-O., et al. Nosocomial Transmission of Severe Fever With Thrombocytopenia Syndrome in Korea. Clin. Infect. Dis. 2015;60:1681–1683. doi: 10.1093/cid/civ128. [DOI] [PubMed] [Google Scholar]
- 19.Couper K.N., Blount D.G., Riley E.M. IL-10: The master regulator of immunity to infection. J. Immunol. 2008;180:5771–5777. doi: 10.4049/jimmunol.180.9.5771. [DOI] [PubMed] [Google Scholar]
- 20.Mege J.-L., Meghari S., Honstettre A., Capo C., Raoult D. The two faces of interleukin 10 in human infectious diseases. Lancet Infect. Dis. 2006;6:557–569. doi: 10.1016/S1473-3099(06)70577-1. [DOI] [PubMed] [Google Scholar]
- 21.Brooks D.G., Trifilo M.J., Edelmann K.H., Teyton L., McGavern D., Oldstone M.B.A. Interleukin-10 determines viral clearance or persistence in vivo. Nat. Med. 2006;12:1301–1309. doi: 10.1038/nm1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choi Y., Park S.-J., Sun Y., Yoo J.-S., Pudupakam R.S., Foo S.-S., Shin W.-J., Chen S.B., Tsichlis P.N., Lee W.-J., et al. Severe fever with thrombocytopenia syndrome phlebovirus non-structural protein activates TPL2 signalling pathway for viral immunopathogenesis. Nat. Microbiol. 2019;4:429–437. doi: 10.1038/s41564-018-0329-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bae S., Hwang H.J., Kim M.Y., Kim M.J., Chong Y.P., Lee S.-O., Choi S.-H., Kim Y.S., Woo J.H., Kim S.-H. Invasive Pulmonary Aspergillosis in Patients with Severe Fever with Thrombocytopenia Syndrome. Clin. Infect. Dis. 2019;70:1491–1494. doi: 10.1093/cid/ciz673. [DOI] [PubMed] [Google Scholar]
- 24.Wuerth J.D., Weber F. Phleboviruses and the Type I Interferon Response. Viruses. 2016;8:174. doi: 10.3390/v8060174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen X., Ye H., Li S., Jiao B., Wu J., Zeng P., Chen L. Severe fever with thrombocytopenia syndrome virus inhibits exogenous Type I IFN signaling pathway through its NSs in vitro. PLoS ONE. 2017;12:e0172744. doi: 10.1371/journal.pone.0172744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murdoch C., Finn A. Chemokine receptors and their role in inflammation and infectious diseases. Blood. 2000;95:3032–3043. doi: 10.1182/blood.V95.10.3032. [DOI] [PubMed] [Google Scholar]
- 27.Zhang Y.-Z., He Y.-W., Dai Y.-A., Xiong Y., Zheng H., Zhou D.-J., Li J., Sun Q., Luo X.-L., Cheng Y.-L., et al. Hemorrhagic Fever Caused by a Novel Bunyavirus in China: Pathogenesis and Correlates of Fatal Outcome. Clin. Infect. Dis. 2012;54:527–533. doi: 10.1093/cid/cir804. [DOI] [PubMed] [Google Scholar]
- 28.McGregor J.C., Rich S.E., Harris A.D., Perencevich E.N., Osih R., Lodise T.P., Miller R.R., Furuno J.P. A Systematic Review of the Methods Used to Assess the Association between Appropriate Antibiotic Therapy and Mortality in Bacteremic Patients. Clin. Infect. Dis. 2007;45:329–337. doi: 10.1086/519283. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable.