Abstract
Background: Smoking is a major public health problem. Although physicians have a key role in the fight against smoking, some of them are still smoking. Thus, we aimed to conduct a systematic review and meta-analysis on the prevalence of smoking among physicians. Methods: PubMed, Cochrane, and Embase databases were searched. The prevalence of smoking among physicians was estimated and stratified, where possible, by specialties, continents, and periods of time. Then, meta-regressions were performed regarding putative influencing factors such as age and sex. Results: Among 246 studies and 497,081 physicians, the smoking prevalence among physicians was 21% (95CI 20 to 23%). Prevalence of smoking was 25% in medical students, 24% in family practitioners, 18% in surgical specialties, 17% in psychiatrists, 16% in medical specialties, 11% in anesthesiologists, 9% in radiologists, and 8% in pediatricians. Physicians in Europe and Asia had a higher smoking prevalence than in Oceania. The smoking prevalence among physicians has decreased over time. Male physicians had a higher smoking prevalence. Age did not influence smoking prevalence. Conclusion: Prevalence of smoking among physicians is high, around 21%. Family practitioners and medical students have the highest percentage of smokers. All physicians should benefit from targeted preventive strategies.
Keywords: tobacco, smoking, physician, doctor, prevalence
1. Introduction
Smoking is a major public health problem [1]. According to the International Classification of Diseases (ICD−10), tobacco smoking disorder is considered a mental and behavioral disease [2]. Furthermore, according to the World Health Organization, there are about a billion smokers around the world and tobacco kills more than seven million of them per year [1]. Tobacco control has been present in many countries for several years. In 2003, the WHO adopted the Framework Convention on Tobacco Control. Despite their knowledge of the health risks linked to smoking [3], some physicians smoke too [4,5]. Prevalence of smoking among physicians can be a public health issue both for themselves and for patients because they play a key role in combating tobacco use [6]. Indeed, it has been demonstrated that physicians who smoke are less likely to promote quitting smoking to their patients [7,8]. However, the prevalence of smoking among physicians has not recently been systematically reported in the literature. Moreover, some medical specialties may be particularly at risk of smoking, due to workload [9] or work conditions [10], for example. In addition, a country’s culture or wealth can influence the perception of smoking [11,12]. Lastly, the perception of smoking has, historically, changed considerably [13], from a rewarding to a negative image [14]. Although there is a dense literature on the impact of tobacco smoking on health among general population, we did not find any systematic review and meta-analysis on smoking among physicians.
Therefore, we aimed to conduct a systematic review and meta-analysis on the prevalence of smoking among physicians. Secondary objectives were to report physicians’ smoking prevalence depending on their specialties, to investigate differences between countries, changes over time and putative effects of sociodemographic factors.
2. Materials and Methods
2.1. Literature Search
We reviewed all studies reporting the smoking prevalence among physicians. Eligible articles had to appear on the PubMed, Cochrane Library, Embase, and ScienceDirect databases with the following keywords: “smoking” and “physician” (or “doctor”) and “prevalence”. The search was conducted up to May 2021 (details for the search strategy used within each database are available in Appendix A. Studies could be cross-sectional studies, cohort studies, or clinical trials. The search was not limited to specific years. We limited our search to English or French articles. To be included, studies needed to describe our primary outcome variable, i.e., the prevalence of smoking among physicians. Two authors (Anaïs Besson and Alice Tarpin) conducted the literature searches, reviewed the abstracts, and, based on the selection criteria, decided the suitability of the articles for inclusion and extracted the data. When necessary, disagreements were solved with a third author (Frédéric Dutheil). We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15].
2.2. Data Extraction
The primary outcome analyzed was the smoking prevalence and type of smoking (occasional or regular) among physicians. Secondary outcomes reported medical specialty, continent, study’s period, ex-smoking prevalence, sociodemographic parameters (age, gender, family status, and workplace setting), workload (mean duration week), clinical parameters (body mass index and physical activity behavior), and smoking prevalence among a population control.
2.3. Quality of Assessment
We used the Newcastle-Ottawa Scale (NOS) to check the quality of included articles [16]. The maximum score was nine for cohort and ten for cross-sectional studies. Additionally, we also used the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) for cohort and cross-sectional studies [17], and the Consolidated Standards of Reporting Trials (CONSORT) for randomized studies [18] (Appendix B).
2.4. Statistical Considerations
Statistical analysis was conducted using Stata software (v16, StataCorp, College Station, TX, USA). Extracted data were summarized for each study and reported as mean (standard deviation) and count (%) for continuous and categorical variables, respectively. Prevalence of smokers and 95% confidence intervals were estimated using random-effects models assuming between and within study variability (DerSimonian and Laird approach) [19]. Then, we stratified results depending on specialties, continents, and periods of time. Statistical heterogeneity between studies was assessed using forest plots, confidence intervals, and I2. The I2 statistic is the most common metric to measure heterogeneity and is easily interpretable: heterogeneity is considered low for I2 < 25%, modest for 25–50%, and high for >50% [20]. We aimed to conduct a sensitivity analysis by excluding studies not evenly distributed around the base of the metafunnel. We also proposed meta-regressions to investigate putative factors influencing the prevalence of smoking in physicians, such as sociodemographic (age, sex), specialties, continents, and periods of time. Results were expressed as regression coefficients and 95% confidence intervals. Type I-error was fixed at α = 0.05.
3. Results
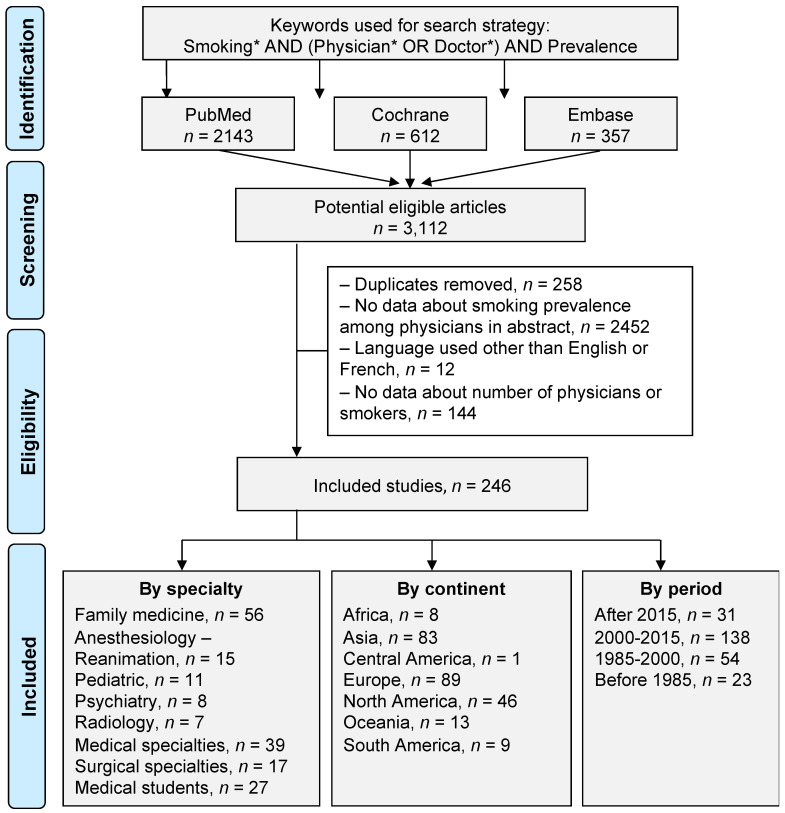
An initial search produced 3112 possible articles. Removal of duplicates and use of the selection criteria reduced the number of articles reporting the smoking prevalence among physicians to 246 articles (Figure 1). Main characteristics of the studies are presented in Table 1.
Figure 1.
Flow chart. Three databases were asked (PubMed, Cochrane, and Embase). Over 3112 eligible articles, 246 were included. Stratification was performed by specialty, by continent, and by time period. *: details for the search strategy used within each database are available in Appendix A.
Table 1.
Characteristics of included studies.
| Study | Country | GDP per Capital | Period of Data Collection | Physicians | Prevalence | (%) of | Smokers | % Men among Smokers | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % Men | Age | Speciality | Regular Smokers | Occasional Smokers | Former Smokers | Total (Regular & Occasional) | |||||
| Aaro 1977 | Norway | 6812 | 1952–1974 | 3544 | Not defined | 58.3 | 92.5 | |||||
| Abdullah 2006 | China | 1149 | 2002 | 757 | 78.2 | Not defined | 2.1 | 4.3 | ||||
| Aboyans 2009 | France | 41,508 | 2007 | 371 | 49.8 | Cardiology | 32.4 | 8.1 | ||||
| Akvardar 2004 | Turkey | 6041 | 319 | Study, Others | 37.6 | |||||||
| Al Alwan 2013 | Saudi Arabia | 16,094 | 2009 | 100 | Not defined | 7 | 12 | |||||
| Alarjan 2015 | Jordan | 4096 | 162 | Not defined | 34.0 | |||||||
| Al-Khateeb 1990 | Bahrain | 7959 | 1988 | 301 | Not defined | 8.6 | 60.1 | |||||
| Al-Lawati 2009 | Oman | 16,784 | 1079 | Family medicine, Biology, Others | 22.2 | 97.5 | ||||||
| Allan 1976 | Australia | 7475 | 1153 | Family medicine, Radiology, Pathology, Anesthesiology-Reanimation, Gynecology, Others | 14 | |||||||
| Al Shahrani 2021 | Saudi Arabia | 23,338 | 2018 | 290 | 59.7 | Not defined | 34.8 | 70.3 | ||||
| Amara 2008 | Morocco | 2885 | 2007 | 75 | 44.4 | Pneumology | 37.5 | 62.5 | 12 | 10,7 | ||
| Amte 2015 | India | 1606 | 242 | 84.7 | 37.9 | Not defined | 36.4 | 63.6 | 13.6 | |||
| An 2004 | USA | 36,334 | 2000 | 750 | 68.9 | Not defined | 16.9 | 1.5 | ||||
| Arnetz 1988 | Sweden | 24,189 | 66 | 100 | 43.9–46.8 | Family medicine, Others | 23.3–33.3 | 22.7 | 100 | |||
| Aryayev 2014 | Ukraine | 3105 | 150 | 31.3 | Family medicine, Paediatry, Study | 42 | 61.9 | |||||
| Baltaci 2014 | Turkey | 10,672 | 2010–2011 | 1233 | 57.1 | 38.94 | Not defined | 14.8 | 34.1 | |||
| Baptista 1993 | Venezuela | 2368 | 1990 | 191 | 49.7 | 31 | Not defined | 20.9 | ||||
| Barengo 2004 | Finland | 1990–2001 | 4546 | 51.4 | Not defined | 38.1 | 61.9 | 16 | ||||
| Barengo 2005 | Finland | 24,913 | 2001 | 707 | Family medicine | 12.7 | ||||||
| Barnoya 2002 | Guatemela | 1702 | 2002 | 174 | 56.9 | Not defined | 35 | 17.8 | 56.9 | |||
| Basnyat 2000 | UK | 28,015 | 1998 | 314 | 97.8 | 51 | Not defined | 37 | 10.2 | 97.8 | ||
| Basu 2011 | India | 1346 | 2010 | 182 | Study | 85.5 | 14.5 | 30.2 | ||||
| Behbehani 2004 | Bahrain, Kuwait | 2000–2001 | 1440 | 66.5 | 44.6–44.7 | Not defined | 62.1 | 37.9 | 14.3–15.9 | 17.2 | 92.7 | |
| Belkić 2007 | Serbie | 2150 | 2002–2004 | 112 | 0 | 48.9 | Not defined | 12.5 | 31.3 | 0 | ||
| Belkić 2012 | Serbie | 2150 | 2002–2004 | 191 | 42.9 | Not defined | 30.4 | 39.7 | ||||
| Bener 1993 | Kuwait, United Arab Emirates | 1990–1992 | 527 | Not defined | 12.7–13.5 | 37 | ||||||
| Borgan 2014 | Bahrain | 24,737 | 2013 | 148 | 33.8 | 45 | Not defined | 3.9 | 10.1 | 80 | ||
| Bortz 1992 | USA | 25,493 | 126 | 77.8 | Not defined | 22.2 | 1.6 | 100 | ||||
| Bostan 2015 | Turkey | 10,672 | 2010–2011 | 699 | 38.7 | Pneumology | 19.5 | 9.9 | ||||
| Bourke 1972 | Ireland | 1152 | 1967–1969 | 1580 | 86 | Not defined | 23.6–42.5 | 45.4 | 91.8 | |||
| Braun 2004 | USA | 38,166 | 2002 | 1067 | 68 | 46 | Not defined | 18.6 | 1.3 | |||
| Brenner 1996 | Germany | 26,334 | 1992–1993 | 696 | 52.6 | Study | 11.9 | 23.7 | 64.8 | |||
| Brink 1994 | USA | 23,954 | 1990 | 132 | Not defined | 1.6 | ||||||
| Brotons 2005 | Croatia, Estonia, Georgia, Greece, Ireland, Malta, Poland, Slovakia, Slovenia, Spain, Sweden | 2000 | 2082 | 40 | 35.6–51.4 | Family medicine | 16.4 | |||||
| Burgess 1970 | USA | 1963–1968 | 1863 | Not defined | 27.3 | |||||||
| Burgess 1978 | USA | 6741 | 1973 | 1234 | 95.1 | Family medicine, Internal medicine, Paediatry, Psychiatry, Radiology, Pathology, Gynecology, Orthopaedy, Anesthesiology-Reanimation, Ear Nose Throat, Others | 35.4 | 19 | 95.7 | |||
| Cao 2011 | USA | 19,705 | 100 | 58.3 | Not defined | 41.7 | 6.7 | 100 | ||||
| Carlos 2020 | Spain | 30,389 | 2018 | 890 | 52 | 51.7 | Not defined | 24 | 16.5 | |||
| Ceraso 2009 | China | 2099 | 2006 | 103 | 100 | Not defined | 49.5 | 100 | ||||
| Chaudhry 2009 | Pakistan | 874 | 2006 | 120 | 75 | Not defined | 23.8 | 100 | ||||
| Cheng 1990 | Hong Kong | 9071 | 1987 | 133 | 81.2 | 25 | Not defined | 33.3 | 66.7 | 15.8 | 90.5 | |
| Coe 1971 | USA | 862 | 1967 | 1572 | Family medicine, Internal medicine | 31.3–34.9 | 29.6 | |||||
| Cofta 2008 | Poland | 14,001 | 117 | Not defined | 81.8 | 18.2 | 10.3 | 9.4 | ||||
| Das 2013 | India | 1462 | 2011 | 600 | 67 | Study | 14.5 | |||||
| Davies 1989 | UK | 13,119 | 1987 | 94 | 83 | Not defined | 26 | 3 | ||||
| De Col 2010 | France | 45,334 | 2008–2009 | 332 | 67.8 | 50.7 | Family medicine | 57.4 | 42.6 | 34 | 18.4 | |
| Dekker 1993 | Netherlands | 17,176 | 1989 | 619 | 70.6 | Family medicine, Study, Others | 29.6 | 83.6 | ||||
| De Oliveira 2013 | USA | 52,782 | 1480 | Study | 6.9 | |||||||
| Desalu 2009 | Nigeria | 1384 | 2008 | 436 | 75.7 | 30.6 | Not defined | 17.7 | ||||
| Djalalinia 2011 | Iran | 1892 | 2002–2003 | 5140 | 74 | 35 | Family medicine | 11.8 | 100 | |||
| Dodds 1979 | Australia | 7763 | 1977 | 275 | 84.7 | Not defined | 30 | 21 | 87.9 | |||
| Doll 1954 | UK | 1951 | 24,389 | 100 | Not defined | 87.3 | 100 | |||||
| Doll 1964 | UK | 1951–1958 | 31,208 | 100 | Not defined | 15.3–26.6 | 61.8 | 100 | ||||
| Doll 1994 | UK | 1951–1990 | 10,812 | 100 | Not defined | 13–60 | 39.9 | 100 | ||||
| Doll 2004 | UK | 19,709 | 1978 | 12,669 | 100 | Not defined | 46.3 | 30.5 | 100 | |||
| Easton 2001 | USA | 26,464 | 1993–1994 | 1590 | 0 | 41 | Not defined | 19.9 | 3.5 | 0 | ||
| Easton 2001 | USA | 26,464 | 1994 | 1397 | 0 | 42 | Not defined | 21.5 | 4.7 | 0 | ||
| Edwards 2008 | New Zealand | 26,671 | 2006 | 10,200 | 60.2 | Family medicine, Study, Radiology, Gynecology, Anesthesiology-Reanimation, Others | 3.5 | 67.6 | ||||
| Edwards 2018 | New Zealand | 42,949 | 2013 | 12,684 | 55.7 | Family medicine, Study, Radiology, Gynecology, Anesthesiology-Reanimation, Others | 12.1 | 2.1 | 61.6 | |||
| Fadhil 2007 | Bahrain | 17,959 | 2005 | 120 | 35.8 | 36.5 | Family medicine | 10 | 24.2 | |||
| Fanello 1990 | France | 1973–1987 | 2718 | Family medicine | 44.6 | |||||||
| Fathi 2016 | Iran | 7833 | 2012–2013 | 225 | Not defined | 21.3 | ||||||
| Fowler 1989 | UK | 15,987 | 1988 | 3240 | 77 | Family medicine | 33 | 13.5 | ||||
| Franceschi 1986 | Italy | 7964 | 1985 | 709 | Family medicine, Internal medicine, Public health, Others | 14–26 | 31.3 | |||||
| Frank 1998 | USA | 27,777 | 1994 | 4501 | 0 | 42.2 | Not defined | 18.6 | 3.7 | 0 | ||
| Frank 2009 | Canada | 44,545 | 2007–2008 | 3213 | 66 | Not defined | 57.1 | 42.9 | 14 | |||
| Freour 2011 | France | 41,575 | 2009 | 337 | Not defined | 30.6 | 12.5 | |||||
| Garfinkel 1976 | USA | 1959–1972 | 8503 | Not defined | 32.7 | |||||||
| Glavas 2003 | Greece | 18,478 | 119 | 76.5 | Not defined | 37 | ||||||
| Grossman 1999 | Costa Rica | 2828 | 1993–1994 | 216 | 70.8 | 41 | Not defined | 40 | 19.4 | 61.9 | ||
| Gunes 2005 | Turkey | 3660 | 2002 | 257 | 77.8 | 31.3 | Not defined | 81.3 | 18.8 | 37.4 | ||
| Gupta 2013 | USA | 47,100 | 2009 | 177 | 41.2 | Internal medicine, Paediatry, Others, Emergency | 99.6 | 0.4 | 0.6 | |||
| Hallett 1983 | UK | 1980 | 385 | Family medicine | 44.4 | 27.8 | ||||||
| Hamadeh 1999 | Bahrain | 10,131 | 1994 | 122 | 52.5 | Family medicine | 66.7 | 33.3 | 14.8 | 17.2 | 81 | |
| Han Zao Li 2008 | China | 1753 | 2005 | 326 | 59.2 | Not defined | 42 | 81.8 | ||||
| Hay 1976 | New Zealand | 1963–1972 | 763 | 0 | 45 | Family medicine, Psychiatry, Anesthesiology-Reanimation, Others | 93.6 | 6.3 | 22.3–26.9 | 20.4 | ||
| Hay 1998 | New Zealand | 1976–1996 | 7335 | 68.5 | Family medicine, Radiology, Gynecology, Anesthesiology-Reanimation, Others | 5 | 71.5 | |||||
| Heloma 1998 | Finland | 26,009 | 332 | 84.3 | 42.6 | Not defined | 40 | 60 | 20.2 | 24.1 | ||
| Hensrud 1993 | USA | 26,387 | 389 | Not defined | 37.3 | 9 | 97.1 | |||||
| Hepburn 2000 | USA | 31,573 | 1997 | 150 | Family medicine | 11 | ||||||
| Heponiemi 2008 | Finland | 41,188 | 2006 | 2652 | 40.8 | 53 | Not defined | 12.4 | ||||
| Hidalgo 2016 | Brazil | 13,246 | 2011 | 182 | 56.6 | Not defined | 12.3 | 5.5 | ||||
| Hill 1997 | USA | 27,777 | 1994 | 121 | 53.7 | Not defined | 4.1 | |||||
| Hodgetts 2004 | Bosnia Herzegovina | 1769 | 2002 | 112 | Not defined | 13.6 | 39.3 | |||||
| Hoseainrezae 2013 | Iran | 6111 | 252 | Not defined | 7.1 | 9.5 | ||||||
| Huang 2013 | China | 5618 | 2011 | 720 | 100 | Not defined | 60 | 40 | 25.7 | 100 | ||
| Hughes 1991 | USA | 20,039 | 1987 | 1733 | 69.4 | 30 | Not defined | 5.3 | ||||
| Hughes 1992 | USA | 22,857 | 1989–1990 | 5426 | 82.4 | Not defined | 3.9 | |||||
| Hughes 1999 | USA | 22,857 | 1989–1990 | 5418 | Family medicine, Internal medicine, Emergency, Pathology, Paediatry, Psychiatry, Anesthesiology-Reanimation, Gynecology, Others | 14.3 | ||||||
| Hung 2013 | USA | 48,467 | 2010 | 1000 | 68.5 | 45.3 | Family medicine | 4 | ||||
| Hussain 1993 | UK | 19,901 | 1991 | 1069 | Not defined | 5 | ||||||
| Içli 1992 | Turkey | 2736 | 1991 | 200 | Study | 34 | ||||||
| Innos 2002 | Estonia | 1982 | 3673 | 23.7 | Not defined | 13.1 | 21.3 | 45.6 | ||||
| Jacot Sadowski 2009 | Swiss | 41,376 | 2002 | 1856 | 78.8 | Not defined | 40.8 | 59.2 | 17.6 | |||
| Jiang 2007 | China | 1509 | 2004 | 3552 | 55.1 | Not defined | 2.7 | 22.9 | 98 | |||
| Jiménez-Ruiz 2015 | Spain | 29,462 | 2014 | 416 | 59.4 | Not defined | 80.4 | 19.6 | 38 | 11.1 | ||
| Jingi 2015 | Cameroon | 1381 | 2012 | 65 | 69.2 | 39.1 | Family medicine | 12.3 | 100 | |||
| John 2003 | Germany | 1989–1999 | 2509 | Not defined | 18.9–22.5 | 20.4 | ||||||
| Joossens 1987 | Belgium | 8846 | 1983 | 2157 | Not defined | 33 | 32 | |||||
| Josseran 2000 | France, Netherlands, Spain, UK, Greece, Brazil | 1992–1997 | 16,788 | Family medicine, Study, Others | 9.5 | |||||||
| Josseran 2005 | France | 24,974 | 1998 | 2073 | 79.3 | 45.1 | Family medicine | 45.5 | 32.1 | 83.6 | ||
| Julião 2013 | Brazil | 8598 | 2009 | 515 | 66.8 | 45.3 | Not defined | 23.3 | 5.8 | |||
| Kaetsu 2002 | Japan | 1983–1990 | 5312 | 95.7 | Not defined | 36.6 | 99.3 | |||||
| Kaetsu 2002 | Japan | 10,425 | 1983 | 4190 | 95.6 | Not defined | 41.9 | 99 | ||||
| Kai 2008 | Japan | 37,217 | 2005 | 1063 | Anesthesiology-Reanimation, Chest surgery | 30 | 12 | |||||
| Kaneita 2010 | Japan | 2000–2008 | 10,890 | 66.4 | Not defined | 16.1 | 88.2 | |||||
| Kawahara 2000 | Japan | 38,437 | 1996–1997 | 709 | 91.8 | 54.7 | Not defined | 46.3 | 26 | 98.4 | ||
| Kawakami 1997 | Japan | 39,269 | 1994 | 323 | 84.8 | 59.8 | Not defined | 46.1 | 21.1 | 95.6 | ||
| Kawane 1993 | Japan | 24,813 | 1989 | 6224 | Pneumology | 39.4 | 24.8 | |||||
| Kono 1985 | Japan | 920 | 1965 | 5446 | 100 | Not defined | 67.8 | |||||
| Kotz 2007 | Netherlands | 29,204 | 2002–2003 | 1180 | 45.9–48.3 | Family medicine, Cardiology, Pneumology | 24.8–29.7 | 6.6 | ||||
| Lam 2011 | China | 2099 | 2006 | 504 | 100 | Not defined | 46.2 | 100 | ||||
| La Vecchia 2000 | Italy | 21,998 | 1999 | 501 | 76.6 | 45 | Not defined | 87.7 | 12.3 | 26.5 | 27.5 | |
| Lefcoe 1970 | UK | 2348 | 310 | 100 | 45.7 | Not defined | 19.7 | 51.9 | 100 | |||
| Legnini 1987 | USA | 18,237 | 1985 | 266 | Public health, Internal medicine, Psychiatry, Others | 17.1–37 | 21.1 | |||||
| Lindfors 2009 | Finland | 37,703 | 2004 | 328 | 53.4 | 47 | Anesthesiology-Reanimation | 16.5 | ||||
| Linn 1986 | USA | 17,134 | 1984 | 211 | 91 | Not defined | 4 | |||||
| Lipp 1972 | USA | 5234 | 1970 | 1061 | Study | 17 | ||||||
| Lipp 1972 | USA | 5609 | 1971 | 1314 | Not defined | 40 | 21 | |||||
| Magee 2017 | Georgia | 4739 | 2014 | 86 | Not defined | 14 | 18.6 | |||||
| Malik 2010 | Pakistan | 1007 | 2009 | 234 | 69.7 | Not defined | 37.2 | 94.3 | ||||
| Manson 2000 | USA | 14,434 | 1982 | 21,068 | 100 | Not defined | 39.2 | 11 | 100 | |||
| Mappin-Kasirer 2020 | UK | 1951–2016 | 29,737 | 100 | Not defined | 14.9–68.4 | 8.4–67.2 | 100 | ||||
| Marakoğlu 2006 | Turkey | 8035 | 363 | 69.1 | 34.2 | Not defined | 9.9 | 28.7 | 85.6 | |||
| Márk 1998 | Hungary | 4495 | 1995 | 170 | 62.9 | Not defined | 25.9 | |||||
| Mathavan 2009 | India | 1102 | 1433 | 65.7 | Not defined | 66.5 | 33.5 | 11.9 | 100 | |||
| McAuliffe 1984 | USA | 14,439 | 1982 | 134 | Not defined | 6 | ||||||
| McEwen 2001 | UK | 28,383 | 1999 | 303 | 68 | Family medicine | 4 | |||||
| McGrady 2007 | Ireland | 47,631 | 2004 | 650 | 46.1 | Family medicine | 15.2 | 4.2 | ||||
| Mejia 2011 | Argentina | 5110 | 2005 | 235 | 54.5 | 45 | Gynecology | 26.3 | 35.3 | |||
| Merrill 2006 | Jordan | 2548 | 2006 | 251 | 69.3 | 45.3 | Not defined | 63 | 37 | 17.5 | 18.3 | 84.8 |
| Meshefedjian 2010 | Canada | 2000–2004 | 610 | 55.1 | Family medicine | 32 | 7.4 | 51.1 | ||||
| Mikalauskas 2012 | Lithuania | 11,837 | 2009 | 59 | 43.8–44.4 | Anesthesiology-Reanimation, Others | 13.6 | |||||
| Misra 2004 | USA | 32,854 | 1998–2000 | 254 | 50.88 | Not defined | 3.5 | |||||
| Miwa 1995 | Japan | 31,465 | 1992 | 17 | 94.1 | Cardiology | 41.2 | |||||
| Mohan 2006 | India | 547 | 2003 | 229 | 66.4 | 42.7 | Not defined | 14.4 | 8.7 | 100 | ||
| Mohseni-Bandpei 2011 | Iran | 5630 | 2008 | 223 | 48.4 | 42.7 | Not defined | 13.5 | ||||
| Moreno 2006 | Spain | 21,463 | 2003 | 147 | 21.5–39.1 | Study, Others | 7.3–26.7 | 47.6 | ||||
| Mostafa 2017 | Egypt | 3525 | 2016 | 521 | 64.3 | Internal medicine, Dermatology, Paediatry, Gynecology, Others | 8.3 | 21.5 | 89.3 | |||
| Movsisyan 2019 | Armenia | 3607 | 2015 | 36 | 25 | Study | 0 | 16.7 | 100 | |||
| Mubeen 2008 | Pakistan | 683 | 2005 | 165 | 43.6 | 20.16–22.89 | Study | 37.5 | 62.5 | 2.4–3.8 | 14.5 | 95.8 |
| Naji 2006 | Ireland | 32,541 | 2002 | 106 | 61.3 | Not defined | 22.6 | 21.7 | 60.9 | |||
| Nakládalová 2005 | Czech Republic | 8033 | 2002–2004 | 370 | 54.9 | Not defined | 16.8 | 62.9 | ||||
| Nardini 1998 | Italy | 20,665 | 1995 | 605 | 81.3 | 44 | Not defined | 34.4 | 25 | |||
| Nawaz 2007 | Pakistan | 625 | 2004–2005 | 1029 | 44.6 | 21 | Study | 63.5 | 36.5 | 22.4 | 11.2 | 89.6 |
| Nawaz 2008 | Pakistan | 837 | 2006–2007 | 227 | Family medicine | 36.1 | ||||||
| Ndiaye 2001 | Senegal | 681 | 1999 | 163 | 78.5 | 41 | Not defined | 6.8 | 27.6 | 93.3 | ||
| Nelson 1994 | USA | 1974–1991 | 379 | Not defined | 27.8–32 | 9 | ||||||
| Ng 2007 | Indonesia | 1065 | 2003 | 447 | Not defined | 11.6 | 96.2 | |||||
| Nollen 2004 | Nigeria | 742 | 2002 | 373 | 83.9 | 33 | Not defined | 2.9 | ||||
| Nutbeam 1990 | UK | 19,096 | 304 | 82.6 | Family medicine | 32 | 13.8 | 100 | ||||
| Obeidat 2017 | Jordan | 4073 | 2014 | 104 | 42.7 | Not defined | 44.2 | |||||
| O’Cathail 2013 | Ireland | 52,105 | 2009–2010 | 248 | Not defined | 20.8–22 | 8.1 | 50 | ||||
| Ohida 2001 | Japan | 38,532 | 2000 | 3771 | 66.3 | Not defined | 20.3 | 88.7 | ||||
| O’Keeffe 2019 | Ireland | 55,413 | 2014 | 1746 | 50.5 | Paediatry, Pathology, Psychiatry, Emergency, Anesthesiology-Reanimation, Gynecology, Ophtalmology, Others | 27.2 | 72.8 | 9.3 | 61.1 | ||
| Öztürk 2012 | Turkey | 11,707 | 80 | 88.8 | Surgery, Study | 10 | 17.5 | 100 | ||||
| Pärna 2005 | Estonia, Finland | 2001–2002 | 4549 | 29.9 | Not defined | 49.1 | 50.2 | 19.6–36.9 | 14.2 | 48.5 | ||
| Pärna 2005 | Estonia | 5345 | 2002 | 2668 | 17.4 | 47.6 | Not defined | 19.6 | 13.3 | 32.8 | ||
| Pärna 2017 | Estonia | 1982–2014 | 9423 | 20.2 | Not defined | 82.5 | 17.5 | 13–19.1 | 14.7 | 41 | ||
| Perrin 2006 | Armenia | 1192 | 2004 | 236 | 43.6 | 43.5 | Not defined | 83.8 | 16.2 | 10.59 | 33.9 | 71.3 |
| Peykari 2010 | Iran | 6603 | 5140 | 74 | 35 | Family medicine | 47.8 | 52.2 | 6.5 | 15.9 | ||
| Phillips 1968 | Canada | 3463 | 1743 | Not defined | 77.2 | 22.8 | 27.2 | 45.8 | ||||
| Pillay 2020 | India | 2005 | 2018 | 692 | 70.4 | 39 | Not defined | 8.5 | 7.7 | |||
| Pipe 2009 | France, Germany, Greece, Italy, Netherlands, Poland, Spain, Sweden, Swiss, Turkey, UK, USA, Canada, Mexico, Japan, Korea | 2006 | 2836 | 76 | 48 | Family medicine, Internal medicine | 42.3 | 78.1 | ||||
| Piryani 2004 | Pakistan | 461 | 1998 | 200 | 71 | Not defined | 32 | 93.8 | ||||
| Pizzo 2003 | Italy | 20,088 | 2000 | 526 | Family medicine | 28.3 | ||||||
| Poanta 2006 | Romania | 5829 | 112 | 35.7 | 39.5 | Not defined | 42 | 46.8 | ||||
| Põld 2017 | Estonia | 2002–2014 | 4877 | 16.9 | Not defined | 67.5 | 32.5 | 10.4 | 34.3 | |||
| Põld 2020 | Estonia | 20,367 | 2014 | 2903 | 54.5 | Not defined | 5.9 | 63.7 | ||||
| Polyzos 1995 | Greece | 11,176 | 1992 | 148 | Not defined | 49.3 | ||||||
| Power 1999 | Ireland | 26,284 | 1999 | 171 | Family medicine | 16.1 | ||||||
| Ramachandran 2008 | India | 628 | 2004–2006 | 2499 | 75.2 | 39 | Not defined | 8 | 100 | |||
| Ranchal 2018 | Spain | 1986–2016 | 938 | Not defined | 3.6–20.1 | 23.2 | ||||||
| Rankin 1975 | Australia | 6993 | 1276 | 87.6 | Not defined | 38 | 14.2 | |||||
| Ravara 2014 | Portugal | 23,030 | 2009 | 608 | 37.3 | 39.1 | Family medicine, Study, Others | 17.3 | 20.9 | 52 | ||
| Reile 2018 | Estonia | 20,367 | 2014 | 1759 | 82.4 | Not defined | 7.9 | 86.3 | ||||
| Roche 1995 | Australia | 20,320 | 1995 | 1365 | 53.1 | 29.8 | Not defined | 6 | 53.7 | |||
| Roche 1996 | Australia | 21,861 | 1996 | 908 | 46.9 | 28.7 | Family medicine | 8.3 | 4 | |||
| Rurik 2008 | Hungary | 10,286 | 2004 | 156 | 42.9 | Family medicine, Others | 8.3 | 23.1 | ||||
| Rurik 2014 | Hungary | 13,046 | 2009 | 208 | 39.9 | 55.2 | Not defined | 5.8 | 33.3 | |||
| Saadat 2012 | Scandinavia | 58 | 53.4 | Anesthesiology-Reanimation | 12.1 | |||||||
| Sachs 1983 | USA | 15,561 | 1983 | 567 | Pneumology | 12 | ||||||
| Saeed 1991 | Saudi Arabia | 7839 | 698 | not defined | 34 | |||||||
| Saeys 2014 | Belgium | 47,349 | 2011 | 626 | 57 | 45 | Family medicine | 50 | 50 | 14 | 8 | 72 |
| Salgado 2014 | Argentina | 12,849 | 2011 | 1659 | 26.9 | Study | 68.7 | 31.3 | 51.72 | 27.3 | 28.7 | |
| Samuels 1997 | Israel | 19,653 | 260 | 74.2 | 41 | Study, Paediatry, Radiology, Others | 20 | 15.8 | ||||
| Schnoll 2006 | Russia | 6920 | 63 | 82.5 | 41.3 | Oncology | 50.8 | 27 | ||||
| Scott 1992 | USA | 1963–1988 | 8589 | Not defined | 13.4 | |||||||
| Sebo 2007 | Swiss, Finland, Bosnia and Herzegovina, USA | 1989–2004 | 1784 | 83.6 | 51 | Family medicine, Internal medicine, Paediatry, Cardiology, Others | 22.4 | 12.3 | 85.5 | |||
| Seiler 1983 | UK | 8692 | 1983 | 607 | Family medicine | 19 | ||||||
| Senior 1982 | Canada | 12,440 | 1982 | 88 | Not defined | 19.3 | ||||||
| Sharma 1988 | India | 1982–1987 | 127 | Not defined | 34.6 | |||||||
| Shi 2010 | China | 3832 | 2009 | 467 | 54.8 | Anesthesiolopgy-Reanimation | 10.9 | 10.1 | ||||
| Shin 2012 | China | 4550 | 2010 | 17 | 47.1 | 39.4 | Not defined | 29.4 | ||||
| Shishani 2008 | Jordan | 3386 | 87 | Not defined | 43.7 | |||||||
| Shishani 2011 | Jordan | 2774 | 2007 | 242 | 86 | Not defined | 12.4 | 46.7 | ||||
| Shkedy 2013 | Isreal | 36,310 | 140 | Internal medicine, Paediatry, Anethesiology -Reanimation, Ear Nose Throat, Gynecology | 10–27.3 | 15.7 | 45.5 | |||||
| Siddiqui 2001 | Saudi Arabia | 8685 | 20 | Not defined | 10 | 20 | ||||||
| Singh 1981 | India | 186 | 1977–1978 | 861 | Study, Others | 27.5 | ||||||
| Smith 2006 | China | 1509 | 2004 | 286 | Not defined | 1 | 15.7 | |||||
| Smith 2007 | New Zealand | 1963–1996 | 22,097 | Not defined | 19–37 | 17.9 | ||||||
| Sotiropoulos 2007 | Greece | 18,478 | 2003–2005 | 1284 | 55.9 | 38.4 | Family medicine, Internal medicine, Biology, Others | 13.8 | 38.6 | 58.3 | ||
| Squier 2006 | Ukraine | 1048 | 2003 | 799 | 35.9 | 45 | Family medicine | 21.6 | 13.9 | |||
| Steinberg 2007 | USA | 38,166 | 2002 | 334 | 70.7 | 49 | Not defined | 23 | 3.3 | |||
| Stuyt 2009 | USA | 47,976 | 2007 | 1319 | 68.8 | 44.3 | Family medicine, Internal medicine, Paediatry, Psychiatry, Emergency, Anesthesiology-Reanimation, Gynecology, Others | 1 | 38.9 | 75.4 | ||
| Sundquist 1999 | Sweden | 32774 | 1996 | 1004 | 46.2 | Family medicine | 8.4 | 50 | ||||
| Svärdsudd 2002 | Sweden | 24,225 | 1993–1999 | 974 | Family medicine, Paediatry, Internal medicine, Psychiatry, Radiology, Orthopaedy, Ear Nose Throat, Gynecology, Others | 3–43 | 7.5 | |||||
| Tapia-Conyer 1997 | Mexico | 5650 | 1993 | 3488 | 66.2 | 37 | Not defined | 20.6 | 26.9 | |||
| Tee 2007 | Malaysia | 5594 | 2005 | 481 | 39.1 | Study | 2.7 | 1.7 | 75 | |||
| Tessier 1996 | France | 22,380 | 1993 | 730 | 90 | 47 | Cardiology | 51.8 | 48.2 | 47 | 27 | |
| Thankappan 2008 | India | 541 | 2003 | 333 | 77.5 | 42.2 | Not defined | 26.1 | 10.8 | 100 | ||
| Thomas 1986 | USA | 19,071 | 106 | 100 | 30.2–30.9 | Not defined | 13.2 | 100 | ||||
| Thomas 1997 | USA | 1957–1965 | 1015 | 24–27 | Study | 55.4 | ||||||
| Tomson 2003 | Laos | 363 | 151 | 49.7 | Not defined | 46.2 | 53.8 | 17.2 | 100 | |||
| Tong 2010 | USA | 39,497 | 2003–2004 | 1245 | 69.7 | Emergency, Psychiatry, Others | 18.4–28.8 | 3.5 | ||||
| Torre 2005 | USA | 1948–1964 | 1158 | 91.9 | Not defined | 51.1 | 91.7 | |||||
| Tosun 2016 | Turkey | 11,336 | 2011–2012 | 224 | 65.2 | 31.71 | Not defined | 28.1 | ||||
| Trédaniel 1993 | France | 16,302 | 1987 | 1012 | 87.5 | Family medicine | 29.1 | 36.9 | 89.3 | |||
| Ulbricht 2009 | Germany | 37 | 51.4 | 47.5 | Family medicine | 24.3 | ||||||
| Unal 2017 | Turkey | 1975–2004 | 7228 | 66 | 43.6 | Not defined | 22.5 | 23.9 | 75.3 | |||
| Underner 2004 | France | 24,177 | 2002 | 257 | Family medicine | 60.6 | 39.4 | 30.7 | 25.7 | |||
| Underner 2006 | France | 24,177 | 2002 | 257 | 48 | Family medicine | 61.2 | 38.8 | 31 | 26.1 | ||
| Uysal 2007 | Turkey | 6041 | 2004 | 374 | 66.8 | 46 | Not defined | 29 | 16 | 70 | ||
| Vanderhoek 2013 | Canada | 52,542 | 2012 | 301 | 48.5 | 24.4 | Study | 15.9 | ||||
| Vanphanom 2011 | Laos | 710 | 2007 | 855 | 52.9 | Not defined | 54.4 | 45.6 | 18.4 | 9.2 | 97.5 | |
| Varona 2005 | Cuba | 2308 | 1997 | 121 | 33.1 | Family medicine | 18.2 | 40.9 | ||||
| Viegas 2007 | Brazil | 4770 | 2005 | 830 | Not defined | 81.7 | 18.3 | 22.7 | 7.2 | |||
| Voigt 2009 | Germany | 34,044 | 2004–2006 | 912 | Not defined | 13.7 | ||||||
| Waalkens 1992 | Netherlands | 17,398 | 1989 | 1085 | 58.3 | Study, Others | 14.5–34 | 28.7 | 68.8 | |||
| Wada 2007 | Japan | 37,218 | 2005 | 196 | 76 | Not defined | 19.4 | |||||
| Wada 2011 | Japan | 40,855 | 2009 | 3864 | 78.3 | Not defined | 12 | 14 | 90.6 | |||
| Wang 2021 | China | 9977 | 2018 | 1046 | 61.2 | Not defined | 14.7 | |||||
| Wilf Miron 2019 | Israel | 35,776 | 2015 | 4832 | 59.7 | Not defined | 8.5 | |||||
| Willaing 2003 | Denmark | 33,441 | 1999 | 40 | Not defined | 23 | 25 | |||||
| Wilson 2020 | Australia | 251 | Family medicine | 21.1 | ||||||||
| Wyshak 1980 | USA | 11,674 | 1979 | 289 | 92 | Not defined | 13.8 | |||||
| Yaacob 1993 | Malaysia | 2654 | 1991 | 120 | 70.8 | Not defined | 13.3 | 17.5 | 100 | |||
| Yan 2008 | China | 1289 | 2003 | 358 | Not defined | 10.6 | 35.8 | |||||
| Young 1997 | Australia | 21,861 | 1996 | 855 | Family medicine | 3.2 | ||||||
| Zabadi 2018 | Paslestine | 2005 | 502 | 80.1 | 34.92 | Family medicine, Study, Others | 12.2 | 39.6 | 64.8 | |||
| Zanetti 1998 | Italy | 23,020 | 1996 | 393 | 74 | Not defined | 31 | 68.9 | ||||
| Zhang 2012 | China | 4550 | 2010 | 84 | 38.1 | 39.4 | Not defined | 17.6 | 82.4 | 2 | 20.2 | |
| Zhang 2015 | China | 8069 | 8725 | Study, Others | 12.8 | 96.7 | ||||||
| Zhou 2010 | China | 2694 | 2007 | 673 | 73.3 | Not defined | 5 | 26.2 | 96.6 | |||
| Zinonos 2016 | Cyprus | 35,391 | 2008 | 119 | 59.7 | Not defined | 16 | 28.6 | ||||
| Zylbersztejn 2015 | Argentina | 13,080 | 2013 | 3033 | 41.3 | Not defined | 21.7 | 19.7 | ||||
3.1. Quality of Articles
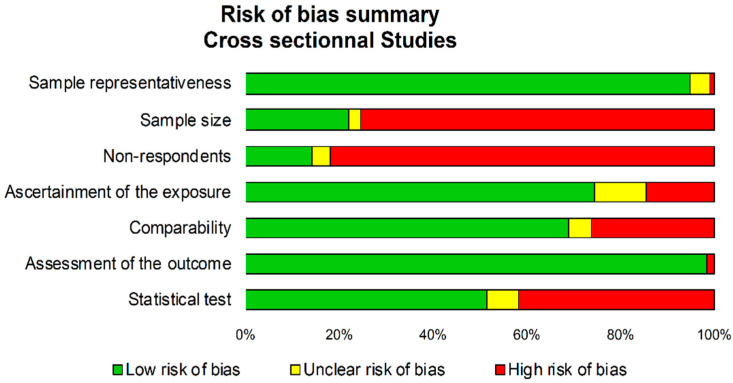
Using the NOS criteria for cross-sectional studies demonstrated a low risk of bias, except for sample size (not clearly defined in 75% of studies), representativeness (comparability bias in 82% of studies), and statistical tests (not or incompletely described in 49% of studies) (Figure 2). NOS for cross-sectional and cohort assessment are shown in Figure S1 in Supplement. STROBE and CONSORT assessment are shown in Table A1.
Figure 2.
Risk of bias using Newcastle Ottawa Scale composed by seven level of bias assessment.
3.2. Study Designs and Objectives
Most (94%) studies were cross-sectional [7,8,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191,192,193,194,195,196,197,198,199,200,201,202,203,204,205,206,207,208,209,210,211,212,213,214,215,216,217,218,219,220,221,222,223,224,225,226,227,228,229,230,231,232,233,234,235,236,237,238,239,240,241,242,243,244,245,246,247,248,249,250]. However, twelve were cohort [251,252,253,254,255,256,257,258,259,260,261,262] and two were clinical trials [263,264]. Every one of the included 246 studies described smoking prevalence among physicians. The main aim of examining smoking prevalence among physicians was reported in most studies (n = 117) [24,26,27,29,32,33,35,36,37,38,39,40,41,44,45,48,49,53,54,55,56,58,59,68,69,72,73,76,78,82,84,85,87,90,91,92,93,94,95,97,98,99,102,103,104,107,108,110,115,119,120,121,126,131,132,133,135,136,137,138,141,142,144,145,146,147,148,149,151,154,156,157,158,160,161,163,164,165,167,169,170,171,172,174,176,178,179,180,182,183,185,187,189,190,191,192,193,194,196,197,199,201,202,203,204,207,211,213,218,224,225,227,231,239,241,242,243]. Fifteen studies also aimed to assess the use of other substances in physicians [29,37,93,94,95,117,118,124,141,161,165,171,193,239,248]. Other outcomes presented were demographic characteristics and health status of physicians in 58 studies [22,23,30,31,42,43,46,57,60,63,64,65,66,74,75,80,88,89,96,100,106,114,116,123,125,128,129,130,134,139,143,153,155,162,176,177,181,184,195,198,208,223,238,239,249,251,252,253,254,255,256,257,258,259,260,261,263,264], the evaluation of smoking cessation counselling among physicians in 50 studies [25,26,28,33,35,40,55,61,62,67,70,79,86,92,97,99,101,104,105,111,136,142,144,145,152,157,168,183,189,190,191,197,201,203,204,205,209,210,212,214,218,219,234,235,236,241,242,244,247,250], the attitude of physicians towards prevention and promotion of a healthy lifestyle in seven studies [122,140,206,208,220,222,228], the knowledge on tobacco effects in 20 studies [24,33,39,44,50,53,61,62,78,91,98,119,154,178,199,204,216,217,240,247], and the examination of the link between smoking habits of physicians and their practice of providing minimal smoking cessation advice in 26 studies [7,8,21,47,58,81,83,109,112,127,150,159,175,186,187,188,208,211,213,224,225,232,237,244,246,262]. Finally, the primary outcome was not clearly defined in 16 studies [34,51,52,71,77,113,166,173,200,215,221,226,229,230,233,245].
3.3. Recruitment of Physicians
Physicians were recruited from health centers in 94 studies, either monocentric in 50 studies [21,26,29,30,37,41,42,43,46,49,56,79,80,97,115,120,121,132,133,134,156,162,163,167,170,179,181,182,184,190,193,194,196,202,204,212,217,225,228,229,232,235,244,250,256,257,259,260,263,264] or multicentric in 44 studies [24,39,53,54,72,83,89,90,91,92,98,111,112,117,119,123,126,128,130,131,141,152,168,169,178,197,201,203,205,207,214,216,219,220,224,227,231,236,237,238,242,243,253,261]. They were also recruited from specific lists in 68 studies, either from specific societies in 14 studies [22,40,47,77,78,110,158,180,183,189,221,222,230,240], associations in 23 studies [7,59,67,87,94,95,106,107,108,118,129,135,142,206,209,223,234,239,245,249,251,254,262], medical or specific registers in 22 studies, [23,38,85,88,113,127,139,144,145,154,159,165,173,177,186,192,199,208,210,246,248,258] and lists from ministries of health in 9 studies [33,35,45,99,116,140,146,166,218]. Finally, recruitment procedure was not defined in 84 studies [8,25,27,28,31,32,34,36,44,48,50,51,52,55,57,58,60,61,62,63,64,65,66,68,69,70,71,73,74,75,76,81,82,84,86,93,96,100,101,102,103,104,105,109,114,122,124,125,136,137,138,143,147,148,149,150,151,153,155,157,160,161,164,171,172,174,175,176,185,187,188,191,195,198,200,211,213,215,226,233,241,247,252,255]. Smoking prevalence was also described in non-physicians in 30 studies [24,39,40,52,69,74,79,86,91,99,102,104,105,110,113,125,129,133,135,139,143,151,161,162,176,185,195,197,202,235].
3.4. Populations Studied
Sample size ranged from 17 [235,237] to 31,208 [64]. In total, 497,081 physicians were included in this meta-analysis.
Age of physicians was reported in 89 studies. Overall, the mean age was 41.5 years old (95%CI 38.4 to 44.6), ranging from 20.2 [132] to 59.8 [109] years old (Table 1).
Gender was reported in more than half of the studies (n = 165) on the total population of physicians, among which 107 studies also reported gender of smoking physicians. The mean number of men was 62% (58 to 65%), ranging from 0 in five studies that included only women, to 100% in thirteen studies that included only men (Table 1).
Specialty was reported in 96 studies. Family practitioners were the most represented (56 studies, n = 64,187 physicians), followed by medical students (27 studies, n = 28,564), medical specialties (39 studies, n = 15,538), anesthesiologists (15 studies, n = 3329), surgical specialties (17 studies, n = 2395), pediatrics (11 studies, n = 1847), psychiatrists (8 studies, n = 1393), and radiologists (7 studies, n = 1193) (Table 1).
Location of studies was always reported. Most studies were conducted in Europe (89 studies, n = 20,509), followed by America (56 studies, n = 126,615), Asia (83 studies, n = 104,325), Oceania (13 studies, n = 59,609), and Africa (8 studies, n = 2023) (Table 1).
Other variables were less well described. Family status was reported in 29 studies [22,42,45,74,79,85,89,92,93,94,103,105,112,121,125,128,130,137,143,161,174,179,195,199,229,244,250,257,264], workplace was the focus in 42 studies (most worked in public sectors) [22,28,40,47,58,61,75,79,88,94,96,104,105,125,130,133,134,135,137,148,149,150,155,161,163,172,174,180,185,186,189,199,203,218,219,223,226,229,234,239,240,242], working hours per week was reported in 8 studies (ranging from 37 [25] to 79 [80] hours per week) [22,25,58,75,80,143,195,213], seniority of physician was reported in 14 studies (ranging from 6.5 [205] to 20.8 [28] years ago) [25,28,36,58,78,96,126,130,137,140,150,184,204,205], BMI in 17 studies (ranging from 21 [260] to 27.7 [257] kg/m2) [23,30,42,66,80,88,96,130,139,140,141,244,249,255,257,259,260], and physical activity in 24 studies (most physicians were active) [30,42,46,57,75,88,89,96,100,121,122,123,125,129,130,134,139,140,143,195,238,239,255,257].
3.5. Smoking Assessment
Most studies used a self-administered questionnaire (postal and email) (209 studies) [7,8,21,22,23,24,25,26,27,28,29,30,31,32,33,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,56,57,59,60,61,62,63,64,65,66,67,68,69,70,71,72,75,76,77,78,79,80,81,82,83,84,85,86,87,88,90,91,92,93,94,95,96,98,99,102,105,106,107,108,109,111,112,114,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,137,139,140,141,142,143,144,145,146,147,148,149,151,153,154,157,158,159,160,161,162,163,164,165,166,167,168,169,170,171,172,173,174,176,177,178,179,180,181,182,184,185,186,189,190,192,193,194,195,196,197,198,199,201,202,203,205,206,207,209,210,211,212,213,214,215,217,218,219,220,221,222,223,224,225,227,228,229,230,231,232,234,235,236,237,238,239,240,241,242,244,245,246,248,249,250,251,252,253,254,255,256,257,259,260,262,263,264]. Other studies collected data by interview (11 studies) [35,55,100,101,150,155,156,175,191,208,261], interview and postal (7 studies) [58,73,74,115,183,187,188], phone (9 studies) [89,103,104,136,152,204,216,226,233], and phone and postal (1 study) [98]. The data collection method was unclear in nine studies [34,97,110,113,138,200,243,247,258]. The definition of smoking used was not explained in most (96.2%) included articles. In eight studies, smoking was defined by one cigarette per day [24,93,142,156,162,202,203,220]. In five studies, a smoker was defined as a person who had smoked at least 100 cigarettes or an equivalent amount of tobacco in their lifetime [24,138,178,202,261]. Two studies specified whether smokers were cigarette, pipe, or cigar smokers [114,115]. Around half of the studies reported the prevalence of ex-smokers (135 studies, n = 47,688) (Table 1). As with smoking, the definition of ex-smoking was not explained in most (95.2%) included articles. In five studies, an ex-smoker was defined as someone who stopped smoking completely for at least 3 [220], 6 [142,261], or 12 months [24,224]. Publication occurred within 2 years of data collection for 31% of studies, within 2 to 5 years for 45%, and more than 5 years for 10%—and was not reported for 14% of studies. Most studies were published between 2000 and 2015 (138 studies, n = 232,323), followed by studies published between 1985 and 2000 (54 studies, n = 85,402), after 2015 (31 studies, n = 94,637), and before 1985 (23 studies, n = 84,719). Studies ranged from 1954 [63] to 2021 [243,247] (Table 1).
3.6. Meta-Analysis on the Smoking Prevalence among Physicians
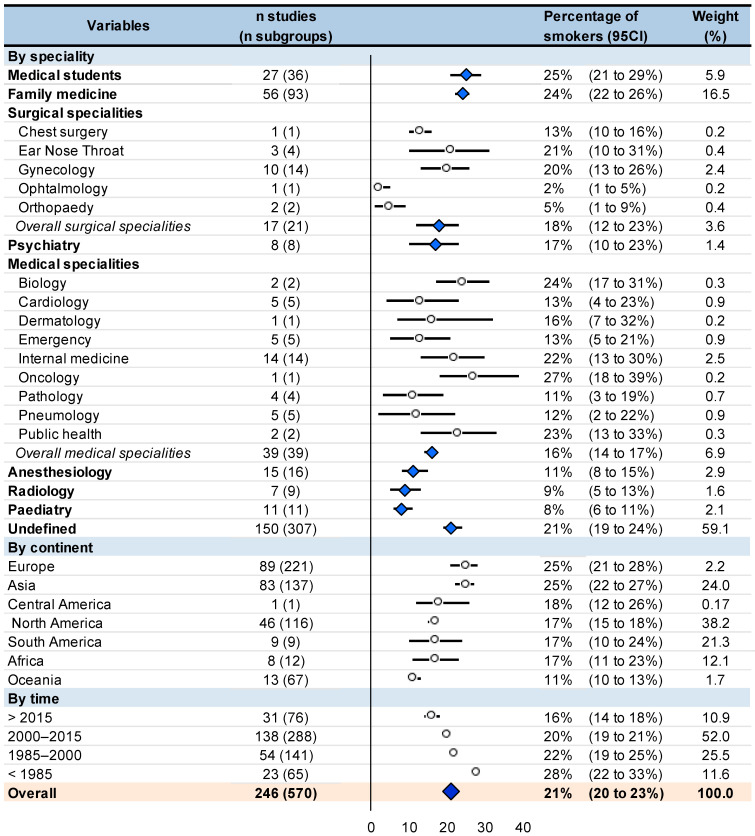
The smoking prevalence among physicians was around 21% (95CI 20 to 23%). Stratified by specialty, prevalence of smoking was 25% (21 to 29%) in medical students, 24% (22 to 26%) in family practitioners, 18% (12 to 23%) in surgical specialties, 17% (10 to 23%) in psychiatrists, 16% (14 to 17%) in medical specialties, 11% (8 to 15%) in anesthesiologists, 9% (5 to 13%) in radiologists, and 8% (6 to 11%) in pediatrics. Stratification by continent showed the prevalence of smoking in physicians ranging from 11% in Oceania to 25% in Europe and Asia. The smoking prevalence among physicians decreased over time: 28% (22 to 33%) before 1985, 22% (19 to 25%) between 1985 and 2000, 20% (19 to 21%) between 2000 and 2015, and 16% (14 to 18%) after 2015. All I2 were extremely high within each stratification, i.e., >99%, except two I2 that were at 86 and 94% (Figure 3).
Figure 3.
Meta-analysis on prevalence among physicians stratified by specialty, continent, and time. Results are expressed in percentage from 0 to 100. Bold represent a stratification or overall result.
3.7. Meta-Regressions
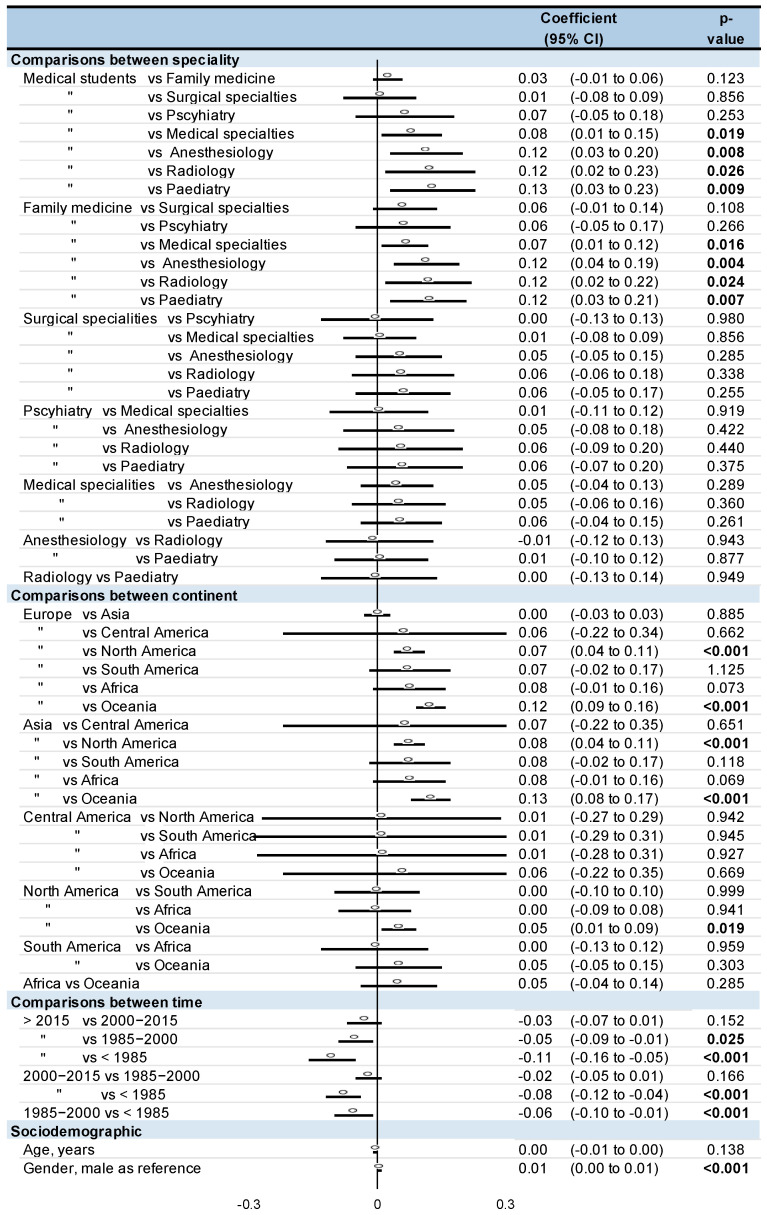
Family practitioners and medical students had a higher smoking prevalence than anesthesiologists (Coefficient 0.12, 95CI 0.04 to 0.19, and 0.12, 0.03 to 0.20, respectively), pediatrics (0.12, 0.03 to 0.21 and 0.13, 0.03 to 0.23), radiologists (0.12, 0.02 to 0.22, and 0.12, 0.02 to 0.23), and other medical specialties (0.07, 0.01 to 0.12, and 0.08, 0.01 to 0.15). For comparisons between continents, physicians in Europe and Asia had a higher smoking prevalence than in North America (0.07, 0.04 to 0.11, and 0.08, 0.04 to 0.11, respectively) and Oceania (0.12, 0.09 to 0.16, and 0.13, 0.08 to 0.17). Smoking prevalence in North America was also significantly higher than in Oceania (0.05, 0.01 to 0.09). Lastly, smoking prevalence was the highest before 1985 (0.06, 0.01 to 0.10 vs. between 1985 to 2000; 0.08, 0.04 to 0.12 vs. between 2000 to 2015; 0.11, 0.05 to 0.16 vs. after to 2015). Moreover, the smoking prevalence between 1985 and 2000 was higher than after 2015 (0.05, 0.01 to 0.09). Male physicians had a higher smoking prevalence than women (0.01, 0.00 to 0.01). Age did not influence smoking prevalence (Figure 4). Insufficient data precluded other meta-regressions.
Figure 4.
Meta-regressions. “means ‘same as’ the line above. Bold represent a stratification.
3.8. Sensitivity Analyses
Funnel plots of meta–analyses analyzing for potential publication bias are presented in Figure 2. Due to the huge heterogeneity (most I2 being >99%), we did not reperform meta–analyses after the exclusion of studies that were not evenly distributed around the base of the funnel. Lastly, we performed all aforementioned analyses on the prevalence of ex-smokers. The prevalence of ex-smokers among physicians was around 23% (95CI 21 to 25%). Psychiatrists also had a high prevalence of ex-smokers (29%, 19 to 40%), followed by other specialties. Contrary to meta-analyses on current smokers, medical students had a low rate of ex-smokers (11%, 6 to 17%). Interestingly, if prevalence of current smokers was similarly high in Europe and Asia (25%), there was greater prevalence of ex-smokers in Europe (25%, 21 to 29%) than in Asia (17, 14 to 20%) (p < 0.001). North America and South America also had a high prevalence of ex-smokers (27%, 20 to 34%; and 26%, 14 to 38%, respectively), whereas Africa had a low prevalence of ex-smokers (8%, 6 to 10%). The prevalence of ex-smokers decreased in similar proportions over time: 31% (26 to 35%) before 1985, 24% (18 to 30%) between 1985 and 2000, 22% (19 to 24%) between 2000 and 2015, and 21% (14 to 28%) after 2015 (Figure 3 and Figure 4).
4. Discussion
The main findings were that the prevalence of smoking among physicians is high, around 21%. Family practitioners and medical students have the highest percentage of smokers and should benefit from targeted preventive strategies. Smoking in physicians is a public health issue that is common, both in developed and developing countries, even if quitting smoking is higher in developed countries. Positively, the prevalence of smoking decreased over time.
4.1. Smoking among Physicians: A Public Health Issue
Surprisingly, prevalence of smoking among physicians is high, which may seem unlikely because they should be an example for their patients and should know the health risks linked to tobacco [21]. This said, even if there is no study determining whether being a physician is a risk factor for smoking compared to the general population, they seem to follow similar trends and are highly concerning [265]. Literature shows that disadvantaged populations smoke more than others [266]. In some way, physicians can also be considered as disadvantaged due to their cumulative risk factors for smoking. They face a huge workload, working over 55 h a week [22]. Stress at work could play a major role in their smoking habits [22]. Overload of stress can even contribute to depressive disorders and high risk of suicides, that are also risk factors of smoking [267,268]. They also work nightshifts [43], disrupting the circadian rhythm that can heighten smoking behavior [269]. Moreover, despite the consequences for themselves, physicians who smoke are less likely to promote quitting smoking for their patients [7,21]. Therefore, there is a need to tackle physicians smoking behavior both for themselves and their patients. Smoking in physicians must be considered as a major public health problem. Alarmingly, even our massive search did not find governmental actions for quitting smoking in physicians. In the research, we found several randomized controlled trials on strategies for smoking cessation in homeless people [270,271], but none in physicians.
4.2. Depending on Specialties
The smoking prevalence was higher among medical students and family practitioners. For medical students, the high prevalence of smoking may be explained due to the stress of hard academic studies [272]. Moreover, medical students can have high risk-taking behaviors such as partying and tobacco consumption [273,274]. The high prevalence among family practitioners might be explained by several putative factors such as workload [22], stress [22], and lack of cohesive teamwork [275]. Workload and stress have been shown in the literature as an important risk factor of smoking [22]. The work environment, such as the lack of cohesive teamwork, is a risk factor of depression and drug use [275], with depression and drug use being linked [60]. Similarly, workload [22] and work stress [22] can also contribute to the high prevalence of smoking in surgical practitioners, who can face legal issues as part of their work [276]. Experiencing judgement in court and repeated trials could promote depression and, in turn, smoking [276]. For psychiatrists, contributing factors of smoking could be the fact that they are routinely faced with traumatic experiences [277], incurable diseases [278], and breaking bad news to patients [278]. Conversely, pediatrics smoked the least, probably because they most often deal with common and curable diseases [279]. Moreover, pediatricians are predominantly women [280]. Although we found a higher prevalence of smoking among women, the literature described a lower rate of smoking among women compare to men in the general population [45,243]. A common characteristic of all specialties is that smoking cessation training during medical studies was poor or not important enough [62,70]. This may contribute to the high prevalence of smoking among physicians. Considering that nearly all physicians will encounter smoking patients, improving smoking cessation training during their studies could help both their patients to quit smoking, as well as the physicians themselves.
4.3. Depending on Continents
Smoking prevalence was not homogeneous between continents. Europe and Asia were continents where the smoking prevalence among physicians was the highest. Conversely, Oceania was the continent where the smoking prevalence among physicians was the lowest. This heterogeneous prevalence was probably in line with tobacco culture [281] and tobacco marketing [281] in many countries. Tobacco culture in Europe was brought by Christopher Colombus in the 16th century [282], firstly as a luxury product [13]. But during the 20th century, tobacco became accessible for all and became a trendy product [13]. Then, in developed countries, tobacco became undesirable [283]. Recent literature shows that tobacco marketing targeted more poor countries [284]. India is the country on the Asian continent with the poorest population, and represents about 17% of the global population [285,286,287]. Moreover, tobacco control is less important in Asia [288]. Studies conducted in Oceania were conducted in rich countries, i.e., Australia and New Zealand, that may be the two countries with the strongest anti-smoking policy [289]. In those two countries, the price of cigarettes is among the most expensive. The increasing taxes aided the decrease in prevalence of smoking, which can be an easy reproducible preventive strategy in other countries [290]. In 2012, Australia was the first country to use plain cigarette packaging [291,292]. A national tobacco campaign in Australia showed the benefits of stopping smoking rather than the negative effects of tobacco [293]. In New Zealand, smoking is prohibited in motor vehicles carrying children under the age of 18 [294]. Finally, except in those two countries that manage smoking, smoking is still a major public health issue worldwide, both in developed and developing countries.
4.4. With a Time Effect
The smoking prevalence among physicians decreased overtime. We showed that physicians’ smoking prevalence has decreased since 1985. The knowledge of the health risks of tobacco during the 1970s changed tobacco from a positive to a negative image [13]. The most recent studies (after 2015) showed that the prevalence of tobacco in physicians continued to decrease. Universally, this decrease was probably related to the tobacco control implemented by the WHO [295], such as a tobacco free-day since 1987 [296]. The WHO Framework Convention on demand and supply reduction [295] probably played a major role in the tobacco consumption decline. Since 2003, European directives limit physicians’ work to 48 h per week [297,298], which may have lessened the stress of physicians. The development of new technologies has encouraged public health advocates to adapt to target a younger cohort, such as the creation of a mobile app for assisting smokers [299], sending emails [300], or sending mobile text messaging [300]. Even if the number of studies on the toxicity of electronic cigarettes remains low, it seems interesting to help with smoking cessation [301]. In Canada, mailed distribution of free nicotine patches seems beneficial, particularly among the financially disadvantaged [302]. In France, nicotine substitutes are reimbursed at 65% by the National Health system as of January 2019 [303]. Our meta-analysis showed that many studies were carried out between 2000 and 2015, probably to assess the effectiveness of tobacco control [295]. Interestingly, preventive strategies sometimes took advantage of context. With the COVID pandemic, Santé Publique France led a digital campaign and special operation to promote the tobacco control [304], based on the fact that tobacco aggravates COVID’s symptoms [305]. That said, the decrease in smoking prevalence could continue in the coming years.
4.5. Other Influencing Variables
Male physicians always smoked more than women, probably because of social habit [306]. There was no significant effect of age on the smoking prevalence of physicians, however, smoking prevalence among the general population decreases with age [307,308]. Insufficient data precluded further analyses on putative influencing factors such as physical activity, BMI, number of hours worked per week, workplace setting, or family status. For example, lower physical activity and higher waist circumference were associated with tobacco consumption [309]. Leisure physical activity of physicians is low [310], which can be limited by their workload [310]. Low levels of physical activity also contribute to burnout [311], that, in turn, increases smoking [22]. No study compared smoking prevalence based on the type of practice (public or private practice). Even if being divorced or separated is a risk factor for smoking in the general population [312,313], the influence of family status in physicians has not been reported. To our knowledge, smoking prevalence of physicians was never compared with smoking prevalence of the general population. Physicians also have protective factors of smoking. For example, their level of study is above the baccalaureate [307], their income is higher than the average population [307], and they are most likely to know tobacco risks [21]. Considering that physicians combine risk and protective factors of smoking, comparisons with the general population may be of particular interest to target appropriate preventive strategies.
4.6. Limitations
Our study has some limitations. We conducted our meta-analyses on only published articles, so our results were, theoretically, exposed to a publication bias. We included only studies reporting physicians’ smoking prevalence and only studies written in English or French, so our results were, theoretically, exposed to a selection bias. Most cross-sectional studies included in our meta-analysis described a bias of self-report. Data were collected by self-administered questionnaire, not always anonymously. Thus, the reporting of smoking might have been underestimated by physicians. Another limitation could be the number of different studies included and the number of physicians included. Although we did not find any double inclusion, it could be possible that some physicians were included twice, creating an overlap that might introduce some bias. Our meta-analysis also had limitations on the definition of smoking. In fact, the definition used to define regular smokers, occasional smokers, or former smokers was different between studies and was rarely detailed. Therefore, the meta-analysis inherited the limitations of the individual studies of which they were comprised: varying quality of studies, multiple variations in study protocols, and evaluation. Comparisons between specialties might suffer from a bias, such as a different number of physicians within each specialty. Moreover, our meta-analysis had a lot of studies with undefined specialties. Similarly, some authors suggested that the medical field was mainly dominated by the male gender and reported a poor status integration of women physicians within the profession [314]. Comparisons between continents or time period might also suffer from a different number of studies within each continent or each period; however, our review provided a massive sample of nearly half a million physicians promoting generalizability of our results.
5. Conclusions
We found that the prevalence of smoking among physicians is high, around 21%. There is an important heterogenicity between specialties, continents, and periods of time. Despite family practitioners and medical students being the heaviest smokers, all physicians should benefit from targeted preventive strategies. Smoking in physicians is a public health issue that is common, both in developed and developing countries, even if quitting smoking is higher in developed countries. Positively, the prevalence of smoking decreased over time, but pursing tobacco control is necessary.
Acknowledgments
To Nathalie Pinol-Domenech for her availability.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph182413328/s1: Figure S1, Funnel plots; Figure S2, Meta-analysis on prevalence of ex-smokers among physicians; Figure S3, Comparisons.
Appendix A. Details for the Search Strategy Used within Each Database
Pubmed
“Smoking”[Mesh:NoExp] OR “smokings”[TW] OR “smoking”[TW] OR “Tobacco Smoking”[MH] OR “Smokers”[MH] OR “smoker”[TW] OR “Smokers”[TW] OR “tobacco”[Title]
AND
“family doctor “[TW] OR “general practitioner”[TW] OR “general practitioners”[TW] OR “practitioner, general”[TW] OR “practitioners, general”[TW] OR “general physician”[TW] OR “general physicians”[TW] OR “physicians, family”[TW] OR “family physicians”[TW] OR “family physician”[TW] OR “physician, family”[TW] OR “physicians, primary care”[TW] OR “physician, primary care”[TW] OR “primary care practitioner “[TW] OR “primary care physician”[TW] OR “primary care physicians”[TW] OR “medical practitioner”[TW] OR “physicians”[MH] OR “physicians”[Title] OR “physician”[Title] OR “doctor”[title] OR “doctors”[title] OR “practitioner” [Title] OR “practitioners”[Title]
AND
“prevalence”[MH] OR “prevalence”[TW] OR “prevalences”[TW] OR “epidemiology”[MH] OR “episode of care”[TW] OR “epidemiological”[TW] OR “epidemiologic”[TW] OR “epidemiology”[TW] OR “epidemiology”[SH] OR “frequency”[TIAB] OR “morbidity”[TIAB] OR “epidemics”[TIAB] OR “outbreaks”[TIAB] OR “endemics”[TIAB] OR “occurrence”[TIAB] OR “surveillance”[TIAB] OR “incidence”[TIAB]
Embase
‘health personnel attitude’/exp AND ‘smoking/exp AND ‘physician’/exp
Cochrane
“smokings”:ti,ab,kw OR “smoking”:ti,ab,kw OR “smoker”:ti,ab,kw OR “Smokers”:ti,ab,kw OR tobacco:ti,ab,kw
AND
“physicians, family”:ti,ab,kw OR “physicians, primary care”:ti,ab,kw OR “family doctor”:ti,ab,kw OR “general practitioner”:ti,ab,kw OR “general practitioners”:ti,ab,kw OR “practitioner, general”:ti,ab,kw OR “practitioners, general”:ti,ab,kw OR “general physician”:ti,ab,kw OR “general physicians”:ti,ab,kw OR “physicians, family”:ti,ab,kw OR “family physicians”:ti,ab,kw OR “family physician”:ti,ab,kw OR “physician, family”:ti,ab,kw OR “physicians, primary care”:ti,ab,kw OR “physician, primary care”:ti,ab,kw OR “primary care practitioner “:ti,ab,kw OR “primary care physician”:ti,ab,kw OR “primary care physicians”:ti,ab,kw OR “physicians”:ti,ab,kw OR “doctor”:ti,ab,kw OR “doctors”:ti,ab,kw OR “medical practitioner”ti,ab,kw OR “physicians”:ti,ab,kw OR “physicians”:ti OR “physician”:ti OR “doctor”:ti OR “doctors”:ti OR “practitioners”:ti OR “practitioner”:ti
AND
“prevalence”:ti,ab,kw OR “prevalences”:ti,ab,kw OR “epidemiology”:ti,ab,kw OR “episode of care”:ti,ab,kw OR “epidemiological”:ti,ab,kw OR “epidemiologic”:ti,ab,kw OR “frequency”:ti,ab,kw OR “morbidity”:ti,ab,kw OR “epidemics”:ti,ab,kw OR “outbreaks”:ti,ab,kw OR “endemics”:ti,ab,kw OR “occurrence”:ti,ab,kw OR “surveillance”:ti,ab,kw
Table A1.
Methodological assessment of studies using STROBE and CONSORT criteria.
| STROBE | ||||||
| Total | Abstract | Methods | Results | Discussion | ||
| Score | Introduction | |||||
| Aaro 1977 | 60 | 100 | 36 | 60 | 75 | |
| Abdullah 2006 | 59 | 100 | 69 | 30 | 75 | |
| Aboyans 2009 | 56 | 100 | 31 | 50 | 100 | |
| Akvardar 2004 | 53 | 100 | 38 | 40 | 75 | |
| Al Alwan 2013 | 50 | 100 | 31 | 40 | 100 | |
| Alarjan 2015 | 53 | 100 | 46 | 40 | 75 | |
| al-Khateeb 1990 | 38 | 100 | 31 | 30 | 25 | |
| Allan 1976 | 13 | 0 | NA | 20 | NA | |
| Al-Lawati 2009 | 44 | 100 | 23 | 20 | 100 | |
| Al Shahrani 2021 | 69 | 100 | 69 | 60 | 75 | |
| An 2004 | 66 | 100 | 69 | 50 | 75 | |
| Amara 2008 | 53 | 100 | 38 | 40 | 100 | |
| Amte 2015 | 56 | 100 | 38 | 50 | 100 | |
| Arnetz 1988 | 66 | 100 | 54 | 60 | 75 | |
| Aryayev 2014 | 48 | 100 | 31 | 33 | 100 | |
| Baltaci 2014 | 53 | 100 | 38 | 40 | 75 | |
| Baptista 1993 | 44 | 100 | 31 | 30 | 100 | |
| Barengo 2004 | 45 | 100 | 42 | 33 | 50 | |
| Barengo 2005 | 44 | 100 | 23 | 30 | 100 | |
| Barnoya 2002 | 28 | 50 | 0 | 20 | 100 | |
| Basnyat 2000 | 34 | 100 | 10 | 20 | 100 | |
| Basu 2011 | 47 | 100 | 23 | 40 | 100 | |
| Behbehani 2004 | 50 | 100 | 54 | 20 | 75 | |
| Belkić 2007 | 59 | 100 | 38 | 50 | 100 | |
| Belkić 2012 | 56 | 100 | 54 | 30 | 100 | |
| Bener 1993 | 38 | 100 | 15 | 30 | 50 | |
| Borgan 2014 | 47 | 100 | 31 | 20 | 100 | |
| Bortz 1992 | 29 | 75 | 10 | 30 | 50 | |
| Bostan 2015 | 56 | 100 | 46 | 40 | 75 | |
| Bourke 1972 | 41 | 100 | 23 | 30 | 50 | |
| Braun 2004 | 41 | 100 | 31 | 30 | 25 | |
| Brenner 1996 | 56 | 100 | 46 | 40 | 100 | |
| Brink 1994 | 53 | 100 | 46 | 50 | 50 | |
| Brotonsc 2005 | 53 | 100 | 46 | 30 | 75 | |
| Burgess 1970 | 19 | 50 | 10 | 20 | 25 | |
| Burgess 1978 | 28 | 75 | 23 | 20 | 50 | |
| Cao 2011 | 41 | 50 | 25 | 44 | 75 | |
| Carlos 2020 | 70 | 100 | 62 | 60 | 75 | |
| Ceraso 2009 | 59 | 100 | 46 | 40 | 100 | |
| Chaudhry 2009 | 32 | 100 | 17 | 20 | 50 | |
| Cheng 1990 | 45 | 100 | 25 | 40 | 75 | |
| Coe 1971 | 34 | 50 | 15 | 30 | 75 | |
| Cofta 2008 | 50 | 100 | 38 | 30 | 75 | |
| Das 2013 | 53 | 100 | 46 | 30 | 75 | |
| Davies 1989 | 47 | 75 | 45 | 40 | 50 | |
| De Col 2010 | 59 | 100 | 54 | 50 | 75 | |
| Dekker 1993 | 44 | 100 | 31 | 40 | 50 | |
| De Oliveira 2013 | 56 | 100 | 46 | 40 | 100 | |
| Desalu 2009 | 47 | 100 | 46 | 30 | 50 | |
| Djalalinia 2011 | 47 | 100 | 46 | 20 | 75 | |
| Dodds 1979 | 38 | 50 | 38 | 43 | 50 | |
| Doll 1954 | 41 | 100 | 31 | 20 | 75 | |
| Doll 1964 | 44 | 100 | 38 | 30 | 50 | |
| Doll 1994 | 50 | 100 | 31 | 50 | 75 | |
| Doll 2004 | 53 | 100 | 31 | 50 | 75 | |
| Easton 2001 | 78 | 100 | 77 | 50 | 100 | |
| Easton 2001 | 61 | 100 | 54 | 56 | 75 | |
| Edwards 2008 | 63 | 75 | 46 | 70 | 75 | |
| Edwards 2018 | 66 | 75 | 46 | 70 | 100 | |
| Fadhil 2007 | 63 | 100 | 55 | 50 | 75 | |
| Fanello 1990 | 56 | 100 | 54 | 50 | 50 | |
| Fathi 2016 | 56 | 100 | 46 | 30 | 100 | |
| Fowler 1989 | 69 | 100 | 77 | 50 | 75 | |
| Franceschi 1986 | 39 | 50 | 31 | 50 | 25 | |
| Frank 1998 | 75 | 100 | 77 | 60 | 100 | |
| Frank 2009 | 63 | 75 | 54 | 50 | 100 | |
| Freour 2011 | 50 | 100 | 38 | 30 | 100 | |
| Garfinkel 1976 | 27 | 50 | 23 | 20 | 25 | |
| Grossman 1999 | 56 | 100 | 46 | 40 | 75 | |
| Gunes 2005 | 60 | 100 | 46 | 50 | 100 | |
| Gupta 2013 | 50 | 100 | 46 | 30 | 75 | |
| Hallett 1983 | 28 | 75 | 10 | 30 | 50 | |
| Hamadeh 1999 | 53 | 100 | 38 | 40 | 75 | |
| Han Zao Li 2008 | 56 | 100 | 46 | 40 | 100 | |
| Hay 1976 | 41 | 100 | 15 | 40 | 75 | |
| Hay 1998 | 53 | 75 | 31 | 60 | 75 | |
| Heloma 1998 | 56 | 100 | 46 | 40 | 75 | |
| Hensrud 1993 | 53 | 100 | 38 | 50 | 75 | |
| Hepburn 2000 | 59 | 100 | 62 | 40 | 75 | |
| Heponiemi 2008 | 59 | 100 | 46 | 40 | 100 | |
| Hidalgo 2016 | 56 | 100 | 46 | 40 | 75 | |
| Hill 1997 | 50 | 100 | 54 | 30 | 50 | |
| Hodgetts 2004 | 56 | 100 | 38 | 50 | 100 | |
| Hoseainrezae 2013 | 44 | 100 | 38 | 30 | 50 | |
| Huang 2013 | 63 | 100 | 46 | 50 | 100 | |
| Hughes 1991 | 63 | 100 | 64 | 40 | 75 | |
| Hughes 1992 | 63 | 75 | 69 | 40 | 75 | |
| Hughes 1999 | 50 | 100 | 46 | 20 | 100 | |
| Hung 2013 | 59 | 100 | 46 | 50 | 100 | |
| Hussain 1993 | 41 | 100 | 38 | 30 | 25 | |
| Içli 1992 | 34 | 100 | 31 | 20 | 25 | |
| Innos 2002 | 52 | 100 | 38 | 44 | 75 | |
| Jacot Sadowski 2009 | 73 | 100 | 82 | 50 | 75 | |
| Jiang 2007 | 63 | 100 | 69 | 50 | 50 | |
| Jiménez-Ruiz 2015 | 56 | 100 | 38 | 40 | 100 | |
| Jingi 2015 | 47 | 100 | 38 | 30 | 75 | |
| John 2003 | 41 | 100 | 31 | 10 | 75 | |
| Joossens 1987 | 38 | 75 | 31 | 40 | 25 | |
| Josseran 2000 | 47 | 100 | 46 | 10 | 100 | |
| Josseran 2005 | 59 | 100 | 46 | 40 | 100 | |
| Julião 2013 | 53 | 100 | 38 | 40 | 100 | |
| Kaetsu 2002 | 63 | 100 | 45 | 70 | 75 | |
| Kaetsu 2002 | 78 | 100 | 77 | 60 | 75 | |
| Kai 2008 | 59 | 100 | 69 | 30 | 75 | |
| Kaneita 2010 | 78 | 100 | 77 | 60 | 100 | |
| Kawahara 2000 | 70 | 100 | 64 | 50 | 100 | |
| Kawakami 1997 | 48 | 75 | 45 | 22 | 75 | |
| Kawane 1993 | 50 | 0 | NA | NA | NA | |
| Kono 1995 | 78 | 100 | 85 | 60 | 100 | |
| Kotz 2007 | 78 | 100 | 77 | 60 | 100 | |
| Lam 2011 | 88 | 100 | 92 | 70 | 100 | |
| La Vecchia 2000 | 20 | 100 | 15 | 20 | NA | |
| Lefcoe 1970 | 52 | 100 | 55 | 22 | 75 | |
| Legnini 1987 | 50 | 100 | 46 | 30 | 75 | |
| Lindfors 2009 | 66 | 100 | 69 | 40 | 100 | |
| Linn 1986 | 56 | 100 | 54 | 50 | 50 | |
| Lipp 1972 | 44 | 100 | 31 | 20 | 100 | |
| Lipp 1972 | 31 | 75 | 15 | 20 | 75 | |
| Magee 2017 | 63 | 100 | 62 | 30 | 100 | |
| Malik 2010 | 47 | 100 | 46 | 30 | 50 | |
| Manson 2000 | 63 | 100 | 62 | 40 | 100 | |
| Mappin-Kasirer 2020 | 63 | 100 | 62 | 50 | 75 | |
| Marakoğlu 2006 | 47 | 100 | 38 | 30 | 75 | |
| Márk 1998 | 53 | 100 | 46 | 30 | 100 | |
| Mathavan 2009 | 63 | 100 | 62 | 40 | 75 | |
| McAuliffe 1984 | 41 | 100 | 31 | 30 | 50 | |
| McEwen 2001 | 56 | 100 | 46 | 50 | 75 | |
| McGrady 2007 | 63 | 100 | 46 | 50 | 100 | |
| Mejia 2011 | 54 | 100 | 50 | 33 | 75 | |
| Merrill 2006 | 56 | 100 | 62 | 20 | 100 | |
| Meshefedjian 2010 | 59 | 100 | 54 | 40 | 100 | |
| Mikalauskas 2012 | 63 | 100 | 54 | 50 | 100 | |
| Misra 2004 | 63 | 100 | 62 | 50 | 75 | |
| Miwa 1995 | 50 | 100 | 46 | 30 | 75 | |
| Mohan 2006 | 50 | 100 | 46 | 40 | 50 | |
| Mohseni-Bandpei 2011 | 63 | 100 | 62 | 30 | 100 | |
| Moreno 2006 | 24 | 100 | 15 | 30 | 25 | |
| Mostafa 2017 | 63 | 100 | 62 | 40 | 100 | |
| Movsisyan 2019 | 56 | 100 | 62 | 40 | 50 | |
| Mubeen 2008 | 59 | 100 | 46 | 40 | 100 | |
| Naji 2006 | 34 | 100 | 15 | 30 | 50 | |
| Nakládalová 2005 | 50 | 100 | 38 | 40 | 50 | |
| Nardini 1998 | 53 | 100 | 54 | 30 | 50 | |
| Nawaz 2007 | 56 | 100 | 62 | 40 | 50 | |
| Nawaz 2008 | 44 | 100 | 31 | 30 | 50 | |
| Ndiaye 2001 | 56 | 100 | 54 | 50 | 50 | |
| Nelson 1994 | 65 | 75 | 77 | 22 | 100 | |
| Ng 2007 | 61 | 100 | 62 | 56 | 50 | |
| Nollen 2004 | 53 | 100 | 54 | 30 | 75 | |
| Nutbeam 1990 | 53 | 100 | 46 | 40 | 50 | |
| Obeidat 2017 | 66 | 100 | 54 | 50 | 100 | |
| Öztürk 2012 | 59 | 100 | 69 | 50 | 25 | |
| O’Cathail 2013 | 63 | 100 | 62 | 40 | 100 | |
| Ohida 2001 | 63 | 100 | 54 | 40 | 100 | |
| O’Keeffe 2019 | 75 | 100 | 69 | 60 | 100 | |
| Pärna 2005 A | 69 | 100 | 69 | 40 | 100 | |
| Pärna 2005 B | 66 | 100 | 62 | 40 | 100 | |
| Pärna 2017 | 59 | 100 | 46 | 40 | 100 | |
| Perrin 2006 | 63 | 100 | 62 | 40 | 100 | |
| Peykari 2010 | 59 | 100 | 46 | 40 | 100 | |
| Phillips 1968 | 41 | 100 | 31 | 30 | 50 | |
| Pillay 2020 | 47 | 50 | 31 | 50 | 50 | |
| Pipe 2009 | 59 | 100 | 54 | 30 | 100 | |
| Piryani 2004 | 34 | 100 | 15 | 30 | 50 | |
| Pizzo 2003 | 47 | 100 | 42 | 30 | 50 | |
| Poanta 2006 | 73 | 75 | 77 | 50 | 100 | |
| Põld 2017 | 72 | 100 | 69 | 50 | 100 | |
| Põld 2020 | 94 | 100 | 92 | 90 | 100 | |
| Polyzos 1995 | 38 | 50 | 38 | 40 | 25 | |
| Power 1999 | 66 | 100 | 77 | 40 | 75 | |
| Ramachandran 2008 | 70 | 75 | 73 | 50 | 75 | |
| Ranchal 2018 | 74 | 100 | 77 | 56 | 100 | |
| Rankin 1975 | 44 | 100 | 8 | 50 | 75 | |
| Ravara 2014 | 55 | 100 | 31 | 60 | 75 | |
| Reile 2018 | 74 | 100 | 46 | 58 | 100 | |
| Roche 1995 | 66 | 100 | 62 | 60 | 75 | |
| Roche 1996 | 69 | 100 | 77 | 60 | 50 | |
| Rurik 2008 | 47 | 100 | 31 | 40 | 75 | |
| Rurik 2014 | 41 | 100 | 31 | 30 | 50 | |
| Sachs 1983 | 44 | 50 | 67 | 44 | 0 | |
| Saeed 1991 | 53 | 75 | 38 | 50 | 75 | |
| Saeys 2014 | 81 | 100 | 77 | 70 | 100 | |
| Salgado 2014 | 72 | 75 | 69 | 80 | 100 | |
| Samuels 1997 | 50 | 75 | 23 | 50 | 100 | |
| Schnoll 2006 | 59 | 100 | 62 | 50 | 50 | |
| Scott 1992 | 41 | 100 | 23 | 30 | 75 | |
| Sebo 2007 | 65 | 100 | 62 | 44 | 100 | |
| Seller 1983 | 42 | 50 | 44 | 50 | 25 | |
| Senior 1982 | 56 | 100 | 62 | 30 | 75 | |
| Sharma 1988 | 24 | 50 | 15 | 17 | 100 | |
| Shkedy 2013 | 59 | 100 | 36 | 44 | 100 | |
| Shi 2010 | 61 | 100 | 67 | 30 | 100 | |
| Shin 2012 | 72 | 100 | 77 | 50 | 100 | |
| Shishani 2008 | 75 | 100 | 85 | 40 | 100 | |
| Shishani 2011 | 75 | 75 | 85 | 60 | 75 | |
| Siddiqui 2001 | 50 | 100 | 46 | 30 | 75 | |
| Singh 1981 | 50 | 100 | 38 | 30 | 75 | |
| Smith 2006 | 67 | 100 | 64 | 50 | 75 | |
| Smith 2007 | 50 | 67 | 50 | 33 | NA | |
| Sotiropoulos 2007 | 70 | 100 | 55 | 80 | 75 | |
| Squier 2006 | 63 | 100 | 54 | 50 | 100 | |
| Steinberg 2007 | 50 | 100 | 46 | 30 | 75 | |
| Stuyt 2009 | 55 | 75 | 31 | 56 | 100 | |
| Sundquist 1999 | 72 | 100 | 69 | 50 | 100 | |
| Svärdsudd 2002 | 69 | 100 | 77 | 50 | 75 | |
| Tapia-Conyer 1997 | 66 | 100 | 62 | 50 | 75 | |
| Tee 2007 | 69 | 100 | 62 | 60 | 75 | |
| Tessier 1996 | 53 | 100 | 38 | 30 | 100 | |
| Thankappan 2008 | 56 | 100 | 62 | 40 | 50 | |
| Thomas 1986 | 66 | 100 | 54 | 50 | 100 | |
| Thomas 1997 | 44 | 100 | 38 | 30 | 50 | |
| Tomson 2003 | 56 | 100 | 46 | 30 | 100 | |
| Tong 2010 | 66 | 100 | 62 | 40 | 100 | |
| Torre 2005 | 53 | 100 | 38 | 30 | 100 | |
| Tosun 2016 | 53 | 100 | 38 | 30 | 100 | |
| Trédaniel 1993 | 50 | 100 | 54 | 30 | 50 | |
| Ulbricht 2009 | 66 | 100 | 54 | 50 | 100 | |
| Unal 2017 | 63 | 100 | 62 | 40 | 75 | |
| Underner 2004 | 63 | 50 | 62 | 50 | 100 | |
| Underner 2006 | 63 | 75 | 62 | 50 | 75 | |
| Uysal 2007 | 69 | 75 | 77 | 60 | 75 | |
| Vanderhoek 2013 | 81 | 100 | 77 | 70 | 100 | |
| Vanphanom 2011 | 73 | 100 | 85 | 25 | 100 | |
| Varona 2005 | 42 | 100 | 30 | 57 | 25 | |
| Viegas 2007 | 63 | 75 | 69 | 38 | 75 | |
| Voigt 2009 | 63 | 75 | 62 | 56 | 75 | |
| Waalkens 1992 | 57 | 75 | 42 | 56 | 75 | |
| Wada 2007 | 66 | 100 | 77 | 40 | 50 | |
| Wada 2011 | 50 | 100 | 38 | 40 | 75 | |
| Wang 2021 | 59 | 75 | 69 | 50 | 50 | |
| Wilf Miron 2019 | 59 | 100 | 54 | 50 | 50 | |
| Waillaing 2003 | 77 | 100 | 92 | 50 | 100 | |
| Wilson 2020 | 69 | 100 | 69 | 60 | 75 | |
| Wyshak 1980 | 34 | 50 | 38 | 22 | 25 | |
| Yaacob 1993 | 69 | 100 | 62 | 50 | 100 | |
| Yan 2008 | 87 | 100 | 100 | 67 | 75 | |
| Young 1997 | 56 | 50 | NA | 50 | NA | |
| Zabadi 2018 | 81 | 100 | 85 | 56 | 100 | |
| Zanetti 1998 | 47 | 75 | 54 | 30 | 50 | |
| Zhang 2012 | 56 | 100 | 69 | 40 | 25 | |
| Zhang 2015 | 70 | 67 | NA | 67 | NA | |
| Zhou 2010 | 35 | 75 | 50 | 60 | 100 | |
| Zinonos 2016 | 100 | 100 | 100 | 100 | 100 | |
| Zylbersztejn 2015 | 78 | 100 | 85 | 50 | 100 | |
| CONSORT | ||||||
| Total | Abstract | Methods | Results | Discussion | Other | |
| Score | Introduction | |||||
| Glavas 2003 | 73 | 100 | 59 | 70 | 67 | 33 |
| Saadat 2012 | 76 | 100 | 59 | 80 | 100 | 33 |
Table A2.
Methodological assessment of studies using NOS criteria. NOS for cross-sectional studies.
| Selection Bias |
Comparability Bias |
Outcome Bias |
|||||
|---|---|---|---|---|---|---|---|

|

|

|
|||||
| Sample representativeness | Sample size | Representativeness | Ascertainment of the exposure | Comparability | Assessment of the outcome | Statistical test | |
| Aaro 1977 |

|

|

|

|

|

|

|
| Abdullah 2006 |

|

|

|

|

|

|

|
| Aboyans 2009 |

|

|

|

|

|

|

|
| Akvardar 2004 |

|

|

|


|

|

|

|
| Al Alwan 2013 |

|

|

|

|

|

|

|
| Alarjan 2015 |

|

|

|

|

|

|

|
| al-Khateeb 1990 |

|

|

|

|

|

|

|
| Allan 1976 |

|

|

|

|

|

|

|
| Al-Lawati 2009 |

|

|

|


|

|

|

|
| Al Shahrani 2021 |

|

|

|

|

|

|

|
| Amara 2008 |

|

|

|

|

|

|

|
| Amte 2015 |

|

|

|


|

|

|

|
| An 2004 |

|

|

|

|

|

|

|
| Arnetz 1988 |

|

|

|

|

|

|

|
| Aryayev 2014 |

|

|

|

|

|

|

|
| Baltaci 2014 |

|

|

|

|

|

|

|
| Baptista 1993 |

|

|

|

|

|

|

|
| Barengo 2004 |

|

|

|

|

|

|

|
| Barengo 2005 |

|

|

|

|

|

|

|
| Barnoya 2002 |

|

|

|

|

|

|

|
| Basnyat 2000 |

|

|

|

|

|

|

|
| Basu 2011 |

|

|

|

|

|

|

|
| Behbehani 2004 |

|

|

|

|

|

|

|
| Belkić 2007 |

|

|

|

|

|

|

|
| Belkić 2012 |

|

|

|


|

|

|

|
| Bener 1993 |

|

|

|

|

|

|

|
| Borgan 2014 |

|

|

|

|

|

|

|
| Bortz 1992 |

|

|

|

|

|

|

|
| Bostan 2015 |

|

|

|

|

|

|

|
| Bourke 1972 |

|

|

|

|

|

|

|
| Braun 2004 |

|

|

|

|

|

|

|
| Brenner 1996 |

|

|

|

|

|

|

|
| Brink 1994 |

|

|

|

|

|

|

|
| Brotonsc 2005 |

|

|

|

|

|

|

|
| Burgess 1970 |

|

|

|

|

|

|

|
| Burgess 1978 |

|

|

|

|

|

|

|
| Carlos 2020 |

|

|

|

|

|

|

|
| Ceraso 2009 |

|

|

|

|

|

|

|
| Chaudhry 2009 |

|

|

|

|

|

|

|
| Cheng 1990 |

|

|

|

|

|

|

|
| Coe 1971 |

|

|

|

|

|

|

|
| Cofta 2008 |

|

|

|

|

|

|

|
| Das 2013 |

|

|

|

|

|

|

|
| Davies 1989 |

|

|

|

|

|

|

|
| De Col 2010 |

|

|

|

|

|

|

|
| Dekker 1993 |

|

|

|

|

|

|

|
| De Oliveira 2013 |

|

|

|

|

|

|

|
| Desalu 2009 |

|

|

|

|

|

|

|
| Djalalinia 2011 |

|

|

|


|

|

|

|
| Dodds 1979 |

|

|

|

|

|

|

|
| Doll 1954 |

|

|

|

|

|

|

|
| Doll 1964 |

|

|

|

|

|

|

|
| Doll 1994 |

|

|

|

|

|

|

|
| Doll 2004 |

|

|

|

|

|

|

|
| Easton 2001 |

|

|

|

|

|

|

|
| Easton 2001 |

|

|

|

|

|

|

|
| Edwards 2008 |

|

|

|


|

|

|

|
| Edwards 2018 |

|

|

|

|

|

|

|
| Fadhil 2007 |

|

|

|

|

|

|

|
| Fanello 1990 |

|

|

|

|

|

|

|
| Fathi 2016 |

|

|

|


|

|

|

|
| Fowler 1989 |

|

|

|

|

|

|

|
| Franceschi 1986 |

|

|

|

|

|

|

|
| Frank 1998 |

|


|

|


|

|

|

|
| Frank 2009 |

|

|

|


|

|

|

|
| Freour 2011 |

|

|

|

|

|

|

|
| Garfinkel 1976 |

|

|

|

|

|

|

|
| Grossman 1999 |

|

|

|

|

|

|

|
| Gunes 2005 |

|

|

|


|

|

|

|
| Gupta 2013 |

|

|

|

|

|

|

|
| Hallett 1983 |

|

|

|

|

|

|

|
| Hamadeh 1999 |

|

|

|


|

|

|

|
| Han Zao Li 2008 |

|

|

|

|

|

|

|
| Hay 1976 |

|

|

|

|

|

|

|
| Hay 1998 |

|

|

|

|

|

|

|
| Heloma 1998 |

|

|

|

|

|

|

|
| Hensrud 1993 |

|

|

|

|

|

|

|
| Hepburn 2000 |

|

|

|

|

|

|

|
| Heponiemi 2008 |

|

|

|

|

|

|

|
| Hidalgo 2016 |

|

|

|

|

|

|

|
| Hill 1997 |

|

|

|

|

|

|

|
| Hodgetts 2004 |

|

|

|

|

|

|

|
| Hoseainrezae 2013 |

|

|

|

|

|

|

|
| Huang 2013 |

|

|

|

|

|

|

|
| Hughes 1991 |

|

|

|

|

|

|

|
| Hughes 1992 |

|

|

|


|

|

|

|
| Hughes 1999 |

|

|

|

|

|

|

|
| Hung 2013 |

|

|

|

|


|

|

|
| Hussain 1993 |

|

|

|

|

|

|

|
| Içli 1992 |

|

|

|

|

|

|

|
| Jacot Sadowski 2009 |

|

|

|

|

|

|

|
| Jiang 2007 |

|

|

|


|

|

|

|
| Jiménez-Ruiz 2015 |

|

|

|

|

|

|

|
| Jingi 2015 |

|

|

|

|

|

|

|
| John 2003 |

|

|

|

|

|

|

|
| Joossens 1987 |

|

|

|

|

|

|

|
| Josseran 2000 |

|

|

|

|

|

|

|
| Josseran 2005 |

|

|

|

|

|

|

|
| Julião 2013 |

|

|

|

|

|

|

|
| Kaetsu 2002 |

|

|

|

|

|

|

|
| Kai 2008 |

|

|

|

|

|

|

|
| Kaneita 2010 |

|

|

|


|

|

|

|
| Kawahara 2000 |

|

|

|

|

|

|

|
| Kawakami 1997 |

|

|

|

|

|

|

|
| Kawane 1993 |

|

|

|

|

|

|

|
| Kotz 2007 |

|

|

|

|

|

|

|
| Lam 2011 |

|

|

|


|

|

|

|
| La Vecchia 2000 |

|

|

|

|

|

|

|
| Lefcoe 1970 |

|

|

|

|

|

|

|
| Legnini 1987 |

|

|

|

|

|

|

|
| Lindfors 2009 |

|

|

|

|

|

|

|
| Linn 1986 |

|

|

|

|

|

|

|
| Lipp 1972 |

|

|

|

|

|

|

|
| Lipp 1972 |

|

|

|

|

|

|

|
| Magee 2017 |

|

|

|

|

|

|

|
| Malik 2010 |

|

|

|


|

|

|

|
| Marakoğlu 2006 |

|

|

|


|

|

|

|
| Márk 1998 |

|

|

|

|

|

|

|
| Mathavan 2009 |

|

|

|


|

|

|

|
| McAuliffe 1984 |

|

|

|

|

|

|

|
| McEwen |

|

|

|

|

|

|

|
| McGrady 2007 |

|

|

|

|

|

|

|
| Mejia 2011 |

|

|

|

|

|

|

|
| Merrill 2006 |

|

|

|


|

|

|

|
| Meshefedjian 2010 |

|

|

|

|

|

|

|
| Mikalauskas 2012 |

|

|

|

|

|

|

|
| Misra 2004 |

|

|

|

|

|

|

|
| Miwa 1995 |

|

|

|

|

|

|

|
| Mohan 2006 |

|

|

|

|

|

|

|
| Mohseni-Bandpei 2011 |

|

|

|

|

|

|

|
| Moreno 2006 |

|

|

|

|

|

|

|
| Mostafa 2017 |

|

|

|

|

|

|

|
| Movsisyan 2019 |

|

|

|

|

|

|

|
| Mubeen 2008 |

|

|

|

|

|

|

|
| Naji 2006 |

|

|

|

|

|

|

|
| Nakládalová 2005 |

|

|

|

|

|

|

|
| Nardini 1998 |

|

|

|

|

|

|

|
| Nawaz 2007 |

|

|

|


|

|

|

|
| Nawaz 2008 |

|

|

|

|

|

|

|
| Ndiaye 2001 |

|

|

|

|

|

|

|
| Nelson 1994 |

|

|

|


|

|

|

|
| Ng 2007 |

|

|

|

|

|

|

|
| Nollen 2004 |

|

|

|

|

|

|

|
| Nutbeam 1990 |

|

|

|

|

|

|

|
| Obeidat 2017 |

|

|

|

|

|

|

|
| Öztürk 2012 |

|

|

|

|

|

|

|
| O’Cathail 2013 |

|

|

|

|

|

|

|
| Ohida 2001 |

|

|

|

|

|

|

|
| O’Keeffe 2019 |

|

|

|

|

|

|

|
| Pärna 2005 A |

|

|

|


|

|

|

|
| Pärna 2005 B |

|

|

|

|

|

|

|
| Pärna 2017 |

|

|

|

|

|

|

|
| Perrin 2006 |

|

|

|


|

|

|

|
| Peykari 2010 |

|

|

|


|

|

|

|
| Phillips 1968 |

|

|

|

|

|

|

|
| Pillay 2020 |

|

|

|

|

|

|

|
| Pipe 2009 |

|

|

|

|

|

|

|
| Piryani 2004 |

|

|

|

|

|

|

|
| Pizzo 2003 |

|

|

|

|

|

|

|
| Poanta 2006 |

|

|

|


|

|

|

|
| Põld 2017 |

|

|

|


|

|

|

|
| Põld 2020 |

|

|

|

|

|

|

|
| Polyzos 1995 |

|

|

|

|

|

|

|
| Power 1999 |

|

|

|

|

|

|

|
| Ramachandran 2008 |

|

|

|


|


|

|

|
| Ranchal 2018 |

|

|

|


|


|

|

|
| Rankin 1975 |

|

|

|

|

|

|

|
| Ravara 2014 |

|

|

|

|


|

|

|
| Reile 2018 |

|

|

|

|

|

|

|
| Roche 1995 |

|

|

|

|

|

|

|
| Roche 1996 |

|

|

|

|

|

|

|
| Sachs 1983 |

|

|

|

|

|

|

|
| Saeed 1991 |

|

|

|

|

|

|

|
| Saeys 2014 |

|

|

|


|

|

|

|
| Salgado 2014 |

|

|

|

|

|

|

|
| Samuels 1997 |

|

|

|

|

|

|

|
| Schnoll 2006 |

|

|

|

|

|

|

|
| Scott 1992 |

|

|

|

|

|

|

|
| Sebo 2007 |

|

|

|


|

|

|

|
| Seiler 1983 |

|

|

|

|

|

|

|
| Senior 1982 |

|

|

|

|

|

|

|
| Sharma 1988 |

|

|

|

|

|

|

|
| Shkedy 2013 |

|

|

|

|


|

|

|
| Shi 2010 |

|

|

|

|

|

|

|
| Shin 2012 |

|

|

|

|

|

|

|
| Shishani 2008 |

|

|

|


|


|

|

|
| Shishani 2011 |

|

|

|


|

|

|

|
| Siddiqui 2001 |

|

|

|

|

|

|

|
| Singh 1981 |

|

|

|

|

|

|

|
| Smith 2006 |

|

|

|


|

|

|

|
| Smith 2007 |

|

|

|

|

|

|

|
| Sotiropoulos 2007 |

|

|

|

|


|

|

|
| Squier 2006 |

|

|

|


|

|

|

|
| Steinberg 2007 |

|

|

|

|

|

|

|
| Stuyt 2009 |

|

|

|

|

|

|

|
| Sundquist 1999 |

|

|

|


|

|

|

|
| Tapia-Conyer 1997 |

|

|

|


|

|

|

|
| Tee 2007 |

|

|

|


|

|

|

|
| Tessier 1996 |

|

|

|


|

|

|

|
| Thankappan 2008 |

|

|

|

|

|

|

|
| Thomas 1986 |

|

|

|


|

|

|

|
| Tomson 2003 |

|

|

|

|

|

|

|
| Tong 2010 |

|

|

|


|

|

|

|
| Tosun 2016 |

|

|

|

|

|

|

|
| Trédaniel 1993 |

|

|

|

|

|

|

|
| Ulbricht 2009 |

|

|

|


|

|

|

|
| Underner 2004 |

|

|

|

|

|

|


|
| Underner 2006 |

|

|

|

|


|

|


|
| Uysal 2007 |

|

|

|

|

|

|

|
| Vanderhoek 2013 |

|

|

|


|

|

|

|
| Vanphanom 2011 |

|

|

|

|

|

|

|
| Varona 2005 |

|

|

|

|

|

|

|
| Viegas 2007 |

|

|

|

|

|

|

|
| Voigt 2009 |

|

|

|


|

|

|

|
| Waalkens 1992 |

|

|

|

|

|

|

|
| Wada 2007 |

|

|

|

|

|

|

|
| Wada 2011 |

|

|

|

|

|

|

|
| Wang 2021 |

|

|

|

|

|

|

|
| Wilf Miron 2019 |

|

|

|

|

|

|

|
| Willaing 2003 |

|

|

|

|

|

|

|
| Wilson 2020 |

|

|

|

|

|

|

|
| Wyshak 1980 |

|

|

|

|

|

|

|
| Yaacob 1993 |

|

|

|

|


|

|

|
| Yan 2008 |

|

|

|


|

|


|

|
| Young 1997 |

|

|

|

|

|

|

|
| Zabadi 2018 |

|

|

|

|


|


|

|
| Zanetti 1998 |

|

|

|

|

|

|

|
| Zhang 2012 |

|

|

|

|

|

|

|
| Zhang 2015 |

|

|

|

|

|

|

|
| Zhou 2010 |

|

|

|


|

|

|

|
| Zinonos 2016 |

|

|

|

|

|

|

|
| Zylbersztejn 2015 |

|

|

|

|

|

|

|
Appendix B
Table A3.
NOS for cohort studies.
| Selection Bias |
Comparability Bias |
Outcome Bias |
||||||
|---|---|---|---|---|---|---|---|---|

|

|

|
||||||
| Representativeness of the exposed | Selection of the non-exposed | Ascertainment of the exposure | Demonstration that outcome of interest was not present at start of study | Comparability | Assessment of the outcome | Follow-up long | Adequacy of follow-up | |
| Cao 2011 |

|

|

|

|

|

|

|

|
| Innos 2002 |

|

|

|

|

|

|

|

|
| Kaetsu 2002 |

|

|

|

|

|

|

|

|
| Kono 1985 |

|

|

|

|

|

|

|

|
| Manson 2000 |

|

|

|

|


|

|

|

|
| Mappin-Kasirer 2020 |

|

|

|

|

|

|

|

|
| Rurik 2008 |

|

|

|

|


|

|

|

|
| Rurik 2014 |

|

|

|

|


|

|

|

|
| Svärdsudd 2002 |

|

|

|

|


|

|

|

|
| Thomas 1997 |

|

|

|

|

|

|

|

|
| Torre 2005 |

|

|

|

|

|

|

|

|
| Unal 2017 |

|

|

|

|

|

|

|

|
Author Contributions
Conceptualization, F.D.; methodology, F.D.; formal analysis, F.D.; investigation, A.T. and A.B. (Amanda Benson); data curation, A.T. and A.B. (Amanda Benson); writing—original draft preparation, A.B. (Anaïs Besson) and A.T.; writing—review and editing, V.F., G.B., C.L., V.N., F.D. and J.-B.B.-M.; visualization, F.D.; supervision, F.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
All relevant data are within the paper.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization . WHO Report on the Global Tobacco Epidemic, 2017: Monitoring Tobacco Use and Prevention Policies. WHO; Geneva, Switzerland: 2017. Bloomberg Philanthropies. [Google Scholar]
- 2.World Health Organization . Regional Office for the Eastern Mediterranean List of Basic Sources in English for a Medical Faculty Library. WHO; Geneva, Switzerland: 2013. [Google Scholar]
- 3.Razzak H.A., Harbi A., Ahli S. Tobacco Smoking Prevalence, Health Risk, and Cessation in the UAE. Oman Med. J. 2020;35:e165. doi: 10.5001/omj.2020.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdullah A.S., Qiming F., Pun V., Stillman F.A., Samet J.M. A Review of Tobacco Smoking and Smoking Cessation Practices among Physicians in China: 1987-2010. Tob. Control. 2013;22:9–14. doi: 10.1136/tobaccocontrol-2011-050135. [DOI] [PubMed] [Google Scholar]
- 5.Smith D.R., Leggat P.A. An International Review of Tobacco Smoking in the Medical Profession: 1974–2004. BMC Public Health. 2007;7:115. doi: 10.1186/1471-2458-7-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tong E.K., Wolf T., Cooke D.T., Fairman N., Chen M.S. The Emergence of a Sustainable Tobacco Treatment Program across the Cancer Care Continuum: A Systems Approach for Implementation at the University of California Davis Comprehensive Cancer Center. Int. J. Environ. Res. Public. Health. 2020;17:3241. doi: 10.3390/ijerph17093241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barengo N.C., Sandström H.P., Jormanainen V.J., Myllykangas M.T. Attitudes and Behaviours in Smoking Cessation among General Practitioners in Finland 2001. Soz. Praventivmed. 2005;50:355–360. doi: 10.1007/s00038-005-4097-z. [DOI] [PubMed] [Google Scholar]
- 8.Behbehani N., Hamadeh R.R., Macklai N.S. Knowledge of and Attitudes towards Tobacco Control among Smoking and Non-Smoking Physicians in 2 Gulf Arab States. Saudi Med. J. 2004;25:585–591. [PubMed] [Google Scholar]
- 9.Bouillon-Minois J.-B., Trousselard M., Pereira B., Schmidt J., Clinchamps M., Thivel D., Ugbolue U.C., Moustafa F., Occelli C., Vallet G., et al. Protocol of the Study on Emergency Health Care Workers’ Responses Evaluated by Karasek Questionnaire: The SEEK-Study Protocol. Int. J. Environ. Res. Public. Health. 2021;18:4068. doi: 10.3390/ijerph18084068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bouillon-Minois J.-B., Raconnat J., Clinchamps M., Schmidt J., Dutheil F. Emergency Department and Overcrowding during COVID-19 Outbreak; a Letter to Editor. Arch. Acad. Emerg. Med. 2021;9:e28. doi: 10.22037/aaem.v9i1.1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wainwright K., Perrotte J.K., Bibriescas N., Baumann M.R., Garza R.T. Smoking Expectancies and Health Perceptions: An Analysis of Hispanic Subgroups. Addict. Behav. 2019;98:106008. doi: 10.1016/j.addbeh.2019.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghadban R., Haddad L., Thacker L.R., An K., Balster R.L., Salyer J. Smoking Behaviors in Arab Americans: Acculturation and Health Beliefs. J. Transcult. Nurs. Off. J. Transcult. Nurs. Soc. 2019;30:115–123. doi: 10.1177/1043659618783235. [DOI] [PubMed] [Google Scholar]
- 13.Musk A.W., de Klerk N.H. History of Tobacco and Health. Respirology. 2003;8:286–290. doi: 10.1046/j.1440-1843.2003.00483.x. [DOI] [PubMed] [Google Scholar]
- 14.Mounach S., Zahrou F.-E., Mahdaoui E., Belakhel L., Khazraji Y.C., El Berri H. Evolution of Attitudes, Trends and Perceptions of Smoking among Middle and Secondary School Students in the Gharb Region, Morocco, 2010–2015. Afr. J. Prim. Health Care Fam. Med. 2019;11:e1–e6. doi: 10.4102/phcfm.v11i1.1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stang A. Critical Evaluation of the Newcastle-Ottawa Scale for the Assessment of the Quality of Nonrandomized Studies in Meta-Analyses. Eur. J. Epidemiol. 2010;25:603–605. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 17.Vandenbroucke J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. Ann. Intern. Med. 2007;147:573–578. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. [DOI] [PubMed] [Google Scholar]
- 18.Schulz K.F., Altman D.G., Moher D. For the CONSORT Group CONSORT 2010 Statement: Updated Guidelines for Reporting Parallel Group Randomised Trials. BMJ. 2010;340:c332. doi: 10.1136/bmj.c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DerSimonian R., Laird N. Meta-Analysis in Clinical Trials. Control. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 20.Thorlund K., Imberger G., Johnston B.C., Walsh M., Awad T., Thabane L., Gluud C., Devereaux P.J., Wetterslev J. Evolution of Heterogeneity (I2) Estimates and Their 95% Confidence Intervals in Large Meta-Analyses. PLoS ONE. 2012;7:e39471. doi: 10.1371/journal.pone.0039471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mostafa N., Momen M. Effect of Physicians’ Smoking Status on Their Knowledge, Attitude, Opinions and Practices of Smoking Cessation in a University Hospital, in Egypt. J. Egypt. Public Health Assoc. 2017;92:96–106. doi: 10.21608/EPX.2018.8947. [DOI] [PubMed] [Google Scholar]
- 22.Amte R., Munta K., Gopal P.B. Stress Levels of Critical Care Doctors in India: A National Survey. Indian J. Crit. Care Med. Peer-Rev. Off. Publ. Indian Soc. Crit. Care Med. 2015;19:257–264. doi: 10.4103/0972-5229.156464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arnetz B.B., Andreasson S., Strandberg M., Eneroth P., Kallner A. Comparison between Surgeons and General Practitioners with Respect to Cardiovascular and Psychosocial Risk Factors among Physicians. Scand. J. Work. Environ. Health. 1988;14:118–124. doi: 10.5271/sjweh.1946. [DOI] [PubMed] [Google Scholar]
- 24.Nawaz H., Imam S.Z., Zubairi A.B.S., Pabaney A.H., Sepah Y.J., Islam M., Khan J.A. Smoking Habits and Beliefs of Future Physicians of Pakistan. Int. J. Tuberc. Lung Dis. Off. J. Int. Union Tuberc. Lung Dis. 2007;11:915–919. [PubMed] [Google Scholar]
- 25.Braun B.L., Fowles J.B., Solberg L.I., Kind E.A., Lando H., Pine D. Smoking-Related Attitudes and Clinical Practices of Medical Personnel in Minnesota. Am. J. Prev. Med. 2004;27:316–322. doi: 10.1016/j.amepre.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 26.Cheng K.K., Lam T.H. Smoking among Young Doctors in Hong Kong: A Message to Medical Educators. Med. Educ. 1990;24:158–163. doi: 10.1111/j.1365-2923.1990.tb02515.x. [DOI] [PubMed] [Google Scholar]
- 27.Aaro L.E., Bjartveit K., Vellar O.D., Berglund E.L. Smoking Habits among Norwegian Doctors 1974. Scand. J. Soc. Med. 1977;5:127–135. doi: 10.1177/140349487700500304. [DOI] [PubMed] [Google Scholar]
- 28.Aboyans V., Pinet P., Lacroix P., Laskar M. Knowledge and Management of Smoking-Cessation Strategies among Cardiologists in France: A Nationwide Survey. Arch. Cardiovasc. Dis. 2009;102:193–199. doi: 10.1016/j.acvd.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 29.Akvardar Y., Demiral Y., Ergor G., Ergor A. Substance Use among Medical Students and Physicians in a Medical School in Turkey. Soc. Psychiatry Psychiatr. Epidemiol. 2004;39:502–506. doi: 10.1007/s00127-004-0765-1. [DOI] [PubMed] [Google Scholar]
- 30.Al Alwan I., Badri M., Al-Ghamdi M., Aljarbou A., Alotaibi H., Tamim H. Prevalence of Self-Reported Cardiovascular Risk Factors among Saudi Physicians: A Comparative Study. Int. J. Health Sci. 2013;7:3–13. doi: 10.12816/0006015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alarjan J.F., Hindawi O.S., Judge L.W., Aleyadh Z.A., Bellar D.M. Prevalence of Obesity and Behaviors Associated with the Development of Metabolic Disease among Medical Practitioners in Jordan. J. Educ. Health Promot. 2015;4:17. doi: 10.4103/2277-9531.154036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al-Khateeb M. Trends of Tobacco Smoking among Physicians, Journalists and Teachers in Bahrain. Hygie. 1990;9:13–15. [PubMed] [Google Scholar]
- 33.Al-Lawati J.A., Nooyi S.C., Al-Lawati A.M. Knowledge, Attitudes and Prevalence of Tobacco Use among Physicians and Dentists in Oman. Ann. Saudi Med. 2009;29:128–131. doi: 10.4103/0256-4947.51803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Letter A.J. Doctors’ Smoking Habits. Med. J. Aust. 1976;1:71. [PubMed] [Google Scholar]
- 35.Aryayev M., Lowe J.B., Kuzmenko T. The Prevalence of and Knowledge about Tobacco Use among Physicians in the Odessa Region, Ukraine. Eur. J. Public Health. 2014;24:474–476. doi: 10.1093/eurpub/cku033. [DOI] [PubMed] [Google Scholar]
- 36.Baltaci D., Bahcebasi T., Aydin L.Y., Ozturk S., Set T., Eroz R., Celer A., Kara I.H. Evaluation of Smoking Habits among Turkish Family Physicians. Toxicol. Ind. Health. 2014;30:3–11. doi: 10.1177/0748233712448113. [DOI] [PubMed] [Google Scholar]
- 37.Baptista T., Uzcàtegui E. Substance Use among Resident Doctors in Venezuela. Drug Alcohol Depend. 1993;32:127–132. doi: 10.1016/0376-8716(93)80005-Y. [DOI] [PubMed] [Google Scholar]
- 38.Barengo N.C., Sandström P.H., Jormanainen V.J., Myllykangas M.T. Changes in Smoking Prevalence among Finnish Physicians 1990–2001. Eur. J. Public Health. 2004;14:201–203. doi: 10.1093/eurpub/14.2.201. [DOI] [PubMed] [Google Scholar]
- 39.Barnoya J., Glantz S. Knowledge and Use of Tobacco among Guatemalan Physicians. Cancer Causes Control. 2002;13:879–881. doi: 10.1023/a:1020658519854. [DOI] [PubMed] [Google Scholar]
- 40.Basnyat P.S., Moseley L.G., al-Rawi M., Galland R.B., Lewis M.H. Smoking—Do Vascular Surgeons Practise What They Preach? Ann. R. Coll. Surg. Engl. 2000;82:424–427. [PMC free article] [PubMed] [Google Scholar]
- 41.Basu M., Das P., Mitra S., Ghosh S., Pal R., Bagchi S. Role of Family and Peers in the Initiation and Continuation of Smoking Behavior of Future Physicians. J. Pharm. Bioallied Sci. 2011;3:407–411. doi: 10.4103/0975-7406.84452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Belkić K., Nedic O. Workplace Stressors and Lifestyle-Related Cancer Risk Factors among Female Physicians: Assessment Using the Occupational Stress Index. J. Occup. Health. 2007;49:61–71. doi: 10.1539/joh.49.61. [DOI] [PubMed] [Google Scholar]
- 43.Belkić K., Nedić O. Night Work, Total Occupational Burden and Cancer/Cardiovascular Risk Factors in Physicians. Med. Pregl. 2012;65:461–469. doi: 10.2298/MPNS1212461B. [DOI] [PubMed] [Google Scholar]
- 44.Bener A., Gomes J., Anderson J.A. Smoking Habits among Physicians in Two Gulf Countries. J. R. Soc. Health. 1993;113:298–301. doi: 10.1177/146642409311300605. [DOI] [PubMed] [Google Scholar]
- 45.Borgan S.M., Jassim G., Marhoon Z.A., Almuqamam M.A., Ebrahim M.A., Soliman P.A. Prevalence of Tobacco Smoking among Health-Care Physicians in Bahrain. BMC Public Health. 2014;14:931. doi: 10.1186/1471-2458-14-931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bortz W.M. Health Behavior and Experiences of Physicians. Results of a Survey of Palo Alto Medical Clinic Physicians. West. J. Med. 1992;156:50–51. [PMC free article] [PubMed] [Google Scholar]
- 47.Bostan P.P., Demir C.K., Elbek O., Akçay Ş. Association between Pulmonologists’ Tobacco Use and Their Effort in Promoting Smoking Cessation in Turkey: A Cross-Sectional Study. BMC Pulm. Med. 2015;15:143. doi: 10.1186/s12890-015-0131-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bourke G.J., Wilson-Davis K., Thornes D. Smoking Habits of the Medical Profession in the Republic of Ireland. Am. J. Public Health. 1972;62:575–580. doi: 10.2105/AJPH.62.4.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Brenner H., Scharrer S. Smoking Habits of Future Physicians: A Survey among Medical Students of a South German University. Soz. Praventivmed. 1996;41:150–157. doi: 10.1007/BF01305385. [DOI] [PubMed] [Google Scholar]
- 50.Brotons C., Björkelund C., Bulc M., Ciurana R., Godycki-Cwirko M., Jurgova E., Kloppe P., Lionis C., Mierzecki A., Piñeiro R., et al. Prevention and Health Promotion in Clinical Practice: The Views of General Practitioners in Europe. Prev. Med. 2005;40:595–601. doi: 10.1016/j.ypmed.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 51.Burgess A.M., Tierney J.T. Bias Due to Nonresponse in a Mail Survey of Rhode Island Physicians’ Smoking Habits—1968. N. Engl. J. Med. 1970;282:908. doi: 10.1056/NEJM197004162821607. [DOI] [PubMed] [Google Scholar]
- 52.Burgess A.M., Casey D.B., Tierney J.T. Cigarette Smoking by Rhode Island Physicians, 1963–1973: Comparison with Lawyers and Other Adult Males. Am. J. Public Health. 1978;68:63–65. doi: 10.2105/AJPH.68.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ceraso M., McElroy J.A., Kuang X., Vila P.M., Jorenby D.E., Fiore M.C., Du X., Qian N., Lu L., Ren H. Smoking, Barriers to Quitting, and Smoking-Related Knowledge, Attitudes, and Patient Practices among Male Physicians in China. Prev. Chronic. Dis. 2008;6:A06. [PMC free article] [PubMed] [Google Scholar]
- 54.Chaudhry M., Chaudhry I., Rahman M. Prevalence of Smoking among Health Care Providers in Tertiary Care Hospitals. RMJ. 2007;34:40–42. [Google Scholar]
- 55.Coe R.M., Brehm H.P. Smoking Habits of Physicians and Preventive Care Practices. HSMHA Health Rep. 1971;86:217–221. doi: 10.2307/4594142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cofta S., Staszewski R. Hospital Staff and Smoking Habits: Do We Need Modification of Smoking Behavior in Polish Hospitals? J. Physiol. Pharmacol. Off. J. Pol. Physiol. Soc. 2008;59((Suppl. S6)):191–199. [PubMed] [Google Scholar]
- 57.Das P., Basu M., Chowdhury K., Mallik S., Dhar G.C., Biswas A. Observational Assessment and Correlates to Blood Pressure of Future Physicians of Bengal. Niger. J. Clin. Pract. 2013;16:433–438. doi: 10.4103/1119-3077.116884. [DOI] [PubMed] [Google Scholar]
- 58.De Col P., Baron C., Guillaumin C., Bouquet E., Fanello S. Influence of smoking among family physicians on their practice of giving minimal smoking cessation advice in 2008. A survey of 332 general practitioners in Maine-et-Loire. Rev. Mal. Respir. 2010;27:431–440. doi: 10.1016/j.rmr.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 59.Dekker H.M., Looman C.W., Adriaanse H.P., van der Maas P.J. Prevalence of Smoking in Physicians and Medical Students, and the Generation Effect in The Netherlands. Soc. Sci. Med. 1993;36:817–822. doi: 10.1016/0277-9536(93)90042-3. [DOI] [PubMed] [Google Scholar]
- 60.de Oliveira G.S., Chang R., Fitzgerald P.C., Almeida M.D., Castro-Alves L.S., Ahmad S., McCarthy R.J. The Prevalence of Burnout and Depression and Their Association with Adherence to Safety and Practice Standards: A Survey of United States Anesthesiology Trainees. Anesth. Analg. 2013;117:182–193. doi: 10.1213/ANE.0b013e3182917da9. [DOI] [PubMed] [Google Scholar]
- 61.Desalu O.O., Adekoya A.O., Elegbede A.O., Dosunmu A., Kolawole T.F., Nwogu K.C. Knowledge of and Practices Related to Smoking Cessation among Physicians in Nigeria. J. Bras. Pneumol. 2009;35:1198–1203. doi: 10.1590/S1806-37132009001200006. [DOI] [PubMed] [Google Scholar]
- 62.Djalalinia S., Tehrani F.R., Malekafzali H., Dovvom M.R., Neot R., Peykari N. Training of General Practitioners about Smoking Cessation Counseling. J. Pak. Med. Assoc. 2011;61:4. [PubMed] [Google Scholar]
- 63.Doll R., Hill A.B. The Mortality of Doctors in Relation to Their Smoking Habits. BMJ. 1954;1:1451–1455. doi: 10.1136/bmj.1.4877.1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Doll R., Hill A.B. Mortality in Relation to Smoking: Ten Years’ Observations of British Doctors. Br. Med. J. 1964;1:1399–1410. doi: 10.1136/bmj.1.5395.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Doll R., Peto R., Wheatley K., Gray R., Sutherland I. Mortality in Relation to Smoking: 40 Years’ Observations on Male British Doctors. BMJ. 1994;309:901–911. doi: 10.1136/bmj.309.6959.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Doll R., Peto R., Boreham J., Sutherland I. Mortality in Relation to Smoking: 50 Years’ Observations on Male British Doctors. BMJ. 2004;328:1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Easton A., Husten C., Malarcher A., Elon L., Caraballo R., Ahluwalia I., Frank E. Smoking Cessation Counseling by Primary Care Women Physicians: Women Physicians’ Health Study. Women Health. 2001;32:77–91. doi: 10.1300/J013v32n04_05. [DOI] [PubMed] [Google Scholar]
- 68.Edwards R., Bowler T., Atkinson J., Wilson N. Low and Declining Cigarette Smoking Rates among Doctors and Nurses: 2006 New Zealand Census Data. N. Z. Med. J. 2008;121:43–51. [PubMed] [Google Scholar]
- 69.Edwards R., Tu D., Stanley J., Martin G., Newcombe R. Smoking Prevalence among Doctors and Nurses—2013 New Zealand Census Data. N. Z. Med. J. 2018;131:10. [PubMed] [Google Scholar]
- 70.Fadhil I., Al Musawi M. Tobacco Training and Educating Primary Care Professionals in Bahrain. J. Bahrain. Med. Soc. 2007;19:23–27. [Google Scholar]
- 71.Fanello S., Ripault B., Le Levier F., Guérin O., Penneau D. [Smoking by general practitioners in Maine-et-Loire] Rev. Epidemiol. Sante Publique. 1990;38:78–79. [PubMed] [Google Scholar]
- 72.Fathi A., Ahari S.S., Amani F., Nikneghad M.R. Study Frequency of Hypertension and Obesity and Their Relationship with Lifestyle Factors (Nutritional Habits, Physical Activity, Cigarette Consumption) in Ardabil City Physicians, 2012–2013. Indian J. Community Med. Off. Publ. Indian Assoc. Prev. Soc. Med. 2016;41:268–272. doi: 10.4103/0970-0218.193332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Franceschi S., Serraino D., Talamini R., Candiani E. Personal Habits and Attitudes towards Smoking in a Sample of Physicians from the North-East of Italy. Int. J. Epidemiol. 1986;15:584–585. doi: 10.1093/ije/15.4.584. [DOI] [PubMed] [Google Scholar]
- 74.Frank E., Brogan D.J., Mokdad A.H., Simoes E.J., Kahn H.S., Greenberg R.S. Health-Related Behaviors of Women Physicians vs. Other Women in the United States. Arch. Intern. Med. 1998;158:342–348. doi: 10.1001/archinte.158.4.342. [DOI] [PubMed] [Google Scholar]
- 75.Frank E., Segura C. Health Practices of Canadian Physicians. Can. Fam. Physician Med. Fam. Can. 2009;55:810–811.e7. [PMC free article] [PubMed] [Google Scholar]
- 76.Freour T., Dessolle L., Jean M., Barriere P. Smoking among French Infertility Specialists: Habits, Opinions and Patients’ Management. Eur. J. Obstet. Gynecol. Reprod. Biol. 2011;155:44–48. doi: 10.1016/j.ejogrb.2010.10.024. [DOI] [PubMed] [Google Scholar]
- 77.Garfinkel L. Cigarette Smoking among Physicians and Other Health Professionals, 1959–1972. CA Cancer J. Clin. 1976;26:373–375. doi: 10.3322/canjclin.26.6.373. [DOI] [PubMed] [Google Scholar]
- 78.Grossman D.W., Knox J.J., Nash C., Jiménez J.G. Smoking: Attitudes of Costa Rican Physicians and Opportunities for Intervention. Bull. World Health Organ. 1999;77:315–322. [PMC free article] [PubMed] [Google Scholar]
- 79.Gunes G., Karaoglu L., Genc M.F., Pehlivan E., Egri M. University Hospital Physicians’ Attitudes and Practices for Smoking Cessation Counseling in Malatya, Turkey. Patient Educ. Couns. 2005;56:147–153. doi: 10.1016/j.pec.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 80.Gupta G., Schleinitz M.D., Reinert S.E., McGarry K.A. Resident Physician Preventive Health Behaviors and Perspectives on Primary Care. R. I. Med. J. 2013;96:43–47. [PubMed] [Google Scholar]
- 81.Hallett R. Intervention against Smoking and Its Relationship to General Practitioners’ Smoking Habits. J. R. Coll. Gen. Pract. 1983;33:565–567. [PMC free article] [PubMed] [Google Scholar]
- 82.Hamadeh R.R. Smoking Habits of Primary Health Care Physicians in Bahrain. J. R. Soc. Promot. Health. 1999;119:36–39. doi: 10.1177/146642409911900107. [DOI] [PubMed] [Google Scholar]
- 83.Li H.Z., Sun W., Cheng F., Wang X., Liu W., Wang A. Cigarette Smoking Status and Smoking Cessation Counseling of Chinese Physicians in Wuhan, Hubei Province. Asia. Pac. J. Public Health. 2008;20:183–192. doi: 10.1177/1010539508317821. [DOI] [PubMed] [Google Scholar]
- 84.Hay D.R., Christmas B.W. The Smoking Habits of Women Doctors and Doctors’ Wives in New Zealand. Prev. Med. 1976;5:78–88. doi: 10.1016/0091-7435(76)90011-6. [DOI] [PubMed] [Google Scholar]
- 85.Hay D.R. Cigarette Smoking by New Zealand Doctors and Nurses: Results from the 1996 Population Census. N. Z. Med. J. 1998;111:102–104. [PubMed] [Google Scholar]
- 86.Heloma A., Reijula K., Tikkanen J., Nykyri E. The Attitudes of Occupational Health Personnel to Smoking at Work. Am. J. Ind. Med. 1998;34:73–78. doi: 10.1002/(SICI)1097-0274(199807)34:1<73::AID-AJIM10>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 87.Hensrud D.D., Sprafka J.M. The Smoking Habits of Minnesota Physicians. Am. J. Public Health. 1993;83:415–417. doi: 10.2105/AJPH.83.3.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Heponiemi T., Kouvonen A., Vänskä J., Halila H., Sinervo T., Kivimäki M., Elovainio M. Effects of Active On-Call Hours on Physicians’ Turnover Intentions and Well-Being. Scand. J. Work. Environ. Health. 2008;34:356–363. doi: 10.5271/sjweh.1278. [DOI] [PubMed] [Google Scholar]
- 89.Hidalgo K.D., Mielke G.I., Parra D.C., Lobelo F., Simões E.J., Gomes G.O., Florindo A.A., Bracco M., Moura L., Brownson R.C., et al. Health Promoting Practices and Personal Lifestyle Behaviors of Brazilian Health Professionals. BMC Public Health. 2016;16:1114. doi: 10.1186/s12889-016-3778-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Hodgetts G., Broers T., Godwin M. Smoking Behaviour, Knowledge and Attitudes among Family Medicine Physicians and Nurses in Bosnia and Herzegovina. BMC Fam. Pract. 2004;5:12. doi: 10.1186/1471-2296-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Hoseainrezaee H., Khodabandeh S., Kheradmand A., Pilehvarzadeh M. Frequency of Smoking and Specialized Awareness among Doctors and Nurses of Hospitals in Kerman, Iran. Addict. Health. 2013;5:51–56. [PMC free article] [PubMed] [Google Scholar]
- 92.Huang C., Guo C., Yu S., Feng Y., Song J., Eriksen M., Redmon P., Koplan J. Smoking Behaviours and Cessation Services among Male Physicians in China: Evidence from a Structural Equation Model. Tob. Control. 2013;22((Suppl. S2)):ii27–ii33. doi: 10.1136/tobaccocontrol-2012-050884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hughes P.H., Conard S.E., Baldwin D.C., Storr C.L., Sheehan D.V. Resident Physician Substance Use in the United States. JAMA. 1991;265:2069–2073. doi: 10.1001/jama.1991.03460160047027. [DOI] [PubMed] [Google Scholar]
- 94.Hughes P.H., Brandenburg N., Baldwin D.C., Storr C.L., Williams K.M., Anthony J.C., Sheehan D.V. Prevalence of Substance Use among US Physicians. JAMA. 1992;267:2333–2339. doi: 10.1001/jama.1992.03480170059029. [DOI] [PubMed] [Google Scholar]
- 95.Hughes P.H., Storr C.L., Brandenburg N.A., Baldwin D.C., Anthony J.C., Sheehan D.V. Physician Substance Use by Medical Specialty. J. Addict. Dis. 1999;18:23–37. doi: 10.1300/J069v18n02_03. [DOI] [PubMed] [Google Scholar]
- 96.Hung O.Y., Keenan N.L., Fang J. Physicians’ Health Habits Are Associated with Lifestyle Counseling for Hypertensive Patients. Am. J. Hypertens. 2013;26:201–208. doi: 10.1093/ajh/hps022. [DOI] [PubMed] [Google Scholar]
- 97.Içli F., Içli T., Günel N., Arikan R. Cigarette Smoking among Young Physicians and Their Approach to the Smoking Problem of Their Patients. J. Cancer Educ. Off. J. Am. Assoc. Cancer Educ. 1992;7:237–240. doi: 10.1080/08858199209528174. [DOI] [PubMed] [Google Scholar]
- 98.Jiang Y., Ong M.K., Tong E.K., Yang Y., Nan Y., Gan Q., Hu T.-W. Chinese Physicians and Their Smoking Knowledge, Attitudes, and Practices. Am. J. Prev. Med. 2007;33:15–22. doi: 10.1016/j.amepre.2007.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jiménez-Ruiz C.A., Riesco Miranda J.A., Ramos Pinedo A., de Higes Martinez E., Marquez F.L., Palomo Cobos L., Solano Reina S., de Granda Orive J.I., de Lucas Ramos P. Prevalence of and Attitudes towards Smoking among Spanish Health Professionals. Respir. Int. Rev. Thorac. Dis. 2015;90:474–480. doi: 10.1159/000441306. [DOI] [PubMed] [Google Scholar]
- 100.Jingi A.M., Noubiap J.J.N. Cardiovascular Risk Factors Awareness and Prevalence among Primary Care Physicians: An Insight from the West Region Awareness Initiative Survey to Fight Cardiovascular Disease (WAIT-CVD) in Cameroon. BMC Res. Notes. 2015;8:762. doi: 10.1186/s13104-015-1747-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.John U., Hanke M. Tobacco-Smoking Prevalence among Physicians and Nurses in Countries with Different Tobacco-Control Activities. Eur. J. Cancer Prev. 2003;12:235–237. doi: 10.1097/00008469-200306000-00011. [DOI] [PubMed] [Google Scholar]
- 102.Joossens L., Demedts M., Prignot J., Bartsch P., Gyselen A. Smoking Habits of Belgian Physicians: Effects of Consonancy Behaviour and of Age. Acta Clin. Belg. 1987;42:457–461. doi: 10.1080/22953337.1987.11719265. [DOI] [PubMed] [Google Scholar]
- 103.Josseran L., King G., Velter A., Dressen C., Grizeau D. Smoking Behavior and Opinions of French General Practitioners. J. Natl. Med. Assoc. 2000;92:382–390. [PMC free article] [PubMed] [Google Scholar]
- 104.Josseran L., King G., Guilbert P., Davis J., Brücker G. Smoking by French General Practitioners: Behaviour, Attitudes and Practice. Eur. J. Public Health. 2005;15:33–38. doi: 10.1093/eurpub/cki108. [DOI] [PubMed] [Google Scholar]
- 105.Julião A.M., Camargo A.L.L.S., Cítero V.D.A., Maranhão M.F., Maluf Neto A., Paes A.T., Glezer M., Cendoroglo Neto M., Schvartsman C. Physicians’ Attitude towards Tobacco Dependence in a Private Hospital in the City of São Paulo, Brazil. Einstein Sao Paulo Braz. 2013;11:158–162. doi: 10.1590/S1679-45082013000200004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kaetsu A., Fukushima T., Moriyama M., Shigematsu T. Smoking Behavior and Related Lifestyle Variables among Physicians in Fukuoka, Japan: A Cross Sectional Study. J. Epidemiol. 2002;12:199–207. doi: 10.2188/jea.12.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kaneita Y., Uchida T., Ohida T. Epidemiological Study of Smoking among Japanese Physicians. Prev. Med. 2010;51:164–167. doi: 10.1016/j.ypmed.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 108.Kawahara K., Ohida T., Osaki Y., Mochizuki Y., Minowa M., Yamaguchi N., Kusaka Y. Study of the Smoking Behavior of Medical Doctors in Fukui, Japan and Their Antismoking Measures. J. Epidemiol. 2000;10:157–162. doi: 10.2188/jea.10.157. [DOI] [PubMed] [Google Scholar]
- 109.Kawakami M., Nakamura S., Fumimoto H., Takizawa J., Baba M. Relation between Smoking Status of Physicians and Their Enthusiasm to Offer Smoking Cessation Advice. Intern. Med. 1997;36:162–165. doi: 10.2169/internalmedicine.36.162. [DOI] [PubMed] [Google Scholar]
- 110.Kawane H. The Prevalence of Smoking among Physicians in Japan. Am. J. Public Health. 1993;83:1640. doi: 10.2105/AJPH.83.11.1640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kotz D., Wagena E.J., Wesseling G. Smoking Cessation Practices of Dutch General Practitioners, Cardiologists, and Lung Physicians. Respir. Med. 2007;101:568–573. doi: 10.1016/j.rmed.2006.06.016. [DOI] [PubMed] [Google Scholar]
- 112.Lam T.H., Jiang C., Chan Y.-F., Chan S.S.C. Smoking Cessation Intervention Practices in Chinese Physicians: Do Gender and Smoking Status Matter? Health Soc. Care Community. 2011;19:126–137. doi: 10.1111/j.1365-2524.2010.00952.x. [DOI] [PubMed] [Google Scholar]
- 113.La Vecchia C., Scarpino V., Malvezzi I., Baldi G. A Survey of Smoking among Italian Doctors. J. Epidemiol. Community Health. 2000;54:320. doi: 10.1136/jech.54.4.320a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Lefcoe N.M., Wonnacott T.H. The Prevalence of Chronic Respiratory Disease in the Male Physicians of London, Ontario. Can. Med. Assoc. J. 1970;102:381–385. [PMC free article] [PubMed] [Google Scholar]
- 115.Legnini M.W., Claus E.B. Smoking among Yale Medical School Faculty. Yale J. Biol. Med. 1987;60:9–18. [PMC free article] [PubMed] [Google Scholar]
- 116.Lindfors P.M., Meretoja O.A., Luukkonen R.A., Elovainio M.J., Leino T.J. Suicidality among Finnish Anaesthesiologists. Acta Anaesthesiol. Scand. 2009;53:1027–1035. doi: 10.1111/j.1399-6576.2009.02014.x. [DOI] [PubMed] [Google Scholar]
- 117.Lipp M., Tinklenberg J., Benson S., Melges F., Taintor Z., Peterson M. Medical Student Use of Marijuana, Alcohol, and Cigarettes: A Study of Four Schools. Int. J. Addict. 1972;7:141–152. doi: 10.3109/10826087209026768. [DOI] [PubMed] [Google Scholar]
- 118.Lipp M.R., Benson S.G. Physician Use of Marijuana, Alcohol, and Tobacco. Am. J. Psychiatry. 1972;129:612–616. doi: 10.1176/ajp.129.5.612. [DOI] [PubMed] [Google Scholar]
- 119.Magee M.J., Darchia L., Kipiani M., Chakhaia T., Kempker R.R., Tukvadze N., Berg C.J., Blumberg H.M. Smoking Behavior and Beliefs about the Impact of Smoking on Anti-Tuberculosis Treatment among Health Care Workers. Int. J. Tuberc. Lung Dis. Off. J. Int. Union Tuberc. Lung Dis. 2017;21:1049–1055. doi: 10.5588/ijtld.17.0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Malik A.K., Chaudhry A., Karamat A., Arif N., Cheema M.A., Rauf A. Cigarette Smoking and Health Care Professionals at Mayo Hospital, Lahore, Pakistan. JPMA J. Pak. Med. Assoc. 2010;60:509–512. [PubMed] [Google Scholar]
- 121.Marakoğlu K., Kutlu R., Sahsivar S. The Frequency of Smoking, Quitting and Socio-Demographic Characteristics of Physicians of a Medical Faculty. West Indian Med. J. 2006;55:160–164. doi: 10.1590/S0043-31442006000300006. [DOI] [PubMed] [Google Scholar]
- 122.Márk L., Nagy E., Kondacs A., Deli L. The Change of Attitude of Hungarian Physicians towards the Importance of Risk Factors of Coronary Heart Disease over the Period 1985–1996. Public Health. 1998;112:197–201. doi: 10.1016/S0033-3506(98)00227-3. [DOI] [PubMed] [Google Scholar]
- 123.Mathavan A., Chockalingam A., Chockalingam S., Bilchik B., Saini V. Madurai Area Physicians Cardiovascular Health Evaluation Survey (MAPCHES)—An Alarming Status. Can. J. Cardiol. 2009;25:303–308. doi: 10.1016/S0828-282X(09)70494-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.McAuliffe W.E., Rohman M., Wechsler H. Alcohol, Substance Use, and Other Risk-Factors of Impairment in a Sample of Physicians-in-Training. Adv. Alcohol Subst. Abuse. 1984;4:67–87. doi: 10.1300/J251v04n02_07. [DOI] [PubMed] [Google Scholar]
- 125.McGrady F.P., McGlade K.J., Cupples M.E., Tully M.A., Hart N., Steele K. Questionnaire Survey of PHysical ActivITy in General Practitioners (PHIT GP Study) Ulster Med. J. 2007;76:91–97. [PMC free article] [PubMed] [Google Scholar]
- 126.Merrill R.M., Madanat H., Layton J.B., Hanson C.L., Madsen C.C. Smoking Prevalence, Attitudes, and Perceived Smoking Prevention and Control Responsibilities and Behaviors among Physicians in Jordan. Int. Q. Community Health Educ. 2006;26:397–413. doi: 10.2190/IQ.26.4.g. [DOI] [PubMed] [Google Scholar]
- 127.Meshefedjian G.A., Gervais A., Tremblay M.D., Villeneuve D., O’loughlin J. Physician Smoking Status May Influence Cessation Counseling Practices. Can. J. Public Health Rev. Can. Sante Publique. 2010;101:290–293. doi: 10.1007/BF03405288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mikalauskas A., Širvinskas E., Marchertienė I., Macas A., Samalavičius R., Kinduris Š., Benetis R. Burnout among Lithuanian Cardiac Surgeons and Cardiac Anesthesiologists. Med. Kaunas Lith. 2012;48:478–484. doi: 10.3390/medicina48090071. [DOI] [PubMed] [Google Scholar]
- 129.Misra R., Vadaparampil S.T. Personal Cancer Prevention and Screening Practices among Asian Indian Physicians in the United States. Cancer Detect. Prev. 2004;28:269–276. doi: 10.1016/j.cdp.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 130.Mohseni-Bandpei M.A., Ahmad-Shirvani M., Golbabaei N., Behtash H., Shahinfar Z., Fernández-de-las-Peñas C. Prevalence and Risk Factors Associated with Low Back Pain in Iranian Surgeons. J. Manip. Physiol. Ther. 2011;34:362–370. doi: 10.1016/j.jmpt.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 131.Moreno San-Pedro E., San-Pedro E.M., Roales-Nieto J.G., Blanco-Coronado J.L. Tobacco Use among Spanish Physicians and Medical Students. Tob. Control. 2006;15:272. doi: 10.1136/tc.2005.014910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mubeen S.M., Morrow M., Barraclough S. Smoking among Future Doctors in a “No-Smoking” University Campus in Karachi, Pakistan: Issues of Tobacco Control. J. Pak. Med. Assoc. 2008;58:6. [PubMed] [Google Scholar]
- 133.Naji N., McLoughlin H., Connell F.O., Clancy L. Smoking Profile of Non-Consultant Hospital Doctors. Ir. J. Med. Sci. 2006;175:29–31. doi: 10.1007/BF03168996. [DOI] [PubMed] [Google Scholar]
- 134.Nakladalova M., Sovova E., Ivanova K., Kaletova M., Lukl J., Fialova J. Risk Factors for Cardiovascular Diseases in Physicians. Biomed. Pap. 2005;149:293–295. doi: 10.5507/bp.2005.045. [DOI] [PubMed] [Google Scholar]
- 135.Nardini S., Bertoletti R., Rastelli V., Donner C.F. The Influence of Personal Tobacco Smoking on the Clinical Practice of Italian Chest Physicians. Eur. Respir. J. 1998;12:1450–1453. doi: 10.1183/09031936.98.12061450. [DOI] [PubMed] [Google Scholar]
- 136.Nawaz A., Naqvi S.A.A. Attitudes, Perceptions, Habits of Smoker, Non-Smoker General Practitioners and Why They Fail to Motivate Patients to Quit Smoking. Pak. J. Med. Sci. 2008;24:152–156. [Google Scholar]
- 137.Ndiaye M., Hane A.A., Ndir M., Ba O., Diop-Dia D., Kandji M., Ndiaye S., Toure N.O., Diatta A., Dia Y., et al. [Smoking habits among physicians in Dakar] Rev. Pneumol. Clin. 2001;57:7–11. [PubMed] [Google Scholar]
- 138.Nelson D.E., Giovino G.A., Emont S.L., Brackbill R., Cameron L.L., Peddicord J., Mowery P.D. Trends in Cigarette Smoking among US Physicians and Nurses. JAMA. 1994;271:1273–1275. doi: 10.1001/jama.1994.03510400059032. [DOI] [PubMed] [Google Scholar]
- 139.Nutbeam D., Catford J. Modifiable Risks for Cardiovascular Disease among General Practitioners in Wales. Public Health. 1990;104:353–361. doi: 10.1016/S0033-3506(05)80528-1. [DOI] [PubMed] [Google Scholar]
- 140.Obeidat N.A., Habashneh M.A., Shihab R.A., Hawari F.I. Are Jordanian Primary Healthcare Practitioners Fulfilling Their Potential in Cancer Prevention and Community Health? Findings from a Cross-Sectional Survey. BMJ Open. 2017;7:e015269. doi: 10.1136/bmjopen-2016-015269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.O’Cathail M., O’Callaghan M. A Profile of Hospital Consultants: The Health Practices of a Cohort of Medical Professionals. Ir. Med. J. 2013;106:134–136. [PubMed] [Google Scholar]
- 142.Ohida T., Sakurai H., Mochizuki Y., Kamal A.M., Takemura S., Minowa M., Kawahara K. Smoking Prevalence and Attitudes toward Smoking among Japanese Physicians. JAMA. 2001;285:2643–2648. doi: 10.1001/jama.285.20.2643. [DOI] [PubMed] [Google Scholar]
- 143.O’ Keeffe A., Hayes B., Prihodova L. “Do as We Say, Not as We Do?” The Lifestyle Behaviours of Hospital Doctors Working in Ireland: A National Cross-Sectional Study. BMC Public Health. 2019;19:179. doi: 10.1186/s12889-019-6451-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Pärna K., Rahu K., Barengo N.C., Rahu M., Sandström P.H., Jormanainen V.J., Myllykangas M.T. Comparison of Knowledge, Attitudes and Behaviour Regarding Smoking among Estonian and Finnish Physicians. Soz. Praventivmed. 2005;50:378–388. doi: 10.1007/s00038-005-4089-z. [DOI] [PubMed] [Google Scholar]
- 145.Pärna K., Rahu K., Rahu M. Smoking Habits and Attitudes towards Smoking among Estonian Physicians. Public Health. 2005;119:390–399. doi: 10.1016/j.puhe.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 146.Pärna K., Põld M., Ringmets I. Trends in Smoking Behaviour among Estonian Physicians in 1982-2014. BMC Public Health. 2017;18:55. doi: 10.1186/s12889-017-4596-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Perrin P.C., Merrill R.M., Lindsay G.B. Patterns of Smoking Behavior among Physicians in Yerevan, Armenia. BMC Public Health. 2006;6:139. doi: 10.1186/1471-2458-6-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Peykari N.F., Tehrani F.R., Afzali H.M., Dovvon M.R., Djalalinia S.S. Smoking Habits among Iranian General Practitioners. J. Egypt. Public Health Assoc. 2010;85:97–112. [PubMed] [Google Scholar]
- 149.Phillips A.J., Taylor R.M. Smoking Habits of Physicians in Canada. Can. Med. Assoc. J. 1968;99:955–957. [PMC free article] [PubMed] [Google Scholar]
- 150.Pipe A., Sorensen M., Reid R. Physician Smoking Status, Attitudes toward Smoking, and Cessation Advice to Patients: An International Survey. Patient Educ. Couns. 2009;74:118–123. doi: 10.1016/j.pec.2008.07.042. [DOI] [PubMed] [Google Scholar]
- 151.Piryani R.M., Rizvi N. Smoking Habits amongst House Physicians Working at Jinnah Postgraduate Medical Center, Karachi, Pakistan. Trop. Doct. 2004;34:44–45. doi: 10.1177/004947550403400123. [DOI] [PubMed] [Google Scholar]
- 152.Pizzo A.M., Chellini E., Grazzini G., Cardone A., Badellino F. Italian General Practitioners and Smoking Cessation Strategies. Tumori. 2003;89:250–254. doi: 10.1177/030089160308900303. [DOI] [PubMed] [Google Scholar]
- 153.Poantă L.I., Zdrenghea D., Albu A. Psychometric Evaluation of Romanian Version of Job Content Questionnaire in Physicians. Rom. J. Intern. Med. Rev. Roum. Med. Interne. 2006;44:183–199. [PubMed] [Google Scholar]
- 154.Põld M., Pärna K. Smoking Prevalence and Attitudes towards Smoking among Estonian Physicians: Results from Cross-Sectional Studies in 2002 and 2014. BMJ Open. 2017;7:e017197. doi: 10.1136/bmjopen-2017-017197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Ramachandran A., Snehalatha C., Yamuna A., Murugesan N. High Prevalence of Cardiometabolic Risk Factors among Young Physicians in India. J. Assoc. Physicians India. 2008;56:17–20. [PubMed] [Google Scholar]
- 156.Ranchal Sánchez A., Pérula de Torres L.Á., Santos Luna F., Ruiz-Moral R. Prevalence of Tobacco Consumption among Young Physicians at a Regional University Hospital in Southern Spain: A Cross-Sectional Study. BMJ Open. 2018;8:e018728. doi: 10.1136/bmjopen-2017-018728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Rankin D.W., Gray N.J., Hill D.J., Evans D.R. Attitudes and Smoking Habits of Australian Doctors. Med. J. Aust. 1975;2:822–824. doi: 10.5694/j.1326-5377.1975.tb106350.x. [DOI] [PubMed] [Google Scholar]
- 158.Ravara S.B., Castelo-Branco M., Aguiar P., Calheiros J.M. Smoking Behaviour Trends among Portuguese Physicians: Are They Role Models? A Conference-Based Survey. Public Health. 2014;128:105–109. doi: 10.1016/j.puhe.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 159.Reile R., Pärna K. Do Physicians Address Their Patients’ Smoking Behavior? Results from a Nationwide Survey among Physicians in Estonia. Public Health. 2018;161:1–4. doi: 10.1016/j.puhe.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 160.Saeed A.A. Attitudes and Behaviour of Physicians towards Smoking in Riyadh City, Saudi Arabia. Trop. Geogr. Med. 1991;43:76–79. [PubMed] [Google Scholar]
- 161.Saeys F., Cammu H. GPs’ Attitudes on a Healthy Lifestyle: A Survey of GPs in Flanders. Br. J. Gen. Pract. 2014;64:e664–e669. doi: 10.3399/bjgp14X681853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Salgado M.V., Mejia R., Kaplan C.P., Perez-Stable E.J. Smoking Behavior and Use of Tobacco Industry Sponsored Websites Among Medical Students and Young Physicians in Argentina. J. Med. Internet Res. 2014;16:e35. doi: 10.2196/jmir.2528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Samuels N. Smoking among Hospital Doctors in Israel and Their Attitudes Regarding Anti-Smoking Legislation. Public Health. 1997;111:285–288. doi: 10.1016/S0033-3506(97)00055-3. [DOI] [PubMed] [Google Scholar]
- 164.Scott H.D., Tierney J.T., Buechner J.S., Waters W.J. Smoking Rates among Rhode Island Physicians: Achieving a Smoke-Free Society. Am. J. Prev. Med. 1992;8:86–90. doi: 10.1016/S0749-3797(18)30839-0. [DOI] [PubMed] [Google Scholar]
- 165.Sebo P., Bouvier Gallacchi M., Goehring C., Künzi B., Bovier P.A. Use of Tobacco and Alcohol by Swiss Primary Care Physicians: A Cross-Sectional Survey. BMC Public Health. 2007;7:5. doi: 10.1186/1471-2458-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Sharma T.D. Smoking Declines in a Group of Indian Doctors. World Health Forum. 1988;9:219–220. [PubMed] [Google Scholar]
- 167.Shkedy Y., Feinmesser R.M., Mizrachi A. Smoking Habits among Israeli Hospital Doctors: A Survey and Historical Review. Isr. Med. Assoc. J. 2013;15:339–341. [PubMed] [Google Scholar]
- 168.Shishani K., Nawafleh H., Sivarajan Froelicher E. Jordanian Nurses’ and Physicians’ Learning Needs for Promoting Smoking Cessation. Prog. Cardiovasc. Nurs. 2008;23:79–83. doi: 10.1111/j.1751-7117.2008.07745.x. [DOI] [PubMed] [Google Scholar]
- 169.Shishani K., Nawafleh H., Jarrah S., Froelicher E.S. Smoking Patterns among Jordanian Health Professionals: A Study about the Impediments to Tobacco Control in Jordan. Eur. J. Cardiovasc. Nurs. J. 2011;10:221–227. doi: 10.1016/j.ejcnurse.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 170.Siddiqui S., Ogbeide D.O. Profile of Smoking amongst Health Staff in a Primary Care Unit at a General Hospital in Riyadh, Saudi Arabia. Saudi Med. J. 2001;22:1101–1104. [PubMed] [Google Scholar]
- 171.Singh G., Singh R., Jindal K.C. Drug Use among Physicians and Medical Students. Indian J. Med. Res. 1981;73:594–602. [PubMed] [Google Scholar]
- 172.Smith D.R., Wei N., Zhang Y.-J., Wang R.-S. Tobacco Smoking Habits among a Cross-Section of Rural Physicians in China. Aust. J. Rural Health. 2006;14:66–71. doi: 10.1111/j.1440-1584.2006.00766.x. [DOI] [PubMed] [Google Scholar]
- 173.Smith D.R., Leggat P.A. Tobacco Smoking Was Dramatically Reduced among New Zealand Health Care Workers between 1963 and 1996, but What Happened after That? N. Z. Med. J. 2007;120:U2758. [PubMed] [Google Scholar]
- 174.Sotiropoulos A., Gikas A., Spanou E., Dimitrelos D., Karakostas F., Skliros E., Apostolou O., Politakis P., Pappas S. Smoking Habits and Associated Factors among Greek Physicians. Public Health. 2007;121:333–340. doi: 10.1016/j.puhe.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 175.Squier C., Hesli V., Lowe J., Ponamorenko V., Medvedovskaya N. Tobacco Use, Cessation Advice to Patients and Attitudes to Tobacco Control among Physicians in Ukraine. Eur. J. Cancer Prev. 2006;15:458–463. doi: 10.1097/00008469-200610000-00012. [DOI] [PubMed] [Google Scholar]
- 176.Stuyt E.B., Gundersen D.C., Shore J.H., Brooks E., Gendel M.H. Tobacco Use by Physicians in a Physician Health Program, Implications for Treatment and Monitoring. Am. J. Addict. 2009;18:103–108. doi: 10.1080/10550490902773015. [DOI] [PubMed] [Google Scholar]
- 177.Sundquist J., Johansson S.E. Impaired Health Status, and Mental Health, Lower Vitality and Social Functioning in Women General Practitioners in Sweden. A Cross-Sectional Survey. Scand. J. Prim. Health Care. 1999;17:81–86. doi: 10.1080/028134399750002692. [DOI] [PubMed] [Google Scholar]
- 178.Tapia-Conyer R., Cravioto P., de la Rosa B., Galván F., García-de la Torre G., Kuri P. Cigarette Smoking; Knowledge and Attitudes among Mexican Physicians. Salud Publica Mex. 1997;39:507–512. doi: 10.1590/S0036-36341997000600003. [DOI] [PubMed] [Google Scholar]
- 179.Tee G.H. Changing Habits and Attitudes Towards Smoking among Future Physicians. Med. J. Malays. 2007;62:5. [PubMed] [Google Scholar]
- 180.Tessier J.F., Thomas D., Nejjari C., Belougne D., Freour P. Attitudes of French cardiologists towards smoking. Arch. Mal. Coeur Vaiss. 1996;89:341–347. doi: 10.1007/BF01720293. [DOI] [PubMed] [Google Scholar]
- 181.Thomas I., Gupta S., Sempos C., Cooper R. Serum Lipids of Indian Physicians Living in the U.S. Compared to U.S.-Born Physicians. Atherosclerosis. 1986;61:99–106. doi: 10.1016/0021-9150(86)90068-7. [DOI] [PubMed] [Google Scholar]
- 182.Tomson T., Boupha K., Gilljam H., Helgason Á.R. Knowledge, Attitudes and Smoking Behavior among Lao Doctors. Southeast Asian J. Trop. Med. Public Health. 2003;34:213–219. [PubMed] [Google Scholar]
- 183.Tong E.K., Strouse R., Hall J., Kovac M., Schroeder S.A. National Survey of U.S. Health Professionals’ Smoking Prevalence, Cessation Practices, and Beliefs. Nicotine Tob. Res. 2010;12:724–733. doi: 10.1093/ntr/ntq071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Tosun O., Dabak R., Sargin M., Dolapcioglu C., Ahishali E. Frequency of Irritable Bowel Syndrome Among Healthcare Personnel. Gastroenterol. Nurs. 2016;39:227–231. doi: 10.1097/SGA.0000000000000188. [DOI] [PubMed] [Google Scholar]
- 185.Trédaniel J., Karsenty S., Chastang C., Slama K., Hirsch A. Smoking habits of French general practitioners. Results of a representative sample of 1012 physicians. Rev. Mal. Respir. 1993;10:35–38. [PubMed] [Google Scholar]
- 186.Ulbricht S., Baumeister S., Meyer C., Schmidt C., Schumann A., Rumpf H., John U. Does the Smoking Status of General Practitioners Affect the Efficacy of Smoking Cessation Counselling? Patient Educ. Couns. 2009;74:23–28. doi: 10.1016/j.pec.2008.07.047. [DOI] [PubMed] [Google Scholar]
- 187.Underner M., Laforgue A.-V., Chabaud F., Meurice J.-C. Influence of doctors’ smoking habits on minimal advice for smoking cessation. A survey of 369 general practitioners in the department of Vienne, France. Presse Med. 2004;33:927–929. doi: 10.1016/S0755-4982(04)98796-9. [DOI] [PubMed] [Google Scholar]
- 188.Underner M., Ingrand P., Allouch A., Laforgue A.V., Migeot V., Defossez G., Meurice J.C. Influence of smoking among family physicians on their practice of giving minimal smoking cessation advice. Rev. Mal. Respir. 2006;23:426–429. doi: 10.1016/S0761-8425(06)71812-5. [DOI] [PubMed] [Google Scholar]
- 189.Uysal M.A., Dilmen N., Karasulu L., Demir T. Smoking Habits among Physicians in Istanbul and Their Attitudes Regarding Anti-Smoking Legislation. Tuberk. Ve Toraks. 2007;55:350–355. [PubMed] [Google Scholar]
- 190.Vanderhoek A.J., Hammal F., Chappell A., Wild T.C., Raupach T., Finegan B.A. Future Physicians and Tobacco: An Online Survey of the Habits, Beliefs and Knowledge Base of Medical Students at a Canadian University. Tob. Induc. Dis. 2013;11:9. doi: 10.1186/1617-9625-11-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Vanphanom S., Morrow M., Phengsavanh A., Hansana V., Phommachanh S., Tomson T. Smoking among Lao Medical Doctors: Challenges and Opportunities for Tobacco Control. Tob. Control. 2011;20:144–150. doi: 10.1136/tc.2009.035196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Viegas C.A.D.A., de Andrade A.P.A., Silvestre R.D.S. Characteristics of Smoking among Physicians in the Federal District of Brazil. J. Bras. Pneumol. 2007;33:76–80. doi: 10.1590/S1806-37132007000100015. [DOI] [PubMed] [Google Scholar]
- 193.Voigt K., Twork S., Mittag D., Göbel A., Voigt R., Klewer J., Kugler J., Bornstein S.R., Bergmann A. Consumption of Alcohol, Cigarettes and Illegal Substances among Physicians and Medical Students in Brandenburg and Saxony (Germany) BMC Health Serv. Res. 2009;9:219. doi: 10.1186/1472-6963-9-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Waalkens H.J., Cohen Schotanus J., Adriaanse H., Knol K. Smoking Habits in Medical Students and Physicians in Groningen, The Netherlands. Eur. Respir. J. 1992;5:49–52. [PubMed] [Google Scholar]
- 195.Wyshak G., Lamb G.A., Lawrence R.S., Curran W.J. A Profile of the Health-Promoting Behaviors of Physicians and Lawyers. N. Engl. J. Med. 1980;303:104–107. doi: 10.1056/NEJM198007103030210. [DOI] [PubMed] [Google Scholar]
- 196.Yaacob I., Abdullah Z.A. Smoking Habits and Attitudes among Doctors in a Malaysian Hospital. Southeast Asian J. Trop. Med. Public Health. 1993;24:28–31. [PubMed] [Google Scholar]
- 197.Yan J., Xiao S., Ouyang D., Jiang D., He C., Yi S. Smoking Behavior, Knowledge, Attitudes and Practice among Health Care Providers in Changsha City, China. Nicotine Tob. Res. 2008;10:737–744. doi: 10.1080/14622200801901930. [DOI] [PubMed] [Google Scholar]
- 198.Young J.M., Ward J.E. Declining Rates of Smoking among Medical Practitioners. Med. J. Aust. 1997;167:232. doi: 10.5694/j.1326-5377.1997.tb138866.x. [DOI] [PubMed] [Google Scholar]
- 199.Zabadi H.A., Musmar S., Hassouna A., Shtaiwi D. Cigarettes and Water Pipe Smoking Prevalence, Knowledge, and Attitudes Among the Palestinian Physicians in the West Bank. Tob. Use Insights. 2018;11:1179173X18813369. doi: 10.1177/1179173X18813369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Zhang H. Cigarette Smoking among Chinese Medical Staff. Lancet Lond. Engl. 2015;385:1621. doi: 10.1016/S0140-6736(15)60792-9. [DOI] [PubMed] [Google Scholar]
- 201.Zhou J., Abdullah A.S., Pun V.C., Huang D., Lu S., Luo S. Smoking Status and Cessation Counseling Practices among Physicians, Guangxi, China, 2007. Prev. Chronic. Dis. 2010;7:A15. [PMC free article] [PubMed] [Google Scholar]
- 202.Zinonos S., Zachariadou T., Zannetos S., Panayiotou A.G., Georgiou A. Smoking Prevalence and Associated Risk Factors among Healthcare Professionals in Nicosia General Hospital, Cyprus: A Cross-Sectional Study. Tob. Induc. Dis. 2016;14:1–8. doi: 10.1186/s12971-016-0079-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Zylbersztejn H., Masson W., Lobo M.L., Manente D., García Aurelio M., Angel A., Mulassi A., Giorgi M., Rostán M.G. The TAMARA II Trial. Smoking Among Physicians in Argentina. Rev. Argent. Cardiol. 2015;83:222–231. doi: 10.7775/rac.v83.i3.5940. [DOI] [Google Scholar]
- 204.Amara B., El Ghazi K., Rahimi H., Elbiaze M., Nejjari C., Chakib Benjelloun M. Attitudes et connaissances des pneumo-phtisiologues marocains vis-à-vis du tabagisme chez leurs patients tuberculeux. Rev. Mal. Respir. 2008;25:569–575. doi: 10.1016/S0761-8425(08)71614-0. [DOI] [PubMed] [Google Scholar]
- 205.Nollen N.L., Adewale S., Okuyemi K.S., Ahluwalia J.S., Parakoyi A. Workplace Tobacco Policies and Smoking Cessation Practices of Physicians. J. Natl. Med. Assoc. 2004;96:838–842. [PMC free article] [PubMed] [Google Scholar]
- 206.Shi Y., Yu C., Luo A., Huang Y., Warner D.O. Perioperative Tobacco Interventions by Chinese Anesthesiologists: Practices and Attitudes. Anesthesiology. 2010;112:338–346. doi: 10.1097/ALN.0b013e3181c91ee7. [DOI] [PubMed] [Google Scholar]
- 207.Mohan S., Pradeepkumar A.S., Thresia C.U., Thankappan K.R., Poston W.S.C., Haddock C.K., Pinkston M.M., Muramoto M.L., Nichter M., Nichter M., et al. Tobacco Use among Medical Professionals in Kerala, India: The Need for Enhanced Tobacco Cessation and Control Efforts. Addict. Behav. 2006;31:2313–2318. doi: 10.1016/j.addbeh.2006.02.013. [DOI] [PubMed] [Google Scholar]
- 208.Varona P. Use of Medical Counseling for the Prevention and Control of Smoking in the Municipality of Old Havana. J. Urban Health Bull. N. Y. Acad. Med. 2005;82:71–75. doi: 10.1093/jurban/jti009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Easton A., Husten C., Elon L., Pederson L., Frank E. Non-Primary Care Physicians and Smoking Cessation Counseling: Women Physicians’ Health Study. Women Health. 2001;34:15–29. doi: 10.1300/J013v34n04_02. [DOI] [PubMed] [Google Scholar]
- 210.Jacot Sadowski I., Ruffieux C., Cornuz J. Self-Reported Smoking Cessation Activities among Swiss Primary Care Physicians. BMC Fam. Pract. 2009;10:22. doi: 10.1186/1471-2296-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Oztürk O., Yılmazer I., Akkaya A. The Attitudes of Surgeons Concerning Preoperative Smoking Cessation: A Questionnaire Study. Hippokratia. 2012;16:124–129. [PMC free article] [PubMed] [Google Scholar]
- 212.Schnoll R.A., Engstrom P.F., Subramanian S., Demidov L., Wielt D.B. Smoking Cessation Counseling by Russian Oncologists: Opportunities for Intervention in the Russian Federation. Int. J. Behav. Med. 2006;13:8–15. doi: 10.1207/s15327558ijbm1301_2. [DOI] [PubMed] [Google Scholar]
- 213.Steinberg M.B., Nanavati K., Delnevo C.D., Abatemarco D.J. Predictors of Self-Reported Discussion of Cessation Medications by Physicians in New Jersey. Addict. Behav. 2007;32:3045–3053. doi: 10.1016/j.addbeh.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 214.Thankappan K.R., Pradeepkumar A.S., Nichter M. Doctors’ Behaviour & Skills for Tobacco Cessation in Kerala. Indian J. Med. Res. 2009;129:249–255. [PubMed] [Google Scholar]
- 215.An L. Treatment of Tobacco Use as a Chronic Medical Condition: Primary Care Physicians’ Self-Reported Practice Patterns. Prev. Med. 2004;38:574–585. doi: 10.1016/j.ypmed.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 216.Power B., Neilson S., Perry I.J. Perception of the Risks of Smoking in the General Population and among General Practitioners in Ireland. Ir. J. Med. Sci. 2004;173:141–144. doi: 10.1007/BF03167928. [DOI] [PubMed] [Google Scholar]
- 217.Willaing I., Jørgensen T., Iversen L. How Does Individual Smoking Behaviour among Hospital Staff Influence Their Knowledge of the Health Consequences of Smoking? Scand. J. Public Health. 2003;31:149–155. doi: 10.1080/14034940210164876. [DOI] [PubMed] [Google Scholar]
- 218.McEwen A., West R. Smoking Cessation Activities by General Practitioners and Practice Nurses. Tob. Control. 2001;10:27–32. doi: 10.1136/tc.10.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Hepburn M.J., Johnson J.M., Ward J.A., Longfield J.N. A Survey of Smoking Cessation Knowledge, Training, and Practice among U.S. Army General Medical Officers. Am. J. Prev. Med. 2000;18:300–304. doi: 10.1016/S0749-3797(00)00123-9. [DOI] [PubMed] [Google Scholar]
- 220.Zanetti F. Smoking Habits, Exposure to Passive Smoking and Attitudes to a Non-Smoking Policy among Hospital Staff. Public Health. 1998;112:57–62. doi: 10.1016/S0033-3506(98)00208-X. [DOI] [PubMed] [Google Scholar]
- 221.Roche A.M., Parle M.D., Saunders J.B. Managing Alcohol and Drug Problems in General Practice: A Survey of Trainees’ Knowledge, Attitudes and Educational Requirements. Aust. N. Z. J. Public Health. 1996;20:401–408. doi: 10.1111/j.1467-842X.1996.tb01053.x. [DOI] [PubMed] [Google Scholar]
- 222.Roche A.M., Parle M.D., Stubbs J.M., Hall W., Saunders J.B. Management and Treatment Efficacy of Drug and Alcohol Problems: What Do Doctors Believe? Addict. Abingdon Engl. 1995;90:1357–1366. doi: 10.1111/j.1360-0443.1995.tb03553.x. [DOI] [PubMed] [Google Scholar]
- 223.Hill H.A., Braithwaite R.L. Attitudes, Beliefs, and Practices Regarding Smoking and Smoking Cessation among African-American Physicians and Dentists. J. Natl. Med. Assoc. 1997;89:745–751. [PMC free article] [PubMed] [Google Scholar]
- 224.Polyzos A., Gennatas C., Veslemes M., Daskalopoulou E., Stamatiadis D., Katsilambros N. The Smoking-Cessation Promotion Practices of Physician Smokers in Greece. J. Cancer Educ. 1995;10:78–81. doi: 10.1080/08858199509528339. [DOI] [PubMed] [Google Scholar]
- 225.Hussain S.F., Tjeder-Burton S., Campbell I.A., Davies P.D. Attitudes to Smoking and Smoking Habits among Hospital Staff. Thorax. 1993;48:174–175. doi: 10.1136/thx.48.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Brink S.G., Gottlieb N.H., McLeroy K.R., Wisotzky M., Burdine J.N. A Community View of Smoking Cessation Counseling in the Practices of Physicians and Dentists. Public Health Rep. 1994;109:135–142. [PMC free article] [PubMed] [Google Scholar]
- 227.Fowler G., Fuller A., Mant D., Jones L. The “Help Your Patient Stop” Initiative: Evaluation of Smoking Prevalence and Dissemination of WHO/UICC Guidelines in UK General Practice. Lancet. 1989;333:1253–1255. doi: 10.1016/S0140-6736(89)92342-8. [DOI] [PubMed] [Google Scholar]
- 228.Davies P.D., Rajan K. Attitudes to Smoking and Smoking Habit among the Staff of a Hospital. Thorax. 1989;44:378–381. doi: 10.1136/thx.44.5.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Linn L.S., Yager J., Cope D., Leake B. Health Habits and Coping Behaviors among Practicing Physicians. West. J. Med. 1986;144:484–489. [PMC free article] [PubMed] [Google Scholar]
- 230.Sachs D.P. Smoking Habits of Pulmonary Physicians. N. Engl. J. Med. 1983;309:799. doi: 10.1056/NEJM198309293091321. [DOI] [PubMed] [Google Scholar]
- 231.Seiler E.R. Smoking Habits of Doctors and Their Spouses in South East Scotland. J. R. Coll. Gen. Pract. 1983;33:598. [PMC free article] [PubMed] [Google Scholar]
- 232.Senior S.L. Study of Smoking Habits in Hospital and Attitudes of Medical Staff towards Smoking. Can. Med. Assoc. J. 1982;126:131–133. [PMC free article] [PubMed] [Google Scholar]
- 233.Dodds A.M., Rankin D.W., Hill D.J., Gray N.J. Attitudes and Smoking Habits of Doctors in Victoria. Community Health Stud. 1979;3:28–31. doi: 10.1111/j.1753-6405.1979.tb00227.x. [DOI] [Google Scholar]
- 234.Abdullah A.S.M., Rahman M.A.S.M., Suen C.W., Wing L.S., Ling L.W., Mei L.Y., Tat L.C., Tai M.N., Wing T.N., Yuen W.T., et al. Investigation of Hong Kong Doctors’ Current Knowledge, Beliefs, Attitudes, Confidence and Practices: Implications for the Treatment of Tobacco Dependency. J. Chin. Med. Assoc. 2006;69:461–471. doi: 10.1016/S1726-4901(09)70310-7. [DOI] [PubMed] [Google Scholar]
- 235.Shin S.S., Xiao D., Cao M., Wang C., Li Q., Chai W.-X., Lindsay R.P., Usita P., Novotny T.E. Patient and Doctor Perspectives on Incorporating Smoking Cessation into Tuberculosis Care in Beijing, China. Int. J. Tuberc. Lung Dis. 2012;16:126–131. doi: 10.5588/ijtld.11.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Zhang C., Xiao D., West R., Michie S., Troughton R., Hajek P., Wang C. Evaluation of 3-Day Smoking Cessation Training Course for Doctors from 38 Cities in China. Chin. Med. J. 2012;125:1338–1340. [PubMed] [Google Scholar]
- 237.Miwa K., Fujita M., Miyagi Y., Inoue H., Sasayama S. Is Smoking Behaviour in Patients with Coronary Heart Disease Influenced by Whether Their Attending Physician Smokes? Tob. Control. 1995;4:236–238. doi: 10.1136/tc.4.3.236. [DOI] [Google Scholar]
- 238.Wada K., Sakata Y., Theriault G., Narai R., Yoshino Y., Tanaka K., Aizawa Y. Associations of Excessive Sleepiness on Duty with Sleeping Hours and Number of Days of Overnight Work among Medical Residents in Japan. J. Occup. Health. 2007;49:523–527. doi: 10.1539/joh.49.523. [DOI] [PubMed] [Google Scholar]
- 239.Wada K. Lifestyle Habits among Physicians Working AtHospitals in Japan. JMAJ. 2011;54:318–324. [Google Scholar]
- 240.Kai T., Maki T., Takahashi S., Warner D. Perioperative Tobacco Use Interventions in Japan: A Survey of Thoracic Surgeons and Anaesthesiologists. Br. J. Anaesth. 2008;100:404–410. doi: 10.1093/bja/aem400. [DOI] [PubMed] [Google Scholar]
- 241.Ng N., Prabandari Y.S., Padmawati R.S., Okah F., Haddock C.K., Nichter M., Nichter M., Muramoto M., Poston W.S.C., Pyle S.A., et al. Physician Assessment of Patient Smoking in Indonesia: A Public Health Priority. Tob. Control. 2007;16:190–196. doi: 10.1136/tc.2006.018895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Mejia R., Martinez V.G., Gregorich S.E., Pérez-Stable E.J. Physician Counseling of Pregnant Women about Active and Secondhand Smoking in Argentina. Acta Obstet. Gynecol. Scand. 2010;89:490–495. doi: 10.3109/00016341003739567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Al Shahrani A.S., Almudaiheem N.R., Bakhsh E.M., Sarhan N.T., Aldossari F.S., bin Huzeim B.A. Understanding Smoking Behavior among Physicians in Riyadh, Saudi Arabia: A Cross-Sectional Study. Tob. Use Insights. 2021;14:1179173X211006652. doi: 10.1177/1179173X211006652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Carlos S., Rico-Campà A., de la Fuente-Arrillaga C., Echavarri M., Fernandez-Montero A., Gea A., Salazar C., Martínez-González M.A. Do Healthy Doctors Deliver Better Messages of Health Promotion to Their Patients?: Data from the SUN Cohort Study. Eur. J. Public Health. 2020;30:466–472. doi: 10.1093/eurpub/ckaa019. [DOI] [PubMed] [Google Scholar]
- 245.Pillay R., Rathish B., Philips G.M., Kumar R.A., Francis A. Cardiovascular and Stroke Disease Risk among Doctors: A Cross-Sectional Study. Trop. Doct. 2020;50:232–234. doi: 10.1177/0049475520911233. [DOI] [PubMed] [Google Scholar]
- 246.Põld M., Pärna K. Nicotine Dependence and Factors Related to Smoking Cessation among Physicians in Estonia. Int. J. Environ. Res. Public. Health. 2020;17:3217. doi: 10.3390/ijerph17093217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Wang Q., Zhang X., Wang Z., Feng S., Li Y., Zhang C., Wang C. Doctors’ Smoking Control Knowledge, Attitudes and Practices: A Cross-Sectional Study Conducted in Shandong Province, China. BMC Public Health. 2021;21:73. doi: 10.1186/s12889-020-10076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Wilson H.H.K., Norris R., Tapley A., Magin P., Klein L. Role Legitimacy, Comfort and Confidence Providing Tobacco, Alcohol and Other Drug Care: A Cross-Sectional Study of Australian Early-Career General Practitioners. Educ. Prim. Care. 2021;32:19–26. doi: 10.1080/14739879.2020.1830720. [DOI] [PubMed] [Google Scholar]
- 249.Wilf Miron R., Malatskey L., Rosen L.J. Health-Related Behaviours and Perceptions among Physicians: Results from a Cross-Sectional Study in Israel. BMJ Open. 2019;9:e031353. doi: 10.1136/bmjopen-2019-031353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Movsisyan N.K., Petrosyan V., Abelyan G., Sochor O., Baghdasaryan S., Etter J.-F. Learning to Assist Smokers through Encounters with Standardized Patients: An Innovative Training for Physicians in an Eastern European Country. PLoS ONE. 2019;14:e0222813. doi: 10.1371/journal.pone.0222813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Kaetsu A., Fukushima T., Moriyama M., Shigematsu T. Change of the Smoking Behavior and Related Lifestyle Variables among Physicians in Fukuoka, Japan: A Longitudinal Study. J. Epidemiol. 2002;12:208–216. doi: 10.2188/jea.12.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Cao Y., Kenfield S., Song Y., Rosner B., Qiu W., Sesso H.D., Gaziano J.M., Ma J. Cigarette Smoking Cessation and Total and Cause-Specific Mortality: A 22-Year Follow-up Study among US Male Physicians. Arch. Intern. Med. 2011;171:1956–1959. doi: 10.1001/archinternmed.2011.539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Innos K., Rahu K., Baburin A., Rahu M. Cancer Incidence and Cause-Specific Mortality in Male and Female Physicians: A Cohort Study in Estonia. Scand. J. Public Health. 2002;30:133–140. doi: 10.1177/14034948020300020701. [DOI] [PubMed] [Google Scholar]
- 254.Kono S., Ikeda M., Tokudome S., Nishizumi M., Kuratsune M. Smoking and Mortalities from Cancer, Coronary Heart Disease and Stroke in Male Japanese Physicians. J. Cancer Res. Clin. Oncol. 1985;110:161–164. doi: 10.1007/BF00402732. [DOI] [PubMed] [Google Scholar]
- 255.Manson J.E., Ajani U.A., Liu S., Nathan D.M., Hennekens C.H. A Prospective Study of Cigarette Smoking and the Incidence of Diabetes Mellitus among US Male Physicians. Am. J. Med. 2000;109:538–542. doi: 10.1016/S0002-9343(00)00568-4. [DOI] [PubMed] [Google Scholar]
- 256.Rurik I., Kalabay L. Morbidity, Demography, Life Style, and Self-Perceived Health of Hungarian Medical Doctors 25 Years after Graduation. Med. Sci. Monit. 2008;14:SR1–SR8. [PubMed] [Google Scholar]
- 257.Rurik I., Szigethy E., Langmár Z. Medical Doctors in Hungary: 30 Years after Graduation. Data on Lifestyle, Morbidity, Demography and Differences between Specialties. Cent. Eur. J. Public Health. 2014;22:183–188. doi: 10.21101/cejph.a3910. [DOI] [PubMed] [Google Scholar]
- 258.Svärdsudd K., Wedel H., Gordh T. Mortality Rates among Swedish Physicians: A Population-Based Nationwide Study with Special Reference to Anesthesiologists. Acta Anaesthesiol. Scand. 2002;46:1187–1195. doi: 10.1034/j.1399-6576.2002.461003.x. [DOI] [PubMed] [Google Scholar]
- 259.Thomas J., Thomas D.J., Pearson T., Klag M., Mead L. Cardiovascular Disease in African American and White Physicians: The Meharry Cohort and Meharry-Hopkins Cohort Studies. J. Health Care Poor Underserved. 1997;8:270–283. doi: 10.1353/hpu.2010.0526. discussion 284. [DOI] [PubMed] [Google Scholar]
- 260.Torre D.M., Wang N.-Y., Meoni L.A., Young J.H., Klag M.J., Ford D.E. Suicide Compared to Other Causes of Mortality in Physicians. Suicide Life. Threat. Behav. 2005;35:146–153. doi: 10.1521/suli.35.2.146.62878. [DOI] [PubMed] [Google Scholar]
- 261.Unal S., Tanriover M.D., Ascioglu S., Demirkazik A., Ertenli I., Eskioglu E., Guler K., Kiraz S., Ozbakkaloglu M., Ozer B., et al. Turkish Doctors’ Cohort: Healthy despite Low Screening. Postgrad. Med. 2017;129:393–398. doi: 10.1080/00325481.2017.1272399. [DOI] [PubMed] [Google Scholar]
- 262.Mappin-Kasirer B., Pan H., Lewington S., Kizza J., Gray R., Clarke R., Peto R. Tobacco Smoking and the Risk of Parkinson Disease: A 65-Year Follow-up of 30,000 Male British Doctors. Neurology. 2020;94:e2132–e2138. doi: 10.1212/WNL.0000000000009437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Glavas D., Rumboldt M., Rumboldt Z. Smoking Cessation with Nicotine Replacement Therapy among Health Care Workers: Randomized Double-Blind Study. Croat. Med. J. 2003;44:219–224. [PubMed] [Google Scholar]
- 264.Saadat H., Snow D., Ottenheimer S., Dai F., Kain Z. Wellness Program for Anesthesiology Residents: A Randomized, Controlled Trial. Acta Anaesthesiol. Scand. 2012;56:1130–1138. doi: 10.1111/j.1399-6576.2012.02705.x. [DOI] [PubMed] [Google Scholar]
- 265.Goffette C. Déterminants individuels et contextuels de la consommation de tabac. Rev. Fr. Sociol. 2016;57:213–239. doi: 10.3917/rfs.572.0213. [DOI] [Google Scholar]
- 266.Le Faou A.-L. Tabac et Populations Défavorisées. Courr. Addict. 2002;4:10–14. [Google Scholar]
- 267.Dutheil F., Aubert C., Pereira B., Dambrun M., Moustafa F., Mermillod M., Baker J.S., Trousselard M., Lesage F.-X., Navel V. Suicide among Physicians and Health-Care Workers: A Systematic Review and Meta-Analysis. PLoS ONE. 2019;14:e0226361. doi: 10.1371/journal.pone.0226361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Dasagi M., Mantey D.S., Harrell M.B., Wilkinson A.V. Self-Reported History of Intensity of Smoking Is Associated with Risk Factors for Suicide among High School Students. PLoS ONE. 2021;16:e0251099. doi: 10.1371/journal.pone.0251099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Nabe-Nielsen K., Quist H.G., Garde A.H., Aust B. Shiftwork and Changes in Health Behaviors. J. Occup. Environ. Med. 2011;53:1413–1417. doi: 10.1097/JOM.0b013e31823401f0. [DOI] [PubMed] [Google Scholar]
- 270.Baggett T.P., McGlave C., Kruse G.R., Yaqubi A., Chang Y., Rigotti N.A. SmokefreeTXT for Homeless Smokers: Pilot Randomized Controlled Trial. JMIR MHealth UHealth. 2019;7:e13162. doi: 10.2196/13162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Pinsker E.A., Hennrikus D.J., Erickson D.J., Call K.T., Forster J.L., Okuyemi K.S. Trends in Self-Efficacy to Quit and Smoking Urges among Homeless Smokers Participating in a Smoking Cessation RCT. Addict. Behav. 2018;78:43–50. doi: 10.1016/j.addbeh.2017.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Dyrbye L.N., Thomas M.R., Shanafelt T.D. Systematic Review of Depression, Anxiety, and Other Indicators of Psychological Distress among U.S. and Canadian Medical Students. Acad. Med. 2006;81:354–373. doi: 10.1097/00001888-200604000-00009. [DOI] [PubMed] [Google Scholar]
- 273.Masson E. Alcoolisation à Risque Chez des étudiants en Médecine Parisiens. [(accessed on 6 June 2021)]. Available online: https://www.em-consulte.com/article/1133310/alcoolisation-a-risque-chez-des-etudiants-en-medec.
- 274.Fond G., Bourbon A., Auquier P., Micoulaud-Franchi J.-A., Lançon C., Boyer L. Venus and Mars on the Benches of the Faculty: Influence of Gender on Mental Health and Behavior of Medical Students. Results from the BOURBON National Study. J. Affect. Disord. 2018;239:146–151. doi: 10.1016/j.jad.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 275.Galleta-Williams H., Esmail A., Grigoroglou C., Zghebi S.S., Zhou A.Y., Hodkinson A., Panagioti M. The Importance of Teamwork Climate for Preventing Burnout in UK General Practices. Eur. J. Public Health. 2020;30:iv36–iv38. doi: 10.1093/eurpub/ckaa128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Wu A.W. Medical Error: The Second Victim. BMJ. 2000;320:726–727. doi: 10.1136/bmj.320.7237.726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Garrabé J. Le traumatisme du point de vue de la psychiatrie de la personne. J. Fr. Psychiatr. 2010;36:26. doi: 10.3917/jfp.036.0026. [DOI] [Google Scholar]
- 278.Galinowski A. L’annonce du diagnostic en psychiatrie. Laennec. 2011;59:44. doi: 10.3917/lae.113.0044. [DOI] [Google Scholar]
- 279.Weill A., Vallier N., Salanave B. La Fréquence Des 30 Affections de Longue Durée. Affect. Longue Durée. 2007;59:18–29. [Google Scholar]
- 280.Deriaz S., Bridel L. Profession médecin : Choix et perspectives selon le genre. Rev. Médicale Suisse. 2010;6:1438–1442. [PubMed] [Google Scholar]
- 281.Goodman J. Tobacco in History: The Cultures of Dependence. Routledge; London, UK: 1995. Reprinted. [Google Scholar]
- 282.Kirsch M. Génèse d’une Épidémie. Lett. Collège Fr. 2010;3:5–14. doi: 10.4000/lettre-cdf.278. [DOI] [Google Scholar]
- 283.Been J.V., Laverty A.A., Tsampi A., Filippidis F.T. European Progress in Working towards a Tobacco-Free Generation. Eur. J. Pediatr. 2021;180:3423–3431. doi: 10.1007/s00431-021-04116-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Commar A., Prasad V.K., Tursan d’Espaignet E., Wolfenden L. WHO Global Report on Trends in Prevalence of Tobacco Smoking 2000–2025. World Health Organization; Geneva, Switzerland: 2018. [Google Scholar]
- 285.World Bank . Poverty and Shared Prosperity 2020: Reversals of Fortune. The World Bank; Washington, DC, USA: 2020. [Google Scholar]
- 286.United Nations. Department of Economic and Social Affairs. Population Division . World Population Prospects Highlights, 2019 Revision Highlights, 2019 Revision. United Nations; New York, NY, USA: 2019. [Google Scholar]
- 287.Aubron C., Lehoux H., Lucas C. Pauvreté et inégalités en Inde rurale. Réflexion à partir de deux diagnostics agraires dans l’État du Gujarat. EchoGéo. 2015 doi: 10.4000/echogeo.14226. [DOI] [Google Scholar]
- 288.Giovino G.A., Mirza S.A., Samet J.M., Gupta P.C., Jarvis M.J., Bhala N., Peto R., Zatonski W., Hsia J., Morton J., et al. Tobacco Use in 3 Billion Individuals from 16 Countries: An Analysis of Nationally Representative Cross-Sectional Household Surveys. Lancet. 2012;380:668–679. doi: 10.1016/S0140-6736(12)61085-X. [DOI] [PubMed] [Google Scholar]
- 289.Health A.G.D. Tobacco Control—Key Facts and Figures. [(accessed on 25 June 2021)]; Available online: https://www.health.gov.au/resources/publications/tobacco-control-key-facts-and-figures.
- 290.Wilkinson A.V. Smoking Prevalence Following Tobacco Tax Increases in Australia between 2001 and 2017: An Interrupted Time-Series Analysis—The Lancet Public Health. Lancet Public Health. 2019;4:e618–e627. doi: 10.1016/S2468-2667(19)30203-8. [DOI] [PubMed] [Google Scholar]
- 291.Moodie C., Bauld L., Ford A., Mackintosh A. Young Women Smokers’ Response to Using Plain Cigarette Packaging: Qualitative Findings from a Naturalistic Study. BMC Public Health. 2014;14:812. doi: 10.1186/1471-2458-14-812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Brousse G., Zerhouni O., Perriot J., Bègue L., Flaudias V. [Plain Packaging: The study that makes tabacologists coff] L’Encephale. 2018;44:489–490. doi: 10.1016/j.encep.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 293.Health A.G.D. National Tobacco Campaign—Resources. [(accessed on 19 June 2021)]; Available online: https://www.health.gov.au/resources/collections/national-tobacco-campaign-resources.
- 294.Prohibiting Smoking in Motor Vehicles Carrying Children under 18 Years of Age. [(accessed on 20 June 2021)]; Available online: https://www.health.govt.nz/about-ministry/information-releases/regulatory-impact-statements/prohibiting-smoking-motor-vehicles-carrying-children-under-18-years-age.
- 295.WHO . WHO Framework Convention on Tobacco Control. WHO; Geneva, Switzerland: 2005. [Google Scholar]
- 296.World No Tobacco Day. [(accessed on 6 June 2021)]. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/tobacco/world-no-tobacco-day.
- 297.Article R6152-27—Code de La Santé Publique—Légifrance. [(accessed on 31 May 2021)]. Available online: https://www.legifrance.gouv.fr/codes/article_lc/LEGIARTI000031304375/
- 298.Clavier C., Hassenteufel P., Fuentes J.F.M., Schweyer F.-X. Les limites de la convergence du temps de travail des médecins hospitaliers en Europe (Allemagne, Danemark, Espagne, Lituanie, Royaume-Uni) Rev. Fr. Aff. Soc. 2011;2:226–251. doi: 10.3917/rfas.112.0226. [DOI] [Google Scholar]
- 299.Pallejà-Millán M., Rey-Reñones C., Barrera Uriarte M.L., Granado-Font E., Basora J., Flores-Mateo G., Duch J. Evaluation of the Tobbstop Mobile App for Smoking Cessation: Cluster Randomized Controlled Clinical Trial. JMIR MHealth UHealth. 2020;8 doi: 10.2196/15951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Gram I.T., Larbi D., Wangberg S.C. Comparing the Efficacy of an Identical, Tailored Smoking Cessation Intervention Delivered by Mobile Text Messaging Versus Email: Randomized Controlled Trial. JMIR MHealth UHealth. 2019;7:e12137. doi: 10.2196/12137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Rahman M.A., Hann N., Wilson A., Mnatzaganian G., Worrall-Carter L. E-Cigarettes and Smoking Cessation: Evidence from a Systematic Review and Meta-Analysis. PLoS ONE. 2015;10:e0122544. doi: 10.1371/journal.pone.0122544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Kushnir V., Sproule B.A., Cunningham J.A. Impact of Large-Scale Distribution and Subsequent Use of Free Nicotine Patches on Primary Care Physician Interaction. BMC Public Health. 2017;18:4. doi: 10.1186/s12889-017-4548-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Prise en Charge des Substituts Nicotiniques. [(accessed on 14 June 2021)]. Available online: https://www.ameli.fr/assure/remboursements/rembourse/medicaments-vaccins-dispositifs-medicaux/prise-charge-substituts-nicotiniques.
- 304.Nouvelle Campagne de Promotion de L’arrêt du Tabac: Et si 2021 était L’année où vous Arrêtez de Fumer? [(accessed on 14 June 2021)]. Available online: https://www.drogues.gouv.fr/actualites/nouvelle-campagne-de-promotion-de-larret-tabac-2021-etait-lannee-arretez-de-fumer.
- 305.Alla F., Berlin I., Nguyen-Thanh V., Guignard R., Pasquereau A., Quelet S., Schwarzinger M., Arwidson P. Tobacco and COVID-19: A Crisis within a Crisis? Can. J. Public Health. 2020;111:995–999. doi: 10.17269/s41997-020-00427-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Clair C. Genre et Disparités: L’exemple du Tabagisme. Rev. Med. Suisse. 2015;11:1298–1303. [PubMed] [Google Scholar]
- 307.Pasquereau A., Andler R., Guignard R., Richard J.-B., Arwidson P., Nguyen-Thanh V. La Consommation de Tabac En France: Premiers Résultats Du Baromètre Santé 2017. Sante Publique Fr. 2018;14–15:265–273. [Google Scholar]
- 308.Marques C., Quatremère G. Les fumeurs français: Qui sont-ils? Résultats du baromètre de santé publique France. Bull. Epidémiologique Hebd. 2020;14:291–294. [Google Scholar]
- 309.Sun M., Jiang Y., Sun C., Li J., Guo X., Lv Y., Yu Y., Yao Y., Jin L. The Associations between Smoking and Obesity in Northeast China: A Quantile Regression Analysis. Sci. Rep. 2019;9:3732. doi: 10.1038/s41598-019-39425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.AL Reshidi F.S. Level of Physical Activity of Physicians among Residency Training Program at Prince Sultan Military Medical City, Riyadh, KSA 2014. Int. J. Health Sci. 2016;10:39–47. doi: 10.12816/0031215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Olson S.M., Odo N.U., Duran A.M., Pereira A.G., Mandel J.H. Burnout and Physical Activity in Minnesota Internal Medicine Resident Physicians. J. Grad. Med. Educ. 2014;6:669–674. doi: 10.4300/JGME-D-13-00396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Ramsey M.W., Chen-Sankey J.C., Reese-Smith J., Choi K. Association between Marital Status and Cigarette Smoking: Variation by Race and Ethnicity. Prev. Med. 2019;119:48–51. doi: 10.1016/j.ypmed.2018.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313.Saraç F., Öztekin K., Çelebi G. Early Menopause Association with Employment, Smoking, Divorced Marital Status and Low Leptin Levels. Gynecol. Endocrinol. 2011;27:273–278. doi: 10.3109/09513590.2010.491165. [DOI] [PubMed] [Google Scholar]
- 314.Lipinska M. Histoire Des Femmes Médecins Depuis l’Antiquité Jusqu’à Nos Jours. Wentworth Press; Paris, France: 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All relevant data are within the paper.