Abstract
Exosomes are nano-sized extracellular vesicles produced and released by almost all cell types. They play an essential role in cell–cell communications by delivering cellular bioactive compounds such as functional proteins, metabolites, and nucleic acids, including microRNA, to recipient cells. Thus, they are involved in various physio-pathological conditions. Exosome-miRNAs are associated with numerous diseases, including type 2 diabetes, a complex multifactorial metabolic disorder linked to obesity. In addition, exosome-miRNAs are emerging as essential regulators in the progression of diabetes, principally for pancreatic β-cell injury and insulin resistance. Here, we have clustered the recent findings concerning exosome-miRNAs associated with β-cell dysfunction to provide a novel approach for the early diagnosis and therapy of diabetes.
Keywords: diabetes, exosomes, insulin resistance, miRNAs, therapy
1. Introduction
Diabetes is a metabolic disorder stemming from defective insulin secretion and the occurrence of insulin resistance in peripheral tissues. Obesity, dietary fat intake, and physical inactivity are recognized as the main risk factors [1,2]. The close link between obesity and the development of this metabolic disorder have led to the creation of the new term “diabesity”, which combines the burden of obesity and diabetes [3]. This condition will affect more than 650 million people by 2045, with a concomitant increase in sanitary health costs concerning diabesity-related diseases [4,5,6]. Despite the considerable advancement in the understanding and treatment of diabetes, the correlated morbidity and mortality rates have continued to increase. Therefore, there is an urgent need for biomarkers to improve the clinical diagnostic process and the therapeutic approach of diabetes [7].
A number of extracellular vesicles (EVs) exist in all human fluids [8,9]. Their classification is based on their size: (i) large EVs (diameter > 200 nm) and (ii) small EVs (diameter < 200 nm) of which exosomes (30–150 nm) belong [10,11]. Exosomes are broadly present in human body fluids such as cerebrospinal fluid, urine, semen, saliva, and breast milk [12,13,14]. Exosomes can carry bioactive molecules and are essential for cell–cell communication [15,16].
With the conclusion of the Human Genome Project and the opening of the postgenomic era, non-coding RNAs (ncRNAs) have gained attention in numerous research fields [17,18,19]. miRNAs are a type of ncRNA with approximately 22 nucleotides encoded by endogenous genes [20]. They act as regulators of post-transcriptional gene expression by directing target mRNA cleavage or translational inhibition. More than one-third of human genes are thought to be regulated by miRNAs, revealing their involvement in various physiological and pathological processes. miRNAs are tissue-specific and more stable as compared with long non-coding RNAs (ln-RNAs) and messenger-RNAs (mRNAs) because of their shorter sequences [21,22]. miRNAs can be packaged within exosomes, which deliver and release them into target tissue cells. Of note, approximately 100 miRNAs have been identified in the exosomes produced by mast cells [23,24]. Exosome-miRNAs participate in normal physiological processes and are also involved in the occurrence and development of several diseases [25,26,27]. In this frame, they are emerging as crucial regulators in the onset and development of diabetes. Moreover, exosome-miRNAs released into systemic circulation can be used as diabetes markers because of their specificity and sensitivity [28,29]. In this review, we provide an overview on the role of exosome-miRNA-mediated mechanisms in the development of diabetes as established to date, outlining a hypothetical basis for the potential use of exosome-miRNA as diabetes healing targets and/or as a possible therapy themselves.
2. Characteristics of Exosome-miRNAs
The first observation of exosomes was by Trams et al. in 1981, who detected “small membranous vesicles in the supernatants of tumor cells cultured in vitro”. Those macrovesicles were called exosomes [30]. At that moment, it was believed that the function of exosomes was only for the waste disposal system for cells. Instead, further research has highlighted exosomes’ role in several biological processes encompassing the immune response, cell differentiation, and cancer [31,32]. Exosomes are a subtype of extracellular vesicles that can be identified based on their endosomal origin and their size, which ranges from 30 to 150 nm. Their biogenesis initiates with the formation of early endosomes by the inward budding of the cell membrane followed by the second inward budding of the endosomal membrane. The second inward budding results in the formation of late endosome (intraluminal vesicles). Late endosomes comprising intraluminal vesicles (ILVs) are identified as multivesicular bodies (MVBs). During the maturation phase from early endosome to MVBs, the cargoes are incorporated into ILVs through endosomal-sorting complex-dependent or endosomal-sorting complex-independent pathways. MVBs can be transported to the trans-Golgi network for endosome recycling, delivered to lysosomes for degradation, or move along microtubules to fuse with the plasma membrane and release exosomes into the extracellular space. MVB fusion with the cellular membrane is a fine-tuned process, which requires several crucial factors. Exosomal cargoes from the source cell can be further delivered to target cells via endocytosis, direct membrane fusion or receptor–ligand interactions [31]. Almost all mammalian cells produce and release exosomes, including the blood cells: (i) B lymphocytes, (ii) T lymphocytes, (iii) platelets, (iv) mast cells, and (v) dendritic cells, but also: epithelial cells, astrocytes, and neurons [33,34,35,36,37,38,39]. Exosomes have been reported in all biological fluids, and their composition reflects the metabolic state of the cell of origin. Of note, exosome can be selectively taken up by neighboring or distant cells far from their release, reprogramming the functional activity of the recipient cells through the delivery of bioactive molecules. Thus, exosomes and their biologically active cargoes may offer potential biomarkers of diagnosis and therapeutic targets in a range of diseases, such as chronic inflammation, cardiovascular and neurodegenerative diseases, cancer, obesity, and metabolic diseases [34]. In addition to specific proteins, exosomes also contain different patterns of RNAs that can be delivered to recipient cells. RNA sequencing analysis demonstrated that miRNAs were the most abundant in human plasma-derived exosomal RNA species [40]. Exosomes-miRNAs undergo unidirectional transfer between cells, leading to an intercellular trafficking network. The latter elicits transient or persistent phenotypic changes in recipient cells [41]. It was proven that after entering a target cell, miRNA released from the exosome can interact with the 3′-UTR region of the targeted mRNA, resulting in inhibition of the specific gene expression [42]. It is worth mentioning that in addition to miRNAs, long RNA species, especially long non-coding RNAs and circular RNAs, have recently been reported to exist in exosomes and affect a variety of biological processes, including the development of cancer [43].
Exosome-miRNAs circulating in body fluid can also act as biomarkers to mirror disease progression. Gathering evidence indicates that exosome-miRNAs are essential in developing diseases; therefore, their use as biomarkers for disease diagnosis, prognosis, and personalized therapy is becoming more apparent [44,45].
3. Dysregulation of Exosome-miRNAs in Diabetes
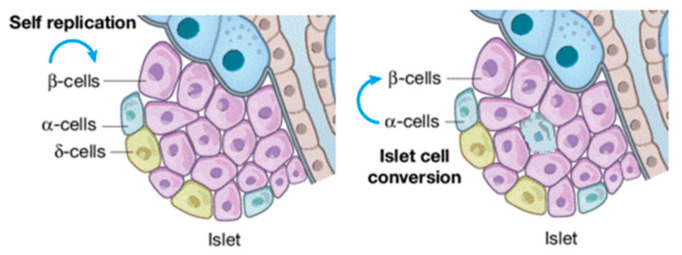
The continuous increase in diabetes prevalence and incidence renders this metabolic disorder a global public health emergency [5]. Diabetes can be categorized into: (i) type 1 diabetes, (ii) type 2 diabetes, also known as alimentary diabetes, and (iii) gestational diabetes (genetic types are rare). Chronic hyperglycemia reshapes islet cellular assets with the infiltration of α-cells in the core of β (Figure 1). More serious is the complication that long-term hyperglycemia does in the damage, dysfunction, and failure of multiple organs, particularly blood vessels, nerves, kidneys, heart, and eyes [46,47]. Therefore, consequences that can be recognized as diabetic are: (i) retinopathy, (ii) macro-vascular complications, (iii) nephropathy, (iv) cardiomyopathy, and (v) foot ulcers [48]. Diabetes-related morbidity and mortality can be reduced by the improvement of preventive care, early clinical diagnosis, and appropriate therapeutic approaches [48,49]. Hence, identifying effective biomarkers to prevent and treat diabetes earlier, as well as its complications, are needed. Since we are in the precision medicine era, increasing attention is being paid to diagnosing and treating diseases [17,30]. In this frame, exosomes are a useful tool for the early diagnosis and treatment of diseases, including diabetes [18,19,31,32]. Furthermore, several miRNAs are being identified in β-cell dysfunction and miRNAs, such as let-7, miR-29, miR-223, and miR-103, are able to control metabolism in disorders such as diabetes. Their modulatory effects involve multiple pathways, spanning from liver metabolism to the fine tuning of insulin secretion [50,51,52]. Protected exosomes-miRNAs also play a critical role in diabetes development and progression, and its associated complications which mostly yield pancreatic β-cell injury and insulin resistance [53,54,55,56,57,58].
Figure 1.
β-cell injuries reshape islet cellular assets.
4. Mechanism of Exosome-miRNAs in Diabetes Progression
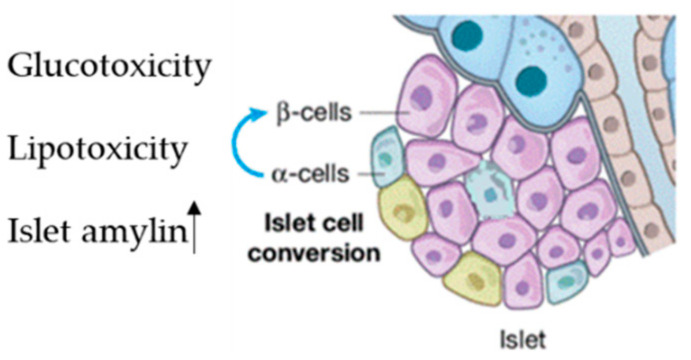
About 70% of pancreatic cells are β-cells, which play a fundamental role in sustaining blood glucose homeostasis via insulin secretion into systemic blood circulation [59]. β-dysfunction due to cell injury leads to the progression of diabetes [60]. This occurs in the early pre-diabetes stage and is characterized by three main mechanisms: (i) the first is hyperglycemia; (ii) the second is elevated free fatty acid levels; (iii) the third is high amylin levels, which is co-secreted with insulin and induces β-cell apoptosis [59] (Figure 2).
Figure 2.
Factor inducing islet reshaping, Lipo and glucotoxicity and increasing of islet amylin.
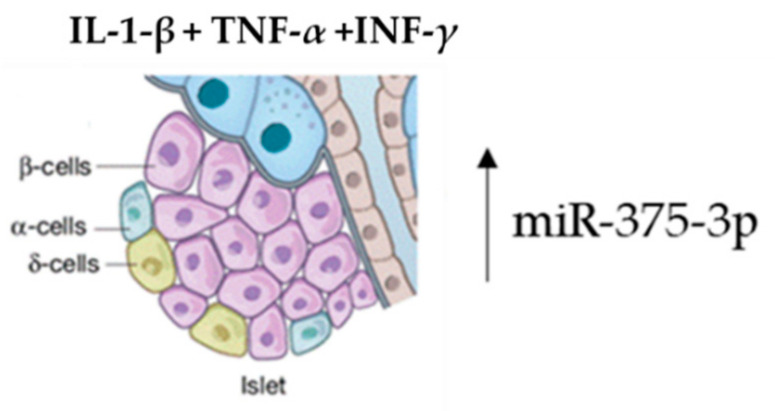
Several studies have proved that the enrichment of specific exosomal miRNAs can target genes having an essential conservation outcome on pancreatic β-cell function in the initial stages of diabetes. Both high glucose and fatty acid levels negatively regulate this pattern, determining an enrichment of exosome-specific miRNAs involved in β-cell dysfunction in diabetes [61,62,63]. Using an ICR mouse model, Fu et al. demonstrated that the concomitant administration of interleukin-1-beta (IL-1-β), tumor necrosis factor-alpha (TNF-α), and interferon-gamma (INF-γ) induced β-cell injury [64]. Islet tissue isolation from these mice and exosome-miRNA revealed a significant change in the miR-375-3p expression levels. Furthermore, this microRNA was also found to be higher in diabetes patients versus normoglycemic patients. Therefore, hsa-miR-375-3p could be considered as an early marker of islet injury (Figure 3).
Figure 3.
Acute β-cell injury using a mixture of cytokines induces an elevation of miR-375-3p.
The pool of exosome-miRNAs deriving from other cells can act on β-cells. This was demonstrated by treating MIN6B1 pancreatic cells with a mixture of IL-1-β, TNF-α and INF-γ cytokines. The exosome enrichment containing miRNAs, secreted in the medium, can be delivered to contiguous β-cells, inducing cell death [54].
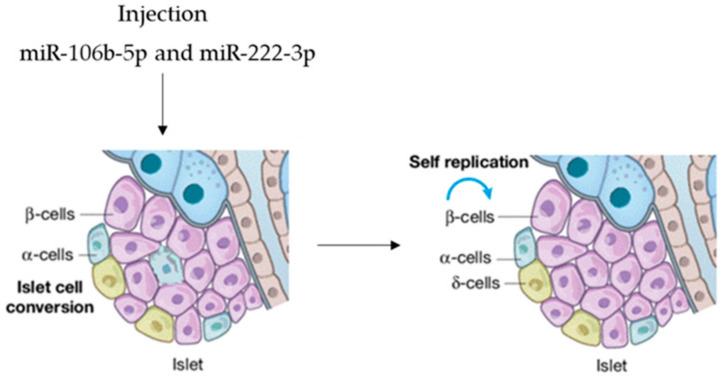
Tsukita et al. screened miRNA levels, pointing out significant changes in the serum exosomes of mice after bone marrow transplantation [65]. Forty-two miRNAs were upregulated after bone marrow transplantation, and of these, miR-106b-5p and miR-222-3p were released by bone marrow cells and transported to pancreatic islet cells, inducing β-cell renewal. In view of possible microRNA-based therapy, agomir miR-106b-5p and miR-222-3p were tail-vein-injected into mice, promoting the proliferation of injured β-cells. It was demonstrated that the injection of both miRNAs leads to the downregulation of the Cip/Kip family, which, in turn, improves hyperglycemia in insulin-deficient diabetes mice. This is evidence that they can function as a therapeutic option to rescue from β-cell dysfunction (Figure 4), so that circulating miRNAs are endocrine factors that facilitate metabolic organ crosstalk.
Figure 4.
microRNAs as therapeutic option.
Exosome-miRNAs secreted by β-cells can be transferred to other acceptor tissue cells which in turn regulates β-cell activity. For example, when exosome miR-26a [66] is transferred to the liver, it improves the insulin sensitivity of the acceptor cells, maintaining metabolic homeostasis. In addition, serum miR-204 is strictly associated with pancreatic β-cell injury, which could be helpful as a novel biomarker for early type 1 diabetes [67]. The findings indicate how exosome-miRNAs are strictly related to β-cell damage and dysfunction in diabetes.
Exosome-miRNAs and Insulin Resistance
Insulin resistance is a pathological condition in which target cells or tissues show reduced sensitivity or reactivity to insulin. It is a distinct feature of diabetes. Under this condition, the physiological levels of the hormone fail to preserve normal glucose homeostasis. Insulin resistance mainly occurs in fat, muscle, and liver cell populations, which use insulin to facilitate glucose uptake [68]. The condition is also characterized by the impairment of insulin signaling encompassing the insulin receptor, the insulin receptor substrate 1/2 (IRS-1/2), the glucose transporter 4 (GLUT4), and the phosphoinositide 3-kinase (PI3K)/AKT serine/threonine kinase (AKT) [69,70,71,72]. The mechanism underlying insulin resistance involves oxidative stress, inflammation, and autophagy. Recently, it has been shown that miRNAs in exosomes contribute to the mechanism of insulin resistance [73,74,75,76,77,78] and high expression of miR-20b-5p in exosomes from diabetic patients was also found. This miRNA modulates glucose metabolism in human skeletal muscle cells through AKT signaling, thus regulating the incidence of insulin resistance [79]. In agreement with these data, a further study pointed out that pancreatic-cancer-derived exosomes miR-450b-3p and miR-151-3p entering in myoblast C2C12 mouse cells can inhibit PI3K/AKT signaling. This mechanism inhibits Glut4 transport and sustains insulin-induced FoxO1 rejection [80]. Furthermore, it was demonstrated that exosomes miR-27a and miR-320a are correlated with metabolic syndrome and diabetes. Exosomes miR-23a, miR-197, and miR-509-5p are linked to dyslipidemia [81]. Exosome-miRNAs are strictly related to aging insulin resistance. In this frame, the involvement of exosome miR-29b-3p from bone marrow mesenchymal stem cells has been reported and its potential role as a therapeutic tool in senescence-induced insulin resistance has also been suggested. Obesity is a further high-risk factor in the occurrence of insulin resistance. Obesity deeply affects the expression profile of plasma exosome-miRNAs in mice and humans [82,83]. In mice, it was reported that the expression of plasma exosome-miRNAs in obese mice compared with lean mice, including miR-27a-3p, miR-27b-3p, miR-122, and miR-192, was increased. Furthermore, glucose tolerance was induced in lean mice exposed to exosomes isolated from obese mice [84]. In line with this evidence, Ying et al. showed that adipose tissue macrophages in obese mice secrete miRNA-containing exosomes, which cause glucose intolerance and insulin resistance when administered to lean mice. The opposite is also true. Altogether, these findings unveil the pivotal role of exosome miRNAs in the pathogenetic mechanisms of insulin resistance [85]. microRNAs involved in metabolic syndrome are summarized in Table 1.
Table 1.
Exosome-miRNA involved in the metabolic syndrome. For each miRNA, the cell of origin and the site of action are reported. BM-MSC, bone marrow mesenchymal stem cells.
| Exosome-miRNA | Cell Type Origin | Action Site | References |
|---|---|---|---|
| Let-7 | Immune cells, Endothelial cells | Liver cells, Pancreatic β-cells | [50] |
| miR-29 | Pancreatic β-cells, Adipocytes, Hepatocytes | Liver cells, Pancreatic β-cells | [52] |
| miR-223 | Pre-adipocytes, Adipocytes, Macrophages | Liver cells, Pancreatic β-cells | [51] |
| miR-103 | Adipocytes, BM-derived stromal cells | Liver cells, Pancreatic β-cells | [53] |
| miR-375-3p | Pancreatic β-cells | Pancreatic β-cells | [63,64] |
| miR-106b-5p | BM-MSC | Pancreatic β-cells | [65] |
| miR-222-3p | BM-MSC | Pancreatic β-cells | [65] |
| miR-26a | Adipocytes, Hepatocytes, Vascular endothelial cells | Pancreatic β-cells | [66] |
| miR-20b-5p | Adipocytes, Hepatocytes | Skeletal muscle cells | [79] |
| miR-27a/b-3p | Endothelial cells, Adipocytes, Hepatocytes Glomerular mesangial cells |
Liver cells Adipocytes |
[82,83] |
| miR-320a | Adipocytes, Hepatocytes, Macrophages, Neutrophils |
Liver cells, Adipocytes, Myocytes | [81,82] |
| miR-23a | Macrophages, Endothelial cells, Adipocytes | Liver cells | [81] |
| miR-197 | Endothelial cells, Adypocytes | Liver cells | [81] |
| miR-509-3p | Adipocytes, Macrophages | Liver cells | [81] |
| miR-29b-3p | BM-MSC | Liver cells, Adipocytes | [84,85] |
| miR-122 | Hepatocytes | Liver cells, Adipocytes | [84,85] |
| miR-192 | Hepatocytes | Liver cells, Adipocytes | [84,85] |
5. Exosome-miRNAs in Diabetes: Potential Clinical Applications
Given that diabetes belongs to chronic metabolic disorder diseases, the early monitoring of glycemia, blood pressure, and cardiovascular risk can improve the potential therapeutic effect of exosome-miRNAs in diabetes patients [7]. Owing to their peculiar structure, exosome-miRNAs are more stable in tissues and cells and can be specifically detected using qRT-PCR or in situ hybridization assay [86]. In addition, they are developmentally regulated [87]. Recent studies have shown that the profile of exosome-miRNAs affects the outcome of diabetes and its associated complications. Further evidence revealed that the exosome miRNAs’ expression profile in sera and urine differs between healthy and diabetic individuals. These findings strongly suggest the potential role of exosome-miRNAs as novel diagnostic biomarkers of diabetes [87,88,89,90,91,92,93,94,95]. In this conceptual framework, miR-1, miR-133a, miR-30a, miR-342, and miR-133b are most promising candidates [88,93]. Furthermore, Sidorkiewicz et al. [94] showed that exosome-miR-491-5p, miR-1307-3p, and miR-298 could be helpful biomarkers in monitoring the progression of diabetes. It is worth mentioning that exosome-miRNAs are closely associated with the gender difference of diabetes, as reported by Deng and co-workers [95]. They found that serum miR-29a/b levels were decreased in diabetic pregnant women and correlated with neonatal pathologic jaundice, showing a diagnostic value for these miRNAs. Exosome-miRNAs cannot only be used as biomarkers, but can also serve as miRNA inhibitors and agonist delivery systems for the treatment of diabetes. In this frame, the widespread application of nanotechnology has fostered the use of exosome-miRNAs in animal models. In addition, several engineered exosome-miRNAs have been developed to accelerate wound healing in diabetic rats, taking advantage of the natural availability and biocompatibility of cellular-derived exosomes as extracellular miRNA-transporting particles. The engineered exosomes exhibited excellent effects on re-epithelization, vessel maturation, angiogenesis, and collagen remodeling, leading to a novel therapeutic strategy in diabetic chronic wound healing [96]. Of note, Shi et al. [97], using diabetic pregnant mouse models, demonstrated that maternal exosomes in diabetes could cross the maternal–fetal barrier and contribute to cardiac development deficiency via miRNAs, providing new insights into chronic heart disease prevention and treatment. Studies on exosome inhibitors or agonists suggest a novel strategy for mitigating exosome-mediated diabetes and associated complications. However, the translation of experimental findings into clinical practice remains challenging, as well as the use of exosome-miRNAs for diabetes treatment. Further research focused on biomaterials and on the function and mechanism of exosome-miRNAs could lead to innovative strategies for the clinical management of diabetes.
6. Challenging Tasks and Opportunities of Exosome miRNAs in Diabetes
The rapid evolution of next-generation sequencing technologies has led to the discovery and identification of an increasing number of exosome miRNAs. Recently, several databases have been developed to identify and predict exosome components (proteins, miRNAs, mRNAs, etc., and lipids) [98,99,100,101,102,103,104,105,106,107,108,109,110,111,112]. Of them, databases such as CMEP, Xeno-miRNet, and Mirandola can be utilized to highlight disease-related exosome miRNAs. The combination of biological sciences and material technology has also prompted the use of nanotechnology in the field of disease treatment [113,114], including diabetes [115]. Differently from the direct administration into the target tissues of the agomir or antagomir, nanocarrier-derived miRNAs displayed higher efficiency and specificity; the use of exosomes as endogenous nanocarriers has several advantages, including multiple drug loading, lack of toxicity, protection from drug degradation, and the delivery of drug cargoes to the disease-associated targeted cells [116]. Regarding exosome-miRNAs’ pivotal role in the progression of diabetes and its associated co-morbidities, the use of exosomes as endogenous nanocarriers has significant potential as a biological tool for diagnosing or treating diabetes.
7. Conclusions
Exosome-miRNAs have been recognized as powerful tools for integrating the diagnosis and treatment of diabetes. As regulatory molecules, they are involved in multiple steps of diabetes by modulating the expression levels of related genes. Furthermore, the possibility of silencing or activating exosome-miRNAs exogenously by incorporating antagomir or agomir into exosomes, followed by their injection in target tissues, has set the fundamentals for a new therapeutic approach in the treatment of diabetes. In any case, much remains to be done before the research findings might be translated into clinical practice. The future of exosome therapy includes combinations of targeted exosomes with antidiabetic drugs and/or exosomes as micronutrients [117], as well as high-precision diabetes diagnostic probes to create multifunctional platforms for in vivo tracking, prognosis monitoring, and therapy. Similarly, the first mRNA-based severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) vaccine encapsulated in lipid nanoparticles mimic exosome now exists [118].
Author Contributions
Conceptualization, E.C. and M.C.C.; resources, all authors; Data curation, writing—original draft preparation, R.C.; writing—review and editing, E.C. and M.C.C.; visualization, L.G.; supervision, G.D.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Alegre-Díaz J., Herrington W., López-Cervantes M., Gnatiuc L., Ramirez R., Hill M., Baigent C., McCarthy M., Lewington S., Collins R., et al. Diabetes and cause–specific mortality in Mexico City. N. Engl. J. Med. 2016;375:1961–1971. doi: 10.1056/NEJMoa1605368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murphy–Chutorian B., Han G., Cohen S.R. Dermatologic manifestations of diabetes mellitus: A review. Endocrinol. Metab. Clin. N. Am. 2013;42:869–898. doi: 10.1016/j.ecl.2013.07.004. [DOI] [PubMed] [Google Scholar]
- 3.Cione E., Caroleo M.C., Cannataro R., Perri M., Pingitore A., Genchi G. Vitamin A and Diabesity: New Insight for Drug Discovery. Mini Rev. Med. Chem. 2016;16:738–742. doi: 10.2174/1389557515666150709112822. [DOI] [PubMed] [Google Scholar]
- 4.King H., Aubert R.E., Herman W.H. Global burden of diabetes, 1995–2025: Prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414–1431. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 5.Cho N.H., Shaw J.E., Karuranga S., Huang Y., da Rocha Fernandes J.D., Ohlrogge A.W., Malanda B. IDF diabetes atlas: Global estimates of diabetes prevalence for 2017 and projections for Diabetes. Res. Clin. Pract. 2018;138:271–281. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 6.Wang L., Kong L., Wu F., Bai Y., Burton R. Preventing chronic diseases in China. Lancet. 2005;366:1821–1824. doi: 10.1016/S0140-6736(05)67344-8. [DOI] [PubMed] [Google Scholar]
- 7.Lysy P.A., Corritore E., Sokal E.M. New insights into diabetes cell therapy. Curr. Diab. Rep. 2016;16:38. doi: 10.1007/s11892-016-0729-3. [DOI] [PubMed] [Google Scholar]
- 8.Seo N., Akiyoshi K., Shiku H. Exosome–mediated regulation of tumor immunology. Cancer Sci. 2018;109:2998–3004. doi: 10.1111/cas.13735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang Y., Yu M., Tian W. Physiological and pathological impact of exosomes of adipose tissue. Cell Prolif. 2016;49:3–13. doi: 10.1111/cpr.12233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kowal J., Tkach M., Thery C. Biogenesis and secretion of exosomes. Curr. Opin. Cell Biol. 2014;29:116–125. doi: 10.1016/j.ceb.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 11.Cione E., Lucente M., Gallelli L., De Sarro G., Luciani F., Caroleo M.C. Innate Immunity and Human Milk MicroRNAs Content: A New Perspective for Premature Newborns. J. Compr. Ped. 2017;8:e43359. doi: 10.5812/compreped.43359. [DOI] [Google Scholar]
- 12.Perri M., Lucente M., Cannataro R., de Luca I.F., Gallelli L., Moro G., de Sarro G., Caroleo M.C., Cione E. Variation in Immune-Related microRNAs Profile in Human Milk Amongst Lactating Women. MicroRNA. 2018;7:107–114. doi: 10.2174/2211536607666180206150503. [DOI] [PubMed] [Google Scholar]
- 13.Zhang H., Deng T., Ge S., Liu Y., Bai M., Zhu K., Fan Q., Li J., Ning T., Tian F., et al. Exosome circRNA secreted from adipocytes promotes the growth of hepatocellular carcinoma by targeting deubiquitination–related. USPOncogene. 2019;38:2844–2859. doi: 10.1038/s41388-018-0619-z. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 14.Gallelli L., Cione E., Caroleo M.C., Carotenuto M., Lagana P., Siniscalchi A., Guidetti V. MicroRNAs to Monitor Pain migraine and Drug Treatment. MicroRNA. 2017;6:152–156. doi: 10.2174/2211536606666170913152821. [DOI] [PubMed] [Google Scholar]
- 15.Wu Y., Wang Y., Wei M., Han X., Xu T., Cui M. Advances in the study of exosomal lncRNAs in tumors and the selection of research methods. Biomed. Pharmacother. 2020;123:109716. doi: 10.1016/j.biopha.2019.109716. [DOI] [PubMed] [Google Scholar]
- 16.Mathieu M., Martin–Jaular L., Lavieu G., Thery C. Specificities of secretion and uptake of exosomes and other extracellular vesicles for cell–to–cell communication. Nat. Cell Biol. 2019;21:9–17. doi: 10.1038/s41556-018-0250-9. [DOI] [PubMed] [Google Scholar]
- 17.Tingö L., Ahlberg E., Johansson L., Pedersen S.A., Chawla K., Sætrom P., Cione E., Simpson M.R. Non-Coding RNAs in Human Breast Milk: A Systematic Review. Front. Immunol. 2021;12:725323. doi: 10.3389/fimmu.2021.725323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carrasco–Ramiro F., Peiro–Pastor R., Aguado B. Human genomics projects and precision medicine. Gene Ther. 2017;24:551–561. doi: 10.1038/gt.2017.77. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y., Nie H., He X., Liao Z., Zhou Y., Zhou J., Ou C. The emerging role of super enhancer–derived non-coding RNAs in human cancer. Theranostics. 2020;10:11049–11062. doi: 10.7150/thno.49168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ou C., Sun Z., Li X., Ren W., Qin Z., Zhang X., Yuan W., Wang J., Yu W., Zhang S., et al. MiR–590–5p, a density–sensitive microRNA, inhibits tumorigenesis by targeting YAP1 in colorectal cancer. Cancer Lett. 2017;399:53–63. doi: 10.1016/j.canlet.2017.04.011. [DOI] [PubMed] [Google Scholar]
- 21.Nie H., Wang Y., Liao Z., Zhou J., Ou C. The function and mechanism of circular RNAs in gastrointestinal tumours. Cell Prolif. 2020;53:e12815. doi: 10.1111/cpr.12815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ou C., Sun Z., He X., Li X., Fan S., Zheng X., Peng Q., Li G., Li X., Ma J. Targeting YAP1/LINC00152/FSCN1 signaling axis prevents the progression of colorectal cancer. Adv. Sci. 2020;7:1901380. doi: 10.1002/advs.201901380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cortez M.A., Bueso–Ramos C., Ferdin J., Lopez–Berestein G., Sood A.K., Calin G.A. MicroRNAs in body fluids–the mix of hormones and biomarkers. Nat. Rev. Clin. Oncol. 2011;8:467–477. doi: 10.1038/nrclinonc.2011.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Valadi H., Ekstrom K., Bossios A., Sjostrand M., Lee J.J., Lotvall J.O. Exosome–mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 25.Yang J.X., Xie P., Li Y.S., Wen T., Yang X.C. Osteoclast–derived miR–23a–5p–containing exosomes inhibit osteogenic differentiation by regulating Runx2. Cell Signal. 2020;70:109504. doi: 10.1016/j.cellsig.2019.109504. [DOI] [PubMed] [Google Scholar]
- 26.Zhang X., Sai B., Wang F., Wang L., Wang Y., Zheng L., Li G., Tang J., Xiang J. Hypoxic BMSC–derived exosomal miRNAs promote metastasis of lung cancer cells via STAT3–induced EMT. Mol. Cancer. 2019;18:40. doi: 10.1186/s12943-019-0959-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhu L.-P., Tian T., Wang J.-Y., He J.-N., Chen T., Pan M., Xu L., Zhang H.-X., Qiu X.-T., Li C.-C., et al. Hypoxia–elicited mesenchymal stem cell–derived exosomes facilitates cardiac repair through miR–125b–mediated prevention of cell death in myocardial infarction. Theranostics. 2018;8:6163–6177. doi: 10.7150/thno.28021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xie Y., Dang W., Zhang S., Yue W., Yang L., Zhai X., Yan Q., Lu J. The role of exosomal non-coding RNAs in cancer. Mol. Cancer. 2019;18:37. doi: 10.1186/s12943-019-0984-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zheng H., Zhan Y., Liu S., Lu J., Luo J., Feng J., Fan S. The roles of tumor–derived exosomes in non–small cell lung cancer and their clinical implications. J. Exp. Clin. Cancer Res. 2018;37:226. doi: 10.1186/s13046-018-0901-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Trams E.G., Lauter C.J., Salem N.J., Heine U. Exfoliation of membrane ecto–enzymes in the form of micro–vesicles. Biochim. Biophys. Acta. 1981;645:63–70. doi: 10.1016/0005-2736(81)90512-5. [DOI] [PubMed] [Google Scholar]
- 31.Johnstone R.M., Adam M., Hammond J.R., Orr L., Turbide C. Vesicle formation during reticulocyte maturation. Association of plasma membrane activities with released vesicles (exosomes) J. Biol. Chem. 1987;262:9412–9420. doi: 10.1016/S0021-9258(18)48095-7. [DOI] [PubMed] [Google Scholar]
- 32.Raposo G., Nijman H.W., Stoorvogel W., Liejendekker R., Harding C.V., Melief C.J., Geuze H.J. B lymphocytes secrete antigen–presenting vesicles. J. Exp. Med. 1996;183:1161–1172. doi: 10.1084/jem.183.3.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoshino A., Kim H.S., Bojmar L., Gyan K.E., Cioffi M., Hernandez J., Zambirinis C.P., Rodrigues G., Molina H., Heissel S., et al. Extracellular vesicle and particle biomarkers define multiple human cancers. Cell. 2020;182:1044–1061. doi: 10.1016/j.cell.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van der Pol E., Boing A.N., Harrison P., Sturk A., Nieuwland R. Classification, functions, and clinical relevance of extracellular vesicles. Pharmacol. Rev. 2012;64:676–705. doi: 10.1124/pr.112.005983. [DOI] [PubMed] [Google Scholar]
- 35.Laulagnier K., Motta C., Hamdi S., Roy S., Fauvelle F., Pageaux J.-F., Kobayashi T., Salles J.-P., Perret B., Bonnerot C., et al. Mast cell– and dendritic cell–derived exosomes display a specific lipid composition and an unusual membrane organization. Biochem. J. 2004;380:161–171. doi: 10.1042/bj20031594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Conde–Vancells J., Rodriguez–Suarez E., Embade N., Gil D., Matthiesen R., Valle M., Elortza F., Lu S.C., Mato J.M., Falcon-Perez J.M. Characterization and comprehensive proteome profiling of exosomes secreted by hepatocytes. J. Proteome Res. 2008;7:5157–5166. doi: 10.1021/pr8004887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fei F., Joo E.J., Tarighat S.S., Schiffer I., Paz H., Fabbri M., Abdel-Azim H., Groffen J., Heisterkamp N. B–cell precursor acute lymphoblastic leukemia and stromal cells communicate through galectin. Oncotarget. 2015;6:11378–11394. doi: 10.18632/oncotarget.3409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhang L., Zhang S., Yao J., Lowery F.J., Zhang Q., Huang W.-C., Li P., Li M., Wang X., Zhang C., et al. Microenvironment–induced PTEN loss by exosomal microRNA primes brain metastasis outgrowth. Nature. 2015;527:100–104. doi: 10.1038/nature15376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bosque A., Dietz L., Gallego–Lleyda A., Sanclemente M., Iturralde M., Naval J., Alava M.A., Martinez-Lostao L., Martinez-Lostao L., Thierse H.J., et al. Comparative proteomics of exosomes secreted by tumoral Jurkat T cells and normal human T cell blasts unravels a potential tumorigenic role for valosin–containing protein. Oncotarget. 2016;7:29287–29305. doi: 10.18632/oncotarget.8678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Huang X., Yuan T., Tschannen M., Sun Z., Jacob H., Du M., Liang M., Dittmar R.L., Liu Y., Liang M., et al. Characterization of human plasma-derived exosomal RNAs by deep sequencing. BMC Genom. 2013;14:319. doi: 10.1186/1471-2164-14-319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mittelbrunn M., Gutierrez-Vazquez C., Villarroya-Beltri C., Gonzalez S., Sanchez-Cabo F., Gonzalez M.A., Bernad A., Sanchez-Madrid F. Unidirectional transfer of microRNA-loaded exosomes from T cells to antigen-presenting cells. Nat. Commun. 2011;2:282. doi: 10.1038/ncomms1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Huang–Doran I., Zhang C.Y., Vidal–Puig A. Extracellular vesicles: Novel mediators of cell communication in metabolic disease. Trends Endocrinol. Metab. 2017;28:3–18. doi: 10.1016/j.tem.2016.10.003. [DOI] [PubMed] [Google Scholar]
- 43.Hewson C., Capraro D., Burdach J., Whitaker N., Morris K.V. Extracellular vesicle associated long non-coding RNAs functionally enhance cell viability. Non-coding RNA Res. 2016;1:3–11. doi: 10.1016/j.ncrna.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.De Jong O.G., Verhaar M.C., Chen Y., Vader P., Gremmels H., Posthuma G., Schiffelers R.M., Gucek M., Van Balkom B.W.M. Cellular stress conditions are reflected in the protein and RNA content of endothelial cell–derived exosomes. J. Extracell Vesicles. 2012;1:18396. doi: 10.3402/jev.v1i0.18396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang Y., Liu D., Chen X., Li J., Li L., Bian Z., Sun F., Lu J., Yin Y., Cai X., et al. Secreted monocytic miR–150 enhances targeted endothelial cell migration. Mol. Cell. 2010;39:133–144. doi: 10.1016/j.molcel.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 46.Daneshgari F., Moore C. Diabetic uropathy. Semin. Nephrol. 2006;26:182–185. doi: 10.1016/j.semnephrol.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 47.Mitrovic–Perisic N., Antic S. Risk factors for coronary heart disease and actual diagnostic criteria for diabetes mellitus. Vojnosanitetski Pregled. 2009;66:973–978. doi: 10.2298/VSP0912973M. [DOI] [PubMed] [Google Scholar]
- 48.Paul P., Chakraborty A., Sarkar D., Langthasa M., Rahman M., Bari M., Singha R.S., Malakar A.K., Chakraborty S. Interplay between miRNAs and human diseases. J. Cell. Physiol. 2018;233:2007–2018. doi: 10.1002/jcp.25854. [DOI] [PubMed] [Google Scholar]
- 49.Eriksson J.G., Laine M.K. Insulin therapy in the elderly with type 2 diabetes. Minerva Endocrinol. 2015;40:283–295. [PubMed] [Google Scholar]
- 50.Brennan E., Wang B., McClelland A., Mohan M., Marai M., Beuscart O., Derouiche S., Gray S., Pickering R., Tikellis C., et al. Protective effect of let–7 miRNA family in regulating inflammation in diabetes–associated atherosclerosis. Diabetes. 2017;66:2266–2277. doi: 10.2337/db16-1405. [DOI] [PubMed] [Google Scholar]
- 51.Vickers K.C., Landstreet S.R., Levin M., Shoucri B.M., Toth C.L., Taylor R.C., Palmisano B.T., Tabet F., Cui H.L., Rye K.-A., et al. MicroRNA–223 coordinates cholesterol homeostasis. Proc. Natl. Acad. Sci. USA. 2014;111:14518–14523. doi: 10.1073/pnas.1215767111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Massart J., Sjogren R., Lundell L.S., Mudry J.M., Franck N., O’Gorman D.J., Egan B., Zierath J.R., Krook A. Altered miR–29 expression in type 2 diabetes influences glucose and lipid metabolism in skeletal muscle. Diabetes. 2017;66:1807–1818. doi: 10.2337/db17-0141. [DOI] [PubMed] [Google Scholar]
- 53.Santovito D., De Nardis V., Marcantonio P., Mandolini C., Paganelli C., Vitale E., Buttitta F., Bucci M., Mezzetti A., Consoli A., et al. Plasma exosome microRNA profiling unravels a new potential modulator of adiponectin pathway in diabetes: Effect of glycemic control. J. Clin. Endocrinol. Metab. 2014;99:E1681–E1685. doi: 10.1210/jc.2013-3843. [DOI] [PubMed] [Google Scholar]
- 54.Guay C., Menoud V., Rome S., Regazzi R. Horizontal transfer of exosomal microRNAs transduce apoptotic signals between pancreatic beta–cells. Cell Commun. Signal. 2015;13:17. doi: 10.1186/s12964-015-0097-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Su T., Xiao Y., Xiao Y.E., Guo Q.I., Li C., Huang Y., Deng Q., Wen J., Zhou F., Luo X.H. Bone marrow mesenchymal stem cells–derived exosomal MiR–29b–3p regulates aging–associated insulin resistance. ACS Nano. 2019;13:2450–2462. doi: 10.1021/acsnano.8b09375. [DOI] [PubMed] [Google Scholar]
- 56.Fan B., Li C., Szalad A., Wang L., Pan W., Zhang R., Chopp M., Zhang Z.G., Liu X.S. Mesenchymal stromal cell–derived exosomes ameliorate peripheral neuropathy in a mouse model of diabetes. Diabetologia. 2020;63:431–443. doi: 10.1007/s00125-019-05043-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Nakano M., Nagaishi K., Konari N., Saito Y., Chikenji T., Mizue Y., Fujimiya M. Bone marrow–derived mesenchymal stem cells improve diabetes–induced cognitive impairment by exosome transfer into damaged neurons and astrocytes. Sci. Rep. 2016;6:24805. doi: 10.1038/srep24805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang C., Zhang C., Liu L., Xi A., Chen B., Li Y., Du J. Macrophage–derived miR–155–containing exosomes suppress fibroblast proliferation and promote fibroblast inflammation during cardiac injury. Mol. Ther. 2017;25:192–204. doi: 10.1016/j.ymthe.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ashcroft F.M., Rorsman P. Diabetes mellitus and the beta cell: The last ten years. Cell. 2012;148:1160–1171. doi: 10.1016/j.cell.2012.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Guay C., Jacovetti C., Nesca V., Motterle A., Tugay K., Regazzi R. Emerging roles of non-coding RNAs in pancreatic beta–cell function and dysfunction. Diabetes Obes. Metab. 2012;14((Suppl. 3)):12–21. doi: 10.1111/j.1463-1326.2012.01654.x. [DOI] [PubMed] [Google Scholar]
- 61.Guay C., Regazzi R. Circulating microRNAs as novel biomarkers for diabetes mellitus. Nat. Rev. Endocrinol. 2013;9:513–521. doi: 10.1038/nrendo.2013.86. [DOI] [PubMed] [Google Scholar]
- 62.Rottiers V., Naar A.M. MicroRNAs in metabolism and metabolic disorders. Nat. Rev. Mol. Cell Biol. 2012;13:239–250. doi: 10.1038/nrm3313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Perri M., Carollo M.C., Liu N., Gallelli L., de Sarro G., Kagechika H., Cione E. 9-cis Retinoic acid modulates myotrophin expression and its miR in physiological and pathophysiological cell models. Exp. Cell Res. 2017;354:25–30. doi: 10.1016/j.yexcr.2017.03.022. [DOI] [PubMed] [Google Scholar]
- 64.Fu Q., Jiang H., Wang Z., Wang X., Chen H., Shen Z., Xiao L., Guo X., Yang T. Injury factors alter miRNAs profiles of exosomes derived from islets and circulation. Aging. 2018;10:3986–3999. doi: 10.18632/aging.101689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tsukita S., Yamada T., Takahashi K., Munakata Y., Hosaka S., Takahashi H., Gao J., Shirai Y., Kodama S., Asai Y., et al. MicroRNAs 106b and 222 improve hyperglycemia in a mouse model of insulin–deficient diabetes via pancreatic beta–cell proliferation. EBioMedicine. 2017;15:163–172. doi: 10.1016/j.ebiom.2016.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xu H., Du X., Xu J., Zhang Y., Tian Y., Liu G., Wang X., Ma M., Du W., Liu Y., et al. Pancreatic beta-cell microRNA–26a alleviates type 2 diabetes by improving peripheral insulin sensitivity and preserving beta cell function. PLoS Biol. 2020;18:e3000603. doi: 10.1371/journal.pbio.3000603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Xu G., Thielen L.A., Chen J., Grayson T.B., Grimes T., Bridges S.L., Tse H.M., Smith B., Patel R., Li P., et al. Serum miR–204 is an early biomarker of type 1 diabetes–associated pancreatic beta–cell loss. Am. J. Physiol. Endocrinol. Metab. 2019;317:E723–E730. doi: 10.1152/ajpendo.00122.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Samuel V.T., Shulman G.I. Mechanisms for insulin resistance: Common threads and missing links. Cell. 2012;148:852–871. doi: 10.1016/j.cell.2012.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Stumvoll M., Goldstein B.J., van Haeften T.W. Type 2 diabetes: Principles of pathogenesis and therapy. Lancet. 2005;365:1333–1346. doi: 10.1016/S0140-6736(05)61032-X. [DOI] [PubMed] [Google Scholar]
- 70.Fernandez–Twinn D.S., Alfaradhi M.Z., Martin–Gronert M.S., Duque-Guimaraes D.E., Piekarz A., Ferland-McCollough D., Bushell M., Ozanne S.E. Downregulation of IRS–1 in adipose tissue of offspring of obese mice is programmed cell–autonomously through post–transcriptional mechanisms. Mol. Metab. 2014;3:325–333. doi: 10.1016/j.molmet.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chen Y.-H., Heneidi S., Lee J.-M., Layman L.C., Stepp D.W., Gamboa G.M., Chen B.-S., Chazenbalk G., Azziz R. miRNA–93 inhibits GLUT4 and is overexpressed in adipose tissue of polycystic ovary syndrome patients and women with insulin resistance. Diabetes. 2013;62:2278–2286. doi: 10.2337/db12-0963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Xu G., Ji C., Song G., Zhao C., Shi C., Song L., Chen L., Yang L., Huang F., Pang L., et al. MiR–26b modulates insulin sensitivity in adipocytes by interrupting the PTEN/PI3K/AKT pathway. Int. J. Obes. 2015;39:1523–1530. doi: 10.1038/ijo.2015.95. [DOI] [PubMed] [Google Scholar]
- 73.Thomou T., Mori M.A., Dreyfuss J.M., Konishi M., Sakaguchi M., Wolfrum C., Rao T.N., Winnay J.N., Garcia-Martin R., Grinspoon S.K., et al. Adipose–derived circulating miRNAs regulate gene expression in other tissues. Nature. 2017;542:450–455. doi: 10.1038/nature21365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Aswad H., Forterre A., Wiklander O.P.B., Vial G., Danty-Berger E., Lab C., Lamazière A., Meugnier E., Pesenti S., Ott C., et al. Exosomes participate in the alteration of muscle homeostasis during lipid–induced insulin resistance in mice. Diabetologia. 2014;57:2155–2164. doi: 10.1007/s00125-014-3337-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Deng Z.-B., Poliakov A., Hardy R.W., Clements R., Liu C., Liu Y., Wang J., Xiang X., Zhang S., Zhuang X., et al. Adipose tissue exosome–like vesicles mediate activation of macrophage–induced insulin resistance. Diabetes. 2009;58:2498–2505. doi: 10.2337/db09-0216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Karolina D.S., Arumugam A., Tavintharan S., Wong M.T.K., Lim S.C., Sum C.F., Jeyaseelan K. MicroRNA 144 impairs insulin signaling by inhibiting the expression of insulin receptor substrate 1 in type 2 diabetes mellitus. PLoS ONE. 2011;6:e22839. doi: 10.1371/annotation/698b7123-174f-4a09-95c9-fd6f5017d622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Guay C., Roggli E., Nesca V., Jacovetti C., Regazzi R. Diabetes mellitus, a microRNA–related disease? Transl. Res. 2011;157:253–264. doi: 10.1016/j.trsl.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 78.Zhao X., Mohan R., Ozcan S., Tang X. MicroRNA–30d induces insulin transcription factor MafA and insulin production by targeting mitogen–activated protein 4 kinase 4 (MAP4K4) in pancreatic beta–cells. J. Biol. Chem. 2012;287:31155–31164. doi: 10.1074/jbc.M112.362632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Katayama M., Wiklander O., Fritz T., Caidahl K., El-Andaloussi S., Zierath J.R., Zierath A. Circulating exosomal miR–20b–5p is elevated in type 2 diabetes and could impair insulin action in human skeletal muscle. Diabetes. 2019;68:515–526. doi: 10.2337/db18-0470. [DOI] [PubMed] [Google Scholar]
- 80.Wang L., Zhang B., Zheng W., Kang M., Chen Q., Qin W., Li C., Zhang Y., Shao Y., Wu Y. Exosomes derived from pancreatic cancer cells induce insulin resistance in C2C12 myotube cells through the PI3K/Akt/FoxO1 pathway. Sci. Rep. 2017;7:5384. doi: 10.1038/s41598-017-05541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Karolina D.S., Tavintharan S., Arumugam A., Sepramaniam S., Pek S.L.T., Wong M.T.K., Lim S.C., Sum C.F., Jeyaseelan K. Circulating miRNA profiles in patients with metabolic syndrome. J. Clin. Endocrinol. Metab. 2012;97:E2271–E2276. doi: 10.1210/jc.2012-1996. [DOI] [PubMed] [Google Scholar]
- 82.Cannataro R., Perri M., Gallelli L., Caroleo M.C., de Sarro G., Cione E. Ketogenic Diet Acts on Body Remodeling and MicroRNAs Expression Profile. Microrna. 2019;8:116–126. doi: 10.2174/2211536608666181126093903. [DOI] [PubMed] [Google Scholar]
- 83.Cannataro R., Caroleo M.C., Fazio A., la Torre C., Plastina P., Gallelli L., Lauria G., Cione E. Ketogenic Diet and microRNAs Linked to Antioxidant Biochemical Homeostasis. Antioxidants. 2019;8:269. doi: 10.3390/antiox8080269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Castano C., Kalko S., Novials A., Parrizas M. Obesity–associated exosomal miRNAs modulate glucose and lipid metabolism in mice. Proc. Natl. Acad. Sci. USA. 2018;115:12158–12163. doi: 10.1073/pnas.1808855115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ying W., Riopel M., Bandyopadhyay G., Dong Y., Birmingham A., Seo J.B., Ofrecio J.M., Wollam J., Hernandez-Carretero A., Fu W., et al. Adipose tissue macrophage–derived exosomal miRNAs can modulate in vivo and in vitro insulin sensitivity. Cell. 2017;171:372–384. doi: 10.1016/j.cell.2017.08.035. [DOI] [PubMed] [Google Scholar]
- 86.Boyiadzis M., Whiteside T.L. The emerging roles of tumor–derived exosomes in hematological malignancies. Leukemia. 2017;31:1259–1268. doi: 10.1038/leu.2017.91. [DOI] [PubMed] [Google Scholar]
- 87.Eissa S., Matboli M., Bekhet M.M. Clinical verification of a novel urinary microRNA panel: 133b, –342 and –30 as biomarkers for diabetic nephropathy identified by bioinformatics analysis. Biomed. Pharmacother. 2016;83:92–99. doi: 10.1016/j.biopha.2016.06.018. [DOI] [PubMed] [Google Scholar]
- 88.Argyropoulos C., Wang K., McClarty S., Huang D., Bernardo J., Ellis D., Johnson J. Urinary microRNA profiling in the nephropathy of type 1 diabetes. PLoS ONE. 2013;8:e54662. doi: 10.1371/journal.pone.0054662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Barutta F., Tricarico M., Corbelli A., Annaratone L., Pinach S., Grimaldi S., Gruden G. Urinary exosomal microRNAs in incipient diabetic nephropathy. PLoS ONE. 2013;8:e73798. doi: 10.1371/journal.pone.0073798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ibrahim A., Marban E. Exosomes: Fundamental biology and roles in cardiovascular physiology. Annu. Rev. Physiol. 2016;78:67–83. doi: 10.1146/annurev-physiol-021115-104929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Eissa S., Matboli M., Aboushahba R., Bekhet M.M., Soliman Y. Urinary exosomal microRNA panel unravels novel biomarkers for diagnosis of type 2 diabetic kidney disease. J. Diabetes Complicat. 2016;30:1585–1592. doi: 10.1016/j.jdiacomp.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 92.Wan S., Wang J., Wu J., Song J., Zhang C.Y., Zhang C., Wang C., Wang J.J. Increased serum miR–7 is a promising biomarker for type 2 diabetes mellitus and its microvascular complications. Diabetes Res. Clin. Pract. 2017;130:171–179. doi: 10.1016/j.diabres.2017.06.005. [DOI] [PubMed] [Google Scholar]
- 93.De Gonzalo-Calvo D., Van Der Meer R.W., Rijzewijk L.J., Smit J.W.A., Revuelta E., Nasarre L., Escola-Gil J.C., Lamb H.J., Llorente-Cortes V. Serum microRNA–1 and microRNA–133a levels reflect myocardial steatosis in uncomplicated type 2 diabetes. Sci. Rep. 2017;7:47. doi: 10.1038/s41598-017-00070-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sidorkiewicz I., Niemira M., Maliszewska K., Erol A., Bielska A., Szalkowska A., Adamska-Patruno E., Szczerbinski L., Gorska M., Kretowski A. Circulating miRNAs as a predictive biomarker of the progression from prediabetes to diabetes: Outcomes of a 5–year prospective observational study. J. Clin. Med. 2020;9:2184. doi: 10.3390/jcm9072184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Deng L., Huang Y., Li L., Chen H., Su J. Serum miR–29a/b expression in gestational diabetes mellitus and its influence on prognosis evaluation. J. Int. Med. Res. 2020;48:300060520954763. doi: 10.1177/0300060520954763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Li M., Ke Q.F., Tao S.C., Guo S.C., Rui B.Y., Guo Y.P. Fabrication of hydroxyapatite/chitosan composite hydrogels loaded with exosomes derived from miR–126–3p overexpressed synovial mesenchymal stem cells for diabetic chronic wound healing. J. Mater. Chem. B. 2016;4:6830–6841. doi: 10.1039/C6TB01560C. [DOI] [PubMed] [Google Scholar]
- 97.Shi R., Zhao L., Cai W., Wei M., Zhou X., Yang G., Yuan L. Maternal exosomes in diabetes contribute to the cardiac development deficiency. Biochem. Biophys. Res. Commun. 2017;483:602–608. doi: 10.1016/j.bbrc.2016.12.097. [DOI] [PubMed] [Google Scholar]
- 98.He X., Li S., Yu B., Kuang G., Wu Y., Zhang M., He Y., Ou C., Cao P. Up–regulation of LINC00467 promotes the tumorigenesis in colorectal cancer. J. Cancer. 2019;10:6405–6413. doi: 10.7150/jca.32216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kim D.K., Lee J., Simpson R.J., Lotvall J., Gho Y.S. Expedia: A community web resource for prokaryotic and eukaryotic extracellular vesicles research. Semin. Cell Dev. Biol. 2015;40:4–7. doi: 10.1016/j.semcdb.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 100.Mathivanan S., Fahner C.J., Reid G.E., Simpson R.J. ExoCarta 2012: Database of exosomal proteins, RNA and lipids. Nucleic Acids Res. 2012;40:D1241–D1244. doi: 10.1093/nar/gkr828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Pathan M., Fonseka P., Chitti S.V., Kang T., Sanwlani R., van Deun J., Hendrix A., Mathivanan S. Vesiclepedia 2019: A compendium of RNA, proteins, lipids and metabolites in extracellular vesicles. Nucleic Acids Res. 2019;47:D516–D519. doi: 10.1093/nar/gky1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Liu T., Zhang Q., Zhang J., Li C., Miao Y.-R., Lei Q., Li Q., Guo A.-Y. EVmiRNA: A database of miRNA profiling in extracellular vesicles. Nucleic Acids Res. 2019;47:D89–D93. doi: 10.1093/nar/gky985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Maity S., Bhat A.H., Giri K., Ambatipudi K. BoMiProt: A database of bovine milk proteins. J Proteom. 2020;215:103648. doi: 10.1016/j.jprot.2020.103648. [DOI] [PubMed] [Google Scholar]
- 104.Li J.R., Tong C.Y., Sung T.J., Kang T.Y., Zhou X.J., Liu C.C. CMEP: A database for circulating microRNA expression profiling. Bioinformatics. 2019;35:3127–3132. doi: 10.1093/bioinformatics/btz042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Fan Y., Habib M., Xia J. Xeno–miRNet: A comprehensive database and analytics platform to explore xeno–miRNAs and their potential targets. PeerJ. 2018;6:e5650. doi: 10.7717/peerj.5650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Li S., Li Y., Chen B., Zhao J., Yu S., Tang Y., Zheng Q., Li Y., Wang P., He X., et al. exoRBase: A database of circRNA, lncRNA and mRNA in human blood exosomes. Nucleic Acids Res. 2018;46:D106–D112. doi: 10.1093/nar/gkx891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Fang S., Zhang L., Guo J., Niu Y., Wu Y., Li H., Zhao L., Li X., Teng X., Sun X., et al. NONCODEV5: A comprehensive annotation database for long non-coding RNAs. Nucleic Acids Res. 2018;46:D308–D314. doi: 10.1093/nar/gkx1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Russo F., Di Bella S., Nigita G., Macca V., Laganà A., Giugno R., Pulvirenti A., Ferro A. miRandola: Extracellular circulating microRNAs database. PLoS ONE. 2012;7:e47786. doi: 10.1371/journal.pone.0047786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Masud M.K., Na J., Younus M., Hossain S.A., Bando Y., Shiddiky M.J.A., Yamauchi Y. Superparamagnetic nanoarchitectures for disease–specific biomarker detection. Chem. Soc. Rev. 2019;48:5717–5751. doi: 10.1039/C9CS00174C. [DOI] [PubMed] [Google Scholar]
- 110.Soda N., Rehm B.H.A., Sonar P., Nguyen N.T., Shiddiky M.J.A. Advanced liquid biopsy technologies for circulating biomarker detection. J Mater Chem. B. 2019;7:6670–6704. doi: 10.1039/C9TB01490J. [DOI] [PubMed] [Google Scholar]
- 111.Nair S., Ormazabal V., Lappas M., McIntyre H.D., Salomon C. Extracellular vesicles and their potential role inducing changes in maternal insulin sensitivity during gestational diabetes mellitus. Am. J. Reprod. Immunol. 2021;85:e13361. doi: 10.1111/aji.13361. [DOI] [PubMed] [Google Scholar]
- 112.Santos K.A.D., Santos I.C.C.D., Silva C.S., Ribeiro H.G., Domingos I.D.F., Silbiger V.N. Circulating exosomal miRNAs as biomarkers for the diagnosis and prognosis of colorectal cancer. Int. J. Mol. Sci. 2020;22:346. doi: 10.3390/ijms22010346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Davis M.E., Chen Z.G. Shin DIABETES. Nanoparticle therapeutics: An emerging treatment modality for cancer. Nat. Rev. Drug. Discov. 2008;7:771–782. doi: 10.1038/nrd2614. [DOI] [PubMed] [Google Scholar]
- 114.Kowal J., Arras G., Colombo M., Jouve M., Morath J.P., Primdal-Bengtson B., Dingli F., Loew D., Tkach M., Théry C. Proteomic comparison defines novel markers to characterize heterogeneous populations of extracellular vesicle subtypes. Proc. Natl. Acad. Sci. USA. 2016;113:E968–E977. doi: 10.1073/pnas.1521230113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Roy B., Ghose S., Biswas S. Therapeutic strategies for miRNA delivery to reduce hepatocellular carcinoma. Semin. Cell Dev. Biol. 2021 doi: 10.1016/j.semcdb.2021.04.006. in press. [DOI] [PubMed] [Google Scholar]
- 116.Su T., Zhang P., Zhao F., Zhang S. Exosomal microRNAs mediating crosstalk between cancer cells with cancer–associated fibroblasts and tumor–associated macrophages in the tumor microenvironment. Front. Oncol. 2021;11:631703. doi: 10.3389/fonc.2021.631703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Cione E., Zambrini A.S., Cannataro R. MicroRNAs and Extracellular Vesicles in Milk: RNA-Based Micronutrients? J. Nutr. 2021;151:1378–1379. doi: 10.1093/jn/nxab134. [DOI] [PubMed] [Google Scholar]
- 118.Baden L.R., el Sahly H.M., Essink B., Kotloff K., Frey S., Novak R., Diemert D., Spector S.A., Rouphael N., Creech C.B., et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med. 2021;384:403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]