Abstract
Recently several patients, who developed Guillain–Barré syndrome characterized by prominent bifacial weakness after ChAdOx1 nCoV-19 vaccination, were described from different centers. We recently observed a patient who developed a similar syndrome, later in the follow up he showed worsening of the neuropathy two months after the initial presentation. Repeat EMG showed reduced nerve sensory and motor conduction velocities of both upper and lower limbs, and a diagnosis of chronic inflammatory demyelinating polyneuropathy (typical CIDP) was made according to established criteria. Our report expands on the possible outcomes in patients who develop Guillain–Barrè syndrome after COVID-19 vaccinations and suggest that close monitoring after the acute phase is needed in these patients to exclude a chronic evolution of the disease, which has important implications for long-term treatment.
Keywords: chronic inflammatory demyelinating polyneuropathy, Guillain–Barrè syndrome, bifacial weakness, COVID-19, SARS-CoV-2 vaccine
1. Introduction
Vaccines are the most cost-effective measures available against the COVID-19 pandemic with more than seven billion doses administered worldwide in November 2021 (https://coronavirus.jhu.edu/map.html) (accessed on 11 December 2021), thus monitoring of rare adverse events is of fundamental importance. COVID-19 vaccinations have mostly been associated with adverse events of little clinical significance such as injection site reaction or non-specific systemic symptoms such as fever and muscle aches, which usually resolve within days [1]. However, more severe adverse events have been reported in a minority of cases, including immune-mediated thrombocytopenia [2], and Guillain–Barrè syndrome, that is a potentially serious complication with a mortality rate of 3–5% despite intensive care treatment [3].
The incidence of GBS is estimated to be around 0.4–4.0 cases per 100,000 person-years [4]. The disease is more common in males especially over the age of 75, and less common among children [5]. GBS is generally classified into various subforms based on the pathophysiological profile and symptomatology (e.g., pharyngeal-cervical weakness syndrome, brachialis and bifacial paralysis with paresthesia) [6]. In some patients GBS can deteriorate again after some weeks from onset and several relapses can occur; in these patients a diagnosis of acute-onset chronic inflammatory demyelinating polyneuropathy (CIDP) should be considered [7].
In GBS an infectious trigger is recognized in >50% of cases while onset following vaccinations is debated [4]. Recently several patients who developed a GBS following CoV-19 vaccinations, were described from different centers [8,9,10,11,12]. In particular, most patients developed bifacial weakness with or without involvement of other peripheral nerves after ChAdOx1 nCoV-19 vaccination, suggesting this might represent a specific neuropathy phenotype associated with the vaccine. Clinical features of these patients are summarized in Table 1.
Table 1.
Clinical and MRI characteristics of patients with bifacial weakness after ChAdOx1 nCoV-19 vaccination.
| Age/Sex (Authors) |
Symptoms/Signs | Respiratory Failure | Days from First Dose of Vaccine | CSF Findings | EMG Findings | MRI | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|
| 54/M [8] |
Ascending distal limbs dysesthesias; bifacial paresis | None | 16 | P: 163 mg/dL; C: 19/mL |
Day 16: Facial NCS showed severely reduced compound muscle action potential amplitude responses and normal terminal latencies bilaterally; sensory and motor NCS: normal | Enhancement of facial nerves | Prednisolone 60 mg/day × 5 days | Stabilized |
| 20/M [8] |
Headache, LL dysesthesias, and bifacial paresis | None | 26 | P: 123 mg/dL; C: 14/mL |
Day 13: Facial NCS showed borderline normal amplitude responses and normal terminal latencies bilaterally; sensory and motor NCS: normal | Normal non-contrast brain MRI |
Prednisolone 60 mg/day × 5 days | Stabilized |
| 57/M [8] |
Lumbar back pain, dysarthria and bifacial paresis; lower limb dysesthesias; proximal limb weakness on exam | None | 21 | P: 247 mg/dL; C: 8/mL |
Day 13: Facial NCS, not performed; sensory and motor NCS: normal | Normal non-contrast brain MRI | IVIg | Stabilized |
| 55/M [8] |
LL paresthesias; bifacial paresis | None | 29 | P: 89 mg/dL; C: <5/mL |
NA | Enhancement of facial nerves | None | Subjective improvement of numbness |
| 43/F [9] |
Bifacial paresis, areflexic quadriparesis, upper back pain | Yes | 10 | P: 72.2 mg/dL C: 5/mL |
Demyelinating neuropathy | NA | IVIg IMV |
Recovered |
| 67/F [9] |
Bifacial paresis, right abducense palsy, bulbar palsy, Distal sensory impairment in the legs, areflexia, limb weakness | Yes | 14 | P: 345 mg/dL C: 3/mL |
Axonal motor-sensory neuropathy | Normal brain and spine MRI | IVIg IMV PLEX |
Still hospitalized |
| 53/F [9] |
Bilateral LL numbness, weakness, right-sided facial, tongue numbness, and back pain, right trigeminal V2-V3 sensory impairment, areflexia | Yes | 12 | P: 120 mg/dL C: 3/mL |
Demyelinating neuropathy | Normal brain and spine MRI | IVIg IMV |
Still hospitalized |
| 68/F [9] |
Facial diplegia, bulbar palsy, bilateral facial numbness, bilateral distal lower and UL numbness, and bilaterally trigeminal sensory loss, areflexia | Yes | 14 | P: 75 mg/dL C: 4/mL |
Demyelinating neuropathy | Normal brain and spine MRI | IVIg IMV |
Still hospitalized |
| 70/M [9] |
Facial diplegia, bulbar palsy. Bilateral distal UL and LL numbness, areflexia | Yes | 11 | P: NA C: NA |
Demyelinating neuropathy | NA | IVIg IMV |
Still hospitalized |
| 69/F [9] |
Facial diplegia, bulbar palsy, complete ophthalmoplegia, UL and LL distal numbness, UL and LL weakness, areflexia |
Yes | 12 | P: NA C: NA |
Demyelinating neuropathy | NA | IVIg PLEX |
Still hospitalized |
| 69/F [9] |
Facial diplegia, bulbar palsy, bilateral UL and LL numbness, areflexia | None | 13 | P: 83 mg/dL C: 2/mL |
Demyelinating neuropathy | NA | IVIg IMV |
Still hospitalized |
| 66/M [10] |
Bilateral facial weakness with numbness of the tongue and mouth, interscapular back and LL pain, paresthesia of both hands and feet Normal tone, power and reflexes in both UL and LL, except absent right ankle jerk. Reduced light touch and pinprick sensation symmetrically in LL to the knee and vibration to the ankles. Gait was ataxic |
None | 7 | P: 1.99 g/L C: 2/mL |
Sensory NCS: UL and LL: reduced SNAP amplitude Motor NCS: UL and LL: Prolonged DMLs, and F-wave latencies Slow CV Dispersed CMAPs and CB. Facial NCS: Prolonged DMLs |
MRI pre and post GAD contrast: normal except for bilateral smooth contrast enhancement along whole facial nerve | IVIg | Facial weakness resolved Pain and paresthesia improving. Intact reflexes including right ankle jerk |
| 43/M [10] |
Severe bilateral facial weakness, Myalgia, paresthesia of both hands and feet, severe neck pain, urinary retention, dysphagia, altered taste and paresthesia of tongue Normal limb tone, with full power except mild weakness in right hip flexion. Reflexes initially present but then subsequently lost. Flexor plantar responses. Patchy, asymmetrical glove and stocking reduction in pinprick sensation and a sensory ataxia |
None | 11 | P: 2.81 g/L C: 23/mL |
Sensory NCS: UL: absent SNAPs LL: normal Motor NCS: UL and LL: Prolonged DMLs, and F-wave latencies Slow CV Dispersed CMAPs and CB Facial NCS: Absent. Facial EMG: Few fibrillations, no volitional motor units |
MRI pre and post GAD contrast: normal except for bilateral smooth contrast enhancement along whole facial nerve | IVIg | 20% improvement in facial weakness. Ataxic gait and pain static. Areflexia persists. No longer in urinary retention |
| 51/M [10] |
3-week history of severe LL cramping pain. Numbness in feet and hands, spreading proximally to the ankles. Progressive right facial weakness became severe and bilateral after 5 days. Tone, power, and reflexes in limbs were normal. Impaired sensation in all modalities in UL and LL with a sensory ataxia |
None | 7 | P: 5.14 g/L C: 1/mL |
Sensory NCS: UL: reduced SNAP amplitudes LL: normal Motor NCS: UL and LL: Dispersed CMAPs Tibial F wave latencies prolonged Facial NCS: Normal except blink reflexes absent Facial EMG: Very reduced volitional motor units |
MRI pre and post GAD contrast: normal except for bilateral smooth contrast enhancement along whole facial nerve | None | 95% improvement in facial weakness. Ataxic gait 80% better. 25% improvement in pain and paresthesia |
| 71/F [10] |
Lower back and abdominal pain. Altered taste and sequential facial weakness within 24 h. Mild proximal LL weakness. Slight weakness in hip flexion bilaterally. Absent knee and left ankle reflexes with normal sensory examination |
None | 12 | P: 0.96 g/L C: 1/mL |
Sensory NCS: UL and LL: reduced/absent SNAP amplitudes and velocities Motor NCS: UL and LL: Prolonged DMLs Dispersed CMAPs Facial NCS: Not tested Facial EMG: Not tested |
Normal MRI. NO post contrast study. Normal CT performed |
None | Residual mild facial weakness, proximal leg weakness and mild paresthesia. Reflexes regained |
| 53/M [10] |
Lower back discomfort and radicular pain. Facial, perioral and LL paresthesia progressing to severe simultaneous bilateral facial weakness. Depressed UL reflexes. Normal LL reflexes. Mild distal LL sensory loss to vibration and pinprick |
None | 8 | P: 1.22 g/L C: 0/mL |
Sensory NCS: Not tested Motor NCS: Not tested Facial NCS: Not tested Facial EMG: Not tested |
Normal MRI. NO post contrast study. Normal CT performed |
None | 95% resolution of facial weakness, pain and paresthesia |
| 48/M [11] |
Severe back pain. Bilateral facial weakness | None | 10 | P: (1264 mg/L C: 8 × 10 × 6 /L lymphocytes |
Severe, multifocal sensorimotor demyelinating polyneuropathy, with reduced compound motor action potentials, reflecting likely hypoexcitability |
Normal CT and MRI of the brain | IVIgs Oral Prednisolone |
Rapid improvement following the treatment |
| 59/M [12] |
Four limb distal paresthesia and postural instability. Bilateral facial palsy (House–Brackmann grade V). Gait ataxia, global areflexia, and distal paresthesia both at the LL and UL; Normal pallesthesia. Segmental strength diffusely preserved (MRC: 5/5). No spine sensory level. No vegetative, or sphincter involvement | None | 10 | P: 140 mg/dL C: normal white blood cell count |
Motor polyradiculoneuropathy with temporal dispersion of the tibial nerve cMAP bilaterally, with F reflex absent in all districts. No sensory involvement, particularly no temporal dispersion of the sural nerve SNAP bilaterally | Unremarkable brain and cervical MRI with gadolinium | IVIg | Slowly improved |
| 49/M (Present case report) |
Headache, bifacial paresis and paresthesias; lower limbs areflexia, lumbar back pain | None | 16 | P: 110 mg/dL C: <5/mL |
First admission: Blink reflex: absence of all potentials (R1i, R2i, R2c) with right-sided stimulation and normal findings after left supraorbital stimulation. NCS: absence of demyelinating/axonal neuropathy at upper and lower extremities Second admission: Blink reflex: delay of R1i, R2i after stimulation of left side and R2c delay with right supraorbital stimulation. Absence of R1i and R2i after right stimulation and absence of R2c with left-sided stimulation. NCS: demyelinating sensorimotor polyneuropathy at upper and lower extremities |
Enhancement of facial nerves and cauda equina | IVIg | Progressed to CIDP |
Abbreviations: C: white cell count; CB: conduction block; CIDP: chronic inflammatory demyelinating polyneuropathy; CMAP: compound muscle action potential; CSF: cerebrospinal fluid; CV: conduction velocities; DML: distal motor latency; EMG: electromyography; F: female; GAD: gadolinium; IVIg; intravenous immunoglobulins; LL: lower limb; M: male; NCS: nerve conduction studies; NA: not available; P: protein levels; PLEX: plasmapheresis; R1i: ipsilateral R1; R2i: ipsilateral R2; R2c: contralateral R2; SNAP: sensory nerve action potential; UL: upper limbs.
We recently observed a patient who developed a similar acute syndrome after the first dose of the ChAdOx1 nCoV-19 vaccine, but with worsening of the neuropathy two months after the initial presentation leading to a final diagnosis of CIDP.
2. Case Presentation
The patient was a 49-year-old man who presented asymmetric bilateral facial weakness, and paresthesias in the tongue and face. Sixteen days before symptoms onset he received the first dose of ChAdOx1 nCoV-19 vaccine. He denied infections within the prior month. Neurologic examination showed severe bilateral facial paresis, more prominent on the right side, and lower limbs areflexia. Brain and spinal cord MRI showed enhancement of the facial nerves and of the cauda equina and lower thoracic nerve roots, respectively (Figure 1). Cerebrospinal fluid analysis revealed elevated proteins (110 mg/dL; normal range <45 mg/dL) without pleocytosis, and absence of intrathecal IgG synthesis. Serum search for ganglioside autoantibodies was negative, including anti-GQ1b, anti-GD1b, and anti-GM1 antibodies. Blink reflex test displayed bilateral impairment of the motor efferent pathway, while the remaining nerve conduction studies (NCS) and electromyography (EMG) examination were normal. A microbiological work-up of cerebrospinal fluid has ruled out infection of campylobacter jejuni, Epstein–Barr virus, cytomegalovirus, influenza A virus, and hepatitis A, B, C virus. An initial clinical diagnosis of GBS was made and intravenous immunoglobulins (IVI g; 0.4 g/kg/die for 5 days) were initiated 3 days after symptoms onset with mild improvement of the bifacial paresis and resolution of the hypoesthesia.
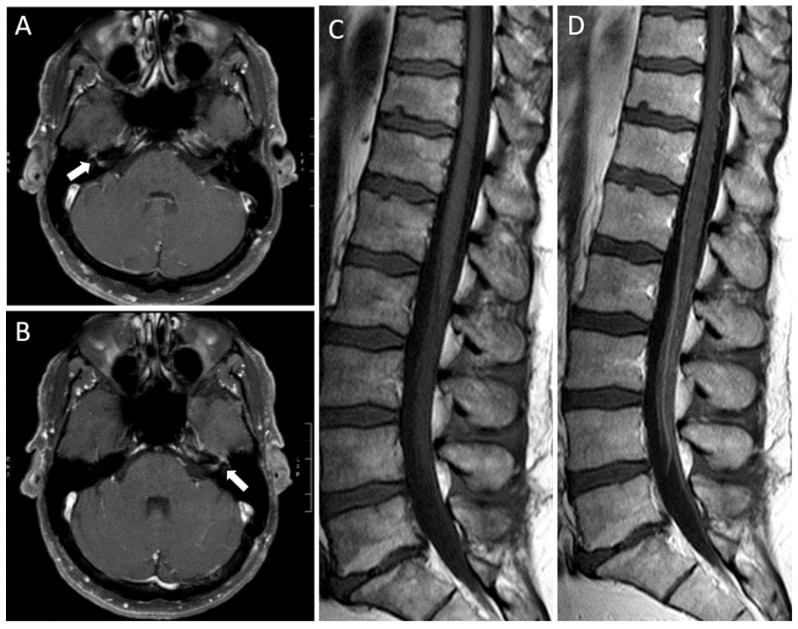
Figure 1.
Brain and spinal cord MRI findings. Axial post-gadolinium T1-weighted images of the brain showing enhancement of the right ((A), arrow) and left ((B), arrow) facial nerves. Sagittal T1-weighted images before (C) and after (D) gadolinium administration showing diffuse enhancement of the cauda equina and lower thoracic nerve roots.
Two months after presentation, his symptoms worsened with painful paresthesias and progressive lower limbs weakness, more prominent during right foot dorsiflexion (4/5 MRC). He developed mild sensory ataxia with wide based gait and postural instability. Repeated nerve conduction study showed marked slowing of sensory and motor conduction velocities of both upper and lower limbs, prolonged distal latency, conduction blocks and absent F response, leading to a diagnosis of chronic inflammatory demyelinating polyneuropathy (CIDP) according to established criteria [13]. He received a second cycle of IVIg with improvement of paresthesias.
Later he was treated with IVIg cycles every six weeks. At last clinical evaluation, six months after presentation, the clinical features were characterized by complete resolution of left facial palsy with persistence of slight weakness in the right upper facial area. Gait ataxia improved but did not resolve completely. Paresthesias on the lower limbs were disabling and thus treatment with pregabalin and alpha lipoic acid was started with benefit. Clinical features and examinations of the patient are summarized in Table 1.
3. Discussion
Acute demyelinating polyneuropathy is a rare, but well recognized complication of COVID-19 vaccines. The disease variant with bifacial weakness has recently been recognized to be more common in patients with adenoviral-vectored (Oxford AstraZeneca, Johnson and Johnson) vs. mRNA-based (Pfizer BioNTech, Moderna) vaccines [14]. In line with these findings, our patients developed an acute demyelinating polyneuropathy with bifacial palsy 2 weeks after the ChAdOx1 nCoV-19 vaccine, but subsequent clinical and EMG worsening prompted a diagnostic revision to CIDP with acute onset. To date, only one patient who developed CIDP after COVID-19 vaccination was reported, with typical gradual onset of ascending lower limb weakness and sensory changes without facial involvement [15].
A difference of the previously described cases of bifacial palsy, in which the clinical course is reported favorable or stabilized or which have been described in the acute phase, in our patient is available the most prolonged follow-up, that is of 6 months. This pro-longed clinical observation led to diagnose a chronic form of demyelinating polyneuropathy, which was an unexpected clinical evolution. Therefore, our report expands on the possible outcomes in patients who develop Guillain–Barrè syndrome after COVID-19 vaccinations and suggest that close monitoring after the acute phase is needed in these patients to exclude a chronic evolution of the disease, which has important implications for long-term treatment.
Our patient presented a clinical onset of GBS with bifacial weakness with paresthesias phenotype; 8 weeks later he presented a clinical deterioration, thus a diagnosis of CIDP was made, supported by neurophysiological findings. The distinction between GBS with fluctuations after start of treatment and CIDP is difficult but it has been recommended that diagnosis of CIDP should be considered when a patient thought to have GBS deteriorates again after 8 weeks from onset or when deterioration occurs 3 times or more [7].
In GBS, acute motor neuropathy may involve facial nerves in various clinical presentations that include unilateral, bilateral facial palsy, bifacial palsy associated with involvement of other cranial nerves and bifacial palsy associated with limb paresthesia, moreover facial involvement is also possible in patients with classical forms of GBS. Interestingly it has been proposed that Bell’s palsy may share similar pathogenic mechanisms with autoimmune neuropathies [16].
The specific clinical phenotype of bifacial weakness with paresthesias is quite uncommon and accounts for about less of 5% of the patients affected with GBS or Miller Fisher spectrum disorders [17], whereas in those patients who have a fluctuating GBS with treatment related fluctuations, who later may become a CIDP, facial involvement was reported to be very common and it is present in about 63% of the patients [7]. On the other hand, CIDP at onset presents uncommonly with cranial nerve involvement, which is reported in about 11% of typical forms mostly with ophthalmological implications rather than facial palsy [13].
GBS and CIDP are immune-mediated disorders in which the exact mechanism of the immune response linked to the pathogenesis is still not clear. In GBS, the pathogenic events are associated with the immune response usually to a previous infection, which subsequently leads to a cross-reaction with the production of antibodies directed to epitopes of the myelin sheath or to peripheral nerves and roots, thus causing an autoimmune process. Antecedent infections are reported in about two-thirds of patients with GBS [17], therefore molecular mimicry between microbial proteins and nerve cell surface has been one of the suggested pathophysiologic mechanisms. CIDP is typically an idiopathic disease, in which an immune response targeting myelin components of the peripheral nervous system develops due to an autoimmune process, which mainly involves immune mechanisms mediated by T cells. In CIDP, the finding of an infection that precedes the onset is rare and unlikely [18]. Numerous antibodies are associated with GBS (such as GD1a, GD1b, GM1, GQ1b), while usually no autoantibodies are identified in CIDP patients, even if variants with antibodies directed against myelin or proteins localized to the Ranvier node have been also described (such as neurofascin, gliomedin, and contactin-1), which appear to result in a more severe disease phenotype [18].
Neuropathies after vaccination are rare event and CIDP developing in the postvaccination period is distinctly unusual, accounting for about 1.5% of patients [19], and poorly described [20]. In our patient, the temporal association between the first dose of ChAdOx1 nCoV-19 vaccine and onset of neuropathy is remarkable so that a triggering role of the vaccine appears to be in causal association. It has been proposed that a postvaccination neurological syndrome could result from the generation of host antibodies that cross-react with proteins present in peripheral myelin [8]. These antibodies may be generated in direct response to the SARS-CoV-2 spike protein, because there is evidence of a cross-reactivity between the SARS-CoV-2 spike protein and peripheral nerve glycolipids [8,21]. This hypothesis is supported by reports of some patients with GBS with bifacial weakness and paresthesias subtype also among patients affected by GBS post COVID-19 [22], even if in these series it does not appear to be the most common phenotype [23]. Therefore, an immune response to other components of the vaccine should be considered, such as a response against the chimpanzee adenovirus vector.
The optimal management and long-term outcomes of these patients remain to be determined. We treated our patient according to the available recommendation with IVIg administration at earliest convenience [17], however, he developed treatment related fluctuations as observed in about 6–10% of all patients with GBS [17]. This may be due to the possibility that the treatment effect has worn off while the inflammatory phase of the disease is still ongoing, and thus further treatment with repeating IVIg cycles was administered and nonetheless, the patient developed a form of CIDP. To our knowledge this is the first case, among GBS with bifacial palsy onset post COVID-19 vaccination, that shows this evolution of the disease, on this regard, it would be interesting to have additional details on the clinical and EMG follow-up of the previous reported cases with short follow up [8,9,12].
In recent months, several case reports have shown that some variants of GBS can occur after the administration of the ChAdOx1 nCoV-19 vaccine, and in particular the bifacial weakness and paresthesia appears to be the prevalent form. This case report clearly shows the need for close monitoring of patients developing GBS after COVID-19 vaccination after the acute phase. We highlight that adequate long-term clinical follow-up is essential in these cases, as evolution to a chronic form is possible, despite adequate treatment. While an eventual causal relationship between different types of COVID-19 vaccines and autoimmune neuropathies remains to be determined, neurologists should be aware of this possibility as prompt diagnosis and treatment is crucial to improve outcomes in patients with GBS or CIDP and other potentially serious neurologic disorders.
Author Contributions
Conceptualization, C.F.B. and D.G.C.; methodology, C.F.B. and A.E.E.; software, P.Z.; validation, A.E.E., E.S. and P.S.; investigation, C.F.B. and E.R.; resources, P.S.; data curation, C.F.B., E.R. and P.Z.; writing—original draft preparation, C.F.B. and D.G.C.; writing—review and editing, C.F.B., D.G.C. and A.E.E.; supervision, P.S.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of University of Sassari.
Informed Consent Statement
Informed consent was obtained from the patient involved in the study.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Voysey M., Clemens S.A.C., Madhi S.A., Weckx L.Y., Folegatti P.M., Aley P.K., Angus B., Baillie B.L., Barnabas S.L., Bhorat Q.E., et al. Oxford COVID Vaccine Trial Group. Safety and efficacy of the ChAdOx1 nCoV-19 vaccine (AZD1222) against SARS-CoV-2: An interim analysis of four randomised controlled trials in Brazil, South Africa, and the UK. Lancet. 2021;397:99–111. doi: 10.1016/S0140-6736(20)32661-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pavord S., Scully M., Hunt B.J., Lester W., Bagot C., Craven B., Rampotas A., Ambler G., Makris M. Clinical Features of Vaccine-Induced Immune Thrombocytopenia and Thrombosis. N. Engl. J. Med. 2021;385:1680–1689. doi: 10.1056/NEJMoa2109908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lunn M.P., Cornblath D.R., Jacobs B.C., Querol L., van Doorn P.A., Hughes R.A., Willison H.J. COVID-19 vaccine and Guillain-Barré syndrome: Let’s not leap to associations. Brain. 2021;144:357–360. doi: 10.1093/brain/awaa444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Principi N., Esposito S. Vaccine-preventable diseases, vaccines and Guillain-Barre’ syndrome. Vaccine. 2019;37:5544–5550. doi: 10.1016/j.vaccine.2018.05.119. [DOI] [PubMed] [Google Scholar]
- 5.Shui I.M., Rett M.D., Weintraub E., Marcy M., Amato A.A., Sheikh S.I., Ho D., Lee G.M., Yih W.K. Vaccine Safety Datalink Research Team. Guillain-Barré syndrome incidence in a large United States cohort (2000–2009) Neuroepidemiology. 2012;39:109–115. doi: 10.1159/000339248. [DOI] [PubMed] [Google Scholar]
- 6.Wakerley B.R., Uncini A., Yuki N. GBS Classification Group; GBS Classification Group. Guillain-Barré and Miller Fisher syndromes--new diagnostic classification. Nat. Rev. Neurol. 2014;10:537–544. doi: 10.1038/nrneurol.2014.138. [DOI] [PubMed] [Google Scholar]
- 7.Ruts L., Drenthen J., Jacobs B.C., Van Doorn P.A. Dutch GBS Study Group. Distinguishing acute-onset CIDP from fluctuating Guillain-Barre syndrome: A prospective study. Neurology. 2010;74:1680–1686. doi: 10.1212/WNL.0b013e3181e07d14. [DOI] [PubMed] [Google Scholar]
- 8.Allen C.M., Ramsamy S., Tarr A.W., Tighe P.J., Irving W.L., Tanasescu R., Evans J.R. Guillain-Barré Syndrome Variant Occurring after SARS-CoV-2 Vaccination. Ann. Neurol. 2021;90:315–318. doi: 10.1002/ana.26144. [DOI] [PubMed] [Google Scholar]
- 9.Maramattom B.V., Krishnan P., Paul R., Padmanabhan S., Cherukudal Vishnu Nampoothiri S., Syed A.A., Mangat H.S. Guillain-Barré Syndrome following ChAdOx1-S/nCoV-19 Vaccine. Ann. Neurol. 2021;90:312–314. doi: 10.1002/ana.26143. [DOI] [PubMed] [Google Scholar]
- 10.Bonifacio G.B., Patel D., Cook S., Purcaru E., Couzins M., Domjan J., Ryan S., Alareed A., Tuohy O., Slaght S., et al. Bilateral facial weakness with paraesthesia variant of Guillain-Barré syndrome following Vaxzevria COVID-19 vaccine. J. Neurol. Neurosurg. Psychiatry. 2021 doi: 10.1136/jnnp-2021-327027. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 11.McKean N., Chircop C. Guillain-Barré syndrome after COVID-19 vaccination. BMJ Case Rep. 2021;14:e244125. doi: 10.1136/bcr-2021-244125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nasuelli N.A., De Marchi F., Cecchin M., De Paoli I., Onorato S., Pettinaroli R., Savoini G., Godi L. A case of acute demyelinating polyradiculoneuropathy with bilateral facial palsy after ChAdOx1 nCoV-19 vaccine. Neurol. Sci. 2021;17:4747–4749. doi: 10.1007/s10072-021-05467-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van den Bergh P.Y.K., van Doorn P.A., Hadden R.D.M., Avau B., Vankrunkelsven P., Allen J.A., Attarian S., Blomkwist-Markens P.H., Cornblath D.R., Eftimov F., et al. European Academy of Neurology/Peripheral Nerve Society guideline on diagnosis and treatment of chronic inflammatory demyelinating polyradiculoneuropathy: Report of a joint Task Force-Second revision. Eur. J. Neurol. 2021 doi: 10.1111/ene.14959. [DOI] [PubMed] [Google Scholar]
- 14.Pegat A., Vogrig A., Khouri C., Masmoudi K., Vial T., Bernard E. Adenovirus COVID-19 vaccines and Guillain-Barré syndrome with facial paralysis. Ann. Neurol. 2021 doi: 10.1002/ana.26258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oo W.M., Giri P., de Souza A. AstraZeneca COVID-19 vaccine and Guillain- Barré Syndrome in Tasmania: A causal link? J. Neuroimmunol. 2021;360:577719. doi: 10.1016/j.jneuroim.2021.577719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mathew T., Hareesh P., Souza D.D., Avati A., Sarma G.R.K., Nadig R., Therambil M., Parry G.J. Bell’s palsy and guillain-barré syndrome may be 2 ends of the same spectrum. Muscle Nerve. 2019;59:E48–E49. doi: 10.1002/mus.26477. [DOI] [PubMed] [Google Scholar]
- 17.Leonhard S.E., Mandarakas M.R., Gondim F.A.A., Bateman K., Ferreira M.L., Cornblath D.R., van Doorn P.A., Dourado M.E., Hughes R.A.C., Islam B., et al. Diagnosis and management of Guillain-Barré syndrome in ten steps. Nat. Rev. Neurol. 2019;15:671–683. doi: 10.1038/s41582-019-0250-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pascual-Goñi E., Martín-Aguilar L., Querol L. Autoantibodies in chronic inflammatory demyelinating polyradiculoneuropathy. Curr. Opin. Neurol. 2019;32:651–657. doi: 10.1097/WCO.0000000000000725. [DOI] [PubMed] [Google Scholar]
- 19.Doneddu P.E., Bianchi E., Cocito D., Manganelli F., Fazio R., Filosto M., Mazzeo G., Cosentino A., Cortese S., Jann A.M., et al. Italian CIDP Database Study Group. Risk factors for chronic inflammatory demyelinating polyradiculoneuropathy (CIDP): Antecedent events, lifestyle and dietary habits. Data from the Italian CIDP Database. Eur. J. Neurol. 2020;27:136–143. doi: 10.1111/ene.14044. [DOI] [PubMed] [Google Scholar]
- 20.Gable K.L., Afshari Z., Sufit R.L., Allen J.A. Distal acquired demyelinating symmetric neuropathy after vaccination. J. Clin. Neuromuscul. Dis. 2013;14:117–122. doi: 10.1097/CND.0b013e318285256b. [DOI] [PubMed] [Google Scholar]
- 21.Fantini J., Di Scala C., Chahinian H., Yahi N. Structural and molecular modelling studies reveal a new mechanism of action of chloroquine and hydroxychloroquine against SARS-CoV-2 infection. Int. J. Antimicrob. Agents. 2020;55:105960. doi: 10.1016/j.ijantimicag.2020.105960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Juliao Caamaño D.S., Alonso Beato R. Facial diplegia, a possible atypical variant of Guillain-Barré Syndrome as a rare neurological complication of SARS-CoV-2. J. Clin. Neurosci. 2020;77:230–232. doi: 10.1016/j.jocn.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Palaiodimou L., Stefanou M.I., Katsanos A.H., Fragkou P.C., Papadopoulou M., Moschovos C., Michopoulos L., Kokotis P., Bakirtzis C., Naska A., et al. Prevalence, clinical characteristics and outcomes of Guillain-Barré syndrome spectrum associated with COVID-19: A systematic review and meta-analysis. Eur. J. Neurol. 2021;28:3517–3529. doi: 10.1111/ene.14860. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.