ABSTRACT
Objective:
Hydrocephalus is one of the most common complications of tuberculous meningitis. Various cerebrospinal fluid diversion procedures, endoscopic third ventriculostomy (ETV) and shunt surgery, are performed for the management of the hydrocephalus associated with tuberculous bacterial meningitis (TBM). There is decreased clarity on the type of procedure to be done. So, this study aims at generating knowledge to understand the conditions in which either of the two procedures, ETV and shunt surgery, is a better option and to develop good practice guidelines for the treatment of tubercular meningitis hydrocephalus (TBMH).
Materials and Methods:
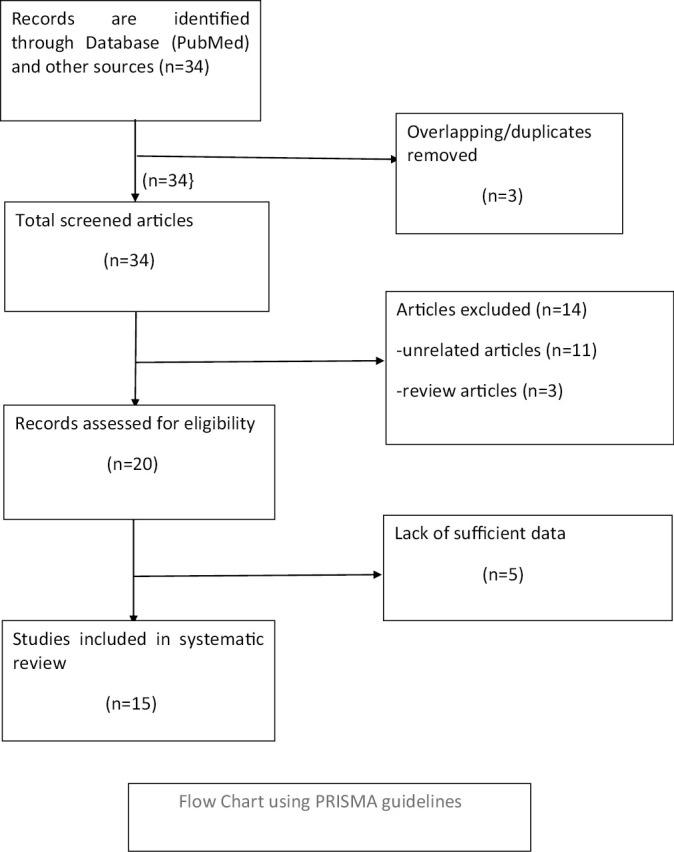
A systematic search of literature was performed by using PubMed and Cochrane Central Register of Controlled Trials (CENTRAL) for articles published from January 2001 to April 2020. A total of 15 studies were included irrespective of their design and having diagnosis with TBMH treated with ventriculoperitoneal shunt surgery (VPS) or ETV. Then, a systemic review was done regarding outcomes, complications, and recommendations made in different studies.
Results:
The total number of patients diagnosed with TBMH was 603; among them, 348 patients had VPS and 255 patients had ETV. In the VPS group, the patient’s good outcome varied from 25% to 68% and complication rate ranged from 10% to 43.8%. The average percentage of good outcome in the VPS group was 51.8%. In the ETV group, the patient’s good outcome varied from 41% to 77% and complication rate ranged from 10% to 23.5%. The average percentage of good outcome in the ETV group was 68%. There was a significant difference in the average percentage of good outcome in the ETV versus the VPS shunt group (P-value was 0.008).
Conclusion:
There was a significant difference in the average percentage of good outcome after ETV than VPS, and complication rate was also slightly lower after ETV than VPS during the chronic phase of illness. So during the acute phase of illness VPS placement is preferred whereas in the chronic burnout phase ETV is preferred because poor anatomy leads to more complications with ETV during the acute phase of the disease.
KEYWORDS: Endoscopic third ventriculostomy, tuberculous meningitis with hydrocephalus, ventriculoperitoneal shunt
INTRODUCTION
Tuberculous meningitis carries a high rate of mortality and morbidity. Hydrocephalus is one of the most common complications of TBM, occurring in up to 85% of children with the disease, and it still remains a major cause of childhood morbidity and mortality in India.[1] It is almost always present in patients who have had the disease for four to six weeks. It is more frequent and severe in children than in adults and also occurs at an earlier stage in the disease process.[2]
Hydrocephalus in patients with TBM could be of either the communicating or the obstructive type, with the former being more common.[3] An obstructive type of hydrocephalus may develop in TBM due to either blockage of fourth ventricle by thick exudates or leptomeningeal scarring.[1] Communicating hydrocephalus may result from an overproduction of cerebrospinal fluid or secondary to reduced absorption of cerebrospinal fluid. Communicating hydrocephalus is seen more commonly in patients with TBM.[1] Schoeman et al. found that the hydrocephalus was of the communicating type in 82% of their patients with TBM.[3]
The management of TBMH includes medical management as well as surgical management. Medical management includes the use of anti-tuberculosis therapy in a combination of steroids, and various dehydrating agents such as acetazolamide, furosemide, and mannitol. Neurosurgical procedures are being used in TBM since 1951. Surgical management of hydrocephalus in patients with TBM included lateral and third ventriculostomy and ventriculo-subarachnoid shunts repeated tapping of the ventricles through burr holes, suboccipital decompression etc.[4] After 1980, shunt surgery and then ETV became popular.
The grade of the patient at admission usually determines the management strategy. There are various grading systems for patients with TBMH. One of the commonly used systems is the Vellore grading system [Table 1] proposed by Palur et al.[5]
Table 1.
Vellore grading of TBMH
| Grade I | Headache, vomiting, fever ± neck stiffness No neurological deficit Normal sensorium |
| Grade II | Neurological deficit present, normal sensorium |
| Grade III | Altered sensorium but easily arousable Dense neurological deficit may or may not be present |
| Grade IV | Deeply comatose Decerebrate or decorticate posturing |
Aims and objectives
To study the comparative outcomes and complications of surgical procedures in TBMH with the aim of endorsing good practice guidelines for the treatment of TBMH.
MATERIALS AND METHODS
A systematic search of literature was performed by using PubMed and CENTRAL for articles published from January 2001 to April 2020. A total of 15 studies [Table 2] on TBMH treated with VPS or ETV, irrespective of their design, were included in this review (flow chart). Most of the studies included pediatric age group patients. A total of 603 patients with TBMH who had undergone VPS surgery or ETV were evaluated. All literature was studied regarding outcomes, complications, and recommendations. A good outcome was defined both clinically and radiologically: clinically as a resolution of signs and symptoms of increased intracranial pressure and radiologically as a reduction in dilatation of the ventricular system and resolution of periventricular ooze. End point of outcome was defined as the resolution of symptoms and signs after VPS and ETV. The success rate of VPS is defined as the resolution of sustained symptoms and working shunt. Statistical analysis of data was made by using the chi-square test to determine P-value (<0.05) to find out significant differences in outcomes after VPS or ETV.
Table 2.
Studies including VP shunt or ETV in patients with TBMH
| S NO. | Study | VPS/ETV | Outcome | Complication | Remark |
|---|---|---|---|---|---|
| 1 | Lampre-ht et al.[6] 2001 | VPS | Total 65 TBMH cases (4–131 months), 38 (noncommunicating) and 27 (communicating) Good outcome: 55.4% cases Mortality: 12.5% cases |
Shunt-related complication: 32.3% cases Shunt infection: 13.5% cases Shunt obstruction: 13.5% cases |
VPS has a high complication rate in TBMH compared with non-tubercular hydrocephalus shunt surgery |
| 2 | Husain et al.[14] 2005 | ETV ± Monroplasty/ septostomy | Total 28 cases (5 months, 68 years) of TBMH Outcome: Overall success rate of 68% (19/28) Satisfactory: 50% (14/28) cases Acceptable: 18% (5/28) cases Unsatisfactory: 32% (9/38) cases |
Complication rate: 10% CSF leak: two cases Perioperative bleed: one case |
He suggested that ETV should be the first surgical option in TBM with communicating hydrocephalus, as outcome was satisfactory (50%) and VP shunt surgery was reserved for cases with ETV failure. |
| 3 | Agrawal et al.[7] 2005 | VPS± EVD | 37 pediatric cases (<18 years) with TBMH Good outcome: 43% (16/37) Moderate disability: 35% (13/37) Severe disability: 16% (6/37) Overall, 62% children in Grade II had good outcome compared with 40% in Grade III All children in Grade III had poor outcome |
Complication rate: 30% Three children had shunt revision multiple times |
Recommend shunt placement in all children of Grade II and III of TBMH. For Grade IV, external ventricular drainage (EVD) followed by shunting, if improvement occurs, remains the most cost-effective procedure. |
| 4 | Jha et al.[15] 2007 | ETV | 14 patients with TBMH ETV was successful in 64.2% (9/14) cases. |
ETV is likely to fail in the presence of advanced clinical grade, extra CNS tuberculosis, dense adhesions in prepontine cistern, and unidentifiable third ventricular floor anatomy. | |
| 5 | Srikantha et al.[8] 2009 | VPS ± EVD | 95 cases of TBMH (Grade IV) Favorable short-term outcome: 33% cases Favorable long-term outcome: 45% cases |
They suggested that direct VP shunt placement is an effective option in patients with Grade IV TBMH, and VP shunt should be considered even in patients who do not exhibit improvement with an EVD. | |
| 6 | Chugh et al.[16] 2009 | ETV | 26 cases of TBMH (7 months, 52 years) Overall success rate was 73.1%. Outcome was better in those cases who were treated with ATT preoperatively for a longer period and it was poor during a higher stage of illness. |
They suggested that ETV should be considered as the first surgical option for CSF diversion in patients with TBM with hydrocephalus. | |
| 7 | Yadav et al.[17] 2011 | ETV | 59 cases (6 months, 76 years) of TBM with obstructive hydrocephalus. Successful outcome: After ETV alone, 58%. After ETV with lumboperitoneal shunt: 80%. |
Blocked stoma: 5.1% cases Malnutrition: 53% Complex hydrocephalus: 22% cases |
ETV was safe and effective in TBMH cases. Complex hydrocephalus and associated cerebral infarct were the major cause of failure to improve. Good results were observed in better grades. ETV was considered the first‑choice treatment in the chronic burnout phase of the disease and in obstructive hydrocephalus. Controversy existed about the role of ETV in the acute phase of the disease and in communicating hydrocephalus. |
| 8 | Peng et al.[9] 2012 | VPS ± EDV | 19 children (one month, 14 years) with TBMH (Grade IV) Full recovery: 21% (4/19) Slight sequelae: 42% (8/19) Severe sequelae : 21%(4/19) Overall success rate: 63% Mortality: 15% (3/19) |
Complication rate was 32% (6/19) | They demonstrated that direct VP shunt placement could improve the outcome in Grade IV TBMH. The response to EVD is not a reliable indication for selecting the patients who would benefit from shunt surgery. |
| 9 | Singh et al.[18] 2005 | ETV | 35 cases of TBMH (6 months, 32 years) Grade I (6) Grade II (7) Grade III (22) The overall success rate of ETV was 77%. Overall, 60% of patients had early recovery and 17% of patients had delayed recovery. Success rate was 87% in patients with thin transparent floor of the third ventricle. |
The presence of a thin and transparent floor of the third ventricle seemed to be associated with a higher success rate of 87%. | |
| 10 | Savardek-ar et al.[19] 2013 | ETV | Overall, 26 cases of TBMH. TBMH Grade III: 21 TBMH Grade IV: 5. After 3 months: In TBMH Grade III Good outcome: 71.4% (15/21) Mortality: 9.5% (2/21). In TBMH Grade IV Good outcome: 20% (1/5) Overall good outcome: 61.5% Mortality: 60% (3/5). |
Complication rate: 23.5% (6/26) | Their opinion was that direct VP shunt placement is a safe and effective option even in poor-grade patients of TBM with hydrocephalus, with a low complication rate. |
| 11 | Goyal et al.[10] 2014 | VPS and ETV each in 24 cases. | 48 pediatric cases with TBMH (<18 years). In the VPS group, successful outcome was 68%. In the ETV group, it was 42%. ETV failure was more in the young age group (<2 years) |
The relative risk of ETV failure is higher than that for shunt, but the risk becomes progressively lower with time. Therefore, if patients survive the early high-risk period, they could experience long-term survival advantage devoid of lifelong shunt-related complications. | |
| 12 | Kankane et al.[11] 2016 | VPS | 50 pediatric cases (3 months, 14 years) with TBMH Grade III and IV (40 & 10). In TBMH Grade III, outcome and mortality were 77.5% and 0%, respectively. In Grade IV, outcome and mortality were 30% and 10%, respectively. Overall outcome: 68% |
Complication rate was 10%. | They suggested the direct placement of the VP shunt in Grade III and IV cases with TBMH without intervening in EVD, and the result was good with a low complication rate. |
| 13 | Aranha et al.[12] 2018 | VPS or ETV each in 26 cases | 52 pediatric patients with TBMH (<18years). Success rate in the ETV group: 65.4% (17/26). In the VP shunt group: 61.54% (16/26). Failure rate in the ETV group: 34.6% (9/26) In the VP shunt group: 38.4% (10/26). Two cases of mortality were seen in each group. |
In the ETV group, one case had CSF leak. In the VPS group, shunt malfunction was seen in seven cases and shunt infection was seen in three cases. |
They found comparable ETV results in communicating hydrocephalus and obstructive hydrocephalus, and they suggested that it can be performed effectively in communicating hydrocephalus, high CSF cell counts, and protein levels, despite an indistinct third ventricular floor anatomy. So, ETV should be attempted as the first-choice CSF diversion procedure in hydrocephalus secondary to TBM where technical expertise and experience with this procedure is available. |
| 14 | Figaji et al.[20] 2007 | ETV | 17 pediatric patients with TBMH (<12years). Success rate: 41% (7/17). Failure rate: 29% (5/17). In five patients, ETV could not be completed due to abnormal anatomy |
Two cases had CSF leak. Thus, complication rate was 11%. | Although ETV is technically possible in this situation, it is imperative that the patients are adequately selected for the procedure to ensure optimal treatment and that the surgeon has experience with difficult cases. |
| 15 | Sil and Chatterjee et al.[13] 2008 | VPS | 32 pediatric patients with TBMH (<12years). Palur Grade II: 22 (62.5%). Palur Grade III: 12 (37.5%). Good outcome: 8 (25%) children. Moderate disability (cognition and ocular motility disorders): 15 (46.9%) children. Severe disability: 5 (15.6%) children. Vegetative state: 1 (3.2%) and death: 3 (9.3%) children. |
Shunt infection: 5 (15.6%). Shunt revisions due to blockade: 14 (43.8%) patients. |
Their opinion was that the VP shunt will remain as the only armamentarium in the arsenal of the neurosurgeon for treating this disease even if it gets replaced by third ventriculostomy in the treatment of other forms of hydrocephalus. |
RESULT
In the ventriculoperitoneal shunt group, good outcome rate varied from 25% to 68% in different studies [Table 3]. Good outcome rate was maximum (68%) in a study performed by Kankane et al. whereas it was minimum (25%) in a study performed by Sil and Chatterjee et al.[6,7,8,9,10,11,12,13] The average percentage of good outcome was 51.8%. It was calculated by the addition of good outcome rate and then by dividing it by the number of VPS studies included in the review.
Table 3.
Comparative studies of good outcome after ETV and VPS in patients with TBMH
| Good outcome after ETV | Good outcome after VPS | p-value | ||
|---|---|---|---|---|
| Husain et al.[14] 2005 | 68% (19/28) | Lamprecht et al.[6] 2001 | 55.4% (36/65) | .008 |
| Jha DK et al.[15] 2007 | 64.2% (9/14) | Agrawal et al.[7] 2005 | 43% (16/37) | |
| Chugh et al.[16] 2009 | 73.1% (19/26) | Srikantha et al.[8] 2009 | 45% (42/95) | |
| Yadav et al.[17] 2011 | 58% (34/59) | Peng et al.[9] 2012 | 63% (12/19) | |
| Singh et al.[18] 2005 | 77% (27/35) | Goyal et al.[10] 2014 | 54.2% (13/24) | |
| Savardekar et al.[19] 2013 | 61.5% (16/26) | Kankane et al.[11] 2016 | 68% (34/50) | |
| Goyal et al.[10] 2014 | 42% (10/24) | Aranha et al.[12] 2018 | 61.5% (16/26) | |
| Aranha et al.[12] 2018 | 65.4% (17/26) | Sil and Chatterjee et al.[13] 2008 | 25% (8/32) | |
| Figaji et al.[20] 2007 | 41% (7/17) | |||
| Average percentage of good outcome | 68% | Average percentage of good outcome | 51.8% | |
In the ETV group, good outcome rate varied from 41% to 77% in different studies and it reached up to 87% in a study performed by Singh et al. when ETV was conducted in patients with a thin and transparent third ventricular wall.[10,12,14,15,16,17,18,19,20] The average percentage of good outcome after ETV was 68%.
There was a significant difference in the average percentage of good outcome after ETV and VPS (p-value was .008), which is statistically confirmed by applying the chi-square test.
The complication rate in the VPS group varied from 10% to 43.8% in different studies: It was minimum (10%) in a study performed by Kankane et al. and maximum (43.8%) in a study done by Sil and Chatterjee et al.[6,7,9,11,12,13,19]
In the ETV group, the complication rate varied from 10% to 23.5% in different studies. It was minimum (10%) in a study done by Husain et al. whereas it was maximum (23.5%) in a study performed by Savardekar et al.[14,17,19,20]
DISCUSSION
Data pertaining to 603 patients were analyzed from all qualified studies for a systematic review. All patients had TBM associated with hydrocephalus, which was treated with either VPS or ETV. Overall, 348 patients underwent VPS whereas 255 patients underwent ETV. For prognostic purposes, various studies divided patients according to different systems of grading for hydrocephalus. In most studies, success rate or good outcome was determined either clinically or radiologically. It was clinically determined by the resolution of signs or symptoms of increased intracranial pressure after VP shunt or ETV. It was radiologically determined by a reduction in the dilatation of the ventricular system and the resolution of periventricular ooze.
In the ventriculoperitoneal shunt group, success rate varied from 25% to 68% in different studies. Success rate was maximum (68%) in a study performed by Kankane et al. whereas it was minimum (25%) in a study performed by Sil and Chatterjee et al.[6,7,8,9,10,11,12,13]
In patients with Grade III TBMH after VPS placement, the studies conducted by Savardekar et al. and Kankane et al. showed comparable good outcomes in 71.4% and 77.5%, respectively.[11,19] However, Agrawal et al., reported good outcome only in 40% patients.[7] Kankane et al. found severe disability in 22.5% patients. As expected, poor outcome in patients with Grade IV TBMH after VP shunt placement varied from 10% to 100% in different studies.[7,8,11]
The complication rate in the VPS group rate varied from 10% to 43.8% in different studies: It was minimum (10%) in a study performed by Kankane et al. and maximum (43.8%) in a study done by Sil and Chatterjee et al.[6,7,9,11,12,13,19] Most of the complications were related to shunt surgery, such as shunt infection, shunt obstruction, which led to shunt failure and frequent shunt revision. It has been reported that the complications of shunt surgery are higher in patients with TBM than in patients with other conditions. The reasons for these complications were the poor general condition of patients and also the presence of higher protein and cellular content in the CSF, leading to more frequent shunt obstruction.
Agarwal et al. reported shunt-related complications in 11 (30%) children, and three of 37 children (8.10%) had to undergo multiple shunt revisions.[7] Kankane et al. found shunt-related complications in 10% cases, among whom 4% had infection and 6% had shunt blockade.[11] Savardekar et al. observed VP shunt-related complications in 23.5% patients.[19] In a study of 26 shunt surgeries, Aranha et al. found 38.4% failure rate and all these required shunt revisions.[12] Sil and Chatterjee et al. found shunt infection in 15.6% cases and shunt blockade in 43.8% cases.[13]
In the ETV group, success rate varied from 41% to 77% in different studies and it reached up to 87% in a study performed by Singh et al. when ETV was done in patients with a thin and transparent third ventricular wall.[10,12,14,15,16,17,18,19,20]
In the ETV group, complication rate varied from 10% to 23.5% in different studies. It was minimum (10%) in a study done by Husain et al. whereas it was maximum (23.5%) in a study performed by Savardekar et al. In the ETV group, the most common reported complications were CSF leak, bleeding during the surgery, and stoma block. Failure to improve after ETV can be due to the blocked stoma, complex hydrocephalus, or vascular compromise. The ETV is technically difficult in post-infective hydrocephalus, especially in the acute phase of the disease due to the presence of inflammation, thick and opaque floor of the third ventricle. This is possibly due to an increased risk of hemorrhage and neurovascular injury, especially in the acute phase.[14,17,19] Endoscopic third ventriculostomy over VPS avoids the insertion of a foreign body in the form of a shunt; it leads to the prevention of complications such as shunt infection, blockage, and abdominal pseudo-cyst formation.
CONCLUSIONS
In this systematic review, there was significant difference in the average percentage of good outcome after ETV than VPS. The outcome was poor in TBM with Grade IV compared with Grade III after VPS. Complication rate was slightly lower in ETV than VPS during the chronic phase of illness. So during the acute phase VP shunt surgery is preferred whereas during the chronic burnout phase ETV is preferred because poor anatomy leads to more complications with ETV during the acute phase of the disease.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rajshekhar V. Management of hydrocephalus in patients with tuberculous meningitis. Neurol India. 2009;57:368–74. doi: 10.4103/0028-3886.55572. [DOI] [PubMed] [Google Scholar]
- 2.Tandon PN. Tuberculous meningitis (cranial and spinal) In: Vinken PJ, Bruyn GW, editors. Handbook of Clinical Neurology. Infections of the Nervous System. Vol. 33. Amsterdam: North-Holland; 1978. pp. 195–262. [Google Scholar]
- 3.Schoeman J, Donald P, van Zyl L, Keet M, Wait J. Tuberculous hydrocephalus: comparison of different treatments with regard to ICP, ventricular size and clinical outcome. Dev Med Child Neurol. 1991;33:396–405. doi: 10.1111/j.1469-8749.1991.tb14899.x. [DOI] [PubMed] [Google Scholar]
- 4.Cairns H. Neurosurgical methods in the treatment of tuberculous meningitis with a note on some unusual manifestations of the disease. Arch Dis Child. 1951;26:373–86. doi: 10.1136/adc.26.129.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Palur R, Rajshekhar V, Chandy MJ, Joseph T, Abraham J. Shunt surgery for hydrocephalus in tuberculous meningitis: A long-term follow-up study. J Neurosurg. 1991;74:64–9. doi: 10.3171/jns.1991.74.1.0064. [DOI] [PubMed] [Google Scholar]
- 6.Lamprecht D, Schoeman J, Donald P, Hartzenberg H. Ventriculoperitoneal shunting in childhood tuberculous meningitis. Br J Neurosurg. 2001;15:119–25. doi: 10.1080/02688690020036801. [DOI] [PubMed] [Google Scholar]
- 7.Agrawal D, Gupta A, Mehta VS. Role of shunt surgery in pediatric tubercular meningitis with hydrocephalus. Indian Pediatr. 2005;42:245–50. [PubMed] [Google Scholar]
- 8.Srikantha U, Morab JV, Sastry S, Abraham R, Balasubramaniam A, Somanna S, et al. Outcome of ventriculoperitoneal shunt placement in grade IV tubercular meningitis with hydrocephalus: A retrospective analysis in 95 patients. Clinical article. J Neurosurg Pediatr. 2009;4:176–83. doi: 10.3171/2009.3.PEDS08308. [DOI] [PubMed] [Google Scholar]
- 9.Peng J, Deng X, He F, Omran A, Zhang C, Yin F, et al. Role of ventriculoperitoneal shunt surgery in grade IV tubercular meningitis with hydrocephalus. Childs Nerv Syst. 2012;28:209–15. doi: 10.1007/s00381-011-1572-0. [DOI] [PubMed] [Google Scholar]
- 10.Goyal P, Srivastava C, Ojha BK, Singh SK, Chandra A, Garg RK, et al. A randomized study of ventriculoperitoneal shunt versus endoscopic third ventriculostomy for the management of tubercular meningitis with hydrocephalus. Childs Nerv Syst. 2014;30:851–7. doi: 10.1007/s00381-014-2371-1. [DOI] [PubMed] [Google Scholar]
- 11.Kankane VK, Gupta TK, Jaiswal G. Outcome of Ventriculoperitoneal shunt surgery, without prior placement of external ventricular drain in Grades III and IV patients of tubercular meningitis with hydrocephalus: a single institution’s experience in the pediatric population and review of literature. J Pediatr Neurosci. 2016;11:35–41. doi: 10.4103/1817-1745.181265. 10.4103/1817-1745.181265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aranha A, Choudhary A, Bhaskar S, Gupta LN. A randomized study comparing endoscopic third ventriculostomy versus ventriculoperitoneal shunt in the management of hydrocephalus due to tuberculous meningitis. Asian J Neurosurg. 2018;13:1140–7. doi: 10.4103/ajns.AJNS_107_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sil K, Chatterjee S. Shuning in tuberculous meningitis: A neurosurgeon’s nightmare. Child Nerv Syst. 2008;24:1029–32. doi: 10.1007/s00381-008-0620-x. 10.1007/s00381-008-0620-x. [DOI] [PubMed] [Google Scholar]
- 14.Husain M, Jha DK, Rastogi M, Husain N, Gupta RK. Role of neuroendoscopy in the management of patients with tuberculous meningitis hydrocephalus. Neurosurg Rev. 2005;28:278–83. doi: 10.1007/s10143-005-0397-2. [DOI] [PubMed] [Google Scholar]
- 15.Jha DK, Mishra V, Choudhary A, Khatri P, Tiwari R, Sural A, et al. Factors affecting the outcome of neuroendoscopy in patients with tuberculous meningitis hydrocephalus: A preliminary study. Surg Neurol. 2007;68:35–42. doi: 10.1016/j.surneu.2006.10.055. 10.1016/j.surneu.2006.10.055. [DOI] [PubMed] [Google Scholar]
- 16.Chugh A, Husain M, Gupta RK, Ojha BK, Chandra A, Rastogi M. Surgical outcome of tuberculous meningitis hydrocephalus treated by endoscopic third ventriculostomy: Prognostic factors and postoperative neuroimaging for functional assessment of ventriculostomy. J Neurosurg Pediatr. 2009;3:371–7. doi: 10.3171/2009.1.PEDS0947. [DOI] [PubMed] [Google Scholar]
- 17.Yadav YR, Parihar V, Agrawal M, Bhatele PR. Endoscopic third ventriculostomy in tubercular meningitis with hydrocephalus. Neurol India. 2011;59:855–60. doi: 10.4103/0028-3886.91365. [DOI] [PubMed] [Google Scholar]
- 18.Singh D, Sachdev V, Singh AK, Sinha S. Endoscopic third ventriculostomy in post-tubercular meningitic hydrocephalus: A preliminary report. Minim Invasive Neurosurg. 2005;48:47–52. doi: 10.1055/s-2004-830183. [DOI] [PubMed] [Google Scholar]
- 19.Savardekar A, Chatterji D, Singhi S, Mohindra S, Gupta S, Chhabra R. The role of ventriculoperitoneal shunt placement in patients of tubercular meningitis with hydrocephalus in poor neurological grade: A prospective study in the pediatric population and review of literature. Childs Nerv Syst. 2013;29:719–25. doi: 10.1007/s00381-013-2048-1. [DOI] [PubMed] [Google Scholar]
- 20.Figaji AA, Fieggen AG, Peter JC. Endoscopy for tuberculous hydrocephalus. Childs Nerv Syst. 2007;23:79–84. doi: 10.1007/s00381-006-0195-3. [DOI] [PubMed] [Google Scholar]


