Abstract
In designing a new drug, considering the preferred route of administration, various requirements must be fulfilled. Active molecules pharmacokinetics should be reliable with a valuable drug profile as well as well-tolerated. Over the past 20 years, nanotechnologies have provided alternative and complementary solutions to those of an exclusively pharmaceutical chemical nature since scientists and clinicians invested in the optimization of materials and methods capable of regulating effective drug delivery at the nanometer scale. Among the many drug delivery carriers, lipid nano vesicular ones successfully support clinical candidates approaching such problems as insolubility, biodegradation, and difficulty in overcoming the skin and biological barriers such as the blood–brain one. In this review, the authors discussed the structure, the biochemical composition, and the drug delivery applications of lipid nanovesicular carriers, namely, niosomes, proniosomes, ethosomes, transferosomes, pharmacosomes, ufasomes, phytosomes, catanionic vesicles, and extracellular vesicles.
Keywords: lipid vesicles, niosomes, proniosomes, ethosomes, transferosomes, pharmacosomes, ufasomes, phytosomes, catanionic vesicles, extracellular vesicles
1. Introduction
Despite relevant technological improvements, developing an effective and safe drug can be a complex, low success rate, time-consuming, and costly practice. As reported on the official webpage of the US Food and Drug Administration (FDA), only a small number of treatment tools (active molecules, nanoparticles, and so on) proposed as skilled medical products, after early testing, result as eligible for further study. In 2020, the FDA’s Center for Drug Evaluation and Research (CDER) authorized 53 novel therapeutics, more than double what happened from 2006–2010. More in details considering the three major therapeutic areas, the new approved drugs are 18 (34%) cancer products, 8 (15%) Neurology products, and 6 (11%) infectious diseases treatments. The average projected peak sales of a just approved drug in 2020 was about USD 700 million, and this is below a long-term average of USD 1.3 billion and a median of USD 500 million [1].
The constant development of technologies and materials resulting from the collaboration between sectors such as bioengineering, physics, chemistry, materials science, pharmacology, and not least medicine, has allowed the advancement of increasingly efficient drug delivery tools. Researchers and clinicians from all over the world daily pursue the design and implementation of increasingly personalized, safe, and cheap care solutions as new pharmacologically active molecules and nanoparticles. Recently, the application of nanoparticles (NPs) has been established to develop drug delivery efficiency. Nanomaterials generally refer to a material characterized by having at least one dimension in the nanometer scale (1–100 nm) [2], include nano-drug delivery systems that thanks to their morphological, optical, mechanical, and electrical characteristics can improve drugs’ stability and solubility by extending their blood circulation time and enhancing their delivery efficiency.
Metallic, polymeric, organic, and inorganic nano scaled materials including dendrimers, nanotubes micelles, and quantum dots (QDs) have been recently assessed as drug delivery carriers (DDC) [3,4,5].
Among the already numerous nanoscale DDCs, nanovesicles represent highly-promising effective approaches to setting up therapies against cancer, inflammation infection, and degenerative disorders.
In this review, we described the most modern lipid-based nanovesicular systems, whether they are of biological or synthetic origin, used for the most distinct biomedical and clinical applications. We left liposomes, already the subject of numerous and recent scientific publications, out of the topics covered in this review, to make room for other lipidic nanovesicles, perhaps less known, but increasingly the target of studies for drug delivery applications such as niosomes, proniosomes, ethosomes, transferosomes, pharmacosomes, ufasomes, phytosomes, and catanionic vesicles. Last, but certainly not least, the type of Lipid NanoVesicles (LNV) discussed in this review are the extracellular vesicles (EVs) and their increasingly wide application as DDC of inorganic NPs, drugs, and nucleic acids. For each type of LNV category covered by the discussion, we provided an updated table listing in a very detailed way, the biochemical composition of each vesicle, its cargo, and the application for which it has been designed and studied referring to the in vitro and in vivo drug delivery applications of the last 10 years.
2. Proniosomes and Niosomes
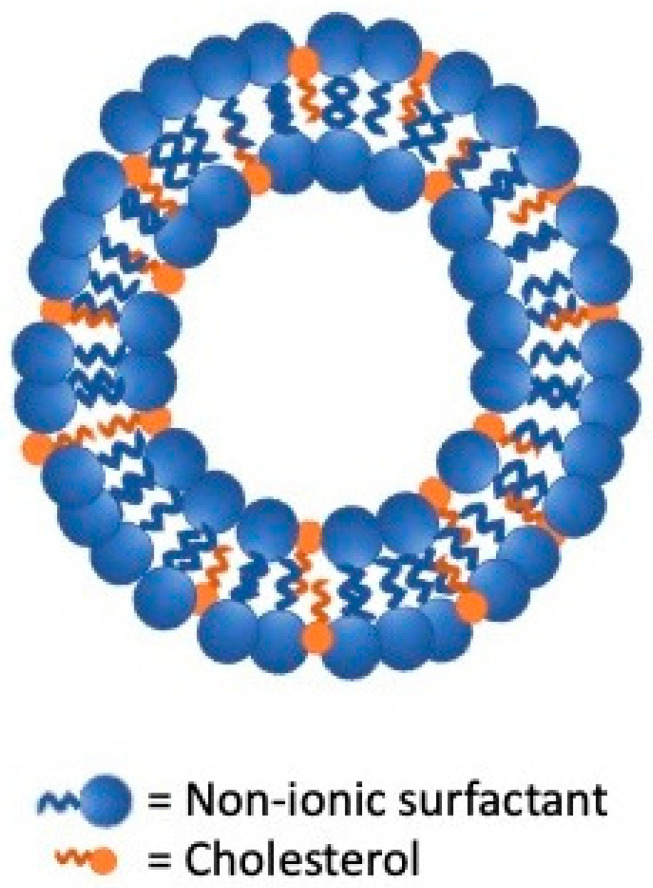
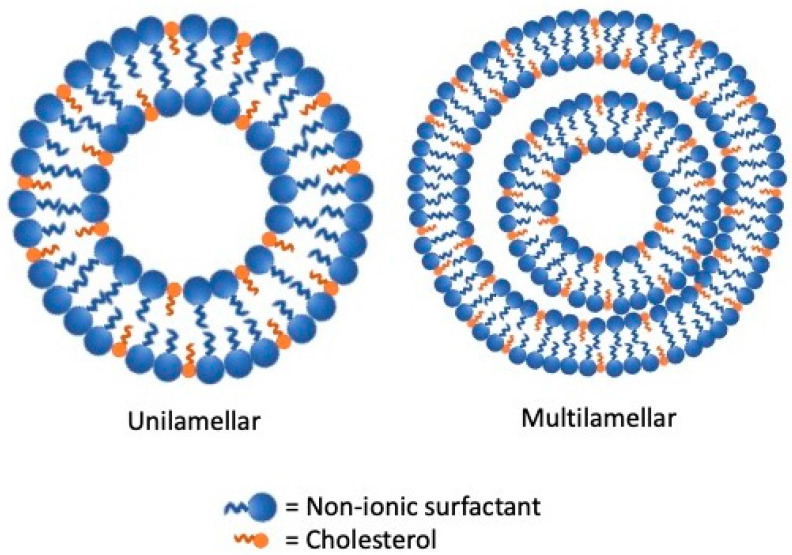
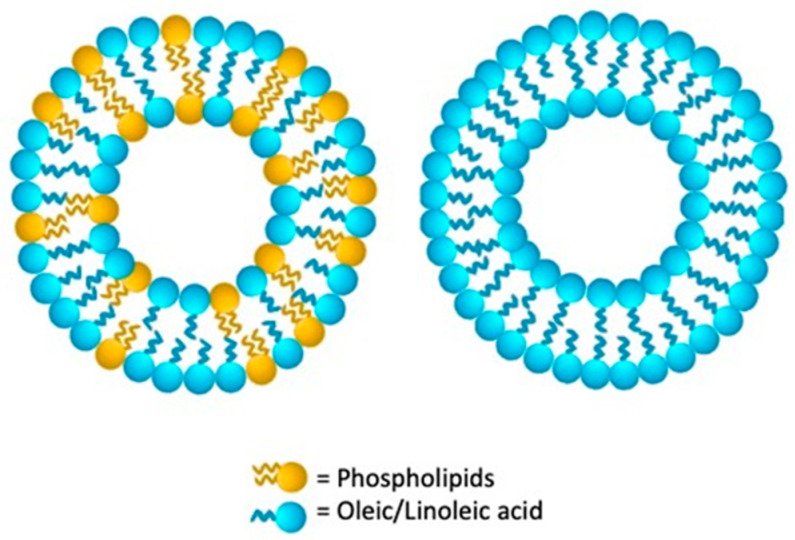
Niosomes and proniosomes are LNV systems characterized by distinctive amphiphilic structures able to improve poorly soluble drugs bioavailability. Their uniqueness is in having a nonionic surfactant backbone while their multilamellar and unilamellar vesicles structures appear similar to that of liposomes [6] (Figure 1 and Figure 2).
Figure 1.
Structure of proniosomes lipid vesicular systems.
Figure 2.
Structure of niosomes lipid vesicular systems.
It is assumed that lipophilic molecules are confined within the lipid bilayers while the hydrophilic ones are retained in the niosomes’ aqueous partitions. This efficient compartmentalization improves the stability of the enclosed drugs preventing their chemical and enzymatic degradation [7]. Proniosomes are nonionic dehydrated structured provesicles in the powdered form or in the gel states. Provesicles are water soluble dry free-flowing granular products that can be immediately rehydrated before use avoiding many issues related to aqueous vesicular dispersions. Proniosomes and niosomes can be produced by using cholesterol, non-ionic surfactants (Tween 20, 40, 80, Span 20, 40, 60, 80, 85), solvents as chloroform and methyl and ethyl alcohols and lecithin. Usually, surfactants utilized to produce niosomes and proniosomes are characterized by low aqueous solubility but Tween can be successfully used to produce micelles on hydration [8].
Niosomes are similar to liposomes, but they are cheaper, exhibit a higher stability, encapsulation efficiency, and permeability for small molecules, avoid the degradation of phospholipids by oxidation, and are easier to store and handle. Indeed, niosomes display some drawbacks, such as aggregation, fusion, and leakage of drugs, while proniosomes can overcome these issues contrasting leakage, aggregation, or hydrolysis of drugs while optimizing their storage and biodistribution, adding the possibility of sterilization, room temperature storage, and being rehydrated instantly to create niosomes [9].
Proniosomes have several pluses over niosomes, contrasting leakage, aggregation, or hydrolysis of drugs while optimizing their storage and biodistribution.
Although the first applications of non-ionic surfactant nanovesicles were cosmetic ones [10,11], in Table 1 and Table 2, we report the numerous and recent drug delivery applications for proniosomes and niosomes, respectively.
Table 1.
Proniosomes’ drug delivery applications.
| Composition | Cargo | Application | Reference |
|---|---|---|---|
| Cholesterol, Span 60 and maltodextrin | Aceclofenac | Anti-inflammatory in osteoarthritis | [12] |
| Cholesterol, Span 60, maltodextrin and stearylamine | Acemetacin | Anti-inflammatory | [13] |
| Cholesterol, lecithin, Span 60 and Span 40 | Atenolol | Hypertension treatment | [14] |
| Cholesterol, lecithin and Tween 80 | Atorvastatin calcium | Anti- hyperlipidemic | [15] |
| Cholesterol, lecithin and Span 40 | Boswellic acid | Anti-inflammatory | [16] |
| Cholesterol, lecithin and Span 60 | Caffeine | Migraine treatment | [17] |
| Cholesterol and Span 60 | Cilostazole | Anti-platelet | [18] |
| Cholesterol, lecithin and Span 60 | Clozapine | Treatment of psychiatric disorders | [19] |
| Cholesterol, lecithin and cremophor RH | Curcumin | Against ocular inflammation | [20] |
| Cholesterol, Span 60 and Tween 80 | Ciprofloxacin | Anti-inflammatory | [6] |
| Cholesterol, Span 40 TPGS | Docetaxel | Anticancer treatment | [21] |
| Cholesterol and Span 60 | Famotidine | H2 receptor antagonist | [22] |
| Cholesterol, Sorbitol and Span 80 | Flurbiprofen | Anti-inflammatory | [23] |
| Cholesterol and Brij35 | D-limonene | Cancer therapy | [24] |
| Cholesterol, Span 60 | Itroconazole | Antimicotic against candida albicans | [25] |
| Cholesterol, lecithin and cremophor RH 40 | Lacidipine | Treatment of hypertension and atherosclerosis | [26] |
| Cholesterol, Tween 80, sorbitol and sucrose | Letrozole | Breast cancer | [27] |
| Cholesterol, Span 80 and lecithin | Lignocaine Hydrochloride | Dental anesthesia | [28] |
| Cholesterol, Span 60 and Tween 60 | Lomefloxacin HCl | Treatment of bacterial conjunctivitis | [29] |
| Cholesterol, lecithin and Lutrol F68 | Lornoxicam | Anti-inflammatory for rheumatoid arthritis, osteoarthritis and surgeries | [30] |
| Cholesterol, lecithin and Span 60 | Embelin | Analgesic and anti-inflammatory | [31,32] |
| Span 40, Span 60, and Brij series 72 | Fluconazole | Management of dental pain | [33] |
| Cholesterol, lecithin and Span 60 | Naproxen | Anti-inflammatory | [32] |
| Cholesterol, Span 60 and maltodextrin | Pentazocine | Management of cancer pain | [34] |
| Cholesterol, Span 60, maltodextrin, pullulan and DPPH | Resveratrol | Controlling free radicals causing oxidative stress-induced cardiovascular diseases, atherosclerosis, cancer | [35] |
| Cholesterol, Span 60, lecithin and stearylamine | Risperidone | Treatment of schizophrenia and other psychiatric disorders | [36] |
| Cholesterol, lecithin and Span 80 | Tramadol | Anti-inflammatory and antinociceptive | [37] |
| Cholesterol, Span 60, lactose and mannitol | Vismodegib | Carrier for the pulmonary route | [38] |
Table 2.
Niosomes’ drug delivery applications.
| Composition | Cargo | Application | Reference |
|---|---|---|---|
| Span 60, cholesterol and bile salt | Acetazolamide | Decrease ocular pressure in glaucoma patients | [39] |
| Span 60, cholesterol, HMPC and carbopol | Acetazolamide and carvedilol | Decrease ocular pression in glaucoma patients | [40] |
| Cholesterol, lecithin, Span 60 and Tween 60 | Acyclovir | Antiviral | [41] |
| Span60, Cholesterol and DCP or Span60, Cholesterol and TPGS | [42] | ||
| Cholesterol and Span 40 | Betaxolol | Glaucoma treatment | [43] |
| Ergosterol, Span 60 and Tween 60 | Carum | Anticancer | [44] |
| Cholesterol and Span/Tween 60 | Carvedilol | Congestive heart failure, coronary artery disease, postmyocardial settings | [45] |
| Bile salt-enriched vesicles, with 20% sodium cholate and 30% sodium taurocholate | Beta receptor blocking activity to preclude angina and cardiac arrhythmias | [46] | |
| Cholesterol, Span 60 and Tween 60 | Cephalexin | Antibacterial | [47] |
| Cholesterol, Span 40 and Tween 40 | Ciprofloxacin | Antibacterial | [48] |
| Cholesterol, Span 60 and Tween 60 | [49] | ||
| Cholesterol, span and tween 20 | Curcumin | Antinociceptive and anti-inflammatory | [50] |
| Cholesterol, Span 80, PEG | Daunorubicin and anti-CD123 | Treatment of acute myeloid leukemia | [51] |
| Cholesterol, Span 40 and tween 40 | D-limonene | Cancer therapy | [52] |
| Pluronic L64, Tween 60, EMG 707 Ferrofluid | Doxorubicin | Therapy against chronic myelogenous leukemia | [53] |
| Pluronic L64, Cholesterol and transferrin | Cancer therapy | [54] | |
| Cholesterol, Span 40 and tween 40 | Doxorubicin and Hydrophobin-1 | Cancer therapy | [55] |
| Cholesterol and Span 60 | Doxorubicin and N-lauryl glucosamine | Targeted cancer therapy | [56] |
| Cholesterol, Span 60 and Tween 60 | Doxycyclin | Treatment of infection-associated prostate cancer | [57] |
| Cholesterol and Span 60 | Doxycyclin hyclate | Management of ocular diseases | [58] |
| Cholesterol, Span 60 and phospholipid 90G | Embelin | Diabetes treatment | [59] |
| Span 40, Span 60, and Brij series 72 | Fluconazole | Antifungal treatments | [60] |
| Cholesterol and Span 60 | Flurbiprofen | Anti-inflammatory | [61] |
| Cholesterol, Span 60 and Tween 65 | Gemcitabine and cisplatin | Lung cancer treatment | [62] |
| Cholesterol, Span 40 and Tween 80 | Levofloxacin | Antibacterial | [63] |
| Cholesterol and Span 60 | Linezolid | Antibacterial | [64] |
| Cholesterol, Span 80 and Tween 80 | Methotrexate | Solid tumor treatment | [65] |
| Span 60, PVA and cremophor RH40 | [66] | ||
| Cholesterol and glucopyranoside | [67] | ||
| Cholesterol and Span 40 | Metformin hydrochloride | Avoid Metformin-associated lactic acidosis in the treatment of diabetes mellitus | [68] |
| Cholesterol and Span 60 | Minocyclin | Antibacterial coating of dental implants | [69] |
| Cholesterol and Tween 60 | Moxifloxacin | Antimicrobial | [70] |
| Cholesterol and tyloxapol | Nevirapine | HIV treatment | [71] |
| Cholesterol, Span 60 and SolulanC24 | N-palmitoylglucosamine | Brain targeting of dynorphin-B | [72] |
| Cholesterol, Span 60 and PEG | Simvastatin | Against myocardial ischemia/reperfusion injury | [73] |
| Cholesterol, Span 20 and Span 60 | Pediatric transdermal dyslipidemia treatment | [74] | |
| Cholesterol and sorbitan monostearate | Tamoxifen citrate | Incorporated in hydrogel as a pH-responsive drug delivery for breast cancer treatment | [75] |
| Cholesterol and Span 20 | Tamoxifen citrate and doxorubicin | Breast cancer treatment | [76] |
| Cholesterol, Span60, PEG and TAT peptide | Tenofovir | HIV treatment | [77] |
| Cholesterol, Span 60 and Tween 40 | Timolol maleate | Glaucoma treatment | [78] |
| Cholesterol and Span 60 | [79] | ||
| Cholesterol and Span 40 | |||
| Cholesterol and Span 60 | Timolol maleate and Brimonidine tartrate | Glaucoma treatment | [80] |
| Cholesterol, Span 60 and Tween 60 | Tobramycin | Antibacterial | [81] |
| Cholesterol, Span 60 and Tween 40 | Vancomycin | Antibacterial | [82] |
| Cholesterol and Span 60 | Antibacterial coating for bone plates | [83] | |
| Cholesterol and Tween 40 | Zolmitriptan | Migraine treatment | [84] |
| Cholesterol and Span 60 | Chlorotoxin and temozolomide | Targeting and treatment of glyomas | [85] |
| Cholesterol, Span 60 and PEG | Doxorubicin, curcumin and tLyp-1 peptide | Glioblastoma treatment | [86] |
| PEG, Tween 80, Octadecylamine | Akt 1 siRNA, Au NPs and Thymoquinone | Treatment of resistance in breast cancer | [87] |
| Span 80 and PEG | BBIQ [Toll-like receptor (TLR) 7 agonist] and D-1MT [Indoleamine2, 3-dioxygenase (IDO) inhibitor] | Cancer vaccine | [88] |
| Tween 80 and DTPA-Cl | BMP-7 plasmid | Bone regeneration | [89,90] |
| Cholesterol and Span 60 | CD9 and CD63 tetraspanins | Exosomes immunoassays | [90] |
| Cholesterol, monopalmitin and Dicetyl phosphate | Influenza antigen | Vaccine and immune response | [91] |
| Cholesterol, Span 80 and Tween 80 | NLS-Mu-Mu fusion protein | Gene delivery | [92] |
| Tween 60, DOTMA and lycopene | pCMS-EGFP plasmid | Gene delivery to the brain | [93] |
| Cholesterol, Span 20 and plier-like cationic lipid A (PCL-A) | pDNA or siRNA | Nucleic acid delivery | [94] |
| DOTMA, Tween 20 and Squalene | pEGFP, pGFP, MC-GFP | Treatment of inherited retinal diseases | [95] |
| Cholesterol and Span 20 | pH (Low) insertion peptide (pHLIP) | Tumor targeting | [96] |
| Cholesterol, Tween 20 and cationic lipid (N1,N1-dimyristeroyloxyethyl-spermine) | plasmid DNA-encoding ovalbumin (pOVA) | Skin vaccination | [97] |
| 2,3-di(tetradecyloxy)propan-1-amine cationic lipid, squalene and Tween 80 | Plasmid pCMS-EGFP | Delivery of genetic materials to the retina | [98] |
| Cholesterol and Span 60 | Protective antigen (PA) and PA domain 4 (D4) of Bacillus anthracis | prophylaxis against anthrax | [99] |
| Span 80, DOTAP, TPGS and indocyanine green | siGFP, anti-miR-138 | Promote osteogenesis in hMSCs, theranostic applications | [100] |
| Cholesterol, Tween 85 and DDAB | siRNA | Melanoma treatment | [101] |
| Cholesterol, Span 20 and plier-like cationic lipid B (PCL-B) | siRNA against anti-apoptotic genes (Mcl-1, Bcl-2 and survivin) and doxorubicin | Breast cancer therapy | [102] |
| Cholesterol, Span 60 and PEG | siRNA/proteamine and iron superparamagnetic NPs | Breast cancer therapy | [103] |
| Cholesterol, DOTAP, PEG and Tween 60 | siRNA targeted the CDC20 mRNA, doxorubicin and quercetin | Cancer treatment | [104] |
| Cholesterol and Tween 80 | Ciprofloxacin, rifabutin and lignin Ag NPs | Antibacterial | [105] |
| Cholesterol and Span 80 | Curcumin and Ag/Cu NPs | Antibacterial | [106] |
| Ergosterol, Span 60 and Tween 60 | Protamine-condensed DNA and Fe3O4 NPs | Magnetic properties and cargo-targeted delivery | [107] |
Thanks to their capability to store and deliver both hydrophilic and hydrophobic medications through topical, oral, transmucosal, pulmonary, ocular, and parenteral/intravenous administration, niosomes and proniosomes are increasingly used as vaccines and treatments for infection, inflammation, cancer, and many other acute or chronic diseases.
3. Ethosomes
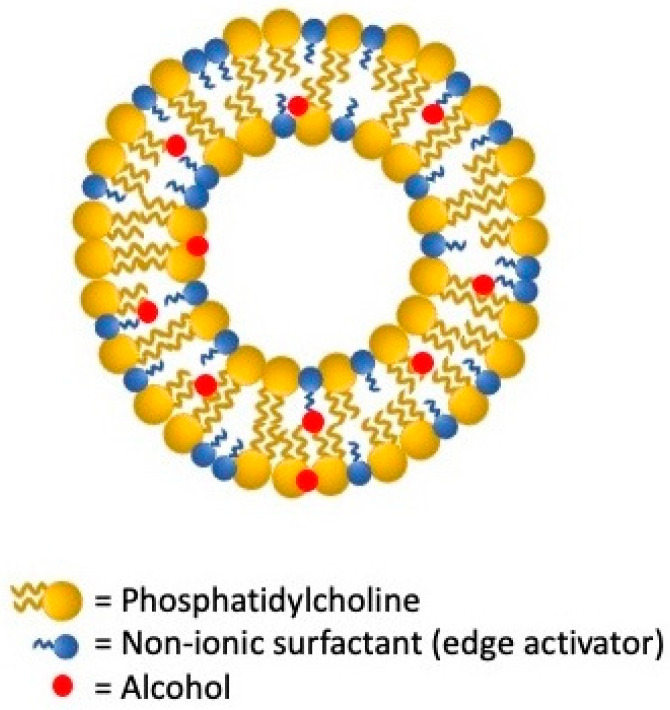
Ethosomes were designed and developed in 2000 by Touitou et al. [108] as an advanced noninvasive passive lipid-based delivery system. As represented in Figure 3, these carriers are lipid bilayers composed of phospholipids, water, and high concentrations of ethanol which gives them remarkable transdermal permeability skills. Ethanol and lipid molecules act in the polar head group region increasing membrane fluidity and permeability. Ethosomes have significantly improved skin delivery, carrying the active compounds in the deeper layers of the skin in occlusive and non-occlusive conditions. In addition, they display high deformability, encapsulation efficiency, stability, biocompatibility, and a negative charge due to ethanol that leads to small vesicles size, enhancing the bioavailability of the compounds. Despite these advantages, there are some drawbacks caused by the volatile nature of ethanol, such as problems related to system instability, drug leakage, and skin irritation [109]. These vesicles are successfully used for topical administration of a considerable variety of drugs such as antifungals, antivirals, antibiotics, anti-inflammatories, and many others as detailed in Table 3.
Figure 3.

Schematic structure of ethosome lipid vesicular system.
Table 3.
Ethosomes’ drug delivery applications.
| Composition | Cargo | Application | Reference |
|---|---|---|---|
| Soy lecithin | 5-Aminolevulinic acid | Treatment of hypertrophic scars | [110] |
| Soy phosphatidylcholine | 5-fluorouracil | Treatment of skin cancers | [111,112] |
| Soy lecithin and cholesterol | Apixaban | Anticoagulant | [113] |
| Soy phosphatidylcholine | Azelaic acid | Treatment of acne | [114] |
| Soy phosphatidylcholine and cholesterol | Boswellic acid | Anti-inflammatory | [115] |
| Phosphatidylcholine | Caffeic acid | Antioxidant | [116] |
| Soy lecithin | Curcumin and glycyrrhetinic acid | Psoriasis treatment | [117] |
| DSPE-PEG2000, hydrogenated soy phospholipids and cholesterol | Curcumin, hyaluronic acid and CD44 | Psoriasis treatment | [118] |
| Soy phosphatidylcholine, polyethylenimine and sodium cholate | Doxorubicin and curcumin | Melanoma treatment | [119] |
| Lecithin and Tween 80 | Fenretinide | Chemopreventive for breast cancer | [120] |
| Soy phosphatidylcholine, cremophor-A25 and chitosan | Ferrous chlorophyllin | Photodynamic therapy for the treatment of squamous cell carcinoma | [121] |
| Phospholipid 90G | Fisetin | Skin cancers treatment | [122] |
| Soy phosphatidylcholine | Flurbiprofen | Anti-inflammatory | [123] |
| Soy phosphatidylcholine | Griseofulvin | Antifungal treatment | [124] |
| Cholesterol and lecithin | Hyaluronic acid | Transdermal delivery of drugs | [125] |
| Soy phosphatidylcholine, cholesterol | HRP IgG | Transdermal delivery of vaccines | [126] |
| Soy phosphatidylcholine, cholesterol and deoxycholic acid | Indomethacin | Treatment of pain and inflammation in rheumatoid arthritis | [127] |
| Soy lecithin and cholesterol | Luteolin | Anti-tumor activity in hepatocellular carcinoma | [128] |
| Soy lecithin | Methotrexate | Treatment of psoriasis | [129] |
| Soy phosphatidylcholine | Methoxsalen | Treatment of vitiligo | [130] |
| Soy phosphatidylcholine, cholesterol and mannitol | Paenolol | Anti-inflammatory, antidiabetic and pain-relieving | [131] |
| Soy phosphatidylcholine | Paeoniflorin | Arthritis therapy | [132] |
| Soy phosphatidylcholine and cholesterol | Phenylethyl resorcinol | Skin Lightening Applications | [133] |
| Soy phosphatidylcholine, stearylamine and propylene glycol | Resveratrol | Antioxidant | [134] |
| Phosphatidylcholine | Retinyl palmitate | Acne treatment | [135] |
| Soy phosphatidylcholine | Sulforaphane | Treatment of skin cancers | [136] |
| Soy phosphatidylcholine | Terbinafine hydrochloride | Antifungal treatment | [137] |
| Phospholipid 90G | Thymoquinone | Treatment of acne | [138] |
| Soy phosphatidylcholine and cholesterol | Thymosin β-4 | Wound repair | [139] |
4. Transfersomes
Many drug delivery systems have been designed over the past decades for transdermal administration, which offers many advantages over other routes thanks to its capability of escaping presystemic metabolism, tune drug release reducing variation in drug levels, enhancing pharmacological response. Compared to most other transdermal delivery methods including chemical permeation enhancers, sonophoresis, microneedles, lipid vesicles thanks to their distinctive composition can transport both hydrophilic and lipophilic drugs [140].
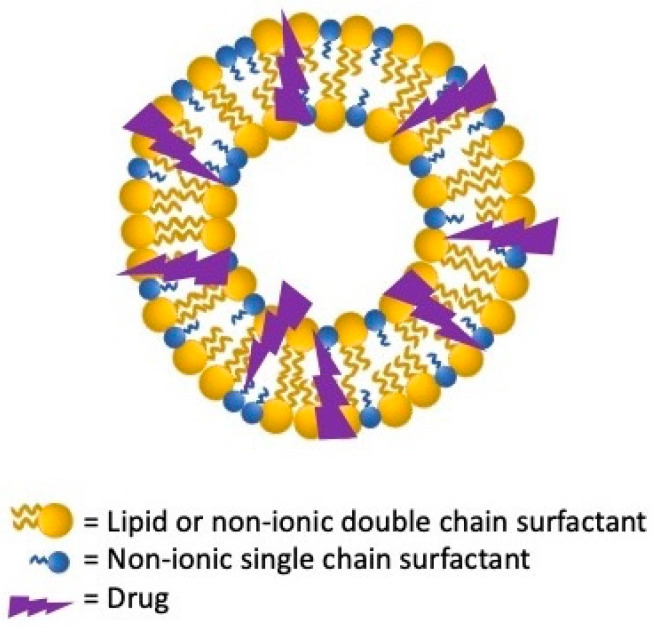
Among the LNV, transfersomes, first proposed in the early 1990s, are ultra-deformable elastic vesicles successfully employed as a non-occluded method able to permeate skin through the stratum corneum reaching the dermis and blood circulation [141]. As schematized in Figure 4, they are firstly characterized by an aqueous core enclosed by a lipid bilayer of amphipathic constituent as phosphatidylcholine, lecithin, or a mixture of lipids. In addition to a very low percentage of alcohol (3–10%), they are made with 10–25% of bilayer-softening complexes, surfactants, or edge activators as Tweens, Spans, sodium cholates, and deoxycholate. The appropriate phospholipids/surfactants ratio tunes transferosomes’ membrane elasticity reducing vesicles’ rupture chances through the skin [142,143]. By having edge activators in their structure, thanks to their remarkable elastic properties, transfersomes defeat many main liposomes’ weaknesses resulting in more apt to squeeze themselves through the skin barrier [144]. Despite these advantageous properties, transfersomes exhibit also some drawbacks, i.e., chemical instability due to the oxidative degradation and expensiveness in the precursors and manufacturing [143].
Figure 4.
Schematic structure of transfersomes lipid vesicular system.
Thanks to their enhanced skin-penetration abilities, transfersomes are competent to set up skin drug storage area for continuous therapeutic molecules delivery releasing low, as well as high, molecular weight drugs as antioxidants, chemotherapy, anti-Inflammatory, and corticosteroids (Table 4).
Table 4.
Transfersomes’ drug delivery applications.
| Composition | Cargo | Application | Reference |
|---|---|---|---|
| Soy lecithin and Span 80 | Aceclofenac | Anti-inflammatory in osteoarthritis | [145] |
| Soy phosphatidylcholine and Tween 80 | Baicalin | Treatment of skin wounds | [146] |
| Soy phosphatidylcholine and Tween 80 | Carvedilol | Prevent skin carcinogenesis | [147] |
| Phospholipon® 90G and sodium cholate | Cilnidipine | Treatment of hypertension | [148] |
| Soy phosphatidylcholine | Deferoxamine | Treatment of pressure ulcers | [149] |
| DPPC, cholesterol, TPGS and folate | Docetaxel | Treatment of glioblastoma multiforme | [150] |
| Soy phosphatidylcholine and sodium cholate | Epigallocatechin-3-gallate and hyaluronic acid | Anti-aging and antioxidant | [151] |
| Soy phosphatidylcholine and Tween 80 | Eprosartan mesylate | Treatment of hypertension | [152] |
| Soy phosphatidylcholine and Span 80 | Genistein (GEN-TF2) | Therapeutic or preventive strategy against neurodegenerative diseases | [153] |
| Soy lecithin and Sodium Lauryl Sulphate | Ivabradine HCl | Treatment of stable angina pectoris | [154] |
| Soy lecithin and Tween 80 | Mangiferin | Treatment of skin wounds | [155] |
| Phospholipon (PL) 90H and Span 60 | Natamycin | Antifungal | [156] |
| Phospholipon 90 G® and sodium cholate | Pentoxifylline | Treatment of intermittent claudication and chronic occlusive arterial diseases | [157] |
| Lecithin and Tween 20/80 | Resveratrol | Antioxidant | [158] |
| Soy phosphatidylcholine, Tween 80 and ceramide III | Retinyl palmitate | Antioxidant | [159] |
| Soy phosphatidylcholine and emu oil | Tamoxifen | Transdermal therapy for breast cancer | [160] |
| Soy lecithin and Tween 80 | Taxifolin | Antioxidant | [161] |
| Soy phosphatidylcholine and Tween 80 | Tocopherol | Antioxidant | [162] |
| Soya lecithin and Tween 80 | Zolmitriptan | Migraine treatment | [163] |
| Soy lecithin and sodium deoxycholate | Human growth hormone | Transdermal hormone delivery | [164] |
| Egg phosphatidylcholine, stearylamine and Tween 20 | PnPP-19 peptide | Treatment of erectile dysfunction | [165] |
5. Pharmacosomes
The name pharmacosomes refers to the amphiphilic, zwitterionic, stoichiometric complexes of polyphenolic compounds with phospholipids, as schematized in Figure 5. The success in the use of pharmacosomes is explained by the surface and bulk interactions of lipids with drugs since the latter possess an active hydrogen atom as –OH, -COOH, -NH2, which can be esterified to the lipid causing an amphiphilic compound [166,167].
Figure 5.
Schematic structure of pharmacosomes lipid vesicular system.
The use of pharmacosomes in drug delivery has several advantages over that of other vesicles such as niosomes, transferosomes, and liposomes. More in detail, any active molecules in which a carboxyl group is present can be esterified without a spacer chain as opposed to those characterized by the presence of amino or hydroxyl groups which, in order to be esterified, require spacer groups. Pharmacosomes design is based on the phospholipids/water superficial and bulk interaction; the drug molecule and the connected lipid molecule, respectively, behave like the polar head group and the lipidic chain giving the molecule an amphipathic character. Thanks to their hydrophilic and lipophilic properties, these lipid LNV improve drugs’ dissolution in gastrointestinal fluid, increasing the bioavailability of low soluble treatments avoiding leak and rupture release [168,169]. Pharmacosomes’ in vivo pharmacokinetic performances are conditioned by vesicles’ dimension, by the drug molecule’s functional groups, by the lipids’ fatty acid chain length, and, last but not least, by the spacer groups’ availability. The high tunability of each of the components listed above makes these types of vesicles excellent candidates for the effective delivery of a wide range of active molecules including anti-cancer and anti-inflammatory remedies (Table 5) [170].
Table 5.
Pharmacosomes’ drug delivery applications.
| Composition | Cargo | Application | Reference |
|---|---|---|---|
| Doxifluridine and DOTAP | miR-122 | Treatment of hepatocellular carcinoma | [173] |
| Etoricoxib and phosphatidylcholine | Rheumatoid arthritis treatment | [174] | |
| Folic Acid-Modified 2-Deoxyglucose and amino ethanol | Targeting anti-tumor therapy | [175] | |
| Ibuprofen and Phosphatidylcholine from soy | Anti-inflammatory | [176] | |
| Levodopa, egg lecithin and chitosan | Parkison’s treatment | [177] | |
| Naproxen and soy lecithin | Rheumatoid arthritis treatment | [178] | |
| Rosuvastatin, soy lecithin and cholesterol | Hyperlipidemia treatment | [179] |
Among the few limitations relating to the use of pharmacoses, reference should be made to their susceptibility to hydrolyzation, fusion, or aggregation during storage or engineering processes [171,172].
6. Ufasomes
Unsaturated fatty acid vesicles preparation, more commonly known as ufasomes, was first reported in 1973 by Gebicki and Hicks [180]. In a controlled pH range, from 7 to 9, they are a closed lipid bilayered suspension, made from unsaturated fats and their ionized species. In detail, fatty acid molecules’ hydrocarbon tails are directed toward the deeper membrane layer while the carboxyl heads are in contact with water [181], as schematized in Figure 6. Oleic and linoleic acid (cis, is-9,12-octadecadienoic acid), the major ufasomes’ constituents, confer to these nanovesicles a more versatile nature than that of the other LNV, by ranking them between different nanosystems formed from double-chain amphiphiles and from single-chain surfactants micelles. Their biochemical composition makes them easily to assemble and real biocompatible [182,183]. By enhancing ufasomes stability with the identification of the appropriate fatty acid, pH range, and lipoxygenase amount, increasingly targeted and effective drug delivery solutions are being developed (Table 6).
Figure 6.
Schematic structure of ufasomes lipid vesicular system.
Table 6.
Ufasomes’ drug delivery applications.
| Composition | Cargo | Application | Reference |
|---|---|---|---|
| Cholesterol and oleic acid | Cinnarizine | Antihistaminic activity | [184] |
| Phosphatidylcholine from soy and oleic acid |
Minoxidil | Hypertension treatment | [185] |
| Phosphatidylcholine from soy oleic and linoleic acid |
Oleuropein | Antioxidant activity | [183] |
| Oleic acid and tea tree oil | Oxiconazole | Candida albicans treatment | [186] |
| Glyceryl oleate | Terbinafine hydrochloride | Candida albicans treatment | [187] |
7. Phytosomes
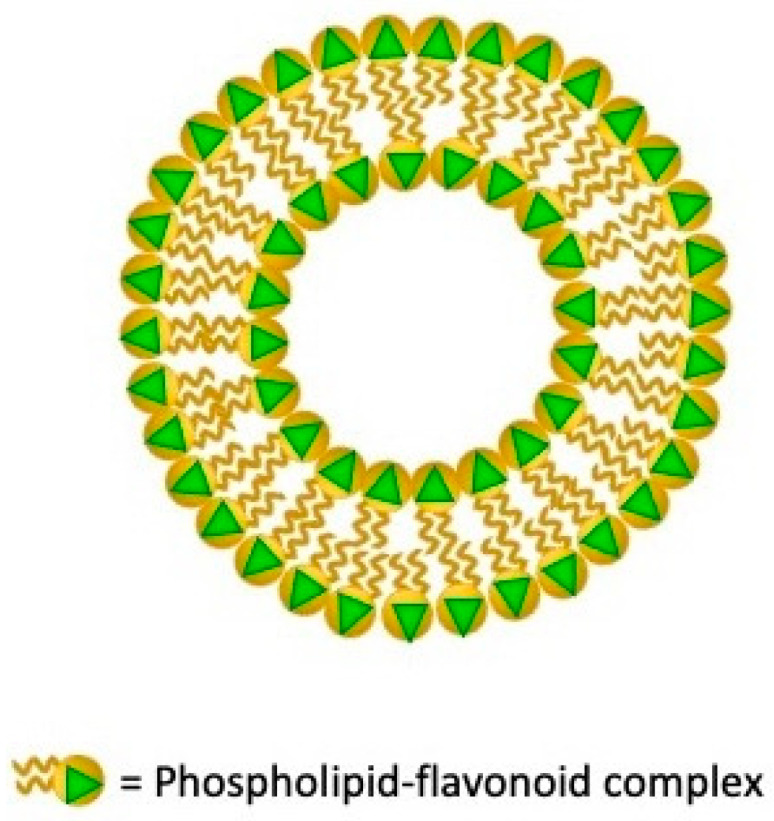
Although for a long time phyto-pharmaceuticals have a prominent position in the therapeutic scene, it should be emphasized how phyto-active constituents as phenolics, flavonoid, and terpenoids demonstrate considerable in-vitro bio-action but are still characterized by low in-vivo effectiveness due to their high molecular weight, low lipid solubility, and bioavailability [188]. Phytosomes nanovesicles originating by Phyto-Phospholipid Complex (PPC), have been developed as a capable strategy to improve natural drugs delivery and bioavailability. PPCs originate by the phospholipids’ polar head and active constituents’ interactions. The two long fatty acid chains do not take part in the formation of the complex, they can interchange encapsulating the polar region of complexes originating a lipophilic side when resuspended in water (Figure 7) [189].
Figure 7.
Schematic structure of phytosomes lipid vesicular system.
Phytosomes have many structural and functional aspects in common with liposomes and tranferosomes such as the capability to improve the solubility of weakly soluble polyphenolic phytochemicals. Otherwise, phytosomes and transferosomes are more stable than liposomes in 4 °C and 25 °C aqueous media up to three months since liposomes should be freeze dried to preserve their stability. Phytosomes, as well as transferosomes, exhibit superior dermal penetration properties leading noticeable accumulation in the epidermis and dermis. Since the phytosomes configuration is grounded on the H-bond interaction between the phospholipid molecules’ polar moiety and the phytoconstituents, the laded compounds permanence is higher than in other lipid nanovesicles [190]. The numerous and very recent drug delivery applications collected in Table 7 show how phytosome nanotechnology will definitely get more efficient the ways of bioactive phytochemicals therapeutic and aesthetic delivery counteracting the bottlenecks of the low absorption and poor penetration rate across biological barriers improving herbal-originated compounds pharmacodynamic and pharmacokinetic and assets [190].
Table 7.
Phytosomes’ drug delivery applications.
| Composition | Cargo | Application | Reference |
|---|---|---|---|
| Phosphatidylcholine | Abutilon indicum and Piper longum | Hepatoprotective effect | [191] |
| Phosphatidylcholine | Annona muricata L. aqueous extract | Treatment of major depressive disorders | [192] |
| Milk phospholipids | Ascorbic acid and α-tocopherol | Antioxidative | [193] |
| Phosphatidylcholine | Berberine | Diabetes treatment | [194] |
| Phosphatidylcholine | Chicoric acid and chlorogenic acid from the Echinacea plant | Antioxidant activity | [195] |
| Egg phospholipid | Chrysin | Diabetes treatment | [196,197] |
| Lecithin | Diosgenin | Lung cancer treatment | [198] |
| Phosphatidylcholine | Diosmin | Vascular protection activity | [199] |
| Phosphatidylcholine and piperine | Domperidone | Anti-emetic effect | [200] |
| Lecithin | Ethanolic extract of leaves of Bombax ceiba | Hepatoprotective effect | [201] |
| Lipoid® S45 | Flavonoids from Citrullus colocynthis, mormodica balsamina l. and mormodica dioica roxb. | Diabetes treatment | [202] |
| Lipoid® S100 and Phosal® 75 SA | Genistein | Hepatocellular carcinoma treatment | [203] |
| Soy Hydrogenated Phosphatidylcholine | Icariin | Treatment of ovarian cancer | [204] |
| Phosphatidylcholine | Momordica charantia extract | Hypoglycemic effect | [205] |
| DPPH and phosphatidylcholine | Persimmon extract | Antioxidative | [206] |
| Phosphatidylcholine | Propolis | Antioxidant activity | [207] |
| DPPC | Rutin | Antioxidant for the prevention of liver inflammation | [208] |
| Lecithin | Silymarin | Antioxidant, hepatoprotective and anticancer activity | [209] |
| Lecithin | Taxifolin rich fraction of Cedrus deodara bark extract | Breast cancer treatment | [210] |
| Soy Hydrogenated Phosphatidylcholine | Thymoquinone | Lung cancer treatment | [211] |
| Phosphatidylcholine | Tripterine | Cancer treatment | [212] |
| Lipoid S100 | Tripterine and selenium | Arthritis treatment | [213] |
| Phosphatidylcholine | Umbelliferone | Photo-protective and antioxidant activity | [214] |
8. Catanionic Vesicles
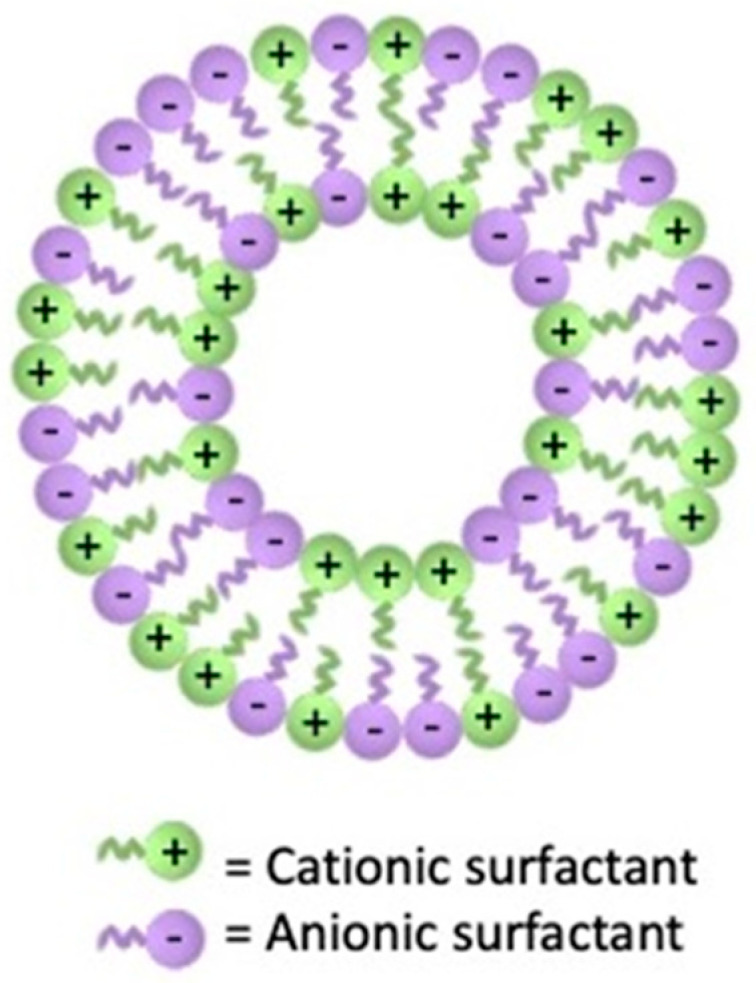
An innovative class of biocompatible and biodegradable drugs lipidic nanovehicle is represented by the catanionic vesicles for their capability to improve the stability and cellular uptake of a wide range of active molecules [215]. These hybrid nanovesicles spontaneously form when unequal amounts of cationic and anionic single-tailed surfactants are dispersed in water [216] (Figure 8).
Figure 8.
Schematic structure of catanionic vesicles.
These nanovesicles are produced by using easily accessible cheap surfactants and, in comparison with phospholipid vesicles, are thermodynamically advantaged in terms of colloidal stability. Alkyl ammonium bromide and gemini surfactants such as bis-quaternary ammonium salts have been used for catanionic vesicles production; however, since they are cytotoxic and not biodegradable, the conjugation with safer molecules is being successfully considered [217]. Their low production costs, higher stability and drug loading capability, together with the fact that they suffer less from ruptures and pressure drops make them excellent drug delivery vehicles for vaccination and anti-microbial, cancer, and inflammatory applications (Table 8). Thus, although catanionic vesicles have a huge applicability in biomedicine, they can suffer safety problems due to their eventual low bio- and emocompatibility. Numerous ongoing researches point to the optimization of their morphology, hydrophobicity, and ionic charge by carefully choosing the proper surfactant and by tuning the anionic/cationic surfactant ratio eventually adding some suited additive [218].
Table 8.
Catanionic vesicles’ drug delivery applications. In the composition column, C is the cationic and A the anionic compound.
| Composition | Cargo | Application | Reference |
|---|---|---|---|
| C: ester functionalized morpholinium and imidazolium-based surface active ionic liquids A: sodium butyrate |
Curcumin | Antimicrobial activity | [219] |
| C: CTAB A: SDS |
Lung cancer treatment | [220] | |
| C: CTAB A: SDS |
Diclofenac sodium | Anti-inflammatory | [221] |
| Serine-based surfactants C: 16Ser A: 8-8Ser |
Doxorubicin | Cancer treatment | [222] |
| C: 4-cholesterocarbonyl-4′-(N,N,N-triethylamine butyloxyl bromide) azobenzene A: SDS |
Antioxidant activity | [223] | |
| C: CTAT A: sodium dodecylbenzenesulfonate |
Francisella tularensis lisate | Tularemia vaccine | [224] |
| C: benzyldimethylhexadecyl ammonium chloride A: sodium 1,4-bis (2-ethylhexyl) sulfosuccinate |
Insulin | Diabetes treatment | [225] |
| C: Azobenzene-based surfactant A: sodium dodecylbenzenesulfonate |
Paclitaxel and Bcl-2 siRNA | Breast cancer treatment | [226] |
| C: hexadecyltrimethyl ammonium copper trichloride A: SDS |
Toluidine blue and Rose Bengal | Antimicrobial Photodynamic Therapy against Escherichia coli | [227,228] |
| C: CTAC A: SDS |
Trans-resveratrol | Antioxidant and radical scavenging activity | [229] |
| C: arginine-based surfactants A: sodium laurate, sodium myristate and 8-SH |
Antimicrobial and antibiofilm activity | [218] | |
| C: cetalkonium chloride A: diclofenac sodium, flurbiprofen sodium or naproxen sodium |
Anti-inflammatory drug release from contact lenses | [230] | |
| C: chlorambucil prodrug A: sodium bis (2-ethylhexyl) sulfosuccinate |
Cancer treatment | [231] | |
| C: Cytarabine hydrochloride A: Sericin protein surfactant |
Cancer treatment | [232] | |
| C: CTAT A: sodium dodecylbenzenesulfonate |
Extraction of cell surface components of Neisseria gonorrhoeae into the leaflet of the vesicles to create artificial pathogens for vaccines | [233] | |
| C: doxorubicin A: gemini surfactant |
Cancer treatment | [234] | |
| C: DTAB A: dioctyl sulfosuccinate sodium salt |
Drug delivery for cystic fibrosis | [235] | |
| C: hexamethylene-1,6-bis (dodecyldimethylammonium) dibromide A: diclofenac sodium |
Antimicrobial activity | [236] | |
| C: methylimidazolium- or pyridinium-based surface active ionic liquids A: sodium N-lauroyl sarcosinate |
Antimicrobial activity | [237] | |
| C: methylimidazolium- or pyridinium-based surface active ionic liquids A: sodium bis(2-ethyl-1-hexyl) sulfosuccinate |
Antimicrobial activity | [238] | |
| C: NαNω-Bis(Nαcaproylarginine) α,ω-propyldiamide A: Lichenysin |
Antimicrobial and antifungal activity | [239] | |
| C: N(π), N(τ)-bis(methyl)-L-Histidine tetradecyl amide A: lysine-based surfactant Nα-lauroyl-Nεacetyl lysine or sodium myristate |
Antimicrobial activity | [240] | |
| C: N-dodecylamino-1-deoxylactitol A: ketoprofen |
Anti-inflammatory activity | [241] |
9. Extracellular Vesicles
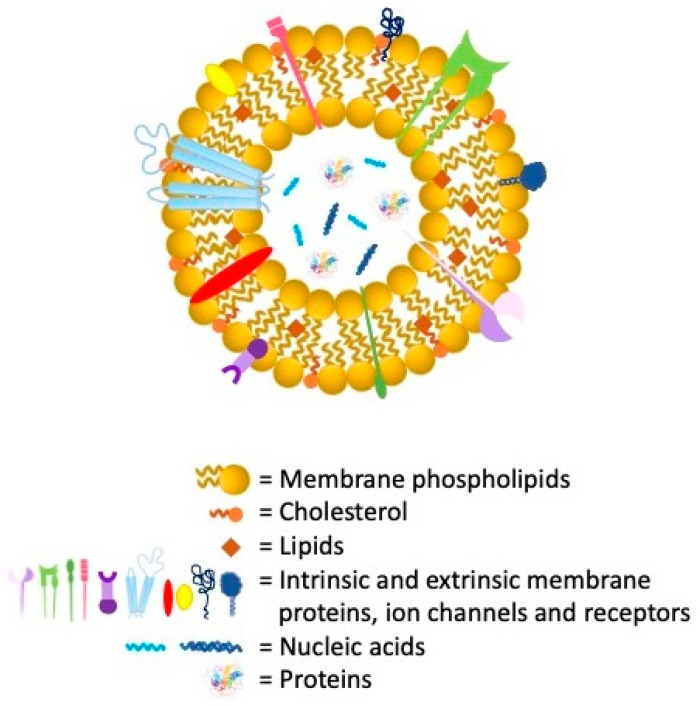
The most heterogeneous and versatile class of lipid vesicles is certainly that of extracellular vesicles (EVs) (Figure 9) including apoptotic bodies, microvesicles, and exosomes. These vesicles are ubiquitarian and can be isolated from cells culture media and from all the major biological fluid as urine, plasma, saliva, amniotic and cerebrospinal fluid, semen, among others [242,243,244,245]. Both apoptotic bodies and microvesicles, with dimensions ranging between 500 nm and 2 µm and from 50 nm to 1 µm, respectively, arise from plasma cell membrane outward blebbing and fragmentation. On the other side, exosomes, deriving from the endocytic pathway, have diameters between 30 to 120 nm [246]. Many authors reported about the EVs use in drug delivery since their surface is characterized by antigens, related to the parental cells, able to direct specific homing or targeting phenomena [247]. Although the EVS, as the main physio-pathological intracellular communication mediators, are already in origin able to transport miRNA, proteins, and other biological molecules, their morpho-functional and biochemical characteristics make them excellent candidates for post isolation nanotechnological modifications. In the last twenty years, numerous studies show the great potential of these vesicles in both the diagnostic and therapeutic fields [248]. Their high biocompatibility, low immunogenicity coupled with a superior loading capability make them proper tools for post isolation drug delivery load and engineering. In addition to a whole series of chemical or biological functionalization, many studies are referring to the possibility of loading them with cellular organelles such as mitochondria, NPs, drugs, and nuclei acids [249,250,251].
Figure 9.
Schematic structure of extracellular vesicles.
Although the intrinsic complexity related to the EVs’ size and natural (batch-to-batch) heterogeneity makes their drug delivery application much more complex than that with merely synthetic production systems, many exogenous EVs’ active molecules loading methods have been successfully proposed for the clinical EVs’ translation [252] (Table 9).
Table 9.
Extracellular vesicles’ drug delivery applications.
| Parental cell | Cargo | Application | Reference |
|---|---|---|---|
| EVs from HEK293T cells | Angiotensin converting enzyme II (ACE2) | Protect from SARS-CoV-2 infection by competitively bound to virus against host cells | [253] |
| Milk-derived exosomes | Anthocyanidins | Anti-proliferative and anti-inflammatory in lung cancer | [254] |
| Exosomes from breast and colorectal cancer cells | Aspirin | Cancer therapy | [255] |
| Exosomes from MIN-6 cells | BAY55-9837 | Increase insulin production for type 2 diabetes mellitus | [256] |
| Exosomes from macrophages | Berberine | Spinal cord injury treatment | [257] |
| EVs from human umbilical cord mesenchymal stem cells | Cannabidiol | Increase the therapeutic efficacy of doxorubicin in triple negative breast cancer | [258] |
| Exosomes from umbilical cord-derived macrophages | Cisplatin | Ovarian cancer cells treatment | [259] |
| EVs from macrophages | Curcumin | Neuroprotection and ischemia-reperfusion injury treatment | [260] |
| Inhibit the phosphorylation of Tau protein | [261] | ||
| Exosomes from mesenchymal stem cells | Attenuate the progression of osteoarthritis | [262] | |
| EVs from HEK293 cells | Myocardial infarction treatment | [263] | |
| Exosomes from bone marrow-derived mesenchymal stem cells | Cerebral ischemia treatment | [264] | |
| Exosomes from HEK293 cells | Curcumin and RAGE-binding peptide | Acute lung injury treatment | [265] |
| EVs from smooth muscle cells | Cystatin C | Protection and healing of the nervous system in different neurotoxic conditions | [266] |
| Exosomes from lung cancer | Docetaxel | Non-small cell lung cancer treatment | [267] |
| Exosomes from cervical cancer | Cervical cancer treatment | [268] | |
| Exosomes from blood samples | Dopamine | Parkinson’s disease treatment | [269] |
| EVs from macrophages | Doxorubicin | Metastatic ovarian cancer treatment | [270] |
| Exosomes from mesenchymal stem cells | Colorectal cancer treatment | [271] | |
| Exosomes from human glioma | Glioma treatment | [272] | |
| Milk-derived exosomes | Cancer treatment | [273] | |
| Exosomes from HEK293 cells | Cancer treatment | [274] | |
| Exosomes from bone marrow-derived mesenchymal stem cells | Osteosarcoma treatment | [275] | |
| Exosomes from colon cancer | Colorectal cancer treatment | [276] | |
| Exosomes from human breast and ovarian cancer | Breast and ovarian cancer treatment | [277] | |
| Exosomes from macrophages | Edaravone | Permanent middle cerebral artery occlusion treatment | [278] |
| Exosomes from human fetal lung fibroblasts | Erastin | Triple-negative breast cancer therapy | [279] |
| Exosomes from pancreatic cells | Gemcitabine | Pancreatic cancer treatment | [280] |
| EVs from human plasma | Imperialine | Non-small cell lung cancer treatment | [281] |
| EVs from human umbilical vascular endothelial cells | Meta-tetra(hydroxyphenyl) chlorine | Cancer photodynamic therapy | [282,283] |
| EVs from fibroblast cells | Methotrexate | Glioblastoma treatment | [284] |
| Exosomes from embryonic stem cells | Paclitaxel | Glioblastoma treatment | [285] |
| Exosomes from mesenchymal stem cells | Carcinoma treatment | [286] | |
| EVs from gingival mesenchymal stromal cells | Cancer treatment | [287,288] | |
| Exosomes from macrophages | Pulmonary metastases treatment | [289] | |
| Milk-derived exosomes | Lung cancer treatment | [290] | |
| EVs from bone marrow mesenchymal stromal cells | Malignant pleural mesothelioma treatment | [291] | |
| Exosomes from macrophages | Multiple drug-resistant cancer treatment | [292] | |
| EVs from lung cancer cells | Paclitaxel and oncolytic virus | Primary and metastatic cancer treatment | [293] |
| EVs from neutrophil-like cells | Piceatannol | Alleviated acute lung inflammation/injury and sepsis induced by lipopolysaccharide | [294] |
| Exosomes from plasma | Quercetin | Relieve symptoms of Alzheimer’s disease by inhibiting phosphorylation of Tau and reducing the formation of insoluble neurofibrillary tangles | [295] |
| Exosomes from human ovarian cancer | Triptolide | Ovarian cancer treatment | [296] |
| Mannosylated exosomes from macrophages | Vancomycin and lysostaphin | Eradication of intracellular quiescent MRSA | [297] |
| Exosomes from fibroblasts | WNT3A | Repair of osteochondral defects | [298] |
Many types of cell-derived exosomes, coming from both plant and human eukaryotic cells, have recently been used to successfully encapsulate inorganic NPs. The cargo can be either loaded by treating parental cells or by post EVs isolation engineering [299]. The potential benefits of a wide range of inorganic NPs-loaded EVs have been proven in various drug delivery applications as extensively listed in Table 10.
Table 10.
Extracellular vesicles’ inorganic NPs delivery applications.
| Parental Cell | Cargo | Application | Reference |
|---|---|---|---|
| Exosomes from human hepatocarcinoma | Doxorubicin-loaded biomimetic porous silicon NPs | Cytotoxicity against bulk cancer cells and cancer stem cells | [300] |
| Grapefruit EVs | Doxorubicin-loaded heparin-based NPs | Glioma treatment | [301] |
| Exosomes from melanoma cells | Gold NPs | Cancer treatment | [302] |
| Exosomes from HEK293T cells | Blood-brain barrier penetration and brain disorders future treatments | [303] | |
| Exosomes from bone marrow mesenchymal stromal cells | Neuroimaging for various brain disorders | [304] | |
| Exosomes from mesenchymal stem cells | [305] | ||
| Exosomes from breast cancer cells | Gold iron oxide hybrid NPs | MRI contrast agent and photodynamic therapy | [306] |
| Exosomes from mesenchymal stem cells | Iron oxide NPs | Myocardial infarction treatment | [307] |
| Wound repair | [308] | ||
| Increase activation and migration ability of macrophage | [309] | ||
| Tumor cell ablation via magnetically induced hyperthermia | [310] | ||
| EVs from human umbilical vascular endothelial cells | Photodynamic and hyperthermia therapy of prostate cancer | [311] | |
| Exosomes from macrophages | Laurate-functionalized Pt(IV) prodrug, human serum albumin, and lecithin NPs | Breast cancer and metastatic breast cancer lung nodules treatment | [312] |
| Exosomes from lung adenocarcinoma cells | Metal-organic framework | Detection of the ATP level in living cancer cells, providing an efficient tool for the cell metabolism study | [313] |
| Exosomes from triple negative breast cancer cells | Delivery of anticancer compounds | [314] | |
| Exosomes from HeLa cells | [315] | ||
| Exosomes from lung cancer or glioma | Palladium nanosheet | Deliver catalytic cargo directly to cancer cells | [316] |
| Exosomes from triple negative breast cancer cells | PLGA NPs | Cancer therapy | [317] |
| Exosomes from lung carcinoma cells | [318] | ||
| EVs from Staphylococcus aureus | Intracellular delivery of antibiotics for intracellular pathogen-associated complications treatment | [319] | |
| Exosomes from breast cancer | Quantum dots of vanadium carbide | Cancer photothermal therapy | [320] |
| Exosomes from hepatocellular carcinoma | Silver and iron NCs | Cancer bioimaging | [321] |
| Exosomes from macrophages | SPIONs and curcumin | Synergistic antitumor therapy in gliomas | [322] |
| Exosomes from plasma | Superparamagnetic magnetite colloidal nanocrystal clusters | Cancer treatment | [323] |
| EVs from KB cells | Zinc oxide NCs | Cancer treatment | [324] |
Since EVs are remarkably involved in genetic information transfer in normal and pathological states [325,326,327], it is not difficult to see their potential as engineered nucleic acids carriers for drug the treatment of ischemic stroke, myocardial infarction [328], traumatic brain injuries [329], and liver fibrosis [330].
The intrinsic properties of EVs such as low immunogenicity and safety make them a suitable candidate for gene cancer therapy with promising advantages with respect to the conventional chemotherapeutic treatments. EVs transfer their RNA or DNA cargo to the target cells with the aim to alter the tumoral genes information and act, e.g., as tumoral suppressors. In addition, the therapeutic properties of EVs-nucleic acids loaded can be further improved by tailoring their surface [331] in order to maximize specificity and successful delivery. In Massaro et al. [332] is reported a list of the ligands used for cancer therapy. Interestingly, attempts to conjugate RNAs to molecules such as cholesterol for EVs surface functionalization were reported [333,334], with the aim to improve loading control and delivery. Therapeutics effects of Plasmid DNA, mRNA, miRNA, and shRNA delivery EV-mediated were reported in Table 11 underlining how gene therapy combined with EVs delivery is a rapidly growing field for safe and effective precision medicine treatments.
Table 11.
Extracellular vesicles’ nucleic acids delivery applications.
| Parental Cell | Cargo | Application | Reference |
|---|---|---|---|
| Microvesicles from breast cancer cells | Minicircle DNA encoding a thymidine kinase /nitroreductase fusion protein | Breast cancer therapy | [335] |
| EVs from mice melanoma cells | Plasmid DNA coding for ESAT-6 | Promote antitumor activity of dendritic cells | [336] |
| EVs from human brain endothelial cells and macrophages | Plasmid DNA encoding for brain-derived neurotrophic factor | Protection of the brain endothelium increasing endothelial ATP levels | [337] |
| EVs from macrophage cells | Tripeptidyl peptidase-1-encoding plasmid DNA | Lysosomal storage disorder, Neuronal Ceroid Lipofuscinoses 2 (CLN2) or Batten disease treatment | [338] |
| EVs from red blood cells | Anti-miR-125b ASOs and Cas9 mRNA | Cancer treatment | [339] |
| Exosomes from mouse neuronal cells | miR-21-5p | Suppression of autophagy after a traumatic brain injury | [340] |
| EVs from frozen human plasma | miR-31 and miR-451a | Promoted apoptosis of hepatocellular carcinoma | [341] |
| Exosomes from human bone marrow mesenchymal stem cells | miR-101-3p | Oral cancer treatment | [342] |
| Exosomes from bone marrow mesenchymal stem cells | miR-124 | Promote neurogenesis after ischemia | [343] |
| EVs from human adipose tissue-derived mesenchymal stromal/ medicinal signaling cells | miR-125b | Inhibits hepatocellular carcinoma proliferation | [344] |
| Exosomes from normal intestinal epithelial FHC cells | miR-128-3p | Increase chemosensitivity of oxaliplatin-resistant colorectal cancer | [345] |
| Exosomes from HKT293T cells | Curcumin, saponin, MiR-143 | Engineered exosomes for anti-HIV agents delivery to solid tissues | [346] |
| Exosomes from human umbilical cord mesenchymal stem cells | miR-145-5p | Inhibit adenocarcinoma progression | [347] |
| EVs from bone-marrow mesenchymal stem cells | miR-146a | Ulcerative colitis treatment | [348] |
| EVs from human mesenchymal stromal cells | miR-146a-5p | Prevent group 2 innate lymphoid cells -dominant allergic airway inflammation | [349] |
| Exosomes from human umbilical cord mesenchymal stem cells | miR-148b-3p | Suppress breast cancer progression | [350] |
| Exosomes from mesenchymal stem cells | miR-199a | Inhibit the growth of glioma by down-regulating AGAP2 | [351] |
| Exosomes from endothelial progenitor cells | miR-210 | Protect endothelial cells against hypoxia/ reoxygenation injury improving mitochondrial function | [352] |
| EVs from mesenchymal stem cells | miR-210 |
Promote angiogenesis in myocardial infarction | [353] |
| EVs from bone mesenchymal stem cells | miR-216a-5p | Promote the proliferation of chondrocytes in osteoarthritis | [354] |
| EVs from human umbilical cord mesenchymal stem cells | miR-302a | Therapy of endometrial cancer | [355] |
| EVs from mesenchymal stem cells | miR-379 | Therapy for metastatic breast cancer | [245] |
| EVs from adipose tissue-mesenchymal stromal cells | miR-424-5p | Therapy for triple negative breast cancer | [356] |
| Exosomes from HEK-293T cells | miR-497 | Inhibit lung cancer growth and angiogenesis | [357] |
| Exosomes from CRC cells | miR-567 | Reverse chemoresistance to Trastuzumab in breast cancer | [358] |
| EVs from HEK-293T cells | miR-1252-5p | Downregulation of heparanase to enhance the chemosensitivity to Bortezomib in multiple myeloma | [359] |
| EVs from HEK-293T cells | miRNA-21 | Myocardial infarction treatment | [360] |
| Exosomes from breast cancer | miRNA-126 | Inhibit the formation of lung cancer metastasis | [361] |
| EVs from glioblastoma stem-like cells | miRNA-139 | Downregulation of glioblastoma | [362] |
| Exosomes from mesenchymal stem cells | miRNA-584-5p | Gliomas treatment | [363] |
| Exosomes 293F cells | mRNA | SARS-CoV-2 vaccine | [364] |
| Exosomes from HEK-293T cells | Catalase mRNA | Attenuated neurotoxicity and neuroinflammation in Parkinson’s disease | [365] |
| EVs from HEK-293T cells | Cytosine deaminase fused to uracil phosphoribosyltransferase mRNA | Glioblastoma treatment | [366] |
| EVs from HEK-293T cells | HChrR6 mRNA | Convert CNOB into MCHB for the treatment of cancers | [367] |
| Exosomes from mesenchymal stem cells, dendritic cells or HEK-293T cells | PTEN mRNA | Restore tumor-suppressor function in PTEN deficient gliomas | [368] |
| EVs from non-pigmented ciliary epithelium cells | anti-fibrotic (SMAD7) siRNA | Lower intraocular pressure in primary open-angle glaucoma | [369] |
| Exosomes from autologous breast cancer cells | Cationic bovine serum albumin conjugated siS100A4 | Suppress postoperative breast cancer metastasis | [370] |
| EVs from murine neuroblastoma cell line and dendritic cells | Cholesterol-conjugated siRNAs | Human antigen R silencing for cancer treatment | [334] |
| Exosomes from HEK-293T cells | c-Met siRNA | Reverse chemoresistance to cisplatin in gastric cancer | [371] |
| Exosomes from HEK-293T cells | Hepatocyte growth factor (HGF) siRNA | Inhibitory effect on tumor growth and angiogenesis in gastric cancer | [372] |
| EVs from mesenchymal stem cells derived from umbilical cord Wharton’s jelly | Hydrophobically modified asymmetric siRNAs conjugated with cholesterol | Huntingtin silencing in neurons | [333] |
| Exosomes from glioblastoma cells | [373] | ||
| Exosomes from human neuroblastoma cells | Heat shock protein-27 (HSP27) siRNA | Decrease of cell differentiation toward mature neuron in neuroblastoma | [374] |
| Exosomes from urine-derived induced pluripotent stem cells | ICAM-1 siRNA | Alleviating inflammation of pulmonary microvascular endothelial cells | [375] |
| Exosomes from HEK-293T cells | KRAS siRNA | Inhibition of tumor growth | [376] |
| EVs from astrocytes | LincRNA-Cox2 siRNA | Lipopolysaccharideinduced microglial proliferation for treatment of CNS disorders | [377] |
| Exosomes from mesenchymal stem cells | PTEN siRNA | Promote recovery for spinal cord injury individuals | [378] |
| EVs from red blood cells | P65 and Snai1 siRNA | Inhibit renal inflammation and fibrosis for acute kidney injury treatment | [379] |
| EVs from HEK-293T cells | RAGE siRNA | Attenuated inflammation in myocarditis | [380] |
| Exosomes from bone-marrow-derived mesenchymal stem cells | siGRP78 | Suppress Sorafenib resistance in hepatocellular carcinoma | [381] |
| Exosomes from bovine milk | siKRAS | Lung tumor treatment | [382] |
| EVs from different cell lines | siRNA | Reducing the therapeutic dose of siRNA for different pathologies | [383] |
| EVs from human umbilical cord mesenchymal stem cells | siRNA-ELFN1-AS1 | Inhibit colon adenocarcinoma cells proliferation | [384] |
| Exosomes from normal human foreskin fibroblast | siRNA or short hairpin RNA specific to oncogenic KrasG12D | Pancreatic ductal adenocarcinoma treatment | [385] |
| Exosomes from HEK-293T cells | Transient receptor potential polycystic 2 (TRPP2) siRNA | Reduce the epithelial-mesenchymal transition in pharyngeal squamous carcinoma | [386] |
| Exosomes from brain endothelial bEND.3 cells | Vascular endothelial growth factor (VEGF) siRNA | Knockdown of VEGF in brain cancer cells | [387] |
| Exosomes from HEK-293T cells | Different viral products including Ebola Virus VP24, VP40 and NP, Influenza Virus NP, Crimean–Congo Hemorrhagic Fever NP, West Nile Virus NS3, and Hepatitis C Virus NS3 | Exosomes-based vaccines | [388] |
10. Conclusions
It is well known that liposomes, assumed to be the oldest category of lipidic nanovesicles, have been broadly considered as the major candidates for biomedical and drug delivery applications. Despite their high biocompatibility and the ability to effectively carry both hydrophilic and/or hydrophobic active molecules to the target site, they still suffer some unresolved weaknesses such as brief shelf-life, low colloidal stability, and limited and expensive preparation methods [389]. The development of new drug delivery approaches has significantly boosted the design and the production of the just reviewed non-liposomal lipid nanovesicles. This new cohort of lipid vesicles can complement liposomes as alternative nanovesicular drug delivery systems and although recently implemented, they have all the chances to overspread as successful engineered nanomaterials.
Considering the existent non-liposomal LNV, those collected in this review, given their countless listed applications, have undoubtedly proved to be the most successful ones by reaching clinical use. Surely among the different types of LNV described in this review, those of cellular origin, the extracellular vesicles, are those that could also give future results closer to the needs of personalized medicine therapeutic plans. The possibility of isolating them from the same patient who is going to be treated reduces the likelihood of rejection phenomena both by increasing the compliance of the therapy and by reducing any adverse effects. Therefore, it would be foreseen that very soon, the LNV carrier’s production will scale-up from the lab scale to the industrial one issuing high-quality competitive outcomes.
In this regard, we would like to conclude with an update on the recent and promising use of lipid nanovesicles for the nucleic acids based-vaccine development. This application has been mainly oriented to the oncologic field, but recently, under the pressure of the latest terrible health emergency that has afflicted the entire globe, anti-viral applications have been reported. EV-based vaccines to deliver mRNA coding for specific molecules such as proteins or by the exposure of specific features on EVs surface have been designed. Since 2020, the SARS-CoV-2 pandemic has boosted additional efforts for the successful design of forceful vaccines [332,390]. Leading approved vaccines provide immunization by the viral Spike (S) protein, injected as purified proteins or codified by the administered mRNAs sequences and showing that “mRNA-based vaccines can fill the gap between emerging pandemic infectious disease and a bountiful supply of effective vaccines” [391]. The mRNA-based vaccine BNT162b2 was developed by Pfizer/BioNTech while the mRNA-1273 SARS-CoV-2 vaccine was developed by Moderna [392]. In Tsai et al. [364] was reported another approach for SARS-CoV-2 vaccines: exosomes are used to deliver mRNAs sequences with the aim to express not only the spike protein but also another artificial protein named “LSNME” and containing the viral spike, nucleocapsid, membrane, and envelope proteins. This approach has been tested on mice with promising results and, along with the many other applications reported in this review, confirmed the growing potential of lipid nanovesicles-mediated delivery as an effective tool for the translation of nanotechnology, bioengineering, and nanomaterials studies from research to clinic.
Author Contributions
Conceptualization, T.L. and F.S.; resources, T.L., F.S.; writing—original draft preparation, T.L. and F.S; writing—review and editing, M.M., B.T., M.A., R.P. and E.d.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Data presented in this manuscript is available from corresponding author upon reseanable requests.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mullard A. 2020 fda drug approvals. Nat. Rev. Drug Discov. 2021;20:85–90. doi: 10.1038/d41573-021-00002-0. [DOI] [PubMed] [Google Scholar]
- 2.Deng Y., Zhang X., Shen H., He Q., Wu Z., Liao W., Yuan M. Application of the nano-drug delivery system in treatment of cardiovascular diseases. Front. Bioeng. Biotechnol. 2020;7:489. doi: 10.3389/fbioe.2019.00489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edis Z., Wang J., Waqas M.K., Ijaz M., Ijaz M. Nanocarriers-mediated drug delivery systems for anticancer agents: An overview and perspectives. Int. J. Nanomed. 2021;16:1313–1330. doi: 10.2147/IJN.S289443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilczewska A.Z., Niemirowicz K., Markiewicz K.H., Car H. Nanoparticles as drug delivery systems. Pharmacol. Rep. 2012;64:1020–1037. doi: 10.1016/S1734-1140(12)70901-5. [DOI] [PubMed] [Google Scholar]
- 5.Ruzycka-Ayoush M., Kowalik P., Kowalczyk A., Bujak P., Nowicka A.M., Wojewodzka M., Kruszewski M., Grudzinski I.P. Quantum dots as targeted doxorubicin drug delivery nanosystems in human lung cancer cells. Cancer Nanotechnol. 2021;12:8. doi: 10.1186/s12645-021-00077-9. [DOI] [Google Scholar]
- 6.Shehata T.M., Ibrahim M.M., Elsewedy H.S. Curcumin niosomes prepared from proniosomal gels: In vitro skin permeability, kinetic and in vivo studies. Polymers. 2021;13:791. doi: 10.3390/polym13050791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ge X., Wei M., He S., Yuan W.E. Advances of non-ionic surfactant vesicles (niosomes) and their application in drug delivery. Pharmaceutics. 2019;11:55. doi: 10.3390/pharmaceutics11020055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vashist S., Kaushik J., Sunil B.K. A review article: Proniosomes. PharmaTutor. 2015;3:25–30. [Google Scholar]
- 9.Khatoon M., Shah K.U., Din F.U., Shah S.U., Rehman A.U., Dilawar N., Khan A.N. Proniosomes derived niosomes: Recent advancements in drug delivery and targeting. Drug Deliv. 2017;24:56–69. doi: 10.1080/10717544.2017.1384520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li D., Wu Z., Martini N., Wen J. Advanced carrier systems in cosmetics and cosmeceuticals: A review. J. Cosmet. Sci. 2011;62:549–563. [PubMed] [Google Scholar]
- 11.Handjani-Vila R.M., Ribier A., Rondot B., Vanlerberghie G. Dispersions of lamellar phases of non-ionic lipids in cosmetic products. Int. J. Cosmet. Sci. 1979;1:303–314. doi: 10.1111/j.1467-2494.1979.tb00224.x. [DOI] [PubMed] [Google Scholar]
- 12.Sammour R.M.F., Taher M., Chatterjee B., Shahiwala A., Mahmood S. Optimization of aceclofenac proniosomes by using different carriers, part 1: Development and characterization. Pharmaceutics. 2019;11:350. doi: 10.3390/pharmaceutics11070350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shehata T.M., Abdallah M.H., Ibrahim M.M. Proniosomal oral tablets for controlled delivery and enhanced pharmacokinetic properties of acemetacin. AAPS PharmSciTech. 2015;16:375–383. doi: 10.1208/s12249-014-0233-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ramkanth S., Chetty C.M., Sudhakar Y., Thiruvengadarajan V.S., Anitha P., Gopinath C. Development, characterization & invivo evaluation of proniosomal based transdermal delivery system of atenolol. Future J. Pharm. Sci. 2018;4:80–87. [Google Scholar]
- 15.Eltellawy Y.A., El-Kayal M., Abdel-Rahman R.F., Salah S., Shaker D.S. Optimization of transdermal atorvastatin calcium—loaded proniosomes: Restoring lipid profile and alleviating hepatotoxicity in poloxamer 407-induced hyperlipidemia. Int. J. Pharm. 2021;593:120163. doi: 10.1016/j.ijpharm.2020.120163. [DOI] [PubMed] [Google Scholar]
- 16.Mehta M., Dureja H., Garg M. Development and optimization of boswellic acid-loaded proniosomal gel. Drug Deliv. 2016;23:3072–3081. doi: 10.3109/10717544.2016.1149744. [DOI] [PubMed] [Google Scholar]
- 17.Aboumanei M.H., Mahmoud A.F. Design and development of a proniosomal transdermal drug delivery system of caffeine for management of migraine: In vitro characterization, 131i-radiolabeling and in vivo biodistribution studies. Process. Biochem. 2020;97:201–212. doi: 10.1016/j.procbio.2020.07.018. [DOI] [Google Scholar]
- 18.Nemr A.A., El-Mahrouk G.M., Badie H.A. Development and evaluation of proniosomes to enhance the transdermal delivery of cilostazole and to ensure the safety of its application. Drug Dev. Ind. Pharm. 2021;47:403–415. doi: 10.1080/03639045.2021.1890111. [DOI] [PubMed] [Google Scholar]
- 19.Tareen F.K., Shah K.U., Ahmad N., Asim.ur.Rehman, Shah S.U., Ullah N. Proniosomes as a carrier system for transdermal delivery of clozapine. Drug Dev. Ind. Pharm. 2020;46:946–954. doi: 10.1080/03639045.2020.1764020. [DOI] [PubMed] [Google Scholar]
- 20.Aboali F.A., Habib D.A., Elbedaiwy H.M., Farid R.M. Curcumin-loaded proniosomal gel as a biofreindly alternative for treatment of ocular inflammation: In-vitro and in-vivo assessment. Int. J. Pharm. 2020;589:119835. doi: 10.1016/j.ijpharm.2020.119835. [DOI] [PubMed] [Google Scholar]
- 21.Liu H., Tu L., Zhou Y., Dang Z., Wang L., Du J., Feng J., Hu K. Improved bioavailability and antitumor effect of docetaxel by tpgs modified proniosomes: In vitro and in vivo evaluations. Sci. Rep. 2017;7:43372. doi: 10.1038/srep43372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mokale V.J., Patil H.I., Patil A.P., Shirude P.R., Naik J.B. Formulation and optimisation of famotidine proniosomes: An in vitro and ex vivo study. J. Exp. Nanosci. 2016;11:97–110. doi: 10.1080/17458080.2015.1030711. [DOI] [Google Scholar]
- 23.Verma P., Prajapati S.K., Yadav R., Senyschyn D., Shea P.R., Trevaskis N.L. Single intravenous dose of novel flurbiprofen-loaded proniosome formulations provides prolonged systemic exposure and anti-inflammatory effect. Mol. Pharm. 2016;13:3688–3699. doi: 10.1021/acs.molpharmaceut.6b00504. [DOI] [PubMed] [Google Scholar]
- 24.Kumar S., Jain P., Pandey N., Saxena G. Comparative study of proniosomal drug delivery system of flurbiprofen. J. Chem. Pharm. Res. 2016;8:222–228. [Google Scholar]
- 25.Wagh V.D., Deshmukh O.J. Itraconazole niosomes drug delivery system and its antimycotic activity against candida albicans. ISRN Pharm. 2012;2012:653465. doi: 10.5402/2012/653465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Soliman S.M., Abdelmalak N.S., El-Gazayerly O.N., Abdelaziz N. Novel non-ionic surfactant proniosomes for transdermal delivery of lacidipine: Optimization using 2(3) factorial design and in vivo evaluation in rabbits. Drug Deliv. 2016;23:1608–1622. doi: 10.3109/10717544.2015.1132797. [DOI] [PubMed] [Google Scholar]
- 27.Khudair N., Agouni A., Elrayess M.A., Najlah M., Younes H.M., Elhissi A. Letrozole-loaded nonionic surfactant vesicles prepared via a slurry-based proniosome technology: Formulation development and characterization. J. Drug Deliv. Sci. Technol. 2020;58:101721. doi: 10.1016/j.jddst.2020.101721. [DOI] [Google Scholar]
- 28.Gadela R., Sai G., Sunayana N., Soujanya G., Charan K. Formulation and evaluation of lignocaine hydrochloride proniosomes loaded orabase for dental anaesthesia. J. Drug Deliv. Ther. 2021;11:27–34. [Google Scholar]
- 29.Khalil R.M., Abdelbary G.A., Basha M., Awad G.E., El-Hashemy H.A. Design and evaluation of proniosomes as a carrier for ocular delivery of lomefloxacin hcl. J. Liposome Res. 2017;27:118–129. doi: 10.3109/08982104.2016.1167737. [DOI] [PubMed] [Google Scholar]
- 30.Madan J.R., Ghuge N.P., Dua K. Formulation and evaluation of proniosomes containing lornoxicam. Drug Deliv. Transl. Res. 2016;6:511–518. doi: 10.1007/s13346-016-0296-9. [DOI] [PubMed] [Google Scholar]
- 31.Shah H., Nair A.B., Shah J., Bharadia P., Al-Dhubiab B.E. Proniosomal gel for transdermal delivery of lornoxicam: Optimization using factorial design and in vivo evaluation in rats. Daru. 2019;27:59–70. doi: 10.1007/s40199-019-00242-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shah H., Nair A.B., Shah J., Jacob S., Bharadia P., Haroun M. Proniosomal vesicles as an effective strategy to optimize naproxen transdermal delivery. J. Drug Deliv. Sci. Technol. 2021;63:102479. doi: 10.1016/j.jddst.2021.102479. [DOI] [Google Scholar]
- 33.Abdelbary G.A., Aburahma M.H. Oro-dental mucoadhesive proniosomal gel formulation loaded with lornoxicam for management of dental pain. J. Liposome Res. 2015;25:107–121. doi: 10.3109/08982104.2014.941861. [DOI] [PubMed] [Google Scholar]
- 34.Madni A., Rahim M.A., Mahmood M.A., Jabar A., Rehman M., Shah H., Khan A., Tahir N., Shah A. Enhancement of dissolution and skin permeability of pentazocine by proniosomes and niosomal gel. AAPS PharmSciTech. 2018;19:1544–1553. doi: 10.1208/s12249-018-0967-6. [DOI] [PubMed] [Google Scholar]
- 35.Shruthi P.A., Pushpadass H.A., Franklin M.E.E., Battula S.N., Laxmana Naik N. Resveratrol-loaded proniosomes: Formulation, characterization and fortification. LWT. 2020;134:110127. doi: 10.1016/j.lwt.2020.110127. [DOI] [Google Scholar]
- 36.Sambhakar S., Paliwal S., Sharma S., Singh B. Formulation of risperidone loaded proniosomes for effective transdermal delivery: An in-vitro and in-vivo study. Bull. Fac. Pharm. Cairo Univ. 2017;55:239–247. doi: 10.1016/j.bfopcu.2017.09.003. [DOI] [Google Scholar]
- 37.Shah J., Nair A.B., Shah H., Jacob S., Shehata T.M., Morsy M.A. Enhancement in antinociceptive and anti-inflammatory effects of tramadol by transdermal proniosome gel. Asian J. Pharm. Sci. 2020;15:786–796. doi: 10.1016/j.ajps.2019.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gamal A., Saeed H., Sayed O.M., Kharshoum R.M., Salem H.F. Proniosomal microcarriers: Impact of constituents on the physicochemical properties of proniosomes as a new approach to enhance inhalation efficiency of dry powder inhalers. AAPS PharmSciTech. 2020;21:156. doi: 10.1208/s12249-020-01705-0. [DOI] [PubMed] [Google Scholar]
- 39.Mohsen A.M., Salama A., Kassem A.A. Development of acetazolamide loaded bilosomes for improved ocular delivery: Preparation, characterization and in vivo evaluation. J. Drug Deliv. Sci. Technol. 2020;59:101910. doi: 10.1016/j.jddst.2020.101910. [DOI] [Google Scholar]
- 40.Abdelmonem R., Elhabal S.F., Abdelmalak N.S., El-Nabarawi M.A., Teaima M.H. Formulation and characterization of acetazolamide/carvedilol niosomal gel for glaucoma treatment: In vitro, and in vivo study. Pharmaceutics. 2021;13:221. doi: 10.3390/pharmaceutics13020221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jacob S., Nair A.B., Al-Dhubiab B.E. Preparation and evaluation of niosome gel containing acyclovir for enhanced dermal deposition. J. Liposome Res. 2017;27:283–292. doi: 10.1080/08982104.2016.1224897. [DOI] [PubMed] [Google Scholar]
- 42.Monavari S.H., Mirzaei Parsa M.J., Bolouri B., Ebrahimi S.A., Ataei-Pirkooh A. The inhibitory effect of acyclovir loaded nano-niosomes against herpes simplex virus type-1 in cell culture. Med. J. Islam Repub. Iran. 2014;28:99. [PMC free article] [PubMed] [Google Scholar]
- 43.Allam A., Elsabahy M., El Badry M., Eleraky N.E. Betaxolol-loaded niosomes integrated within ph-sensitive in situ forming gel for management of glaucoma. Int. J. Pharm. 2021;598:120380. doi: 10.1016/j.ijpharm.2021.120380. [DOI] [PubMed] [Google Scholar]
- 44.Barani M., Mirzaei M., Torkzadeh-Mahani M., Adeli-sardou M. Evaluation of carum-loaded niosomes on breast cancer cells:Physicochemical properties, in vitro cytotoxicity, flow cytometric, DNA fragmentation and cell migration assay. Sci. Rep. 2019;9:7139. doi: 10.1038/s41598-019-43755-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Taymouri S., Varshosaz J. Effect of different types of surfactants on the physical properties and stability of carvedilol nano-niosomes. Adv. Biomed. Res. 2016;5:48. doi: 10.4103/2277-9175.178781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Arzani G., Haeri A., Daeihamed M., Bakhtiari-Kaboutaraki H., Dadashzadeh S. Niosomal carriers enhance oral bioavailability of carvedilol: Effects of bile salt-enriched vesicles and carrier surface charge. Int. J. Nanomed. 2015;10:4797–4813. doi: 10.2147/IJN.S84703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ghafelehbashi R., Akbarzadeh I., Tavakkoli Yaraki M., Lajevardi A., Fatemizadeh M., Heidarpoor Saremi L. Preparation, physicochemical properties, in vitro evaluation and release behavior of cephalexin-loaded niosomes. Int. J. Pharm. 2019;569:118580. doi: 10.1016/j.ijpharm.2019.118580. [DOI] [PubMed] [Google Scholar]
- 48.Kashef M.T., Saleh N.M., Assar N.H., Ramadan M.A. The antimicrobial activity of ciprofloxacin-loaded niosomes against ciprofloxacin-resistant and biofilm-forming staphylococcus aureus. Infect. Drug Resist. 2020;13:1619–1629. doi: 10.2147/IDR.S249628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mirzaie A., Peirovi N., Akbarzadeh I., Moghtaderi M., Heidari F., Yeganeh F.E., Noorbazargan H., Mirzazadeh S., Bakhtiari R. Preparation and optimization of ciprofloxacin encapsulated niosomes: A new approach for enhanced antibacterial activity, biofilm inhibition and reduced antibiotic resistance in ciprofloxacin-resistant methicillin-resistance staphylococcus aureus. Bioorganic Chem. 2020;103:104231. doi: 10.1016/j.bioorg.2020.104231. [DOI] [PubMed] [Google Scholar]
- 50.Akbari J., Saeedi M., Enayatifard R., Morteza-Semnani K., Hassan Hashemi S.M., Babaei A., Rahimnia S.M., Rostamkalaei S.S., Nokhodchi A. Curcumin niosomes (curcusomes) as an alternative to conventional vehicles: A potential for efficient dermal delivery. J. Drug Deliv. Sci. Technol. 2020;60:102035. doi: 10.1016/j.jddst.2020.102035. [DOI] [Google Scholar]
- 51.Liu F.R., Jin H., Wang Y., Chen C., Li M., Mao S.J., Wang Q., Li H. Anti-cd123 antibody-modified niosomes for targeted delivery of daunorubicin against acute myeloid leukemia. Drug Deliv. 2017;24:882–890. doi: 10.1080/10717544.2017.1333170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hajizadeh M.R., Maleki H., Barani M., Fahmidehkar M.A., Mahmoodi M., Torkzadeh-Mahani M. In vitro cytotoxicity assay of d-limonene niosomes: An efficient nano-carrier for enhancing solubility of plant-extracted agents. Res. Pharm. Sci. 2019;14:448–458. doi: 10.4103/1735-5362.268206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Tavano L., Vivacqua M., Carito V., Muzzalupo R., Caroleo M.C., Nicoletta F. Doxorubicin loaded magneto-niosomes for targeted drug delivery. Colloids Surf. B Biointerfaces. 2013;102:803–807. doi: 10.1016/j.colsurfb.2012.09.019. [DOI] [PubMed] [Google Scholar]
- 54.Tavano L., Muzzalupo R., Mauro L., Pellegrino M., Andò S., Picci N. Transferrin-conjugated pluronic niosomes as a new drug delivery system for anticancer therapy. Langmuir. 2013;29:12638–12646. doi: 10.1021/la4021383. [DOI] [PubMed] [Google Scholar]
- 55.Barani M., Mirzaei M., Torkzadeh-Mahani M., Lohrasbi-Nejad A., Nematollahi M.H. A new formulation of hydrophobin-coated niosome as a drug carrier to cancer cells. Mater. Sci. Eng. C. 2020;113:110975. doi: 10.1016/j.msec.2020.110975. [DOI] [PubMed] [Google Scholar]
- 56.Pawar S., Shevalkar G., Vavia P. Glucosamine-anchored doxorubicin-loaded targeted nano-niosomes: Pharmacokinetic, toxicity and pharmacodynamic evaluation. J. Drug Target. 2016;24:730–743. doi: 10.3109/1061186X.2016.1154560. [DOI] [PubMed] [Google Scholar]
- 57.Akbarzadeh I., Tavakkoli Yaraki M., Bourbour M., Noorbazargan H., Lajevardi A., Sadat Shilsar S.M., Heidari F., Mousavian S.M. Optimized doxycycline-loaded niosomal formulation for treatment of infection-associated prostate cancer: An in-vitro investigation. J. Drug Deliv. Sci. Technol. 2020;57:101715. doi: 10.1016/j.jddst.2020.101715. [DOI] [Google Scholar]
- 58.Gugleva V., Titeva S., Rangelov S., Momekova D. Design and in vitro evaluation of doxycycline hyclate niosomes as a potential ocular delivery system. Int. J. Pharm. 2019;567:118431. doi: 10.1016/j.ijpharm.2019.06.022. [DOI] [PubMed] [Google Scholar]
- 59.Alam M.S., Ahad A., Abidin L., Aqil M., Mir S.R., Mujeeb M. Embelin-loaded oral niosomes ameliorate streptozotocin-induced diabetes in wistar rats. Biomed. Pharm. 2018;97:1514–1520. doi: 10.1016/j.biopha.2017.11.073. [DOI] [PubMed] [Google Scholar]
- 60.Gupta M., Vaidya B., Mishra N., Vyas S.P. Effect of surfactants on the characteristics of fluconazole niosomes for enhanced cutaneous delivery. Artif Cells Blood Substit. Immobil. Biotechnol. 2011;39:376–384. doi: 10.3109/10731199.2011.611476. [DOI] [PubMed] [Google Scholar]
- 61.El-Sayed M.M., Hussein A.K., Sarhan H.A., Mansour H.F. Flurbiprofen-loaded niosomes-in-gel system improves the ocular bioavailability of flurbiprofen in the aqueous humor. Drug Dev. Ind. Pharm. 2017;43:902–910. doi: 10.1080/03639045.2016.1272120. [DOI] [PubMed] [Google Scholar]
- 62.Mohamad Saimi N.I., Salim N., Ahmad N., Abdulmalek E., Abdul Rahman M.B. Aerosolized niosome formulation containing gemcitabine and cisplatin for lung cancer treatment: Optimization, characterization and in vitro evaluation. Pharmaceutics. 2021;13:59. doi: 10.3390/pharmaceutics13010059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khan S., Akhtar M.U., Khan S., Javed F., Khan A.A. Nanoniosome-encapsulated levoflaxicin as an antibacterial agent against brucella. J. Basic Microbiol. 2020;60:281–290. doi: 10.1002/jobm.201900454. [DOI] [PubMed] [Google Scholar]
- 64.Dandagi P., Naik V., Gadad A., Mastiholimath V., Shedbal S., Rangoli S., Kazi T. Formulation and evaluation of linezolid niosomal gel for topical drug delivery. World J. Pharm. Res. 2020;9:674–690. [Google Scholar]
- 65.Demirbolat G.M., Aktas E., Coskun G.P., Erdogan O., Cevik O. New approach to formulate methotrexate-loaded niosomes: In vitro characterization and cellular effectiveness. J. Pharm. Innov. 2021;1:1–16. doi: 10.1007/s12247-021-09539-4. [DOI] [Google Scholar]
- 66.Al-Mahallawi A.M., Fares A.R., Abd-Elsalam W.H. Enhanced permeation of methotrexate via loading into ultra-permeable niosomal vesicles: Fabrication, statistical optimization, ex vivo studies, and in vivo skin deposition and tolerability. AAPS PharmSciTech. 2019;20:171. doi: 10.1208/s12249-019-1380-5. [DOI] [PubMed] [Google Scholar]
- 67.Muzzalupo R., Tavano L., La Mesa C. Alkyl glucopyranoside-based niosomes containing methotrexate for pharmaceutical applications: Evaluation of physico-chemical and biological properties. Int. J. Pharm. 2013;458:224–229. doi: 10.1016/j.ijpharm.2013.09.011. [DOI] [PubMed] [Google Scholar]
- 68.Hasan A.A., Madkor H., Wageh S. Formulation and evaluation of metformin hydrochloride-loaded niosomes as controlled release drug delivery system. Drug Deliv. 2013;20:120–126. doi: 10.3109/10717544.2013.779332. [DOI] [PubMed] [Google Scholar]
- 69.Wongsuwan N., Dwivedi A., Tancharoen S., Nasongkla N. Development of dental implant coating with minocycline-loaded niosome for antibacterial application. J. Drug Deliv. Sci. Technol. 2020;56:101555. doi: 10.1016/j.jddst.2020.101555. [DOI] [Google Scholar]
- 70.Sohrabi S., Haeri A., Mahboubi A., Mortazavi A., Dadashzadeh S. Chitosan gel-embedded moxifloxacin niosomes: An efficient antimicrobial hybrid system for burn infection. Int. J. Biol. Macromol. 2016;85:625–633. doi: 10.1016/j.ijbiomac.2016.01.013. [DOI] [PubMed] [Google Scholar]
- 71.Mehta S.K., Jindal N. Tyloxapol niosomes as prospective drug delivery module for antiretroviral drug nevirapine. AAPS Pharm. Sci. Tech. . 2015;16:67–75. doi: 10.1208/s12249-014-0183-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bragagni M., Mennini N., Furlanetto S., Orlandini S., Ghelardini C., Mura P. Development and characterization of functionalized niosomes for brain targeting of dynorphin-b. Eur. J. Pharm. Biopharm. 2014;87:73–79. doi: 10.1016/j.ejpb.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 73.Naseroleslami M., Niri N.M., Akbarzade I., Sharifi M., Aboutaleb N. Simvastatin-loaded nano-niosomes confer cardioprotection against myocardial ischemia/reperfusion injury. Drug Deliv. Transl. Res. 2021:1–10. doi: 10.1007/s13346-021-01019-z. [DOI] [PubMed] [Google Scholar]
- 74.Zidan A.S., Hosny K.M., Ahmed O.A., Fahmy U.A. Assessment of simvastatin niosomes for pediatric transdermal drug delivery. Drug Deliv. 2016;23:1536–1549. doi: 10.3109/10717544.2014.980896. [DOI] [PubMed] [Google Scholar]
- 75.Salem H.F., Kharshoum R.M., El-Ela F.I.A., Abdellatif K.R.A. Evaluation and optimization of ph-responsive niosomes as a carrier for efficient treatment of breast cancer. Drug Deliv. Transl. Res. 2018;8:633–644. doi: 10.1007/s13346-018-0499-3. [DOI] [PubMed] [Google Scholar]
- 76.Kulkarni P., Rawtani D. Application of box-behnken design in the preparation, optimization, and in vitro evaluation of self-assembly-based tamoxifen- and doxorubicin-loaded and dual drug-loaded niosomes for combinatorial breast cancer treatment. J. Pharm. Sci. 2019;108:2643–2653. doi: 10.1016/j.xphs.2019.03.020. [DOI] [PubMed] [Google Scholar]
- 77.Yadavar-Nikravesh M.-S., Ahmadi S., Milani A., Akbarzadeh I., Khoobi M., Vahabpour R., Bolhassani A., Bakhshandeh H. Construction and characterization of a novel tenofovir-loaded pegylated niosome conjugated with tat peptide for evaluation of its cytotoxicity and anti-hiv effects. Adv. Powder Technol. 2021;32:3161–3173. doi: 10.1016/j.apt.2021.05.047. [DOI] [Google Scholar]
- 78.Ramadan A.A., Eladawy S.A., El-Enin A.S.M.A., Hussein Z.M. Development and investigation of timolol maleate niosomal formulations for the treatment of glaucoma. J. Pharm. Investig. 2020;50:59–70. doi: 10.1007/s40005-019-00427-1. [DOI] [Google Scholar]
- 79.Soni P.S.T. Non-ionic surfactant vesicles (niosomes) based novel ophthalmic formulation of timolol maleate. J. Drug Deliv. Ther. 2017;7:59–61. [Google Scholar]
- 80.Dubey A., Prabhu P. Development and investigation of niosomes of brimonidine tartrate and timolol maleate for the treatment of glaucoma. Int. J. Pharm.Tech. Res. 2014;6:942–950. doi: 10.4103/2230-973X.138340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hedayati Ch M., Abolhassani Targhi A., Shamsi F., Heidari F., Salehi Moghadam Z., Mirzaie A., Behdad R., Moghtaderi M., Akbarzadeh I. Niosome-encapsulated tobramycin reduced antibiotic resistance and enhanced antibacterial activity against multidrug-resistant clinical strains of pseudomonas aeruginosa. J. Biomed. Mater. Res. Part. A. 2021;109:966–980. doi: 10.1002/jbm.a.37086. [DOI] [PubMed] [Google Scholar]
- 82.Allam A., El-Mokhtar M.A., Elsabahy M. Vancomycin-loaded niosomes integrated within ph-sensitive in-situ forming gel for treatment of ocular infections while minimizing drug irritation. J. Pharm. Pharm. 2019;71:1209–1221. doi: 10.1111/jphp.13106. [DOI] [PubMed] [Google Scholar]
- 83.Dwivedi A., Mazumder A., Nasongkla N. In vitro and in vivo biocompatibility of orthopedic bone plate nano-coated with vancomycin loaded niosomes. J. Drug Deliv. Sci. Technol. 2019;52:215–223. doi: 10.1016/j.jddst.2019.04.018. [DOI] [Google Scholar]
- 84.Shinde A.J., Swami K.B., Tamboli F.A., More H.N. Design and development of zolmitriptan niosomal in situ nasal gel for the treatment of migrain. Int. J. Res. Pharm. Sci. 2021;12:1861–1869. doi: 10.26452/ijrps.v12i3.4786. [DOI] [Google Scholar]
- 85.De A., Venkatesh N., Senthil M., Sanapalli B.K.R., Shanmugham R., Karri V. Smart niosomes of temozolomide for enhancement of brain targeting. Nanobiomedicine. 2018;5:1849543518805355. doi: 10.1177/1849543518805355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ag Seleci D., Seleci M., Stahl F., Scheper T. Tumor homing and penetrating peptide-conjugated niosomes as multi-drug carriers for tumor-targeted drug delivery. RSC Adv. 2017;7:33378–33384. doi: 10.1039/C7RA05071B. [DOI] [Google Scholar]
- 87.Rajput S., Puvvada N., Kumar B.N., Sarkar S., Konar S., Bharti R., Dey G., Mazumdar A., Pathak A., Fisher P.B., et al. Overcoming akt induced therapeutic resistance in breast cancer through sirna and thymoquinone encapsulated multilamellar gold niosomes. Mol. Pharm. 2015;12:4214–4225. doi: 10.1021/acs.molpharmaceut.5b00692. [DOI] [PubMed] [Google Scholar]
- 88.Rathee J., Kanwar R., Kaushik D., Salunke D.B., Mehta S.K. Niosomes as efficient drug delivery modules for encapsulation of toll-like receptor 7 agonists and ido-inhibitor. Appl. Surf. Sci. 2020;505:144078. doi: 10.1016/j.apsusc.2019.144078. [DOI] [Google Scholar]
- 89.Attia N., Mashal M., Grijalvo S., Eritja R., Zárate J., Puras G., Pedraz J.L. Stem cell-based gene delivery mediated by cationic niosomes for bone regeneration. Nanomedicine. 2018;14:521–531. doi: 10.1016/j.nano.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 90.García-Manrique P., Serrano-Pertierra E., Lozano-Andrés E., López-Martín S., Matos M., Gutiérrez G., Yáñez-Mó M., Blanco-López M.C. Selected tetraspanins functionalized niosomes as potential standards for exosome immunoassays. Nanomaterials. 2020;10:971. doi: 10.3390/nano10050971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Obeid M.A., Teeravatcharoenchai T., Connell D., Niwasabutra K., Hussain M., Carter K., Ferro V.A. Examination of the effect of niosome preparation methods in encapsulating model antigens on the vesicle characteristics and their ability to induce immune responses. J. Liposome Res. 2021;31:195–202. doi: 10.1080/08982104.2020.1768110. [DOI] [PubMed] [Google Scholar]
- 92.Nematollahi M.H., Torkzadeh-Mahanai M., Pardakhty A., Ebrahimi Meimand H.A., Asadikaram G. Ternary complex of plasmid DNA with nls-mu-mu protein and cationic niosome for biocompatible and efficient gene delivery: A comparative study with protamine and lipofectamine. Artif Cells Nanomed. Biotechnol. 2018;46:1781–1791. doi: 10.1080/21691401.2017.1392316. [DOI] [PubMed] [Google Scholar]
- 93.Mashal M., Attia N., Soto-Sánchez C., Martínez-Navarrete G., Fernández E., Puras G., Pedraz J.L. Non-viral vectors based on cationic niosomes as efficient gene delivery vehicles to central nervous system cells into the brain. Int. J. Pharm. 2018;552:48–55. doi: 10.1016/j.ijpharm.2018.09.038. [DOI] [PubMed] [Google Scholar]
- 94.Pengnam S., Patrojanasophon P., Rojanarata T., Ngawhirunpat T., Yingyongnarongkul B.-E., Radchatawedchakoon W., Opanasopit P. A novel plier-like gemini cationic niosome for nucleic acid delivery. J. Drug Deliv. Sci. Technol. 2019;52:325–333. doi: 10.1016/j.jddst.2019.04.032. [DOI] [Google Scholar]
- 95.Gallego I., Villate-Beitia I., Martínez-Navarrete G., Menéndez M., López-Méndez T., Soto-Sánchez C., Zárate J., Puras G., Fernández E., Pedraz J.L. Non-viral vectors based on cationic niosomes and minicircle DNA technology enhance gene delivery efficiency for biomedical applications in retinal disorders. Nanomedicine. 2019;17:308–318. doi: 10.1016/j.nano.2018.12.018. [DOI] [PubMed] [Google Scholar]
- 96.Pereira M.C., Pianella M., Wei D., Moshnikova A., Marianecci C., Carafa M., Andreev O.A., Reshetnyak Y.K. Ph-sensitive phlip(®) coated niosomes. Mol. Membr. Biol. 2016;33:51–63. doi: 10.1080/09687688.2017.1342969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Pamornpathomkul B., Niyomtham N., Yingyongnarongkul B.E., Prasitpuriprecha C., Rojanarata T., Ngawhirunpat T., Opanasopit P. Cationic niosomes for enhanced skin immunization of plasmid DNA-encoding ovalbumin via hollow microneedles. AAPS PharmSciTech. 2018;19:481–488. doi: 10.1208/s12249-017-0855-5. [DOI] [PubMed] [Google Scholar]
- 98.Puras G., Mashal M., Zárate J., Agirre M., Ojeda E., Grijalvo S., Eritja R., Diaz-Tahoces A., Martínez Navarrete G., Avilés-Trigueros M., et al. A novel cationic niosome formulation for gene delivery to the retina. J. Control. Release. 2014;174:27–36. doi: 10.1016/j.jconrel.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 99.Gogoi H., Mani R., Bhatnagar R. A niosome formulation modulates the th1/th2 bias immune response in mice and also provides protection against anthrax spore challenge. Int. J. Nanomed. 2018;13:7427–7440. doi: 10.2147/IJN.S153150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Yang C., Gao S., Song P., Dagnæs-Hansen F., Jakobsen M., Kjems J. Theranostic niosomes for efficient sirna/microrna delivery and activatable near-infrared fluorescent tracking of stem cells. ACS Appl. Mater. Interfaces. 2018;10:19494–19503. doi: 10.1021/acsami.8b05513. [DOI] [PubMed] [Google Scholar]
- 101.Obeid M.A., Alyamani H., Amawi H., Aljabali A.A.A., Rezigue M., Abdeljaber S.N., Ferro V.A. Sirna delivery to melanoma cells with cationic niosomes. Methods Mol. Biol. 2021;2265:621–634. doi: 10.1007/978-1-0716-1205-7_42. [DOI] [PubMed] [Google Scholar]
- 102.Pengnam S., Plianwong S., Patrojanasophon P., Radchatawedchakoon W., Yingyongnarongkul B.E., Opanasopit P., Charoensuksai P. Synergistic effect of doxorubicin and sirna-mediated silencing of mcl-1 using cationic niosomes against 3d mcf-7 spheroids. Pharmaceutics. 2021;13:550. doi: 10.3390/pharmaceutics13040550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Maurer V., Altin S., Ag Seleci D., Zarinwall A., Temel B., Vogt P.M., Strauß S., Stahl F., Scheper T., Bucan V., et al. In-vitro application of magnetic hybrid niosomes: Targeted sirna-delivery for enhanced breast cancer therapy. Pharmaceutics. 2021;13:394. doi: 10.3390/pharmaceutics13030394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hemati M., Haghiralsadat F., Yazdian F., Jafari F., Moradi A., Malekpour-Dehkordi Z. Development and characterization of a novel cationic pegylated niosome-encapsulated forms of doxorubicin, quercetin and sirna for the treatment of cancer by using combination therapy. Artif. Cells Nanomed. Biotechnol. 2019;47:1295–1311. doi: 10.1080/21691401.2018.1489271. [DOI] [PubMed] [Google Scholar]
- 105.Slavin Y.N., Ivanova K., Tang W.-l., Tzanov T., Li S.-d., Bach H. Targeting intracellular mycobacteria using nanosized niosomes loaded with antibacterial agents. Nanomaterials. 2021;11:1984. doi: 10.3390/nano11081984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Targhi A.A., Moammeri A., Jamshidifar E., Abbaspour K., Sadeghi S., Lamakani L., Akbarzadeh I. Synergistic effect of curcumin-cu and curcumin-ag nanoparticle loaded niosome: Enhanced antibacterial and anti-biofilm activities. Bioorganic Chem. 2021;115:105116. doi: 10.1016/j.bioorg.2021.105116. [DOI] [PubMed] [Google Scholar]
- 107.Barani M., Nematollahi M.H., Zaboli M., Mirzaei M., Torkzadeh-Mahani M., Pardakhty A., Karam G.A. In silico and in vitro study of magnetic niosomes for gene delivery: The effect of ergosterol and cholesterol. Mater. Sci. Eng. C Mater. Biol. Appl. 2019;94:234–246. doi: 10.1016/j.msec.2018.09.026. [DOI] [PubMed] [Google Scholar]
- 108.Touitou E., Dayan N., Bergelson L., Godin B., Eliaz M. Ethosomes—Novel vesicular carriers for enhanced delivery: Characterization and skin penetration properties. J. Control. Release. 2000;65:403–418. doi: 10.1016/S0168-3659(99)00222-9. [DOI] [PubMed] [Google Scholar]
- 109.Lu J., Guo T., Fan Y., Li Z., He Z., Yin S., Feng N. Recent developments in the principles, modification and application prospects of functionalized ethosomes for topical delivery. Curr. Drug Deliv. 2021;18:570–582. doi: 10.2174/1567201817666200826093102. [DOI] [PubMed] [Google Scholar]
- 110.Zhang Z., Chen Y., Xu H., Wo Y., Zhang Z., Liu Y., Su W., Cui D., Zhang Y. 5-aminolevulinic acid loaded ethosomal vesicles with high entrapment efficiency for in vitro topical transdermal delivery and photodynamic therapy of hypertrophic scars. Nanoscale. 2016;8:19270–19279. doi: 10.1039/C6NR06872C. [DOI] [PubMed] [Google Scholar]
- 111.Khan N.R., Wong T.W. Microwave-aided skin drug penetration and retention of 5-fluorouracil-loaded ethosomes. Expert Opin. Drug Deliv. 2016;13:1209–1219. doi: 10.1080/17425247.2016.1193152. [DOI] [PubMed] [Google Scholar]
- 112.Khan N.R., Wong T.W. 5-fluorouracil ethosomes—Skin deposition and melanoma permeation synergism with microwave. Artif. Cells Nanomed. Biotechnol. 2018;46:568–577. doi: 10.1080/21691401.2018.1431650. [DOI] [PubMed] [Google Scholar]
- 113.El-Shenawy A.A., Mahmoud R.A., Mahmoud E.A., Mohamed M.S. Int.ranasal in situ gel of apixaban-loaded nanoethosomes: Preparation, optimization, and in vivo evaluation. AAPS PharmSciTech. 2021;22:147. doi: 10.1208/s12249-021-02020-y. [DOI] [PubMed] [Google Scholar]
- 114.Apriani E.F., Rosana Y., Iskandarsyah I. Formulation, characterization, and in vitro testing of azelaic acid ethosome-based cream against propionibacterium acnes for the treatment of acne. J. Adv. Pharm. Technol. Res. 2019;10:75–80. doi: 10.4103/japtr.JAPTR_289_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Mistry A., Ravikumar P. Development and evaluation of azelaic acid based ethosomes for topical delivery for the treatment of acne. Indian J. Pharm. Educ. Res. 2016;50:S232–S243. doi: 10.5530/ijper.50.3.34. [DOI] [Google Scholar]
- 116.Hallan S.S., Sguizzato M., Mariani P., Cortesi R., Huang N., Simelière F., Marchetti N., Drechsler M., Ruzgas T., Esposito E. Design and characterization of ethosomes for transdermal delivery of caffeic acid. Pharmaceutics. 2020;12:740. doi: 10.3390/pharmaceutics12080740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Guo T., Lu J., Fan Y., Zhang Y., Yin S., Sha X., Feng N. Tpgs assists the percutaneous administration of curcumin and glycyrrhetinic acid coloaded functionalized ethosomes for the synergistic treatment of psoriasis. Int. J. Pharm. 2021;604:120762. doi: 10.1016/j.ijpharm.2021.120762. [DOI] [PubMed] [Google Scholar]
- 118.Zhang Y., Xia Q., Li Y., He Z., Li Z., Guo T., Wu Z., Feng N. Cd44 assists the topical anti-psoriatic efficacy of curcumin-loaded hyaluronan-modified ethosomes: A new strategy for clustering drug in inflammatory skin. Theranostics. 2019;9:48–64. doi: 10.7150/thno.29715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ma L., Wang X., Wu J., Zhang D., Zhang L., Song X., Hong H., He C., Mo X., Wu S., et al. Polyethylenimine and sodium cholate-modified ethosomes complex as multidrug carriers for the treatment of melanoma through transdermal delivery. Nanomedicine. 2019;14:2395–2408. doi: 10.2217/nnm-2018-0398. [DOI] [PubMed] [Google Scholar]
- 120.Apolinário A.C., Hauschke L., Nunes J.R., Lourenço F.R., Lopes L.B. Design of multifunctional ethosomes for topical fenretinide delivery and breast cancer chemoprevention. Colloids Surf. A Physicochem. Eng. Asp. 2021;623:126745. doi: 10.1016/j.colsurfa.2021.126745. [DOI] [Google Scholar]
- 121.Nasr S., Rady M., Gomaa I., Syrovets T., Simmet T., Fayad W., Abdel-Kader M. Ethosomes and lipid-coated chitosan nanocarriers for skin delivery of a chlorophyll derivative: A potential treatment of squamous cell carcinoma by photodynamic therapy. Int. J. Pharm. 2019;568:118528. doi: 10.1016/j.ijpharm.2019.118528. [DOI] [PubMed] [Google Scholar]
- 122.Moolakkadath T., Aqil M., Ahad A., Imam S.S., Praveen A., Sultana Y., Mujeeb M., Iqbal Z. Fisetin loaded binary ethosomes for management of skin cancer by dermal application on uv exposed mice. Int. J. Pharm. 2019;560:78–91. doi: 10.1016/j.ijpharm.2019.01.067. [DOI] [PubMed] [Google Scholar]
- 123.Paliwal S., Tilak A., Sharma J., Dave V., Sharma S., Yadav R., Patel S., Verma K., Tak K. Flurbiprofen loaded ethosomes—Transdermal delivery of anti-inflammatory effect in rat model. Lipids Health Dis. 2019;18:133. doi: 10.1186/s12944-019-1064-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Marto J., Vitor C., Guerreiro A., Severino C., Eleutério C., Ascenso A., Simões S. Ethosomes for enhanced skin delivery of griseofulvin. Colloids Surf. B Biointerfaces. 2016;146:616–623. doi: 10.1016/j.colsurfb.2016.07.021. [DOI] [PubMed] [Google Scholar]
- 125.Xie J., Ji Y., Xue W., Ma D., Hu Y. Hyaluronic acid-containing ethosomes as a potential carrier for transdermal drug delivery. Colloids Surf. B Biointerfaces. 2018;172:323–329. doi: 10.1016/j.colsurfb.2018.08.061. [DOI] [PubMed] [Google Scholar]
- 126.Zhang Y., Ng W., Hu J., Mussa S.S., Ge Y., Xu H. Formulation and in vitro stability evaluation of ethosomal carbomer hydrogel for transdermal vaccine delivery. Colloids Surf. B Biointerfaces. 2018;163:184–191. doi: 10.1016/j.colsurfb.2017.12.031. [DOI] [PubMed] [Google Scholar]
- 127.Sakdiset P., Amnuaikit T., Pichayakorn W., Pinsuwan S. Formulation development of ethosomes containing indomethacin for transdermal delivery. J. Drug Deliv. Sci. Technol. 2019;52:760–768. doi: 10.1016/j.jddst.2019.05.048. [DOI] [Google Scholar]
- 128.Elsayed M.M.A., Okda T.M., Atwa G.M.K., Omran G.A., Abd Elbaky A.E., Ramadan A.E.H. Design and optimization of orally administered luteolin nanoethosomes to enhance its anti-tumor activity against hepatocellular carcinoma. Pharmaceutics. 2021;13:648. doi: 10.3390/pharmaceutics13050648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chandra A., Aggarwal G., Manchanda S., Narula A. Development of topical gel of methotrexate incorporated ethosomes and salicylic acid for the treatment of psoriasis. Pharm. Nanotechnol. 2019;7:362–374. doi: 10.2174/2211738507666190906123643. [DOI] [PubMed] [Google Scholar]
- 130.Garg B.J., Garg N.K., Beg S., Singh B., Katare O.P. Nanosized ethosomes-based hydrogel formulations of methoxsalen for enhanced topical delivery against vitiligo: Formulation optimization, in vitro evaluation and preclinical assessment. J. Drug Target. 2016;24:233–246. doi: 10.3109/1061186X.2015.1070855. [DOI] [PubMed] [Google Scholar]
- 131.Ma H., Guo D., Fan Y., Wang J., Cheng J., Zhang X. Paeonol-loaded ethosomes as transdermal delivery carriers: Design, preparation and evaluation. Molecules. 2018;23:1756. doi: 10.3390/molecules23071756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Cui Y., Mo Y., Zhang Q., Tian W., Xue Y., Bai J., Du S. Microneedle-assisted percutaneous delivery of paeoniflorin-loaded ethosomes. Molecules. 2018;23:3371. doi: 10.3390/molecules23123371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Limsuwan T., Boonme P., Khongkow P., Amnuaikit T. Ethosomes of phenylethyl resorcinol as vesicular delivery system for skin lightening applications. BioMed. Res. Int. 2017;2017:8310979. doi: 10.1155/2017/8310979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Arora D., Nanda S. Quality by design driven development of resveratrol loaded ethosomal hydrogel for improved dermatological benefits via enhanced skin permeation and retention. Int. J. Pharm. 2019;567:118448. doi: 10.1016/j.ijpharm.2019.118448. [DOI] [PubMed] [Google Scholar]
- 135.Salem H.F., Kharshoum R.M., Awad S.M., Ahmed Mostafa M., Abou-Taleb H.A. Tailoring of retinyl palmitate-based ethosomal hydrogel as a novel nanoplatform for acne vulgaris management: Fabrication, optimization, and clinical evaluation employing a split-face comparative study. Int. J. Nanomed. 2021;16:4251–4276. doi: 10.2147/IJN.S301597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Cristiano M.C., Froiio F., Spaccapelo R., Mancuso A., Nisticò S.P., Udongo B.P., Fresta M., Paolino D. Sulforaphane-loaded ultradeformable vesicles as a potential natural nanomedicine for the treatment of skin cancer diseases. Pharmaceutics. 2019;12:6. doi: 10.3390/pharmaceutics12010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Iizhar S.A., Syed I.A., Satar R., Ansari S.A. In vitro assessment of pharmaceutical potential of ethosomes entrapped with terbinafine hydrochloride. J. Adv. Res. 2016;7:453–461. doi: 10.1016/j.jare.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Kausar H., Mujeeb M., Ahad A., Moolakkadath T., Aqil M., Ahmad A., Akhter M.H. Optimization of ethosomes for topical thymoquinone delivery for the treatment of skin acne. J. Drug Deliv. Sci. Technol. 2019;49:177–187. doi: 10.1016/j.jddst.2018.11.016. [DOI] [Google Scholar]
- 139.Fu X., Shi Y., Wang H., Zhao X., Sun Q., Huang Y., Qi T., Lin G. Ethosomal gel for improving transdermal delivery of thymosin β-4. Int. J. Nanomed. 2019;14:9275–9284. doi: 10.2147/IJN.S228863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Venkatesh D., Kalyani K., Tulasi K., Priyanka V., Ali S.K.A., Kiran H.C. Transfersomes: A novel technique for transdermal drug delivery. J. Drug Deliv. Ther. 2019;9:279–285. [Google Scholar]
- 141.Benson H.A. Transfersomes for transdermal drug delivery. Expert Opin. Drug Deliv. 2006;3:727–737. doi: 10.1517/17425247.3.6.727. [DOI] [PubMed] [Google Scholar]
- 142.Jiang T., Wang T., Li T., Ma Y., Shen S., He B., Mo R. Enhanced transdermal drug delivery by transfersome-embedded oligopeptide hydrogel for topical chemotherapy of melanoma. ACS Nano. 2018;12:9693–9701. doi: 10.1021/acsnano.8b03800. [DOI] [PubMed] [Google Scholar]
- 143.Opatha S.A.T., Titapiwatanakun V., Chutoprapat R. Transfersomes: A promising nanoencapsulation technique for transdermal drug delivery. Pharmaceutics. 2020;12:855. doi: 10.3390/pharmaceutics12090855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Pandey A. Role of surfactants as penetration enhancer in transdermal drug delivery system. J. Mol. Pharm. Org. Process. Res. 2014;2:2–7. doi: 10.4172/2329-9053.1000113. [DOI] [Google Scholar]
- 145.Dudhipala N., Phasha Mohammed R., Adel Ali Youssef A., Banala N. Effect of lipid and edge activator concentration on development of aceclofenac-loaded transfersomes gel for transdermal application: In vitro and ex vivo skin permeation. Drug Dev. Ind. Pharm. 2020;46:1334–1344. doi: 10.1080/03639045.2020.1788069. [DOI] [PubMed] [Google Scholar]
- 146.Manconi M., Manca M.L., Caddeo C., Valenti D., Cencetti C., Diez-Sales O., Nacher A., Mir-Palomo S., Terencio M.C., Demurtas D., et al. Nanodesign of new self-assembling core-shell gellan-transfersomes loading baicalin and in vivo evaluation of repair response in skin. Nanomedicine. 2018;14:569–579. doi: 10.1016/j.nano.2017.12.001. [DOI] [PubMed] [Google Scholar]
- 147.Chen M., Shamim M.A., Shahid A., Yeung S., Andresen B.T., Wang J., Nekkanti V., Meyskens F.L., Jr., Kelly K.M., Huang Y. Topical delivery of carvedilol loaded nano-transfersomes for skin cancer chemoprevention. Pharmaceutics. 2020;12:1151. doi: 10.3390/pharmaceutics12121151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Khatoon K., Rizwanullah M., Amin S., Mir S.R., Akhter S. Cilnidipine loaded transfersomes for transdermal application: Formulation optimization, in-vitro and in-vivo study. J. Drug Deliv. Sci. Technol. 2019;54:101303. doi: 10.1016/j.jddst.2019.101303. [DOI] [Google Scholar]
- 149.El-Gizawy S.A., Nouh A., Saber S., Kira A.Y. Deferoxamine-loaded transfersomes accelerates healing of pressure ulcers in streptozotocin-induced diabetic rats. J. Drug Deliv. Sci. Technol. 2020;58:101732. doi: 10.1016/j.jddst.2020.101732. [DOI] [Google Scholar]
- 150.Luiz M.T., Viegas J.S.R., Abriata J.P., Tofani L.B., Vaidergorn M.d.M., Emery F.d.S., Chorilli M., Marchetti J.M. Docetaxel-loaded folate-modified tpgs-transfersomes for glioblastoma multiforme treatment. Mater. Sci. Eng. C. 2021;124:112033. doi: 10.1016/j.msec.2021.112033. [DOI] [PubMed] [Google Scholar]
- 151.Avadhani K.S., Manikkath J., Tiwari M., Chandrasekhar M., Godavarthi A., Vidya S.M., Hariharapura R.C., Kalthur G., Udupa N., Mutalik S. Skin delivery of epigallocatechin-3-gallate (egcg) and hyaluronic acid loaded nano-transfersomes for antioxidant and anti-aging effects in uv radiation induced skin damage. Drug Deliv. 2017;24:61–74. doi: 10.1080/10717544.2016.1228718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Ahad A., Al-Saleh A.A., Al-Mohizea A.M., Al-Jenoobi F.I., Raish M., Yassin A.E.B., Alam M.A. Formulation and characterization of phospholipon 90 g and tween 80 based transfersomes for transdermal delivery of eprosartan mesylate. Pharm. Dev. Technol. 2018;23:787–793. doi: 10.1080/10837450.2017.1330345. [DOI] [PubMed] [Google Scholar]
- 153.Langasco R., Fancello S., Rassu G., Cossu M., Cavalli R., Galleri G., Giunchedi P., Migheli R., Gavini E. Increasing protective activity of genistein by loading into transfersomes: A new potential adjuvant in the oxidative stress-related neurodegenerative diseases? Phytomedicine. 2019;52:23–31. doi: 10.1016/j.phymed.2018.09.207. [DOI] [PubMed] [Google Scholar]
- 154.Balata G.F., Faisal M.M., Elghamry H.A., Sabry S.A. Preparation and characterization of ivabradine hcl transfersomes for enhanced transdermal delivery. J. Drug Deliv. Sci. Technol. 2020;60:101921. doi: 10.1016/j.jddst.2020.101921. [DOI] [Google Scholar]
- 155.Allaw M., Pleguezuelos-Villa M., Manca M.L., Caddeo C., Aroffu M., Nacher A., Diez-Sales O., Saurí A.R., Ferrer E.E., Fadda A.M., et al. Innovative strategies to treat skin wounds with mangiferin: Fabrication of transfersomes modified with glycols and mucin. Nanomedicine. 2020;15:1671–1685. doi: 10.2217/nnm-2020-0116. [DOI] [PubMed] [Google Scholar]
- 156.Janga K.Y., Tatke A., Dudhipala N., Balguri S.P., Ibrahim M.M., Maria D.N., Jablonski M.M., Majumdar S. Gellan gum based sol-to-gel transforming system of natamycin transfersomes improves topical ocular delivery. J. Pharm. Exp. 2019;370:814–822. doi: 10.1124/jpet.119.256446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Al Shuwaili A.H., Rasool B.K., Abdulrasool A.A. Optimization of elastic transfersomes formulations for transdermal delivery of pentoxifylline. Eur. J. Pharm. Biopharm. 2016;102:101–114. doi: 10.1016/j.ejpb.2016.02.013. [DOI] [PubMed] [Google Scholar]
- 158.Wu P.S., Li Y.S., Kuo Y.C., Tsai S.J., Lin C.C. Preparation and evaluation of novel transfersomes combined with the natural antioxidant resveratrol. Molecules. 2019;24:600. doi: 10.3390/molecules24030600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Pena-Rodríguez E., Moreno M.C., Blanco-Fernandez B., González J., Fernández-Campos F. Epidermal delivery of retinyl palmitate loaded transfersomes: Penetration and biodistribution studies. Pharmaceutics. 2020;12:112. doi: 10.3390/pharmaceutics12020112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Sundralingam U., Chakravarthi S., Radhakrishnan A.K., Muniyandy S., Palanisamy U.D. Efficacy of emu oil transfersomes for local transdermal delivery of 4-oh tamoxifen in the treatment of breast cancer. Pharmaceutics. 2020;12:807. doi: 10.3390/pharmaceutics12090807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Hasibi F., Nasirpour A., Varshosaz J., García-Manrique P., Blanco-López M.C., Gutiérrez G., Matos M. Formulation and characterization of taxifolin-loaded lipid nanovesicles (liposomes, niosomes, and transfersomes) for beverage fortification. Eur. J. Lipid Sci. Technol. 2020;122:1900105. doi: 10.1002/ejlt.201900105. [DOI] [Google Scholar]
- 162.Caddeo C., Manca M.L., Peris J.E., Usach I., Diez-Sales O., Matos M., Fernàndez-Busquets X., Fadda A.M., Manconi M. Tocopherol-loaded transfersomes: In vitro antioxidant activity and efficacy in skin regeneration. Int. J. Pharm. 2018;551:34–41. doi: 10.1016/j.ijpharm.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 163.Pitta S.K., Dudhipala N., Narala A., Veerabrahma K. Development of zolmitriptan transfersomes by box-behnken design for nasal delivery: In vitro and in vivo evaluation. Drug Dev. Ind. Pharm. 2018;44:484–492. doi: 10.1080/03639045.2017.1402918. [DOI] [PubMed] [Google Scholar]
- 164.Kateh Shamshiri M., Momtazi-Borojeni A.A., Khodabandeh Shahraky M., Rahimi F. Lecithin soybean phospholipid nano-transfersomes as potential carriers for transdermal delivery of the human growth hormone. J. Cell Biochem. 2019;120:9023–9033. doi: 10.1002/jcb.28176. [DOI] [PubMed] [Google Scholar]
- 165.De Marco Almeida F., Silva C.N., de Araujo Lopes S.C., Santos D.M., Torres F.S., Cardoso F.L., Martinelli P.M., da Silva E.R., de Lima M.E., Miranda L.A.F., et al. Physicochemical characterization and skin permeation of cationic transfersomes containing the synthetic peptide pnpp-19. Curr. Drug Deliv. 2018;15:1064–1071. doi: 10.2174/1567201815666180108170206. [DOI] [PubMed] [Google Scholar]
- 166.Semalty A., Semalty M., Rawat B.S., Singh D., Rawat M.S. Pharmacosomes: The lipid-based new drug delivery system. Expert Opin. Drug Deliv. 2009;6:599–612. doi: 10.1517/17425240902967607. [DOI] [PubMed] [Google Scholar]
- 167.Patel J.L., Bharadia P.D. A review on: Pharmacosomes as a novel vesicular drug delivery system. World J. Pharm. Res. 2012;1:456–469. [Google Scholar]
- 168.Pathak K., Keshri L., Shah M. Lipid nanocarriers: Influence of lipids on product development and pharmacokinetics. Crit. Rev. Drug Carr. Syst. 2011;28:357–393. doi: 10.1615/CritRevTherDrugCarrierSyst.v28.i4.20. [DOI] [PubMed] [Google Scholar]
- 169.Kapoor B., Gupta R., Singh S.K., Gulati M., Singh S. Prodrugs, phospholipids and vesicular delivery—An effective triumvirate of pharmacosomes. Adv. Colloid Interface Sci. 2018;253:35–65. doi: 10.1016/j.cis.2018.01.003. [DOI] [PubMed] [Google Scholar]
- 170.K R Veena S.K.S. Pharmacosomes: A novel strategy for controlled drug delivery. J. Pharm. Sci. Res. 2019;11:2590–2593. [Google Scholar]
- 171.Al-kaf A.G.A., Othman A.M. A review on pharmacosomes: An emerging novel vesicular drug delivery system. Univers. J. Pharm. Res. 2017;2:21-4. [Google Scholar]
- 172.Semalty A., Semalty M., Rawat B.S., Singh D., Rawat M.S. Development and evaluation of pharmacosomes of aceclofenac. Indian J. Pharm. Sci. 2010;72:576–581. doi: 10.4103/0250-474X.78523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Xue F., Lin X., Cai Z., Liu X., Ma Y., Wu M. Doxifluridine-based pharmacosomes delivering mir-122 as tumor microenvironments-activated nanoplatforms for synergistic treatment of hepatocellular carcinoma. Colloids Surf. B Biointerfaces. 2021;197:111367. doi: 10.1016/j.colsurfb.2020.111367. [DOI] [PubMed] [Google Scholar]
- 174.Soman M.D., Dharan S.S., Mathew L.T. Formulation and evaluation of selective cox-2 inhibitor loaded pharmacosomes for the treatment of rheumatoid arthritis. J. Pharm. Sci. Res. 2020;12:1502–1509. [Google Scholar]
- 175.Jin S., Du Z., Guo H., Zhang H., Ren F., Wang P. Novel targeted anti-tumor nanoparticles developed from folic acid-modified 2-deoxyglucose. Int. J. Mol. Sci. 2019;20:697. doi: 10.3390/ijms20030697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Amirinejad M., Davoodi J., Abbaspour M.R., Akhgari A., Hadizadeh F., Badiee A. Preparation, characterization and improved release profile of ibuprofen-phospholipid association. J. Drug Deliv. Sci. Technol. 2020;60:101951. doi: 10.1016/j.jddst.2020.101951. [DOI] [Google Scholar]
- 177.Kotha Y., Kandhula A.G., Janapareddi K. Development and characterization of levodopa loaded pharmacosomes for brain targeting via intranasal route: Pharmacodynamic evaluation in rats. J. Young Pharm. 2020;12:s56–s62. doi: 10.5530/jyp.2020.12s.47. [DOI] [Google Scholar]
- 178.Kusuma D.P.J.K. Sundaraseelan. Formulation and evaluation of pharmacosomal gel loaded with nsaid. World J. Pharm. Med. Res. 2018;4:81–88. [Google Scholar]
- 179.Pal T. Design, fabrication and evaluation of rosuvastatin pharmacosome—A novel sustained release drug delivery system. Eur. J. Pharm. Med. Res. 2016;3:332–350. [Google Scholar]
- 180.Gebicki J.M., Hicks M. Ufasomes are stable particles surrounded by unsaturated fatty acid membranes. Nature. 1973;243:232–234. doi: 10.1038/243232a0. [DOI] [PubMed] [Google Scholar]
- 181.Arundhasree R., Aiswarya R., Kumar A.R., Kumar S., Nair S. Ufasomes: Unsaturated fatty acid based vesicular drug delivery system. Int. J. Appl. Pharm. 2021;13:76–83. doi: 10.22159/ijap.2021v13i2.39526. [DOI] [Google Scholar]
- 182.Morigaki K., Walde P. Fatty acid vesicles. Curr. Opin. Colloid Interface Sci. 2007;12:75–80. doi: 10.1016/j.cocis.2007.05.005. [DOI] [Google Scholar]
- 183.Cristiano M.C., Froiio F., Mancuso A., Cosco D., Dini L., Di Marzio L., Fresta M., Paolino D. Oleuropein-laded ufasomes improve the nutraceutical efficacy. Nanomaterials. 2021;11:105. doi: 10.3390/nano11010105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Salama A.H., Aburahma M.H. Ufasomes nano-vesicles-based lyophilized platforms for intranasal delivery of cinnarizine: Preparation, optimization, ex-vivo histopathological safety assessment and mucosal confocal imaging. Pharm. Dev. Technol. 2016;21:706–715. doi: 10.3109/10837450.2015.1048553. [DOI] [PubMed] [Google Scholar]
- 185.Kumar P., Singh S.K., Handa V., Kathuria H. Oleic acid nanovesicles of minoxidil for enhanced follicular delivery. Medicines. 2018;5:103. doi: 10.3390/medicines5030103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Kaur N., Garg R., Devgan M., Singh A. Optimization and antifungal activity determination of tea tree oil containing oxiconazole loaded ufasomes gel against candida albicans. Energy Environ. Focus. 2016;5:287–294. doi: 10.1166/eef.2016.1230. [DOI] [Google Scholar]
- 187.Bhattacharya S. Preparation and characterizations of glyceryl oleate ufasomes of terbinafine hydrochloride: A novel approach to trigger candida albicans fungal infection. Future J. Pharm. Sci. 2021;7:3. doi: 10.1186/s43094-020-00143-w. [DOI] [Google Scholar]
- 188.Ting Y., Jiang Y., Ho C.-T., Huang Q. Common delivery systems for enhancing in vivo bioavailability and biological efficacy of nutraceuticals. J. Funct. Foods. 2014;7:112–128. doi: 10.1016/j.jff.2013.12.010. [DOI] [Google Scholar]
- 189.Khan J., Alexander A., Ajazuddin, Saraf S., Saraf S. Recent advances and future prospects of phyto-phospholipid complexation technique for improving pharmacokinetic profile of plant actives. J. Control. Release. 2013;168:50–60. doi: 10.1016/j.jconrel.2013.02.025. [DOI] [PubMed] [Google Scholar]
- 190.Alharbi W.S., Almughem F.A., Almehmady A.M., Jarallah S.J., Alsharif W.K., Alzahrani N.M., Alshehri A.A. Phytosomes as an emerging nanotechnology platform for the topical delivery of bioactive phytochemicals. Pharmaceutics. 2021;13:1475. doi: 10.3390/pharmaceutics13091475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Sharma S., Sahu A.N. Development, characterization, and evaluation of hepatoprotective effect of abutilon indicum and piper longum phytosomes. Pharmacogn. Res. 2016;8:29–36. doi: 10.4103/0974-8490.171102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Mancini S., Nardo L., Gregori M., Ribeiro I., Mantegazza F., Delerue-Matos C., Masserini M., Grosso C. Functionalized liposomes and phytosomes loading annona muricata l. Aqueous extract: Potential nanoshuttles for brain-delivery of phenolic compounds. Phytomedicine. 2018;42:233–244. doi: 10.1016/j.phymed.2018.03.053. [DOI] [PubMed] [Google Scholar]
- 193.Huang Z., Brennan C.S., Zhao H., Liu J., Guan W., Mohan M.S., Stipkovits L., Zheng H., Kulasiri D. Fabrication and assessment of milk phospholipid-complexed antioxidant phytosomes with vitamin c and e: A comparison with liposomes. Food Chem. 2020;324:126837. doi: 10.1016/j.foodchem.2020.126837. [DOI] [PubMed] [Google Scholar]
- 194.Yu F., Li Y., Chen Q., He Y., Wang H., Yang L., Guo S., Meng Z., Cui J., Xue M., et al. Monodisperse microparticles loaded with the self-assembled berberine-phospholipid complex-based phytosomes for improving oral bioavailability and enhancing hypoglycemic efficiency. Eur. J. Pharm. Biopharm. 2016;103:136–148. doi: 10.1016/j.ejpb.2016.03.019. [DOI] [PubMed] [Google Scholar]
- 195.Molaveisi M., Shahidi Noghabi M., Parastouei K., Taheri R.A. Fate of nano-phytosomes containing bioactive compounds of echinacea extract in an acidic food beverage. Food Struct. 2021;27:100177. doi: 10.1016/j.foostr.2021.100177. [DOI] [Google Scholar]
- 196.Kim S.M., Jung J.I., Chai C., Imm J.Y. Characteristics and glucose uptake promoting effect of chrysin-loaded phytosomes prepared with different phospholipid matrices. Nutrients. 2019;11:2549. doi: 10.3390/nu11102549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Kim S.M., Imm J.Y. The effect of chrysin-loaded phytosomes on insulin resistance and blood sugar control in type 2 diabetic db/db mice. Molecules. 2020;25:5503. doi: 10.3390/molecules25235503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Xu L., Xu D., Li Z., Gao Y., Chen H. Synthesis and potent cytotoxic activity of a novel diosgenin derivative and its phytosomes against lung cancer cells. Beilstein J. Nanotechnol. 2019;10:1933–1942. doi: 10.3762/bjnano.10.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Udapurkar P., Bhusnure D.O., Kamble S. Diosmin phytosomes: Development, optimization and physicochemical characterization. Indian J. Pharm. Educ. Res. 2018;52:s29–s36. doi: 10.5530/ijper.52.4s.73. [DOI] [Google Scholar]
- 200.Islam N., Irfan M., Hussain T., Mushtaq M., Khan I.U., Yousaf A.M., Ghori M.U., Shahzad Y. Piperine phytosomes for bioavailability enhancement of domperidone. J. Liposome Res. 2021;4:1–9. doi: 10.1080/08982104.2021.1918153. [DOI] [PubMed] [Google Scholar]
- 201.Karole S., Gautam G.K., Gupta S.K. Preparation and evaluation of phytosomes containing ethanolic extract of leaves of bombax ceiba for hepatoprotective activity. Pharma Innov. 2019;8:22–26. [Google Scholar]
- 202.Rathee S., Kamboj A. Optimization and development of antidiabetic phytosomes by the box-behnken design. J. Liposome Res. 2018;28:161–172. doi: 10.1080/08982104.2017.1311913. [DOI] [PubMed] [Google Scholar]
- 203.Komeil I.A., El-Refaie W.M., Gowayed M.A., El-Ganainy S.O., El Achy S.N., Huttunen K.M., Abdallah O.Y. Oral genistein-loaded phytosomes with enhanced hepatic uptake, residence and improved therapeutic efficacy against hepatocellular carcinoma. Int. J. Pharm. 2021;601:120564. doi: 10.1016/j.ijpharm.2021.120564. [DOI] [PubMed] [Google Scholar]
- 204.Alhakamy N.A., A Fahmy U., Badr-Eldin S.M., Ahmed O.A.A., Asfour H.Z., Aldawsari H.M., Algandaby M.M., Eid B.G., Abdel-Naim A.B., Awan Z.A., et al. Optimized icariin phytosomes exhibit enhanced cytotoxicity and apoptosis-inducing activities in ovarian cancer cells. Pharmaceutics. 2020;12:346. doi: 10.3390/pharmaceutics12040346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Rhatih Eka S., Silvia S., Fadlina Chany S. Formulation and characterization of bitter melon extract (momordica charantia) loaded phytosomes. Pharmacogn. J. 2019;11:1235–1241. doi: 10.5530/pj.2019.11.192. [DOI] [Google Scholar]
- 206.Direito R., Reis C., Roque L., Gonçalves M., Sanches-Silva A., Gaspar M.M., Pinto R., Rocha J., Sepodes B., Rosário Bronze M., et al. Phytosomes with persimmon (diospyros kaki l.) extract: Preparation and preliminary demonstration of in vivo tolerability. Pharmaceutics. 2019;11:296. doi: 10.3390/pharmaceutics11060296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Permana A.D., Utami R.N., Courtenay A.J., Manggau M.A., Donnelly R.F., Rahman L. Phytosomal nanocarriers as platforms for improved delivery of natural antioxidant and photoprotective compounds in propolis: An approach for enhanced both dissolution behaviour in biorelevant media and skin retention profiles. J. Photochem. Photobiol. B Biol. 2020;205:111846. doi: 10.1016/j.jphotobiol.2020.111846. [DOI] [PubMed] [Google Scholar]
- 208.Vu H.T.H., Hook S.M., Siqueira S.D., Müllertz A., Rades T., McDowell A. Are phytosomes a superior nanodelivery system for the antioxidant rutin? Int. J. Pharm. 2018;548:82–91. doi: 10.1016/j.ijpharm.2018.06.042. [DOI] [PubMed] [Google Scholar]
- 209.El-Batal A., Elmenshawi S., Ali A., Eldbaiky E. Preparation and characterization of silymarin nanocrystals and phytosomes with investigation of their stability using gamma irradiation. Indian J. Pharm. Educ. Res. 2018;52:S174–S183. doi: 10.5530/ijper.52.4s.96. [DOI] [Google Scholar]
- 210.Kumar S., Baldi A., Sharma D.K. In vitro antioxidant assay guided ex vivo investigation of cytotoxic effect of phytosomes assimilating taxifolin rich fraction of cedrus deodara bark extract on human breast cancer cell lines (mcf7) J. Drug Deliv. Sci. Technol. 2021;63:102486. doi: 10.1016/j.jddst.2021.102486. [DOI] [Google Scholar]
- 211.Alhakamy N.A., Badr-Eldin S.M., Fahmy U.A., Alruwaili N.K., Awan Z.A., Caruso G., Alfaleh M.A., Alaofi A.L., Arif F.O., Ahmed O.A.A., et al. Thymoquinone-loaded soy-phospholipid-based phytosomes exhibit anticancer potential against human lung cancer cells. Pharmaceutics. 2020;12:761. doi: 10.3390/pharmaceutics12080761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Freag M.S., Saleh W.M., Abdallah O.Y. Laminated chitosan-based composite sponges for transmucosal delivery of novel protamine-decorated tripterine phytosomes: Ex-vivo mucopenetration and in-vivo pharmacokinetic assessments. Carbohydr. Polym. 2018;188:108–120. doi: 10.1016/j.carbpol.2018.01.095. [DOI] [PubMed] [Google Scholar]
- 213.Zhu S., Luo C., Feng W., Li Y., Zhu M., Sun S., Zhang X. Selenium-deposited tripterine phytosomes ameliorate the antiarthritic efficacy of the phytomedicine via a synergistic sensitization. Int. J. Pharm. 2020;578:119104. doi: 10.1016/j.ijpharm.2020.119104. [DOI] [PubMed] [Google Scholar]
- 214.Ittadwar P., Puranik P. Novel umbelliferone phytosomes: Development and optimization using experimental design approach and evaluation of photo-protective and antioxidant activity. Int. J. Pharm. Pharm. Sci. 2016;9:218. doi: 10.22159/ijpps.2017v9i1.14635. [DOI] [Google Scholar]
- 215.Xie X., He D., Wu Y., Wang T., Zhong C., Zhang J. Catanionic hybrid lipid nanovesicles for improved bioavailability and efficacy of chemotherapeutic drugs. In: Narayanan K., editor. Bio-Carrier Vectors: Methods and Protocols. Springer US; New York, NY, USA: 2021. pp. 57–68. [DOI] [PubMed] [Google Scholar]
- 216.Safran S.A., Pincus P., Andelman D. Theory of spontaneous vesicle formation in surfactant mixtures. Science. 1990;248:354–356. doi: 10.1126/science.248.4953.354. [DOI] [PubMed] [Google Scholar]
- 217.Lozano N., Pérez L., Pons R., Pinazo A. Diacyl glycerol arginine-based surfactants: Biological and physicochemical properties of catanionic formulations. Amino Acids. 2011;40:721–729. doi: 10.1007/s00726-010-0710-4. [DOI] [PubMed] [Google Scholar]
- 218.Pinazo A., Pons R., Marqués A., Farfan M., da Silva A., Perez L. Biocompatible catanionic vesicles from arginine-based surfactants: A new strategy to tune the antimicrobial activity and cytotoxicity of vesicular systems. Pharmaceutics. 2020;12:857. doi: 10.3390/pharmaceutics12090857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Jain M., Marfatia A., Imam N., Ray D., Aswal V.K., Patel N.Y., Raval V.H., Kailasa S.K., Malek N.I. Ionic liquid-based catanionic vesicles: A de novo system to judiciously improve the solubility, stability and antimicrobial activity of curcumin. J. Mol. Liq. 2021;341:117396. doi: 10.1016/j.molliq.2021.117396. [DOI] [Google Scholar]
- 220.Li S., Fang C., Zhang J., Liu B., Wei Z., Fan X., Sui Z., Tan Q. Catanionic lipid nanosystems improve pharmacokinetics and anti-lung cancer activity of curcumin. Nanomedicine. 2016;12:1567–1579. doi: 10.1016/j.nano.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 221.Patel R., Ahmad Wani F., Mahfooz F., Mishra P., Abrar Siddiquee M. Interaction of human serum albumin with diclofenac incorporated in catanionic vesicles. Mater. Today Proc. 2021;36:736–742. doi: 10.1016/j.matpr.2020.05.179. [DOI] [Google Scholar]
- 222.Gonçalves Lopes R.C.F., Silvestre O.F., Faria A.R., do Vale M.L.C., Marques E.F., Nieder J.B. Surface charge tunable catanionic vesicles based on serine-derived surfactants as efficient nanocarriers for the delivery of the anticancer drug doxorubicin. Nanoscale. 2019;11:5932–5941. doi: 10.1039/C8NR06346J. [DOI] [PubMed] [Google Scholar]
- 223.Geng S., Wang Y., Wang L., Kouyama T., Gotoh T., Wada S., Wang J.-Y. A light-responsive self-assembly formed by a cationic azobenzene derivative and sds as a drug delivery system. Sci. Rep. 2017;7:39202. doi: 10.1038/srep39202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Richard K., Mann B.J., Qin A., Barry E.M., Ernst R.K., Vogel S.N. Monophosphoryl lipid a enhances efficacy of a francisella tularensis lvs-catanionic nanoparticle subunit vaccine against f. Tularensis schu s4 challenge by augmenting both humoral and cellular immunity. Clin. Vaccine Immunol. 2017;24:e00574-16. doi: 10.1128/CVI.00574-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Stagnoli S., Sosa Alderete L., Luna M.A., Agostini E., Falcone R.D., Niebylski A.M., Correa N.M. Catanionic nanocarriers as a potential vehicle for insulin delivery. Colloids Surf. B Biointerfaces. 2020;188:110759. doi: 10.1016/j.colsurfb.2019.110759. [DOI] [PubMed] [Google Scholar]
- 226.Seidel Z.P., Zhang X., MacMullan M.A., Graham N.A., Wang P., Lee C.T. Photo-triggered delivery of sirna and paclitaxel into breast cancer cells using catanionic vesicles. ACS Appl. Bio Mater. 2020;3:7388–7398. doi: 10.1021/acsabm.0c00503. [DOI] [PubMed] [Google Scholar]
- 227.Kaur G., Berwal K., Sharma B., Chaudhary G.R., Gawali S.L., Hassan P.A. Enhanced antimicrobial photodynamic activity of photosensitizer encapsulated copper based metallocatanionic vesicles against e.Coli using visible light. J. Mol. Liq. 2021;324:114688. doi: 10.1016/j.molliq.2020.114688. [DOI] [Google Scholar]
- 228.Sharma B., Thakur V., Kaur G., Chaudhary G.R. Efficient photodynamic therapy against gram-positive and gram-negative bacteria using rose bengal encapsulated in metallocatanionic vesicles in the presence of visible light. ACS Appl. Bio Mater. 2020;3:8515–8524. doi: 10.1021/acsabm.0c00901. [DOI] [PubMed] [Google Scholar]
- 229.Russo Krauss I., Imperatore R., De Santis A., Luchini A., Paduano L., D’Errico G. Structure and dynamics of cetyltrimethylammonium chloride-sodium dodecylsulfate (ctac-sds) catanionic vesicles: High-value nano-vehicles from low-cost surfactants. J. Colloid Interface Sci. 2017;501:112–122. doi: 10.1016/j.jcis.2017.04.032. [DOI] [PubMed] [Google Scholar]
- 230.Torres-Luna C., Koolivand A., Fan X., Agrawal N.R., Hu N., Zhu Y., Domszy R., Briber R.M., Wang N.S., Yang A. Formation of drug-participating catanionic aggregates for extended delivery of non-steroidal anti-inflammatory drugs from contact lenses. Biomolecules. 2019;9:593. doi: 10.3390/biom9100593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Jiang Y., Hu X., Zhang J., Jin G., Luan Y. Chlorambucil prodrug-participating catanionic aggregates for sustained drug release and improved antitumour activity. J. Mol. Liq. 2018;274:556–561. doi: 10.1016/j.molliq.2018.10.165. [DOI] [Google Scholar]
- 232.Zhang M., Zhao S.X., Ding B., Zhang Y.Q. Sodium n-lauryl amino acids derived from silk protein can form catanionic aggregates with cytarabine as novel anti-tumor drug delivery systems. Drug Deliv. 2020;27:482–490. doi: 10.1080/10717544.2020.1742250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Stein D.C., H. Stocker L., Powell A.E., Kebede S., Watts D., Williams E., Soto N., Dhabaria A., Fenselau C., Ganapati S., et al. Extraction of membrane components from neisseria gonorrhoeae using catanionic surfactant vesicles: A new approach for the study of bacterial surface molecules. Pharmaceutics. 2020;12:787. doi: 10.3390/pharmaceutics12090787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Srivastava D., Liu C., Lv J., Deb D., Qiao W. Enhanced intercellular release of anticancer drug by using nano-sized catanionic vesicles of doxorubicin hydrochloride and gemini surfactants. J. Mol. Liq. 2018;259:398–410. doi: 10.1016/j.molliq.2018.03.065. [DOI] [Google Scholar]
- 235.Alp G., Aydogan N. Enhancing the spreading behavior on pulmonary mucus mimicking subphase via catanionic surfactant solutions: Toward effective drug delivery through the lungs. Mol. Pharm. 2018;15:1361–1370. doi: 10.1021/acs.molpharmaceut.8b00086. [DOI] [PubMed] [Google Scholar]
- 236.Rajput S.M., Kumar S., Aswal V.K., El Seoud O.A., Malek N.I., Kailasa S.K. Drug-induced micelle-to-vesicle transition of a cationic gemini surfactant: Potential applications in drug delivery. Chemphyschem. 2018;19:865–872. doi: 10.1002/cphc.201701134. [DOI] [PubMed] [Google Scholar]
- 237.Garcia M.T., Ribosa I., Gonzalez J.J., Comelles F. Catanionic mixtures of surface-active ionic liquids and n-lauroyl sarcosinate: Surface adsorption, aggregation behavior and microbial toxicity. J. Mol. Liq. 2020;318:114040. doi: 10.1016/j.molliq.2020.114040. [DOI] [Google Scholar]
- 238.Garcia M.T., Ribosa I., González J., Comelles F. Surface activity, self-aggregation and antimicrobial activity of catanionic mixtures of surface active imidazolium- or pyridinium-based ionic liquids and sodium bis(2-ethylhexyl) sulfosuccionate. J. Mol. Liq. 2020;303:112637. doi: 10.1016/j.molliq.2020.112637. [DOI] [Google Scholar]
- 239.Ruiz A., Pinazo A., Pérez L., Manresa A., Marqués A.M. Green catanionic gemini surfactant–lichenysin mixture: Improved surface, antimicrobial, and physiological properties. ACS Appl. Mater. Interfaces. 2017;9:22121–22131. doi: 10.1021/acsami.7b03348. [DOI] [PubMed] [Google Scholar]
- 240.Pérez L., Pinazo A., Morán M.C., Pons R. Aggregation behavior, antibacterial activity and biocompatibility of catanionic assemblies based on amino acid-derived surfactants. Int. J. Mol. Sci. 2020;21:8912. doi: 10.3390/ijms21238912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Roig F., Blanzat M., Solans C., Esquena J., García-Celma M.J. Hyaluronan based materials with catanionic sugar-derived surfactants as drug delivery systems. Colloids Surf. B Biointerfaces. 2018;164:218–223. doi: 10.1016/j.colsurfb.2018.01.037. [DOI] [PubMed] [Google Scholar]
- 242.Simeone P., Bologna G., Lanuti P., Pierdomenico L., Guagnano M.T., Pieragostino D., Del Boccio P., Vergara D., Marchisio M., Miscia S., et al. Extracellular vesicles as signaling mediators and disease biomarkers across biological barriers. Int. J. Mol. Sci. 2020;21:2514. doi: 10.3390/ijms21072514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Rimmer M.P., Gregory C.D., Mitchell R.T. Extracellular vesicles in urological malignancies. Biochim. Biophys. Acta Rev. Cancer. 2021;1876:188570. doi: 10.1016/j.bbcan.2021.188570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.O’Brien K., Breyne K., Ughetto S., Laurent L.C., Breakefield X.O. Rna delivery by extracellular vesicles in mammalian cells and its applications. Nat. Rev. Mol. Cell Biol. 2020;21:585–606. doi: 10.1038/s41580-020-0251-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.O’Brien K.P., Khan S., Gilligan K.E., Zafar H., Lalor P., Glynn C., O’Flatharta C., Ingoldsby H., Dockery P., De Bhulbh A., et al. Employing mesenchymal stem cells to support tumor-targeted delivery of extracellular vesicle (ev)-encapsulated microrna-379. Oncogene. 2018;37:2137–2149. doi: 10.1038/s41388-017-0116-9. [DOI] [PubMed] [Google Scholar]
- 246.Limongi T., Susa F., Dumontel B., Racca L., Perrone Donnorso M., Debellis D., Cauda V. Extracellular vesicles tropism: A comparative study between passive innate tropism and the active engineered targeting capability of lymphocyte-derived evs. Membranes. 2021;11:886. doi: 10.3390/membranes11110886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Susa F., Limongi T., Dumontel B., Vighetto V., Cauda V. Engineered extracellular vesicles as a reliable tool in cancer nanomedicine. Cancers. 2019;11:1979. doi: 10.3390/cancers11121979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Coleman L.G. The emerging world of subcellular biological medicine: Extracellular vesicles as novel biomarkers, targets, and therapeutics. Neural. Regen. Res. 2022;17:1020–1022. doi: 10.4103/1673-5374.324846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Ikeda G., Santoso M.R., Tada Y., Li A.M., Vaskova E., Jung J.-H., O’Brien C., Egan E., Ye J., Yang P.C. Mitochondria-rich extracellular vesicles from autologous stem cell–derived cardiomyocytes restore energetics of ischemic myocardium. J. Am. Coll. Cardiol. 2021;77:1073–1088. doi: 10.1016/j.jacc.2020.12.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.de Jong O.G., Kooijmans S.A.A., Murphy D.E., Jiang L., Evers M.J.W., Sluijter J.P.G., Vader P., Schiffelers R.M. Drug delivery with extracellular vesicles: From imagination to innovation. Acc. Chem. Res. 2019;52:1761–1770. doi: 10.1021/acs.accounts.9b00109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Elsharkasy O.M., Nordin J.Z., Hagey D.W., de Jong O.G., Schiffelers R.M., Andaloussi S.E.L., Vader P. Extracellular vesicles as drug delivery systems: Why and how? Adv. Drug Deliv. Rev. 2020;159:332–343. doi: 10.1016/j.addr.2020.04.004. [DOI] [PubMed] [Google Scholar]
- 252.Herrmann I.K., Wood M.J.A., Fuhrmann G. Extracellular vesicles as a next-generation drug delivery platform. Nat. Nanotechnol. 2021;16:748–759. doi: 10.1038/s41565-021-00931-2. [DOI] [PubMed] [Google Scholar]
- 253.Rao L., Xia S., Xu W., Tian R., Yu G., Gu C., Pan P., Meng Q.F., Cai X., Qu D., et al. Decoy nanoparticles protect against COVID-19 by concurrently adsorbing viruses and inflammatory cytokines. Proc. Natl Acad Sci USA. 2020;117:27141–27147. doi: 10.1073/pnas.2014352117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Munagala R., Aqil F., Jeyabalan J., Agrawal A.K., Mudd A.M., Kyakulaga A.H., Singh I.P., Vadhanam M.V., Gupta R.C. Exosomal formulation of anthocyanidins against multiple cancer types. Cancer Lett. 2017;393:94–102. doi: 10.1016/j.canlet.2017.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Tran P.H.L., Wang T., Yin W., Tran T.T.D., Nguyen T.N.G., Lee B.-J., Duan W. Aspirin-loaded nanoexosomes as cancer therapeutics. Int. J. Pharm. 2019;572:118786. doi: 10.1016/j.ijpharm.2019.118786. [DOI] [PubMed] [Google Scholar]
- 256.Zhuang M., Du D., Pu L., Song H., Deng M., Long Q., Yin X., Wang Y., Rao L. Spion-decorated exosome delivered bay55-9837 targeting the pancreas through magnetism to improve the blood glc response. Small. 2019;15:1903135. doi: 10.1002/smll.201903135. [DOI] [PubMed] [Google Scholar]
- 257.Gao Z.S., Zhang C.J., Xia N., Tian H., Li D.Y., Lin J.Q., Mei X.F., Wu C. Berberine-loaded m2 macrophage-derived exosomes for spinal cord injury therapy. Acta Biomater. 2021;126:211–223. doi: 10.1016/j.actbio.2021.03.018. [DOI] [PubMed] [Google Scholar]
- 258.Patel N., Kommineni N., Surapaneni S.K., Kalvala A., Yaun X., Gebeyehu A., Arthur P., Duke L.C., York S.B., Bagde A., et al. Cannabidiol loaded extracellular vesicles sensitize triple-negative breast cancer to doxorubicin in both in-vitro and in vivo models. Int. J. Pharm. 2021;607:120943. doi: 10.1016/j.ijpharm.2021.120943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Zhang X., Liu L., Tang M., Li H., Guo X., Yang X. The effects of umbilical cord-derived macrophage exosomes loaded with cisplatin on the growth and drug resistance of ovarian cancer cells. Drug Dev. Ind. Pharm. 2020;46:1150–1162. doi: 10.1080/03639045.2020.1776320. [DOI] [PubMed] [Google Scholar]
- 260.He R., Jiang Y., Shi Y., Liang J., Zhao L. Curcumin-laden exosomes target ischemic brain tissue and alleviate cerebral ischemia-reperfusion injury by inhibiting ros-mediated mitochondrial apoptosis. Mater. Sci. Eng. C. 2020;117:111314. doi: 10.1016/j.msec.2020.111314. [DOI] [PubMed] [Google Scholar]
- 261.Wang H., Sui H., Zheng Y., Jiang Y., Shi Y., Liang J., Zhao L. Curcumin-primed exosomes potently ameliorate cognitive function in ad mice by inhibiting hyperphosphorylation of the tau protein through the akt/gsk-3β pathway. Nanoscale. 2019;11:7481–7496. doi: 10.1039/C9NR01255A. [DOI] [PubMed] [Google Scholar]
- 262.Qiu B., Xu X., Yi P., Hao Y. Curcumin reinforces msc-derived exosomes in attenuating osteoarthritis via modulating the mir-124/nf-kb and mir-143/rock1/tlr9 signalling pathways. J. Cell Mol. Med. 2020;24:10855–10865. doi: 10.1111/jcmm.15714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Kang J.Y., Kim H.E., Mun D.S., Yun N.R., Joung B.Y. Curcumin-loaded extracellular vesicles endowed with heart targeting properties facilitate treatment of myocardial infarction. Eur. Heart J. 2020;41:3609. doi: 10.1093/ehjci/ehaa946.3609. [DOI] [Google Scholar]
- 264.Tian T., Zhang H.-X., He C.-P., Fan S., Zhu Y.-L., Qi C., Huang N.-P., Xiao Z.-D., Lu Z.-H., Tannous B.A., et al. Surface functionalized exosomes as targeted drug delivery vehicles for cerebral ischemia therapy. Biomaterials. 2018;150:137–149. doi: 10.1016/j.biomaterials.2017.10.012. [DOI] [PubMed] [Google Scholar]
- 265.Kim G., Lee Y., Ha J., Han S., Lee M. Engineering exosomes for pulmonary delivery of peptides and drugs to inflammatory lung cells by inhalation. J. Control. Release. 2021;330:684–695. doi: 10.1016/j.jconrel.2020.12.053. [DOI] [PubMed] [Google Scholar]
- 266.Pérez-González R., Sahoo S., Gauthier S.A., Kim Y., Li M., Kumar A., Pawlik M., Benussi L., Ghidoni R., Levy E. Neuroprotection mediated by cystatin c-loaded extracellular vesicles. Sci. Rep. 2019;9:11104. doi: 10.1038/s41598-019-47524-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Wang Y., Guo M., Lin D., Liang D., Zhao L., Zhao R., Wang Y. Docetaxel-loaded exosomes for targeting non-small cell lung cancer: Preparation and evaluation in vitro and in vivo. Drug Deliv. 2021;28:1510–1523. doi: 10.1080/10717544.2021.1951894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Cenik M., Abas B.I., Kocabiyik B., Demirbolat G.M., Cevik O. Development of a new drug delivery system from hela-derived exosomes and the effect of docetaxel-loaded exosomes on mitochondrial apoptosis. J. Pharm. Innov. 2021:1–9. doi: 10.1007/s12247-021-09566-1. [DOI] [Google Scholar]
- 269.Qu M., Lin Q., Huang L., Fu Y., Wang L., He S., Fu Y., Yang S., Zhang Z., Zhang L., et al. Dopamine-loaded blood exosomes targeted to brain for better treatment of parkinson’s disease. J. Control. Release. 2018;287:156–166. doi: 10.1016/j.jconrel.2018.08.035. [DOI] [PubMed] [Google Scholar]
- 270.Guo L., Zhang Y., Wei R., Zhang X., Wang C., Feng M. Proinflammatory macrophage-derived microvesicles exhibit tumor tropism dependent on ccl2/ccr2 signaling axis and promote drug delivery via snare-mediated membrane fusion. Theranostics. 2020;10:6581–6598. doi: 10.7150/thno.45528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Bagheri E., Abnous K., Farzad S.A., Taghdisi S.M., Ramezani M., Alibolandi M. Targeted doxorubicin-loaded mesenchymal stem cells-derived exosomes as a versatile platform for fighting against colorectal cancer. Life Sci. 2020;261:118369. doi: 10.1016/j.lfs.2020.118369. [DOI] [PubMed] [Google Scholar]
- 272.Thakur A., Sidu R.K., Zou H., Alam M.K., Yang M., Lee Y. Inhibition of glioma cells’ proliferation by doxorubicin-loaded exosomes via microfluidics. Int. J. Nanomed. 2020;15:8331–8343. doi: 10.2147/IJN.S263956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Li D., Yao S., Zhou Z., Shi J., Huang Z., Wu Z. Hyaluronan decoration of milk exosomes directs tumor-specific delivery of doxorubicin. Carbohydr. Res. 2020;493:108032. doi: 10.1016/j.carres.2020.108032. [DOI] [PubMed] [Google Scholar]
- 274.Schindler C., Collinson A., Matthews C., Pointon A., Jenkinson L., Minter R.R., Vaughan T.J., Tigue N.J. Exosomal delivery of doxorubicin enables rapid cell entry and enhanced in vitro potency. PLoS ONE. 2019;14:e0214545. doi: 10.1371/journal.pone.0214545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Wei H., Chen J., Wang S., Fu F., Zhu X., Wu C., Liu Z., Zhong G., Lin J. A nanodrug consisting of doxorubicin and exosome derived from mesenchymal stem cells for osteosarcoma treatment in vitro. Int. J. Nanomed. 2019;14:8603–8610. doi: 10.2147/IJN.S218988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Li Y., Gao Y., Gong C., Wang Z., Xia Q., Gu F., Hu C., Zhang L., Guo H., Gao S. A33 antibody-functionalized exosomes for targeted delivery of doxorubicin against colorectal cancer. Nanomedicine. 2018;14:1973–1985. doi: 10.1016/j.nano.2018.05.020. [DOI] [PubMed] [Google Scholar]
- 277.Hadla M., Palazzolo S., Corona G., Caligiuri I., Canzonieri V., Toffoli G., Rizzolio F. Exosomes increase the therapeutic index of doxorubicin in breast and ovarian cancer mouse models. Nanomedicine. 2016;11:2431–2441. doi: 10.2217/nnm-2016-0154. [DOI] [PubMed] [Google Scholar]
- 278.Li F., Zhao L., Shi Y., Liang J. Edaravone-loaded macrophage-derived exosomes enhance neuroprotection in the rat permanent middle cerebral artery occlusion model of stroke. Mol. Pharm. 2020;17:3192–3201. doi: 10.1021/acs.molpharmaceut.0c00245. [DOI] [PubMed] [Google Scholar]
- 279.Yu M., Gai C., Li Z., Ding D., Zheng J., Zhang W., Lv S., Li W. Targeted exosome-encapsulated erastin induced ferroptosis in triple negative breast cancer cells. Cancer Sci. 2019;110:3173–3182. doi: 10.1111/cas.14181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Li Y.J., Wu J.Y., Wang J.M., Hu X.B., Cai J.X., Xiang D.X. Gemcitabine loaded autologous exosomes for effective and safe chemotherapy of pancreatic cancer. Acta Biomater. 2020;101:519–530. doi: 10.1016/j.actbio.2019.10.022. [DOI] [PubMed] [Google Scholar]
- 281.Lin Q., Qu M., Zhou B., Patra H.K., Sun Z., Luo Q., Yang W., Wu Y., Zhang Y., Li L., et al. Exosome-like nanoplatform modified with targeting ligand improves anti-cancer and anti-inflammation effects of imperialine. J. Control. Release. 2019;311–312:104–116. doi: 10.1016/j.jconrel.2019.08.037. [DOI] [PubMed] [Google Scholar]
- 282.Millard M., Posty S., Piffoux M., Jasniewski J., Lassalle H.-P., Yakavets I., Gazeau F., Wilhelm C., Silva A.K.A., Bezdetnaya L. Mthpc-loaded extracellular vesicles significantly improve mthpc diffusion and photodynamic activity in preclinical models. Pharmaceutics. 2020;12:676. doi: 10.3390/pharmaceutics12070676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Millard M., Yakavets I., Piffoux M., Brun A., Gazeau F., Guigner J.-M., Jasniewski J., Lassalle H.-P., Wilhelm C., Bezdetnaya L. Mthpc-loaded extracellular vesicles outperform liposomal and free mthpc formulations by an increased stability, drug delivery efficiency and cytotoxic effect in tridimensional model of tumors. Drug Deliv. 2018;25:1790–1801. doi: 10.1080/10717544.2018.1513609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Ye Z., Zhang T., He W., Jin H., Liu C., Yang Z., Ren J. Methotrexate-loaded extracellular vesicles functionalized with therapeutic and targeted peptides for the treatment of glioblastoma multiforme. ACS Appl. Mater. Interfaces. 2018;10:12341–12350. doi: 10.1021/acsami.7b18135. [DOI] [PubMed] [Google Scholar]
- 285.Zhu Q., Ling X., Yang Y., Zhang J., Li Q., Niu X., Hu G., Chen B., Li H., Wang Y., et al. Embryonic stem cells-derived exosomes endowed with targeting properties as chemotherapeutics delivery vehicles for glioblastoma therapy. Adv. Sci. 2019;6:1801899. doi: 10.1002/advs.201801899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Melzer C., Rehn V., Yang Y., Bähre H., von der Ohe J., Hass R. Taxol-loaded msc-derived exosomes provide a therapeutic vehicle to target metastatic breast cancer and other carcinoma cells. Cancers. 2019;11:798. doi: 10.3390/cancers11060798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Coccè V., Franzè S., Brini A.T., Giannì A.B., Pascucci L., Ciusani E., Alessandri G., Farronato G., Cavicchini L., Sordi V., et al. In vitro anticancer activity of extracellular vesicles (evs) secreted by gingival mesenchymal stromal cells primed with paclitaxel. Pharmaceutics. 2019;11:61. doi: 10.3390/pharmaceutics11020061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Brini A.T., Coccè V., Ferreira L.M.J., Giannasi C., Cossellu G., Giannì A.B., Angiero F., Bonomi A., Pascucci L., Falchetti M.L., et al. Cell-mediated drug delivery by gingival interdental papilla mesenchymal stromal cells (ginpa-mscs) loaded with paclitaxel. Expert Opin. Drug Deliv. 2016;13:789–798. doi: 10.1517/17425247.2016.1167037. [DOI] [PubMed] [Google Scholar]
- 289.Kim M.S., Haney M.J., Zhao Y., Yuan D., Deygen I., Klyachko N.L., Kabanov A.V., Batrakova E.V. Engineering macrophage-derived exosomes for targeted paclitaxel delivery to pulmonary metastases: In vitro and in vivo evaluations. Nanomedicine. 2018;14:195–204. doi: 10.1016/j.nano.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 290.Agrawal A.K., Aqil F., Jeyabalan J., Spencer W.A., Beck J., Gachuki B.W., Alhakeem S.S., Oben K., Munagala R., Bondada S., et al. Milk-derived exosomes for oral delivery of paclitaxel. Nanomedicine. 2017;13:1627–1636. doi: 10.1016/j.nano.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 291.Petrella F., Coccè V., Masia C., Milani M., Salè E.O., Alessandri G., Parati E., Sisto F., Pentimalli F., Brini A.T., et al. Paclitaxel-releasing mesenchymal stromal cells inhibit in vitro proliferation of human mesothelioma cells. Biomed. Pharm. 2017;87:755–758. doi: 10.1016/j.biopha.2017.01.118. [DOI] [PubMed] [Google Scholar]
- 292.Kim M.S., Haney M.J., Zhao Y., Mahajan V., Deygen I., Klyachko N.L., Inskoe E., Piroyan A., Sokolsky M., Okolie O., et al. Development of exosome-encapsulated paclitaxel to overcome mdr in cancer cells. Nanomed. Nanotechnol. Biol. Med. 2016;12:655–664. doi: 10.1016/j.nano.2015.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Garofalo M., Villa A., Rizzi N., Kuryk L., Rinner B., Cerullo V., Yliperttula M., Mazzaferro V., Ciana P. Extracellular vesicles enhance the targeted delivery of immunogenic oncolytic adenovirus and paclitaxel in immunocompetent mice. J. Control. Release. 2019;294:165–175. doi: 10.1016/j.jconrel.2018.12.022. [DOI] [PubMed] [Google Scholar]
- 294.Gao J., Wang S., Wang Z. High yield, scalable and remotely drug-loaded neutrophil-derived extracellular vesicles (evs) for anti-inflammation therapy. Biomaterials. 2017;135:62–73. doi: 10.1016/j.biomaterials.2017.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Qi Y., Guo L., Jiang Y., Shi Y., Sui H., Zhao L. Brain delivery of quercetin-loaded exosomes improved cognitive function in ad mice by inhibiting phosphorylated tau-mediated neurofibrillary tangles. Drug Deliv. 2020;27:745–755. doi: 10.1080/10717544.2020.1762262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Liu H., Shen M., Zhao D., Ru D., Duan Y., Ding C., Li H. The effect of triptolide-loaded exosomes on the proliferation and apoptosis of human ovarian cancer skov3 cells. Biomed. Res. Int. 2019;2019:2595801. doi: 10.1155/2019/2595801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Yang X., Xie B., Peng H., Shi G., Sreenivas B., Guo J., Wang C., He Y. Eradicating intracellular mrsa via targeted delivery of lysostaphin and vancomycin with mannose-modified exosomes. J. Control. Release. 2021;329:454–467. doi: 10.1016/j.jconrel.2020.11.045. [DOI] [PubMed] [Google Scholar]
- 298.Thomas B.L., Eldridge S.E., Nosrati B., Alvarez M., Thorup A.-S., Nalesso G., Caxaria S., Barawi A., Nicholson J.G., Perretti M., et al. Wnt3a-loaded exosomes enable cartilage repair. J. Extracell. Vesicles. 2021;10:e12088. doi: 10.1002/jev2.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Barjesteh T., Mansur S., Bao Y. Inorganic nanoparticle-loaded exosomes for biomedical applications. Molecules. 2021;26:1135. doi: 10.3390/molecules26041135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Yong T., Zhang X., Bie N., Zhang H., Zhang X., Li F., Hakeem A., Hu J., Gan L., Santos H.A., et al. Tumor exosome-based nanoparticles are efficient drug carriers for chemotherapy. Nat. Commun. 2019;10:3838. doi: 10.1038/s41467-019-11718-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Niu W., Xiao Q., Wang X., Zhu J., Li J., Liang X., Peng Y., Wu C., Lu R., Pan Y., et al. A biomimetic drug delivery system by integrating grapefruit extracellular vesicles and doxorubicin-loaded heparin-based nanoparticles for glioma therapy. Nano Lett. 2021;21:1484–1492. doi: 10.1021/acs.nanolett.0c04753. [DOI] [PubMed] [Google Scholar]
- 302.Sancho-Albero M., Encabo-Berzosa M.d.M., Beltrán-Visiedo M., Fernández-Messina L., Sebastián V., Sánchez-Madrid F., Arruebo M., Santamaría J., Martín-Duque P. Efficient encapsulation of theranostic nanoparticles in cell-derived exosomes: Leveraging the exosomal biogenesis pathway to obtain hollow gold nanoparticle-hybrids. Nanoscale. 2019;11:18825–18836. doi: 10.1039/C9NR06183E. [DOI] [PubMed] [Google Scholar]
- 303.Khongkow M., Yata T., Boonrungsiman S., Ruktanonchai U.R., Graham D., Namdee K. Surface modification of gold nanoparticles with neuron-targeted exosome for enhanced blood–brain barrier penetration. Sci. Rep. 2019;9:8278. doi: 10.1038/s41598-019-44569-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Perets N., Betzer O., Shapira R., Brenstein S., Angel A., Sadan T., Ashery U., Popovtzer R., Offen D. Golden exosomes selectively target brain pathologies in neurodegenerative and neurodevelopmental disorders. Nano Lett. 2019;19:3422–3431. doi: 10.1021/acs.nanolett.8b04148. [DOI] [PubMed] [Google Scholar]
- 305.Betzer O., Perets N., Angel A., Motiei M., Sadan T., Yadid G., Offen D., Popovtzer R. In vivo neuroimaging of exosomes using gold nanoparticles. ACS Nano. 2017;11:10883–10893. doi: 10.1021/acsnano.7b04495. [DOI] [PubMed] [Google Scholar]
- 306.Jc Bose R., Uday Kumar S., Zeng Y., Afjei R., Robinson E., Lau K., Bermudez A., Habte F., Pitteri S.J., Sinclair R., et al. Tumor cell-derived extracellular vesicle-coated nanocarriers: An efficient theranostic platform for the cancer-specific delivery of anti-mir-21 and imaging agents. ACS Nano. 2018;12:10817–10832. doi: 10.1021/acsnano.8b02587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Lee J.R., Park B.W., Kim J., Choo Y.W., Kim H.Y., Yoon J.K., Kim H., Hwang J.W., Kang M., Kwon S.P., et al. Nanovesicles derived from iron oxide nanoparticles-incorporated mesenchymal stem cells for cardiac repair. Sci. Adv. 2020;6:eaaz0952. doi: 10.1126/sciadv.aaz0952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Li X., Wang Y., Shi L., Li B., Li J., Wei Z., Lv H., Wu L., Zhang H., Yang B., et al. Magnetic targeting enhances the cutaneous wound healing effects of human mesenchymal stem cell-derived iron oxide exosomes. J. Nanobiotechnol. 2020;18:113. doi: 10.1186/s12951-020-00670-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Mulens-Arias V., Nicolás-Boluda A., Silva A.K.A., Gazeau F. Theranostic iron oxide nanoparticle cargo defines extracellular vesicle-dependent modulation of macrophage activation and migratory behavior. Adv. Biosyst. 2018;2:1800079. doi: 10.1002/adbi.201800079. [DOI] [Google Scholar]
- 310.Altanerova U., Babincova M., Babinec P., Benejova K., Jakubechova J., Altanerova V., Zduriencikova M., Repiska V., Altaner C. Human mesenchymal stem cell-derived iron oxide exosomes allow targeted ablation of tumor cells via magnetic hyperthermia. Int. J. Nanomed. 2017;12:7923–7936. doi: 10.2147/IJN.S145096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Piffoux M., Silva A.K.A., Lugagne J.-B., Hersen P., Wilhelm C., Gazeau F. Extracellular vesicle production loaded with nanoparticles and drugs in a trade-off between loading, yield and purity: Towards a personalized drug delivery system. Adv. Biosyst. 2017;1:1700044. doi: 10.1002/adbi.201700044. [DOI] [PubMed] [Google Scholar]
- 312.Xiong F., Ling X., Chen X., Chen J., Tan J., Cao W., Ge L., Ma M., Wu J. Pursuing specific chemotherapy of orthotopic breast cancer with lung metastasis from docking nanoparticles driven by bioinspired exosomes. Nano Lett. 2019;19:3256–3266. doi: 10.1021/acs.nanolett.9b00824. [DOI] [PubMed] [Google Scholar]
- 313.Lv W., Han Z., Li Y., Huang Y., Sun J., Lu X., Liu C. Exosome-coated zeolitic imidazolate framework nanoparticles for intracellular detection of ATP†. Chin. J. Chem. 2021;39:2107–2112. doi: 10.1002/cjoc.202100162. [DOI] [Google Scholar]
- 314.Cheng G., Li W., Ha L., Han X., Hao S., Wan Y., Wang Z., Dong F., Zou X., Mao Y., et al. Self-assembly of extracellular vesicle-like metal-organic framework nanoparticles for protection and intracellular delivery of biofunctional proteins. J. Am. Chem. Soc. 2018;140:7282–7291. doi: 10.1021/jacs.8b03584. [DOI] [PubMed] [Google Scholar]
- 315.Illes B., Hirschle P., Barnert S., Cauda V., Wuttke S., Engelke H. Exosome-coated metal–organic framework nanoparticles: An efficient drug delivery platform. Chem. Mater. 2017;29:8042–8046. doi: 10.1021/acs.chemmater.7b02358. [DOI] [Google Scholar]
- 316.Sancho-Albero M., Rubio-Ruiz B., Pérez-López A.M., Sebastián V., Martín-Duque P., Arruebo M., Santamaría J., Unciti-Broceta A. Cancer-derived exosomes loaded with ultrathin palladium nanosheets for targeted bioorthogonal catalysis. Nat. Catal. 2019;2:864–872. doi: 10.1038/s41929-019-0333-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Han Z., Lv W., Li Y., Chang J., Zhang W., Liu C., Sun J. Improving tumor targeting of exosomal membrane-coated polymeric nanoparticles by conjugation with aptamers. ACS Appl. Bio Mater. 2020;3:2666–2673. doi: 10.1021/acsabm.0c00181. [DOI] [PubMed] [Google Scholar]
- 318.Liu C., Zhang W., Li Y., Chang J., Tian F., Zhao F., Ma Y., Sun J. Microfluidic sonication to assemble exosome membrane-coated nanoparticles for immune evasion-mediated targeting. Nano Lett. 2019;19:7836–7844. doi: 10.1021/acs.nanolett.9b02841. [DOI] [PubMed] [Google Scholar]
- 319.Gao F., Xu L., Yang B., Fan F., Yang L. Kill the real with the fake: Eliminate intracellular staphylococcus aureus using nanoparticle coated with its extracellular vesicle membrane as active-targeting drug carrier. ACS Infect. Dis. 2019;5:218–227. doi: 10.1021/acsinfecdis.8b00212. [DOI] [PubMed] [Google Scholar]
- 320.Cao Y., Wu T., Zhang K., Meng X., Dai W., Wang D., Dong H., Zhang X. Engineered exosome-mediated near-infrared-ii region v(2)c quantum dot delivery for nucleus-target low-temperature photothermal therapy. ACS Nano. 2019;13:1499–1510. doi: 10.1021/acsnano.8b07224. [DOI] [PubMed] [Google Scholar]
- 321.Tayyaba, Rehman F.U., Shaikh S., Tanziela, Semcheddine F., Du T., Jiang H., Wang X. In situ self-assembled ag–fe3o4 nanoclusters in exosomes for cancer diagnosis. J. Mater. Chem. B. 2020;8:2845–2855. doi: 10.1039/C9TB02610J. [DOI] [PubMed] [Google Scholar]
- 322.Jia G., Han Y., An Y., Ding Y., He C., Wang X., Tang Q. Nrp-1 targeted and cargo-loaded exosomes facilitate simultaneous imaging and therapy of glioma in vitro and in vivo. Biomaterials. 2018;178:302–316. doi: 10.1016/j.biomaterials.2018.06.029. [DOI] [PubMed] [Google Scholar]
- 323.Qi H., Liu C., Long L., Ren Y., Zhang S., Chang X., Qian X., Jia H., Zhao J., Sun J., et al. Blood exosomes endowed with magnetic and targeting properties for cancer therapy. ACS Nano. 2016;10:3323–3333. doi: 10.1021/acsnano.5b06939. [DOI] [PubMed] [Google Scholar]
- 324.Dumontel B., Susa F., Limongi T., Canta M., Racca L., Chiodoni A., Garino N., Chiabotto G., Centomo M.L., Pignochino Y., et al. Zno nanocrystals shuttled by extracellular vesicles as effective trojan nano-horses against cancer cells. Nanomedicine. 2019;14:2815–2833. doi: 10.2217/nnm-2019-0231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325.Hill A.F. Extracellular vesicles and neurodegenerative diseases. J. Neurosci. 2019;39:9269–9273. doi: 10.1523/JNEUROSCI.0147-18.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Yuan Q., Li X.-D., Zhang S.-M., Wang H.-W., Wang Y.-L. Extracellular vesicles in neurodegenerative diseases: Insights and new perspectives. Genes Dis. 2021;8:124–132. doi: 10.1016/j.gendis.2019.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Umwali Y., Yue C.B., Gabriel A.N.A., Zhang Y., Zhang X. Roles of exosomes in diagnosis and treatment of colorectal cancer. World J. Clin. Cases. 2021;9:4467–4479. doi: 10.12998/wjcc.v9.i18.4467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Zheng X., Hermann D.M., Bähr M., Doeppner T.R. The role of small extracellular vesicles in cerebral and myocardial ischemia—molecular signals, treatment targets, and future clinical translation. Stem Cells. 2021;39:403–413. doi: 10.1002/stem.3329. [DOI] [PubMed] [Google Scholar]
- 329.Jin Q., Wu P., Zhou X., Qian H., Xu W. Extracellular vesicles: Novel roles in neurological disorders. Stem Cells Int. 2021;2021:6640836. doi: 10.1155/2021/6640836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Bruno S., Chiabotto G., Camussi G. Extracellular vesicles: A therapeutic option for liver fibrosis. Int. J. Mol. Sci. 2020;21:4255. doi: 10.3390/ijms21124255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Ruan S., Greenberg Z., Pan X., Zhuang P., Erwin N., He M. Extracellular vesicles as an advanced delivery biomaterial for precision cancer immunotherapy. Adv. Healthc. Mater. 2021:2100650. doi: 10.1002/adhm.202100650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Massaro C., Sgueglia G., Frattolillo V., Baglio S.R., Altucci L., Dell’Aversana C. Extracellular vesicle-based nucleic acid delivery: Current advances and future perspectives in cancer therapeutic strategies. Pharmaceutics. 2020;12:980. doi: 10.3390/pharmaceutics12100980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 333.Haraszti R.A., Miller R., Didiot M.C., Biscans A., Alterman J.F., Hassler M.R., Roux L., Echeverria D., Sapp E., DiFiglia M., et al. Optimized cholesterol-sirna chemistry improves productive loading onto extracellular vesicles. Mol. Ther. 2018;26:1973–1982. doi: 10.1016/j.ymthe.2018.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.O’Loughlin A.J., Mäger I., de Jong O.G., Varela M.A., Schiffelers R.M., El Andaloussi S., Wood M.J.A., Vader P. Functional delivery of lipid-conjugated sirna by extracellular vesicles. Mol. Ther. 2017;25:1580–1587. doi: 10.1016/j.ymthe.2017.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Kanada M., Kim B.D., Hardy J.W., Ronald J.A., Bachmann M.H., Bernard M.P., Perez G.I., Zarea A.A., Ge T.J., Withrow A., et al. Microvesicle-mediated delivery of minicircle DNA results in effective gene-directed enzyme prodrug cancer therapy. Mol. Cancer Ther. 2019;18:2331–2342. doi: 10.1158/1535-7163.MCT-19-0299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Ito T., Sugiura K., Hasegawa A., Ouchi W., Yoshimoto T., Mizoguchi I., Inaba T., Hamada K., Eriguchi M., Koyama Y. Microbial antigen-presenting extracellular vesicles derived from genetically modified tumor cells promote antitumor activity of dendritic cells. Pharmaceutics. 2021;13:57. doi: 10.3390/pharmaceutics13010057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Dave K.M., Zhao W., Hoover C., D’Souza A., Manickam D.S. Extracellular vesicles derived from a human brain endothelial cell line increase cellular atp levels. AAPS PharmSciTech. 2021;22:18. doi: 10.1208/s12249-020-01892-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Haney M.J., Klyachko N.L., Harrison E.B., Zhao Y., Kabanov A.V., Batrakova E.V. Tpp1 delivery to lysosomes with extracellular vesicles and their enhanced brain distribution in the animal model of batten disease. Adv. Healthc. Mater. 2019;8:1801271. doi: 10.1002/adhm.201801271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Usman W.M., Pham T.C., Kwok Y.Y., Vu L.T., Ma V., Peng B., Chan Y.S., Wei L., Chin S.M., Azad A., et al. Efficient rna drug delivery using red blood cell extracellular vesicles. Nat. Commun. 2018;9:2359. doi: 10.1038/s41467-018-04791-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 340.Li D., Huang S., Zhu J., Hu T., Han Z., Zhang S., Zhao J., Chen F., Lei P. Exosomes from mir-21-5p-increased neurons play a role in neuroprotection by suppressing rab11a-mediated neuronal autophagy in vitro after traumatic brain injury. Med. Sci. Monit. 2019;25:1871–1885. doi: 10.12659/MSM.915727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Pomatto M.A.C., Bussolati B., D’Antico S., Ghiotto S., Tetta C., Brizzi M.F., Camussi G. Improved loading of plasma-derived extracellular vesicles to encapsulate antitumor mirnas. Mol. Ther. Methods Clin. Dev. 2019;13:133–144. doi: 10.1016/j.omtm.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Xie C., Du L.Y., Guo F., Li X., Cheng B. Exosomes derived from microrna-101-3p-overexpressing human bone marrow mesenchymal stem cells suppress oral cancer cell proliferation, invasion, and migration. Mol. Cell Biochem. 2019;458:11–26. doi: 10.1007/s11010-019-03526-7. [DOI] [PubMed] [Google Scholar]
- 343.Yang J., Zhang X., Chen X., Wang L., Yang G. Exosome mediated delivery of mir-124 promotes neurogenesis after ischemia. Mol. Ther. Nucleic. Acids. 2017;7:278–287. doi: 10.1016/j.omtn.2017.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Baldari S., Di Rocco G., Magenta A., Picozza M., Toietta G. Extracellular vesicles-encapsulated microrna-125b produced in genetically modified mesenchymal stromal cells inhibits hepatocellular carcinoma cell proliferation. Cells. 2019;8:1560. doi: 10.3390/cells8121560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Liu T., Zhang X., Du L., Wang Y., Liu X., Tian H., Wang L., Li P., Zhao Y., Duan W., et al. Exosome-transmitted mir-128-3p increase chemosensitivity of oxaliplatin-resistant colorectal cancer. Mol. Cancer. 2019;18:43. doi: 10.1186/s12943-019-0981-7. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 346.Zou X., Yuan M., Zhang T., Wei H., Xu S., Jiang N., Zheng N., Wu Z. Extracellular vesicles expressing a single-chain variable fragment of an hiv-1 specific antibody selectively target env(+) tissues. Theranostics. 2019;9:5657–5671. doi: 10.7150/thno.33925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Ding Y., Cao F., Sun H., Wang Y., Liu S., Wu Y., Cui Q., Mei W., Li F. Exosomes derived from human umbilical cord mesenchymal stromal cells deliver exogenous mir-145-5p to inhibit pancreatic ductal adenocarcinoma progression. Cancer Lett. 2019;442:351–361. doi: 10.1016/j.canlet.2018.10.039. [DOI] [PubMed] [Google Scholar]
- 348.Wu H., Fan H., Shou Z., Xu M., Chen Q., Ai C., Dong Y., Liu Y., Nan Z., Wang Y., et al. Extracellular vesicles containing mir-146a attenuate experimental colitis by targeting traf6 and irak1. Int. Immunopharmacol. 2019;68:204–212. doi: 10.1016/j.intimp.2018.12.043. [DOI] [PubMed] [Google Scholar]
- 349.Fang S.B., Zhang H.Y., Wang C., He B.X., Liu X.Q., Meng X.C., Peng Y.Q., Xu Z.B., Fan X.L., Wu Z.J., et al. Small extracellular vesicles derived from human mesenchymal stromal cells prevent group 2 innate lymphoid cell-dominant allergic airway inflammation through delivery of mir-146a-5p. J. Extracell Vesicles. 2020;9:1723260. doi: 10.1080/20013078.2020.1723260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Yuan L., Liu Y., Qu Y., Liu L., Li H. Exosomes derived from microrna-148b-3p-overexpressing human umbilical cord mesenchymal stem cells restrain breast cancer progression. Front. Oncol. 2019;9:1076. doi: 10.3389/fonc.2019.01076. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 351.Yu L., Gui S., Liu Y., Qiu X., Zhang G., Zhang X.a., Pan J., Fan J., Qi S., Qiu B. Exosomes derived from microrna-199a-overexpressing mesenchymal stem cells inhibit glioma progression by down-regulating agap2. Aging (Albany NY) 2019;11:5300–5318. doi: 10.18632/aging.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352.Ma X., Wang J., Li J., Ma C., Chen S., Lei W., Yang Y., Liu S., Bihl J., Chen C. Loading mir-210 in endothelial progenitor cells derived exosomes boosts their beneficial effects on hypoxia/reoxygeneation-injured human endothelial cells via protecting mitochondrial function. Cell Physiol. Biochem. 2018;46:664–675. doi: 10.1159/000488635. [DOI] [PubMed] [Google Scholar]
- 353.Wang N., Chen C., Yang D., Liao Q., Luo H., Wang X., Zhou F., Yang X., Yang J., Zeng C., et al. Mesenchymal stem cells-derived extracellular vesicles, via mir-210, improve infarcted cardiac function by promotion of angiogenesis. Biochim. Biophys. Acta Mol. Basis Dis. 2017;1863:2085–2092. doi: 10.1016/j.bbadis.2017.02.023. [DOI] [PubMed] [Google Scholar]
- 354.Rong Y., Zhang J., Jiang D., Ji C., Liu W., Wang J., Ge X., Tang P., Yu S., Cui W., et al. Hypoxic pretreatment of small extracellular vesicles mediates cartilage repair in osteoarthritis by delivering mir-216a-5p. Acta Biomater. 2021;122:325–342. doi: 10.1016/j.actbio.2020.12.034. [DOI] [PubMed] [Google Scholar]
- 355.Li X., Liu L.L., Yao J.L., Wang K., Ai H. Human umbilical cord mesenchymal stem cell-derived extracellular vesicles inhibit endometrial cancer cell proliferation and migration through delivery of exogenous mir-302a. Stem Cells Int. 2019;2019:8108576. doi: 10.1155/2019/8108576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Zhou Y., Yamamoto Y., Takeshita F., Yamamoto T., Xiao Z., Ochiya T. Delivery of mir-424-5p via extracellular vesicles promotes the apoptosis of mda-mb-231 tnbc cells in the tumor microenvironment. Int. J. Mol. Sci. 2021;22:844. doi: 10.3390/ijms22020844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Jeong K., Yu Y.J., You J.Y., Rhee W.J., Kim J.A. Exosome-mediated microrna-497 delivery for anti-cancer therapy in a microfluidic 3d lung cancer model. Lab. A Chip. 2020;20:548–557. doi: 10.1039/C9LC00958B. [DOI] [PubMed] [Google Scholar]
- 358.Han M., Hu J., Lu P., Cao H., Yu C., Li X., Qian X., Yang X., Yang Y., Han N., et al. Exosome-transmitted mir-567 reverses trastuzumab resistance by inhibiting atg5 in breast cancer. Cell Death Dis. 2020;11:43. doi: 10.1038/s41419-020-2250-5. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 359.Rodrigues-Junior D.M., Pelarin M.F.A., Nader H.B., Vettore A.L., Pinhal M.A.S. Microrna-1252-5p associated with extracellular vesicles enhances bortezomib sensitivity in multiple myeloma cells by targeting heparanase. Onco Targets Ther. 2021;14:455–467. doi: 10.2147/OTT.S286751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Song Y., Zhang C., Zhang J., Jiao Z., Dong N., Wang G., Wang Z., Wang L. Localized injection of mirna-21-enriched extracellular vesicles effectively restores cardiac function after myocardial infarction. Theranostics. 2019;9:2346–2360. doi: 10.7150/thno.29945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Nie H., Xie X., Zhang D., Zhou Y., Li B., Li F., Li F., Cheng Y., Mei H., Meng H., et al. Use of lung-specific exosomes for mirna-126 delivery in non-small cell lung cancer. Nanoscale. 2020;12:877–887. doi: 10.1039/C9NR09011H. [DOI] [PubMed] [Google Scholar]
- 362.Bhaskaran V., Nowicki M.O., Idriss M., Jimenez M.A., Lugli G., Hayes J.L., Mahmoud A.B., Zane R.E., Passaro C., Ligon K.L., et al. The functional synergism of microrna clustering provides therapeutically relevant epigenetic interference in glioblastoma. Nat. Commun. 2019;10:442. doi: 10.1038/s41467-019-08390-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Kim R., Lee S., Lee J., Kim M., Kim W.J., Lee H.W., Lee M.Y., Kim J., Chang W. Exosomes derived from microrna-584 transfected mesenchymal stem cells: Novel alternative therapeutic vehicles for cancer therapy. BMB Rep. 2018;51:406–411. doi: 10.5483/BMBRep.2018.51.8.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364.Tsai S.-J., Guo C., Atai N.A., Gould S.J. Exosome-mediated mrna delivery for SARS-CoV-2 vaccination. bioRxiv. 2020;297:2020-11. doi: 10.1101/2020.11.06.371419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Kojima R., Bojar D., Rizzi G., Hamri G.C.-E., El-Baba M.D., Saxena P., Ausländer S., Tan K.R., Fussenegger M. Designer exosomes produced by implanted cells intracerebrally deliver therapeutic cargo for parkinson’s disease treatment. Nat. Commun. 2018;9:1305. doi: 10.1038/s41467-018-03733-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Erkan E.P., Senfter D., Madlener S., Jungwirth G., Ströbel T., Saydam N., Saydam O. Extracellular vesicle-mediated suicide mrna/protein delivery inhibits glioblastoma tumor growth in vivo. Cancer Gene Ther. 2017;24:38–44. doi: 10.1038/cgt.2016.78. [DOI] [PubMed] [Google Scholar]
- 367.Forterre A.V., Wang J.H., Delcayre A., Kim K., Green C., Pegram M.D., Jeffrey S.S., Matin A.C. Extracellular vesicle-mediated in vitro transcribed mrna delivery for treatment of her2(+) breast cancer xenografts in mice by prodrug cb1954 without general toxicity. Mol. Cancer Ther. 2020;19:858–867. doi: 10.1158/1535-7163.MCT-19-0928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Yang Z., Shi J., Xie J., Wang Y., Sun J., Liu T., Zhao Y., Zhao X., Wang X., Ma Y., et al. Large-scale generation of functional mrna-encapsulating exosomes via cellular nanoporation. Nat. Biomed. Eng. 2020;4:69–83. doi: 10.1038/s41551-019-0485-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Tabak S., Feinshtein V., Schreiber-Avissar S., Beit-Yannai E. Non-pigmented ciliary epithelium-derived extracellular vesicles loaded with smad7 sirna attenuate wnt signaling in trabecular meshwork cells in vitro. Pharmaceuticals. 2021;14:858. doi: 10.3390/ph14090858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370.Zhao L., Gu C., Gan Y., Shao L., Chen H., Zhu H. Exosome-mediated sirna delivery to suppress postoperative breast cancer metastasis. J. Control. Release. 2020;318:1–15. doi: 10.1016/j.jconrel.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 371.Zhang Q., Zhang H., Ning T., Liu D., Deng T., Liu R., Bai M., Zhu K., Li J., Fan Q., et al. Exosome-delivered c-met sirna could reverse chemoresistance to cisplatin in gastric cancer. Int. J. Nanomed. 2020;15:2323–2335. doi: 10.2147/IJN.S231214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Zhang H., Wang Y., Bai M., Wang J., Zhu K., Liu R., Ge S., Li J., Ning T., Deng T., et al. Exosomes serve as nanoparticles to suppress tumor growth and angiogenesis in gastric cancer by delivering hepatocyte growth factor sirna. Cancer Sci. 2018;109:629–641. doi: 10.1111/cas.13488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Didiot M.C., Hall L.M., Coles A.H., Haraszti R.A., Godinho B.M., Chase K., Sapp E., Ly S., Alterman J.F., Hassler M.R., et al. Exosome-mediated delivery of hydrophobically modified sirna for huntingtin mrna silencing. Mol. Ther. 2016;24:1836–1847. doi: 10.1038/mt.2016.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Shokrollahi E., Nourazarian A., Rahbarghazi R., Salimi L., Karbasforush S., Khaksar M., Salarinasab S., Abhari A., Heidarzadeh M. Treatment of human neuroblastoma cell line sh-sy5y with hsp27 sirna tagged-exosomes decreased differentiation rate into mature neurons. J. Cell Physiol. 2019;234:21005–21013. doi: 10.1002/jcp.28704. [DOI] [PubMed] [Google Scholar]
- 375.Ju Z., Ma J., Wang C., Yu J., Qiao Y., Hei F. Exosomes from ipscs delivering sirna attenuate intracellular adhesion molecule-1 expression and neutrophils adhesion in pulmonary microvascular endothelial cells. Inflammation. 2017;40:486–496. doi: 10.1007/s10753-016-0494-0. [DOI] [PubMed] [Google Scholar]
- 376.Zhou Y., Yuan Y., Liu M., Hu X., Quan Y., Chen X. Tumor-specific delivery of kras sirna with irgd-exosomes efficiently inhibits tumor growth. ExRNA. 2019;1:28. doi: 10.1186/s41544-019-0034-9. [DOI] [Google Scholar]
- 377.Liao K., Niu F., Dagur R.S., He M., Tian C., Hu G. Int.ranasal delivery of lincrna-cox2 sirna loaded extracellular vesicles decreases lipopolysaccharide-induced microglial proliferation in mice. J. Neuroimmune Pharm. 2020;15:390–399. doi: 10.1007/s11481-019-09864-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378.Guo S., Perets N., Betzer O., Ben-Shaul S., Sheinin A., Michaelevski I., Popovtzer R., Offen D., Levenberg S. Intranasal delivery of mesenchymal stem cell derived exosomes loaded with phosphatase and tensin homolog sirna repairs complete spinal cord injury. ACS Nano. 2019;13:10015–10028. doi: 10.1021/acsnano.9b01892. [DOI] [PubMed] [Google Scholar]
- 379.Tang T.T., Wang B., Li Z.L., Wen Y., Feng S.T., Wu M., Liu D., Cao J.Y., Yin Q., Yin D., et al. Kim-1 targeted extracellular vesicles: A new therapeutic platform for rnai to treat aki. J. Am. Soc. Nephrol. 2021;32:2467–2483. doi: 10.1681/ASN.2020111561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Kim H., Mun D., Kang J.Y., Lee S.H., Yun N., Joung B. Improved cardiac-specific delivery of rage sirna within small extracellular vesicles engineered to express intense cardiac targeting peptide attenuates myocarditis. Mol. Ther. Nucleic Acids. 2021;24:1024–1032. doi: 10.1016/j.omtn.2021.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Li H., Yang C., Shi Y., Zhao L. Exosomes derived from sirna against grp78 modified bone-marrow-derived mesenchymal stem cells suppress sorafenib resistance in hepatocellular carcinoma. J. Nanobiotechnol. 2018;16:103. doi: 10.1186/s12951-018-0429-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Aqil F., Munagala R., Jeyabalan J., Agrawal A.K., Kyakulaga A.-H., Wilcher S.A., Gupta R.C. Milk exosomes—Natural nanoparticles for sirna delivery. Cancer Lett. 2019;449:186–195. doi: 10.1016/j.canlet.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 383.Reshke R., Taylor J.A., Savard A., Guo H., Rhym L.H., Kowalski P.S., Trung M.T., Campbell C., Little W., Anderson D.G., et al. Reduction of the therapeutic dose of silencing rna by packaging it in extracellular vesicles via a pre-microrna backbone. Nat. Biomed. Eng. 2020;4:52–68. doi: 10.1038/s41551-019-0502-4. [DOI] [PubMed] [Google Scholar]
- 384.Dong L., Ding C., Zheng T., Pu Y., Liu J., Zhang W., Xue F., Kang P., Ma Y., Wang X., et al. Extracellular vesicles from human umbilical cord mesenchymal stem cells treated with sirna against elfn1-as1 suppress colon adenocarcinoma proliferation and migration. Am. J. Transl Res. 2019;11:6989–6999. [PMC free article] [PubMed] [Google Scholar]
- 385.Kamerkar S., LeBleu V.S., Sugimoto H., Yang S., Ruivo C.F., Melo S.A., Lee J.J., Kalluri R. Exosomes facilitate therapeutic targeting of oncogenic kras in pancreatic cancer. Nature. 2017;546:498–503. doi: 10.1038/nature22341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Wang C., Chen L., Huang Y., Li K., Jinye A., Fan T., Zhao R., Xia X., Shen B., Du J., et al. Exosome-delivered trpp2 sirna inhibits the epithelial-mesenchymal transition of fadu cells. Oncol. Lett. 2019;17:1953–1961. doi: 10.3892/ol.2018.9752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387.Yang T., Fogarty B., LaForge B., Aziz S., Pham T., Lai L., Bai S. Delivery of small interfering rna to inhibit vascular endothelial growth factor in zebrafish using natural brain endothelia cell-secreted exosome nanovesicles for the treatment of brain cancer. AAPS. J. 2017;19:475–486. doi: 10.1208/s12248-016-0015-y. [DOI] [PubMed] [Google Scholar]
- 388.Anticoli S., Manfredi F., Chiozzini C., Arenaccio C., Olivetta E., Ferrantelli F., Capocefalo A., Falcone E., Ruggieri A., Federico M. An exosome-based vaccine platform imparts cytotoxic t lymphocyte immunity against viral antigens. Biotechnol. J. 2018;13:e1700443. doi: 10.1002/biot.201700443. [DOI] [PubMed] [Google Scholar]
- 389.Daraee H., Etemadi A., Kouhi M., Alimirzalu S., Akbarzadeh A. Application of liposomes in medicine and drug delivery. Artif. Cells Nanomed. Biotechnol. 2016;44:381–391. doi: 10.3109/21691401.2014.953633. [DOI] [PubMed] [Google Scholar]
- 390.Sabanovic B., Piva F., Cecati M., Giulietti M. Promising extracellular vesicle-based vaccines against viruses, including SARS-CoV-2. Biology. 2021;10:94. doi: 10.3390/biology10020094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Zhang C., Maruggi G., Shan H., Li J. Advances in mrna vaccines for infectious diseases. Front. Immunol. 2019;10:594. doi: 10.3389/fimmu.2019.00594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Baden L.R., El Sahly H.M., Essink B., Kotloff K., Frey S., Novak R., Diemert D., Spector S.A., Rouphael N., Creech C.B., et al. Efficacy and safety of the mrna-1273 SARS-CoV-2 vaccine. N. Engl. J. Med. 2020;384:403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data presented in this manuscript is available from corresponding author upon reseanable requests.