Abstract
Recent years have witnessed major progress in development of novel therapeutic agents such as chemotherapy, targeted therapy and immune checkpoint inhibitors for breast cancer. However, cancer-related death remains high especially in triple-negative breast cancer (TNBC) due limited therapeutic options. Development of targeted therapies for TNBC requires better understanding of biology and signaling networks that promote disease progression. Fascin, an actin bundling protein, was identified as a key regulator of many signaling pathways that contribute to breast cancer progression. Herein, fascin ShRNA was used to generate stable fascin knockdown (FSCN1KD) in the MDA-MB-231 TNBC cell line and then were subjected to comprehensive mRNA and miRNA transcriptome analysis. We identified 129 upregulated and 114 downregulated mRNA transcripts, while 14 miRNAs were differentially expressed in FSCN1KD. Ingenuity pathway analysis (IPA) was used to predict the impact of differentially expressed transcripts on signaling pathways and functional categories and to construct miRNA-mRNA regulatory networks in the context of FSCN1 knockdown. Compared to FSCN1KD, fascin-positive (FSCN1CON) breast cancer cells showed enrichment in genes promoting cellular proliferation, migration, survival, DNA replication and repair. Expression of FSCN1high (identified in BRCA dataset from TCGA) in conjunction with elevated expression of the top 10 upregulated or decreased expression of the top 10 downregulated genes (identified in our FSCN1CON vs. FSCN1KD) correlates with worst survival outcome. Taken together, these data confirmed fascin’s role in promoting TNBC progression, and identified a novel opportunity for therapeutic interventions via targeting those FSCN1-related transcripts.
Keywords: fascin, breast cancer, miRNA, pathway analysis, transcriptome, IPA
1. Introduction
Breast cancer is the most common cancer in women worldwide and is the leading cause of cancer-related mortality in women. Overall and disease-free survival of breast cancer patients were both improved by the early detection and introduction of targeted therapy and immune checkpoint inhibitors in combination with conventional treatment modalities [1]. Nonetheless, breast cancer-related death remains high mainly due to drug resistance and metastasis [2], thus stressing the need for better understanding of breast cancer biology to develop more effective targeted therapies. Triple-negative breast cancer (TNBC) accounts for 12–20% of all breast cancer subtypes [3]. Compared to other breast cancer subtypes, TNBC has the most aggressive behavior with high recurrence rate and worst outcome [4]. This has been mainly attributed to limited therapeutic options due to lack of biomarkers or valid treatment targets. Therefore, identification of biomarkers or signaling pathways that are differentially enriched in TNBC could potentially expand our knowledge and accelerate therapeutic development with the aim to hinder or slow the disease progression.
Fascin is an actin bundling protein with high expression in the filopodia, critical cell protrusions at the leading edge of migrating cells [5]. Moreover, it was reported to regulate adhesion and filopodia formation in migrating cancer cells [6]. Inhibition of fascin using RNA interference reduced the number of filopodia and disrupted the organization of the actin bundles [7,8]. Fascin expression is induced in many transformed epithelial cells including breast, and its expression level is considered a biomarker of worst clinical outcome [9,10,11,12]. Fascin expression was reported in high percentage (87.8%) of TNBC as compared to the other breast cancer subtypes [13] and thus has been proposed as a diagnostic marker for TNBC and potential therapeutic target [13,14,15]. Most importantly, fascin inhibitors were shown to block TNBC metastasis in tumor metastasis mouse model [16,17,18] and to reduce the growth of specific TNBC, which express high levels of epidermal growth factor receptor [18,19]. We have previously reported a crucial role for fascin in regulating drug resistance [20] and metastasis [9] and have identified several underlying mechanisms that have contributed in this process [21,22,23]. More inclusive studies are needed to identify enriched molecular signature in fascin-positive TNBC for potential therapeutic targeting.
Comprehensive transcriptomic studies that compare differentially expressed transcripts upon manipulation of fascin expression in TNBC is expected to expand our understanding of the underlying mechanisms of fascin contribution to breast cancer progression, which eventually will stimulate therapeutic target development. Herein, we carried a comprehensive transcriptome analysis on fascin knockdown TNBC cell line (MDA-MB-231) in comparison to their fascin-expressing counterparts. Results from our fascin knockdown cells showed enrichment of genes that promoted disease progression in fascin-positive breast cancer cells. Collectively, this study provides more comprehensive understanding of the oncogenic role of fascin and its effectors, which might represent valuable tumor biomarkers and therapeutic targets for TNBC. Therefore, targeting of signaling pathways that are enriched in fascin-positive breast cancer may provide a novel therapeutic window for halting the disease progression, especially in light of the limited therapeutic options for TNBC.
2. Results
2.1. FSCN1 Is Enriched with Prognostic Markers of Poor Survival
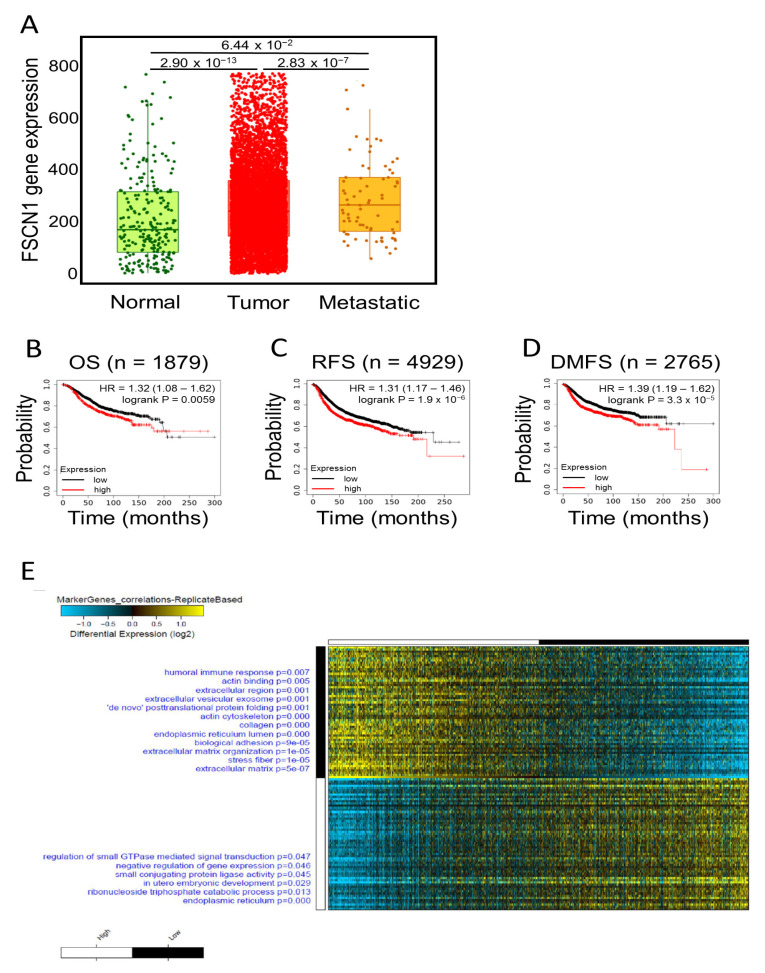
We have previously reported a critical role for fascin in regulating breast cancer chemoresistance, resulting in poor survival [20]. Subsequently, we delineated some underlying mechanism that promote fascin contribution in poor survival [21,22]. Here we aimed to define novel genes that are enriched in fascin-positive breast cancer cells and contribute in the disease progression. A large cohort of breast cancer patients from the publicly available Kaplan–Meier plotter portal dataset [24] was used to assess fascin expression and its impact on overall survival (OS; n = 1879), recurrence-free survival (RFS; n = 4929) and distant metastasis-free survival (DMFS; n = 2764). Remarkable increase in fascin expression was observed in the breast cancer cohort (n = 7569) compared to samples from the normal group (n = 242) (Figure 1A). Furthermore, metastatic patients (n = 82) exhibited higher expression of fascin as compared to the normal group. Concordantly, FSCN1high breast cancer patients showed the worst OS, RFS and DMFS as compared to FSCN1low group (Figure 1B–D). Importantly, the power of significance (p value) between FSCN1high and FSCN1low groups increased from 0.0059 in OS to 1.9 × 10−6 and 3.3 × 10−5 for RFS and DMFS, respectively. These data emphasize the role of fascin not only in predicting the OS, but its contribution to RFS and DMFS, making it useful biomarker for assessing the prognosis of the disease.
Figure 1.
Expression, survival and differential gene expression in FSCN1high compared to FSCN1low breast cancer patients from TCGA dataset. (A) Boxplot showing fascin expression in normal (n = 242), tumor (n = 7569) and metastatic (n = 82) breast cancer patients. Kaplan-Meier plots showing (B) overall survival (OS; n = 1879), (C) recurrence-free survival (RFS; n = 4929) and (D) distant metastasis-free survival (DMFS; n = 2765) as function of median FSCN1 expression in breast cancer patients. The significance between FSCN1high and FSCN1low groups was calculated using the log-rank test. p-values are indicated on each plot. (E) Marker discovery analysis to identify putative markers selectively expressed in FSCN1high (n = 534) vs. FSCN1low (n = 545) stratified according to median FSCN1 expression from TCGA BRCA dataset (n = 1217). Enriched gene ontology (GO) associations are indicated on the y axis.
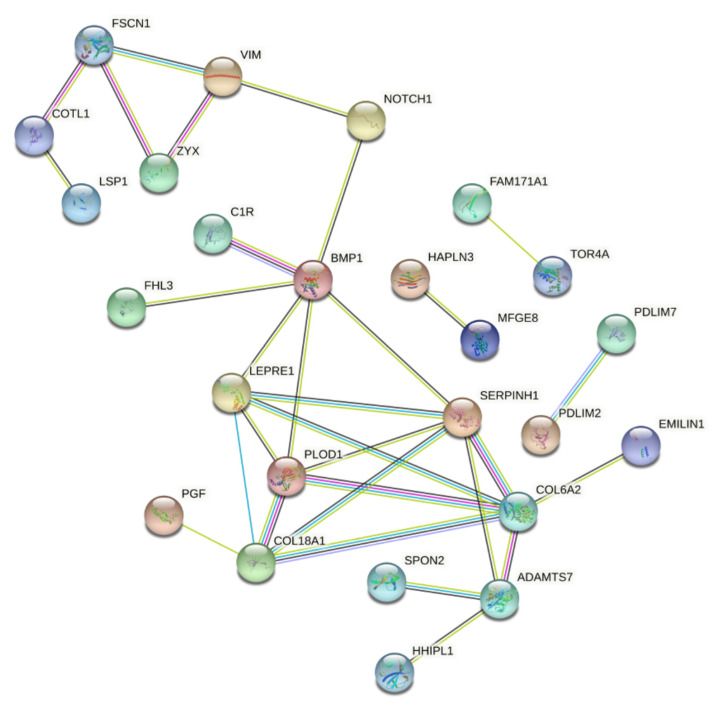
To identify putative markers that are selectively associated with high fascin expression, we have used the publicly available breast cancer patients’ gene expression dataset from The Cancer Genome Atlas (TCGA; n = 1217). These data were subjected to marker discovery analysis comparing FSCN1high (n = 534) vs. FSCN1low (n = 545). FSCN1high group showed enrichment in genes that are involved in regulating many cellular processes such as the extracellular matrix organization, stress fibers, biological adhesion, actin binding and posttranslational protein folding (Figure 1E). On the contrary, FSCN1low group showed enrichment of genes that are involved in regulation of other cellular process such as small GTPase mediated signal transduction, negative regulation of gene expression and endoplasmic reticulum. The top 60 enriched genes in FSCN1high vs. FSCN1low breast cancer patients from TCGA dataset were then subjected for network analysis using AltAnalyze software to construct protein-protein interaction. These data showed nodes with evidence of protein-protein interaction (Figure 2). Some of the enriched (such as VIM and NOTCH1) and reduced (such as ESR) genes in FSCN1high groups are consistent with our previous results [9,23]. These data establish that the level of fascin expression in breast cancer samples is associated with differentially expressed genes that regulate key cellular process and promote disease progression.
Figure 2.
Protein-protein interaction network in FSCN1high compared to FSCN1low BRCA. Constructed protein-protein interaction network of 60 enriched genes in FSCN1high (n = 534) vs. FSCN1low (n = 545) breast cancer patients from TCGA dataset. Nodes represent proteins and different line intensities denote the type of evidence for the interaction. Statistical analysis results for the network: number of nodes: 59, number of edges: 28; average node degree: 0.94; average local clustering coefficient: 0.26; expected number of edges: 7; PPI enrichment p-value = 5.7–10.
2.2. Differential Genes Enrichment in FSCN1 Breast Cancer Cells
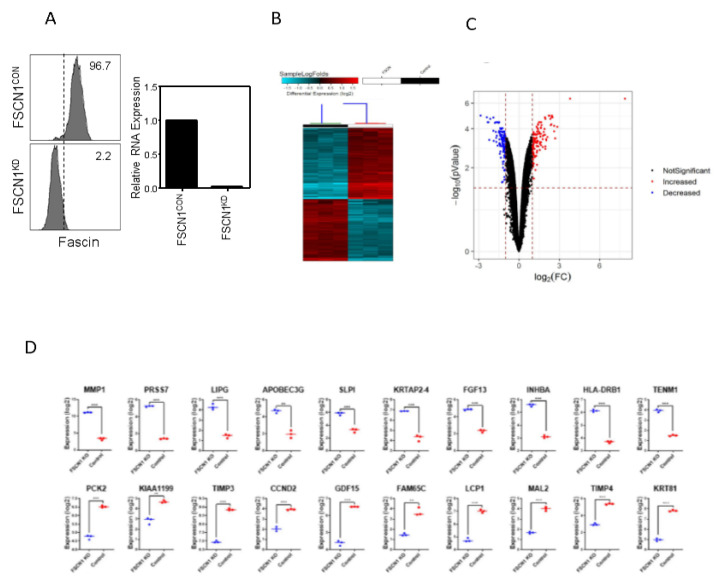
To provide mechanistic insight into the role of FSCN1 in promoting TNBC progression, stable fascin knockdown MDA-MB-231 TNBC model [23] was used to characterize the alterations in gene expression and signaling networks. Fascin-positive (FSCN1CON) and -negative (FSCN1KD) cells (Figure 3A) were subjected for comparative transcriptome analysis. Hierarchical clustering and volcano plot based on differentially expressed RNA transcripts showed clear clustering of (FSCN1CON) from (FSCN1KD) breast cancer cells (Figure 3B,C).
Figure 3.
Differential gene expression analysis on FSCN1KD compared to FSCN1CON MDA-MB-231 cells. (A) Left: FACS histograms showing the levels of fascin expression in FSCN1CON and FSCN1KD MDA-MB-231 cells. Right: Bar graph showing the relative RNA expression of fascin in FSCN1CON and FSCN1KD MDA-MB-231 cells. (B) Heatmap depicting the relative expression levels of differentially expressed genes in FSCN1KD compared to FSCN1CON MDA-MB-231 cells. Each column represents one replica, and each row represents a single transcript. The expression level of each transcript in a single sample is depicted according to the color scale. (C) Volcano plot representation of significantly altered genes in FSCN1KD compared to FSCN1CON MDA-MB-231 cells. Red and blue colors indicate the genes with significantly increased or decreased expression, respectively. Black color indicates no significant change. (D) Expression of top 10 upregulated and top 10 downregulated transcripts in FSCN1KD compared to FSCN1CON MDA-MB-231 cells based on microarray data (n = 3). ** p < 0.005, *** p < 0.0005.
Based on −2.0 ≥ FC ≥ 2.0 with significant value (p < 0.05), 129 upregulated and 114 downregulated transcripts were identified (Table S1). Figure 3D shows expression of top 10 upregulated and top 10 downregulated transcripts in FSCN1KD compared to FSCN1CON MDA-MB-231 cells based on microarray data. We subsequently used TCGA dataset to assess the prognostic value of FSCN1KD-derived gene signature on the survival of all breast cancer subtypes or TNBC patients. Interestingly, FSCN1high in conjunction with high expression of the top 10 upregulated genes (identified in our FSCN1CON MDA-MB-231 cells) significantly correlates with poor RFS survival in all breast cancer subtypes (Figure 4A).
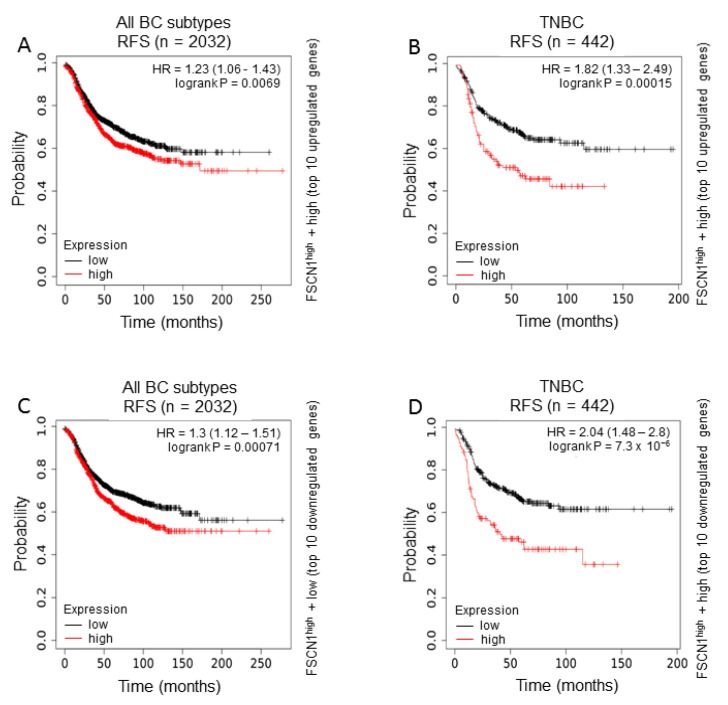
Figure 4.
Effect of the differentially identified genes in MDA-MB-231 breast cancer cells on survival of FSCN1high compared to FSCN1low breast cancer patients from TCGA dataset. Kaplan-Meier plots from TCGA dataset showing survival of (A,C) all breast cancer subtypes (RFS; n = 2032) or (B,D) TNBC subtype (RFS; n = 442). Survival of FSCN1high in conjunction with (A,B) high expression of the top 10 upregulated genes or (C,D) low expression of the top 10 downregulated genes identified in FSCN1CON MDA-MB-231 cells. The significance between FSCN1high and FSCN1low groups was calculated using the log-rank test. p-values are indicated on each plot.
This correlation become more pronounced in TNBC subtype than all subtypes combined as reflected by the increase in hazard ratio from 1.23 to 1.82 and the power of significance (p value) from 0.0069 to 0.00015 (Figure 4B). Similarly, FSCN1high in conjunction with low expression of the top 10 downregulated genes (identified in our FSCN1CON MDA-MB-231 cells) significantly correlates with poor RFS survival in all breast cancer subtypes (Figure 4C). This correlation become more pronounced in TNBC subtype than all subtypes combined as reflected by the increase in hazard ratio from 1.3 to 2.04 and the power of significance (p value) from 0.00071 to 7.3 × 10−6 (Figure 4D). The poor RFS of FSCN1high patients with the differentially expressed genes that become more significant in TNBC subtype demonstrated a clinical relevance to our in vitro findings. Collectively, these data suggest that fascin co-expression with these genes could serve as prognostic biomarkers for breast cancer.
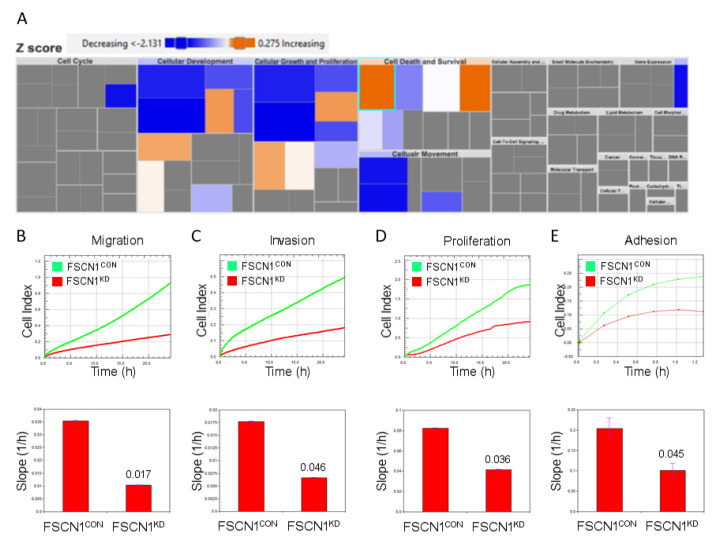
2.3. Mechanistic Network Analysis Predicts Activation of Cell Proliferation and Survival Networks in FSCN1CON Breast Cancer
To gain insight into the putative effect of fascin clustering with the differentially expressed genes on downstream biological activities and functions, we have subjected differentially expressed genes in FSCN1CON vs. FSCN1KD to IPA analysis. Figure 5A showed rectangles with different color code, dimension and intensity that indicate a family of associated biological functions or diseases. The rectangle dimension indicates the associated functions that are predicted to be most significantly affected. The color intensity indicates higher absolute Z-scores, where blue and orange reflects decrease and increase, respectively. Functional categories associated with cellular movement and invasion as well as cell growth and proliferation were enriched, while those associated with cellular development as well as cell death and survival were diminished in FSCN1CON cells. In agreement with those data, in vitro live assays showed reduced migration, invasion, proliferation, and adhesion in our FSCN1KD breast cancer cells (Figure 5B–E). Further upstream regulator analysis using IPA showed activated GLI1, CBX5 and TRIB3 (Figure 5F) and suppressed EZH2 and ATF4 (Figure 5G) networks in FSCN1KD breast cancer cells. Collectively, these data demonstrated association between the differentially regulated transcripts in FSCN1KD compared to FSCN1CON MDA-MB-231 cells and increase in cell proliferation, migration, while the cell death-associated functional categories were suppressed.
Figure 5.
Effector analysis of differentially regulated gene transcripts in FSCN1KD MDA-MB-231 breast cancer cells. (A) Tree map (hierarchical heat map) depicting affected functional categories based on differentially expressed genes in FSCN1KD compared to FSCN1CON MDA-MB-231 cells where the major boxes represent a category of diseases and functions. Each colored rectangle is a particular biological function or disease and the color range indicates its predicted activation state—increasing (orange) or decreasing (blue). Darker colors indicate higher absolute Z-scores. In this default view, the size of the rectangles is correlated with increasing overlap significance. Live cell assays showing migration (B), invasion (C), proliferation (D) and adhesion to collagen IV (E) in FSCN1KD compared to FSCN1CON MDA-MB-231 cells. Results in B-E are the mean of triplicates ± SD and are representative of three independent experiments. Upstream regulator analysis depicted activated GLI1, CBX5 and TRIB3 (F) and suppressed EZH2 and ATF4 (G) networks based on IPA analysis of data in Table S1.
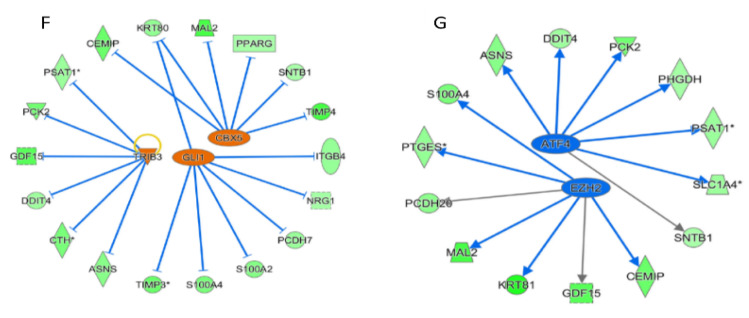
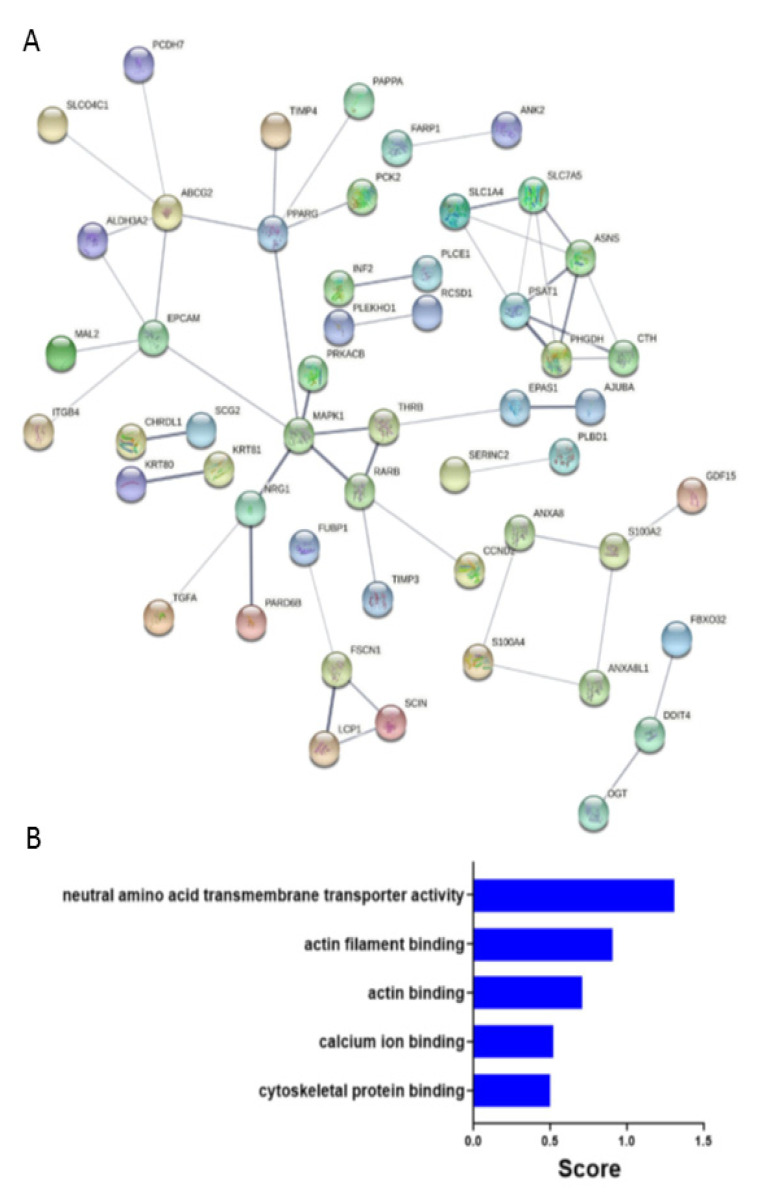
2.4. Predicated Protein-Protein Interaction Network in FSCN1CON Breast Cancer
We subjected the 93 downregulated genes in FSCN1KD compared to FSCN1CON MDA-MB-231 cells to construct protein-protein interaction network using STRING. Result analysis of the network based on statistical difference identified 88 nodes (Figure 6A).
Figure 6.
Protein-protein interaction network and gene ontology (GO) enrichment. (A) Constructed protein-protein interaction network of 93 downregulated genes in FSCN1KD compared to FSCN1CON MDA-MB-231 cells. Nodes represent proteins and different line intensities denote the type of evidence for the interaction. Statistical analysis results for the network: number of nodes: 88, number of edges: 49; average node degree: 1.1; average local clustering coefficient: 0.44; expected number of edges: 31; PPI enrichment p-value =0.001. (B) GO enrichment bar chart of downregulated genes in FSCN1KD compared to FSCN1CON MDA-MB-231 cells showing most enriched GO terms.
MAPK1, EPCAM, and ABCG2 are examples of some of the key nodes that were identified and are found to be relevant for the disease progression [25,26,27]. Indeed, gene ontology enrichment bar chart of downregulated genes in FSCN1KD compared to FSCN1CON MDA-MB-231 cells showing most enriched GO categories that are related to neutral amino acid transmembrane transport activity, actin and cytoskeletal binding, and calcium ion binding (Figure 6B). Altogether, these data suggest an active role for fascin in regulating a number of key PPI networks and functional categories promoting tumorigenesis.
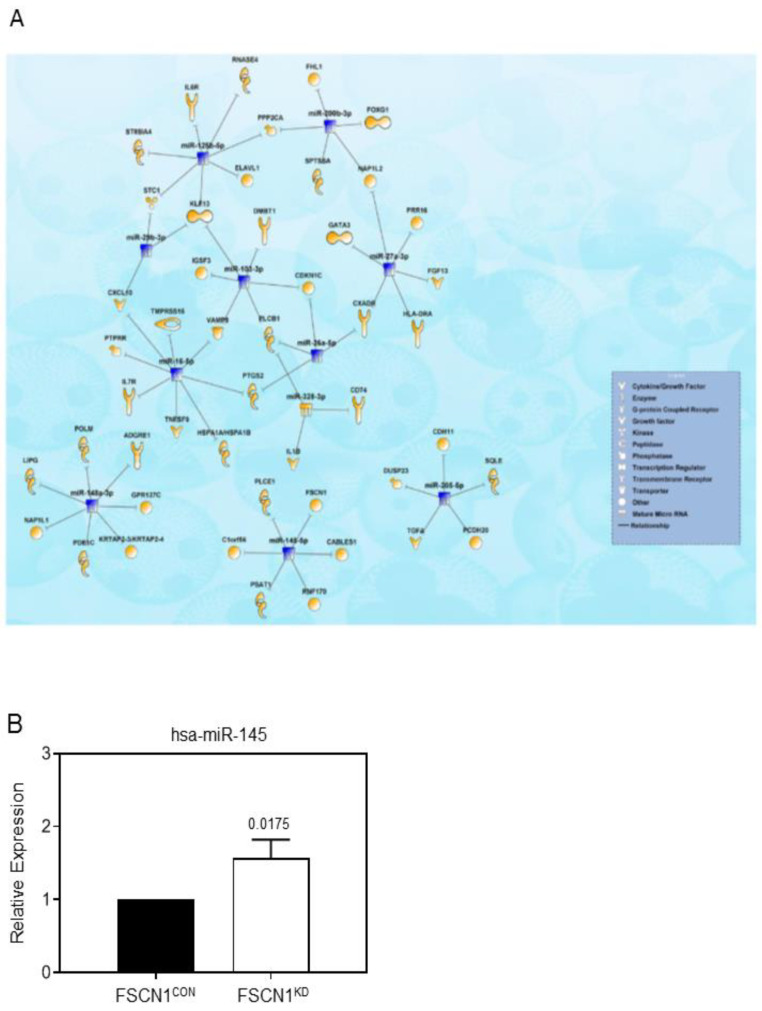
To gain more insight into the molecular mechanisms by which fascin regulates breast cancer progression, we performed microRNA array analysis of FSCN1KD compared to FSCN1CON MDA-MB-231 cells. We identified 2 upregulated and 12 downregulated miRNAs (2.0-fold change, p < 0.05, Table S2) in FSCN1KD cells, which subsequently were subjected to IPA microRNA target filter analysis utilizing both miRNA and mRNA data. Data presented in Figure 7A illustrates miRNA-mRNA networks based on transcriptomic data from the FSCN1KD and FSCN1CON models. The interaction network is illustrated as mature miRNA (presented as nodes) and biological relationships, which are displayed using different shapes representing the functional class of the target gene as illustrated in the corresponding legend (Figure 7A). We have confirmed the differential expression of hsa-miR-145 miRNA following fascin knockdown in our MDA-MB-231 breast cancer cells. FSCN1KD cells express increased levels of hsa-miR-145, indicating an inverse relationship between hsa-miR-145 and FSCN1 expression (Figure 7B). In addition to the hsa-miR-145-FSCN1 network, IPA analysis revealed regulation of several genes belonging to different functional categories, including cytokines, enzymes, growth factors, transporters, transcription regulators. Altogether, these differentially regulated miRNAs are indicative of breast cancer-related functional categories with more confidence and high level of predicted relationship.
Figure 7.
Network Analysis illustrating the interactions between differentially expressed miRNAs and mRNAs in FSCN1KD MDA-MB-231 breast cancer cells. (A) Network illustrating the interaction between differentially expressed miRNAs and mRNAs in FSCN1KD MDA-MB-231 based on IPA microRNA target filter analysis. (B) Bar graph showing relative RNA expression of hsa-miR-145 in FSCN1KD compared to FSCN1CON MDA-MB-231 cells.
3. Discussion
Breast cancer is a heterogeneous disease that can be classified into four major subtypes: luminal A, luminal B, HER+, and TNBC. Luminal subtypes, especially luminal A, have the best prognosis and survival outcome mainly due to the availability of endocrine therapies [28]. On the contrary, TNBC are the most aggressive subtype with the worst survival outcome mainly due limited alternative therapeutic options [29,30]. In this study, we identified the transcriptional landscape enriched in TNBC expressing high fascin, which is associated with shorter survival of FSCN1high patients particularly the TNBC subtype, demonstrating a clinical relevance of our in vitro findings in this breast cancer subtype.
Fascin knockdown in MDA-MB-231 TNBC model reveal a number of differentially expressed transcripts (129 upregulated and 114 downregulated). Some of the enriched transcripts in our FSCN1CON breast cancer cells are in high concordances with those that are found in FSCN1high group of the publicly available TCGA database. The fact that proteins identified based on differential gene expression from TCGA dataset are from breast cancer patients, which include various cell types, while those identified from FSCN1KD are from cell line data may explain this inconsistency between the two lists. The decrease in ESR and the increase in NOTCH1 and VIM that was observed in FSCN1high group of BCRA cohort from the TCGA database are in line with our previous results, which demonstrated promotion of NOTCH1 and VIM by fascin [9,23]. Most importantly, the association between the differentially expressed genes in FSCN1high and increase in functional categories related to cellular movement, invasion, growth and proliferation as well as decrease in those related to cellular development, death and survival is consistent with oncogenic roles of fascin that were demonstrated in previous studies [9,21,22,23].
The finding of increased expression of KIAA1199 [31], GDF15 [32] and KRT81 [33] in our FSCN1CON compared to FSCN1KD TNBC is consistent with its over-expression in this breast cancer subtype and promotion of their migration. Enrichment of CCND2 in TNBC especially post neoadjuvant chemotherapy [34] is consistent with its increased expression in our FSCN1CON. Similarly, the over-expression of MAL2 in TNBC and its contribution to immune evasion and poorer survival [35] supports our finding of increased expression of MAL2 in FSCN1CON. The elevated level of TIMP4 in early stage estrogen receptor-negative breast cancer and association with poorer clinical outcome [36] is consistent with the finding of increased expression of TIMP4 in FSCN1CON. On the other hand, the decreased expression of APOBEC3G in our FSCN1CON compared to FSCN1KD is consistent with positive correlation between its increased expression and favorable prognosis in TNBC [37]. In addition, the decreased expression of KRTAP2-4 in FSCN1CON is consistent with its downregulation by miRNA-200c in TNBC to promote metastasis and reduce survival [38]. There is association between high expression of HLA-DRB1 with increased tumor-infiltrating lymphocytes and therapeutic response in TNBC [39] consistent with its reduced expression in our FSCN1CON. No known function for TENM-1 in TNBC, but if it serves a tumor suppressor role like what has been suggested for TENM2 in various type of tumors [40] then that is consistent with the decreased expression in our FSCN1CON. To large extent, our transcriptome data fit well with the oncogenic role of fascin in TNBC, further supports its use as a prognostic marker in this subtype and shed light on the pathway that could be used for therapeutic targeting.
Deregulated expression of miRNAs has been implicated in regulating many diseases including cancer. For example, miRNA-145 is under-expressed in various tumors including breast and is considered to be a tumor suppressor gene due to its inhibitory effect on tumor cell proliferation, invasion, and metastasis [41]. High miRNA-145 expression has also been reported to increase tumor cell sensitivity to chemotherapy. Importantly, miRNA-145 was reported to target fascin and inhibit metastasis or invasion in many cancer types including colorectal [42], nasopharyngeal [43], gastric [44] and non-small-cell lung cancer [45]. Our findings of repressed miRNA-145, increased migration, invasion, proliferation and adhesion in our FSCN1CON TNBC may explain the poor prognosis and shorter survival. The expression level of miRNA-145 following treatment of TNBC with fascin inhibitors has not been assessed [16,17,18], which could validate the miRNA-145 repression by fascin. miRNA-145 was also predicted to regulate several other genes in our FSCN1KD model. Similarly, the reduced expression of miRNA-205 in our FSCN1CON TNBC is consistent with previous study, where its upregulation was reported to inhibit proliferation, cell cycle progression and tumor growth [46]. The increase expression of the onco-suppressor miRNA-424 in our FSCN1CON TNBC is consistent with its association with aggressive state including advanced clinical stage, tumor size and distance metastases [47]. The increase expression of miRNA-200c in our FSCN1CON TNBC is consistent with its role in promoting migration and invasiveness of TNBC [48]. Moreover, the increase expression of miRNA-27b in our fascin expressing TNBC is consistent with its role in regulating migration and association with poor clinical outcome [49]. Of the differentially regulated miRNAs upon fascin knockdown in TNBC, miRNA-145, miRNA-205, miRNA-424, miRNA-200c, miRNA-27b may explain the aggressive behavior of fascin-expressing TNBC. The remaining identified miRNA-mRNA networks in the FSCN1KD model and their plausible role in driving TNBC progression warrants further investigation.
We previously have delineated many of the underlying mechanisms of fascin regulation of key signaling pathways that promote cancer progression such as AKT, NF-kB, [9], FAK [20], NOTCH1 [23], ITGB1 [22] and CTNNB [21]. However, fascin involvement in regulating many other signaling pathways remained largely unexplored and the results reported in this study should stimulate further investigations toward this direction. For example, one could speculate that fascin, via its actin bundling activity, may act as scaffold to promote or suppress complex formation between interacting partners. While the exact mechanism of fascin regulation of the differentially expressed transcripts in this study are not elucidated, these findings shed lights on the oncogenic effect of fascin in promoting disease progression particularly in TNBC via modulating other biomarkers and signaling pathways. Therefore, targeting fascin or its associated network may present a novel therapeutic window as single or in combination with other treatment modalities for better clinical outcome.
4. Materials and Methods
4.1. Cells
The human triple-negative breast cancer (TNBC) cell line MDA-MB-231 (HTB-26) was purchased from ATCC (Manassas, VA, USA) and were maintained in DMEM supplemented with 10% fetal bovine serum (Invitrogen, Paisley, UK), 200 mM L-glutamine (Invitrogen) and antibiotic-antimycotic liquid (Invitrogen) at 37 °C in a 5% CO2 humidified atmosphere.
4.2. Fascin Knockdown
Stable fascin knockdown in MDA-MB-231 cells were generated as previously described [9]. Briefly, lentiviral vectors (Thermo Scientific, Paisley, UK) expressing either fascin shRNA (clone Id: TRCN0000123039; sequence TTCCAGTTTGAAAGGCAAGGG) or scrambled shRNA were used to generate fascin knockdown (FSCN1KD) or control (FSCN1CON) MDA-MB-231 cells, respectively. Fascin knockdown was confirmed using flow cytometery and western blot.
4.3. Differential Gene Expression Analysis
Total RNA was extracted from FSCN1KD or FSCN1CON cells using QIAGEN RNeasy Mini Kit (QIAGEN, Valencia, CA, USA) following the manufacturer’s instructions. Integrity of the extracted RNA was determined using the Agilent Bioanalyzer 2100 system (Agilent Technologies, Santa Clara, CA, USA) before the cDNA synthesis using High Capacity RNA-to-cDNA Kit (Applied Biosystems, Paisley, UK). The cDNA was then subjected for global gene transcription using GeneChip (Affymetrix, Santa Clara, CA, USA), where generated fluorescent oligonucleotide probes were hybridized to the GeneChips® Human Genome HG-U133 Array in a GeneChip® hybridization oven as per the manufacturer’s instructions. This array has around 55,000 probe sets, which represent over 39,000 transcripts from 33,000 previously identified human genes. Gene Array scanner (Affymetrix) was used for visualization and GeneChip® Operating Software was utilized for image quantitation.
4.4. Microarray Data Analysis
Microarray expression data from FSCN1KD vs FSCN1CON MDA-MB-231 cells were then subjected to quantile normalization and differential analysis and hierarchical clustering as described before [50]. Transcripts exhibiting −2.0 ≥ FC ≥ 2.0 and p < 0.05 were considered significant and were used for Ingenuity Pathway Analysis (IPA) analysis. Volcano plots were generated using R studio Version 1.2.5001.
4.5. qRT-PCR for Mature MicroRNAs and Bioinformatics Analysis
Total RNA was isolated from FSCN1KD vs FSCN1CON MDA-MB-231 cells as above and qRT-PCR for mature miRNA was run using miScript miRNA PCR Array Human Breast Cancer-MIHS-109Z (Qiagen, Hilden, Germany) as previously described [51]. This miRNA PCR Array Panel contains 84 mature miRNAs that are most relevant to breast cancer tumorigenesis and all qPCR reactions were run in duplicate. The relative expression of a given miRNA was assessed by computing 2(−ddCt) (2(−ΔΔCt)). The miRNA targets and the biological pathways they were involved in were predicted using IPA microRNA filter as previously described [52].
4.6. Ingenuity Pathways Analysis (IPA)
Differentially expressed genes from the microarray data (2.0 FC, p < 0.05 Adj) were imported into the IPA Software (Ingenuity Systems Inc., Germantown, MD, USA) as we previously described [53]. Functional regulatory networks and canonical pathways were determined using upstream regulator analysis (URA), downstream effects analysis (DEA), mechanistic networks (MN), and casual network analysis (CNA) prediction algorithms. Disease and function analysis were used to identify the disease and functional categories affected by FSCN1 depletion based on alteration in transcriptome data. The biological functions assigned to each network are ranked according to the significance of that biological function to the network [54].
4.7. BRCA TCGA Data Analysis
Gene expression data from BRCA TCGA data were retrieved from Xena Browser (https://xenabrowser.net/ accessed on 1 June 2021). Patients were divided into high and low according to median FSCN1 expression. Expression data were then subjected to the marker finder algorithm as described before [50,55].
4.8. Protein-Protein Interaction (PPI) Network
PPI network and Gene ontology (GO) analysis were conducted on FSCN1high as well as genes downregulated in MDA-MB-231 FSCN1KD model using STRING database https://string-db.org/ (accessed on 1 June 2021) as described before [56].
4.9. Survival Analysis of Human Breast Tumor Microarray Datasets
Breast cancer survival data were downloaded in accordance with Kaplan–Meier plotter portal Access Policies and were assessed using the Kaplan–Meier plotter portal website (https://kmplot.com/analysis/ accessed on 1 September 2021) [24] as previously described [21]. Briefly, the different genes in the tumor samples were categorized into high and low expression, and the survival curves of samples with high and low gene expression were compared by log-rank test.
4.10. Live Cell Assays
Quantitative kinetic measurements of cell migration, invasion, proliferation and adhesion assays were performed using CIM-plate 16 on xCELLigence Real Time Cell Analysis instrument, from ACEA Biosciences Inc. (San Diego, CA, USA) as previously described [21,22]. The xCELLigence software was used to acquire data and calculate the average migration, invasion, proliferation, and adhesion to collagen IV of all the replicates by increases in the slope (1/h) of the curve during 24 h. Graph displaying change in the slope between the different groups was generated.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ph14121228/s1, Table S1. List of differentially expressed mRNA transcripts in FSCN1 knockdown vs control MDA-MB-231 cells (2.0 FC, p-value < 0.05). Table S2. List of differentially expressed miRNAs in FSCN1 knockdown vs control MDA-MB-231 cells (2.0 FC, p-value < 0.05).
Author Contributions
R.B., S.A.-K.: performed the in vitro experiments and analyzed some of the data. S.M.: performed the transcriptome profiling. A.Q.: performed miRNA profiling. T.B.: performed all kmplot patient survival analysis. M.F.: obtained fund for SA and provided materials support. H.G.: performed some data interpretation and edited the manuscript. N.M.A.: performed all the transcriptome and miRNA data analysis and interpretation and edited the manuscript. M.A.-A.: conceived and designed the experiments, analyzed the data and wrote the paper. All authors have read and agreed to the published version of the manuscript.
Funding
This work was approved and supported by King Faisal Specialist Hospital and Research Centre (Research Advisory Council, RAC# 2190 008 and 2170 003). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Processed data are provided as supplementary tables.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Balduzzi A., Bagnardi V., Rotmensz N., Dellapasqua S., Montagna E., Cardillo A., Viale G., Veronesi P., Intra M., Luini A., et al. Survival Outcomes in Breast Cancer Patients with Low Estrogen/Progesterone Receptor Expression. Clin. Breast Cancer. 2013;14:258–264. doi: 10.1016/j.clbc.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 2.Dellapasqua S., Bagnardi V., Balduzzi A., Iorfida M., Rotmensz N., Santillo B., Viale G., Ghisini R., Veronesi P., Luini A., et al. Outcomes of patients with breast cancer who present with ipsilateral supraclavicular or internal mammary lymph node metastases. Clin. Breast Cancer. 2014;14:53–60. doi: 10.1016/j.clbc.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 3.Wang Q., Xu M., Sun Y., Chen J., Chen C., Qian C., Chen Y., Cao L., Xu Q., Du X., et al. Gene Expression Profiling for Diagnosis of Triple-Negative Breast Cancer: A Multicenter, Retrospective Cohort Study. Front. Oncol. 2019;9:354. doi: 10.3389/fonc.2019.00354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hudis C.A., Gianni L. Triple-negative breast cancer: An unmet medical need. Oncologist. 2011;16((Suppl. 1)):1–11. doi: 10.1634/theoncologist.2011-S1-01. [DOI] [PubMed] [Google Scholar]
- 5.Faix J., Grosse R. Staying in shape with formins. Dev. Cell. 2006;10:693–706. doi: 10.1016/j.devcel.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 6.Wolff J.R., Stuke K., Missler M., Tytko H., Schwarz P., Rohlmann A., Chao T.I. Autocellular coupling by gap junctions in cultured astrocytes: A new view on cellular autoregulation during process formation. Glia. 1998;24:121–140. doi: 10.1002/(SICI)1098-1136(199809)24:1<121::AID-GLIA12>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 7.Parsons M., Adams J.C. Rac regulates the interaction of fascin with protein kinase C in cell migration. J. Cell Sci. 2008;121:2805–2813. doi: 10.1242/jcs.022509. [DOI] [PubMed] [Google Scholar]
- 8.Vignjevic D., Kojima S., Aratyn Y., Danciu O., Svitkina T., Borisy G.G. Role of fascin in filopodial protrusion. J. Cell Biol. 2006;174:863–875. doi: 10.1083/jcb.200603013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Alwan M., Olabi S., Ghebeh H., Barhoush E., Tulbah A., Al-Tweigeri T., Ajarim D., Adra C. Fascin is a key regulator of breast cancer invasion that acts via the modification of metastasis-associated molecules. PLoS ONE. 2011;6:e27339. doi: 10.1371/journal.pone.0027339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Min K.W., Chae S.W., Kim D.H., Do S.I., Kim K., Lee H.J., Sohn J.H., Pyo J.S., Kim D.H., Oh S., et al. Fascin expression predicts an aggressive clinical course in patients with advanced breast cancer. Oncol. Lett. 2015;10:121–130. doi: 10.3892/ol.2015.3191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Omran O.M., Al Sheeha M. Cytoskeletal Focal Adhesion Proteins Fascin-1 and Paxillin Are Predictors of Malignant Progression and Poor Prognosis in Human Breast Cancer. J. Environ. Pathol. Toxicol. Oncol. 2015;34:201–212. doi: 10.1615/JEnvironPatholToxicolOncol.2015013663. [DOI] [PubMed] [Google Scholar]
- 12.Yoder B.J., Tso E., Skacel M., Pettay J., Tarr S., Budd T., Tubbs R.R., Adams J.C., Hicks D.G. The expression of fascin, an actin-bundling motility protein, correlates with hormone receptor-negative breast cancer and a more aggressive clinical course. Clin. Cancer Res. 2005;11:186–192. [PubMed] [Google Scholar]
- 13.Wang C.Q., Tang C.H., Chang H.T., Li X.N., Zhao Y.M., Su C.M., Hu G.N., Zhang T., Sun X.X., Zeng Y., et al. Fascin-1 as a novel diagnostic marker of triple-negative breast cancer. Cancer Med. 2016;5:1983–1988. doi: 10.1002/cam4.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Esnakula A.K., Ricks-Santi L., Kwagyan J., Kanaan Y.M., DeWitty R.L., Wilson L.L., Gold B., Frederick W.A., Naab T.J. Strong association of fascin expression with triple negative breast cancer and basal-like phenotype in African-American women. J. Clin. Pathol. 2014;67:153–160. doi: 10.1136/jclinpath-2013-201698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsuchiya H., Sasaki A., Tsunoda Y., Takimoto M., Sawada T. Fascin is Expressed in Basal-Liketype Triple Negative Breast Cancer Associated with High Malignant Potential in Japanese Women. Int. J. Cancer Clin. Res. 2015;2:035. doi: 10.23937/2378-3419/2/5/1035. [DOI] [Google Scholar]
- 16.Chen L., Yang S., Jakoncic J., Zhang J.J., Huang X.Y. Migrastatin analogues target fascin to block tumour metastasis. Nature. 2010;464:1062–1066. doi: 10.1038/nature08978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang F.K., Han S., Xing B., Huang J., Liu B., Bordeleau F., Reinhart-King C.A., Zhang J.J., Huang X.Y. Targeted inhibition of fascin function blocks tumour invasion and metastatic colonization. Nat. Commun. 2015;6:7465. doi: 10.1038/ncomms8465. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y., Zhang J.J., Huang X.Y. Anti-Metastasis Fascin Inhibitors Decrease the Growth of Specific Subtypes of Cancers. Cancers. 2020;12:2287. doi: 10.3390/cancers12082287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang C.Q., Li Y., Huang B.F., Zhao Y.M., Yuan H., Guo D., Su C.M., Hu G.N., Wang Q., Long T., et al. EGFR conjunct FSCN1 as a Novel Therapeutic Strategy in Triple-Negative Breast Cancer. Sci. Rep. 2017;7:15654. doi: 10.1038/s41598-017-15939-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ghebeh H., Al-Khaldi S., Olabi S., Al-Dhfyan A., Al-Mohanna F., Barnawi R., Tulbah A., Al-Tweigeri T., Ajarim D., Al-Alwan M. Fascin is involved in the chemotherapeutic resistance of breast cancer cells predominantly via the PI3K/Akt pathway. Br. J. Cancer. 2014;111:1552–1561. doi: 10.1038/bjc.2014.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barnawi R., Al-Khaldi S., Bakheet T., Fallatah M., Alaiya A., Ghebeh H., Al-Alwan M. Fascin Activates beta-Catenin Signaling and Promotes Breast Cancer Stem Cell Function Mainly Through Focal Adhesion Kinase (FAK): Relation With Disease Progression. Front. Oncol. 2020;10:440. doi: 10.3389/fonc.2020.00440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barnawi R., Al-Khaldi S., Colak D., Tulbah A., Al-Tweigeri T., Fallatah M., Monies D., Ghebeh H., Al-Alwan M. beta1 Integrin is essential for fascin-mediated breast cancer stem cell function and disease progression. Int. J. Cancer. 2019;145:830–841. doi: 10.1002/ijc.32183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barnawi R., Al-Khaldi S., Majed Sleiman G., Sarkar A., Al-Dhfyan A., Al-Mohanna F., Ghebeh H., Al-Alwan M. Fascin Is Critical for the Maintenance of Breast Cancer Stem Cell Pool Predominantly via the Activation of the Notch Self-Renewal Pathway. Stem Cells. 2016;34:2799–2813. doi: 10.1002/stem.2473. [DOI] [PubMed] [Google Scholar]
- 24.Gyorffy B., Lanczky A., Eklund A.C., Denkert C., Budczies J., Li Q., Szallasi Z. An online survival analysis tool to rapidly assess the effect of 22,277 genes on breast cancer prognosis using microarray data of 1809 patients. Breast Cancer Res. Treat. 2010;123:725–731. doi: 10.1007/s10549-009-0674-9. [DOI] [PubMed] [Google Scholar]
- 25.Osta W.A., Chen Y., Mikhitarian K., Mitas M., Salem M., Hannun Y.A., Cole D.J., Gillanders W.E. EpCAM is overexpressed in breast cancer and is a potential target for breast cancer gene therapy. Cancer Res. 2004;64:5818–5824. doi: 10.1158/0008-5472.CAN-04-0754. [DOI] [PubMed] [Google Scholar]
- 26.Santen R.J., Song R.X., McPherson R., Kumar R., Adam L., Jeng M.H., Yue W. The role of mitogen-activated protein (MAP) kinase in breast cancer. J. Steroid Biochem. Mol. Biol. 2002;80:239–256. doi: 10.1016/S0960-0760(01)00189-3. [DOI] [PubMed] [Google Scholar]
- 27.Xiang L., Su P., Xia S., Liu Z., Wang Y., Gao P., Zhou G. ABCG2 is associated with HER-2 expression, lymph node metastasis and clinical stage in breast invasive ductal carcinoma. Diagn Pathol. 2011;6:90. doi: 10.1186/1746-1596-6-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vasconcelos I., Hussainzada A., Berger S., Fietze E., Linke J., Siedentopf F., Schoenegg W. The St. Gallen surrogate classification for breast cancer subtypes successfully predicts tumor presenting features, nodal involvement, recurrence patterns and disease free survival. Breast. 2016;29:181–185. doi: 10.1016/j.breast.2016.07.016. [DOI] [PubMed] [Google Scholar]
- 29.Collignon J., Lousberg L., Schroeder H., Jerusalem G. Triple-negative breast cancer: Treatment challenges and solutions. Breast Cancer (Dove Med. Press) 2016;8:93–107. doi: 10.2147/BCTT.S69488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Papadimitriou M., Mountzios G., Papadimitriou C.A. The role of PARP inhibition in triple-negative breast cancer: Unraveling the wide spectrum of synthetic lethality. Cancer Treat. Rev. 2018;67:34–44. doi: 10.1016/j.ctrv.2018.04.010. [DOI] [PubMed] [Google Scholar]
- 31.Kuscu C., Evensen N., Kim D., Hu Y.J., Zucker S., Cao J. Transcriptional and epigenetic regulation of KIAA1199 gene expression in human breast cancer. PLoS ONE. 2012;7:e44661. doi: 10.1371/journal.pone.0044661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peake B.F., Eze S.M., Yang L., Castellino R.C., Nahta R. Growth differentiation factor 15 mediates epithelial mesenchymal transition and invasion of breast cancers through IGF-1R-FoxM1 signaling. Oncotarget. 2017;8:94393–94406. doi: 10.18632/oncotarget.21765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nanashima N., Horie K., Yamada T., Shimizu T., Tsuchida S. Hair keratin KRT81 is expressed in normal and breast cancer cells and contributes to their invasiveness. Oncol. Rep. 2017;37:2964–2970. doi: 10.3892/or.2017.5564. [DOI] [PubMed] [Google Scholar]
- 34.Balko J.M., Giltnane J.M., Wang K., Schwarz L.J., Young C.D., Cook R.S., Owens P., Sanders M.E., Kuba M.G., Sanchez V., et al. Molecular profiling of the residual disease of triple-negative breast cancers after neoadjuvant chemotherapy identifies actionable therapeutic targets. Cancer Discov. 2014;4:232–245. doi: 10.1158/2159-8290.CD-13-0286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fang Y., Wang L., Wan C., Sun Y., Van der Jeught K., Zhou Z., Dong T., So K.M., Yu T., Li Y., et al. MAL2 drives immune evasion in breast cancer by suppressing tumor antigen presentation. J. Clin. Investig. 2021;13:e140837. doi: 10.1172/JCI140837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liss M., Sreedhar N., Keshgegian A., Sauter G., Chernick M.R., Prendergast G.C., Wallon U.M. Tissue inhibitor of metalloproteinase-4 is elevated in early-stage breast cancers with accelerated progression and poor clinical course. Am. J. Pathol. 2009;175:940–946. doi: 10.2353/ajpath.2009.081094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yuan Y. Modelling the spatial heterogeneity and molecular correlates of lymphocytic infiltration in triple-negative breast cancer. J. R. Soc. Interface. 2015;12:20141153. doi: 10.1098/rsif.2014.1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jin T., Suk Kim H., Ki Choi S., Hye Hwang E., Woo J., Suk Ryu H., Kim K., Moon A., Kyung Moon W. microRNA-200c/141 upregulates SerpinB2 to promote breast cancer cell metastasis and reduce patient survival. Oncotarget. 2017;8:32769–32782. doi: 10.18632/oncotarget.15680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Park I.A., Hwang S.H., Song I.H., Heo S.H., Kim Y.A., Bang W.S., Park H.S., Lee M., Gong G., Lee H.J. Expression of the MHC class II in triple-negative breast cancer is associated with tumor-infiltrating lymphocytes and interferon signaling. PLoS ONE. 2017;12:e0182786. doi: 10.1371/journal.pone.0182786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peppino G., Ruiu R., Arigoni M., Riccardo F., Iacoviello A., Barutello G., Quaglino E. Teneurins: Role in Cancer and Potential Role as Diagnostic Biomarkers and Targets for Therapy. Int. J. Mol. Sci. 2021;22:2321. doi: 10.3390/ijms22052321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sachdeva M., Mo Y.Y. miR-145-mediated suppression of cell growth, invasion and metastasis. Am. J. Transl. Res. 2010;2:170–180. [PMC free article] [PubMed] [Google Scholar]
- 42.Feng Y., Zhu J., Ou C., Deng Z., Chen M., Huang W., Li L. MicroRNA-145 inhibits tumour growth and metastasis in colorectal cancer by targeting fascin-1. Br. J. Cancer. 2014;110:2300–2309. doi: 10.1038/bjc.2014.122. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 43.Li Y.Q., He Q.M., Ren X.Y., Tang X.R., Xu Y.F., Wen X., Yang X.J., Ma J., Liu N. MiR-145 inhibits metastasis by targeting fascin actin-bundling protein 1 in nasopharyngeal carcinoma. PLoS ONE. 2015;10:e0122228. doi: 10.1371/journal.pone.0122228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xue M., Zhao L., Yang F., Li Z., Li G. MicroRNA145 inhibits the malignant phenotypes of gastric carcinoma cells via downregulation of fascin 1 expression. Mol. Med. Rep. 2016;13:1033–1039. doi: 10.3892/mmr.2015.4609. [DOI] [PubMed] [Google Scholar]
- 45.Zhang Y., Yang X., Wu H., Zhou W., Liu Z. MicroRNA-145 inhibits migration and invasion via inhibition of fascin 1 protein expression in non-small-cell lung cancer cells. Mol. Med. Rep. 2015;12:6193–6198. doi: 10.3892/mmr.2015.4163. [DOI] [PubMed] [Google Scholar]
- 46.Radojicic J., Zaravinos A., Vrekoussis T., Kafousi M., Spandidos D.A., Stathopoulos E.N. MicroRNA expression analysis in triple-negative (ER, PR and Her2/neu) breast cancer. Cell Cycle. 2011;10:507–517. doi: 10.4161/cc.10.3.14754. [DOI] [PubMed] [Google Scholar]
- 47.Wang J., Wang S., Zhou J., Qian Q. miR-424-5p regulates cell proliferation, migration and invasion by targeting doublecortin-like kinase 1 in basal-like breast cancer. Biomed. Pharmacother. 2018;102:147–152. doi: 10.1016/j.biopha.2018.03.018. [DOI] [PubMed] [Google Scholar]
- 48.Choi S.K., Kim H.S., Jin T., Hwang E.H., Jung M., Moon W.K. Overexpression of the miR-141/200c cluster promotes the migratory and invasive ability of triple-negative breast cancer cells through the activation of the FAK and PI3K/AKT signaling pathways by secreting VEGF-A. BMC Cancer. 2016;16:570. doi: 10.1186/s12885-016-2620-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu Y., Cai Q., Bao P.P., Su Y., Cai H., Wu J., Ye F., Guo X., Zheng W., Zheng Y., et al. Tumor tissue microRNA expression in association with triple-negative breast cancer outcomes. Breast Cancer Res. Treat. 2015;152:183–191. doi: 10.1007/s10549-015-3460-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Emig D., Salomonis N., Baumbach J., Lengauer T., Conklin B.R., Albrecht M. AltAnalyze and DomainGraph: Analyzing and visualizing exon expression data. Nucleic Acids Research. 2010;38:W755–W762. doi: 10.1093/nar/gkq405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Qattan A., Intabli H., Alkhayal W., Eltabache C., Tweigieri T., Amer S.B. Robust expression of tumor suppressor miRNA’s let-7 and miR-195 detected in plasma of Saudi female breast cancer patients. BMC Cancer. 2017;17:799. doi: 10.1186/s12885-017-3776-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shaath H., Toor S.M., Nada M.A., Elkord E., Alajez N.M. Integrated whole transcriptome and small RNA analysis revealed multiple regulatory networks in colorectal cancer. Sci. Rep. 2021;11:14456. doi: 10.1038/s41598-021-93531-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vishnubalaji R., Elango R., Al-Toub M., Manikandan M., Al-Rikabi A., Harkness L., Ditzel N., Atteya M., Hamam R., Alfayez M., et al. Neoplastic Transformation of Human Mesenchymal Stromal Cells Mediated via LIN28B. Sci. Rep. 2019;9:8101. doi: 10.1038/s41598-019-44536-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kramer A., Green J., Pollard J., Jr., Tugendreich S. Causal analysis approaches in Ingenuity Pathway Analysis. Bioinformatics. 2014;30:523–530. doi: 10.1093/bioinformatics/btt703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vishnubalaji R., Shaath H., Alajez N.M. Protein Coding and Long Noncoding RNA (lncRNA) Transcriptional Landscape in SARS-CoV-2 Infected Bronchial Epithelial Cells Highlight a Role for Interferon and Inflammatory Response. Genes. 2020;11:760. doi: 10.3390/genes11070760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Snel B., Lehmann G., Bork P., Huynen M.A. STRING: A web-server to retrieve and display the repeatedly occurring neighbourhood of a gene. Nucleic Acids Res. 2000;28:3442–3444. doi: 10.1093/nar/28.18.3442. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Processed data are provided as supplementary tables.