Abstract
Old age is associated with disease severity and poor prognosis among coronavirus disease 2019 (COVID-19) cases; however, characteristics of elderly patients with severe COVID-19 are limited. We aimed to assess the clinical characteristics and outcomes of patients hospitalized with severe COVID-19 at tertiary care centers in South Korea. This retrospective multicenter study included patients with severe COVID-19 who were admitted at seven hospitals in South Korea from 2 February 2020 to 28 February 2021. The Cox regression analyses were performed to assess factors associated with the in-hospital mortality. Of 488 patients with severe COVID-19, 318 (65.2%) were elderly (≥65 years). The older patient group had more underlying diseases and a higher severity score than the younger patient group. The older patient group had a higher in-hospital mortality rate than the younger patient group (25.5% versus 4.7%, p-value < 0.001). The in-hospital mortality risk factors among patients with severe COVID-19 included age, acute physiology and chronic health evaluation II score, presence of diabetes and chronic obstructive lung disease, high white blood cell count, low neutrophil-lymphocyte ratio and platelet count, do-not-resuscitate order, and treatment with invasive mechanical ventilation. In addition to old age, disease severity and examination results must be considered in treatment decision-making.
Keywords: aged, COVID-19, elderly
1. Introduction
Coronavirus disease 2019 (COVID-19) is primarily caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which is transmitted from person to person via close contact with an infected individual. A pandemic outbreak was declared by the World Health Organization (WHO) in March 2020 [1]. In South Korea, from 3 January 2020 to 15 November 2021, there have been 397,466 confirmed cases of COVID-19, with 3115 deaths, reported to WHO. As of 6 November 2021, a total of 79,356,440 vaccine doses have been administered [2]. Vaccination [3,4,5] is currently in place worldwide and this is expected to reduce the incidence of COVID-19, but the world is still struggling with COVID-19.
The most common underlying diseases as predictors of mortality among COVID-19 patients were hypertension, diabetes, and cardiovascular diseases [6]. In addition, PaO2/FiO2 ratio (p/F ratio) ≤ 200 mmHg, respiratory failure at admission, high neutrophil and low lymphocyte, platelet, and albumin levels, and high sequential organ failure assessment (SOFA) score are known to be associated with mortality [7,8,9]. Old age is associated with greater disease severity and poor prognosis among patients with COVID-19 [7,8,9,10].
Elderly patients with COVID-19 present with more atypical symptoms and commonly experience progression to severe COVID-19 compared with younger patients [11,12]. In addition, they have a higher in-hospital mortality rate and a longer length of hospital stay [13,14]. The higher risk of COVID-19 mortality among older people occurs because older people are more likely to have other risk factors such as underlying disease and a high frailty scale. Also, older age is independently associated with COVID-19 mortality without other risk factors [15,16]. However, data regarding the prognostic factors and characteristics of elderly patients with severe COVID-19 in a rapidly aging society are limited. Therefore, the current study aimed to assess the clinical characteristics and outcomes of patients hospitalized with severe COVID-19 at tertiary care centers in South Korea.
2. Materials and Methods
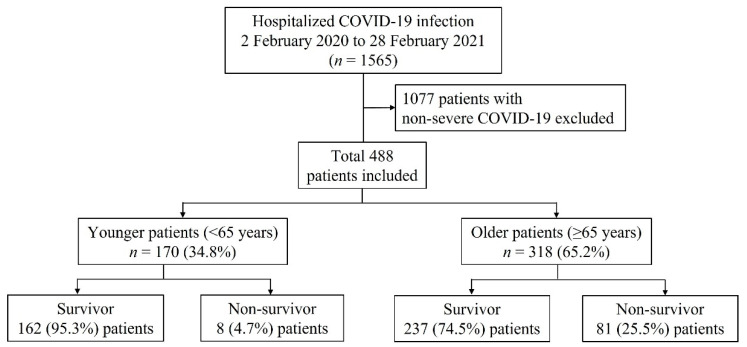
This multicenter retrospective study analyzed data collected from all patients with severe COVID-19 who were hospitalized at seven hospitals in Korea from 2 February 2020 to 28 February 2021. The research was approved by the ethical committee of the promoting center (institutional review board of Chungnam National University Hospital, approval no. 2021-04-053, approval date: 30 April 2021) and by the local ethical committees. The need for a written informed consent was waived because of the retrospective nature of the study. During the study period, 1565 patients were screened (Figure 1). A total of 1077 patients were excluded due to non-severe COVID-19.
Figure 1.
Patient flowchart, COVID-19: coronavirus disease 2019.
All data were retrieved from the electronic medical records. Information about the characteristics of patients, including sex, age, symptoms, and initial laboratory and radiologic findings, was collected. Moreover, data about the need for invasive treatment (mechanical ventilation, treatment with vasopressor, and continuous renal replacement therapy (CRRT), in-hospital mortality, and duration of hospital stay were extracted. The initial Acute Physiology and Chronic Health Evaluation II (APACHE II) score, Charlson Comorbidity Index (CCI), and Clinical Frailty Scale (CFS) score were analyzed to evaluate the patient’s condition upon admission.
2.1. Definition
The approval of requests was reserved for hospitalized patients who had SARS-CoV-2 infection confirmed via reverse-transcriptase polymerase-chain-reaction (PCR). Severe COVID-19 infection was defined as including an oxygen saturation level of 94% or less while the patient was breathing ambient air, and a need for oxygen support [17]. Secondary infection was defined as the presence of clinical signs and/or symptoms of infection and the presence of a pathogen based on the diagnostic tests, including respiratory bacterial PCR (using endotracheal aspirates and expectorated sputum), nasopharyngeal PCR, blood culture, and urine culture during illness or hospital stay [18].
2.2. Statistical Analysis
All values were expressed as median (interquartile range (IQR): 25–75 percentile) for continuous variables or as percentages for categorical variables. The student’s t-test or the Mann–Whitney U test was used for continuous data, and the Pearson’s chi-squared test or the Fisher’s exact test for categorical data. The risk factors for mortality were analyzed using the Cox proportional hazards model with backward, stepwise elimination, and variables with p < 0.1 in the univariate analysis were entered into the multivariate models. All p-values were two-tailed, and a p value of <0.05 was considered statistically significant. All statistical analyses were performed using the Statistical Package for the Social Sciences software (version 22.0; IBM Corporation, Somers, NY, USA).
3. Results
3.1. Baseline Characteristics of Patients with Severe COVID-19
Of the total 1565 COVID-19 patients hospitalized, 488 who had severe COVID-19 were included in this study. Moreover, 170 (34.8%) and 318 (65.2%) patients were aged <65 years (younger patient group) and ≥65 years (older patient group), respectively (Figure 1).
Table 1 shows the baseline characteristics of patients. The median ages of younger and older patient groups were 58 (IQR: 51–62) years and 78 (IQR: 71–84) years, respectively. The older patient group had a lower proportion of male patients and fewer symptoms upon admission. Further, the older patient group had a lower body mass index (BMI) and a higher proportion of nursing facility residents. Older patients had higher APACHE II scores (11.5 (9.0–15.0) versus. 7.0 (5.0–10.0), p < 0.001), CCI (4.0 (3.0–5.0) versus 2.0 (1.0–2.0), p < 0.001), and CFS scores (4.0 (3.0–7.0) versus 2.0 (1.0–3.0), p < 0.001) than younger patients. Hypertension, diabetes mellitus (DM), chronic obstructive pulmonary disease (COPD), cardiovascular disease, and heart failure were more common in older patients than in younger patients. In terms of vital signs, the older patients had a lower diastolic blood pressure (DBP), heart rate (HR), and body temperature than the younger patients. Regarding the initial laboratory data, compared with the younger patients, the older patients had lower neutrophil-to-lymphocyte ratios (NLRs), hemoglobin levels, and albumin levels, and higher blood urea nitrogen (BUN) levels. Based on the initial radiography result, unilateral lesions were more common in older patients than in younger patients.
Table 1.
Baseline characteristics of patients with severe COVID-19.
| Variables | All Patients (n = 488) |
Younger Patients (n = 170) |
Older Patients (n = 318) |
p-Value |
|---|---|---|---|---|
| Age | 70 (62–80) | 58 (51–62) | 78 (71–84) | <0.001 |
| Male (%) | 234 (48.0) | 98 (57.6) | 136 (42.8) | 0.002 |
| Smoking (%) | 87 (17.8) | 30 (17.6) | 57 (17.9) | 0.939 |
| Symptom at admission (%) | 398 (81.6) | 154 (90.6) | 244 (76.7) | <0.001 |
| Symptom to admission, days | 4.0 (1.0–8.0) | 5.0 (2.0–8.0) | 3.0 (1.0–7.0) | 0.860 |
| Body mass index | 24.3 (21.8–27.1) | 26.0 (24.0–28.9) | 23.1 (20.7–25.9) | <0.001 |
| Resident of a nursing facilities | 81 (16.6) | 5 (2.9) | 76 (23.9) | <0.001 |
| Scoring systems | ||||
| APACHE II score | 10.0 (7.0–13.3) | 7.0 (5.0–10.0) | 11.5 (9.0–15.0) | <0.001 |
| Clinical Frailty Scale | 3.0 (2.0–6.0) | 2.0 (1.0–3.0) | 4.0 (3.0–7.0) | <0.001 |
| Charlson Comorbidity Index | 3.0 (2.0–5.0) | 2.0 (1.0–2.0) | 4.0 (3.0–5.0) | <0.001 |
| Comorbidity (%) | ||||
| Hypertension | 266 (54.5) | 65 (38.2) | 201 (63.2) | <0.001 |
| DM | 150 (30.7) | 34 (20.0) | 116 (36.5) | <0.001 |
| COPD | 13 (2.7) | 1 (0.6) | 12 (3.8) | 0.037 |
| Cerebrovascular disease | 49 (10.0) | 7 (4.1) | 42 (13.2) | 0.001 |
| Heart failure | 17 (3.5) | 1 (0.6) | 16 (5.0) | 0.011 |
| Liver cirrhosis | 5 (1.0) | 1 (0.6) | 4 (1.3) | 0.484 |
| Chronic kidney disease | 5 (1.0) | 0 (0) | 5 (1.6) | 0.100 |
| Malignancy | 27 (5.5) | 9 (5.3) | 18 (5.7) | 0.866 |
| Organ transplantation | 1 (0.2) | 1 (0.6) | 0 (0) | 0.171 |
| Vital signs | ||||
| SBP, mmHg | 121 (108–138) | 122 (108–137) | 121 (108–140) | 0.906 |
| DBP, mmHg | 72 (63–83) | 76 (66–86) | 71 (61–81) | 0.019 |
| HR,/min | 87 (75–100) | 88 (80–102) | 86 (73–99) | 0.009 |
| RR,/min | 20 (20–22) | 20 (20–22) | 20 (19–24) | 0.345 |
| Body Temperature, ℃ | 36.8 (36.4–37.8) | 37.4 (36.5–38.2) | 36.7 (36.4–37.4) | <0.001 |
| SpO2, % | 96.0 (93.0–98.0) | 96.0 (94.0–98.0) | 95.0 (92.0–98.0) | 0.129 |
| GCS | 15 (15–15) | 15 (15–15) | 15 (14–15) | 0.002 |
| Duration of fever | 2.0 (0.0–5.0) | 3.0 (1.0–5.3) | 2.0 (0.0–4.3) | 0.760 |
| Laboratory data | ||||
| White cell count, 1000/mm3 | 5.87 (4.32–8.04) | 5.77 (4.32–8.48) | 5.91 (4.36–7.98) | 0.767 |
| Neutrophil-to-lymphocyte ratio | 4.63 (2.71–8.88) | 4.65 (2.62–7.79) | 4.56 (2.75–9.60) | 0.013 |
| Hemoglobin, g/dL | 12.9 (11.6–14.1) | 13.8 (12.3–14.8) | 12.6 (11.2–13.8) | <0.001 |
| Platelet count, 1000/mm3 | 182 (136–229) | 189 (150–237) | 179 (134–228) | 0.106 |
| Total bilirubin, mg/dL | 0.5 (0.4–0.7) | 0.5 (0.4–0.8) | 0.5 (0.3–0.7) | 0.089 |
| Albumin, g/dL | 3.5 (3.1–4.0) | 3.7 (3.3–4.2) | 3.5 (3.1–3.8) | <0.001 |
| BUN, mg/dL | 15 (11–22) | 13 (10–17) | 16 (12–24) | 0.003 |
| Creatinine, mg/dL | 0.76 (0.60–0.95) | 0.73 (0.61–0.89) | 0.78 (0.60–1.00) | 0.992 |
| C-reactive protein, mg/dL | 5.93 (2.10–11.67) | 6.40 (2.10–13.20) | 5.70 (2.07–10.58) | 0.322 |
| Chest X-ray | ||||
| Normal | 74 (15.2) | 23 (13.5) | 51 (16.0) | 0.462 |
| Unilateral | 67 (13.7) | 15 (8.8) | 52 (16.4) | 0.021 |
| Bilateral | 217 (44.5) | 79 (46.5) | 138 (43.4) | 0.515 |
| Multifocal | 130 (26.6) | 53 (31.2) | 77 (24.2) | 0.097 |
Data are presented as median and interquartile range or number (%), unless otherwise indicated. COVID-19: coronavirus disease 2019, APACHE II: Acute Physiology and Chronic Health Evaluation II, DM: diabetes mellitus, COPD: chronic obstructive pulmonary disease, SBP: systolic blood pressure, DBP: diastolic blood pressure, HR: heart rate, RR: respiratory rate, SpO2: saturation pulse oxygen, GCS: Glasgow Coma Scale, BUN: blood urea nitrogen.
3.2. Treatment and Clinical Outcomes of Patients with Severe COVID-19
Table 2 shows the treatment and outcomes of patients with severe COVID-19. The use of antibiotics (66.4% versus 48.8%, p < 0.001) and vasopressors (15.1% versus 7.6%, p = 0.018) was higher in older patients than in younger patients. In terms of the oxygen delivery system, nasal prongs (88.8% versus 80.8%, p = 0.023) were more commonly used in younger patients. The overall in-hospital mortality rate was 18.2% (89 of 488), and the older group had a higher mortality rate than the younger group (25.5% versus 4.7%, p < 0.001). The older patient group had a higher incidence of secondary infection (32.4% versus 23.5%, p = 0.040) and a higher proportion of patients with a do-not-resuscitate (DNR) order (23.9% versus 2.9%, p < 0.001) than the younger patient group.
Table 2.
Treatment and clinical outcomes of patients with severe COVID-19.
| Variables | All Patients (n = 488) |
Younger Patients (n = 170) |
Older Patients (n = 318) |
p-Value |
|---|---|---|---|---|
| Treatment (%) | ||||
| Remdesivir | 244 (50.0) | 76 (44.7) | 168 (52.8) | 0.087 |
| Antibiotics | 294 (60.2) | 83 (48.8) | 211 (66.4) | <0.001 |
| Vasopressor | 61 (12.5) | 13 (7.6) | 48 (15.1) | 0.018 |
| CRRT | 24 (4.9) | 4 (2.4) | 20 (6.3) | 0.055 |
| Corticosteroid | 369 (75.6) | 125 (73.5) | 244 (76.7) | 0.433 |
| Oxygen supply device | ||||
| Nasal prong | 408 (83.6) | 151 (88.8) | 257 (80.8) | 0.023 |
| HFNC | 157 (32.2) | 47 (27.6) | 110 (34.6) | 0.118 |
| Invasive mechanical ventilation | 120 (24.6) | 40 (23.5) | 80 (25.2) | 0.691 |
| ECMO | 19 (3.9) | 9 (5.3) | 10 (3.1) | 0.242 |
| Tracheostomy (%) | 37 (7.6) | 10 (5.9) | 27 (8.5) | 0.300 |
| Outcomes | ||||
| In-hospital mortality (%) | 89 (18.2) | 8 (4.7) | 81 (25.5) | <0.001 |
| Length of hospital stay (days) | 16.0 (12.0–25.0) | 16.0 (12.0–22.0) | 17.0 (12.0–26.0) | 0.396 |
| Secondary infection | 143 (29.3) | 40 (23.5) | 103 (32.4) | 0.040 |
| DNR order | 81 (16.6) | 5 (2.9) | 76 (23.9) | <0.001 |
Data are presented as median and interquartile range or number (%), unless otherwise indicated. COVID-19: coronavirus disease 2019, CRRT: continuous renal replacement therapy, HFNC: high flow nasal cannula, ECMO: extracorporeal membrane oxygenation, DNR: do not resuscitate.
3.3. Factors Associated with In-Hospital Mortality
Table 3 shows the results of the multivariate analysis of factors associated with in-hospital mortality. After adjusting for confounders, the independent predictors of in-hospital mortality included age (hazard ratio (HR): 1.031, 95% confidence interval (CI): 1.008–1.054; p = 0.008), APACHE II score (HR: 1.038, 95% CI: 1.006–1.071; p = 0.018), presence of DM (HR: 1.622, 95% CI: 1.029–2.559; p = 0.037) and COPD (HR: 4.294, 95% CI: 1.874–9.837; p = 0.001), high white blood cell (WBC) count (HR: 1.104, 95% CI: 1.056–1.153; p < 0.001), low NLR (HR: 0.984, 95% CI: 0.968–1.000; p = 0.044), low platelet count (HR: 0.996, 95% CI: 0.993–0.999; p = 0.024), DNR order (HR: 6.260, 95% CI: 3.792–10.333; p < 0.001), and treatment with invasive mechanical ventilation (HR: 1.824, 95% CI: 1.070–3.107; p = 0.027).
Table 3.
Univariate and multivariate risk factors associated with in hospital mortality (Cox regression model).
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p-Value | HR | 95% CI | p-Value | |
| Age | 1.055 | 1.035–1.075 | <0.001 | 1.031 | 1.008–1.054 | 0.008 |
| Scoring systems | ||||||
| APACHE II score | 1.092 | 1.062–1.123 | <0.001 | 1.038 | 1.006–1.071 | 0.018 |
| Frailty scale | 1.289 | 1.173–1.417 | <0.001 | 1.022 | 0.887–1.178 | 0.764 |
| Comorbidity (%) | ||||||
| DM | 2.115 | 1.391–3.214 | <0.001 | 1.622 | 1.029–2.559 | 0.037 |
| COPD | 4.507 | 2.063–9.844 | <0.001 | 4.294 | 1.874–9.837 | 0.001 |
| Cerebrovascular disease | 1.739 | 0.942–3.212 | 0.077 | 1.491 | 0.780–2.848 | 0.227 |
| Liver cirrhosis | 4.551 | 1.431–14.469 | 0.010 | 1.287 | 0.270–6.147 | 0.752 |
| Laboratory findings | ||||||
| White blood cell count, 1000/mm3 | 1.058 | 1.017–1.100 | 0.005 | 1.104 | 1.056–1.153 | <0.001 |
| Neutrophil lymphocyte ratio | 1.020 | 1.007–1.032 | 0.002 | 0.984 | 0.968–1.000 | 0.044 |
| Platelet count, 1000/mm3 | 0.994 | 0.991–0.998 | 0.001 | 0.996 | 0.993–0.999 | 0.024 |
| Albumin, g/dL | 0.451 | 0.312–0.652 | <0.001 | 0.794 | 0.481–1.310 | 0.366 |
| Creatinine, mg/dL | 1.112 | 1.019–1.212 | 0.017 | 0.944 | 0.813–1.095 | 0.446 |
| DNR order | 9.618 | 6.102–15.159 | <0.001 | 6.260 | 3.792–10.333 | <0.001 |
| Treatment | ||||||
| Invasive mechanical ventilation | 1.754 | 1.104–2.785 | 0.017 | 1.824 | 1.070–3.107 | 0.027 |
| Vasopressor use | 2.416 | 1.536–3.800 | <0.001 | 1.069 | 0.583–1.961 | 0.829 |
HR: hazard ratio, CI: confidence interval, APACHE II: Acute Physiology and Chronic Health Evaluation II, DM: diabetes mellitus, COPD: chronic obstructive pulmonary disease, DNR: do not resuscitate.
4. Discussion
This multicenter study investigated the correlation between in-hospital mortality and some factors among elderly patients with severe COVID-19. Approximately 65.2% of hospitalized patients with severe COVID-19 were aged over 65 years. Older patients had higher initial APACHE II, CCI, and CFS scores than younger patients. Moreover, they commonly presented with underlying diseases, lower NLRs and hemoglobin and albumin levels, and higher BUN levels. The use of antibiotics and vasopressors was higher in older patients than in younger patients. Older patients had a higher in-hospital mortality rate and incidence of secondary infection than younger patients, and DNR order were more common in older patients than in younger patients. The risk factors for in-hospital mortality in patients with severe COVID-19 included high APACHE II score and WBC count, low platelet count, DNR order, and treatment with invasive mechanical ventilation. The in-hospital mortality rate of the older patient group was 25.5%.
There is a large population of older patients with severe COVID-19. Tan et al. showed that 47.2% of patients who died from COVID-19 were elderly (≥70 years) [19]. Singhal et al. revealed that 51% of older patients with COVID-19 (≥60 years) had severe infection and 22% of patients were critically ill [20]. In the study by Agnieszka et al., 50% of elderly patients with COVID-19 (≥60 years) were hospitalized (50.5%), of whom 23.5% were admitted at the ICU [21]. Although several studies have reported the proportion of elderly patients with COVID-19, different age criteria were used, and patients of varying severity were included. Nevertheless, they showed that elderly patients account for a large proportion of patients with severe or critical COVID-19. This result is similar to that of our research.
This study showed that hypertension was the most common comorbidity in this study, and elderly patients frequently presented with DM, COPD, cardiovascular disease, and heart failure. These results are similar to those of other studies showing that patients commonly had hypertension, and diabetes, cardiovascular disease, hypercholesterolemia, chronic lung disease, and malignancy were the frequent comorbidities [20,21,22,23,24]. In this research, elderly patients had lower NLRs, hemoglobin and albumin levels, and higher BUN levels. Other studies showed that patients presented with anemia, lymphopenia, thrombocytopenia, slightly abnormal creatinine and BUN levels, low albumin levels, high d-dimer, CRP, and procalcitonin levels [20,21,22,23,24,25]. Although the findings slightly differed, this study only included patients with severe COVID-19, and this might have influenced the results. Nevertheless, most laboratory data trends were similar.
In this study, the risk factors for in-hospital mortality among patients with severe COVID-19 included age, higher APACHE II score, presence of DM and COPD, higher WBC count, lower NLR, platelet count, DNR order, and treatment with invasive mechanical ventilation. Based on the study of Grasselli, which included patients with COVID-19 admitted to the ICU, the independent risk factors associated with mortality included old age (HR: 1.75, 95% CI: 1.60–1.92), male sex (HR: 1.57, 95% CI: 1.31–1.88), high fraction of inspired oxygen (HR: 1.14, 95% CI: 1.10–1.19), or low partial pressure of oxygen-to-fraction of inspired oxygen ratio (HR: 0.80, 95% CI: 0.74–0.87) upon ICU admission, and history of COPD (HR: 1.68, 95% CI: 1.28–2.19), hypercholesterolemia (HR: 1.25, 95% CI: 1.02–1.52), and type 2 diabetes (HR: 1.18, 95% CI: 1.01–1.39) [26]. According to Kim et al., the independent factors associated with in-hospital mortality among hospitalized patients with COVID-19 were old age, immunosuppression, renal, chronic lung, cardiovascular, and neurologic disorders, and diabetes [27]. Other studies have shown that patient severity and malnutrition could affect patient prognosis [28,29]. Therefore, higher severity scores, malnutrition, poor laboratory data, and DNR orders were associated with in-hospital mortality even in the patient group with severe COVID-19.
Elderly patients with severe COVID-19 had higher severity and Clinical Frailty Scale scores, and they commonly presented with underlying diseases such as DM and COPD. These results are similar to those of other studies [30,31,32,33,34,35]. In Guo et al.'s study, elderly patients had more underlying diseases, and common comorbidities included hypertension, diabetes, and cardiac disease [25]. In the study by Gao et al., which included elderly patients with COVID-19 (≥65 years), the common morbidities included cardiovascular diseases (49% versus 20%), respiratory diseases (51% versus 11%), and chronic kidney disease (29% versus 5%) in the deceased group in elderly COVID-19 patients (aged ≥65 years), and cerebrovascular disease than in the discharged group. In addition, high CRP and BUN level and lymphopenia were associated with poor prognosis [35]. Similar to our study, several studies showed that underlying disease was more common and mortality rate was higher in the elderly group.
This study had several limitations. First, it included patients admitted at tertiary or referral hospitals capable of critical care. This might have affected the results, as patients who had been transferred from other hospitals or from living treatment centers due to worsening conditions were included. Second, instead of manually reviewing medical records, data were collected from the electronic health record database. Hence, some details could have been missing. Third, patients’ economic status was not assessed even though inferior economic conditions are associated with poor outcomes [36,37]. Nevertheless, in Korea, the National Health Insurance provides free COVID-19 treatment. Hence the impact is likely low. Fourth, in South Korea, at the beginning of the COVID-19 outbreak, regardless of severity, all patients were hospitalized and then discharged. Therefore, the number of severe cases admitted to the hospital may be small compared to studies in other countries.
5. Conclusions
In conclusion, this study informed the clinical characteristics and prognosis of elderly patients with severe COVID-19 in Korea and assessed the risk factors for in-hospital mortality. Elderly patients with severe COVID-19 had higher APACHE II score, were frailer and had more underlying diseases than younger patients. Therefore, they commonly required vasopressors and invasive mechanical ventilation, and had a poor prognosis. As the COVID-19 pandemic continues, the number of elderly patients infected keeps increasing. Nevertheless, we believe that the results of this paper can help understand characteristics and predict the prognosis of elderly patients with severe COVID-19.
Author Contributions
S.-I.L.: conceptualization, data curation, formal analysis, investigation, methodology, supervision, validation, visualization, writing-original draft, writing-review and editing; G.M.S.: conceptualization, data curation, formal analysis, investigation, methodology, validation, visualization, writing-original draft, writing-review and editing; A.-R.B.: data curation, writing-original draft; M.S.B.: data curation, writing-original draft; W.-Y.K.: data curation, writing—original draft; J.H.K.: data curation, writing-original draft; B.Y.L.: data curation, writing—original draft, Y.S.N.: data curation, writing-original draft. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the institutional review board of Chungnam National University Hospital (approval no. 2021-04-053, approval date: 30 April 2021), and the requirement to obtain informed consent was waived due to the retrospective nature of the study.
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO COVID-19, Korea. [(accessed on 16 November 2021)]. Available online: https://covid19.who.int/region/wpro/country/kr.
- 3.Baden L.R., Sahly H.M.E., Essink B., Kotloff K., Frey S., Novak R., Diemert D., Spector S.A., Rouphael N., Creech C.B., et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N. Engl. J. Med. 2021;384:403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Polack F.P., Thomas S.J., Kitchin N., Absalon J., Gurtman A., Lockhart S., Perez J.L., Pérez Marc G., Moreira E.D., Zerbini C., et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 vaccine. N. Engl. J. Med. 2020;383:2603–2615. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soiza R.L., Scicluna C., Thomson E.C. Efficacy and safety of COVID-19 vaccines in older people. Age Ageing. 2021;50:279–283. doi: 10.1093/ageing/afaa274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Javanmardi F., Keshavarzi A., Akbari A., Emami A., Pirbonyeh N. Prevalence of underlying diseases in died cases of COVID-19. A systematic review and meta-analysis. PLoS ONE. 2020;15:e0241265. doi: 10.1371/journal.pone.0241265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Booth A., Reed A.B., Ponzo S., Yassaee A., Aral M., Plans D., Labrique A., Mohan D. Population risk factors for severe disease and mortality in COVID-19: A global systematic review and meta-analysis. PLoS ONE. 2021;16:e0247461. doi: 10.1371/journal.pone.0247461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang L., Hou J., Ma F.Z., Li J., Xue S., Xu Z.G. The common risk factors for progression and mortality in COVID-19 patients: A meta-analysis. Arch. Virol. 2021;166:2071–2081. doi: 10.1007/s00705-021-05012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gan J.M., Kho J., Akhunbay-Fudge M., Choo H.M., Wright M., Batt F., Mandal A.K.J., Chauhan R., Missouris C.G. Atypical presentation of COVID-19 in hospitalised older adults. Ir. J. Med. Sci. 2021;190:469–474. doi: 10.1007/s11845-020-02372-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bavaro D.F., Diella L., Fabrizio C., Sulpasso R., Bottalico I.F., Calamo A., Santoro C.R., Brindicci G., Bruno G., Mastroianni A., et al. Peculiar clinical presentation of COVID-19 and predictors of mortality in the elderly. A multicentre retrospective cohort study. Int. J. Infect. Dis. 2021;105:709–715. doi: 10.1016/j.ijid.2021.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Malhotra V., Basu S., Sharma N., Kumar S., Garg S., Dushyant K., Borle A. Outcomes among 10,314 hospitalized COVID-19 patients at a tertiary care government hospital in Delhi, India. J. Med. Virol. 2021;93:4553–4558. doi: 10.1002/jmv.26956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li X., Xu S., Yu M., Wang K., Tao Y., Zhou Y., Shi J., Zhou M., Wu B., Yang Z., et al. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J. Allergy Clin. Immunol. 2020;146:110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ho F.K., Petermann-Rocha F., Gray S.R., Jani B.D., Katikireddi S.V., Niedzwiedz C.L., Foster H., Hastie C.E., Mackay D.F., Gill J.M.R., et al. Is older age associated with COVID-19 mortality in the absence of other risk factors? General population cohort study of 470,034 participants. PLoS ONE. 2020;15:e0241824. doi: 10.1371/journal.pone.0241824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Owen R.K., Conroy S.P., Taub N., Jones W., Bryden D., Pareek M., Faull C., Abrams K.R., Davis D., Banerjee J. Comparing associations between frailty and mortality in hospitalised older adults with or without COVID-19 infection: A retrospective observational study using electronic health records. Age Ageing. 2021;50:307–316. doi: 10.1093/ageing/afaa167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berlin D.A., Gulick R.M., Martinez F.J. Severe Covid-19. N. Engl. J. Med. 2020;383:2451–2460. doi: 10.1056/NEJMcp2009575. [DOI] [PubMed] [Google Scholar]
- 18.Langford B.J., So M., Raybardhan S., Leung V., Westwood D., MacFadden D.R., Soucy J.R., Daneman N. Bacterial co-infection and secondary infection in patients with COVID-19: A living rapid review and meta-analysis. Clin. Microbiol. Infect. 2020;26:1622–1629. doi: 10.1016/j.cmi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tan X., Zhang S., Xu J., Zhou M., Huang Q., Duan L., Lv Z., Xia H., Xiao W., Yin Z., et al. Comparison of clinical characteristics among younger and elderly deceased patients with COVID-19: A retrospective study. Aging. 2020;13:16–26. doi: 10.18632/aging.202139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singhal S., Kumar P., Singh S., Saha S., Dey A.B. Clinical features and outcomes of COVID-19 in older adults: A systematic review and meta-analysis. BMC Geriatr. 2021;21:321. doi: 10.1186/s12877-021-02261-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neumann-Podczaska A., Al-Saad S.R., Karbowski L.M., Chojnicki M., Tobis S., Wieczorowska-Tobis K. COVID 19—Clinical Picture in the Elderly Population: A Qualitative Systematic Review. Aging Dis. 2020;11:988–1008. doi: 10.14336/AD.2020.0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Song J., Hu W., Yu Y., Shen X., Wang Y., Yan J., Yang X., Gong S., Wang M. A Comparison of Clinical Characteristics and Outcomes in Elderly and Younger Patients with COVID-19. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2020;26:e925047. doi: 10.12659/MSM.925047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pepe M., Maroun-Eid C., Romero R., Arroyo-Espliguero R., Fernàndez-Rozas I., Aparisi A., Becerra-Muñoz V.M., Aguado M.G., Brindicci G., Huang J., et al. Clinical presentation, therapeutic approach, and outcome of young patients admitted for COVID-19, with respect to the elderly counterpart. Clin. Exp. Med. 2021;21:249–268. doi: 10.1007/s10238-021-00684-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li P., Chen L., Liu Z., Pan J., Zhou D., Wang H., Gong H., Fu Z., Song Q., Min Q., et al. Clinical features and short-term outcomes of elderly patients with COVID-19. Int. J. Infect. Dis. 2020;97:245–250. doi: 10.1016/j.ijid.2020.05.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guo T., Shen Q., Guo W., He W., Li J., Zhang Y., Wang Y., Zhou Z., Deng D., Ouyang X., et al. Clinical Characteristics of Elderly Patients with COVID-19 in Hunan Province, China: A Multicenter, Retrospective Study. Gerontology. 2020;66:467–475. doi: 10.1159/000508734. [DOI] [PubMed] [Google Scholar]
- 26.Grasselli G., Greco M., Zanella A., Albano G., Antonelli M., Bellani G., Bonanomi E., Cabrini L., Carlesso E., Castelli G., et al. Risk Factors Associated With Mortality Among Patients With COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern. Med. 2020;180:1345. doi: 10.1001/jamainternmed.2020.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim L., Garg S., O’Halloran A., Whitaker M., Pham H., Anderson E.J., Armistead I., Bennett N.M., Billing L., Como-Sabetti K., et al. Risk Factors for Intensive Care Unit Admission and In-hospital Mortality Among Hospitalized Adults Identified through the US Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET) Clin. Infect. Dis. 2021;72:e206–e214. doi: 10.1093/cid/ciaa1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giannasi S.E., Venuti M.S., Midley A.D., Roux N., Kecskes C., San Román E. Mortality risk factors in elderly patients in intensive care without limitation of therapeutic effort. Med. Intensiva. 2018;42:482–489. doi: 10.1016/j.medin.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 29.Wang C.H., Lin H.C., Chang Y.C., Maa S.H., Wang J.S., Tang W.R. Predictive factors of in-hospital mortality in ventilated intensive care unit: A prospective cohort study. Medicine. 2017;96:e9165. doi: 10.1097/MD.0000000000009165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vrillon A., Hourregue C., Azuar J., Grosset L., Boutelier A., Tan S., Roger M., Mourman V., Mouly S., Sène D., et al. COVID -19 in Older Adults: A Series of 76 Patients Aged 85 Years and Older with COVID-19. J. Am. Geriatr. Soc. 2020;68:2735–2743. doi: 10.1111/jgs.16894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herrmann M.L., Hahn J.-M., Walter-Frank B., Bollinger D.M., Schmauder K., Schnauder G., Bitzer M., Malek N.P., Eschweiler G.W., Göpel S. COVID-19 in persons aged 70+ in an early affected German district: Risk factors, mortality and post-COVID care needs—A retrospective observational study of hospitalized and non-hospitalized patients. PLoS ONE. 2021;16:e0253154. doi: 10.1371/journal.pone.0253154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Knopp P., Miles A., Webb T.E., McLoughlin B.C., Mannan I., Raja N., Wan B., Davis D. Presenting features of COVID-19 in older people: Relationships with frailty, inflammation and mortality. Eur. Geriatr. Med. 2020;11:1089–1094. doi: 10.1007/s41999-020-00373-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee J.Y., Kim H.A., Huh K., Hyun M., Rhee J.-Y., Jang S., Kim J.-Y., Peck K.R., Chang H.-H. Risk Factors for Mortality and Respiratory Support in Elderly Patients Hospitalized with COVID-19 in Korea. J. Korean Med Sci. 2020;35:e223. doi: 10.3346/jkms.2020.35.e223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leung C. Risk factors for predicting mortality in elderly patients with COVID-19: A review of clinical data in China. Mech. Ageing Dev. 2020;188:111255. doi: 10.1016/j.mad.2020.111255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gao S., Jiang F., Jin W., Shi Y., Yang L., Xia Y., Jia L., Wang B., Lin H., Cai Y., et al. Risk factors influencing the prognosis of elderly patients infected with COVID-19: A clinical retrospective study in Wuhan, China. Aging. 2020;12:12504–12516. doi: 10.18632/aging.103631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wernly B., Beil M., Bruno R.R., Binnebössel S., Kelm M., Sigal S., van Heerden P.V., Boumendil A., Artigas A., Cecconi M., et al. Provision of critical care for the elderly in Europe: A retrospective comparison of national healthcare frameworks in intensive care units. BMJ Open. 2021;11:e046909. doi: 10.1136/bmjopen-2020-046909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Baldwin M.R., Sell J.L., Heyden N., Javaid A., Berlin D.A., Gonzalez W.C., Bach P.B., Maurer M.S., Lovasi G., Lederer D. Race, Ethnicity, Health Insurance, and Mortality in Older Survivors of Critical Illness. Crit. Care Med. 2017;45:e583–e591. doi: 10.1097/CCM.0000000000002313. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.