Abstract
Crimean-Congo hemorrhagic fever virus (CCHFV) is endemic in Africa, Asia, and Eastern Europe where it circulates among animals and ticks causing sporadic outbreaks in humans. Although CCHF is endemic in sub-Saharan Africa, epidemiological information is lacking in many countries, including Malawi. To assess the risk of CCHF in Malawi, we conducted an epidemiological study in cattle reared by smallholder livestock farmers in central Malawi. A cross-sectional study was conducted in April 2020 involving seven districts, four from Kasungu and three from Lilongwe Agriculture Development Divisions. A structured questionnaire was administered to farmers to obtain demographic, animal management, and ecological risk factors data. Sera were collected from randomly selected cattle and screened for CCHF virus (CCHFV) specific antibodies using a commercial ELISA kit. Ticks were collected from cattle and classified morphologically to species level. An overall CCHFV seropositivity rate of 46.9% (n = 416; 95% CI: 42.0–51.8%) was observed. The seropositivity was significantly associated with the age of cattle (p < 0.001), sex (p < 0.001), presence of ticks in herds (p = 0.01), district (p = 0.025), and type of grazing lands (p = 0.013). Five species of ticks were identified, including Hyalomma truncatum, a known vector of CCHFV. Ticks of the species Hyalomma truncatum were not detected in two districts with the highest seroprevalence for CCHF and vector competency must be further explored in the study area. To our knowledge, this is the first report of serologic evidence of the presence of CCHV among smallholder cattle in central Malawi. This study emphasizes the need for continued monitoring of CCHFV infection among livestock, ticks, and humans for the development of data-based risk mitigation strategies.
Keywords: cattle, Crimean-Congo hemorrhagic fever virus, Malawi, seroprevalence
1. Introduction
Crimean-Congo hemorrhagic fever (CCHF), caused by the Crimean-Congo hemorrhagic fever virus (CCHFV), is a tick-borne zoonotic disease that may cause severe disease in humans [1]. CCHFV is a member of the order Bunyavirales, family Nairoviridae, and genus Orthonairovirus [2] and is considered one of the widely distributed arbovirus infecting both wild and domestic vertebrates [3]. Serological and molecular studies have provided evidence of CCHFV presence in ticks and clinically healthy non-human mammals and avian species [1,4,5,6,7], suggesting natural circulation in these hosts. When spillover to humans occurs, CCHFV can cause fatal outbreaks [8,9]. The seasonality of tick dynamics in endemic regions appears to correspond to seasonal waves of CCHF episodes in humans [1,10]. Transmission to susceptible humans is commonly by bites of Hyalomma ticks, which are known principal vectors of CCHFV [11,12] as well as through direct contact with body fluids and tissues of viremic animals and infected humans [8,11,13].
Whilst most infections in humans are asymptomatic (≈88%), the clinical disease does occur and is characterized by signs that range from mild fever to severe hemorrhagic disease along with multiple organ failure and often result in death. Further, high case fatality rate (10–50%) has been recorded [14,15,16,17]. Although CCHF is of great public health significance, to date, no approved curative chemotherapy nor vaccine is available to mitigate its impact [18,19,20,21,22].
Geographically, about 50 countries across Africa, Asia, and Eastern Europe are considered endemic to CCHFV and Hyalomma ticks [21,23]. It is estimated that over three billion people are at risk of infection, with 10,000–15,000 infections annually resulting in about 500 deaths per annum [17]. Through a meta-analysis, the global mean seroprevalence of CCHFV was estimated at 18.6% for cattle alone and 24.7% for all domestic animals [23]. In Africa, the seroprevalence in animals ranges from 0.4 to 75% [4,24]. Its spatial distribution drivers include long-distance live animal trade, habitat fragmentation, expansion of agricultural/cultivation lands, and increase in environmental mean temperatures [17,25]. Migratory birds are also implicated in the spread of CCHFV by carrying infected ticks over long distances [26,27].
CCHFV is considered a serious occupational hazard among people working along the livestock production value chain, which includes farmers, animal handlers, abattoir workers, and veterinarians because of increased exposure to tick bites and viremic animal body fluids [12,13,27,28]. Further, human-to-human transmission occurs commonly in healthcare facilities [4,29,30]. In recent years, there have been increased reports of CCHF amongst travelers (tourists) who are diagnosed with the infection upon return to their respective non-endemic countries [31]. These increased reports in tourists could be associated with engagement in high-risk activities (game trekking) but could be also indicative of the lack of diagnostic and surveillance capacity in these endemic developing countries [32].
There is a lack of epidemiologic information about the presence of CCHF in Malawi despite serologic and/or molecular evidence for its presence in surrounding countries, including Mozambique, Tanzania, Zimbabwe, Namibia, South Africa, Democratic Republic of Congo, Kenya, Uganda, and Zambia [3,4,24,29,33,34]. Malawi’s agriculture sector has changed in various aspects such as tick control strategy (from public-owned to community-owned, in the mid-1990s), increased within and cross border animal movements, and expansion of cultivation and grazing lands into natural forests and marginalized lands following human population growth [35,36,37,38]. Currently, dambos (seasonally waterlogged depressions or wetlands) and uplands (elevated and generally dry areas) are the main source of grazing land for livestock. The concurrent existence of the competent vectors (Hyalomma ticks) and favorable ecological risk factors [39,40], suggests an increased potential risk of CCHF emergence in Malawi. Hence, this study aimed at providing epidemiological data on the seroprevalence of CCHFV infection and assessing its associated risk factors in cattle in central Malawi.
2. Results
2.1. Description of the Study Population
A total of 416 cattle, with 208 being male, from 117 cattle herds were sampled. The calculated sample size was 436 cattle (see Section 4). The determined sample size could not be achieved due to poor roads in some veterinary stations. A structured questionnaire was administered to 108 (103 males; 5 females) cattle owners. Figure 1 below shows the study cattle population herd structure. The population had many cattle aged >24 months, and most of them belonged to small herd sizes.
Figure 1.
The study cattle population structure by sex, age, and herd size. NB: Herd size categories: small = 1–6 animals, medium = 7–14 animals, and large >14 animals.
Management of cattle and tick infestation levels varied among the cattle herds (Table 1). About 80.3% (94/117) of cattle herds were grazed in dambo lands. Ticks were present in 90.6% (106/117) of the cattle herds. Tick control was reported to be practiced in 62.0% (67/108) of the herds. The majority of the cattle farmers, 50.9% (55/108), used the spraying method, and only one farmer, 0.9% (1/108), plunge dipped his cattle.
Table 1.
Distribution of cattle herds across different cattle management factors.
| Factor (n) | Category | Number of Herds per Category | Percentage (95% CI) |
|---|---|---|---|
| Grazing land type (n =117) | Dambo | 94 | 80.3 (72.0–87.1) |
| Both (dambo and upland) | 12 | 10.3 (05.1–17.2) | |
| Upland | 11 | 9.4 (4.79–16.20) | |
| Ticks on herd (n = 117) | Present | 106 | 90.6 (83.8–95.2) |
| Absent | 11 | 9.4 (4.8–16.2) | |
| Tick control (n = 108) | Done | 67 | 62.0 (52.2–71.2) |
| Not done | 41 | 38.0 (28.8–47.8) | |
| Method of tick control (n = 108) | No tick control | 41 | 38.0 (28.8–47.8) |
| Spraying | 55 | 50.9 (41.1–60.7) | |
| Dipping | 1 | 0.9 (0.0–5.1) | |
| Mixed methods | 11 | 10.2 (5.2–17.5) | |
| Tick control frequency (n = 108) | None | 41 | 38.0 (28.8–47.1) |
| Whenever necessary | 33 | 30.6 (22.2–40.2) | |
| Monthly | 19 | 17.6 (10.9–26.1) | |
| Fortnightly | 11 | 10.2 (5.2–17.5) | |
| Weekly | 4 | 3.7 (1.0–9.2) | |
| Farmer keeping other stock species (n = 108) | Yes | 107 | 99.1 (95.0–100.0) |
| No | 1 | 0.9 (0.0–5.1) |
n = number of herds included per factor; CI = Confidence Interval.
2.2. Tick Species Identified on Cattle
Five species of ticks were identified from the sampled cattle herds. Rhipicephalus decoloratus was present in all the sampled districts with herd infestation ranging from about 10.0% in Lilongwe West to 100% in Mchinji district. Hyalomma truncatum was present in 5 (Ntchisi, Dowa, Lilongwe East, Kasungu, and Mchinji) of the 7 study districts. Dowa had the highest herd infestation level of Hyalomma truncatum (70.0%) and whereas this species of tick was not observed in Dedza and Lilongwe West districts. Amblyomma variegetum, Rhipicephalus microplus, and Rhipecephalus appendiculatus were also present in the cattle herds. Figure 2 shows the distribution of the ticks in the cattle herds for each study district.
Figure 2.
Proportions of cattle herds infested with various tick species in the study districts. Abrevattions: A. var. = Amblyomma variegetum; Rh. dec. = Rhipicephalus decoloratus; Rh. mic. = Rhipicephalus microplus; Rh. App. = Rhipecephalus appendiculatus; and H. tru. = Hyalomma truncatum.
2.3. Seroprevalence of CCHFV Infection in Cattle
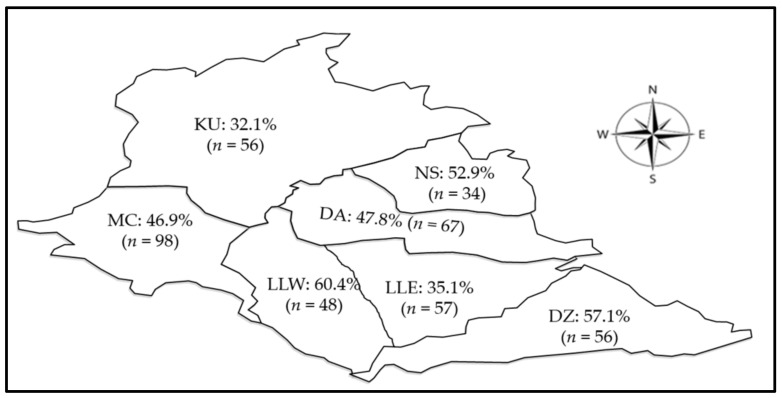
Individual cattle optic densities data used for the determination of cattle being positive for CCHFV antibody are shown in Figure S1 (Supplementary Materials available online). Out of 416 cattle, CCHFV antibodies were detected in 195 cattle, representing a seroprevalence of 46.9% (95% CI = 42.0–51.8). The seropositivity varied across the study sites (Figure 3), with the highest seroprevalence being observed in Lilongwe West (60.4%; 95% CI = 45.3–74.3%), followed by Dedza (57.1%; 95% CI = 43.2–70.3%) and the least seroprevalence was in Kasungu (32.1%; 95% CI = 20.3–46.0%).
Figure 3.
Spatial distribution of seropositivity (%) to CCHFV in cattle in the study area. Abbreviations: DZ = Dedza, DA = Dowa, LLE = Lilongwe East, LLW = Lilongwe West, KU = Kasungu, MC = Mchinji, and NS = Ntchisi.
2.4. Risk Factors Associated with Detection of CCHFV-Specific Antibodies in Cattle
Bivariate analysis (p-value < 0.25 cut-off point) was used to determine which risk factors were significantly associated with CCHF seropositivity (Table 2). These risk factors were district, age, sex, ticks on the herd, grazing land type, animal source, and herd size.
Table 2.
Summary of test of association analysis between potential risk factors and CCHFV seropositivity.
| Risk Factor | Category | n | Seroprevalence (%) | 95% CI | p-Value |
|---|---|---|---|---|---|
| District | Dedza | 56 | 57.1 | 43.2–70.3 | 0.025 * |
| Dowa | 67 | 47.8 | 35.4–60.3 | ||
| Kasungu | 56 | 32.1 | 20.3–46.0 | ||
| Lilongwe East | 57 | 35.1 | 22.9–48.9 | ||
| Lilongwe West | 48 | 60.4 | 45.3–74.2 | ||
| Mchinji | 98 | 46.9 | 36.9–57.3 | ||
| Ntchisi | 34 | 59.9 | 35.1–70.2 | ||
| Sex | Male | 208 | 36.5 | 30.0–43.5 | <0.001 * |
| Female | 208 | 57.2 | 50.2–64.0 | ||
| Age (Months) | 1–12 | 83 | 25.3 | 16.4–36.0 | <0.001 * |
| 13–24 | 80 | 31.3 | 21.4–42.6 | ||
| 25–48 | 151 | 58.3 | 50.0–66.2 | ||
| >48 | 102 | 59.8 | 49.6–69.4 | ||
| Ticks on herd | Present | 384 | 48.7 | 43.6–53.8 | 0.016 * |
| Absent | 32 | 25.0 | 11.5–43.4 | ||
| Grazing land type | Dambo | 326 | 44.8 | 39.3–50.4 | 0.013 * |
| Both (Dambo and upland) | 40 | 40.0 | 24.9–56.7 | ||
| Upland | 50 | 33.0 | 51.2–78.8 | ||
| Tick control | Done | 254 | 46.9 | 40.6–53.2 | 0.854 |
| Not done | 133 | 45.9 | 37.2–54.7 | ||
| Animal source | Within district | 331 | 57.7 | 42.2–53.3 | 0.241 * |
| Outside district | 56 | 39.3 | 26.5–53.3 | ||
| Presence of other stocks in herd | Present | 383 | 46.7 | 41.7–51.9 | 0.336 |
| Absent | 4 | 25.0 | 0.1–80.6 | ||
| Herd size | Small | 127 | 52.0 | 42.9–60.9 | 0.210 * |
| Medium | 113 | 48.7 | 39.2–58.3 | ||
| Large | 176 | 42.1 | 34.7–49.7 |
n= number of cattle involved, CI = confidence interval, * = statistically significant difference at p-value ≤ 0.25.
The maximum likelihood estimates for the risk factors that were significantly associated with CCHFV seropositivity in bivariate analysis (Table 3) were estimated. The odds of cattle being seropositive for CCHFV were more than four times for those older than 24 months when compared to those of twelve months and below. In addition, The odds of female cattle being seropositive were more than twice that of male cattle, while those with ticks were more than three times more likely to be seropositive than those that had no ticks. Cattle grazing in uplands were more than four times more likely to be seropositive than those grazing in the dambo. Further, seroprevalence differed significantly among some of the study districts.
Table 3.
Summary of maximum likelihood estimates for CCHFV seropositivity by risk factors determined.
| Risk Factor | Category | OR | CI | p-Value |
|---|---|---|---|---|
| District | Mchinji | r | ||
| Dedza | 2.2 | 1.0–4.9 | 0.050 * | |
| Dowa | 0.6 | 0.3–1.5 | 0.309 | |
| Kasungu | 0.7 | 0.3–1.6 | 0.408 | |
| Lilongwe East | 1.2 | 0.5–2.6 | 0.669 | |
| Lilongwe West | 2.8 | 1.2–6.5 | 0.016 * | |
| Ntchisi | 5.1 | 1.4–18.6 | 0.013 * | |
| Age (Months) | 1–12 | r | ||
| 13–24 | 1.2 | 0.6–2.6 | 0.626 | |
| 25–48 | 4.4 | 2.2–8.6 | <0.001 * | |
| >48 | 4.3 | 2.1–9.0 | <0.001 * | |
| Animal Sex | Male | r | ||
| Female | 2.5 | 1.6–4.0 | <0.001 * | |
| Ticks on herd | Absent | r | ||
| Present | 3.2 | 1.2–8.5 | 0.02 * | |
| Grazing land type | Dambo | r | ||
| Both (Dambo and Upland) | 0.5 | 0.2–1.5 | 0.244 | |
| Upland | 4.4 | 1.8–10.9 | 0.001 * |
* Statistically significant difference at p ≤ 0.05, OR = Odds Ratio, CI = confidence interval, and r = reference category.
3. Discussion
As the potential of emerging and re-emerging infectious diseases to cause public health emergencies such as pandemics is on the rise [41], epidemiological data of different pathogenic infectious agents is urgently needed to inform risk mitigation strategies. CCHF is increasingly becoming a global threat with the increased number of human cases being reported in the Middle East and the Balkans peninsula in the past decade [42]. In Africa, apart from South Africa where cases have been reported for decades [3,43], a number of human cases of CCHF were reported recently in Uganda [9] and Namibia [3]. CCHFV has been reported in several African countries in humans, animals, or ticks [4,23,44,45]. However, there are some countries whose CCHFV status is not known, and such countries are considered CCHFV free. The lack of, or poor, surveillance systems has been assumed to account for the failure of CCHFV detection in such countries. Malawi’s health surveillance system has been described as poor [46], with no surveillance system specific for CCHF, but the country is considered to be CCHF free. However, Malawi falls within a high potential risk region for CCHF occurrence because of the presence of Hyalomma ticks and conducive tropical climate [39,40,45]. Furthermore, CCHFV has been detected in cattle and ticks in the eastern province of Zambia [34], a region sharing a boundary with the study areas of this report. As such, the country requires close monitoring of CCHFV as well as other emerging and re-emerging vector-borne infectious diseases.
For the first time in Malawi, we report the exposure of cattle to CCHFV in the central region. These results support the idea of CCHFV infections occurring in animals in African countries where no human cases of CCHF have previously been reported. CCHF may be undetected due to lack of diagnostic capacity or lack of knowledge on CCHF among clinicians. Local and cross-border uncontrolled animal movement (through movements of viremic hosts) in Africa, Europe, and the Middle East, has been suggested as one of the mechanisms by which a vector-borne virus closely related to CCHFV, Rift Valley Fever virus is spreading in these regions [47,48,49]. In addition, uncontrolled animal movement due to porous borders in eastern, central, and southern Africa, has contributed to the spreading of different genotypes of the African swine fever virus (ASF) [50,51]. Similarly, this may also explain the spread of other infectious agents such as CCHFV within the region. The cattle seroprevalence reported in this study (46.9%) is comparatively higher than the global mean cattle CCHFV seroprevalence of 18.6% [23]. It was also high when compared to CCHFV seroprevalence reported in the Democratic Republic of Congo (DRC) (0.4%) [4,52]. However, it is less than what has been reported in Uganda (75.0%), Mali (66.0%), Mauritania (67.0%), and Senegal (57.1%) [24,53,54,55].
Apart from the true variation in seroprevalence, the reported seroprevalence rates are also dependent on the diagnostic tests used [4,24]. For instance, the CCHFV double antigen ELISA test employed in the present study detects both IgG and IgM [56] and uses a larger volume of serum sample [57], compared to other forms of ELISA tests that detect either IgG or IgM only, a scenario which may contribute higher seroprevalence. However, some studies which have used an ELISA method that detects only IgG or IgM CCHFV antibodies have reported higher seroprevalence than those of the present study [4,58,59], indicating that other factors could be at play.
The seroprevalence of CCHFV is associated with many risk factors. Geographical location, sex, age, and presence of ticks in cattle herds have been reported and discussed in previous studies as among the risk factors for CCHFV [55,59,60,61]. In addition, this study found high seroprevalence in cattle grazed in uplands compared to those grazed in dambos. Hyalomma ticks prefer drier environments [62], making uplands more likely to have CCHFV vector ticks compared to the dambos, which are wet most of the time. However, in this study, high seroprevalence was observed in Lilongwe West and Dedza, districts that had no Hyalomma ticks. Since tick activity varies with the season of the year [62] and in the present study samples were collected at a single point in time, the generated results on prevailing ticks are not enough evidence to conclude the absence of Hyalomma ticks and other tick species in other districts. Further, CCHFV had been detected in many other tick genera as Rhipicephalus, Amblyomma, though, vector competency has not been confirmed in these ticks [1,63,64,65]. Based on these observations, vector competency of tick species other than Hyalomma species has to be explored in this study area.
Some studies have reported no association between the sex of cattle [60] and of camels [61] and being CCHFV seropositive. However, one study reported that cattle gender was associated with the risk of an animal being infected with CCHFV [55], a finding which is similar to the results of this present study where female cattle were observed to have a higher risk than males. Female cattle are raised mainly for breeding purposes making them spend more time in the fields grazing and thus have an increased risk of being exposed to ticks. In contrast, older male cattle are used for drought power and stay away from grazing areas longer than female and young cattle, particularly during the rainy season when cultivation of crops is at its peak. This period also coincides with increased tick activity. Consequently, we surmise that male cattle may be less frequently exposed to ticks and this could explain why female animals are at increased risk of CCHFV exposure.
Older cattle had a higher odds of being CCHFV seropositive compared to younger ones (12 months or less). Cumulative exposure to ticks and tick-borne pathogens increases as animals age [66], thus explaining the higher odds of CCHFV seropositivity in older animals. The presence of other livestock species was not found to be a risk factor for CCHFV seropositivity in the present study. This is similar to the findings of Adam et al. [60], who also observed no significant association between the presence of other livestock and increased CCHFV seropositivity. In the current study, a larger proportion (99.1%) of farmers also kept other livestock species. Thus, there was not enough representation of farmers keeping cattle only to generate enough statistical power to detect such a difference if it existed in our study population.
This study found that the absence of ticks on cattle was associated with reduced odds of cattle being seropositive for CCHFV. A reduced CCHFV seropositivity was also observed to be associated with the absence of ticks in camels (Camelus dromedaries) [61]. However, the odds ratio was not statistically significant between cattle where ticks were controlled and those in which ticks were not controlled, an observation that has been reported previously [60]. Cattle raised communally mingle during grazing with other cattle herds and other livestock in general. Such communal cattle grazing along with irregular tick control protocols in some cattle herds can render tick control efforts ineffective.
This study is not without limitations. A limitation in this study includes the use of a questionnaire to obtain information regarding farmer demographics and the management of animals. This approach is subject to recall liabilities and truthfulness of the respondents. The study was also limited by a lack of supportive information like information on tick resistance to acaricides, in the study area, which could also help to explain or justify the ineffectiveness of tick control measures.
4. Materials and Methods
4.1. Study Sites
The study was conducted in the central region of Malawi in April 2020. Malawi, located in southern Africa, is a landlocked and agriculture-based country covering 118,484 km2. It is located within latitudes 9° and 18°S, and longitudes 32° to 36° E and is bordered by Tanzania to the north, Mozambique to the east, south, and southwest, and Zambia to the west. The study was conducted in the Lilongwe-Kasungu plain (covering Kasungu and part of Lilongwe agricultural development divisions (ADD) in the central part of the country (Figure 4). The plain has a savanna tropical climate and experiences a hot-dry summer (September to November), hot-wet summer (December to April; rainfall ranges from 750 to 1200 mm per annum), and moderate winter (May to August) seasons. The study area for the present study, Lilongwe-Kasungu plain, is known to be infested with Hyalomma ticks [37] and was thus purposefully selected.
Figure 4.
Map of Malawi showing the seven study districts and Malawi’s neighboring countries.
4.2. Study and Sampling Design
The study was cross-sectional in design. Sample collection centers (village centers or veterinary stations) were randomly identified in the study districts. A herd was defined as all cattle groupings under one management custody [67]. Smallholder cattle farmer registers were used as sampling frames. As such, herds were selected using a systematic random sampling technique. Since individual cattle were not identified within herds, arbitrary numbers were assigned to individual animals within a herd which was later used for simple random selection by a raffle draw. The study included cattle of all ages and sexes that were raised communally in the study area. However, the study excluded heavily pregnant (second and third trimesters) cows and clinically ill cattle to avoid stressing the animals.
The sample size was determined through proportional probability using Ausvet EpiTools software (http://epitools.ausvet.com.au/ accessed on 6 May 2019). A total sample size of 436 cattle was determined using the following parameters: 50% prevalence (no established prevalence in the study area was available), 6% relative precision, 95% confidence level, and 1.5 design effect [68].
4.3. Questionnaire Administration
A structured questionnaire, in the local language (Chewa), was administered to cattle farmers through face-to-face interviews. The questionnaire was designed to collect information such as smallholder farmer demographics, herd size categorized as small (1–6 animals), medium (7–14 animals), and large (>14), source of animals (within or outside the district); ticks on herd (present or absent), tick control measures (spraying or dipping), and type of grazing land (dambo = low lying waterlogged wetlands; upland = elevated and generally drier; or in both (dambo and upland)). Selected cattle owners who did not consent to participate in the questionnaire or to allow their animals to be sampled were replaced by other cattle owners from the same sample collection center.
4.4. Cattle Attributes
Due to lack of written records, cattle owners recalled the age of the sampled animals, and when in doubt, the investigator estimated the age by dentition method [69,70]. Animal sex and the presence of ticks were recorded as male or female and present or absent, respectively, following a visual inspection.
4.5. Sample (Sera and Tick) Collection from Cattle, Storage, and Transportation
Approximately five (5) milliliters of whole blood was aseptically collected in a plain vacutainer tube from each sampled animal through the jugular or coccygeal venipuncture approaches. Iodine, to clean the blood collection site, and sterile disposable needles were used to achieve aseptic standards. Sample tube labeling included animal number, district, collection center, herd number, date of sample collection, and sample type. Whole blood samples were allowed to clot overnight before serum was separated by centrifugation at 1000× g for 15 min as per World Organization for Animal Health protocol [71] and later aliquoted into two milliliter Eppendorf tubes.
Ticks were handpicked from cattle body surfaces. The picked ticks were collected in 50 mL falcon tubes with perforated lids for ventilation. Fresh pieces of grass/leaves were added to each tube to provide humidity for the ticks. Each tube was labeled according to the district, collection center, herd number, and date of tick collection. Ticks were transported to the Central Veterinary Laboratory (CVL) in Lilongwe, where they were stored at 18 °C until identification using morphological features [62]. Thereafter, both sera and ticks were then stored at −80 °C at the African Union Centre of Excellence for Tick and Tick-borne diseases (AU-CTTBD), Lilongwe, Malawi.
4.6. Enzyme-Linked Immunosorbent Assay (ELISA)
All the 416 serum samples were subjected to sandwich ID Screen© CCHF Double Antigen Multi-Species Enzyme-Linked Immunosorbent Assay test (IDvet, Grabels, France). All the reagents and controls were provided in the kit and were reconstituted and tests were carried out following the manufacturer’s instructions. All samples and controls were run in duplicates, and the average of the duplicates was considered as the test result. This assay, simultaneously and indiscriminately, detected both IgM and IgG with the sensitivity of 98.9% and specificity of 100% [56]. A test run was considered valid if the mean optic density of the positive control (ODpc) was greater than 0.35, and the ratio of the mean ODpc to mean optic density for negative control (ODnc) was greater than 3. Interpretations of the test ODs were based on the ratio of the mean sample optic density to ODpc, expressed as a percentage (S/p × 100). Samples with S/p% less or equal to 30% were considered negative, and samples with S/p% greater than 30% were considered positive. Table S1 shows validation data for all (10) plates that were run and all the runs were valid on both criteria.
4.7. Data Analysis
All data were entered, cleaned, and validated in Microsoft™ excel spreadsheet. The CCHFV ELISA test results (positive or negative) were the only dependent variable in this study. Descriptive and inferential analyses were performed in IBM SPSS version 20 (IBM Corp, Armonk, NY, USA) and MS Office Excel® 2016. Bivariate analysis was performed using the Pearson Chi-Square test of association (and Fisher’s exact test, where appropriate) at a significance level of p < 0.25. All the factors that were significant at bivariate analysis were used to model the odds ratios of CCHFV seropositivity. Multivariate analysis was done using a stepwise binary logistic regression model for categorical outcome at the significance level of p ≤ 0.05. All the tests were performed at a 95% confidence level. Missing data were coded as −99 and were non-informative in all the models. A significant Omnibus Test for Model coefficients (p < 0.050) and a non-significant Hosmer and Lemeshow Test (p > 0.050) were used to check whether the model fitted the data.
5. Conclusions
This study, for the first time, has provided serologic evidence of the circulation of CCHFV in cattle kept by smallholder farmers in central Malawi and identified several risk factors for CCHFV seropositivity. The study stresses the need for continued monitoring of CCHFV infection among livestock, ticks, and humans to assist with the development of evidence-based control strategies. Countrywide studies to identify potential CCHFV hot spots in animals, vectors and humans are highly recommended for prudent risk mitigation.
Acknowledgments
The authors would like to acknowledge the support from P. Chikungwa, and J. Chulu; staff of Central Veterinary Laboratory, Kasungu ADD and Lilongwe ADD during the study implementation. Authors also acknowledge the special support from smallholder cattle farmers of Kasungu and Lilongwe ADDS in making this study possible.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/pathogens10121613/s1, Table S1: mean Optic Densities (OD) for positive and negative controls and their calculated ratios; and Figure S1: Ratios of Optic densities for the sample to Optic density for the positive control in percentages.
Author Contributions
Conceptualization, M.C.P., M.C.S. and E.S.; data curation, M.C.P., M.C.S. and E.S.; formal analysis, M.C.P., M.C.S., S.K. and E.S.; funding acquisition, M.C.S., H.S. and E.S.; investigation, M.C.P., M.C.S., H.K., J.N., M.C., K.C., W.M., M.K. and E.S.; methodology, M.C.P., M.C.S., M.K. and E.S.; project administration, M.C.P., M.C.S., G.N. and E.S.; resources, M.C.S., H.S., G.N. and E.S.; supervision, M.C.S., G.N. and E.S.; validation, M.C.P., M.C.S. and E.S.; visualization, M.C.P., M.C.S., E.C. and E.S.; writing—original draft, M.C.P. and E.S.; writing—review & editing, M.C.P., M.C.S., H.K., M.C., E.C., S.K., K.C., W.M., B.M., S.C., M.K., H.S., G.N., A.T. and E.S. All authors have read and agreed to the published version of the manuscript.
Funding
The study was supported in-part by: the Africa Centre of Excellence for Infectious Diseases of Humans and Animals (ACEIDHA) project (grant # P151847) funded by the World Bank; grant for the AMED and Japan International Cooperation Agency (JICA) within the framework of the Science and Technology Research Partnership for Sustainable Development (SATREPS) (JP22212m0110019), the Japan Agency for Medical Research and Development (JP21wm0125008), and the Government of the Republic of Malawi.
Institutional Review Board Statement
The Animal Health Committee of the Department of Animal Health and Livestock Development (DAHLD-AHC: Ref. AHC/01/2020), Malawi and the University of Zambia Biomedical Research Ethical Committee (UNZABREC: Ref. 780-2020), Zambia; independently reviewed and approved the research protocol. Samples were imported into Zambia with authorization from the Department of Veterinary Services of the Ministry of Livestock and Fisheries, Zambia: permit number 56/2020(VTHQ/8/3/18).
Informed Consent Statement
Cattle herd owners (farmers) verbally consented before being interviewed and samples being collected from their cattle. Animal safety and welfare were guaranteed by use of appropriate restraining methods (Barley rope or halter methods) and observance of aseptic techniques when bleeding cattle.
Data Availability Statement
All data have been provided in the article and/or as Supplementary Materials.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hoogstraal H. Changing Patterns of Tick-borne Diseases in Modern Society. Annu. Rev. Entomol. 1981;26:75–99. doi: 10.1146/annurev.en.26.010181.000451. [DOI] [PubMed] [Google Scholar]
- 2.Maes P., Alkhovsky S.V., Bào Y., Beer M., Birkhead M., Briese T., Buchmeier M.J., Calisher C.H., Charrel R.N., Choi I.R., et al. Taxonomy of the order Bunyavirales: Second update 2018. Arch. Virol. 2019;164:927–941. doi: 10.1007/s00705-018-04127-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kuehnert P.A., Stefan C.P., Badger C.V., Ricks K.M. Crimean-Congo Hemorrhagic Fever Virus (CCHFV): A Silent but Widespread Threat. Curr. Trop. Med. Rep. 2021;8:141–147. doi: 10.1007/s40475-021-00235-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spengler J.R., Bergeron E., Rollin P.E. Seroepidemiological Studies of Crimean-Congo Hemorrhagic Fever Virus in Domestic and Wild Animals. PLoS Negl. Trop. Dis. 2016;10:e0004210. doi: 10.1371/journal.pntd.0004210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mourya D.T., Yadav P.D., Shete A.M., Gurav Y.K., Raut C.G., Jadi R.S., Pawar S.D., Nichol S.T., Mishra A.C. Detection, Isolation and Confirmation of Crimean-Congo Hemorrhagic Fever Virus in Human, Ticks and Animals in Ahmadabad, India, 2010–2011. PLoS Negl. Trop. Dis. 2012;6:e1653. doi: 10.1371/journal.pntd.0001653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Müller M.A., Devignot S., Lattwein E., Corman M.V., Maganga G.D., Gloza-Rausch F., Binger T., Vallo P., Emmerich P., Cottontail V.M., et al. Evidence for Widespread Infection of African Bats with Crimean-Congo Hemorrhagic Fever-like Viruses. Nat. Publ. Group. 2016;6:1–10. doi: 10.1038/srep26637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeller H.G., Cornet J.P., Camicas J.L. Crimean-Congo Haemorrhagic Fever Virus Infection in Birds: Field Investigations in Senegal. Res. Virol. 1994;145:105–109. doi: 10.1016/S0923-2516(07)80012-4. [DOI] [PubMed] [Google Scholar]
- 8.Verma R., Khanna P., Prinja S., Rajput M. Crimean-Congo hemorrhagic fever: An outbreak in India. Aust. Med. J. 2011;4:589–591. doi: 10.4066/AMJ.2011.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balinandi S., Patel K., Ojwang J., Kyondo J., Mulei S., Tumusiime A., Lubwama B., Nyakarahuka L., Klena J.D., Lutwama J., et al. Investigation of an isolated case of human Crimean-Congo hemorrhagic fever in Central Uganda. Int. J. Infect. Dis. 2015;68:88–93. doi: 10.1016/j.ijid.2018.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abbas T., Xu Z., Younus M., Qayyum A., Riaz M.T. Seasonality in hospital admissions of Crimean-Congo hemorrhagic fever and its dependence on ambient temperature-empirical evidence from Pakistan. Int. J. Biometeorol. 2017;61:1893–1897. doi: 10.1007/s00484-017-1359-4. [DOI] [PubMed] [Google Scholar]
- 11.Hoogstraal H. The epidemiology of tick-borne Crimean-Congo hemorrhagic fever in Asia, Europe, and Africa. J. Med. Entomol. 1979;15:307–417. doi: 10.1093/jmedent/15.4.307. [DOI] [PubMed] [Google Scholar]
- 12.Hawman D.W., Feldmann H. Recent advances in understanding Crimean-Congo hemorrhagic fever virus. F1000 Fac. Rev. 2018;7:1715. doi: 10.12688/f1000research.16189.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-Abri S.S., Abaidani I.A., Fazlalipour M., Mostafavi E., Leblebicioglu H., Pshenichnaya N., Memish Z.A., Hewson R., Petersen E., Mala P., et al. Current status of Crimean-Congo hemorrhagic fever in the World Health Organization Eastern Mediterranean Region: Issues, challenges, and future directions. Int. J. Infect Dis. 2017;58:82–89. doi: 10.1016/j.ijid.2017.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goswami T.K., Singh D.K., Saminathan M., Verma A.K., Dhama K. An Emerging Threat of Crimean Congo Hemorrhagic Fever: Call for Preparedness. Adv. Anim. Vet. Sci. 2014;2:8–14. doi: 10.14737/journal.aavs/2014.2.1.8.14. [DOI] [Google Scholar]
- 15.Mertens M., Vatansever Z., Mrenoshki S., Krstevski K., Stefanovska J., Djadjovski I., Cvetkovikj I., Farkas R., Schuster I., Donnet F., et al. Circulation of Crimean-Congo Hemorrhagic Fever Virus in the Former Yugoslav Republic of Macedonia Revealed by Screening of Cattle Sera Using a Novel Enzyme-linked Immunosorbent Assay. PLoS Negl. Trop. Dis. 2015;9:e0003519. doi: 10.1371/journal.pntd.0003519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fajs L., Jakupi X., Ahmeti S., Humolli I., Dedushaj I., Avsic-Zupanc T. Molecular Epidemiology of Crimean-Congo Hemorrhagic Fever Virus in Kosovo. PLoS Negl. Trop. Dis. 2014;8:e2647. doi: 10.1371/journal.pntd.0002647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.WHO Introduction to Crimean-Congo Hemorrhagic Fever. 2018. [(accessed on 23 November 2020)]. Available online: https://www.who.int/publications/i/item/introduction-to-crimean-congo-haemorrhaigc-feveron.
- 18.Sorvillo T.E., Rodriguez S.E., Hudson P., Carey M., Rodriguez L.L., Spiropoulou C.F., Bird B.H., Spengler J.R., Bente D.A. Towards a Sustainable One Health Approach to Crimean-Congo Hemorrhagic Fever Prevention: Focus Areas and Gaps in Knowledge. Trop. Med. Infect. Dis. 2020;5:113. doi: 10.3390/tropicalmed5030113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bartolini B., Gruber C.E.M., Koopmans M., Avšič T., Bino S., Christova I., Grunow R., Hewson R., Korukluoglu G., Lemos C.M., et al. Laboratory management of Crimean-Congo haemorrhagic fever virus infections: Perspectives from two European networks. Eurosurveillance. 2019;24:1800093. doi: 10.2807/1560-7917.ES.2019.24.5.1800093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bergeron E., Zivcec M., Chakrabarti A.K., Nichol S.T., Albariño C.G., Spiropoulou C.F. Recovery of Recombinant Crimean Congo Hemorrhagic Fever Virus Reveals a Function for Non-structural Glycoproteins Cleavage by Furin. PLoS Pathog. 2015;11:e1004879. doi: 10.1371/journal.ppat.1004879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Escadafal C., Ölschläger S., Avšič-Županc T., Papa A., Vanhomwegen J., Wolf R., Mirazimi A., Teichmann A., Donoso-Mantke O., Niedrig M. First International External Quality Assessment of Molecular Detection of Crimean-Congo Hemorrhagic Fever Virus. PLoS Negl. Trop. Dis. 2012;6:e1706. doi: 10.1371/journal.pntd.0001706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Munibullah, Yousaf A., Shah M.A., Habibullah, Sadia H., Sohoo. M.R. Crimean—Congo Hemorrhagic Fever a Threat to Public Health. [(accessed on 23 June 2020)];J. Bacteriol. Infec. Dis. 2018 2:1–7. Available online: https://www.alliedacademies.org/articles/crimeancongo-hemorrhagic-fever-a-threat-to-public-health-10191.html. [Google Scholar]
- 23.Nasirian H. Crimean-Congo hemorrhagic fever (CCHF) seroprevalence: A systematic review and meta-analysis. Acta. Trop. 2019;196:102–120. doi: 10.1016/j.actatropica.2019.05.019. [DOI] [PubMed] [Google Scholar]
- 24.Balinandi S., von Brömssen C., Tumusiime A., Kyondo J., Kwon H., Monteil V.M., Ali Mirazimi A., Lutwama J., Mugisha L., Malmberg M. Serological and molecular study of Crimean-Congo Hemorrhagic Fever Virus in cattle from selected districts in Uganda. J. Virol. Methods. 2021;290:114075. doi: 10.1016/j.jviromet.2021.114075. [DOI] [PubMed] [Google Scholar]
- 25.Vescio F.M., Busani L., Mughini-Gras L., Khoury C., Avellis L., Taseva E., Rezza G., Christova I. Environmental correlates of Crimean-Congo hemorrhagic fever incidence in Bulgaria. BMC Public Health. 2012;12:1116. doi: 10.1186/1471-2458-12-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Palomar A.M., Portillo A., Santibáñez P., Mazuelas D., Arizaga J., Crespo A., Gutiérrez O., Cuadrado J.F., Oteo J.A. Crimean-Congo Hemorrhagic Fever Virus in Ticks from Migratory Birds, Morocco. Emerg. Infect. Dis. 2013;19:260–263. doi: 10.3201/eid1902.121193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wahid B., Altaf S., Naeem N., Ilyas N., Idrees M. Scoping Review of Crimean-Congo Hemorrhagic Fever (CCHF) Literature and Implications of Future Research. J. Coll. Physicians Surg. Pak. 2019;29:563–573. doi: 10.29271/jcpsp.2019.06.563. [DOI] [PubMed] [Google Scholar]
- 28.Rehman K., Bettani M.A.K., Veletzky L., Afridi S., Ramharter M. Outbreak of Crimean-Congo hemorrhagic fever with atypical clinical presentation in the Karak District of Khyber Pakhtunkhwa, Pakistan. Infect. Dis. Poverty. 2018;7:116. doi: 10.1186/s40249-018-0499-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Richards G.A., Weyer J., Blumberg L. Viral Haemorrhagic Fevers in South Africa. S. Afr. Med. J. 2015;105:748–751. doi: 10.7196/SAMJnew.8330. [DOI] [PubMed] [Google Scholar]
- 30.Jauréguiberry S., Tattevin P., Tarantola A., Legay F., Tall A., Nabeth P., Zeller H., Michelet C. Imported Crimean-Congo hemorrhagic Fever. J. Clin. Microbiol. 2005;43:4905–4907. doi: 10.1128/JCM.43.9.4905-4907.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leblebicioglu H., Ozaras R., Fletcher T.E., Beeching N.J., ESCMID Study Group for Infections in Travelers and Migrants (ESGITM) Crimean-Congo hemorrhagic fever in travelers: A systematic review. Travel Med. Infect. Dis. 2016;14:73–80. doi: 10.1016/j.tmaid.2016.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Temur A.I., Jens H.K., David B.P., Dmitry A., Maryam K. Epidemiology of Crimean-Congo Hemorrhagic Fever (CCHF) in Africa—Underestimated for Decades. Am. J. Trop. Med. Hyg. 2021;104:1978–1990. doi: 10.4269/ajtmh.20-1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Muianga A.F., Watson R., Varghese A., Chongo I.S., Ali S., Monteiro V., Inalda F., Chelene I., António V., Hewson R., et al. First serological evidence of Crimean-Congo haemorrhagic fever in febrile patients in Mozambique. Int. J. Infect. Dis. 2017;62:119–123. doi: 10.1016/j.ijid.2017.07.024. [DOI] [PubMed] [Google Scholar]
- 34.Kajihara M., Simuunza M., Saasa N., Dautu G., Mori-Kajihara A., Qiu Y., Nakao R., Eto Y., Furumoto H., Bernard M., et al. Serologic and molecular evidence for circulation of Crimean-Congo hemorrhagic fever virus in ticks and cattle in Zambia. PLoS Negl. Trop. Dis. 2021;15:e0009452. doi: 10.1371/journal.pntd.0009452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mares R.G. Animal health and production in Malawi past, present and future. Trop. Anim. Health Prod. 1973;5:272–277. doi: 10.1007/BF02240428. [DOI] [PubMed] [Google Scholar]
- 36.National Statistical Office of Malawi Malawi Population and Housing Main Report 2018 (May) [(accessed on 2 January 2021)]. Available online: https://malawi.unfpa.org/sites/default/files/resourcepdf/2018.
- 37.Ministry of Agriculture, Department of Animal Health and Livestock Development . Ministry of Agriculture, Department of Animal Health and Livestock Development; Lilongwe, Malawi: 2006. [(accessed on 2 January 2021)]. Policy Document on Livestock in Malawi. Available online: http://extwprlegs1.fao.org/docs/pdf/mlw169552.pdf. [Google Scholar]
- 38.Li G., Messina J.P., Peter B.G., Snapp S.S. Mapping Land Suitability for Agriculture in Malawi. Land Degrad. Dev. 2017;28:2001–2016. doi: 10.1002/ldr.2723. [DOI] [Google Scholar]
- 39.Pigott D.M., Deshpande A., Letourneau I., Morozoff C., Reiner Jr R.C., Kraemer M.U.G., Brent S.E., Bogoch I.I., Khan K., Biehl M.H., et al. Local, National, and Regional Viral Haemorrhagic Fever Pandemic Potential in Africa: A Multistage Analysis. Lancet. 2017;390:2662–2672. doi: 10.1016/S0140-6736(17)32092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Berggren S.A. Cattle ticks in Malawi. Vet. Parasitol. 1978;4:289–297. doi: 10.1016/0304-4017(78)90055-9. [DOI] [Google Scholar]
- 41.Schwartz J., Yen M.Y. Toward a Collaborative Model of Pandemic Preparedness and Response: Taiwan’s Changing Approach to Pandemics. J. Microbiol. Immunol. Infect. 2017;50:125–132. doi: 10.1016/j.jmii.2016.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nasirian H. New Aspects about Crimean-Congo Hemorrhagic Fever (CCHF) Cases and Associated Fatality Trends: A Global Systematic Review and Meta-Analysis. Comp. Immunol. Microbiol. Infect. Dis. 2020;69:e101429. doi: 10.1016/j.cimid.2020.101429. [DOI] [PubMed] [Google Scholar]
- 43.Swanepoel R., Shepherd A.J., Leman P.A., Shepherd S.P., McGillivray G.M., Erasmus M.J., . Searle L.A., Gill D.E. Epidemiologic and clinical features of Crimean-Congo hemorrhagic fever in southern Africa. Am. J. Trop. Med. Hyg. 1987;36:120–132. doi: 10.4269/ajtmh.1987.36.120. [DOI] [PubMed] [Google Scholar]
- 44.Chauhan R.P., Zelalem G.D., Noreddin A., El Zowalaty M.E. Systematic Review of Important Viral Diseases in Africa in Light of the ‘One Health’ Concept. Pathogens. 2020;9:301. doi: 10.3390/pathogens9040301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Messina J.P., Pigott D.M., Golding N., Duda K.A., Brownstein J.S., Weissa D.J., Gibsona H., Robinsond T.P., Gilberte M., Winta G.R.W., et al. The global distribution of Crimean-Congo hemorrhagic fever. Trans. R. Soc. Trop. Med. Hyg. 2015;109:503–513. doi: 10.1093/trstmh/trv050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Joseph Wu T.S., Kagoli M., Kaasbøll J.J., Bjune G.A. Integrated Disease Surveillance and Response (IDSR) in Malawi: Implementation gaps and challenges for timely alert. PLoS ONE. 2018;13:e0200858. doi: 10.1371/journal.pone.0200858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Himeidan Y.E., Kweka E.J., Mahgoub M.M., El Amin A., El Rayah A., Ouma J.O. Recent Outbreaks of Rift Valley Fever in East Africa and the Middle East. Front. Public Health. 2014;2:169. doi: 10.3389/fpubh.2014.00169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nielsen S.S., Alvarez J., Bicout D.J., Calistri P., Depner K., Drewe J.A., Garin-Bastuji B., Rojas J.L.G., Schmidt C.G., Michel V., et al. Rift Valley Fever—Epidemiological Update and Risk of Introduction into Europe. EFSA J. 2020;18:e06041. doi: 10.2903/j.efsa.2020.6041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tran A., Lutwama J., Sserugga J., Gély M., Pittiglio C., Pinto J., Chevalier V. Development and Assessment of a Geographic Knowledge-Based Model for Mapping Suitable Areas for Rift Valley Fever Transmission in Eastern Africa. PLoS Negl. Trop. Dis. 2016;10:e0004999. doi: 10.1371/journal.pntd.0004999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hakizimana J.N., Yona C., Kamana O., Nauwynck H., Misinzo G. African Swine fever Virus Circulation between Tanzania and Neighboring Countries: A Systematic Review and Meta-Analysis. Viruses. 2021;13:306. doi: 10.3390/v13020306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Simulundu E., Chambaro. H.M., Sinkala Y., Kajihara M., Ogawa H., Mori A., Ndebe J., Dautu G., Mataa L., Lubaba C.H., et al. Co-circulation of multiple genotypes of African swine fever viruses among domestic pigs in Zambia (2013–2015) Transbound. Emerg. Dis. 2018;65:114–122. doi: 10.1111/tbed.12635. [DOI] [PubMed] [Google Scholar]
- 52.Sas M.A., Mertens M., Kadiat J.G., Schuster I., Pongombo C.P.S., Maloba A.G.K., Groschup M.H. Serosurvey for Crimean-Congo Hemorrhagic Fever Virus Infections in Ruminants in Katanga Province, the Democratic Republic of the Congo. Ticks Tick Borne Dis. 2017;8:858–861. doi: 10.1016/j.ttbdis.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 53.Maiga O., Sas M.A., Rosenke K., Kamissoko B., Mertens M., Sogoba N., Traore A., Sangare M., Niang M., Schwan T.G., et al. Serosurvey of Crimean-Congo Hemorrhagic Fever Virus in Cattle, Mali, West Africa. Am. J. Trop. Med. Hyg. 2017;96:1341–1345. doi: 10.4269/ajtmh.16-0818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sas M.A., Mertens M., Isselmou E., Reimer N., Mamy B., Doumbia B., Groschup M.H. Crimean-Congo Hemorrhagic Fever Virus-Specific Antibody Detection in Cattle in Mauritania. Vector Borne Zoonotic Dis. 2017;17:582–587. doi: 10.1089/vbz.2016.2084. [DOI] [PubMed] [Google Scholar]
- 55.Mangombi J.B., Roqueplo C., Sambou M., Dahmani M., Mediannikov O., Comtet L., Davoust B. Seroprevalence of Crimean-Congo Hemorrhagic Fever in Domesticated Animals in Northwestern Senegal. Vector Borne Zoonotic Dis. 2020;20:797–799. doi: 10.1089/vbz.2019.2592. [DOI] [PubMed] [Google Scholar]
- 56.Sas M.A., Loic Comtet L., Donnet F., Mertens M., Tordo N., Pourquier P., Groschup M.H. A Novel Double-Antigen Sandwich ELISA for the Species-Independent Detection of Crimean-Congo Hemorrhagic Fever Virus-Specific Antibodies. Antivir. Res. 2018;151:24–26. doi: 10.1016/j.antiviral.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 57.Ibrahim A.M., Adam I.A., Osman B.T., Aradaib I.E. Epidemiological survey of Crimean Congo hemorrhagic fever virus in cattle in East Darfur State, Sudan. Ticks Tick Borne Dis. 2015;6:439–444. doi: 10.1016/j.ttbdis.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 58.Msimang V., Weyer j., Le Roux C., Kemp A., Burt F.J., Tempia S., Grobbelaar A., Moolla N., Rostal M.K., Bagge W., et al. Risk Factors Associated with Exposure to Crimean-Congo Haemorrhagic Fever Virus in Animal Workers and Cattle, and Molecular Detection in Ticks, South Africa. PLoS Negl. Trop. Dis. 2021;15:e0009384. doi: 10.1371/journal.pntd.0009384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Schulz A., Barry Y., Stoek F., Ba A., Schulz J., Haki M.L., Sas M.A., Doumbia B.A., Kirkland P., Bah M.Y., et al. Crimean-Congo Hemorrhagic Fever Virus Antibody Prevalence in Mauritanian Livestock (Cattle, Goats, Sheep and Camels) Is Stratified by the Animal’s Age. PLoS Negl. Trop. Dis. 2021;15:e0009228. doi: 10.1371/journal.pntd.0009228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Adam I.A., Mahmoud M.A.M., Aradaib I.E. A seroepidemiological survey of Crimean Congo hemorrhagic fever among Cattle in North Kordufan State, Sudan. Virol. J. 2013;10:178. doi: 10.1186/1743-422X-10-178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Suliman H.M., Adam I.A., Saeed S.I., Abdelaziz S.A., Haroun E.M., Aradaib I.E. Crimean Congo Hemorrhagic Fever among the One-Humped Camel (Camelus Dromedaries) in Central Sudan. Virol. J. 2017;14:147. doi: 10.1186/s12985-017-0816-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Walker A.R., Bouattor A., Camicas J.L., Estrada-Pena A., Horak I.G., Latif A.A., Pegram R.G., Preston P.M. Ticks of Domestic Animals in Africa: A Guide to Identification of Species. Bioscience Reports; Edinburgh, UK: 2003. pp. 1–221. [Google Scholar]
- 63.Akuffo R., Brandful J.A.M., Zayed A., Adjei A., Watany N., Fahmy N.T., Hughes R., Doman B., Voegborlo S.V., Aziati D., et al. Crimean-Congo Hemorrhagic Fever Virus in Livestock Ticks and Animal Handler Seroprevalence at an Abattoir in Ghana. BMC Infect. Dis. 2016;16:324. doi: 10.1186/s12879-016-1660-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ozdarendeli A., Aydin K., Tonbak S., Aktas M., Altay K., Koksal I.Y., Bolat Y., Dumanli N., Kalkan A. Genetic Analysis of the M RNA Segment of Crimean-Congo Hemorrhagic Fever Virus Strains in Turkey. Arch. Virol. 2008;153:37–44. doi: 10.1007/s00705-007-1056-4. [DOI] [PubMed] [Google Scholar]
- 65.Telmadarraiy Z., Ghiasi S.M., Moradi M., Vatandoost H., Eshraghian M.R., Faghihi F., Zarei Z., Haeri A., Chinikar S. A Survey of Crimean-Congo Haemorrhagic Fever in Livestock and Ticks in Ardabil Province, Iran during 2004-2005. Scand. J. Infect. Dis. 2010;42:137–141. doi: 10.3109/00365540903362501. [DOI] [PubMed] [Google Scholar]
- 66.Simuunza M., Weir W., Courcier E., Tait A., Shiels B. Epidemiological Analysis of Tick-Borne Diseases in Zambia. Vet. Parasitol. 2011;175:331–342. doi: 10.1016/j.vetpar.2010.09.027. [DOI] [PubMed] [Google Scholar]
- 67.Munyeme M., Muma J.B., Munang’andu H.M., Kankya C., Skjerve E., Tryland M. Cattle Owners’ Awareness of Bovine Tuberculosis in High and Low Prevalence Settings of the Wildlife-Livestock Interface Areas in Zambia. BMC Vet. Res. 2010;6:21. doi: 10.1186/1746-6148-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dohoo I., Martin W., Stryhn H. Vol. 88. AVC Inc.; Charlottetown, PE, Canada: 2004. [(accessed on 6 March 2021)]. Veterinary Epidemiologic Research; pp. 38–49. Available online: https://epdf.pub/veterinary-epidemiologic-research.html. [Google Scholar]
- 69.Torell R., Bruce B., Kvasnicka B. University of Nevada; Reno, NV, USA: 2003. [(accessed on 6 February 2021)]. Methods of Determining Age of Cattle. Cattle Producer’s Library: CL712; pp. 1–3. Available online: www.avc-beef.org/AgingCattle-Griffin/AgingCattle-CL712.pdf. [Google Scholar]
- 70.Mushonga B., Shinexuugi I., Mbiri P., Samkange A., Madzingira O., Kandiwa E. Applicability of teeth examination as a tool for age estimation in a semi-arid cattle production environment in Namibia. Trop. Anim. Health Prod. 2020;52:1649–1654. doi: 10.1007/s11250-019-02172-x. [DOI] [PubMed] [Google Scholar]
- 71.OIE. Collection and Shipment of Diagnostic Specimens. 2018. [(accessed on 22 January 2020)]. Available online: https://www.oie.int/fileadmin/Home/eng/Animal_Health_in_the_World/docs/pdf/1.1.01_COLLECTION.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data have been provided in the article and/or as Supplementary Materials.