Abstract
The Fagerstrom test for nicotine dependence (FTND) is a widely used test for assessing physical nicotine dependence. However, there is a need to assess the psychometric properties of FTND to assess its role in treatment outcome studies. The aim of the present investigation was to review the psychometric properties of the FTND. A broad systematic literature search was performed from Pubmed and PsycINFO from 2000 to 2019. The publication language was limited to English. Two review authors performed the study selection and extracted the data. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and the Rayyan software used to screen relevant studies. A total of 1471 articles retrieved from the search, of which 33 studies fulfilled the inclusion criteria. Eleven studies related to testing the reliability of the FTND were analyzed. Twenty-five studies evaluated the Cronbach alpha of the test. Analysis of the studies revealed the questionable psychometric qualities of the adapted versions of the test across different cultures and ethnicity. It also suggested that it may not tap the appropriate constructs that would predict smoking patterns in light smokers, e-cigarette smokers, and smokeless tobacco users. Thus, further research must focus on improving the psychometric properties of FTND to enhance the measurement of nicotine dependence.
Keywords: Cigarette smoking, Fagerstrom test, psychometric properties, tobacco use disorder
The Fagerstrom Test of Nicotine Dependence (FTND)[1] includes an assessment of physical dependence to overcome the psychometric and validity limitation of the Fagerstrom Tolerance Questionnaire (FTQ).[2] However, FTND may also have limitations, due to questionable psychometric properties. The FTND included six of the original FTQeight scale items. It did not include item two (i.e., What brand do you smoke?) and item three (i.e., Do you inhale?) of the FTQ. They appeared to be the main confounder to the psychometric deficiencies of the FTQ.[1] The FTND also adopted a wide range of scoring for two items (Number of cigarettes per day and Time to the first cigarette). It was assumed that these scale modifications would enhance the measurement of nicotine dependence. However, these changes have improved the psychometrics properties only marginally from the FTQ.[1,2] The available literature shows that these alterations have failed to make substantial improvements to the psychometric properties of the FTND.[3]
A meta-analytical study shows that further studies of the FTND are needed to assess inter-rater reliability and define its sensitivity, specificity, positive predictive value, and negative predictive value.[4] The adaptation of FTND was carried out for assessing e-cigarette users and smokeless tobacco users. Although these adaptions of FTND to assess e-cigarette/smokeless tobacco dependence have utility in the clinical setting, it has limitations. However, few empirical studies have been carried out till date to understand the psychometric properties and applicability of the modified version of FTND in assessing dependence in nicotine product users and dual users. Therefore, the aim of the present study was to review of the psychometric properties of the FTND.
MATERIALS AND METHODS
Literature search
A systematic search of the literature was carried out in electronic databases such as PsychInfo, Pubmed, and others. We searched using the terms “Fagerstrom test” “Nicotine Dependence” “FTND,” “Fagerstrom test for cigarette dependence,” “Psychometric Properties,” “Validity,” “Reliability” and “Factor Analysis.” Search terms also describing “Smoking Behavior,” “Smokeless Tobacco,” “Tobacco Use Disorder,” “e-cigarettes” were used. All searches were limited to full-text papers published from 2000 to 2019. Studies were selected using Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) to assess the psychometric properties of the FTND.[4]
Study selection criteria
Inclusion criteria for the study
Original scientific research articles from peer-reviewed journals published between 2000 and 2019
Publications of psychometric properties, i.e. Reliability, Cronbach alpha of the FTND
Publications focusing on the study of smoking behavior, smokeless tobacco use, and e-cigarettes
Publications selected based on adaptation to different language/modified version of FTND.
Exclusion criteria for the study
Articles related to the efficacy of treatment for dependence
Systematic reviews and meta-analytical studies
Studies focusing on Fagerstrom test application in different areas
Publications studies that included biochemical/medical components such as biomarkers cotinine content, psychopharmacology, etc.
Published in other than the English language.
Selection process
Two reviewers did the study selection process. One researcher extracted the data and another researcher checked the studies for consistency with the aim and the inclusion criteria. All titles and abstracts were screened, and the decision to include or exclude studies was recorded using the Rayyan software.[5] The obtained articles from the databases were reviewed for duplication. Cross-referencing of selected and excluded studies was done with the agreement of the co-authors. The reference lists of relevant articles were reviewed using recommended Reference Screening technique to identify additional papers.[6]
RESULTS
The initial search strategy identified 1471 papers. After systematically screening titles and abstracts, 139 papers were selected as potential studies for inclusion in the full-text review. Figure 1 summarizes the process. After a complete reading of these papers using the inclusion and exclusion criteria, we identified 33 papers that met the inclusion criteria. These 33 papers were evaluated for psychometric properties of FTND developed in various countries, languages, and settings.
Figure 1.
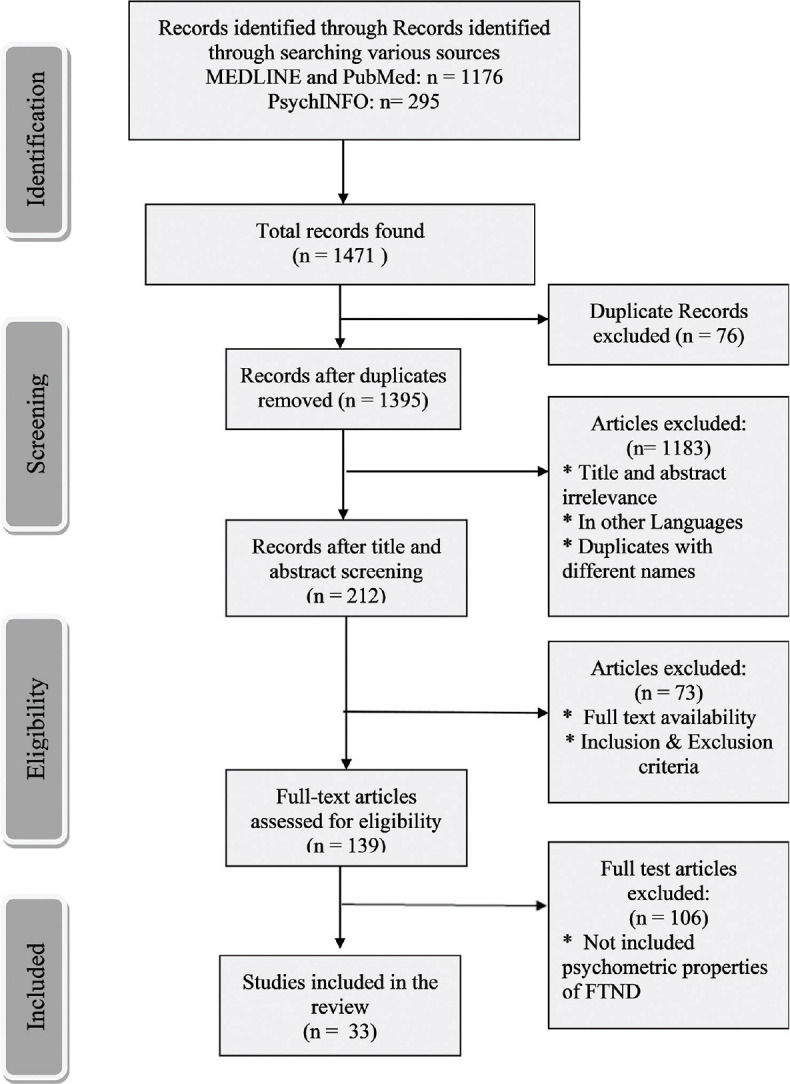
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of the study selection for the review
Psychometric properties: test-retest reliability for Fagerstrom test for nicotine dependence
Table 1 summarizes the articles representing the test-retest reliability of the FTND. This review identified that the time duration between tests varied from 1 week to 12 years. The obtained low-moderate reliability scores may be also due to inconsistency in the time duration between the tests.
Table 1.
Test-retest reliability of Fagerstrom test for nicotine dependence in various included studies
| Authors | Study title | Year | Country | Target population/n | Application setting | Interval | Reliability |
|---|---|---|---|---|---|---|---|
| Huang et al.[7] | The psychometric properties of the Chinese version of the FTND | 2006 | China | 245 smokers with an age range from 18 to 88 years | Survey | Correlated with biomarkers | 0.74 |
| Buckley et al.[8] | A psychometric evaluation of the FTND in PTSD smokers | 2005 | USA | 513 adult smokers with PTSD | Clinical | Test-retest intervals of 1 week | 0.82 |
| Hudmon et al.[9] | Validity of retrospective assessments of nicotine dependence: A preliminary report | 2005 | France | 306 Pregnant smoker Older than 18 years |
Randomized, double-blind, placebo-controlled, parallel-group Multicenter Study |
Intervals of 5-12 years | FTND=0.72 FTQ=0.62 |
| Vink et al.[10] | FTND in a dutch sample of daily smokers and ex-smokers | 2005 | Holland | 1378 daily smokers and 1058 ex-smokers | Survey method | 1.8 years | FTND Male smokers=0.70 Female smokers=0.83 Male ex-smokers=0.91 Female ex-smokers=0.83 |
| Weinberger et al.[11] | Reliability of the FTND, minnesota nicotine withdrawal scale, and tiffany questionnaire for smoking urges in smokers with and without schizophrenia | 2007 | USA | n=181 cigarette smokers and n=151 smokers with Schizophrenia | Clinical | 7 days | Smokers with schizophrenia FTND=0.65 MNWS=0.58 T-QSU F1=0.65 T-QSU F2=0.69 Smokers without psychotic symptoms FTND=0.82 MNWS=0.64 T-QSU F1=0.79 T-QSU F 2=0.81 |
| Uysal et al.[12] | FTND: Reliability in a Turkish sample and factor analysis | 2004 | Turkey | 169 smokers | Clinical | 10-14 days apart | FTND=0.56 |
| de Meneses-Gaya et al.[13] | Psychometric qualities of the Brazilian versions of the FTND and the heaviness of smoking index | 2009 | Brazil | 61 students Age range from 18 to 70 years |
Survey | 15 days | FTND=0.92 |
| Jayakrishnan et al.[14] | Assessment of nicotine dependence among smokers in a selected rural population in Kerala, India | 2012 | India | 928 smokers 18-60 years |
Survey | 2 months | FTND=0.77 |
| Stavem et al.[15] | Properties of the CDS and the Fagerström test of nicotine dependence in a representative sample of smokers in Norway | 2008 | Norway | 1265 participants 290 were daily smokers |
Cross-sectional telephone survey | 12 months | FTND=0.90 CDS-12=0.97 |
| Courvoisier and Etter[16] | Comparing the predictive validity of five cigarette dependence questionnaires | 2010 | Switzerland | 2206 daily smokers and 137 occasional (nondaily) smokers | Survey method | Survey 2-8 days Survey 3-31 days |
FTND=0.70 CDS-5=0.87 NDSS-T=0.87 |
| Breteler et al.[17] | Compulsive smoking: The development of a rasch homogeneous scale of nicotine dependence | 2004 | Holland | 1525 smokers Aged 15 years and older |
National survey | - | FTND=0.66 |
PTSD – Posttraumatic stress disorder; FTND – Fagerstrom test for nicotine dependence; FTQ – Fagerstrom Tolerance Questionnaire; MNWS – Minnesota Nicotine Withdrawal Scale; T- QSU – Tiffany questionnaire for smoking urges; CDS – Cigarette Dependence Scale; NDSS – Nicotine Dependence Syndrome Scale
Our current study identified 11 articles assessing test re-test reliability of FTND across the different populations. Studies included adolescent groups, psychiatric groups, and the general population. Overall, the obtained reliability score ranged from 0.56 to 0.92, on an average 0.75, indicating moderate test reliability. One study on psychometric qualities of the Brazilian versions of the FTND and the Heaviness of Smoking Index showed higher reliability (0.92); this could be due to re-assessment within 15 days.[13] The shorter time duration could have influenced the scores due to familiarity with the test. However, other studies reported lower reliability (0.56) assessed within 10–14 days of the time interval.[18] Whereas higher reliability was found for FNTD (0.82) in comparison with Minnesota Nicotine Withdrawal Scale (MNWS) (0.64), Tiffany questionnaire for Smoking Urges (T-QSU) F1 (0.79), and T-QSU F 2 (0.81) in assessing smokers without psychotic symptoms.[11]
Internal consistency of the Fagerstrom test for nicotine dependence and factor analysis
Table 2 presents a summary of the articles demonstrating the internal consistency of the FTND. It is recommended that instrument reliability be assessed according to internal consistency and inter-rater reliability.[36] An alpha coefficient of 0.70–0.79 considered as “fair;” an alpha of 0.80–0.89 is “good,” and an alpha of 0.090 or higher is “excellent.” However, reliability estimates should be 0.90 for clinical decision-making and 0.70 for research purposes.[37] Cronbach's alpha coefficients for all instruments generally fell in the range of 0.70–0.90. Our current research identified 24 studies that evaluated the internal consistency of the FTND and additionally, three studies evaluated a modified version of FTND in assessing smokeless tobacco use and e-cigarettes [as mentioned in Table 3]. The Cronbach's alpha coefficient ranged from 0.45 to 0.83, indicating that the FTND has low to moderate internal consistency.
Table 2.
Internal consistency of Fagerstrom test for nicotine dependence in various included studies
| Authors | Study title | Year | Country | Target population/n | Application setting | Assessment tools | Cronbach alpha |
|---|---|---|---|---|---|---|---|
| Weinberger et al.[11] | Reliability of the FTND, minnesota nicotine withdrawal scale, and tiffany questionnaire for smoking urges in smokers with and without schizophrenia | 2007 | USA | n=181 cigarette smokers and n=151 smokers with Schizophrenia | Clinical | FTND MNSW TQSU |
Smokers with schizophrenia FTND=0.74 MNWS=0.88 T-QSU F1=0.79 T-QSU F2=0.88 Smokers without psychotic symptoms FTND=0.72 MNWS=0.90 T-QSU F1=0.86 T-QSU F 2=0.89 |
| Jayakrishnan et al.[14] | Assessment of nicotine dependence among smokers in a selected rural population in Kerala, India | 2012 | India | 928 smokers, age group of 18-60 years | Survey Resident males |
FTND (6 items) |
Cronbach’s alpha 0.70 |
| Huang et al.[7] | Psychometric evaluation of the Cigarette Withdrawal Scale (Chinese Version) in male smokers in Taiwan | 2015 | France | 306 pregnant smoker 18 years and above |
Clinical Multicenter study | Randomized, double-blind, placebo-controlled, parallel-group FTND CDS-5 |
Cronbach’s alpha CDS-5=0.62 FTCD=0.55 |
| Vink et al.[10] | The FTND in a dutch sample of daily smokers and ex-smokers | 2005 | Holland | 1378 daily smokers 1058 ex-smokers |
Survey | FTND | Cronbach alpha Male smoker=0.65 Female smoker=0.69 Male ex-smoker=0.66 Female ex-smoker=0.71 |
| de Meneses-Gaya et al.[13] | Psychometric qualities of the brazilian versions of the FTND and the heaviness of smoking index | 2009 | Brazil (University of Franca, São Paulo) | 61 students Age range from 18 to 70 years |
Survey | FTND | Cronbach alpha FTND=0.83 HSI=0.56 |
| Kassim et al.[19] | Validity and reliability of the Fagerstrom test for Cigarette dependence in a sample of Arabic speaking UK-resident Yemeni khat chewers | 2012 | UK | 91 regular cigarette smokers of purposively selected 204 UK-resident Yemeni khat chewers | Survey | FTCD | Cronbach alpha=0.68 2 subscales=0.60 and 0.62 |
| Uysal et al.[18] | Psychometric properties of the Turkish version of the FTND | 2015 | Turkey | 502 patients | Clinical | FTND | Cronbach alpha=0.586 |
| Burling and Burling[20] | A comparison of self-report measures of nicotine dependence among male drug/alcohol-dependent cigarette smokers | 2003 | USA | 191 Drug/alcohol dependent smoker |
Clinical | FTND FTQ HSI |
FTND=0.59 FTQ=0.49 HSI=0.49 |
| Etter[21] | A comparison of the content-, construct-and predictive validity of the CDS and the FTND | 2005 | Switzerland | 802 people | Internet Survey in 2002-2003 | CDS FTND HSI |
Cronbach alpha CDS-12=0.91 CDS-5=0.77 FTND=0.68 HSI=0.63 |
| Wellman et al.[22] | A comparison of the hooked on nicotine checklist and the FTND in adult smokers | 2006 | USA | 1130 smokers | Survey | FTND HONC |
Cronbach’s alpha: FTND=0.61 HONC=0.82 |
| Stavem et al.[15] | Properties of the CDS and the Fagerström test of nicotine dependence in a representative sample of smokers in Norway | 2008 | Norway | 1265 respondents. 290 were daily smokers | Cross sectional telephone survey | FTND CDS FTND=0.61 (n=267) CDS=0.81 (n=266). |
|
| Berlin et al.[23] | A comparison of the Fagerström test for cigarette dependence and CDS in a treatment-seeking sample of pregnant smokers | 2015 | France | 73 subjects | Randomized, double-blind, placebo-controlled, parallel-group, multicenter study | CDS FTCD |
Cronbach’s alpha CDS-5=0.62 FTCD=0.55 |
| DiFranza et al.[22] | What aspect of dependence does the FTND measure? | 2012 | US | 422 current smokers | Web based survey | FTND HIS AUTOS |
Cronbach’s alpha FTND=0.73 HSI=0.57 AUTOS=0.94 |
| Korte et al.[24] | The FTND: Do revisions in the item scoring enhance the psychometric properties? | 2013 | US | 343 smokers | Community | FTND FTQ |
FTND-R (α=0.69) FTND (α=0.63) and the FTQ (α=0.48). |
| Etter[25] | Comparing the validity of the CDS and the FTND | 2008 | Switzerland | 13,697 participants | Internet survey in 2004-2007 | FTND | Cronbach alpha CDS-12=0.89 CDS-5=0.76 FTND=0.68 HSI=0.65 MINI=0.49 |
| Wu et al.[26] | Nicotine dependence among rural-urban migrants in China | 2011 | China | 894 daily smokers | Survey | Chinese version of FTND | The Cronbach alpha 0.67 |
| John et al.[27] | A short form of the FTND and the heaviness of smoking index in two adult population samples | 2004 | Germany | Sample 1 included 1462 and sample 2 included 1042 current daily cigarette smokers aged 20-64 years | Survey | FTND | Cronbach’s α 0.55 (sample 1) 0.60 (sample 2) |
| Nakajima et al.[28] | An examination of the FTND among concurrent tobacco and khat users | 2012 | Middle Eastern societies | 103 participants Age range from 18 to 40 years Yemen |
Taiz University and Sana’a University, Yemen | Arabic version of FTND | Cronbach alpha 0.58 |
| de Lima Osório et al.[29] | Screening for smoking in a general hospital: Scale validation, indicators of prevalence, and comorbidity | 2013 | Brazil | 264 inpatients | Clinical | FTND Brazilian Portuguese Translated version |
0.82 |
| Sledjeski et al.[30] | Predictive validity of four nicotine dependence measures in a college sample. | 2007 | United States | 912 college students | Survey | FTND English version | 0.58 |
| Grassi et al.[31] | Validity of the Italian version of the SDS for nicotine dependence in smokers intending to quit | 2014 | Rome | 635 participants 18 and above |
Survey | FTND Italian version |
FTND=0.57 SDS=0.44 |
| Park et al.[32] | A preliminary investigation of early smoking initiation and nicotine dependence in Korean adults | 2004 | Korea | 268 current smokers who visited the Center for Cancer Prevention and Early Detection in the National Cancer Center, Korea | Clinical | FTND-K | Cronbach’s alpha of FTND-K was 0.72 |
| Ma et al.[33] | Comparison of the Fagerström test for cigarette dependence and the heaviness of smoking index in the second and third trimester of pregnancy | 2016 | Canada | 167 women | Clinical | FTCD HSI |
The Cronbach’s alpha for FTCD was 0.45 and for HSI 0.46 |
| Okuyemi et al.[34] | Nicotine dependence among African American light smokers: A comparison of three scales | 2007 | United States | 700 participants | Clinical | FTND | Cronbach’s alpha CDS=0.64 FTND=0.63 NDSS=0.80 |
| Jhanjee and Sethi[35] | The Fagerström test for nicotine Dependence in an Indian sample of daily Smokers with poly drug use |
2010 | India | 75 adult male daily smokers | Clinical | FTND | 0.57 |
SDS – Severity of Dependence Scale; FTND – Fagerstrom test for nicotine dependence; FTQ – Fagerstrom Tolerance Questionnaire; MNWS – Minnesota Nicotine Withdrawal Scale; T- QSU – Tiffany questionnaire for smoking urges; CDS – Cigarette Dependence Scale; FTCD – Fagerström test for cigarette dependence; NDSS – Nicotine Dependence Syndrome Scale; AUTOS – Autonomy over Tobacco Scale; HSI – Heaviness of Smoking Index
Table 3.
Psychometric evaluation of modified Fagerstrom test for nicotine dependence in assessing smokeless tobacco use, e-cigarettes, and vaping
| Authors | Study title | Year | Country | Target population/n | Application setting | Assessment tools | Cronbach alpha |
|---|---|---|---|---|---|---|---|
| Mushtaq and Beebe[38] | Psychometric properties of FTND-ST | 2017 | USA | 95 ST-users living in Oklahoma | Survey | FTND-ST | 0.72 |
| Piper et al.[39] | E-cigarette dependence measures in dual users: Reliability and relations with dependence criteria and e-cigarette cessation | 2019 | US | 256 participants Age range above 18 years |
Longitudinal observational cohort study | The e-cigarette FTCD | e-FTCD=0.51 PS-ECDI=0.74 e-WISDM=0.80 |
| Browne and Todd[40] | Then and now: Consumption and dependence in e-cigarette users who formerly smoked cigarettes | 2018 | Australia | 350 participants from Western countries | Survey | Retrospective version of FTND FTND-Vaping |
FTND-R=0.69 FTND-V=0.54 |
FTND – Fagerstrom test for nicotine dependence, FTQ – Fagerstrom Tolerance Qustionnaire; FTND-ST – FTND-smokeless tobacco users, ST – Smokeless tobacco; PS-ECDI – Penn State-electronic cigarette dependence index; e-WISDM – e-cigarette Wisconsin inventory of smoking dependence motives; e-FTCD – e-cigarette Fagerström test for cigarette dependence
Overall, the FTND demonstrated unsatisfactory internal consistency, with the highest number of studies (n = 17) reporting alpha values ranging from 0.45 to 0.68 and only 7 studies demonstrating moderate alpha value ranging from 0.70 to 0.83, indicating moderate internal consistency. Notably, studies conducted on college students and inpatients demonstrated a high range of IC (0.82).[13,29] Other studies also demonstrated better Internal consistency of FNTD compared to HSI among light smokers.[20,41]
An Indian study also confirmed that FTND had low reliability (Cronbach's alpha: 0.57) in the Indian setting.[35] FTND was found to have low internal consistency reliability in this study. The study validates the presence of a 2-factor structure of the FTND in a sample of polysubstance users. Thus, it implicates that FTND may assess 2 separate dimensions of nicotine addiction. These factors explain the good amount of variance (56.34%). They have Cronbach's alpha, of 0.66 and 0.58, respectively. Another Indian study reported the internal consistency of 0.70 of the FTND for smokers.[14] This low internal consistency may also be due to a small number of items, ambiguity in the factor structure or may be due to a limited range of responses in the test. It suggests that a two-factor FTND in clinical practice would more accurately determine the nicotine dependence of patients.[12,20,21]
Smokeless tobacco use, e-cigarettes
Table 3 shows the current application of the modified Fagerstrom test in assessing nicotine dependence in different products. With the increase in the use of smokeless tobacco in the general population, FTND has been adapted for smokeless tobacco (snuff and/or chew) users in the form of the FTND-ST. FTND-ST is a modified version of the FTND for the assessment of smokeless tobacco users. The modified FTND-ST scale got moderate internal consistency (0.72) for smokeless tobacco users.[38] The adapted version of the test also demonstrated moderate internal consistency (Cronbach's α = 0.47) for smokeless tobacco users.[1,21]
Cross-national adaptation of Fagerstrom test for nicotine dependence start from here
The cross-national/cross-cultural adaptation of the FTQ/FTND has moderate reliability ranging from 0.55 to 0.65. The study concluded that the internal reliability (Cronbach's alpha coefficient) of the whole FTND is low (0.68) as well as for the two subscales (0.60) and (0.62) respectively.[19] Whereas Cronbach's alpha coefficient of the Persian version of FTND was 0.71.[42]
Turkish version of the FTND has a two-factor structure with moderate reliability.[18] The use of the total score of FTND for measuring nicotine dependence may limit the assessment of specific smoking dependency and tailoring intervention approaches. The validity of the FTND has shown inconsistent results. The Cronbach's alpha was 0.58 for one-factorial FTND. Considering the cultural variation in tobacco use in different countries, the level of nicotine content in bidi, cigarette, e-cigarettes, tobacco products, and other nicotine products varies. FTND assessment in understanding the dependence of nicotine across various cultural products will be limited.
DISCUSSION
Despite the widespread application of the tool in the clinical and research area, the psychometric qualities of the questionnaire are still questionable. From this systematic review of various scientific papers published between 2000 and 2019, it can be seen that the FTND scores have found a weaker correlation with other smoking questionnaires with moderate internal consistency.[21] Similarly, a recent study from India based on the FTND among smokers with poly-drug abuse concluded that FTND had low internal consistency and reliability and suggested a two-factor structure of FTND based assessment.[14,35]
Both WHO in its International Classification of Diseases-11[43] and the APA in its Diagnostic and Statistical Manual-V[44] have issued diagnostic criteria to assess nicotine dependence and withdrawal. However, in several studies, researchers have reported that FTND focuses only on physical tobacco dependence and is not consistent with diagnostic criteria for identifying tobacco dependence as a psychological disorder.[45,46]
In the adolescent population, one study found that many of the items in FTND are not appropriate for assessing tobacco dependence.[47] The study, further reported that the FTND tool does not focus on the early signs of dependence that typically characterize adolescent nicotine dependence.[48] It highlights that the tool may not be ideal for adolescent populations, especially when studying the onset and early manifestations of nicotine dependence. The questionable FTND psychometric properties can also be attributed to the use of the forced-choice response format for assessing the dimensional construct of FTND.
Psychometric properties of the FTND among tobacco smokers who use khat (Catha edulis), a widely used substance in East Africa and Arabian Peninsula, were examined, The scale was found to have low internal consistency (Cronbach's α = 0.58).[49] It highlights the need for considering the sociocultural factors in association with patterns of smoking behavior. The study strengths were the use of PRISMA guidelines to analyze the psychometric properties of the FTND. Second, this review analyzed the cross-national adaptation of the FTND and its reliability and validity across different cultures and languages. Third, this review utilized the Reference Screening method recommended for searching for articles from the database, which ensured the inclusion of all significant relevant studies for the analysis.
Limitations
The study's limitations exist in identifying certain relevant publications containing measures, a common challenge when conducting systematic reviews. Secondly, in this review, the use of only two databases would have limited the possibility of missing some relevant publications. However, we accessed the most relevant databases for this topic using the reference screening method. It also has limitations for tools for upcoming e-cigarette, smokeless tobacco use, and their management. Finally, this review was limited in analyzing the reliability, validity, and cross-national adaptation of the test; further research is required to understand the test's predictive validity and construct validity.
CONCLUSION
The review indicates a greater need for revision of the test and its psychometric qualities, especially the forced-choice response format for FTND in clinical and research areas. Further investigation is needed to develop an adapted version of the test across different cultures and ethnicities. The current measure of nicotine use may not be tapping the appropriate constructs that would predict smoking patterns in light smokers, e-cigarette smokers, smokeless tobacco users, and adolescent users. From this perspective, further research must focus on assessing inter-rater reliability, correlation with other assessment tools of nicotine use, and applicability of the tool in future studies on e-cigarette, smokeless tobacco use, adolescents users, and management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The fagerström test for nicotine dependence: A revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 2.Fagerström KO. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addict Behav. 1978;3:235–41. doi: 10.1016/0306-4603(78)90024-2. [DOI] [PubMed] [Google Scholar]
- 3.Payne TJ, Smith PO, McCracken LM, McSherry WC, Antony MM. Assessing nicotine dependence: A comparison of the fagerström tolerance questionnaire (FTQ) with the fagerström test for nicotine dependence (FTND) in a clinical sample. Addict Behav. 1994;19:307–17. doi: 10.1016/0306-4603(94)90032-9. [DOI] [PubMed] [Google Scholar]
- 4.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 5.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Whiting P, Westwood M, Burke M, Sterne J, Glanville J. Systematic reviews of test accuracy should search a range of databases to identify primary studies. J Clin Epidemiol. 2008;61:357–64. doi: 10.1016/j.jclinepi.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 7.Huang HW, Hsueh KC, Lu CC, Huang CL. Psychometric evaluation of the cigarette withdrawal scale (Chinese Version) in male smokers in Taiwan. J Nurs Res. 2016;24:118–25. doi: 10.1097/jnr.0000000000000113. [DOI] [PubMed] [Google Scholar]
- 8.Buckley TC, Mozley SL, Holohan DR, Walsh K, Beckham JC, Kassel JD. A psychometric evaluation of the Fagerström Test for Nicotine Dependence in PTSD smokers. Addict Behav. 2005;30:1029–33. doi: 10.1016/j.addbeh.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Suchanek Hudmon K, Pomerleau CS, Brigham J, Javitz H, Swan GE. Validity of retrospective assessments of nicotine dependence: A preliminary report. Addict Behav. 2005;30:613–7. doi: 10.1016/j.addbeh.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Vink JM, Willemsen G, Beem AL, Boomsma DI. The Fagerström Test for Nicotine Dependence in a Dutch sample of daily smokers and ex-smokers. Addict Behav. 2005;30:575–9. doi: 10.1016/j.addbeh.2004.05.023. [DOI] [PubMed] [Google Scholar]
- 11.Weinberger AH, Reutenauer EL, Allen TM, Termine A, Vessicchio JC, Sacco KA, et al. Reliability of the fagerström test for nicotine dependence, minnesota nicotine withdrawal scale, and tiffany questionnaire for smoking urges in smokers with and without schizophrenia. Drug Alcohol Depend. 2007;86:278–82. doi: 10.1016/j.drugalcdep.2006.06.005. [DOI] [PubMed] [Google Scholar]
- 12.Uysal MA, Kadakal F, Karşidag C, Bayram NG, Uysal O, Yilmaz V. Fagerstrom test for nicotine dependence: Reliability in a Turkish sample and factor analysis. Tuberk Toraks. 2004;52:115–21. [PubMed] [Google Scholar]
- 13.de Meneses-Gaya C, Zuardi AW, de Azevedo Marques JM, Souza RM, Loureiro SR, Crippa JA. Psychometric qualities of the Brazilian versions of the Fagerström Test for Nicotine Dependence and the Heaviness of Smoking Index. Nicotine Tob Res. 2009;11:1160–5. doi: 10.1093/ntr/ntp114. [DOI] [PubMed] [Google Scholar]
- 14.Jayakrishnan R, Mathew A, Lekshmi K, Sebastian P, Finne P, Uutela A. Assessment of nicotine dependence among smokers in a selected rural population in Kerala, India. Asian Pac J Cancer Prev. 2012;13:2663–7. doi: 10.7314/apjcp.2012.13.6.2663. [DOI] [PubMed] [Google Scholar]
- 15.Stavem K, Røgeberg OJ, Olsen JA, Boe J. Properties of the Cigarette Dependence Scale and the Fagerström Test of Nicotine Dependence in a representative sample of smokers in Norway. Addiction. 2008;103:1441–9. doi: 10.1111/j.1360-0443.2008.02278.x. [DOI] [PubMed] [Google Scholar]
- 16.Courvoisier DS, Etter JF. Comparing the predictive validity of five cigarette dependence questionnaires. Drug Alcohol Depend. 2010;107:128–33. doi: 10.1016/j.drugalcdep.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 17.Breteler MH, Hilberink SR, Zeeman G, Lammers SM. Compulsive smoking: The development of a Rasch homogeneous scale of nicotine dependence. Addict Behav. 2004;29:199–205. doi: 10.1016/s0306-4603(03)00089-3. [DOI] [PubMed] [Google Scholar]
- 18.Uysal MA, Öztuna D, Bahadır A, Görek Dilektaşlı A, Karşıdağ Ç, Horoz A, et al. Psychometric properties of the Turkish version of the Fagerström test for nicotine dependence. Tuberk Toraks. 2015;63:250–6. doi: 10.5578/tt.8878. [DOI] [PubMed] [Google Scholar]
- 19.Kassim S, Salam M, Croucher R. Validity and reliability of the Fagerstrom Test for Cigarette Dependence in a sample of Arabic speaking UK-resident Yemeni khat chewers. Asian Pac J Cancer Prev. 2012;13:1285–8. doi: 10.7314/apjcp.2012.13.4.1285. [DOI] [PubMed] [Google Scholar]
- 20.Burling AS, Burling TA. A comparison of self-report measures of nicotine dependence among male drug/alcohol-dependent cigarette smokers. Nicotine Tob Res. 2003;5:625–33. doi: 10.1080/1462220031000158708. [DOI] [PubMed] [Google Scholar]
- 21.Etter JF. A comparison of the content-, construct- and predictive validity of the cigarette dependence scale and the Fagerström test for nicotine dependence. Drug Alcohol Depend. 2005;77:259–68. doi: 10.1016/j.drugalcdep.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 22.DiFranza JR, Wellman RJ, Savageau JA, Beccia A, Ursprung WW, McMillen R. What aspect of dependence does the fagerström test for nicotine dependence measure? ISRN Addict. 2013;2013:1–8. doi: 10.1155/2013/906276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berlin I, Singleton EG, Heishman SJ. A comparison of the fagerström test for cigarette dependence and cigarette dependence scale in a treatment-seeking sample of pregnant smokers. Nicotine Tob Res. 2016;18:477–83. doi: 10.1093/ntr/ntv108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Korte KJ, Capron DW, Zvolensky M, Schmidt NB. The Fagerström Test for Nicotine Dependence: Do revisions in the item scoring enhance the psychometric properties? Addict Behav. 2013;38:1757–63. doi: 10.1016/j.addbeh.2012.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Etter JF. Comparing the validity of the cigarette dependence scale and the fagerström test for nicotine dependence. Drug Alcohol Depend. 2008;95:152–9. doi: 10.1016/j.drugalcdep.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 26.Wu J, Yang T, Rockett IR, Xing R, Karalic S, Li Y, et al. Nicotine dependence among rural-urban migrants in China. BMC Public Health. 2011;11:296. doi: 10.1186/1471-2458-11-296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.John U, Meyer C, Schumann A, Hapke U, Rumpf HJ, Adam C, et al. A short form of the Fagerström Test for Nicotine Dependence and the Heaviness of Smoking Index in two adult population samples. Addict Behav. 2004;29:1207–12. doi: 10.1016/j.addbeh.2004.03.019. [DOI] [PubMed] [Google Scholar]
- 28.Nakajima M, Al'Absi M, Dokam A, Alsoofi M, Khalil NS. An examination of the fagerström test for nicotine dependence among concurrent tobacco and khat users. J Psychoactive Drugs. 2012;44:437–41. doi: 10.1080/02791072.2012.737224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Lima Osório F, Franco De Carvalho AC, Alexandre De Souza Crippa J, Loureiro SR. Screening for smoking in a general hospital: Scale validation, indicators of prevalence, and comorbidityp pc_330 5.12. Perspect Psychiatr Care. 2013;49:5–12. doi: 10.1111/j.1744-6163.2012.00330.x. [DOI] [PubMed] [Google Scholar]
- 30.Sledjeski EM, Dierker LC, Costello D, Shiffman S, Donny E, Flay BR, et al. Predictive validity of four nicotine dependence measures in a college sample. Drug Alcohol Depend. 2007;87:10–9. doi: 10.1016/j.drugalcdep.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 31.Grassi MC, Ferketich AK, Enea D, Culasso F, Nencini P. Validity of the Italian version of the Severity of Dependence Scale (SDS) for nicotine dependence in smokers intending to quit. Psychol Rep. 2014;114:1–3. doi: 10.2466/18.15.PR0.114k16w7. [DOI] [PubMed] [Google Scholar]
- 32.Park SM, Son KY, Lee YJ, Lee HC, Kang JH, Lee YJ, et al. A preliminary investigation of early smoking initiation and nicotine dependence in Korean adults. Drug Alcohol Depend. 2004;74:197–203. doi: 10.1016/j.drugalcdep.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 33.Ma E, Brown N, Alshaikh B, Slater D, Yusuf K. Comparison of the fagerström test for cigarette dependence and the heaviness of smoking index in the second and third trimester of pregnancy. Nicotine Tob Res. 2017;20:124–9. doi: 10.1093/ntr/ntw271. [DOI] [PubMed] [Google Scholar]
- 34.Okuyemi KS, Pulvers KM, Cox LS, Thomas JL, Kaur H, Mayo MS, et al. Nicotine dependence among African American light smokers: A comparison of three scales. Addict Behav. 2007;32:1989–2002. doi: 10.1016/j.addbeh.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jhanjee S, Sethi H. The Fagerström test for nicotine dependence in an Indian sample of daily smokers with poly drug use. Nicotine Tob Res. 2010;12:1162–6. doi: 10.1093/ntr/ntq148. [DOI] [PubMed] [Google Scholar]
- 36.Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6:284–90. [Google Scholar]
- 37.Groth-Marnat G. Handbook of Psychological Assessment. 4th ed., Vol. 44. Global Shadows: Africa in the Neoliberal World Order. New Jersey: John-Wiley and Sons, Inc; 2003. pp. 8–10. [Google Scholar]
- 38.Mushtaq N, Beebe LA. Psychometric properties of fagerström test for nicotine dependence for smokeless tobacco users (FTND-ST) Nicotine Tob Res. 2017;19:1095–101. doi: 10.1093/ntr/ntx076. [DOI] [PubMed] [Google Scholar]
- 39.Piper ME, Baker TB, Benowitz NL, Smith SS, Jorenby DE. E-cigarette dependence measures in dual users: Reliability and relations with dependence criteria and E-cigarette cessation. Nicotine Tob Res. 2020;22:756–63. doi: 10.1093/ntr/ntz040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Browne M, Todd DG. Then and now: Consumption and dependence in e-cigarette users who formerly smoked cigarettes. Addict Behav. 2018;76:113–21. doi: 10.1016/j.addbeh.2017.07.034. [DOI] [PubMed] [Google Scholar]
- 41.Etter JF. Electronic cigarettes: A survey of users. BMC Public Health. 2010;10:231. doi: 10.1186/1471-2458-10-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Robabeh S, Mohammad JM, Mahnaz F, Amir ZA. Psychometric properties of the Persian version of the fagerstrom test for nicotine dependence in patients with opioid use disorder/cigarette smokers under methadone maintenance treatment. Neuroquantology. 2017;15:253–60. [Google Scholar]
- 43.World Health Organization: International classification of diseases for mortality and morbidity statistics (11th Revision) Geneva, Switzerland: WHO; 2018. [Google Scholar]
- 44.Del Barrio V. Diagnostic and statistical manual of mental disorders. In: The Curated Reference Collection in Neuroscience and Biobehavioral Psychology. Oxford, UK: Elsevier Science Ltd; 2016. [Google Scholar]
- 45.Breslau N, Johnson EO. Predicting smoking cessation and major depression in nicotine-dependent smokers. Am J Public Health. 2000;90:1122–7. doi: 10.2105/ajph.90.7.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Moolchan ET, Radzius A, Epstein DH, Uhl G, Gorelick DA, Cadet JL, et al. The fagerstrom test for nicotine dependence and the diagnostic interview schedule: Do they diagnose the same smokers? Addict Behav. 2002;27:101–13. doi: 10.1016/s0306-4603(00)00171-4. [DOI] [PubMed] [Google Scholar]
- 47.Brook DW, Brook JS, Zhang C, Whiteman M, Cohen P, Finch SJ. Developmental trajectories of cigarette smoking from adolescence to the early thirties: Personality and behavioral risk factors. Nicotine Tob Res. 2008;10:1283–91. doi: 10.1080/14622200802238993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.DiFranza JR, Savageau JA, Rigotti NA, Fletcher K, Ockene JK, McNeill AD, et al. Development of symptoms of tobacco dependence in youths: 30 month follow up data from the DANDY study. Tob Control. 2002;11:228–35. doi: 10.1136/tc.11.3.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nakajima M, Al’Absi M. Predictors of risk for smoking relapse in men and women: A prospective examination. Psychol Addict Behav. 2012;26:633–7. doi: 10.1037/a0027280. [DOI] [PMC free article] [PubMed] [Google Scholar]


