Abstract
Objective
Due to introduction of a new curriculum and the related stressors that medical students might encounter, we aimed to assess the quality of the students’ learning environment across academic years at Umm Al-Qura University (UQU), by evaluating stress levels, their sources, and impacts on students, to help improve the quality of learning environment and protect students from personal and academic burnout.
Methods
We conducted a descriptive cross-sectional study in August and September of 2020 on 572 students enrolled in the new Bachelor of Medicine and Bachelor of Surgery (MBBS) curriculum at UQU. All statistical analyses were performed using SPSS software and two-tailed tests.
Results
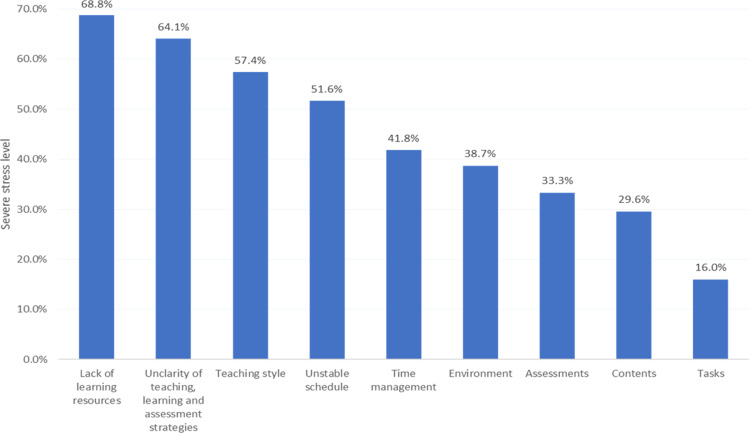
In total, 46.5% of participants encountered severe stress levels during their studies at UQU. In term of stressor sources, the highest prevalence of severe stress was found among students who lacked learning resources (68.8%), followed by those who complained of ambiguity in teaching, learning, and assessment strategies (64.1%). Self-study strategy issues (58.4%) and difficulty in reading textbooks (58.2%) also ranked high. Anxiety was often reported by the students as an impact of stress (62.9%), followed by mood swings (60%). Severe stress levels showed a statistically significant relationship to gender, being highest among females (P = 0.001). For a solution to manage the stress, 79% of the students suggested a supportive learning environment and identification of students’ struggles at early stages.
Conclusion
Almost half the medical students were severely stressed after the new curriculum was introduced. Therefore, professors and universities should look out for potential stressors and help students overcome them. Universities can also help by offering counseling services to students, improving the student tutoring system, providing appropriate learning environment and resources, and including stress management courses as a part of the overall curriculum.
Keywords: medical students, stress, curriculum change, learning environment, teaching styles, medical school
Introduction
Stress is a mental, emotional, or physical response to environmental challenges and threats that cause mental or physical tension.1 In particular, the educational environment may impose stress challenges. Slight stress is normal and may increase productivity in certain individuals. However, extremely high levels of stress experienced over a long period can cause significant mental and physical issues, such as poor academic performance, reduced commitment, stress-related anxiety, depression, drug usage, and even suicidal thoughts.2,3
Tertiary education has always been considered a stressful environment for students. Medical education adds to an already stressful environment.4,5 Medical students encounter many stressors during their journey to achieve their goals;5 these include an extensive medical curriculum, information overload, long study hours, high academic and family expectations, competition, and frequent and varied examinations.3 Several studies have reported moderate to high levels of stress among medical students in different countries worldwide, including 91.1% in India,6 84.5% in Pakistan,7 83.5% in Thailand,8 and 49% in Malaysia.9 In Saudi Arabia, stress was reported in Imam Abdulrahman Bin Faisal University, Dammam, at 67.9% in 2018,5 in Rabigh Medical College, Jeddah, at 59.2% in 2015,3 in Umm Al-Qura University (UQU), Makkah, at 70.9% in 2015,10 and in King Saud University, Riyadh, at 63% in 2011.11 A previous study performed at UQU suggests the causes of distress to be the following factors: large volumes of information that must be retained, students’ academic competition, grade point average (GPA), and fear of failure. These factors may be accentuated in the preclinical years, when coursework units are more theoretical.10 Another study at UQU medical school found that the majority of students were dissatisfied with the passive, lecture-based method of teaching and wanted to see introduction of the concepts of active learning and effective studying habits.10,12
Therefore, in 2016, the Medicine and Bachelor of Surgery program (MBBS) at UQU was updated. The new curriculum was written in association with the University College London, which has one of the highest-ranking medical schools in the United Kingdom. The MBBS program was updated in content, learning style, and teaching and assessment methods.13 This update revolutionized the educational experience for the entire staff, as well as students and lecturers. It also bought a new set of challenges to the medical education experience.
After this curriculum update, it became particularly important to detect stress and stressors among medical students. Our understanding of the matter helps us to implement strategies to reduce the incidence of stress and prevent its adverse effects on the students’ health, their academic performance, and their subsequent careers. Our theory suggests that, with the new curriculum, students have more responsibilities and thereby more stress. Studies mentioned earlier covered stress and depression in medical students, but such studies were conducted in the context of the traditional educational system.6–11 The present study is different, having been conducted to evaluate the learning environment quality after the updated MBBS curriculum was introduced. The aim of the present study was to fill in the gap regarding the effect of the curriculum change on the stress of medical students, as well as identifying the source of that stress and its impact on their quality of life.
Methods
Research Design, Population, and Sample Size Determination
We designed this as a descriptive cross-sectional study, performed using a self-administered online questionnaire from August 22, 2020, to September 6, 2020. Ethical approval was obtained from the Biomedical Ethics Committee of the Faculty of Medicine at UQU, Makkah, Saudi Arabia (approval number HAPO-02-K-012-2020-08-430), and we conducted it in accordance with the Declaration of Helsinki. The targeted population is medical students in years 2 to 5 (batch of 2019–2016) who passed the first academic year and are following the updated MBBS curriculum. The first academic year is the foundation year, designed to prepare students for the MBBS program (including intensive English language course and basic sciences). We excluded students who studied at another university before studying at UQU and sixth-year students, who are still studying the traditional MBBS curriculum. The required sample size was calculated, using OpenEpi version 3.0,14 by considering a population size of approximately 1300 students, confidence interval (CI) level of 95%, anticipated frequency percentage of 50%, and took the design effect of 1. These factors gave us a sample size of 297 participants. In case of any possible data loss, the total sample size required was 340 participants. However, the final collected data comprised 572 students.
Questionnaire Structure
We designed an online questionnaire using Google Forms and distributed it in English via different platforms on social media. The questionnaire was modified in accordance with previously published studies.10,12,15–18 The format and content of the questionnaire were reviewed by three experts in the field of family medicine, medical education, and public health to evaluate the relevance, clarity, and adequacy of the questions. There are five main parts. The first part asks participants to describe their demographic characteristics, including gender, age, year of study, and financial status. The second part is the Kessler Psychological Distress Scale (K10), which assesses the students’ stress levels.16; It involves 10 questions on emotional states, each with a five-level response scale (from one being “never” to 5 being “always”). The third part assesses the sources of stress, including academic, psychological, health-related, and environmental stress. The fourth part assesses the impact of this stress. Finally, the fifth part discusses students’ suggestions and solutions for stress. The questions in the third, fourth and fifth parts consisted of different statements that were inspired by previous studies10,12,15–18 and revised for appropriateness, relevance, clarity, and adequacy by a panel of experts consisting of three assistant professors: one in family medicine, one in medical education, and one in public health. The participants’ opinions of these questions for each section were measured using a 3-point Likert scale (“disagree,” “natural,” and “agree”). The reliability of the questionnaire items was tested using Cronbach’s test and they were observed to be reliable, with a minimum reliability score of 0.68 for “(nominate a question)” and a maximum of 0.82 for “(nominate another question).”
Statistical Analysis
After data collection from participants who met the eligibility criteria of the study, we coded the data and fed it into the statistical software IBM SPSS version 22. We constructed graphs using Microsoft Excel software. All statistical analyses were performed using two-tailed tests, with an alpha error of 0.05. Statistical significance was set at P < 0.05. Frequency and percentages were used to describe the frequency distribution of students’ demographic data, stressors, stress levels, impacts, and suggestions to minimize stress. The K10 score was used to assess the level of stress. The scores of the 10 items were summed, yielding a minimum score of 10 and a maximum of 50. Low scores indicate low levels of psychological distress, and vice versa. The overall score is categorized as normal (10–19 points), mild stress (20–24), moderate stress (25–29), and severe stress (30–50). We performed cross-tabulation between different student-related factors and stress levels, to detect the most significant stress determinants based on the Pearson chi-square test or exact probability test (for small frequencies).
Results
Participant Characteristics
Table 1 shows participant characteristics. The survey included 572 medical students who completed the questionnaire. Their ages ranged from 18 to 25, with a mean age of 21.9 ± 3.5 years. Females accounted for 52.1% of respondents. Additionally, 36% of the students were in their second year, 24.7% in the third year, 29.4% in the fourth year, and 10% in the fifth year. The average monthly income was recorded by 84.3% of participants.
Table 1.
General Characteristics for Undergraduate Medical School Students in Saudi Arabia
| Personal Characteristics | No. | % | |
|---|---|---|---|
| Gender | Male | 274 | 47.9% |
| Female | 298 | 52.1% | |
| Age (years) | 18–21 | 326 | 57.0% |
| 22–23 | 223 | 39.0% | |
| 24–25 | 23 | 4.0% | |
| Academic year/batch | Second year (batch 2019) | 206 | 36.0% |
| Third year (batch 2018) | 141 | 24.7% | |
| Fourth year (batch 2017) | 168 | 29.4% | |
| Fifth year (batch 2016) | 57 | 10.0% | |
| Income level | Low | 19 | 3.3% |
| Average | 482 | 84.3% | |
| High | 71 | 12.4% | |
K10 Questionnaire and the Presence of Stress
We carried out the stress assessment (Table 2) using the Kessler10 Psychological Distress instrument. Of the students, 98.6% felt nervous during MBBS courses; 108 students reported this feeling as “always” occurring, 191 students reported it as occurring “most” of the time, and only 80 students reported it “seldomly.” Of the students, 94.8% felt tired for no good reason, including 57 students who reported this fatigue as “always” occurring, 180 students who reported it “most” of the time, and 109 students who reported it “seldomly.” Of the participants, 93.7% felt that everything was an effort, 90.4% felt restless or fidgety, 88.3% felt depressed, 81.5% felt so sad that nothing could cheer them up, 79.2% felt so nervous that nothing could calm them down, and 68.7% felt worthless. In total, 18.9% of the students had mild stress, 17.1% had moderate stress, and 46.5% had severe stress.
Table 2.
Stress Level Assessment for Students in Bachelor of Medicine and Bachelor of Surgery Program
| Kessler 10 Psychological Distress Instrument | Never | Seldom | Sometimes | Mostly | Always | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | % | No | % | No | % | No | % | No | % | |
| How often did you feel tired for no good reason? | 30 | 5.2% | 109 | 19.1% | 196 | 34.3% | 180 | 31.5% | 57 | 10.0% |
| How often did you feel nervous? | 8 | 1.4% | 80 | 14.0% | 185 | 32.3% | 191 | 33.4% | 108 | 18.9% |
| How often did you feel so nervous that nothing could calm you down? | 119 | 20.8% | 174 | 30.4% | 141 | 24.7% | 96 | 16.8% | 42 | 7.3% |
| How often did you feel hopeless? | 120 | 21.0% | 146 | 25.5% | 125 | 21.9% | 123 | 21.5% | 58 | 10.1% |
| How often did you feel restless or fidgety? | 55 | 9.6% | 124 | 21.7% | 194 | 33.9% | 128 | 22.4% | 71 | 12.4% |
| How often did you felt so restless that you could not sit still? | 149 | 26.0% | 161 | 28.1% | 162 | 28.3% | 63 | 11.0% | 37 | 6.5% |
| How often did you feel depressed? | 67 | 11.7% | 139 | 24.3% | 149 | 26.0% | 108 | 18.9% | 109 | 19.1% |
| How often did you feel that all activities seemed like an effort? | 36 | 6.3% | 144 | 25.2% | 186 | 32.5% | 130 | 22.7% | 76 | 13.3% |
| How often did you feel so sad that nothing could cheer you up? | 106 | 18.5% | 169 | 29.5% | 150 | 26.2% | 95 | 16.6% | 52 | 9.1% |
| How often did you feel worthless? | 179 | 31.3% | 130 | 22.7% | 117 | 20.5% | 75 | 13.1% | 71 | 12.4% |
| Overall stress level | Normal | Mild | Moderate | Severe | ||||||
| 100 (17.5%) | 108 (18.9%) | 98 (17.1%) | 266 (46.5%) | |||||||
Personal Sources of Stress
The most-reported academic sources of stress (Table 3) are self-study strategy issues (58.4%), followed by difficulty in reading textbooks (58.2%), dissatisfaction with exam performance (50.5%), and concern about future careers (49%). Regarding psychological sources of stress, a lack of time management was the most frequently reported (56.5%), followed by less time for family or social life (48.4%), an inability to overcome distractors (36.4%), and peer competition (34.6%). Regarding health-related stress sources, 51.7% of the students reported sleeping difficulty, followed by depression (43.2%), food quality (29.2%), and chronic health problems (16.3%). Regarding environmental sources, uncomfortable classroom chairs was the most selected (61.4%), followed by overcrowded classrooms (39.5%), unclean classrooms (35.7%), and poor ventilation in the classrooms (34.3%).
Table 3.
Personal Sources of Stress for Bachelor of Medicine and Bachelor of Surgery Students
| Domain | Items | Disagree | Neutral | Agree |
|---|---|---|---|---|
| % | % | % | ||
| Academic sources | Skipping classes | 41.8% | 37.9% | 20.3% |
| Difficulty reading textbooks | 11.5% | 30.2% | 58.2% | |
| Self-study strategy issues | 9.8% | 31.8% | 58.4% | |
| Teamwork | 22.7% | 50.7% | 26.6% | |
| Dissatisfaction regarding exam performance | 11.2% | 38.3% | 50.5% | |
| Exposure to cadaver dissection and human suffering | 40.4% | 39.9% | 19.8% | |
| Concern for future careers | 13.5% | 37.6% | 49.0% | |
| Lack of interest in a subject/medicine | 39.9% | 38.1% | 22.0% | |
| Psychological sources | Inability to communicate with others in the field | 38.1% | 38.3% | 23.6% |
| Self-underestimation | 26.6% | 40.9% | 32.5% | |
| Lack of time for family or social life | 14.0% | 37.6% | 48.4% | |
| Lack of time management | 11.5% | 32.0% | 56.5% | |
| Peer competition | 21.9% | 43.5% | 34.6% | |
| Inability to overcome distractions; for example, smartphone addiction | 19.8% | 43.9% | 36.4% | |
| Health-related sources | Sleeping difficulties | 17.7% | 30.6% | 51.7% |
| Depression | 19.8% | 37.1% | 43.2% | |
| Chronic diseases (diabetes mellitus, asthma, anemia, hormones disturbances, thyroid disorders, vitamin D deficiency, etc.) | 64.7% | 19.1% | 16.3% | |
| Obesity | 61.7% | 24.8% | 13.5% | |
| Food quality | 29.7% | 41.1% | 29.2% | |
| Environmental sources | Poor classroom ventilation | 32.0% | 33.7% | 34.3% |
| Unclean classroom | 33.7% | 30.6% | 35.7% | |
| Uncomfortable classroom chairs | 15.2% | 23.4% | 61.4% | |
| High classroom temperature | 34.4% | 40.4% | 25.2% | |
| Low classroom temperature | 32.3% | 46.2% | 21.5% | |
| Overcrowded classroom | 25.5% | 35.0% | 39.5% | |
| Transportation issues | 44.6% | 30.1% | 25.3% | |
| Home environment | 50.2% | 25.9% | 24.0% |
Impact of Stress
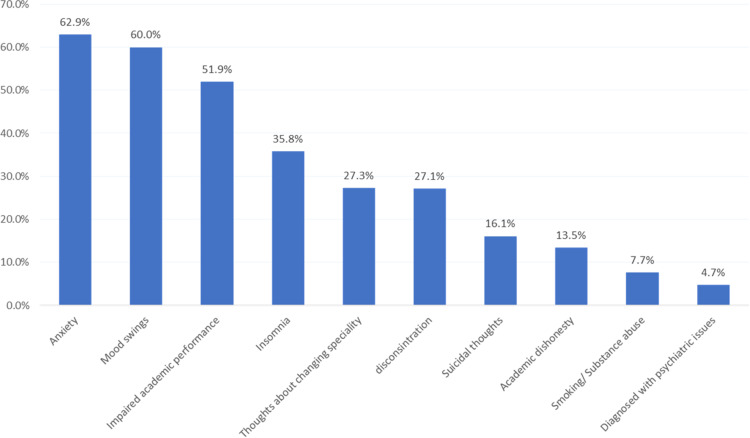
The most-reported impact of stress (Figure 1) was anxiety (62.9%), followed by mood swings (60%), impaired academic performance (51.9%), insomnia (35.8%), thoughts of changing specialties (27.3%), and bioconcentration (27.1%), while the least reported was developing psychiatric disorders (4.7%).
Figure 1.
Impact of stress on Bachelor of Medicine and Bachelor of Surgery students.
Suggested Solutions
Table 4 shows solutions the students suggested for stress management during the MBBS program. Exactly 71.9% of students rated the creation of a nurturing learning environment as an acceptable or excellent suggestion for minimizing stress, and 76% suggested identifying struggling students and giving them individualized support. Furthermore, 79.9% rated it acceptable or excellent for teachers to ensure a supportive learning environment, 73.6% suggested teaching students skills for stress management and promoting self-awareness, and 72.2% suggested encouraging students to promote personal health through regular physical activity and adequate sleep.
Table 4.
Suggestions and Solutions for Stress Management
| Suggestions | Completely Ineffective | Low level of Effectiveness | Acceptable | Good | Excellent | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | % | No | % | No | % | No | % | No | % | |
| Creating a nurturing learning environment | 47 | 8.2% | 114 | 19.9% | 175 | 30.6% | 127 | 22.2% | 109 | 19.1% |
| Identifying struggling students and providing specialized support | 56 | 9.8% | 81 | 14.2% | 145 | 25.3% | 115 | 20.1% | 175 | 30.6% |
| Teaching students stress management skills and promoting self-awareness | 51 | 8.9% | 100 | 17.5% | 124 | 21.7% | 144 | 25.2% | 153 | 26.7% |
| Encouraging students to promote personal health through regular physical activities and adequate sleep | 55 | 9.6% | 104 | 18.2% | 141 | 24.7% | 150 | 26.2% | 122 | 21.3% |
| Teachers ensuring a supportive learning environment for students | 38 | 6.6% | 77 | 13.5% | 124 | 21.7% | 131 | 22.9% | 202 | 35.3% |
Association Between Stress and Study Variables or Sociodemographic Data
Table 5 and Figure 2 show the determinants of stress in medical school during the MBBS course. Severe stress levels were detected among 60.7% of female students and 31% of male students, with statistical significance (P = 0.001). The highest prevalence of severe stress was detected among students who lacked learning resources (68.8%), followed by those who complained of ambiguity in teaching, learning, and assessment strategies (64.1%), and those who had problems with the teaching style (57.4%). The lowest stress level was detected among students who had tasks (16%) with statistically significant differences (P = 0.001). Other associations between variables are shown in Table 5. There are insignificant associations between stress levels and other sociodemographic data such as age (P = 0.085) and income level (P = 0.156), as seen in Table 5.
Table 5.
Determinants of Stress for Bachelor of Medicine and Bachelor of Surgery Students
| Factors | Stress Level | P-value* | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Normal | Mild | Moderate | Severe | ||||||
| No | % | No | % | No | % | No | % | ||
| Gender | |||||||||
| Male | 67 | 24.5% | 72 | 26.3% | 50 | 18.2% | 85 | 31.0% | 0.001 |
| Female | 33 | 11.1% | 36 | 12.1% | 48 | 16.1% | 181 | 60.7% | |
| Age (years) | |||||||||
| 18–21 | 64 | 19.6% | 71 | 21.8% | 51 | 15.6% | 140 | 42.9% | 0.085 |
| 22–23 | 33 | 14.8% | 36 | 16.1% | 43 | 19.3% | 111 | 49.8% | |
| 24–25 | 3 | 13.0% | 1 | 4.3% | 4 | 17.4% | 15 | 65.2% | |
| Academic year/batch | |||||||||
| Second year (batch 2019) | 38 | 18.4% | 52 | 25.2% | 28 | 13.6% | 88 | 42.7% | 0.107 |
| Third year (batch 2018) | 27 | 19.1% | 24 | 17.0% | 24 | 17.0% | 66 | 46.8% | |
| Fourth year (batch 2017) | 23 | 13.7% | 26 | 15.5% | 36 | 21.4% | 83 | 49.4% | |
| Fifth year (batch 2016) | 12 | 21.1% | 6 | 10.5% | 10 | 17.5% | 29 | 50.9% | |
| Income level | |||||||||
| Low | 0 | 0.0% | 6 | 31.6% | 2 | 10.5% | 11 | 57.9% | 0.156 |
| Average | 92 | 19.1% | 90 | 18.7% | 82 | 17.0% | 218 | 45.2% | |
| High | 8 | 11.3% | 12 | 16.9% | 14 | 19.7% | 37 | 52.1% | |
Notes: *Pearson chi-square test or exact probability test as appropriate. The difference is significant at P value < 0.05.
Figure 2.
Distribution of severe stress levels from most-reported stressor.
Discussion
Stress Levels
Almost half (46.5%) of the sampled students were severely distressed, according to the K10 test scores. Previous studies had shown high stress scores for medical students, particularly in the first year and decreasing significantly and progressively in the following years.2,5 Our results were similar to those of a university in Malaysia (48.6%)17 but showed lower stress levels than local universities: King Saud University, Riyadh (78.7%),11 and Imam Abdulrahman Bin Faisal University, Dammam (82.6%).5 This could be due to the different stress-assessment measurements used, or because of the higher ranking of those universities compared to UQU, which could add more pressure on students to keep their rankings high and meet their visions. The high levels of stress among UQU medical students may be related to the university’s recent changes in applying the new MBBS curriculum, teaching, and assessment methods. This update has revolutionized the educational experience for all staff, students, and lecturers and brought more challenges that may increase stress. The stress may be related to the nature of the reformed MBBS curriculum, which consists of integrated modules taught by different departments. This structure directs students to become more independent in studying and in linking the medical information together, thus adding much more responsibility and workload on the students. This is in line with previous studies that investigated the impact of curriculum changes on medical students’ stress.18,19 Conducting continuous training workshops about learning and studying skills may help students acquire the necessary skills and reduce their stress.
Personal Sources of Stress
The students revealed stressors regarding self-study strategy issues, followed by difficulty in reading textbooks; therefore, a learning skills course should be developed to address students’ needs and prepare them for new environments and challenges. A previous study conducted at UQU College of Medicine reported that most students understood the value of taking a learning skills course to meet the demands of university life during the transitional period.10 Interestingly, the present study adds certain environmental stressors, including uncomfortable chairs and overcrowded, unclean, and poorly ventilated classrooms. According to recent systematic reviews, a less favorable learning environment is one of the factors associated with the development of stress.20 Hence, UQU College of Medicine should adopt techniques to solve these problems. Developing and enhancing the college building may decrease students’ stress. Furthermore, several studies have found psychological and health-related issues resulting from stress, such as sleeplessness and depression.11,15,21,22
Predictors of Stress
Our study reports a statistically significant association between severe stress levels and the female gender. This result is consistent with other studies in the literature which reported that female medical students are significantly predisposed to a high level of stress.11,12,15,23,24 This might be due to the effect of gender differences in perceived stress and coping, as the genders are physiologically different.25 Other studies, however, found no significant association between gender and stress levels.2,26,27 This disagreement might be a result of different stress assessment methods or learning environments. Nevertheless, further studies are required to investigate this relationship. Furthermore, the current study did not find a significant association between stress levels and age or income level. This is consistent with the findings of other studies that stated that the severity of stress level was not significantly associated with age or income level of medical students.2,27,28,29 However, this is inconsistent with other studies in the literature that suggest that age and financial status are factors influencing the severity of stress.30–32 This disagreement might be explained by the fact that most participants in the present study are from a younger-generation age group (19–25 years) and about 84% of them are on an average monthly income.
For the most stressful aspects of the MBBS curriculum, a significant relationship to lack of learning resources was found, followed by unclear teaching, learning, and assessment strategies. Our findings can be explained by a lack of guidance and clarity. One reason is the focus of the new curriculum, which encourages medical students to use textbooks and understand the information without “spoon feeding.” It is worth mentioning that a previous study, conducted at UQU College of Medicine in 2010 during the period of the traditional curriculum, showed that medical students ranked peer competition (followed by poor English language skills) as the most difficult aspect during the MBBS course.10 Clearly, we can observe that these factors are not currently causing stress, because English language teaching has since improved.
Interestingly, the current study found a higher prevalence of severe stress levels during MBBS courses among the fifth-year students (batch 36, 2016) compared to a lower prevalence for the second-year students (batch 39, 2019). A study conducted in the United States demonstrated that there was a significant increase in risk of depression and perceived stress among third-year students, compared to first-year students.11 In contrast, another study conducted in the College of Medicine of King Saud University found that the level of stress decreased as the year of study progressed.2 This discrepancy can be explained by several factors: First, our study was conducted during the special circumstances of the coronavirus (COVID-19) pandemic of 2020, when schooling was halted at the beginning of the second semester. Hence, second-year students did not complete the entire year’s experience and the comprehensive exams. Second, fifth-year students were the first batch learning the new MBBS curriculum at UQU College of Medicine, which put additional pressure on them. In comparison, the second-year students are the fourth batch following the curriculum update. Moreover, the fifth-year students are near graduation; hence, they are more likely to work hard on the requirements of the Saudi Commission for Health Specialties to gain acceptance for postgraduate training programs, which adds more pressure on them.
Impact of Stress
Our study demonstrates that anxiety was the most common stress symptom in medical students (62.9%), followed by mood swings (60%), impaired academic performance (51.9), insomnia (35.8%), thoughts of changing specialties (27.3%), and poor concentration (27.1%). These findings are similar to those of several other studies in the literature.32,33 Studies conducted by Lakhiar et al.34 Yadav et al35 and Inam et al36 found that medical students had the highest level of anxiety and depression compared to students of other specialties. An Indian study reported that medical students with high stress levels suffer from low concentration (86%) and mood changes (80%). These statistics are far higher than our findings;37 this could be due to differences in lifestyles and the study curriculum. A local study in Riyadh demonstrated that medical students had a high level of stress, and that there was a significant correlation between high stress and low GPA (P = 0.01).27 Another local study in Rabigh exhibited similar findings: students with high stress had lower grades in comparison to those with low stress.3 Consistent results in a Pakistani study found an inverse correlation between stress and academic performance; the higher the stress, the lower the academic performance.36 This may be because stress leads to overthinking, affecting preparation and concentration during studying, and decreasing sleep quality. This was proved by the study of Almojali et al, which found that high stress was associated with poor sleep quality, which correlated with lower GPA.26 Unfortunately, there is no specific study focused on medical students’ thoughts on changing specialties, but a similar study, involving medical students and residents, found that 12.1% of participants thought about withdrawing from medical school.37
Limitations, Strengths, and Recommendations
This study examines stress and the learning environment among medical students in the new MBBS curriculum of UQU from novel and multifaceted perspectives. However, our study has certain limitations. First, the shared-method bias is probable, since medical students were the only reporters for all study variables and a self-report survey was the only tool used for data collection. Second, the data of the present study is perception-based data and was collected during the COVID-19 pandemic, which presents more challenges for medical students. Despite these limitations, our study’s findings emphasize the presence of high stress levels among medical students at UQU and clarify the aspects needing improvement within the learning environment. It also sheds light on the difficulties that students face in medical schools and proposes solutions. We recommend further studies on female medical students to examine possible precipitating factors of their stress levels. Further follow-up studies are necessary to elucidate the determinants of our observed and severe stress levels among fifth-year medical students, and to promote the planning of interventions that can help students cope with future challenges. The COVID-19 pandemic could have influenced students’ responses. Hence, future investigations should be conducted under more favorable circumstances.
Conclusion
The current study concluded that medical students face high stress, which is potentially expensive to both the student and society in terms of maladaptive stress coping mechanisms, personal and academic burnout, and decrease in resiliency. Therefore, professors and universities should look out for potential stressors and help students overcome them. Universities can also improve this situation by offering counseling services to students. Another way to overcome this problem would be to introduce compulsory stress-management training, as a part of the medical syllabus that students would not be able to skip due to academic pressure. Moreover, extracurricular activities such as physical activities or arts and music might help.
Changing the MBBS curriculum could be the reason for the increased stress levels, as the current study observed a statistically significant association between severe stress levels and a lack of learning resources, as well as complaints regarding unclear teaching. Thus, it may be worthwhile to consider orientation programs each year for students and staff, to increase their awareness and knowledge about the program structure, assessment method, and learning styles and resources. In addition, improving the learning resources—particularly the library services—will help students see their accomplishments in a more positive light and help protect them from academic burnout.
Acknowledgment
We would like to express our gratitude to the Umm Al-Qura University medical students who generously answered the study’s questionnaire.
Data Sharing Statement
The original contributions presented in the study are included in the article. Further inquiries can be directed to the corresponding author.
Ethical Approval
Ethical approval was obtained from the Biomedical Ethics Committee of the Faculty of Medicine at Umm Al-Qura University (approval number HAPO-02-K-012-2020-08-430) and was conducted in accordance with the Declaration of Helsinki. Electronic informed consent was obtained from each participant prior to their answering the questionnaire. Participant privacy was ensured. No names or telephone numbers were requested from any participant.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Spielberger CD. Stress and anxiety in sports. In: Anxiety in Sports. Taylor & Francis; 2021:3–17. [Google Scholar]
- 2.Rahman AGA, Al Hashim BN, Al Hiji NK, Al-Abbad Z. Stress among medical Saudi students at college of medicine, King Faisal University. J Prev Med Hyg. 2013;54(4):195. [PMC free article] [PubMed] [Google Scholar]
- 3.Gazzaz ZJ, Baig M, Al Alhendi BSM, et al. Perceived stress, reasons for and sources of stress among medical students at Rabigh Medical College, King Abdulaziz University, Jeddah, Saudi Arabia. BMC Med Educ. 2018;18(1):1–9. doi: 10.1186/s12909-018-1133-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Habeeb KA. Prevalence of stressors among female medical students Taibah university. J Taibah Univ Med Sci. 2010;5(2):110–119. doi: 10.1016/S1658-3612(10)70140-2 [DOI] [Google Scholar]
- 5.Rafique N, Al-Asoom LI, Latif R, Al Sunni A, Wasi S. Comparing levels of psychological stress and its inducing factors among medical students. J Taibah Univ Med Sci. 2019;14(6):488–494. doi: 10.1016/j.jtumed.2019.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta S, Choudhury S, Das M, Mondol A, Pradhan R. Factors causing stress among students of a medical college in Kolkata, India. Educ Health. 2015;28(1):92. doi: 10.4103/1357-6283.161924 [DOI] [PubMed] [Google Scholar]
- 7.Khan TM, Bibi S, Shoaib T, et al. Perceived Stress and food consumption frequency among medical students of Rawalpindi Medical University, Pakistan. Eur J Med Health Sci. 2020;2(6):612. [Google Scholar]
- 8.Norphun N, Pitanupong J, Jiraphan A. Stress and coping strategies among Thai Medical Students in a Southern Medical School. Siriraj Med J. 2020;72:238–244. [Google Scholar]
- 9.Salam A, Mahadevan R, Rahman AA, Abdullah N, Abd Harith AA, Shan CP. Stress among first and third year medical students at University Kebangsaan Malaysia. Pak J Med Sci. 2015;31(1):169. doi: 10.12669/pjms.311.6473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Almoallim H, Aldahlawi S, Alqahtani E, Alqurashi S, Munshi A. Difficulties facing first-year medical students at Umm Alqura University in Saudi Arabia. East Mediterr Health J. 2010;16(12):1272–1277. doi: 10.26719/2010.16.12.1272 [DOI] [PubMed] [Google Scholar]
- 11.Abdulghani HM, AlKanhal AA, Mahmoud ES, Ponnamperuma GG, Alfaris EA. Stress and its effects on medical students: a cross-sectional study at a college of medicine in Saudi Arabia. J Health Popul Nutr. 2011;29(5):516. doi: 10.3329/jhpn.v29i5.8906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aboalshamat K, Hou XY, Strodl E. Psychological well-being status among medical and dental students in Makkah, Saudi Arabia: a cross-sectional study. Med Teach. 2015;37(sup1):S75–S81. doi: 10.3109/0142159X.2015.1006612 [DOI] [PubMed] [Google Scholar]
- 13.University UAQ. General Introduction of UQU MED Reformed MBBS Curriculum. Umm Al-Qura university; 2016. Availabe from: https://uqu.edu.sa/en/colmedsc/80135. Accessed December 14, 2021 [Google Scholar]
- 14.Dean AG, Sullivan KM, Soe MM. OpenEpi open source epidemiologic statistics for public health. Open EPI; 2013. Availabe from: https://www.openepi.com/Menu/OE_Menu.htm. Accessed August 01, 2020. [Google Scholar]
- 15.Muzafar Y, Khan HH, Ashraf H, et al. Burnout and its associated factors in medical students of Lahore, Pakistan. Cureus. 2015;7(11):e390. doi: 10.7759/cureus.390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silva BFPD, Santos-Vitti L, Faro A. Kessler Psychological distress scale: internal structure and relation to other variables. Psico-USF. 2021;26(1):91–101. doi: 10.1590/1413-82712021260108 [DOI] [Google Scholar]
- 17.Sherina MS, Rampal L, Kaneson N. Psychological stress among undergraduate medical students. Med J Malaysia. 2004;59(2):207–211. [PubMed] [Google Scholar]
- 18.Lyndon MP, Henning MA, Alyami H, Krishna S, Yu TC, Hill AG. The impact of a revised curriculum on academic motivation, Burnout, and Quality of Life Among Medical Students. J Med Educ Curric Dev. 2017;4:238212051772190. doi: 10.1177/2382120517721901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woloschuk W, Mandin H, Harasym PH. The impact of curriculum change on student stress and workload. In: Advances in Medical Education. Netherlands: Springer; 1997:812–814. doi: 10.1007/978-94-011-4886-3_249 [DOI] [Google Scholar]
- 20.Bhurtun HD, Azimirad M, Saaranen T, Turunen H. Stress and coping among nursing students during clinical training: an integrative review. J Nurs Educ. 2019;58(5):266–272. doi: 10.3928/01484834-20190422-04 [DOI] [PubMed] [Google Scholar]
- 21.Moutinho ILD, Maddalena NDCP, Roland RK, et al. Depression, stress and anxiety in medical students: a cross-sectional comparison between students from different semesters. Rev Assoc Med Bras. 2017;63(1):21–28. doi: 10.1590/1806-9282.63.01.21 [DOI] [PubMed] [Google Scholar]
- 22.Saipanish R. Stress among medical students in a Thai medical school. Med Teach. 2003;25(5):502–506. doi: 10.1080/0142159031000136716 [DOI] [PubMed] [Google Scholar]
- 23.Shah M, Hasan S, Malik S, Sreeramareddy CT. Perceived stress, sources and severity of stress among medical undergraduates in a Pakistani medical school. BMC Med Educ. 2010;10:2. doi: 10.1186/1472-6920-10-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Backović DV, Zivojinović JI, Maksimović J, Maksimović M. Gender differences in academic stress and burnout among medical students in final years of education. Psychiatr Danub. 2012;24(2):175–181. [PubMed] [Google Scholar]
- 25.Graves BS, Hall ME, Dias-Karch C, Haischer MH, Apter C. Gender differences in perceived stress and coping among college students. PLoS One. 2021;16(8):e0255634. doi: 10.1371/journal.pone.0255634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Almojali AI, Almalki SA, Alothman AS, Masuadi EM, Alaqeel MK. The prevalence and association of stress with sleep quality among medical students. J Epidemiol Glob Health. 2017;7(3):169–174. doi: 10.1016/j.jegh.2017.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Waqas A, Khan S, Sharif W, Khalid U, Ali A. Association of academic stress with sleeping difficulties in medical students of a Pakistani medical school: a cross sectional survey. PeerJ. 2015;3:e840. doi: 10.7717/peerj.840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shadid A, Shadid AM, Shadid A, et al. Stress, burnout, and associated risk factors in medical students. Cureus. 2020. doi: 10.7759/cureus.6633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Faisal M, Ali Khalid M, Bin Khalid M. Comparison of level of stress among medical students of private and government medical college in Pakistan. Malays J Med Sci. 2018;3(1):12–18. [Google Scholar]
- 30.Babar V, Gedam SR, Manore S, Dewangan K, Gaikwad P, Patond S. Study of stress, anxiety, depression, coping, and associated factors among medical students from central India. J Datta Meghe Inst Med Sci Univ. 2020;15:391–396. doi: 10.4103/jdmimsu.jdmimsu_226_20 [DOI] [Google Scholar]
- 31.Hammer LB, Grigsby TD, Woods S. The Conflicting Demands of Work, Family, and School Among Students at an Urban University. J Psychol. 1998;132(2):220–226. doi: 10.1080/00223989809599161 [DOI] [Google Scholar]
- 32.Sreeramareddy CT, Shankar PR, Binu V, Mukhopadhyay C, Ray B, Menezes RG. Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Med Educ. 2007;7(1):26. doi: 10.1186/1472-6920-7-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ludwig AB, Burton W, Weingarten J, Milan F, Myers DC, Kligler B. Depression and stress amongst undergraduate medical students. BMC Med Educ. 2015;15:141. doi: 10.1186/s12909-015-0425-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lakhiar MA, Mughal SA, Bhattia MR. Anxiety & Depression; Prevalence Among the Students of Peoples University of Medical and Health Sciences for Women Nawabshah: a Rural Perspective. Prof Med J. 2017;24(4). doi: 10.29309/TPMJ/2017.24.04.1457 [DOI] [Google Scholar]
- 35.Yadav R, Gupta S, Malhotra AK. A cross sectional study on depression, anxiety and their associated factors among medical students in Jhansi, Uttar Pradesh, India. Int J Community Med Public Health. 2016;3(5):1209–1214. doi: 10.18203/2394-6040.ijcmph20161386 [DOI] [Google Scholar]
- 36.Inam SNB, Saqib A, Alam E. Prevalence of anxiety and depression among medical students of private university. J Pak Med Assoc. 2003;53(2):44–46. [PubMed] [Google Scholar]
- 37.Ranade A, Kulkarni G, Dhanumali S. Stress study in 1st year medical students. Int J Biomed Adv Res. 2015;6(6):499e503. [Google Scholar]
- 38.Sohail N. Stress and academic performance among medical students. J Coll Physicians Surg Pak. 2013;23(1):67–71. [PubMed] [Google Scholar]
- 39.Pokhrel NB, Khadayat R, Tulachan P. Depression, anxiety, and burnout among medical students and residents of a medical school in Nepal: a cross-sectional study. BMC Psychiatry. 2020;20(1):1–18. doi: 10.1186/s12888-020-02645-6 [DOI] [PMC free article] [PubMed] [Google Scholar]