Abstract
To assess the impact of COVID-19 lockdown measures on dry-eye symptoms in a community-based population, a cross-sectional study was conducted during the first wave of the COVID-19 outbreak in Thailand. An online survey was distributed via social media between June and July 2020. The questionnaire elicited information on demographics, dry-eye symptoms, use of visual display terminals, and mental health status. There were 535 respondents. Thirty-seven percent reported having been diagnosed with dry-eye disease (DED). During the lockdown, the mean dry-eye symptom score (DESS) of overall participants dropped significantly from 81.6 ± 15.9 to 79.8 ± 17.4 (P < 0.001). The mean, daily, visual display terminal (VDT) usage increased from 10.55 ± 5.16 to 13.08 ± 5.65 h (P < 0.001). A negative correlation between age and VDT usage was observed in both the normal and lockdown situations. One-quarter of all participants had an abnormal mental health status. The female gender (OR 1.86; 95% CI 1.14–3.04) and increased VDT usage during the lockdown (OR 5.68; 95% CI 3.49–9.23) were independently associated with worsening dry-eye symptoms. The lockdown measures abruptly altered the behaviors and lifestyles of the overall population. Excessive exposure to VDTs were associated with deteriorated dry-eye symptoms, and it possibly contributed to the increased DED incidence in the surveyed population.
Subject terms: Corneal diseases, SARS-CoV-2, Risk factors
Introduction
The outbreak of coronavirus disease 2019 (COVID-19) had a massive impact on global health systems1. In March 2020, COVID-19 was declared a pandemic disease by the World Health Organization. The disease is highly contagious in aerosol form and on contaminated surfaces2. As of July 2021, there had been 179.9 million cases in 222 countries, with 3.9 million mortalities. To curb the spread of COVID-19, numerous countries, including Thailand, imposed extraordinary measures, such as lockdowns, flight restrictions, social distancing, working from home, and department-store closures.
The COVID-19 lockdown measures enforced during 2020 had a major impact on the lifestyles and viewing habits of the world population. People were reported to be spending more time indoors, in some cases, up to 20–24 h per day3. Students and company employees were forced to study, work, and attend meetings online. The use of visual display terminals (VDTs), which include computer screens, tablets and smartphones, rose significantly, whereas the undertaking of physical activities declined4–6. While focusing on VDTs, a longer blinking interval exacerbates the evaporation of tears and eventually increases the risk of developing dry-eye disease (DED)7–10.
Moreover, the pandemic outbreak along with self-isolation measures impaired the overall population’s mental health status3. Community-based adults spent excessive amounts of time following COVID-19 news updates, which was found to be positively associated with mental health problems such as acute stress, anxiety, and depression11–14. Moreover, an association between psychiatric disorders and DED was reported by several studies15–20.
In the past, when people used VDTs relatively infrequently, the prevalence of DED was reported to range from 5 to 50%, to increase with age, and to disproportionately affect women more than men21–23. However, the marked rise in VDT usage during the last decade has corresponds to a shift in the epidemiology of DED. The condition now affects younger ages as well as both genders equally10,24. DED symptoms include discomfort, grittiness, tearing, a burning sensation, and vision fluctuation. The main treatments are the administration of tear substitutes, secretagogues, and anti-inflammatory drugs25. DED was reported to negatively impact work productivity and the quality of life26,27. Moreover, the increasing number of cases of DED was estimated to have an enormous negative impact upon economies and healthcare systems across Asia, Europe, and the United States28.
The objective of this study was to assess the impact of the COVID-19 lockdown measures on dry-eye symptoms in the Thai population. The study also examined how the lockdown affected mental health and VDT-viewing habits in Thailand, and their associations with dry-eye symptoms.
Materials and methods
This cross-sectional study was carried out online during the first COVID-19 lockdown period in Thailand (June to July 2020). The procedures followed the tenets of the Declaration of Helsinki. Before commencement of this research, its protocol was approved by the Committee for the Protection of Human Participants in Research, Faculty of Medicine, Siriraj Hospital (approval number: 517/2020). The work was registered at the Thai Clinical Trials Registry (TCTR20200709002).
The survey was conducted using an online survey portal, Google Forms. Responses were voluntary and anonymous. An online link targeting a community-based population was sent via social networks such as Facebook, Line, and WhatsApp. In all, 535 individuals responded. The survey questionnaire was divided into 4 sections: demographic data, dry-eye symptoms, VDT-viewing habits, and mental health.
The respondents who reported having been diagnosed with DED by an ophthalmologist were assigned to a “DED group” for analysis purposes. The remaining participants became the controls and were allotted to a “non-DED group”. The dry-eye-symptom portion of the study questionnaire was modified and translated from a symptom questionnaire developed by Kojima and associates in 201129. The questionnaire was culturally adapted and translated into Thai by 3 qualified native-Thai cornea specialists proficient in spoken and written English (PP, CC, PN). To do this, the specialists made independent translations of the original English version, and the final Thai version was decided after discussion by the specialists. The scale's internal consistency was calculated using Cronbach's alpha coefficient (Cronbach's alpha = 0.912). The construct validity was evaluated by using the correlation between the total scores of a Thai version of the Dry Eye–Related Quality-of-Life Score (DEQS-Th) questionnaire30 and the dry-eye symptom score (DESS) of this study. Higher DESS scores indicate fewer dry-eye symptoms, whereas DEQS-Th scores indicate the opposite. The correlation coefficient between the total scores of the scales was − 0.805 (P < 0.001). The test–retest reliability showed a significant correlation between the first and second applications, with r = 0.921 (P < 0.001). The DESS consisted of 14 self-assessment questions addressing the common dry-eye-related ocular symptoms. They were dryness; irritation; grittiness; soreness; fatigue; eye strain; redness; itching; difficulty opening the eyelids; discomfort; drowsiness; and limitations while reading, operating a computer, or watching television. Each question was graded by frequency: no symptoms, 4 points; hardly ever, 3 points; sometimes, 2 points; often, 1 point; and always, 0 points. The final DESS was calculated by (the sum of scores for all answered questions × 100)/(number of answered questions × 4). The DESS ranged from 0 to 100, with higher scores signifying fewer dry-eye symptoms.
To evaluate the VDT-viewing habits of the participants, the average number of hours they were exposed to VDTs each day, by purpose, were asked. Averages were obtained for both the pre-lockdown (“normal”) and lockdown situations. The lockdown period was defined as the time between March 22, 2020 and the day the survey was completed. Four categories of VDT usage were identified: (1) work/study, (2) social media, (3) video logs/TV series/movies, and (4) news updates. The term “long-time VDT usage” was defined as a daily average of 6 or more hours exposure to VDTs31.
The Thai General Health Questionnaire-12 (Thai GHQ-12) was used to evaluate the mental health status of the respondents32. It contained 4 questions related to major mental health problems: anxiety, social impairment, unhappiness, and hypochondriasis. Each question assessed the severity of mental problems over the preceding few weeks. The total-score range was 0 to 12, with higher scores indicating worse conditions. A total score greater than or equal to 2 was considered to represent an abnormal mental health status.
Statistical analysis
The data analyses were performed using PASW Statistics for Windows (version 18.0; SPSS Inc., Chicago, IL, USA). Categorical variables are reported as N (%), and continuous variables as mean (SD). Associations between variables were tested using univariate analysis (chi-squared test). Factors with P < 0.1 in the univariate analysis were entered in a multivariate logistic regression model to identify the variables contributing to the worsening of dry-eye symptoms during COVID-19. Spearman’s correlation was used to identify relationships between pairs of ordinal or continuous data. The odds ratios (OR) and corresponding 95% CI were used to determine strengths of association. A P value of < 0.05 was deemed statistically significant.
Human rights statements and informed consent
This study was performed in accordance with the Declaration of Helsinki and approved by the ethical committee on human experimentation of Faculty of Medicine Siriraj Hospital, Thailand. Informed consent was obtained, by requiring all respondents to answer the acceptance checkbox, before being included in the study.
Animal rights
This study did not associate with any animal subject.
Results
A total of 535 survey responses were recorded. The ages of the participants ranged from 18 to over 80 years, with the most frequent age range being 51–60 years (37.2%; Fig. 1). Sixty-seven percent (67.3%) were women. Thirty-seven percent (37.2%) of all participants reported they had been diagnosed with DED by an ophthalmologist. Concurrent ocular disorders were predominantly refractive error (73.2%), followed by vitreous degeneration (13.1%) and allergy (10.1%). Most DED patients used 1 or 2 types of dry-eye medication (88.9%), with 59.8% of the patients using only 1 type. The frequency of dry-eye medication usage was generally less than 4 times a day (90.9%), and 41.7% used it less than once daily.
Figure 1.
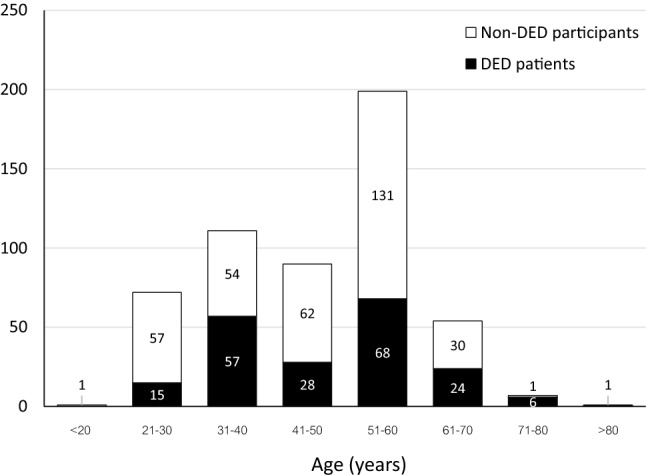
Distribution of ages of participants.
During the COVID-19 lockdown, the overall DESS dropped significantly from a mean of 81.6 ± 15.9 to 79.8 ± 17.4 (P < 0.001). The DESS also decreased significantly for the DED patients during the lockdown, from 74.1 ± 14.6 to 72.2 ± 16.0 (P < 0.001). Similarly, for the non-DED group, the DESS fell from 86.0 ± 15.0 to 84.3 ± 16.7 (P < 0.001). However, there was no statistical difference in the degrees by which the DESS of the DED and non-DED groups declined (P = 0.69). In terms of age, the DESS was lowest for the 21–30 age group (normal situation, 75.97 ± 17.62; during the lockdown, 73.46 ± 18.68; P < 0.001). The DESS was highest for the 51–60 age group (normal, 85.86 ± 13.41; lockdown, 84.08 ± 15.30; P < 0.001; Fig. 2). For the participants who were 60 years old or less, the DESS dropped significantly during the lockdown for both the DED and the control group (DED group, from 74.16 ± 13.94 to 71.96 ± 15.21, with P < 0.001; non-DED group, from 85.9 ± 15.36 to 84.05 ± 17.18, with P < 0.001). In the case of the respondents who were older than 60 years, there was a nonsignificant change in the DESS for both the DED and non-DED groups (DED group, from 73.8 ± 17.7 to 73.2 ± 19.9, with P = 0.64; non-DED group, from 87.0 ± 10.2 to 86.2 ± 10.9, with P = 0.17; Table 1). When the subjects experienced eye discomfort, 40.3% rested their eyes, 31.9% used artificial tears, 15.8% increased their eye-blinking rate, and 2.5% rinsed their eyes with tap water. During the lockdown, 10.6% of the DED patients used artificial tears more often while 8.6% used them less frequently; the rest maintained their normal frequency.
Figure 2.
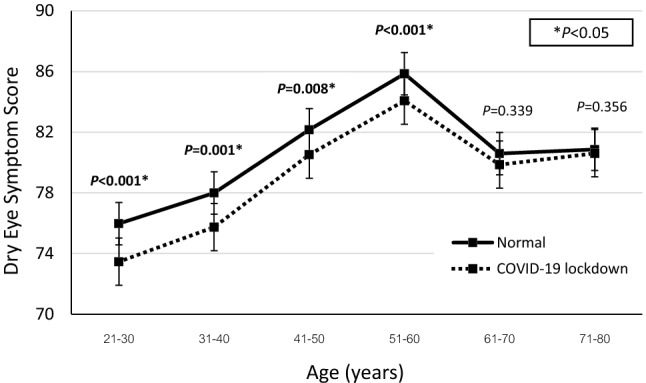
Dry-eye symptom scores (DESS) of each age group for normal and COVID-19 lockdown situations.
Table 1.
Comparison of the mean dry-eye symptom scores of the dry-eye and non-dry-eye participants.
| Dry-eye symptom score | P | ||
|---|---|---|---|
| Normal situation | COVID-19 lockdown | ||
| Mean (SD) | Mean (SD) | ||
| Dry-eye participants | |||
| Total | 74.10 (14.55) | 72.16 (15.98) | < 0.001* |
| Age ≤ 60 years | 74.16 (13.94) | 71.96 (15.21) | < 0.001* |
| Age > 60 years | 73.79 (17.73) | 73.21 (19.88) | 0.639 |
| Non-dry-eye participants | |||
| Total | 86.00 (14.95) | 84.25 (16.70) | < 0.001* |
| Age ≤ 60 years | 85.9 (15.36) | 84.05 (17.18) | < 0.001* |
| Age > 60 years | 86.98 (10.15) | 86.23 (10.88) | 0.167 |
*P < 0.05; higher dry-eye symptom score indicates fewer dry-eye symptoms.
Daily VDT usage rose significantly during the lockdown, from a mean of 10.55 ± 5.16 h to 13.08 ± 5.65 h (P < 0.001). For the participants aged up to 60 years, the daily hours went up from 11.03 ± 5.17 to 13.74 ± 5.50 (P < 0.001). As to the participants older than 60 years, their average grew from 6.84 ± 3.32 to 8.05 ± 4.15 h (P < 0.001; Table 2). There was a negative correlation between age and VDT usage during both the normal and lockdown situations (normal, Spearman’s rho = − 0.386, with P < 0.001; lockdown, rho = -0.374, with P < 0.001). The prevalence of long-time VDT usage climbed for all purposes: news updates, watching movies and videos, social media surfing, and work/study (Fig. 3). In both the normal and lockdown situations, work/study was the major activity contributing to prolonged VDT usage. However, the greatest increase in the number of participants using VDTs for extended periods was demonstrated by those using VDTs for entertainment purposes (such as watching movies and videos).
Table 2.
Visual display terminal usage of each age group during the normal and COVID-19 lockdown situations.
| Age range | VDT usage (h) | P | |
|---|---|---|---|
| Normal situation | COVID-19 lockdown | ||
| Mean (SD) | Mean (SD) | ||
| Age ≤ 60 years | |||
| Total | 11.03 (5.17) | 13.74 (5.50) | < 0.001* |
| 21–30 | 13.64 (4.59) | 15.92 (4.96) | < 0.001* |
| 31–40 | 12.29 (5.47) | 14.69 (5.60) | < 0.001* |
| 41–50 | 10.47 (5.03) | 13.78 (5.09) | < 0.001* |
| 51–60 | 9.61 (4.73) | 12.36 (5.43) | < 0.001* |
| Age > 60 years | |||
| Total | 6.84 (3.32) | 8.05 (4.15) | < 0.001* |
| 61–70 | 6.84 (3.08) | 8.15 (4.13) | < 0.001* |
| 71–80 | 6.71 (5.28) | 7.36 (4.87) | 0.001* |
*P < 0.05.
Figure 3.
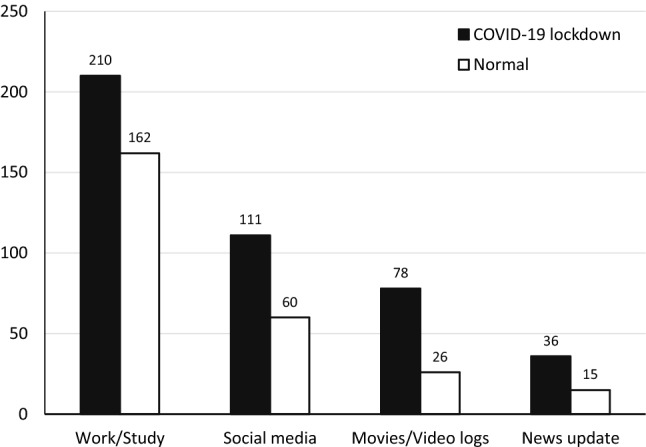
The number of participants using long-time visual display terminals, by purpose, during the normal and COVID-19 lockdown situations.
During the lockdown, one-quarter of all participants reported mental health problems (25.9%). The top-rated abnormalities were feeling constantly under strain, feeling unhappy, and not enjoying normal daily activities. The overall Thai GHQ-12 score during the lockdown showed nonsignificant differences between age groups (1.84 ± 2.65 for participants aged up to 60, vs 1.23 ± 2.09 for older respondents; P = 0.082); genders (1.69 ± 2.60 for males, vs 1.80 ± 2.59 for females; P = 0.650); and the presence of concurrent DED (1.71 ± 2.48 for the DED group, vs 1.79 ± 2.66 for the non-DED group; P = 0.727). Participants with a DESS of less than 75 were associated with having abnormal mental health during the lockdown (OR 1.91; 95% CI 1.28–2.84; Table 3). Actions to cope with the stress during the pandemic were buying personal protective equipment such as face masks (30.8%); following COVID-news updates (24.8%); exercising (24.4%); minimizing watching, reading, or listening to COVID-19 news (9.4%); meditation/praying (8.4%); and staying at home (2.1%).
Table 3.
Risk factors for abnormal Thai GHQ-12 score during the lockdown.
| Thai GHQ-12 score; n (%) | P | OR | 95% CI | ||
|---|---|---|---|---|---|
| Normal | Abnormal | ||||
| Age ≤ 60 years | 347 (87) | 126 (92) | 0.163 | 1.68 | (0.85–3.33) |
| Female | 264 (66) | 96 (70) | 0.461 | 1.19 | (0.78–1.81) |
| DED patients | 149 (37) | 50 (36) | 0.918 | 0.96 | (0.64–1.44) |
| DESS < 75 | 118 (30) | 61 (45) | 0.002* | 1.91 | (1.28–2.84) |
*P < 0.05; DED dry-eye disease, DESS dry-eye symptom score.
In the univariate analysis, the risk factors found to be associated with worsened dry-eye symptoms during the COVID-19 lockdown were an age up to 60 (OR 2.56; 95% CI 1.19–5.52); female (OR 2.07; 95% CI 1.32–3.26); increased VDT usage during the lockdown (OR 6.49; 95% CI 4.03–10.46); having concurrent ocular allergic diseases (OR 2.16; 95% CI 1.21–3.87); and an abnormal Thai GHQ-12 score (OR 1.93; 95% CI 1.27–2.95). DED, glaucoma, and a decreased frequency of artificial-tear use were not significantly associated. The multivariate analysis showed that being female (OR 1.86; 95% CI 1.14–3.04) and a greater VDT usage during the lockdown (OR 5.68; 95% CI 3.49–9.23) were independently associated with deteriorating dry-eye symptoms (Table 4).
Table 4.
Univariate and multivariate analyses of risk factors that worsened dry-eye symptoms during the lockdown.
| Risk factors | DED symptoms worsened | DED symptoms not worsened | P | OR | 95% CI |
|---|---|---|---|---|---|
| N (%) | N (%) | ||||
| Age ≤ 60 years | 130 (94.2) | 343 (86.4) | 0.02* | 2.56 | 1.19–5.52 |
| DED | 56 (40.6) | 143 (36.0) | 0.36 | 1.21 | 0.82–1.80 |
| Female | 108 (78.3) | 145 (36.5) | 0.001* | 2.07 | 1.32–3.26 |
| Increased VDT usage during the lockdown | 113 (81.9) | 163 (41.1) | < 0.001* | 6.49 | 4.03–10.46 |
| Ocular allergic disease | 22 (15.9) | 32 (8.1) | 0.01* | 2.16 | 1.21–3.87 |
| Glaucoma | 6 (4.3) | 11 (2.8) | 0.4 | 1.6 | 0.58–4.40 |
| Abnormal Thai GHQ-12 score | 49 (35.5) | 88 (22.2) | 0.002* | 1.93 | 1.27–2.95 |
| In DED participants | N = 56 | N = 143 | |||
| Decreased frequency of artificial tear use during COVID-19 lockdown | 6 (10.7) | 20 (14.0) | 0.64 | 0.72 | 0.27–1.91 |
| Risk factors | P | OR | 95% CI | ||
|---|---|---|---|---|---|
| Multivariate analysis | |||||
| Age ≤ 60 years | 0.11 | 1.959 | 0.86–4.47 | ||
| Female | 0.012* | 1.864 | 1.14–3.04 | ||
| Increased VDT usage during the lockdown | < 0.001* | 5.676 | 3.49–9.23 | ||
| Ocular allergic disease | 0.263 | 1.437 | 0.76–2.71 | ||
| Abnormal Thai GHQ-12 score | 0.06 | 1.549 | 0.98–2.45 | ||
* P < 0.05; DED, dry-eye disease; VDT, visual display terminal.
Discussion
COVID-19 lockdowns around the world vastly altered people’s lifestyles, activities, and behaviors. To date, several waves of the COVID-19 pandemic have occurred globally, including in Thailand. Since the first wave caused the most abrupt changes in personal behaviors and mental stress, the present cross-sectional study was carried out to determine the effects of the lockdown in Thailand on dry-eye symptoms, and their potential risk factors.
Based-on the participants’ responses, 37.2% had been diagnosed with DED by an ophthalmologist. More than half of the DED participants had a mild severity, indicated by only 1 kind of medication being used and a usage frequency of less than once daily. Dry-eye symptoms were worst among the young adults, but better in the middle to older age groups. This study proved that the COVID-19 lockdown exacerbated the dry-eye symptoms of both DED patients and normal subjects aged up to 60. The correlated risk factors were being female and increased VDT usage. Viewing habits were significantly altered by the COVID-19 lockdown. There was an obvious rise in the average daily VDT usage for all purposes. The number of participants engaging in prolonged VDT usage for entertainment purposes during the lockdown was triple that during pre-lockdown. Moreover, a quarter of all participants experienced mental health problems during the lockdown. Having a mental health abnormality was also associated with having more severe dry-eye symptoms.
This community-based survey reflected the dry-eye symptoms of the overall population. It demonstrated that there was an abundance of people who suffered with dry-eye symptoms but were not seeking medical care or were unaware of the importance of DED treatment and prevention. Surprisingly, this study revealed a shift in that the younger adults reported having more severe dry-eye symptoms than the elderly respondents, especially during the lockdown (Fig. 2). Also, the prevalence of DED was relatively high in participants aged 31–40 years (51% of them had a diagnosis of DED). This result contrasted with those of other studies, which showed that DED prevalence increased with age and mostly affected women23,33. However, the epidemiology report of TFOS DEWS II (Tear Film and Ocular Surface Society Dry Eye Workshop II) declared that relatively high DED prevalence rates were present in younger people and school children34. Nowadays, the rise in VDT usage might be affecting DED prevalence10,24, especially during COVID-19 outbreaks when work-from-home and lockdown measures are instituted. This study identified that younger adults were exposed to VDTs longer than the elderly in both the normal and lockdown situations (Table 2) as there was a negative correlation between age and VDT usage. A rise in VDT usage was noticeably associated with worsened dry-eye symptoms, regardless of the presence of DED, which resulted in a lower DESS for the younger adults than the elderly respondents. This implies that the negative impact of VDT usage, as an external factor, could even overcome the internal risk factors of DED. Therefore, DED could eventually cause a bigger problem than we are presently experiencing. The change in lifestyles and viewing habits of the new generation could progressively increase the prevalence of DED. This would place a sizeable burden on national economies, health care systems, and workplace productivity.
The overall dry-eye symptoms were worse during the lockdown than in the normal situation. However, there was no statistical difference in the degree of reduction in the DESS of the DED and non-DED groups during the lockdown. This might be because most of our DED participants had only a mild degree of the disease. Alternatively, it might be that the potential risk factors during the lockdown (for instance, VDT usage8,9, lower indoor humidity35,36, and more mental health problems16,17) affected both groups equally.
Interestingly, while young to middle-aged adults suffered from a worsening of dry-eye symptoms during the lockdown, only the participants older than 60 showed no significant change. This result can be supported by the observation that during the COVID-19 lockdown, the lifestyles of mostly retired participants were not as altered as much as those of the younger ones. During both the normal and the lockdown situation, elderly Thais would typically spend most of their time indoors, away from sunlight, smoke, and wind. Even though there was an overall rise in daily VDT exposure among the elderly participants, the increment in VDT usage was still only half as much as that of the younger viewers. Further studies on behavioral changes during the lockdown of elderly people would be required to confirm this hypothesis.
In the univariate analysis, several risk factors were found to be correlated with the worsening of the dry-eye symptoms during the lockdown. However, the multivariate analysis identified only 2 independent risk factors: greater VDT usage, and the female gender. During the lockdown, people mostly stayed indoors and spent more time using digital devices5,6. Home confinement and limited access to public spaces led to a markedly diminished engagement in physical activities. In a recent paper, Saldanha et al.37 reported that the daily screen time during the pandemic doubled. The participants in that investigation also suffered with dry-eye symptoms, which eventually led to a reduction in their work efficiency37. The findings were consistent with that of a European survey, which reported that increased screen time was significantly associated with worsening dry-eye symptoms in DED respondents38. Although previous research predominantly focused on overall VDT exposure during the lockdown, our results revealed details about the purposes of the daily VDT usage. This study confirmed that the overall VDT exposure was greater during the lockdown. The prolonging of the VDT usage was chiefly attributed by our respondents to their work or study needs. Surprisingly, the number of people who binge-watched TV series, video logs, and movies was 3 times higher than normal. This might be a consequence of their limited access to other entertainment activities and public areas. Moreover, the rise in VDT usage was greatly associated with a deterioration in dry-eye symptoms. This finding is consistent with work by Uchino et al.10, which suggested that prolonged VDT usage shortened the tear break-up time and significantly increased the risk of DED. Other studies hypothesized that longer blinking intervals that were experienced while focusing on VDTs contributed to an acceleration of tear evaporation and eventually led to DED10,39,40.
Female gender is a well-known risk factor for DED. Women are disproportionately susceptible to DED, and they tend to experience more severe symptoms than men21–23. Sex hormones have an abundant impact on tear and lipid production as well as the immune system, which plays a major role in DED41. DED in females is related to their low androgen and high estrogen levels, relative to males. Therefore, as women are predisposed to having more severe dry-eye symptoms, exposure to aggravating conditions might produce worse symptoms in women than in men.
Social distancing and avoiding mass gatherings limited physical interactions between family members, friends, and colleagues. Moreover, restrictions on access to public areas like gymnasiums, fitness centers, and parks decreased the level of physical activity by the overall population. The distress caused by the COVID-19 pandemic, isolation measures, and sedentary lifestyles, contributed to an excess of mental health problems3,6,11. Our study found that 25.7% of the participants had developed mental health abnormalities. The prevalence was similar to those of other studies, which reported values ranging from 11 to 43.7%11,12,42. Furthermore, the current investigation revealed that having mental health problems correlated with having more severe dry-eye symptoms (a DESS of less than 75) during the lockdown. According to a recent European survey report, increased mental stress and poor sleep quality were listed in the top three most common causes of worsening DED symptoms during the lockdown38. This result was consistent with studies which had found an association between psychiatric problems and DED15–20. The reason is that the perception of dry-eye symptoms was influenced by several psychological traits, such as anxiety and depression43,44.
The study’s strength is that it provided a large-scale, community-based survey which assessed not only patients seeking medical care but also members of the general population. Moreover, the research assessed a broad range of potential risk factors for dry-eye symptoms that might be affected by the lockdown. Only a few reports revealed that the impact of a lockdown aggravated DED symptoms through excessive VDT use37,45.
One of the limitations of this study is that it relied on self-reported online survey, distributing the questionnaire via social media may result in sampling bias. The survey's accessibility was influenced by factors such as the use of screen-based devices and social media accounts. Another disadvantage was the lack of an objective assessment tool to determine the average daily VDT usage. As well, weekday and weekend usage might vary greatly in terms of purpose and time. This limitation should be considered during the conduct of a further study. Also, the symptoms of dry eye surveyed are nonspecific and can be attributable to other ocular surface diseases such as allergic conjunctivitis, exposure keratopathy, ocular rosacea, blepharitis and episcleritis. Finally, it might be challenging to use a question to ascertain whether there had been a previous ophthalmologic diagnosis of DED in order to assess the prevalence of the disease. This is because the criteria for the clinical diagnoses might have differed among the clinicians concerned. Unfortunately, objective evaluations of DED could not be employed for the present research due to the social distancing measures in force during the pandemic.
The lockdown measures implemented to curb the spread of the COVID-19 pandemic abruptly altered the way of living and established a new normal. The social isolation measures restricted individuals’ ability to interact with one another. This resulted in an increased usage of VDTs and frequently excessive exposure to digital devices. These behavioral changes during the lockdown deteriorated dry-eye symptoms, and they possibly led to an increase in the DED incidence.
Acknowledgements
We acknowledge the support of our contributors from the Research Division of Siriraj Hospital, Mahidol University: Anupong Veeraburinon, for manuscript editing assistance; and Julaporn Pooliam for advice on the statistical analyses and interpretation.
Author contributions
N.N., C.C. and P.P. designed the study and collected data. N.N., P.N., and P.P. interpreted the results. N.N. wrote the manuscript with support from C.C., P.N. and P.P. All authors provided critical feedback and helped shape the research.
Funding
This research received no specific Grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data availability
All data generated or analyzed during this study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433. doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang C, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pietrobelli A, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: A longitudinal study. Obesity (Silver Spring, Md) 2020 doi: 10.1002/oby.22861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Majumdar P, Biswas A, Sahu S. COVID-19 pandemic and lockdown: Cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronobiol. Int. 2020;37:1191–1200. doi: 10.1080/07420528.2020.1786107. [DOI] [PubMed] [Google Scholar]
- 6.Meyer J, et al. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int. J. Environ. Res. Public health. 2020 doi: 10.3390/ijerph17186469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenfield M. Computer vision syndrome: A review of ocular causes and potential treatments. Ophthalm. Physiol. Opt. j. Brit. Coll. Ophthalm. Opt. (Optom.) 2011;31:502–515. doi: 10.1111/j.1475-1313.2011.00834.x. [DOI] [PubMed] [Google Scholar]
- 8.Courtin R, et al. Prevalence of dry eye disease in visual display terminal workers: A systematic review and meta-analysis. BMJ Open. 2016;6:e009675. doi: 10.1136/bmjopen-2015-009675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rossi GCM, Scudeller L, Bettio F, Pasinetti GM, Bianchi PE. Prevalence of dry eye in video display terminal users: A cross-sectional Caucasian study in Italy. Int. Ophthalmol. 2019;39:1315–1322. doi: 10.1007/s10792-018-0947-6. [DOI] [PubMed] [Google Scholar]
- 10.Uchino M, et al. Prevalence of dry eye disease and its risk factors in visual display terminal users: The Osaka study. Am. J. Ophthalmol. 2013;156:759–766. doi: 10.1016/j.ajo.2013.05.040. [DOI] [PubMed] [Google Scholar]
- 11.Zhou SJ, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry. 2020;29:749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ma Z, et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020;29:e181. doi: 10.1017/s2045796020000931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gao J, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15:e0231924. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ni MY, et al. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China. JMIR Public Health Surveill. 2020 doi: 10.2196/19009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hallak JA, Tibrewal S, Jain S. Depressive symptoms in patients with dry eye disease: A case–control study using the beck depression inventory. Cornea. 2015;34:1545–1550. doi: 10.1097/ico.0000000000000641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tiskaoglu NS, et al. Dry eye disease in patients with newly diagnosed depressive disorder. Curr. Eye Res. 2017;42:672–676. doi: 10.1080/02713683.2016.1236966. [DOI] [PubMed] [Google Scholar]
- 17.Szakáts I, Sebestyén M, Németh J, Birkás E, Purebl G. The role of health anxiety and depressive symptoms in dry eye disease. Curr. Eye Res. 2016;41:1044–1049. doi: 10.3109/02713683.2015.1088955. [DOI] [PubMed] [Google Scholar]
- 18.Li M, Gong L, Sun X, Chapin WJ. Anxiety and depression in patients with dry eye syndrome. Curr. Eye Res. 2011;36:1–7. doi: 10.3109/02713683.2010.519850. [DOI] [PubMed] [Google Scholar]
- 19.Wan KH, Chen LJ, Young AL. Depression and anxiety in dry eye disease: A systematic review and meta-analysis. Eye (Lond.) 2016;30:1558–1567. doi: 10.1038/eye.2016.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ayaki M, et al. Sleep and mood disorders in women with dry eye disease. Sci. Rep. 2016;6:35276–35276. doi: 10.1038/srep35276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chia EM, et al. Prevalence and associations of dry eye syndrome in an older population: The Blue Mountains Eye Study. Clin. Exp. Ophthalmol. 2003;31:229–232. doi: 10.1046/j.1442-9071.2003.00634.x. [DOI] [PubMed] [Google Scholar]
- 22.Shah S, Jani H. Prevalence and associated factors of dry eye: Our experience in patients above 40 years of age at a Tertiary Care Center. Oman J. Ophthalmol. 2015;8:151–156. doi: 10.4103/0974-620x.169910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ahn JM, et al. Prevalence of and risk factors associated with dry eye: The Korea National Health and Nutrition Examination Survey 2010–2011. Am. J. Ophthalmol. 2014;158:1205–1214.e1207. doi: 10.1016/j.ajo.2014.08.021. [DOI] [PubMed] [Google Scholar]
- 24.Farrand KF, Fridman M, Stillman IO, Schaumberg DA. Prevalence of diagnosed dry eye disease in the United States among adults aged 18 years and older. Am. J. Ophthalmol. 2017;182:90–98. doi: 10.1016/j.ajo.2017.06.033. [DOI] [PubMed] [Google Scholar]
- 25.Messmer EM. The pathophysiology, diagnosis, and treatment of dry eye disease. Deutsches Arzteblatt Int. 2015;112:71–81. doi: 10.3238/arztebl.2015.0071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Uchino M, et al. Dry eye disease and work productivity loss in visual display users: The Osaka study. Am. J. Ophthalmol. 2014;157:294–300. doi: 10.1016/j.ajo.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 27.Yamada M, Mizuno Y, Shigeyasu C. Impact of dry eye on work productivity. ClinicoEcon. Outcomes Res. 2012;4:307–312. doi: 10.2147/ceor.S36352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McDonald M, Patel DA, Keith MS, Snedecor SJ. Economic and humanistic burden of dry eye disease in Europe, North America, and Asia: A systematic literature review. Ocul. Surf. 2016;14:144–167. doi: 10.1016/j.jtos.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 29.Kojima T, et al. The impact of contact lens wear and visual display terminal work on ocular surface and tear functions in office workers. Am. J. Ophthalmol. 2011;152:933–940.e932. doi: 10.1016/j.ajo.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 30.Tansanguan S, Tananuvat N, Wongpakaran N, Wongpakaran T, Ausayakhun S. Thai version of the dry eye-related quality-of-life score questionnaire: Preliminary assessment for psychometric properties. BMC Ophthalmol. 2021;21:310. doi: 10.1186/s12886-021-02077-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cheng X, et al. Influence of prolonged visual display terminal use and exercise on physical and mental conditions of internet staff in Hangzhou, China. Int. J. Environ. Res. Public Health. 2019 doi: 10.3390/ijerph16101829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nilchaikovit T, Sukying C, Silpakit C. Reliability and validity of the Thai version of the General Health Questionnaire. J. Psychiatr. Assoc. Thailand. 1996;41:2–17. [Google Scholar]
- 33.Rouen PA, White ML. Dry eye disease: Prevalence, assessment, and management. Home Healthc. Now. 2018;36:25. doi: 10.1097/NHH.0000000000000652. [DOI] [PubMed] [Google Scholar]
- 34.Stapleton F, et al. TFOS DEWS II epidemiology report. Ocul. Surf. 2017;15:334–365. doi: 10.1016/j.jtos.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 35.Alex A, et al. Factors predicting the ocular surface response to desiccating environmental stress. Invest. Ophthalmol. Vis. Sci. 2013;54:3325–3332. doi: 10.1167/iovs.12-11322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Franck C. Eye symptoms and signs in buildings with indoor climate problems ('office eye syndrome') Acta Ophthalmol. 1986;64:306–311. doi: 10.1111/j.1755-3768.1986.tb06925.x. [DOI] [PubMed] [Google Scholar]
- 37.Saldanha IJ, Petris R, Makara M, Channa P, Akpek EK. Impact of the COVID-19 pandemic on eye strain and dry eye symptoms. Ocul. Surf. 2021 doi: 10.1016/j.jtos.2021.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barabino S. A narrative review of current understanding and classification of dry eye disease with new insights on the impact of dry eye during the COVID-19 Pandemic. Ophthalmol. Ther. 2021;10:495–507. doi: 10.1007/s40123-021-00373-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cardona G, Garcia C, Seres C, Vilaseca M, Gispets J. Blink rate, blink amplitude, and tear film integrity during dynamic visual display terminal tasks. Curr. Eye Res. 2011;36:190–197. doi: 10.3109/02713683.2010.544442. [DOI] [PubMed] [Google Scholar]
- 40.Himebaugh NL, Begley CG, Bradley A, Wilkinson JA. Blinking and tear break-up during four visual tasks. Optom. Vis. Sci. 2009;86:E106–114. doi: 10.1097/OPX.0b013e318194e962. [DOI] [PubMed] [Google Scholar]
- 41.Truong S, Cole N, Stapleton F, Golebiowski B. Sex hormones and the dry eye. Clin. Exp. Optom. 2014;97:324–336. doi: 10.1111/cxo.12147. [DOI] [PubMed] [Google Scholar]
- 42.Liang L, et al. The effect of COVID-19 on youth mental health. Psychiatr. Q. 2020;91:841–852. doi: 10.1007/s11126-020-09744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kawashima M, et al. Associations between subjective happiness and dry eye disease: A new perspective from the Osaka study. PLoS One. 2015;10:e0123299. doi: 10.1371/journal.pone.0123299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ichinohe S, Igarashi T, Nakajima D, Ono M, Takahashi H. Symptoms of dry eye disease and personality traits. PLoS One. 2016;11:e0166838. doi: 10.1371/journal.pone.0166838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Giannaccare G, Vaccaro S, Mancini A, Scorcia V. Dry eye in the COVID-19 era: How the measures for controlling pandemic might harm ocular surface. Graefe's Arch. Clin. Exp. Ophthalmol. 2020;258:2567–2568. doi: 10.1007/s00417-020-04808-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are available from the corresponding author on reasonable request.


