Abstract
Perceived insufficient milk supply (PIMS) is one of the major reasons for discontinued breastfeeding. We aimed to estimate the rates and evaluate related factors of PIMS. We searched four databases for relevant articles published from January 2000 to March 2021. We then performed a meta‐analysis of the pooled data to estimate the rates and related factors of PIMS using Stata 15.0. Descriptive analyses of textual data were performed to summarise the related factors of PIMS if data could not be synthesised quantitatively. The quality of included studies was assessed using Newcastle–Ottawa scale (NOS), AHRQ checklist or Consolidated Criteria for Reporting Qualitative Research (COREQ). Overall, 27 studies were included in this review. At different periods after delivery, approximately 50% of mothers reported PIMS as the reason for stopping breastfeeding, while for breastfeeding mothers, the incidence of PIMS ranged from 10% to 25%. Breastfeeding initiation (OR 4.22, 95%CI 1.57–11.34) and breastfeeding knowledge (OR 7.10, 95%CI 2.00–25.26) were two factors influencing PIMS. Besides, PIMS had a strong negative relationship with breastfeeding self‐efficacy (r = −0.57); moderate negative association with infant suck ability (r = −0.46) and planned breastfeeding duration (r = −0.45); and a moderate positive correlation with formula supplementation (r = 0.42). Descriptive analyses revealed that infant crying was reported to be a sign of PIMS, and inadequate intake of energy/liquids was a reported cause of it. This review identified a high proportion of women reporting PIMS, particularly among those who stopped breastfeeding. Deliberate interventions were needed to improve breastfeeding for mothers at risk.
Keywords: breastfeeding, perceived insufficient milk supply, review
Key messages.
Perceived insufficient milk supply (PIMS) is one of the major reasons for discontinued breastfeeding.
Among breastfeeding mothers, the greatest percentage reporting PIMS occurs in the earlier months. Among those who have abandoned breastfeeding, the report of PIMS as a reason for not breastfeeding remains high throughout the initial 6 month period.
The main factors contributing to PIMS are delayed breastfeeding initiation, limited knowledge on exclusive breastfeeding, and formula supplementation, whereas main barriers of PIMS are breastfeeding self‐efficacy, efficient sucking by infants and long breastfeeding duration plan.
To limit PIMS, women should be supported to initiate early breastfeeding, provided with education on exclusive breastfeeding, and advised to avoid formula supplementation during the first 6 months of breastfeeding.
1. INTRODUCTION
Exclusive breastfeeding during the first 6 months of infancy, provides infants with sufficient nutrients for healthy growth and development. Reports show that optimal breastfeeding between 0 to 23 months of age could save up to 820,000 child lives (Victora et al., 2016). Breastfeeding prevents malnutrition, obesity and diabetes, promotes healthy brain development and minimises chances of life‐threatening illnesses (Victora et al., 2016). WHO targets to increase the rate of exclusive breastfeeding during the first 6 months to at least 50% by 2025, up from the current 40% (WHO, 2020).
Currently, perceived insufficient milk supply (PIMS) is one of the main reasons given for formula supplementation and breastfeeding discontinuation (Gatti, 2008; Peacock‐Chambers et al., 2017; Rodrigo et al., 2018). PIMS is the mother's belief that the quality or quantity of her breast milk is insufficient to meet the infant's hunger or nutritional needs (Hill & Aldag, 1993; McCarter‐Spaulding & Kearney, 2001). Approximately 30% to 80% of mothers have cited PIMS as the prime reason for formula supplementation or early abandonment of breastfeeding (Gatti, 2008). Given its significance, studies have explored factors influencing PIMS. Women have reported persistent infant crying as a major symptom of PIMS (Sacco et al., 2006). Ineffective sucking also contributes to doubts over whether milk is enough for the infants (Galipeau et al., 2017). On the contrary, breastfeeding self‐efficacy and having sufficient access to information are the two main factors that prevent reports of PIMS (Galipeau et al., 2017; Nurhayati & Fikawati, 2019; Safon et al., 2017).
An earlier integrative review of PIMS concluded that PIMS was one of the most common reasons for the continuing low rates of breastfeeding duration and exclusivity throughout much of the world (Gatti, 2008). Our paper adds to the evidence base by providing a pooled analysis of data published in the last 20 years relating to the prevalence of and factors influencing PIMS.
2. METHODS
2.1. Search strategy
We searched though the Web of Science, the CINAHL, Embase and PubMed databases for relevant articles on PIMS published between January 2000 and March 2021. The key search terms used were ‘perceived OR perception OR self‐reported’ AND ‘insufficient OR low OR inadequate OR enough’ AND ‘milk’. Medical Subject Headings (MeSH) terms of PIMS and insufficient milk supply (IMS) were also searched. Reference lists of the retrieved articles were also searched manually.
2.2. Selection criteria
To be included in this review, studies had to meet the following criteria: (1) exploring the rate and/or related factors of PIMS; (2) PIMS referred to the mother's belief that the quality or quantity of her breast milk was insufficient to meet the infant's hunger or nutritional needs. Studies on (1) mothers with underlying conditions such as endocrine disorders, neurological disorders, psychological disorders, hypoplasia of mammary gland, breast surgery or Sheehan's syndrome, etc, that influenced milk production; (2) mothers with multiple deliveries; (3) infants with birth defects or severe diseases such as congenital anomaly, cleft palate, cleft lip, or neurological disorders, etc., that affected breastfeeding and (4) infants with prior‐hospitalisation in Neonatal Intensive Care Unit (NICU) were all excluded. Search, extraction and selection of relevant studies were performed independently by two authors. Disagreements were arbitrated by a third researcher.
2.3. Data extraction and quality assessment
For quantitative studies, we recorded the rates, adjusted odds ratios and correlation coefficients of analysed variables, whereas for qualitative studies, we captured the main themes or factors related to PIMS. For all studies, information on study characteristics (author, country, year of publication, sample size, study design, sample characteristic, findings and quality of research) were recorded. Missing data was requested from the corresponding author. If no response was received within 15 days of request, the respective article was excluded from the review. The Newcastle‐Ottawa scale (NOS) was used for quality assessment of cohort studies, whereas the AHRQ checklist was used for cross‐sectional studies. Consolidated Criteria for Reporting Qualitative Research (COREQ) was used for qualitative studies. To facilitate comparison, we converted AHRQ scores to NOS scores (Nila et al., 2020). The final quality assessment of the quantitative study will be displayed as the NOS score. Quality assessment was also performed independently by two authors, with disagreements resolved through discussion.
2.4. Data analysis
All literature was systematically reviewed to provide a comprehensive summary of the evidence on the rates of and factors influencing PIMS. There were two types of report of PIMS. One was when the mother directly reported PIMS (yes/no) and its association with predictors was reported in the form of Odds Ratios. The other used questionnaires with a continuous score to assess PIMS and measured coefficient correlations. If predictors of PIMS were the same across studies, we then combined them for meta‐analysis. Meta‐analyses were performed using Stata 15.0. Standard error was calculated for each original study using the binomial distribution. As for the studies reporting correlation coefficients, Fisher's r‐to‐z transformation was used to obtain variance‐stabilised correlation coefficients which were calculated in meta‐analysis (Schmidt & Hunter, 2015). Then pooled correlation coefficients were transformed back to the raw scale (r). The strength of association was either weak (r ≦ 0.29), moderate (r = 0.30 to 0.49) or strong (r > 0.49) (Cohen, 1988). For the studies that only reported mean and standard deviation, we converted them into correlation coefficients and then included them in the meta‐analysis for calculation (Lipsey & Wilson, 2000). The heterogeneity among studies was evaluated using Chi‐square tests based on Q test and I 2 statistics (Rücker et al., 2008). Pooled data for heterogenetic studies were analysed using the random effect model. Publication bias was assessed using the Egger's and Begg's tests (Borenstein et al., 2010). Non quantitative findings were presented descriptively as previously described (Thomas & Harden, 2008). The reporting of this meta‐analysis was in line with the PRISMA guidelines (Moher et al., 2015).
3. RESULTS
3.1. Search outcomes
Our search in the four databases generated 3533 reports on PIMS, with 4 additional articles obtained from manual search of references and websites (Figure 1). After removing 2199 duplicates and reading through titles and abstracts of the remaining 1338 studies, we retained 267 full‐text articles for detailed eligibility assessment. In the end, 27 articles, 4 qualitative and 23 quantitative studies met the inclusion criteria.
Figure 1.

Flow diagram for the selection of the included studies
3.2. Study characteristics
The 27 studies incorporated 6331 mothers for PIMS rates and 2739 mothers for factors influencing PIMS. Of the studies, five were performed in USA, five in China, three in Indonesia, two each in Australia, Tanzania and Mexico, and one each in Nicaragua, Turkey, Canada, Brazil, Japan, Singapore, Italy and Pakistan. Seven studies used questionnaires to measure PIMS. Detailed characteristics of the included studies were shown in Tables 1 and 2.
Table 1.
General characteristics of the 16 studies on the rates of perceived insufficient milk supply (PIMS)
| No | Author (year) country | Study design (quality score) | Participants characteristics (n) | PIMS rates (n/N) |
|---|---|---|---|---|
| 1 |
Mohebati et al. (2021) Mexico |
Longitudinal study (11) | ①first‐time mothers with singleton, healthy and full‐term infants who planned to breastfeed their child were assessed at 1, 2 and 4 weeks (n = 475) | 23.3% (65/278) a ; 14.9% (45/303) b ; 23.6% (64/271) b |
| 2 |
Wang et al. (2020) China |
Cross‐sectional study (10) | ①mothers were assessed at 3 to 5 days after birth (n = 450) | 41.1% (185/450) a |
| 3 |
De Roza et al. (2019) Singapore |
Longitudinal study (10) | ①mothers were assessed with infants aged 2 days to 2 months and followed up to 6 months (n = 400) | 37.3% (149/399) b |
| 4 |
Colombo et al. (2018) Italy |
Longitudinal study (9) | ①mothers were assessed at 48 h after delivery and follow up at 15, 40, and 90 days (n = 746) | 2.7% (20/746) a ; 4.7% (34/719) b ; 6% (43/711) b ; 7.1% (48/676) c ; 6.7% (43/640) c |
| 5 |
Galipeau et al. (2017) Canada |
Longitudinal study (9) | ①mothers were assessed if they were primiparas and had term birth (n = 98) | 18.0%(16/89) a ; 7.5%(4/53) b |
| 6 |
Sun et al. (2017) China |
Cohort study (4) | ②mothers were assessed at 2 to 3 days after birth and followed up at 1 month, 4 months, and 6 months (n = 180) | 38.5% (10/25) b ; 56.7% (53/94) c ; 52.4% (32/61) d |
| 7 |
Lal et al. (2017) Pakistan |
Cross‐sectional study (5) | ③mothers were assessed if their infants under 6 months of age (n = 176) | 60.2% (106/176) d |
| 8 |
Murase et al. (2016) USA |
Cohort study (7) | ①mothers were assessed at 7 days after delivery (n = 196) | 18.4% (36/196) a |
| 9 |
Magarey et al. (2016) Australia |
Longitudinal study (10) | ②mothers were assessed before 1 month, 1 to <2 months, 2 to <4 months and 4 to <6 months (n = 1470) | 52.0 (51/98) b ; 55.0 (33/60) c ; 55.7 (34/61) c ; 50.0 (32/64) d |
| 10 |
Prabasiwi et al. (2015) Indonesia |
Cross‐sectional study (10) | ③mothers were assessed with infants aged less than 6 months (n = 88) | 51% (45/88) b |
| 11 |
Wagner et al. (2013) USA |
Cohort study (8) | ①mothers who indicated prenatally intent to provide breast milk as the sole source of milk >2 months were assessed at 0, 3, 7, 14, 30 days postpartum (n = 353) | 28.3% (100/353) a ; 41.6% (146/351) a ; 26.9% (92/342) a ; 19.3% (65/336) b ; 19.5% (64/328) b ; |
| 12 |
Monteiro et al. (2011) Brazil |
Cross‐sectional study (8) | ①mothers were assessed with infants at 0–4 months of age (n = 231) | 29.0% (67/231) c |
| 13 |
Otsuka et al. (2008) Japan |
Cross‐sectional study (10) | ③mothers were assessed at 4 weeks postpartum (n = 108) | 73.1% (79/108) b |
| 14 |
McCann et al. (2007) USA |
Longitudinal study (7) | ①mothers were assessed at each month in 12 months after birth (n = 874) | 17.2% (34/198) b ; 15.3% (25/163) c ; 10.5% (15/143) d |
| 15 |
Lewallen et al. (2006) USA |
Cross‐sectional study (6) | ②mothers were assessed at 8 weeks after delivery (n = 121) | 34.7% (42/121) c |
| 16 |
Cooke et al. (2003) Australia |
Longitudinal study (10) | ①mothers were assessed at 2 weeks, 6 weeks and 3 months after delivery (n = 365) | 14.1% (40/284) b ; 17.2% (46/268) c ; 11.7% (30/255) c |
Note: ①: The rates of PIMS were assessed among EBF/PBF mothers; ②: The rates of PIMS were assessed among NBF mothers; ③: The rates of PIMS were assessed among NEBF mothers. EBF: exclusive breastfeeding; PBF: partial breastfeeding; NEBF: non‐exclusive breastfeeding; NBF: non‐breastfeeding. Evaluation time of perceived insufficient milk supply:
Less than 1 week.
One week to 1 month.
1 month to 4 months.
Four to 6 months.
Table 2.
General characteristics of the 16 studies on the factors related to perceived insufficient milk supply (PIMS)
| No | Author Year Country | Study design (quality score) PIMS assessment | Participants (n) | Factors related to PIMS |
|---|---|---|---|---|
| 1 |
Mohebati et al., 2021 Mexico |
Longitudinal study (11) Self‐designed |
①first‐time mothers with singleton, healthy and full‐term infants who planned to breastfeed their child were assessed at 1, 2 and 4 weeks (n = 475) | Crying expectations (OR 2.07 95%CI 1.37, 3.12); lactation problem (OR 1.85 95%CI 1.22, 2.79); delayed onset of lactation (2.49 95%CI 1.05, 5.91) |
| 2 |
Sandhi et al., 2020 Indonesia |
Cross‐sectional study (9) a H&H lactation scale |
①mothers were included with infants under 6 months of age (n = 237) | Skin‐to‐skin contact (β = 3.2, SE = 1.31, p = 0.02); BF self‐efficacy (β = 10.78, SE = 1.81, p = < 0.0001); EBF (OR 3.58 95%CI 2.05, 6.25) |
| 3 |
Nurhayati & Fikawati, 2019 Indonesia |
Cross‐sectional study (8) Self‐designed |
②mothers were included with infants aged 0–6 months who failed in giving EBF with a maximum time of 2 weeks at the time of the study (n = 71) | EBF counselling during antenatal care (AOR 19.746 95%CI 1.926, 202.456); BF initiation (AOR 7.803 95%CI 1.266, 48.107) |
| 4 |
Cooper et al., 2019 Tanzania |
Qualitative (25) | ②mothers were included with infants up to 1 year of age (n = 24) | Infants' crying; maternal traditional beliefs about food intake and breast milk production during BF; the breast ‘feeling empty’; the inability ‘to squeeze out much milk from the breast’; ‘light milk’ |
| 5 |
Mgongo et al., 2018 Tanzania |
Qualitative (23) | ①mothers were included with infants aged 0–12 months who were still BF (n = 78) | Infants' crying; poor energy intake |
| 6 |
Safon et al., 2017 Nicaragua |
Qualitative (23) | ②mothers were included with infants aged 2 years or younger (N = 21) | Maternal anxiety about infants' and own nutrition status; BF negative advice and role modelling; perceived infant feeding norms about the provision of breast milk substitutes |
| 7 |
Gokceoglu & Kucukoglu, 2017 Turkey |
Descriptive study (8) a PIM questionnaire |
③mothers were included who produce at least 30 cc breast milk and exclusively breastfeed their infants (n = 200) | Delivery method (p = 0.032); number of children (p = 0.000); education (p = 0.043); income (p = 0.000); age (p = 0.006); previous BF experience (p = 0.000); BF training (p = 0.000); planned pregnancy (p = 0.024); BF plan (p = 0.000); Infant's gender (p = 0.001); BF self‐efficacy (r = 0.741, p = 0.000) |
| 8 |
Galipeau et al., 2017 Canada |
Longitudinal study (9) a PIM questionnaire |
①Primiparas were included with term birth (n = 98) | Infants' negative temperament during feeds (r = −0.45, p < 0.01); EBF (t = 2.87, p = 0.005); Infants' capacity to suckle (r = 0.538, p < 0.01), BF self‐efficacy (r 1 = 0.38, p < 0.01; r 2 = 0.725, p < 0.01); infant BF demand (number of breastfeeds per 24 h) (r = 0.499, p < 0.01) |
| 9 |
Prabasiwi et al., 2015 Indonesia |
Cross‐sectional study (10) Self‐designed |
②mothers were included with infants aged less than 6 months and ceasing EBF (n = 88) | Energy intake (AOR 3.770 95%CI 1.241, 11.448); BF knowledge (AOR 12.415 95%CI 2.832, 54.430); BF initiation (AOR 3.268 95%CI 1.008, 10.596) |
| 10 |
Lou et al., 2014 China |
Cross‐sectional study (8) Self‐designed |
④mothers were included with term infants aged between 1 and 6 months (n = 341) | Infant cried a lot and/or willing to take formula after nursing; maternal poor appetite; the absence of feeling milk; intermittent BF; inadequate intake of liquids |
| 11 |
Monteiro et al., 2011 Brazil |
Cross‐sectional study (8) Self‐designed |
①mothers were included with infants at 0–4 months of age (n = 231) | Mothers' negative perception on infants' satiety after BF (AOR 32.70 95%CI 14.73, 72.59) |
| 12 |
Lin et al., 2011 China |
Descriptive study (10) a H&H lactation scale |
①mothers who underwent caesarean section were included with infants being breastfed (n = 141) | Delayed timing of BF initiation (adjusted R 2 = 0.109, t = −1.98); formula supplementation (adjusted R 2 = 0.231, t = −3.72); multiparous (adjusted R 2 = 0.051, t = 2.19) |
| 13 |
Huang et al., 2009 China |
Cross‐sectional study (10) a H&H lactation scale |
①mothers who underwent vaginal delivery were included (n = 205) | Formula supplementation (adjusted R 2 = 0.187, t = −5.78); family support (adjusted R 2 = 0.334, t = −2.65); positive infant sucking behaviour (adjusted R 2 = 0.266, t = 3.85); planned duration of BF (adjusted R 2 = 0.312, t = 3.40); effective infant sucking pattern (adjusted R 2 = 0.353, t = 2.48) |
| 14 |
Otsuka et al., 2008 Japan |
Cross‐sectional study (10) a PIM questionnaire |
②mothers were included with term infants (n = 262) | Higher education (p = 0.04); formula supplementation (p = 0.001); BF self‐efficacy (adjusted R 2 = 0.260, p < 0.01). |
| 15 |
Sacco et al., 2006 Mexico |
Qualitative (23) | ①Primiparas were included if they were primary caregivers of infant younger than 6 months or women in last trimester who intended to breastfeed (n = 207) | Infants' crying; infants' dissatisfaction; no/little milk comes out; empty, sagging breasts; maternal poor diet and inadequate liquids |
| 16 |
McCarter‐Spaulding & Kearney, 2001 USA |
Cross‐sectional study (9) a PIM questionnaire |
①mothers were included with infants aged 1 to 11 weeks who were still breastfed (n = 60) | BF self‐efficacy (adjusted R 2 = 0.250, p < 0.01); the number of wet and dirty diapers (48%), infant weight gain (32%), signs of contentedness (32%), breast milk leaking (17%) |
Note: ①: The factors related to PIMS were assessed among EBF/PBF mothers; ②: The factors related to PIMS were assessed among NEBF mothers; ③: The factors related to PIMS were assessed among EBF mothers; ④: The factors related to PIMS were assessed among NBF mothers. BF: breastfeeding; EBF: exclusive breastfeeding; PBF: partial breastfeeding; NEBF: non‐exclusive breastfeeding; NBF: non‐breastfeeding.
The questionnaire is used to assess the perception of breast milk. The higher the score, the more sufficient the perceived breast milk is.
The quality of the 23 quantitative studies ranged from poor to good, with the majority of the studies meeting 5 to 11 out of 11 items in the AHRQ checklist (mean = 8.85 ± 1.49). Few studies met four to eight out of nine items of the NOS (mean = 6.33 ± 1.70). Lack of processing, categorisation or description to non‐respondents were the most common sources of limited quality. Four qualitative studies of moderate quality meet 23 to 25 out of the 32 items in COREQ. Most studies did not provide detailed information on the researchers and did not provide interview feedback to participants for comments or corrections.
3.3. Rates of perceived insufficient milk supply
The pooled PIMS rates reported in 16 studies are shown in Figure 2. PIMS rates were divided into three groups (EBF/PBF: exclusive or partial breastfeeding; NEBF: non‐exclusive breastfeeding; NBF: non‐breastfeeding) based on four time periods (a. less than 1 week; b. 1 week to 1 month; c. 1 to 4 months; d. 4 to 6 months). EBF/PBF group includes mothers who exclusively or partially breastfeed. NEBF group includes mothers who partially or not breastfeed. NBF group includes mothers who not breastfeed. PIMS rate was 25% at less than 1 week postpartum and then dropped to 15% at 4 to 6 months in EBF/PBF group; it reached 62% at 1 week to 2 month in NEBF group; it was around 50% from 1 week to 6 months in NBF group.
Figure 2.
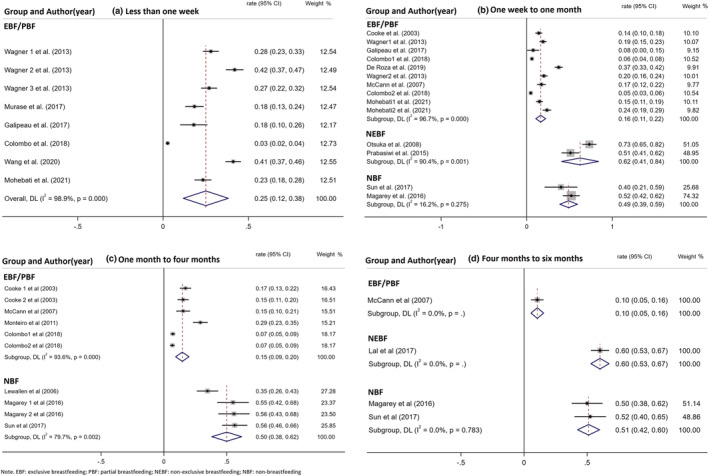
The rates of perceived insufficient milk supply (PIMS)
Egger's and Begg's tests revealed significant publication bias for studies reporting PIMS rates (Begg's tests: Pr > |z| = 0.001; Egger's tests: P > |t| = 0.000). Sensitivity analysis did not reveal the main sources of heterogeneity among studies reporting on PIMS rates. Meta‐regression analysis was not utilised in dealing with heterogeneity because of the small number of relevant studies.
3.4. Factors influencing perceived insufficient milk supply
The factors related to PIMS reported in 16 studies are shown in Table 2. Nineteen facilitators categorised into nine domains and 16 barriers categorised into eight domains are presented in Table 3. According to breastfeeding status, PIMS rates were divided into two groups (EBF&EBF/PBF, and NEBF&NBF). Comparing the factors between these two groups, effective infant sucking can make mothers in EBF&EBF/PBF group more confident that they have sufficient breast milk supply, while mothers who have already abandoned EBF or PBF (NEBF&NBF group) often use PIMS to justify not breastfeeding exclusively or at all. From the common ground between two groups, mothers regard infant crying as a sign of PIMS; inadequate intake of energy/liquids as a cause of it; and breastfeeding self‐efficacy as a barrier of it.
Table 3.
Summary of barriers and facilitators of perceived insufficient Milk supply (PIMS)
| Groups (n) | Barriers | Facilitators |
|---|---|---|
| EBF&EBF/PBF (10) |
Social‐demographic factors: ≥36; high education; high income; male infants; BF experience; multiparous Medical‐health factors: Vaginal delivery; planned pregnancy; planned long BF time Maternal Psychologic factors: BF self‐efficacy Breastfeeding information: Training Infants' behaviour: Skin‐to‐skin contact; effective infant sucking; signs of contentedness Breastfeeding behaviour: EBF; feeding infant on demand Infants' physiologic factors: The number of wet and dirty diapers; infant weight gain Breast milk factors: Breast milk leaking |
Medical‐health factors: Lactation problem Maternal Psychologic factors: Mothers' negative perception on infants' satiety Maternal nutrition status: Maternal poor diet and inadequate liquids Infants' behaviour: Infants' crying Breastfeeding behaviour: Delayed BF initiation; formula supplementation Breast appearance: Empty, sagging breasts Breast milk factors: No/little milk comes out |
| NEBF&NBF (6) |
Social‐demographic factors: High education Maternal Psychologic factors: BF self‐efficacy |
Maternal Psychologic factors: Maternal anxiety about infants' and own nutrition status Maternal nutrition status: Maternal poor diet and inadequate liquids Sociocultural factors: Maternal traditional beliefs about food intake and breast milk production during BF; negative BF environment Infants' behaviour: Infants' crying Breastfeeding behaviour: Delayed BF initiation; intermittent BF Breast milk factors: The absence of feeling milk Breast appearance: The breast ‘feeling empty’ Breastfeeding information: Less BF knowledge |
Note: BF: breastfeeding; EBF: exclusive breastfeeding; PBF: partial breastfeeding; NEBF: non‐exclusive breastfeeding; NBF: non‐breastfeeding.
We found delayed initiation of breastfeeding and lack of exclusive breastfeeding knowledge increased the likelihood of PIMS by 4.22 and 7.10 folds among mothers not exclusively breastfeeding (Figure 3). As for the correlation results among mothers in EBF&EBF/PBF group (Figure 4), PIMS had a strong negative association with breastfeeding self‐efficacy (r = −0.57 95%CI −0.72, −0.38), moderate negative association with planned duration of breastfeeding (r = −0.45 95%CI −0.65, −0.19) and infant suck ability (r = −0.46 95%CI −0.64, −0.22), and a weak negative association with parity (r = −0.24 95%CI −0.38, −0.09). Contrarily, there was a moderate positive correlation between formula supplementation and PIMS (r = 0.42 95%CI 0.32, 0.51). Because of the small number of included studies, publication bias and meta‐regression analyses were not performed. Sensitivity analysis did not reveal the main sources of heterogeneity in included studies.
Figure 3.

Factors influencing perceived insufficient milk supply (PIMS) based on odds ratio
Figure 4.

The correlation between various factors and perceived insufficient milk supply (PIMS)
4. DISCUSSION
PIMS was reported by significant proportions of women while breastfeeding and even higher proportions after the abandonment of breastfeeding before 6 months. Even though the small number of studies available limited the conclusions we were able to draw from this review, we found that women feeding their infants formula in addition to breastmilk were more likely to report PIMS. These results were similar to our other result that formula supplementation had a positive association with PIMS. One review also confirmed that PIMS lead to decreased exclusivity or early weaning (Gatti, 2008). The first week after delivery was a critical time, during which 25% of breastfeeding mothers reported PIMS. If mothers continued breastfeeding, PIMS rates would decrease (McCann et al., 2007). Within 48 h after delivery, only a small amount of breast milk is produced, mainly colostrum (McGuire, 2018), which leads mothers to believe that they cannot produce enough milk (Safon et al., 2017). Around 3–4 days postpartum, milk supply becomes more abundant (Kent et al., 2012; Neville & Morton, 2001). If the stimulation to breasts persists, breast milk will peak in response to infant sucking within a month of delivery; but if mothers add formula supplementation due to PIMS and gradually cease breastfeeding, prolactin will return to pre‐pregnant levels and milk production will stop (Dahl, 2015; McGuire, 2018).
The factors affecting PIMS are multifaceted, with different but potentially related to psychological, social or biological characteristics. One main factor is breastfeeding self‐efficacy. Mothers with high breastfeeding self‐efficacy will believe that they can produce enough breast milk to satisfy their babies; however, mothers who doubt their breastfeeding ability do not think that they can breastfeed their babies without a supplement (De Roza et al., 2019; Gokceoglu & Kucukoglu, 2017). Mothers' concerns about breast milk supply occur before breastfeeding and exist in entire breastfeeding period (Peacock‐Chambers et al., 2017). Even if health providers confirm sufficient milk supply through the use of 24‐h test‐weights, mothers are still anxious once it is no longer objectively measured (Hill et al., 2007).
Some influencing factors can affect each other and act on PIMS. Early breastfeeding initiation has positive association with exclusive breastfeeding knowledge and higher education level (Vieira et al., 2010). Primiparous mothers were more likely to report delayed breastfeeding initiation, limited breastfeeding knowledge, lower breastfeeding self‐efficacy or unrealistic expectations of breastfeeding (DaMota et al., 2012; Dewey et al., 2003; Sunita et al., 2016). Having a long‐term breastfeeding plan is positively associated with breastfeeding self‐efficacy (Gokceoglu & Kucukoglu, 2017). Maternal nutrition is considered by breastfeeding mothers as an important factor affecting the amount of breast milk (Cooper et al., 2019; Safon et al., 2017). A study has reported that malnourished mothers also can produce enough milk to breastfeed successfully (Minato et al., 2019). If a mother is under‐nourished, it is safer to improve mother's nutrition than to provide formula supplementation (Academy for Educational Development, 2000). There is also no need for mothers to consume excessive amounts of liquids, as a study has shown that doing so does not increase breastmilk production per se (Ndikom et al., 2014).
For most mothers, the perception that her milk is insufficient often stems from infant behaviours, such as crying and sucking. An infant who sucks effectively will show a sense of satiety, but an infant who shows signs of sucking ineffectively may cry or be irritable (Newman & Pitman, 2015). But not all crying means hunger—it is also the main signal to express various unmet needs (e.g., physical discomfort, insecurity and tiredness) (Mohebati et al., 2021; Prabasiwi et al., 2015). Every infant has different personality and feeding habit. Many infants are unsettled in early months, but this behaviour (‘cry‐fuss’) is usually transient (Wake et al., 2006). Mothers who expect their infant to cry more were also found to be more likely to report PIMS at 2 and 4 weeks (Mohebati et al., 2021). Mothers have also been found to perceive that breastfed infants will cry more than formula fed infants (Brown et al., 2011). In order to restore the sense of control, they may introduce formula supplementation when infants cry (Peacock‐Chambers et al., 2017).
A report found that only 5% of mothers experienced actual milk insufficiency due to pathological abnormalities (Neifert, 2001), suggesting that the remaining mothers have the physiological ability to produce enough breastmilk. Some influencing factors were shown to affect the secretion of actual milk production, such as caesarean section, delayed breastfeeding initiation, formula supplementation, and infants' ineffective sucking (Amir, 2006; Geddes, 2007; Hill et al., 2007; Hobbs et al., 2016; Huang et al., 2009; Kent et al., 2012, 2016; Neville & Morton, 2001; Newman & Pitman, 2015). If mothers fail to achieve adequate breastfeeding frequency, duration, or necessary degree of breast emptying, especially the first month after delivery, actual milk insufficiency might occur (Dahl, 2015).
Addressing PIMS is necessary to enhance breastfeeding rates. Importantly, mothers should be confident that they can produce enough milk to meet the needs of their babies even in the first few days after delivery (McGuire, 2018). In order to reinforce mothers' breastfeeding self‐efficacy, it is necessary to provide mothers and their family members with breastfeeding knowledge in the prenatal period, including breastfeeding techniques, breastfeeding benefits, normal patterns of infant breastfeeding behaviour, physiology of breast milk production, resolution of breastfeeding problems, etc., (Demirci et al., 2020; Lauwers & Swisher, 2010; Rodrigo et al., 2018; Safon et al., 2017). If a mother is concerned that her baby is not getting sufficient breast milk, health professionals can use more reliable parameters to evaluate her baby, such as the number of wet diapers and stools (American Academy of Pediatrics, 2005), infant alertness, skin colour, muscle tone, and consistent weight gain and growth (Amir, 2006; Neifert, 2004; Shrago et al., 2006). To achieve optimal breastfeeding, it is recommended that mothers increase their physical contact with their babies, which can help them be more attentive to the frequency with which their infant wishes to be fed (Little et al., 2018). In addition, mothers need to learn how to observe and respond to feeding cues, such as rooting, increasing alertness, wiggling, sucking on a fist or finger, and moving the mouth or tongue (Cadwell et al., 2006).
No matter the source of the mother's concern for her milk supply, timely assessment is the key to finding successful solutions. Hence, greater focus should be put on breastfeeding mothers at risk, especially in the first week, and offer lactation support to keep adequate stimulation on the breasts, which can prevent the use of formula supplementation and limit PIMS to a perception rather than a self‐fulfilling prophecy (Kent et al., 2021). Notably, PIMS may also be used as a justification for early supplementation with formula or abandonment of breastfeeding for a mother who feels pressure to breastfeed but simply does not wish to or is finding it too tiresome or difficult (Huang et al., 2009). Therefore, reports of PIMS call for extensive and deep investigation to fully unravel and solve possible underlying causes.
4.1. Limitations
Regarding limitations, firstly, although PIMS rates were analysed along stratified groups and time periods, the significant heterogeneity in the included studies weakens the strength of the findings. Heterogeneity based on I2 should be interpreted with caution when a meta‐analysis includes only a limited number of events (Thorlund et al., 2012). Herein, publication bias may result from exclusion of studies that included ineligible populations. Secondly, some studies included both exclusive and partial breastfeeding, and some studies reported non‐exclusive breastfeeding. We cannot get the separate PIMS rates and influencing factors of exclusive breastfeeding, partial breastfeeding and non‐breastfeeding, which might obscure important findings. Future studies need to take this into consideration and report PIMS rates and influencing factors among mothers with the same breastfeeding status. Thirdly, because PIMS comes from mother's subjective feelings, the assessments are based on mother's self‐report rather than objective measurements. To explore the influencing factors, four studies use PIM questionnaire, three studies use H&H questionnaire, and the other nine studies use self‐designed questions to assess PIMS, which limited comparability across studies. Fourthly, some factors were not analysed due to the small number of relevant studies.
5. CONCLUSIONS
PIMS is a major reason given by mothers for formula supplementation or the abandonment of breastfeeding. Those at greater risk for reporting PIMS should receive additional accompaniment and support prior to and especially in the first weeks of breastfeeding. Interventions to mitigate PIMS include early breastfeeding initiation, breastfeeding knowledge education, breastfeeding self‐efficacy improvement, breastfeeding behaviour guidance. Overall, findings of this research provide the foundation for improving breastfeeding practices.
CONFLICTS OF INTEREST
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
CONTRIBUTIONS
YH: Study design; identified, screened and evaluated the study; analysed the data; wrote the first draft of the manuscript. YL: Study design, identified, screened and evaluated the study; manuscript revision. XYY: Study design; identified, screened and evaluated the study; manuscript revision. TYZ: Study design; identified, screened and evaluated the study; manuscript revision.
ACKNOWLEDGMENTS
The authors gratefully acknowledged the support by the National Natural Science Foundation of China (71974061) for writing guide. No paid writing assistance from commercial corporation has been received. The author gratefully acknowledged XY and TYZ for their recommendations to the development of this manuscript.
Huang, Y. , Liu, Y. , Yu, X.‐Y. , & Zeng, T.‐Y. (2021). The rates and factors of perceived insufficient milk supply: A systematic review. Maternal & Child Nutrition, 18:e13255. 10.1111/mcn.13255
DATA AVAILABILITY STATEMENT
Since this article is a systematic review, the data come from articles in academic journals that have been published in the public domain. Data sharing is not applicable to this article.
REFERENCES
- Academy for Educational Development . (2000). Frequently asked questions on: Breastfeeding and maternal nutrition. http://www.linkagesproject.org
- American Academy of Pediatrics . (2005). Breastfeeding and the use of human milk. Pediatrics, 115(2), 496–506. 10.1542/peds.2004-2491 [DOI] [PubMed] [Google Scholar]
- Amir, L. H. (2006). Breastfeeding‐‐managing ‘supply’ difficulties. Australian Family Physician, 35(9), 686–689. [PubMed] [Google Scholar]
- Borenstein, M. , Hedges, L. V. , Higgins, J. P. T. , & Rothstein, H. R. (2010). A basic introduction to fixed‐effect and random‐effects models for meta‐analysis. Research Synthesis Methods, 1(2), 97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- Brown, A. , Raynor, P. , & Lee, M. (2011). Maternal control of child‐feeding during breast and formula feeding in the first 6 months post‐partum. Journal of Human Nutrition and Dietetics, 24(2), 177–186. 10.1111/j.1365-277X.2010.01145.x [DOI] [PubMed] [Google Scholar]
- Cadwell, K. , Turner‐Maffei, C. , O'Conno, B. , & Blair, A. C. (2006). Maternal and infant assessment for breastfeeding and human lactation: A guide for the practitioner (2nd ed.). Sudbury MA: Jones and Bartlett Publishers. [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum. [Google Scholar]
- Colombo, L. , Crippa, B. L. , Consonni, D. , Bettinelli, M. E. , Agosti, V. , Mangino, G. , … Mosca, F. (2018). Breastfeeding Determinants in Healthy Term Newborns. Nutrients, 10(1). 10.3390/nu10010048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke, M. , Sheehan, A. , & Schmied, V. (2003). A description of the relationship between breastfeeding experiences, breastfeeding satisfaction, and weaning in the first 3 months after birth. Journal of Human Lactation, 19(2), 145–156. 10.1177/0890334403252472 [DOI] [PubMed] [Google Scholar]
- Cooper, C. M. , Kavle, J. A. , Nyoni, J. , Drake, M. , Lemwayi, R. , Mabuga, L. , & Pfitzer, A. (2019). Perspectives on maternal, infant, and young child nutrition and family planning: Considerations for rollout of integrated services in Mara and Kagera, Tanzania. Maternal and Child Nutrition, 15. 10.1111/mcn.12735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl, L. (2015). Milk supply and regulation. Springer International Publishing. 10.1007/978-3-319-18194-3_3 [DOI] [Google Scholar]
- DaMota, K. , Banuelos, J. , Goldbronn, J. , Vera‐Beccera, L. E. , & Heinig, M. J. (2012). Maternal request for in‐hospital supplementation of healthy breastfed infants among low‐income women. Journal of Human Lactation, 28(4), 476–482. 10.1177/0890334412445299 [DOI] [PubMed] [Google Scholar]
- De Roza, J. G. , Fong, M. K. , Ang, B. L. , Sadon, R. B. , Koh, E. Y. L. , & Teo, S. S. H. (2019). Exclusive breastfeeding, breastfeeding self‐efficacy and perception of milk supply among mothers in Singapore: A longitudinal study. Midwifery, 79, 102532. 10.1016/j.midw.2019.102532 [DOI] [PubMed] [Google Scholar]
- Demirci, J. R. , Suffoletto, B. , Doman, J. , Glasser, M. , Chang, J. C. , Sereika, S. M. , & Bogen, D. L. (2020). The development and evaluation of a text message program to prevent perceived insufficient milk among first‐time mothers: Retrospective analysis of a randomized controlled trial. JMIR mHealth and uHealth, 8(4), e17328. 10.2196/17328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewey, K. G. , Nommsen‐Rivers, L. A. , Heinig, M. J. , & Cohen, R. J. (2003). Risk factors for suboptimal infant breastfeeding behavior, delayed onset of lactation, and excess neonatal weight loss. Pediatrics, 112(3 Pt 1), 607–619. 10.1542/peds.112.3.607 [DOI] [PubMed] [Google Scholar]
- Galipeau, R. , Dumas, L. , & Lepage, M. (2017). Perception of not having enough milk and actual milk production of first‐time breastfeeding mothers: Is there a difference? Breastfeeding Medicine, 12, 210–217. 10.1089/bfm.2016.0183 [DOI] [PubMed] [Google Scholar]
- Gatti, L. (2008). Maternal perceptions of insufficient milk supply in breastfeeding. Journal of Nursing Scholarship, 40(4), 355–363. 10.1111/j.1547-5069.2008.00234.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geddes, D. T. (2007). Inside the lactating breast: The latest anatomy research. Journal of Midwifery and Womens Health, 52(6), 556–563. 10.1016/j.jmwh.2007.05.004 [DOI] [PubMed] [Google Scholar]
- Gokceoglu, E. , & Kucukoglu, S. (2017). The relationship between insufficient milk perception and breastfeeding self‐efficacy among Turkish mothers. Global Health Promotion, 24(4), 53–61. 10.1177/1757975916635080 [DOI] [PubMed] [Google Scholar]
- Hill, P. D. , & Aldag, J. C. (1993). Insufficient milk supply among black and white breast‐feeding mothers. Research in Nursing & Health, 16(3), 203–211. 10.1002/nur.4770160307 [DOI] [PubMed] [Google Scholar]
- Hill, P. D. , Aldag, J. C. , Zinaman, M. , & Chatterton, R. T. (2007). Predictors of preterm infant feeding methods and perceived insufficient milk supply at week 12 postpartum. Journal of Human Lactation, 23(1), 32–38quiz 39‐43. 10.1177/0890334406297277 [DOI] [PubMed] [Google Scholar]
- Hobbs, A. J. , Mannion, C. A. , Mcdonald, S. W. , Brockway, M. , & Tough, S. C. (2016). The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum. BMC Pregnancy & Childbirth, 16(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, Y. Y. , Lee, J. T. , Huang, C. M. , & Gau, M. L. (2009). Factors related to maternal perception of milk supply while in the hospital. The Journal of Nursing Research, 17(3), 179–188. 10.1097/JNR.0b013e3181b25558 [DOI] [PubMed] [Google Scholar]
- Kent, J. C. , Prime, D. K. , & Garbin, C. P. (2012). Principles for maintaining or increasing breast milk production. Journal of Obstetric Gynecologic & Neonatal Nursing, 41(1), 114–121. 10.1111/j.1552-6909.2011.01313.x [DOI] [PubMed] [Google Scholar]
- Kent, J. C. , Gardner, H. , & Geddes, D. T. (2016). Breastmilk production in the first 4 weeks after birth of term infants. Nutrients, 8(12). 10.3390/nu8120756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kent, J. C. , Ashton, E. , Hardwick, C. M. , Rea, A. , Murray, K. , & Geddes, D. T. (2021). Causes of perception of insufficient milk supply in Western Australian mothers. Maternal & Child Nutrition, 17(1), e13080. 10.1111/mcn.13080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lal, S. , Shaikh, A. B. , Dilijan, Z. A. M. , Lal, S. , & Jamro, S. (2017). Frequency of mothers who are not exclusively breast feeding and its factors in tertiary care hospital. Rawal Medical Journal, 42(1), 23–27. [Google Scholar]
- Lauwers, J. , & Swisher, A. (2010). Counseling the nursing mother: A lactation consultant's guide (5th ed.). Sudbury MA: Jones and Bartlett Publishers. [Google Scholar]
- Lewallen, L. P. , Dick, M. J. , Flowers, J. , Powell, W. , Zickefoose, K. T. , Wall, Y. G. , & Price, Z. M. (2006). Breastfeeding support and early cessation. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 35(2), 166–172. 10.1111/j.1552-6909.2006.00031.x [DOI] [PubMed] [Google Scholar]
- Lin, S. Y. , Lee, J. T. , Yang, C. C. , & Gau, M. L. (2011). Factors related to milk supply perception in women who underwent cesarean section. The Journal of Nursing Research, 19(2), 94–101. 10.1097/JNR.0b013e31821988e9 [DOI] [PubMed] [Google Scholar]
- Lipsey, M. W. , & Wilson, D. B. (2000). Practical meta‐analysis (applied social research methods) (1st ed.). SAGE publication. [Google Scholar]
- Little, E. E. , Legare, C. H. , & Carver, L. J. (2018). Mother‐infant physical contact predicts responsive feeding among U.S. breastfeeding mothers. Nutrients, 10(9). 10.3390/nu10091251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lou, Z. , Zeng, G. , Huang, L. , Wang, Y. , Zhou, L. , & Kavanagh, K. F. (2014). Maternal reported indicators and causes of insufficient milk supply. Journal of Human Lactation, 30(4), 466–473quiz 511‐462. 10.1177/0890334414542685 [DOI] [PubMed] [Google Scholar]
- Magarey, A. , Kavian, F. , Scott, J. A. , Markow, K. , & Daniels, L. (2016). Feeding mode of Australian infants in the first 12 months of life. Journal of Human Lactation, 32(4), 95–104. 10.1177/0890334415605835 [DOI] [PubMed] [Google Scholar]
- McCann, M. F. , Baydar, N. , & Williams, R. L. (2007). Breastfeeding attitudes and reported problems in a national sample of WIC participants. Journal of Human Lactation, 23(4), 314–324. 10.1177/0890334407307882 [DOI] [PubMed] [Google Scholar]
- McCarter‐Spaulding, D. E. , & Kearney, M. H. (2001). Parenting Self‐Efficacy and Perception of Insufficient Breast Milk. Journal of Obstetric, Gynecologic & Neonatal Nursing, 30(5), 515–522. 10.1111/j.1552-6909.2001.tb01571.x [DOI] [PubMed] [Google Scholar]
- McGuire, T. M. (2018). Drugs affecting milk supply during lactation. Australian Prescriber, 41(1), 7–9. 10.18773/austprescr.2018.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mgongo, M. , Hussein, T. H. , Stray‐Pedersen, B. , Vangen, S. , Msuya, S. E. , & Wandel, M. (2018). “We give water or porridge, but we don't really know what the child wants:” a qualitative study on women's perceptions and practises regarding exclusive breastfeeding in Kilimanjaro region, Tanzania. BMC Pregnancy and Childbirth, 18(1), 323. 10.1186/s12884-018-1962-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minato, T. , Nomura, K. , Asakura, H. , Aihara, A. , Hiraike, H. , Hino, Y. , Isojima, T. , & Kodama, H. (2019). Maternal undernutrition and breast milk macronutrient content are not associated with weight in breastfed infants at 1 and 3 months after delivery. International Journal of Environmental Research and Public Health, 16(18), 3315. 10.3390/ijerph16183315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohebati, L. M. , Hilpert, P. , Bath, S. , Rayman, M. P. , Raats, M. M. , Martinez, H. , & Caulfield, L. E. (2021). Perceived insufficient milk among primiparous, fully breastfeeding women: Is infant crying important? Maternal & Child Nutrition., 17, e13133. 10.1111/mcn.13133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D. , Shamseer, L. , Clarke, M. , Ghersi, D. , Liberati, A. , & Petticrew, M. (2015). Preferred reporting items for systematic review and meta‐analysis protocols (prisma‐p) 2015 statement. Systematic Reviews, 4(1), 1–9. 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteiro, J. C. D. , Gomes, F. A. , Stefanello, J. , & Nakano, A. M. S. (2011). Women's perceptions on milk produced and child satisfaction during exclusive breast feeding. Texto & Contexto Enfermagem, 20(2), 359–367. 10.1590/S0104-07072011000200019 [DOI] [Google Scholar]
- Murase, M. , Wagner, E. A. , Chantry, C. , Dewey, K. G. , & Nommsen‐Rivers, L. A. (2016). The relation between breast milk sodium to potassium ratio and maternal report of a milk supply concern. The Journal of Pediatrics, 181, 294–297. 10.1016/j.jpeds.2016.10.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ndikom, C. M. , Fawole, B. , & Ilesanmi, R. E. (2014). Extra fluids for breastfeeding mothers for increasing milk production. Cochrane Database Systym Review, (6), Cd008758. 10.1002/14651858.CD008758.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neifert, M. R (2001). Prevention of breastfeeding tragedies. Pediatric Clinics of North America, 48(2), 273–297. 10.1016/s0031-3955(08)70026-9 [DOI] [PubMed] [Google Scholar]
- Neifert, M. R. (2004). Breastmilk transfer: Positioning, latch‐on, and screening for problems in milk transfer. Clinical Obstetrics and Gynecology, 47(3), 656–675. 10.1097/01.grf.0000136183.12304.96 [DOI] [PubMed] [Google Scholar]
- Neville, M. C. , & Morton, J. (2001). Physiology and Endocrine Changes Underlying Human Lactogenesis II. Journal of Nutrition, 131, 3005S–3008S. 10.1093/jn/131.11.3005S [DOI] [PubMed] [Google Scholar]
- Newman, J. , & Pitman, T. (2015). Guide to breastfeeding. Pinter & Martin Ltd. [Google Scholar]
- Nila, P. , Pequeno, F. , Natália, L. , Araújo, C. , & Lyra, O. (2020). Quality of life assessment instruments for adults: A systematic review of population‐ based studies. Health and Quality of Life Outcomes, 18(208), 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nurhayati, E. , & Fikawati, S. (2019). Counseling of exclusive breastfeeding during antenatal care (ANC) and perceptions of insufficient milk supply. Indonesian Journal of Nutrition and Dietetics, 7(2). 10.21927/ijnd.2019.7(2).65-73 [DOI] [Google Scholar]
- Otsuka, K. , Dennis, C. L. , Tatsuoka, H. , & Jimba, M. (2008). The relationship between breastfeeding self‐efficacy and perceived insufficient milk among Japanese mothers. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 37(5), 546–555. 10.1111/j.1552-6909.2008.00277.x [DOI] [PubMed] [Google Scholar]
- Peacock‐Chambers, E. , Dicks, K. , Sarathy, L. , Brown, A. A. , & Boynton‐Jarrett, R. (2017). Perceived maternal behavioral control, infant behavior, and milk supply: A qualitative study. Journal of Developmental and Behavioral Pediatrics, 38(6), 401–408. 10.1097/dbp.0000000000000455 [DOI] [PubMed] [Google Scholar]
- Prabasiwi, A. , Fikawati, S. , & Syafiq, A. (2015). Exclusive breastfeeding and perception of insufficient milk supply. Kesmas‐National Public Health Journal, 9(3), 282–287. 10.21109/kesmas.v9i3.691 [DOI] [Google Scholar]
- Rodrigo, R. , Rodrigo, A. , Liyanage, N. , Hatahagoda, W. , & Hewavitharana, U. (2018). Maternal Perception of Adequacy of Mother's Milk Among Mothers Giving Birth at a Teaching Hospital in Sri Lanka. Journal of Human Lactation, 35, 171–180. 10.1177/0890334418773304 [DOI] [PubMed] [Google Scholar]
- Rücker, G. , Schwarzer, G. , Carpenter, J. R. , & Schumacher, M. (2008). Undue reliance on I(2) in assessing heterogeneity may mislead. BMC Medical Research Methodology, 8, 79. 10.1186/1471-2288-8-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sacco, L. M. , Caulfield, L. E. , Gittelsohn, J. , & Martinez, H. (2006). The conceptualization of perceived insufficient milk among Mexican mothers. Journal of Human Lactation, 22(3), 277–286. 10.1177/0890334406287817 [DOI] [PubMed] [Google Scholar]
- Safon, C. , Keene, D. , Guevara, W. J. U. , Kiani, S. , Herkert, D. , Muñoz, E. E. , & Pérez‐Escamilla, R. (2017). Determinants of perceived insufficient milk among new mothers in León, Nicaragua. Maternal and Child Nutrition, 13(3), e12369. 10.1111/mcn.12369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandhi, A. , Lee, G. T. , Chipojola, R. , Huda, M. H. , & Kuo, S. Y. (2020). The relationship between perceived milk supply and exclusive breastfeeding during the first six months postpartum: a cross‐sectional study. International Breastfeeding Journal, 15(1), 65. 10.1186/s13006-020-00310-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt, F. L. , & Hunter, J. E. (2015). Methods of meta‐analysis (3rd ed.). Los Angeles, CA: Sage Publications. [Google Scholar]
- Shrago, L. C. , Reifsnider, E. , & Insel, K. (2006). The neonatal bowel output study: Indicators of adequate breast milk intake in neonates. Pediatric Nursing, 32(3), 195–201. [PubMed] [Google Scholar]
- Sun, K. , Chen, M. X. , Yin, Y. Z. , Wu, L. L. , & Gao, L. L. (2017). Why Chinese mothers stop breastfeeding: Mothers' self‐reported reasons for stopping during the first six months. Journal of Child Health Care, 21(3), 353–363. 10.1177/1367493517719160 [DOI] [PubMed] [Google Scholar]
- Sunita, L. , Simmy, C. , & Mamta, N. (2016). Effect of antenatal breast milk expression at term pregnancy to improve post natal lactational performance. Journal of Obstetrics and Gynecology of India, 66(1), 30–34. 10.1007/s13224-014-0648-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, J. , & Harden, A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology, 8, 45. 10.1186/1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorlund, K. , Imberger, G. , Johnston, B. C. , Walsh, M. , Awad, T. , Thabane, L. , … Wetterslev, J. (2012). Evolution of heterogeneity (I2) estimates and their 95% confidence intervals in large meta‐analyses. PLoS ONE, 7(7), e39471. 10.1371/journal.pone.0039471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora, C. G. , Bahl, R. , Barros, A. J. , França, G. V. , Horton, S. , Krasevec, J. , Murch, S. , Sankar, M. J. , Walker, N. , Rollins, N. C. , & Lancet Breastfeeding Series Group . (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet (London, England), 387(10017), 475–490. 10.1016/S0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- Vieira, T. O. , Vieira, G. O. , Giugliani, E. , Mendes, C. M. , Martins, C. C. , & Silva, L. R. (2010). Determinants of breastfeeding initiation within the first hour of life in a Brazilian population: Cross‐sectional study. BMC Public Health, 10(1), 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner, E. A. , Chantry, C. J. , Dewey, K. G. , & Nommsen‐Rivers, L. A. (2013). Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics, 132(4), e865–e875. 10.1542/peds.2013-0724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wake, M. , Morton‐Allen, E. , Poulakis, Z. , Hiscock, H. , Gallagher, S. , & Oberklaid, F. (2006). Prevalence, stability, and outcomes of cry‐fuss and sleep problems in the first 2 years of life: Prospective community based study. Pediatrics, 117, 836–842. 10.1542/peds.2005-0775 [DOI] [PubMed] [Google Scholar]
- Wang, S. , Liu, J. , Guo, N. , & Jiang, H. (2020). The relationship between birthing related factors and maternal breastfeeding confidence in China. Women and Birth, 34, 196–202. 10.1016/j.wombi.2020.02.014 [DOI] [PubMed] [Google Scholar]
- WHO . (2020, July 10). Infant and young child feeding. Retrieved from https://www.who.int/features/factfiles/breastfeeding/en/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Since this article is a systematic review, the data come from articles in academic journals that have been published in the public domain. Data sharing is not applicable to this article.


