Abstract
Adequate dietary diversity among infants is often suboptimal in developing countries. We assessed the impact of nutrition counselling using a digital job aid on dietary diversity of children aged 6–23 months using data from a cluster randomised controlled trial in Bangladesh. The trial had five arms, each with 25 clusters. The four intervention arms provided counselling using a digital job aid and different prenatal and post‐natal combinations of lipid‐based supplements and the comparison arm with usual practice. We enrolled 1500 pregnant women and followed them until the children reached their second birthday. We developed a tablet‐based system for intervention delivery, data collection and project supervision. We combined the four intervention arms (n = 855), in which community health workers (CHWs) provided age‐appropriate complementary feeding counselling, to compare against the comparison arm (n = 403). We calculated the outcome indicators from the children's 24‐h dietary recalls. Overall, the intervention increased the mean dietary diversity score by 0.09 (95% confidence interval [CI]: 0.2–0.16) and odds of minimum dietary diversity by 18% (95% CI: 0.99–1.40). However, there was a significant interaction on the effect of the intervention on dietary diversity by age. The mean dietary diversity score was 0.24 (95% CI: 0.11–0.37) higher in the intervention than in the comparison arm at 9 months and 0.14 (95% CI: 0.01–27) at 12 months of age. The intervention effect was non‐significant at an older age. Overall, consumption of flesh food was 1.32 times higher in the intervention arm (odds ratio [OR] 1.32, 95% CI: 1.11–1.57) in 6–23 months of age. The intervention significantly improved child dietary diversity score in households with mild and moderate food insecurity by 0.27 (95% CI: 0.06–0.49) and 0.16 (0.05–27), respectively, but not with food‐secure and severely food‐insecure households. Although the study did not evaluate the impact of digital job aid alone, the findings indicate the utility of nutrition counselling by CHWs using a digital job aid to improve child feeding practices in broader programmes.
Keywords: cluster randomised controlled trial, community based, counselling, dietary patterns, infant feeding, mHealth, nutrition education
Key messages.
Nutrition counselling of mothers by community health workers using a digital job aid can improve dietary diversity and consumption of animal‐sourced protein among 6‐ to 23‐month‐old children.
Household food insecurity is an important modifying factor for the impact of nutrition counselling on a child's dietary diversity.
Nutrition counselling can result in the early introduction of multiple food groups but may have less effect at older ages.
Policymakers should consider wider programmatic use of digital device‐aided nutrition counselling for community‐based programmes.
1. INTRODUCTION
Childhood undernutrition remains a significant global challenge and is at the core of the Sustainable Development Goals. A recent analysis of data from low‐ and middle‐income countries (LMICs) suggested a moderate reduction in childhood stunting but slow progress in wasting between 2000 and 2015 with high socio‐economic inequity, especially in low‐income countries (Victora et al., 2021). About 22% of the world's under‐five children remains stunted, mostly (54%) from South Asia (Micha et al., 2020). Infant and young child feeding (IYCF) practices, including dietary diversity during 6 to 23 months of life, are critical for a child's growth and development (World Health Organization [WHO], 2003). Inadequate dietary patterns have been linked to acute and chronic childhood undernutrition and can result in long‐term adverse consequences (Bhutta et al., 2013; Victora et al., 2021). Promoting appropriate IYCF is a recommended priority intervention to reduce childhood undernutrition (Keats et al., 2021). Evidence from Bangladesh has also shown a positive impact of appropriate IYCF practices, including adequate dietary diversity on better growth outcomes (K. K. Saha et al., 2008). In addition to promoting appropriate IYCF practices, small‐quantity lipid‐based complementary nutrient supplementation (SQ‐LNS) effectively reduced childhood stunting, wasting and anaemia (Dewey et al., 2021; Keats et al., 2021).
The WHO recommends that children between 6 and 23 months eat a minimum of four out of seven standard food groups daily to meet nutritional demand for optimal growth (WHO, 2010). Further, WHO recommends children consume animal‐sourced foods from 6 months of age because of the high bioavailability of protein, iron and other essential nutrients in these foods (Shapiro et al., 2019). There are reports from resource‐poor settings like Bangladesh of suboptimal nutrition due to a low protein intake in children's daily diet (Choudhury et al., 2019; Islam et al., 2018).
Despite Bangladesh having one of the fastest declining rates of chronic childhood undernutrition in the last two decades, it was still among the 27 high burden countries with more than 20% of children stunted in 2017–2018 (Fanzo et al., 2018; Headey, 2013). Further, there is heterogeneity across geographic and socio‐economic groups (U. R. Saha et al., 2019). Notably, health sector nutrition interventions contributed to 16% of the change in childhood stunting over recent decades (Headey et al., 2015). Nutrition‐specific interventions like promoting of appropriate IYCF practices have not led to consistent improvements in child feeding indicators (NIPORT et al., 2016). The minimum acceptable dietary practices, including continued breastfeeding, consumption from four or more food groups and appropriate meal frequency, stagnated at ~21%–23% between 2011 and 2014 and only improved to 34% in the latest 2017–2018 national survey (Manikam et al., 2018; NIPORT et al., 2019). Dietary diversity remained low, with only 39% of children aged 6–23 months consuming from ≥4 food groups in the last 24 h (NIPORT et al., 2019).
Ensuring adequate dietary diversity among 6‐ to 23‐month‐old children in resource‐poor settings like Bangladesh appears to depend on a variety of background characteristics including socio‐economic status, paternal education, maternal knowledge on child feeding, household food security, engagement in agriculture and location of residence (Choudhury et al., 2019; Dangura & Gebremedhin, 2017; Issaka et al., 2015; Manikam et al., 2018; Solomon et al., 2017). Improved dietary practices are associated with receiving routine maternal care services throughout pregnancy and the post‐partum period and receiving IYCF messages during health care contacts or through targeted counselling demonstration visits (Blackstone & Sanghvi, 2018; Iqbal et al., 2017). Introduction and regular provision of different groups of complementary foods, especially animal‐sourced protein, often rely on the caregiver's perception and knowledge about appropriate feeding practices (Rasheed et al., 2011).
The positive impact of face‐to‐face nutrition counselling of caregivers, either delivered alone or with other behaviour change interventions to improve children's feeding practices, is well documented (Kim et al., 2020). Multiple studies in Bangladesh have demonstrated that nutrition counselling, either one‐to‐one or in small groups of mothers, improved feeding practices among children aged <2 years (Menon et al., 2016; Mistry et al., 2019; Owais et al., 2017). Another study found that group counselling intervention leads to ‘spill‐over’ impact on dietary diversity among children of neighbouring women (Hoddinott et al., 2017).
In Bangladesh, frontline workers at community‐based contacts or primary health care centres are the primary providers of nutrition interventions like IYCF counselling (Menon et al., 2016; K. K. Saha et al., 2015). These services are often of substandard quality due to gaps in service providers' knowledge and skills, high workloads and lack of proper logistics and job aids (Billah et al., 2017). In similar settings, the use of mobile devices (called mHealth) has improved health worker's knowledge and skills, quality of child health services and caretaker's recall of counselling messages (Källander et al., 2013; Perri‐Moore et al., 2015). A recent review of grey literature and a survey of experts identified that 53 digital tools had been implemented in different countries at a pilot or large scale to improve quality nutrition service delivery. Thirty‐six of these tools provided decision support to service providers on nutrition service protocols, and 25 tools supported IYCF counselling (USAID Advancing Nutrition, 2020). However, documented evidence about the likely effects of counselling of mothers using digital job aids on children's dietary practices is scarce.
We implemented a community‐based cluster randomised controlled trial (cRCT) in Bangladesh to explore the effect of four bundles of selected nutrition‐specific interventions on the children's linear growth at 2 years of age (Billah et al., 2017). Individual counselling by community health workers (CHWs) using a custom‐designed electronic application to mothers of children aged 6–23 months old on appropriate IYCF practices was the common component in all four intervention bundles. In this manuscript, we present the findings on the effect of this nutrition counselling of mothers using a digital job aid on the dietary diversity of their 6‐ to 23‐month‐old children, a secondary outcome of the trial.
2. METHODS
2.1. Study design and setting
We conducted a parallel five‐arm cRCT between 2015 and 2019. The trial's primary objective was to assess the impact of four maternal and child nutrition‐specific intervention bundles on children's length‐for‐age Z‐score at 2 years of age. The intervention bundles consisted of three basic nutrition‐specific interventions in four different combinations, delivered during the ‘first 1000 days’ of the child's life. These interventions were (1) counselling using a digital job aid on maternal nutrition during pregnancy, and child nutrition through exclusive breastfeeding up to 6 months and appropriate complementary feeding from 6 to 23 completed months; (2) lipid‐based prenatal nutrient supplement; and (3) lipid‐based complementary nutrient supplement during 6–23 months of age. Arm‐wise intervention combinations included nutrition counselling, prenatal nutrient supplement and complementary nutrient supplement (arm1); nutrition counselling and perinatal nutrient supplement (arm2); nutrition counselling and complementary nutrient supplement (arm3); nutrition counselling alone (arm4); and a natural practice comparison arm (arm5) (Figure 1). We identified women within 125 days of gestation in the intervention and comparison clusters and followed them until the children were 2 years of age. A detailed description of the study design, interventions and data collection methods has been previously published (Billah et al., 2017).
Figure 1.
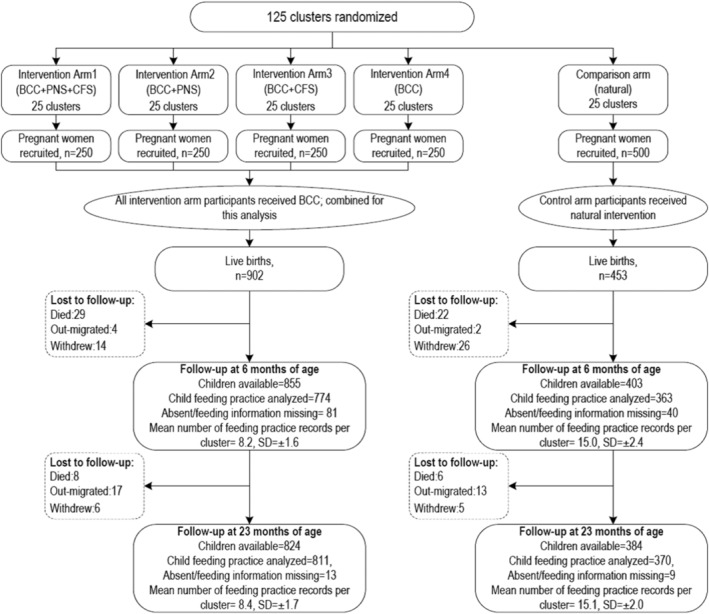
CONSORT diagram showing study arms and the number of participants available at follow‐up visits. BCC, behaviour change communication refers digital platform‐aided nutrition counselling; CNS, lipid‐based complementary nutrient supplement during 6–23 months of age; PNS, lipid‐based prenatal nutrient supplement
This paper focuses on nutrition counselling using digital job aids provided in all four intervention arms to improve child feeding practices. To assess counselling's effect on dietary diversity among 6‐ to 23‐month‐old children, we combined the intervention arms and compared this with the comparison arm. Previous studies showed no impact of lipid‐based complementary nutrient supplement (LNS) on infants' dietary diversity (Arimond et al., 2017). Nonetheless, before combing the intervention arms, we examined the intervention's effect on dietary diversity in each intervention arm compared with the comparison arm. We combined the intervention arms to increase the statistical power for subgroup analysis of the impact of nutrition counselling using a digital job aid. Figure 1 shows the original trial design, the arms we combined for this analysis and the number of study participants available at follow‐up visits. We conducted the study in two rural subdistricts, Bahubal and Nabiganj of Habiganj district, a north‐east district in Bangladesh with a high level of childhood undernutrition (NIPORT et al., 2016). We selected 12 unions, the lowest administrative unit, each comprising ~25,000 people. We defined 125 study clusters each with ~2000 people. Using Stata software, we randomly allocated 25 clusters to each of the five study arms using a block randomisation process with block sizes of 5–15. We had allocation concealment at the cluster level. A statistician assigned deidentified clusters into study arms before starting enrolment of participants. A field manager unmasked cluster identity and disclosed to the CHWs about the interventions to be provided to participants in each cluster according to the assigned study arm. Blinding of CHWs and the participants was not possible due to the type of interventions, that is, counselling and LNS.
We implemented a monthly house‐to‐house surveillance of married women of reproductive age by community‐based surveillance workers to prospectively identify and enrol new pregnancies in the study, 10 in each intervention and 20 in each comparison cluster. We enrolled 1500 pregnant women between November 2015 and May 2016, 250 in each intervention and 500 in the comparison arm. The enrolled pregnant women had 1355 live births (902 in the intervention arms and 453 in the comparison arm), and we followed the newborns for 2 years (Figure 1). This paper included 1258 children (855 in intervention and 403 in comparison) who were alive at 6 months of age and followed up to 2 years between August 2016 and January 2019. The sample size was determined to detect an effect size of 0.4 difference of mean length‐for‐age Z‐score, the primary trial outcome (Billah et al., 2017).
2.2. Intervention description
We adapted maternal and child nutrition counselling messages recommended by WHO‐UNICEF (UNICEF, 2012). We consulted the National IYCF training package for health workers to ensure convergence with locally customised messages and appropriate terminologies in the native language Bangla. Nutrition counselling messages for children 6–23 months included the importance and techniques of timely initiation of complementary feeding, age‐appropriate thickness, quantity, frequency and diversity in complementary feeding, continued breastfeeding, responsive feeding, feeding sick children and picky eaters and basic hygiene practices. We introduced the participants to the concept of different food groups, which they would remember easily, without burdening them with excessive information. We highlighted the importance of animal‐sourced protein (meat, fish, organ meat and egg) and fresh fruits and vegetables in daily complementary feeding. The health workers showed participants the relevant pictorial illustrations of food groups and ‘recommended to avoid’ practices included in the counselling application to facilitate communications. Each counselling session continued for about an hour but varied according to the mothers' situation. Half of the intervention children also received LNS consisting of selected micronutrients (~70%–75% of recommended dietary allowance) in peanut‐and‐oil paste. Participants in the natural practice comparison arm received no intervention from the study but had access to routine care and nutrition counselling for children from local paediatric outpatient health service contacts. However, previous literature reported that current curative service platforms have very low coverage and quality in providing preventive nutrition service like nutrition counselling (K. K. Saha et al., 2015).
We developed an android‐based software application to aid in scheduling and providing nutrition counselling by CHWs. The counselling app had built‐in age‐appropriate messages on feeding practices, to guide the CHWs. The messages provided focused guidance to the CHWs during their counselling sessions aiding them in the challenges of recalling a broad spectrum of age‐wise IYCF messages. The digital tool also helped them navigate across the topics as required. During children's 6–23 months of age, each mother–child pair received up to seven counselling visits at 3‐month intervals starting from six completed months. After notification and entry of a live birth into the system, the counselling app synchronised the birthdate and auto‐generated post‐partum intervention visit plans. The CHWs conducted home visits within ±7 days of the scheduled date for intervention delivery. They made one repeat visit to attempt within the month of the visit schedule if the caregiver was absent.
All CHWs and their immediate supervisors were female, locally recruited and spoke the local dialects of Bangla. We trained the CHWs for 6 days in two phases (3 days each) on the content, counselling techniques and use of the counselling app on the mobile device. The training emphasised the importance and ways of introducing complementary food, multiple food groups, age‐appropriate meal consistency, frequency and quantity. A content expert initially observed each CHW to ensure that they provided appropriate nutrition messages using suitable techniques. Further, we conducted monthly supervision‐monitoring meetings and periodic refresher training throughout the study.
We established a web‐based Project Management Information System (MIS) in which we linked intervention delivery through an android‐based tablet to a central database. The application recorded the completion status in different colour codes of all visits made by CHWs to provide nutrition counselling. The CHWs synced the visit status and relevant information from the application with the central server every day. Field supervisors and the central team regularly used the web‐based desktop dashboard system to monitor activities/performance and provide appropriate feedback. We have reported a detailed description of this system elsewhere (Billah et al., 2017).
2.3. Outcome variables
This paper's outcome variable of interest is the dietary diversity score, a secondary outcome of the trial. We calculated the score using the WHO definition of the number of food groups consumed by a child in the 24 h preceding the interview from seven food groups (WHO, 2008). These food groups include grains, roots and tubers; legumes and nuts; dairy products (milk, yoghurt and cheese); flesh foods (meat, fish, poultry and organ meats); eggs; vitamin‐A‐rich fruits and vegetables; and other fruits and vegetables. We assigned 1 point to a food group if the child consumed any food of that group in the previous 24 h. For composite meals, we assigned each food component separately to its associated food group. Thus, the dietary diversity score for each child could have values from 0 to 7. We calculated the minimum dietary diversity indicator from the dietary diversity scores, defined as ‘children aged 6–23 months fed foods from four or more food groups in the 24 h before the interview’ (WHO, 2008). We also considered the consumption of each of the seven food groups as outcome indicators.
2.4. Data collection
We conducted structured interviews with the study participants (pregnant women) at enrolment to collect their background characteristics, reproductive history, household asset and food security. We conducted structured interviews within 10 days of childbirth to collect the birth outcome, mode and type of birth from the current pregnancy and health care seeking. We collected information on feeding practices for children aged 6–23 months by 24‐h recall method using a structured questionnaire. We adapted the IYCF module of the Bangladesh Demographic and Health Survey for contextualisation of the common food items and local terms (NIPORT et al., 2016). Interviewers asked the mothers if they had fed the child each of the food items listed in the questionnaire in the 24 h preceding the interview. We collected children's feeding practice information at a maximum of seven time points at 6, 9, 12, 15, 18, 21 and 23 completed months of age. An electronic app, which included all questionnaire modules, was developed for conducting interviews using internet‐connected tablets. The app had options for conducting the interview offline and uploaded stored information to a central server when the tablet had internet connectivity. Data collectors, independent from the intervention implementation team, were recruited and trained in interviewing skills, questionnaires and using the app for data collection. The evaluation team supervisors monitored the completion of scheduled visits and quality of interviews by spot checks.
2.5. Statistical analysis
We followed the intention‐to‐treat principle in data analysis. Child feeding practices evaluated by a 24‐h recall interview differ by the child's age (NIPORT et al., 2019). We excluded the data collected more than ±1 month from the scheduled visit except for the 6‐month visit. We included the interviews conducted between 6 and 7 months as 6‐month visit data in the analysis.
We compared the distribution of household socio‐economic status and food security, maternal background characteristics and health care practices at birth across the intervention and comparison arms. We applied principal component analysis to data on household assets to construct a wealth index and divided participants into wealth quintiles based on the index (Vyas & Kumaranayake, 2006). We analysed the intervention effect on the continuous outcome variable, that is, dietary diversity score and binary outcome variables, including minimum dietary diversity and consumption from each food group by linear and logistic mixed models. We included the intervention, that is, receiving nutrition counselling as a binary variable and adjusted for follow‐up visits at different age and randomisation blocks as categorical explanatory variables (fixed effect) in the models. We included two random effects: one for the cluster randomisation and another for repeated measurements of children nested within the clusters. We also assessed whether the intervention effect varied by child's age, maternal education, socio‐economic status and household food security by fitting additional models that included an interaction term between intervention and those variables. We tested statistical significance for the interactions and summarised the estimated intervention effects as mean differences and odds ratios (ORs) for continuous and categorical outcomes, respectively. We calculated 95% confidence intervals (CIs) and p‐values for point estimates of the intervention effect. The difference in outcome between the intervention and comparison arms was considered statistically significant at a level of p‐value < 0.05. We conducted all analyses using Stata Version 14.
2.6. Ethical consideration
This study was registered with ClinicalTrials.gov and approved by the Ethical Review Committee of icddr,b. We completed trial registration in May 2016 after the start of participant recruitment but before completion of enrolment and any of the outcome assessments. However, we did not deviate from the original ethics approved protocol, which we published in 2017 (Billah et al., 2017). We analysed the entire cohort of recruited trial participants. We obtained written informed consent from study participants at two enrolment points. The first was during enrolment, and the second was at the first follow‐up visit after birth. At each follow‐up visit, we obtained verbal consent and confirmed voluntary participation.
3. RESULTS
This analysis included complementary feeding practice data from 1258 children: 855 in the intervention and 403 in the comparison arm. We followed up 1013 children to a maximum of seven scheduled visits between 6 and 23 months of age (Figure 1) with 689 in the intervention and 324 in the comparison arm. Data availability from each visit ranged from ~90% at the 6‐month visit (lowest availability) to ~95% at the 9‐month visit (highest availability). Data were missing mainly due to the absence of the mother at the scheduled household visits. Nonetheless, there were also some refusals, permanent relocations out of the study area and child deaths (Figure 1 and Table S1). The mean age at the follow‐up visits was close to the targeted age in the planned schedule and had small standard deviations (Table S1). The study implementation monitoring reports suggested >90% completion of scheduled counselling visits by CHWs between 6 and 23 months of child's age (data not shown). Exposure to nutrition counselling from existing government and NGO providers was low, 11% and 13% in the intervention and comparison arms at 12 months of child's age, respectively.
Overall, maternal background, household characteristics and health care‐seeking practices at birth were similar in the intervention and comparison arms, except for the distribution of the sex of the child (female 53% vs. 46% in intervention and comparison, respectively) (Table 1). Analyses of dietary diversity score showed a significant interaction of the effect of the intervention by age and household food security status (Figure 2). The mean dietary diversity scores (out of 7) were significantly higher at 9 months (mean difference 0.24, 95% CI: 0.11–0.37) and at 12 months (mean difference 0.14, 95% CI: 0.01–0.27) among children in the intervention arm than in the comparison arm. Counselling interventions had no effect on the dietary diversity score among children in the two extreme groups of food insecurity, that is, participants with no household food insecurity and severe food insecurity. However, we observed a larger impact of the intervention on diet diversity score among participants with mild food insecurity (mean difference between intervention and comparison participants: 0.27, 95% CI: 0.06–0.49) and moderate food insecurity (mean difference 0.16, 95% CI: 0.05–0.27) (Figure 2).
Table 1.
Maternal background and household characteristics at enrolment and health care‐seeking behaviour at birth among mothers with live births
| Characteristics | Intervention a N = 902 | Comparison N = 453 |
|---|---|---|
| % (n) or mean (±SD) | % (n) or mean (±SD) | |
| Maternal age | ||
| <24 | 53.1 (479) | 48.8 (221) |
| 25–29 | 30.3 (273) | 30.2 (137) |
| 30+ | 16.6 (150) | 21.0 (95) |
| Maternal education | ||
| Mean (±SD) years of schooling | 5.93 (±2.9) | 6.13 (±2.9) |
| Maternal occupation | ||
| Engaged in income‐generating activities | 4.2 (38) | 4.4 (20) |
| Homemaker | 95.8 (864) | 95.6 (433) |
| Mother's exposure to mass media | 25.5 (230) | 24.7 (112) |
| Parity b | ||
| Nulliparous | 46.2 (417) | 43.5 (197) |
| Multiparous | 53.8 (485) | 56.5 (256) |
| Gestational age at birth (weeks) | ||
| ≥37 | 83.7 (755) | 79.0 (358) |
| 32–36 | 15.0 (135) | 18.5 (84) |
| ≤31 | 1.3 (12) | 2.4 (11) |
| Sex of the child* | ||
| Male | 47.2 (426) | 53.9 (244) |
| Female | 52.8 (476) | 46.1 (209) |
| Type of birth | ||
| Singleton | 98.7 (890) | 98.0 (444) |
| Multiple | 1.3 (12) | 2.0 (9) |
| Mode of childbirth | ||
| Normal vaginal birth | 76.3 (688) | 75.3 (341) |
| Assisted birth | 6.1 (55) | 7.5 (34) |
| Caesarean section | 17.6 (159) | 17.2 (78) |
| Place of birth | ||
| Home | 59.7 (538) | 60.5 (274) |
| Health facility | 39.9 (360) | 39.3 (178) |
| Other | 0.4 (4) | 0.2 (1) |
| Attendance at birth c | ||
| Skilled birth attendant | 46.8 (422) | 42.6 (193) |
| Unskilled/traditional health care provider | 48.8 (440) | 53.6 (243) |
| Other | 4.0 (36) | 3.3 (15) |
| Household wealth quintile d | ||
| Lowest | 20.7 (187) | 17.6 (80) |
| Second | 18.1 (163) | 22.5 (102) |
| Middle | 20.7 (187) | 20.8 (94) |
| Fourth | 20.0 (180) | 20.8 (94) |
| Highest | 20.5 (185) | 18.3 (83) |
| Household food security e | ||
| Secure | 43.2 (390) | 44.8 (203) |
| Mildly food insecure | 10.8 (97) | 8.4 (38) |
| Moderately food insecure | 33.6 (303) | 36.0 (163) |
| Severely food insecure | 12.2 (110) | 10.8 (49) |
All intervention arms combined.
Included multiple births in the count of firstborns.
Information missing for six participants.
The household wealth quintile was calculated from a composite asset score estimated by principal component analysis of roof, wall and floor materials, toilet facility, electricity, ownership of television, mobile phone, refrigerator, almirah/wardrobe, table, chair, electric fan, water pump, motorcycle/three‐wheelers, livestock and poultry, homestead and farmland.
Information missing for two participants.
p‐value < 0.05.
Figure 2.
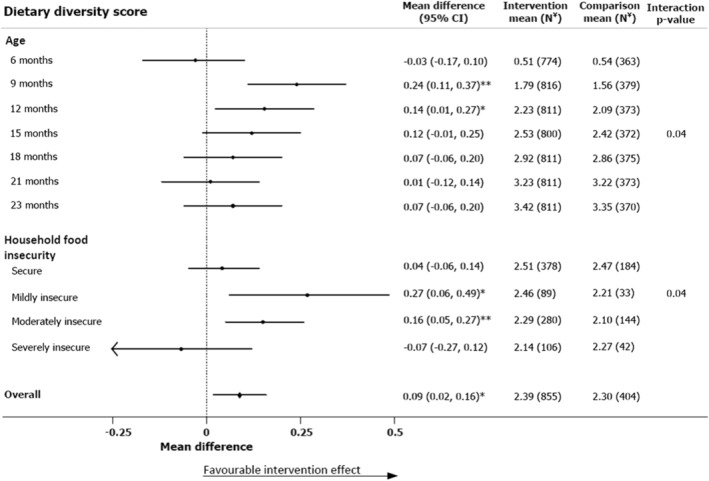
Effect of nutrition counselling using a digital job aid on dietary diversity score at different follow‐up visits between children 6 and 23 months of age and by household food security. *p‐value < 0.05, **p‐value < 0.01 indicate that the intervention effect is significant; interaction p‐value tests the null hypothesis that the effect of intervention is the same across all subgroups; Ψ Ns in household food insecurity subgroups represent number of children had feeding practice data for at least one follow‐up visit. CI, confidence interval
There was a similar pattern of effect of nutrition counselling on minimum dietary diversity by child's age and food security status (Figure 3). The minimum dietary diversity was 2.13 times (95% CI: 1.18–3.82) higher among intervention children at 9 months of age and 1.49 times (95% CI: 1.16–1.90) higher among moderately food‐insecure children in the intervention arm than those in the comparison arm. Among children from households with mild food insecurity, 21% of the intervention children had minimum dietary diversity compared with 15% in comparison children, although statistical significance was marginal (OR 1.54, 95% CI: 0.98–98.03). We found very similar effects for mean dietary diversity score and minimum dietary diversity in each of the four original intervention arms compared with the comparison (Table S2).
Figure 3.
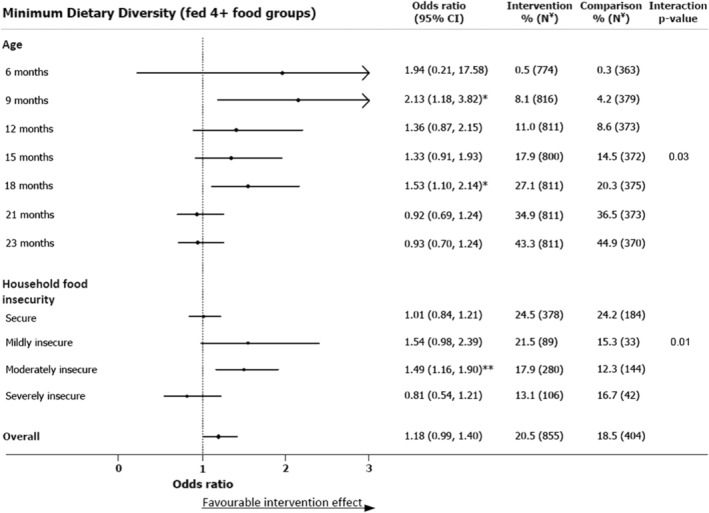
Effect of nutrition counselling using a digital job aid on minimum dietary diversity at different follow‐up visits between children 6 and 23 months of age and by household food security. *p‐value < 0.05, **p‐value < 0.01 indicate that the intervention effect is significant; interaction p‐value tests the null hypothesis that the effect of intervention is the same across all subgroups; Ψ Ns in household food insecurity subgroups represent number of children had feeding practice data for at least one follow‐up visit
The nutrition counselling intervention showed a significant overall effect during 6–23 months on intake of flesh food and eggs (Table 2). Consumption of animal‐sourced protein (eggs, meat, organ meat or fish) was 1.33 times higher in the intervention arm (intervention 60% vs. comparison 56%, OR 1.33, 95% CI: 1.11–1.60). However, the intervention effect on these food groups was higher at younger ages. Consumption of egg was 68% higher among intervention children than the comparison arm at 9 months of age (OR 1.68, 95% CI: 1.14–2.48); but the differences were not detectable at older ages (Table S3). Nutrition counselling had a consistently positive impact on the flesh food intake throughout 6 to 15 months of age (Table S3). Children in the intervention arm were more likely to start the consumption of flesh foods early, at 9 months (intervention 22% vs. comparison 17%, OR 13.16, 95% CI: 1.77–98.03) and continued to have a higher intake of meat, fish or organ meat till 15 months of age (intervention 62% vs. comparison 56%, OR 1.36, 95% CI: 1.02–1.83). Nutrition counselling intervention resulted in increased egg consumption among intervention children with moderate household food insecurity only (intervention 17% vs. comparison 12%, OR 1.46, 95% CI: 1.11–1.92) (Table S4). However, the intervention was effective in boosting flesh food consumption among both mild and moderate food‐insecure participants, 52% in the intervention versus 45% in the comparison, OR 1.41 (95% CI: 1.02–1.95), and 52% in the intervention versus 45% in the comparison group, OR 1.29 (95% CI: 1.10–1.53), respectively (Table S4).
Table 2.
Overall effect of nutrition counselling using a digital job aid on dietary practices among 6‐ to 23‐month‐old children
| Indicator | Intervention [N = 855] | Comparison [N = 404] | OR a | 95% CI |
|---|---|---|---|---|
| Dietary diversity score (mean [±SD]) | 2.39 [±1.39] | 2.30 [±1.38] | 0.09* | 0.02–0.16 |
| MDD (% of children) | 20.5 | 18.5 | 1.18 | 0.99–1.40 |
| Individual food groups (%) | ||||
| Egg | 19.2 | 16.6 | 1.22* | 1.03–1.45 |
| Flesh food | 53.7 | 49.6 | 1.32** | 1.11–1.57 |
| Dairy products | 7.2 | 7.4 | 0.95 | 0.77–1.19 |
| Grains, roots and tubers | 87.5 | 86.7 | 1.11 | 0.88–1.40 |
| Vitamin‐A‐rich fruits and vegetables | 23.5 | 22.3 | 1.10 | 0.97–1.24 |
| Legumes and nuts | 20.2 | 19.4 | 1.05 | 0.91–1.20 |
| Other fruits and vegetables b | 31.7 | 32.1 | 0.96 | 0.85–1.10 |
Note: Overall effect of intervention was estimated including visits at all ages and levels of food insecurity.
Abbreviations: CI, confidence interval; MDD, minimum dietary diversity (consumption of 4+ food groups).
Odds ratio (OR) from a logistic mixed‐effect model with randomisation block and individual‐level (child) clustering; OR represents the ratio of odds of having reported consuming a food group in past 24 h.
Analysed excluding 6 months of observations as comparison samples had zero value resulting estimate of OR to infinity.
p‐value < 0.05.
p‐value < 0.01.
Although a lower proportion of intervention participants consumed grains, roots and tubers at 6 months age (OR 0.70, 95% CI: 0.51–0.96), they were 1.70 (95% CI: 1.15–2.52) times more likely to consume grains than comparison participants at 9 months of age (Table S3). Consumption of dairy products was low in both groups across all ages. Consumption of legumes and nuts was similar in the intervention and comparison arms at different ages. However, intervention children were 1.60 times (95% CI: 1.03–2.48) and 1.32 times (95% CI: 1.05–1.67) more likely to consume legumes and nuts in mild and moderate food‐insecure groups, respectively (Table S4). The intervention effect was also non‐significant for consumption of dairy products, vitamin‐A‐rich fruits and vegetables and other fruits and vegetables in any food security status subgroups (Table S4). Subgroup analysis by the participants' socio‐economic status and maternal education status did not show any critical differences in intervention effects on the dietary practices among 6‐ to 23‐month‐old children (data not shown).
4. DISCUSSION
We found that individual nutrition counselling of mothers by CHWs using a customised, mobile application improved feeding practices among 6‐ to 23‐month‐old children in rural Bangladesh. We showed that seven counselling visits between 6 and 23 months of age could improve the mean number of food groups fed to 6‐ to 23‐month‐old children. We also showed that nutrition counselling could improve the early introduction of egg, flesh food and grains in the diet of 6‐ to 23‐month‐old children. We observed improved dietary diversity among intervention children up to 12 months of age and for flesh food for up to 15 months. We also found that nutrition counselling improved children's feeding practices in mild and moderately food‐insecure households but not in food‐secure or severely food‐insecure households. Our findings also identified household food security to be an important contextual consideration when designing nutrition education programmes.
The original study had four intervention arms. Combining these arms to explore nutrition counselling's impact on dietary diversity among children 6–23 months is valid. Counselling on appropriate IYCF practices was the same in all intervention arms by the same staff. Furthermore, we saw that the effects were similar across the four intervention arms including the arm with nutrition counselling alone (Table S2). Previous studies reported that the provision of LNS had no impact on children's dietary diversity (Arimond et al., 2017). Consistent with these findings, we did not see any difference in dietary diversity across the intervention arms with or without LNS.
Our findings of a positive impact of nutrition counselling on improved dietary diversity and higher consumption of egg, flesh food and grains are consistent with similar community‐based studies in LMICs. Most other studies assessed the impact of nutrition education up to 18 months of children (Bhandari et al., 2004; Guldan et al., 2000; Penny et al., 2005; Shi et al., 2010; Vazir et al., 2013), whereas we evaluated the effect until 23 completed months. We found that nutrition counselling had its greatest impact on flesh flood consumption up to 15 months of the children's age. Considering the suboptimal consumption of animal‐sourced protein in rural 6‐ to 23‐month‐old children, we included relevant messages on animal‐sourced protein in children's diet in our nutrition counselling module. The CHWs emphasised this issue while counselling. A study in China also showed that prioritising messages on animal‐sourced protein during nutrition counselling doubled its consumption among intervention children compared with the controls (Shi et al., 2010). Higher consumption of flesh foods among the intervention children between 6 and 15 months of age was mainly from increased fish consumption (data not presented). Consumption of dairy food was low among both intervention and comparison children, consistent with general child feeding practice in Bangladesh (NIPORT et al., 2019).
We did not find an intervention impact on dietary diversity and individual food groups beyond 15 months of age, which can be explained by the gradual improvement of dietary diversity with age and a reduced intervention effect in older children. The positive impact of counselling on earlier introduction and continuation of diverse and specific food groups was followed by a plateauing of dietary diversity, a finding that is consistent with other studies. In India, a study showed higher rice, milk and vegetable consumption in children at 9 months but no difference at 18 months between intervention and control arms (Bhandari et al., 2004). Another intervention study in Peru found a higher egg, chicken liver or fish consumption at 6 and 8 months in the intervention arm but no statistically significant difference from 9 months onwards (Penny et al., 2005).
In contrast to a study in China (Shi et al., 2010), we found no difference in the mean dietary diversity score between intervention and control arms at 6 months of age. The WHO‐UNICEF IYCF guideline recommends the initiation of complementary feeding at six completed months (UNICEF, 2012). We assessed feeding practice at the beginning of the seventh month of age; the mean age at the visit was 6.2 and 6.1 months for the intervention and comparison arms, respectively (Table S1). It is reasonable to assume that dietary diversity would not be noticeable at the earliest stage of initiating complementary food. Nonetheless, we observed a higher proportion of children in the comparison arm, consuming grains and dairy products at 6 months. We assume that these children were introduced to complementary food before 6 months, despite the recommendation to breastfeed exclusively until this age. In future analyses, we will test this hypothesis and analyse exclusive breastfeeding practice in the cohort.
The minimum dietary diversity was 18% higher in the intervention arm irrespective of the child's age and household food insecurity, although the finding was not statistically significant (p = 0.07). One explanation is that the nutrition counselling intervention could improve consumption of some of the food groups, but not all, in the study population where poor dietary diversity among children 6–23 months is common (NIPORT et al., 2019). The findings on the overall effect of nutrition counselling on dietary diversity should be interpreted with caution. The substantial effect modification by age and limited effect beyond 12 months have resulted in an overall low effect size on dietary diversity. A recent study from urban Bangladesh reported 1.95‐fold increase in minimum dietary diversity among 7‐ to 12‐month‐old children whose mothers received peer counselling, consistent with the intervention effect observed at 9 months of children's age in our study (Ara et al., 2019). A meta‐analysis of three studies that involved nutrition counselling, including one from rural Bangladesh, showed 1.64‐fold increase (95% CI: 0.92–2.03) in minimum dietary diversity among 6‐ to 23‐month‐old children (Janmohamed et al., 2020). However, it is difficult to compare these studies with our findings directly as none of these studies reported the effect by age groups or any effect modification by age. These earlier studies did not use digital job aids and are too diverse to easily compare with our trial to elucidate any added impact from the use of digital technology.
Household food security has played a role too, because about 45% of our study children belonged to food‐insecure households. Our subgroup analysis suggested that nutrition counselling had a statistically significant effect on improving minimum dietary diversity (OR 1.49, 95% CI: 1.16–1.90) among children from moderately food‐insecure households. We observed a similar effect on minimum dietary diversity (OR 1.59, 95% CI: 0.99–2.39) in participants from mildly food‐insecure households. But this effect was marginally significant (p = 0.06) with a wide CI due to the small sample. Studies from similar settings suggest that household food security is strongly associated with dietary diversity among 6‐ to 23‐month‐old children (Agbadi et al., 2017; Chandrasekhar et al., 2017). High levels of food insecurity may also explain greater consumption of grains and low consumption of dairy products, legumes and nuts, vitamin‐A‐rich food and fruits and vegetables in both intervention and comparison children resulting in no significant intervention effect on these food groups. A Malawian nutrition education study in a high food‐insecure population also found no effect of the intervention on these outcomes (Kuchenbecker et al., 2017). Adding nutrition‐sensitive interventions like cash transfers with nutrition counselling might have a better outcome for all food groups and minimum dietary diversity in food‐insecure settings, as was found in a social safety net study in Bangladesh (Ahmed et al., 2016).
Our study's strength is the longitudinal follow‐up of intervention and comparison children, which let us explore the impact of counselling on feeding practices from 6 months to 2 years of age, including early introduction of different food groups. The balance in the maternal background and health care characteristics and low loss to follow‐up in both arms are likely to ensure the study's internal validity. The cluster randomised design and provision of individual counselling of enrolled mothers at home by CHWs reduced the likelihood of contamination of our intervention. The digital data collection with consistency, logic and range checks reduced the chance of errors in data entry and ensured timely visits by evaluation data collectors.
Our study has some limitations. First, our findings are generalisable to populations similar to our resource‐poor study area with household food insecurity and where suboptimal child feeding practices are common. Second, blinding of the participants and interviewers who collected feeding practice information about the intervention was not possible due to the nature of the intervention. However, we expect a very low or no information bias. The evaluation team was independent of the intervention delivery team and collected data on feeding practices using structured and validated tools. Third, we did not collect information on quantities of the food consumed and therefore are unable to report the intervention impact on the nutrient content of complementary foods. However, dietary diversity is much easier to collect and is reliable in terms of data quality on food intake and is considered a good proxy for understanding diet quality. We did not collect data on the cost of nutrition counselling with digital job aid intervention and therefore did not conduct an economic analysis in the study. Fourth, although contamination was unlikely, it was not impossible. Mothers in the comparison arm may have received nutrition messages at routine childcare contacts. We did not assess if providing small‐quantity lipid‐based complementary nutrient supplements in two intervention arms influenced the child's dietary diversity. A previous study reported an equal or greater minimum dietary diversity in complementary food supplemented arms compared with a child feeding counselling only arm (Campbell et al., 2016). The authors speculated that food supplements might have improved appetite among children and influenced mothers' active and responsive child feeding behaviours. Nonetheless, we found a similar effect size for each of the intervention arms with or without complementary nutrient supplement compared with the comparison arm.
In our study, CHWs delivered nutrition counselling using a digital job aid. However, we cannot conclude that improved practices in dietary diversity among intervention children are attributable to the application of the digital job aid as we did not have an arm with nutrition counselling without a digital job aid. Limited evidence is available in LMICs of the impact on digital job aid supported nutrition education interventions on complementary feeding practices and dietary diversity outcomes (Mildon & Sellen, 2019). One study in India used a digital job aid tool for nutrition counselling, which reported significant improvements in solid and semi‐solid food consumption among children aged 6 months or older (Borkum et al., 2015). However, our findings reinforce the benefits of nutrition counselling interventions for improving optimal dietary diversity among infants and young children and support integration of digital job aids in nutrition service delivery in settings like Bangladesh, where the quality of nutrition services is poor (Billah et al., 2017).
Further research to explore the consistency of the findings in similar settings would be useful. Although other studies have reported the effect of nutrition education on child growth outcomes in food‐insecure settings (Lassi et al., 2020), there is little evidence about whether or not educational interventions alone can improve dietary diversity in food‐insecure environments. We found that nutrition counselling was effective for children from mild or moderate food‐insecure households in subgroup analyses. Integration of social protection interventions with nutrition counselling (Ahmed et al., 2016) should be tested to improve early and sustained dietary diversity among 6‐ to 23‐month‐old children in food‐insecure settings.
CONFLICTS OF INTEREST
The authors declared no conflict of interest.
CONTRIBUTIONS
SEA, PM, TA, SG, JH, SMB and MJD conceptualised and designed the study; SMB and TF implemented the study under the supervision of SEA and TA; NC guided the counselling package and evaluation tools development; ABS managed and cleaned the data; SMB analysed data under the guidance of PK, MJD and CRG; SMB prepared the first draft. MJD, CRG, TF and PK reviewed multiple drafts and guided revisions. All authors read and approved the final manuscript.
Supporting information
Table S1: Data availability and age at follow up visits for assessing dietary intake of 6–23 months old children
Table S2: Effect of nutrition counselling using a digital job aid on dietary practices among 6–23 months old children in each of the four intervention arms
Table S3: Effect of nutrition counselling using a digital job aid on the consumption of seven individual food groups at different follow‐up visits between children 6–23 months of age
Table S4: Effect of nutrition counselling using a digital job aid on the consumption of seven individual food groups among 6–23 months old children by household food insecurity status
ACKNOWLEDGMENTS
We are grateful to all study participants, study implementation and data collection team. This research was funded by the UKAID, the then Department for International Development (DfID) through the Transform Nutrition Research Consortium (PO5243, Aries Code 201448), and Swedish International Development Cooperation Agency (Sida [Styrelsen för Internationellt Utvecklingssamarbete]), Sweden (54100089). icddr,b acknowledges with gratitude the commitment of UKAID to its research efforts. icddr,b also gratefully acknowledges the following donors who provide unrestricted support: Governments of Bangladesh, Canada, Sweden and the United Kingdom.
Billah, S. M. , Ferdous, T. E. , Kelly, P. , Raynes‐Greenow, C. , Siddique, A. B. , Choudhury, N. , Ahmed, T. , Gillespie, S. , Hoddinott, J. , Menon, P. , Dibley, M. J. , & Arifeen, S. E. (2021). Effect of nutrition counselling with a digital job aid on child dietary diversity: Analysis of secondary outcomes from a cluster randomised controlled trial in rural Bangladesh. Maternal & Child Nutrition, 18:e13267. 10.1111/mcn.13267
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Agbadi, P. , Urke, H. B. , & Mittelmark, M. B. (2017). Household food security and adequacy of child diet in the food insecure region north in Ghana. PLoS ONE, 12(5), e0177377. 10.1371/journal.pone.0177377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed, A. U. , Hoddinott, J. F. , Roy, S. , Sraboni, E. , Quabili, W. R. , & Margolies, A. (2016). Which kinds of social safety net transfers work best for the ultra poor in Bangladesh?: Operation and impacts of the transfer modality research initiative. Retrieved from Dhaka.
- Ara, G. , Khanam, M. , Papri, N. , Nahar, B. , Kabir, I. , Sanin, K. I. , Khan, S. S. , Sarker, M. S. A. , & Dibley, M. J. (2019). Peer counseling promotes appropriate infant feeding practices and improves infant growth and development in an urban slum in Bangladesh: A community‐based cluster randomized controlled trial. Current Developments in Nutrition, 3(7), nzz072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arimond, M. , Abbeddou, S. , Kumwenda, C. , Okronipa, H. , Hemsworth, J. , Jimenez, E. Y. , Ocansey, E. , Lartey, A. , Ashorn, U. , Adu‐Afarwuah, S. , Vosti, S. A. , Hess, S. Y. , & Dewey, K. G. (2017). Impact of small quantity lipid‐based nutrient supplements on infant and young child feeding practices at 18 months of age: Results from four randomized controlled trials in Africa. Maternal & Child Nutrition, 13(3), e12377. 10.1111/mcn.12377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhandari, N. , Mazumder, S. , Bahl, R. , Martines, J. , Black, R. E. , Bhan, M. K. , & Infant Feeding Study Group . (2004). An educational intervention to promote appropriate complementary feeding practices and physical growth in infants and young children in rural Haryana, India. The Journal of Nutrition, 134(9), 2342–2348. 10.1093/jn/134.9.2342 [DOI] [PubMed] [Google Scholar]
- Bhutta, Z. A. , Das, J. K. , Rizvi, A. , Gaffey, M. F. , Walker, N. , Horton, S. , Webb, P. , Lartey, A. , & Black, R. E. (2013). Evidence‐based interventions for improvement of maternal and child nutrition: what can be done and at what cost? The Lancet, 382(9890), 452–477. 10.1016/S0140-6736(13)60996-4 [DOI] [PubMed] [Google Scholar]
- Billah, S. M. , Saha, K. K. , Khan, A. N. S. , Chowdhury, A. H. , Garnett, S. P. , El Arifeen, S. , & Menon, P. (2017). Quality of nutrition services in primary health care facilities: Implications for integrating nutrition into the health system in Bangladesh. PLoS ONE, 12(5), e0178121. 10.1371/journal.pone.0178121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackstone, S. , & Sanghvi, T. (2018). A comparison of minimum dietary diversity in Bangladesh in 2011 and 2014. Maternal & Child Nutrition, 14(4), e12609. 10.1111/mcn.12609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borkum, E. , Sivasankaran, A. , Sridharan, S. , Rotz, D. , Sethi, S. , Manoranjini, M. , Ramakrishnan, L. , & Rangarajan, A. (2015). Evaluation of the information and communication technology (ICT) continuum of care services (CCS) intervention in Bihar. Mathematica Policy Research. [Google Scholar]
- Campbell, R. K. , Hurley, K. M. , Shamim, A. A. , Shaikh, S. , Chowdhury, Z. T. , Mehra, S. , de Pee, S. , Ahmed, T. , West, K. P. Jr. , & Christian, P. (2016). Effect of complementary food supplementation on breastfeeding and home diet in rural Bangladeshi children. The American Journal of Clinical Nutrition, 104(5), 1450–1458. 10.3945/ajcn.116.135509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandrasekhar, S. , Aguayo, V. M. , Krishna, V. , & Nair, R. (2017). Household food insecurity and children's dietary diversity and nutrition in India. Evidence from the comprehensive nutrition survey in Maharashtra. Maternal & Child Nutrition, 13, e12447. 10.1111/mcn.12447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choudhury, S. , Headey, D. D. , & Masters, W. A. (2019). First foods: Diet quality among infants aged 6–23 months in 42 countries. Food Policy, 88, 101762. 10.1016/j.foodpol.2019.101762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dangura, D. , & Gebremedhin, S. (2017). Dietary diversity and associated factors among children 6–23 months of age in Gorche district, Southern Ethiopia: Cross‐sectional study. BMC Pediatrics, 17(1), 6. 10.1186/s12887-016-0764-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewey, K. G. , Wessells, K. R. , Arnold, C. D. , Prado, E. L. , Abbeddou, S. , Adu‐Afarwuah, S. , Ali, H. , Arnold, B. F. , Ashorn, P. , Ashorn, U. , Ashraf, S. , Becquey, E. , Bendabenda, J. , Brown, K. H. , Christian, P. , Colford, J. M. Jr. , Dulience, S. J. L. , Fernald, L. C. H. , Galasso, E. , … Stewart, C. P. (2021). Characteristics that modify the effect of small‐quantity lipid‐based nutrient supplementation on child growth: an individual participant data meta‐analysis of randomized controlled trials. MedRxiv. 10.1101/2021.02.05.21251105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fanzo, J. , Hawkes, C. , Udomkesmalee, E. , Afshin, A. , Allemandi, L. , Assery, O. Baker, P. , Battersby, J. , Bhutta, Z. , Chen, K. , Corvalan, C. , Di Cesare, M. , Dolan, C. , Fonseca, J. , Grummer‐Strawn, L. , Hayashi, C. , McArthur, J. , Rao, A. , Rosenzweig, C. , & Schofield, D. (2018) 2018 Global Nutrition Report: Shining a light to spur action on nutrition. Technical Report. Bristol, UK: Development Initiatives. [Monograph] [Google Scholar]
- Guldan, G. S. , Fan, H.‐C. , Ma, X. , Ni, Z.‐Z. , Xiang, X. , & Tang, M.‐Z. (2000). Culturally appropriate nutrition education improves infant feeding and growth in rural Sichuan, China. The Journal of Nutrition, 130(5), 1204–1211. 10.1093/jn/130.5.1204 [DOI] [PubMed] [Google Scholar]
- Headey, D. , Hoddinott, J. , Ali, D. , Tesfaye, R. , & Dereje, M. (2015). The other Asian enigma: Explaining the rapid reduction of undernutrition in Bangladesh. World Development, 66, 749–761. 10.1016/j.worlddev.2014.09.022 [DOI] [Google Scholar]
- Headey, D. D. (2013). Developmental drivers of nutritional change: A cross‐country analysis. World Development, 42, 76–88. 10.1016/j.worlddev.2012.07.002 [DOI] [Google Scholar]
- Hoddinott, J. , Ahmed, I. , Ahmed, A. , & Roy, S. (2017). Behavior change communication activities improve infant and young child nutrition knowledge and practice of neighboring non‐participants in a cluster‐randomized trial in rural Bangladesh. PLoS ONE, 12(6), e0179866. 10.1371/journal.pone.0179866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal, S. , Zakar, R. , Zakar, M. Z. , & Fischer, F. (2017). Factors associated with infants' and young children's (6–23 months) dietary diversity in Pakistan: Evidence from the demographic and health survey 2012–13. Nutrition Journal, 16(1), 78. 10.1186/s12937-017-0297-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam, M. M. , Sanin, K. I. , Mahfuz, M. , Ahmed, A. S. , Mondal, D. , Haque, R. , & Ahmed, T. (2018). Risk factors of stunting among children living in an urban slum of Bangladesh: Findings of a prospective cohort study. BMC Public Health, 18(1), 197. 10.1186/s12889-018-5101-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Issaka, A. I. , Agho, K. E. N. , Page, A. L. , Burns, P. , Stevens, G. J. , & Dibley, M. J. (2015). The problem of suboptimal complementary feeding practices in West Africa: What is the way forward? Maternal & Child Nutrition, 11, 53–60. 10.1111/mcn.12195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janmohamed, A. , Sohani, N. , Lassi, Z. S. , & Bhutta, Z. A. (2020). The effects of community home visit and peer group nutrition intervention delivery platforms on nutrition outcomes in low and middle‐income countries: A systematic review and meta‐analysis. Nutrients, 12(2), 440. 10.3390/nu12020440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Källander, K. , Tibenderana, J. K. , Akpogheneta, O. J. , Strachan, D. L. , Hill, Z. , ten Asbroek, A. H. , Conteh, L. , Kirkwood, B. R. , & Meek, S. R. (2013). Mobile health (mHealth) approaches and lessons for increased performance and retention of community health workers in low‐and middle‐income countries: A review. Journal of Medical Internet Research, 15(1), e17. 10.2196/jmir.2130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keats, E. C. , Das, J. K. , Salam, R. A. , Lassi, Z. S. , Imdad, A. , Black, R. E. , & Bhutta, Z. A. (2021). Effective interventions to address maternal and child malnutrition: An update of the evidence. The Lancet Child & Adolescent Health. [DOI] [PubMed] [Google Scholar]
- Kim, S. , Phuong, N. H. , Lan, T. M. , & Menon, P. (2020). Different combinations of behavior change interventions and frequencies of interpersonal contacts are associated with infant and young child feeding practices in Bangladesh, Ethiopia, and Vietnam. Current Developments in Nutrition., 4. 10.1093/cdn/nzz140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuchenbecker, J. , Reinbott, A. , Mtimuni, B. , Krawinkel, M. B. , & Jordan, I. (2017). Nutrition education improves dietary diversity of children 6–23 months at community‐level: Results from a cluster randomized controlled trial in Malawi. PLoS ONE, 12(4), e0175216. 10.1371/journal.pone.0175216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassi, Z. S. , Rind, F. , Irfan, O. , Hadi, R. , Das, J. K. , & Bhutta, Z. A. (2020). Impact of infant and young child feeding (IYCF) nutrition interventions on breastfeeding practices, growth and mortality in low‐and middle‐income countries: Systematic review. Nutrients, 12(3), 722. 10.3390/nu12030722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manikam, L. , Prasad, A. , Dharmaratnam, A. , Moen, C. , Robinson, A. , Light, A. , Ahmed, S. , Lingam, R. , & Lakhanpaul, M. (2018). Systematic review of infant and young child complementary feeding practices in South Asian families: The India perspective. Public Health Nutrition, 21(4), 637–654. 10.1017/S136898001700297X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon, P. , Nguyen, P. H. , Saha, K. K. , Khaled, A. , Sanghvi, T. , Baker, J. , Afsana, K. , Haque, R. , Frongillo, E. A. , Ruel, M. T. , & Rawat, R. (2016). Combining intensive counseling by frontline workers with a nationwide mass media campaign has large differential impacts on complementary feeding practices but not on child growth: Results of a cluster‐randomized program evaluation in Bangladesh. The Journal of Nutrition, 146(10), 2075–2084. 10.3945/jn.116.232314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micha, R. , Mannar, V. , Afshin, A. , Allemandi, L. , Baker, P. , & Battersby, J. (2020). Global nutrition report: Action on equity to end malnutrition 2020.
- Mildon, A. , & Sellen, D. (2019). Use of mobile phones for behavior change communication to improve maternal, newborn and child health: A scoping review. Journal of Global Health, 9(2). 10.7189/jogh.09.020425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mistry, S. K. , Hossain, M. B. , & Arora, A. (2019). Maternal nutrition counselling is associated with reduced stunting prevalence and improved feeding practices in early childhood: A post‐program comparison study. Nutrition Journal, 18(1), 47. 10.1186/s12937-019-0473-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIPORT , Mitra and Associates , & ICF International . (2016). Bangladesh Demographic and Health Survey 2014. Retrieved from Dhaka, Bangladesh, and Rockville, Maryland, USA:
- NIPORT , Mitra and Associates , & ICF International . (2019). Bangladesh Demographic and Health Survey 2017–18: Key indicators. Retrieved from Dhaka, Bangladesh, and Rockville, Maryland, USA:
- Owais, A. , Schwartz, B. , Kleinbaum, D. G. , Suchdev, P. S. , Faruque, A. S. G. , Das, S. K. , Rahman, S. , & Stein, A. D. (2017). A nutrition education program in rural Bangladesh was associated with improved feeding practices but not with child growth. The Journal of Nutrition, 147(5), 948–954. 10.3945/jn.116.243956 [DOI] [PubMed] [Google Scholar]
- Penny, M. E. , Creed‐Kanashiro, H. M. , Robert, R. C. , Narro, M. R. , Caulfield, L. E. , & Black, R. E. (2005). Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: A cluster‐randomised controlled trial. The Lancet, 365(9474), 1863–1872. 10.1016/S0140-6736(05)66426-4 [DOI] [PubMed] [Google Scholar]
- Perri‐Moore, S. , Routen, T. , Shao, A. F. , Rambaud‐Althaus, C. , Swai, N. , Kahama‐Maro, J. , D'Acremont, V. , Genton, B. , & Mitchell, M. (2015). Using an eIMCI‐derived decision support protocol to improve provider–caretaker communication for treatment of children under 5 in Tanzania. Global Health Communication, 1(1), 41–47. 10.1080/23762004.2016.1181486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasheed, S. , Haider, R. , Hassan, N. , Pachón, H. , Islam, S. , Jalal, C. S. , & Sanghvi, T. G. (2011). Why does nutrition deteriorate rapidly among children under 2 years of age? Using qualitative methods to understand community perspectives on complementary feeding practices in Bangladesh. Food and Nutrition Bulletin, 32(3), 192–200. 10.1177/156482651103200302 [DOI] [PubMed] [Google Scholar]
- Saha, K. K. , Billah, M. , Menon, P. , El Arifeen, S. , & Mbuya, N. V. (2015). Bangladesh National Nutrition Services: Assessment of implementation status. The World Bank. 10.1596/978-1-4648-0640-7 [DOI] [Google Scholar]
- Saha, K. K. , Frongillo, E. A. , Alam, D. S. , Arifeen, S. E. , Persson, L. Å. , & Rasmussen, K. M. (2008). Appropriate infant feeding practices result in better growth of infants and young children in rural Bangladesh. The American Journal of Clinical Nutrition, 87(6), 1852–1859. 10.1093/ajcn/87.6.1852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha, U. R. , Chattapadhayay, A. , & Richardus, J. H. (2019). Trends, prevalence and determinants of childhood chronic undernutrition in regional divisions of Bangladesh: Evidence from demographic health surveys, 2011 and 2014. PloS One, 14(8), e0229677. 10.1371/journal.pone.0229677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro, M. J. , Downs, S. M. , Swartz, H. J. , Parker, M. , Quelhas, D. , Kreis, K. , Kraemer, K. , West, K. P. Jr. , & Fanzo, J. (2019). A systematic review investigating the relation between animal‐source food consumption and stunting in children aged 6–60 months in low and middle‐income countries. Advances in Nutrition, 10(5), 827–847. 10.1093/advances/nmz018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi, L. , Zhang, J. , Wang, Y. , Caulfield, L. E. , & Guyer, B. (2010). Effectiveness of an educational intervention on complementary feeding practices and growth in rural China: A cluster randomised controlled trial. Public Health Nutrition, 13(4), 556–565. 10.1017/S1368980009991364 [DOI] [PubMed] [Google Scholar]
- Solomon, D. , Aderaw, Z. , & Tegegne, T. K. (2017). Minimum dietary diversity and associated factors among children aged 6–23 months in Addis Ababa, Ethiopia. International Journal for Equity in Health, 16(1), 181. 10.1186/s12939-017-0680-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . (2012). The community infant and young child feeding counselling package: Key messages booklet. Retrieved from New York: https://www.unicef.org/nutrition/files/Key_Message_Booklet_2012_small.pdf
- USAID Advancing Nutrition . (2020). Using digital tools to strengthen nutrition service delivery: An overview. Retrieved from Arlington, VA.
- Vazir, S. , Engle, P. , Balakrishna, N. , Griffiths, P. L. , Johnson, S. L. , Creed‐Kanashiro, H. , Fernandez Rao, S. , Shroff, M. R. , & Bentley, M. E. (2013). Cluster‐randomized trial on complementary and responsive feeding education to caregivers found improved dietary intake, growth and development among rural Indian toddlers. Maternal & Child Nutrition, 9(1), 99–117. 10.1111/j.1740-8709.2012.00413.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora, C. G. , Christian, P. , Vidaletti, L. P. , Gatica‐Domínguez, G. , Menon, P. , & Black, R. E. (2021). Revisiting maternal and child undernutrition in low‐income and middle‐income countries: Variable progress towards an unfinished agenda. The Lancet. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyas, S. , & Kumaranayake, L. (2006). Constructing socio‐economic status indices: How to use principal components analysis. Health Policy and Planning, 21(6), 459–468. 10.1093/heapol/czl029 [DOI] [PubMed] [Google Scholar]
- WHO . (2003). Global strategy for infant and young child feeding. Retrieved from Geneva.
- WHO . (2008). Indicators for assessing infant and young child feeding practices: Part1 Definitions (9241599294). Retrieved from Geneva, Switzerland.
- WHO . (2010). Indicators for assessing infant and young child feeding practices: Part 2: Measurement. Retrieved from
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Data availability and age at follow up visits for assessing dietary intake of 6–23 months old children
Table S2: Effect of nutrition counselling using a digital job aid on dietary practices among 6–23 months old children in each of the four intervention arms
Table S3: Effect of nutrition counselling using a digital job aid on the consumption of seven individual food groups at different follow‐up visits between children 6–23 months of age
Table S4: Effect of nutrition counselling using a digital job aid on the consumption of seven individual food groups among 6–23 months old children by household food insecurity status
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


