Abstract
This systematic review and meta‐analysis aimed to assess the robustness of designs and tools used in nutrition social behaviour change communication (NSBCC) interventions and establish their effectiveness. EBSCOhost as an umbrella database including Medline (Ovid) and CINAHL, EMBASE, and ProQUEST databases were searched for peer‐reviewed articles from January 1960 to October 2018. Additional sources were searched to identify all relevant studies including grey literature. Studies' biases were assessed according to Cochrane handbook. Pooled estimate of effectiveness of interventions on infant and young child feeding (IYCF) practices and child nutritional status with 95% confidence intervals were measured using random‐effects models. Eighty studies were included in this review: Fifty‐one (64%) were cluster randomised controlled trials (RCTs), 13 (16%) were RCTs and 16 (20%) quasi‐experimental. Of the included studies, 22 (27%) measured early initiation of breastfeeding, 38 (47%) measured exclusive breastfeeding, 29 (36%) measured minimum dietary diversity, 21 (26%) measured minimum meal frequency, 26 (32%) measured height for age z‐scores (HAZ), 23 (29%) measured weight for height z‐scores (WHZ), 27 (34%) measured weight for age z‐scores (WAZ), 20 (25%) measured stunting, 14 (17%) measured wasting, and 11 (14%) measured underweight. The overall intervention's effect was significant for exclusive breastfeeding (EBF) (odds ratio = 1.73; 95% confidence interval [CI]: 1.35–2.11, p < 0.001), HAZ (standardized mean differences [SMD] = 0.19; 95% CI: 0.17–0.21; p < 0.001), WHZ (SMD = 0.02; 95% CI: 0.004–0.04; p < 0.001), and WAZ (SMD = 0.04; 95% CI: 0.02–0.06; p < 0.001). Evidence shows the effectiveness of NSBCC in improving EBF and child anthropometric outcomes. Further research should test the impact on child nutritional status with clearly specified and detailed NSBCC interventions.
Keywords: 1000 days, child nutrition, infant and young child feeding, IYCF, NSBCC, nutrition BCC, nutrition education, nutrition social behaviour change communication
Key messages
Some nutrition social behaviour change communication (NSBCC) interventions significantly improved exclusive breastfeeding (EBF) practices and child anthropometric outcomes and need to be considered while planning child nutrition interventions.
Studies used different intervention protocols and operational definitions. Most studies employed a mix of the NSBCC interventions often with unspecified frequency and dosage.
Future intervention studies should provide detailed implementation strategies for NSBCC interventions and use standard indicators to measure child nutritional status outcome indicators.
1. INTRODUCTION
Nutrition, a fundamental driver of sustainable development goals (SDG), is crucial to achieve both nutrition specific and nutrition sensitive goals and targets (UNSCN, 2015). Child undernutrition rates have declined globally but still continue to be unacceptably high and disproportionately affect the low and middle‐income countries (Development Initiatives, 2018; UN, 2015). Malnutrition in infancy is associated with impaired cognitive, physical, and metabolic functions, leading to poor mental development and school achievement and behavioural abnormalities (Martins et al., 2011). Child undernutrition increases the risk of cardiovascular diseases in adulthood (Victora et al., 2008). There is now tremendous opportunity to accelerate actions to improve child nutrition given the unprecedented and sustained global momentum for nutrition. The UNICEF conceptual framework of malnutrition shows a wide range of determinants at immediate, underlying and basic levels (UNICEF, 2013) which are interrelated and multi‐dimentional, across many sectors, making nutrition a multisector responsibility (Bhutta et al., 2013; Keats et al., 2021; Ruel & Alderman, 2013).
Social behaviour change communication (SBCC) is defined as an integrated approach that improves health outcomes through processes that foster community dialogue and action, strengthen social contexts and systems that underpin health, and sustain healthful individual and group behaviours. The SBCC encompasses three complementary domains: (1) communication using community appropriate and preferred channels of communication to address community health needs, (2) behaviour change to facilitate and maximise health actions, and (3) social change to achieve shifts that enable communities' engagement and participation in health interventions and/or policies (Remsberg, 2021). The SBCC interventions focusing on nutrition, that is, nutrition SBCC (NSBCC), are critical in addressing infant and young child feeding (IYCF) and child anthropometric outcomes. The NSBCC interventions combine elements of interpersonal communication, social change and community mobilization activities, mass media, and advocacy to support individuals, families, communities, institutions, and countries to adopt and maintain high‐impact nutrition‐related practices (SPRING, 2019). The ‘first 1000 days of life’ from conception till 2 years of age, are considered particularly crucial for child development (Victora et al., 2008), and thus have been a particular focus of the NSBCC interventions.
Although previous studies including systematic reviews have identified effectiveness of the NSBCC interventions in improving nutritional status and IYCF practices among children under 2 years of age (Arikpo et al., 2018; Caulfield et al., 1999; Dewey & Adu‐Afarwuah, 2008; Graziose et al., 2018; Lamstein et al., 2014; Sanghvi et al., 2017; Shi & Zhang, 2010), important gaps exist in evidence. For instance, the World Health Organization (WHO) defined eight core IYCF indicators in 2008 including early initiation of breastfeeding (EIBF), exclusive breastfeeding (EBF), continued breastfeeding, introduction of complementary food, minimum dietary diversity (MDD), minimum meal frequency (MMF), minimum acceptable diet, consumption of iron‐rich or iron‐fortified foods (WHO, 2008). However, even after the standard indicators were defined, there have been very limited systematic reviews and/or meta‐analysis that use these core indicators to report the impact on IYCF. Hence, the reported effectiveness on the IYCF outcomes has been varied and the results difficult to compare.
Previous systematic reviews with meta‐analysis that looked at the impact of nutrition education and/or NSBCC on child growth differed in terms of study designs, intervention dose and intensity, and reported anthropometric measures, leading to contradictory and/or inconclusive results: one reported a modest effect (Dewey & Adu‐Afarwuah, 2008), four reported a significant impact (Girard & Olude, 2012; Imdad et al., 2011; Lassi et al., 2013; Panjwani & Heidkamp, 2017), and two reported limited or no impact (Arikpo et al., 2018; Gresham et al., 2014). Additionally, not all systematic reviews have consistently assessed the robustness and quality of included studies (Arikpo et al., 2018; Dewey & Adu‐Afarwuah, 2008; Graziose et al., 2018), while others have excluded non‐peer‐reviewed publications (Lamstein et al., 2014) and quasi‐experimental studies (Arikpo et al., 2018) and limited their analyses to nutrition education and mass media intervention (Graziose et al., 2018). These limitations do not allow for comparative analyses of the effectiveness of the NSBCC interventions and their approaches. Therefore, the aim of our study was to assess the robustness of the NSBCC intervention designs and their effectiveness on child nutrition indicators reflected in the Sustainable Development Goals (SDGs) 2, SDG target 2.2 as well as the key IYCF indicators that are important for child nutritional outcomes. The NSBCC approaches employed by each study were also closely examined to understand what works for each outcome. We anticipate that our study findings will provide a comprehensive understanding on the impact of the NSBCC interventions and will inform policies and programmes.
2. METHODS AND MATERIALS
This study was performed and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) guidelines for systematic reviews (Moher et al., 2009).
2.1. Search strategy
EBSCOhost as an umbrella database for Medline (Ovid) and CINAHL as well as EMBASE and ProQUEST databases were searched for peer‐reviewed articles covering the period from January 1960 to October 2018. The search strategy, as below, was used for all databases. Full search syntax is provided in Supporting Information Material 1:
(“Pregnant and Lactating women” OR famil* OR communit* OR household*)
AND
(Nutrition education OR “Behavior Change communication)”
AND
(“Child nutrition status” OR Stunt* OR Underweight* OR Wast* OR “Child Body Mass Index” OR “Child undernutrition” OR breastfe* OR “exclusive breastfeeding” OR “complementary feeding” OR “supplementary feeding” OR “diet diversity” OR “infant and young child feeding”)
AND
(“randomised control trial” OR “cluster randomised” OR “quasi experiment” OR “quasi‐experiment”)
Reference list of included studies were further screened to identify any additional relevant papers. Furthermore, references in other systematic reviews that specifically focused on nutrition education or behaviour change communication for complementary feeding in developing countries were also reviewed. The International Clinical Trial Registry Platform of the WHO was also searched. The clinical trials registry search included—bringing together 15 national and regional clinical trial registries, with a combined data access to more than 200,000 trials.
Internet searches were conducted in resources repository within the websites of 29 organisations: Action Against Hunger (ACF), Alive and Thrive, Bill and Melinda Gates Foundation, Center for Disease Control and Prevention (CDC), Children's Investment Fund Foundation (CIFF), Food and Agriculture Organisation (FAO), Food and Nutrition Technical Assistance, Global Alliance for Improved Nutrition, Helen Keller International (HKI), IFAD, International Food Policy Research Institute (IFPRI), International Atomic Agency, John Snow Inc. (JSI), MANOFF Group, MQSUN, Nutrition Innovation Lab (NIL), PATH, Renewed Efforts Against Child Hunger and undernutrition (REACH), Results for Development (R4D), Save the Children, SPRING, Scaling Up Nutrition (SUN), United Nations Children's Fund (UNICEF), UNHCR, URC‐University Research Centre, World Bank, World Food Programme (WFP), World Health Organisation (WHO), and World Vision International (WVI).
Individuals and organisations working on nutrition in developing countries were contacted for any additional studies.
2.2. Inclusion and exclusion criteria
Studies were included if they met the following criteria: (i) original randomised controlled trials (RCTs), or quasi‐experimental studies with a primary focus on at least one separate experimental arm that addresses NSBCC activities and/or nutrition education (promotion of breastfeeding plus quantity, quality and frequency of complementary feeding) and with child nutritional status and/or IYCF indicators as outcome variables among children under 2 years of age (or within the first 1000 days); (ii) peer reviewed papers and grey literature published in English language and available in full text; (iii) conducted in low and middle income countries (including both lower middle and upper middle income categories) based on the World Bank country classification by income level (World Bank, 2018).
Studies were excluded if: (i) they were not RCTs or quasi experimental studies; (ii) were reviews, editorials, letters, perspectives, commentaries, reports, study/review protocols or studies with ‘insufficient related data’; (iii) conducted in high income countries (World Bank, 2018); (iv) nutrition education or behaviour change component that primarily focused on the promotion or uptake of food supplementation or lipid‐based nutrient supplementation or multiple micronutrient supplementation; (v) focused only on neonatal outcomes (with only exclusive breastfeeding outcomes as a possible indicator); (vi) focused on overweight/obesity and noncommunicable diseases.
2.3. Study selection and data extraction
All retrieved studies were exported to Endnote libraries by two researchers. Titles and abstract were screened for relevance by two researchers (SU & NW). Those deemed not relevant were excluded. Abstracts and full texts were then reviewed independently by two researchers (SU & NW) for inclusion. Any discrepancies related to inclusion were resolved through discussion. One researcher (SU) identified additional relevant studies from other sources which were reviewed by all authors and concurred for inclusion. A standard data extraction format was developed. One researcher (SU) extracted data from all included studies. A random subsample of 40% of included articles were extracted by the second researcher (NW) to ensure accuracy and completeness of data extraction procedure.
2.3.1. Data analysis
Study summary
Findings have been synthesized to provide a narrative summary of study characteristics and study effectiveness. The analysis was iterative and involved continuously reading the included studies to familiarise with and recheck the content. Three broad categorisation of SBCC approaches and the subapproaches or activities within each category recommended by SPRING 2014 were adapted and used as follows: interpersonal communication (one‐on‐one counseling, group education, support groups); use of media (mass media, community radio/video, local billboards, brochures, posters, flyers, newsletters, calendars, reminder cards, songs, drama, cooking demonstration, and social media); and community/social mobilization (campaigns, events, celebrations, special days, rallies, and issue groups) (Lamstein et al., 2014).
Statistical analysis
A meta‐analysis was performed to examine the effectiveness of nutritional interventions on IYCF practices (i.e., EIBF, EBF, and MDD), and their impacts on child growth (i.e., height for age z‐scores, HAZ; weight for height z‐scores, WHZ; and weight for age z‐scores, WAZ). Dichotomous data were reported as odds ratios (ORs) or prevalence ratios (PR) with 95% confidence interval (CI) and continuous data as the standardized mean differences with 95% CIs. Data were pooled using a random‐effects models, whereas the high heterogeneity was detected between studies (I 2 > 50%) (Higgins & Thompson, 2002), with a sensitivity analysis to examine the effects of outliers. Heterogeneity was identified through visual inspection of the forest plots and also considered the I 2 statistic, which quantifies the heterogeneity of the data in studies contained. Furthermore, publication bias was assessed using the Begg's test (Begg & Mazumdar, 1994) and Egger's test (Egger et al., 1997). Both of the tests are commonly used to measure the tendency for the effects estimated in small sample size studies to differ from those estimated in larger studies. The risk of publication bias was analysed in terms of EIBF, EBF, MDD, HAZ, WHZ, and WAZ. Subgroup and meta‐regression analyses were employed to investigate the effectiveness of interventions on IYCF practices and child growths, where moderate or higher heterogeneity was reported (Knapp & Hartung, 2003; Sharp, 1998). Finally, a permutation test was performed based on Monte Carlo simulation by controlling the risk of spurious findings from meta‐regression (Higgins & Thompson, 2004), wherein unadjusted and adjusted estimation procedures were also used to calculate probability values (p values) in meta‐regression. In a permutation test, the covariates were randomly reallocated to the outcomes for 1000 times to adjust for multiple testing.
2.4. Assessment of risk of bias in included studies
‘Risk of bias’ assessment tool of Cochrane Handbook for Systematic Reviews of Interventions was used to assess the risks of bias of all included studies (The Cochrane Public Health Group, 2011). It encompassed the following domains: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting, and adequate protection against contamination. Our assessment of risk of bias of the included studies also involved reviewing study protocols where available and previous papers if they were cross referenced for details on the study designs. The risk of bias assessment was carried out by two researchers. One researcher (SU) conducted risk of bias assessment for all studies and a sample of 10% of studies was simultaneously and independently assessed by the second researcher (NW) for congruence and accuracy.
3. RESULTS
3.1. Search overview
Database search yielded 1201 publications. After removing 289 duplicates, 834 abstracts were reviewed based on inclusion/exclusion criteria, of these, 63 papers were retained for full text review. Finally, 47 studies met the study inclusion criteria. Thirty‐one additional peer reviewed papers were identified from searching the reference lists of retained papers and through contacting individuals and organization. Two studies identified from the grey literature also met the inclusion criteria, giving a final sample of 80 papers for review. The PRISMA flowchart is provided in Figure 1.
Figure 1.
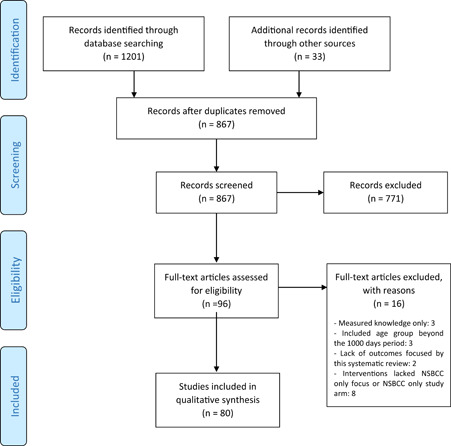
PRISMA flow chart
3.2. Risk of bias in included studies
The summary of risk of bias of the included studies is given (Appendix Figure A1). The detailed ‘risk of bias’ assessment of each study is provided in Supporting Information Material 2. Due to the nature of the NSBCC interventions, blinding of participants was reported to be difficult, with less than half of the RCTs and cluster randomised trials including some forms of blinding. This increased the risk of bias, especially for the self‐reported outcome measures. More than three quarters of the included studies had low risk of attrition bias and retention rate was 80% or more in both intervention and control arms. Similarly, more than three quarters of the studies accounted for losses to follow‐up.
3.3. Study characteristics
Fifty‐one (64%) studies were cluster randomised trials, 13 (16%) were RCTs and 16 (20%) were quasi‐experimental with or without control groups (Supporting Information Material 3). Thirty‐eight (48%) studies were from Asia, 35 (44%) from Africa, 6 (8%) from South America and 1 (1%) from Europe (Belarus). The highest number of the included studies were conducted in Bangladesh 14 (17%) followed by India 9 (11%) from Asia; and 4 (5%) each in Malawi and Uganda from Africa. Majority of studies, 56 (70%), were conducted in rural community setting. Around a third were conducted in various urban contexts: urban community, 10 (13%), urban health center, 8 (10%), and urban/peri‐urban slum, 3 (4%). The remaining 3 (4%) studies were conducted in multicountry settings. Only 1 (1%) conducted before 1999 met the inclusion criteria. Forty‐six (58%) studies were conducted during the MDG period of 2000–2015, while the remaining 33 (41%) studies were conducted from 2016 onwards, that is, during the SDG era. Detailed characteristics of each study is provided (Appendix Tables A1–A2).
3.4. Intervention characteristics, their impacts on IYCF practices and the associated NSBCC approaches
We focused on four of the core IYCF indicators recommended by the WHO: EIBF, EBF, MDD, and MMF as they were most commonly reported across the included studies and also being key indicators from a programmatic point of view. Of the 80 included studies, 22 (27%) reported on EIBF, 38 (47%) on EBF, 29 (36%) on MDD, and 21 (26%) on MMF. Results of the meta‐analysis and systematic review are presented below. A summary of the NSBCC approaches and their effect on the four standard IYCF outcomes by study designs are given (Appendix Table A1). The specific changes and effect sizes for the measured indicators by each included study are provided (Supporting Information Material 4).
3.4.1. Early initiation of breastfeeding
Out of the 22 studies reporting on EIBF, 14 (64%) found a statistically significant positive impact. Among all included studies across all designs: none of the RCTs measured or reported on EIBF; 15 out of the 51 (29%) RCTs measured and reported on EIBF, of which, 7 (47%) reported statistically a significant positive impact (Ara et al., 2018; Bhandari et al., 2003; Engebretsen et al., 2014; Flax et al., 2014; Haider et al., 2000; Kim et al., 2018; Menon et al., 2016; Waiswa et al., 2015); and 7 (47%) did not report any significant effect (Lewycka et al., 2013; More et al., 2017; Nguyen et al., 2017; Nikièma et al., 2017; Penfold et al., 2014; Saville et al., 2018; Tomlinson et al., 2014). One cluster randomised controlled trial was a multicountry which found a significant positive effect in two countries (Burkina Faso and Uganda) while no significant effect in one country (South Africa) (Engebretsen et al., 2014). Seven out of 16 (44%) quasi‐experimental studies measured and reported on EIBF and of those seven studies, 6 (86%) reported a statistically significant positive impact (Dougherty et al., 2018; Guldan et al., 2000; Kim et al., 2016; Kushwaha et al., 2014; Lamstein et al., 2018; Saggurti et al., 2018); and one did not find any significant effect (Singh et al., 2018).
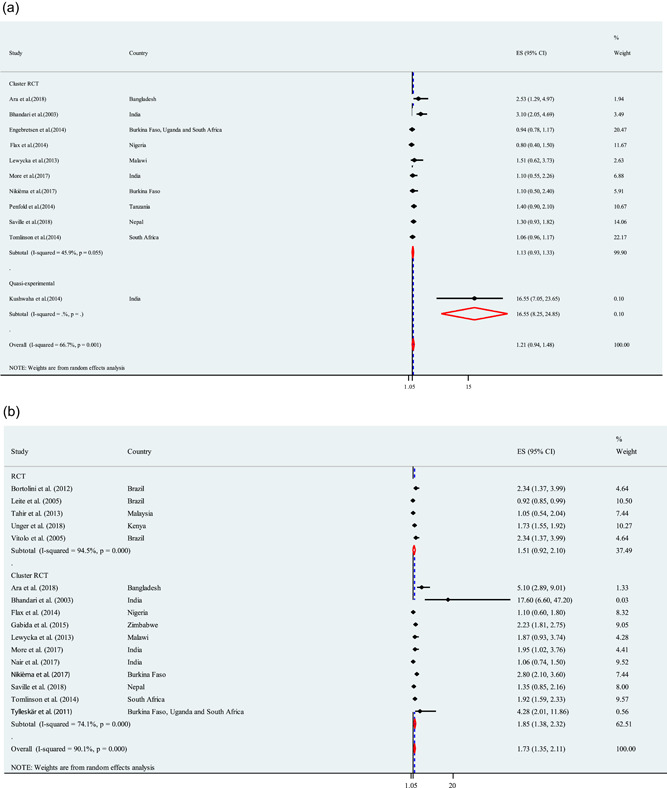
Overall, almost two‐thirds of the studies reported a significant positive effect on EIBF. The studies were of varying durations ranging from less than 6 months to more than 2 years. However, the length of studies—whether short or long—seemed to have no association with the outcome effect. Some studies that reported positive impact had employed interpersonal counselling during home visits and/or group learning approaches at communities while others used varying combination of additional NSBCC elements including use of media (IEC materials, mass media) and community mobilization. However, some studies using the similar approach, and/or their combinations did not find any significant effect (Appendix Table A1). The forest plot for EIBF is shown in Figure 2a. The odds of EIBF in the NBCC component were 21% higher than the placebo or control group, with the true population effect between −6% and 48%. This result was not statistically significant. Most of the studies found limitted positive effects on EIBF, and some even had negative effects. However, the studies were moderate heterogeneous with respect to intervention (I 2 = 66.7%; p = 0.001), preventing analysis among similar studies.
Figure 2.
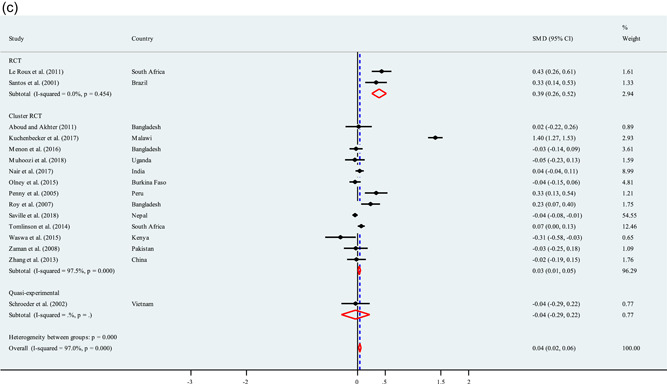
(a) Effect of intervention on EIBF. (b) Effect of interventions on EBF. (c) Effect of interventions on MDD. (d) Effect of interventions on MMF. EBF, exclusive breastfeeding; EIBF, early initiation of breastfeeding; MDD, minimum dietary diversity; MMF, minimum meal frequency
3.4.2. Exclusive breastfeeding
Of the 38 studies reporting on EBF, 33 (87%) found a statistically significant positive impact (Appendix Table A1). All studies across all study designs: six out of 13 (46%) RCTs measured or reported on EBF and of these, 5 (83%) found a significant positive effect (Aidam et al., 2005; Bortolini & Vitolo, 2012; Leite et al., 2005; Unger et al., 2018; Vitolo et al., 2005); and one RCT did not find any significant effect (Tahir & Al‐Sadat, 2013). Twenty‐two out of the 51 (43%) cluster randomised trials measured and reported on EBF and of these, 20 (91%) reported a statistically significant positive impact (Ara et al., 2018; Arifeen et al., 2009; Bhandari et al., 2003; Engebretsen et al., 2014; Flax et al., 2014; Gabida et al., 2015; Greenland et al., 2016; Haider et al., 2000; Kang et al., 2017; Kim et al., 2018; Le Roux et al., 2014; Lewycka et al., 2013; Menon et al., 2016; More et al., 2017; Nguyen et al., 2017; Nikièma et al., 2017; Tomlinson et al., 2014; Tylleskär et al., 2011; Waiswa et al., 2015; White et al., 2016); and 2 (9%) did not find any significant effect (Nair et al., 2017; Saville et al., 2018). Ten out of 16 (62%) quasi‐experimental studies measured and reported on EBF and of these 10 studies, 8 (80%) reported a statistically significant positive impact (Aristiati Guldan et al., 2000; Kim et al., 2016; Kimani‐Murage et al., 2016; Kushwaha et al., 2014; Lamstein et al., 2018; Saggurti et al., 2018; Susiloretni et al., 2013; Younes et al., 2015); while 2 (20%) did not report any significant effect (Brasington et al., 2016; Dougherty et al., 2018).
Overall, almost all studies reported a significant positive effect on EBF. Similar to EIBF, the length of the studies that reported EBF also varied from less than 6 months to more than 2 years and the duration seemed to have no association with outcome effect (Appendix Table A1). Some studies reporting positive impact employed interpersonal counselling during home visits and/or group learning approaches at communities while others used varying combination with additional NSBCC elements including use of media (IEC materials, mass media, phone messaging) and community mobilization. However, few studies using the same approach, and/or their combinations did not find significant effect. Nineteen studies measured and reported on both EIBF and EBF, five of which found impact on EBF but not on EIBF (Lewycka et al., 2013; More et al., 2017; Nguyen et al., 2017; Nikièma et al., 2017; Tomlinson et al., 2014) while 12 found impact on both (Ara et al., 2018; Bhandari et al., 2003; Flax et al., 2014; Guldan et al., 2000; Haider et al., 2000; Kim et al., 2016, 2018; Kushwaha et al., 2014; Lamstein et al., 2018; Menon et al., 2016; Saggurti et al., 2018; Waiswa et al., 2015); one documented impact on EIBF but not on EBF (Dougherty et al., 2018) and one that had no impact on both (Saville et al., 2018). It appears that between the two standard indicators of breastfeeding, the NSBCC was likely to have more positive impact on EBF.
The overall effects of interventions on EBF is reported in forest plot (Figure 2b). The meta‐analysis found that NSBCC interventions on EBF was 1.73 times significantly higher among mothers in intervention group compared with thier counterparts (placebo or control group) (OR = 1.73; 95% CI: 1.35–2.11, p < 0.001). Heterogeneity was present in this analysis (I 2 = 90.1%, p < 0.001), however, CI of some of the studies overlap to some degree.
3.4.3. Minimum dietary diversity
Of the 29 studies reporting on MDD, 23 (79%) found a statistically significant positive impact (Appendix Table A1). All studies across all study designs: one of the RCTs measured and reported a significant positive effect on MDD (Negash et al., 2014); 21 out of the 51 (41%) cluster randomised trials measured and reported on MDD and of these, 16 (76%) reported a statistically significant positive impact (Aboud & Akhter, 2011; Aboud et al., 2013; Gelli et al., 2018; Jannat et al., 2018; Kang et al., 2017; Kim et al., 2018; Kuchenbecker et al., 2017; Menon et al., 2016; More et al., 2017; Nair et al., 2017; Nikièma et al., 2017; Rawat et al., 2017; Shi et al., 2010; Waswa et al., 2015; White et al., 2016; Zhang et al., 2013); and 5 (24%) did not report any significant effect (Byrd et al., 2018; Campbell et al., 2016; Olney et al., 2015; Rockers et al., 2018; Saville et al., 2018). Seven out of the 16 (44%) quasi‐experimental studies measured and reported on MDD and of them, 6 (86%) reported a statistically significant positive impact (Kilaru et al., 2005; Kim et al., 2016; Lamstein et al., 2018; Mukuria et al., 2016; Pachon et al., 2002; Singh et al., 2018).
Overall, more than two‐thirds of the studies reported a significant positive effect on MDD. Duration of the interventions on MDD varied from less than 6 months to more than 2 years does not seem to be strongly associated with positive or no effect. The NSBCC tools and/or approaches employed were interpersonal counselling and/or group learning sessions or in combination with use of media (IEC materials, cooking demonstration promoting locally available foods, mass media) and community mobilisation. Few studies employing similar approaches however did not find any significant impact. The overall effects of interventions related to NSBCC found a positive effect on MDD (PR = 1.17; 95% CI: 0.61–1.73) (Figure 2c), however, this association was not statistically significant.
3.4.4. Minimum meal frequency (MMF)
Of the 21 studies reporting on MMF, 17 (81%) reported a statistically significant positive impact (Appendix Table A1). All studies across all study designs: one RCT measured and reported a significant positive effect on MMF (Negash et al., 2014); sixteen out of the 51 (31%) cluster randomised trials measured and reported on MMF and of these 12 (75%) reported a statistically significant positive impact (Arifeen et al., 2009; Bhandari et al., 2004; Jannat et al., 2018; Kuchenbecker et al., 2017; Menon et al., 2016; Nair et al., 2017; Nikièma et al., 2017; Roy et al., 2005, 2007; Shi et al., 2010; Waswa et al., 2015; Zhang et al., 2013); and four did not report any significant impact (Byrd et al., 2018; Kim et al., 2018; More et al., 2017; Rawat et al., 2017). Four out of the 16 (25%) quasi‐experimental studies measured and reported on MMF and all of them (100%) reported a statistically significant positive impact (Kilaru et al., 2005; Kim et al., 2016; Lamstein et al., 2018; Mukuria et al., 2016).
Overall, more than two‐thirds of the studies reported a significant positive effect on MMF too. Similar to MDD, the duration of intervention seemed to vary from less than 6 months to more than 2 years. However, the length of studies—whether short or long—seemed to have no association with the outcome effect. The NSBCC tools and/or approaches employed were interpersonal counselling and/or group learning sessions or in combination with use of media (IEC materials, cooking demonstration promoting locally available foods, mass media) and community mobilization activities. Few studies employing similar approaches however did not find any significant impact on MMF. The overall effects of interventions on MMF (prevalence ratio, PR = 2.62; 95% CI: 0.80‐4.45) (Figure 2d) was not statistically significant.
3.4.5. MDD and MMF
Fourteen out of the 80 (17%) studies measured both MDD and MMF (Byrd et al., 2018; Jannat et al., 2018; Kilaru et al., 2005; Kim et al., 2016, 2018; Kuchenbecker et al., 2017; Lamstein et al., 2018; Menon et al., 2016; Mukuria et al., 2016; Nair et al., 2017; Negash et al., 2014; Nikièma et al., 2017; Waswa et al., 2015; Zhang et al., 2013). Out of these, 12 (86%) found a significant positive impact on both MDD and MMF (Jannat et al., 2018; Kilaru et al., 2005; Kim et al., 2016; Kuchenbecker et al., 2017; Lamstein et al., 2018; Menon et al., 2016; Mukuria et al., 2016; Nair et al., 2017; Negash et al., 2014; Nikièma et al., 2017; Waswa et al., 2015; Zhang et al., 2013); while one study found a significant positive impact only on MDD (Kim et al., 2018); there were none that had significant positive impact only on MMF and one study did not have any significant impact on both (Byrd et al., 2018). It appears that NSBCC is likely to have significant positive effects on both MDD and MMF.
3.5. Intervention characteristics, their impacts on child nutritional status and the associated NSBCC tools
Our study focused on six standard indicators of child nutritional status among children less than 2 years of age (stunting, wasting, underweight, LAZ/HAZ [referred as only HAZ from here onward], WLZ/WHZ [referred only as WHZ from here onward] and WAZ [Appendix Table A2]). Of the 80 included studies, 26 (32%) reported on HAZ, 23 (29%) reported on WHZ score, 27 (34%) reported on WAZ, 20 (25%) reported on stunting, 14 (17%) reported on wasting and 11 (14%) reported on underweight. Results of the meta‐analysis (conducted for HAZ, WHZ, and WAZ) and systematic review are presented below. A summary of their impact by study designs and the associated NSBCC tools are presented in Appendix Table A2. The specific changes and effect sizes for the measured indicators by each included study are given in Appendix Table A2.
3.5.1. Height for age z‐scores
Of the 26 studies that reported on HAZ, 9 (35%) found a statistically significant positive impact. All studies across the study designs: two out of the 13 (15%) RCTs measured or reported on HAZ and both did not find any significant positive impact (Santos et al., 2001; Seetha et al., 2018); 22 out of the 51 (43%) cluster randomised trials measured and reported on HAZ and of these 22 studies, 7 (32%) reported a statistically significant positive impact (Gelli et al., 2018; Marquis et al., 2018; Penny et al., 2005; Roy et al., 2007; Ruel et al., 2008; Tomlinson et al., 2014; Vazir et al., 2013); and 14 did not report any significant effect (Aboud et al., 2013; Arifeen et al., 2009; Bhandari et al., 2004; Engebretsen et al., 2014; Kuchenbecker et al., 2017; Menon et al., 2016; Muhoozi et al., 2018; Nair et al., 2017; Rockers et al., 2018; Saville et al., 2018; Singla et al., 2015; Waswa et al., 2015; Zaman et al., 2008; Zhang et al., 2013); and one reported a significant negative effect (Fadnes et al., 2016). Two out of the 16 (12%) quasi‐experimental studies measured and reported on HAZ and both (100%) reported a statistically significant positive impact (Guldan et al., 2000; Schroeder et al., 2002).
Overall, more than one‐third of the studies reported a significant positive impact on HAZ. There is no evidence of significant positive effect from RCTs, around a third of the cluster randomised trials reported a significant positive effect while the significant positive effect from quasi‐experimental studies was based on two studies only. Most of the studies reporting a significant positive effect were conducted for a period of 6 months to 1 year, while most of the longer duration studies did not report any significant effect and study duration of less than 6 month either did not report any impact or reported a negative impact. The studies reporting a significant positive effects on HAZ used interpersonal counselling and/or group learning sessions or in combination with other tools such as use of media (IEC materials, cooking demonstration promoting locally available foods, mass media) and community mobilization activities. However, studies that did not find any impact also employed same or similar approaches. Hence, it is difficult to associate any particular NSBCC tool or approach with improvement in HAZ.
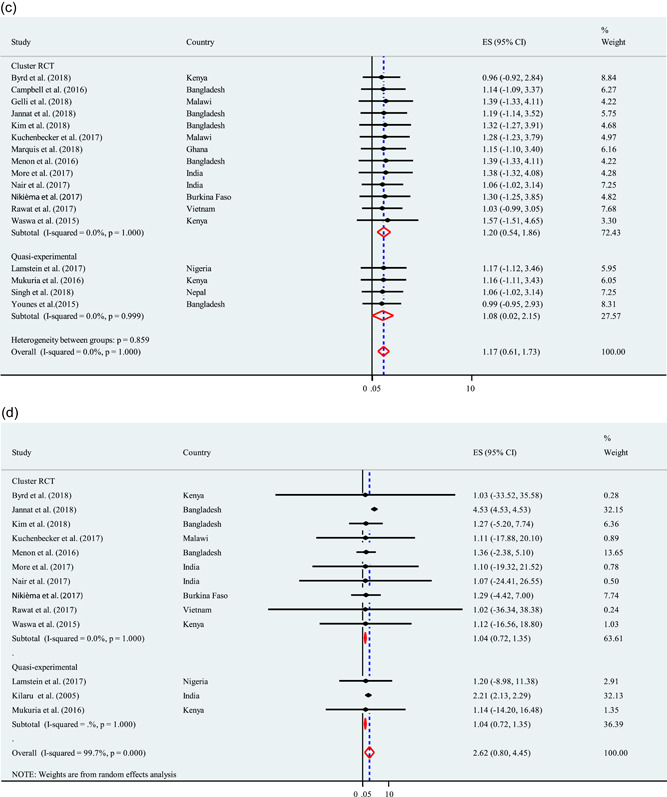
The meta‐analysis showed that NSBCC intervention had a significance positive effect on HAZ (SMD = 0.19; 95% CI: 0.17‐0.21; p < 0.001; Figure 3a). A considerable heterogeneity was present in this analysis (I 2 = 99.5%).
Figure 3.
(a) Effects of interventions on HAZ. (b) Effects of interventions on WHZ. (c) Effects of interventions on weight for WAZ. HAZ, height for age z‐scores; WAZ, weight for age z‐scores; WHZ, weight for height z‐scores
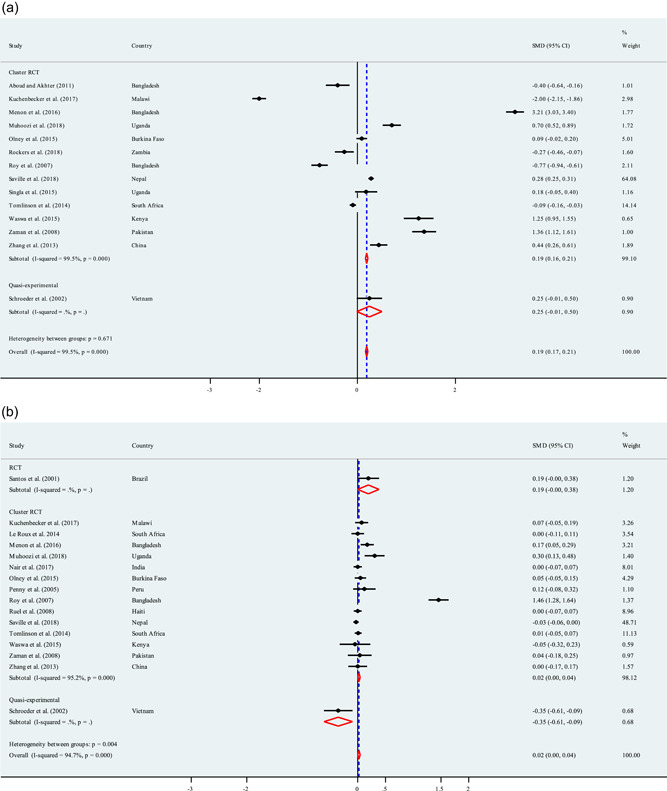
3.5.2. Weight for height z‐scores
Of the 23 studies that reported WHZ, 6 (26%) found a statistically significant positive impact (Appendix Table A2). All studies across the study designs: two out of the 13 (15%) RCTs measured or reported on WHZ and among them, one reported a significant positive impact (Seetha et al., 2018) while another did not find any significant impact (Santos et al., 2001). Nineteen out of the 51 (37%) cluster randomised trials measured and reported on WHZ and of these 19 studies, 4 (21%) reported a statistically significant positive impact (Penny et al., 2005; Ruel et al., 2008; Zaman et al., 2008; Zhang et al., 2013). One multicountry randomised controlled trial documented a positive impact in one country (South Africa) but a statistically significant negative impact in two countries (Burkina Faso and Uganda) (Engebretsen et al., 2014). Fourteen out of 19 studies (74%) did not report any significant positive impact (Arifeen et al., 2009; Gelli et al., 2018; Kuchenbecker et al., 2017; Le Roux et al., 2014; Marquis et al., 2018; Menon et al., 2016; Muhoozi et al., 2018; Nair et al., 2017; Nikièma et al., 2017; Roy et al., 2007; Saville et al., 2018; Tomlinson et al., 2014; Vazir et al., 2013; Waswa et al., 2015). Two out of the 16 (12%) quasi‐experimental studies measured and reported on WHZ and both (100%) did not report any significant impact (Guldan et al., 2000; Schroeder et al., 2002).
Overall, less than a third of studies reported a significant positive effect on WHZ while the majority of the included studies did not find any significant positive impact, across the three study designs. Duration of the intervention does not seem to have much association with any significant effects on WHZ also. The studies reporting significant positive effects on WHZ used interpersonal counselling and/or group learning sessions or in combination with use of media (IEC materials, cooking demonstration promoting locally available foods, mass media) and community mobilization activities. Most studies reporting significant positive effect included cooking demonstration promoting local foods. However, majority of studies that did not find any impact had also employed same or similar approaches. Hence, it is difficult to strongly associate any particular NSBCC tool or approach with improvement in WHZ.
The meta‐analysis show a significance impact of the NBCC, with WHZ significantly increasing by 0.02 units (SMD = 0.02; 95% CI: 0.001–0.04; p < 0.001; Figure 3b), whereas a considerable heterogeneity was noticed among these studies (I 2 = 94.7%).
3.5.3. Weight for age z‐scores
Of the 27 studies that reported WAZ, 14 (52%) found a statistically significant positive impact (Appendix Table A2). All studies across the study designs: five out of the 13 (38%) RCTs measured or reported on WAZ and among these, 3 (60%) reported a significant positive impact (Brown et al., 1992; Le Roux et al., 2011; Seetha et al., 2018); one reported no significant impact (Santos et al., 2001) while one reported a significant negative impact (Jakobsen et al., 2008). Twenty out of the 51 (39%) RCTs measured and reported on WAZ and of them, 9 (45%) reported a statistically significant positive impact (Marquis et al., 2018; Penny et al., 2005; Roy et al., 2005, 2007; Ruel et al., 2008; Waswa et al., 2015; Zaman et al., 2008; Zhang et al., 2013); and 9 (45%) did not report any significant effect (Bhandari et al., 2004; Gelli et al., 2018; Kuchenbecker et al., 2017; Le Roux et al., 2014; Menon et al., 2016; Muhoozi et al., 2018; Nair et al., 2017; Saville et al., 2018; Vazir et al., 2013); while one multicountry study documented no significant impact in two countries (Burkina Faso and South Africa) but a statistically significant negative impact in one country (Uganda) (Engebretsen et al., 2014); and one study reported a significant negative impact (Fadnes et al., 2016). Two out of the 16 (12%) quasi‐experimental studies measured and reported on WAZ and both reported a statistically significant positive impact (Guldan et al., 2000; Schroeder et al., 2002).
Consistent with the overall effects of intervention, an increase in WAZ of 0.04 (SMD = 0.04; 95% CI: 0.02–0.06; p < 0.001; Figure 3c). Our analysis showed that a high heterogeneity (I 2 > 75%) was also observed for meta‐analysis (97%) in terms of WAZ.
3.5.4. Stunting
Of the 20 studies that reported stunting, 7 (35%) found a statistically significant positive impact (Appendix Table A2). Among all included studies across the study designs: 1 (8%) of the 13 RCTs had measured and reported on stunting and it did not find any significant impact (Bhandari et al., 2001); 17 out of 51 (33%) of the RCTs had measured or reported on stunting and of those 17 studies, 6 (35%) reported a significant positive impact (Gelli et al., 2018; Penny et al., 2005; Rockers et al., 2018; Ruel et al., 2008; Saleem et al., 2014; Zhang et al., 2013); 9 (53%) did not report any significant effect (Aboud et al., 2013; Arifeen et al., 2009; Bhandari et al., 2003; Engebretsen et al., 2014; Menon et al., 2016; Nair et al., 2017; Nikièma et al., 2017; Olney et al., 2015; Saville et al., 2018); and 2 (12%) reported a significant negative effect (Fadnes et al., 2016; Waswa et al., 2015). Out of 16, 2 (12%) of the quasi‐experimental studies reported on stunting and one ongoing study reported a positive effect as its midline finding (Sherburne et al., 2018) while one did not find any significant effect (Schroeder et al., 2002).
Overall, around a third of the studies reported a significant positive impact on stunting. There is no evidence of a positive significant effect from the RCTs, only around a third of the cluster randomised trials have reported the positive evidence and the significant positive effect from quasi‐experimental studies was based on one study only. Most of the studies reporting a significant positive effect were conducted for a period of 6 months to 1 year while most of the longer studies did not report any significant effect and study duration of less than 6 month either did not report any impact or reported a significant negative impact. The studies reporting a significant positive effects on stunting had used interpersonal counselling and/or group learning sessions or in combination with use of media (IEC materials, cooking demonstration promoting locally available foods and mass media). However, studies that did not find any impact had also employed same or similar approaches. Hence, it is difficult to associate any particular NSBCC tool or approach with improvement in stunting.
3.5.5. Wasting
Of the 14 studies that reported wasting, 4 (29%) found a statistically significant positive effect (Appendix Table A2). Among all included studies across the study designs: only one of the 13 RCTs measured and reported on wasting and it did not find any significant impact (Bhandari et al., 2001). Twelve out of the 51 (23%) RCTs measured or reported on wasting and of those 12 studies, 3 (25%) reported a significant positive impact (Olney et al., 2015; Ruel et al., 2008; Saleem et al., 2014); and 8 (61%) did not find any significant impact (Arifeen et al., 2009; Bhandari et al., 2003; Gelli et al., 2018; Menon et al., 2016; Nair et al., 2017; Nikièma et al., 2017; Saville et al., 2018; Waswa et al., 2015). One multicountry RCT documented no significant effect in two countries (Burkina Faso and South Africa) while a statistically significant negative impact in one country (Uganda) (Engebretsen et al., 2014). One out of the 16 (6%) quasi‐experimental studies measured and reported on wasting and it did not find any significant impact (Schroeder et al., 2002).
Overall, less than one‐third of the studies found a significant positive impact on wasting. There is no evidence of significant positive effect from the RCTs, around a third of the cluster randomised trials have reported significant positive effect and none from the quasi‐experimental studies. Duration of intervention varied between less than a year to more than 2 years which does not seem to have an association with the effect on wasting. The studies reporting a significant positive effect on wasting had used interpersonal counselling and/or group learning sessions or in combination with media (IEC materials, cooking demonstration promoting locally available foods) and community mobilisation. However, studies that did not find any impact had also employed same or similar approaches. Hence, it is difficult to associate any particular NSBCC tool or approach with improvement in wasting.
3.5.6. Underweight
Of the 11 studies that reported underweight, 3 (27%) reported a statistically significant positive effect (Appendix Table A2). Among all included studies across all study designs: none of the RCTs measured and reported on underweight; 10 out of 51 (20%) of the cluster randomised trials measured and reported on underweight and of these 10 studies, 3 (30%) reported a statistically significant positive impact (Nair et al., 2017; Ruel et al., 2008; Saleem et al., 2014); while 6 (60%) did not report any significant effect (Engebretsen et al., 2014; Gelli et al., 2018; Menon et al., 2016; Olney et al., 2015; Saville et al., 2018; Waswa et al., 2015); and one study reported a significant negative impact (Fadnes et al., 2016). One out of the 16 (12%) quasi‐experimental studies measured and reported on underweight and it did not report any statistically significant positive impact (Schroeder et al., 2002).
3.5.7. Publication bias and meta‐regression
The results of Egger's test were presented (Table 1). Publication bias was only observed in studies identified to estimate the effectiveness of interventions on EBF (p = 0.012), MDD (p < 0.001), and MMF (p < 0.001). However, the p values for the Egger's test were 0.096 (for EIBF), 0.969 (for HAZ), 0.120 (for WHZ), and 0.194 (for WAZ), respectively, denoting absent of publication bias (Table 1). To examine the sources of heterogeneity, a stratified analysis was conducted for the core IYCF indicators and standard indicators of child growth in terms of number of participants and duration on intervention (Table 2). This study found that only EIBF was significantly associated with increased duration of intervention (OR = 1.31, 95% CI: 1.22–1.41; p < 0.001) and increased number of participants (OR = 1.12, 95% CI: 1.03–1.29; p < 0.001) (Table 2).
Table 1.
Assessing publication bias
| Parameters | Number of study | Egger's testa | Begg's testb | ||||
|---|---|---|---|---|---|---|---|
| Odds ratios (OR)/Coe‐efficient (β) (95% CI) | p values | Bias (OR or β) (95% CI) | p values | Adj. Kendall's score (P‐Q)c | Continuity corrected test | ||
| EIBF | 11 | OR = 0.99 (0.89, 1.10) | p = 0.885 | OR = 1.81 (0.88, 3.72) | p = 0.096 | 13 (Z = 1.01, p = 0.312) | Z = 0.93 (p = 0.350) |
| EBF | 16 | OR = 0.94 (0.81, 1.09) | p = 0.363 | OR = 4.94 (1.51, 16.18) | p = 0.012 | −18 (Z = −0.81, p = 0.417) | Z = 0.77 (p = 0.444) |
| MDD | 17 | β = −0.83 (−0.87, −0.79) | p < 0.001 | β = 0.83 (0.80, 0.87) | p < 0.001 | 134 (Z = 5.52, p < 0.001) | Z = 5.48 (p < 0.001) |
| MMF | 13 | β = −0.45 (−0.57, −0.33) | p < 0.001 | β = 0.51 (0.41, 0.61) | p < 0.001 | 78 (Z = 4.76, p < 0.001) | Z = 4.70 (p < 0.001) |
| HAZ | 14 | β = −0.18 (−0.75, 0.38) | p = 0.494 | β = −0.22 (−12.35, 11.91) | p = 0.969 | −17 (Z = −0.93, p = 0.352) | Z = 0.88 (p = 0.381) |
| WHZ | 16 | β = 0.08 (−0.08, 0.23) | p = 0.323 | β = −2.84 (−6.52, 0.84) | p = 0.120 | 32 (Z = −1.44, p = 0.150) | Z = 1.40 (p = 0.163) |
| WAZ | 16 | β = 0.06 (−0.15, 0.28) | p = 0.532 | β = −3.01 (−7.73, 1.72) | p = 0.194 | −6 (Z = −0.27, p = 0.787) | Z = 0.23 (p = 0.822) |
Abbreviations: EBF, exclusive breastfeeding; EIBF, early initiation of breastfeeding; HAZ, height for age z‐scores; MDD, minimum dietary diversity, MMF, minimum meal frequency; WAZ, weight for age z‐scores; WHZ, weight for height z‐scores.
Egger's test for small‐study effects was performed in terms of regress standard normal deviate of effect estimate against its standard error.
Begg's test was performed to detect publication bias for small‐study effects.
Rank correlation between standardized effect estimate and its standard error.
Table 2.
Stratified analysis of the effectiveness of interventions on infant and young child feeding (IYCF) practices and anthropometric outcomes
| Parameters | Meta‐regression | Monte Carlo permutation test for meta‐regression | ||
|---|---|---|---|---|
| Pooled estimate (odds ratios, OR or coefficient, β) (95% CI) | Probability values (p values) | Unadjusted p values | Adjusted p values | |
| EIBF (n = 11 studies) | ||||
| Number of study participants | OR = 1.31 (1.22, 1.41) | <0.001 | 0.025 | 0.109 |
| Intervention duration | OR = 1.12 (1.03, 1.29) | <0.001 | 0.067 | 0.074 |
| Permutations | – | – | 1000 | |
| EBF (n = 16 studies) | ||||
| Number of study participants | OR = 0.99 (0.99, 1.00) | 0.904 | 0.776 | 0.878 |
| Intervention duration | OR = 1.02 (0.86, 1.19) | 0.640 | 0.608 | 0.752 |
| Permutations | – | – | 1000 | |
| MDD (n = 16 studies) | ||||
| Number of study participants | β = 0.002 (−0.001, 0.002) | 0.960 | 0.697 | 0.913 |
| Intervention duration | β = 0.001 (−0.046, 0.048) | 0.981 | 0.865 | 0.982 |
| Permutations | – | – | 1000 | |
| MMF (n = 12 studies) | ||||
| Number of study participants | β = 0.003 (−0.051, 0.053) | 0.958 | 0.626 | 0.847 |
| Intervention duration | β = −0.005 (−0.001, 0.001) | 0.984 | 0.682 | 0.905 |
| Permutations | – | – | 1000 | |
| HAZ (n = 14 studies) | ||||
| Number of study participants | β = −0.018 (−0.075, 0.038) | 0.493 | 0.574 | 0.745 |
| Intervention duration | β = 0.001 (−0.001, 0.002) | 0.638 | 0.607 | 0.853 |
| Permutations | – | – | 1000 | |
| WHZ (n = 16 studies) | ||||
| Number of study participants | β = −0.069 (−0.009, 0.023) | 0.372 | 0.447 | 0.520 |
| Intervention duration | β = −0.002 (−0.008, 0.006) | 0.576 | 0.408 | 0.766 |
| Permutations | – | – | 1000 | |
| WAZ (n = 16 studies) | ||||
| Number of study participants | β = 0.001 (−0.001, 0.004) | 0.223 | 0.302 | 0.311 |
| Intervention duration | β = −0.01 (−0.03, 0.01) | 0.395 | 0.231 | 0.514 |
| Permutations | – | – | 1000 | |
Abbreviations: EBF, exclusive breastfeeding; EIBF, early initiation of breastfeeding; HAZ, height for age z‐scores; MDD, minimum dietary diversity, MMF, minimum meal frequency; WAZ, weight for age z‐scores; WHZ, weight for height z‐scores.
4. DISCUSSIONS
We documented evidence on the effectiveness of the NSBCC interventions on child growth. Our study showed a significant positive effect of NSBCC on the anthropometric outcomes (HAZ, WHZ, and WAZ). These are encouraging and important findings for low and middle income countries in view of meeting the WHA and the SDG targets. We also found that more studies had reported positive impact on HAZ and stunting in comparison to WHZ and wasting, respectively. This reinforces that in addition to feeding, there are other acute factors such as childhood illnesses like diarrhea, unsafe water, poor sanitation, and hygiene that are contributing to poor growth (Li et al., 2020) indicating that the NSBCC interventions need to incorporate multisectoral health and hygiene interventions. Other authors conducting meta‐analysis on education interventions and child growth have reported varied findings. Panjwani and Heidkamp found that interventions which provide nutrition education or counselling had small but significant impact on linear growth but not on ponderal growth (Panjwani & Heidkamp, 2017). On the other hand, Lassi et al. reported similar results to ours that complementary feeding education alone resulted in significant impact on both height and length growth (Lassi et al., 2013). Few specific studies included in our review reporting significant negative impacts on child growth need to be interpreted with caution, in light of their short duration of less than 6 months (Engebretsen et al., 2014; Fadnes et al., 2016; Waswa et al., 2015) and of them, two had limited focus only on breastfeeding promotion (Engebretsen et al., 2014; Fadnes et al., 2016).
Our study results showed statistically significant positive effects of the NSBCC on EBF practices. Our findings are supported by existing literature which indicates that nutrition education or behavior change interventions significantly improve the IYCF practices (Arikpo et al., 2018; Graziose et al., 2018; Lamstein et al., 2014; Sanghvi et al., 2017; Shi & Zhang, 2010). Our meta‐analysis showed that there was overall no effect on EIBF. There could be other factors beyond knowledge and behavior that hinder EIBF, such as deep‐rooted cultural issues or issues with health service providers, which are perhaps not adequately addressed by the NSBCC approaches (Ahishakiye et al., 2020; Rujumba et al., 2020). The nonsignificant impact observed for MDD and MMF could also be due to the NSBCC approaches being used to convey messages on young children's diet were not adequate and easy for the target groups to understand. Hence, this may point towards the need to adjust some of the NSBCC approaches and to use the more effective models.
We also attempted to understand the characteristics of the studies that reported nonsignificant findings across all the outcomes. However, we could not document a consistent link either with the risk of bias elements or with other characteristics of the studies such as design, sample size or duration. Significant as well as nonsignificant results have been reported by studies with similar pattern of risk of bias and other characteristics. Furthermore, some studies investigating multiple outcomes have reported significant findings for one or more outcomes while not for other outcomes. Hence, in our synthesis of 80 studies, it is difficult to associate a particular reason or a pattern for the nonsignificant findings.
We also aimed to understand the effectiveness of NSBCC tools or approaches. For EBF, interpersonal counselling (individual and/or group) alone or in combination with the use of media (IEC materials, mass media, phone messaging) and community mobilization activities were reported to be effective in most studies. On the other hand, it was less clear for EIBF as some studies documented positive impacts using interpersonal counselling (individual and/or group) with or without additional NSBCC elements while others did not find any impact with similar approaches. For MDD and MMF, the effective NSBCC tools ranged from interpersonal counselling (individual and/or group) only or in combination with other approaches like use of media (such as IEC materials, cooking demonstration promoting locally available foods, mass media) and community mobilization activities. For child growth, it did not emerge clearly which NSBCC tools were more effective. Whilst a few studies employing tools like interpersonal counselling (individual and/or group) with or without use of media (such as IEC materials, cooking demonstration, mass media) and community mobilization activities were found to have a significant positive impact; but most studies using similar approaches did not find such impact. Given the complex multisector, multidimensional, and multi‐impact pathways of nutrition, it is also difficult to tease out the impact of NSBCC alone on growth. Overall, interpersonal counselling is the most widely used and tested approach followed by its combination with large, medium or small media while community mobilization is the least integrated NSBCC approach.
One of our objectives was also to understand what NSBCC approaches or their combinations work best to improve IYCF and child nutrition. Through this study, we were unable to understand these associations as the NSBCC tools and approaches employed were heterogeneous, with varying intervention dosage and duration and dose frequency. It also did not clearly and consistently emerge whether use of a single or multiple approaches were better to produce positive impacts on child feeding practices and nutritional status (Appendix A1 and A2).
We also looked into further details of the NSBCC interventions provided in the included studies such as dosage/intensity, delivery agent and targeted audience in terms of their impact on the outcomes. The pattern that emerged was slightly different for IYCF practices and nutritional status. For the IYCF outcomes, more studies tended to report positive impact due to higher intensity or frequency of the NSBCC interventions (for instance, at least monthly home visits by trained personnel or more frequent contact via phone messages or mass media exposure). However, some studies with the same interventions' frequency did not report any positive impact. Some of the studies demonstrating positive impact on IYCF practices had also involved other family members such as fathers and grandparents. No clear conclusions could be made whether the type of delivery agents, for instance, counselling delivered by trained personnel including peer volunteers, community health and/or nutrition workers or health workers, made any difference. With regard to child nutrition status, there was no clear or consistent pattern that emerged by intervention dosage, delivery agent, or targeted household members. Some of the included papers did not adequately provide the necessary information to distill such important nuances. Though most papers mentioned the frequency of interventions, only a few have specified the length of each interaction sessions and the household members targeted. Hence, it is important for studies to specify and clearly report the details of the implementation strategies to better understand the success factors of the NSBCC interventions (Proctor et al., 2013). Furthermore, the differences in findings between multicountry and multisetting studies point that local factors might determine the outcomes, highlighting the importance of tailoring the NSBCC approaches, tools and content to the specific contexts and places.
5. RECOMMENDATIONS
Future studies need to align with the globally standardized and harmonized indicators recommended by the WHO on IYCF (WHO, 2008) and that of the WHA and the SDG targets on child growth (UNSCN, 2015; WHO, 2014) while reporting their outcomes. This will allow comparison and to measure the difference in outcomes.
Our findings had more than half of the included studies (56%) conducted in rural setting. However, it is projected that almost 70% of the world's population will live in urban areas by 2050 (UN DESA, 2018). In view of the rapid urbanization and to embrace SDG principle of ‘leaving no one behind’, future research settings need to increasingly encompass urban and peri‐urban areas.
Future need for further robust research is also highlighted by other literatures (Arikpo et al., 2018; Girard & Olude, 2012; Graziose et al., 2018; Gresham et al., 2014; Lamstein et al., 2014; Lassi et al., 2013; Shi & Zhang, 2010). In this study, we recommend future studies to specify the exact types and combinations NSBCC interventions (e.g., interpersonal and/or group counselling with paper‐based IEC materials; or interpersonal and/or group counselling with actual demonstrations; interpersonal and/or group counselling plus IEC materials and real demonstrations with usage of digital media, etc.) as well as their exact intervention dosage and duration, and dose frequency. Future studies should also clearly specify the exact nutrition messages promoted through the interventions including quality and quantity of food, frequency of feeding, timely introduction of complementary foods, the types of meal and/or snacks foods, and so on.
Future studies should also be conducted to reflect the varying contexts—different countries or geographic locations, urban and rural, food secure, and food insecure. There is the necessity as well as the scope for innovations within all three categories of NSBCC approaches. Innovative methods need to be tested for interpersonal counselling while existing innovative media and community mobilization activities should be explored and studied for their effectiveness. Given the global galvanization of healthy diet movement and its environmental considerations by the recent EAT‐Lancet commission report (Willett et al., 2019), the promotion of locally available foods through food and/or cooking demonstrations, in particular to promote healthy diet and optimal dietary diversity, ought to be separately and robustly evaluated as a potential and key NSBCC tools for widespread use. Specific tools or learning methodologies could also be adopted from other disciplines like education (e.g., effective learning methodologies) and psychology (e.g., emotional drivers of behavior change).
6. STRENGTHS AND LIMITATIONS
Our systematic review and meta‐analysis has several strengths. It adopted a comprehensive search strategy including systematic search of appropriate databases, combing through the relevant reference lists and websites as well as reaching out to some of the concerned experts that resulted in a high number of papers identified for final inclusion. We were able to have a large pool of data as we looked through various data sources including grey literature, over a period a time. The review focused on different study designs—RCT, cluster randomised and quasi‐experimental designs that provided a scope to distill the most rigorous evidence available. To our knowledge, this review is the first of its kind to look at four of the standard IYCF indicators as recommended by the WHO, including both breastfeeding and complementary feeding, as well as standard indicators of child growth. The review findings can be generalized to rural and urban settings as well as all countries across the developing context.
Some limitations of the review process need to be outlined. We only looked at four out of the eight core indicators recommended by the WHO and our meta‐analysis was not conducted for stunting, underweight and wasting. The use of printed communication materials in the included studies may be underreported: if the studies only mentioned ‘counselling’, or ‘group learning’, we assumed that it was the only approach used while printed materials usage was included only when they were clearly stated in the study. Furthermore, we were not able to analyse the findings by dose and/or frequency of the interventions due to the heterogeneous and combined nature of the NSBCC interventions and lack of information in some studies. In addition, the potential publication biases cannot be ruled out.
7. CONCLUSIONS
Improvement in IYCF practices and child nutritional status are imperative to attain the SDGs. Findings from our study show that the NSBCC interventions improve EBF and child anthropometric outcomes. The existing evidence thus indicate the importance of the NSBCC tools while planning all child nutrition programmes. More specific and rigorous research is required to further test the impact on child nutritional status with clearly specified and detailed NSBCC interventions.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
Andre M.N. Renzaho and Stanley Chitekwe conceptualised the systematic review. Sophiya Uprety and Nidhi Wali conducted the search, data extraction and risk of bias assessment, under the supervision of Andre M.N. Renzaho and Stanley Chitekwe. Rashidul A. Mahumud and Sophiya Uprety performed the data synthesis, analysis and drafted the paper. Rashidul A. Mahumud conducted the meta‐analysis and generated the associated tables and figures, under the supervision of Andre M.N. Renzaho. Nidhi Wali, Rashidul A. Mahumud, Stanley Chitekwe, and Andre M.N. Renzaho provided inputs to finalise the draft paper. Stanley Chitekwe and Andre M.N. Renzaho provided guidance throughout the review process.
ETHICS STATEMENT
Not applicable.
Supporting information
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
ACKNOWLEDGEMENT
The research was funded by UNICEF Nepal and Western Sydney University.
Mahumud, R. A. , Uprety, S. , Wali, N. , Renzaho, A. M. , & Chitekwe, S. (2022). The effectiveness of interventions on nutrition social behaviour change communication in improving child nutritional status within the first 1000 days: Evidence from a systematic review and meta‐analysis. Maternal & Child Nutrition, 18:e13286. 10.1111/mcn.13286
*Join‐first author contribution.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- Aboud, F. E. , & Akhter, S. (2011). A cluster‐randomized evaluation of a responsive stimulation and feeding intervention in bangladesh. Pediatrics, 127(5), e1191–e1197. 10.1542/peds.2010-2160 [DOI] [PubMed] [Google Scholar]
- Aboud, F. E. , Singla, D. R. , Nahil, M. I. , & Borisova, I. (2013). Effectiveness of a parenting program in Bangladesh to address early childhood health, growth and development. Social Science and Medicine, 97, 250–258. 10.1016/j.socscimed.2013.06.020 [DOI] [PubMed] [Google Scholar]
- Ahishakiye, J. , Bouwman, L. , Brouwer, I. D. , Vaandrager, L. , & Koelen, M. (2020). Prenatal infant feeding intentions and actual feeding practices during the first six months postpartum in rural Rwanda: A qualitative, longitudinal cohort study. International Breastfeeding Journal, 15(1), 29. 10.1186/s13006-020-00275-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aidam, B. A. , Perez‐Escamilla, R. , & Lartey, A. (2005). Lactation counseling increases exclusive breast‐feeding rates in Ghana. Journal of Nutrition, 135(7), 1691–1695. 10.1093/jn/135.7.1691 [DOI] [PubMed] [Google Scholar]
- Ara, G. , Khanam, M. , Papri, N. , Nahar, B. , Haque, M. A. , Kabir, I. , & Dibley, M. J. (2018). Peer counselling improves breastfeeding practices: A cluster randomized controlled trial in urban Bangladesh. Maternal & Child Nutrition, 14(3), 1. 10.1111/mcn.12605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arifeen, S. E. , Hoque, D. E. , Akter, T. , Rahman, M. , Hoque, M. E. , Begum, K. , Chowdhury, E. K. , Khan, R. , Blum, L. S. , Ahmed, S. , Hossain, M. A. , Siddik, A. , Begum, N. , Rahman, Q. S. , Haque, T. M. , Billah, S. M. , Islam, M. , Rumi, R. A. , Law, E. , … Black, R. E. (2009). Effect of the integrated management of childhood illness strategy on childhood mortality and nutrition in a rural area in Bangladesh: A cluster randomised trial. The Lancet, 374(9687), 393–403. 10.1016/S0140-6736(09)60828-X [DOI] [PubMed] [Google Scholar]
- Arikpo, D. , Edet, E. S. , Chibuzor, M. T. , Odey, F. , & Caldwell, D. M. (2018). Educational interventions for improving primary caregiver complementary feeding practices for children aged 24 months and under. Cochrane Library, 2018(5), CD011768. 10.1002/14651858.cd011768.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begg, C. B. , & Mazumdar, M. (1994). Operating characteristics of a rank correlation test for publication bias. Biometrics, 50(4), 1088–1101. 10.2307/2533446 [DOI] [PubMed] [Google Scholar]
- Bhandari, N. , Bahl, R. , Mazumdar, S. , Martines, J. , Black, R. E. , & Bhan, M. K. (2003). Effect of community‐based promotion of exclusive breastfeeding on diarrhoeal illness and growth: A cluster randomised controlled trial. Lancet, 361(9367), 1418–1423. 10.1016/s0140-6736(03)13134-0 [DOI] [PubMed] [Google Scholar]
- Bhandari, N. , Bahl, R. , Nayyar, B. , Khokhar, P. , Rohde, J. E. , & Bhan, M. K. (2001). Food supplementation with encouragement to feed it to infants from 4 to 12 months of age has a small impact on weight gain. Journal of Nutrition, 131(7), 1946–1951. 10.1093/jn/131.7.1946 [DOI] [PubMed] [Google Scholar]
- Bhandari, N. , Mazumder, S. , Bahl, R. , Martines, J. , Black, R. E. , & Bhan, M. K. (2004). An educational intervention to promote appropriate complementary feeding practices and physical growth in infants and young children in Rural Haryana, India. Journal of Nutrition, 134(9), 2342–2348. [DOI] [PubMed] [Google Scholar]
- Bhutta, Z. A. , Das, J. K. , Rizvi, A. , Gaffey, M. F. , Walker, N. , Horton, S. , Webb, P. , Lartey, A. , Black, R. E. , & Lancet Nutrition Interventions Review Group, the Maternal and Child Nutrition Study, G . (2013). Evidence‐based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet, 382(9890), 452–477. 10.1016/s0140-6736(13)60996-4 [DOI] [PubMed] [Google Scholar]
- Bortolini, G. A. , & Vitolo, M. R. (2012). The impact of systematic dietary counseling during the first year of life on prevalence rates of anemia and iron deficiency at 12–16 months. Journal of Pediatrics, 88(1), 33–39. 10.2223/jped.2156 [DOI] [PubMed] [Google Scholar]
- Brasington, A. , Abdelmegeid, A. , Dwivedi, V. , Kols, A. , Kim, Y. M. , Khadka, N. , Rawlins, B. , & Gibson, A. (2016). Promoting healthy behaviors among Egyptian mothers: A quasi‐experimental study of a health communication package delivered by community organizations. PLOS One, 11(3), e0151783. 10.1371/journal.pone.0151783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, L. V. , Zeitlin, M. F. , Peterson, K. E. , Chowdhury, A. M. , Rogers, B. L. , Weld, L. H. , & Gershoff, S. N. (1992). Evaluation of the impact of weaning food messages on infant feeding practices and child growth in rural Bangladesh. American Journal of Clinical Nutrition, 56(6), 994–1003. 10.1093/ajcn/56.6.994 [DOI] [PubMed] [Google Scholar]
- Byrd, K. , Dentz, H. N. , Williams, A. , Kiprotich, M. , Pickering, A. J. , Omondi, R. , Kwena, O. , Rao, G. , Arnold, C. D. , Arnold, B. F. , Dewey, K. G. , Colford JM, J. r , Null, C. , & Stewart, C. P. (2018). A behaviour change intervention with lipid‐based nutrient supplements had little impact on young child feeding indicators in rural Kenya. Maternal and Child Nutrition, 15(1), e12660. 10.1111/mcn.12660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, R. K. , Hurley, K. M. , Shamim, A. A. , Shaikh, S. , Chowdhury, Z. T. , Mehra, S. , de Pee, S. , Ahmed, T. , West KP, J. r , & Christian, P. (2016). Effect of complementary food supplementation on breastfeeding and home diet in rural Bangladeshi children. American Journal of Clinical Nutrition, 104(5), 1450–1458. 10.3945/ajcn.116.135509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caulfield, L. E. , Huffman, S. L. , & Piwoz, E. G. (1999). Interventions to improve intake of complementary foods by infants 6 to 12 months of age in developing countries: Impact on growth and on the prevalence of malnutrition and potential contribution to child survival. Food and Nutrition Bulletin, 20(2), 183–200. 10.1177/156482659902000203 [DOI] [Google Scholar]
- Development Initiatives . (2018). 2018 Global Nutrition Report: Shining a light to spur action on nutrition. Bristol, UK: Development Initiatives.North Quay House, Quay Side, Temple Back, Bristol, BS1 6FL, UK. [Google Scholar]
- Dewey, K. G. , & Adu‐Afarwuah, S. (2008). Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Maternal and Child Nutrition, 4(s1), 24–85. 10.1111/j.1740-8709.2007.00124.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty, L. , Stammer, E. , Derbile, E. , Dery, M. , Yahaya, W. , Gle, D. B. , Otieno, J. , & Fotso, J. C. (2018). A mixed‐methods evaluation of a community‐based behavior change program to improve maternal health outcomes in the Upper West Region of Ghana. Journal of Health Communication, 23(1), 80–90. 10.1080/10810730.2017.1414901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger, M. , Davey Smith, G. , Schneider, M. , & Minder, C. (1997). Bias in meta‐analysis detected by a simple, graphical test. BMJ, 315(629), 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engebretsen, I. M. , Jackson, D. , Fadnes, L. T. , Nankabirwa, V. , Diallo, A. H. , Doherty, T. , Lombard, C. , Swanvelder, S. , Nankunda, J. , Ramokolo, V. , Sanders, D. , Wamani, H. , Meda, N. , Tumwine, J. K. , Ekström, E. C. , Van de Perre, P. , Kankasa, C. , Sommerfelt, H. , Tylleskär, T. , & PROMISE EBF‐Study Group (2014). Growth effects of exclusive breastfeeding promotion by peer counsellors in sub‐Saharan Africa: The cluster‐randomised PROMISE EBF trial. BMC Public Health, 14(633), 1–12. 10.1186/1471-2458-14-633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engebretsen, I. M. , Nankabirwa, V. , Doherty, T. , Diallo, A. H. , Nankunda, J. , Fadnes, L. T. , Ekström, E. C. , Ramokolo, V. , Meda, N. , Sommerfelt, H. , Jackson, D. , Tylleskär, T. , Tumwine, J. K. , & Promise‐Ebf Study, g (2014). Early infant feeding practices in three African countries: The PROMISE‐EBF trial promoting exclusive breastfeeding by peer counsellors. International Breastfeeding Journal, 9, 9. 10.1186/1746-4358-9-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fadnes, L. T. , Nankabirwa, V. , Engebretsen, I. M. , Sommerfelt, H. , Birungi, N. , Lombard, C. , Swanevelder, S. , Van den Broeck, J. , Tylleskär, T. , Tumwine, J. K. , & Promise‐Ebf Study Group (2016). Effects of an exclusive breastfeeding intervention for six months on growth patterns of 4‐5 year old children in Uganda: The cluster‐randomised PROMISE EBF trial. BMC Public Health, 16(1), 1–9. 10.1186/s12889-016-3234-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flax, V. L. , Negerie, M. , Ibrahim, A. U. , Leatherman, S. , Daza, E. J. , & Bentley, M. E. (2014). Integrating group counseling, cell phone messaging, and participant‐generated songs and dramas into a microcredit program increases Nigerian women's adherence to international breastfeeding recommendations. Journal of Nutrition, 144(7), 1120–1124. 10.3945/jn.113.190124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabida, M. , Chemhuru, M. , Tshimanga, M. , Gombe, N. T. , Takundwa, L. , & Bangure, D. (2015). Effect of distribution of educational material to mothers on duration and severity of diarrhoea and pneumonia, Midlands Province, Zimbabwe: A cluster randomized controlled trial. International Breastfeeding Journal, 10(1), 1–12. 10.1186/s13006-015-0037-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelli, A. , Margolies, A. , Santacroce, M. , Roschnik, N. , Twalibu, A. , Katundu, M. , Moestue, H. , Alderman, H. , & Ruel, M. (2018). Using a community‐based early childhood development center as a platform to promote production and consumption diversity increases children's dietary intake and reduces stunting in Malawi: A cluster‐randomized trial. Journal of Nutrition, 148(10), 1587–1597. 10.1093/jn/nxy148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girard, A. W. , & Olude, O. (2012). Nutrition education and counselling provided during pregnancy: Effects on maternal, neonatal and child health outcomes: Nutrition education and counseling during pregnancy. Paediatric and Perinatal Epidemiology, 26(S1), 191–204. 10.1111/j.1365-3016.2012.01278.x [DOI] [PubMed] [Google Scholar]
- Graziose, M. M. , Downs, S. M. , O'Brien, Q. , & Fanzo, J. (2018). Systematic review of the design, implementation and effectiveness of mass media and nutrition education interventions for infant and young child feeding. Public Health Nutrition, 21(2), 273–287. 10.1017/S1368980017002786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenland, K. , Chipungu, J. , Curtis, V. , Schmidt, W. P. , Siwale, Z. , Mudenda, M. , Chilekwa, J. , Lewis, J. J. , & Chilengi, R. (2016). Multiple behaviour change intervention for diarrhoea control in Lusaka, Zambia: A cluster randomised trial. Lancet Global Health, 4(12), e966–e977. 10.1016/S2214-109X(16)30262-5 [DOI] [PubMed] [Google Scholar]
- Gresham, E. , Byles, J. E. , Bisquera, A. , & Hure, A. J. (2014). Effects of dietary interventions on neonatal and infant outcomes: A systematic review and meta‐analysis. The American Journal of Clinical Nutrition, 100(5), 1298–1321. 10.3945/ajcn.113.080655 [DOI] [PubMed] [Google Scholar]
- Guldan, G. S. , Fan, H. C. , Ma, X. , Ni, Z. Z. , Xiang, X. , & Tang, M. Z. (2000). Culturally appropriate nutrition education improves infant feeding and growth in rural Sichuan, China. Journal of Nutrition, 130(5), 1204–1211. 10.1093/jn/130.5.1204 [DOI] [PubMed] [Google Scholar]
- Haider, R. , Ashworth, A. , Kabir, I. , & Huttly, S. R. (2000). Effect of community‐based peer counsellors on exclusive breastfeeding practices in Dhaka, Bangladesh: A randomised controlled trial. Lancet, 356(9242), 1643–1647. 10.1016/S0140-6736(00)03159-7 [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T. , & Thompson, S. G. (2002). Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine, 21(11), 1539–1558. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- Higgins, J. P. T. , & Thompson, S. G. (2004). Controlling the risk of spurious findings from meta‐regression. Statistics in Medicine, 23(11), 1663–1682. 10.1002/sim.1752 [DOI] [PubMed] [Google Scholar]
- Imdad, A. , Yakoob, M. Y. , & Bhutta, Z. A. (2011). Impact of maternal education about complementary feeding and provision of complementary foods on child growth in developing countries. BMC Public Health, 11(S3), S25. 10.1186/1471-2458-11-s3-s25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakobsen, M. S. , Sodemann, M. , Biai, S. , Nielsen, J. , & Aaby, P. (2008). Promotion of exclusive breastfeeding is not likely to be cost effective in West Africa. A randomized intervention study from Guinea‐Bissau. Acta Paediatrica, 97(1), 68–75. 10.1111/j.1651-2227.2007.00532.x [DOI] [PubMed] [Google Scholar]
- Jannat, K. , Luby, S. P. , Unicomb, L. , Rahman, M. , Winch, P. J. , Parvez, S. M. , Das, K. K. , Leontsini, E. , Ram, P. K. , & Stewart, C. P. (2018). Complementary feeding practices among rural Bangladeshi mothers: Results from WASH Benefits study. Maternal and Child Nutrition, 15(1), e12654. 10.1111/mcn.12654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang, Y. , Suh, Y. K. , Debele, L. , Juon, H.‐S. , & Christian, P. (2017). Effects of a community‐based nutrition promotion programme on child feeding and hygiene practices among caregivers in rural Eastern Ethiopia. Public Health Nutrition, 20(8), 1461–1472. 10.1017/S1368980016003347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keats, E. C. , Das, J. K. , Salam, R. A. , Lassi, Z. S. , Imdad, A. , Black, R. E. , & Bhutta, Z. A. (2021). Effective interventions to address maternal and child malnutrition: An update of the evidence. The Lancet Child & Adolescent Health, 5(5), 367–384. 10.1016/S2352-4642(20)30274-1. [DOI] [PubMed] [Google Scholar]
- Kilaru, A. , Griffiths, P. L. , Ganapathy, S. , & Ghosh, S. (2005). Community‐based nutrition education for improving infant growth in rural Karnataka. Indian Pediatrics, 42(5), 425–432. [PubMed] [Google Scholar]
- Kim, S. S. , Nguyen, P. H. , Tran, L. M. , Sanghvi, T. , Mahmud, Z. , Haque, M. R. , Afsana, K. , Frongillo, E. A. , Ruel, M. T. , & Menon, P. (2018). Large‐scale social and behavior change communication interventions have sustained impacts on infant and young child feeding knowledge and practices: Results of a 2‐year follow‐up study in Bangladesh. Journal of Nutrition, 148(10), 1605–1614. 10.1093/jn/nxy147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, S. S. , Rawat, R. , Mwangi, E. M. , Tesfaye, R. , Abebe, Y. , Baker, J. , Frongillo, E. A. , Ruel, M. T. , & Menon, P. (2016). Exposure to large‐scale social and behavior change communication interventions is associated with improvements in infant and young child feeding practices in Ethiopia. PLOS One, 11(10), e0164800. 10.1371/journal.pone.0164800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimani‐Murage, E. W. , Norris, S. A. , Mutua, M. K. , Wekesah, F. , Wanjohi, M. , Muhia, N. , Muriuki, P. , Egondi, T. , Kyobutungi, C. , Ezeh, A. C. , Musoke, R. N. , McGarvey, S. T. , Madise, N. J. , & Griffiths, P. L. (2016). Potential effectiveness of community health strategy to promote exclusive breastfeeding in urban poor settings in Nairobi, Kenya: A quasi‐experimental study. Journal of Developmental Origins of Health and Disease, 7(2), 172–184. 10.1017/S2040174415007941 [DOI] [PubMed] [Google Scholar]
- Knapp, G. , & Hartung, J. (2003). Improved tests for a random effects meta‐regression with a single covariate. Statistics in Medicine, 22(17), 2693–2710. 10.1002/sim.1482 [DOI] [PubMed] [Google Scholar]
- Kuchenbecker, J. , Reinbott, A. , Mtimuni, B. , Krawinkel, M. B. , & Jordan, I. (2017). Nutrition education improves dietary diversity of children 6‐23 months at community‐level: Results from a cluster randomized controlled trial in Malawi. PLOS One, 12(4), 0175216. 10.1371/journal.pone.0175216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushwaha, K. P. , Sankar, J. , Sankar, M. J. , Gupta, A. , Dadhich, J. P. , Gupta, Y. P. , Bhatt, G. C. , Ansari, D. A. , & Sharma, B. (2014). Effect of peer counselling by mother support groups on infant and young child feeding practices: The Lalitpur experience. PLOS One, 9(11), e109181. 10.1371/journal.pone.0109181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamstein, S. , Perez‐Escamilla, R. , Koniz‐Booher, P. , Begin, F. , Adeyemi, S. , Kaligirwa, C. & Adebisi, B. (2018). The community infant and young child feeding counselling package in Kaduna State, Nigeria: A mixed methods evaluation. Final report. Arlington, VA: Strengthening Partnerships, Results, and Innovations in Nutrition Globally (SPRING) project.
- Lamstein, S. , Stillman, T. , Koniz‐Booher, P. , Aakesson, A. , Collaiezzi, B. , Williams, T. , & Anson, M. (2014). Evidence of effective approaches to social and behavior change communication for preventing and reducing stunting and anemia: Findings from a systematic literature review. Arlington, VA: USAID/Strengthening Partnerships, Results, and Innovations in Nutrition Globally (SPRING) Project.
- Lassi, Z. S. , Das, J. K. , Zahid, G. , Imdad, A. , & Bhutta, Z. A. (2013). Impact of education and provision of complementary feeding on growth and morbidity in children less than 2 years of age in developing countries: A systematic review, BMC Public Health, 13(S3), S13. 10.1186/1471-2458-13-s3-s13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Roux, I. M. , le Roux, K. , Mbeutu, K. , Comulada, W. S. , Desmond, K. A. , & Rotheram‐Borus, M. J. (2011). A randomized controlled trial of home visits by neighborhood mentor mothers to improve children's nutrition in South Africa. Vulnerable Child Youth Studies, 6(2), 91–102. 10.1080/17450128.2011.564224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Roux, I. M. , Rotheram‐Borus, M. J. , Stein, J. , & Tomlinson, M. (2014). The impact of paraprofessional home visitors on infants' growth and health at 18 months. Vulnerable Children & Youth Studies, 9(4), 291–304. 10.1080/17450128.2014.940413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leite, A. J. , Puccini, R. F. , Atalah, A. N. , Alves Da Cunha, A. L. , & Machado, M. T. (2005). Effectiveness of home‐based peer counselling to promote breastfeeding in the northeast of Brazil: A randomized clinical trial. Acta Paediatrica, 94(6), 741–746. 10.1111/j.1651-2227.2005.tb01974.x [DOI] [PubMed] [Google Scholar]
- Lewycka, S. , Mwansambo, C. , Rosato, M. , Kazembe, P. , Phiri, T. , Mganga, A. , Chapota, H. , Malamba, F. , Kainja, E. , Newell, M. L. , Greco, G. , Pulkki‐Brännström, A. M. , Skordis‐Worrall, J. , Vergnano, S. , Osrin, D. , & Costello, A. (2013). Effect of women's groups and volunteer peer counselling on rates of mortality, morbidity, and health behaviours in mothers and children in rural Malawi (MaiMwana): A factorial, cluster‐randomised controlled trial. The Lancet, 381(9879), 1721–1735. 10.1016/S0140-6736(12)61959-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Z. , Kim, R. , Vollmer, S. , & Subramanian, S. V. (2020). Factors associated with child stunting, wasting, and underweight in 35 low‐ and middle‐income countries. JAMA Network Open, 3(4), e203386. 10.1001/jamanetworkopen.2020.3386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquis, G. S. , Colecraft, E. K. , Kanlisi, R. , Aidam, B. A. , Atuobi‐Yeboah, A. , Pinto, C. , & Aryeetey, R. (2018). An agriculture–nutrition intervention improved children's diet and growth in a randomized trial in Ghana. Maternal & Child Nutrition, 14(S3), e12677. 10.1111/mcn.12677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins, V. J. , Toledo Florêncio, T. M. , Grillo, L. P. , do Carmo P Franco, M. , Martins, P. A. , Clemente, A. P. , Santos, C. D. , de Fatima A Vieira, M. , & Sawaya, A. L. (2011). Long‐lasting effects of undernutrition. International Journal of Environmental Research and Public Health, 8(6), 1817–1846. 10.3390/ijerph8061817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon, P. , Nguyen, P. H. , Saha, K. K. , Khaled, A. , Kennedy, A. , Tran, L. M. , Sanghvi, T. , Hajeebhoy, N. , Baker, J. , Alayon, S. , Afsana, K. , Haque, R. , Frongillo, E. A. , Ruel, M. T. , & Rawat, R. (2016). Impacts on breastfeeding practices of at‐scale strategies that combine intensive interpersonal counseling, mass media, and community mobilization: Results of cluster‐randomized program evaluations in Bangladesh and Viet Nam. PLOS Medicine, 13(10), e1002159. 10.1371/journal.pmed.1002159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon, P. , Nguyen, P. H. , Saha, K. K. , Khaled, A. , Sanghvi, T. , Baker, J. , Afsana, K. , Haque, R. , Frongillo, E. A. , Ruel, M. T. , & Rawat, R. (2016). Combining intensive counseling by frontline workers with a nationwide mass media campaign has large differential impacts on complementary feeding practices but not on child growth: Results of a cluster‐randomized program evaluation in Bangladesh1‐3. Journal of Nutrition, 146(10), 2075–2084. 10.3945/JN.116.232314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. PLOS Medicine, 6(7), e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- More, N. S. , Das, S. , Bapat, U. , Alcock, G. , Manjrekar, S. , Kamble, V. , Sawant, R. , Shende, S. , Daruwalla, N. , Pantvaidya, S. , & Osrin, D. (2017). Community resource centres to improve the health of women and children in informal settlements in Mumbai: A cluster‐randomised, controlled trial. The Lancet Global Health, 5(3), e335–e349. 10.1016/S2214-109X(16)30363-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhoozi, G. , Atukunda, P. , Diep, L. M. , Mwadime, R. , Kaaya, A. N. , Skaare, A. B. , Willumsen, T. , Westerberg, A. C. , & Iversen, P. O. (2018). Nutrition, hygiene, and stimulation education to improve growth, cognitive, language, and motor development among infants in Uganda: A cluster‐randomized trial. Maternal and Child Nutrition, 14(2), e12527. 10.1111/mcn.12527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukuria, A. G. , Martin, S. L. , Egondi, T. , Bingham, A. , & Thuita, F. M. (2016). Role of social support in improving infant feeding practices in Western Kenya: A quasi‐experimental study. Global Health, Science and Practice, 4(1), 55–72. 10.9745/GHSP-D-15-00197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair, N. , Tripathy, P. , Sachdev, H. S. , Pradhan, H. , Bhattacharyya, S. , Gope, R. , Gagrai, S. , Rath, S. , Rath, S. , Sinha, R. , Roy, S. S. , Shewale, S. , Singh, V. , Srivastava, A. , Costello, A. , Copas, A. , Skordis‐Worrall, J. , Haghparast‐Bidgoli, H. , Saville, N. , & Prost, A. (2017). Effect of participatory women's groups and counselling through home visits on children's linear growth in rural eastern India (CARING trial): A cluster‐randomised controlled trial. The Lancet Global Health, 5(10), e1004–e1016. 10.1016/S2214-109X(17)30339-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Negash, C. , Belachew, T. , Henry, C. J. , Kebebu, A. , Abegaz, K. , & Whiting, S. J. (2014). Nutrition education and introduction of broad bean‐based complementary food improves knowledge and dietary practices of caregivers and nutritional status of their young children in Hula, Ethiopia. Food and Nutrition Bulletin, 35(4), 480–486. 10.1177/156482651403500409 [DOI] [PubMed] [Google Scholar]
- Nguyen, P. H. , Kim, S. S. , Sanghvi, T. , Mahmud, Z. , Tran, L. M. , Shabnam, S. , Aktar, B. , Haque, R. , Afsana, K. , Frongillo, E. A. , Ruel, M. T. , & Menon, P. (2017). Integrating nutrition interventions into an existing maternal, neonatal, and child health program increased maternal dietary diversity, micronutrient intake, and exclusive breastfeeding practices in Bangladesh: Results of a cluster‐randomized program evaluation. The Journal of Nutrition, 147(12), 2326–2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikièma, L. , Huybregts, L. , Martin‐Prevel, Y. , Donnen, P. , Lanou, H. , Grosemans, J. , Offoh, P. , Dramaix‐Wilmet, M. , Sondo, B. , Roberfroid, D. , & Kolsteren, P. (2017). Effectiveness of facility‐based personalized maternal nutrition counseling in improving child growth and morbidity up to 18 months: A cluster‐randomized controlled trial in rural Burkina Faso. PLOS One, 12(5), e0177839. 10.1371/journal.pone.0177839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olney, D. K. , Pedehombga, A. , Ruel, M. T. , & Dillon, A. (2015). A 2‐year integrated agriculture and nutrition and health behavior change communication program targeted to women in Burkina Faso reduces anemia, wasting, and diarrhea in children 3‐12.9 months of age at baseline: A cluster‐randomized controlled trial 1‐3. The Journal of Nutrition, 145(6), 1317–1324. 10.3945/jn.114.203539 [DOI] [PubMed] [Google Scholar]
- Pachon, H. , Schroeder, D. G. , Marsh, D. R. , Dearden, K. A. , Ha, T. T. , & Lang, T. T. (2002). Effect of an integrated child nutrition intervention on the complementary food intake of young children in rural north Vietnam. Food and Nutrition Bulletin, 23(4 Suppl), 59–66. 10.1177/15648265020234S209 [DOI] [PubMed] [Google Scholar]
- Panjwani, A. , & Heidkamp, R. (2017). Complementary feeding interventions have a small but significant impact on linear and ponderal growth of children in low‐ and middle‐income countries: A systematic review and meta‐analysis. Journal of Nutrition, 147(11), 2169s–2178s. 10.3945/jn.116.243857 [DOI] [PubMed] [Google Scholar]
- Penfold, S. , Manzi, F. , Mkumbo, E. , Temu, S. , Jaribu, J. , Shamba, D. D. , Mshinda, H. , Cousens, S. , Marchant, T. , Tanner, M. , Schellenberg, D. , & Schellenberg, J. A. (2014). Effect of home‐based counselling on newborn care practices in southern tanzania one year after implementation: A cluster‐randomised controlled trial. BMC Pediatrics, 14(1), 187. 10.1186/1471-2431-14-187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penny, M. E. , Creed‐Kanashiro, H. M. , Robert, R. C. , Narro, M. R. , Caulfield, L. E. , & Black, R. E. (2005). Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: A cluster‐randomised controlled trial. The Lancet, 365(9474), 1863–1872. 10.1016/S0140-6736(05)66426-4 [DOI] [PubMed] [Google Scholar]
- Proctor, E. K. , Powell, B. J. , & McMillen, J. C. (2013). Implementation strategies: Recommendations for specifying and reporting. Implementation Science, 8(139), 1–11. 10.1186/1748-5908-8-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remsberg . (2021). Defining social and behavior change communication (SBCC) and other essential health communication terms. Policy and Practice Blogs. https://www.comminit.com/policy-blogs/content/defining-social-and-behavior-change-communication-sbcc-and-other-essential-health-commun [Google Scholar]
- Rawat, R. , Nguyen, P. H. , Tran, L. M. , Hajeebhoy, N. , Nguyen, H. V. , Baker, J. , Frongillo, E. A. , Ruel, M. T. , & Menon, P. (2017). Social franchising and a nationwide mass media campaign increased the prevalence of adequate complementary feeding in Vietnam: A cluster‐randomized program evaluation. Journal of Nutrition, 147(4), 670–679. 10.3945/jn.116.243907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockers, P. C. , Zanolini, A. , Bowen, B. , Mwaba Moono, C. , Hughes, R. C. , Hamer, D. H. , & Fink, G. (2018). Two‐year impact of community‐based health screening and parenting groups on child development in Zambia: Follow‐up to a cluster‐randomized controlled trial. PLOS Medicine, 15(4), 1002555. 10.1371/journal.pmed.1002555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy, S. K. , Fuchs, G. J. , Mahmud, Z. , Ara, G. , Islam, S. , Shafique, S. , Akter, S. S. , & Chakraborty, B. (2005). Intensive nutrition education with or without supplementary feeding improves the nutritional status of moderately‐malnourished children in Bangladesh. Journal of Health, Population, and Nutrition, 23(4), 320–330. [PubMed] [Google Scholar]
- Roy, S. K. , Jolly, S. P. , Shafique, S. , Fuchs, G. J. , Mahmud, Z. , Chakraborty, B. , & Roy, S. (2007). Prevention of malnutrition among young children in rural Bangladesh by a food‐health‐care educational intervention: A randomized, controlled trial. Food and Nutrition Bulletin, 28(4), 375–383. 10.1177/156482650702800401 [DOI] [PubMed] [Google Scholar]
- Ruel, M. T. , & Alderman, H. (2013). Nutrition‐sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition? Lancet, 382(9891), 536–551. 10.1016/s0140-6736(13)60843-0 [DOI] [PubMed] [Google Scholar]
- Ruel, M. T. , Menon, P. , Habicht, J.‐P. , Loechl, C. , Bergeron, G. , Pelto, G. , Arimond, M. , Maluccio, J. , Michaud, L. , & Hankebo, B. (2008). Age‐based preventive targeting of food assistance and behaviour change and communication for reduction of childhood undernutrition in Haiti: A cluster randomised trial. The Lancet, 371(9612), 588–595. 10.1016/S0140-6736(08)60271-8 [DOI] [PubMed] [Google Scholar]
- Rujumba, J. , Ndeezi, G. , Nankabirwa, V. , Kwagala, M. , Mukochi, M. , Diallo, A. H. , Meda, N. , Engebretsen, I. , Tylleskär, T. , & Tumwine, J. (2020). “If I have money, I cannot allow my baby to breastfeed only …” barriers and facilitators to scale‐up of peer counselling for exclusive breastfeeding in Uganda. International Breastfeeding Journal, 15(1), 1–12. 10.1186/s13006-020-00287-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Susiloretni, K. A. , Krisnamurni, S. , Sunarto, Widiyanto, Y. D. , Yazid, A. , & Wilopo, S. A. (2013). The Effectiveness of multilevel promotion of exclusive breastfeeding in rural Indonesia. American Journal of Health Promotion, 28(2), e44–e55. 10.4278/ajhp.120425-QUAN-221 [DOI] [PubMed] [Google Scholar]
- Saggurti, N. , Atmavilas, Y. , Porwal, A. , Schooley, J. , Das, R. , Kande, N. , Irani, L. , & Hay, K. (2018). Effect of health intervention integration within women's self‐help groups on collectivization and healthy practices around reproductive, maternal, neonatal and child health in rural India. PLOS One, 13(8), e0202562. 10.1371/journal.pone.0202562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleem, A. F. , Mahmud, S. , Baig‐Ansari, N. , & Zaidi, A. K. (2014). Impact of maternal education about complementary feeding on their infants' nutritional outcomes in low‐ and middle‐income households: A community‐based randomized interventional study in Karachi, Pakistan. Journal of Health, Population, and Nutrition, 32(4), 623–633. [PMC free article] [PubMed] [Google Scholar]
- Sanghvi, T. , Seidel, R. , Baker, J. , & Jimerson, A. (2017). Using behavior change approaches to improve complementary feeding practices. Maternal & Child Nutrition, 13(S2), e12406. 10.1111/mcn.12406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos, I. , Victora, C. G. , Martines, J. , Goncalves, H. , Gigante, D. P. , Valle, N. J. , & Pelto, G. (2001). Nutrition counseling increases weight gain among Brazilian children. Journal of Nutrition, 131(11), 2866–2873. 10.1093/jn/131.11.2866 [DOI] [PubMed] [Google Scholar]
- Saville, N. M. , Shrestha, B. P. , Style, S. , Harris‐Fry, H. , Beard, B. J. , Sen, A. , Jha, S. , Rai, A. , Paudel, V. , Sah, R. , Paudel, P. , Copas, A. , Bhandari, B. , Neupane, R. , Morrison, J. , Gram, L. , Pulkki‐Brännström, A. M. , Skordis‐Worrall, J. , Basnet, M. , … Costello, A. (2018). Impact on birth weight and child growth of Participatory Learning and Action women's groups with and without transfers of food or cash during pregnancy: Findings of the low birth weight South Asia cluster‐randomised controlled trial (LBWSAT) in Nepal. PLOS One, 13(5), 0194064. 10.1371/journal.pone.0194064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder, D. G. , Pachon, H. , Dearden, K. A. , Kwon, C. B. , Ha, T. T. , Lang, T. T. , & Marsh, D. R. (2002). An integrated child nutrition intervention improved growth of younger, more malnourished children in northern Vietnam. Food and Nutrition Bulletin, 23(S4), 53–61. [PubMed] [Google Scholar]
- Seetha, A. , Tsusaka, T. W. , Munthali, T. W. , Musukwa, M. , Mwangwela, A. , Kalumikiza, Z. , Manani, T. , Kachulu, L. , Kumwenda, N. , Musoke, M. , & Okori, P. (2018). How immediate and significant is the outcome of training on diversified diets, hygiene and food safety? An effort to mitigate child undernutrition in rural Malawi. Public Health Nutrition, 21(6), 1156–1166. 10.1017/S1368980017003652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp, S. (1998). Meta‐analysis regression. Stata Technical Bulletin, 7(42), 16–22. https://EconPapers.repec.org/RePEc:tsj:stbull:y:1998:v:7:i:42:sbe23 [Google Scholar]
- Sherburne, L. , Math, S. , Griffiths, M. , Sacci, I. & O'Donnell, C. (2018). “Grow Together” campaign in Cambodia: A game‐changer for children's healthy growth. https://www.advancingnutrition.org/sites/default/files/2020-02/grow_together_paper.pdf
- Shi, L. , & Zhang, J. (2010). Recent evidence of the effectiveness of educational interventions for improving complementary feeding practices in developing countries. Journal of Tropical Pediatrics, 57(2), 91–98. 10.1093/tropej/fmq053 [DOI] [PubMed] [Google Scholar]
- Shi, L. , Zhang, J. , Wang, Y. , Caulfield, L. E. , & Guyer, B. (2010). Effectiveness of an educational intervention on complementary feeding practices and growth in rural China: A cluster randomised controlled trial. Public Health Nutrition, 13(4), 556–565. 10.1017/s1368980009991364 [DOI] [PubMed] [Google Scholar]
- Singh, A. , Klemm, R. D. W. , Mundy, G. , Pandey Rana, P. , Pun, B. , & Cunningham, K. (2018). Improving maternal, infant and young child nutrition in Nepal via peer mobilization. Public Health Nutrition, 21(4), 796–806. 10.1017/s1368980017002993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla, D. R. , Kumbakumba, E. , & Aboud, F. E. (2015). Effects of a parenting intervention to address maternal psychological wellbeing and child development and growth in rural Uganda: A community‐based, cluster randomised trial. Lancet Global Health, 3(8), e458–e469. 10.1016/s2214-109x(15)00099-6 [DOI] [PubMed] [Google Scholar]
- SPRING . (2019). Moving nutrition social and behavior change forward. https://www.spring-nutrition.org/publications/briefs/moving-nutrition-social-and-behavior-change-forward
- Tahir, N. M. , & Al‐Sadat, N. (2013). Does telephone lactation counselling improve breastfeeding practices?: A randomised controlled trial. International Journal of Nursing Studies, 50(1), 16–25. 10.1016/j.ijnurstu.2012.09.006 [DOI] [PubMed] [Google Scholar]
- The Cochrane Public Health Group . (2011). Guide for developing a public health protocol.
- Tomlinson, M. , Doherty, T. , Ijumba, P. , Jackson, D. , Lawn, J. , Persson, L. Å. , Lombard, C. , Sanders, D. , Daviaud, E. , Nkonki, L. , Goga, A. , Rohde, S. , Sitrin, D. , Colvin, M. , & Chopra, M. (2014). Goodstart: A cluster randomised effectiveness trial of an integrated, community‐based package for maternal and newborn care, with prevention of mother‐to‐child transmission of HIV in a South African township. Tropical Medicine & International Health, 19(3), 256–266. 10.1111/tmi.12257 [DOI] [PubMed] [Google Scholar]
- Tylleskär, T. , Jackson, D. , Meda, N. , Engebretsen, I. M. , Chopra, M. , Diallo, A. H. , Doherty, T. , Ekström, E. C. , Fadnes, L. T. , Goga, A. , Kankasa, C. , Klungsøyr, J. I. , Lombard, C. , Nankabirwa, V. , Nankunda, J. K. , Van de Perre, P. , Sanders, D. , Shanmugam, R. , Sommerfelt, H. , … Promise‐Ebf Study Group . (2011). Exclusive breastfeeding promotion by peer counsellors in sub‐Saharan Africa (PROMISE‐EBF): A cluster‐randomised trial. The Lancet, 378(9789), 420–427. 10.1016/S0140-6736(11)60738-1 [DOI] [PubMed] [Google Scholar]
- UN . (2015). The millenium development goals report. https://www.un.org/millenniumgoals/2015_MDG_Report/pdf/MDG%202015%20rev%20(July%201).pdf
- UN DESA . (2018). World urbanisation prospects 2018. Department of Economic and Social Affairs Population Dynamics. https://population.un.org/wup/
- Unger, J. A. , Ronen, K. , Perrier, T. , DeRenzi, B. , Slyker, J. , Drake, A. L. , Mogaka, D. , Kinuthia, J. , & John‐Stewart, G. (2018). Short message service communication improves exclusive breastfeeding and early postpartum contraception in a low‐ to middle‐income country setting: A randomised trial. BJOG: An International Journal of Obstetrics & Gynaecology, 125(12), 1620–1629. 10.1111/1471-0528.15337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . (2013). Improving child nutrition: The achievable imperative for global progress. UNICEF. https://data.unicef.org/resources/improving-child-nutrition-the-achievable-imperative-for-global-progress/
- UNSCN . (2015). Nutrition targets and indicators for the post‐2015 sustainable development goals: Accountability for the measurement of results in nutrition: A technical note. https://www.unscn.org/files/Publications/Briefs_on_Nutrition/Final_Nutrition%20and_the_SDGs.pdf
- Vazir, S. , Engle, P. , Balakrishna, N. , Griffiths, P. L. , Johnson, S. L. , Creed‐Kanashiro, H. , Fernandez Rao, S. , Shroff, M. R. , & Bentley, M. E. (2013). Cluster‐randomized trial on complementary and responsive feeding education to caregivers found improved dietary intake, growth and development among rural Indian toddlers. Maternal & Child Nutrition, 9(1), 99–117. 10.1111/j.1740-8709.2012.00413.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora, C. G. , Adair, L. , Fall, C. , Hallal, P. C. , Martorell, R. , Richter, L. , Sachdev, H. S. , & Maternal and Child Undernutrition Study, G. (2008). Maternal and child undernutrition: Consequences for adult health and human capital. Lancet, 371, 340–357. 10.1016/S0140-6736(07)61692-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vitolo, M. R. , Bortolini, G. A. , Feldens, C. A. , & Drachler Mde, L. (2005). Impacts of the 10 steps to healthy feeding in infants: A randomized field trial. Cadernos de Saude Publica, 21(5), 1448–1457. 10.1111/S0102-311x2005000500018 [DOI] [PubMed] [Google Scholar]
- Waiswa, P. , Pariyo, G. , Kallander, K. , Akuze, J. , Namazzi, G. , Ekirapa‐Kiracho, E. , Kerber, K. , Sengendo, H. , Aliganyira, P. , Lawn, J. E. , Peterson, S. , & Uganda Newborn Study, T. (2015). Effect of the Uganda newborn study on care‐seeking and care practices: A cluster‐randomised controlled trial. Global Health Action, 8, 24584. 10.3402/gha.v8.24584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waswa, L. M. , Jordan, I. , Herrmann, J. , Krawinkel, M. B. , & Keding, G. B. (2015). Community‐based educational intervention improved the diversity of complementary diets in western Kenya: Results from a randomized controlled trial. Public Health Nutrition, 18(18), 3406–3419. 10.1017/s1368980015000920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White, S. , Schmidt, W. , Sahanggamu, D. , Fatmaningrum, D. , van Liere, M. , & Curtis, V. (2016). Can gossip change nutrition behaviour? Results of a mass media and community‐based intervention trial in East Java, Indonesia. Tropical Medicine and International Health, 21(3), 348–364. 10.1111/tmi.12660 [DOI] [PubMed] [Google Scholar]
- WHO . (2008). Indicators for assessing infant and young child feeding practices: Part 1: Definitions.
- WHO . (2014). Global nutrition targets 2025: Policy brief series (WHO/NMH/NHD/14.2). Geneva: World Health Organization: Author. https://www.who.int/publications/i/item/WHO-NMH-NHD-14.2 [Google Scholar]
- Willett, W. , Rockström, J. , Loken, B. , Springmann, M. , Lang, T. , Vermeulen, S. , Garnett, T. , Tilman, D. , DeClerck, F. , Wood, A. , Jonell, M. , Clark, M. , Gordon, L. J. , Fanzo, J. , Hawkes, C. , Zurayk, R. , Rivera, J. A. , De Vries, W. , Majele Sibanda, L. , … Murray, C. (2019). Food in the anthropocene: The EAT‐lancet commission on healthy diets from sustainable food systems. Lancet, 393(10170), 447–492. 10.1016/s0140-6736(18)31788-4 [DOI] [PubMed] [Google Scholar]
- World Bank . (2018). World bank list of economies (June 2018).
- Younes, L. , Houweling, T. A. , Azad, K. , Kuddus, A. , Shaha, S. , Haq, B. , Nahar, T. , Hossen, M. , Beard, J. , Copas, A. , Prost, A. , Costello, A. , & Fottrell, E. (2015). The effect of participatory women's groups on infant feeding and child health knowledge, behaviour and outcomes in rural Bangladesh: A controlled before‐and‐after study. Journal of Epidemiology and Community Health, 69(4), 374–381. 10.1136/jech-2014-204271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaman, S. , Ashraf, R. N. , & Martines, J. (2008). Training in complementary feeding counselling of healthcare workers and its influence on maternal behaviours and child growth: A cluster‐randomized controlled trial in Lahore, Pakistan. Journal of Health, Population, and Nutrition, 26(2), 210–222. [PMC free article] [PubMed] [Google Scholar]
- Zhang, J. , Shi, L. , Chen, D. F. , Wang, J. , & Wang, Y. (2013). Effectiveness of an educational intervention to improve child feeding practices and growth in rural China: Updated results at 18 months of age. Maternal and Child Nutrition, 9(1), 118–129. 10.1111/j.1740-8709.2012.00447.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Supporting information.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


