Abstract
Background
The aim of this study was to evaluate the rate of depression during the COVID-19 pandemic compared to that during the prepandemic period.
Methods
Data from participants in the Korean Community Health Survey in 2019 and 2020 aged ≥ 19 years old were analyzed. In total, the data of 223,306 participants from the 2020 group were compared with the data of 217,133 participants from the 2019 group regarding the experience and severity of depression. The experience of depression was surveyed in terms of a history of sadness or despair for ≥2 weeks in the last year. In addition, the PHQ-9 scores were used, and participants with PHQ-9 scores ≥10 were recategorized as having moderate to severe depression. The odds for depression of the 2020 group compared to the 2019 group based on the survey and PHQ-9 scores were calculated using simple or multiple logistic regression with complex sampling with weighted values.
Results
The rate of depression experience was lower in the 2020 group than in the 2019 group. The odds of experiencing depression were lower in the 2020 group than in the 2019 group (adjusted odds ratio [aOR] = 0.95, 95% confidence intervals [95% CI] = 0.91–0.98, P = 0.004). The odds of moderate to severe depression were also lower in the 2020 group than in the 2019 group (aOR=0.92, 95% CI=0.88–0.97, P = 0.001).
Conclusion
The rate of depression experience was not higher during the COVID-19 pandemic than during the prepandemic period in Korea.
Keywords: Depression, COVID-19, Risk factors, Cohort studies, Epidemiology
1. Introduction
The novel coronavirus disease 19 (COVID-19) pandemic broke out in December 2019 (Zhu et al., 2020; Park et al., 2020b). Global concerns about the COVID-19 pandemic have persisted due to the lack of therapeutics, which has increased the uncertainty and awareness of SARS-CoV-2 infection. To prevent the spread of SARS-CoV-2 infection, quarantine and social distancing measures have limited the physical and social activities of the population. In addition, economic distress followed, with increased disparities due to job loss and economic uncertainty. Furthermore, nationwide strategies to suppress SARS-CoV-2 contraction have been suggested to have adverse impacts in terms of the prevalence of psychological disorders (Brooks et al., 2020; Bauerle et al., 2020; Luo et al., 2020). In a meta-analysis study, the prevalence of depression was found to be approximately 33% worldwide during the COVID-19 pandemic (95% confidence intervals [95% CI] = 28%–38%) (Luo et al., 2020). Quarantine increased posttraumatic stress, confusion, and anger due to social isolation, fears of infection, inadequate supplies, uncertainties, financial deficits, and stigma (Brooks et al., 2020).
In Korea, the first patient was diagnosed with COVID-19 on January 20, 2020. From that time, Korea underwent the first wave of the COVID-19 crisis until April 2020 (Kim and Ashihara, 2020). To cope with the COVID-19 pandemic, the Korean government implemented several strategies, including quarantine, levels of social distancing, a wide range of SARS-CoV-2 testing, tracking of the SARS-CoV-2 infection route, and the coverage of all treatment costs for all patients with COVID-19 (Kim and Ashihara, 2020). Although these government efforts have prevented nationwide disasters, concerns about mental health were inevitable in Korea (Hyun et al., 2020). COVID-19 patients with mental illness had more severe COVID-19 than COVID-19 patients without mental illness (adjusted odds ratio [aOR] = 1.27, 95% CI = 1.01–1.66) (Lee et al., 2020b). In addition to patients contracting SARS-CoV-2, the potential risk of depression associated with the COVID-19 pandemic has been suggested, such as among healthcare workers and physical therapists in Korea (Park et al., 2020a; Yang et al., 2020). In addition to healthcare workers being exposed to patients with COVID-19, workers with low exposure also suffered from depression and anxiety (Park et al., 2020a). Thus, it can be supposed that the COVID-19 pandemic has had an adverse impact on the rate of depression in the Korean population. However, to our knowledge, a comparison of depression between the periods before and during the pandemic considering socioeconomic status has not been performed in a large cohort population.
This study aimed to evaluate the impact of the COVID-19 pandemic on the rates of depression experience and rates of moderate to severe degrees of depression in the Korean population. The primary outcome was the rate of depression experience surveyed by questionnaire, and the secondary outcome was the rate of moderate to severe depression based on the Patient Health Questionnaire-9 (PHQ-9) score. In addition, the differential impact of the COVID-19 pandemic on depression was analyzed according to age and sex.
2. Methods
2.1. Study population and data collection
This study was approved by the Institutional Review Board of the Korea Centers for Disease Control and Prevention (KCDC) (2016-10-01-T-A). All Korean Community Health Survey (KCHS) data analyses were conducted in accordance with the guidelines and regulations provided by the KCDC (see the S1 description for a detailed description) (Kim et al., 2018; Lim et al., 2017). The nationwide representative population was sampled from all of Korea based on the region of residence using the registered address (Tong Ban/Lee) of all administrative areas (Si-Gun-Gu) (Kang et al., 2015). The average sample size of each community health center (total 235 centers) was 900 people, and the valid sample was about 75–90% for each community health center with quality control (Kang et al., 2015). Weighting of data was conducted for household, personal response rate, age, and sex.
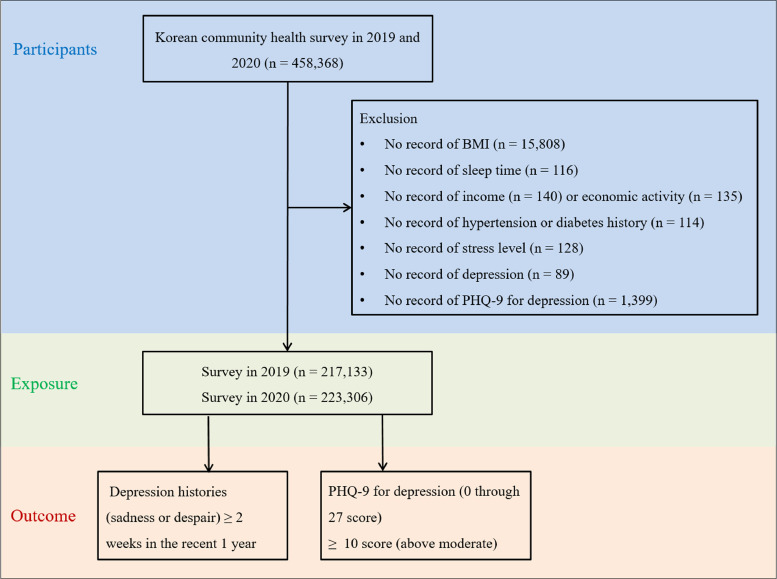
This study was a cross-sectional study using data from the KCHS in 2019 and 2020. The 2019 KCHS survey was conducted from August 16, 2019 – October 31, 2019, and the 2020 KCHS survey was conducted from August 16, 2020 – October 31, 2020. The first COVID-19 patient in Korea was reported in December 2019. Thus, the 2019 KCHS survey provided the pre-COVID-19 pandemic data. Because the COVID-19 pandemic has continued during 2020 and stratified social distancing policies have been enacted in Korea, the 2020 KCHS survey data reflected the COVID-19 pandemic era. Of the 458,368 total participants, we excluded participants who met the following criteria from this study: no record of BMI (n = 15,808), sleep time (n = 116), income (n = 140) or economic activity (n = 135), hypertension or diabetes history (n = 114), subjective stress level (n = 128), depression questionnaire responses (n = 89), and PHQ-9 responses for depression (n = 1399). The age range of the participants was 19 to 110 years old.
Finally, 217,133 participants surveyed in 2019 and 223,306 participants surveyed in 2020 were included (Fig. 1 ). Then, we analyzed the data from the depression questionnaire and PHQ-9 for depression.
Fig. 1.
A schematic illustration of participant selection in the present study.
2.2. Survey
2.2.1. Exposure
In the 2019 and 2020 groups, adult participants were selected as stated above to represent the entire Korean adult population. The 2019 participants were not followed up. The 2020 participants were newly selected from the entire Korean population.
2.2.2. Outcome
Experience of depression was surveyed with the following question: “Did you feel sadness or despair enough to bother you in your daily life more than 2 weeks in the last 1 year?” Their answer was recorded as yes or no. For the validity of the study, depression was surveyed again using the PHQ-9 (Han et al., 2008). This variable was measured as a continuous variable based on a score of 0–27 calculated from 9 items. We divided the PHQ-9 score into scores ≥ 10 and scores < 10 to clarify the description of the results. A PHQ-9 score ≥ 10 was considered to indicate moderate to severe depression, enough to consider cognitive behavioral therapy or pharmacotherapy.
2.2.3. Covariates
Age, BMI (kg/m2), yearly household income (amount earned/year), and sleep time (hours/day) were surveyed as continuous variables (Kim et al., 2021a). Sex, educational level, smoking, frequency of alcohol drinking, histories of diabetes mellitus, hypertension, subjective stress level, and current economic activity (Did you work for income more than one hour or work for a family business without income more than 18 h in the last 1 week?) were surveyed as categorical variables (Table 1 ) (Kim et al., 2018). The detailed survey questionnaire is described on the KCDC website for the KCHS (Korea Disease Control and Prevention Agency, 2021).
Table 1.
General characteristics of participants.
| General characteristics | The participated year | |||
|---|---|---|---|---|
| 2019 | 2020 | P-value | ||
| Total Number, n (%) | 217,113 (100.0) | 223,306 (100.0) | ||
| Age (years, mean, [SD]) | 54.8 (17.4) | 54.1 (17.6) | <0.001* | |
| BMI (kg/m2, mean, [SD]) | 24.0 (3.6) | 23.6 (3.3) | <0.001* | |
| Current economic activity, n (%) | 136,278 (62.8) | 136,729 (61.2) | <0.001† | |
| Income (won/year, mean, [SD]) | 41,386,557 (3391) | 41,403,862 (3501) | 0.868 | |
| Income group (n,%) | <0.001† | |||
| Low (< 24,000,000 won/year) | 70,021 (32.2) | 73,010 (32.7) | ||
| Middle (24,000,000 to <48,000,000 won/year) | 62,333 (28.7) | 64,738 (29.0) | ||
| High (≥ 48,000,000 won/year) | 84,779 (39.0) | 85,558 (38.3) | ||
| Region | 0.012† | |||
| Urban area | 57,941 (26.7) | 60,382 (27.0) | ||
| Rural area | 131,179 (60.4) | 134,544 (60.3) | ||
| Pandemic area (Deagu, Kyeongbuk) | 28,013 (12.9) | 28,380 (12.7) | ||
| Sleep time (hours/day, mean, [SD]) | 6.6 (1.3) | 6.8 (1.3) | <0.001* | |
| Sex, n (%) | <0.001† | |||
| Male | 98,317 (45.3) | 102,830 (46.0) | ||
| Female | 118,816 (54.7) | 120,476 (54.0) | ||
| Education, n (%) | <0.001† | |||
| Middle school or below | 76,029 (35.0) | 71,540 (32.0) | ||
| High school | 62,650 (28.9) | 66,025 (29.6) | ||
| College or over | 78,454 (36.1) | 85,741 (38.4) | ||
| Smoking status, n (%) | <0.001† | |||
| Non-smoker | 136,640 (62.9) | 144,975 (64.9) | ||
| Past smoker | 44,197 (20.4) | 41,285 (18.5) | ||
| Current smoker | 36,296 (16.7) | 37,046 (16.6) | ||
| Frequency of alcohol drinking, n (%) | <0.001† | |||
| Non-drinker | 77,074 (35.0) | 92,630 (41.5) | ||
| ≤1 time a month | 80,604 (37.1) | 74,338 (33.3) | ||
| ≥ 2 times a week | 59,455 (27.4) | 56,338 (25.2) | ||
| Diabetes mellitus, n (%) | 24,934 (11.5) | 25,837 (11.6) | 0.366 | |
| Hypertension, n (%) | 61,779 (28.5) | 60,979 (27.3) | <0.001† | |
| Subjective stress level, n (%) | <0.001† | |||
| No | 53,124 (24.5) | 55,821 (25.0) | ||
| A little | 116,423 (53.6) | 117,871 (52.8) | ||
| Severe | 41,544 (19.1) | 42,918 (19.2) | ||
| Very severe | 6042 (2.8) | 6696 (3.0) | ||
| Depression (%) | 13,065 (6.0) | 12,471 (5.6) | <0.001† | |
| PHQ-9 for depression (mean, [SD]) | 2.1 (3.0) | 1.9 (2.9) | <0.001* | |
| PHQ-9 for depression ≥ 10 score, n (%) | 6698 (3.1) | 6147 (2.8) | <0.001† | |
| Little interest or pleasure in doing things? ≥ 2 score, n (%) | 9476 (4.2) | 9460 (4.2) | 0.037* | |
| Feeling down, depressed, or hopeless? ≥ 2 score, n (%) | 6275 (2.9) | 5861 (2.6) | <0.001† | |
| Trouble falling or staying asleep, or sleeping too much? ≥ 2 score, n (%) | 20,768 (9.6) | 18,787 (8.4) | <0.001† | |
| Feeling tired or having little energy? ≥ 2 score, n (%) | 19,140 (8.8) | 15,116 (6.8) | <0.001† | |
| Poor appetite or overeating? ≥ 2 score, n (%) | 8056 (3.7) | 7224 (3.2) | <0.001† | |
| Feeling bad about yourself - or that you are a failure or have let yourself or your family down? ≥ 2 score, n (%) | 2516 (1.2) | 2510 (1.1) | 0.278 | |
| Trouble concentrating on things, such as reading the newspaper or watching television? ≥ 2 score, n (%) | 2281 (1.1) | 2214 (1.0) | 0.051 | |
| Moving or speaking so slowly that other people could have noticed? Or the opposite - being so fidgety or restless that you have been moving around a lot more than usual? ≥ 2 score, n (%) |
1370 (0.6) | 1246 (0.6) | 0.002* | |
| Thoughts that you would be better off dead, or of hurting yourself in some way? ≥ 2 score, n (%) | 1891 (0.9) | 1783 (0.8) | 0.008* | |
SCD, subjective cognitive decline; SD, standard deviation.
Independent T-test, Significance at P < 0.05.
Chi-square test, Significance at P < 0.05.
2.3. Statistical analysis
The mean values and rates of variables were measured with independent T-tests or chi-square tests. The odds ratio (OR) for the depression questionnaire was calculated with simple or multiple logistic regression with complex sampling with weighted values. Crude and adjusted (by age, BMI, income, sleep time, sex, education level, smoking, alcohol consumption, history of diabetes mellitus, hypertension, subjective stress level, and current economic activity) models were presented. We performed subgroup analyses according to age (≤ 40 years old, 41–60 years old, ≥ 61 years old) and sex.
Two-tailed analyses were conducted, and P-values lower than 0.05 were considered to indicate significance; 95% confidence intervals (CIs) were calculated. The results were analyzed statistically using SPSS ver. 25.0 (IBM, Armonk, NY, USA).
3. Results
A total of 5.6% (12,471/223,306) and 6.0% (13,065/217,133) of the 2020 and 2019 populations, respectively, had experienced depression (P < 0.001, Table 1). The mean PHQ-9 score was higher in the 2019 group than in the 2020 group (2.1 [standard deviation, SD = 3.0] vs. 1.9 [SD = 2.9], P < 0.001). There were more participants with moderate to severe depression in the 2019 group than in the 2020 group (3.1% vs. 2.8%, P < 0.001). The 2019 group showed higher rates of having little interest or pleasure in doing things; feeling down, depressed, or hopeless; having trouble falling or staying asleep or sleeping too much; feeling tired or having little energy; having a poor appetite or overeating; moving or speaking so slowly that other people could have noticed or the opposite, i.e., being so fidgety or restless that they had been moving around a lot more than usual; and having thoughts that they would be better off dead or thoughts of hurting themselves in some way (all P < 0.05). The level of subjective stress was higher in the 2019 group than in the 2020 group (P < 0.001). The distribution of region of residence was not different between the 2019 group and the 2020 group (P = 0.012). Age, BMI, frequency of alcohol consumption, and the rate of hypertension were higher in the 2019 group than in the 2020 group (all P < 0.001). On the other hand, income, sleep duration, education level, and the rate of diabetes mellitus were higher in the 2020 group than in the 2019 group (all P < 0.001).
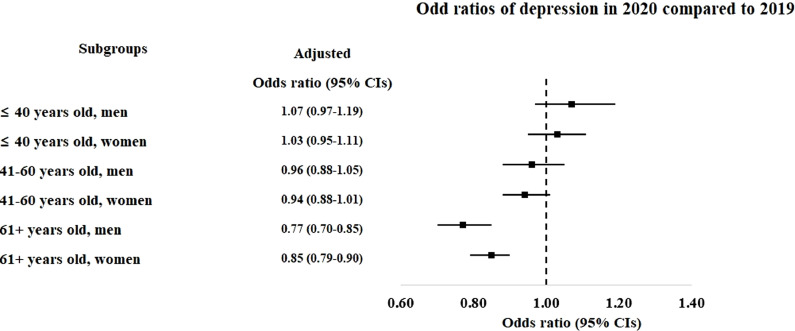
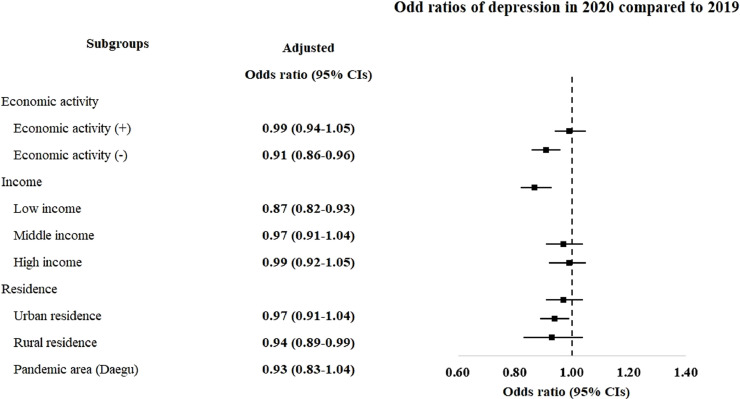
The 2020 group had a lower odds of experiencing depression (adjusted OR [aOR] = 0.95, 95% CI = 0.91–0.98, P = 0.004, Fig. 2 and Table S2). Among the age and sex subgroups, the older age groups (> 60 years old) showed lower odds of experiencing depression in the 2020 group than in the 2019 group (aOR = 0.77, 95% CI = 0.70–0.85, P < 0.001 for > 60-year-old men and aOR = 0.85, 95% CI = 0.79–0.90, P < 0.001 for > 60-year-old women). The negative association of depression with the 2020 group was maintained without adjusting income levels (Fig. 3 and Table S3). Compared to the 2019 group, the 2020 group demonstrated lower odds for depression without considering income levels (aOR = 0.95, 95% CI = 0.92–0.99, P = 0.017). The subgroups without economic activity, low income level, and rural residence showed lower odds for depression in the 2020 group than the 2019 group.
Fig. 2.
Odd ratios of depression in 2020 compared to 2019 in total participants and subgroup by age and sex.
Fig. 3.
Odd ratios of depression in 2020 compared to 2019 in subgroup age economic activity, income level, and region of residence.
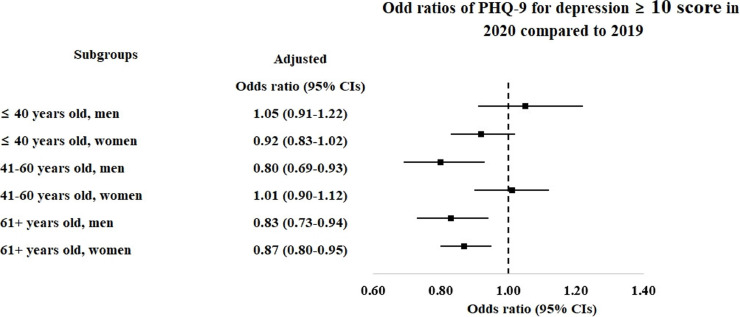
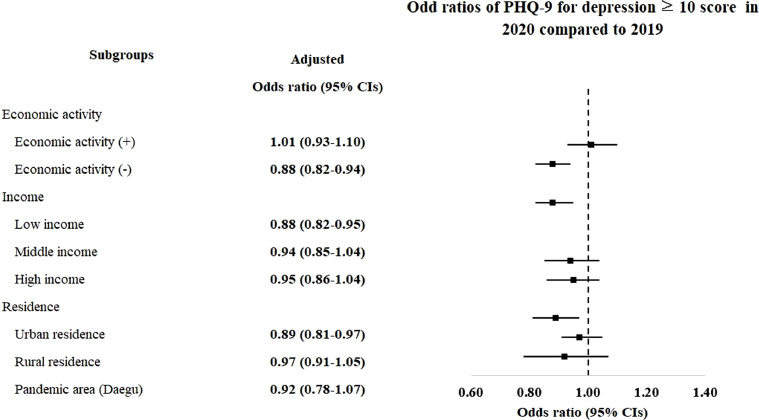
The odds for moderate to severe depression were also lower in the 2020 group (aOR = 0.92, 95% CI = 0.88–0.97, P = 0.001, Fig. 4 and Table S4). The 41–60-year-old male group showed lower odds of moderate to severe depression in the 2020 group than in the 2019 group (aOR = 0.80, 95% CI = 0.69–0.93, P = 0.004). Both > 60-year-old men and > 60-year-old women demonstrated lower odds for moderate to severe depression in the 2020 group than in the 2019 group (aOR = 0.83, 95% CI = 0.73–0.94, P < 0.004 for > 60-year-old men and aOR = 0.87, 95% CI = 0.80–0.95, P = 0.002 for > 60-year-old women). The negative association of moderate to severe depression with the 2020 group was consistent without adjusting income level (aOR = 0.94, 95% CI = 0.89–0.99, P = 0.014, Fig. 5 and Table S5). The subgroups without economic activity, low income, and urban residence showed lower odds for moderate to severe depression in the 2020 group.
Fig. 4.
Odd ratios of PHQ-9 for depression ≥ 10 score in 2020 compared to 2019 in total participants and subgroup by age and sex.
Fig. 5.
Odd ratios of PHQ-9 for depression ≥ 10 score in 2020 compared to 2019 in subgroup age economic activity, income level, and region of residence.
4. Discussion
The rate of depression was not increased during the COVID-19 pandemic in the Korean population. The COVID-19 pandemic was associated with a lower rate of depression. In particular, the older population demonstrated a lower rate of depression during the COVID-19 pandemic. This study extended previous findings by analyzing a large study population and considering many potential covariables, which alleviated possible confounding effects.
A number of clinical studies have described the high level of depression during the COVID-19 pandemic (Wang et al., 2020). Approximately 16.5% of participants were reported to suffer from moderate to severe depressive symptoms during the initial stage of the COVID-19 pandemic in China (Wang et al., 2020). Moreover, several previous studies reported an initial increase and then decreases in depressive distress during the COVID-19 crisis (Daly and Robinson, 2021b; Robinson and Daly, 2021; Daly and Robinson, 2021a). In US study, the PHQ-4 score was found to increase by 0.27 standard deviations (SD) (95% CI = 0.23–0.31, P < 0.001) during the initial phase of the COVID-19 crisis (from March 10 to April 14, 2020) and then decrease by 0.31 SD (95% CI = 0.27–0.34, P < 0.001) by June 2020 (Daly and Robinson, 2021b). In a UK study, the level of psychological distress measured by the General Health Questionnaire-12 initially increased until June 2020 (26.9%, 95% CI = 25.4–28.3) and then decreased to the prepandemic level in July 2020 (21.4%, 95% CI = 20.1–22.7) (Daly and Robinson, 2021a). A few mediating factors were identified in a longitudinal study, including perceived risk of infection (decreased by 7.33%, 95% CI = 6.38–8.28), perceived risk of death (decreased by 5.43%, 95% CI = 4.56–6.28), perceived financial risk (decreased by 6.33%, 95% CI = 5.22–7.43), and perceived discrimination (decreased by 4.44%, 95% CI = 2.95–5.94) (Robinson and Daly, 2021). Resilience to the COVID-19 pandemic could have been induced by the effect of the honeymoon period and social support (Blanc et al., 2021).
The early phase of the COVID-19 pandemic may have been a honeymoon period in terms of psychological response. The psychological response to the COVID-19 pandemic was reported to follow a sequence of the preimpact, impact, heroic, honeymoon, disillusionment, and recovery phases (Everly et al., 2021). The honeymoon phase was defined as a period of hopefulness and optimism due to social connectedness (Benedek et al., 2017). A spirit of community bonding was developed based on common experience and collaborative management strategies against the COVID-19 pandemic (Kolves et al., 2013). Social support and government management systems for COVID-19 may have attenuated possible negative emotional factors and COVID-19-related stress in our cohort population. A cross-sectional study in Spain found that social networks and resilience were associated with increased positive emotions and decreased negative emotions (Facal et al., 2021). In a cross-sectional qualitative survey, it was found the Korean population accepted, endured, and adapted to lifestyle changes during the strong quarantine measures and social distancing in the COVID-19 pandemic period, although they also expressed boredom and fear of SARS-CoV-2 infection (Kim et al., 2021b).
The relatively low rate of contraction of COVID-19 in the Korean population may have attenuated the psychological impact of COVID-19 in the present study. From January 20, 2020, to December 31, 2020, the cumulative number of SARS-CoV-2 infections was calculated to be 61,758 among the 51 million people in the entire Korean population, which accounted for only 0.12%. The social distancing policy was stratified according to the number of infected patients with COVID-19 and minimized the lockdown of economic and social activities in Korea. Although there have been some limitations on social gatherings or private meetings, social isolation was prevented by online communication and work from home. Because there was no industrial shut down, Koreans did not encounter grocery shortages or daily necessities. Medical accessibility and resources were supported enough to cover the COVID-19 crisis. Thus, there was no collapse of medical facilities in Korea.
The older age group demonstrated an association of the pandemic era with a lower risk of depression in this study. The elderly population is a high-risk group for both COVID-19 and depression (Lee et al., 2020a). Pandemic-associated factors, such as social restraint, social distancing, and isolation, could increase the risk of depression, especially in elderly individuals (Lee et al., 2020a; Armitage and Nellums, 2020). However, resilience to these factors has been suggested to be higher in elderly individuals (Morales-Vives et al., 2020). Regarding differences according to sex, middle-aged men, but not women, showed lower odds of depression in this study. A cross-sectional study described that during the lockdown period to control the COVID-19 outbreak in Spain, women tended to have greater stress, higher levels of extraversion and neuroticism, and lower self-esteem, which were estimated using a general health questionnaire, a satisfaction with life scale, and a subjective happiness scale, than men (all P < 0.001) (Morales-Vives et al., 2020). In addition to having a large amount of life experience and wisdom, most individuals in the older population are not engaged in economic activities and are retired, so they may be less influenced by unemployment or a decreased salary due to COVID-19 outbreak than the economically active population. Moreover, economic support by the Korean government may have attenuated the economic difficulties and social isolation of the older population.
This study used a large representative population cohort. The quality of the cohort data was guaranteed by the KCDC. Moreover, demographic factors, socioeconomic factors, lifestyle-related variables, and comorbidities were extensively collected and adjusted for the analyses. Depression was surveyed using two methods, namely, an indicator of the experience of depression and the PHQ-9 score. The impact of the COVID-19 pandemic on the presence of depression was consistent in both measures of depression. However, a few limitations need to be considered in the interpretation of the present results. This study could not follow each participant for changes in depression. The 2019 group and 2020 group were independently enrolled each year. In addition, the severity of depression and treatment histories of depression could not be specified. Although many covariables were considered, there may be some variables that could influence the association of the COVID-19 pandemic and depression, such as marital status, occupation, and number of family members. This study used a Korean population cohort, but there may be ethnic and regional differences in the relationship between the COVID-19 pandemic and depression (Kim and Kim, 2020). Last, the participants were surveyed during the early COVID-19 pandemic period; therefore, the delayed impact of the COVID-19 pandemic on depression needs to be studied in future studies.
In conclusion, depression was not higher during the COVID-19 pandemic than during the prepandemic period in Korea. The elderly population showed a lower rate of depression during the COVID-19 pandemic than during the prepandemic period, which indicated their resilience in coping with the potential risk of depression during the COVID-19 pandemic.
CRediT authorship contribution statement
So Young Kim: Investigation, Software, Validation, Writing – original draft, Writing – review & editing. Dae Myoung Yoo: Data curation, Formal analysis, Visualization, Writing – review & editing. Chanyang Min: Data curation, Formal analysis, Writing – review & editing. Hyo Geun Choi: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing.
Declaration of Competing Interest
The authors declared that there is no conflicts of interests.
Acknowledgements
This work was supported in part by a research grant (NRF-2018-R1D1A1A0–2085328; NRF-2021-R1C1C1004986) from the National Research Foundation (NRF) of Korea.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.12.107.
Appendix. Supplementary materials
References
- Armitage R., Nellums L.B. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5:e256. doi: 10.1016/S2468-2667(20)30061-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauerle A., Teufel M., Musche V., Weismuller B., Kohler H., Hetkamp M., Dorrie N., Schweda A., Skoda E.M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J. Public Health. 2020;42:672–678. doi: 10.1093/pubmed/fdaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benedek D.M., Morganstein J.C., Holloway H.C., Ursano R.J. Lippincott Williams & Wilkins; Baltimore: 2017. Disaster Psychiatry: Disasters, Terrorism, and War. [Google Scholar]
- Blanc J., Briggs A.Q., Seixas A.A., Reid M., Jean-Louis G., Pandi-Perumal S.R. Addressing psychological resilience during the coronavirus disease 2019 pandemic: a rapid review. Curr. Opin. Psychiatry. 2021;34:29–35. doi: 10.1097/YCO.0000000000000665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Robinson E. Longitudinal changes in psychological distress in the UK from 2019 to September 2020 during the COVID-19 pandemic: evidence from a large nationally representative study. Psychiatry Res. 2021;300 doi: 10.1016/j.psychres.2021.113920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly M., Robinson E. Psychological distress and adaptation to the COVID-19 crisis in the United States. J. Psychiatr. Res. 2021;136:603–609. doi: 10.1016/j.jpsychires.2020.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everly G.S., Wu A.W., Potash J.B. Phases of psychological response in COVID-19: a preliminary heuristic. Am. J. Disaster Med. 2021;16:5–12. doi: 10.5055/ajdm.2021.0381. [DOI] [PubMed] [Google Scholar]
- Facal D., Rodriguez-Gonzalez R., Martinez-Santos A.E., Gandoy-Crego M. Positive and negative feelings among spanish young-old and old-old during the lockdown of the COVID-19 first wave. Clin. Gerontol. 2021:1–5. doi: 10.1080/07317115.2021.1929633. [DOI] [PubMed] [Google Scholar]
- Han C., Jo S.A., Kwak J.H., Pae C.U., Steffens D., Jo I., Park M.H. Validation of the patient health questionnaire-9 Korean version in the elderly population: the Ansan Geriatric study. Compr. Psychiatry. 2008;49:218–223. doi: 10.1016/j.comppsych.2007.08.006. [DOI] [PubMed] [Google Scholar]
- Hyun J., You S., Sohn S., Kim S.J., Bae J., Baik M., Cho I.H., Choi H., Choi K.S., Chung C.S., Jeong C., Joo H., Kim E., Kim H., Kim H.S., Ko J., Lee J.H., Lee S.M., Lee S.H., Chung U.S. Psychosocial support during the COVID-19 outbreak in Korea: activities of multidisciplinary mental health professionals. J. Korean Med. Sci. 2020;35:e211. doi: 10.3346/jkms.2020.35.e211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang Y.W., Ko Y.S., Kim Y.J., Sung K.M., Kim H.J., Choi H.Y., Sung C., Jeong E. Korea community health survey data profiles. Osong Public Health Res. Perspect. 2015;6:211–217. doi: 10.1016/j.phrp.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J., Ashihara K. National disaster management system: COVID-19 case in Korea. Int. J. Environ. Res. Public Health. 2020;17(18) doi: 10.3390/ijerph17186691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J.H., Ahn J.H., Min C.Y., Yoo D.M., Choi H.G. Association between sleep quality and subjective cognitive decline: evidence from a community health survey. Sleep Med. 2021;83:123–131. doi: 10.1016/j.sleep.2021.04.031. [DOI] [PubMed] [Google Scholar]
- Kim J., Kim Y., Ha J. Changes in daily life during the COVID-19 pandemic among south korean older adults with chronic diseases: a qualitative study. Int. J. Environ. Res. Public Health. 2021;18(13):6781. doi: 10.3390/ijerph18136781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.Y., Kim D.W. Does the clinical spectrum of coronavirus disease 2019 (COVID-19) show regional differences? Clin. Exp. Otorhinolaryngol. 2020;13:83–84. doi: 10.21053/ceo.2020.00612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.Y., Sim S., Choi H.G. Active and passive smoking impacts on asthma with quantitative and temporal relations: a Korean Community Health Survey. Sci. Rep. 2018;8:8614. doi: 10.1038/s41598-018-26895-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolves K., Kolves K.E., De Leo D. Natural disasters and suicidal behaviours: a systematic literature review. J. Affect. Disord. 2013;146:1–14. doi: 10.1016/j.jad.2012.07.037. [DOI] [PubMed] [Google Scholar]
- Korea Disease Control and Prevention Agency. http://kdca.go.kr/index.es?sid=a3.2021.
- Lee K., Jeong G.C., Yim J. Consideration of the psychological and mental health of the elderly during COVID-19: a theoretical review. Int. J. Environ. Res. Public Health. 2020;17(21) doi: 10.3390/ijerph17218098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.W., Yang J.M., Moon S.Y., Yoo I.K., Ha E.K., Kim S.Y., Park U.M., Choi S., Lee S.H., Ahn Y.M., Kim J.M., Koh H.Y., Yon D.K. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry. 2020;7:1025–1031. doi: 10.1016/S2215-0366(20)30421-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim M.S., Park B., Kong I.G., Sim S., Kim S.Y., Kim J.H., Choi H.G. Leisure sedentary time is differentially associated with hypertension, diabetes mellitus, and hyperlipidemia depending on occupation. BMC Public Health. 2017;17:278. doi: 10.1186/s12889-017-4192-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Guo L., Yu M., Jiang W., Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public - a systematic review and meta-analysis. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morales-Vives F., Duenas J.M., Vigil-Colet A., Camarero-Figuerola M. Psychological variables related to adaptation to the COVID-19 lockdown in Spain. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.565634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park C., Hwang J.M., Jo S., Bae S.J., Sakong J. COVID-19 outbreak and its association with healthcare workers' emotional stress: a cross-sectional study. J. Korean Med. Sci. 2020;35:e372. doi: 10.3346/jkms.2020.35.e372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J.H., Jang W., Kim S.W., Lee J., Lim Y.S., Cho C.G., Park S.W., Kim B.H. The clinical manifestations and chest computed tomography findings of coronavirus disease 2019 (COVID-19) patients in China: a proportion meta-analysis. Clin. Exp. Otorhinolaryngol. 2020;13:95–105. doi: 10.21053/ceo.2020.00570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E., Daly M. Explaining the rise and fall of psychological distress during the COVID-19 crisis in the United States: longitudinal evidence from the Understanding America Study. Br. J. Health Psychol. 2021;26:570–587. doi: 10.1111/bjhp.12493. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang S., Kwak S.G., Ko E.J., Chang M.C. The mental health burden of the COVID-19 pandemic on physical therapists. Int. J. Environ. Res. Public Health. 2020;17(10):3723. doi: 10.3390/ijerph17103723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W., Investigating China Novel Coronavirus, and Team Research A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.