To the Editor: Although regional anesthesia provides prolonged post-operative analgesia, there is no suitable method that can facilitate an early reversal of the blockade until the duration of action of the local anesthetic has elapsed. A large quantity of saline is used to reverse the central neuraxial block.[1,2] However, to our knowledge, no study has reported a method for reversing nerve blockade in peripheral nerve blocks, especially costoclavicular blocks. Herein, we report a case of dramatic recovery of both motor and sensory functions after saline injection through the catheter in a patient who was administered a continuous costoclavicular block for analgesia after shoulder surgery.
A 75-year-old man underwent right shoulder rotator cuff repair under general anesthesia. A continuous costoclavicular block was administered for post-operative analgesia after standard monitoring. The position of the axillary artery and vein and three cords of the brachial plexus was confirmed using 5- to 12-MHz linear probe ultrasonography, followed by injection of 0.375% ropivacaine (10 mL) using the in-plane technique, in a medial to the lateral direction. A continuous catheter (18 G, 51 mm; E-Cath, Pajunk, Germany) was inserted between the lateral cord and fascia above the medial and posterior cord in the costoclavicular space under real-time ultrasonographic guidance. The position of the catheter was confirmed with a 10-mL residual volume. General anesthesia was maintained with desflurane and remifentanil. Perineural patient-controlled analgesia (PCA) (0.75% ropivacaine 70 mL, normal saline 240 mL, epinephrine 1 mg) was continuously infused at 6 mL/h, with a 4-mL bolus dose and lockout time interval of 30 min at the end of surgery. The patient developed mild discomfort due to immobility of the right arm in the post-anesthesia care unit. However, this was thought to have occurred because of the blockade induced by the initial injection, and the patient was shifted to the general ward.
The post-operative pain was well-controlled without the need of a rescue drug or PCA bolus button at the time of consultation with the acute pain service (APS) team, approximately 25 h post-operatively. The pain score at that time was 0 on the visual analog scale (VAS). Proprioception along the median, ulnar, radial, and musculocutaneous nerves was absent. He was unable to move his arm and fingers, which showed signs of a complete anesthesia.
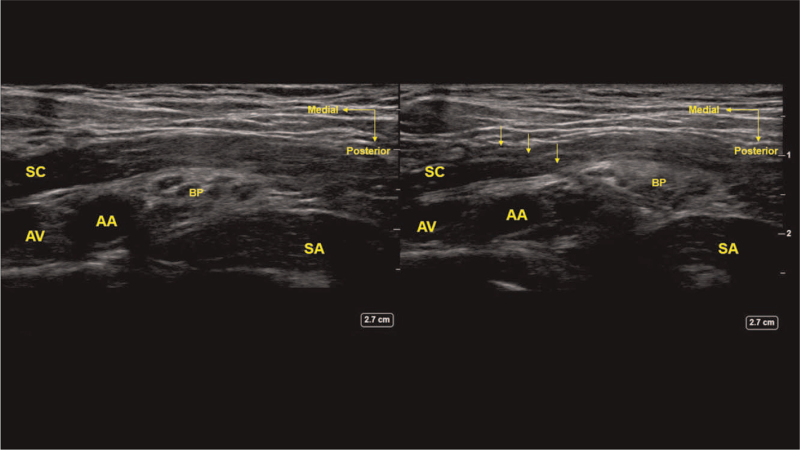
The APS team shifted the patient to the block room to examine the location of the catheter and nerve swelling, as they suspected the presence of nerve injury. Real-time ultrasonography confirmed that the catheter had not penetrated the cords of the brachial plexus, but could not detect the end of the catheter because of post-operative swelling in the surrounding tissue. Thus, a small amount of saline (total volume: 15 mL) was injected several times to confirm the pattern of spread and the absence of nerve swelling due to injection. The APS team reassured the patient that his motor function would recover after the cessation of PCA. There were no signs of the needle- and catheter-induced nerve damage [Figure 1].
Figure 1.
Ultrasound image of the continuous costoclavicular block. AA: Axillary artery; Arrows: Catheter; AV: Axillary vein; BP: Brachial plexus; SA: Serratus anterior muscle; SC: Subclavius muscle.
After being transferred to the general ward, the surgeon reported that the patient's arm was repositioned and pulled several times because of poor positioning during surgery. We decided to perform a neurological examination as we suspected traction injury and asked the ward personnel to stop the PCA. However, the patient could move his hands and complained of pain at the surgical site, immediately after being transferred to the general ward, and requested that the PCA should not be stopped. Hence, we examined the patient again in the general ward. The patient reported a VAS score of 3 to 4 during the physical examination. Dramatic reversal to normal sensory and motor function was observed, except for the tingling sensation in the superficial radial nerve. The patient did not want an additional bolus of local anesthetic owing to the discomfort caused by motor paresis and PCA was resumed. The PCA catheter was removed after post-operative day 3. No complications, including neurological symptoms, were observed after follow-up in the outpatient department after 1 week.
Our patient's motor and sensory function recovered rapidly within approximately 15 min after the injection of 15 mL of saline. We hypothesized the following mechanism to provide a plausible explanation for this phenomenon. The patient received a 15-mL saline injection into the costoclavicular space, which could have further lowered the concentration of the local anesthetic. This dilutional effect could have increased the concentration gradient between the neuronal membranes, which is believed to normalize nerve conduction of the motor and sensory nerves by reducing the intraneuronal concentration of the local anesthetic below the threshold concentration.[3,4] Moreover, we believe that saline injection increased the sodium concentration or gradient around the nerve, which caused an alteration in the pH and ionization levels.[5] Our patient had been injected with approximately 0.2% (low concentration) ropivacaine. Thus, the intraneural concentration fell below the threshold within a short duration of time.
To conclude, we observed a dramatic reversal of sensory and motor nerve blockade within a short time following 0.9% saline injection after a costoclavicular block. Our findings suggest that saline injection can be used to reverse the local anesthesia induced by the costoclavicular block. Further studies are needed to verify this effect.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that his name and initial will not be published, and due efforts will be made to conceal his identity but anonymity cannot be guaranteed.
Conflicts of interest
None.
Footnotes
How to cite this article: Chung J, Bang S, Lee Y, Kwon W, Chung K. Novel saline injection technique for the reversal of the continuous costoclavicular block. Chin Med J 2021;134:3023–3024. doi: 10.1097/CM9.0000000000001774
References
- 1.Rodríguez J, Rodríguez V, Naveira A, Quintela O, Bárcena M, Gallardo E, et al. Epidural washout with high volumes of saline to accelerate recovery from epidural anaesthesia. Acta Anaesthesiol Scand 2001; 45:893–898. doi: 10.1034/j.1399-6576.2001.045007893.x. [DOI] [PubMed] [Google Scholar]
- 2.Park EY, Kil HK, Park WS, Lee NH, Hong JY. Effect of epidural saline washout on regression of sensory and motor block after epidural anaesthesia with 2% lidocaine and fentanyl in elderly patients. Anaesthesia 2009; 64:273–276. doi: 10.1111/j.1365-2044.2008.05746.x. [DOI] [PubMed] [Google Scholar]
- 3.Fleming IO, Boddu K. Novel technique for reversing phrenic nerve paresis secondary to interscalene brachial plexus block. S Afr J Anaesth Analg 2018; 24:86–89. doi: 10.1080/22201181.2018.1461318. [Google Scholar]
- 4.Byrne KP, Smith CL, Termaat J, Tsui BCH. Reversing the effects of a peripheral nerve block with normal saline: a randomised controlled trial. Turk J Anaesthesiol Reanim 2020; 48:115–119. doi: 10.5152/tjar.2019.09076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ibusuki S, Katsuki H, Takasaki M. The effects of extracellular pH with and without bicarbonate on intracellular procaine concentrations and anesthetic effects in crayfish giant axons. Anesthesiology 1998; 88:1549–1557. doi: 10.1097/00000542-199806000-00019. [DOI] [PubMed] [Google Scholar]