Abstract
Fibrosing mediastinitis (FM) is a rare fibroinflammatory disease of the mediastinum with an etiology and clinical features that vary by world region. The characteristics of FM in Japan are still unknown. We herein report two Japanese patients with FM who were treated with corticosteroids and responded well. We also reviewed the Japanese literature on PubMedⓇ and summarized the characteristics of 27 Japanese FM patients, including our two patients. In Japan, the predominant cases were those without a specific cause, were diffusely distributed, and responded well to corticosteroid therapy.
Keywords: fibrosing mediastinitis, sclerosing mediastinitis, mediastinal fibrosis, corticosteroid therapy, Japanese
Introduction
Fibrosing mediastinitis (FM), also known as sclerosing mediastinitis or mediastinal fibrosis, is a rare disease characterized by the proliferation of fibrous tissue within the mediastinum (1). Patients with FM may present with symptoms of compression and obstruction of the mediastinal structures including the superior vena cava (SVC), pulmonary vessels, tracheobronchial airways, and esophagus (2).
The etiology of FM can be divided into idiopathic and secondary. The causes of secondary FM include granulomatous infections (histoplasmosis, tuberculosis, aspergillosis, blastomycosis, or other fungal infections), sarcoidosis, and mediastinal irradiation (3). Many reviews from the United States show that the most common cause is histoplasmosis (4). The causes of FM differ depending on the world region. In some reviews, sarcoidosis was the most common cause in France (5), whereas in China, many cases were related to tuberculosis (6). Except in the United States, patients in the reviews were seldom associated with histoplasmosis. When no specific cause can be found, FM is classified as idiopathic. The pathogenesis of idiopathic FM is unknown, but many case reports describe the pathophysiology of FM as being related to autoimmune disease or idiopathic fibroinflammatory disorders (3). Examples of autoimmune disease include anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis, Behçet disease, and large-vessel arteritis. Examples of idiopathic fibroinflammatory disorders include retroperitoneal fibrosis, sclerosing cholangitis, and Riedel thyroiditis, and these may coexist with IgG4-related disease (1,3).
Depending on the etiology, the medical features of FM vary in terms of symptoms, extent of lesions, response, and outcome. It is believed that there is no curative treatment for FM, so the purpose of treatment is to relieve symptoms and avoid life-threatening situations by using vascular or airway stents or performing surgery (1,7). Corticosteroid therapy is not considered to benefit the typical FM patient (1,2,8). Some cases of FM have been reported in Japan, but the characteristics of FM in Japan remain unknown.
We herein report two cases of FM and review the Japanese literature on FM to compare the features, etiologies, and treatments with those of other countries.
Case Reports
Case 1
A 62-year-old woman was admitted to our hospital with a 3-month history of dull back pain. Her medical history was unremarkable. Her physical examination was normal, and she had no fever. Chest computed tomography (CT) showed a diffuse mass surrounding the descending aorta and the thoracic and lumbar spine (Fig. 1a, b). The lymph nodes were free of calcification. Gallium-67 scintigraphy showed accumulation in the mass (Fig. 1c). Laboratory examinations revealed an elevated erythrocyte sedimentation rate of 84 mm/h and C-reactive protein (CRP) level of 8.17 mg/dL. IgG4 and tumor markers were within the normal range. Her serologic tests were negative for anti-histoplasma antibody and interferon-γ release assay (IGRA).
Figure 1.
(a, b) Chest computed tomography (CT) showed a diffuse mass surrounding the descending aorta and the thoracic and lumbar spine. (c) Gallium-67 scintigraphy showed accumulation in the mass. (d) CT showed the recurrence of lesions around the descending aorta 4 months after discontinuation of corticosteroids.
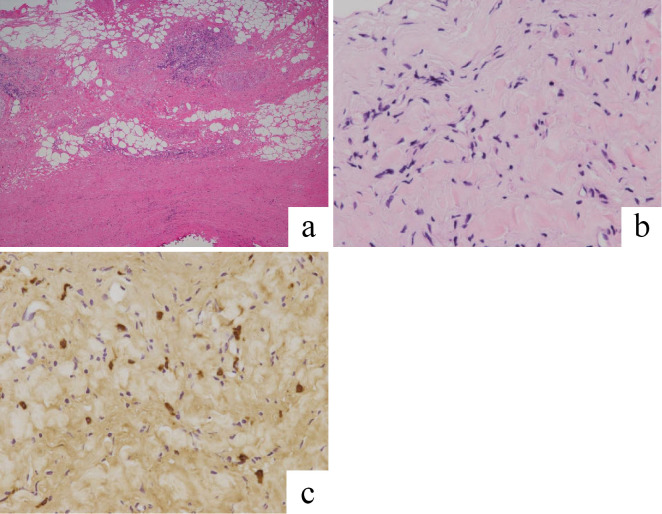
A thoracoscopic surgical biopsy was performed to obtain a histological diagnosis. Biopsy specimens revealed diffuse fibrotic lesions with hyalinization and the focal infiltration of lymphocytes (Fig. 2a, b). No neoplastic lesions or granulomas were observed. Immunostaining for IgG4 is shown in Fig. 2c. The IgG4+/CD138+ plasma cell ratio was about 3%, so we judged the specimen to not be immunoreactive for IgG4. Therefore, the pathological diagnosis was FM.
Figure 2.
(a, b) A thoracoscopic biopsy specimen revealed diffuse fibrotic lesions with hyalinization and focal infiltration of lymphocytes. Hematoxylin and Eosin staining (a: ×20, b: ×200). (c) The specimen was not immunoreactive for IgG4 (×200).
Corticosteroid treatment (prednisolone 30 mg/day) was started. Thereafter, her back pain improved, and her CRP level returned to the normal range. CT showed a reduction in the size of the mediastinal mass. She continued on low-dose corticosteroids for about 3 years but discontinued them due to her good health condition. However, after 4 months, the lesions and symptoms recurred (Fig. 1d), and her CRP level rose to 2.67 mg/dL. Corticosteroid treatment (prednisolone 10 mg/day) was restarted, which relieved her symptoms and improved the mediastinal lesions. She then continued to take prednisolone 5 mg/day, and her symptoms have remained stable for about one year after restarting the corticosteroid treatment.
Case 2
A 77-year-old man was admitted to our hospital because a routine medical checkup revealed an abnormal mediastinal contour on his chest X-ray. His medical history was unremarkable. His medical examination was normal, and he was afebrile. CT showed a diffuse mass surrounding the aortic arch and thoracic vertebrae and a discontinuous retroperitoneal mass along the bilateral common iliac arteries (Fig. 3a-c). There were no calcifications in the lymph nodes. 18F-fluorodeoxyglucose-positron emission tomography-CT showed accumulation in the mass (standardized uptake value max: 4.97) (Fig. 3d). Laboratory tests revealed elevated levels of IgG of 2,675 mg/dL and IgG4 of 487 mg/dL. CRP and tumor markers were within normal limits. Autoimmune antibodies were negative, as were his serologic tests for anti-histoplasma antibody.
Figure 3.
(a, b) Chest computed tomography (CT) showed a diffuse mass surrounding the aortic arch and thoracic vertebrae. (c) Abdominal CT showed a discontinuous retroperitoneal mass along the bilateral common iliac arteries. (d) 18F-fluorodeoxyglucose-positron emission tomography-CT showed accumulation in the mass.
A thoracoscopic surgical biopsy was performed to obtain a histological diagnosis. Biopsy specimens revealed diffuse fibrotic lesions with hyalinization and the focal infiltration of lymphocytes (Fig. 4a, b). No neoplastic lesions or granulomas were observed. Immunostaining for IgG4 is shown in Fig. 4c. The IgG4+/CD138+ plasma cell ratio was about 8%, so we judged the specimen to not be immunoreactive for IgG4. Therefore, the pathological diagnosis was FM.
Figure 4.
(a, b) A thoracoscopic biopsy specimen revealed diffuse fibrotic lesions with hyalinization and focal infiltration of lymphocytes. Hematoxylin and Eosin staining (a: ×20, b: ×200). (c) The specimen was not immunoreactive for IgG4 (×200).
Corticosteroid treatment (prednisolone 30 mg/day) was started. After that, CT showed a reduction in the size of the mediastinal and retroperitoneal lesions. Thereafter, the dose of prednisolone was reduced to 3 mg/day, and the mediastinal lesions have not relapsed for about 5 years after onset.
Discussion
We herein describe two cases of FM diagnosed by thoracoscopic biopsy. In both cases, the lesions were located along the aorta and spine, did not compress or obstruct mediastinal organs such as blood vessels, trachea, and esophagus, and responded well to corticosteroid therapy. The etiologies of both cases could not be identified.
FM is considered to be a clinicopathologic syndrome rather than a single disease (2). Many etiologies cause an excessive fibrotic reaction in the mediastinum. The cause of FM clearly relates to the area of the world from which it was reported, and each etiology can produce different phenotypic variations. Therefore, the FM characteristics may vary depending on the region. For example, a case series from the United States described 86 FM patients with 71 clinical and 15 histological diagnoses (2). The median age was 42 years and 54% were female. Only 5% were asymptomatic, and 83% had conclusive or suggestive evidence of histoplasmosis. Among the therapeutic interventions, 6% of patients received corticosteroids, 19% underwent nonsurgical intervention, and 21% underwent surgical treatment. Anti-inflammatory therapies including corticosteroids provided little benefit. In a French study reviewing 27 FM patients with pulmonary hypertension, the etiology was sarcoidosis in 13 (48%), confirmed or estimated tuberculosis in 9 (33%), and idiopathic in 3 (11%) (5). Twelve patients (44%) received corticosteroids. A case series in China reported on 20 FM patients (6). Their average age was 69.5 years and 60% were female. Among them, 40% had a history of old tuberculosis, 20% were diagnosed as having a latent tuberculosis infection based on the results of IGRA, with the strong involvement of tuberculosis, 45% received anti-tuberculosis drugs, and only 5% received corticosteroids. The therapeutic effect of corticosteroids was poor. As these examples illustrate, the clinical picture of FM depends on the area in which it occurs.
To date, the characteristics of Japanese FM patients are still unclear. We therefore conducted a comprehensive search of the literature on MEDLINEⓇ/PubMedⓇ from 1992 to May 2020, using the terms “fibrosing mediastinitis”, “sclerosing mediastinitis”, and “mediastinal fibrosis”. We thus found 25 case reports of Japanese patients with FM (9-32). The clinical characteristics of the 27 Japanese patients with FM, including the two present cases, are summarized in Table. We excluded some articles in commercial journals from medical publishers or case reports with an unclear clinical course. Regarding the distribution of the disease, we followed Sherrick's criteria (33), in which a pattern showing a localized soft-tissue mass is classified as localized type, and a pattern showing a diffuse homogenous soft-tissue process throughout the mediastinum is classified as diffuse type. The median age at diagnosis was 61 years, and 14 of the 27 patients (52%) were male. The main complaints were chest and back pain, face-to-arm swelling, dyspnea, and hoarseness, but 8 of the 27 (30%) were asymptomatic. Regarding distribution, 17 cases (63%) were of the diffuse type. Only one patient (case 6) had a history of old tuberculosis suffered 40 years ago, and the relationship between FM and tuberculosis was unknown. Four patients tested for IGRA received negative results. Nine of the 27 (33%) were tested for histoplasmosis, 5 had serological antibody tests, and 5 had immunostaining of histological specimens, but all results were negative. Six patients (22%) were serologically or histologically IgG4 positive. Serum IgG4 was measured in 9 patients and ranged from 7.9 to 1,940 mg/dL. When the serum IgG4 cutoff value was set at 135 mg/dL (34), 5 of the patients were positive. Of the 10 patients with histological staining of IgG4, 5 were pathologically diagnosed as having IgG4-related FM. In one patient (case 21), because serum myeloperoxidase-ANCA was positive, FM was suspected to be related to ANCA. A specific etiology was not detected in 20 of the 27 patients (74%). The main treatment was corticosteroid therapy, which was administered to 18 patients (67%), of whom 13 responded well, 3 partially responded (i.e., improvements in symptoms and lesion size were described as mild or partial), and 2 patients (case 2 and case 13 with chylous effusion) did not respond at all.
Table.
Characteristics of 27 Japanese Cases of Fibrosing Mediastinitis.
| Case | Age | Sex | Main symptoms | Location | Histological stage | Histoplasma (Serum Ab/Tissue) | Serum IgG4 (mg/dL) | Immunostaining of IgG4 | Serum CRP (mg/dL) | Symptomatic compressed organs | Main treatment | Outcome/ Recurrence | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 32 | M | Facial swelling, neck tightening | Diffuse | NA | NA | NA | NA | 2.23 | SVC | Bypass surgery | Improved | 9 |
| 2 | 54 | M | Dyspnea, leg edema | Diffuse | NA | NA | NA | NA | Elevated | Thoracic duct | Steroid | Not improved | 10 |
| 3 | 28 | F | Chest pain, left shoulder pain, hoarseness | Diffuse | NA | NA | NA | NA | NA | Nerves | Resection, steroid, tranilast | Improved | 11 |
| 4 | 51 | F | Fever | Local | NA | NA | NA | NA | 6.8 | No | Resection | Improved | 12 |
| 5 | 56 | M | Dyspnea | Diffuse | NA | NA | NA | NA | 7.66 | No | Steroid | Partially improved | 13 |
| 6 | 68 | M | Hoarseness | Diffuse | II | NA/negative | NA | NA | 6.69 | Nerves | Steroid | Improved | 14 |
| 7 | 63 | F | Facial swelling | Local | NA | NA | NA | NA | NA | SVC | Resection, bypass surgery | Improved/partially recurred | 15 |
| 8 | 62 | M | Headache, face and right shoulder swelling | Local | NA | NA | NA | NA | NA | SVC | Balloon dilatation, stenting | Improved/partially recurred | 16 |
| 9 | 7 | M | None | Local | II | Negative/NA | NA | NA | NA | No | Medical observation | Stable | 17 |
| 10 | 67 | F | Fever | Local | NA | NA | NA | NA | NA | No | Resection | Improved | 18 |
| 11 | 52 | M | Back pain | Diffuse | NA | NA | 392* | Positive | 9.3 | No | Steroid | Improved | 19 |
| 12 | 65 | F | Hoarseness | Diffuse | NA | NA/negative | NA | NA | 0.4 | Nerves | Steroid | Improved | 20 |
| 13 | 61 | M | None | Diffuse | NA | NA | 583* | Positive | NA | Ureter | Steroid | Improved | 21 |
| 14 | 75 | F | Left neck swelling | Diffuse | NA | NA/negative | NA | NA | NA | Carotid artery | Steroid | Improved | 22 |
| 15 | 56 | F | Dyspnea | Diffuse | NA | NA | 127 | Positive | NA | Main bronchus | Steroid | Improved | 23 |
| 16 | 54 | M | None | Local | NA | NA | NA | NA | NA | No | Resection | Stable | 24 |
| 17 | 68 | M | Intermittent claudication | Diffuse | NA | NA | NA | NA | 0.26 | Iliac artery | Steroid, saireito | Partially improved | 25 |
| 18 | 28 | M | Dyspnea | Local | NA | Negative/negative | 20.9 | Negative | NA | Thoracic duct | Steroid, octreotide | Improved (steroid ineffective) | 26 |
| 19 | 36 | M | Abdominal pain | Local | II | Negative/NA | NA | NA | 5.2 | No | Resection | Improved | 27 |
| 20 | 54 | M | Chest pain, dyspnea | Diffuse | II | NA | NA | Negative | 0.07 | Pulmonary artery, main bronchus | Steroid | Partially improved | 28 |
| 21 | 52 | F | Malaise, weight loss | Diffuse | NA | NA/negative | NA | NA | 12.6 | No | Steroid, CPA | Improved | 29 |
| 22 | 61 | F | None | Local | NA | NA | 7.9 | Negative | NA | No | Resection, bypass surgery | Stable | 30 |
| 23 | 68 | F | None | Local | NA | NA | NA | NA | NA | No | Resection, steroid | Improved | 31 |
| 24 | 66 | F | None | Diffuse | NA | NA | 276* | Positive | 4.11 | No | Steroid | Improved | 32 |
| 25 | 78 | F | None | Diffuse | NA | NA | 1940* | Positive | 0.03 | No | Steroid | Improved | 32 |
| 26 | 62 | F | Chest pain | Diffuse | II | Negative/NA | 97.5 | Negative | 8.17 | No | Steroid | Improved/recurred | Present Case |
| 27 | 77 | M | None | Diffuse | II | Negative/NA | 487* | Negative | 0.27 | No | Steroid | Improved | Present Case |
Ab: antibody, NA: not available, SVC: superior vena cava, CPA: cyclophosphamide
* Cutoff value of serum IgG4>135 mg/dL
In Japan, although the possibility of IgG4-related disease was not investigated in more than half of the patients, there were many cases in which a specific cause could not be detected, so more cases were diagnosed as “idiopathic” than in other countries. The etiology of FM depends on the prevalence of each disease. As histoplasmosis is rarely detected in Japan, it is unlikely to cause FM. Although sarcoidosis is a common disease in Japan, it has a lower incidence than that in France, where sarcoidosis was the main cause of FM (5). The incidence of sarcoidosis per 100,000 person-years was reported to be 1.01 in Japan (35) and 4.9 in France (36). Japan is a country with a moderate prevalence of tuberculosis, but compared to China, where tuberculosis was the main cause of FM, as mentioned above (6), fewer people are affected. According to a World Health Organization report, the estimated incidence of tuberculosis per 100,000 person-years in 2018 was 61 in China and 14 in Japan (37). International comparisons of the prevalence of autoimmune diseases including IgG4-related diseases are not easy. In Japan, the prevalence of IgG4-related diseases was reported to be 0.28 to 1.08 per 100,000 (38), but, in fact, many potential cases may exist. It is unclear whether many FM cases in Japan are truly “idiopathic”. Likely, the cause could not be identified because of the low prevalence of specific diseases that cause FM, resulting in the high rate of idiopathic cases.
It is worth noting that more Japanese patients were given corticosteroids and that their response to corticosteroid therapy was better than elsewhere in the world. In general, corticosteroid responsiveness is expected to be higher with a higher degree of infiltration of inflammatory cells and lower with a higher degree of fibrosis. Flieder et al. divided FM into three stages based on histological patterns such as cell infiltration and fibrotic changes (39): stage I with edematous fibrous mucinous tissue with inflammatory cells; stage II with a thick glassy band of collagen with focal stromal spindle cells, lymphocytes, and plasma cells; and stage III with dense acellular collagen interspersed with lymphoid follicles. Of the 27 FM cases in Japan, 6, including the present two, were evaluated by these criteria, and all were judged to be stage II. Among the other cases, lymphocyte infiltration was common in most of them. Meanwhile, in the US report, 13 of 30 (43%) patients were in stage III, with few inflammatory cells (39). Thus, we consider the cause for the good response to corticosteroid therapy in Japanese FM patients to be incomplete fibrosis and relatively high cell infiltration. In addition, more patients in Japan were diagnosed as being asymptomatic than in other regions, and it is possible that many patients were able to start treatment early before fibrosis progressed. This could be another reason why the steroid response was good in Japan. It is also thought that specific genotypes, including human leukocyte antigen (HLA)-A2 and HLA DQB1*04:02, contribute to the onset of FM (40,41). Differences in genetic background may also be associated with clinical differences.
Our report is associated with several limitations. First, our review is a collection of published case reports, not a case series from a single center. There may be some selection bias in that the collected cases received good therapeutic effect from corticosteroids. Therefore, the Japanese case series cannot be easily compared to reports from the case series of other countries. However, in Japan, where the number of FM cases is small, it is difficult to create a case series with an adequate number of cases. Second, this review may have been insufficient in searching for the cause of FM. Screening for infectious diseases, including histoplasmosis, and autoimmune diseases, including IgG4-RD, was often insufficient. In particular, IgG4-RD is a relatively new disease concept and it has not been well investigated so far. There are many latent cases, which therefore need to be investigated actively in the future. To undertake international comparisons, it will be necessary to create diagnostic guidelines for FM and perform comparisons under the same conditions.
In conclusion, we reviewed 27 cases of FM in Japan whose cause could not be identified and found that corticosteroid therapy was effective in treating many of them. In patients with incomplete fibrosis or suspected autoimmune disease, it may therefore be worthwhile to try corticosteroid therapy.
The authors state that they have no Conflict of Interest (COI).
Acknowledgement
We thank Katsuhiko Kamei at Chiba University Medical Mycology Research Center for the measurement of antibodies to histoplasmosis.
References
- 1.Rossi SE, McAdams HP, Rosado-de-Christenson ML, Franks TJ, Galvin JR. Fibrosing mediastinitis. Radiographics 21: 373-357, 2001. [DOI] [PubMed] [Google Scholar]
- 2.Peikert T, Colby TV, Midthun DE, et al. Fibrosing mediastinitis: clinical presentation, therapeutic outcomes, and adaptive immune response. Medicine (Baltimore) 90: 412-423, 2011. [DOI] [PubMed] [Google Scholar]
- 3.Rossi GM, Emmi G, Corradi D, et al. Idiopathic mediastinal fibrosis: a systemic immune-mediated disorder. A case series and a review of the literature. Clin Rev Allergy Immunol 52: 446-459, 2017. [DOI] [PubMed] [Google Scholar]
- 4.Hage CA, Azar MM, Bahr N, Loyd J, Wheat LJ. Histoplasmosis: up-to-date evidence-based approach to diagnosis and management. Semin Respir Crit Care Med 36: 729-745, 2015. [DOI] [PubMed] [Google Scholar]
- 5.Seferian A, Steriade A, Jaïs X, et al. Pulmonary hypertension complicating fibrosing mediastinitis. Medicine (Baltimore) 94: e1800, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hu Y, Qiu JX, Liao JP, Zhang H, Jin Z, Wang GF. Clinical manifestations of fibrosing mediastinitis in Chinese patients. Chin Med J 129: 2697-2702, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loyd JE, Tillman BF, Atkinson JB, Des Prez RM. Mediastinal fibrosis complicating histoplasmosis. Medicine (Baltimore) 67: 298-310, 1988. [DOI] [PubMed] [Google Scholar]
- 8.Mathisen DJ, Grillo HC. Clinical manifestation of mediastinal fibrosis and histoplasmosis. Ann Thorac Surg 54: 1053-1057, 1992. [DOI] [PubMed] [Google Scholar]
- 9.Fukushima K, Hasegawa T, Oohara T, Take A, Yamaguchi T, Saito K. A case of chronic fibrosing mediastinitis. Nihon Kyobu Geka Gakkai Zasshi 40: 2258-2261, 1992(in Japanese, Abstract in English). [PubMed] [Google Scholar]
- 10.Sugimoto N, Yoneshima M, Abe T, Sawada T, Watanabe H. A case of systemic lupus erythematosus associated with mediastinal fibrosis. Nihon Naika Gakkai Zasshi 81: 114-116, 1992(in Japanese). [DOI] [PubMed] [Google Scholar]
- 11.Kinugasa S, Tachibana S, Kawakami M, Orino T, Yamamoto R, Sasaki S. Idiopathic mediastinal fibrosis: report of a case. Surg Today 28: 335-338, 1998. [DOI] [PubMed] [Google Scholar]
- 12.Toubai T, Akama H, Ichikawa K, et al. Fever of unknown origin due to sclerosing mediastinitis. Nihon Naika Gakkai Zasshi 90: 123-126, 2001(in Japanese). [DOI] [PubMed] [Google Scholar]
- 13.Tada Y, Onoue H, Koarada S, et al. A case of idiopathic fibrosing mediastinitis presented with bilateral pleural effusion. Nihon Rinsho Meneki Gakkai Kaishi 25: 177-180, 2002(in Japanese, Abstract in English). [DOI] [PubMed] [Google Scholar]
- 14.Minami S, Asai M, Iwahori K, Utsumi T, Kido T, Komuta K. A case of fibrosing mediastinitis manifesting recurrent nerve palsy. Nihon Kokyuki Gakkai Zasshi 40: 583-587, 2002(in Japanese, Abstract in English). [PubMed] [Google Scholar]
- 15.Kojima S, Sumiyoshi M, Suwa S, et al. Superior vena cava syndrome due to fibrosing mediastinitis histologically identical to xanthogranulomatous pyelonephritis. Intern Med 42: 56-59, 2003. [DOI] [PubMed] [Google Scholar]
- 16.Eguchi K, Kobayashi K, Hasegawa I, Nakatsuka S. Restenosis of superior vena cava after treatment using a self-expanding metallic stent in a patient with idiopathic fibrosing mediastinitis. Interact Cardiovasc Thorac Surg 2: 355-357, 2003. [DOI] [PubMed] [Google Scholar]
- 17.Shinkawa T, Nakajima M, Kishimoto T, et al. A case of idiopathic sclerosing mediastinitis in a 7-year-old Japanese boy. Eur J Pediatr 164: 302-305, 2005. [DOI] [PubMed] [Google Scholar]
- 18.Nakanishi R, Nishikawa H. Successful management of idiopathic fibrosing mediastinitis with superior vena cava thrombosis. J Cardiovasc Surg (Torino) 46: 95, 2005. [PubMed] [Google Scholar]
- 19.Zen Y, Sawazaki A, Miyayama S, Notsumata K, Tanaka N, Nakanuma Y. A case of retroperitoneal and mediastinal fibrosis exhibiting elevated levels of IgG4 in the absence of sclerosing pancreatitis (autoimmune pancreatitis). Hum Pathol 37: 239-243, 2006. [DOI] [PubMed] [Google Scholar]
- 20.Ichimura H, Ishikawa S, Yamamoto T, et al. Effectiveness of steroid treatment for hoarseness caused by idiopathic fibrosing mediastinitis: report of a case. Surg Today 36: 382-384, 2006. [DOI] [PubMed] [Google Scholar]
- 21.Taniguchi T, Kobayashi H, Fukui S, Ogura K, Saiga T, Okamoto M. A case of multifocal fibrosclerosis involving posterior mediastinal fibrosis, retroperitoneal fibrosis, and a left seminal vesicle with elevated serum IgG4. Hum Pathol 37: 1237-1239, 2006. [DOI] [PubMed] [Google Scholar]
- 22.Ikeda K, Nomori H, Mori T, et al. Successful steroid treatment for fibrosing mediastinitis and sclerosing cervicitis. Ann Thorac Surg 83: 1199-1201, 2007. [DOI] [PubMed] [Google Scholar]
- 23.Inoue M, Nose N, Nishikawa H, Takahashi M, Zen Y, Kawaguchi M. Successful treatment of sclerosing mediastinitis with a high serum IgG4 level. Gen Thorac Cardiovasc Surg 55: 431-433, 2007. [DOI] [PubMed] [Google Scholar]
- 24.Miyata T, Takahama M, Yamamoto R, Nakajima R, Tada H. Sclerosing mediastinitis mimicking anterior mediastinal tumor. Ann Thorac Surg 88: 293-295, 2009. [DOI] [PubMed] [Google Scholar]
- 25.Washino S, Hirai M, Matsuzaki A, Kobayashi Y. 18F-Fluorodeoxyglucose positron emission tomography for diagnosis and monitoring of idiopathic retroperitoneal fibrosis associated with mediastinal fibrosis. Ann Nucl Med 24: 225-229, 2010. [DOI] [PubMed] [Google Scholar]
- 26.Togashi Y, Kim YH, Miyahara R, et al. Octreotide, a somatostatin analogue, in the treatment of chylothorax associated with idiopathic fibrosing mediastinitis. Tohoku J Exp Med 222: 51-53, 2010. [DOI] [PubMed] [Google Scholar]
- 27.Onuki T, Ishikawa S, Matsuoka T, Iguchi K, Inagaki M. Dual-phase FDG-PET imaging shows suspected malignancy that histological examination later confirmed as sclerosing mediastinitis: report of a case. Ann Thorac Cardiovasc Surg 17: 304-306, 2011. [DOI] [PubMed] [Google Scholar]
- 28.Kato G, Takahashi K, Abe T, et al. Effective glucocorticoid treatment in a case of idiopathic fibrosing mediastinitis. Nihon Kokyuki Gakkai Zasshi 49: 822-826, 2011(in Japanese, Abstract in English). [PubMed] [Google Scholar]
- 29.Santo H, Nishiyama O, Sano H, Kitaichi M, Kume H, Tohda Y. Mediastinal fibrosis and positive antineutrophil cytoplasmic antibodies: coincidence or common etiology? Intern Med 53: 275-277, 2014. [DOI] [PubMed] [Google Scholar]
- 30.Oka S, Uramoto H, Yamada S, Tanaka F. Sclerosing mediastinitis of unknown origin: report of a case. Int J Surg Case Rep 10: 5-7, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Okamoto K, Ichinose M. Idiopathic fibrosing mediastinitis mimicking nodal metastasis from breast cancer. Asian Cardiovasc Thorac Ann 25: 663-664, 2017. [DOI] [PubMed] [Google Scholar]
- 32.Takanashi S, Akiyama M, Suzuki K, Otomo K, Takeuchi T. IgG4-related fibrosing mediastinitis diagnosed with computed tomography-guided percutaneous needle biopsy: two case reports and a review of the literature. Medicine (Baltimore) 97: e10935, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sherrick AD, Brown LR, Harms GF, Myers JL. The radiographic findings of fibrosing mediastinitis. Chest 106: 484-489, 1994. [DOI] [PubMed] [Google Scholar]
- 34.Umehara H, Okazaki K, Masaki Y, et al. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD), 2011. Mod Rheumatol 22: 21-30, 2012. [DOI] [PubMed] [Google Scholar]
- 35.Morimoto T, Azuma A, Abe S, et al. Epidemiology of sarcoidosis in Japan. Eur Respir J 31: 372-379, 2008. [DOI] [PubMed] [Google Scholar]
- 36.Duchemann B, Annesi-Maesano I, Jacobe de Naurois C, et al. Prevalence and incidence of interstitial lung diseases in a multi-ethnic county of Greater Paris. Eur Respir J 50: 1602419, 2017. [DOI] [PubMed] [Google Scholar]
- 37. WHO (World Health Organization). Global tuberculosis report 2019 [Internet]. [cited 2020 Jun 7]. Available from: https://www.who.int/tb/publications/global_report/en/.
- 38.Umehara H, Okazaki K, Masaki Y, et al. A novel clinical entity, IgG4-related disease (IgG4RD): general concept and details. Mod Rheumatol 22: 1-14, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Flieder DB, Suster S, Moran CA. Idiopathic fibroinflammatory (fibrosing/sclerosing) lesions of the mediastinum: a study of 30 cases with emphasis on morphologic heterogeneity. Mod Pathol 12: 257-264, 1999. [PubMed] [Google Scholar]
- 40.Peebles RS, Carpenter CT, Dupont WD, Loyd JE. Mediastinal fibrosis is associated with human leukocyte antigen-A2. Chest 117: 482-485, 2000. [DOI] [PubMed] [Google Scholar]
- 41.Strock SB, Gaudieri S, Mallal S, et al. Fibrosing mediastinitis complicating prior histoplasmosis is associated with human leukocyte antigen DQB1*04:02 - a case control study. BMC Infect Dis 15: 206, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]