Abstract
Background
Heightened familial stress and distress during the COVID-19 pandemic may lead to increased negative parenting practices, particularly for parents with substantial adverse childhood experiences (ACES).
Objective
To determine whether families' COVID-19-related distress is associated with young children's emotional/behavioral functioning via negative parenting, and whether these relationships vary based on parents' ACEs.
Participants and setting
Participants were 267 parents of children ages 1.5–5 years recruited from five primary care sites across the United States.
Methods
Participants completed internet questionnaires including measures of demographics, parent ACES, negative parenting, parent mental health, and COVID-19 distress. We used regression analyses to test a moderated mediation model in which the relationship between COVID-19 distress and child emotional/behavioral problems is mediated by negative parenting, and both the direct and indirect effects of COVID-19 distress on child emotional/behavioral problems is moderated by parents' ACEs.
Results
Negative parenting significantly mediated the relationship between COVID-19 distress and child emotional/behavioral problems (indirect effect β = 0.07). Parents' ACEs moderated the associations between COVID-19 distress and both negative parenting and child emotional/behavioral problems, such that each relationship was stronger in the context of higher parental ACEs. The model accounted for 42% of the variance in child emotional/behavioral problems.
Conclusions
Findings have implications for managing risk and promoting well-being in young children during periods of significant stress and routine disruption. This study advances understanding of factors influencing negative outcomes in children during the pandemic's acute phase and may have implications for the development of targeted interventions to improve families' adjustment in the future.
Keywords: COVID-19, Parenting, Child emotional and behavioral problems, Family stress, Adverse childhood experiences
The COVID-19 pandemic has induced and exacerbated a variety of stressors that impact children and their families, including but not limited to collective trauma in the wake of widespread illness and death; fear of a novel, dangerous pathogen; social isolation; and enduring disruptions to families' routines and financial security (Fosco et al., 2021; Patrick et al., 2020; Russell et al., 2020). Parents report increased stress as a result of the pandemic (Brown et al., 2020; Calvano et al., 2021), which can lead to increased psychological distress when individuals perceive a lack of available resources to manage stressors (Yan et al., 2021). Indeed, both parents and children appear to be experiencing greater psychological problems in the wake of the pandemic (Francisco et al., 2020; Horiuchi et al., 2020; Lee et al., 2021; Waller et al., 2021). Pandemic-related increases in familial stress and distress are critically important to examine, because they may lead to dysfunctional parent-child interactions that negatively impact the health and development of children (Prime et al., 2020). This is especially important for families with young children, because maladaptive parent-child patterns during sensitive neurodevelopmental periods can lead to long-term dysfunction if left unaddressed (Dishion & Patterson, 2016; Shonkoff & Garner, 2012).
Prime et al. (2020) proposed a conceptual framework of familial risk and resilience during the COVID-19 pandemic grounded in several prominent theories of human development and functioning, including family systems theory (Carr, 2015), the bioecological model (Bronfenbrenner & Morris, 2006) the family stress model (Masarik & Conger, 2017), and developmental systems theory (Lerner & Damon, 2006). The framework posits that a wide range of pandemic-induced stressors (e.g., job loss, social isolation) influences parents' psychological distress, which in turn impacts child adjustment via parent-child interactions. A large body of literature supports the idea that parents' psychological distress has a negative impact on their parenting and increases the risk for child maltreatment (Holden & Banez, 1996; Warren & Font, 2015), so it is unsurprising that negative parenting practices including neglectful, harsh, and coercive parenting have increased during the pandemic (Chung et al., 2020; Connell & Strambler, 2021; Lee et al., 2021; Wolf et al., 2021). This is worrying, given extensive research demonstrates the detrimental impact of negative parenting on child behavioral and emotional functioning (Pinquart, 2017). One study of Italian parents of predominantly school-age children found that parent psychological distress during the pandemic was significantly associated with child emotional and hyperactive/inattentive symptoms (Marchetti et al., 2020). That relationship was partially mediated by parent verbal hostility, suggesting negative parenting as a possible mechanism through which parents' distress impacts child functioning. Beyond the potential impact on child emotional/behavior symptoms, negative parenting practices are concerning because of their known association with greater child abuse potential (Rodriguez, 2010). Some evidence indicates that pandemic-related stress is associated with increased abuse, neglect, and physical discipline of children (Calvano et al., 2021; Chung et al., 2020; Lee et al., 2021). Determining which parents and families are susceptible to increased negative parenting in the context of COVID-19 is an important goal, as such knowledge might aid the targeted deployment of resources and interventions (MacKinnon & Luecken, 2008).
The Prime et al. (2020) COVID-19 framework postulates that pre-existing factors place certain families at higher risk for negative interactions and poor outcomes. One potentially critical risk factor is parents' own exposure to adverse childhood experiences (ACEs). Experiencing childhood adversity is quite common, with one recent study suggesting that most U.S. adults have experienced at least one ACE and 13% reporting four or more ACEs (Giano et al., 2020). Importantly, ACEs are associated with psychological distress in adults, especially in the presence of contemporary stressful life events (Manyema et al., 2018). Parents with more ACEs are also more likely to experience greater parenting distress (Steele et al., 2016) and have children with emotional/behavioral problems (Haynes et al., 2020; Schickedanz et al., 2018). However, whether ACEs influence parenting practices in the presence of heightened family distress is unknown. Given the growing literature on the intergenerational transmission of adversity and trauma (Narayan et al., 2021), parental ACEs is a crucial variable to consider as a moderator with regard to how prolonged periods of stress may impact parenting and subsequently child emotional and behavioral adjustment. Parents' ACEs were found to be associated with negative parenting behaviors during the pandemic in a German sample (Clemens et al., 2021), but ACEs have not been tested as a moderator of the effect of COVID-19 family distress on parenting behaviors. Theoretically, high levels of parental ACEs would exacerbate the influence of pandemic-related family distress on their negative parenting behaviors due to higher likelihood of potentially problematic strategies for coping with distress (Leitenberg et al., 2004).
In this study, we aimed to test whether COVID-19 family distress influences child adjustment through negative parenting, and whether parents' ACEs moderate the influence of COVID-19 family distress on both negative parenting and child emotional/behavioral problems. Specifically, we hypothesized that COVID-19 family distress is positively associated with greater child emotional/behavioral problems, and that negative parenting mediates this association. Regarding the moderating effect of parents' ACEs, we expected that the associations between COVID-19 distress and negative parenting, as well as COVID-19 distress and child emotional/behavioral problems, would be stronger at higher levels of parent ACEs.
1. Methods
1.1. Participants & design
We recruited 301 English- and Spanish-speaking parents of children ages 1.5–5 years through five primary care practices: a pediatric clinic based in an academic medical center in Oregon, a Federally Qualified Health Center family medicine practice in Kansas, and three hospital-affiliated community clinics in Ohio. Families were eligible to complete the survey only once, and those parents with more than one child in the designated age range were asked to respond to the questionnaires about their eldest child within study age range. The sample size was determined to be adequate to power the planned analyses. Data collection took place between July 2020 and January 2021. All methods were approved by the Institutional Review Boards of the participating institutions.
We used a combination of patient portal messages, text messages, and in-clinic recruitment strategies to recruit participants. All recruitment materials were available in both English and Spanish. We attempted to contact the parents of a total of 1938 children for study participation. A total of 301 (16%) unique participants eventually enrolled in the study and completed one or more measures. This likely underestimates the true recruitment rate, as parents with multiple children in the target age range likely received multiple recruitment attempts, but were only eligible to participate once. The total percentage of text and patient portal messages that were received is unknown. Thirty-five cases were deleted because the same participant completed the survey more than once (the first survey completed was retained).
Participating parents completed a number of online questionnaires in REDCap (Harris et al., 2009). Each of the previously validated measures was available in English and Spanish versions. All additional questionnaires (e.g., demographics) or instructions were professionally translated from English to Spanish. The questionnaires took approximately 40 min to complete, after which families were provided a $20 gift card.
1.2. Measures
1.2.1. Demographics
Parents completed a questionnaire about basic child and parent demographics (e.g., sex, race, and ethnicity), family structure (e.g., number of children and parental marital/cohabitation status), and family income.
1.2.2. Parents' adverse childhood experiences (ACEs)
Parents' ACEs were measured using the ACEs Questionnaire (Murphy et al., 2016), a brief report measure that asks parents to report on their own adverse experiences during their first 18 years of life. These experiences included, but were not limited to, verbal and emotional abuse, physical or sexual abuse, limited access to basic needs (e.g., clothing or food), witnessing domestic violence, and parental mental illness or substance abuse. Internal consistency for the measure was found to be moderate in the current sample (α = 0.80).
1.2.3. COVID-19 family distress
The Distress Scale from the COVID-19 Exposure and Family Impact Survey (CEFIS; Kazak et al., 2021) was used to capture COVID-19 family distress in the current study. The CEFIS is a 25-item questionnaire that measures exposure to COVID-19-related stressful events and the impact of COVID-19 on specific family domains. The CEFIS Distress Scale consists of two items, the first asking the parent to rate how much distress they have experienced related to COVID-19 and the second reflecting the parent's perception of how much distress the children in their family have experienced related to COVID-19. Both items use a 10-point scale with a score of 10 indicating higher distress. The mean of the two distress items was used to capture COVID-19 family distress in the current study. Internal consistency for the two items was moderate (α = 0.70) in the current sample.
1.2.4. Negative parenting
Negative parenting was assessed using the Negative Parenting scale from the Multidimensional Assessment of Parenting Scale (MAPS; Parent & Forehand, 2017). The MAPS is a 34-item questionnaire reflecting parents' awareness and attention paid to their child’s behavior, receptivity and acceptance of their child’s thoughts and emotions, and ability to regulate their reactivity to their child’s behaviors. Each item was rated on a 5-point Likert scale, with higher scores reflecting more mindful parenting. In this study, the 18-item Negative Parenting broadband scale was used, which is comprised of the Hostility, Physical Control, and Lax Control subscales. The Negative Parenting Scale of the MAPS has been demonstrated to have adequate internal consistency (α = 0.88), as was true in the current sample (α = 0.87).
1.2.5. Parental depressive symptoms
The Depression subscale of the Patient-Reported Outcomes Measurement Information System – 29 (PROMIS-29; Hays et al., 2018) was used to measure parental depressive symptoms, which was included as a covariate in the current study. The Depression subscale has four items assessing depressive symptoms (feeling, worthless, helpless, depressed, and hopeless) in the past seven days. Items are rated on a 5-point Likert scale, with higher scores indicating greater depressive symptoms. Internal consistency in the current sample was (α = 0.92).
1.2.6. Child emotional/behavioral problems
The Preschool Pediatric Symptom Checklist (PPSC; Sheldrick et al., 2012) was used to measure child emotional/behavioral problems. The PPSC is an 18-item socioemotional screening instrument that assesses parents' report of externalizing behaviors, internalizing behaviors, attentional problems, and parenting challenges in children ages 18–60 months. Prior research has demonstrated the PPSC to have adequate internal reliability (α’s ranging from 0.86–0.92) and retest reliability (ICC = 0.75). In the current study, internal consistency was good (α = 0.90).
1.3. Statistical analyses
We conducted all analyses using IBM SPSS Statistics Version 27 and the SPSS PROCESS macro (Hayes, 2017). We used listwise deletion to handle missing data, yielding a final analytic sample of 267. Little’s Missing Completely at Random test did not indicate any systematic bias of missing data (χ2 [1397] = 1459.70, p = .12).
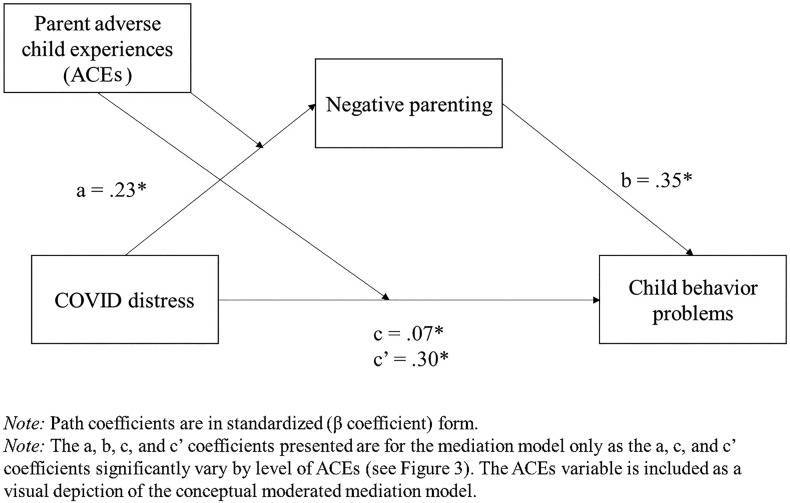
To select covariates for analyses, we tested bivariate correlations between demographic variables and key study variables (i.e., COVID-19 distress, negative parenting, child emotional/behavioral problems, and parent ACEs). We used multiple linear regression analysis to test the hypothesis that COVID-19 distress would be significantly associated with child emotional/behavioral problems. Then, we used the PROCESS macro to test the hypothesis that negative parenting significantly mediates the association between COVID-19 distress and child emotional/behavioral problems. Finally, we tested the full moderated mediation model (Fig. 1), which included parent ACEs as a moderator of associations between COVID-19 distress and negative parenting and child emotional/behavioral problems, using Model 8 in PROCESS. Mediation analyses utilized the bootstrap analysis (5000 samples).
Fig. 1.
Conceptual moderated mediation model and path coefficients for mediation analysis. Note: Path coefficients are in standardized form (β coefficient). The a, b, c, and c’ coefficients are for the mediation model only, as they vary significantly by level of ACEs (see Fig. 2). The ACEs variable is included as a visual depiction of the conceptual moderated mediation model.
2. Results
Means, standard deviations, and correlations between study variables are presented in Table 1 . Parental depressive symptoms, family income, and single parent status were all significantly associated with at least one of the main study variables (see Table 2 ). Single-parent status was significantly associated with COVID-19 family distress (r = 0.13, p < .05), ACEs (r = 0.13, p < .05), and child emotional and behavioral problems (r = 0.29, p < .05). Family income was significantly associated with ACEs (r = −0.24, p < .05) and child emotional and behavioral problems (r = −0.19, p < .05). Parental depressive symptoms were significantly associated with COVID-19 family distress (r = 0.40, p < .05), ACEs (r = 0.31, p < .05), negative parenting (r = 0.31, p < .05), and child emotional and behavioral problems (r = 0.40, p < .05). None of the race/ethnicity variables were significantly associated with the main study variables and thus were not retained as covariates. Of the three subscales of the MAPS Negative Parenting (Hostility, Lax Control, Physical Control), only Physical Control (i.e., corporal punishment) was significantly positively correlated with parent ACEs. All three subscales were significantly positively correlated with both COVID-19 family distress and with child emotional/behavioral problems.
Table 1.
Participant characteristics and descriptive results.
| Participant characteristics (N = 267) | % | M (SD) | Range |
|---|---|---|---|
| Recruitment site | |||
| Oregon | 67% | ||
| Ohio | 24% | ||
| Kansas | 8% | ||
| Respondent | |||
| Biological or adoptive mother | 85% | ||
| Biological or adoptive father | 8% | ||
| Other (e.g., stepparent, grandparent) | 4% | ||
| Annual family income < $50,000 | 39% | ||
| Single parent, % | 17% | ||
| Parent race, % | |||
| White | 58% | ||
| Asian | 15% | ||
| Black | 14% | ||
| Other | 7% | ||
| Parent Latino/Hispanic ethnicity | 11% | ||
| Child age | 3.43 (1.2) | 1.5–5.8 | |
| Study outcome variables | |||
| Parent depressive symptoms T score (PROMIS)a | 50.25 (9.0) | 41–79.4 | |
| COVID-19 family distress (CEFIS) | 5.34 (2.1) | 1–10 | |
| Parent ACEs (ACEs Questionnaire) | 2.20 (2.4) | 0–10 | |
| Negative parenting (MAPS), | |||
| Total | 1.73 (0.5) | 1–3.43 | |
| MAPS Hostility subscale | 1.87 (0.6) | 1–4.00 | |
| MAPS Lax Control subscale | 2.02 (0.6) | 1–4.86 | |
| MAPS Physical Control subscale | 1.29 (0.5) | 1–3.50 | |
| Child emotional/behavioral problems (PPSC) | |||
| Total | 9.62 (7.1) | 0–33 | |
| Exceeding clinical cutoffb | 49% | ||
Note: PROMIS = Patient-reported outcomes measurement information system; CEFIS = Child emotional/behavioral problems (PPSC); ACES = adverse child experiences; MAPS = Multidimensional Assessment of Parenting Scale; PPSC = Preschool Pediatric Symptom Checklist.
Scores of 60 and above considered clinically significant.
Clinical cutoff score is 9.
Table 2.
Correlations among study variables.
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. |
|---|---|---|---|---|---|---|---|---|---|
| 1. COVID-19 distress | – | ||||||||
| 2. ACEs | 0.21⁎ | – | |||||||
| 3. Negative parenting (MAPS) | 0.29⁎ | 0.13⁎ | – | ||||||
| 4. MAPS hostility | 0.26⁎ | 0.10 | 0.84⁎ | – | |||||
| 5. MAPS lax control | 0.19⁎ | 0.02 | 0.76⁎ | 0.45⁎ | – | ||||
| 6. MAPS physical control | 0.22⁎ | 0.21⁎ | 0.71⁎ | 0.46⁎ | 0.25⁎ | – | |||
| 7. Child emotional/behavioral problems (PPSC) | 0.43⁎ | 0.27⁎ | 0.48⁎ | 0.37⁎ | 0.43⁎ | 0.29⁎ | – | ||
| 8. Parent depressive symptoms T-score | 0.40⁎ | 0.31⁎ | 0.31⁎ | 0.28⁎ | 0.27⁎ | 0.17⁎ | 0.40⁎ | – | |
| 9. Family income | −0.11 | −0.24⁎ | −0.03 | 0.17⁎ | −0.03 | −0.23⁎ | −0.19⁎ | −0.21⁎ | – |
| 10. Single parent † | 0.13⁎ | 0.13⁎ | 0.03 | −0.16⁎ | 0.17⁎ | 0.06 | 0.29⁎ | 0.18⁎ | −0.40⁎ |
Note: Correlations were tested using the analytic sample of N = 267.
† As the single parent variable was measured on a dichotomous scale, bivariate correlations between this variable and all others are point-biserial correlations. All other bivariate correlations are Pearson’s correlations.
Denotes significance at p < .05.
After accounting for covariates, COVID-19 family distress was significantly associated with child emotional/behavioral problems (β = 0.30, p < .01) in a multiple linear regression analysis. Next, we tested negative parenting as a mediator in the association between COVID-19 family distress and child emotional/behavioral problems. After accounting for covariates, COVID-19 family distress was significantly associated with negative parenting (β = 0.23, p < .01), and negative parenting was significantly associated with child emotional/behavioral problems (β = 0.35, p < .01). COVID-19 family distress had a significant indirect effect on child emotional/behavioral problems through negative parenting (β = 0.07, 95% confidence interval [CI] = 0.02 to 0.13). The direct effect of COVID-19 family distress on child emotional/behavioral problems was also significant (β = 0.23, p < .01), indicating that negative parenting partially mediates the association between COVID-19 family distress and child emotional/behavioral problems.
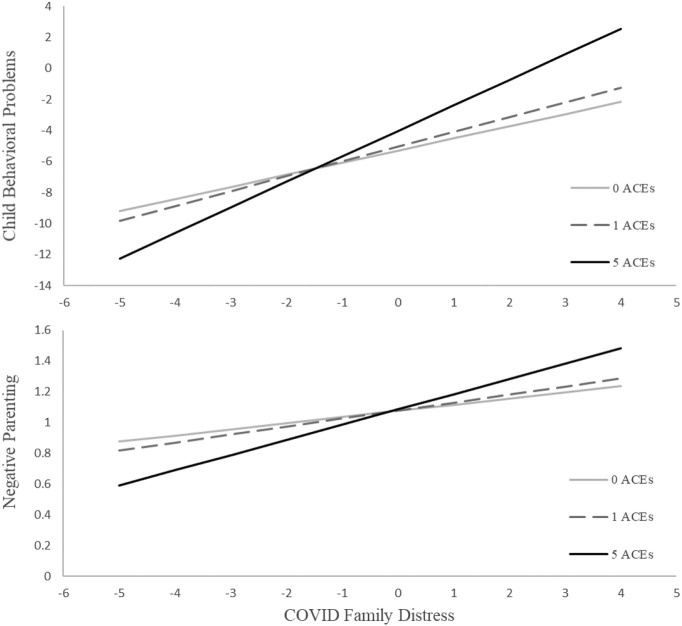
Finally, we tested the moderating influence of parent ACEs on the mediating effect of negative parenting in the relationship between COVID-19 family distress and child emotional/behavioral problems. Parents' ACEs significantly moderated the association between COVID-19 family distress and negative parenting, as well as the association between COVID-19 family distress and child emotional/behavioral problems (see Table 3 ). Specifically, the associations between COVID-19 distress and negative parenting and between COVID-19 distress and child emotional/behavioral problems were stronger at higher levels of ACEs (see Fig. 2 ). The index of moderated mediation (Hayes, 2015) was statistically significant (B = 0.06, 95% CI = 0.002–0.141). The overall model was statistically significant (F [7259] = 24.69, p < .01) and accounted for 42% of the variance in child emotional/behavioral problems.
Table 3.
Coefficients, standard errors, and summary of moderated mediation model.
| Adjusted model |
Unadjusted model |
|||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | t | p | B | SE | t | p | |
| Mediator: negative parenting | ||||||||
| Constant | 0.99 | 0.18 | 5.56 | 0.00⁎⁎ | 1.53 | 0.09 | 17.00 | 0.00⁎⁎ |
| Family income | 0.01 | 0.02 | 0.73 | 0.47 | ||||
| Parent depression | 0.01 | 0.00 | 3.72 | 0.00⁎⁎ | ||||
| Single parent | −0.04 | 0.08 | −0.47 | 0.64 | ||||
| COVID-19 family distress | 0.02 | 0.02 | 0.92 | 0.36 | 0.03 | 0.02 | 1.82 | 0.07 |
| Parent ACEs | −0.06 | 0.03 | −1.92 | 0.06 | −0.06 | 0.03 | −1.74 | 0.08 |
| COVID-19 distress X ACEs | 0.01 | 0.01 | 2.25 | 0.03⁎ | 0.01 | 0.01 | 2.30 | 0.02⁎ |
| Outcome: child behavior | ||||||||
| Constant | −8.00 | 2.47 | −3.24 | 0.00⁎ | −5.09 | 1.72 | −2.96 | 0.00⁎⁎ |
| Family income | −0.08 | 0.21 | −0.37 | 0.71 | ||||
| Parent depression | 0.10 | 0.04 | 2.32 | 0.02⁎ | ||||
| Single parent | 3.82 | 1.00 | 3.82 | 0.00⁎⁎ | ||||
| COVID-19 family distress | 0.40 | 0.23 | 1.74 | 0.08 | 0.62 | 0.22 | 2.81 | 0.01⁎⁎ |
| Negative parenting | 5.32 | 0.82 | 6.51 | 0.00⁎⁎ | 5.94 | 0.80 | 7.40 | 0.00⁎⁎ |
| COVID-19 distress X ACEs | 0.17 | 0.07 | 2.45 | 0.01⁎ | 0.17 | 0.07 | 2.48 | 0.01⁎ |
| B | Boot SE | BootLLCI | BootULCI | B | Boot SE | BootLLCI | BootULCI | |
| Conditional indirect effects of COVID-19 distress on child behavior (at 16th, 50th, and 84th %ile of ACEs) | ||||||||
| 0 ACEs | 0.09 | 0.11 | −0.15 | 0.30 | 0.18 | 0.12 | −0.07 | 0.43 |
| 1 ACE | 0.15 | 0.10 | −0.04 | 0.34 | 0.25 | 0.11 | 0.05 | 0.47 |
| 5 ACEs | 0.40 | 0.15 | 0.15 | 0.72 | 0.48 | 0.14 | 0.24 | 0.78 |
LLCI: lower limit 95% confidence interval; ULCI: upper limit 95% confidence interval.
p < .05.
p <.
Fig. 2.
Associations between COVID-19 family distress and negative parenting and child emotional/behavioral problems, as moderated by parent adverse childhood experiences (ACEs).
3. Discussion
The purpose of this study was to test whether family distress related to COVID-19 is associated with child emotional/behavioral, both directly and indirectly through negative parenting, as well as whether these relationships are conditional based on parents' ACEs. This is among the first studies to examine how parental ACEs influence parenting practices and child emotional/behavioral problems during the pandemic, and consistent with the risk and resilience framework proposed by Prime et al. (2020).
Consistent with previous findings (Bate et al., 2021; Giannotti et al., 2021), pandemic-related family distress was significantly associated with increased child emotional/behavioral problems after controlling for covariates. Further, parents who reported greater levels of distress during the pandemic were more likely to use negative parenting practices, and these parenting practices were associated with more child emotional/behavioral problems. The pathway of increased family distress affecting child emotional/behavioral problems via parenting practices has been found in other studies conducted after large-scale crises (Kelley et al., 2010), suggesting that this pattern may not be unique to COVID-19, but a common reaction to societal stressors.
This study is the first to show that the associations between COVID-19 distress and negative parenting and between COVID-19 distress and child emotional/behavioral problems are stronger for parents with higher levels of ACEs, consistent with long-standing research showing a cumulative, dose-response relationship between risk factors and negative outcomes (Appleyard et al., 2005; Gach et al., 2018; Sameroff et al., 1987). Family distress related to COVID-19 may be particularly impairing for parents with a history of ACEs or other traumatic experiences, which is consistent with research indicating that persons with exposure to child maltreatment and/or intimate partner violence may be more vulnerable to experiencing distress as parents (Guyon-Harris et al., 2017), and that acute stressors exacerbate existing relational vulnerabilities (Randall & Bodenmann, 2017) such as in the parent-child relationship. This is particularly problematic as responsive parenting is a key protective factor for children experiencing higher cumulative risk exposures (Evans et al., 2007), and disruption of responsive parenting could contribute to the intergenerational transmission of trauma (Narayan et al., 2021).
The results from this study provide support for some aspects of Prime and colleagues' conceptual model of risk and resilience in family well-being during the COVID-19 pandemic (Prime et al., 2020), with important implications for managing risk and promoting well-being in youth during and after the pandemic. For example, screening for parental ACE exposure may be helpful to identify families who are at the highest risk for negative emotional/behavioral outcomes during the pandemic and would most benefit intervention. Negative parenting is a modifiable factor, and well-established interventions that focus on reducing negative parenting practices such as Parent-Child Interaction Therapy (McNeil & Hembree-Kigin, 2010), Triple P (Sanders et al., 2014), Incredible Years (Menting et al., 2013) and the Chicago Parent Program (Gross et al., 2009) may promote resilience and positive adjustment for parents and children during and after the pandemic. Importantly, some small-scale evidence indicates such programs may disrupt the association between parent ACEs and child externalizing problems and exert the highest effects for parents with higher ACEs (Blair et al., 2019). Primary care may be a particularly salient setting to screen for ACEs (American Academy of Pediatrics, 2014) and address parenting practices (Smith et al., 2020), as primary care medical homes often serve large populations of youth within their community context and are an important setting for delivering early childhood parenting interventions (Leslie et al., 2016). Our findings also underscore the importance and need for trauma-informed approaches to care in pediatric healthcare (e.g., awareness of trauma and related symptoms, provision of emotionally safe environments, availability of interventions to address the effects of trauma) for both children and their caregivers (Duffee et al., 2021). Further, policy actions and community support that lessen COVID-19 related family distress may help to decrease the use of negative parenting practices thereby reducing the risks of youth emotional/behavioral problems and child maltreatment.
Participants in this study were recruited from five primary care practices in three states across different geographic regions of the United States, with the largest proportion coming from the Pacific Northwest. The sample was diverse in terms of race, ethnicity, and other family demographics. However, the COVID-19 pandemic affected regions of the country differently, limiting the generalizability of these results. Similarly, data were collected from a single informant, typically mothers, which may bias findings (e.g., parents who utilize more negative parenting behaviors may view their children's behavior more negatively (Moens et al., 2018)) and thus may not be indicative of other parent or caregiver experiences during the pandemic. An additional limitation is that our measure of COVID family distress included an item about parent perception of children's distress, which could overlap with the outcome of child emotional and behavioral problems and potentially result in the artificial inflation of estimated associations. Finally, data were collected cross-sectionally across six months of the pandemic (July 2020–January 2021), which limits our ability to infer causal associations between the variables tested in our model, particularly with regards to mediation. However, the consistency of the results with Prime et al.'s (2020) a priori model lends some additional credence to the findings. The longitudinal effects of the pandemic on family distress, parenting practices, and child behavior will be an important area to study, particularly as families re-adjust to changes during the post-pandemic phase. Future research may benefit from targeting a more representative group of parents across time within diverse regions of the United States to examine risk and resiliency factors related to the pandemic. It would also be beneficial for future research to include multi-informant measures of child emotional/behavioral adjustment (e.g., observational or teacher report measures).
This study adds to the growing literature base documenting the effects of pandemic-related stressors on families of young children in the United States. Consistent with Prime and colleagues' conceptual model (Prime et al., 2020), we found that parents' reported use of negative parenting practices helps to explain the relationship between family COVID-19 distress and child emotional/behavioral problems, particularly for parents with a history of childhood adversity or trauma. Understanding what factors are contributing to negative outcomes in children and families during the acute phase of the pandemic may have implications for targeted intervention to improve the adjustment and well-being of families, post-pandemic, and for preventing child maltreatment.
Declaration of competing interest
The authors declare no conflicts of interest.
Acknowledgments
Acknowledgements
Source of funding
This work was supported by the Agency for Healthcare Research and Quality [#K12HS022981], the Health Resources and Services Administration Graduate Psychology Education Program [#D40HP26865], and the National Center for Advancing Translational Sciences of the National Institutes of Health [#UL1TR002369]. Funding sources had no involvement in the study design, data collection, analysis, interpretation, manuscript preparation, or decision to publish.
References
- American Academy of Pediatrics . 2014. Addressing adverse childhood experiences and other types of trauma in the primary care setting.https://downloads.aap.org/AAP/PDF/ttb_addressing_aces.pdf [Google Scholar]
- Appleyard K., Egeland B., Dulmen M.H.M., Alan Sroufe L. When more is not better: The role of cumulative risk in child behavior outcomes. Journal of Child Psychology and Psychiatry. 2005;46(3):235–245. doi: 10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- Bate J., Pham P.T., Borelli J.L. Be my safe haven: Parent-child relationships and emotional health during COVID-19. Journal of Pediatric Psychology. 2021;46(6):624–634. doi: 10.1093/jpepsy/jsab046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair K., Topitzes J., Mersky J.P. Do parents’ adverse childhood experiences influence treatment responses to parent-child interaction therapy? An exploratory study with a child welfare sample. Child & Family Behavior Therapy. 2019;41(2):73–83. [Google Scholar]
- Bronfenbrenner U., Morris P. In: <book-title>Handbook of child psychology: Vol. 1. Theoretical models of human developmen</book-title>t. 6th ed. Lerner R.M., Damon W., editors. Wiley; Hoboken, NJ: 2006. The bioecological model of human development; pp. 793–828. [Google Scholar]
- Brown S.M., Doom J.R., Lechuga-Peña S., Watamura S.E., Koppels T. Stress and parenting during the global COVID-19 pandemic. Child Abuse & Neglect. 2020;110 doi: 10.1016/j.chiabu.2020.104699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvano C., Engelke L., Di Bella J., Kindermann J., Renneberg B., Winter S.M. Families in the COVID-19 pandemic: Parental stress, parent mental health and the occurrence of adverse childhood experiences—Results of a representative survey in Germany. European Child & Adolescent Psychiatry. 2021 doi: 10.1007/s00787-021-01739-0. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr A. In: Handbook of family therapy. Sexton T.L., Lebow J., editors. 2015. The evolution of systems theory; pp. 13–29. [DOI] [Google Scholar]
- Chung G., Lanier P., Wong P.Y.J. Mediating effects of parental stress on harsh parenting and parent-child relationship during coronavirus (COVID-19) pandemic in Singapore. Journal of Family Violence. 2020 doi: 10.1007/s10896-020-00200-1. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemens V., Köhler-Dauner F., Ziegenhain U., Fegert J.M. Predictors of parental coping during the Covid-19 pandemic: A survey in Germany. Frontiers in Psychology. 2021;3830 doi: 10.3389/fpsyg.2021.715327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell C.M., Strambler M.J. Experiences with COVID-19 stressors and parents’ use of neglectful, harsh, and positive parenting practices in the northeastern United States. Child Maltreatment. 2021;26(3):255–266. doi: 10.1177/10775595211006465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion T.J., Patterson G.R. In: Developmental Psychopathology. Cicchetti D., editor. John Wiley & Sons, Inc.; New York, NY: 2016. The development and ecology of antisocial behavior: Linking etiology, prevention, and treatment. [Google Scholar]
- Duffee J., Szilagyi M., Forkey H., Kelly E.T. Trauma-informed care in child health systems. Pediatrics. 2021;148(2) doi: 10.1542/peds.2021-052579. [DOI] [PubMed] [Google Scholar]
- Evans G.W., Kim P., Ting A.H., Tesher H.B., Shannis D. Cumulative risk, maternal responsiveness, and allostatic load among young adolescents. Developmental Psychology. 2007;43(2):341–351. doi: 10.1037/0012-1649.43.2.341. [DOI] [PubMed] [Google Scholar]
- Fosco G.M., Sloan C.J., Fang S., Feinberg M.E. Family vulnerability and disruption during the COVID-19 pandemic: Prospective pathways to child maladjustment. Journal of Child Psychology and Psychiatry. 2021 doi: 10.1111/jcpp.13458. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francisco R., Pedro M., Delvecchio E., Espada J.P., Morales A., Mazzeschi C., Orgilés M. Psychological symptoms and behavioral changes in children and adolescents during the early phase of COVID-19 quarantine in three European countries. Frontiers in Psychiatry. 2020;11:1329. doi: 10.3389/fpsyt.2020.570164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gach E.J., Ip K.I., Sameroff A.J., Olson S.L. Early cumulative risk predicts externalizing behavior at age 10: The mediating role of adverse parenting. Journal of Family Psychology. 2018;32(1):92–102. doi: 10.1037/fam0000360. [DOI] [PubMed] [Google Scholar]
- Giannotti M., Mazzoni N., Bentenuto A., Venuti P., de Falco S. Family adjustment to COVID-19 lockdown in Italy: Parental stress, coparenting, and child externalizing behavior. Family Process. 2021 doi: 10.1111/famp.12686. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giano Z., Wheeler D.L., Hubach R.D. The frequencies and disparities of adverse childhood experiences in the US. BMC Public Health. 2020;20(1):1–12. doi: 10.1186/s12889-020-09411-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross D., Garvey C., Julion W., Fogg L., Tucker S., Mokros H. Efficacy of the Chicago parent program with low-income African American and Latino parents of young children. Prevention Science. 2009;10(1):54–65. doi: 10.1007/s11121-008-0116-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyon-Harris K.L., Ahlfs-Dunn S., Huth-Bocks A. PTSD symptom trajectories among mothers reporting interpersonal trauma: Protective factors and parenting outcomes. Journal of Family Violence. 2017;32(7):657–667. [Google Scholar]
- Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. An index and test of linear moderated mediation. Multivariate Behavioral Research. 2015;50(1):1–22. doi: 10.1080/00273171.2014.962683. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. Guilford publications; 2017. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Haynes E., Crouch E., Probst J., Radcliff E., Bennett K., Glover S. Exploring the association between a parent’s exposure to adverse childhood experiences (ACEs) and outcomes of depression and anxiety among their children. Children and Youth Services Review. 2020;113 [Google Scholar]
- Hays R.D., Spritzer K.L., Schalet B.D., Cella D. PROMIS((R))-29 v2.0 profile physical and mental health summary scores. Quality of Life Research. 2018;27(7):1885–1891. doi: 10.1007/s11136-018-1842-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holden E.W., Banez G.A. Child abuse potential and parenting stress within maltreating families. Journal of Family Violence. 1996;11(1):1–12. [Google Scholar]
- Horiuchi S., Shinohara R., Otawa S., Akiyama Y., Ooka T., Kojima R., Yokomichi H., Miyake K., Yamagata Z. Caregivers’ mental distress and child health during the COVID-19 outbreak in Japan. PLoS One. 2020;15(12) doi: 10.1371/journal.pone.0243702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazak A.E., Alderfer M., Enlow P.T., Lewis A.M., Vega G., Barakat L., Hildenbrand A.K. COVID-19 exposure and family impact scales: factor structure and initial psychometrics. Journal of Pediatric Psychology. 2021;46(5):504–513. doi: 10.1093/jpepsy/jsab026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley M.L., Self-Brown S., Le B., Bosson J.V., Hernandez B.C., Gordon A.T. Predicting posttraumatic stress symptoms in children following hurricane Katrina: A prospective analysis of the effect of parental distress and parenting practices. Journal of Traumatic Stress. 2010;23(5):582–590. doi: 10.1002/jts.20573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.J., Ward K.P., Lee J.Y., Rodriguez C.M. Parental social isolation and child maltreatment risk during the COVID-19 pandemic. Journal of Family Violence. 2021 doi: 10.1007/s10896-020-00244-3. Advanced online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leitenberg H., Gibson L.E., Novy P.L. Individual differences among undergraduate women in methods of coping with stressful events: The impact of cumulative childhood stressors and abuse. Child Abuse & Neglect. 2004;28(2):181–192. doi: 10.1016/j.chiabu.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Lerner R.M., Damon W.E. 6th ed. Vol. 1. Wiley; Hoboken, NJ: 2006. Handbook of child psychology. (Theoretical models of human development). [Google Scholar]
- Leslie L.K., Mehus C.J., Hawkins J.D., Boat T., McCabe M.A., Barkin S., Perrin E.C., Metzler C.W., Prado G., Tait V.F. Primary health care: Potential home for family-focused preventive interventions. American Journal of Preventive Medicine. 2016;51(4):S106–S118. doi: 10.1016/j.amepre.2016.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon D.P., Luecken L.J. How and for whom? Mediation and moderation in health psychology. Health Psychology. 2008;27(2S):S99. doi: 10.1037/0278-6133.27.2(Suppl.).S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manyema M., Norris S.A., Richter L.M. Stress begets stress: The association of adverse childhood experiences with psychological distress in the presence of adult life stress. BMC Public Health. 2018;18(1):1–12. doi: 10.1186/s12889-018-5767-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchetti D., Fontanesi L., Di Giandomenico S., Mazza C., Roma P., Verrocchio M.C. The effect of parent psychological distress on child hyperactivity/inattention during the COVID-19 lockdown: Testing the mediation of parent verbal hostility and child emotional symptoms. Frontiers in Psychology. 2020;11:3417. doi: 10.3389/fpsyg.2020.567052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masarik A.S., Conger R.D. Stress and child development: A review of the family stress model. Opinion in Psychology Current. 2017;13:85–90. doi: 10.1016/j.copsyc.2016.05.008. [DOI] [PubMed] [Google Scholar]
- McNeil C., Hembree-Kigin T.L. Springer Science & Business Media; 2010. Parent-child interaction therapy. [Google Scholar]
- Menting A.T.A., Orobio De Castro B., Matthys W. Effectiveness of the incredible years parent training to modify disruptive and prosocial child behavior: A meta-analytic review. Clinical Psychology Review. 2013;33(8):901–913. doi: 10.1016/j.cpr.2013.07.006. [DOI] [PubMed] [Google Scholar]
- Moens M.A., Weeland J., Van der Giessen D., Chhangur R.R., Overbeek G. In the eye of the beholder? Parent-observer discrepancies in parenting and child disruptive behavior assessments. Journal of Abnormal Child Psychology. 2018;46(6):1147–1159. doi: 10.1007/s10802-017-0381-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy A., Steele H., Steele M., Allman B., Kastner T., Dube S.R. Integrated Early Childhood Behavioral Health in Primary Care. Springer; 2016. The clinical Adverse Childhood Experiences (ACEs) questionnaire: Implications for trauma-informed behavioral healthcare; pp. 7–16. [Google Scholar]
- Narayan A.J., Lieberman A.F., Masten A.S. Intergenerational transmission and prevention of adverse childhood experiences (ACEs) Clinical Psychology Review. 2021;85:1–11. doi: 10.1016/j.cpr.2021.101997. 101997. [DOI] [PubMed] [Google Scholar]
- Parent J., Forehand R. The Multidimensional Assessment of Parenting Scale (MAPS): Development and psychometric properties. Journal of Child and Family Studies. 2017;26(8):2136–2151. doi: 10.1007/s10826-017-0741-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick S.W., Henkhaus L.E., Zickafoose J.S., Lovell K., Halvorson A., Loch S., Davis M.M. Well-being of parents and children during the COVID-19 pandemic: A national survey. Pediatrics. 2020;146(4) doi: 10.1542/peds.2020-016824. [DOI] [PubMed] [Google Scholar]
- Pinquart M. Associations of parenting dimensions and styles with externalizing problems of children and adolescents: An updated meta-analysis. Developmental Psychology. 2017;53(5):873–932. doi: 10.1037/dev0000295. [DOI] [PubMed] [Google Scholar]
- Prime H., Wade M., Browne D.T. Risk and resilience in family well-being during the COVID-19 pandemic. American Psychologist. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Randall A.K., Bodenmann G. Stress and its associations with relationship satisfaction. Current Opinion in Psychology. 2017;13:96–106. doi: 10.1016/j.copsyc.2016.05.010. [DOI] [PubMed] [Google Scholar]
- Rodriguez C.M. Parent–child aggression: Association with child abuse potential and parenting styles. Violence and Victims. 2010;25(6):728–741. doi: 10.1891/0886-6708.25.6.728. [DOI] [PubMed] [Google Scholar]
- Russell B.S., Hutchison M., Tambling R., Tomkunas A.J., Horton A.L. Initial challenges of caregiving during COVID-19: Caregiver burden, mental health, and the parent–child relationship. Child Psychiatry & Human Development. 2020;51(5):671–682. doi: 10.1007/s10578-020-01037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sameroff A.J., Seifer R., Barocas R., Zax M., Greenspan S. Intelligence quotient scores of 4-year-old children: Social-environmental risk factors. Pediatrics. 1987;79(3):343–350. [PubMed] [Google Scholar]
- Sanders M.R., Kirby J.N., Tellegen C.L., Day J.J. The triple P-positive parenting program: A systematic review and meta-analysis of a multi-level system of parenting support. Clinical Psychology Review. 2014;34(4):337–357. doi: 10.1016/j.cpr.2014.04.003. [DOI] [PubMed] [Google Scholar]
- Schickedanz A., Halfon N., Sastry N., Chung P.J. Parents’ adverse childhood experiences and their children’s behavioral health problems. Pediatrics. 2018;142(2) doi: 10.1542/peds.2018-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheldrick R.C., Henson B.S., Merchant S., Neger E.N., Murphy J.M., Perrin E.C. The preschool pediatric symptom checklist (PPSC): Development and initial validation of a new social/emotional screening instrument. Academic Pediatrics. 2012;12(5):456–467. doi: 10.1016/j.acap.2012.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff J.P., Garner A.S. Committee on psychosocial aspects of child and family health; Committee on early childhood, adoption, and dependent care; section on developmental and behavioral pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics. 2012;129(1):e232–e246. doi: 10.1542/peds.2011-2663. http://pediatrics.aappublications.org/content/pediatrics/129/1/e232.full.pdf [DOI] [PubMed] [Google Scholar]
- Smith J.D., Cruden G.H., Rojas L.M., Van Ryzin M., Fu E., Davis M.M., Brown C.H. Parenting interventions in pediatric primary care: A systematic review. Pediatrics. 2020;146(1) doi: 10.1542/peds.2019-3548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele H., Bate J., Steele M., Dube S.R., Danskin K., Knafo H., Murphy A. Adverse childhood experiences, poverty, and parenting stress. Canadian Journal of Behavioural Science/Revue canadienne des sciences du comportement. 2016;48(1):32–38. doi: 10.1037/cbs0000034. [DOI] [Google Scholar]
- Waller R., Powell T., Rodriguez Y., Corbett N., Perlstein S., White L.K., Wagner N.J. The impact of the COVID-19 pandemic on children’s conduct problems and callous-unemotional traits. Child Psychiatry & Human Development. 2021;52(6):1012–1023. doi: 10.1007/s10578-020-01109-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren E.J., Font S.A. Housing insecurity, maternal stress, and child maltreatment: An application of the family stress model. Social Service Review. 2015;89(1):9–39. [Google Scholar]
- Wolf J.P., Freisthler B., Chadwick C. Stress, alcohol use, and punitive parenting during the COVID-19 pandemic. Child Abuse & Neglect. 2021;117 doi: 10.1016/j.chiabu.2021.105090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan L., Gan Y., Ding X., Wu J., Duan H. The relationship between perceived stress and emotional distress during the COVID-19 outbreak: Effects of boredom proneness and coping style. Journal of Anxiety Disorders. 2021;77 doi: 10.1016/j.janxdis.2020.102328. [DOI] [PMC free article] [PubMed] [Google Scholar]