Abstract
Background & aim
Psychological disorders are an important health problem worldwide. A healthy diet is recommended as one of the measures to prevent and control mental disorders. Epidemiological studies have shown important associations between the consumption of diets rich in nutrients and a lower risk of developing anxiety and depression. Therefore, the aim of this study was to evaluate the association between the prevalence of anxiety and depression symptoms and food consumption, according to the degree of processing, during the COVID-19 pandemic.
Methods
An epidemiological household survey was conducted in two cities in Brazil. Anxiety and depression symptoms were assessed using validated scales (Generalized Anxiety Disorder 7-item/Patient Health Questionnaire-9), and food consumption was assessed using a qualitative food frequency questionnaire referring to consumption within the last 3 months. The foods were categorized according to the NOVA classification for fresh/minimally processed food and ultra-processed food, using the average weekly consumption as the cutoff. For data analysis, adjusted Poisson regression with robust variance was utilized to estimate the prevalence ratio and 95% confidence interval (CI).
Results
The consumption of fresh/minimally processed foods above the weekly average frequency was associated with a lower prevalence of symptoms of depression (PR: 0.5, 95% CI: 0.3; 0.7). Consumption above the weekly average of ultra-processed foods was associated with a higher prevalence of anxiety (PR: 1.5 and 95% CI: 1.03; 2.3) and depression symptoms (PR: 1.5, 95% CI: 1.0; 2.1, P = 0.034).
Conclusion
Increased consumption of ultra-processed foods is associated with a higher occurrence of anxiety and depression symptoms; therefore, we recommend an increase in the consumption of fresh/minimally processed foods, as endorsed by the Dietary Guidelines for the Brazilian Population.
Keywords: Depression, Anxiety, Food consumption, Food processing industry, Mental health, Nutrition
1. Introduction
Psychological disorders, including depressive and anxiety symptoms, are considered worldwide health problems [1]. It is estimated that depression is the biggest cause of disability, in addition to being the biggest contributor to suicide, with up to 800,000 cases per year [1,2]. Among the prevention and control measures for mental disorders, an adequate and healthy diet is recommended [3]. Epidemiological studies have shown important associations between the consumption of healthy diets and a lower risk of developing depression [[4], [5], [6]]. On the other hand, studies have observed that diets characterized by high consumption of ultra-processed foods (UPF), in general, are associated with poor mental health [3,7,8]. Such foods are characterized by the addition of synthetic substances, sugar, salt, fat, and stabilizers [9], and the consumption of these ingredients is harmful and capable of increasing inflammation, decreasing hippocampal volume, impairing cognitive function including memory, impacting psychomotor efficiency, and increasing vulnerability to depression and anxiety [[10], [11], [12]].
During the SARS-CoV-2 pandemic, we speculated on the possible impact of illness and social distancing on lifestyle and other health conditions [[13], [14], [15]], emphasizing important changes in food consumption, such as the increase in UPF consumption, as well as the global increase in the occurrence of anxiety, depression, and stress [16,17].
Considering that depression, anxiety and other mental disorders are the major diseases of the 21st century and are leading causes of disability across the globe [1], there is a strong need for scientific investigations that are capable of revealing possible associations between the consumption of foods with different degrees of processing, and the occurrence of comorbidities related to mental health [[18], [19], [20], [21]]. Furthermore, it is important to consider that the nutritional transition has been characterized by an increase in the consumption of UPF as a replacement for fresh foods, resulting in important health outcomes [3,[22], [23], [24], [25], [26], [27]], and that the COVID-19 pandemic can be a catalyst of both processes, as well as being responsible for exacerbating inequities. Thus, the aim of this study was to evaluate the association between the prevalence of anxiety and depression symptoms and food consumption, according to the degree of processing, during the COVID-19 pandemic.
2. Materials and methods
2.1. Study design and location
This study is part of a larger research effort: “Epidemiological surveillance of COVID-19 in the Inconfidentes Region/MG,” conducted in two cities in the Quadrilátero Ferrífero region of Southeast Brazil. The study employed an epidemiological household survey conducted in three stages, between October and December 2020, and its methodology was previously described by Meireles [28].
According to the 2010 [29] demographic census, these urban cities have populations of 60,775 people in Ouro Preto and 47,395 people in Mariana, distributed in 17,753 and 14,078 households, respectively.
2.2. Study population
Residents of households in the urban areas of Ouro Preto and Mariana, over 18 years old, were considered eligible for this study.
Sample calculation was performed using the OpenEpi tool, using the 2010 population estimate [29] for the urban areas, 95% confidence level, design effect equal to 1.5, estimated proportion of infection, and precision. In addition, a 20% re-composition percentage was added to the sample size of each city, accounting for any losses.
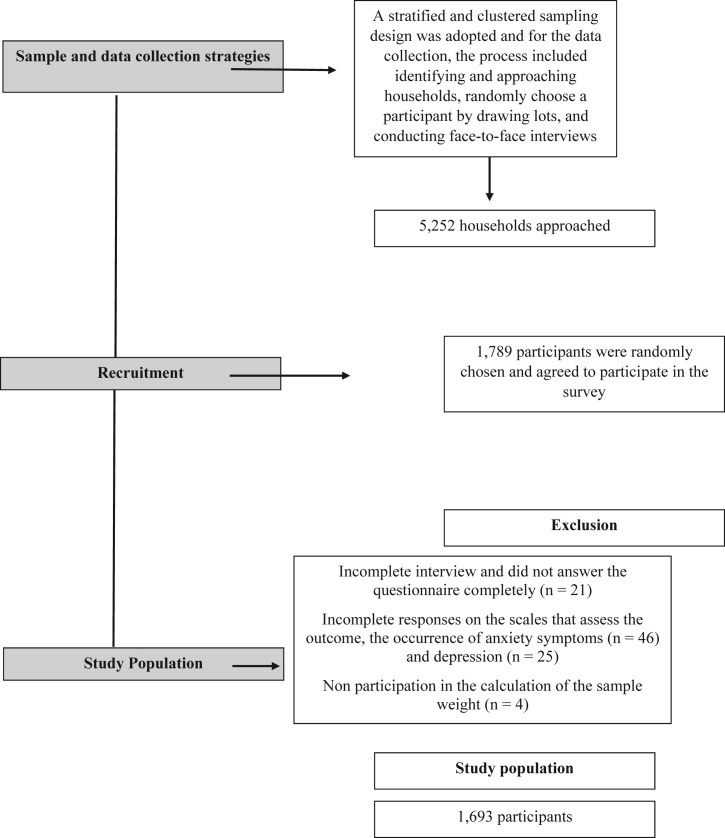
A stratified and clustered sampling design was adopted in three stages as follows: census sector (probability proportional to the number of households), household (systematic sampling), and resident (randomly). For each city, four strata were defined according to the average monthly incomes available in the 2010 census [29], with the objective of guaranteeing the representation of the different socioeconomic statuses in the sample. This study included 1693 individuals as shown in Fig. 1 .
Fig. 1.
Flowchart of sample and data collection strategies and exclusion criteria, COVID Inconfidentes, 2021.
2.3. Data collection
The data collection process included identifying and approaching households, randomly choose a participant by drawing lots, and conducting face-to-face interviews. Data collection occurred on weekends, with the purpose of enhancing and increasing the participation of residents who work during the week. During the week before the collection, the research team recruited and registered households in pre-selected census sectors and raised awareness among the population, which included 5252 households.
Interviews were conducted by trained undergraduate and graduate students. During data collection, the entire team underwent health monitoring through periodic evaluation prior to the beginning of each stage of the survey by serological testing for anti-SARS-CoV-2 antibodies (immunochromatography reaction). All recommendations from national protocols against coronavirus were consistently implemented, with an emphasis on hand washing, use of personal protective equipment (apron, cap, disposable surgical mask, and goggles), and conduction of interviews in an open and ventilated area. Interviewers maintained a minimum distance of 1.5 meters from the interviewees, and physical contact was restricted to solely biological material collection.
Interviews lasted between 30 and 45 min. Using the DataGoal® application, the geographic coordinates (latitude and longitude) of the respondent's residence were captured. Participant questionnaires contained registration data, sociodemographic and economic variables, lifestyle variables, medical history, and food and nutrition information.
2.4. Anxiety and depression
The presence of anxiety and depression symptoms was assessed using two scales validated for use in adults. The Generalized Anxiety Disorder 7-item (GAD-7) [30] assessed anxiety symptoms, and the Patient Health Questionnaire-9 (PHQ-9) [31] assessed depression symptoms.
The scales include questions that assess the frequency of situations that triggered symptoms of anxiety and depression in the last two weeks, with answer options as follows: i) none; ii) several days; iii) more than half of the days; and iv) almost every day. Each of the answer options equals 0 to 3 points.
The final score was classified as described by Kroenke [31] and Lowe [30]. Scores below 10 points on the GAD-7 scale were considered as indicating minimal or mild anxiety symptoms, while a score of 10 points or more was considered as indicating moderate or severe anxiety symptoms. Regarding the PHQ-9 scale, scores lower than 10 points indicated minimal or mild symptoms of depression, and scores ≥10 indicated moderate, moderately severe, and severe depression symptoms.
2.5. Food consumption
Food consumption was assessed using a qualitative food frequency questionnaire (FFQ), which was used to assess food consumption of the Brazilian population in a national survey [32], referring to consumption in the last 3 months (Fig. 1). The frequency of food consumption was reported on weekdays, with five possible answers: i) never; ii) 1–2 days/per week; iii) 3–4 days/week; iv) 5–6 days/week v) Every day, including Saturday and Sunday. Daily food consumption was considered as a descriptive analysis variable.
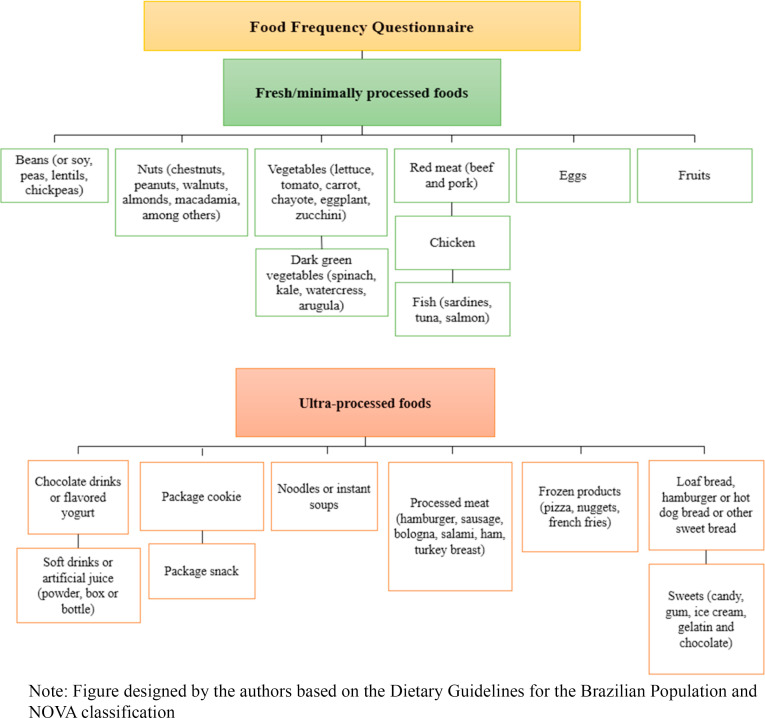
The FFQ foods were used to create the two explanatory variables: fresh/minimally processed foods and ultra-processed foods, according to the Dietary Guidelines for the Brazilian Population [9] and the NOVA classification [33,34] (Fig. 2 ).
Fig. 2.
Fresh/minimally processed and ultra-processed foods, based on the Food Frequency Questionnaire.
The NOVA classification was first documented by Monteiro et al., in 2010 [33], and is an important tool for describing foods based on the extent and purpose of industrial processing and its implications of food processing on food systems and dietary patterns, and how these may affect health and well-being patterns and the risk of disease. The Dietary Guidelines for the Brazilian Population (2014) [9] was the first worldwide guideline to be established that considered the NOVA classification system as a way to assess food processing. NOVA classifies foods into four major groups: i) fresh or minimally processed foods prepared with minimal processing techniques for preserving the food and making it suitable for storage; ii) culinary ingredients that are substances obtained industrially from natural foods and used to prepare, cook, and season food; iii) processed foods that are fresh/minimally processed foods modified by the addition of salt, sugar, oils or fats; iv) ultra-processed foods, e.g. foods with the highest degree of industrial processing, formulated using several industrial techniques and many ingredients, including salt, sugar, oils, fats, and substances exclusively for industrial use [9].
To evaluate the association between the prevalence of anxiety and depression symptoms and the food consumption according to the degree of processing, we used the NOVA categories of fresh/minimally processed and ultra-processed foods. These two variables were assessed as the sum of the weekly frequency of consumption of all foods in each respective group.
2.6. Descriptive variables
The sociodemographic variables investigated were sex, age (grouped: 18–34 years old, 35–59 years old, and 60 years old or more) [35], marital status (having a partner or not), and family income (up to two minimum wages, two minimum wages, four minimum wages, and more than four minimum wages at the time of the study).
The Presence of a medical diagnosis of anxiety disorder or depression was assessed through medical history.
2.7. Statistical analysis
The sample weight of each selected unit (census sector, household, and individual) was calculated according to the methodology described by Silva et al.[38], separately for each city, as demonstrated by Meireles and collaborators [28].
The analyses were performed using Stata software version 15.1 (Stata Corporation, College Station, Texas), using the “svy” command, which considers a complex sample design.
For sample description, the proportion and 95% confidence interval (95% CI) were used for comparison analyses using Pearson's chi-square test.
To verify the association between the consumption of fresh/minimally processed and ultra-processed foods, and symptoms of anxiety and depression, multivariate analysis was performed using Poisson regression with the prevalence ratio and respective 95% CI for binary outcomes. A multivariate model was adjusted for sex, age, marital status, educational background, family income and medical diagnosis of depression or anxiety disorders. Furthermore, the parameters for model evaluation were appreciated (Prob > F < 0.001), indicating that the variables comprising the model were appropriate for the analysis.
2.8. Ethical considerations
The project was approved by the Research Ethics Committee of the Federal University of Minas Gerais (Protocol No. 4.135.077).
3. Results
Among the 1693 individuals evaluated, most (45.9%) were 35–59 years old and were female (51.1%). Anxiety and depression symptoms were present in 23.3% and 15.6% of the participants, respectively.
The sociodemographic characteristics and medical history, according to the presence of anxiety and depression symptoms, are shown in Table 1 . It was observed that being female was related to both outcomes (Table 1) and a medical diagnosis of anxiety disorder or depression was related to a higher prevalence of depression symptoms.
Table 1.
Sociodemographic characteristics and medical history according to the presence of anxiety and depression symptoms, COVID Inconfidentes, 2021.
| Total | Anxiety symptomsa 23.3% (95% CI: 19.5; 27.6) |
P-valueb | Depression symptomsa 15.6% (95% CI: 12.5; 19.4) |
P-valueb | |
|---|---|---|---|---|---|
| Sociodemographic characteristics | |||||
| Sex | 0.009∗ | <0.001∗ | |||
| Male | 48.90 (41.67; 56.18) | 35.90 (23.48; 50.57) | 25.12 (17.35; 34.89) | ||
| Female | 51.10 (43.82; 58.33) | 64.10 (49.43; 76.52) | 74.88 (65.11; 82.65) | ||
| Age | 0.126 | 0.218 | |||
| 18–34 years old | 36.52 (31.92; 41.38) | 41.25 (28.69; 55.06) | 42.12 (29.94; 55.34) | ||
| 35–59 years old | 45.87 (41.34; 50.47) | 49.76 (37.95; 61.60) | 47.15 (36.27; 58.30) | ||
| ≥60 years old | 17.61 (14.46; 21.28) | 8.98 (5.71; 13.86) | 10.74 (6.68; 16.81) | ||
| Marital status | 0.412 | 0.036∗ | |||
| Married | 46.59 (40.66; 52.62) | 49.77 (37.87–61.69) | 41.57 (30.68; 53.35) | ||
| Not married | 53.41 (47.38; 59.34) | 50.23 (38.31; 62.13) | 58.43 (46.65; 69.32) | ||
| Family income | 0.420 | 0.664 | |||
| ≤2 minimum wages | 40.59 (35.20; 46.21) | 34.26 (24.69; 45.32) | 38.42 (27.23; 50.98) | ||
| >2 to ≤4 minimum wages | 31.99 (26.81; 37.64) | 32.78 (23.89; 43.11) | 29.60 (20.63; 40.49) | ||
| >4 minimum wages | 27.42 (22.41; 33.08) | 32.96 (19.67; 49.67) | 31.98 (21.00; 45.39) | ||
| Medical history | |||||
| Diagnosis of anxiety disorder or depression | <0.001∗ | <0.001∗ | |||
| No | 77.25 (72.82; 81.15) | 55.30 (44.30; 65.79) | 48.80 (38.05; 59.67) | ||
| Yes | 22.75 (18.85; 27.18) | 44.70 (34.21; 55.70) | 51.20 (40.33; 61.95) | ||
∗ P-values < 0.05.
Proportion and 95% confidence interval (95% CI).
Probability values.
When we analyzed the participants' food consumption (Table 2 ), we observed non-daily consumption of some fresh/minimally processed foods such as: vegetables, dark green vegetables, and red meat, among individuals with depression symptoms, as well as reduced fruit consumption among those with anxiety symptoms. Regarding the consumption of ultra-processed foods, we observed higher daily consumption of instant noodles among those with symptoms of anxiety or depression, and higher daily consumption of soft drinks or artificial juice drinks among those with symptoms of anxiety.
Table 2.
Daily food intake according to the presence of anxiety and depression symptoms, COVIDInconfidentes, 2021.
| Total (%/95% CI) | Anxiety symptoms (%/95% CI)a | P-valueb | Depression symptoms (%/95% CI)a | P-valueb | |
|---|---|---|---|---|---|
| Fresh/minimally processed foods | |||||
| Beans | 0.702 | 0.044∗ | |||
| Daily | 72.23 (67.24; 76.73) | 73.68 (63.88; 81.59) | 60.44 (46.76; 72.67) | ||
| Not daily | 27.77 (23.27; 32.76) | 26.32 (18.41; 36.12) | 39.56 (27.33; 53.24) | ||
| Nuts | 0.405 | 0.234 | |||
| Daily | 6.62 (3.96; 10.84) | 5.00 (2.51; 9.70) | 4.13 (1.92; 8.66) | ||
| Not daily | 93.38 (89.16; 96.04) | 95.00 (90.30; 97.49) | 95.87 (91.34; 98.08) | ||
| Vegetables | 0.131 | 0.005∗ | |||
| Daily | 56.95 (52.44; 61.34) | 48.06 (36.04; 60.31) | 41.08 (30.72; 53.77) | ||
| Not daily | 43.05 (38.66; 47.56) | 51.94 (39.69; 63.96) | 58.20 (46.23; 69.28) | ||
| Dark-green vegetables | 0.192 | 0.035∗ | |||
| Daily | 24.03 (19.74; 28.90) | 18.77 (13.65; 25.25) | 17.11 (11.97; 23.87) | ||
| Not daily | 75.97 (71.10; 80.26) | 81.23 (74.75; 86.35) | 82.89 (76.13; 88.03) | ||
| Fruits | 0.031∗ | 0.127 | |||
| Daily | 43.33 (38.33; 48.48) | 32.13 (23.45; 42.26) | 34.73 (24.60; 46.47) | ||
| Not daily | 56.67 (51.52; 61.67) | 67.87 (57.74; 76.55) | 65.27 (53.53; 75.40) | ||
| Red meat | 0.201 | 0.031∗ | |||
| Daily | 21.89 (18.27; 25.99) | 29.03 (16.96; 45.03) | 14.60 (9.72; 21.35) | ||
| Not daily | 78.11 (74.01; 81.73) | 70.97 (54.97; 83.04) | 85.40 (78.65; 90.28) | ||
| Chicken | 0.098 | 0.314 | |||
| Daily | 10.84 (7.47; 15.46) | 18.78 (7.73; 38.95) | 14.65 (8.51; 24.06) | ||
| Not daily | 89.16 (84.54; 92.53) | 81.22 (61.05; 92.27) | 85.35 (75.94; 91.49) | ||
| Fish | 0.429 | 0.979 | |||
| Daily | 0.84 (0.33; 2.12) | 1.34 (0.42; 4.22) | 0.86 (0.25; 2.93) | ||
| Not daily | 99.16 (97.88; 99.67) | 98.66 (95.78; 99.58) | 99.14 (97.07; 99.75) | ||
| Eggs | 0.311 | 0.597 | |||
| Daily | 17.45 (14.27; 21.16) | 20.33 (13.86; 28.82) | 19.34 (13.06; 27.67) | ||
| Not daily | 82.55 (78.84; 85.73) | 79.67 (71.18; 86.14) | 80.66 (72.33; 86.94) | ||
| Ultra-processed foods | |||||
| Soft drinks or artificial juice | 0.047∗ | 0.110 | |||
| Daily | 20.32 (16.32; 25.01) | 31.39 (18.87; 47.37) | 29.60 (18.00; 44.59) | ||
| Not daily | 79.68 (74.99; 83.68) | 68.61 (52.63; 81.13) | 70.40 (55.41; 82.00) | ||
| Chocolate drink or flavored yogurt | 0.208 | 0.764 | |||
| Daily | 7.68 (5.44; 10.73) | 5.67 (3.34; 9.45) | 6.99 (3.74; 12.70) | ||
| Not daily | 92.32 (89.27; 94.56) | 94.33 (90.55; 96.66) | 93.01 (87.30; 96.26) | ||
| Package cookie | 0.098 | 0.184 | |||
| Daily | 20.06 (16.12; 24.69) | 25.71 (18.13; 35.10) | 25.41 (18.01; 34.56) | ||
| Not daily | 79.94 (75.31; 83.88) | 74.29 (64.90; 81.87) | 74.59 (65.44; 81.99) | ||
| Package snack | 0.174 | 0.082 | |||
| Daily | 0.87 (0.45; 1.68) | 1.62 (0.57; 4.51) | 2.13 (0.66; 6.66) | ||
| Not daily | 99.13 (98.32; 99.55) | 98.38 (95.49; 99.43) | 97.87 (93.34; 99.34) | ||
| Noodles or instant soups | 0.014∗ | 0.017∗ | |||
| Daily | 1.24 (0.70; 2.19) | 3.14 (1.31; 7.35) | 3.65 (1.35; 9.50) | ||
| Not daily | 98.76 (97.81; 99.30) | 96.86 (92.65; 98.69) | 96.35 (90.50; 98.65) | ||
| Processed meat | 0.409 | 0.892 | |||
| Daily | 2.82 (1.93; 4.08) | 2.14 (0.98; 4.63) | 2.97 (1.26; 6.83) | ||
| Not daily | 97.18 (95.92; 98.07) | 97.86 (95.37; 99.02) | 97.03 (93.17; 98.74) | ||
| Frozen products | 0.364 | 0.836 | |||
| Daily | 1.45 (0.44; 4.69) | 0.80 (0.31; 2.01) | 1.72 (0.46; 6.13) | ||
| Not daily | 98.55 (95.31; 99.56) | 99.20 (97.99; 99.69) | 98.28 (93.87; 99.54) | ||
| Sweet bread | 0.068 | 0.134 | |||
| Daily | 10.37 (7.93; 13.45) | 13.79 (9.22; 20.12) | 13.97 (9.36; 20.35) | ||
| Not daily | 89.63 (86.55; 92.07) | 86.21 (79.88; 90.78) | 86.03 (79.65; 90.64) | ||
| Sweets | 0.125 | 0.432 | |||
| Daily | 7.97 (5.31; 11.80) | 10.94 (6.64; 17.51) | 9.82 (5.78; 16.21) | ||
| Not daily | 92.03 (88.20; 94.69) | 89.06 (82.49; 93.36) | 90.18 (83.79; 94.22) | ||
∗ P-values < 0.05.
Proportion and 95% confidence interval (95% CI)
Probability values.
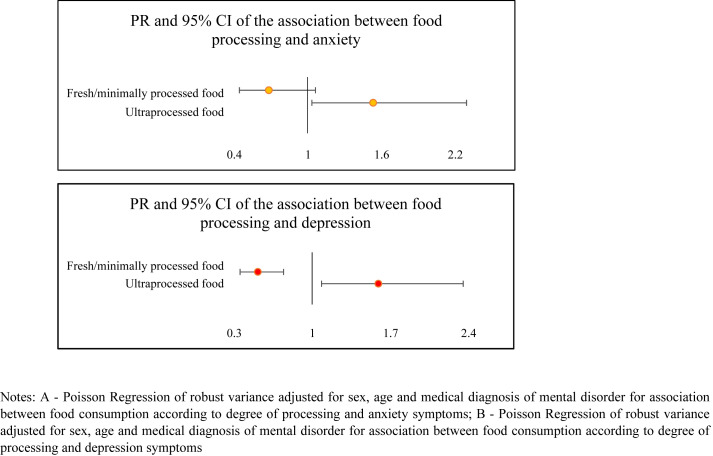
Through multivariate regression analysis of the relationship between food consumption according to the degree of processing and the presence of anxiety and depression symptoms (Fig. 3 ), it was observed that those with above-average weekly consumption of fresh and minimally processed foods had a lower prevalence ratio for depression symptoms (PR: 0.5 and 95% CI: 0.3–0.7). Above average consumption of ultra-processed foods was associated with a higher prevalence of anxiety and depression symptoms, respectively (PR: 1.5 and 95% CI: 1.03; 2.3/PR: 1.5 and 95% CI: 1.1; 2.1).
Fig. 3.
Prevalence ratio (PR) and 95% confidence interval (95% CI) for the association between consumption of fresh/minimally processed and ultra-processed foods and symptoms of anxiety and depression.
4. Discussion
This study revealed that the higher weekly frequency of consumption of fresh/minimally processed food, the lower the prevalence of depression symptoms, and the higher the weekly frequency of consumption of UPF, the higher the prevalence ratio of anxiety and depression symptoms. Moreover, a high prevalence of anxiety (23.3%) and depression (15.6%) symptoms were identified in the study population.
The prevalence identified by these results is close to the reported in studies conducted in other populations. Choi and colleagues [39] observed similar prevalence for both anxiety (19.8%) and depression (14.0%) in a sample of 500 adults in Hong Kong. Gao [17] found a 22.6% prevalence of anxiety symptoms in a sample of 4827 Chinese, while a study conducted by Solomou et al. [40] in the Mediterranean region, found that 23.1% of their sample had anxiety symptoms and 9.2% had depression symptoms. In Brazil, at the beginning of the pandemic, Barros [41] observed that 35.2% of the participants often felt depressed, while 41.3% felt anxious. The difference observed in the prevalence of anxiety and depression symptoms in this study, compared to a study conducted by Barros et al., both conducted in Brazil, may be attributed to the respective evaluation periods of each study. Barros and collaborators collected data concerning anxiety and depression at the beginning of the COVID-19 pandemic from April to May 2020, a period when fear, anguish, and insecurity were reported by most people [42,43]. Furthermore, the sampling method used in their study corresponds to a non-probability sample based on the snowball method using online interviews, while the present study used a stratified and conglomerate sample using face-to-face interviews. Additional longitudinal studies are necessary to fully understand this phenomenon.
The recent spread of the SARS-Cov-2 virus and its evolution into a pandemic, seems to be associated with an increase in the prevalence of mental illness [44]. Data suggest that infected individuals can be afflicted with symptoms of insomnia, anxiety, and depression [45]. Moreover, sudden changes in routine and lifestyle are associated with mental illness. Such changes, present in the context of a pandemic, are characterized by the imposition of social distancing with consequent reduction of social interaction [[46], [47], [48]], feelings of insecurity and fear [[48], [49], [50]], changes in the work routine [51], food insecurity, and changes in food consumption [[14], [48], [52]].
The results presented in this study should be interpreted in light of the current epidemiological and nutritional scenario of the Brazilian and global population, which shows a trend towards lower consumption of food sources of nutrients capable of mitigating the symptoms of anxiety and depression [53], with a significant increase in the consumption of ultra-processed foods that are poor in micronutrients [54,55]. In Brazil, the lower consumption of traditional Brazilian food was observed through the Family Budget Survey, and there was an observed increase in consumption of UPF [56]. This reversal in food consumption is related to maladaptive health outcomes, which are described as public health problems, including depression [3,27].
Recent scientific evidence suggests that food consumption plays an important role in the occurrence of mental illness [3,8,57,58]. Epidemiological data related food consumption to poor mental health through inflammatory reactions and deficiency of nutrients and neurotransmitters [[59], [60], [61]]. It is noteworthy that excessive consumption of carbohydrates and sugar has been described as a risk factor for mental illness due to being related to an increase in neuroinflammation within the hippocampus [62]. In contrast, the consumption of complex carbohydrates, such as vegetables, fruits, and fibers, is encouraged because they are sources of vitamins and polyphenols, and are metabolized into short-chain fatty acids, which are important anti-inflammatory agents [62,63].
Furthermore, fatty acids have been widely studied for their anti-inflammatory properties [59] and neuroendocrine modulation of neurotransmitters, such as serotonin and dopamine [[64], [65]]. Complex B, D, and E vitamins, which are richly present in fresh/minimally processed foods, are important in modulating brain functions related to cognitive performance, prevention of neurodegenerative disorders, protection against oxidative stress, and myelination of neurotransmitters [[66], [67], [68]].
Therefore, it is understood that a diet rich in fresh foods and nutrients is important in promoting health, while a diet rich in UPF, deficient in vitamins, minerals, and proteins, and high in saturated fat, sugar, salt, strongly flavored ingredients, and chemical additives, is capable of disrupting natural satiety mechanisms and acting on hyper stimulation of reward-related brain regions (i.e., striatum and orbitofrontal medial cortex), leading to binge eating and food addiction [[69], [70], [71], [72], [73]], as well as being related to all causes of mortality [74,75].
Thus, there is a strong need for the reformulation of public health policies, with the inclusion of regulatory standards for consumption of UPF and incentivization of consumption of fresh/minimally processed foods, in order to promote policies to improve food quality and health [76,77], based on the Dietary Guidelines for the Brazilian Population [9], which considers the degree of food processing and reinforces conscious consumption, considering various aspects of food. Political action is necessary to encourage healthy choices and to control the food industry that creates easily distributed products and advertising [76]. Thus, fiscal policies [[78], [79], [80]], mandatory warning labels [81 [82], [83]], marketing restrictions [83,84], and incentives for food and nutrition education, are fundamental to controlling the UPF consumption [9].
However, the results of this study should be interpreted with caution. First, this is a cross-sectional study, which does not allow us to establish causal inferences or the bidirectionality of the data. The explanatory variables were measured from a qualitative point of view, making it impossible to analyze the precise quantities of each food group that was consumed, and food consumption was measured using a non-validated questionnaire used in a national survey. In addition, the outcome was assessed according to the presence anxiety and depression symptoms, measured using scales, and not via medical diagnosis. However, the scales used have been validated and have good diagnostic accuracy [85,86]. It should be highlighted that face-to-face interviews allowed for greater accuracy of the information obtained and promoted methodological robustness, while probabilistic sample selection and sample weight provided statistical power to the study, as well as internal and external validity.
In conclusion, the present study revealed the existence of an inverse association between a higher frequency of consumption of fresh/minimally processed food and the prevalence of depression symptoms, as well as an association between the higher frequency of consumption of UPF and a higher prevalence ratio of depression symptoms, thus encouraging the consumption of food with a lower degree of processing, referenced by the Brazilian food culture, recommended by the Dietary Guidelines for the Brazilian Population [9]. Thus, further studies are needed to explore the consequences of food consumption, according to the degree of processing, and the development of anxiety and depression.
Ethical approval
The study was approved by the Research Ethic Committee of the Universidade Federal de Minas Gerais (Protocol no 4.135.077) and all participants signed the written informed consent.
Funding statement
This work was supported by the Universidade Federal de Ouro Preto and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Funding Code: CAPES 09/2020 – no 23038.003012/2020-16.
Author's contributions
Hillary Nascimento Coletro – conception and study design; analysis and interpretation of data; writing the manuscript, critical review and final approval.
Raquel de Deus Mendonça – analysis and interpretation of data, critical review and final approval.
Adriana Lúcia Meireles – conception and coordination of data collection, critical review, management of financial resources and final approval.
George Luiz Lins Machado-Coelho – conception and coordination of data collection, critical review, management of financial resources and final approval.
Mariana Carvalho de Menezes – conception and study design, analysis and interpretation of data; critical review, supervision and final approval.
Declaration of competing interest
The authors declare no conflict of interest, they are fully responsible for the content and writing of the manuscript.
Acknowledgments
The authors thank the Grupo de Pesquisa e Ensino em Nutrição e Saúde Coletiva for their support and encouragement. We also thank the Universidade Federal de Ouro Preto, Fundação de Amparo à Pesquisa do Estado de Minas Gerais, Conselho Nacional de Desenvolvimento Científico e Tecnológico and the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior for their financial support, Financial Code 88881.504995/2020-01 and we thank the Ouro Preto and Mariana City Halls and Municipal Health Offices for the partnership.
References
- 1.World Health Organization . vol. 48. 2017. (Depression and other common mental disorders). [Google Scholar]
- 2.Friedrich M.J. Depression is the leading cause of disability around the world. JAMA. 2017;317(15):529–545. doi: 10.4337/9781783478651. [DOI] [PubMed] [Google Scholar]
- 3.Adjibade Moufidath, Julia Chantal, Allès Benjamin, Touvier Mathilde, Lemogne Cédric, Srour Bernard, et al. Prospective association between ultra-processed food consumption and incident depressive symptoms in the French NutriNet-Santé cohort. BMC Med. 2019;17(1):1–13. doi: 10.1186/s12916-019-1312-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rahe C., Unrath M., Berger K. Dietary patterns and the risk of depression in adults: a systematic review of observational studies. Eur J Nutr. 2014;53(4):997–1013. doi: 10.1007/s00394-014-0652-9. [DOI] [PubMed] [Google Scholar]
- 5.Molendijk M., Molero P., Ortuño Sánchez-Pedreño F., Van der Does W., Angel Martínez-González M. Diet quality and depression risk: a systematic review and dose-response meta-analysis of prospective studies. J Affect Disord. 2018;226:346–354. doi: 10.1016/j.jad.2017.09.022. [DOI] [PubMed] [Google Scholar]
- 6.Li Y., Lv M.R., Wei Y.J., Sun Ling, Zhang J.X., Zhang H.G., et al. Dietary patterns and depression risk: a meta-analysis. Psychiatry Res. 2017;253:373–382. doi: 10.1016/j.psychres.2017.04.020. [DOI] [PubMed] [Google Scholar]
- 7.Wang J., Zhou Y., Chen K., Jing Y, He J, Sun H, et al. Dietary inflammatory index and depression: a meta-analysis. Public Health Nutr. 2019;22(4):654–660. doi: 10.1017/S1368980018002628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El Ansari W., Adetunji H., Oskrochi R. Food and mental health: relationship between food and perceived stress and depressive symptoms among university students in the United Kingdom. Cent Eur J Public Health. 2014;22(2):90–97. doi: 10.21101/cejph.a3941. [DOI] [PubMed] [Google Scholar]
- 9.Brasil . 2014. Guia Alimentar Para a População Brasileira Guia Alimentar Para a População Brasileira. [Google Scholar]
- 10.Dutheil S., Ota K.T., Wohleb E.S., Rasmussen K., Duman R.S. High-fat diet induced anxiety and anhedonia: impact on brain homeostasis and inflammation. Neuropsychopharmacology. 2016;41(7):1874–1887. doi: 10.1038/npp.2015.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cook N.R., He F.J., MacGregor G.A., Graudal N. Sodium and health-concordance and controversy. BMJ. 2020;369:m2440. doi: 10.1136/bmj.m2440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacka F.N., Cherbuin N., Anstey K.J., Sachdev P., Butterworth P. Western diet is associated with a smaller hippocampus: a longitudinal investigation. BMC Med. 2015;13(1):1–8. doi: 10.1186/s12916-015-0461-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith W., Do F. Isolation, quarantine, social distancing and community containment: pivotal role for old- style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;27(2) doi: 10.1093/jtm/taaa020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huizar M.I., Arena R., Laddu D.R. The global food syndemic: the impact of food insecurity, malnutrition and obesity on the healthspan amid the COVID-19 pandemic. Prog Cardiovasc Dis. 2021;64:105–107. doi: 10.1016/j.pcad.2020.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Di Renzo L., Gualtieri P., Pivari F., Soldati L, Attinà A, Cinelli G, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020;18(1):1–15. doi: 10.1186/s12967-020-02399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Talevi D., Socci V., Carai M., Carnaghi G, Faleri S, Trebbi E, et al. Mental health outcomes of the covid-19 pandemic. Riv Psichiatr. 2020;55(3):137–144. doi: 10.1708/3382.33569. [DOI] [PubMed] [Google Scholar]
- 17.Gao J., Zheng P., Jia Y., Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One. 2020;15(4):1–10. doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whiteford H.A., Degenhardt L., Rehm J., Baxter A.J, Ferrari A.J., Erskine H.E., et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- 19.Vigo D., Thornicroft G., Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–178. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- 20.Liu Q., He H., Yang J., Feng X., Zhao F., Lyu J. Changes in the global burden of depression from 1990 to 2017: findings from the global burden of disease study. J Psychiatr Res. 2020;126(August):134–140. doi: 10.1016/j.jpsychires.2019.08.002. [DOI] [PubMed] [Google Scholar]
- 21.Rehm J., Shield K.D. Global burden of disease and the impact of mental and addictive disorders. Curr Psychiatry Rep. 2019;21(2):1–7. doi: 10.1007/s11920-019-0997-0. [DOI] [PubMed] [Google Scholar]
- 22.Rauber F., Louzada ML. da C., Steele E.M., Millett C., Monteiro C.A., Levy R.B. Ultra-processed food consumption and chronic non-communicable diseases-related dietary nutrient profile in the UK (2008–2014) Nutrients. 2018;10(5) doi: 10.3390/nu10050587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Juul F., Martinez-Steele E., Parekh N., Monteiro C.A., Chang V.W. Ultra-processed food consumption and excess weight among US adults. Br J Nutr. 2018;120(1):90–100. doi: 10.1017/S0007114518001046. [DOI] [PubMed] [Google Scholar]
- 24.Fiolet T., Srour B., Sellem L., Kesse-Guyot E., Allès B., Deschasaux M., et al. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ. 2018;360 doi: 10.1136/bmj.k322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Monteiro C.A., Moubarac J.C., Levy R.B., Canella D.S., Da Costa Louzada M.L., Cannon G. Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutr. 2018;21(1):18–26. doi: 10.1017/S1368980017001379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Passos CM dos, Maia E.G., Levy R.B., Martins A.P.B., Claro R.M. Association between the price of ultra-processed foods and obesity in Brazil. Nutr Metab Cardiovasc Dis. 2020;30(4):589–598. doi: 10.1016/j.numecd.2019.12.011. [DOI] [PubMed] [Google Scholar]
- 27.Gómez-Donoso C., Sánchez-Villegas A., Martínez-González M.A., Gea A., Mendonça R.D., Lahortiga-Ramos F., et al. Ultra-processed food consumption and the incidence of depression in a Mediterranean cohort: the SUN project. Eur J Nutr. 2019:1093–1103. doi: 10.1007/s00394-019-01970-1. [Published online 2020] [DOI] [PubMed] [Google Scholar]
- 28.Meireles A.L., Lourenção L.G., Antônio L., Coletro H.N., Justiniano I.C.S., Moura S.S., et al. COVID-inconfidentes – SARS-CoV-2 seroprevalence in two Brazilian urban areas during the pandemic first wave: study protocol and initial results. Scielo preprint. 2021;29 (Scielo preprint) [Google Scholar]
- 29.IBGE . 2013. Atlas do Censo Demografico. [Google Scholar]
- 30.Löwe B., Decker O., Müller S., Brähler E., Schellberg D., Herzog W., et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care. 2008;46(3):266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 31.Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ministério da Saúde Vigitel Brasil 2019. 2020. https://www.saude.gov.br/images/pdf/2020/April/27/vigitel-brasil-2019-vigilancia-fatores-risco.pdf
- 33.Monteiro C.A., Levy R.B., Claro R.M., Castro IRR de, Cannon G. A new classification of foods based on the extent and purpose of their processing. Cad Saúde Pública. 2010;26(11):2039–2049. doi: 10.1590/s0102-311x2010001100005. [DOI] [PubMed] [Google Scholar]
- 34.Wang L, Martínez Steele E, Du M, Pomeranz J.L., O’Connor L.E., Herrick K.A., et al. Trends in Consumption of Ultraprocessed Foods Among US Youths Aged 2–19 Years, 1999–2018. JAMA. 2021;326(6):519–530. doi: 10.1001/jama.2021.10238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ministério da Saúde Censo 2010. 2011. http://www2.datasus.gov.br/DATASUS/index.php?area=0206&id=6942
- 38.Silva PL do N., Pessoa D.G.C., Lila M.F. Análise estatística de dados da PNAD: incorporando a estrutura do plano amostral - statistical analysis of data from PNAD: incorporating the sample design. Cien Saude Colet. 2002;7(4):659–670. http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1413-81232002000400005&nrm=iso [Google Scholar]
- 39.Choi E.P.H., Hui B.P.H., Wan E.Y.F. Depression and anxiety in Hong Kong during covid-19. Int J Environ Res Public Health. 2020;17(10) doi: 10.3390/ijerph17103740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Solomou I., Constantinidou F. Prevalence and predictors of anxiety and depression symptoms during the COVID-19 pandemic and compliance with precautionary measures: age and sex matter. Int J Environ Res Public Health. 2020;17(14):1–19. doi: 10.3390/ijerph17144924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barros MB. de A., Lima M.G., Malta D.C., Szwarcwald C.L, Azevedo R.C.S., Romero Dalia, et al. Relato de tristeza/depressão, nervosismo/ansiedade e problemas de sono na população adulta brasileira durante a pandemia de COVID-19. Epidemiol Serv Saude Rev Sist Unico Saude Bras. 2020;29(4) doi: 10.1590/s1679-49742020000400018. [DOI] [PubMed] [Google Scholar]
- 42.Ornell Felipe, Schuch Jaqueline B., Sordi Anne O., Kessler Felix Henrique Paim. ‘Pandemic fear’ and COVID-19: mental health burden and strategies. Braz J Psychiatry. 2020;42(3):232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saúde Pública. 2020;36(4) doi: 10.1590/0102-311X00054020. [DOI] [PubMed] [Google Scholar]
- 44.Troyer E.A., Kohn J.N., Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020;87(April):34–39. doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rogers J.P., Chesney E., Oliver D., Pollak T.A., McGuire P., Fusar-Poli P., et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry. 2020;7(7):611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marroquín B, Vine V, Morgan R. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- 19. The COVID-19 resource centre is hosted on Elsevier Connect, the company's public news and information. 2020 (January).
- 47.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hamadani Jena Derakhshani, Hasan Mohammed Imrul, Baldi Andrew J., Hossain Sheikh Jamal, Shiraji Shamima, Alam Bhuiyan Mohammad Saiful, et al. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Heal. 2020;(January):19–21. doi: 10.1016/S2214-109X(20)30366-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li S., Wang Y., Xue J., Zhao N., Zhu T. The impact of covid-19 epidemic declaration on psychological consequences: a study on active weibo users. Int J Environ Res Public Health. 2020;17(6) doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xiao Y., Becerik-Gerber B., Lucas G., Roll S.C. Impacts of working from home during COVID-19 pandemic on physical and mental well-being of office workstation users. J Occup Environ Med. 2021;63(3):181–190. doi: 10.1097/JOM.0000000000002097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Elgar F.J., Pickett W., Pförtner T.K., Gariépy G., Gordon D., Georgiades K., et al. Relative food insecurity, mental health and wellbeing in 160 countries. Soc Sci Med. 2021;268:113556. doi: 10.1016/j.socscimed.2020.113556. [DOI] [PubMed] [Google Scholar]
- 53.Lassale C., Batty G.D., Baghdadli A., Jacka F., Sánchez-Villegas A., Kivimäki M., et al. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatry. 2019;24(7):965–986. doi: 10.1038/s41380-018-0237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Luiten C.M., Steenhuis I.H.M., Eyles H., Mhurchu C.N., Waterlander W.E. Ultra-processed foods have the worst nutrient profile, yet they are the most available packaged products in a sample of New Zealand supermarkets. Public Health Nutr. 2016;19(3):530–538. doi: 10.1017/S1368980015002177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Julia C., Martinez L., Allès B., Touvier M., Hercberg S., Méjean C., et al. Contribution of ultra-processed foods in the diet of adults from the French NutriNet-Santé study. Public Health Nutr. 2018;21(1):27–37. doi: 10.1017/S1368980017001367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Instituto Brasileiro de Geografia e Estatística Pesquisa de Orçamentos Familiares 2017-2018: Primeiros resultados. 2019. https://biblioteca.ibge.gov.br/visualizacao/livros/liv101670.pdf
- 57.Gibson-Smith D., Bot M., Brouwer I.A., Visser M., Penninx B.W.J.H. Diet quality in persons with and without depressive and anxiety disorders. J Psychiatr Res. 2018;106:1–7. doi: 10.1016/j.jpsychires.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 58.Saghafian F., Malmir H., Saneei P., Keshteli A.H., Hosseinzadeh-Attar M.J., Afshar H., et al. Consumption of fruit and vegetables in relation with psychological disorders in Iranian adults. Eur J Nutr. 2018;57(6):2295–2306. doi: 10.1007/s00394-018-1652-y. [DOI] [PubMed] [Google Scholar]
- 59.Kris-Etherton P.M., Petersen K.S., Hibbeln J.R., Hurley D., Kolick V., Peoples S., et al. Nutrition and behavioral health disorders: depression and anxiety. Nutr Rev. 2021;79(3):247–260. doi: 10.1093/nutrit/nuaa025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Adan R.A.H., van der Beek E.M., Buitelaar J.K., Cryan J.F., Hebebrand J., Higgs S., et al. Nutritional psychiatry: towards improving mental health by what you eat. Eur Neuropsychopharmacol. 2019;29(12):1321–1332. doi: 10.1016/j.euroneuro.2019.10.011. [DOI] [PubMed] [Google Scholar]
- 61.Godos J., Currenti W., Angelino D., Mena P., Castellano S., Caraci F., et al. Diet and mental health: review of the recent updates on molecular mechanisms. Antioxidants. 2020;9(4):1–13. doi: 10.3390/antiox9040346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Irwin Michael R., Olmstead Richard, Carroll Judith E. sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80(1):40–52. doi: 10.1016/j.biopsych.2015.05.014.Sleep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Minihane A.M., Vinoy S., Russell W.R., Baka A., Roche H.M., Tuohy K.M., et al. Low-grade inflammation, diet composition and health: current research evidence and its translation. Br J Nutr. 2015;114(7):999–1012. doi: 10.1017/S0007114515002093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Grosso G., Galvano F., Marventano S., Malaguarnera M., Bucolo C., Drago F., et al. Omega-3 fatty acids and depression: scientific evidence and biological mechanisms. Oxid Med Cell Longev. 2014;2014(figure 1) doi: 10.1155/2014/313570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Oddy W.H., Hickling S., Smith M.A., O’Sullivan T.A., Robinson M., Klerk N.H, et al. Dietary intake of omega-3 fatty acids and risk of depressive symptoms in adolescents. Depress Anxiety. 2011;28(7):582–588. doi: 10.1002/da.20822. [DOI] [PubMed] [Google Scholar]
- 66.Zeng Y., Yang J., Du J., Pu X., Yang X., Yang S., et al. Strategies of functional foods promote sleep in human being. Curr Signal Transduct Ther. 2015;9(3):148–155. doi: 10.2174/1574362410666150205165504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Smith A.D., Refsum H. Homocysteine, B vitamins, and cognitive impairment. Annu Rev Nutr. 2016;36:211–239. doi: 10.1146/annurev-nutr-071715-050947. [DOI] [PubMed] [Google Scholar]
- 68.Guenther B.D., Christensen C.R., Upatnieks J. Coherent optical processing: another approach. IEEE J Quantum Electron. 1979;15(12):1348–1362. doi: 10.1109/JQE.1979.1069953. [DOI] [Google Scholar]
- 69.Drewnowski A., Gupta S., Darmon N. An overlap between “ultraprocessed” foods and the preexisting nutrient rich foods index? Nutr Today. 2020;55(2):75–81. doi: 10.1097/NT.0000000000000400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lawrence M. Ultraprocessed foods and cardiovascular health: it's not just about the nutrients. Am J Clin Nutr. 2021;113(2):257–258. doi: 10.1093/ajcn/nqaa333. [DOI] [PubMed] [Google Scholar]
- 71.Schulte E.M., Avena N.M., Gearhardt A.N. Which foods may be addictive? The roles of processing, fat content, and glycemic load. PLoS One. 2015;10(2):1–18. doi: 10.1371/journal.pone.0117959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhang Z., Jackson S.L., Martinez E., Gillespie C., Yang Q. Association between ultraprocessed food intake and cardiovascular health in US adults: a cross-sectional analysis of the NHANES 2011-2016. Am J Clin Nutr. 2021;113(2):428–436. doi: 10.1093/ajcn/nqaa276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schulte E.M., Gearhardt A.N. Attributes of the food addiction phenotype within overweight and obesity. Eat Weight Disord. 2021;26(6):2043–2049. doi: 10.1007/s40519-020-01055-7. [DOI] [PubMed] [Google Scholar]
- 74.Blanco-Rojo R., Sandoval-Insausti H., López-Garcia E., Graciani A., Ordovás J.M., Banegas J.R., et al. Consumption of ultra-processed foods and mortality: a national prospective cohort in Spain. Mayo Clin Proc. 2019;94(11):2178–2188. doi: 10.1016/j.mayocp.2019.03.035. [DOI] [PubMed] [Google Scholar]
- 75.Rico-Campà A., Martínez-González M.A., Alvarez-Alvarez I., Mendonça R.D., de la Fuente-Arrillaga C., Gómez-Donoso C., et al. Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ. 2019;365 doi: 10.1136/bmj.l1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Monteiro C.A., Lawrence M., Millett C., Nestle M., Popkin B.M., Scrinis G., et al. The need to reshape global food processing: a call to the United Nations Food Systems Summit. BMJ Glob Heal. 2021;6(7) doi: 10.1136/bmjgh-2021-006885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Popkin Barry M., Barquera Simon, Corvalan Camila, Hofman Karen J., Monteiro Carlos, Ng Shu Wen, et al. Towards unified and impactful policies to reduce ultra-processed food consumption and promote healthier eating. Lancet. 2021;Jul;9(7):462–470. doi: 10.1016/S2213-8587(21)00078-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bíró A. Did the junk food tax make the Hungarians eat healthier? Food Policy. 2015;54:107–115. doi: 10.1016/j.foodpol.2015.05.003. [DOI] [Google Scholar]
- 79.Teng A.M., Jones A.C., Mizdrak A., Signal L., Genç M., Wilson N. Impact of sugar-sweetened beverage taxes on purchases and dietary intake: systematic review and meta-analysis. Obes Rev. 2019;20(9):1187–1204. doi: 10.1111/obr.12868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sánchez-Romero L.M., Canto-Osorio F., González-Morales R., Colchero M.A., Ng S-W., Ramírez-Palacios P., et al. Association between tax on sugar sweetened beverages and soft drink consumption in adults in Mexico: open cohort longitudinal analysis of Health Workers Cohort Study. BMJ. 2020;369 doi: 10.1136/bmj.m1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Corvalán C., Reyes M., Garmendia M.L., Uauy R. Structural responses to the obesity and non-communicable diseases epidemic: update on the Chilean law of food labelling and advertising. Obes Rev. 2019;20(3):367–374. doi: 10.1111/obr.12802. [DOI] [PubMed] [Google Scholar]
- 82.Taillie L.S., Reyes M., Colchero M.A., Popkin B., Corvalán C. An evaluation of Chile's law of food labeling and advertising on sugar-sweetened beverage purchases from 2015 to 2017: a before-and-after study. PLoS Med. 2020;17(2):1–22. doi: 10.1371/JOURNAL.PMED.1003015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.World Health Organization. Framework for implementing the set of recommendations on the marketing of foods and non-alcoholic beverages to children. World Heal Organ. Published online 2012:1-16. http://www.who.int/about/licensing/.
- 84.World Health Organization. Tackling food marketing to children in a digital world: trans-disciplinary perspectives Children's rights, evidence of impact, methodological challenges, regulatory options and policy implications for the WHO European Region. Published online 2016.
- 85.Plummer F., Manea L., Trepel D., McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24–31. doi: 10.1016/j.genhosppsych.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 86.Levis B., Benedetti A., Thombs B.D. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. 2019;365 doi: 10.1136/bmj.l1476. [DOI] [PMC free article] [PubMed] [Google Scholar]