Dear editor,
We read with interest the recent systematic review by Fricke et al., showing that the number and positivity rate of influenza cases have decreased in result of non-pharmaceutic interventions targeted at the COVID-19 pandemic.1 Similarly, a report in the United States had shown that the incidences of acute otitis media and streptococcal pharyngitis decreased, while gonorrhea increased during quarantine.2 These studies show that COVID-19 containment measures and the overall behavioral changes in the communities are likely to have an effect in the transmission and/or reporting of other infections. We here show the results of Norovirus (NoV) surveillance data in Germany, and describe the effect of the containment measures taken in the context of the COVID-19 pandemic on the number and rate of NoV-positive tests in Germany.
NoV is the leading cause of acute gastroenteritis (AGE) globally across all age groups, causing an estimated 18% of all diarrheal disease cases worldwide,3 and over 200,000 deaths every year.4 In Germany, NoV is notifiable to the Robert Koch Institute, which has registered nearly 100,000 cases of NoV notified infections every year since 2010 (https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2020/24/Art_01.html). NoV hospitalizations account for 11–16% of all AGE hospitalizations, and they show a seasonal distribution with a peak from December-March each year.5 NoV diagnosis is related to reimbursement rates for gastroenteritis hospitalization in Germany, providing a strong incentive to test for NoV in the hospital setting. Taking advantage of the routine testing in one of the largest commercial laboratories, a surveillance study was designed to provide up-to-date evidence on the occurrence of NoV across all ages, circulating genotypes and co-infections in Germany.
The 2020 COVID-19 pandemic has triggered the implementation of different containment measures across the globe. Germany reported the first cases in late January6 and responded by implementing community mitigation and mobility restriction measures since the first COVID-related deaths were reported in March.7 From mid-March until early May, schools and bars were closed, borders with neighboring countries were controlled, travel was restricted, and general social distancing measures were adopted. With the mandatory use of masks in place since the end of April, reopening was gradual, but several limitations were still in place by the date this article was submitted.7
This study is based on a larger prospective, laboratory-based surveillance study on NoV infection. The surveillance relies upon results from all clinical specimens tested for NoV and other enteropathogens submitted to the Limbach Laboratory (MVZ Dr. Limbach & Kollegen GbR, Heidelberg MVZ), from patients of all ages and all genders. The Limbach Laboratory tests samples referred by hospitals across all of Germany. These samples can originate from all age groups, all types of inpatients across various departments as well as outpatients whose specimens are sent to the laboratory for testing. Here we report data from the start of the surveillance (February 2018) to December 2020. Data collected includes aggregated totals of samples tested for NoV and PCR testing results. Data is provided per setting (inpatients or outpatients) and per age group, although we only report totals for all ages. To analyze trends in NoV gastroenteritis, we summarized monthly positivity rates of NoV per setting. The proportions of positives were estimated with exact 95% confidence intervals using R v.4.0.2.8
From February 2018 to December 2020, 31,765 specimens were tested for NoV and other enteropathogens. Most specimens (27,795, 87.5%) were collected from hospitalized patients (reasons for hospitalization are unknown). Of all specimens tested, 3970 (12.5%) yielded positive PCR results for NoV. The overall percentage of NoV-positive specimens was similar in the hospital (12.4%) and outpatient (12.8%) settings.
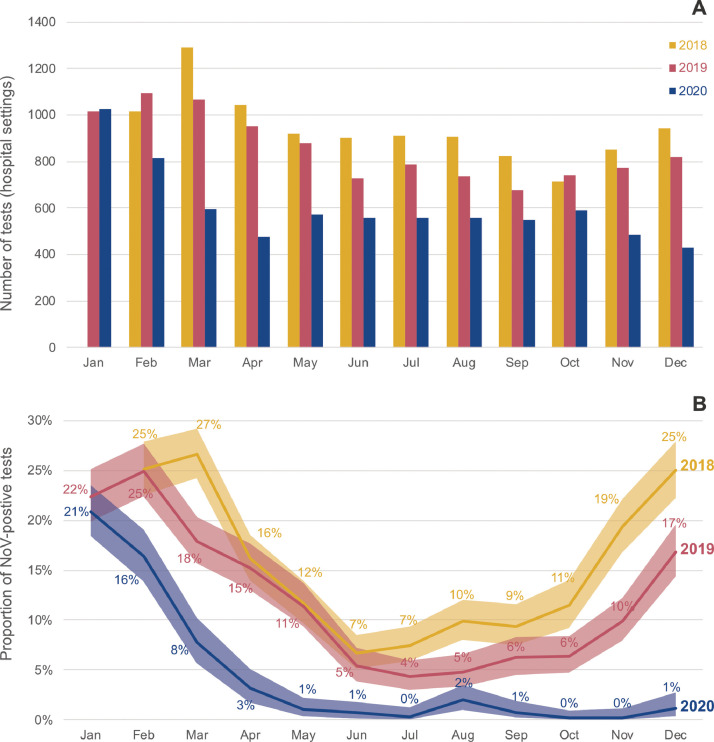
Fig. 1 shows the monthly distribution of stool samples tested for NoV, and the NoV-positive proportion among hospitalized patients. The distribution among outpatients was similar, but with larger confidence intervals due to the smaller sample size (data not shown). As expected, a strong seasonal effect is visible in the proportion of NoV-positive specimens in the years 2018 and 2019, with the proportion of NoV positives increasing from November/December until March. In these two years, the lowest proportion of NoV-positive tests were observed in July (4.3%) and August (4.8%) 2019 (Fig. 1). The overall number of tests performed in the years 2018 and 2019 shows a weaker seasonal pattern, with the number of tests never below 600 per month.
Fig. 1.
Monthly distribution of total tests performed (A) and proportion of NoV-positive samples (B) among hospitalized patients, from February 2018 to December 2020. The shaded areas represent 95% confidence intervals.
In 2020, the percentage of NoV-positive specimens decreased sharply after January, reaching near 0% as of May and continuing around 0% thereafter. The total number of samples tested for NoV also decreased from February to May, but never went below 400 per month.
The surveillance data suggest a significant impact of the COVID-19 control measures on the NoV positivity rates among stool samples from patients hospitalized in Germany after January 2020. As previously reported for Germany,5 the number of NoV hospitalizations typically starts to increase in November-December, until the peak is reached in January-March. In the 2019–2020 season, the peak in January was followed by a steep decrease in the number of tests and proportion of NoV-positives. The months of February to May 2020 have registered a significantly lower proportion of NoV-positive specimens than in previous years, until they almost disappeared from May onwards.
Starting in March 2020, Germany has adopted several measures to contain the COVID pandemic, including closure of schools, bars and large events. At the same time, the population adopted preventive behaviors such as social distancing measures and the use of hand sanitizer. It is safe to assume that these measures could result in a decrease of other infections. NoV is highly contagious via the fecal-oral route, through contaminated hands or by consumption of contaminated food and water, giving rise to frequent outbreaks in institutions or restaurants.9 The sharp decrease in the proportion of NoV-positive cases observed in 2020 is likely related to the closure of schools, restaurants and other institutions, as well as of other containment measures. Behavioral changes preceding the containment measures, which only became effective in March, may have caused the decrease in the NoV positivity rates to start already in February, triggered by reports from Italy or Spain. In fact, the number of cases exploded in Italy from February 22nd. On March 10th, when Germany reported its first two COVID-related deaths, Italy already counted 464 deaths and over 9000 cases, and Spain had over 2000 reported cases.6
Our study has some limitations. We do not possess clinical information on the patients whose samples were tested. Though this is unlikely, we cannot exclude that patients infected with norovirus presented less frequently to medical care than other AGE patients in 2020. Our analyses are ecological in nature and we can also not exclude that there is a natural decline of NoV circulation, independent of the COVID-19 control measures. However, since NoV is known to be transmitted primarily via person-to-person contacts, it is fair to assume the control measures have played a major role in this decline. Finally, it is unknown whether NoV incidence will return to pre-COVID-19 values once behavioral restrictions are relaxed.
This study shows that NoV infections have become less frequent in Germany since the beginning of the COVID-19 epidemic in Europe. Whereas this is a positive observation from a public health perspective, it also has a significant impact on NoV vaccine development programs. Several NoV vaccines are under development, with one vaccine entering Phase II trials.10 The COVID-19 pandemic hinders the conduct of these trials by the logistical challenges in enrolling and following up subjects, and Phase III trials are unlikely to show efficiency due to the current low NoV positivity rates. It is unknown how NoV infections will evolve once containment measures are loosened.
Declaration of Competing Interest
Ulrich Eigner and Thomas Verstraeten report consulting grants from Takeda Pharmaceuticals AG to Labor Limbach and P95. John Weil is an employee of Takeda Pharmaceuticals International AG.
Acknowledgments
Acknowledgements
The authors are grateful to Dr. Daniela Bertsch, Ulrike Betz and Melissa Kolb for their contribution to the study in the field. The authors acknowledge Ana Goios for medical writing and editorial support, and Anirudh Tomer for data analysis support (both affiliated to P95 Epidemiology and Pharmacovigilance, Leuven, Belgium).
Funding
This work was supported by Takeda Vaccines, Inc. The sponsor provided some input on the study design of this study. The authors had responsibility for the submission of this manuscript for publication.
References
- 1.Fricke L.M., Glockner S., Dreier M., Lange B. Impact of non-pharmaceutical interventions targeted at COVID-19 pandemic on influenza burden - a systematic review. J Infect. 2021;82(1):1–35. doi: 10.1016/j.jinf.2020.11.039. PubMed PMID: 33278399Epub 2020/12/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McBride J.A., Eickhoff J., Wald E.R. Impact of Covid-19 quarantine and school cancelation on other common infectious diseases. Pediatr. Infect. Dis. J. 2020 doi: 10.1097/INF.0000000000002883. PubMed PMID: 33031142Epub 2020/10/09. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed S.M., Hall A.J., Robinson A.E., Verhoef L., Premkumar P., Parashar U.D., et al. Global prevalence of norovirus in cases of gastroenteritis: a systematic review and meta-analysis. The Lancet Infect Dis. 2014;14(8):725–730. doi: 10.1016/S1473-3099(14)70767-4. PubMed PMID: 24981041Epub 2014/07/02. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bartsch S.M., Lopman B.A., Ozawa S., Hall A.J., Lee B.Y. Global economic burden of norovirus gastroenteritis. PLoS ONE. 2016;11(4) doi: 10.1371/journal.pone.0151219. PubMed PMID: 27115736Pubmed Central PMCID: PMC4846012. Epub 2016/04/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kowalzik F., Binder H., Zoller D., Riera-Montes M., Clemens R., Verstraeten T., et al. Norovirus gastroenteritis among hospitalized patients, Germany, 2007-2012. Emerg Infect Dis. 2018;24(11):2021–2028. doi: 10.3201/eid2411.170820. PubMed PMID: 30334712Pubmed Central PMCID: PMC6199990. Epub 2018/10/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Global Change Data Lab. Our World in Data: coronavirus Pandemic (COVID-19) [2020]. Available from: https://ourworldindata.org/coronavirus.
- 7.Wieler L., Rexroth U., Gottschalk R. 2020. Emerging COVID-19 success story: Germany's strong enabling environment 2020.https://ourworldindata.org/covid-exemplar-germany Available from: [Google Scholar]
- 8.R Development Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2020. R: A language and environment for statistical computing. [Google Scholar]
- 9.Banyai K., Estes M.K., Martella V., Parashar U.D. Viral gastroenteritis. Lancet. 2018;392(10142):175–186. doi: 10.1016/S0140-6736(18)31128-0. PubMed PMID: 30025810Epub 2018/07/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Esposito S., Principi N. Norovirus vaccine: priorities for future research and development. Front Immunol. 2020;11:1383. doi: 10.3389/fimmu.2020.01383. PubMed PMID: 32733458Pubmed Central PMCID: PMC7358258. Epub 2020/08/01. [DOI] [PMC free article] [PubMed] [Google Scholar]