Abstract
The visual system offers unparalleled precision in the assessment of neuroaxonal damage. With the majority of patients with multiple sclerosis (MS) experiencing afferent and efferent visual dysfunction, outcome measures capturing these deficits provide insight into neuroaxonal injury, even in those with minimal disability. Ideal for use in clinical trials, visual measures are generally inexpensive, accessible, and reproducible. Quantification of visual acuity, visual fields, visual quality of life, and electrophysiologic parameters allows assessment of function, whereas optical coherence tomography (OCT) provides reliable measures of the structural integrity of the anterior afferent visual pathway. The technology of oculomotor biometrics continues to advance, and discrete measures of fixation, smooth pursuit, and saccadic eye movement abnormalities are ready for inclusion in future trials of MS progression. Visual outcomes allow tracking of neuroaxonal injury and aid in distinguishing MS from diseases such as neuromyelitis optica spectrum disorder (NMOSD) or myelin oligodendrocyte glycoprotein antibody–associated diseases (MOGAD). OCT has also provided unique insights into pathophysiology, including the identification of foveal pitting in NMOSD, possibly from damage to Müller cells, which carry an abundance of aquaporin-4 channels. For some study designs, the cost-benefit ratio favors visual outcomes over more expensive MRI outcomes. With the next frontier of therapeutics focused on remyelination and neuroprotection, visual outcomes are likely to take center stage. As an international community of collaborative, committed, vision scientists, this review by the International MS Visual System Consortium (IMSVISUAL) outlines the quality standards, informatics, and framework needed to routinely incorporate vision outcomes into MS and NMOSD trials.
The first revolution in ophthalmology occurred in 1845 with the invention of the ophthalmoscope. Before this time, there was no clear way to differentiate visual disorders; diseases were categorized only as either ophthalmia or blindness.1 Progress was made into the early 20th century when optic neuritis (ON) was distinguished from other forms of optic disc swelling and linked to MS.1 A century later, we now have tools that visualize retinal damage to 5–6 μm resolution and hold strong promise as outcome measures for clinical trials.
At least 50% of patients with MS experience ON during the course of their disease, with many more experiencing subclinical damage to retinal ganglion cells.2 Up to 70% will also experience efferent dysfunction from oscillopsia to subtle smooth pursuit dysfunction and impaired gaze stabilization.2 In neuromyelitis optica spectrum disorders (NMOSDs), nearly half of patients may have a risk of developing clinical blindness in the first 5 years of disease.3 Recently, myelin oligodendrocyte glycoprotein antibody–associated disease (MOGAD) has emerged as pathophysiologically distinct from classic NMOSD with an even stronger preponderance for optic nerve involvement.
The visual system is highly amenable to quantification, with well-understood structure-function relationships, and yet it has been underutilized in clinical trials. Rigorous methods have recently emerged to quantify visual injury in neuroinflammatory diseases. Herein, the International MS Visual System Consortium (IMSVISUAL) (imsvisual.org) reviews structure-function relationship and utility in clinical trials of both afferent and efferent visual system outcome measures that have—in light of relatively low costs, high reliability, and exquisite sensitivity for pathology—the potential to transform the next generation of MS, NMOSD, and MOGAD clinical trials.
Afferent Visual System Anatomy
Retinal ganglion cells (RGCs) represent the anterior visual pathway and are affected by inflammation, demyelination, and neuroaxonal degeneration during ON or subclinical optic neuropathy (Figure 1A). RGC axons track along the inner retinal nerve fiber layer (RNFL) and converge at the optic nerve head (ONH) to form the optic nerve. RGC cell bodies are in the retinal ganglion cell layer (GCL). Subjacent to the GCL, the inner nuclear layer (INL) may also be affected by neuroimmunologic diseases.4,e1-e5 Minimal changes in outer retinal layers have been reported after ON but may be transient5 or specific to progressive forms of MS.6 Nonneuronal retinal cells have not been as well studied, but astrocyte reactivity plays a crucial role in neuroimmunologic disease, especially in NMOSD, and advancing metrics targeting these cell types are of interest.7
Figure 1. Afferent Visual System Anatomy.
(A) Phototransduction occurs in photoreceptor cells in the outer retina. These visual signals are processed and transmitted by horizontal and bipolar cells residing in the inner nuclear layer (INL). Bipolar cell axons form synapses with the dendrites of retinal ganglion cells (RGCs) in the inner plexiform retinal layer. The optic nerve is formed by the unmyelinated axons of RGCs, tracking along the inner retinal surface in the nerve fiber layer (RNFL) and converging at the optic nerve head. Subjacent to the ganglion cell layer (GCL), the INL consists of the bipolar, horizontal, and amacrine cells as well the cell bodies of astrocytic Müller cells. (B) Beyond the cribiform plate, the RGC axons of the optic nerve are myelinated and travel approximately 4 cm to the optic chiasm. The optic nerve partially decussates at the chiasm: The axons from the contralateral nasal and ipsilateral temporal hemiretinas join to form the optic tract (OT). The OT carries visual signals to the thalamic lateral geniculate nucleus (LGN). The secondary LGN neurons project to the primary visual cortex through the optic radiations (OR). From the primary visual cortex, projections go through the extrastriate cortex of the occipital lobe to the parietal lobe (the dorsal pathway for visually guided movements) and the temporal lobe (the ventral pathway for object recognition). Parts of the figure are provided by courtesy of neurodial.de (neurodial.de/2017/08/25/schematic-figure-retina-creative-commons-license/).
Beyond the cribriform plate, the optic nerve is myelinated and travels approximately 4 cm to the optic chiasm, where the axons from the contralateral nasal and ipsilateral temporal hemiretinas join to form the optic tract (OT). Lesions that involve the chiasm or OT8 are more common in aquaporin-4 (AQP4)-IgG+ NMOSD than in MS, and longitudinally extensive intraorbital optic nerve involvement is more frequent in MOGAD than in AQP4-IgG+ NMOSD.e6 The OT carries visual signals through the dorsal thalamic lateral geniculate nucleus (LGN) and secondary LGN neurons within the optic radiation (OR) to the primary visual cortex (Figure 1B). Anterograde and retrograde transsynaptic degeneration can occur across the synapse in the dorsal LGN9e7 and is of interest in the context of visual outcome measures in trials. The primary visual (calcarine/striate) cortex is organized into columns in which neurons are grouped according to their function. The occipital cortical thickness reflects this complex cytoarchitecture, and this thickness can be captured with MRI surface-based cortical reconstruction.e8 From the primary visual cortex, there are projections to the parietal (dorsal pathway for visually guided movements) and temporal lobes (ventral pathway for object recognition) (Figure 1B). The extrastriate occipital cortex also has areas with functional specificity that may be involved in neuroplasticity recovery processes after ON.e9
Afferent Visual Function Measures
An array of tools captures complementary measures of afferent visual function. These include assessments of visual acuity, formal perimetry, electrophysiology, and self-reported visual quality of life (QoL). Key to applying these measures is recognizing that the magnitudes of deficits are expected to be different in eyes with prior ON vs subclinical injury. Consistent across most clinical trials has been the application of the ON diagnostic criteria used in the optic neuritis treatment trial (ONTT).e10
High- and Low-Contrast Visual Acuity in ON and MS
High-contrast visual acuity (HCVA), black letters on a white background, is part of the visual functional system score in the Expanded Disability Status Scale (EDSS). Standardized HCVA tools include the 100% Early Treatment Diabetic Retinopathy Study (ETDRS) charts (Precision Vision, La Salle, USA) and Snellen Charts. Methods that generate continuous variables amenable to statistical models (letters correct, logMAR, and decimal vision scores) are preferable for clinical trials. A clinically meaningful change in HCVA is generally accepted as a minimum 5-letter difference.e11
A normal HCVA result, however, does not exclude MS-related optic nerve injury.10 Low-contrast vision assessments are more sensitive and include measures of contrast sensitivity (CS) and low-contrast letter acuity (LCLA). In the former, the patient is asked to read letters of constant size but decreasing contrast to determine the CS threshold. In the ONTT, CS determined by the Pelli-Robson Chart11 demonstrated greater sensitivity to detect visual injury than HCVA.12 For LCLA, the level of contrast is held constant and the letters decrease in size, similar to how HCVA is measured, but instead of 100% black on white contrast, light gray colors are used (e.g., 2.5% or 1.25% contrast). The Sloan low-contrast chartse12 have been frequently used to provide LCLA measurements, but other tools are also available. As an example, the standardized low-contrast Landolt C Broken Rings Chart (at 3 M) with direct data entry into an electronic data capture system was used for visual outcomes in the N-Momentum trial of inebilizumab (NCT02200770) in NMOSD. As the level of contrast required for letter perception is affected by letter size,e13-e14 the Sloan LCLA may be more sensitive than CS in detecting subtle losses.13 Furthermore, Sloan LCLA correlates strongly with optical coherence tomography (OCT), electrophysiologic, brain imaging, and self-reported QoL outcomes.13 Consequently, Sloan LCVA has been proposed as a primary outcome measure for visual function in ON, MS, and NMOSD and recommended as a potential (4th) component of the MS Functional Composite (MSFC) scale of MS disability.13 A seven-letter loss in LCVA has been validated as clinically meaningful.e13 LCVA is the primary outcome for an ongoing trial of nanocrystalline gold as a remyelinating agent (NCT03536559).
For assessment of neurologic acuity deficits, it is critical to address confounding refractive error. Ideally, a formal refraction and lens correction is performed; however, correction with pinhole devices has also been accepted. Assessments should be performed under standard lighting conditions throughout a trial.
Digital tools created to capture both HCVA and LCLAe15-e16 may have challenges with backlighting on devices, but these tools can provide standardization across trial sites (less issue with ambient lighting in traditional testing), allow home use, and ease data collection processes.
Visual Fields
Substantial visual deficits may be missed if outcomes focus on central acuity measures alone. In MS, NMOSD, and MOGAD, VF defects may vary, but a diffuse central scotoma is most commonly observed in acute ON.14 After recovery, patients may show an arcuate scotoma due to the predominant temporal loss of retinal nerve fibers and ganglion cells.14 VF defects are not limited to optic nerve patterns and may include those consistent with injury to the optic chiasm, optic tract, optic radiations, or occipital lobe.
VF can be assessed with different techniques. Standard static automated perimetry evaluates the central 10–30 degrees of vision and provides a qualitative depiction of field loss pattern and 2 quantitative indices: the mean deviation (MD), which measures the sensitivity deviation at each test location from the age-adjusted healthy population, and the pattern SD (PSD), which is the average sensitivity deviation from the normal slope after correction for global sensitivity differences. Kinetic perimetry can be used in patients with difficulty focusing or those with expected peripheral field loss, but quantification of results can be challenging for clinical trials.
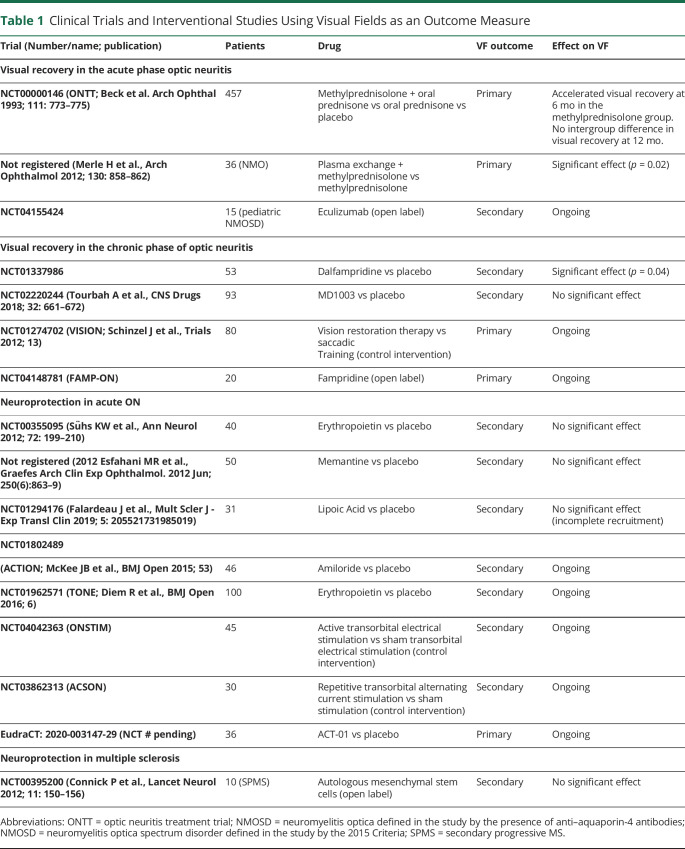
VF interpretation can be limited because of defect variability, severely impaired VA, or impaired cognition. Standardization can be reached in trials by defining light conditions and predefining cutoffs for loss of fixation frequency, false negatives, and false positives.15 In acute ON, automated perimetry has been successfully used as a primary outcome as in the ONTT12,15 and in a recent NMO trial (Table 1).16 For trials using acute ON as a model for remyelination and neuroprotection, perimetry has been used as a secondary outcome.e16-e18
Table 1.
Clinical Trials and Interventional Studies Using Visual Fields as an Outcome Measure
Electrophysiology
Across electrophysiology methods, recordings are dependent on stimulus parameters, the patient's anatomy, and the testing environment. To differentiate true signal from electrical background potentials, signal amplification and averaging techniques are used. When using electrophysiologic outcomes for clinical trials, clear and standardized protocols are essential.e19
Visual Evoked Potentials
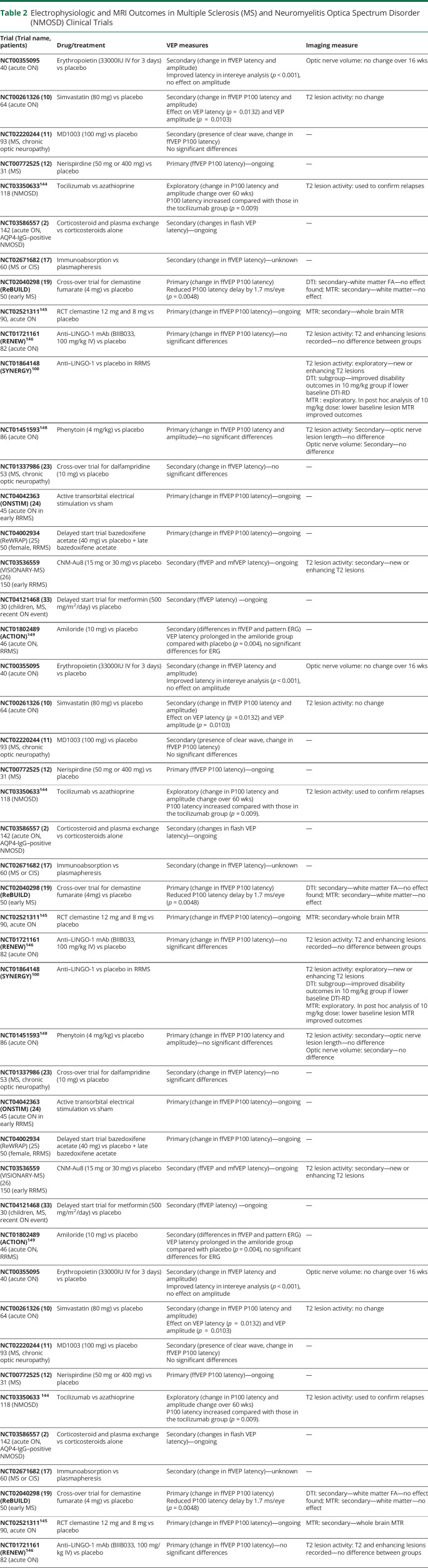
Visual Evoked Potentials (VEPs) have been successfully used as outcomes in trials for acute ON or MS-related chronic optic neuropathy (Table 2, eTable 1, links.lww.com/NXI/A675). They are electrical potentials generated in the occipital cortex (captured with occipital electrodes) in response to visual stimuli.e19 As VEPs are hidden in EEG signals, they are evaluated with averaged waveform signals from repetitive stimulation. For quality control, the International Society for Clinical Electrophysiology of Vision (ISCEV) standards should be applied. A variety of stimulation paradigms may be used. Flash VEPs (using bright-light stimuli) have been shown to be inferior to pattern-reversal VEPs (using mostly checkerboard stimuli) and are reserved for patients unable to fixate or with severe central vision loss (e.g., NMOSD-ON).e19 Pattern-reversal (or full-field) VEP analysis is based on the first major positive deflection of the signal waveform, which occurs approximately 100 ms after the stimulus (P100 latency).e19 This latency reflects conduction speed and myelin integrity. The upper P100 latency limit of normal differs according to the reference population and VEP method, and values should always be interpreted within the context of the individual, taking previous and contralateral eye measurements into account. The P100 amplitude peak is more variable than latency and should be used with caution in clinical trials, but it may help differentiate demyelinating ON from noninflammatory/ischemic optic neuropathies.e19
Table 2.
Electrophysiologic and MRI Outcomes in Multiple Sclerosis (MS) and Neuromyelitis Optica Spectrum Disorder (NMOSD) Clinical Trials
During acute demyelinating ON, the P100 latency is typically delayed (>125 ms) and the peak amplitude reduced. In cases of severe vision loss (central acuity <20/100–20/200), the patient may be unable to fixate to complete a pattern-reversal VEP, or the response may be absent.e20 For this reason, it is challenging to measure correlation between VEP and visual acuity during an acute episode of ON. With remittance of the ON, the amplitude recovers, and the latency may slowly shorten over weeks to 2 years.16 Latency improvement is most pronounced in the first 3–6 months with decreasing inflammation and presumed early remyelination. Lack of latency recovery or insidious worsening of latency delay is associated with overall disability.e21-e23 Latency insidious worsening in ON or non-ON eyes may indicate chronic global demyelination without sufficient remyelination.17,18 In recovered ON or non-ON MS eyes, correlations between LCLA and VEP latency are observable in cross-sectional analyses.e24
Given the changes of VEP latencies over time following ON, the timing of when to measure VEPs in a clinical trial requires consideration of the intervention and desired effect/outcome. For remyelinating therapies, given the lack of a widely accepted gold standard for MRI-based myelin measurements, P100 latency has been prominent as a primary or secondary outcome measure.19 Two recent trials using VEP as the primary outcome for remyelination interventions demonstrated greater P100 latency reduction by clemastine in chronic MS optic nerve injury19 and by liothyronine sodium in an acute ON model.20 Other potential remyelinating or neuroprotective agents showed negative VEP results for treatment effects, including the phase 2 trials of anti–LINGO-1 antibodies21 and phenytoin.22 Advancement in the basic science of evoked potentials and several ongoing trials with remyelinating therapies (NCT03586557, NCT03605238, NCT03062579, NCT01883661, NCT01364246, NCT02671682, NCT01337986, NCT04042363, NCT04002934, NCT03774407, and NCT04121468) will enlighten and continue to improve the application of VEP for clinical trials.
Electroretinograms
Electroretinograms (ERGs) recorded from the cornea or periorbital skin capture electrical potentials generated in the retina.e19 For flash ERGs, the first negative (consisting of rod and cone photoreceptor cell signals; ca. 14 msec) and positive (b-wave consisting of the slower bipolar cell signals; ca. 30–35 msec) waveform deflections are evaluated.e19 In contrast, a pattern ERG records the response to a pattern-reversal stimulus (e.g., alternating checkerboard); the resulting b-wave (N95; ca. 95 msec) is suggested to reflect the activation of RGCs.e19 In MS and NMOSD—especially but not exclusively after ON—N95 is prolonged, and the amplitude is diminished, indicative of retinal damage.23,e25-26 A novel ERG protocol recently identified b-wave changes in AQP4-IgG–seropositive NMOSD in line with Müller glial dysfunction, suggesting a potential relevance of ERG for differential diagnosis and trial outcome parameters in NMOSD.7
Multifocal VEP and ERG
Multifocal VEP and ERG approaches divide the visual field into sectors, which are stimulated and assessed separately.e27-28 The waveforms are comparable to those of full-field approaches, and multifocal methods are objective alternatives to VF measurements.e29 However, a high demand for patient alertness and fixation as well as issues of intersubject variability, especially for multifocal VEP (mfVEP), has been limiting. Newer stimulation and analysis algorithms may provide a better standardization and user friendliness. These mfVEP devices have been used in a subanalysis of the anti–LINGO-1 remyelination clinical trial24 and are currently used as in an ongoing study investigating the effects of nanocrystalline gold to treat remyelinating failure (NCT03536559). Multifocal ERG responses have been studied in MS and NMOSD,31 albeit without application in neuroimmunology clinical trials.
Additional Measures
Other afferent measures include the analog and digital flicker tests, object from motion (OFM), and critical flicker frequency (CFF). Digital administration may expand the accessibility of new visual outcomes for trials. As an example, the digital Aulhorn flicker test showed superior diagnostic sensitivity (sensitivity 93% and specificity 96%) compared with the Aulhorn analog flicker test (sensitivity 76% and specificity 100%).e32 The digital CFF test associates with disability in patients with MS.e33 OFM generates a hidden object that is perceived through motion detection and can be used to assess de/remyelination.e34 These tests, while not yet in trials, may hold promise for use in future designs.
Vision QOL
Although patients with MS rate visual function as a top concern,25 vision-related patient-reported outcomes have been widely neglected in pivotal trials of MS immunotherapy.e35 Visual QoL in both MS and NMOSD correlates with LCLA and structural measures of retinal damage.26-28 The commonly used 51-item National Eye Institute Visual Function Questionnaire (NEI-VFQ) comprises 12 individual subscales for general health, general vision, ocular pain, near activities, distance activities, driving, color vision, peripheral vision and vision-specific social functioning, mental health, role difficulties, and dependencies. A final composite score is generated by averaging all subscale scores except the general health item. An additional version with 39 and 25 items and a neuro-ophthalmic supplement have since been established and have been applied to measure vision-related QoL in MS.29,30 Use of the NEI-VFQ with the neuro-ophthalmic supplement would be recommended for neuroimmunology trials.
Afferent Visual System Structural Measures
Optical Coherence Tomography (OCT) Peripapillary and Macular Measurements
OCT uses light waves passing through the pupil, vitreous, and retinal layers and then reflecting off the pigmented retinal epithelium to reconstruct images of the retina and assess tissue integrity. Over the past 20 years, studies describing OCT outcomes in MS, NMOSD, and MOGAD have exponentially increased.31 Initial work used time-domain OCT, whereas recent studies have leveraged the faster acquisition speeds, higher-resolution images (axial resolution 4–6 µm), and improved reproducibility of spectral domain OCT.e36-e37 Segmentation of the images, typically performed using automated algorithms, allows the quantitative assessment of discrete retinal neuronal and axonal layers (Figure 2). With appropriate quality control in acquisition,32 these quantitative measures demonstrate excellent test-retest reliability, a critical feature for clinical trial outcomes.33
Figure 2. Optical Coherence Tomography Peripapillary and Macular Measurements.
Upper left: Fundus image with superimposed macular GCIPL thickness map. Bottom: Horizontal macular OCT B-scan traversing the fovea, corresponding to the red horizontal line shown in the fundus photograph (upper left). The scan has been automatically segmented (boundaries between retinal layers are outlined in red). Upper right: Peripapillary RNFL ring scan; the shown OCT B-scan shown corresponds to the purple peripapillary ring shown superimposed on the fundus image. RNFL = retinal nerve fiber layer; GCIPL = ganglion cell + inner plexiform layer; INL = inner nuclear layer; OPL = outer plexiform layer; ONL = outer nuclear layer.
MS, NMOSD, and MOGAD observational OCT studies have largely focused on the macular ganglion cell + inner plexiform layer (GCIPL) and peripapillary RNFL (pRNFL) thickness, representing the integrity of RGC cell bodies and axons, respectively. Following acute ON, there is rapid thinning of the GCIPL, often within the first month of onset, and this process is largely completed by 3 months.34,35 The pRNFL frequently exhibits increased thickness during acute ON due to swelling, which confounds the baseline measurement and leads to a delayed time course of detecting atrophy of the pRNFL compared with the GCIPL.34,35 It is best to measure pRNFL 6 months after onset for assessment of axonal loss from an acute ON event.34,35
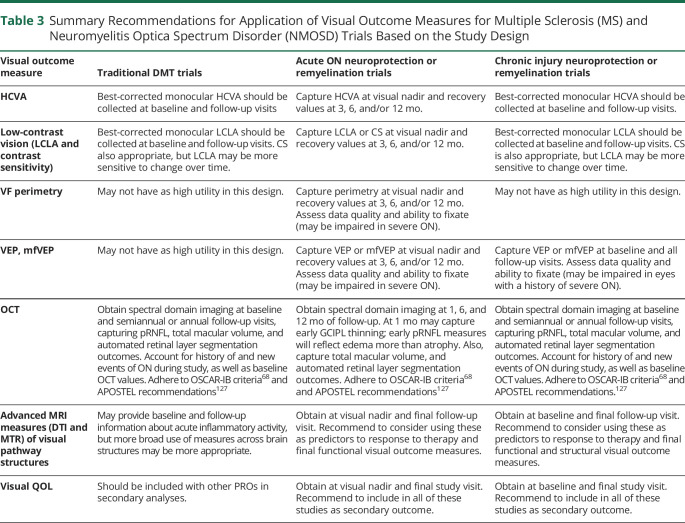
Selecting the specific OCT outcome for a trial depends on the disease state and time course of interest (Table 3). Important considerations for incorporating OCT measures in trials of putative neuroprotective agents in acute ON include the following: 1) GCIPL thickness is superior to pRNFL thickness at early time points, given the lack of swelling at baseline, 2) GCIPL thinning occurs rapidly during the first month after ON, and participants should be enrolled shortly after symptom onset; very early intervention (within 2–4 weeks) with therapeutics may be required to change the outcome,36 3) a 6-month trial duration could be sufficient to detect a difference in GCIPL or pRNFL thinning between treatment groups (though should consider if investigative medication could alter typical time course of retinal layer thinning).
Table 3.
Summary Recommendations for Application of Visual Outcome Measures for Multiple Sclerosis (MS) and Neuromyelitis Optica Spectrum Disorder (NMOSD) Trials Based on the Study Design
Consistent with postmortem findings,e2 pRNFL and GCIPL thicknesses are lower than in the healthy population even in those without a history of clinical ON, but thinning is more severe in ON eyes.37 The etiology of insidious optic nerve injury in MS is not fully understood but may have contributions from subclinical optic nerve inflammation or transsynaptic retrograde degeneration from posterior visual pathway injury. Compared with MS ON eyes, eyes with AQP4-IgG and MOGAD-associated ON have greater pRNFL and GCIPL thinning, which appears to be commensurate with greater losses in HCVA and LCLA in AQP4-IgG, but not MOG-IgG, associated ON.38 While not as prominent as in MS, there is some evidence to suggest that subclinical retinal neuroaxonal loss may occur in NMOSD, possibly caused by an attack-independent astrocytopathy.e4, e38-e41 Consistent with this, attack-independent tissue loss and associated functional changes were found in the parafoveal region, which is rich in astrocytes and AQP4-expressing Müller cells.7,e40-e42
Accelerated rates of inner retinal atrophy in MS eyes are associated with inflammatory disease activity, global disability progression, and increased brain atrophy.6,39,e43-e44 Disease-modifying therapies (DMTs) may differentially affect pRNFL and GCIPL thinning in MS, mainly in the relapsing-remitting stage.40 Important to trial design, there are floor effects in eyes that have already had significant retinal injury. This is in part why one might consider adjusting for baseline OCT values, even in randomized trials. Also relevant for study design and inclusion criteria, the proportion of pRNFL and GCIPL thinning attributable to MS decreases with older age. After age 65 years, >80% of the rate of thinning in these layers is attributable to normal aging.6 pRNFL and GCIPL thinning is faster earlier in the RRMS disease course (when there is more tissue to lose), whereas progressive disease subtype (which is associated with older age) is independently associated with faster inner retinal layer thinning.6 Normative values of retinal layer thicknesses differ by race, with African American patients with MS exhibiting faster rates of retinal atrophy.41,e45 Differential effects of sex on levels of retinal injury exist, with men and boys demonstrating worse atrophy after ON.42,43 These data highlight the importance of accounting for patient demographics on rates of pRNFL/GCIPL thinning when designing trials.
In addition to pRNFL and GCIPL, deeper retinal neuronal layers have been proposed as biomarkers of chronic neurodegeneration, with accelerated INL and ONL atrophy reported in progressive MS compared with both relapsing-remitting MS and healthy controls.6 Notably, the INL exhibits a complex spectrum of abnormalities in MS including microcystoid macular pathology, increased thickness in association with inflammatory disease activity, reduction in thickness following DMT initiation, and atrophy in late, progressive disease.e2-e4
OCT has also been used to support the identification of clinical and subclinical ON by identifying intereye differences in the pRNFL and GCIPL layers.44,e46-e47 OCT has also been used for participant selection criteria to identify those who may be more likely to benefit from remyelination therapies.19
A special consideration for MOGAD trials is the relative preserved central acuity despite moderate to severe retinal injury. Compared with NMOSD, for a given level of pRNFL thinning, there are better HCVA outcomes in MOGAD.38 This may be due to less involvement of the papillomacular bundle in MOGAD, but definitive studies are needed.
OCT outcomes have been studied in the pediatric population. As in the adult MS population, decreased RNFL and GCIPL are noted early in the disease course43,45 with evidence for progressive RNFL and GCIPL loss through time. Thus, despite having better visual function recovery, children have similar burden of retinal thinning.43,45 As in adult patients, distinct OCT patterns can distinguish pediatric neuroinflammatory disorders such as MOG-IgG– and AQP4-IgG–related neuroinflammation from MS.e48
MRI Visual System Structural Measures
Complementary to OCT, MRI outcomes evaluate anterior and posterior afferent visual pathway injury. Methodological advances have overcome the challenges of optic nerve imaging posed by its small size, mobility, and location adjacent to nasal cavities, orbital fat, and CSF.e49 Particularly in MOGAD, optic nerve MRI can speed diagnosis—showing characteristic features including anterior longitudinal extensive optic nerve lesions and perineural or periorbital gadolinium enhancement.e50-e52
Optic nerve cross-sectional area can be reliably assessed using a short-echo fast fluid-attenuated inversion recovery sequence with fat and CSF suppression.e53 In a 12-month acute ON longitudinal study of this method, there was an 11.7% greater decline in affected vs unaffected optic nerve volumes.46 Optic nerve atrophy correlated with RNFL thinning47 after ON, and with both HCVA and P100 latency in chronic optic neuropathye49, supporting potential use of this approach in trials (Table 1).
Diffusion tensor imaging (DTI) captures three-dimensional magnitude and direction of water diffusion. After acute ON, diffusion parallel to axons (axial diffusivity, AD) is low, whereas diffusion perpendicular to the axon, or radial diffusivity (RD), remains in a normal range.48 In a 12-month longitudinal study of 37 patients with acute ON,49 reduced AD at baseline correlated with pRNFL thinning and mfVEP amplitude loss at 6 and 12 months. Importantly, early reductions in AD also predict VA recovery at 6 months,49,e54 suggesting that acute ON therapies that normalize optic nerve AD could also promote axon survival and improve visual outcomes. Baseline measurements of optic nerve DTI (Table 2) may also help select patients who are most likely to benefit from intervention.50 DTI can be obtained on most commercial scanners but, unfortunately, adds significant acquisition time and cost. Advanced image processing and analytical requirements are additional barriers to widespread implementation, but we anticipate reduction of these barriers with improved, standardized software.
Application of optic nerve DTI in acute NMOSD-ON has not been as well studied. In 1 retrospective study of 57 patients with NMOSD-ON,e55 a radiomics model using whole-brain DTI measures correlated strongly with visual outcomes after IV methylprednisolone, suggesting its potential as a predictor of response to acute therapy.
The magnetization transfer ratio (MTR) indicates the balance between protons bound to molecules (protein and lipids) vs free protons. Postmortem studies have confirmed a strong association between a reduced MTR and demyelination,e56 whereas others have shown a similar correlation between MTR and axonal density or both.e57 It is accepted that a higher MTR indicates more bound protons, as seen in normal, myelinated tissue. MTR decreases in acute ONe58 with an approximate 8-month nadir46 and correlates with P100 latency, HCVA,46 mfVEP amplitude, and RNFL thinning.e59,e60 MTR in the optic nerve, whole brain, or T2 lesions have been used in clinical trials (Table 2, Table e1, links.lww.com/NXI/A675). Timing and location of MTR measurement in relation to the acute injury is critical for interpretation of results. In the anti–LINGO-1 RRMS trial, baseline lesional MTR was associated with disability outcomes in the 10 mg/kg group.50
New Structural Biomarkers
OCT advances may offer novel biomarkers for future trials.e61-e62 New machine learning retinal segmentation algorithms decrease rater dependence, improve reliability, and allow automatic quantification of disease-specific changes such as microcystic macular edema.e63 Novel 3D methods resample standard OCT images to depict retinal shape changes,e40,e64-e65 which may be especially useful to standardize assessment of NMOSD foveal morphology changes.e40,e42,e66
Another new addition, OCT angiography (OCTA), uses the movement of erythrocytes to create maps of the superficial and deep retinal vascular plexuses and to calculate retinal vascular flow rates. In MS and NMOSD, vessel reduction in OCTA images is correlated with neuroaxonal damage, and in MS, also with general disability (EDSS).51,e67-e68 Relative blood flow velocity is decreased around the optic nerve head and fovea in patients with MS and AQP4-IgG–seropositive ON.52,53
Finally, new MRI sequences such as double-inversion recovery sequences can help detect early optic nerve injury and improve timely trial inclusion.e69 Atlas-based automated segmentation and volumetry of the LGN may facilitate understanding of anterograde and retrograde neurodegeneration and visual function.
Recommendations for Implementation of Afferent Assessments in Clinical Trials
With the increasing use of afferent visual assessments, it is important to understand the best methods in a specific study design and the main challenges and pitfalls in applying them (Tables 3 and 4).
Table 4.
Systematic Approach to Common Pitfalls in Visual System Assessments for Clinical Trials and Observational Studies
Study Design
Balancing the needs of generalizability vs risks of heterogeneity impairing detection of treatment effects, clinical trials should clearly define the disease state measured (e.g., acute optic neuritis and chronic optic neuropathy), inclusion and exclusion criteria, and measurement protocols. Depending on the intervention's mechanism of action, different time points or assessments should be considered; these decisions can be critical to the success of the trial.
It is important to take into account differential pathophysiologic features of MS, NMOSD, and MOGAD as well as to consider aging effects and potential basement effects (e.g., testing putative neuroprotective therapies in eyes with severe optic neuropathy), and disease- or treatment-related retinal changes such as microcystoid and/or fingolimod-associated macular edema.e5,e70
Other important considerations are excluding patients with confounding primary ophthalmologic pathologies (e.g., severe myopia, glaucoma, central serous retinopathy, or diabetic retinopathy) and identifying the up to 16% of patients with MS who may have unrelated morphologic macular abnormalities such as drusen or epiretinal membranes, which can induce OCT segmentation errors or be associated with nonneurologic causes of visual dysfunction.e71
In ON, conduction block and inflammatory edema may limit the use of standard VEP and pRNFL OCT measurements at early time points. For chronic optic neuropathy, pathologic sensitivity of some measures may change in the setting of gliosise72 or visual repair (e.g., functional neuroplasticity).e9 Importantly, regulatory authorities are likely to always prefer a clinical outcome for phase III RCTs, and trial duration of up to 12 months may be needed to fully capture the effects of an intervention on visual recovery.12
Advanced imaging techniques may provide the means to better stratify and select trial participants most likely to benefit from early intervention with a potential neuroprotective therapy. Optic nerve DTI measurements such as AD, especially if assessed outside the anatomical segment with acute inflammatory change, could more directly assess the degree of axonal involvement. Similarly, MTR could also potentially be used as an early stratification tool when allocating patients to different treatment groups.e73
Data Acquisition
A strong study protocol defines the specific device(s), measurement parameters, required environment (e.g., illumination and noise level), and patient needs (e.g., refractive correction). Frequency of assessments needs to be tailored to the clinical model (acute or chronic ON), temporal flux in visual and paraclinical measures, and safety requirements. For assessments requiring focus and alertness such as electrophysiologic or VF perimetry, patients with fatigue or cognitive dysfunction may require accommodations.54,e74 Efferent dysfunction can negatively affect fixation and acquisition of afferent measures. Severe acute ON can impair ability to fixate, resulting in poor-quality electrophysiology and OCT studies. Awareness of these pitfalls can help troubleshoot ways to acquire the best data (e.g., fixate with the unaffected or less affected eye during OCT acquisition).
Data Analysis
Ideally, multicenter trials should use identical devices and protocols for data acquisition. When this is not feasible, the statistical analysis plan should account for device and protocol effects. Efforts to harmonize data from different OCT devices are under way, and initial results are promising. Multisite success has been demonstrated for automated retinal segmentation software.55 In nonrandomized studies, multivariable modeling to account for confounding variables (sex, age, ethnicity, history of ON, and baseline disability measures) is important. Even in randomized studies, tracking the ON status of each eye and considering adjustments for baseline values of measurements are important as the meaning and magnitude of change in measures may notably differ based on these variables, particularly for OCT studies. In analyses for which each participant contributes data from both eyes, intereye correlations must be adjusted for using mixed-effects models or generalized estimating equations. When possible, both eyes of a patient should be included, but for correlations with MRI outcomes, either the best or worst eye in terms of the outcome measure could be used. Averaging values between eyes may result in losing information about injury as the worse eye may be more informative about disease injury than an averaged value. Eyes should be tested individually for HCVA and LCLA. If binocular measures are included, the impact of the neuroimmunologic disease on binocular summation/inhibition should be considered. In adult MS, binocular summation may be impairede75 and could be an outcome measure to consider if appropriate for the research question.
Quality Control and Reporting of OCT Results
Given the complexity of OCT technology, as well as its susceptibility to artifacts or confounding pathologies, complete reporting of methodology and quality control are of paramount importance. Investigators are recommended to adhere to the OSCAR-IB criteria32 and APOSTEL recommendations56 for quality control and reporting of OCT studies, respectively.
Efferent Visual System and Oculometrics
Most people with MS experience efferent visual dysfunction from disorders of fixation to intereye misalignment. Efferent oculometric assessments may reveal deficits not readily appreciated at bedside and associate with overall disability in MS.57 An eye-tracking paradigm was able to detect subtle cerebellar dysfunction in participants without ataxia.58 Even in the very young, with pediatric onset MS and no discernible disability on examination, saccadic latencies can distinguish eyes of patients with MS from those of healthy controls.59 For rapidly quantifying disease burden largely driven by the brainstem and cerebellum (key contributors to overall disability scores), eye-tracking approaches offer objective, reliable means to collect these data.
Despite the great promise of efferent oculometric techniques in quantifying neuroimmunologic disease burden, these approaches have not percolated significantly into clinical trials. One interventional neuromodulation study lists video nystagmography as an exploratory outcome of treatment efficacy (NCT02252666). A primary reason may be the variety of eye-tracking devices and software and a lack of widely accepted protocol parameters for data quality. However, these are surmountable obstacles, and similar consensus and quality approaches could be applied as has been done for the afferent measurements highlighted here.
Advantages of Assessments in the Visual System
Low Cost and Correlations With Other Outcome Measures—Atrophy, Cognition, and Employment Status
RNFL and GCIPL thinning on OCT are low-cost measures that have shown considerable cross-sectional and longitudinal associations with other outcome measures of tissue damage in MS, including brain volume loss,39,e76-e77 in particular when ON eyes are removed from analyses.e78-e79 These associations likely emerge from a common pathophysiologic denominator and suggest that in some settings, retinal measures may be used as surrogates of MRI measures. Anterograde or retrograde transsynaptic degeneration involving retrogeniculate parts of the visual pathway may influence these associations.e80-e81 Retinal damage may also relate to functional connectivity changes in the visual system and other networks in ON, MS, and NMOSD.e82-e84
RNFL and GCIPL thinning have been associated with worse cognitive performance,e85-e86 suggesting a shared underlying pathobiology of diffuse CNS tissue destruction. However, reduced visual function might affect cognitive test performance, and cognitive dysfunction may alter the capability to execute more demanding visual tests such as LCLA testing.e74 Finally, higher serum neurofilament light chain (NfL) has been associated with lower RNFL and GCIPL thickness values in the non-ON eyes of participants with MS.e87
Precision and in Vivo Human Microstructural/Sensitive Functional Assessments Unparalleled in the Other Systems Affected by MS
The availability of sensitive measures has enabled rigorous measurement of structural and functional changes in the injured visual system to a greater degree than is possible in other regions of the CNS.e88 Structural changes on OCT are strongly correlated with changes in LCLA and visual QOL. One can estimate the functional consequence of a 5–10-μm change in RNFL thickness. Such precision has not been clearly recorded for the corticospinal tracts, for example.
IMSVISUAL View of the Landscape and Proposed Role of Visual System for Trials of Agents in the Pipeline
IMSVISUAL aims to improve care, research, and education in MS and other neuroinflammatory disorders by advancing our understanding of the visual system and by providing a framework and international standards for applying vision tools in clinical trials. These methods are sensitive, reliable, and cost-effective with strong structure-function correlations. Different tools provide complementary information and have ideal time points for use along the temporal course of visual injury (Table 4). Best practices and even published standard criteria exist to guide rigorous study design in visual outcome applications. For all paradigms of trials in MS and NMOSD (and future trials in MOGAD), from standard DMT trials or those of neuroprotection and remyelination, and even trials of comparative efficacy, applicationse90-e94 of visual outcome tools offer cost-effective mechanisms to capture widespread and focal injury across disease subtypes and may lead to more rapid development of new therapeutics for these disabling diseases.
Glossary
- AQP4
aquaporin-4
- CS
contrast sensitivity
- EDSS
Expanded Disability Status Scale
- EDTRS
Early Treatment Diabetic Retinopathy Study
- ERGs
Electroretinograms
- GCIPL
ganglion cell + inner plexiform layer
- GCL
ganglion cell layer
- HCVA
High-contrast visual acuity
- IMSVISUAL
International MS Visual System Consortium
- INL
inner nuclear layer
- ISCEV
International Society for Clinical Electrophysiology of Vision
- LCLA
low-contrast letter acuity
- LGN
lateral geniculate nucleus
- MD
mean deviation
- MOGAD
myelin oligodendrocyte glycoprotein antibody–associated disease
- MSFC
MS Functional Composite
- NEI-VFQ
National Eye Institute Visual Function Questionnaire
- NMOSDs
neuromyelitis optica spectrum disorders
- OCT
optical coherence tomography
- ON
optic neuritis
- ONH
optic nerve head
- ONL
outer nuclear layer
- OPL
outer plexiform layer
- ONTT
optic neuritis treatment trial
- OR
optic radiation
- OT
optic tract
- QoL
quality of life
- RGC
Retinal ganglion cells
- RNFL
retinal nerve fiber layer
- VEPs
Visual Evoked Potentials
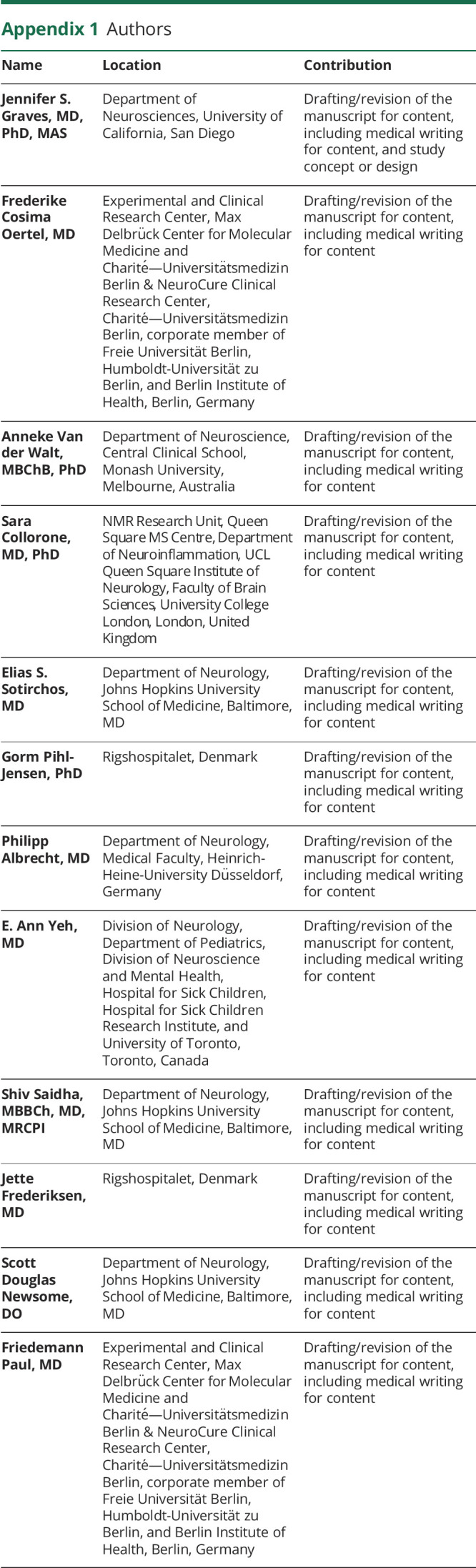
Appendix 1. Authors
Appendix 2. Coinvestigators
Contributor Information
Frederike Cosima Oertel, Email: frederike-cosima.oertel@charite.de.
Anneke Van der Walt, Email: anneke.vanderwalt@monash.edu.
Sara Collorone, Email: s.collorone@ucl.ac.uk.
Elias S. Sotirchos, Email: ess@jhmi.edu.
Gorm Pihl-Jensen, Email: gormpihl@gmail.com.
Philipp Albrecht, Email: phil.albrecht@gmail.com.
E. Ann Yeh, Email: ann.yeh@sickkids.ca.
Shiv Saidha, Email: ssaidha2@jhmi.edu.
Jette Frederiksen, Email: jetfre01@regionh.dk.
Scott Douglas Newsome, Email: snewsom2@jhmi.edu.
Friedemann Paul, Email: friedemann.paul@charite.de.
Study Funding
The authors report no targeted funding.
Disclosure
Unrelated to the current work, Dr. Graves over the past year has grant/contract research support from the National MS Society, Biogen, and Octave Biosciences. She serves on a steering committee for a trial supported by Novartis. She has received honoraria for a nonpromotional, educational activity for Sanofi-Genzyme. She has received speaker fees from Alexion and BMS and served on an advisory board for Genentech. Unrelated to the current work, Dr. Sotirchos receives research support from the NIH and National MS Society. He has served on scientific advisory boards for Alexion, Viela Bio, and Genentech and has received speaker honoraria from Viela Bio and Biogen. Unrelated to the current work, Dr. Oertel receives research support from the American Academy of Neurology and National MS Society. Unrelated to the current work, Dr. Van der Walt has received research funding and served on advisory boards to Novartis Australia, Biogen, Roche, Merck, and NervGen. She received speakers' honoraria from Novartis, Biogen Roche, and Merk. Her research is funded by the National Health and Medical Research Council of Australia. Unrelated to the current work, Dr. Collorone was supported by the Rosetrees Trust (MS632), and she was awarded a MAGNIMS-ECTRIMS fellowship in 2016. Unrelated to the current work, Dr. Albrecht reports grants, personal fees, and nonfinancial support from Allergan, Biogen, Celgene, Ipsen, Merck, Merz, Novartis, and Roche and speaking honoraria and nonfinancial support from Janssen- Cilag, Teva, and Bayer HealthCare. Unrelated to the current work, Dr. Saidha has received consulting fees from Medical Logix for the development of CME programs in neurology and has served on scientific advisory boards for Biogen, Genzyme, Genentech Corporation, EMD Serono, and Celgene. He is the PI of investigator-initiated studies funded by Genentech Corporation and Biogen Idec, received support from the Race to Erase MS foundation, and was the site investigator of a trial sponsored by MedDay Pharmaceuticals. He has received equity compensation for consulting from JuneBrain LLC, a retinal imaging device developer. Unrelated to the current work, Dr. Newsome has received consultant fees for scientific advisory boards from Biogen, Genentech, Bristol Myers Squibb, EMD Serono, Novartis, and Greenwich Biosciences. He is an advisor for Autobahn Therapeutics and BioIncept, a clinical adjudication committee member for a MedDay Pharmaceuticals clinical trial. He has received research funding (paid directly to institution) from Biogen, Novartis, Genentech, National MS Society, Department of Defense, and Patient Centered Outcomes Institute. Unrelated to the current work, Dr. Yeh has received research funding from NMSS,CMSC, CIHR,NIH,OIRM, SCN, CBMHChase an Idea, SickKids Foundation, Rare Diseases Foundation, MS Scientific Foundation (Canada), McLaughlin Centre, and Mario Battaglia Foundation; investigator-initiated research funding from Biogen; scientific advisory: Biogen, Hoffman- LaRoche, and Viela Bio; and speaker honoraria: Saudi Epilepsy Society, NYU, MS-ATL, ACRS, and PRIME.funding. Go to Neurology.org/NN for full disclosures.
References
- 1.Volpe NJ. Optic neuritis: historical aspects. J Neuroophthalmol. 2001;21(4):302-309. [DOI] [PubMed] [Google Scholar]
- 2.Graves J, Balcer LJ. Eye disorders in patients with multiple sclerosis: natural history and management. Clin Ophthalmol. 2010;4:1409-1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wingerchuk DM, Hogancamp WF, O'Brien PC, Weinshenker BG. The clinical course of neuromyelitis optica (Devic's syndrome). Neurology. 1999;53(5):1107-1114. [DOI] [PubMed] [Google Scholar]
- 4.Balk LJ, Coric D, Knier B, et al. Retinal inner nuclear layer volume reflects inflammatory disease activity in multiple sclerosis; a longitudinal OCT study. Mult Scler J Exp Transl Clin. 2019;5(3):2055217319871582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Al-Louzi OA, Bhargava P, Newsome SD, et al. Outer retinal changes following acute optic neuritis. Mult Scler. 2016;22(3):362-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sotirchos ES, Gonzalez Caldito N, Filippatou A, et al. Progressive multiple sclerosis is associated with faster and specific retinal layer atrophy. Ann Neurol. 2020;87(6):885-896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.You Y, Zhu L, Zhang T, et al. Evidence of müller glial dysfunction in patients with aquaporin-4 immunoglobulin G-positive neuromyelitis optica spectrum disorder. Ophthalmology. 2019;126(6):801-810. [DOI] [PubMed] [Google Scholar]
- 8.Kim HJ, Paul F, Lana-Peixoto MA, et al. MRI characteristics of neuromyelitis optica spectrum disorder: an international update. Neurology. 2015;84(11):1165-1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tur C, Goodkin O, Altmann DR, et al. Longitudinal evidence for anterograde trans-synaptic degeneration after optic neuritis. Brain. 2016;139(Pt 3):816-828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frederiksen JL, Larsson HB, Ottovay E, Stigsby B, Olesen J. Acute optic neuritis with normal visual acuity. Comparison of symptoms and signs with psychophysiological, electrophysiological and magnetic resonance imaging data. Acta Ophthalmol (Copenh). 1991;69(3):357-366. [DOI] [PubMed] [Google Scholar]
- 11.Pelli DG, Robson JG, Wilkins AJ. The design of a new letter chart for measuring contrast sensitivity. Clin Vis Sci. 1988;2. [Google Scholar]
- 12.Beck RW, Cleary PA. Optic neuritis treatment trial. One-year follow-up results. Arch Ophthalmol. 1993;111(6):773-775. [DOI] [PubMed] [Google Scholar]
- 13.Balcer LJ, Baier ML, Cohen JA, et al. Contrast letter acuity as a visual component for the multiple sclerosis functional composite. Neurology. 2003;61(10):1367-1373. [DOI] [PubMed] [Google Scholar]
- 14.Keltner JL, Johnson CA, Cello KE, Dontchev M, Gal RL, Beck RW. Visual field profile of optic neuritis: a final follow-up report from the optic neuritis treatment trial from baseline through 15 years. Arch Ophthalmol. 2010;128(3):330-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keltner JL, Johnson CA, Beck RW, Cleary PA, Spurr JO. Quality control functions of the visual field reading center (VFRC) for the optic neuritis treatment trial (ONTT). Control Clin Trials. 1993;14(2):143-159. [DOI] [PubMed] [Google Scholar]
- 16.Brusa A, Jones SJ, Plant GT. Long-term remyelination after optic neuritis: a 2-year visual evoked potential and psychophysical serial study. Brain. 2001;124(Pt 3):468-479. [DOI] [PubMed] [Google Scholar]
- 17.Jones SJ, Brusa A. Neurophysiological evidence for long-term repair of MS lesions: implications for axon protection. J Neurol Sci. 2003;206(2):193-198. [DOI] [PubMed] [Google Scholar]
- 18.Ringelstein M, Harmel J, Zimmermann H, et al. Longitudinal optic neuritis-unrelated visual evoked potential changes in NMO spectrum disorders. Neurology. 2020;94(4):e407-e418. [DOI] [PubMed] [Google Scholar]
- 19.Green AJ, Gelfand JM, Cree BA, et al. Clemastine fumarate as a remyelinating therapy for multiple sclerosis (ReBUILD): a randomised, controlled, double-blind, crossover trial. Lancet. 2017;390(10111):2481-2489. [DOI] [PubMed] [Google Scholar]
- 20.Wooliscroft L, Altowaijri G, Hildebrand A, et al. Phase I randomized trial of iodothyronine for remyelination in multiple sclerosis: a dose-ranging study with assessment of reliability of visual outcomes. Mult Scler Relat Disord. 2020;41:102015. [DOI] [PubMed] [Google Scholar]
- 21.Cadavid D, Balcer L, Galetta S, et al. Safety and efficacy of ipilimumab in acute optic neuritis (RENEW): a randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2017;16(3):189-199. [DOI] [PubMed] [Google Scholar]
- 22.Raftopoulos R, Hickman SJ, Toosy A, et al. Phenytoin for neuroprotection in patients with acute optic neuritis: a randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2016;15(3):259-269. [DOI] [PubMed] [Google Scholar]
- 23.Coupland SG, Kirkham TH. Flash electroretinogram abnormalities in patients with clinically definite multiple sclerosis. Can J Neurol Sci. 1982;9(3):325-330. [DOI] [PubMed] [Google Scholar]
- 24.Klistorner A, Chai Y, Leocani L, et al. Assessment of opicinumab in acute optic neuritis using multifocal visual evoked potential. CNS Drugs. 2018;32(12):1159-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heesen C, Haase R, Melzig S, et al. Perceptions on the value of bodily functions in multiple sclerosis. Acta Neurol Scand. 2018;137(3):356-362. [DOI] [PubMed] [Google Scholar]
- 26.Schinzel J, Zimmermann H, Paul F, et al. Relations of low contrast visual acuity, quality of life and multiple sclerosis functional composite: a cross-sectional analysis. BMC Neurol. 2014;14:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walter SD, Ishikawa H, Galetta KM, et al. Ganglion cell loss in relation to visual disability in multiple sclerosis. Ophthalmology. 2012;119(6):1250-1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schmidt F, Zimmermann H, Mikolajczak J, et al. Severe structural and functional visual system damage leads to profound loss of vision-related quality of life in patients with neuromyelitis optica spectrum disorders. Mult Scler Relat Disord. 2017;11:45-50. [DOI] [PubMed] [Google Scholar]
- 29.Mowry EM, Loguidice MJ, Daniels AB, et al. Vision related quality of life in multiple sclerosis: correlation with new measures of low and high contrast letter acuity. J Neurol Neurosurg Psychiatry. 2009;80(7):767-772. [DOI] [PubMed] [Google Scholar]
- 30.Ma SL, Shea JA, Galetta SL, et al. Self-reported visual dysfunction in multiple sclerosis: new data from the VFQ-25 and development of an MS-specific vision questionnaire. Am J Ophthalmol. 2002;133(5):686-692. [DOI] [PubMed] [Google Scholar]
- 31.Graves JS. Optical coherence tomography in multiple sclerosis. Semin Neurol. 2019;39(6):711-717. [DOI] [PubMed] [Google Scholar]
- 32.Schippling S, Balk LJ, Costello F, et al. Quality control for retinal OCT in multiple sclerosis: validation of the OSCAR-IB criteria. Mult Scler. 2015;21(2):163-170. [DOI] [PubMed] [Google Scholar]
- 33.Syc SB, Warner CV, Hiremath GS, et al. Reproducibility of high-resolution optical coherence tomography in multiple sclerosis. Mult Scler. 2010;16(7):829-839. [DOI] [PubMed] [Google Scholar]
- 34.Syc SB, Saidha S, Newsome SD, et al. Optical coherence tomography segmentation reveals ganglion cell layer pathology after optic neuritis. Brain. 2012;135(Pt 2):521-533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kupersmith MJ, Garvin MK, Wang JK, Durbin M, Kardon R. Retinal ganglion cell layer thinning within one month of presentation for optic neuritis. Mult Scler. 2016;22(5):641-648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stiebel-Kalish H, Hellmann MA, Mimouni M, et al. Does time equal vision in the acute treatment of a cohort of AQP4 and MOG optic neuritis?. Neurol Neuroimmunol Neuroinflamm. 2019;6:e572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Petzold A, Balcer LJ, Calabresi PA, et al. Retinal layer segmentation in multiple sclerosis: a systematic review and meta-analysis. Lancet Neurol. 2017;16(10):797-812. [DOI] [PubMed] [Google Scholar]
- 38.Sotirchos ES, Filippatou A, Fitzgerald KC, et al. Aquaporin-4 IgG seropositivity is associated with worse visual outcomes after optic neuritis than MOG-IgG seropositivity and multiple sclerosis, independent of macular ganglion cell layer thinning. Mult Scler. 2020;26(11):1360-1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saidha S, Al-Louzi O, Ratchford JN, et al. Optical coherence tomography reflects brain atrophy in multiple sclerosis: a four-year study. Ann Neurol. 2015;78(5):801-813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Button J, Al-Louzi O, Lang A, et al. Disease-modifying therapies modulate retinal atrophy in multiple sclerosis: a retrospective study. Neurology 2017;88(6):525-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kimbrough DJ, Sotirchos ES, Wilson JA, et al. Retinal damage and vision loss in African American multiple sclerosis patients. Ann Neurol. 2015;77(2):228-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Costello F, Hodge W, Pan YI, et al. Sex-specific differences in retinal nerve fiber layer thinning after acute optic neuritis. Neurology. 2012;79(18):1866-1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Graves JS, Chohan H, Cedars B, et al. Sex differences and subclinical retinal injury in pediatric-onset MS. Mult Scler. 2017;23(3):447-455. [DOI] [PubMed] [Google Scholar]
- 44.Lambe J, Saidha S, Bermel RA. Optical coherence tomography and multiple sclerosis: update on clinical application and role in clinical trials. Mult Scler. 2020;26(6):624-639. [DOI] [PubMed] [Google Scholar]
- 45.Wilbur C, Reginald YA, Longoni G, et al. Early neuroaxonal injury is seen in the acute phase of pediatric optic neuritis. Mult Scler Relat Disord. 2019;36:101387. [DOI] [PubMed] [Google Scholar]
- 46.Hickman SJ, Toosy AT, Jones SJ, et al. A serial MRI study following optic nerve mean area in acute optic neuritis. Brain. 2004;127(Pt 11):2498-2505. [DOI] [PubMed] [Google Scholar]
- 47.Trip SA, Schlottmann PG, Jones SJ, et al. Optic nerve atrophy and retinal nerve fibre layer thinning following optic neuritis: evidence that axonal loss is a substrate of MRI-detected atrophy. Neuroimage. 2006;31(1):286-293. [DOI] [PubMed] [Google Scholar]
- 48.Naismith RT, Xu J, Tutlam NT, et al. Disability in optic neuritis correlates with diffusion tensor-derived directional diffusivities. Neurology. 2009;72(7):589-594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van der Walt A, Kolbe SC, Wang YE, et al. Optic nerve diffusion tensor imaging after acute optic neuritis predicts axonal and visual outcomes. PLoS One. 2013;8:e83825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cadavid D, Mellion M, Hupperts R, et al. Safety and efficacy of ipilimumab in patients with relapsing multiple sclerosis (SYNERGY): a randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2019;18(9):845-856. [DOI] [PubMed] [Google Scholar]
- 51.Feucht N, Maier M, Lepennetier G, et al. Optical coherence tomography angiography indicates associations of the retinal vascular network and disease activity in multiple sclerosis. Mult Scler. 2019;25(2):224-234. [DOI] [PubMed] [Google Scholar]
- 52.Spain RI, Liu L, Zhang X, et al. Optical coherence tomography angiography enhances the detection of optic nerve damage in multiple sclerosis. Br J Ophthalmol. 2018;102(4):520-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Huang Y, Zhou L, ZhangBao J, et al. Peripapillary and parafoveal vascular network assessment by optical coherence tomography angiography in aquaporin-4 antibody-positive neuromyelitis optica spectrum disorders. Br J Ophthalmol. 2019;103(6):789-796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chahin S, Miller D, Sakai RE, et al. Relation of quantitative visual and neurologic outcomes to fatigue in multiple sclerosis. Mult Scler Relat Disord. 2015;4(4):304-310. [DOI] [PubMed] [Google Scholar]
- 55.Oberwahrenbrock T, Traber GL, Lukas S, et al. Multicenter reliability of semiautomatic retinal layer segmentation using OCT. Neurol Neuroimmunol Neuroinflamm. 2018;5(3):e449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aytulun A, Cruz-Herranz A, Aktas O, et al. APOSTLE 2.0 recommendations for reporting quantitative optical coherence tomography studies. Neurology. 2021;97(2):68-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Roberg BL, Bruce JM, Feaster HT, O'Bryan SR, Westervelt HJ, Glusman M. Speedy eye movements in multiple sclerosis: association with performance on visual and nonvisual cognitive tests. J Clin Exp Neuropsychol. 2015;37(1):1-15. [DOI] [PubMed] [Google Scholar]
- 58.Moroso A, Ruet A, Deloire M, et al. Cerebellar assessment in early multiple sclerosis. Cerebellum. 2017;16(2):607-611. [DOI] [PubMed] [Google Scholar]
- 59.Yousef A, Devereux M, Gourraud PA, et al. Subclinical saccadic eye movement dysfunction in pediatric multiple sclerosis. J Child Neurol. 2019;34(1):38-43. [DOI] [PubMed] [Google Scholar]
- Data available. Additional eReferences e1-e94 available at: links.lww.com/NXI/A675.