Abstract
Introduction:
Dysphagia is a highly prevalent disorder in Parkinson’s Disease (PD) characterized by changes in swallowing kinematics, residue, and airway invasion. These changes can lead to serious medical morbidities including malnutrition, aspiration pneumonia, and death. However, little is known about the most predictive causes of residue and airway invasion in this patient population. Therefore, the aims of this study were to: 1) assess how disease severity affects residue, airway invasion, and swallowing kinematics in PD; and 2) determine which swallowing kinematic variables were most predictive of residue and airway invasion.
Methods:
A secondary analysis of forty videofluoroscopic swallow studies (VFSS) from individuals with early through mid-stage PD was performed. Airway invasion (Penetration-Aspiration Scale ‘PAS’), residue (Bolus Clearance Ratio ‘BCR’), and ten spatiotemporal swallowing kinematic variables were analyzed. Statistical analyses were used to determine if disease severity predicted residue, depth of airway invasion, and swallowing kinematics, and to examine which swallowing kinematic variables were most predictive of residue and the presence of airway invasion.
Results:
Results revealed that residue and the presence airway invasion were significantly predicted by swallowing kinematics. Specifically, airway invasion was primarily influenced by the extent and timing of airway closure, while residue was primarily influenced by pharyngeal constriction. However, disease severity did not significantly predict changes to swallowing kinematics, extent of residue, or depth of airway invasion during VFSS assessment.
Discussion:
This study comprehensively examined the pathophysiology underlying dysphagia in people with early to mid-stage PD. The results of the present study indicate that disease severity alone does not predict swallowing changes in PD, and therefore may not be the best factor to identify risk for dysphagia in PD. However, the swallowing kinematics most predictive of residue and the presence of airway invasion were identified. These findings may help to guide the selection of more effective therapy approaches for improving swallowing safety and efficiency in people with early to mid-stage PD.
Introduction
Parkinson’s disease (PD) is a highly prevalent neurodegenerative disorder of the central nervous system, affecting 1% of all individuals over 60 years of age [1,2]. Eleven to 97% of individuals with PD will be diagnosed with dysphagia at some point during their disease progression [3-6]. When dysphagia is present, impairments in swallowing kinematics, swallowing safety (penetration and aspiration/’airway invasion’), and swallowing efficiency (residue) are observed. These impairments increase the risk of developing serious medical conditions including dehydration [7,8], malnutrition [8-10], and aspiration pneumonia [11,12] – a leading cause of death in PD [13,14].
Given the high prevalence and impact of dysphagia in PD, a substantial amount of research has evaluated the effects of PD on swallowing physiology and function. Studies have found that, when compared to healthy controls, people with PD have compromised swallowing safety and efficiency [15-19], reduced velocity and displacement of pharyngeal and laryngeal structures during swallowing [17,20], delayed pharyngeal swallow initiation and airway closure [15,16,18-20], abnormal sequencing and duration of swallowing gestures [19], and increased variability in swallowing pressures [21,22]. While the effects of antiparkinsonian medications [23-26] and deep brain stimulation [27-29] on swallowing has been previously evaluated, investigations into the effects of disease severity on swallowing are currently limited and inconclusive [30], and no research has previously examined which swallowing kinematics most strongly influence impairments in swallowing safety and swallowing efficiency. By identifying if disease severity impacts swallowing in PD, clinicians may better identify patients at risk of dysphagia, and by identifying which physiologic impairments most strongly influence compromised swallowing safety and efficiency, clinicians and researchers can improve the accuracy of their intervention planning for improved rehabilitation outcomes.
Therefore, the aims of this study were to: 1) assess how swallowing kinematics, residue, and depth of airway invasion change as a function of disease severity; and 2) determine which spatiotemporal swallowing kinematic variables contribute most significantly to residue and the presence of airway invasion. We hypothesized that disease severity would significantly influence changes to swallowing kinematics, residue, and airway invasion, and that specific swallowing kinematics could be identified that would be most related to residue and the presence of airway invasion.
Methods
Participants
This was a secondary analysis of videofluoroscopic swallow studies (VFSS) in people with PD being considered for deep brain stimulation (DBS) surgery. Participants were recruited consecutively if presenting with a diagnosis of idiopathic PD and referred for DBS surgery by a fellowship trained movement disorder specialist neurologist. Other inclusion criteria included: (1) non-smoking or no smoking within the previous five years, and no smoking for more than five years at any time; (2) Neurologic and mental status permitting participation and cooperation (Mini-Mental Status Examination score above 24) [31]; and (3) a medical status permitting participation in the VFSS. Exclusion criteria were designed to exclude any potential study biases or patient safety issues, and included any history of stroke, head and neck cancer, respiratory diseases/disorders, severe diabetes mellitus, or dysphagia from something other than PD. Patient demographic information was recorded for each participant, including: age, sex, disease duration, and Unified Parkinson’s Disease Rating Scale (UPDRS) [32]. The UPDRS is a four-part rating scale that includes a patient interview and clinical observations to measure of disease severity. This rating scale was completed by a trained movement disorders specialist neurologist.
Swallowing Evaluations
Each participant underwent a VFSS during the “on” stage of their PD medication. During the VFSS, participants were seated in the upright position and self-administered the following boluses: 5 cc cued thin liquid; 5 cc non-cued thin liquid; one self-administered (non-measured) thin liquid cup sip; 90 cc thin liquid cup sips; 5 cc semisolid by teaspoon; and, a dry solid cracker with barium semisolid for contrast. Forty percent w/v Varibar Barium Sulfate Suspension™ (Bracco Imaging) was used for all liquid boluses, and Varibar Pudding Oral Paste™ (Bracco Imaging) was used for the semisolid boluses. With the exception of the first 5 cc bolus, all swallows were “non-cued” boluses to avoid changes associated with cued swallowing [33]. For the cued bolus trial, participants were asked to hold the 5 cc liquid in their mouth, and to swallow only when verbally cued by the examining clinician. For the purposes of this study, only the following four swallowing conditions had kinematic analyses performed: 5 cc cued thin liquids; 5 cc non-cued thin liquids; self-administered thin liquid cup sips; and, 5 cc non-cued semisolids.
A high resolution, videofluoroscopic recording device was used for signal acquisition (Digital Swallowing Workstation, model 7100, Lincoln Park, NJ: Kay Elemetrics). Images were captured in the lateral viewing plane, using a continuous image capturing rate of 30 images per second, with a magnification of 1x, and collimated to include (at minimum) the lips anteriorly, the nasal cavity floor superiorly, the cervical spine posteriorly, and the cervical esophagus and trachea inferiorly. Fluoroscopic capture included (at minimum) one second before initiation of oral bolus transit, and one second following pharyngeal swallow completion. Video recordings were stored digitally to a picture archiving systems (PACS) for subsequent analysis. Recordings were uploaded into ImageJ software (http://rsb.info.nih.gov/nih-image) for frame-by-frame fluoroscopic analysis.
Outcome Measures
Airway Invasion
Airway invasion was captured using the Penetration Aspiration Scale (PAS) (Table 1) [34] – a visual-perceptual scale describing the presence of and reaction to penetrant and aspirate material. PAS scores were recorded for each of the four swallowing conditions. Additionally, the “worst” PAS score seen across the entire VFSS protocol was also recorded.
Table 1.
Swallowing Safety Categorized by the Penetration Aspiration Scale (PAS)
| Swallowing Safety | PAS Score | PAS Score Description |
|---|---|---|
| No Penetration | 1 | Material does not enter the airway |
| Penetration | 2 | Material enters the airway, remains above the vocal folds, and is ejected from the airway |
| 3 | Material enters the airway, remains above the vocal folds, and is not ejected from the airway | |
| 4 | Material enters the airway, contacts the vocal folds, and is ejected from the airway | |
| 5 | Material enters the airway, contacts the vocal folds, and is not ejected from the airway | |
| Aspiration | 6 | Material enters the airway, passes below the vocal folds, and is ejected into the larynx or out of the airway |
| 7 | Material enters the airway, passes below the vocal folds, and is not ejected out of the trachea despite effort | |
| 8 | Material enters the airway, passes below the vocal folds, and no effort is made to eject |
Residue
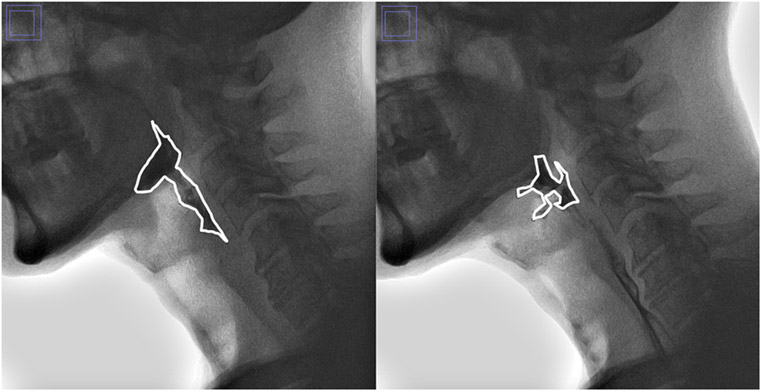
Residue was measured using the bolus clearance ratio (BCR) (Figure 1) [35] – a quantitative measure tracing the area of the bolus in the pharynx immediately before pharyngoesophageal segment (PES) opening to immediately after PES closing. A larger value indicates greater amounts of residue and worse bolus clearance. The BCR was measured for each of the four swallowing conditions. In instances where more than one swallow was elicited within the same trial, the BCR was measured for only the initial swallow.
Figure 1.
Bolus Clearance Ratio (BCR): area outlining bolus immediately prior to PES opening (left) and immediately after PES closing (right).
Swallowing Kinematics
A comprehensive assessment of swallowing kinematics was completed for each of the four swallowing conditions. In total, ten measures were selected to capture both spatial and temporal swallowing kinematics of the pharynx, larynx, and PES, including:
Peak hyoid position (Hpeak) [36]
Laryngeal constriction ratio (LCR)
Pharyngeal constriction ratio (PCR) [37]
Maximal PES displacement (PESmax) [38]
Onset of hyoid displacement (Honset) [39]
Onset of laryngeal vestibule closure (LVConset)
Laryngeal vestibule closure reaction time (LVCrt) [40]
Laryngeal vestibule closure to PES opening (LVC-PES) [39]
Duration of laryngeal vestibule closure (LVCduration) [39]
Duration of PES opening (PESduration) [39]
Descriptions of the kinematic measures are outlined in Table 2. The temporal measures (5-10 above) were derived by subtracting one swallowing event or gesture from another and dividing by 30 frames per second. For peak hyoid position (Hpeak), the anterior-inferior points of the C2 and C4 were marked to serve as both an internal anatomic scalar (%C2-C4 spine length [36]) and as the Y-axis in a participant-defined Cartesian coordinate system. Maximal PES distention (PESmax) was also expressed as a percentage of the C2-C4 length, to control for size-based variation across subjects.
Table 2.
Descripting of the Kinematic Variables Analyzed
| Kinematic | Description |
|---|---|
| Hpeak | The maximal position of the anterior-inferior point of the hyoid bone during swallowing from the anterior-inferior point of cervical vertebra C4, expressed as a percentage of the length from anterior-inferior C2-C4 (%C2-C4). |
| PCR | The area of the pharynx during maximal pharyngeal swallowing constriction, relative to the area of the pharynx at rest. A smaller value indicates greater pharyngeal constriction. |
| LCR | The area of the laryngeal vestibule during maximal laryngeal swallowing constriction, relative to the area of the laryngeal vestibule at rest. A smaller value represents greater laryngeal constriction. |
| PESmax | The narrowest width within the lumen located between cervical vertebrae C4 to C6 during maximal, uniform opening of the PES, expressed as a percentage of the length from anterior-inferior C2-C4 (%C2-C4). |
| Honset | The duration (seconds) between when the bolus head first passes the ramus of the mandible and when the hyoid first demonstrates brisk, uninterrupted movement leading to the swallow (also known as ‘Stage Transition Duration’). |
| LVConset | The duration (seconds) between when the bolus head first passes the ramus of the mandible and when complete closure of the laryngeal vestibule is first achieved. |
| LVCrt | The duration (seconds) between when the pharyngeal swallow is initiated (Honset) and when obliteration of the laryngeal vestibule airspace is first achieved (LVConset). |
| LVC-PES | The duration (seconds) between when the PES first opens and when obliteration of the laryngeal vestibule airspace is first achieved (LVConset). |
| LVCduration | The duration (seconds) between the first frame displaying complete laryngeal vestibule closure and to the first frame displaying offset of laryngeal vestibule closure. |
| PESduration | The duration (seconds) between initial opening of the PES and initial closing of the PES. |
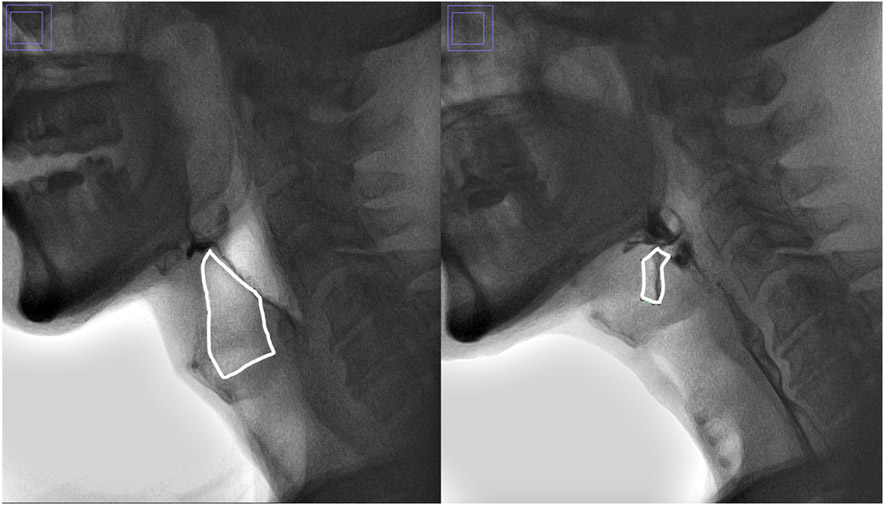
To derive pharyngeal constriction ratio (PCR), the area of the pharynx at rest was compared to the area of the pharynx at the point of maximal constriction during the swallow. The boundaries for tracing the pharynx included those originally outlined by Stokely et al. [37], defined superiorly as the top of the C2 vertebrae to the tongue base; inferiorly as the base of the piriform sinuses; posteriorly as the pharyngeal wall; and anteriorly as the wall formed by the base of tongue and aryepiglottic folds. To derive laryngeal constriction ratio (LCR), the area of the laryngeal vestibule at rest was compared to the area of the laryngeal vestibule at the point of maximal closure during the swallow (LCR – Figure 2). The boundaries for the laryngeal vestibule were defined antero-superiorly by the epiglottic petiole, inferiorly by the vocal folds, and posteriorly by the arytenoids and aryepiglottic folds.
Figure 2.
Laryngeal Constriction Ratio (LCR): area outlining the larynx at rest (left) and at maximal closure during the swallow (right). This is traced by beginning at the junction between the laryngeal surface of the epiglottis and the epiglottic petiole superiorly, tracing anteriorly and inferiorly to the vocal folds (about halfway between the thyroid notch and superior border of the tracheal air column), posteriorly along the vocal folds to the level of the posterior border of the tracheal air column, superiorly to the top of the arytenoids, and back to the epiglottic petiole.
Statistical Analysis
Statistical analyses were conducted using IBM SPSS Statistics for Macintosh, Version 25.0 (ICM Corp, Armonk, NY, USA). A p < 0.05 level was used to determine level of statistical significance.
Reliability
A primary rater, with 5 years of experience and expertise in the assessment and measurement of VFSSs, blindly analyzed all outcome measures. Twenty percent of the videos were selected at random for repeat analysis by the primary rater and a second rater, to capture intra- and inter-rater reliability. Interpretation of ICC was judged to be ‘excellent’ if ≥ 0.90, ‘good’ if between 0.75 and 0.90, ‘moderate’ if between 0.50 and 0.75, and ‘poor’ if < 0.50 [41]. Weighted kappas (κW) were run to calculate intra- and inter-rater reliability for the PAS. Interpretation for the κW was judged to be ‘excellent’ if ≥.81, ‘good’ if between 0.61 to 0.80, ‘moderate’ if between 0.41 to 0.60, ‘fair’ if between 0.21 to 0.40, and ‘poor’ if <.20 [42].Two-way random effects, absolute agreement, and intraclass correlation coefficients (ICC) were used to calculate intra- and inter-rater reliabilities for BCR and all kinematic variables.
Aim 1: Effects of Disease Severity on Airway Invasion, Residue, and Swallowing Kinematics
An ordinal logistic regression was used to determine the influence of disease severity on depth of airway invasion while controlling for age and sex. Depth of airway invasion was captured by grouping the ‘worst PAS’ into four ordinal categories: no airway invasion (PAS 1), penetration above the vocal folds (PAS 2-3), penetration to the vocal folds (PAS 4-5), and aspiration (PAS 6-8). Additionally, a linear regression was used to examine the influence of disease severity on residue while controlling for age and sex. Residue was captured using the largest BCR measured across the four swallowing trials. Lastly, a multivariate linear regression was run to determine the influence of disease severity on swallowing kinematics during 5 cc non-cued thin liquid swallows. This bolus was selected in order to control for bolus size across individuals, while also allowing for a more “natural” (i.e., non-cued) swallowing condition.
Aim 2: Effects of Swallowing Kinematics on Airway Invasion and Residue
A binomial logistic regression was used to examine the influence of swallowing kinematics on the presence/absence of airway invasion across each of the four swallowing conditions. Airway invasion was captured by grouping the PAS measured for each of the four swallowing conditions into two nominal categories: no airway invasion (PAS 1) and airway invasion (PAS 2-8). Additionally, a linear regression was used to determine the influence of swallowing kinematics on BCR for each of the four swallowing conditions. For both regression models, a forward selection approach was used by: 1) identifying the amount of variance that each kinematic variable explained in airway invasion and residue, respectively; 2) entering the most significantly influential kinematic variable into the regression model; 3) determining if a significant change to the model was achieved with the addition of the significant variable; and 4) repeating steps 1 through 3 until no significant change to the model was observed. The final model for each swallowing condition was reported.
Results
Forty participants met the inclusion-exclusion criteria and were included in these analyses. Participants included 29 males and 11 females with idiopathic PD. They had an average age of 63.2 years (± 8.9 years), an average disease duration of 7.7 years (± 4.1 years), and an average UPDRS disease severity score of 28.0 (± 10.5). Swallowing severity (worst PAS) ranged in this patient population from normal to severe, with a median and mode PAS score of 3.0, and a PAS range from no airway invasion (PAS 1) to silent aspiration (PAS 8). Descriptive of measures of airway invasion, residue, and swallowing kinematics are outlined in Table 3.
Table 3.
Descriptive Statistics of Swallowing Kinematics, Residue, and Airway Invasion
| Worst PAS | ||||||||
|---|---|---|---|---|---|---|---|---|
| Depth of Airway Invasion (n = 40) | No Airway Invasion (PAS 1) n = 6 (15%) | Penetration Above the Vocal Folds (PAS 2-3) n = 22 (55%) | Penetration to the Vocal Folds (PAS 4-5) n = 8 (20%) | Aspiration Below the Vocal Folds (PAS 6-8) n = 4 (10%) | ||||
| Worst PAS | Median Score = 3.0 (Inter-Quartile Range = 2.0-5.0); Mean = 3.5 (Standard Deviation = 1.9); Range = 1.0 to 8.0 | |||||||
| 5 cc Cued Thin Liquid (n = 40) |
5 cc Non-Cued Thin Liquid (n = 39) |
Self-Administered Thin Liquid (n = 32) |
5 cc Non-Cued Semisolid (n = 38) |
|||||
| Measure | Mean ± SD | Range | Mean ± SD | Range | Mean ± SD | Range | Mean ± SD | Range |
| Hpeak (% C2-C4) | 1.647 ± .235 | 1.24 to 2.15 | 1.643 ± .215 | 1.18 to 2.15 | 1.671 ± .188 | 1.25 to 2.09 | 1.693 ± .231 | 1.28 to 2.27 |
| PCR | .039 ± .042 | .000 to .180 | .041 ± .037 | .000 to .170 | .060 ± .046 | .010 to .180 | .049 ± .040 | .000 to .200 |
| LCR | .003 ± .021 | .000 to .134 | .006 ± .030 | .000 to .187 | .010 ± .043 | .000 to .239 | .000 ± .000 | .000 to .000 |
| PESmax (% C2-C4) | .168 ± .064 | .070 to .410 | .171 ± .063 | .090 to .360 | .219 ± .057 | .140 to .440 | .224 ± .067 | .130 to .420 |
| Honset (seconds) | .147 ± .347 | −.333 to 1.50 | .138 ± .452 | −.567 to 1.80 | .109 ± .370 | −.533 to 1.77 | .306 ± .831 | −.767 to 2.90 |
| LVConset (seconds) | .403 ± .290 | .000 to 1.700 | .364 ± .403 | −.133 to 1.93 | .241 ± .240 | −.300 to 1.20 | .581 ± .840 | −.267 to 3.10 |
| LVCrt (seconds) | .294 ± .139 | .030 to .600 | .261 ± .240 | −.600 to .900 | .200 ± .185 | −.330 to .630 | .232 ± .371 | −1.43 to 1.30 |
| LVC-PES (seconds) | −.056 ± .117 | −.400 to .200 | −.003 ± .183 | −.400 to .733 | −.024 ± .172 | −.267 to .533 | .063 ± .236 | −.133 to 1.43 |
| LVCduration (seconds) | .379 ± .152 | .000 to .700 | .433 ± .263 | .000 to 1.60 | .454 ± .228 | .000 to 1.13 | .467 ± .305 | .233 to 2.17 |
| PESduration (seconds) | .533 ± .138 | .300 to .867 | .568 ± .122 | .267 to .833 | .631 ± .122 | .367 to .800 | .534 ± .145 | .300 to .933 |
| BCR | .070 ± .062 | .000 to .220 | .083 ± .071 | .000 to .330 | .058 ± .041 | .010 to .170 | .080 ± .066 | .000 to .290 |
| PAS | 1.5 ± 1.0 | 1.0 to 6.0 | 1.5 ± 1.0 | 1.0 to 5.0 | 1.9 ± 1.6 | 1.0 to 7.0 | 1.1 ± .4 | 1.0 to 3.0 |
| No Airway Invasion | n = 27 (67.5%) | n = 29 (74.4%) | n = 23 (71.9% | n = 35 (92.1%) | ||||
| Airway Invasion | n = 13 (32.5%) | n = 10 (25.6%) | n = 9 (28.1%) | n = 3 (7.9%) | ||||
Reliability
Intra-rater reliability was classified as ‘excellent’ for ten of the 12 measures, and ‘good’ for the remaining two measures. Inter-rater reliability was classified as ‘excellent’ for five of the 12 measures, ‘good’ for six of the 12 measures, and ‘moderate’ for the remaining measure (Table 4).
Table 4.
Intra- & Inter-Rater Reliability
| Measure | Intra-Rater | 95% C.I. | Classification | p-value | Inter-Rater | 95% C.I. | Classification | p-value |
|---|---|---|---|---|---|---|---|---|
| PAS | κW = .845 | .658 to .981 | Excellent | <.0005 | κW = .660 | .473 to .848 | Good | <.0005 |
| BCR | ICC = .954 | .905 to .978 | Excellent | <.0005 | ICC = .945 | .885 to .974 | Excellent | <.0005 |
| Hpeak | ICC = .942 | .879 to .972 | Excellent | <.0005 | ICC = .811 | .608 to .910 | Good | <.0005 |
| PCR | ICC = .917 | .827 to .960 | Excellent | <.0005 | ICC = .911 | .814 to .958 | Excellent | <.0005 |
| LCR | ICC = .962 | .920 to .982 | Excellent | <.0005 | ICC = .895 | .781 to .950 | Good | <.0005 |
| PESmax | ICC = .930 | .853 to .966 | Excellent | <.0005 | ICC = .847 | .342 to .966 | Good | <.0005 |
| Honset | ICC = .988 | .974 to .994 | Excellent | <.0005 | ICC = .943 | .842 to .976 | Excellent | <.0005 |
| LVConset | ICC = .986 | .962 to .994 | Excellent | <.0005 | ICC = .940 | .874 to .972 | Excellent | <.0005 |
| LVCrt | ICC = .950 | .897 to .976 | Excellent | <.0005 | ICC = .882 | .753 to .944 | Good | <.0005 |
| LVC-PES | ICC = .943 | .881 to .973 | Excellent | <.0005 | ICC = .854 | .592 to .939 | Excellent | <.0005 |
| LVCduration | ICC = .884 | .755 to .945 | Good | <.0005 | ICC = .898 | .786 to .951 | Good | <.0005 |
| PESduration | ICC = .810 | .601 to .910 | Good | <.0005 | ICC = .663 | .249 to .845 | Moderate | <.0005 |
Aim 1: Effects of Disease Severity on Swallowing Safety, Efficiency, and Kinematics
Disease severity did not significantly influence airway invasion, χ2(3) = 2.236, p = .525, Pseudo R2 (Nagelkerke) = .060 (Figure 3), nor did it significantly influence BCR, F(3, 39) = .215, p = .886, adjusted R2 = .018 (Figure 4). Additionally, disease severity did not significantly influence changes in swallowing kinematics, F(9, 26) = 1.345, Λ = .714, p = .363, canonical R2 = .285.
Figure 3.
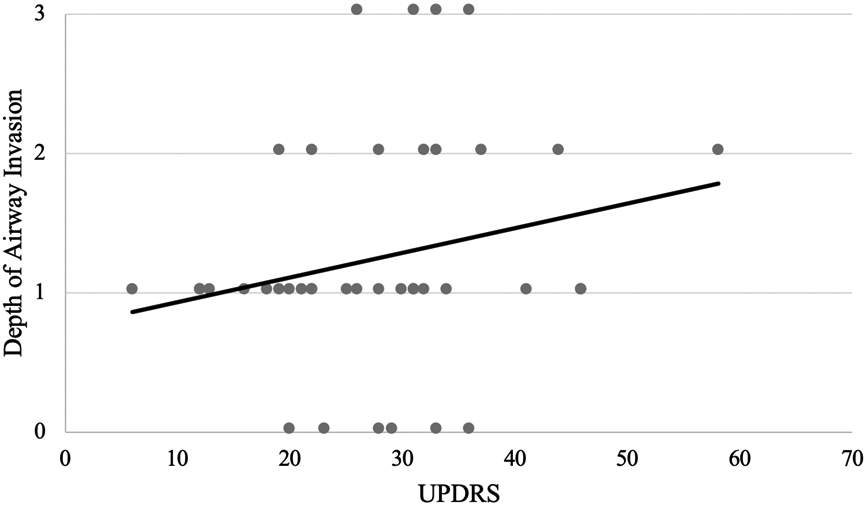
Influence of disease severity (UPDRS’ on depth of airway invasion
Figure 4.
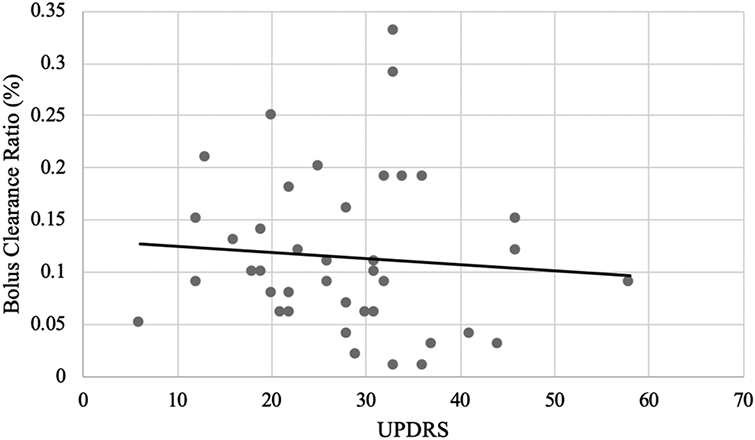
Influence of disease severity (using the Unified Parkinson’s Disease Rating Scale/’UPDRS’) on the residue (using the Bolus Clearance Ratio).
Aim 2: Effects of Swallowing Kinematics on Swallowing Safety and Efficiency Across Swallowing Conditions
Kinematic variables most related to airway invasion and BCR are presented below in order of highest effect size for each swallowing condition. Kinematic variables not reported below did not contribute significantly to the forward entry regression models.
Airway Invasion
During 5 cc cued thin liquids, airway invasion was significantly influenced by reduced pharyngeal constriction (larger PCR). During 5 cc non-cued thin liquid liquids, the presence of airway invasion was significantly influenced by a larger temporal latency between pharyngeal swallow initiation and when complete airway closure was first achieved (larger LVCrt). During self-administered thin liquid cup sips, the presence of airway invasion was significantly influenced by a combination of less complete airway closure (larger LCR) and a shorter duration of PES opening (smaller PESduration). And for 5 cc non-cued semisolids, airway invasion was most influenced by reduced pharyngeal constriction (larger PCR); however, this model did not reach statistical significance. Results summary of the regression models for airway invasion can be found in Table 5, and specific results for regression coefficients and standard errors can be found in Table 6.
Table 5.
Omnibus Results of Final Regression Models
| Swallow Condition | Outcome Measure | χ2 value | p-value | Pseudo-R2 (Nagelkerke) |
|---|---|---|---|---|
| 5 cc Cued Thin Liquid | Airway Invasion | χ2(1) = 6.256 | p = .012 | .209 |
| 5 cc Non-Cued Thin Liquid | Airway Invasion | χ2(1) = 7.682 | p = .006 | .289 |
| Self-Administered Thin Liquid | Airway Invasion | χ2(1) = 10.732 | p = .005 | .454 |
| 5 cc Non-Cued Semisolid | Airway Invasion | χ2(1) = 2.973 | p = .085 | .177 |
| Swallow Condition | Outcome Measure | F value | p-value | R2 |
| 5 cc Cued Thin Liquid | BCR | F(1, 37) = 61.185 | p < .0005 | .623 |
| 5 cc Non-Cued Thin Liquid | BCR | F(1, 35) = 44.745 | p < .0005 | .561 |
| Self-Administered | BCR | F(3, 26) = 8.920 | p < .0005 | .507 |
| 5 cc Non-Cued Semisolid | BCR | F(1, 36) = 47.441 | p < .0005 | .569 |
Table 6.
Results for Swallowing Kinematic Regression Models Predicting Airway Invasion Across Swallowing Conditions
| 5 cc Cued Thin Liquid | |||||
|---|---|---|---|---|---|
| Variable | B | SEB | Wald | df | p-value |
| Constant | −1.851 | .618 | 8.970 | 1 | .003 |
| PCR | 26.418 | 12.194 | 4.694 | 1 | .030 |
| 5 cc Non-Cued Thin Liquid | |||||
| Variable | B | SEB | Wald | df | p-value |
| Constant | −3.055 | .934 | 10.702 | 1 | .001 |
| LVCrt | 5.645 | 2.398 | 5.540 | 1 | .019 |
| Self-Administered Thin Liquid Cup Sip | |||||
| Variable | B | SEB | Wald | df | p-value |
| Constant | 3.319 | 2.906 | 1.304 | 1 | .253 |
| LCR | 290.620 | 216.078 | 1.809 | 1 | .179 |
| PESduration | −10.790 | 5.438 | 3.937 | 1 | .047 |
| 5 cc Non-Cued Semisolid | |||||
| Variable | B | SEB | Wald | df | p-value |
| Constant | −3.761 | 1.116 | 11.352 | 1 | .001 |
| PCR | 20.415 | 11.754 | 3.017 | 1 | .082 |
Residue
Larger BCR (more residue) was significantly influenced by less pharyngeal constriction (larger PCR) during 5 cc cued thin liquids, 5 cc non-cued thin liquids, and 5 cc semisolids. During self-administered thin liquid cup sips, larger BCR was significantly influenced by larger PCR in addition to shorter duration of PES opening (smaller PESduration) and greater extent of PES opening (larger PESmax). Results summary of significant models for BCR can be found in Table 5, and specific results for regression coefficients and standard errors can be found in Table 7.
Table 7.
Results for Swallowing Kinematic Regression Models Predicting BCR Across Swallowing Conditions
| 5 cc Cued Thin Liquid | ||||
|---|---|---|---|---|
| Variable | B | SEB | β | Semi-Partial R2 |
| Constant | .021 | .009 | ||
| PCR | 1.381 | .177 | .789 | .789 |
| 5 cc Normal Thin Liquid | ||||
| Variable | B | SEB | β | Semi-Partial R2 |
| Constant | .016 | .013 | ||
| PCR | 1.751 | .262 | .749 | .749 |
| Normal Thin Liquid Cup Sip | ||||
| Variable | B | SEB | β | Semi-Partial R2 |
| Constant | .054 | .037 | ||
| PCR | .457 | .145 | .452 | .433 |
| PESduration | −.123 | .050 | −.343 | −.341 |
| PESmax | .250 | .105 | .344 | .328 |
| 5 cc Normal Semisolid | ||||
| Variable | B | SEB | β | Semi-Partial R2 |
| Constant | .019 | .011 | ||
| PCR | 1.249 | .181 | .754 | .754 |
Discussion
This study comprehensively examined the influence of swallowing kinematics and disease severity on post-swallow residue and the presence/absence of penetration and aspiration in PD. Swallowing kinematics were found to significantly influence impairments in swallowing safety and efficiency, supporting the notion that residue, penetration, and aspiration can be explained by changes in swallowing mechanics. This study also found that the kinematic variables most related to residue and the presence of airway invasion differed across swallowing conditions (i.e., cued vs. non-cued conditions, controlled bolus sizes versus self-administered, and liquid consistency versus semisolid consistency).
Safely swallowing liquid boluses was most frequently associated with laryngeal swallowing kinematics. Specifically, the extent (LCR) and timing (LVCrt) of airway closure were the kinematic variables that most highly influenced presence of airway invasion for non-cued thin liquid swallows. This finding is perhaps intuitive, given that previous literature has identified airway invasion to be commonly associated with the extent, timeliness, and duration of airway closure [43-46]. Therefore, establishing an intervention that targets these spatial and temporal deficits in airway closure may work to reduce the extent and frequency of airway invasion when present in people with PD.
Efficiently swallowing liquid boluses was primarily associated with pharyngeal constriction. In fact, for both the cued and non-cued 5 cc liquid boluses, no other kinematic variable was predictive of residue after accounting for pharyngeal constriction. Additionally, for the self-administered cup sips, pharyngeal constriction was the most influential kinematic predictor for safety impairments, followed by duration and extent of PES opening, respectively.
For semisolid boluses, residue was influenced almost exclusively by pharyngeal constriction. Specifically, less pharyngeal constriction (greater PCR) was associated with greater amounts of residue. In fact, once accounting for pharyngeal constriction, no other kinematic variable significantly influenced residue. This finding supports previous research which demonstrates that semisolids require greater force to clear boluses through the pharynx and into the esophagus [47-49]. Airway invasion for semisolid boluses was also only associated with pharyngeal constriction. However, only three of the 38 semisolid trials demonstrated instances of airway invasion, and therefore the regression model for this association was underpowered and did not reach statistical significance. The limited number of airway invasion events for the semisolid bolus trials in this study is consistent with previous work which has also demonstrated airway invasion to be significantly less frequent and severe for thicker consistencies when compared to thin liquids in people with PD [50,51].
While not a primary aim of this study, the kinematic variables related to residue and the presence of airway invasion were also found to differ between cued and non-cued swallowing conditions. Specifically, timing of airway closure significantly predicted swallowing safety impairments for non-cued swallows, while extent of pharyngeal constriction was the primary predictor for swallowing safety impairments during cued swallows. In part, these findings support previously completed research in healthy adults, which also identified that non-cued swallows tend to demonstrate slower temporal measurements when compared to cued swallows [33,52]. However, while these studies found slower pharyngeal swallow initiation (‘Honset’ or ‘stage transition duration’) and longer bolus transit times, the current study did not. Instead, it was the timing of airway closure (LVCrt) that was found to be the strongest predictor for swallowing safety during the non-cued swallows, but not the cued swallows. More research is warranted to continue to evaluate the effects of verbal cueing on swallowing in people with PD.
The findings of the present study provide significant insight into the physiologic variables most related to functional swallowing impairments in people with early to mid-stage PD. By outlining these kinematic variables that influenced residue, penetration, and aspiration, we can begin to provide more targeted and effective swallowing interventions for people with PD. For example, expiratory muscle strength training (EMST), which has been found to increase the extent and duration of PES opening [53], may be an efficacious therapy approach for individuals with functional impairments for self-administered cup sips, which, as outlined, tend to be influenced by PES kinematics. Alternatively, volitional laryngeal vestibule closure (vLVC), which has been found to reduce LVCrt and increase LVCduration [54], may be a useful approach for individuals demonstrating airway invasion when swallowing liquid boluses.
Interestingly, disease severity did not significantly influence changes in swallowing kinematics, residue, or depth of airway invasion on videofluoroscopy in people with early to mid-stage PD. This finding is in partial contrast to previous research which has found associations between disease severity and swallowing disturbances [21,22,30]. There are several possible explanations for this discrepancy. First, the work by Jones and colleagues found differences between early and mid-stage PD using high-resolution pharyngeal manometry but not videofluoroscopy [21,22]. Therefore, it is possible that physiologic changes may have been present but were not being detected with the fluoroscopic analyses used in this study. Secondly, our study sample included a relatively small sample size and some of the outcome measures demonstrated a reliability level less than ‘excellent’ – both of which may have impacted the results. Considering the heterogeneity of PD, this study may have been underpowered to detect a potentially small effect of disease severity in our study sample. Additionally, the UPDRS, although a gold standard for assessing general PD severity, is a severity rating scale which is focused much more on appendicular function rather than axial function. Future studies should include a larger sample size with a greater range of disease severities. Lastly, the kinematic analyses in the present study focused on pharyngeal, laryngeal, and PES swallowing kinematics for 5 mL boluses and self-administered cups sips and did not include oral kinematics. The 5 mL bolus size is a smaller than average bolus size for healthy older adults [55], but was selected in an effort to maximize the number of participants who could complete the trials within a single swallow (a requirement for the kinematic analyses). As a result, this bolus size may have been too small to elicit observable differences in swallowing kinematics, residue, and airway invasion across disease severities. Therefore, future studies should consider the inclusion of oral kinematics and larger bolus volumes and assess how these change as a function of disease severity, and how these changes may impact residue, penetration, and aspiration.
Conclusions
This study is the first to identify the kinematic factors which influence residue, penetration, and aspiration in individuals with early through mid-stage PD. A variety of spatial and temporal swallowing kinematics were identified that significantly influenced the presence of residue, penetration, and aspiration. This information provides insight into potential therapy targets for improved swallowing safety and efficiency in people with PD which should ultimately improve health outcomes in this patient population.
Acknowledgements:
This work was supported in part by an NIH (NCATS) CTSA through the University of Florida (UL1TR000064 and KL2TR000065), awarded to Dr. Michelle S. Troche.
References
- 1.de Lau L, Breteler M. Epidemiology of Parkinson’s disease. Lancet Neurol. 2006:5. doi: 10.1007/s00702-017-1686-y. [DOI] [PubMed] [Google Scholar]
- 2.Suttrup I, Warnecke T. Dysphagia in Parkinson’s Disease. Dysphagia. 2016;31:24–32. doi: 10.1007/s00455-015-9671-9. [DOI] [PubMed] [Google Scholar]
- 3.Takizawa C, Gemmell E, Kenworthy J, Speyer R. A Systematic Review of the Prevalence of Oropharyngeal Dysphagia in Stroke, Parkinson’s Disease, Alzheimer’s Disease, Head Injury, and Pneumonia. Dysphagia. 2016:1–8. doi: 10.1007/s00455-016-9695-9. [DOI] [PubMed] [Google Scholar]
- 4.Kalf JG, De Swart BJM, Bloem BR, Munneke M. Prevalence of oropharyngeal dysphagia in Parkinson’s disease: A meta-analysis. Park Relat Disord. 2012;18:311–315. doi: 10.1016/j.parkreldis.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Cereda E, Cilia R, Klersy C, et al. Swallowing disturbances in Parkinson’s disease: A multivariate analysis of contributing factors. Park Relat Disord. 2014;20:1382–1387. doi: 10.1016/j.parkreldis.2014.09.031. [DOI] [PubMed] [Google Scholar]
- 6.Pflug C, Bihler M, Emich K, et al. Critical Dysphagia is Common in Parkinson Disease and Occurs Even in Early Stages: A Prospective Cohort Study. Dysphagia. 2018;33(1):41–50. doi: 10.1007/s00455-017-9831-1. [DOI] [PubMed] [Google Scholar]
- 7.Leibovitz A, Baumoehl Y, Lubart E, Yaina A, Platinovitz N, Segal R. Dehydration among long-term care elderly patients with oropharyngeal dysphagia. Gerontology. 2007;53:179–183. doi: 10.1159/000099144. [DOI] [PubMed] [Google Scholar]
- 8.Streicher M, Wirth R, Schindler K, Sieber CC, Hiesmayr M, Volkert D. Dysphagia in Nursing Homes—Results From the NutritionDay Project. J Am Med Dir Assoc. 2018;19:141–147. doi: 10.1016/j.jamda.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Serra-Prat M, Palomera M, Gomez C, et al. Oropharyngeal dysphagia as a risk factor for malnutrition and lower respiratory tract infection in independently living older persons: A population-based prospective study. Age Ageing. 2012;41:376–381. doi: 10.1093/ageing/afs006. [DOI] [PubMed] [Google Scholar]
- 10.Namasivayam-MacDonald AM, Morrison JM, Steele CM, Keller H. How Swallow Pressures and Dysphagia Affect Malnutrition and Mealtime Outcomes in Long-Term Care. Dysphagia. 2017;32:785–796. doi: 10.1007/s00455-017-9825-z. [DOI] [PubMed] [Google Scholar]
- 11.Langmore SE, Terpenning MS, Schork A, et al. Predictors of aspiration pneumonia: How important is dysphagia? Dysphagia. 1998;13:69–81. doi: 10.1007/PL00009559. [DOI] [PubMed] [Google Scholar]
- 12.Daniels SK, Ballo LA, Mahoney MC, Foundas AL. Clinical predictors of dysphagia and aspiration risk: Outcome measures in acute stroke patients. Arch Phys Med Rehabil. 2000;81:1031–1033. doi: 10.1053/apmr.2000.6301. [DOI] [PubMed] [Google Scholar]
- 13.Beyer MK, Herlofson K, Arsland D, Larsen JP. Causes of death in a community-based study of Parkinson’s disease. Acta Neurol Scand. 2001;103(1):7–11. doi: 10.1034/j.1600-0404.2001.00191.x. [DOI] [PubMed] [Google Scholar]
- 14.Fall P, Saleh a, Fredrickson M, Olsson J, Granerus a. Survival time, mortality, and cause of death in elderly patients with Parkinson’s disease. Mov Disord. 2003;18(11):1312–1316. [DOI] [PubMed] [Google Scholar]
- 15.Bird MR, Woodward MC, Gibson EM, Phyland DJ, Fonda D. Asymptomatic Swallowing Disorders in Elderly Patients with Parkinson’s Disease: A Description of Findings on Clinical Examination and Videofluoroscopy in Sixteen Patients. Age Ageing. 1994;23:251–254. [DOI] [PubMed] [Google Scholar]
- 16.Robbins JA, Logemann JA, Kirshner HS. Swallowing and speech production in Parkinson’s disease. Ann Neurol. 1986;19:283–287. doi: 10.1002/ana.410190310. [DOI] [PubMed] [Google Scholar]
- 17.Kim YH, Oh BM, Jung IY, Lee JC, Lee GJ, Han TR. Spatiotemporal characteristics of swallowing in Parkinson’s disease. Laryngoscope. 2015;125:389–395. doi: 10.1002/lary.24869. [DOI] [PubMed] [Google Scholar]
- 18.Fuh JL, Lee RC, Wang SJ, et al. Swallowing difficulty in Parkinson’s disease. Clin Neurol Neurosurg. 1997;99:106–112. doi: 10.1016/S0303-8467(97)00606-9. [DOI] [PubMed] [Google Scholar]
- 19.Nagaya M, Kachi T, Yamada T, Igata A. Videofluorographic Study of Swallowing in Parkinson’s Disease. Dysphagia. 1998;13:95–100. [DOI] [PubMed] [Google Scholar]
- 20.Ellerston JK, Heller AC, House DR, Kendall KA. Quantitative Measures of Swallowing Deficits in Patients with Parkinson’s Disease. Ann Otol Rhinol Laryngol. 2016;125(5):385–392. [DOI] [PubMed] [Google Scholar]
- 21.Jones CA, Hoffman MR, Lin L, Abdelhalim S, Jiang JJ, McCulloch TM. Identification of swallowing disorders in early and mid-stage Parkinson’s disease using pattern recognition of pharyngeal high-resolution manometry data. Neurogastroenterol Motil. 2018;30(4):e13236. doi: 10.1111/nmo.13236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jones CA, Ciucci MR. Multimodal Swallowing Evaluation with High-Resolution Manometry Reveals Subtle Swallowing Changes in Early and Mid-Stage Parkinson Disease. J Parkinsons Dis. 2016. doi: 10.3233/JPD-150687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Warnecke T, Suttrup I, Schröder JB, et al. Levodopa responsiveness of dysphagia in advanced Parkinson’s disease and reliability testing of the FEES-Levodopa-test. Park Relat Disord. 2016. doi: 10.1016/j.parkreldis.2016.04.034. [DOI] [PubMed] [Google Scholar]
- 24.Sutton JP. Dysphagia in Parkinson’s disease is responsive to levodopa. Park Relat Disord. 2013. doi: 10.1016/j.parkreldis.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 25.Hunter PC, Crameri J, Austin S, Woodward MC, Hughes AJ. Response of parkinsonian swallowing dysfunction to dopaminergic stimulation. J Neurol Neurosurg Psychiatry. 1997;63:579–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bushmann M, Dobmeyer SM, Leeker L, Perlmutter JS. Swallowing abnormalities and their response to treatment in Parkinson’s disease. Neurology. 1989;39(10):1309–1309. [DOI] [PubMed] [Google Scholar]
- 27.Troche MS, Brandimore AE, Foote KD, et al. Swallowing outcomes following unilateral STN vs. GPi surgery: A retrospective analysis. Dysphagia. 2014;29:425–431. doi: 10.1007/s00455-014-9522-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Troche MS, Brandimore AE, Foote KD, Okun MS. Swallowing and deep brain stimulation in Parkinson’s disease: A systematic review. 2013;19:783–788. doi: 10.1016/j.parkreldis.2013.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Troche MS, Brandimore AE, Hegland KW, Zeilman PR, Foote KD, Okun MS. Tailored deep brain stimulation optimization for improved airway protective outcomes in Parkinson’s disease. Interdiscip Neurosurg. 2016;5:3–5. doi: 10.1016/j.inat.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalf JG, De Swart BJM, Bloem BR, Munneke M. Prevalence of oropharyngeal dysphagia in Parkinson’s disease: A meta-analysis. Park Relat Disord. 2012;18:311–315. doi: 10.1016/j.parkreldis.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 31.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 32.Disease MDSTF on RS for P. The Unified Parkinson ’ s Disease Rating Scale (UPDRS): Status and Recommendations. Mov Disord. 2003;18(7):738–750. doi: 10.1002/mds.10473. [DOI] [PubMed] [Google Scholar]
- 33.Daniels SK, Schroeder MF, Degeorge PC, Corey DM, Rosenbek JC. Effects of Verbal Cue on Bolus Flow During Swallowing. Am J Speech-Language Pathol. 2007;16:140–147. doi: 10.1044/1058-0360(2007/018. [DOI] [PubMed] [Google Scholar]
- 34.Rosenbek JC, Robbins J, Roecker EB, Coyle JL, Wood JL. A Penetration-Aspiration Scale. Dysphagia. 1996;11:93–98. [DOI] [PubMed] [Google Scholar]
- 35.Leonard R. Two Methods for Quantifying Pharyngeal Residue on Fluoroscopic Swallow Studies: Reliability Assessment. Ann Otolaryngolg Rhinol. 2017;4(3):1–5. [Google Scholar]
- 36.Molfenter SM, Steele CM. Use of an Anatomical Scalar to Control for Sex-Based Size Differences in Measures of Hyoid Excursion During Swallowing. J Speech Lang Hear Res. 2014;57:768–778. doi: 10.1044/2014_JSLHR-S-13-0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stokely SL, Peladeau-Pigeon M, Leigh C, Molfenter SM, Steele CM. The Relationship Between Pharyngeal Constriction and Post-swallow Residue. Dysphagia. 2015;30:349–356. doi: 10.1007/s00455-015-9606-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leonard RJ, Kendall KA, McKenzie S, Gonçalves MI, Walker A. Structural Displacements in Normal Swallowing: A Videofluoroscopic Study. Dysphagia. 2000;15(3):146–152. doi: 10.1007/s004550010017. [DOI] [PubMed] [Google Scholar]
- 39.Molfenter SM, Steele CM. Variation in temporal measures of swallowing: Sex and volume effects. Dysphagia. 2013;28:226–233. doi: 10.1007/s00455-012-9437-6. [DOI] [PubMed] [Google Scholar]
- 40.Anderson C, Macrae P, Taylor-Kamara I, Serel S, Vose A, Humbert IA. The perturbation paradigm modulates error-based learning in a highly automated task: outcomes in swallowing kinematics. J Appl Physiol. 2015;119(4):334–341. doi: 10.1152/japplphysiol.00155.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Koo TK, Li MY. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J Chiropr Med. 2016;15:155–163. doi: 10.1016/j.jcm.2016.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Altman DG. Practical Statistics for Medical Research. London: Chapman & Hall; 1991. [Google Scholar]
- 43.Lundy DS, Smith C, Colangelo L, et al. Aspiration - Cause and implications. Otolaryngol - Head Neck Surg. 1999;120:474–478. [DOI] [PubMed] [Google Scholar]
- 44.Steele CM, Cichero JAY. Physiological factors related to aspiration risk: A systematic review. Dysphagia. 2014. doi: 10.1007/s00455-014-9516-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kahrilas PJ, Lin S, Rademaker AW, Logemann JA. Impaired deglutitive airway protection: A videofluoroscopic analysis of severity and mechanism. Gastroenterology. 1997;113:1457–1464. doi: 10.1053/gast.1997.v113.pm9352847. [DOI] [PubMed] [Google Scholar]
- 46.Morton R, Minford J, Ellis R, Pinnington LL. Aspiration with dysphagia: The interaction between oropharyngeal and respiratory impairments. Dysphagia. 2002;17:192–196. doi: 10.1007/s00455-002-0051-x. [DOI] [PubMed] [Google Scholar]
- 47.Park D, Shin CM, Ryu JS. Effect of Different Viscosities on Pharyngeal Pressure During Swallowing: A Study Using High-Resolution Manometry. Arch Phys Med Rehabil. 2017;98:487–494. doi: 10.1016/j.apmr.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 48.Hwang J, Kim DK, Bae JH, et al. The effect of rheological properties of foods on bolus characteristics after mastication. Ann Rehabil Med. 2012. doi: 10.5535/arm.2012.36.6.776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Leonard R, Rees CJ, Belafsky P, Allen J. Fluoroscopic surrogate for pharyngeal strength: The pharyngeal constriction ratio (PCR). Dysphagia. 2011;26:13–17. doi: 10.1007/s00455-009-9258-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Logemann JA, Gensler G, Robbins J, et al. A Randomized Study of Three Interventions for Aspiration of Thin Liquids in Patients With Dementia or Parkinson’s Disease. J Speech Lang Hear Res. 2008;51:173–183. doi: 10.1044/1092-4388(2008/013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Troche MS, Sapienza CM, Rosenbek JC. Effects of bolus consistency on timing and safety of swallow in patients with Parkinson’s disease. Dysphagia. 2008;23:26–32. doi: 10.1007/s00455-007-9090-7. [DOI] [PubMed] [Google Scholar]
- 52.Nagy A, Leigh C, Hori SF, Molfenter SM, Shariff T, Steele CM. Timing differences between cued and noncued swallows in healthy young adults. Dysphagia. 2013;28:428–434. doi: 10.1007/s00455-013-9456-y. [DOI] [PubMed] [Google Scholar]
- 53.Troche M, Okun M, Rosenbek J, et al. Aspiration and swallowing in Parkinson’s disease and rehabilitation with EMST: A randomized trial. Mov Disord. 2010;75:1912–1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guedes R, Azola A, Macrae P, et al. Examination of swallowing maneuver training and transfer of practiced behaviors to laryngeal vestibule kinematics in functional swallowing of healthy adults. 2017. doi: 10.1016/j.physbeh.2017.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lawless HT, Bender S, Oman C, Pelletier C. Gender, age, vessel size, cup vs. straw sipping, and sequence effects on sip volume. Dysphagia. 2003. doi: 10.1007/s00455-002-0105-0. [DOI] [PubMed] [Google Scholar]