Abstract
Background
Subcapital fractures of the fifth metacarpal bone, meaning fractures just below the knuckle of the little finger, account for approximately 20% of all hand fractures. Currently, there is no consensus concerning the optimal management of these fractures. Traditionally, treatment consists of closed reduction and external splinting in a neutral position using plaster of Paris (POP), involving the metacarpal joint, the proximal interphalangeal joint and the carpo‐metacarpal joint. An alternative treatment strategy is functional treatment using taping or bracing that does not restrict movement.
Objectives
To compare functional treatment with immobilization, and to compare different periods and types of immobilization, for the treatment of closed fifth metacarpal neck fractures in adults.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialized Register (June 2008), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2008, Issue 3), OVID OldMEDLINE (1951 to 1965), OVID MEDLINE (1966 to May Week 3 2008), EMBASE (1988 to 2008, Week 22), and reference lists of articles. No language restrictions were applied.
Selection criteria
All randomized and quasi‐randomized controlled trials which compare functional treatment with immobilization or different types of immobilization for closed fifth metacarpal neck fractures.
Data collection and analysis
Two review authors assessed abstracts of all studies identified by the initial search, identified studies meeting the selection criteria, independently assessed the quality of the trial reports, and extracted and analysed the data.
Main results
Five studies met the inclusion criteria including a total of 252 participants. Most studies were of poor quality. The primary outcome measure, function of the hand, was not used in any studies. There was no evidence that any of the treatment modalities was statistically significantly superior.
Authors' conclusions
No included studies reported our primary outcome measure of interest, validated hand function. There was heterogeneity between the studies, which were of limited quality and size. Consequently, no single non‐operative treatment regimen for fracture of the neck of the fifth metacarpal can be recommended as superior to another. Further research is definitely warranted.
Keywords: Humans; Bandages; Braces; Casts, Surgical; Finger Injuries; Finger Injuries/therapy; Fracture Fixation; Fracture Fixation/methods; Fractures, Bone; Fractures, Bone/therapy; Metacarpal Bones; Metacarpal Bones/injuries; Randomized Controlled Trials as Topic; Recovery of Function; Treatment Outcome
Plain language summary
Conservative treatment for closed fifth (small finger) metacarpal neck fractures
A closed (the overlying skin remains intact) fifth metacarpal neck fracture occurs when the bone is broken just below the knuckle of the little finger. These account for approximately one in five of all hand fractures. The typical patient is a young man who sustained this injury, which is often called a boxer's fracture, as a result of throwing a punch. Currently, there is no consensus concerning the best way to treat these fractures, which because they are common and affect a mainly working‐age population have important economic consequences. Usually they are treated without surgery. Conservative or non‐surgical treatment generally involves fracture reduction, where the bone fragments are put back into place, followed by immobilisation by various means (e,g, plaster cast, splint, brace or strapping of adjacent fingers) and to various extents, including none at all. If one particular treatment method could be shown to be superior to all others in terms of functional outcome or allow earlier return to work, then the economic impact of this would be considerable. By examining the evidence from randomised controlled trials, this review aimed to answer “which treatment results in the best functional outcome in adults?”. Other outcomes of interest sought included pain, time to return to work and cosmetic outcome.
Five small studies, which included a total of 252 patients, met the inclusion criteria. Most studies were of poor quality and the patient numbers were small and none reported on hand function. There was no evidence that any of the treatments under test was significantly superior. Based upon current evidence, no single conservative method for fracture of the neck of the fifth metacarpal can be recommended as superior to another. Recovery though was generally excellent whichever method of treatment was used.
Background
Fractures of the fifth (small finger) metacarpal neck are common injuries, accounting for approximately 20% of all hand fractures (Hunter 1970). The fractures are usually sustained by an axial blow on the metacarpal phalangeal (MCP) joint in flexed position, hence the name 'Boxer's fracture'.
At the time of injury, the normal pre‐existing angulation in a palmar direction of the metacarpal head increases. This is due to the force causing the fracture and the flexion forces across the metacarpal‐phalangeal joint produced by the resting tension of the intrinsic and extrinsic muscles of the hand. This angulation causes a shortening of the metacarpal neck, which can result in loss of the normal prominence of the fifth knuckle. This may give rise to cosmetic complaints (Ali 1999).
At present, there is no consensus on the optimal management of these fractures. The extent of acceptable palmar angulation remains under debate; recommendations in the literature vary from 20 degrees to 70 degrees (Braakman 1998a; Ford 1989; Hansen 1998a; Konradsen 1990; Kuokkanen 1999; McMahon 1994; Sorensen 1993; Statius Muller 2003;Theeuwen 1991). A biomechanical study concluded that 30 degrees is the upper limit for acceptable final angulation (Ali 1999). Although investigations have shown that palmar angulation of the neck of the fifth metacarpal rarely gives rise to any functional disability, no clinical study has provided a conclusive answer to the question of how much angulation is acceptable in terms of functional recovery or residual symptoms.
Another undetermined variable is the optimal length of treatment by cast or bandage. In different studies this period varies from one week of immobilization followed by functional treatment, to longer periods of pure immobilization.
Traditionally, treatment of this fracture consists of closed reduction and external splinting in a neutral position using plaster of Paris. A cast is applied as an ulnar gutter cast in which the MCP and PIP (proximal interphalangeal) joints are immobilized, as well as the wrist (Statius Muller 2003). An alternative is functional treatment, either by casting or taping. Functional casting allows the wrist and the finger joints free range of motion and is applied circularly around the metacarpals (Hansen 1998). Functional taping techniques may be used. Typically, tape is applied to splint the fourth finger against the fifth, thus preventing rotational deformity; a broad circular strap supports the fingers (Braakman 1998a); a compression glove is placed over the entire hand, which does not limit the range of movement in any joint (McMahon 1994). A third alternative is that patients may be given full dynamic treatment (no immobilization) and are advised to use the hand as normally as possible. In this case, no support is used.
Delayed union, or nonunion, is uncommon. Therefore functional treatment is advocated by some groups. Published studies conducted in the last 10 years have shown acceptable results for both immobilization and functional treatment. The purpose of this systematic review is to identify evidence for the optimal conservative treatment for fifth metacarpal neck fractures. Another review looking at randomized controlled trials of operative treatment options is planned by the authors.
Objectives
To compare functional treatment with immobilization, and to compare differing periods and types of immobilization for the treatment of closed fifth metacarpal neck fractures in adults.
Methods
Criteria for considering studies for this review
Types of studies
All randomised and quasi‐randomised (methods of allocating participants to a treatment which are not strictly random: e.g. date of birth, hospital record number or alternation) controlled trials which compare functional treatment with immobilization for closed fifth metacarpal neck fractures.
Types of participants
In our protocol, we planned to focus on adults with closed fifth metacarpal neck fractures. However, for practical reasons we decided to include children and adolescents where the original studies had done so. If data were presented on different groups with this injury, e.g. sports people, we planned to analyse these groups separately.
Types of interventions
The interventions of interest were:
splinting with plaster of Paris with immobilization of both the MCP and wrist joint;
functional bracing with free movement in both the MCP and wrist joint;
functional taping with free movement in both the MCP and wrist joint;
elastic (or compression) bandage with free movement in both the MCP and wrist joint;
full dynamic treatment with no external support with free movement in both the MCP and wrist joint.
Types of outcome measures
Primary outcomes
Functional outcome (based on activities of daily living (ADL) assessments and validated hand function scores)
Secondary outcomes
Patient satisfaction
Cosmetic appearance
Pain
Non‐union (failure of fracture to unite more than six months post injury, with radiographic evidence of fracture line or pain at the fracture site)
Malunion
Rotational deformity
Fracture angulation
Range of motion: flexion and extension in MCP
Grip strength
Time to union
Re‐intervention
Infection
Skin damage
Time to return to work (days off) or return to previous activity (e.g. sports)
Cost of treatment
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialized Register (June 2008), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2008, Issue 3), OVID OldMEDLINE (1951 to 1965), OVID MEDLINE (1966 to May Week 3 2008), EMBASE (1988 to 2008, Week 22). No language restrictions were applied.
In MEDLINE (OVID‐WEB), the first two phases of the Cochrane optimal trial search strategy (Higgins 2006) was combined with the subject specific search (seeAppendix 1). Search strategies for EMBASE (OVID‐WEB) and The Cochrane Library (Wiley InterScience) are shown in Appendix 2 and Appendix 3 respectively.
Searching other resources
We also searched Google Scholar and reference lists of articles.
Data collection and analysis
Selection of studies
Two authors (JCG and RWP) assessed abstracts of all studies identified by the initial search and excluded clearly non‐relevant studies. Full copies of the reports of potentially relevant studies were independently assessed by two authors (JCG and RWP) using the above mentioned inclusion criteria. Disagreements on inclusion were resolved by discussion and, if necessary, by scrutiny by an independent third author (JBL).
Assessment of methodological quality of included studies
In this review, risk of bias is implicitly assessed in terms of methodological quality.
The quality of the selected studies was independently assessed, without masking of the source and authorship of the trial reports, by two authors (JCG and RWP) using a quality assessment tool derived from the generic scheme formerly used by the Cochrane Bone, Joint and Muscle Trauma Group (seeTable 1). This scoring scheme considers various aspects of internal and external validity. From Issue 4, 2008, overall scores were no longer calculated. Disagreement was resolved by discussion and, if necessary, by scrutiny by an independent third author (JBL).
1. Quality assessment tool.
| Items | Scores |
| A. Was the assigned treatment adequately concealed prior to allocation? | 2 = (Cochrane code A) yes; method did not allow disclosure of assignment 1 = (Cochrane code B) not sure; small but possible chance of disclosure of assignment or unclear 0 = (Cochrane code C) clearly no; quasi‐randomized or open list/tables |
| B. Were the outcomes of participants who withdrew described and included in the analysis (intention‐to‐treat)? | 2 = intention‐to‐treat analysis based on all cases randomized possible or carried out 1 = states number and reasons for withdrawal but intention‐to‐treat analysis not possible 0 = not mentioned, or states number of withdrawals only |
| C. Were the outcome assessors blinded to treatment status? | 2 = effective action taken to blind assessors 1 = small or moderate chance of unblinding of assessors 0 = not mentioned or not possible |
| D. Were the treatment and control group comparable at entry? | 2 = good comparability of groups, or confounding adjusted for in analysis 1 = confounding small; mentioned but not adjusted for 0 = large potential for confounding, or not discussed |
| E. Were the treatment providers blind to assignment status? | 2 = effective action taken to blind treatment providers 1 = small or moderate chance of unblinding of treatment providers 0 = not possible, or not mentioned (unless double blind), or possible but not done |
| F. Were care programmes, other than the trial options, identical? | 2 = care programmes clearly identical 1 = clear but trivial differences 0 = not mentioned or clear and important differences in care programmes |
| G. Were the inclusion and exclusion criteria clearly defined? | 2 = clearly defined 1 = inadequately defined 0 = not defined |
| H. Were the interventions clearly defined? | 2 = clearly defined interventions are applied with a standardized protocol 1 = clearly defined interventions are applied but the application protocol is not standardized 0 = intervention and/or application protocol are poorly or not defined |
| I. Were the outcome measures used clearly defined? | 2 = clearly defined 1 = inadequately defined 0 = not defined |
| J. Were diagnostic tests used in outcome assessment clinically useful? (by outcome) | 2 = optimal 1 = adequate 0 = not defined, not adequate |
| K. Was the surveillance active, and of clinically appropriate duration? | 2 = active surveillance and appropriate duration (set visits up to six months or longer) 1 = active surveillance, but inadequate duration (set visits for three months) 0 = surveillance not active or not defined (no set visits or time of follow up not detailed). |
Data analysis
Data were extracted from all relevant studies independently by two authors. If data were incomplete or require clarification, attempts were made to contact the authors for further information. Agreement on data extraction discrepancies was reached by consensus. For each study, relative risks and 95% confidence intervals were calculated for dichotomous outcomes. We would have calculated the mean difference and 95% confidence intervals for continuous data. Where appropriate, results of comparable groups of trials were pooled using the fixed‐effect model. Heterogeneity was assessed using the standard chi‐squared test in conjunction with the I2 test (Higgins 2003). Where there was clear heterogeneity we pooled data using the random‐effects model.
Patient satisfaction
Where satisfaction was reported in three categories as "fully satisfied", "satisfied" or "dissatisfied", the data were dichotomized by combining the "satisfied" and "dissatisfied" categories to become "not fully satisfied". If participants had any residual complaints, they were analysed in the "not fully satisfied" group. Cosmetic appearance judged by the patient was grouped in patient satisfaction as well in the same manner.
Pain
Where pain was reported in three categories, "no pain", "moderate pain" or "severe pain", the data were dichotomized by combining the "moderate pain" and "severe pain" categories to become "pain". If participants had any residual complaints, they were analysed in the "pain" group.
Range of motion (ROM)
Numbers of participants with decreased ROM at three to six weeks and final follow up were extracted from tables and text where possible. If percentages were given numbers were calculated. Data were dichotomized into two groups: participants with decreased ROM and participants with full ROM.
Grip strength
Numbers of participants with decreased grip strength at three to six weeks follow up were extracted from tables and text where possible. Data were dichotomized to participants with loss of grip strength and participants with normal grip strength.
Results
Description of studies
Results of the search
In the first published version of this review (2004), we reported that the MEDLINE search retrieved 50 studies and the EMBASE search 76. The updated search (June 2004 to June 2008) identified a total of 117 new references, none of which were for eligible studies.
Included studies
Overall five studies met the inclusion criteria. Numbers of participants meeting the inclusion criteria, excluded before randomization, randomized in each treatment group, excluded post randomization, analysed in each treatment group and dropouts are described in Table 2.
2. Numbers of patients analyzed in each group.
| Study ID | Anand 1999 | Braakman 1998b | Harding 2001 | Kuokkanen 1999 | Statius Muller 2003 |
| Number meeting inclusion criteria | 60 | 50 | 73 | 29 | 40 |
| Excluded before randomization | nd | nd | nd | nd | 0 |
| Number randomized in control group | 28 | 25 | 42 | 15 | 20 |
| Post randomization exclusion in control group | nd | nd | nd | nd | 0 |
| Number analyzed in control group | 28 | 25 | 37 | 15 | 15 |
| Number of dropouts in control group | nd | nd | 5 | nd | 5 |
| Number randomized in first treatment group | 32 | 25 | 31 | 14 | 20 |
| Post randomization exclusion in first treatment group | nd | nd | nd | nd | 0 |
| Number analyzed in first treatment group | 32 | 23 | 28 | 14 | 20 |
| Number of dropouts in first treatment group | nd | 2 | 3 | nd | 0 |
nd: not described
Types of participants
Anand 1999 reported 60 participants aged 11 to 48 years with fractures of the neck of the fifth metacarpal. Gender was not described. No data were presented on different groups: e.g. sports or occupation.
Braakman 1998b described 50 consecutive participants with a fracture of the fifth metacarpal. Follow up was available for 43 men and five women aged between 14 and 44 years. No data were presented on different groups: e.g. sports or occupation.
Harding 2001 analysed 65 participants with minimally angulated (less than 40 degrees), closed fractures of the little finger metacarpal neck with no rotational deformity or associated injury. No data were recorded regarding age and gender of the participants.
Kuokkanen 1999 included 29 participants (26 men and three women) with subcapital fractures of the fifth metacarpal bone. Participants with fractures angulated more than 70 degrees, fractures with pronounced deviation or rotation deformity and open fractures were excluded. Median age was 29 years (range 11 to 68).
Statius Muller 2003 studied 40 participants (38 men and two women) with a mean age of 29 years (range 15 to 84), with fractures of the fifth metacarpal neck.
Types of interventions
For further details, please see Table 3.
3. Cross tabulation of interventions.
| Splinting with plaster of Paris with immobilization of both the MCP and wrist joint | Functional bracing with free movement in both the MCP and wrist joint | Functional taping with free movement in both the MCP and wrist joint | Elastic bandage with free movement in both the MCP and wrist joint | Neighbour strapping with free movement in both the MCP and wrist joint | Full dynamic treatment with no external support with free movement in both the MCP and wrist joint | |
| Splinting with plaster of Paris with immobilization of both the MCP and wrist joint | x | Braakman 1998b | Anand 1999 Kuokkanen 1999 Statius Muller 2003 | |||
| Functional bracing with free movement in both the MCP and wrist joint | x | Harding 2001 | ||||
| Functional taping with free movement in both the MCP and wrist joint | Braakman 1998b | x | ||||
| Elastic bandage with free movement in both the MCP and wrist joint | Anand 1999 Kuokkanen 1999 Statius Muller 2003 | x | ||||
| Neighbour strapping with free movement in both the MCP and wrist joint | Harding 2001 | x | ||||
| Full dynamic treatment with no external support with free movement in both the MCP and wrist joint | x |
Anand 1999: splinting with ulnar gutter splint for three weeks after attempted reduction compared to immediate mobilization in a "bulky dressing" (compression bandage).
Braakman 1998b: ulnar gutter cast with the wrist in 45 degrees dorsiflexion, the MCP joints in 90 degrees flexion and the IP joints in 0 to 10 degrees flexion compared to functional taping (also known as neighbour strapping).
Harding 2001: metacarpal brace compared to neighbour strapping (also known as functional taping).
Kuokkanen 1999: reduction of fracture and splinting with the MCP joints in 60 degrees flexion with the splint reaching to the level of the proximal IP joint leaving the joint free for movement for four weeks compared to an elastic bandage 5 cm wide applied circumferentially and with slight compression (compression bandage) from the MCP level to 10 cm above the wrist, following which the participants were encouraged to move the fingers immediately and they removed the bandages after one week.
Statius Muller 2003: ulnar gutter plaster cast for a period of three weeks followed by mobilization compared to a "pressure bandage" (compression bandage) or one week and immediate mobilization within limits imposed by pain.
Types of outcome measures
The primary outcome measure, which we had chosen a priori (functional outcome based on activities of daily living (ADL) assessments and validated hand function scores) was not described in any of the included studies.
Excluded studies
The 'Characteristics of excluded studies' lists 10 studies. Four excluded studies were randomized controlled trials of participants with metacarpal fractures (Hansen 1998; Konradsen 1990; McMahon 1994; Sorensen 1993), but analysis was not possible as data were not presented separately for fractures of the fifth metacarpal.
Risk of bias in included studies
The quality assessment scores for the individual studies are presented in Table 4. We include here a summary for the individual items.
4. Results: quality assessment.
| Anand 1999 | Braakman 1998b | Harding 2001 | Kuokkanen 1999 | Statius Muller 2003 | |
| A. Was the assigned treatment adequately concealed prior to allocation? | 0 | 1 | 1 | 1 | 1 |
| B. Were the outcomes of participants who withdrew described and included in the analysis (intention‐to‐treat)? | 0 | 1 | 0 | 2 | 1 |
| C. Were the outcome assessors blinded to treatment status? | 0 | 0 | 2 | 0 | 2 |
| D. Were the treatment and control group comparable at entry? | 0 | 1 | 1 | 1 | 1 |
| E. Were the treatment providers blind to assignment status? | 0 | 0 | 0 | 0 | 0 |
| F. Were care programmes, other than the trial options, identical? | 0 | 2 | 0 | 0 | 2 |
| G. Were the inclusion and exclusion criteria clearly defined? | 1 | 1 | 1 | 1 | 2 |
| H. Were the interventions clearly defined? | 0 | 2 | 1 | 2 | 2 |
| I. Were the outcome measures used clearly defined? | 1 | 2 | 1 | 2 | 1 |
| J. Were diagnostic tests used in outcome assessment clinically useful? (by outcome) | 1 | 1 | 1 | 1 | 1 |
| K. Was the surveillance active, and of clinically appropriate duration? | 1 | 2 | 0 | 1 | 1 |
A. Concealment of allocation Three studies used sealed envelopes for concealment. No computer or telephone randomization was used. Anand 1999 used medical record numbers for randomization.
B. Intention‐to‐treat analysis Description of the participants excluded was provided by Braakman 1998b, Kuokkanen 1999 and Statius Muller 2003.
C. Blinding outcome assessors Only Harding 2001 and Statius Muller 2003 blinded the outcome assessors.
D. Comparability of treatment groups at entry Comparability was poorly described in most studies. Braakman 1998b, Harding 2001, Kuokkanen 1999 and Statius Muller 2003 mentioned participants demography but no adjustment was made.
E. Blinding of treatment providers Blinding of treatment providers was impossible in these studies..
F. Care programmes, other than trial options, identical In all studies describing the care programmes, identical programmes were used. In studies which did not describe care programmes other than the intervention, this item was scored as unknown.
G. Inclusion and exclusion criteria clearly defined Inclusion criteria were described in all studies but Anand 1999. Exclusion criteria were described in Statius Muller 2003.
H. Interventions clearly defined All studies used a clearly defined and standardized intervention protocol.
I. Outcome measures clearly defined All studies clearly described the outcome measures used.
J. Diagnostic tests None of the studies used a validated patient outcome score. Plain radiographs were used in most studies to determine fracture angulation. Leung 2002 clearly described that the measurement of fracture angulation on plain radiographs of small finger metacarpal neck fractures seems to be subject to a high degree of inter‐ and intraobserver variability.
K. Follow‐up period Only Braakman 1998b followed the participants for a sufficient period. Most studies limited the follow‐up period to three months. Harding 2001 limited the follow‐up period to three weeks.
Effects of interventions
A total of 252 participants were included in the five included studies. Of these participants, 117 were available for analysis in the treatment group and 120 participants were available for analysis in the control group (seeTable 2). Table 5 and Table 6 show all available outcome measures and results for the included studies.
5. Results.
| Study ID | Treatment group | Patient satisfaction | Cosmetic appearance | Pain | Fracture angulation |
| Anand 1999 | Cast | nd | 20 of 21 patients satisfied | None of the patients at 3 months | Dorsal angulation post Rx: 27º (5º‐45º) |
| Compression bandage | nd | 28 of 28 patients satisfied | None of the patients at 3 months | Dorsal angulation post Rx: 41º (15º‐80º) | |
| Braakman 1998b | Cast | Number of patients with subjective residual symptoms 9 of 25. | nd | nd | Mean angulation (range): 27.4º (0º‐67º) |
| Tape | Number of patients with subjective residual symptoms 8 of 23. | nd | nd | Mean 24.7º, range (2º‐46º) | |
| Harding 2001 | Metacarpal brace | Overall satisfaction: fully satisfied 6, satisfied 22, dissatisfied 9. | One patient complaint about a lump at the fracture side. | Mean pain score (possible range 0‐3): 0.6 (0‐2) | nd |
| Neighbour strapping | Overall satisfaction: fully satisfied 5, satisfied 15, dissatisfied 8. | One patient complaint about a lump at the fracture side. | Mean pain score (possible range 0‐3): 1.6 (0‐3) | nd | |
| Kuokkanen 1999 | Cast | nd | nd | nd | Median (range) 35º (10º‐55º), at 4 weeks 30º (10º‐50º), at 3 months 29º (10º‐50º) |
| Compression bandage | nd | nd | nd | Median (range) 48º (35º‐60º), at 4 weeks 42º (20º‐60º), at 3 months 42º (20º‐60º) | |
| Statius Muller 2003 | Cast | At 6 weeks fully satisfied 60%, at 12 weeks 80%. | nd | At 6 weeks no pain: 87%, at 12 weeks 93% | nd |
| Compression bandage | At 6 weeks fully satisfied 60%, at 12 weeks 80%. | nd | At 6 weeks no pain: 70%, at 12 weeks 95% | nd |
nd: not described Rx: treatment
6. Results (continued).
| Study ID | Intervention | ROM in MCP joint | Grip strength | Skin damage | Return to work |
| Anand 1999 | Cast | Extensor lag at 3 months: 5 degrees in 2 participants | At 6 weeks: 69% of normal (17 participants) At 3 months: 99% of normal (13 participants) |
nd | Return to pre‐injury status at 3 months: 100% (21 participants) |
| Compression bandage | Extensor lag at 3 months: 5 degrees in 2 participants | At 6 weeks: 91% of normal (24 participants) At 3 months: 98% of normal (22 participants) |
nd | Return to pre‐injury status at 3 months: 100% (28 participants) | |
| Braakman 1998b | Cast | At 1 week: extension deficit 19 participants, flexion deficit 11 participants At 4 weeks: extension deficit 11 participants, flexion deficit 4 participants At 3 months: extension deficit 6 participants, flexion deficit 2 participants At 6 months: flexion deficit 1 participant |
The 50% recovery limit of power‐grip and pulling strength was reached within four weeks in 52% of the participants. | nd | nd |
| Tape | At 1 week: extension deficit 8 participants, flexion deficit 2 participants No extension or flexion deficit at 4 weeks, 3 and 6 months |
Restoration of pulling strength was significantly better in the tape group after one and four weeks (P<0.001). The 50% recovery limit of power‐grip and pulling strength was reached within four weeks in all participants. | nd | nd | |
| Harding 2001 | Metacarpal brace | Mean (range) ROM of MCPJ: active 78 (40‐130), passive 107 (70‐150) | nd | One participant | Return to work by 3 weeks: 92% (34 of 37 participants) |
| Neighbour strapping | Mean (range) ROM of MCPJ: active 65 (20‐90), passive 97 (40‐130) | nd | None | Return to work by 3 weeks: 29% (8 of 28 participants) | |
| Kuokkanen 1999 | Cast | ROM in degrees (range): At 4 weeks: 57 (10‐100). At 3 months: 90 (80‐95) |
Kg, fractured hand/healthy hand: At 4 weeks: 21 (10‐50)/34 (18‐54)Kg. At 3 months: 36 (26‐54)/41 (22‐59) Kg. |
None | nd |
| Compression bandage | ROM in degrees (range): At 4 weeks: 81 (45‐90) At 3 months: 90 (80‐95) |
Kg, fractured hand/healthy hand: At 4 weeks: 37 (20‐54)/44 (25‐72) Kg. At 3 months: 49 (30‐69)/51 (30‐74) Kg. |
None | nd | |
| Statius Muller 2003 | Cast | Full ROM at 6 weeks: 67% Full ROM at 12 weeks: 93% |
nd | nd | Return to work or hobby at 6 weeks: 2 participants Return to work or hobby at 12 weeks: all participants |
| Compression bandage | Full ROM at 6 weeks: 70% Full ROM 12 weeks: 95% |
nd | nd | Return to work or hobby at 6 weeks: 2 participants Return to work or hobby at 12 weeks: all participants |
MCPJ: metacarpo‐phalangeal joint nd: not described ROM: range of motion or movement
Primary outcome measure
Functional outcome (based on activities of daily living (ADL) assessments and validated hand function scores)
None of the included studies used functional outcome assessments and validated hand function scores.
Secondary outcome measures
Patient satisfaction (see Table 4 and Analyses 1.1, 2.1, 3.1 and 4.1)
Anand 1999 described this outcome measure in terms of cosmetic satisfaction. Braakman 1998b described patient satisfaction as participants with residual symptoms consisting of loss of power‐grip, and pulling and torque strengths, as well as pain, stiffness, intolerance to change in temperature and a non‐aesthetic appearance. Harding 2001 described patient satisfaction in three categories: fully satisfied, satisfied and dissatisfied. Statius Muller 2003 found that 60% of the participants were fully satisfied at six weeks follow up and 80% at 12 weeks follow up in both the cast and the bandage group.
Pooling of data was possible after dichotomizing in the following three studies (Anand 1999; Braakman 1998b; Statius Muller 2003). The pooling in analyses 2.1 and 4.1 is exploratory only.
Cosmetic appearance (see Table 4 and Analyses 2.2, 3.2 and 4.2)
Anand 1999 did not define satisfaction with cosmetic appearance, but all participants were satisfied in the mobilized group and 20 out of 21 in the cast group. In Harding 2001 participants in neither group complained of a short metacarpal compared to the other side, but one patient in each group expressed concern at the lump at the fracture site.
Pain (see Table 4 and Analyses 02.03 and 04.03)
In Anand 1999, none of the participants had pain at three months follow up in either group. Participants treated with a brace in Harding 2001 complained of less pain at three weeks follow up. A three point scale was used. Statius Muller 2003 reported three pain groups: no pain, moderate pain and severe pain. At six weeks follow up 87% of the participants in the cast group had no pain and 13% had moderate pain. In the bandage group 70% had no pain and 30% had moderate pain at six weeks. By 12 weeks 93% had no pain and 7% had moderate pain in the cast group, while 95% had no pain and 5% had moderate pain in the bandage group.
Fracture angulation (see Table 4)
From the table in the abstract of Anand 1999 we extracted the following data, assuming that "Rx" means treatment, or reduction.
Dorsal angulation prior to treatment: mobilization group 41º (range 15º to 80º); immobilization group 38º (range 15º to 70º).
Dorsal angulation after treatment: mobilization group 41º (range 15º to 80º); immobilization group 27º (range 5º to 45º).
Ulnar angulation prior to treatment: mobilization group 18º (range 0º to 40º); immobilization group 15º (range 0º to 40º).
Ulnar angulation after treatment: mobilization group 18º (range 0º to 40º); immobilization group: 1º (range 0º to 10º)
Braakman 1998b did not find a relation between functional recovery or existence of residual symptoms and the initial fracture angulation. In Kuokkanen 1999 the median primary angulation of the fracture was higher in the functional group than in the repositioned and splinted group. The angulation of the fracture remained at practically the same level compared with the primary angulation in both groups. In Statius Muller 2003, the fracture of the participants with a good ROM had a mean angulation of 39º (range 15º to 70º), while the participants with a moderate ROM had a mean fracture angulation of 37.5º (range 35º to 40º). The fracture of the participants whose satisfaction was good had a mean angulation of 43º (range 15º to 70º), while the participants whose satisfaction was moderate had a mean fracture angulation of 38º (range 30º to 55º). This was not described for each treatment group separately.
Range of motion (ROM) in MCP joint (see Table 5 and Analyses 1.2, 2.4 and 4.4)
We were able to pool the data for Braakman 1998b and Statius Muller 2003 at three to six weeks follow up. Participants with a decreased ROM were pooled for Anand 1999,Braakman 1998b and Statius Muller 2003 at final follow up. Anand 1999 described ROM in term of extensor lag at three months follow up. In the mobilized group two participants had an extensor lag of five degrees, as had two participants in the cast group. Braakman 1998b showed a significant difference in extension deficit after one week (P = 0.0002) At one week follow up an extension deficit of up to 30 degrees was seen in 76% of the participants treated in a cast. Likewise a flexion deficit was seen in 44% in this group. At one week follow up an extension deficit did not exceed 12 degrees in 26% of the functionally taped participants. A flexion deficit at one week was seen in 8% of this group. Only the extension deficit was significantly different after four weeks (P = 0.009). Normal mobility was restored in all participants treated by tape. In the cast group, however, the mobility was still limited in 44% after four weeks and in 8% after three months.
Harding 2001 showed that participants treated with a brace had a slightly better ROM than the participants in the neighbour strapping group.
In Kuokkanen 1999, the ROM of MCP joint was higher in the functional group at four weeks, but there was no difference at three months.
In Statius Muller 2003, full range of motion was achieved in 67% of the participants in the cast group at six weeks, and in 93% at 12 weeks. In the bandage group 70% had reached full ROM at six weeks and 95% at 12 weeks.
Grip strength (see Table 5 and Analyses 1.3 and 4.5)
Anand 1999 utilized the Jamar dynamometer for recording grip strength of both hands. Grip strength at six weeks follow up was 91% of normal in the mobilization group (24 participants tested) and 69% of normal in the cast group (17 participants tested). At three months it was 98% of normal in the mobilized group (22 participants tested) and 99% of normal in the cast group (13 participants tested).
Braakman 1998b showed restoration of pulling strength was significantly better in the tape group after one and four weeks (P < 0.001). The 50% recovery limit of power‐grip and pulling strength was reached within four weeks in every patient of the tape group, compared with 52% of the participants in a cast. The tape group also showed better performance after three months. After one week and four weeks all torque strengths were significantly better in the tape group (P < 0.01) with the exception of the one week pronation strength. Full functional recovery took place in all but one patient treated in a cast, in whom severe loss of power‐grip, pulling strength and moderate loss of torque strength persisted. No obvious explanation could be found for the poor outcome in this patient.
In Kuokkanen 1999, the grip force of the affected hand was considerably better in the functional group at four weeks and still slightly better at three months.
Skin damage (see Table 5 and Analysis 3.3)
In Harding 2001, one patient complained that the brace rubbed on the ulnar border of his hand, though this did not cause any significant damage. Kuokkanen 1999 found no skin damage in all participants.
Time to return to work or previous activity (see Table 5 and Analyses 02.05, 03.04 and 04.06)
In Anand 1999, all participants returned to their pre injury status. Thirty‐four out of 37 participants treated with a brace and eight out of 28 participants treated by neighbour strapping in Harding 2001 had returned to work by three weeks. No data were described for working status at final follow up. At six weeks two participants in Statius Muller 2003 had not returned to their work or hobby, but all had by 12 weeks.
Other secondary outcome measures
The following outcome measures were not described in any included trials.
Non‐union
Malunion
Rotational deformity
Time to union
Re‐intervention
Infection
Cost of treatment
Summary of results
There was no statistically significant difference in range of motion between any functional treatment (functional taping or compression bandage) and immobilization (plaster cast with immobilization of the MCP and wrist joints) at any point in time (one week, three to six weeks or three to six months follow up) (Anand 1999; Braakman 1998b; Statius Muller 2003). The random‐effects model was used to pool data as there was substantial heterogeneity at three to six weeks follow up (I2 = 82.7%). Although we cannot determine the source (or sources) of this heterogeneity, itmay reflect, amoungst other possibilities, differences in treatment interventions (tape versus compression bandage), in study populations, or in the care programs other than the trial options.
Anand 1999, Braakman 1998b and Kuokkanen 1999 all reported significantly reduced grip strength at three to 6 weeks in participants immobilized in plaster of Paris (POP) splints compared to participants treated with mobilization in a bulky dressing (compression bandage), functional taping, and circular elastic bandage (compression bandage) respectively. These data could not be pooled since no standard deviations were reported and Braakman 1998b reported the results in a graph.
Since none of the studies presented data on different patient groups with fracture of the neck of the fifth metacarpal, e.g. sports people, these groups could not be analysed separately.
Braakman 1998b was contacted to provide extra information, but was not able to provide any. We were unable to make contact with the authors of the other trials, with the exception of Statius Muller 2003.
Discussion
The objective of this Cochrane review was to compare functional treatment with immobilization, and to compare different periods and types of immobilization, for the treatment of closed fifth metacarpal neck fractures in adults. The results are disappointing. Our a priori primary outcome measure, validated hand function, was not reported in any study. The small number of eligible studies and variation in outcome measures between studies meant that pooling of data was only feasible for a minority of secondary outcome measures. We also need to note that, although range of movement sounds like a validated and reproducible measure, it is not so.
Researchers measuring true fracture angulation have compared radiographs of the contralateral (uninjured) hand (Abdon 1984) or subtracted a 'normal' angulation value (Ford 1989), most frequently quoted as 15 degrees. One problem with this approach is that the contralateral fifth metacarpal has not infrequently been fractured previously (Greer 1999). The most valid reference value appears to be that derived by Braakman 1996, who measured the metacarpal head/neck/shaft angle of fifth metacarpals in 225 cadaver hands on lateral and 30 oblique radiographic views. The subcapital‐axis angulation (the angle measured most commonly by clinicians) was 14.6 degrees in the lateral view and 11 degrees in the oblique view, with a capital‐axis angle of 26 degrees. Age, gender and hand dominance did not affect the angle measured. It can be seen that there is 15 degree difference as to what constitutes normal angulation of the fifth metacarpal neck, dependent on which axis is chosen and on which radiographic view it is measured. To complicate matters further, Leung 2002 demonstrated poor intra‐ and inter‐observer agreement on measured angulation by hand surgeons using agreed landmarks on plain radiographs.
Particularly disappointing were the paucity of patient‐related quality of life data using validated instruments, and the quality of data on outcomes of personal and social importance to the person with the fracture. Of the included studies, only Harding 2001 reported a case of skin damage, in a patient whose metacarpal brace rubbed on the ulnar border of his hand. Skin necrosis from metacarpal braces has been documented elsewhere (Breddam 1995; Geiger 1989; Harvie 1990; Ros 1996). Not all the studies considered pain to be an important outcome measure. None documented the type or amount of analgesia taken. Furthermore, assessing pain at week six or 12 when the fracture has healed does not appear to be a particularly useful outcome measure. Although average pain was documented, pain in the first week and the number of times the injured area was unintentionally knocked, with resultant severe pain was not. Intuitively, this may be the main benefit of rigid support.
Anand 1999 and Statius Muller 2003 noted that all participants had returned to work at three months but did not record a mean time to return, nor describe the occupational groups. Harding 2001, who found that 34 of 37 participants treated with a metacarpal brace had returned to work by three weeks compared to only 8 of 28 participants treated with neighbour strapping, failed to describe patient occupations.
No included study noted non‐union, malunion or rotational deformity. It is known that non‐union is rare, probably due to the impacted nature of the fracture. Only Kuokkanen 1999 documented time to union.
Some methodological limitations of the included studies warrant mention. Notably, the CONSORT guideline for publishing of RCTs was not followed by any author. Few studies described treatment or control groups in detail and most employed the sealed envelope method of allocation concealment, which is considered sub‐optimal. Blinding of treatment providers was accepted to be impossible, but blinding of outcome assessors, which was possible, was only performed by Kuokkanen 1999 and Statius Muller 2003. No study clearly described the number or reason for patient exclusion prior to randomization, and follow up proved a major handicap in three included studies (Braakman 1998b; Harding 2001; Statius Muller 2003). Patients with Boxer's fractures are known for poor compliance with follow up arrangements (Hall 1987). However, the data should be subject to intention to treat analysis. Of the 163 participants in the three studies mentioned, 15 participants (9%) were lost to follow up and not analysed in the treatment group assigned. Sensitivity analysis of these studies would not have allowed conclusions of particular treatment benefits to have been drawn.
Authors' conclusions
Implications for practice.
This review included no study that documented our primary outcome measure of interest, validated hand function. Therefore, no single treatment regimen can be recommended for all participants. However, certain interventions may offer advantages in outcome measures such as pain reduction or early return to work. 'One size may not fit all'. The informed patient should decide if their personal priority is maximum pain reduction, earliest return to work or other outcome, and subsequently choose the intervention most likely to confer that benefit.
Implications for research.
Fracture of the fifth metacarpal neck remains an exceedingly common injury with no consensus on optimum management. A multi‐centre randomized controlled trial of multiple interventions is warranted. Large patient numbers will be needed to identify real differences between treatment regimes with respect to the incidence of uncommon complications such as non union and clinical rotation. Both intermediate‐term and long‐term (12 to 24 months) follow up would be preferable. Outcome measures should include validated hand function scoring, daily pain scoring on validated scales, mean time of return to work, incidence of complications and the cost of each treatment regime. Both direct and indirect costs should be studied to be able to draw definitive conclusions on cost effectiveness of each intervention. Analgesia taken and occupational categories should be documented. Outcome assessors should be blinded to the treatment provided, and agreement on landmarks and radiographic views used to measure fracture angulation should be agreed a priori.
What's new
| Date | Event | Description |
|---|---|---|
| 13 May 2009 | Amended | No changes ‐ republished to fix technical problem. |
History
Protocol first published: Issue 3, 2001 Review first published: Issue 3, 2005
| Date | Event | Description |
|---|---|---|
| 4 August 2008 | New search has been performed | For the first update, published in Issue 4, 2008, the following changes were made: (1) the search was updated to June 2008, which resulted in the identification of no new studies; (2) the 'Synopsis' was converted to a 'Plain language summary'; (3) methodological quality assessment scores were no longer totalled; (4) some reformatting of the review and completion of one formerly incomplete table. There were no changes made to the conclusions. |
| 10 July 2008 | Amended | Converted to new review format. |
| 16 May 2005 | New citation required and conclusions have changed | First version of the review. |
Acknowledgements
We thank Prof William Gillespie, Prof Rajan Madhok, Dr Janet Wale, Prof Peter Herbison, Ms Leeann Morton, Mr Geoffrey Hooper, Dr Vicki Livingstone, Mr Piet de Boer, and Mrs Lesley Gillespie for helpful comments on the protocol and review. We are grateful to Zimmer Inc, Netherlands for the loan of a laptop to assist with this and other research projects.
We thank Dr Joanne Elliott, Mrs Lindsey Elstub and Dr Helen Handoll for their help with the first update of the review
Appendices
Appendix 1. Search strategy for MEDLINE
| MEDLINE (OVID‐WEB) |
| 1. Metacarpus/ 2. boxer$ fracture$.tw. 3. little finger$.tw. 4. metacarp$.tw. 5. (fifth adj3 finger$).tw. 6. or/1‐5 7. Fractures/ 8. fracture$.tw. 9. or/7‐8 10. and/6,9 11. randomized controlled trial.pt. 12. controlled clinical trial.pt. 13. Randomized Controlled Trials/ 14. Random Allocation/ 15. Double Blind Method/ 16. Single Blind Method/ 17. or/11‐16 18. Animals/ not Humans/ 19. 17 not 18 20. clinical trial.pt. 21. exp Clinical Trials/ 22. (clinic$ adj25 trial$).tw 23. ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).tw. 24. Placebos/ 25. placebo$.tw. 26. random$.tw. 27. Research Design/ 28. or/20‐27 29. 28 not 18 30. 29 not 19 31. or/19,30 32. and/10,31 |
Appendix 2. Search strategy for EMBASE
| EMBASE (OVID‐WEB) |
| 1. Metacarpal Bone Fracture/ 2. boxer$ fracture$.tw. 3. or/1‐2 4. little finger$.tw. 5. metacarp$.tw. 6. (fifth adj3 finger$).tw. 7. or/4‐6 8. Fracture/ 9. fracture$.tw. 10. or/8‐9 11. and/7,10 12. or/3,11 13. exp Randomized Controlled trial/ 14. exp Double Blind Procedure/ 15. exp Single Blind Procedure/ 16. exp Crossover Procedure/ 17. Controlled Study/ 18. or/13‐17 19. ((clinical or controlled or comparative or placebo or prospective$ or randomi#ed) adj3 (trial or study)).tw. 20. (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. 21. ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. 22. (cross?over$ or (cross adj1 over$)).tw. 23. ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. 24. or/19‐23 25. or/18,24 26. limit 25 to human 27. and/12,26 |
Appendix 3. Search strategy for The Cochrane Library
| The Cochrane Library (Wiley InterScience) |
| #1 MeSH descriptor Metacarpal Bones, this term only #2 (boxer* fracture*):ti,ab,kw #3 (little finger*):ti,ab,kw #4 (metacarp*):ti,ab,kw #5 (fifth near3 finger*):ti,ab,kw #6 (#1 OR #2 OR #3 OR #4 OR #5) #7 MeSH descriptor Fractures, Bone explode all trees #8 (fracture*):ti,ab,kw #9 (#7 OR #8) #10 (#6 AND #9) |
Data and analyses
Comparison 1. Functional (taping) vs immobilization (POP splinting with immobilization of MCP and wrist joint).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not fully satisfied at final follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Decreased range of motion | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2.1 At 1 week follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 At 3 to 6 weeks follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 At final follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Loss of grip strength | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 At 3 to 6 weeks follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 At final follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.1. Analysis.
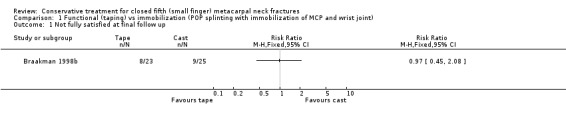
Comparison 1 Functional (taping) vs immobilization (POP splinting with immobilization of MCP and wrist joint), Outcome 1 Not fully satisfied at final follow up.
1.2. Analysis.
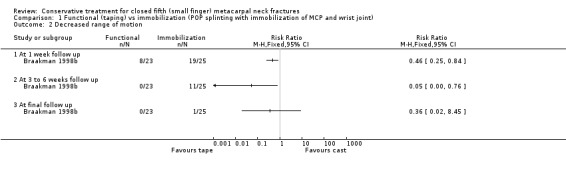
Comparison 1 Functional (taping) vs immobilization (POP splinting with immobilization of MCP and wrist joint), Outcome 2 Decreased range of motion.
1.3. Analysis.
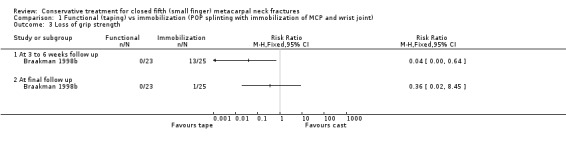
Comparison 1 Functional (taping) vs immobilization (POP splinting with immobilization of MCP and wrist joint), Outcome 3 Loss of grip strength.
Comparison 2. Functional (compression bandage) vs immobilization (POP splinting with immobilization of MCP and wrist joint).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not fully satisfied at final follow up (3 months) | 2 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.23, 2.49] |
| 2 Not satisfied with cosmetic appearance | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Pain | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 At 3 to 6 weeks follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 At final follow up (3 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Decreased range of motion | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 At 3 to 6 weeks follow up | 1 | 35 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.9 [0.34, 2.40] |
| 4.2 At final follow up (3 months) | 2 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.16, 3.50] |
| 5 Not returned to work at follow up | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 At 3 to 6 weeks follow up | 1 | 35 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.05, 11.05] |
| 5.2 At final follow up (3 months) | 2 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6 Radiological non union (3 months) | 1 | 29 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
2.1. Analysis.
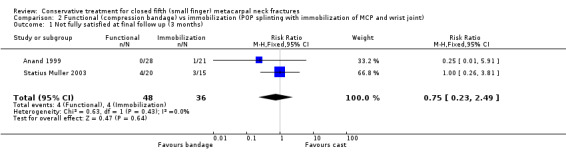
Comparison 2 Functional (compression bandage) vs immobilization (POP splinting with immobilization of MCP and wrist joint), Outcome 1 Not fully satisfied at final follow up (3 months).
2.2. Analysis.
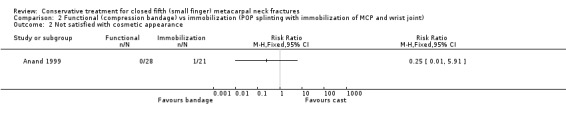
Comparison 2 Functional (compression bandage) vs immobilization (POP splinting with immobilization of MCP and wrist joint), Outcome 2 Not satisfied with cosmetic appearance.
2.3. Analysis.
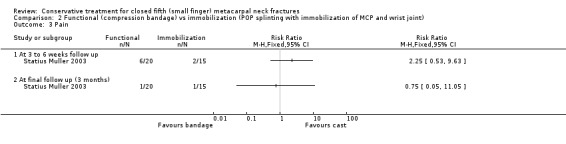
Comparison 2 Functional (compression bandage) vs immobilization (POP splinting with immobilization of MCP and wrist joint), Outcome 3 Pain.
2.4. Analysis.
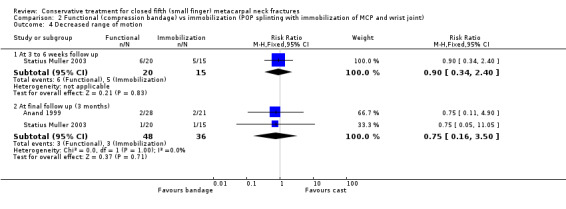
Comparison 2 Functional (compression bandage) vs immobilization (POP splinting with immobilization of MCP and wrist joint), Outcome 4 Decreased range of motion.
2.5. Analysis.
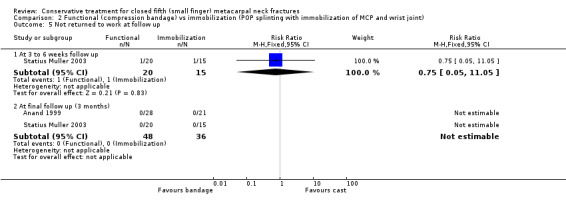
Comparison 2 Functional (compression bandage) vs immobilization (POP splinting with immobilization of MCP and wrist joint), Outcome 5 Not returned to work at follow up.
2.6. Analysis.
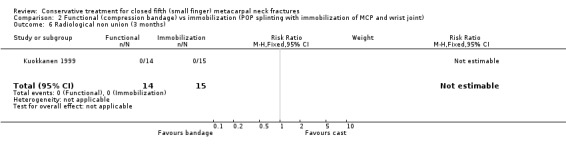
Comparison 2 Functional (compression bandage) vs immobilization (POP splinting with immobilization of MCP and wrist joint), Outcome 6 Radiological non union (3 months).
Comparison 3. Functional (neighbour strapping) vs functional brace (bracing with free movement in MCP and wrist joint).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not fully satisfied at final follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Not satisfied with cosmetic apperance | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Skin damage | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Not returned to work at 3 weeks follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
3.1. Analysis.
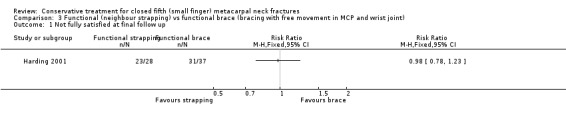
Comparison 3 Functional (neighbour strapping) vs functional brace (bracing with free movement in MCP and wrist joint), Outcome 1 Not fully satisfied at final follow up.
3.2. Analysis.
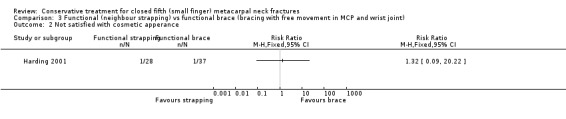
Comparison 3 Functional (neighbour strapping) vs functional brace (bracing with free movement in MCP and wrist joint), Outcome 2 Not satisfied with cosmetic apperance.
3.3. Analysis.
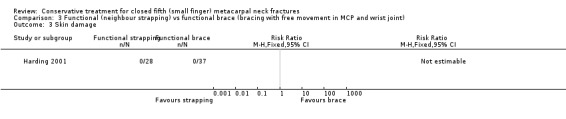
Comparison 3 Functional (neighbour strapping) vs functional brace (bracing with free movement in MCP and wrist joint), Outcome 3 Skin damage.
3.4. Analysis.

Comparison 3 Functional (neighbour strapping) vs functional brace (bracing with free movement in MCP and wrist joint), Outcome 4 Not returned to work at 3 weeks follow up.
Comparison 4. All functional vs all immobilization treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Not fully satisfied at final follow up | 3 | 132 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.46, 1.69] |
| 2 Not satisfied with cosmetic apperance | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Pain | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3.1 At 3 to 6 weeks follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 At final follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Decreased range of motion | 3 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 At 1 week follow up | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.25, 0.84] |
| 4.2 At 3 to 6 weeks follow up | 2 | 83 | Risk Ratio (M‐H, Random, 95% CI) | 0.25 [0.01, 8.36] |
| 4.3 At final follow up (3 to 6 months) | 3 | 132 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.16, 2.60] |
| 5 Loss of grip strength | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5.1 At 3 to 6 weeks follow up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 5.2 At final follow up ( 6 months) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Not returned to work at follow up | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 At 3‐6 weeks follow up | 1 | 35 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.05, 11.05] |
| 6.2 At final follow up | 2 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
4.1. Analysis.
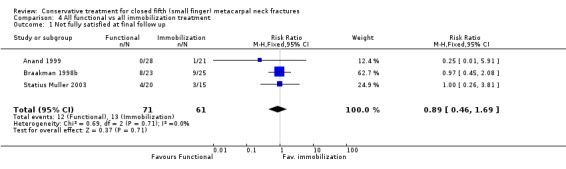
Comparison 4 All functional vs all immobilization treatment, Outcome 1 Not fully satisfied at final follow up.
4.2. Analysis.
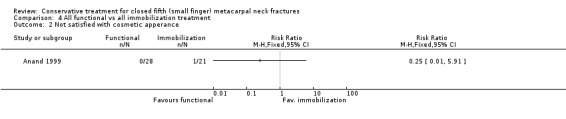
Comparison 4 All functional vs all immobilization treatment, Outcome 2 Not satisfied with cosmetic apperance.
4.3. Analysis.
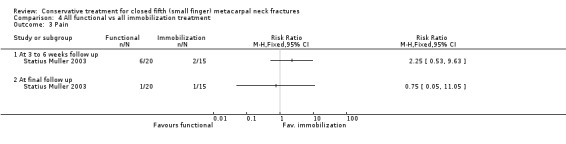
Comparison 4 All functional vs all immobilization treatment, Outcome 3 Pain.
4.4. Analysis.
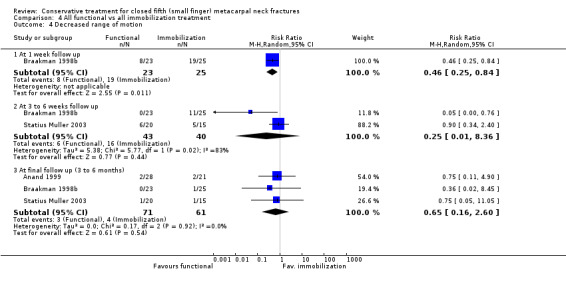
Comparison 4 All functional vs all immobilization treatment, Outcome 4 Decreased range of motion.
4.5. Analysis.
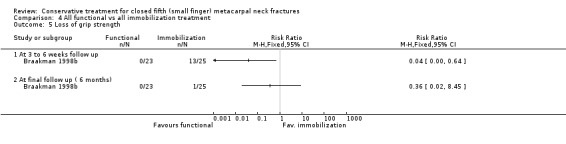
Comparison 4 All functional vs all immobilization treatment, Outcome 5 Loss of grip strength.
4.6. Analysis.
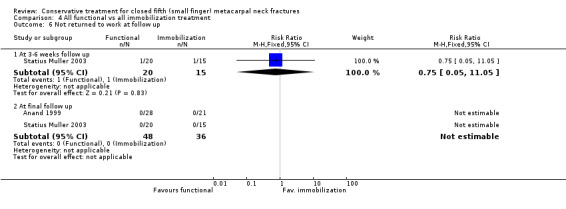
Comparison 4 All functional vs all immobilization treatment, Outcome 6 Not returned to work at follow up.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Anand 1999.
| Methods | Method of randomisation: Medical record number Blinding of outcome assessors: No blinding Length of follow up: Three months |
|
| Participants | 60 patients with fractures of the neck of the fifth metacarpal. | |
| Interventions | (1) Immediate mobilization with a bulky dressing. (2) Immobilization with an ulnar gutter splint for 3 weeks and attempt to reduction. |
|
| Outcomes | Angulation Cosmetic satisfaction Extensor lag Pain Return to pre‐injury status Grip strength | |
| Notes | Randomization based on medical record number | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | High risk | C ‐ Inadequate |
Braakman 1998b.
| Methods | Method of randomisation: No description of method, only states randomised. Blinding of outcome assessors: No blinding Length of follow up: Six months |
|
| Participants | 50 patients with fractures of the fifth metacarpal proximal, shaft and neck. | |
| Interventions | (1) Immediate mobilization with a tape splinting the fourth digit against the fifth, a broad circular strap was supporting the metacarpals. (2) Immobilization with a U shaped ulnar gutter splint with the wrist in 45 degrees dorsiflexion, MCP joints in 90 degrees flexion and IP joint in 0‐10 flexion surrounding the fourth and fifth metacarpal for 4 weeks and attempt to reduction only in patients with rotational deformity, midshaft angulation exceeding 20 degrees, and subcapital angulation exceeding 50 degrees. |
|
| Outcomes | Volar angulation ROM Grip strength | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Harding 2001.
| Methods | Method of randomisation: Sealed envelopes Blinding of outcome assessors: Blinded Length of follow up: Three weeks |
|
| Participants | 73 patients with minimally angulated (< 40 degrees) closed fractures of the little finger metacarpal neck with no rotational deformity or associated injury. | |
| Interventions | (1) Neighbour strapping with early active mobilization of the MCP and IP joints for 3 weeks. (2) Metacarpal brace heat moulded to the contours of the patient's hand while the metacarpal head was supported and held in place by a bandage. Early active mobilization of the MCP and IP joints for 3 weeks. |
|
| Outcomes | Pain 0‐3 scale Malunion Volar angulation Rotational deformity ROM Patient satisfaction Skin damage Time to work | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Kuokkanen 1999.
| Methods | Method of randomisation: Sealed envelopes Blinding of outcome assessors: No blinding Length of follow up: Three months |
|
| Participants | 29 patients with closed subcapital fractures of the fifth metacarpal bone not exceeding more than 70 degrees of angulation or deviation or rotation deformity. | |
| Interventions | (1) Immediate mobilization by an elastic bandage 5 cm wide applied circumferentially and with slight compression from the MCP level to 10 cm above the wrist for one week. (2) Immobilization after reposition and splinting as described by O'Brien. MCP joint was immobilized in 60 degrees flexion and the splint reached to the level of the PIP joint leaving the joint free for movement for 4 weeks. |
|
| Outcomes | Non‐union Volar angulation ROM Grip strength Time to union Skin damage | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Statius Muller 2003.
| Methods | Method of randomisation: Sealed envelopes Blinding of outcome assessors: Blinded Length of follow up: Three months |
|
| Participants | 40 patients with subcapital fractures of the fifth metacarpal, except those angulated more than 70 degrees, older than 3 days, re‐fractures, pathologic fractures and fractures with a rotation deformity. | |
| Interventions | (1) Immediate mobilization with a pressure bandage applied to splint the fourth and fifth metacarpals together with a broad circular bandage from the metacarpal level to 10 cm above the wrist. The patients were encouraged to move the fingers immediately and they removed the bandages after one week. (2) Immobilization in an ulnar gutter cast applied with the wrist in 45 dorsiflexion and the metacarpal joints in 90 flexion. The cast was U‐shaped and surrounded the fourth and fifth metacarpals for 3 weeks, no reposition. |
|
| Outcomes | Pain ROM Patient satisfaction Volar angulation | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
IP: inter‐phalangeal MCP: metacarpo‐phalangeal ROM: range of motion VAS: visual analogue score
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Cohen 2001 | RCT. Fractures of the base of the fifth metacarpal and distal radius fractures. No separate data analysis was possible for the fifth metacarpal fractures. |
| De Kleuver 1996 | RCT. In this abstract of a Dutch orthopaedic meeting insufficient data were given to be interpreted. |
| Garramone 1996 | RCT. In this abstract a short arm cast was compared to volar splint. Insufficient data were given on the exact treatment modalities. Unclear if free motion in MCP was possible in one of the treatment groups. |
| Hansen 1998 | RCT. The type of participants did not meet the inclusion criteria. Described fourth and fifth metacarpal fractures. No separate data analysis was possible for the fifth metacarpal fractures. |
| Hutchison 1996 | This was a study on the ability to make a cast by surgical trainees. Not an RCT. |
| Konradsen 1990 | RCT. The type of participants did not meet the inclusion criteria. Described fractures of the second to fifth metacarpal. No separate data analysis was possible for the fifth metacarpal fractures. |
| McMahon 1994 | RCT. The type of participants did not meet the inclusion criteria. Patients with metacarpal shaft fractures were included, not subcapital fractures. No specific data were given on which metacarpal was fractured. |
| Randall 1992 | RCT. The type of participants did not meet the inclusion criteria. This study included fractures of the base, shaft and neck of the metacarpal bone. All hands had to be immobilized for at least one week. |
| Sorensen 1993 | RCT. The type of participants did not meet the inclusion criteria. Described fractures of the second to fifth metacarpal. No separate data were given on fifth metacarpal. |
MCP: metacarpal phalangeal joint RCT: randomized controlled trial
Contributions of authors
Rudolf Poolman is the guarantor of the review. Conceiving the review: Poolman, Steller, Statius Muller. Designing the review: Poolman. Coordinating the review: Poolman. Data collection for the review: Poolman, Goslings, Lee. Screening search results: Poolman. Organising retrieval of papers: Poolman. Screening retrieved papers against inclusion criteria: Poolman, Goslings, Lee. Appraising quality of papers: Poolman, Goslings, Lee. Abstracting data from papers: Poolman, Lee. Writing to authors of papers for additional information: Poolman. Obtaining and screening data on unpublished studies: Poolman. Entering data into RevMan: Poolman, Struijs. Analysis of data: Struijs, Poolman. Interpretation of data: Poolman, Struijs, Lee. Providing a methodological perspective: Struijs. Providing a clinical perspective: Steller, Goslings, Poolman. Providing a policy perspective: Steller, Goslings, Poolman. Writing the review: Poolman, Lee, Struijs, Goslings, Statius Muller, Steller. Providing general advice on the review: Steller, Goslings. Performing previous work that was the foundation of current study: Statius Muller, Poolman, Steller.
Sources of support
Internal sources
Academic Medical Center, Amsterdam, Netherlands.
St Lucas Andreas Ziekenhuis, Amsterdam, Netherlands.
Ziekenhuis Hilversum, Hilversum, Netherlands.
External sources
No sources of support supplied
Declarations of interest
Two authors, RW Poolman and M Statius Muller, were investigators for one included study (Statius Muller 2003). Investigators did not carry out quality assessment on their own study. No other conflicts are declared.
Edited (no change to conclusions)
References
References to studies included in this review
Anand 1999 {published and unpublished data}
- Anand N, Tannoury TY, Mey S, Weinstein RN. Boxer's fracture: a prospective randomized study comparing immediate mobilization to immobilization [abstract]. American Academy of Orthopaedic Surgeons Annual Meeting; 1999 Feb 4‐8; Anaheim (CA) http://www.aaos.org/wordhtml/anmeet99/sciprog/010.htm (accessed 27/06/02).
Braakman 1998b {published data only}
- Braakman M, Oderwald EE. Faster recovery of metacarpal 5‐fractures using functional taping [abstract]. Nederlands Tijdschrift voor Orthopaedie 1997;4:24. [Google Scholar]
- Braakman M, Oderwald EE, Haentjens MH. Functional taping of fractures of the 5th metacarpal results in a quicker recovery. Injury 1998;29(1):5‐9. [DOI] [PubMed] [Google Scholar]
- Braakman M, Oderwald EE, Haentjens MHHJ. More rapid healing of fractures of the 5th metacarpal bone due to functional taping [abstract]. Acta Orthopaedica Scandinavica ‐ Supplementum 1997;274:26. [Google Scholar]
Harding 2001 {published data only}
- Harding IJ, Parry D, Barrington RL. The use of a moulded metacarpal brace versus neighbour strapping for fractures of the little finger metacarpal neck. Journal of Hand Surgery ‐ British Volume 2001;26(3):261‐3. [DOI] [PubMed] [Google Scholar]
Kuokkanen 1999 {published data only}
- Kuokkanen HO, Mulari‐Keranen SK, Niskanen RO, Haapala JK, Korkala OL. Treatment of subcapital fractures of the fifth metacarpal bone: A prospective randomised comparison between functional treatment and reposition and splinting. Scandinavian Journal of Plastic & Reconstructive Surgery & Hand Surgery 1999;33(3):315‐7. [DOI] [PubMed] [Google Scholar]
Statius Muller 2003 {published data only}
- Statius Muller MG, Poolman RW, Hoogstraten MJ, Stellar EP. The boxers' fracture: a prospective randomised comparison between functional and immobilization treatment [abstract]. Dutch Orthopaedic Society; 2003 January 9‐10; Nijmegen (Netherlands) http://home.pi.se/actaorthopscand/Pages/framabst.html (accessed 07/04/03). (accessed 07 April 2003).
- Statius Muller MG, Poolman RW, Hoogstraten MJ, Steller EP. Immediate mobilization gives good results in boxer's fractures with volar angulation up to 70 degrees: a prospective randomized trial comparing immediate mobilization with cast immobilization. Archives of Orthopaedic and Trauma Surgery 2003;123(10):534‐7. [PMID: 14639483 [PubMed ‐ indexed for MEDLINE]] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Cohen 2001 {published data only}
- Cohen AP, Shaw DL. Focused rigidity casting: a prospective randomised study. Journal of the Royal College of Surgeons of Edinburgh 2001;46(5):265‐70. [PubMed] [Google Scholar]
De Kleuver 1996 {published data only}
- Kleuver M, Winters HAH. Treatment of metacarpal fractures with a functional three‐point brace [abstract]. Acta Orthopaedica Scandinavica ‐ Supplementum 1996;267:50‐1. [Google Scholar]
- Kleuver M, Winters HAH. Treatment of metacarpal fractures with a functional three‐point brace [abstract]. Nederlands voor Orthopaedie 1995;2:120. [Google Scholar]
Garramone 1996 {published data only}
- Garramone JA. A functional analysis of short arm cast vs volar splint immobilization in the treatment of small finger metacarpal neck fractures [abstract]. Orthopaedic Transactions 1996;20(4):910. [Google Scholar]
- Garramone JA. A functional analysis of short arm cast vs. volar splint immobilisation in the treatment of small finger meta‐carpal neck fractures [abstract]. Orthopaedic Transactions 1997;21(1):320‐1. [Google Scholar]
- Garramone JA. A functional analysis of short arm cast vs. volar splint immobilisation in the treatment of small finger meta‐carpal neck fractures [abstract]. Orthopaedic Transactions 1998;22(1):175. [Google Scholar]
- Garramone JA. A functional analysis of short arm cast vs. volar splint immobilisation in the treatment of small finger meta‐carpal neck fractures [abstract]. Orthopaedic Transactions 1998;22(4):1304. [Google Scholar]
- Garramone JA. A functional analysis of short arm cast vs. volar splint immobilization in the treatment of small finger metacarpal neck fractures [abstract]. Orthopaedic Transactions 1996;20(4):880. [Google Scholar]
Hansen 1998 {published data only}
- Hansen PB, Hansen TB. The treatment of fractures of the ring and little metacarpal necks. A prospective randomized study of three different types of treatment. Journal of Hand Surgery ‐ British Volume 1998;23(2):245‐7. [DOI] [PubMed] [Google Scholar]
- Hansen PB, Hansen TB. The treatment of subcapital fractures of the fourth and fifth metacarpals ‐ a prospective randomised study of three different types of immobilisation [abstract]. Acta Orthopaedica Scandinavica ‐ Supplementum 1997;274:31. [Google Scholar]
Hutchison 1996 {published data only}
- Hutchison CR, Brown M, Regher G, Backstein D, Murnaghan J, Reznick R. Improving the technical performance of our surgical trainees [abstract]. Orthopaedic Transactions 1996;20(4):999. [Google Scholar]
Konradsen 1990 {published data only}
- Konradsen L, Nielsen PT, Albrecht Beste E. Functional treatment of metacarpal fractures 100 randomized cases with or without fixation. Acta Orthopaedica Scandinavica 1990;61(6):531‐4. [DOI] [PubMed] [Google Scholar]
McMahon 1994 {published data only}
- McMahon PJ, Woods DA, Burge PD. Initial treatment of closed metacarpal fractures. A controlled comparison of compression glove and splintage. Journal of Hand Surgery ‐ British Volume 1994;19(5):597‐600. [DOI] [PubMed] [Google Scholar]
Randall 1992 {published data only}
- Randall T, Poutney L, Harris BA. Effects of joint mobilization on joint stiffness and active motion of the metacarpo‐phalangeal joint. Journal of Orthopaedic and Sports Physical Therapy 1992;16:30‐6. [DOI] [PubMed] [Google Scholar]
Sorensen 1993 {published data only}
- Sorensen JS, Freund KG, Kejla G. Functional fracture bracing in metacarpal fractures: the Galveston metacarpal brace versus a plaster‐of‐Paris bandage in a prospective study. Journal of Hand Therapy 1993;6(4):263‐5. [DOI] [PubMed] [Google Scholar]
Additional references
Abdon 1984
- Abdon P, Muhlow A, Stigsson L, Thorngren KG, Werner CO, Westman L. Subcapital fractures of the fifth metacarpal bones. Archives of Orthopaedic & Traumatic Surgery 1984;103(4):231‐4. [DOI] [PubMed] [Google Scholar]
Ali 1999
- Ali A, Hamman J, Mass DP. The biomechanical effects of angulated boxer's fractures. Journal of Hand Surgery ‐ American Volume 1999;24(4):835‐44. [DOI] [PubMed] [Google Scholar]
Braakman 1996
- Braakman M. Normal radiographic angulation in the 4th and 5th metacarpal: a reference guide. European Journal of Radiology 1996;22(1):38‐41. [DOI] [PubMed] [Google Scholar]
Braakman 1998a
- Braakman M, Oderwald EE, Haentjens MH. Functional taping of fractures of the 5th metacarpal results in a quicker recovery. Injury 1998;29(1):5‐9. [DOI] [PubMed] [Google Scholar]
Breddam 1995
- Breddam M, Hansen TB. Subcapital fractures of the fourth and fifth metacarpals treated without splinting and reposition. Scandinavian Journal of Plastic & Reconstructive Surgery & Hand Surgery 1995;29(3):269‐70. [DOI] [PubMed] [Google Scholar]
Ford 1989
- Ford DJ, Ali MS, Steel WM. Fractures of the fifth metacarpal neck: is reduction or immobilisation necessary?. Journal of Hand Surgery ‐ British Volume 1989;14(2):165‐7. [DOI] [PubMed] [Google Scholar]
Geiger 1989
- Geiger KR, Karpan RR. Necrosis of the skin over the metacarpal as a result of functional fracture‐bracing. A report of three cases. Journal of Bone and Joint Surgery ‐ British Volume 1989;71(8):1199‐202. [PubMed] [Google Scholar]
Greer 1999
- Greer SE, Williams JM. Boxer's fracture: an indicator of intentional and recurrent injury. American Journal of Emergency Medicine 1999;17(4):357‐60. [DOI] [PubMed] [Google Scholar]
Hall 1987
- Hall Jr RF. Treatment of metacarpal and phalangeal fractures in noncompliant patients. Clinical Orthopaedics and Related Research 1987;(214):31‐6. [PubMed] [Google Scholar]
Hansen 1998a
- Hansen PB, Hansen TB. The treatment of fractures of the ring and little metacarpal necks. A prospective randomized study of three different types of treatment. Journal of Hand Surgery ‐ British Volume 1998;23(2):245‐7. [DOI] [PubMed] [Google Scholar]
Harvie 1990
- Harvie KW. Necrosis of the skin over the metacarpal as a result of functional fracture‐bracing. Journal of Bone and Joint Surgery ‐ American Volume 1990;72(7):1114‐5. [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2006
- Higgins JPT, Green S, editors. Highly sensitive search strategies for identifying reports of randomized controlled trials in MEDLINE. Cochrane Handbook for Systematic Reviews of Interventions 4.2.6 [updated September 2006]; Appendix 5b. www.cochrane.org/resources/handbook/hbook.htm (accessed 01 May 2007).
Hunter 1970
- Hunter JM, Cowen M. Fifth metacarpal fractures in a compensation clinic population. A report on one hundred and thirty‐three cases. Journal of Bone and Joint Surgery ‐ American Volume 1970;52(6):1159‐65. [PubMed] [Google Scholar]
Leung 2002
- Leung YL, Beredjiklian PK, Monaghan BA, Bozentka DJ. Radiographic assessment of small finger metacarpal neck fractures. Journal of Hand Surgery ‐ American Version 2002;27(3):443‐8. [DOI] [PubMed] [Google Scholar]
Ros 1996
- Ros NOJ, Mora F, Canovas A. Orthopaedic functional treatment of fractures of the fifth metacarpal [Tratamiento ortopedico funcional de las fracturas del tercio distal del quinto metacarpiano]. Revista de Ortopedia y Traumatologia 1996;41(1):64‐72. [Google Scholar]
Theeuwen 1991
- Theewen GA, Lemmens JA, Niekerk JL. Conservative treatment of boxer's fracture: a retrospective analysis. Injury 1991;22(5):394‐6. [DOI] [PubMed] [Google Scholar]


