Purpose of review
This article reviews the literature on COVID-19 related anosmia, focusing on the epidemiology, pathophysiology recovery rates, current available treatment options, and research regarding novel treatments.
Recent findings
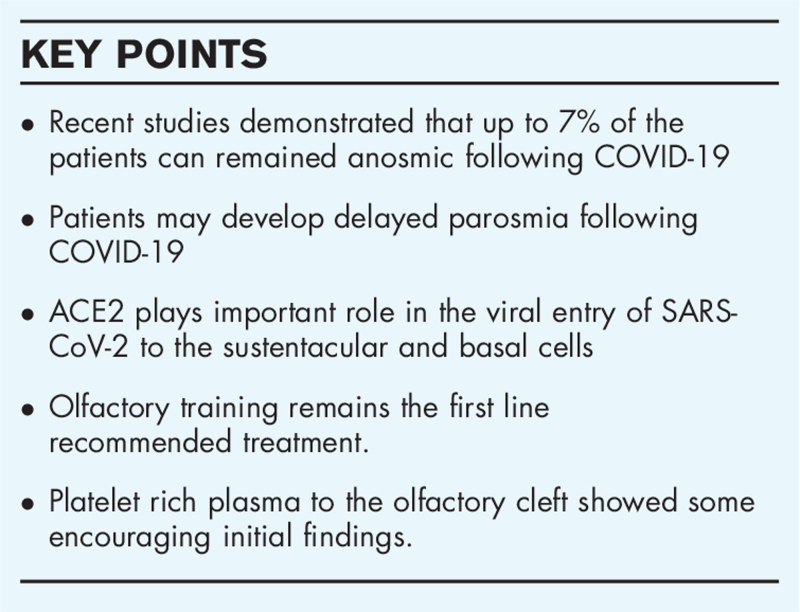
Loss of sense of smell is one of the most prevalent symptoms reported by patients after COVID-19 infection. Even though there is a high self-reported recovery rate, recent studies have demonstrated that up to 7% of the patients remain anosmic more than 12 months after onset, leaving millions worldwide with severe olfactory dysfunction. Olfactory training remains the first line recommended treatment. Given the paucity of effective medical treatments options researchers are exploring novel therapeutic options.
Summary
Olfactory dysfunction remains a significant and persistent legacy of the COVID-19 pandemic, but heightened awareness may stimulate research that leads to the development of much-needed treatment options.
Keywords: anosmia, COVID-19, olfactory loss
INTRODUCTION
Postviral anosmia is the leading cause of adult olfactory dysfunction, accounting for up to 40% of all cases [1,2] It was therefore perhaps unsurprising to see an increase at the onset of the SARS-CoV-2 pandemic. However, the high prevalence of olfactory dysfunction and importance as a diagnostic marker has shone a spotlight on what has hitherto been a largely neglected sense. Here, we aim to review olfactory dysfunction that occurs as a consequence of COVID-19, the underlying pathophysiology, recovery rates and potential therapeutic options
Box 1.
no caption available
PREVALENCE AND PRESENTATION OF OLFACTORY LOSS IN COVID-19
After early newspaper reports in Germany, Korea and Iran, olfactory loss emerged as a potential marker of COVID-19 in March 2020, generating intense media interest [3]. A large body of evidence now demonstrates loss of sense of smell to be one of the most common symptoms of COVID-19 infection; a meta-analysis of 3563 patients published in May 2020 found the mean prevalence of self-reported loss to be 47% (95% CI: 36%–59%) in, ranging from 11% to 84% in included case series [4▪].
Self-reporting of loss of smell has been shown to underestimate the true prevalence of OD when evaluated with psychophysical tests, as demonstrated by Moein et al. in 60 hospitalised participants; 98% had some degree of OD on formal testing, whereas only 35% of participants self-reported loss of taste or smell [5▪]. In contrast, evaluation with psychophysical tests alone could overestimate prevalence of residual COVID-19-related olfactory loss by including all those subjects who were unaware of having premorbid olfactory dysfunction [6▪].
Loss of smell may be the only presenting feature for patients with COVID-19 [3];preceding other symptoms in 20% (95% CI: 13%–29%) of reported cases included in a systematic review from May 2020, and presenting concomitantly with other g symptoms in a further 28% (95% CI: 22%–36%) of cases [4▪]. A French study [7▪] of 114 patients with confirmed COVID-19 infection showed that 47% of the patients developed loss of sense of smell but less than 5% of the patients had other sinonasal symptoms such as rhinorrhoea and nasal congestion. Other studies [8] have also found that patients with COVID-19 related anosmia do not report rhinitic symptoms typically associated with a common cold.
It has been postulated that olfactory dysfunction may have prognostic value in predicting the severity of COVID-19. An early study by Yan et al.[9▪] suggested that olfactory loss associated with milder disease not requiring admission; admitted patients were significantly less likely to report anosmia/hyposmia (26.9% vs 66.7%, P < 0.001) [9▪]. This aligns with systematic reviews that have found the prevalence of self-reported smell loss was highly dependent on setting; in hospitalised patients the overall prevalence was 31% but rising to 67% in mild-to-moderate symptomatic home-isolated patients [4▪]. In contrast, a prospective study of 106 patients [10▪] found no correlation between olfactory function in the first week of infection and disease severity. In a different study [11▪], the same group demonstrated no correlation between viral load and severity of olfactory loss. In a third prospective study [12▪] the same group again failed to demonstrate any significant statistical correlation between baseline olfactory loss and the severity of chest CT findings. The authors speculate that short lived olfactory dysfunction may simply be overlooked in more severe disease due to over-riding respiratory symptoms and associated anorexia leading to reduced dietary intake and they suggest that any association between OD and a milder course is an artefact. Similar findings were reported by an independent research group in Spain [13]
One study has suggested that anosmia may be more frequent among women (72.4%; 95% CI, 62.8%–80.7%) than among men (55.7%; 95% CI, 45.2%–65.8%; P = 0.02) [14]. A systematic review suggested a lower reporting of OD with increasing age [15], in keeping with age dependent reduced expression of Angiotensin-converting enzyme 2. (ACE2) receptor in the olfactory epithelium [16]. However, this may also reflect the increasing background prevalence of underlying OD. There also appears to be significant differences in the prevalence of olfactory dysfunction with different viral variants, with widely varying geographical rates being reported [17▪], but also variable rates at different time points in the pandemic [18▪].
PATHOPHYSIOLOGICAL MECHANISMS OF OLFACTORY DYSFUNCTION IN COVID-19
Despite a growing body of evidence, the underlying pathophysiological mechanism of anosmia in COVID-19 remains uncertain. Proposed mechanisms include conductive loss due to olfactory cleft oedema, injury to the olfactory epithelium (OE) and injury to the olfactory bulb (OB) itself.
Localised obstruction caused by oedema within the olfactory cleft may contribute to early OD restricting the delivery of odorants to the OE, although nasal congestion is less frequently reported in COVID-19 compared to other endemic coronaviruses [19,20]. Although one study [21▪] found a high prevalence of complete obstruction of the olfactory cleft in MRI scans performed within 15 days of onset of COVID-19 related OD), other radiological studies of patients with more persistent loss [22▪] have found this to be an uncommon finding.
Olfactory epithelial injury has previously been demonstrated in cases of postviral olfactory loss [23]. Postmortem studies of COVID-19 patients reporting anosmia showed focal atrophy of the OE, leukocytic infiltration of the lamina propria and evidence of axonal damage in the olfactory nerve fibres [24]. Animal models of SARS-CoV-2 [25▪] demonstrated massive destruction of olfactory epithelium after nasal inoculation and loss of cilia; evidence of recovery was observed as early as day 4 although incomplete by day 14 [26▪].
ACE2 receptors, important for viral entry of SARS-CoV-2, are expressed by the sustentacular supporting and basal cells of the OE [27▪,28▪]. Damage to these cells may induce reduced sensitivity and loss of cilia from the ORNs, resulting in OD even though the ORNs do not themselves express ACE2 or become directly infected. This hypothesis is consistent with the pattern of early recovery as direct ORN injury would require a significantly longer period to achieve resolution of OD. More recent in vivo studies using mucosa brush sampling demonstrate both infected mature sensory neurones as well as sustentacular cells, confirming entry into the ORNs themselves, with evidence of apoptosis of both cell groups [26▪].
Some of the most recent studies propose an inflammatory-mediated loss of odorant receptor expression on otherwise intact ORNs; this is supported by animal models, and in olfactory epithelial biopsies harvested from COVID-19 patients postmortem. A study of SARS-CoV-2 in golden Syrian hamsters has demonstrated that the local immune response increases macrophage expression in the OE and lamina propria, which may prevent recovery of the OE and restoration of the ORNs [25▪]. In an in vivo study of patients with persistent loss, viral persistence has been demonstrated in the olfactory epithelium with associated on going inflammation, elevated IL6 and apoptosis.[26▪]. The regenerative capacity of basal stem cells has been shown to be significantly impaired by inflammation and this mechanism may therefore account for prolonged olfactory dysfunction [29]. Anecdotal reports of enhanced recovery after vaccination perhaps reflect more effective viral clearance [30▪].
Propagation of viruses by retrograde axonal transport to the OB and to the CNS is well described [31,32]. Animal models of OC43 coronavirus infection have demonstrated viral particles within the OB 3 days after inoculation and the cortex by day 7 [33]. ACE2 transgenic mice inoculated with SARS-CoV-1 similarly supported a route of viral entry through the OB with rapid invasion of the CNS [34]; similarly high viral RNA loads were found along the entire routine form the olfactory endothelium to the bulb [26▪]. Several case reports documented hyperintensity in the olfactory bulb which resolved on repeat imaging one month later with subsequent loss of volume of the OB [35,36,37], whereas one neuroimaging cohort reported signal abnormalities of the OB in 19% of cases [38]. One patient with persistent COVID-19 induced OD had MRI imaging prior to COVID-19 infection which provided baseline volumes and confirmed significant atrophy of their OB in images performed 2 months after onset [39]. PET imaging found hypometabolism in the gyrus rectus in 2 patients with persistent COVID-19 OD [40]. Although these studies have reported evidence of neurotropism, atrophy and hypometabolism, this may be an indirect consequence of loss of function at the level of the OE and they do not provide direct proof of retrograde transport of SARS-CoV-2 into the OB.
Progress in our understanding of the mechanism of olfactory loss will help to drive therapeutic options and therefore further research in this area is essential.
RECOVERY OF OLFACTORY LOSS AFTER COVID-19
Many studies have now been performed to evaluate recovery rates, and risk factors for persistence, using questionnaires or objective olfactory tests. Early reports suggested very high rates of rapid recovery [41] with many self-reporting complete recovery within a mean duration of olfactory loss of 10 days [42]. The recovery rates in self-reported studies [43,44▪,45,46▪] varies from 31.7% to 89%.
However, it has become clear that self-reporting likely over-estimates the degree of recovery (in contrast to under-estimating the initial prevalence of olfactory loss.) In a study performed by Boscolo-Rizzo et al.[46▪] a significant mismatch was found between self-reported olfactory function and psychophysical evaluation; interestingly, of 112 patients with self-reported normal sense of smell at 6 months only 41% revealed normosmia with UPSIT testing.
A number of studies have now published outcomes at 6 months and beyond. Leedman et al.[47▪] report that in a consecutive series of patients with proven COVID-19, 64% were normosmic at 6 months, 3.5% were anosmic and the remainder hyposmic, based on evaluation with UPSIT tests. Boscolo-Rizzo [48▪] has undertaken a case-controled study, with mean follow-up of 401 days after infection; 46% and 10% of cases and controls were found to have olfactory dysfunction, with 7% of COVID-19 cases being anosmic. Given the high numbers of people affected by COVID-19, even with the best-reported recovery rates, a significant number worldwide will be left with severe olfactory dysfunction.
QUALITATIVE OLFACTORY DYSFUNCTION – PAROSMIA AND PHANTOSMIA
Many patients report the development of parosmia, typically after a period of 2 to 3 months and often following a period of apparent recovery [49▪]. Some patients may develop parosmia even without reporting the initial loss of sense of smell. The ‘COVID smell’ is generally unpleasant, with a burnt of chemical like odour. Common triggers are coffee, onion, garlic, meat and citrus along with toiletries such as toothpaste [50▪].
The underlying mechanism of parosmia and phantosmia remains unclear. One theory is that a decreased number of functioning olfactory neurones leads to incomplete odorant characterization [51], supported by findings of reduced numbers of ORNs and a predominance of immature neurones in histopathological examination of the olfactory epithelium. There has also been a proposal that parosmia may reflect ephaptic firing in demyelinated neurones [52] or a central mechanism, with evidence of abnormal activity on positron emission tomography or functional MRI [51].
There is a near absence of evidence to inform treatment recommendations for qualitative loss, although anecdotal evidence exists for the use of anticonvulsants, such as gabapentin to suppress distortions in severe cases [51].
CURRENT THERAPEUTIC OPTIONS FOR ANOSMIA AND HYPOSMIA FOLLOWING COVID-19
There are a paucity of established interventions for postviral olfactory dysfunction, and although a number of trials are ongoing, there is currently very little evidence to inform treatment choices specifically in COVID-19 related olfactory dysfunction. A living systematic review [53▪] has included only one eligible RCT study but identified 8 ongoing registered randomised trials where results are currently unavailable.
The study that was included [54] provides weak evidence regarding the effect of the intranasal steroids (INCS) and oral steroids (OCS) compared to no intervention, administered in a small group of patients 30 days after onset, with olfactory scores measured at baseline, 20 and 40 days. 5 out of 9 participants in the active treatment group achieved normosmia, compared to no control arm participants. Larger numbers, longer follow-up and further studies to look at the individual components are required before strong recommendations can be made.
In a systematic review published in 2019, it was concluded that topical steroid sprays do not improve olfactory dysfunction in nonchronic rhinosinusitis-related olfactory loss [55]. In constrast, there is one study showing benefit of budesonide irrigation combined with olfactory training, with 44% showing improvement in the active arm compared with 27% using olfactory training (OT) [56]. Given the low risk of harm from topical steroids, steroid irrigations could be considered for patients with persistent OD after COVID-19.
In one systematic review looking specifically at the use of OCS in PVOL [57], the authors note that placebo arms usually achieve a similar level of benefit as oral steroids, but conclude that Level 4 evidence supported benefit from use. A more recent review looking at all non-CRS aetiologies concludes that there is weak evidence supporting use [55]. Guidelines published to support treatment decisions in COVID-19 olfactory loss [58▪] suggest that oral steroids are an option in patients with loss persisting beyond 28 days. However, OCS are associated with a high rate of adverse events; it is clear that caution is required and given the high early recovery, systemic corticosteroids are not indicated in the first few weeks after onset in order to avoid overtreatment of those who will recover spontaneously. However, recovery plateaus after 30 days and this would seem an optimal time to discuss potential risks and benefits in those with persistent loss who seek treatment.
Current guidance on management with other interventions is therefore largely extrapolated from trials in postviral or idiopathic loss.
There is evidence to support that olfactory training improves olfactory function in patients with PVOL. A meta-analysis in 2016 [59] including all aetiologies of OD concluded that olfactory training achieved statistically significant improvement in discrimination and identification but not threshold, although subgroup analysis for patients with PVOL reduced level of confidence. A meta-analysis in 2017 [60] included 6 studies and 455 patients with PVOL., reporting that identification, discrimination and odour threshold improved significantly. A prospective single-blinded study published in 2017 [61] after the SRs, included 70 patients with PVOL. Patients were followed for 5 months. 45% of patients with PVOL achieved a significant and clinically meaningful improvement in TDI. There is evidence that longer training, change in odors every 12 weeks and higher odorant concentration yields better outcomes. Most included studies lacked control groups, and therefore spontaneous recovery contributing to benefit shown cannot be excluded. However, given the very low risk of harm, all guidelines recommend that patients should undertake olfactory training. Patients should be directed towards patient groups such as AbScent (AbSent.org) and Fifth Sense (www.Fifthsense.co.uk) to provide further support, information and instructions on performing OT.
There is limited nonrandomised evidence that considers other treatments, applied in a variety if underlying aetiologies in olfactory loss, including topical Vitamin A, Omega-3 supplements, Alpha-lipoic acid, theophylline and sodium citrate but these require further evaluation before recommendations on use can be made. Certainly, the COVID-19 pandemic has led to heighted awareness of the impact of olfactory loss, and stimulated research into new treatments. Guidelines and systematic reviews will need to be updated regularly to capture new evidence.
POTENTIAL FUTURE THERAPEUTIC APPROACHES TO ANOSMIA
In the absence of spontaneous recovery of olfactory function, what more can be done?
Recognising that stem cells activation may be suppressed, stimulating these cells may promote recovery. Platelet-rich plasma (PRP) is known to have anti-inflammatory and pro-regenerative properties, which include upregulation of growth factors including transforming growth factor, vascular endothelial growth factor, epidermal growth factor, and insulin-like growth factor, and may neurodegeneration. A small pilot study [62▪] examined the effectiveness of PRP injection into the olfactory cleft in seven patients. Results were recorded on the 1st and the 3rd month using Sniffin’ Sticks; two patients with anosmia have no improvement, five patients with hyposmia showed improvement. A trial in COVID-19 patients is underway and results are eagerly awaited.
If stem cells are irreversibly damaged by disease, can they be transplanted into the OE? In 2009 a team undertook mucosal transplants from the olfactory cleft of transgenic mice with an 83% 30-day survival rate in the olfactory bulb (83%, 5 out of 6 grafts). histological examination demonstrated the development of dendritic processes similar to those seen from olfactory sensory [63]. A more recent study in knock-out mice where genetically induced hyposmia was improved after infusion of purified tissue-specific stem cells intranasally. Engraftment-derived olfactory neuron clusters were confirmed throughout the OE (≥5 clusters/section, n = 6 mice) and functional improvements were measured via electrophysiology and behavioural assay 3 weeks after the infusion [64].
Finally, if a functioning olfactory epithelium cannot be restored can the olfactory bulb be directly stimulated? A team identified the tonotopic function of the olfactory bulb in rats in 2016. They obtained localized negative evoked potentials deep within the olfactory bulb after stimulating the olfactory bulb with surface electrodes in different positions and confirmed that different odors produced specific spatial response patterns; this tonotopic function has been successfully used in cochlear implants and may help to develop olfactory implants [65]. Subsequently, a novel pilot in 5 patients attempted to stimulate the olfactory bulb, whilst patients were awake [66]. A graded stimulation was administered to the lateral lamella of the cribriform plate and cortical evoked potentials were recorded simultaneously in patients with previous ethmoidectomy and normal sense of smell. Three out of five patients reported having perception of smell, but the experiment failed to record olfactory cleft evoked potentials to support subjective findings.
Much further work is required to develop effective treatment strategies but COVID-19 may facilitate future research by enhanced access to funding.
CONCLUSIONS
As the cumulative number of patients infected by SARS-COV-2 surpasses 250 million worldwide, as many as 10 million people may have long-lasting anosmia. The COVID-19 pandemic has exposed decades of underfunding of research and neglect of our one of our senses, with limited availability of diagnostic testing and few therapeutic options. For those suffering persistent loss, the importance of sense of smell has never been more apparent, but the heightened awareness of the impact of olfactory dysfunction will surely pave the way for major advances in this field in years to come
Acknowledgements
None.
Financial support and sponsorship
No funding has been received for this article from any source.
There was no financial support to this work.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Welge-Lüssen A, Wolfensberger M. Olfactory disorders following upper respiratory tract infections [Internet]. Adv Oto-Rhino-Laryngol Adv Otorhinolaryngol 2006; 63:125–132. [DOI] [PubMed] [Google Scholar]
- 2.Seiden A. Postviral olfactory loss. Otolaryngol Clin North Am 2004; 37:1159–1166. [DOI] [PubMed] [Google Scholar]
- 3.Hopkins C, Surda P, Nirmal Kumar B. Presentation of new onset anosmia during the COVID-19 pandemic. Rhinology 2020; 58:295–298. [DOI] [PubMed] [Google Scholar]
- 4▪.Borsetto D, Hopkins C, Philips V, et al. Self-reported alteration of sense of smell or taste in patients with COVID-19: a systematic review and meta-analysis on 3563 patients. Rhinology [Internet] 2020; 58:1–7. [DOI] [PubMed] [Google Scholar]; This meta-analysis demonstrated that the loss of smell and taste preceded other symptoms in 20% of cases and it was concomitant in 28%
- 5▪.Moein S, Hashemian S, Mansourafshar B, et al. Smell dysfunction: a biomarker for COVID-19. Int Forum Allergy Rhinol 2020; 10:944–950. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study demonstrated with UPSIT the strong correlation between COVID-19 and anomsia or hyposmia.
- 6▪.Vaira L, Hopkins C, Petrocelli M, et al. Smell and taste recovery in coronavirus disease 2019 patients: a 60-day objective and prospective study. J Laryngol Otol 2020; 134:703–709. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a proscpective study which shows that 7.2% per cent of the patients have remaining chemosensitive disturbances.
- 7▪.Klopfenstein T, Kadiane-Oussou N, Toko L, et al. Features of anosmia in COVID-19. Med Mal Infect 2020; 50:436–439. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study is an additional evidence of the correlation between covid-19 and anosmia
- 8.Huart C, Philpott C, Konstantinidis I, et al. Comparison of COVID-19 and common cold chemosensory dysfunction. Rhinology [Internet] 2020; 58:1–3. [DOI] [PubMed] [Google Scholar]
- 9▪.Yan CH, Faraji F, Prajapati D, et al. Self-reported olfactory loss associates with outpatient clinical course in COVID-19. Int Forum Allergy Rhinol 2020; 10:821–831. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is an early study in the pandemic that suggested that anosmia might be associated with milder symptoms
- 10▪.Vaira LA, Hopkins C, Petrocelli M, et al. Do olfactory and gustatory psychophysical scores have prognostic value in COVID-19 patients? A prospective study of 106 patients,. Journal of Otolaryngol - Head Neck Surg 2020; 49:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this study objective assessment of olfactory function was used and they found that the anosmia is not prognostic factor of the severity of COVID-19 symptoms
- 11▪.Vaira L, Deiana G, Lechien J, et al. Correlations between olfactory psychophysical scores and SARS-CoV-2 viral load in COVID-19 patients. Laryngoscope [Internet] 2021; 131:2312–2318. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study excluded the possibility of patients with anosmia to be superspreaders
- 12▪.Amadu AM, Vaira LA, Lechien JR, et al. Analysis of the correlations between the severity of lung involvement and olfactory psychophysical scores in coronavirus disease 2019 (COVID-19) patients. Int Forum Allergy RhinolD 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]; This is an important objective study which analyze the ct chest findings with smell test.
- 13.Inciarte A, Cardozo C, Chumbita M, et al. Original research: Gustatory and olfactory dysfunctions in hospitalised patients with COVID-19 pneumonia: a prospective study. BMJ Open 2021; 11:e040775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spinato G, Fabbris C, Polesel J, et al. Alterations in smell or taste in mildly symptomatic outpatients with SARS-CoV-2 infection. JAMA [Internet] 2020; 323:2089–2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bartheld CSvon, Hagen MM, Butowt R. Prevalence of chemosensory dysfunction in COVID-19 patients: a systematic review and meta-analysis reveals significant ethnic differences. medRxiv [Internet] 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoon HE, Kim EN, Kim MY, et al. Age-Associated Changes in the Vascular Renin-Angiotensin System in Mice. Oxid Med Cell Longev 2016; 2016: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17▪.Soh S, See A, Teo N, et al. Prevalence of olfactory and taste dysfunction in COVID-19 patients: a community care facility study. Eur Arch Otorhinolaryngol 2021; 278:3375–3380. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a big cohort study underlying the prevelance of anosmia in covid patients
- 18▪.Thakur, Sagayaraj A, Prasad K, Gupta A. Olfactory dysfunction in COVID-19 patients: findings from a tertiary rural centre. Indian J Otolaryngol Head Neck Surg 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]; This was one more study which showed the strong correlation between COVID-19 and anosmia.
- 19.Akerlund A, Bende M, Murphy C. Olfactory threshold and nasal mucosal changes in experimentally induced common cold. Acta Otolaryngol 1995; 115:88–92. [DOI] [PubMed] [Google Scholar]
- 20.Greenberg S. Update on rhinovirus and coronavirus infections. Semin Respir Crit Care Med 2011; 32:433–446. [DOI] [PubMed] [Google Scholar]
- 21▪.Eliezer M, Hamel A, Houdart E, et al. Loss of smell in patients with COVID-19: MRI data reveal a transient edema of the olfactory clefts. Neurology [Internet] 2020; 95:e3145–e3152. [DOI] [PubMed] [Google Scholar]; This study showed that OFL in SARS-CoV2-infected patients is associated with a reversible obstruction of the Olfactory cleft on the MRI scan.
- 22▪.Lechien JR, Michel J, Radulesco T, et al. Clinical and Radiological Evaluations of COVID-19 Patients with Anosmia: Preliminary Report. Laryngoscope [Internet] 2020; 130:2526–2531. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is another radiological study which that anosmia is not related to edema of the olfactory cleft
- 23.Yamagishi M, Hasegawa S, Nakano Y. Examination and classification of human olfactory mucosa in patients with clinical olfactory disturbances. Arch Otorhinolaryngol 1988; 245:316–320. [DOI] [PubMed] [Google Scholar]
- 24.Kirschenbaum D, Imbach LL, Ulrich S, et al. Inflammatory olfactory neuropathy in two patients with COVID-19. Lancet 2020; 396:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25▪.Bryche B, Albin AS, Murri S, et al. Massive transient damage of the olfactory epithelium associated with infection of sustentacular cells by SARS-CoV-2 in golden Syrian hamsters. Brain Behav Immun 2020; 89:579. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a landmark laboratory study which showed damage of the sustentacular cells but of the olfactory neurons
- 26▪.de Melo GD, Lazarini F, Levallois S, et al. COVID-19-related anosmia is associated with viral persistence and inflammation in human olfactory epithelium and brain infection in hamsters. Sci Transl Med 2021; 13:8396. [DOI] [PMC free article] [PubMed] [Google Scholar]; This a significant study which showed that inflammation in the olfactory neuroepithelium may account for prolonged or relapsing symptoms of COVID-19
- 27▪.Brann D, Tsukahara T, Weinreb C, et al. Non-neuronal expression of SARS-CoV-2 entry genes in the olfactory system suggests mechanisms underlying anosmia Sci Adv 2020; 6:eabc5801. [DOI] [PMC free article] [PubMed] [Google Scholar]; This revealed that the infectin of nonneuronal cell types leads to anosmia; possibly through expression of ACE-2 genes.
- 28▪.Bilinska K, Jakubowska P, Bartheld CSVon, Butowt R. Expression of the SARS-CoV-2 entry proteins, ACE2 and TMPRSS2, in cells of the olfactory epithelium: identification of cell types and trends with age. ACS Chem Neurosci 2020; 11:1555–1562. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study showed how sustentacular cells are involved in the SARS-COV2 virus entry in the mouse models and how their expression increased with age.
- 29.Chen M, Reed RR, Lane AP. Chronic inflammation directs an olfactory stem cell functional switch from neuroregeneration to immune defense. Cell Stem Cell 2019; 25:501–513.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30▪.2021; Lechien JR, Hopkins C, Vaira LA, Saussez S. SARS-CoV-2 vaccination may help patients with persistent COVID-19 smell dysfunction. 0:1–2. [DOI] [PubMed] [Google Scholar]; This study showed that SARS-COV2 vaccination may improve olfactory dysfunction in patients with persistant smell diusturbance by stimulating a local, as well as systemic immune response
- 31.Dubé M, Coupanec ALe, Wong AHM, Rini JM, et al. Axonal transport enables neuron-to-neuron propagation of human coronavirus OC43. J Virol 2018; 92: [cited 2021 Oct 4]. Available from: /pmc/articles/PMC6096804/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Landis B, Vodicka J, Hummel T. Olfactory dysfunction following herpetic meningoencephalitis. J Neurol 2010; 257:439–443. [DOI] [PubMed] [Google Scholar]
- 33.Perlman S, Jacobsen G, Afifi A. Spread of a neurotropic murine coronavirus into the CNS via the trigeminal and olfactory nerves. Virology 1989; 170:556–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McCray P, Pewe L, Wohlford-Lenane C, et al. Lethal infection of K18-hACE2 mice infected with severe acute respiratory syndrome coronavirus. J Virol 2007; 81:813–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aragão M, Leal M, Cartaxo Filho O, et al. Anosmia in COVID-19 Associated with Injury to the Olfactory Bulbs Evident on MRI. AJNR Am J Neuroradiol 2020; 41:1703–1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Politi L, Salsano E, Grimaldi M. Magnetic resonance imaging alteration of the brain in a patient with coronavirus disease 2019 (COVID-19) and anosmia. JAMA Neurol 2020; 77:1028–1029. [DOI] [PubMed] [Google Scholar]
- 37.Laurendon T, Radulesco T, Mugnier J, et al. Bilateral transient olfactory bulb edema during COVID-19-related anosmia. Neurology [Internet] 2020; 95:224–225. [DOI] [PubMed] [Google Scholar]
- 38.Klironomos S, Tzortzakakis A, Kits A, Öhberg C, et al. Nervous system involvement in coronavirus disease 2019: results from a retrospective consecutive neuroimaging cohort. Radiology [Internet] 2020; 297:E324–E334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chiu A, Fischbein N, Wintermark M, et al. COVID-19-induced anosmia associated with olfactory bulb atrophy. Neuroradiology [Internet] 2021; 63:147–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guedj E, Million M, Dudouet P, Tissot-Dupont H, et al. 18F-FDG brain PET hypometabolism in post-SARS-CoV-2 infection: substrate for persistent/delayed disorders? Eur J Nucl Med Mol Imag 2021; 48:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hopkins C, Surda P, Whitehead E, Nirmal Kumar B. Early recovery following new onset anosmia during the COVID-19 pandemic-an observational cohort study. [cited 2021 Oct 4]; Available from: 10.1186/s40463-020-00423-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chiesa-Estomba C, Lechien J, Radulesco T, et al. Patterns of smell recovery in 751 patients affected by the COVID-19 outbreak. Eur J Neurol 2020; 27:2318–2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Riestra-Ayora J, Yanes-Diaz J, Esteban-Sanchez J, et al. Long-term follow-up of olfactory and gustatory dysfunction in COVID-19: 6 months case-control study of health workers. Oto-Rhino-Laryngol - Head and Neck Surg [Internet] 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44▪.Lucidi D, Molinar G, Silvestri M, et al. Patient-reported olfactory recovery after SARS-CoV-2 infection: a 6-month follow-up study. Int Forum Allergy Rhinol 2021; 11:1249–1252. [DOI] [PubMed] [Google Scholar]; This study showed that recovery time from anosmia/hyposmia associated with COVID-19 infection varied from less than 7 days to more than 3 months
- 45.Hopkins C, Surda P, Vaira LA, et al. Six month follow-up of self-reported loss of smell during the covid-19 pandemic. Rhinology 2021; 59:26–31. [DOI] [PubMed] [Google Scholar]
- 46▪.Boscolo-Rizzo P, Guida F, Polesel J, et al. Self-reported smell and taste recovery in coronavirus disease 2019 patients: a one-year prospective study. Eur Arch Otorhinolaryngol 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study revelead that patients who suffered from mild-moderate COVID-19 symptoms of chemosensory dysfunction still experienced these symptoms 1 year after the infection.
- 47▪.Leedman SR, Sheeraz M, Sanfilippo PG, Edgar DW, et al. Olfactory dysfunction at six months after coronavirus disease 2019 infection. J Laryngol Otol 2021; 135:839–843. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study is the first to describe six-month outcomes for postcoronavirus disease 2019 patients in terms of olfactory dysfunction
- 48▪.Boscolo-Rizzo P, Hummel T, Hopkins C, et al. High prevalence of long-term olfactory, gustatory, and chemesthesis dysfunction in post-COVID-19 patients: a matched case-control study with one-year follow-up using a comprehensive psychophysical evaluation. Rhinology 2021; 0:0–0. [DOI] [PubMed] [Google Scholar]; This control study found that symptoms of COVID-19 patients was important in raising awareness of this rare side affect associated with the virus.
- 49▪.Duyan M, Ozturan IU, Altas M. Delayed Parosmia Following SARS-CoV-2 Infection: a Rare Late Complication of COVID-19. SN Compr Clin Med 2021; 3:1. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study on parosmia in COVID-19 patients was important in raising awareness of this rare side effect associated with the virus.
- 50▪.Watson DLB, Campbell M, Hopkins C, et al. Altered smell and taste: Anosmia, parosmia and the impact of long Covid-19. PLpS One [Internet] 2021; 16:e0256998. [DOI] [PMC free article] [PubMed] [Google Scholar]; This was an important study in highlighting the impact that disruption of smell and taste linked to COVID-19 can have on the psychological and physical health of affected individuals.
- 51.Leopold D. Distortion of olfactory perception: diagnosis and treatment. Chem Senses [Internet] 2002; 27:611–615. [DOI] [PubMed] [Google Scholar]
- 52.Hawkes C. Parosmia: treatment, mechanism, and types. BMJ [Internet] 2020; 371. [DOI] [PubMed] [Google Scholar]
- 53▪.Webster KE, O’Byrne L, MacKeith S, et al. Interventions for the prevention of persistent post-COVID-19 olfactory dysfunction. Cochrane Database Syst Rev 2021; 7:CD013877. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a living systematic review in progress with the aim to assess the effects (benefits and harms) of interventions that have been used, or proposed, to prevent persisting olfactory dysfunction due to COVID-19 infection
- 54.Vaira LA, Hopkins C, Petrocelli M, et al. Efficacy of corticosteroid therapy in the treatment of long-lasting olfactory disorders in covid-19 patients. Rhinology 2021; 59:20–25. [DOI] [PubMed] [Google Scholar]
- 55.Yan CH, Overdevest JB, Patel ZM. Therapeutic use of steroids in nonchronic rhinosinusitis olfactory dysfunction: a systematic evidence-based review with recommendations. Int Forum Allergy Rhinol 2019; 9:165–176. [DOI] [PubMed] [Google Scholar]
- 56.Nguyen TP, Patel ZM. Budesonide irrigation with olfactory training improves outcomes compared with olfactory training alone in patients with olfactory loss. Int Forum Allergy Rhinol 2018; 8:977–981. [DOI] [PubMed] [Google Scholar]
- 57.Harless L, Liang J. Pharmacologic treatment for postviral olfactory dysfunction: a systematic review. Int Forum Allergy Rhinol 2016; 6:760–767. [DOI] [PubMed] [Google Scholar]
- 58▪.Hopkins C, Alanin M, Philpott C, et al. Management of new onset loss of sense of smell during the COVID-19 pandemic - BRS Consensus Guidelines. Clin Otolaryngol 2021; 46:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study identified the appropriateness of olfactory training, different medical treatment options, referral guidelines and imaging for patients with COVID-19-related loss of sense of smell.
- 59.Pekala K, Chandra RK, Turner JH. Efficacy of olfactory training in patients with olfactory loss: a systematic review and meta-analysis. Int Forum Allergy Rhinol 2016; 6:299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sorokowska A, Drechsler E, Karwowski M, Hummel T. Effects of olfactory training: a meta-analysis. Rhinology 2017; 55:17–26. [DOI] [PubMed] [Google Scholar]
- 61.Poletti SC, Michel E, Hummel T. Olfactory training using heavy and light weight molecule odors. Perception [Internet] 2017; 46 (3–4):343–351. [DOI] [PubMed] [Google Scholar]
- 62▪.Yan CH, Mundy DC, Patel ZM. The use of platelet-rich plasma in treatment of olfactory dysfunction: A pilot study. Laryngosc Invest Otolaryngol 2020; 5:187–193. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is a landmark research study which will lead to the next phase with more resutls.
- 63.Yagi S, Costanzo RM. Grafting the olfactory epithelium to the olfactory bulb. Am J Rhinol Allergy 2009; 23:239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kurtenbach S, Goss GM, Goncalves S, et al. Stem cell reports article cell-based therapy restores olfactory function in an inducible model of hyposmia. Stem Cell Rep 2019; 12:1354–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Coelho DH, Costanzo RM. Spatial mapping in the rat olfactory bulb by odor and direct electrical stimulation. Otolaryngol Head Neck Surg 2016; 155:526–532. [DOI] [PubMed] [Google Scholar]
- 66.Holbrook EH, Puram SV, See RB, et al. Induction of smell through transethmoid electrical stimulation of the olfactory bulb. Int Forum Allergy Rhinol 2019; 9:158–164. [DOI] [PubMed] [Google Scholar]