Purpose of review
To review current evidence on the pathophysiology of COVID-19-related acute respiratory distress syndrome (ARDS) and on the implementation of lung protective ventilation.
Recent findings
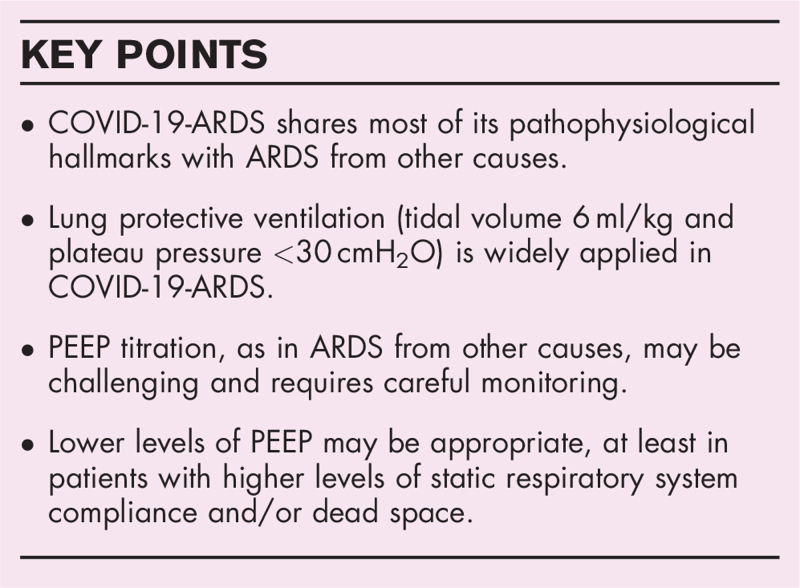
Although multiple observations and physiological studies seem to show a different pathophysiological behaviour in COVID-19-ARDS compared with ‘classical’ ARDS, numerous studies on thousands of patients do not confirm these findings and COVID-19-ARDS indeed shares similar characteristics and interindividual heterogeneity with ARDS from other causes. Although still scarce, present evidence on the application of lung protective ventilation in COVID-19-ARDS shows that it is indeed consistently applied in ICUs worldwide with a possible signal towards better survival at least in one study. The levels of positive end-expiratory pressure (PEEP) usually applied in these patients are higher than in ‘classical’ ARDS, proposing once again the issue of PEEP personalization in hypoxemic patients. In the absence of robust evidence, careful evaluation of the patient is needed, and empiric settings should be oriented towards lower levels of PEEP.
Summary
According to the present evidence, a lung protective strategy based on low tidal volume and plateau pressures is indicated in COVID-19-ARDS as in ARDS from other causes; however, there are still uncertainties on the appropriate levels of PEEP.
Keywords: acute respiratory distress syndrome, coronavirus disease 2019, lung protective ventilation, mechanical ventilation
INTRODUCTION
Before answering the question whether and when lung protective ventilation should be applied to patients with acute respiratory distress syndrome due to coronavirus disease-19 (COVID-19-ARDS), it is useful to briefly recall why this question is so relevant both from a clinical and a research standpoint.
Box 1.
no caption available
As the first cases of COVID-19 began to emerge in early 2020, it became clear that the consistent observation of bilateral interstitial pneumonia and severe hypoxemia allowed to classify the most severe cases of COVID-19 as having ARDS [1▪]. However, in a matter of weeks, clinical observations and expert opinions began to emerge, suggesting that COVID-19-ARDS was in fact a different form of ARDS [2]. Most of these conclusions were based on the observation that COVID-19 patients showed ‘abnormally high’ levels of static compliance and lung volumes and ‘abnormally low’ oxygenation parameters, not totally justified by the amount of nonventilated parenchyma on computed tomography (CT) scan [3].
These doubts, which are still partially unsolved, led many to the conclusion that ‘atypical’ ARDS does not need ‘typical’ lung protective ventilation [4]. A wide debate among experts in the field followed and fuelled a number of important studies [5▪,6,7▪▪,8–10] that we will review in the second part of this article. Before that, however, we shall briefly review the state of the art of lung protective ventilation in ARDS.
LUNG PROTECTIVE MECHANICAL VENTILATION IN ACUTE RESPIRATORY DISTRESS SYNDROME
Mechanical ventilation is a lifesaving technique in several forms of acute respiratory failure. At the same time, extensive studies have demonstrated that the inappropriate application of mechanical ventilation can worsen/induce lung injury (so-called ‘ventilator induced lung injury’ (VILI)) [11–14].
The main ‘classical’ determinants of VILI are barotrauma and volutrauma, that occur because of high volumes or pressures [14]; atelectrauma and biotrauma occur at lower lung volumes by the cyclic opening and closing of lung units [14]. More recently, the ‘unifying’ concept of ergotrauma (damage because of excessive mechanical energy) has been developed and the mechanical power has been proposed as a single variable encompassing all the factors involved in VILI development [15].
Increasing understanding of the mechanisms behind VILI has led to the development of the concept of protective mechanical ventilation. The two main aspects of protective mechanical ventilation are to limit tidal volume (VT) and plateau pressures to prevent lung damage caused by overdistension [13] and to set the appropriate positive end-expiratory pressure (PEEP) level to minimize the cyclic opening and closing of airways and lung units [16].
The landmark ARMA trial has shown significant mortality reduction when a protective ventilatory strategy of VT 6 ml/kg predicted body weight (PBW) and plateau pressure less than 30 cmH2O was used compared with traditional ventilatory setting [13], and this strategy is still strongly recommended in adult patients with ARDS [17,18]. More recently, airway driving pressure (ΔP) has been shown to be a strong predictor of mortality even in patients receiving ‘protective’ plateau pressures and VT[19]. In fact, at least from a physiological standpoint, driving pressure is a more precise way of normalizing tidal volume to the size of the ARDS lung (surrogated by respiratory system compliance) [18].
The main concern about setting PEEP remains the selection of its optimum level that can simultaneously minimize VILI, improve oxygenation with no hemodynamics effects. In fact, excessive PEEP levels to counteract atelectrauma may lead to excessive lung parenchymal strain and finally to barotrauma, which could be worse than atelectrauma itself [20]. An individual meta-analysis summed up results of three RCTs that studied the effect of high vs. low PEEP level [21–23] and showed no statistical difference in overall hospital mortality but a relative mortality reduction in moderate and severe ARDS patients when a high PEEP level strategy was used [16]. These results suggest that adult patients with moderate or severe ARDS may benefit from higher rather than lower levels of PEEP [17]. However, a more recent trial applying a strategy of high PEEP combined with aggressive recruitment maneuvers (targeted at obtaining an ‘open lung’) showed increased mortality compared with a more conservative protective strategy with relatively high incidence of barotrauma [24]. Moreover, several methods and approaches for estimating lung recruitability (and consequently guide PEEP titration) have been proposed in the last three decades based on respiratory system mechanics [19], transpulmonary pressure measurements [25,26], CT-scan analysis [27], electrical impedance tomography [28,29] and others [13,21] but none of those provided compelling evidence of superiority [18,30] as the individual response to PEEP is highly variable.
All these controversial results lead many to doubt on whether an open lung should be the target of a protective ventilatory strategy in ARDS [31]. Moreover, the notion that PEEP could be increasing the energy load delivered to the lung in the theoretical framework of ergotrauma, further supports the hypothesis that tolerating at least small amounts of ‘closed’ (or cyclically opening–closing) lung can be less dangerous than barotrauma and volutrauma because of high levels of distending pressure [20,31,32].
CORONAVIRUS DISEASE 2019-ACUTE RESPIRATORY DISTRESS SYNDROME: SIMILARITIES AND DIFFERENCES FROM ‘CLASSICAL’ ACUTE RESPIRATORY DISTRESS SYNDROME
As briefly stated in the introduction, bilateral infiltrates developing less than a week from COVID-19 onset, accompanied by oxygenation deficit with PaO2/FiO2 ratio 300 mmHg or less are common in COVID-19 patients with pneumonia; consequently, these patients can be classified as having ARDS, according to the Berlin definition [33]. The incidence of ARDS in more than 2000 hospitalized COVID-19 patients was reported to be ∼30%, with a mortality rate ∼45% [34]. Although initial case series reported much higher mortality rate in mechanically ventilated patients compared with ARDS from other causes, recent data reported a 28-day mortality consistent with classical ARDS, ranging between 15 and 50% [34]. Decreasing in mortality rate from the early pandemic to current days may be due mostly to organizational factors and the initial overwhelming pressure on limited healthcare resources [35].
Soon after the pandemics began, physiologic data underlining the heterogeneity of COVID-19-ARDS patients began to emerge [2–4]. In particular, the presence of severe hypoxemia often associated with near normal respiratory system compliance seemed to suggest the presence of two distinct phenotypes of COVID-19-ARDS: one, supposed to be more common during the early stage of COVID-19 disease (type L), characterized by lower elastance, ventilation to perfusion (VA/Q) ratio, lung weight and recruitability; the other phenotype (type H) was characterized by higher elastance, right-to-left shunt because of more nonaerated tissue for increased edema and high lung weight and lung recruitability, similar to classical ARDS [3]. These two phenotypes were also supposed to be the expression of different phases of the same disease. Thus, patients with type L may evolve into type H phenotypes for disease progression because of viral replication and the worsening pneumonia or to patient self-inflicted lung injury. Type H patients were suggested to be treated as classical severe ARDS, including lung protective ventilation strategies, higher PEEP, prone positioning, and extracorporeal supports. When mechanical ventilation is required in type L, same authors suggested lower levels of PEEP because of low recruitability and possible detrimental hemodynamic effects; ventilation with volumes greater than 6 ml/kg was also proposed (up to 8–9 ml/kg) [3].
These early observations incited conduction and publication of several studies, investigating differences and similarities between classical ARDS and COVID-19-ARDS. The focus was especially pointed at static compliance and its possible use for patient phenotyping and consequent clinical management. The tendency to higher compliance with median values higher than 40 ml/cmH2O was shown by some studies [5▪,7▪▪,9] but not confirmed in several other studies, where compliance was lower and similar to classical ARDS [6,8,10,36,37]. Interestingly, in the study by Grasselli et al., although showing higher median values of static compliance, only 6% of patients with COVID-19-associated ARDS had compliances greater than the 95th percentile of the classical ARDS cohort [5▪]. The wide range of static compliance reported in literature becomes narrower in studies with more than 100 patients, and the inclusion of higher numbers of patients seems to be associated to a lower tendency to differ from classical ARDS.
Furthermore, a recent secondary analysis of the LUNG SAFE study investigated the distribution of compliance phenotypes in classical ARDS and their relationship with mortality. Among more than 1000 patients included in the analysis, more than 10% had preserved compliance (>50 ml/cmH2O) with a significant lower mortality compared with patients with lower compliance (<40 ml/cmH2O) (32 vs. 45%); moderate and severe hypoxemia were also found in a significant proportion of patients with relatively high static compliance [38▪▪]. We can conclude that respiratory static compliance is a heterogeneous parameter either in COVID-19 or classical ARDS. An important additional finding is the absence of correlation between respiratory static compliance and PaO2/FiO2 ratio, especially in COVID-19-ARDS [5▪].
Different mechanisms may play a role in causing severe hypoxemia in COVID-19 patients, such as intravascular disorder. During SARS-CoV-2 infection, one of the most reported alteration is a hypercoagulability state with high incidence of disseminate intravascular coagulation, pulmonary intravascular coagulation, venous thromboembolism, pulmonary embolism and arterial thrombosis [39]. In a cohort physiologic study performed on 10 patients affected by COVID-19 related ARDS, Mauri and colleagues showed an elevated ventilation/perfusion mismatch, with larger prevalence of ventilated non perfused lung units (dead space) compared with perfused nonventilated units (shunts). This report suggested a larger dead space and increased pulmonary vessel resistance caused by micro–macro thrombosis [40▪▪]. Serum concentration of D-dimer is an independent risk of mortality, and, whenever combined with static respiratory compliance evaluation may enhances the prediction of mortality in COVID-19 patients [5▪,41].
Other authors proposed the classification into two phenotypic subgroups of COVID-19-ARDS based on demographic, respiratory and laboratory data including markers of coagulopathy (D-dimer, PT and aPTT) and end-organ dysfunction (decreased pH, increased lactate, creatinine and troponin-T). A minority of patients (27%), included in the group (class 2) with increased organ dysfunction (prevalently renal and cardiac abnormalities), relative lactic acidosis and increased coagulopathy, showed an almost doubled 28-day mortality compared with class 1 (40 vs. 23.3%) [42].
All in all, the data we presented leads us to underline following points: patients with COVID-19-ARDS are clinically heterogeneous as the patients with ARDS from other causes (this is not surprising as ARDS is a syndrome and not a disease) [43]; lung mechanics and gas exchange appear to be comparable between COVID-19-ARDS and ARDS because of other causes [44]; COVID-19-ARDS patients are possibly characterized by more widespread vascular and thrombotic involvement than patients with classical ARDS (although thrombotic manifestations in these patients are known since the 1980s) [5▪].
Table 1 presents relevant respiratory and outcome variables in patients with ‘classical’ ARDS and COVID-19-ARDS in important observational studies [5▪,6,7▪▪,8,33,38▪▪,45].
Table 1.
Characteristics and outcomes of patients with classical acute respiratory distress syndrome and coronavirus disease 2019-acute respiratory distress syndrome in observational studies
| Classical ARDS | COVID 19-ARDS | |||||
| Berlin definition physiologic database (n = 269) [33] | LUNG SAFE (n = 2377) [38▪▪,45] | Grasselli et al. (n = 301) [5▪] | Ferrando et al. (n = 742) [8] | Botta et al. (n = 553) [6] | Chiumello et al. (n = 32) [7▪▪] | |
| Crs (ml/cmH2O) | 38 ± 15.2 | 34.7 ± 21.1 | 41 (33–52) | 35 (27–45) | 31.9 (26–39.9) | 49.9 ± 15.4 |
| PaO2/FiO2 ratio | 162 ± 57.1 | 161 (158–163) | 124 (89–164) | 120 (83–177) | 158.8 (128.6–200.5) | 106.5 ± 59.6 |
| PEEP (cmH2O) | 11.5 ± 3.4 | 8.4 (8.3–8.6) | 13 (10–15) | 12 (11–14) | 14 (11–15) | -- |
| VT/PBW (ml/kg) | -- | 7.6 (7.5–7.7) | 7 (6.3–7.6) | 6.9 (6.3–7.8) | 6.3 (5.7–7.1) | 7.7 ± 0.9 |
| Pplat (cmH2O) | -- | 23.2 (22.6–23.7) | 24 (22–26) | 25 (22–29) | -- | 17.2 ± 3.8 |
| 28-day mortality (%) | 37 | 34.8 | 36 | 32 | 35 | 37.5 |
| Ventilator-free days at day 28 | 8.5 (0–23.5)a 0 (0–16.5)b 0 (0–6.5)c | 10 (0–22) | -- | 4 (0–18) | 0 (0–15) | -- |
| Ventilatory ratio (units) | -- | -- | 1.76 (1.42–2.14) | 2 (1.49–2.63) | -- | 1.76 ± 0.45 |
| Total lung weight (g) | 1466 (1213–1816) | -- | 1676 (1375–1876) | -- | -- | 1596 ± 385 |
Data are presented either as mean ± SD or as median (IQR). Crs, static compliance of the respiratory system; PaO2/FiO2, ratio of arterial partial pressure of oxygen to fraction of inspired oxygen; PBW, predicted body weight; PEEP, positive end-expiratory pressure; VT, tidal volume.
Mild ARDS.
Moderate ARDS.
Severe ARDS.
LUNG PROTECTIVE VENTILATION IN CORONAVIRUS DISEASE 2019-ACUTE RESPIRATORY DISTRESS SYNDROME PATIENTS
We should now integrate the elements of the previous paragraphs with the evidence on lung protective strategies in COVID-19-ARDS patients and consequently try to answer the question whether ‘classical’ lung protective ventilation is indicated in these patients. Unfortunately, specific evidence to date is still scarce and does not allow for definite conclusions. Many other strategies already used in moderate-to-severe ARDS, such as prone positioning, muscle relaxation, nitric oxide and extracorporeal membrane oxygenation have been implemented in COVID-19-ARDS but are outside the scope of this review.
In a recent cohort study on 1503 critically ill COVID-19 patients conducted in Brazil, use of protective ventilatory settings (defined as tidal volume ≤8 ml/kg PBW and plateau pressure ≤30 cmH2O) during the first 24 h of the ICU stay was associated (in a Cox proportional hazards model adjusted for compliance, PaO2/FiO2 ratio, PEEP and pH) with a statistically significant benefit in 28-day mortality (aHR 0.73, 95% CI 0.57–0.94). Moreover, nonsurvivors had slightly (but significantly) higher mean plateau pressure and driving pressure, compared with nonsurvivors (23 vs. 22 cmH2O and 13 vs. 12 cmH2O, respectively), while median PEEP was 10 cmH2O both in survivors and nonsurvivors. By analyzing static compliance distribution, the authors could not show any bimodal distribution that could possibly lead to identification of phenotypes [46].
In a multicenter, retrospective observational study performed in 18 ICUs in the Netherlands on a total of 553 patients, Botta and coworkers showed that lung protective ventilation (in terms of low tidal volume and plateau pressure) was applied regularly on most COVID-19-ARDS patients, while PEEP setting was less consistent, with wider variability and a high median level of ∼14 cmH2O. However, although increasing tidal volume (normalized by PBW) was significantly associated with worse outcome, PEEP was not, and the authors conclude that their data do not support the suggestion that there are distinct phenotypes needing different approaches in the titration of PEEP [6].
A scoping review of mechanical ventilation use in critically ill COVID-19 patients showed that, among more than 14 000 mechanically ventilated COVID-19 patients, the settings used for mechanical ventilation were relatively consistent across studies and generally followed usual recommendation for lung protective ventilation: median plateau pressures ranged between 20.5 and 31 cmH2O, median driving pressures between 9.5 and 15 cmH2O and set tidal volume rarely exceeded 7.5 ml/kg PBW [47]. However, median PEEP level was almost always at least 10 cmH2O, a value substantially higher than recorded in the LUNG SAFE study [45].
A recent consensus statement using the Delphi method among 39 experts in the field shows wide agreement on the fact that COVID-19-ARDS is clinically similar to other forms of ARDS. A strong recommendation is to use lung protective ventilation (considered as tidal volume 4–6 ml/kg PBW, plateau pressure ≤30 cmH2O and driving pressure ≤15 cmH2O strong statement), while there was neither agreement for higher vs. lower PEEP strategy nor the method of PEEP selection in these patients [48].
The Surviving Sepsis Campaign Guidelines on the Management of Adults With COVID-19 in the ICU, even in their 2021 update continue to recommend a strategy of ventilation based on low tidal volume (4–8 ml/kg PBW), low plateau pressure (<30 cmH2O) and higher PEEP (>10 cmH2O), although they underline the need for close patient monitoring in order to avoid barotrauma [49,50].
As for classical ARDS, we think that there are more doubts than certainties on the correct setting of PEEP [31] and personalization according to physiologic measurements is of paramount importance. Nevertheless, current knowledge seems to point in the direction of caution in the use of higher PEEP strategies in these patients for at least two reasons. First, hyperinflation is a common occurring phenomenon both in classical ARDS [51] and in COVID-19-ARDS [5▪], and there is growing evidence of increased alveolar dead space [5▪,7▪▪] and limited recruitability in COVID-19-ARDS [52▪]. Second, there is a worryingly high incidence of barotrauma and gas leak manifestations (pneumothorax and pneumomediastinum) in COVID-19-ARDS patients [53,54], which is probably because of specific characteristics of the lung parenchyma (so-called ‘lung frailty’) [55].
Nevertheless, we think that the principle of limiting tidal volume and distending pressure is still undisputed, even in the time of COVID-19; however, we could not insist too much in stressing the importance of measuring relevant physiological variables (such as transpulmonary pressure and mechanical power) whenever possible and continuously re-evaluate the patient for obtaining the best possible ventilatory settings. Although we begin to understand more on the pathophysiology of COVID-19-ARDS and of other forms of ARDS, researchers and clinicians need to keep a ‘watchful eye’ and continue to explore the field, keeping in mind that there is probably not a single therapy for such a complex and heterogeneous syndrome.
CONCLUSION
With few exceptions, COVID-19-ARDS patients should be ventilated with usual lung protective settings, constituting low tidal volumes (6 ml/kg PBW), plateau pressures lower than 30 cmH2O (always considering the wide variations in the resulting transpulmonary pressure), airway driving pressures lower than 15 cmH2O and mechanical power possibly lower than 16 J/min. PEEP selection, as in classical ARDS, is the most challenging decision and requires careful evaluation of the patient; we suggest using lower PEEP levels whenever possible.
Acknowledgements
None.
Financial support and sponsorship
Supported in part by Progetti di Ricerca di Interesse Nazionale (PRIN 2017, project J4BE7A) of the Italian Ministry of University.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1▪.Grasselli G, Zangrillo A, Zanella A, et al. COVID-19 Lombardy ICU Network. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA 2020; 323:1574–1581. [DOI] [PMC free article] [PubMed] [Google Scholar]; Important epidemiological study on critical COVID-19 patients.
- 2.Gattinoni L, Coppola S, Cressoni M, et al. COVID-19 does not lead to a ‘typical’ acute respiratory distress syndrome. Am J Respir Crit Care Med 2020; 201:1299–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gattinoni L, Chiumello D, Caironi P, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med 2020; 46:1099–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marini JJ, Gattinoni L. Management of COVID-19 respiratory distress. JAMA 2020; 323:2329–2330. [DOI] [PubMed] [Google Scholar]
- 5▪.Grasselli G, Tonetti T, Protti A, et al. Pathophysiology of COVID-19-associated acute respiratory distress syndrome: a multicentre prospective observational study. Lancet Respir Med 2020; 8:1201–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]; Prospective observational study describing relevant pathophysiological aspects of COVID-19-ARDS patients with a comparison with cohorts of ‘classical’ ARDS patients.
- 6.Botta M, Tsonas AM, Pillay J, et al. PRoVENT-COVID Collaborative Group. Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): a national, multicentre, observational cohort study. Lancet Respir Med 2021; 9:139–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7▪▪.Chiumello D, Busana M, Coppola S, et al. Physiological and quantitative CT-scan characterization of COVID-19 and typical ARDS: a matched cohort study. Intensive Care Med 2020; 46:2187–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]; Detailed physiological study describing quantitative CT scan variables in COVID-19-ARDS patients and comparison with classical ARDS.
- 8.Ferrando C, Suarez-Sipmann F, Mellado-Artigas R, et al. COVID-19 Spanish ICU Network. Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive Care Med 2020; 46:2200–2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grieco DL, Bongiovanni F, Chen L, et al. Respiratory physiology of COVID-19-induced respiratory failure compared to ARDS of other etiologies. Crit Care 2020; 24:529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vandenbunder B, Ehrmann S, Piagnerelli M, et al. COVADIS study group. Static compliance of the respiratory system in COVID-19 related ARDS: an international multicenter study. Critical Care 2021; 25:52–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dreyfuss D, Saumon G. Ventilator-induced lung injury: lessons from experimental studies. Am J Respir Crit Care Med 1998; 157:294–323. [DOI] [PubMed] [Google Scholar]
- 12.Ranieri VM, Suter PM, Tortorella C, et al. Effect of mechanical ventilation on inflammatory mediators in patients with acute respiratory distress syndrome: a randomized controlled trial. JAMA 1999; 282:54–61. [DOI] [PubMed] [Google Scholar]
- 13.Brower RG, Matthay MA, et al. Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. New Engl J Med 2000; 342:1301–1308. [DOI] [PubMed] [Google Scholar]
- 14.Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med 2013; 369:2126–2136. [DOI] [PubMed] [Google Scholar]
- 15.Gattinoni L, Tonetti T, Cressoni M, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med 2016; 42:1567–1575. [DOI] [PubMed] [Google Scholar]
- 16.Briel M, Meade M, Mercat A, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA 2010; 303:865–873. [DOI] [PubMed] [Google Scholar]
- 17.Fan E, Del Sorbo L, Goligher EC, et al. American Thoracic Society, European Society of Intensive Care Medicine, and Society of Critical Care Medicine. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med 2017; 195:1253–1263. [DOI] [PubMed] [Google Scholar]
- 18.Chiumello D, Brochard L, Marini JJ, et al. Respiratory support in patients with acute respiratory distress syndrome: an expert opinion. Crit Care 2017; 21:240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015; 372:747–755. [DOI] [PubMed] [Google Scholar]
- 20.Gattinoni L, Quintel M, Marini JJ. Volutrauma and atelectrauma: which is worse? Crit Care 2018; 22:264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brower RG, Lanken PN, MacIntyre N, et al. National Heart, Lung, and Blood Institute ARDS Clinical Trials Network. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med 2004; 351:327–336. [DOI] [PubMed] [Google Scholar]
- 22.Meade MO, Cook DJ, Guyatt GH, et al. Lung Open Ventilation Study Investigators. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 2008; 299:637–645. [DOI] [PubMed] [Google Scholar]
- 23.Mercat A, Richard JC, Vielle B, et al. Expiratory Pressure (Express) Study Group. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 2008; 299:646–655. [DOI] [PubMed] [Google Scholar]
- 24.Cavalcanti AB, Suzumura EA, et al. Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial Investigators. Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 2017; 318:1335–1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Talmor D, Sarge T, Malhotra A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med 2008; 359:2095–2104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beitler JR, Sarge T, Banner-Goodspeed VM, et al. Effect of Titrating Positive End-Expiratory Pressure (PEEP) With an Esophageal Pressure-Guided Strategy vs an Empirical High PEEP-Fio2 Strategy on Death and Days Free From Mechanical Ventilation Among Patients With Acute Respiratory Distress Syndrome: a randomized clinical trial. JAMA 2019; 321:846–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gattinoni L, Caironi P, Cressoni M, et al. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med 2006; 354:1775–1786. [DOI] [PubMed] [Google Scholar]
- 28.Meier T, Luepschen H, Karsten J, et al. Assessment of regional lung recruitment and derecruitment during a PEEP trial based on electrical impedance tomography. Intensive Care Med 2008; 34:543–550. [DOI] [PubMed] [Google Scholar]
- 29.Franchineau G, Brechot N, Lebreton G, et al. Bedside Contribution of electrical impedance tomography to setting positive end-expiratory pressure for extracorporeal membrane oxygenation-treated patients with severe acute respiratory distress syndrome. Am J Respir Crit Care Med 2017; 196:447–457. [DOI] [PubMed] [Google Scholar]
- 30.Gattinoni L, Collino F, Maiolo G, et al. Positive end-expiratory pressure: how to set it at the individual level. Ann Transl Med 2017; 5:288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Del Sorbo L, Tonetti T, Ranieri VM. Alveolar recruitment in acute respiratory distress syndrome: should we open the lung (no matter what) or may accept (part of) the lung closed? Intensive Care Med 2019; 45:1436–1439. [DOI] [PubMed] [Google Scholar]
- 32.Tonetti T, Vasques F, Rapetti F, et al. Driving pressure and mechanical power: new targets for VILI prevention. Ann Transl Med 2017; 5:286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ranieri VM, Rubenfeld GD, et al. ARDS Definition Task Force. Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012; 307:2526–2533. [DOI] [PubMed] [Google Scholar]
- 34.Tzotzos SJ, Fischer B, Fischer H, Zeitlinger M. Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey. Critical Care 2020; 24:516–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Attaway AH, Scheraga RG, Bhimraj A, et al. Severe covid-19 pneumonia: pathogenesis and clinical management. BMJ 2021; 372:n436. [DOI] [PubMed] [Google Scholar]
- 36.Cummings MJ, Baldwin MR, Abrams D, et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet 2020; 395:1763–1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schenck EJ, Hoffman K, Goyal P, et al. Respiratory mechanics and gas exchange in COVID-19-associated respiratory failure. Ann Am Thorac Soc 2020; 17:1158–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38▪▪.Panwar R, Madotto F, Laffey JG, van Haren FMP. Compliance phenotypes in early acute respiratory distress syndrome before the COVID-19 pandemic. Am J Respir Crit Care Med 2020; 202:1244–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]; Posthoc analysis of a wide observational study on ‘classical’ ARDS patients. Important observations on the presence of high compliance phenotypes before COVID-19.
- 39.Ostergaard L. SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiol Rep 2021; 9:e14726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40▪▪.Mauri T, Spinelli E, Scotti E, et al. Potential for lung recruitment and ventilation-perfusion mismatch in patients with the acute respiratory distress syndrome from coronavirus disease. Crit Care Med 2020; 48:1129–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]; Interesting physiological study, detailing pathophysiological characteristics of the COVID-19-ARDS lung, both in terms of recruitability and ventilator-perfusion mismatch.
- 41.Bartoletti M, Giannella M, Scudeller L, et al. PREDICO study group. Development and validation of a prediction model for severe respiratory failure in hospitalized patients with SARS-CoV-2 infection: a multicentre cohort study (PREDI-CO study). Clin Microbiol Infect 2020; 26:1545–1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ranjeva S, Pinciroli R, Hodell E, et al. Identifying clinical and biochemical phenotypes in acute respiratory distress syndrome secondary to coronavirus disease. EClinicalMedicine 2021; 34:100829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fan E, Beitler JR, Brochard L, et al. COVID-19-associated acute respiratory distress syndrome: is a different approach to management warranted? Lancet Respir Med 2020; 8:816–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Goligher EC, Ranieri VM, Slutsky AS. Is severe COVID-19 pneumonia a typical or atypical form of ARDS? And does it matter? Intensive Care Med 2021; 47:83–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bellani G, Laffey JG, Pham T, et al. LUNG SAFE Investigators, ESICM Trials Group. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016; 315:788–800. [DOI] [PubMed] [Google Scholar]
- 46.Ferreira JC, Ho YL, Besen B, et al. Protective ventilation and outcomes of critically ill patients with COVID-19: a cohort study. Ann Intensive Care 2021; 11:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Grasselli G, Cattaneo E, Florio G, et al. Mechanical ventilation parameters in critically ill COVID-19 patients: a scoping review. Crit Care 2021; 25:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nasa P, Azoulay E, Khanna AK, et al. Expert consensus statements for the management of COVID-19-related acute respiratory failure using a Delphi method. Crit Care 2021; 25:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Alhazzani W, Moller MH, Arabi YM, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med 2020; 46:854–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Alhazzani W, Evans L, Alshamsi F, et al. Surviving sepsis campaign guidelines on the management of adults with coronavirus disease 2019 (COVID-19) in the ICU: first update. Crit Care Med 2021; 49:e219–e234. [DOI] [PubMed] [Google Scholar]
- 51.Terragni PP, Rosboch G, Tealdi A, et al. Tidal hyperinflation during low tidal volume ventilation in acute respiratory distress syndrome. Am J Respir Crit Care Med 2007; 175:160–166. [DOI] [PubMed] [Google Scholar]
- 52▪.Ball L, Robba C, Maiello L, et al. GECOVID (GEnoa COVID-19) group. Computed tomography assessment of PEEP-induced alveolar recruitment in patients with severe COVID-19 pneumonia. Crit Care 2021; 25:81. [DOI] [PMC free article] [PubMed] [Google Scholar]; Quantitative CT-scan study showing limited recruitability of lungs oin COVID-19-ARDS.
- 53.Belletti A, Palumbo D, Zangrillo A, et al. COVID-BioB Study Group. Predictors of pneumothorax/pneumomediastinum in mechanically ventilated COVID-19 patients. J Cardiothorac Vasc Anesth 2021; doi: 10.1053/j.jvca.2021.02.008. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Belletti A, Landoni G, Zangrillo A. Pneumothorax and barotrauma in invasively ventilated patients with COVID-19. Respir Med 2021; 187:106552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lemmers DHL, Abu Hilal M, Bna C, et al. Pneumomediastinum and subcutaneous emphysema in COVID-19: barotrauma or lung frailty? ERJ Open Res 2020; 6:00385–2020. [DOI] [PMC free article] [PubMed] [Google Scholar]