Purpose of review
Prone position has been widely used in the COVID-19 pandemic, with an extension of its use in patients with spontaneous breathing (’awake prone’). We herein propose a review of the current literature on prone position in mechanical ventilation and while spontaneous breathing in patients with COVID-19 pneumonia or COVID-19 ARDS.
Recent findings
A literature search retrieved 70 studies separating whether patient was intubated (24 studies) or nonintubated (46 studies). The outcomes analyzed were intubation rate, mortality and respiratory response to prone. In nonintubated patient receiving prone position, the main finding was mortality reduction in ICU and outside ICU setting.
Summary
The final results of the several randomized control trials completed or ongoing are needed to confirm the trend of these results. In intubated patients, observational studies showed that responders to prone in terms of oxygenation had a better survival than nonresponders.
Keywords: acute respiratory distress syndrome, awake prone position, coronavirus disease 2019, mechanical ventilation, prone position
INTRODUCTION
During the coronavirus disease 2019 (COVID-19) pandemic, the use of prone position has been exponential. A rate of use of prone as high as 70% or more has been reported in large prospective cohorts [1▪,2▪,3▪▪], to be compared with less than 20% before the pandemic [4,5]. This finding was observed even though the level of evidence and the strength of recommendation had not changed [6]. With the COVID-19 pandemic, prone position has reached its true significance. Furthermore, proning was offered to patients not intubated. Even though this option started before the COVID-19, its use in nonintubated COVID-19 patients also increased dramatically and a new terminology was created: awake prone position (aPP) or self-proning. Moreover, it was carried out in the non-ICU environment. The rationale of using pronation in intubated and nonintubated patients differ. In the former, the benefits of prone position are oxygenation improvement, drainage of respiratory secretions, stabilization/improvement of hemodynamics and prevention of ventilator-induced lung injury, all these are mechanisms by which proning can improve survival [7]. In the nonintubated patients, the expected benefit is to improve oxygenation and hence to avoid intubation, and therefore, prevent the ICU resources from overcrowding. It is speculated that aPP could prevent self-induced lung injury by decreasing the swing of respiratory muscle pressure during inspiration. Although we are awaiting for the publication of several trials on pronation in nonintubated patients (NCT04325906, NCT04347941, NCT04358939, NCT04395144, NCT04391140, and NCT04477655), prospective studies have shown that this strategy was feasible and tolerated in most of the cases in a non-ICU environment [8▪▪,9▪▪] with seldom adverse effects described. Furthermore, these studies confirm that prone position can improve oxygenation in these patients.
Box 1.
no caption available
The goal of the present study is to review the available literature on prone position in patients with COVID-19. Nonintubated and intubated patients were analyzed separately. For the nonintubated patients, the primary end-points are intubation and mortality outcomes, and hence we used the articles, which provided a control group in the supine position. For the intubated patients, the main end-point is the patient mortality and the secondary end-point the physiological response to prone. We, therefore, used articles, which provided a control group in the supine position to address the main end-point, and the articles, which analyzed responders and nonresponders in the prone position. We also considered articles, which compared COVID and non-COVID patients in whom prone position was used. Indeed, it has been claimed that the pathophysiology of COVID-19-related acute respiratory syndrome (ARDS) may be different from the classic ARDS [10▪,11,12▪▪], casting some doubt about the usefulness of prone position in patients without severe impairment of respiratory system compliance [10▪].
METHODS
PICOS
The medical question according to the PICOS method involved the following:
-
(1)
Patients: patients with COVID-19 hospitalized for acute respiratory failure.
-
(2)
Intervention: intervention is the prone position whether the patient is intubated or not.
-
(3)
Comparison: comparison is the supine position or the non-COVID patients.
-
(4)
Outcomes: in nonintubated patients the outcomes are intubation, mortality (at ICU, hospital discharge or at the latest time point reported), and physiological response of proning on oxygenation and respiratory mechanics. In intubated patients, the outcomes are mortality (at ICU, hospital discharge, or at the latest time point reported) and physiological response of proning on oxygenation and respiratory mechanics.
-
(5)
Study design includes prospective or retrospective, observational or randomized or quasi-randomized controlled trials.
Literature search
The literature search was performed in PubMed by entering the following words: (((((Prone) OR (Prone position) OR (prone positioning) OR (pronation)) AND COVID-19) to any field. The literature search was done from inception to 10 April 2021. To be selected, the articles had to meet all the following inclusion criteria: being an original research, being a prospective or a retrospective study, being an observational or a randomized or a quasi-randomized controlled trial, dealing with prone position in intubated or in nonintubated patients, having included adult patients with a suspected or confirmed COVID-19 pneumonia, and written in English. Articles were excluded for any of the following noninclusion criteria: case reports (five or less), narrative or systematic reviews or meta-analysis, articles not specifically dedicated to prone position, that is, reporting on the overall rate of proning in a cohort of patients, or on prone position during patient transport, or during cardiac arrest, or during ECMO, or dealing with the feasibility of echocardiography in prone position or with the correct position of EKG leads, editorial or view point or expert(s) opinion papers, articles without abstract, not written in English in the main text. A snowball strategy was also applied to the retrieved articles by reading the references.
The retrieved articles were further excluded first by reading the title (level 1), then by reading the abstract and the whole text (level 2).
Case record form
A specific case record form was set up and included for each included article the following information: first author name, journal name, year of publication, kind of patients (mild, moderate or severe COVID-19), ARDS (Berlin definition), location of prone position delivery (ICU or outside); Sequential Organ Failure Assessment (SOFA), Simplified Acute Physiology Score (SAPS), Acute Physiology and Chronic Health Evaluation (APACHE), at time of ICU admission; baseline characteristics (before proning): length of COVD-19 before admission, age, sex, BMI; kind of respiratory support [intubation, oxygen, high-flow oxygen nasal cannula, noninvasive ventilation (NIV), continuous positive airway pressure (CPAP)], ventilator settings [tidal volume, respiratory rate, positive-end expiratory pressure (PEEP), FIO2]; respiratory rate, FIO2, PaO2/FIO2 measured at baseline, before proning, during proning and after proning; characteristics of proning: mean duration of proning sessions, number of proning sessions; date and status (intubation or not in patients nonintubated, alive or dead) at ICU, hospital discharge and at specific time points (longest reported follow-up, which varied from D14 to D90). If not available, SpO2/FIO2 was computed as equal to 64 + 0.84 × PaO2/FIO2 according to Rice et al.[13].
Data analysis
The continuous variables were expressed as mean values. If the original article provided the median, we used published equations to translate it into mean. When the continuous data were not available as numbers in the main text or in tables but available as points in figures, we extracted them by using the WebPlotDigitizer 4.4 version free software.
The pooled data were expressed as mean difference [95% confidence intervals (CI)] for the continuous variables and odds ratio (OR) (95% CI) for the binary variables. A random effects model was used. The heterogeneity was assessed by using I2 statistic. The overall effect was tested with the z score. The data were displayed as Forrest plots. For the primary outcomes (intubation and mortality), contour-enhanced funnel plots were used to detect publication bias and to assess causes of funnel plot asymmetry. Subgroup analysis were performed: we compared the ICU versus the non-ICU application of prone position for the nonintubated patients. A P value less than 0.05 was deemed as statistically significant. The analysis was performed by using the meta package of the R software version 4.0.3.
RESULTS
The literature search retrieved 947 articles of which 717 were excluded after reading the title (Figure 1 Supplemental Material). Among the remaining 230, 164 were further excluded after reading the abstract and the manuscript. Therefore, 70 articles were analyzed, 24 in intubated and 46 in nonintubated patients, that is, nearly twice higher number of articles were dedicated to nonintubated than to intubated patients, which is worth mentioning (Figure 1 Supplemental Material) and reflects the current trend of using prone position outside ICU. All data retrieved from the studies included were reviewed by authors (A.K., C.G.) and differences were discussed during several distant meetings and a consensus made. The quality of the observational articles was evaluated based on QUIPS criteria [14]. Overall, the studies had a moderate-to-high risk of bias (Table 1 Supplemental Material).
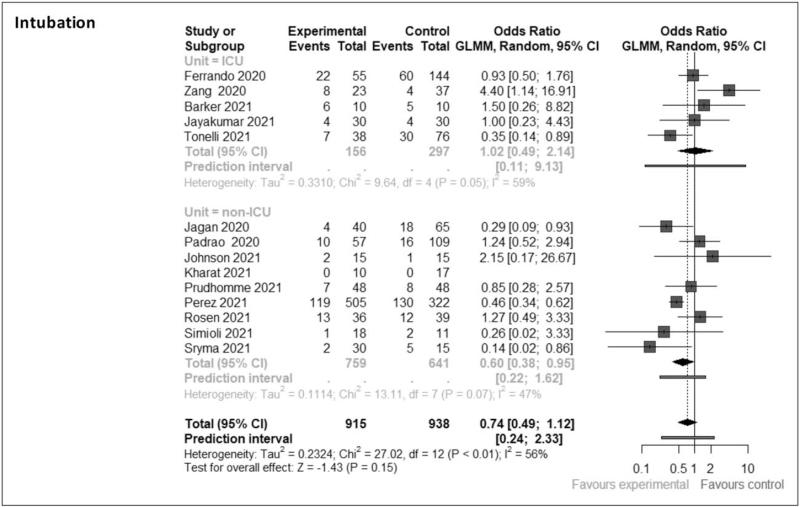
Prone position in nonintubated patients
Seventeen studies (12 observational, 9 retrospective [15–23] and 3 prospective [24–26], and 5 RCTs [27–31]) met our inclusion criteria (Table 1). Six studies were done in the ICU and 11 outside the ICU (Table 1). The baseline respiratory support was mixed. At baseline, supine and prone groups were similar except for age and SpO2/FIO2 ratio, the patients in the prone group being younger and more hypoxemic than those in the supine group (Table 2 Supplemental Material). The pooled analysis found that the intubation rate was not different between supine and prone groups, overall (OR 0.74 [0.49–1.12]) (Fig. 1). However, when prone position was applied outside the ICU, the intubation rate was significantly lower than in the supine group (Fig. 1). In nonintubated patients, the mean number and duration of proning sessions were 3 and 14 h, respectively.
Table 1.
Studies of prone position in nonintubated patients
| Study rank, first author | Country | Kind of study | Inclusion | Location | Oxygen | HFNC | NIV | CPAP | Other | Criteria to prone | Planned proning session duration | N prone | N supine |
| 1. Barker | UK | O,R | March–June 2020 | S, ICU | 4 | 0 | 16 | 0 | 0 | Not defined | As long as possible | 10 | 10 |
| 2. Ferrando | Spain | O,P | March–June 2020 | M, ICU | 0 | 199 | 0 | 0 | 0 | Not defined | 16 h | 55 | 144 |
| 3. Jagan | USA | O,R | March–May 2020 | S, Other | NA | NA | NA | NA | NA | Not defined | NA | 40 | 65 |
| 4. Jayakumar | India | RCT | NA | M, Other | 56 | 1 | 2 | 0 | 1 | SpO2 ≥92% O2 >4 l/min or PaO2/FIO2 100–300 mmHg | 6 h | 30 | 30 |
| 5. Johnson | USA | RCT | April–August 2020 | S, Other | 11 | 0 | 0 | 0 | 0 | Not defined | 2 h | 15 | 15 |
| 6. Jouffroy | France | O,R | February–April 2020 | M, ICU | 2 | 37 | 0 | 1 | 0 | Clinican discretion | 3 h | 40 | 339 |
| 7. Kharat | Switzerland | RCT | April 2020 | M, Acute Care | 27 | 0 | 0 | 0 | 0 | SpO2 90–92% O2 1–6 l/min | As long as possible | 10 | 17 |
| 8. Liu | China | O,R | January–March 2020 | S, Other | NA | NA | NA | NA | NA | Not defined | 10–14 h | 13 | 16 |
| 9. Padrao | Brazil | O,R | March–April 2020 | S, ER | 93 | 72 | 0 | 0 | 0 | Not defined | 4 h | 57 | 109 |
| 10. Prudhomme | France | O,R | March–April 2020 | M, ER | NA | NA | NA | NA | NA | Not defined | 3 h | 48 | 48 |
| 11. Perez | Mexico/Ecuador | O,R | May–June 2020 | M, ER &ICU | 744 | 83 | 0 | 0 | 0 | Clinican discretion | 2 h | 505 | 322 |
| 12. Rosen | Sweden | RCT | October 2020–February 2021 | M, Other | 0 | 60 | 15 | 0 | 0 | PaO2/FIO2 ≤50 mmHg | 16 h | 36 | 39 |
| 13. Simioli | Italy | O,R | March–April 2020 | S, Step Down | 0 | 6 | 0 | 23 | 0 | Not defined | 10 h | 18 | 11 |
| 14. Sryma | India | O,P | NA | ICU | 42 | 1 | 2 | 0 | 0 | Not defined | 8 h | 30 | 15 |
| 15. Taylor | USA | RCT | June–August 2020 | M, Other | 38 | 0 | 1 | 0 | 0 | SpO2 <93% or O2 >3 l/min | As long as possible | 27 | 13 |
| 16. Tonelli | Italy | O,R | March–June 2020 | M, ICU | 0 | 69 | 19 | 25 | 0 | Not defined | 3 h | 38 | 76 |
| 17. Zang | China | O,P | February–April 2020 | S, ICU | 0 | 15 | 15 | 0 | 0 | Not defined | 3–8 h | 23 | 37 |
CPAP, continuous positive airway pressure; ER, emergency room; HFNC, high flow nasal cannula; M, multicenter; NA, not available; NIV, noninvasive ventilation; O, observational; P, prospective; R, retrospective; RCT, randomized controlled trial; S, single center.
FIGURE 1.
Forrest plot for intubation at the latest recording time. CI, confidence interval; GLMM, general linear mixed model.
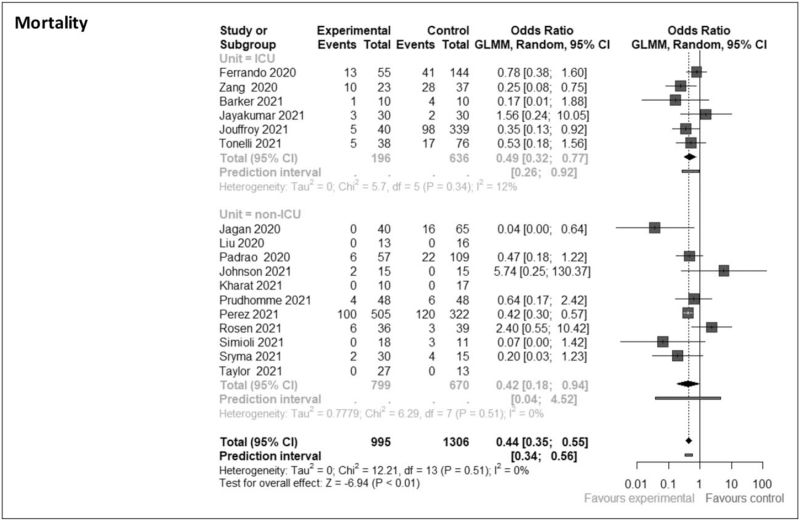
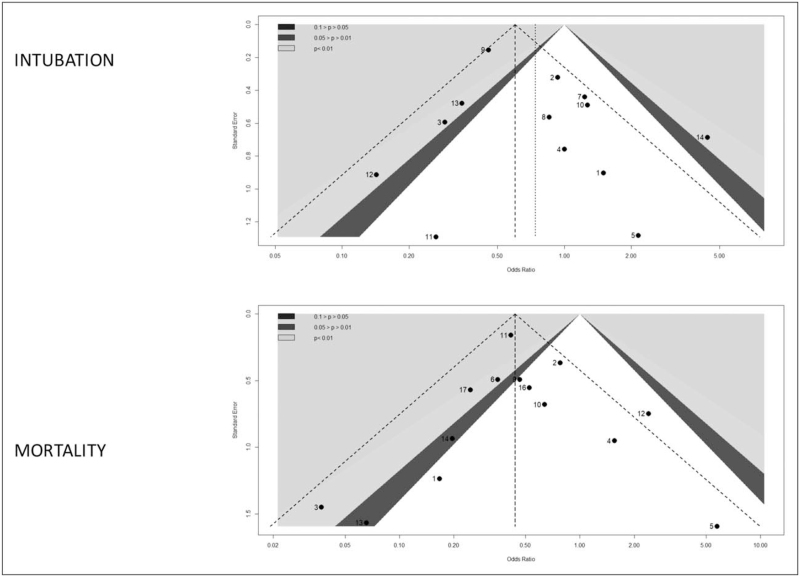
By contrast, the mortality measured at the latest time recorded was significantly lower in the prone than in the supine group [OR 0.44 (0.35–0.55)], the benefit being observed in the patients managed in the ICU but not outside (Fig. 2). The funnel plots were asymmetrical, which suggested a publication bias for both intubation and mortality outcomes (Fig. 3). In particular, the funnel plot in Fig. 3 suggests missing publications that would have been favoring the effect of prone for preventing intubation risk (superior quadrant). Clearly, there is strong need to acknowledge the results of the RCT previously mentioned.
FIGURE 2.
Forrest plot for mortality at the latest recording time. CI, confidence interval; GLMM, general linear mixed model.
FIGURE 3.
Contoured-Funnel plots displaying the relationship between the effect of size on the x-axis and the standard error on the y-axis for intubation and mortality at the latest recording time. Grey, dark grey, and light grey contours pertain to less than 0.1, less than 0.05, and less than 0.01 levels of significance, respectively. The favorable effect of the experimental group, that is, the prone position, is shown in the left hand side of the funnel plots.
No severe adverse complication was reported.
There was only three studies that categorized prone position effect as responders and nonresponders [8▪▪,9▪▪,32]. The definition of responders was variable, such as prepost prone lung ultrasound (LUS) score reduction, PaO2 increase and SpO2/FiO2 increase.
In responders vs. nonresponders, intubation rate was of 0% (0/16) and 50% (3/6), respectively in Avdeev et al.[32], and 30% (7/23) and 26% (6/23) in Coppo et al.[8▪▪].
Prone position in intubated patients
As discussed above, all the studies on prone position in intubated COVID-19 are observational.
Studies comparing prone to supine position in intubated coronavirus disease 2019 patients
Three studies compared COVID-19-related ARDS patients who were proned to patients who were not [3▪▪,33,34]. The mortality was not significantly different between groups [OR 0.45 (0.09–2.18)] but the heterogeneity was extremely high (I2 = 91%).
Physiological response to prone position in intubated coronavirus disease 2019 patients
On the basis of respiratory physiology and COVID-19 infection specificity, it is thought that not all patients respond in the same manner to prone positioning. Therefore, the aim to identify patient who will respond most positively to prone position is crucial. Fifteen studies had PaO2/FIO2 data available before and during proning [3▪▪,35–48]. The ratio increased by 52 (38–66) mmHg (P < 0.01), when the heterogeneity was significant (I2 = 93%). Except in two studies only, the mean increase in PaO2/FIO2 ratio in prone was more than 20 mmHg from its value before proning, a common threshold used to define responders. The rate of responders ranged from 9 to 77%. Seven studies provided data on static compliance of the respiratory system in supine preprone and in prone in intubated patients [3▪▪,35,37,42,45–48]. It significantly increased after a few hours in prone by 2 ml/cmH2O on average (z = −2.68, P < 0.01) (I2 = 30%). Therefore, in present analysis, the short-term physiological response is consistent with what is known in the classic non-COVID-19 ARDS.
An important finding came up regarding the mortality of patients based on their response to prone in terms of oxygenation, a question that was subjected to debate in the classic ARDS. Three studies in intubated COVID-19 patients found that the outcome was better in responders than in nonresponders [OR 0.44 (0.27–0.71), P < 0.01] without any heterogeneity (I2 = 0%) [3▪▪,49,50▪▪]. One study compared prone position in intubated COVID-19 and non-COVID-19 patients [51]. This is the only study describing spontaneous breathing in intubated and mechanically ventilated patients. The authors conclude that the use of prone position in pressure support ventilation mode reduced the use of neuromuscular blockade agents.
DISCUSSION
During the current pandemic, prone position was widely used in patients admitted with COVID-19 pneumonia and ARDS. This was based on the known evidence that prone position reduces mortality in intubated patients with moderate-to-severe non-COVID-19 ARDS [7]. Nevertheless, while there is no strong medical evidence supporting the effect of prone position in mild-to-moderate intubated and in nonintubated patients, numerous studies were carried out on prone position in those specific settings during the ongoing COVID-19 pandemic.
Even though patients with COVID-19 present the same respiratory disorder, the severity of disease, the setting of management and the pathophysiology, were also a source of heterogeneity, as discussed previously.
In nonintubated patients, the pooled results in our present review do not show a beneficial effect of proning on intubation. The potential risk of broadened use of aPP is delaying intubation, therefore, invasive and protective mechanical ventilation. This aspect could potentially counter-balance the beneficial effect of prone position in ICU patient as suggested by the study of Ferrando et al.[24]. The fact that intubation would not be done in the appropriate time when needed could be a concern with the prone position applied outside the ICU. Whereas our results cannot answer this question, present findings do not support a harmful effect of prone position performed outside the ICU.
In our review, there is an effect on mortality of aPP whether it is performed in or outside ICU. This could be because of the fact that proning could avoid immediate mortality from severe hypoxemia. However, it should be pointed out that this result was obtained after merging RCTs and observational studies and that mortality was recorded at different times across the studies. An important meta-trial merging the above-mentioned RCTs is undergoing review for imminent publication to assess the effect of aPP on intubation rate and mortality. We are impatiently awaiting those results to establish more precisely the expected effect of this treatment.
In intubated patients, no new randomized control trial on prone position has been conducted and the outcome of physiological respiratory effect analyzed show a significant increase in the static respiratory compliance prepost proning. Our data show that the outcome in terms of survival was significantly better in responders than in nonresponders, which is an important new finding. The implication of this will be a better selection of patients and a better definition to stop the treatment. However, this could be because of a potential specificity of the COVID-19 phenotypes, and therefore, should not be extended to non-COVID-19 unless further studies are performed. These results were obtained during a unique context of pandemic with a large number of patients in a short time-frame, therefore, leaving out some confounders, such a heterogeneity in practice and management.
Limitations of our review are that most studies included are observational and retrospective, and that the definition of prone position ‘responder’ was not similar throughout the studies. There is also a heterogeneity in the studies regarding the criteria of proning, its definition and use.
Between submission and reviewing of this article, the above mentioned ongoing RCTs have been published as a meta-trial [52]. The conclusion of the authors is that aPP reduces the risk of intubation in patients with COVID-19 with no effect on the mortality.
CONCLUSION
Prone position and awake prone position are therapies developing rapidly in the management of COVID-19 pneumonia. This review of the available literature on the subject in intubated and nonintubated patient focuses on patient's centered outcomes, such as intubation and death. The main finding is that the use of aPP might be associated with lower mortality. High-quality studies on aPP will be available very soon and should confirm beneficial effect of aPP on COVID-19 patient's outcome.
In intubated patients, those who exhibited a positive response to prone in term of oxygenation had a lower mortality than those who did not.
Acknowledgements
The authors would like to thank Chiara Robba MD, Jie Li MD, Rohit Khullar MD, Prateek Prasanna MD, Sujith Cherian MD for sharing some of their data with us for this review.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Supplemental digital content is available for this article.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1▪.Covid-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med 2021; 47:60–73. [DOI] [PMC free article] [PubMed] [Google Scholar]; A large prospective multicenter study in France describing the practice of mechanical ventilation in COVID-19 patients.
- 2▪.Ferrando C, Suarez-Sipmann F, Mellado-Artigas R, et al. COVID-19 Spanish ICU Network. Clinical features, ventilatory management, and outcome of ARDS caused by COVID-19 are similar to other causes of ARDS. Intensive Care Med 2020; 46:2200–2211. [DOI] [PMC free article] [PubMed] [Google Scholar]; A large prospective multicenter study in Spain on intubated patients with COVID-related ARDS describing mechanical ventilation settings, respiratory mechanics and outcome.
- 3▪▪.Langer T, Brioni M, Guzzardella A, et al. Prone position in intubated, mechanically ventilated patients with COVID-19: a multicentric study of more than 1000 patients. Crit Care 2021; 25:128. [DOI] [PMC free article] [PubMed] [Google Scholar]; A large multicenter study in Italy describing the practice of invasive mechanical ventilation in COVID ARDS. In addition, a subset of patients was analyzed based on their response to prone position. The mortality was lower in responders than in non responders.
- 4.Guerin C, Beuret P, Constantin JM, et al. Investigators of the APRONET Study Group, the REVA Network, the Réseau recherche de la Société Française d’Anesthésie-Réanimation (SFAR-recherche) and the ESICM Trials Group. A prospective international observational prevalence study on prone positioning of ARDS patients: the APRONET (ARDS Prone Position Network) study. Intensive Care Med 2018; 44:22–37. [DOI] [PubMed] [Google Scholar]
- 5.Bellani G, Laffey JG, Pham T, et al. LUNG SAFE Investigators, ESICM Trials Group. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 2016; 315:788–800. [DOI] [PubMed] [Google Scholar]
- 6.Papazian L, Aubron C, Brochard L, et al. Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care 2019; 9:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guérin C, Reignier J, Richard J-C, et al. PROSEVA Study Group. Prone positioning in severe acute respiratory distress syndrome. New Engl J Med 2013; 368:2159–2168. [DOI] [PubMed] [Google Scholar]
- 8▪▪.Coppo A, Bellani G, Winterton D, et al. Feasibility and physiological effects of prone positioning in nonintubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir Med 2020; 8:765–774. [DOI] [PMC free article] [PubMed] [Google Scholar]; A large prospective study on awake prone position in COVID patients concluding to the feasibility and defining responders and nonresponders to prone in terms of oxygenation.
- 9▪▪.Elharrar X, Trigui Y, Dols AM, et al. Use of prone positioning in nonintubated patients with COVID-19 and hypoxemic acute respiratory failure. JAMA 2020; 323:2336–2338. [DOI] [PMC free article] [PubMed] [Google Scholar]; One of the earliest report of use of awake prone position in COVID patients.
- 10▪.Gattinoni L, Chiumello D, Caironi P, et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med 2020; 46:1099–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors were the first to propose the concept of two distinct phenotypes in COVID ARDS based on respiratory physiological data recorded in patients. The phenotype L was characterized by a normal compliance indicating that the aerated lung mass was preserved in COVID and that the severity of hypoxemia was mainly because of ventilation to perfusion mismatch across the lungs.
- 11.Gattinoni L, Coppola S, Cressoni M, et al. Covid-19 does not lead to a ‘typical’ acute respiratory distress syndrome. Am J Respir Crit Care Med 2020; 201:1299–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12▪▪.Chiumello D, Busana M, Coppola S, et al. Physiological and quantitative CT-scan characterization of COVID-19 and typical ARDS: a matched cohort study. Intensive Care Med 2020; 46:2187–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]; A study that compared COVID ARDS to non-COVID ARDS matched by oxygenation and compliance. In both matched analyzes, the authors found that the amount of intra-pulmonary shunt was not related to the amount of -nonaerated lung mass in COVID when it was in non COVID patients. This finding suggests that the distribution of pulmonary blood flow is impaired in COVID and that this impairment explains the severity of hypoxemia by mismatching ventilation to perfusion throughout the lungs.
- 13.Rice TW, Wheeler AP, Bernard GR, et al. National Institutes of Health, National Heart, Lung, and Blood Institute ARDS Network. Comparison of the SpO2/FIO2 ratio and the PaO2/FIO2 ratio in patients with acute lung injury or ARDS. Chest 2007; 132:410–417. [DOI] [PubMed] [Google Scholar]
- 14.Hayden JA, van der Windt DA, Cartwright JL, et al. Assessing bias in studies of prognostic factors. Ann Intern Med 2013; 158:280–286. [DOI] [PubMed] [Google Scholar]
- 15.Barker J, Pan D, Koeckerling D, et al. Effect of serial awake prone positioning on oxygenation in patients admitted to intensive care with COVID-19. Postgrad Med J 2021; doi: 10.1136/postgradmedj-2020-139631. [DOI] [PubMed] [Google Scholar]
- 16.Jagan N, Morrow LE, Walters RW, et al. The POSITIONED Study: prone positioning in nonventilated coronavirus disease 2019 patients-a retrospective analysis. Crit Care Explor 2020; 2:e0229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Padrao EMH, Valente FS, Besen B, et al. COVIDTEAM. Awake prone positioning in COVID-19 hypoxemic respiratory failure: exploratory findings in a single-center retrospective cohort study. Acad Emerg Med 2020; 27:1249–1259. [DOI] [PubMed] [Google Scholar]
- 18.Prud’homme E, Trigui Y, Elharrar X, et al. Effect of prone positioning on the respiratory support of nonintubated patients with coronavirus disease 2019 and acute hypoxemic respiratory failure: a retrospective matching cohort study. Chest 2021; 160:85–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tonelli R, Pisani L, Tabbi L, et al. Early awake proning in critical and severe COVID-19 patients undergoing noninvasive respiratory support: a retrospective multicenter cohort study. Pulmonology 2021; doi: 10.1016/j.pulmoe.2021.03.002. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jouffroy R, Darmon M, Isnard F, et al. Impact of prone position in nonintubated spontaneously breathing patients admitted to the ICU for severe acute respiratory failure due to COVID-19. J Crit Care 2021; 64:199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu X, Liu H, Lan Q, et al. Early prone positioning therapy for patients with mild COVID-19 disease. Med Clin (Engl Ed) 2021; 156:386–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perez-Nieto OR, Escarraman-Martinez D, Guerrero-Gutierrez MA, et al. APRONOX group. Awake prone positioning and oxygen therapy in patients with COVID-19: The APRONOX study. Eur Respir J 2021; doi: 10.1183/13993003.00265-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Simioli F, Annunziata A, Langella G, et al. Early prone positioning and non-invasive ventilation in a critical COVID-19 subset. A single centre experience in Southern Italy. Turk Thorac J 2021; 22:57–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ferrando C, Mellado-Artigas R, Gea A, et al. COVID-19 Spanish ICU Network. Awake prone positioning does not reduce the risk of intubation in COVID-19 treated with high-flow nasal oxygen therapy: a multicenter, adjusted cohort study. Crit Care 2020; 24:597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sryma PB, Mittal S, Mohan A, et al. Effect of proning in patients with COVID-19 acute hypoxemic respiratory failure receiving noninvasive oxygen therapy. Lung India 2021; 38: (Suppl): S6–S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zang X, Wang Q, Zhou H, et al. Group C-EPPS: efficacy of early prone position for COVID-19 patients with severe hypoxia: a single-center prospective cohort study. Intensive Care Med 2020; 46:1927–1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnson SA, Horton DJ, Fuller MJ, et al. Patient-directed prone positioning in awake patients with COVID-19 requiring hospitalization (PAPR). Ann Am Thorac Soc 2021; 18:1424–1426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kharat A, Dupuis-Lozeron E, Cantero C, et al. Self-proning in COVID-19 patients on low-flow oxygen therapy: a cluster randomised controlled trial. ERJ Open Res 2021; 7: 00692-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor SP, Bundy H, Smith WM, et al. Awake-prone positioning strategy for non-intubated hypoxic patients with COVID-19: a pilot trial with embedded implementation evaluation. Ann Am Thorac Soc 2021; 18:1360–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jayakumar D, Ramachandran Dnb P, Rabindrarajan Dnb E, et al. Standard care versus awake prone position in adult nonintubated patients with acute hypoxemic respiratory failure secondary to COVID-19 infection-a multicenter feasibility randomized controlled trial. J Intensive Care Med 2021; 36:918–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rosen J, von Oelreich E, Fors D, et al. Awake prone positioning in patients with hypoxemic respiratory failure due to COVID-19: the PROFLO multicenter randomized clinical trial. Crit Care 2021; 25:209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Avdeev SN, Nekludova GV, Trushenko NV, et al. Lung ultrasound can predict response to the prone position in awake nonintubated patients with COVID19 associated acute respiratory distress syndrome. Crit Care 2021; 25:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen Y, Zhang J, Feng H, et al. Prone positioning in intubated and mechanically ventilated patients with SARS-CoV-2. J Clin Anesth 2021; 71:110258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shelhamer MC, Wesson PD, Solari IL, et al. Prone positioning in moderate to severe acute respiratory distress syndrome due to COVID-19: a cohort study and analysis of physiology. J Intensive Care Med 2021; 36:241–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abou-Arab O, Haye G, Beyls C, et al. Hypoxemia and prone position in mechanically ventilated COVID-19 patients: a prospective cohort study. Can J Anaesth 2021; 68:262–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khullar R, Shah S, Singh G, et al. Effects of prone ventilation on oxygenation, inflammation, and lung infiltrates in COVID-19 related acute respiratory distress syndrome: a retrospective cohort study. J Clin Med 2020; 9:4129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li J, Fink JB, Augustynovich AE, et al. Effects of inhaled epoprostenol and prone positioning in intubated coronavirus disease 2019 patients with refractory hypoxemia. Crit Care Explor 2020; 2:e0307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee RM, Tan GP, Puah SH, et al. Physiological changes during prone positioning in COVID-19 acute respiratory distress syndrome. Ann Acad Med Singap 2020; 49:509–513. [PubMed] [Google Scholar]
- 39.Mittermaier M, Pickerodt P, Kurth F, et al. Evaluation of PEEP and prone positioning in early COVID-19 ARDS. EClinicalMedicine 2020; 28:100579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Astua AJ, Michaels EK, Michaels AJ. Prone during pandemic: development and implementation of a quality-based protocol for proning severe COVID-19 hypoxic lung failure patients in situationally or historically low resource hospitals. BMC Pulm Med 2021; 21:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Berrill M. Evaluation of oxygenation in 129 proning sessions in 34 mechanically ventilated COVID-19 patients. J Intensive Care Med 2021; 36:229–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Clarke J, Geoghegan P, McEvoy N, et al. Prone positioning improves oxygenation and lung recruitment in patients with SARS-CoV-2 acute respiratory distress syndrome; a single centre cohort study of 20 consecutive patients. BMC Res Notes 2021; 14:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Douglas IS, Rosenthal CA, Swanson DD, et al. Safety and outcomes of prolonged usual care prone position mechanical ventilation to treat acute coronavirus disease 2019 hypoxemic respiratory failure. Crit Care Med 2021; 49:490–502. [DOI] [PubMed] [Google Scholar]
- 44.Gleissman H, Forsgren A, Andersson E, et al. Prone positioning in mechanically ventilated patients with severe acute respiratory distress syndrome and coronavirus disease. Acta Anaesthesiol Scand 2021; 65:360–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Robba C, Ball L, Battaglini D, et al. collaborators. Early effects of ventilatory rescue therapies on systemic and cerebral oxygenation in mechanically ventilated COVID-19 patients with acute respiratory distress syndrome: a prospective observational study. Crit Care 2021; 25:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sang L, Zheng X, Zhao Z, et al. Lung recruitment, individualized PEEP, and prone position ventilation for COVID-19-associated severe ARDS: a single center observational study. Front Med (Lausanne) 2020; 7:603943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vollenberg R, Matern P, Nowacki T, et al. Prone position in mechanically ventilated COVID-19 patients: a multicenter study. J Clin Med 2021; 10:1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Weiss TT, Cerda F, Scott JB, et al. Prone positioning for patients intubated for severe acute respiratory distress syndrome (ARDS) secondary to COVID-19: a retrospective observational cohort study. Br J Anaesth 2021; 126:48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mathews KS, Soh H, Shaefi S, et al. STOP-COVID Investigators. Prone positioning and survival in mechanically ventilated patients with coronavirus disease 2019-related respiratory failure. Crit Care Med 2021; 49:1026–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50▪▪.Scaramuzzo G, Gamberini L, Tonetti T, et al. ICU-RER COVID-19 Collaboration. Sustained oxygenation improvement after first prone positioning is associated with liberation from mechanical ventilation and mortality in critically ill COVID-19 patients: a cohort study. Ann Intensive Care 2021; 11:63. [DOI] [PMC free article] [PubMed] [Google Scholar]; A large prospective multicenter study in Italy comparing responders to nonresponders to prone in terms of oxygenation once the patients were moved back to supine. The mortality was significantly lower in responders than in nonresponders.
- 51.Wiart A, Castanares-Zapatero D, Wittebole X, et al. Prone positioning in spontaneously breathing subjects with moderate or severe ARDS during invasive ventilation. Respir Care 2021; 66:724–732. [DOI] [PubMed] [Google Scholar]
- 52.Ehrmann S, Li J, Ibarra-Estrada M, et al. Awake Prone Positioning Meta-Trial Group. Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: a randomised, controlled, multinational, open-label meta-trial. Lancet Respir Med 2021; doi: 10.1016/S2213-2600(21)00356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.