Abstract
Background:
Advance care planning (ACP) is low among older adults with cancer. In secondary analysis of randomized trial data, we compared the efficacy of the PREPARE website plus easy-to-read advance directive (AD) versus AD-only among older adults with and without cancer.
Methods:
Safety-net primary care patients in San Francisco were included if they were ≥55 years old, English- or Spanish-speaking, and had ≥2 chronic conditions. We determined cancer diagnoses using ICD-9/10 codes. The primary outcome was new ACP documentation in the medical record at 15 months; secondary outcomes were self-reported ACP engagement, ease-of-use, satisfaction, and depression/anxiety. We used mixed effects logistic and linear regression adjusted for prior ACP, health literacy, and clinician, including a cancer interaction term.
Results:
Of 986 participants, 220 (22%) had cancer; mean age was 63 (SD 6), 61% were women, 81% minority race/ethnicity, 45% Spanish-speaking, 39% had limited health literacy, 27% had prior ACP. New ACP documentation was higher in the PREPARE versus AD-only arm among participants with cancer (62% versus 43%; P=0.01) and without cancer (38% versus 28%; P=0.01), as was ACP engagement in both arms (P<0.001), with no interactions by cancer. Ease-of-use and satisfaction were high, and depression/anxiety were low, with no differences by study arm or by cancer/no cancer.
Conclusions:
PREPARE plus an easy-to-read AD increased ACP documentation and engagement among diverse, older adults with cancer more than an AD alone, with no increase in depression or anxiety between study arm or by cancer. PREPARE may help decrease ACP disparities among cancer patients.
Keywords: advance care planning, vulnerable populations, safety-net providers, healthcare disparities
Lay Summary:
Advance care planning (ACP) is the process of sharing values, goals, and preferences for medical care; yet it is low among older adults with cancer. Among 986 English- and Spanish-speaking older adults from a safety-net hospital, an interactive, multi-media, web-based ACP program (PREPARE-prepareforyourcare.org) plus an easy-to-read advance directive increased ACP documentation and engagement more than an advance directive alone. There were no differences in this increase in ACP between older adults with cancer or without cancer. Also, engaging in ACP did not result in increased depression or anxiety.
Precis:
The PREPARE for Your Care program plus an easy-to-read advance directive significantly increased new advance care planning (ACP) documentation and engagement among diverse, older adults with cancer in a safety-net setting, compared to an advance directive alone. PREPARE may help reduce ACP disparities among patients with cancer.
INTRODUCTION
Advance care planning (ACP) is a dynamic and iterative process by which adults share their values, goals, and preferences for future medical care, and may include naming a medical decision-maker, discussing goals of care with loved ones and clinicians, and completing advance directives.1 Among older adults with cancer, ACP is associated with higher patient and family satisfaction with end of life care, a higher likelihood of patients receiving care consistent with their goals, and a lower likelihood of high-intensity end-of-life care.2–5 Furthermore, studies show most older adults with cancer want to engage in ACP to have control over their care and alleviate family burden, among other reasons.6, 7 Most want to do so early—with many wishing they had done so prior to time of diagnosis—and to revisit their wishes with changes in their disease course.6 Yet, engagement in ACP is low among older adults with cancer.8 For example, it is estimated that 30-70% of patients with cancer have not had goals of care discussions with their loved ones or named a medical decision-maker, more than 75% have not had goals of care discussions with clinicians, and 50-85% have not completed advance directives.5–7 Given the low ACP engagement among older adults with cancer as well as the high morbidity and mortality associated with many cancers compared to other chronic diseases, it is imperative to evaluate efficacy of ACP programs in this population specifically.
Patient-level barriers to engagement include low awareness and knowledge about ACP,9, 10 which are significantly lower among persons of color and those with lower socioeconomic status and limited health literacy.8–10 Barriers at the clinician level include a lack of clinician training in communication and comfort in discussing ACP, limited time during visits, and concern that patients will lose hope or have increased anxiety or depression.6, 8, 11–13 Given disparities in ACP engagement and end-of-life communication, both of which contribute more broadly to disparities in cancer care, it is important to develop and test promising patient-centered ACP tools for diverse populations in particular, including persons of color and those living in poverty.14
A patient-centered, online, interactive ACP program called PREPARE for Your Care (PREPARE) plus an easy-to-read advance directive (AD) has been shown in randomized trials to increase ACP documentation in the medical record and increase self-reported ACP among diverse English- and Spanish-speaking older adults from safety-net hospitals more than an AD alone.15 Our prior qualitative work has demonstrated that PREPARE is acceptable and applicable to patients with cancer.16 However, it is unknown whether PREPARE is efficacious among diverse older adults with cancer. PREPARE was developed based on behavior change theory, acknowledging ACP as a behavior and as an iterative process, and focuses therefore on preparing patients for the medical decision-making skills needed to engage in ACP.17 Because of the challenges in prognostication and frequently changing disease course unique to many cancers,8, 11 PREPARE may be particularly beneficial for patients with cancer, whose goals and preferences are likely to change multiple times over the trajectory of their illness.
In this study, using secondary data from the prior PREPARE trial, we evaluate the efficacy of PREPARE to increase new ACP documentation in the medical record and increase self-reported ACP engagement among diverse English- and Spanish-speaking older adults with cancer compared to those without cancer. We hypothesize that the effects of PREPARE to increase ACP documentation and engagement will be greater in patients with cancer versus without cancer.
METHODS
Participants & Study Setting
This is a secondary analysis of data collected from a randomized controlled trial conducted from 2014 to 2017 evaluating the efficacy of PREPARE, a video-based, interactive ACP website plus an easy-to-read AD (PREPARE) versus an AD alone. The trial methods and results have been previously published.15, 18 Patients with cancer were not an identified subgroup of interest in the trial protocol.15 Written informed consent was obtained for all participants and the study was approved by the Institutional Review Board of the University of California San Francisco.
We recruited participants from primary care clinics in the San Francisco Health Network (SFHN), a public health delivery system. Participants were included if they were 55 years of age or older, spoke English or Spanish, had at least two chronic diseases (i.e., billing codes for conditions that require ongoing medical attention), and had two or more visits with a primary care provider in the past year and two additional clinic, emergency department, or hospital visits in the past year.15, 18 Exclusion criteria included dementia or moderate to severe cognitive impairment using validated measures,19 blindness, deafness, delirium, psychosis, active drug or alcohol abuse within the past three months, lack of a telephone, or inability to answer informed consent teach-back questions within three attempts.20 Participants were block randomized by health literacy level using a random number generator.
Cancer diagnoses were determined by International Classification of Diseases, Ninth Edition (ICD-9) and ICD-10 diagnostic codes assigned to at least one visit diagnosis in the electronic health record in the prior five years from baseline enrollment. Because ACP is an iterative process that patients with cancer prefer to start early, we did not exclude any cancer diagnoses by type or stage.
Measures
The primary outcome was new documentation of ACP in the medical record 15 months after study enrollment for patients with cancer and patients without cancer. This outcome was defined as the presence of an advance directive, living will, durable power of attorney, Physician Orders for Life-Sustaining Treatment forms, code status orders, or documented discussions with a provider about goals of care. The data collection process has been previously described.15
Secondary outcomes included the validated ACP Engagement Survey21 at baseline, 1 week, 3 months, 6 months, and 12 months by study arm and cancer group. The Survey assesses both behavior change process measures (e.g., self-efficacy and readiness assessed on a 5-point Likert scale and averaged into a 5-point score) and action measures (e.g., reported goals of care discussion, yes/no; assessed on a 0-25-point scale). We measured feasibility by assessing the retention rate at 12 months, self-reported ease of use measured on an ordinal response scale (range 1-10; 10 indicating very easy), and satisfaction by asking about comfort using the materials, helpfulness, and likelihood of recommending to others (all on a 5-point Likert scale; 5 indicating extremely). To assess potential adverse outcomes, we measured depression and anxiety at 12 months with validated questionnaires (defined as a score of ≥10 on the Patient Health Questionnaire-822 and Generalized Anxiety Disorder-723).
We assessed the following patient characteristics at baseline: self-reported age, gender, race/ethnicity, language (as well as patient-clinician language concordance for Spanish speakers), educational level, health literacy,24 health and functional status, finances, internet access at home, religion or spirituality, social support,25 marital status, desired role in decision-making, presence of a possible medical decision-maker, prior planning (i.e., burial, wills), prior engagement in ACP.
Statistical Analyses
We compared baseline characteristics using unpaired t tests, χ2 tests, or Fisher’s exact tests. We stratified all analyses by patients with cancer versus patients without cancer. For our primary outcome of ACP documentation, we used mixed effects logistic regression with fixed effects for time (baseline and 15 months), study arm (PREPARE vs AD-only), and study arm-by-time interaction. For our secondary outcomes, we used mixed effects linear regression with fixed effects for time (baseline, 1 week, 3 months, 6 months, 12 months), study arm, and study arm-by-time interaction. All models were adjusted for health literacy (as patients were block randomized by health literacy), baseline documentation of ACP (which was the only patient characteristic that differed between study arms in the parent trial),15 and any clustering effects by physician. To explore effect modification (i.e., whether PREPARE affected outcomes among patients with versus without cancer differently), we added interaction terms to the study arm-by-time variable for cancer group (yes/no). We assessed differences in retention rate by cancer group (yes/no) using a χ2 test, ease of use and satisfaction by study arm and cancer group using Wilcoxon rank-sum tests, and depression and anxiety by study arm and cancer group using analysis of variance tests. All analyses were intention-to-treat and performed using STATA version 16.0 (Stata Corp); P-values were 2-tailed, set at P<0.05 for the primary outcome and secondary outcomes and tests for interactions were Bonferroni adjusted with a P-value set at <0.025).
RESULTS
Of the 986 patients included in the study, mean age was 63 (SD 6.3), 603 (61%) were women, 797 (81%) identified as minority race or ethnicity, 445 (45%) were Spanish speakers, 387 (39%) had limited health literacy, 269 (27%) had previously engaged in ACP, and 220 (22%) had cancer (Table 1). The most prevalent types of cancer were gastrointestinal (16%), breast (16%), skin (15%), urologic (12%), hematologic (11%), and gynecologic (10%). Patients with cancer, compared to those without cancer, were older (65 versus 63 years old; P<0.001), and more likely to have been born in the United States (49 versus 40%, P=0.03), be English-speaking (64% versus 52%, P=0.002), have higher educational attainment (49 versus 41% >high school; P=0.02), have fair-to-poor self-reported health (58 versus 50%; P=0.04), and have previously completed ACP documentation (42 versus 23%; P<0.001). We further stratified each cancer group by PREPARE versus AD-only study arms, and there were no differences in patient characteristics by study arm, P>0.05 for all (data not shown).
Table 1.
Participant Characteristics.a
| Characteristicb | Cancer (n=220) | Non-Cancer (n=766) | P-value |
|---|---|---|---|
|
| |||
| Age, mean (SD) | 65 (6.4) | 63 (6.3) | <0.001 |
|
| |||
| Women, n (%) | 130 (59.1) | 473 (61.8) | 0.48 |
|
| |||
| Race/Ethnicity, n (%) | 0.12 | ||
| Latino or Hispanic | 96 (43.6) | 403 (52.6) | |
| White non-Latino or Hispanic | 53 (24.1) | 136 (17.7) | |
| Black or African American | 45 (20.5) | 133 (17.4) | |
| Asian or Pacific Islander | 16 (7.3) | 62 (8.1) | |
| Multiethnic or Other | 10 (4.5) | 32 (4.2) | |
|
| |||
| US acculturation | |||
| Place of birth, n (%) | 0.03 | ||
| United States | 108 (49.3) | 304 (39.7) | |
| South America | 2 (0.9) | 28 (3.7) | |
| Central America | 59 (26.9) | 256 (33.4) | |
| Mexico and Caribbean | 26 (11.9) | 104 (13.6) | |
| Other | 24 (11.0) | 74 (9.6) | |
| If born outside of United States, years in the United States, mean (SD) | 31 (13.8) | 27 (13.0) | 0.003 |
|
| |||
| Spanish-speaking, n (%) | 79 (35.9) | 366 (47.8) | 0.002 |
|
| |||
| Education ≤ high school, n (%) | 113 (51.4) | 463 (60.4) | 0.02 |
|
| |||
| Limited Health Literacy, n (%) | 83 (38.1) | 304 (40.2) | 0.58 |
|
| |||
| Finances, not enough to make ends meet, n (%) | 54 (24.9) | 189 (25.1) | 0.95 |
|
| |||
| Financial social standing 1-10 score, mean (SD) | 5.3 (2.1) | 5.5 (2.2) | 0.2 |
|
| |||
| Religious, fairly to extremely, n (%) | 104 (48.6) | 408 (53.6) | 0.19 |
|
| |||
| Spiritual, fairly to extremely, n (%) | 129 (59.5) | 499 (65.6) | 0.1 |
|
| |||
| Social Support | |||
| Measure of Social Support (11-55 score), mean (SD) | 37.9 (11.5) | 38.1 (11.8) | 0.79 |
| In a married or long-term relationship, n (%) | 73 (33.3) | 272 (35.6) | 0.54 |
| Have adult children, n (%) | 145 (66.5) | 591 (77.2) | 0.001 |
| Have a potential surrogate, n (%) | 212 (96.4) | 733 (95.8) | 0.72 |
|
| |||
| Health Status | |||
| Self-rated Health, fair-to-poor, n (%) | 126 (57.5) | 378 (49.5) | 0.04 |
| Instrumental activities of daily living difficulty score 0-16, mean (SD) | 3.0 (3.9) | 2.6 (3.6) | 0.11 |
| Activities of daily living difficulty score 0-12, mean (SD) | 2.1 (2.3) | 1.7 (2.1) | 0.02 |
| Depression, moderate to severe, n (%) | 31 (14.1) | 93 (12.2) | 0.45 |
| Anxiety, moderate to severe, n (%) | 29 (13.2) | 74 (9.7) | 0.13 |
|
| |||
| Low decision control preference (i.e., physicians make all medical decisions), n (%) | 20 (9.3) | 76 (10.1) | 0.73 |
|
| |||
| Access to the internet in the home, n (%) | 107 (48.6) | 386 (50.5) | 0.62 |
|
| |||
| Prior planning activities | |||
| Completed a will, n (%) | 36 (16.5) | 92 (12.1) | 0.08 |
| Made funeral arrangements, n (%) | 60 (27.5) | 172 (22.7) | 0.14 |
| Any prior ACP documentation,c n (%) | 92 (41.8) | 177 (23.1) | <0.001 |
| Legal forms and orders | 59 (26.8) | 109 (14.2) | <0.001 |
| Documented discussions | 52 (23.6) | 93 (12.1) | <0.001 |
| Baseline ACP documentation rate 12 month before intervention exposure, n (%) | 32 (14.6) | 67 (8.8) | 0.01 |
|
| |||
| Cancer diagnoses,d n (%) | |||
| Gastrointestinal | 36 (16.4) | - | |
| Breast | 34 (15.5) | - | |
| Skin | 33 (15.0) | - | |
| Urologic | 27 (12.3) | - | |
| Hematologic | 25 (11.4) | - | |
| Gynecologic | 22 (10.0) | - | |
| Unknown site | 20 (9.1) | - | |
| Skeletal & Soft Tissue | 14 (6.4) | - | |
| Lung | 11 (5.0) | - | |
| Hepatobiliary | 11 (5.0) | - | |
| Nervous system | 10 (4.6) | - | |
| Head & Neck | 8 (3.6) | - | |
| Pancreatic | 4 (1.8) | - | |
| Prostate | 3 (1.4) | - | |
| Endocrine | 3 (1.4) | - | |
| Testicular | 1 (0.5) | - | |
Percentages reported in the table correspond to denominators that correct for missing data (overall <5% missing). Missing data include: place of birth: 1 in Cancer group; limited health literacy: 2 in cancer group, 9 in non-cancer group; finances: 3 in cancer group, 13 in non-cancer group; financial social standing: 4 in cancer group, 10 in non-cancer group; religious: 6 in cancer group; 5 in non-cancer group; spiritual: 3 in cancer group; 5 in non-cancer group; measure of social support: 8 in cancer group; 21 in non-cancer group; relationship: 1 in cancer group, 1 in non-cancer group; children: 2 in cancer group; surrogate: 1 in non-cancer group; self-rated health: 1 in cancer group; 2 in non-cancer group; depression: 3 in non-cancer group; instrumental activities of daily living difficulty: 1 in cancer group; activities of daily living difficulty: 1 in cancer group; internet access: 2 in non-cancer group; completed a will: 2 in cancer group; 3 in non-cancer group; made funeral arrangements: 2 in cancer group; 7 in non-cancer group; decision control preference: 4 in cancer group, 11 in non-cancer group.
All variables are defined including reliability, validity, response options, scoring, and references in the online protocol and the published trial protocol.18
ACP = advance care planning. Any prior ACP documentation includes any prior legal forms (i.e., advance directives, durable power of attorney for health care, and Physicians Orders for Life Sustaining Treatment) and documented ACP discussions in the past 5 years (i.e., oral directives or goals of care notes by clinicians).
Cancer diagnoses were determined by International Classification of Diseases, Ninth Edition (ICD-9) and ICD-10 diagnostic codes assigned to the problem list or at least 1 visit diagnosis in the electronic health record. Gastrointestinal includes esophageal, stomach, duodenal, colorectal, and anal cancers. Skin includes melanoma, non-melanoma, and choroid cancers, and Kaposi sarcoma. Urologic includes renal, ureteral, and bladder cancers. Unknown site includes diagnostic codes “Neoplasm of unspecified nature, site unspecified,” “Encounter for antineoplastic chemotherapy,” “Secondary malignant neoplasm of mediastinum” (primary cancer unknown), and “Secondary malignant neoplasm of genital organs” (primary cancer unknown, male patient). Nervous system includes brain, spinal cord, and neurofibromatosis-related cancers. Endocrine includes neuroendocrine and adrenal cancers.
ACP Documentation
New ACP documentation at 15 months was significantly higher in the PREPARE versus AD-only arm among both participants with cancer (62% versus 43%; P=0.01) and those without cancer (38% versus 28%; P=0.01) (Figure 1). There were no significant interactions by cancer or no cancer for ACP documentation (i.e., no effect modification—PREPARE affected the outcome similarly in both groups; P=0.28).
Figure 1. New Advance Care Planning (ACP) Documentation in the Medical Record at 15 months.a.
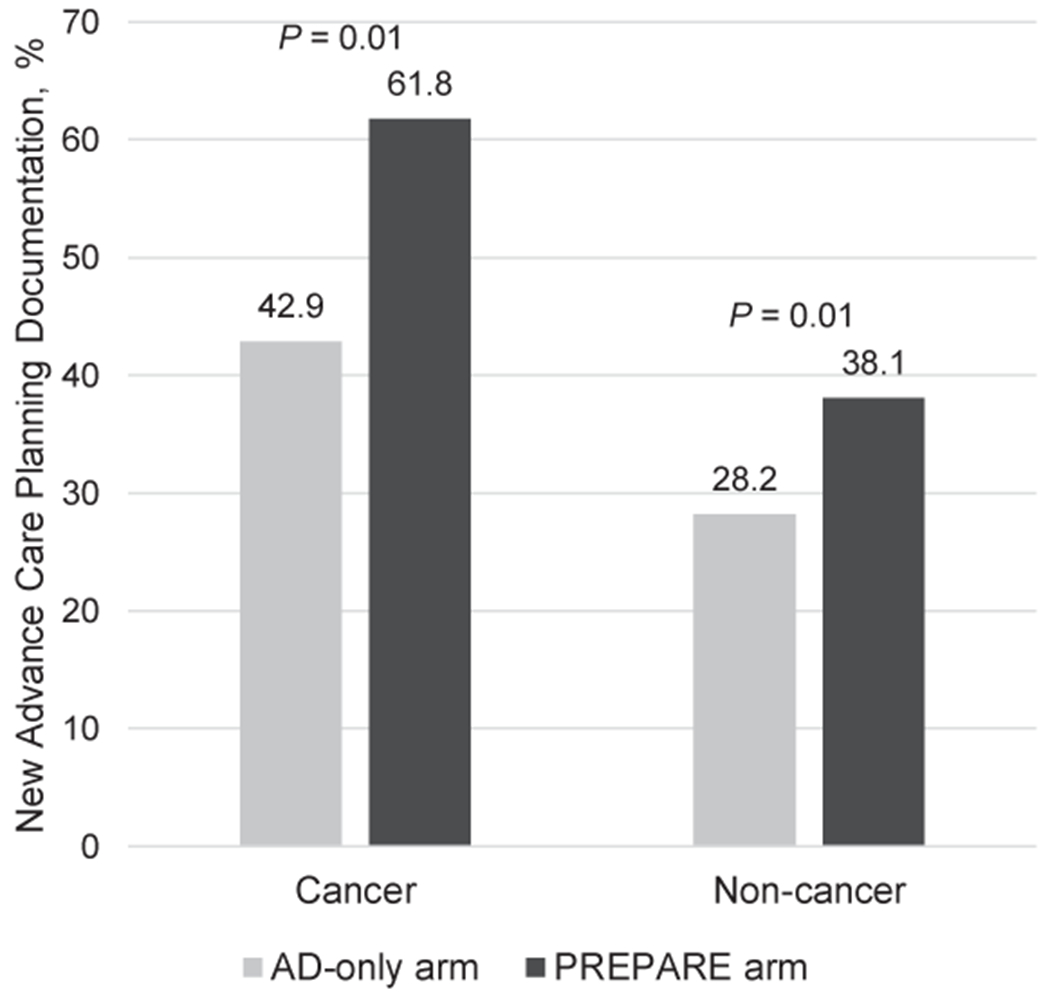
a Mixed effects logistic regression model adjusted for baseline documentation of ACP and health literacy, clustered by clinician, and stratified by cancer group.
ACP Engagement
The 5-point ACP Engagement behavior change process score from baseline to 12 months increased more in the PREPARE versus AD-only arm among participants with cancer (increased from 2.7 to 3.5 versus 2.8 to 3.2) and those without cancer (2.6 to 3.3 versus 2.6 to 3.1), P<0.001 (Figure 2). In addition, the 25-point ACP action score increased more in the PREPARE versus AD-only arm among participants with cancer (8.1 to 14.6 versus 9.4 to 12.4) and those without cancer (7.6 to 12.4 versus 7.5 to 10.6.), P<0.001. There were no significant interactions by cancer or no cancer for ACP behavior change (P=0.37) or action (P=0.20) scores (i.e., no effect modification—PREPARE affected the outcome similarly in both groups).
Figure 2. Advance Care Planning (ACP) Engagement Behavior Change Process and Action Scores.a.
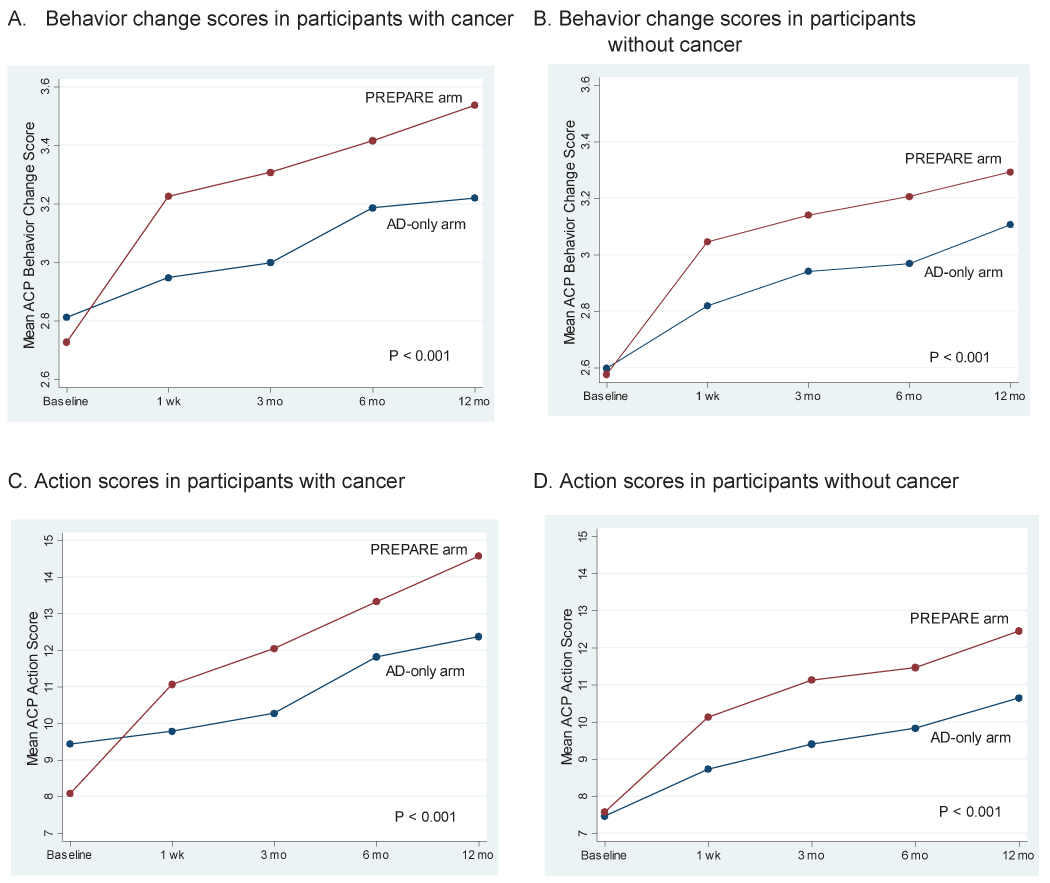
A. Behavior change scores in participants with cancer.
B. Behavior change scores in participants without cancer.
C. Action scores in participants with cancer.
D. Action scores in participants without cancer.
a Mixed effects linear regression models adjusted for baseline documentation of ACP and health literacy, clustered by clinician, and stratified by cancer group. Behavior change process scores (e.g., self-efficacy and readiness) were measured on a 5-point Likert scale and action scores (e.g., reported goals of care discussion) on a 0-25 scale.
Feasibility and Safety
The retention rate at 12 months was similar between participants with cancer (88%) versus without cancer (85%; P=0.31). Ease of use and satisfaction were rated highly among all participants, and there were no significant differences in ease of use, comfort viewing, or likelihood of recommending to others between PREPARE and AD-only arms in participants with or without cancer (Table 2). Helpfulness was rated significantly higher on a 5-point scale in the PREPARE versus AD-only arm for participants with cancer (4.4 versus 4.2; P=0.05) and without cancer (4.4 versus 4.2; P=0.001). Mean depression and anxiety scores at 12 months were low in both study arms and for both cancer groups and there were no differences by arm or group (Table 3).
Table 2. Ease of use and Satisfaction by Cancer and Non-Cancer and by Study Arm (PREPARE versus AD-only).
PREPARE = Prepare for Your Care; AD = advance directive.
| Cancer (n=220) | Non-Cancer (n=766) | |||||
|---|---|---|---|---|---|---|
| AD-only | PREPARE | P-valuea | AD-only | PREPARE | P-valuea | |
| Ease of use,b mean (SD) | 8.0 (2.0) | 8.0 (2.3) | 0.43 | 8.0 (2.2) | 8.2 (1.9) | 0.70 |
| Satisfaction,c mean (SD) | ||||||
| Comfortable viewing | 4.0 (0.9) | 4.2 (0.8) | 0.32 | 4.0 (1.0) | 4.1 (0.8) | 0.62 |
| Helpfulness | 4.2 (0.7) | 4.4 (0.6) | 0.05 | 4.2 (0.8) | 4.4 (0.7) | 0.001 |
| Recommend | 4.1 (0.8) | 4.1 (0.9) | 0.70 | 4.1 (0.9) | 4.2 (0.8) | 0.42 |
Wilcoxon rank sum tests.
Measured on a 1 (very hard) to 10 (very easy) point scale.
Measured by, “How comfortable…”, “How helpful…”, and “How likely are you to recommend this guide to others?” using a “not-at-all” to “extremely” 5-point Likert scale.
Table 3. Depression and Anxiety Scores by Cancer and Non-Cancer and by Study Arm (PREPARE versus AD-only).
Depression was measured using the validated Patient Health Questionnaire (PHQ)-8 (range 0-24) and anxiety was measured with the Generalized Anxiety Disorder (GAD)-7 (range 0-21). PREPARE = Prepare for Your Care; AD = advance directive.
| Cancer (n=220) | Non-Cancer (n=766) | |||||
|---|---|---|---|---|---|---|
| AD-only | PREPARE | P-value | AD-only | PREPARE | P-value | |
| Depression Score, meana (95% CI) | 4.8 (4.1-5.6) | 4.0 (3.1-4.8) | 0.16 | 4.1 (3.7-4.5) | 4.2 (3.8-4.7) | 0.72 |
| Anxiety Score, meana (95% CI) | 3.7 (3.0-4.3) | 3.2 (2.4-3.9) | 0.32 | 3.4 (3.0-3.7) | 3.2 (2.8-3.6) | 0.59 |
Adjusted for baseline depression and anxiety scores. Scores less than 5 represent no anxiety or depression.
DISCUSSION
PREPARE was found to be equally efficacious in increasing ACP documentation in the medical record and self-reported ACP engagement among diverse, older adults with cancer as those without cancer, and significantly more efficacious in both groups when compared to an easy-to-read AD alone. Study participants rated PREPARE and the easy-to-read AD highly in terms of ease of use and satisfaction. Notably, there were no differences in study retention or depression or anxiety between those with and without cancer.
Baseline ACP engagement was nearly twice as high among those with cancer (42%) compared to those without cancer (23%). Nevertheless, after adjusting for baseline engagement, PREPARE still increased new ACP documentation by 62% among older adults with cancer and by 38% in those without cancer. The greater increase of new ACP documentation among those with cancer compared to those without cancer, though not statistically significant, is notable, and may reflect the morbidity, mortality, and disease trajectory associated with many cancer diagnoses, even compared to other serious illness or chronic disease diagnoses. ACP is a dynamic and iterative process,1 and survey studies of patients with cancer have demonstrated that the majority prefer to readdress ACP with changes in their disease course.6, 7 Our findings reinforce this, as ACP engagement increased despite high prior engagement. PREPARE is grounded in behavior change theory and focused not only on increasing ACP engagement at a single point in time, but more broadly on equipping adults with medical decision-making skills needed to engage in ACP.17 This may have contributed to its efficacy in increasing ACP engagement over time among both groups.
The efficacy of PREPARE in increasing ACP documentation and engagement among racially, ethnically, socioeconomically, and linguistically diverse older adults has been previously demonstrated.15, 26 This study confirms that PREPARE’s benefits extend to underserved cancer patients and suggests that PREPARE may help reduce disparities in ACP and clinical care14 among this vulnerable population.8–10 Other video-based, patient-facing tools have been shown to facilitate ACP discussions and increase ACP knowledge among patients with cancer; however, these studies have included predominantly white, male patients with high educational attainment, and have not included Spanish-speakers or assessed or demonstrated an increased rate of ACP documentation.27–29 ACP communication tools focused primarily on clinician facilitators have also been shown to increase patient-clinician ACP communication.27, 30–32 However, given the limited resources for cancer patients in safety-net hospitals, a facilitated discussion may not always be possible. PREPARE may help to bridge this gap as it has been shown to empower patients to begin the ACP process on their own, and empower them to speak up and discuss ACP with their clinicians.33
Although there has been concern that ACP may increase anxiety or depression among cancer patients, overall rates were low and there were no differences in between study arms or cancer group. While other research has also shown that ACP is not associated with reduced hope or increased anxiety, clinicians’ concern that patients will lose hope if they discuss ACP remains a significant barrier to ACP engagement, particularly among patients with cancer.6, 34 Our findings underscore that ACP engagement is not associated with higher depression or anxiety. In fact, among patients with cancer, depression and anxiety were slightly lower in the PREPARE compared to the AD-only arm, though these differences did not reach statistical significance. Furthermore, participants in each group rated ease of use and satisfaction with both the easy-to-read AD and PREPARE highly. This may be because PREPARE videos depict a range of diagnoses (including non-cancer) and prognoses rather than focus specifically on end-stage cancer or end-of-life. While developing PREPARE and co-creating the materials with diverse patients and caregivers, our prior qualitative work revealed that patients with cancer preferred to review stories with a range of experiences.16 This strength of PREPARE likely contributes to both its efficacy and its acceptability among patients with cancer.
This study has some limitations. Data are from a single health system, limiting the generalizability of our findings. Nevertheless, the study population is racially, ethnically, and socioeconomically diverse. We also included individuals from a primary care clinic with a range of cancer diagnoses. Results may be different if participants were recruited from a cancer clinic or if PREPARE were studied among patients with one type of cancer diagnosis. Although helpfulness was statistically significant higher in the PREPARE arm compared to the AD-only arm, the magnitude of change was limited.
PREPARE was equally efficacious in increasing ACP documentation in the medical record and self-reported ACP engagement among diverse, older adults with cancer as those without cancer compared with an AD alone. Moreover, there were no differences in depression or anxiety between those with and without cancer. Both groups rated PREPARE and the easy-to-read AD highly in terms of ease of use, and found PREPARE to be more helpful than the easy-to-read AD. Our findings suggest that among diverse, older adults with cancer, PREPARE may help decrease health disparities related to ACP.
Acknowledgments:
This study was funded in part by the National Institute on Aging (R01 AG045043) and the Patient-Centered Outcomes Research Institute (CDR-1306-01500). Dr. Nouri is funded in part by a National Research Service Award fellowship training grant (T32HP19025). Dr. Sudore is funded in part by the National Institute in Aging (K24AG054415).
Footnotes
Conflicts of Interest:
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Sudore RL, Lum HD, You JJ, et al. Defining Advance Care Planning for Adults: A Consensus Definition From a Multidisciplinary Delphi Panel. J Pain Symptom Manage. May 2017;53(5):821–832 e1. doi: 10.1016/j.jpainsymman.2016.12.331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Detering KM, Hancock AD, Reade MC, Silvester W. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ. March 23 2010;340:c1345. doi: 10.1136/bmj.c1345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silveira MJ, Kim SYH, Langa KM Advance Directives and Outcomes of Surrogate Decision Making before Death. N Engl J Med. 2010;362(13):1211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McDermott CL, Engelberg RA, Sibley J, Sorror ML, Curtis JR. The Association between Chronic Conditions, End-of-Life Health Care Use, and Documentation of Advance Care Planning among Patients with Cancer. J Palliat Med. March 16 2020;doi: 10.1089/jpm.2019.0530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levoy K, Buck H, Behar-Zusman V. The Impact of Varying Levels of Advance Care Planning Engagement on Perceptions of the End-of-Life Experience Among Caregivers of Deceased Patients With Cancer. Am J Hosp Palliat Care. April 13 2020:1049909120917899. doi: 10.1177/1049909120917899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kubi B, Istl AC, Lee KT, Conca-Cheng A, Johnston FM. Advance Care Planning in Cancer: Patient Preferences for Personnel and Timing. JCO Oncol Pract. 2020; [DOI] [PubMed] [Google Scholar]
- 7.Waller A, Turon H, Bryant J, Zucca A, Evans TJ, Sanson-Fisher R. Medical oncology outpatients’ preferences and experiences with advanced care planning: a cross-sectional study. BMC Cancer. January 14 2019;19(1):63. doi: 10.1186/s12885-019-5272-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saraiya B, Bodnar-Deren S, Leventhal E, Leventhal H. End-of-life planning and its relevance for patients’ and oncologists’ decisions in choosing cancer therapy. Cancer. 2008;113(S12):3540–3547. doi: 10.1002/cncr.23946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nouri SS, Barnes DE, Volow AM, et al. Health Literacy Matters More Than Experience for Advance Care Planning Knowledge Among Older Adults. J Am Geriatr Soc. October 2019;67(10):2151–2156. doi: 10.1111/jgs.16129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spelten ER, Geerse O, Vuuren J, et al. Factors influencing the engagement of cancer patients with advance care planning: A scoping review. European Journal of Cancer Care. 2019;28(3)doi: 10.1111/ecc.13091 [DOI] [PubMed] [Google Scholar]
- 11.Kuusisto A, Santavirta J, Saranto K, Korhonen P, Haavisto E. Advance care planning for patients with cancer in palliative care: A scoping review from a professional perspective. J Clin Nurs. February 11 2020;doi: 10.1111/jocn.15216 [DOI] [PubMed] [Google Scholar]
- 12.Ahluwalia SC, Levin JR, Lorenz KA, Gordon HS. Missed opportunities for advance care planning communication during outpatient clinic visits. J Gen Intern Med. April 2012;27(4):445–51. doi: 10.1007/s11606-011-1917-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schickedanz AD, Schillinger D, Landefeld CS, Knight SJ, Williams BA, Sudore RL. A clinical framework for improving the advance care planning process: start with patients’ self-identified barriers. J Am Geriatr Soc. January 2009;57(1):31–9. doi: 10.1111/j.1532-5415.2008.02093.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Printz C Disparities in cancer care: Are we making progress? A look at how researchers and organizations are working to reduce cancer health disparities. Cancer. 2012;118(4):867–8. [DOI] [PubMed] [Google Scholar]
- 15.Sudore RL, Schillinger D, Katen MT, et al. Engaging Diverse English- and Spanish-Speaking Older Adults in Advance Care Planning: The PREPARE Randomized Clinical Trial. JAMA Intern Med. December 1 2018;178(12):1616–1625. doi: 10.1001/jamainternmed.2018.4657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cresswell MA, Robinson CA, Fyles G, Bottorff JL, Sudore R. Evaluation of an advance care planning web-based resource: applicability for cancer treatment patients. Support Care Cancer. March 2018;26(3):853–860. doi: 10.1007/s00520-017-3901-7 [DOI] [PubMed] [Google Scholar]
- 17.Sudore RL KS, McMahan RD, Feuz M, Farrell D, Miao Y, Barnes DE. A Novel Website to Prepare Diverse Older Adults for Decision Making and Advance Care Planning: A Pilot Study. J Pain Symptom Manage. 2013;47(4):674–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sudore RL, Barnes DE, Le GM, et al. Improving advance care planning for English-speaking and Spanish-speaking older adults: study protocol for the PREPARE randomised controlled trial. BMJ Open. July 11 2016;6(7):e011705. doi: 10.1136/bmjopen-2016-011705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Erkinjuntti T, Sulkava R, Wikström J, Autio L. Short Portable Mental Status Questionnaire as a screening test for dementia and delirium among the elderly. J Am Geriatr Soc. 1987;35(5):412–6. [DOI] [PubMed] [Google Scholar]
- 20.Sudore RL, Landefeld CS, Williams BA, Barnes DE, Lindquist K, Schillinger D. Use of a modified informed consent process among vulnerable patients: a descriptive study. J Gen Intern Med. August 2006;21(8):867–73. doi: 10.1111/j.1525-1497.2006.00535.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sudore RL, Heyland DK, Barnes DE, et al. Measuring Advance Care Planning: Optimizing the Advance Care Planning Engagement Survey. J Pain Symptom Manage. April 2017;53(4):669–681 e8. doi: 10.1016/j.jpainsymman.2016.10.367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. April 2009;114(1–3):163–73. doi: 10.1016/j.jad.2008.06.026 [DOI] [PubMed] [Google Scholar]
- 23.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch Intern Med. 2006;166(10):1092–7. [DOI] [PubMed] [Google Scholar]
- 24.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. [DOI] [PubMed] [Google Scholar]
- 25.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–14. [DOI] [PubMed] [Google Scholar]
- 26.Sudore RL, Boscardin J, Feuz MA, McMahan RD, Katen MT, Barnes DE. Effect of the PREPARE Website vs an Easy-to-Read Advance Directive on Advance Care Planning Documentation and Engagement Among Veterans: A Randomized Clinical Trial. JAMA Intern Med. August 1 2017;177(8):1102–1109. doi: 10.1001/jamainternmed.2017.1607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Agarwal R, Epstein AS. Advance Care Planning and End-of-Life Decision Making for Patients with Cancer. Semin Oncol Nurs. August 2018;34(3):316–326. doi: 10.1016/j.soncn.2018.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Volandes AE, Levin TT, Slovin S, et al. Augmenting advance care planning in poor prognosis cancer with a video decision aid: a preintervention-postintervention study. Cancer. Sep 1 2012;118(17):4331–8. doi: 10.1002/cncr.27423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.El-Jawahri A, Podgurski LM, Eichler AF, et al. Use of video to facilitate end-of-life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol January 10 2010;28(2):305–10. doi: 10.1200/JCO.2009.24.7502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Back AL, Fromme EK, Meier DE. Training Clinicians with Communication Skills Needed to Match Medical Treatments to Patient Values. J Am Geriatr Soc. May 2019;67(S2):S435–S441. doi: 10.1111/jgs.15709 [DOI] [PubMed] [Google Scholar]
- 31.Myers J, Cosby R, Gzik D, et al. Provider Tools for Advance Care Planning and Goals of Care Discussions: A Systematic Review. Am J Hosp Palliat Care. August 2018;35(8):1123–1132. doi: 10.1177/1049909118760303 [DOI] [PubMed] [Google Scholar]
- 32.Epstein AS, O’Reilly EM, Shuk E, et al. A Randomized Trial of Acceptability and Effects of Values-Based Advance Care Planning in Outpatient Oncology: Person-Centered Oncologic Care and Choices. J Pain Symptom Manage. August 2018;56(2):169–177 e1. doi: 10.1016/j.jpainsymman.2018.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Freytag J, Street RL Jr., Barnes DE, et al. Empowering Older Adults to Discuss Advance Care Planning During Clinical Visits: The PREPARE Randomized Trial. J Am Geriatr Soc. March 10 2020;doi: 10.1111/jgs.16405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Green MJ, Schubart JR, Whitehead MM, Farace E, Lehman E, Levi BH. Advance Care Planning Does Not Adversely Affect Hope or Anxiety Among Patients With Advanced Cancer. J Pain Symptom Manage. June 2015;49(6):1088–96. doi: 10.1016/j.jpainsymman.2014.11.293 [DOI] [PubMed] [Google Scholar]


