Abstract
PURPOSE
To improve the clinical effects of complete denture use and simplify its clinical application, a digital complete denture restoration workflow (Functional Suitable Digital Complete Denture System, FSD) was proposed and preliminary clinical evaluation was done.
MATERIALS AND METHODS
Forty edentulous patients were enrolled, of which half were treated by a prosthodontic chief physician, and the others were treated by a postgraduate student. Based on the primary impression and jaw relation obtained at the first visit, diagnostic denture was designed and printed to create a definitive impression, jaw relation, and esthetic confirmation at the second visit. A redesigned complete denture was printed as a mold to fabricate final denture that was delivered at the third visit. To evaluate accuracy of impression made by diagnostic denture, the final denture was used as a tray to make impression, and 3D comparison was used to analyze their difference. To evaluate the clinical effect of FSD, visual analogue scores (VAS) were determined by both dentists and patients.
RESULTS
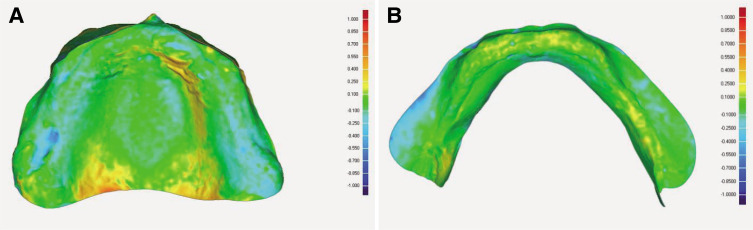
Two visits were reduced before denture delivery. The RMS values of 3D comparison between the impression made via diagnostic dentures and the final dentures were 0.165 ± 0.033 mm in the upper jaw and 0.139 ± 0.031 mm in the lower jaw. VAS ratings were between 8.5 and 9.6 in the chief physician group, while 7.7 and 9.5 in the student group; there was no statistical difference between the two groups.
CONCLUSION
FSD can simplify the complete denture restoration process and reduce the number of visits. The accuracy of impressions made by diagnostic dentures was acceptable in clinic. The VASs of both dentists and patients were satisfied.
Keywords: CAD, Complete denture, Edentulous, Removable prosthodontics, Three-dimensional printing
INTRODUCTION
Fabrication of conventional complete dentures involves a complex restoration method, requiring significant time and typically involving primary impressions, definitive impressions, jaw relation records, clinical try-in, and complete denture placement,1 which has been used for nearly a century without change. However, inexperienced dentists or students often face difficulty with achieving satisfactory retention, stabilization, and balanced occlusion of complete dentures, especially in some elderly patients and those with severe alveolar ridge absorption. In recent years, digital complete denture systems has been developed that can improve the accuracy and efficiency of denture fabrication and reduce the required number of clinic visits.2,3 These systems involve different protocols for clinical and laboratory processes, requiring two to five clinical visits.
The clinical protocols recommended by different denture systems vary. Baltic (Merz Dental GmbH)3,4 provides the least number of visits among the existing digital complete denture systems. Impressions, jaw relation records, occlusion planes, and esthetic information are all obtained at the first visit via its BD Key set, and denture can be delivered at the second visit. AvaDent (Global Dental Science LLC) and Dentca (Dentca Inc) offer a three-visit protocol.4,5,6 System-specific anatomical measuring device (AMD, AvaDent) or two-piece impression trays (Dentca) supplied by the manufacturer are used to record the jaw relationship and make the definitive impressions. Later, milled or printed monochrome trial denture is offered to clinician at the second appointment. Wieland digital denture (Ivoclar Vivadent Inc) offers a three or four appointments workflow. Based on a given primary impression and jaw relation record obtained at the patient’s first visit, the milled or printed trial complete dentures are delivered for intraoral evaluation (three appointments protocol), or a specially designed occlusion base that can install Gothic arch is milled and definitive impression and jaw relation records are determined at the second visit. Try-in dentures are given at third visit (four appointments protocol). Other systems, such as the Ceramill Full Denture System (Amann Girrbach)6 and Vita Vionic (Vita Zahnfabrik)7 still rely on conventional methods to develop custom trays and occlusion rims, but they can also apply other simplified program that only requires three or four visits. Subtraction production is the primary protocol used by the currently available commercial digital denture system: AvaDent, Ivoclar, Vita, and Ceramill FDS fabricate dentures by milling the denture base from a pink polymethyl methacrylate (PMMA) disks and bonding commercial teeth or milled teeth to it.3,8 The data-based shell geometry of Ivoclar disc and AvaDent XCL allow the fabrication of monolithic complete dentures. Ceramill FDS can provide a milled wax base with artificial teeth inserted on it, which is then transferred to acrylic, as in conventional protocols.4 Baltic mills blanks with preformed denture teeth that correspond to the dentition data contained in its own CAD software.3 Dentca uses 3D printing to fabricate the denture base with recesses into which the printed teeth are bonded.3,4
The high efficiency, reduced need for clinic visits, decreased clinical chair time, elimination of denture base polymerization shrinkage, and ability to fabricate additional dentures with existing saved data are key advantages of digital complete denture.6 However, there are still some disadvantages of current commercial digital complete denture systems. In most complete denture systems, required system-specific tools like AMD (AvaDent), two-piece trays (Dentca), BD Key set (Baltic), and facebow UTS CAD device (Ivoclar) have a learning curve for dentists and are not friendly to novices. In two-part construction for fabricating complete denture, slight movements in artificial teeth when bonded to a milled base result in increased clinical grinding, while monolithic denture fabrication requires its supporting design software and PMMA disc. Besides, in some parts of the world, the milling machine and materials are still a relatively large cost for some laboratories compared with conventional fabrication processes.4,9 CAD/CAM dentures may not be applicable in some patients: when the patient has a short interocclusal distance, tooth sockets cannot be well-generated on the denture base during design due to the insufficient prosthetic space, or the patient’s edentulous arch or dentition exceeds the range of the PMMA disc.9 Metal framework or baseplate cannot be added in the CAD/CAM denture, which is quite important for the patient with strong occlusion who needs the metal to strengthen the denture. Therefore, the purpose of this study was to establish a digital complete denture system (Functional Suitable Digital Complete Denture System, FSD), which can reduce the number of visits, does not require specific supporting tools, has a wide range of applications (not limited by the size of the dental arch and can add a metal mesh into denture base), and has a low cost for those regions where CAD/CAM fabrication fees are more expensive than that of conventional processing. In this system, a closed mouth custom trays in the shape of complete dentures were designed and printed based on the primary impression and jaw relation obtained at the first visit. These were used to make definitive impression, jaw relation and esthetic confirmation, so the denture could be delivered in the third visit. Forty clinical cases were included in this study and preliminary clinical outcomes were evaluated.
MATERIALS AND METHODS
Forty edentulous patients were enrolled and randomly divided into two groups, in which 20 were treated by a chief physician and the other 20 were treated by a postgraduate student. All patients were treated using FSD technology. Written informed consents were provided by all participants. Inclusion criteria were that all the teeth were extracted more than 3 months prior. Exclusion criteria were comorbid illness resulting in inability to care for patients themselves, any denture material allergies, severe oral mucosal disease not effectively treated or controlled, and pharyngeal reflex sensitivity causing inability to tolerate impression making. For their participation, all patients received treatment and processing of their complete dentures for free.
Upon their first visit, the primary impressions were made using commercial aluminum trays suitable for the patient’s arch form with impression compound (Shanghai Rongxiang Dental Material Co. Ltd., Shanghai, China). The jaw relation was recorded using the following steps: first, the patient’s occlusal vertical dimension was determined by 2 mm subtraction from rest vertical dimension (the distance between the nasal point and chin point). Next, a softened impression compound was placed on the back of the upper aluminum tray and was set into the patient’s mouth. Patient was told to bite until the distance between the two points reached the previously measured occlusal vertical dimension. The impression compound was only placed in the posterior arch area and the patient was told to bite repeatedly, to avoid habitual protrusion due to contact in the anterior arch area. Silicone rubber impressions can be used in the jaw relation record (Fig. 1A, B) to improve its accuracy (optional, not necessary). The lip support was adjusted, and midline, maxillary canine line, the smile line, and upper lip line were drawn using a marker pen (Fig. 1C). If the patient has full lip support, the labial area of the tray can be cut off in advance so that it can be shaped to the appropriate lip support (Fig. 1D). The primary impressions and jaw relation records were scanned with a 3D dental cast scanner (Dentscan Y500; Nanjing Geosmart3D Information Technology Co. Ltd., Nanjing, China).
Fig. 1. (A) Maxillary primary impression, (B) primary jaw relation record, (C) esthetic information acquired in the first visit, (D) labial area of the tray can be cut off in advance to form the lip support.
Scan data were imported into a reverse engineering software (Geomagic Studio 2013, Raindrop Geomagic, Rockhill, SC, USA). The extraneous area was deleted from the obtained occlusal impression to avoid the interference of the other area on registration. The occlusal impression remained fixed and the lower impression was set as floating, and n-point registration was used for the alignment of occlusal impression and lower impression (Fig. 2A). The registered maxillary and mandibular impression and labial esthetic information data were imported into a complete denture design software (Hoteamsoft Co. Ltd., Jinan, China) for designing diagnostic complete dentures (Fig. 2B, C). These dentures were used for impression making, having the characteristics of custom trays: the border of diagnostic dentures was retreated 2 mm for the space of border molding, offsetting the intaglio surface of the diagnostic dentures 1 mm for impression materials, and the hemispherical tissue stops were set to ensure the correct positioning of diagnostic dentures when making impressions (Fig. 2D). The diagnostic dentures were printed using a 3D printer (Lingtong I, 0.8 mm diameter nozzle; Beijing SHINO, Beijing, China) with the materials of polylactic acid at a print layer thickness of 0.2 mm (Fig. 3A, B).
Fig. 2. Design of diagnostic denture. (A) registration of jaw relationship (the data in the upper left corner corresponds to the occlusion record in Fig. 1B), (B) registered impression and esthetic information data were imported into CAD software, (C) selection of dentition, (D) intaglio surface of diagnostic denture.
Fig. 3. (A) Intaglio surface of printed upper diagnostic denture, (B) intaglio surface of printed lower diagnostic denture, (C) try-in of diagnostic denture, (D) definitive impression and jaw relation.
In the second visit, the printed complete diagnostic denture was used to assess the border, vertical dimension and occlusion (Fig. 3C). The vertical dimension can be adjusted by grinding the teeth or adding wax on the teeth. The occlusion can be adjusted by grinding to achieve stability. Lip support, teeth midline, and the length and size of the teeth were all checked and some adjustments were made if either the patient or dentist was unsatisfied with the esthetic quality of the dentures. After this, heavy body silicone (Type 1; Shandong Huge Dental Material Corporation, Rizhao, China) was used for border molding, and light body silicone (Type 3; Shandong Huge Dental Material Corporation, Rizhao, China) was used to create a definitive impression and record the jaw relation (Fig. 3D).
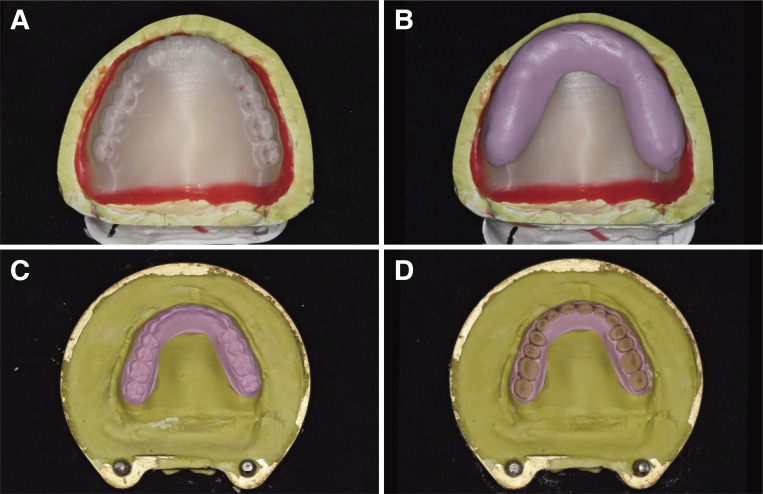
Definitive impressions were scanned to design a complete denture and was printed as a mold using a 3D printer (Lingtong II, 0.4 mm diameter nozzle; BeijingSHINO, Beijing, China). The printed denture was affixed to the plaster model perfused by the definitive impression, where the dentition was embedded with a thin layer of silicone rubber. Next, after flasking, the printed denture was removed and artificial teeth (Kaili series, Shandong Huge Dental Material Corporation, Rizhao, China) corresponding to the teeth selected in the design were inserted into the holes formed by the printed denture (Fig. 4). Then, conventional technique was done: filling acrylic resin (Type 2-1; Shandong Huge Dental Material Corporation, Rizhao, China), boiling, deflasking, occlusal adjustment with remounting the dentures on an articulator, and polishing to finish the denture fabrication.
Fig. 4. (A) Printed denture affixed to the plaster model, (B) invest the dentition with silicone, (C) denture was removed to form the mold of complete denture, (D) artificial tooth inserted into the teeth location holes.
Dentures were delivered to patients at their third visit (Fig. 5). Some clinical indicators such as retention, stability, margin extension, pronunciation, and esthetics were assessed and the dentist (another dentist) assigned dentures a Visual Analogue Score (VAS) (Table 1). As with the conventional process of denture delivery, the denture was adjusted by the clinician to appropriate.
Fig. 5. Complete denture delivery.
Table 1. Denture score criteria for patients.
| Items | 8 - 10 | 6 - 7 | < 6 |
|---|---|---|---|
| Overall satisfaction | Satisfied | General satisfied | Not satisfied |
| Masticatory efficiency | Able to eat normally | Can chew most food but difficulty chewing vegetables and other fibrous foods | Can only chew crispy foods |
| Stability | No dislodgement when speaking/with large muscle movement/eating | Dislodgement with large muscle movements/eating sticky food | Easily dislodged while speaking/eating |
| Comfort | No tenderness, no discomfort | Discomfort and tenderness after wearing dentures for a little longer | Excessive discomfort and tenderness in the alveolar mucosa |
| Pronunciation | Having little or no effect on pronunciation. | Affecting pronunciation but acceptable | Unacceptable |
| Esthetics | Satisfaction | Acceptable | Unacceptable |
Patients were told to return for denture adjustments once a week. When the dentures were adjusted properly, patients were told to provide VASs next week. At the time the patients provided the VASs, the final appropriate dentures were used as trays to make impressions (Type 3; Shandong Huge Dental Material Corporation, Rizhao, China) to evaluate the precision of impressions made with the diagnostic dentures and were then scanned to save as .stl files.
The following data were collected for analysis.
(1) The number of visit until denture delivery, and return visit after denture delivery (visits for patients to provide VASs alone were not included).
(2) Impression accuracy: the data of impressions obtained using diagnostic dentures and final dentures were imported into Geomagic software in which the diagnostic denture impressions were registered to the final denture impression using the best fit alignment. 3D comparison was then performed and the root mean square value (RMS value) was recorded. The margin extension area was excluded for 3D comparison because there was no space for border molding when making impression using final dentures.
(3) Patients’ evaluation of complete dentures: the retention, stability, masticatory efficiency, comfort, and esthetics of the dentures were evaluated by the patients. The highest score for each item was 10 points and the lowest score was 0 points. Satisfaction score criteria are shown in Table 1. Each patient was asked to carefully read the score table before scoring.
(4) Dentist’s evaluation of complete dentures: the tissue surface adaptation, retention, stability, and border extension of all complete denture were evaluated by a dentist via the VAS (Table 2). To ensure consistency and objectivity, all questionnaires were completed by another dentist (non-operating dentist).
Table 2. Dentists’ denture scoring criteria.
| Items | Content | 8 - 10 | 6 - 7 | < 6 |
|---|---|---|---|---|
| Tissue surface adaptation | Amount of grinding, grinding time | Little | Some | Excess |
| Retention | Dislocation when the dentures were pulled in the direction of insertion after wearing | Obvious resistance | Some resistance, dentures easily dislocated | No resistance, easily dislocated |
| Stability | Pressure exerted on the first molar at the same time, apply pressure and rotational force separately | Stable without movement | Some movement | Shifting and sliding |
| Border extension of denture base | Labial, buccal, and lingual borders reached sulcus; posterior area of upper denture reached vibrating line; posterior of lower denture reached 1/2 of retromolar pad; denture base border morphology fit with soft tissue morphology | All consistent | Consistent with three criteria | Consistent with two or fewer criteria |
The results of all scoring in two groups were statistically analyzed using the two-independent Samples Nonparametric Test (Mann-Whitney U Test).
RESULTS
The average age of the 40 examined patients was 73 years old. Patients included 21 males and 19 females, in which 22 of them had old complete denture (10 in chief physician group and 12 in student group). The number of patients with alveolar ridge Atwood class III/IV absorption (most of the alveolar ridge absorbed or reached the basal bone) was 8 in the chief physician group and 5 in postgraduate group. The average number of visits before dentures insertion was 3.1 and the return visit number was 1.2 in the chief physician group. One patient had a small mouth opening and unstable mandible, so a visit was added for try-in denture; one patient’s facial midline was inconsistent with the lip midline, and the patient thought the midline was skewed after the denture delivery, so we reworked once. The average number of visits for the postgraduate group before dentures insertion was 3.3 times, and the return visits was 1.6 times. Two patients had high requirements for esthetics, one patient had severe absorption of the mandibular alveolar ridge, and the other patient had an unstable jaw relationship, so they added another visit for try-in denture; one denture was reworked due to the inappropriate jaw relation.
Impression precision analyses revealed that the RMS value of 3D deviation between the impressions made via diagnostic dentures and the final dentures were 0.165 ± 0.033 mm in the upper jaw and 0.139 ± 0.031 mm in the lower jaw (Fig. 6). VAS scores of dentist and patients were shown in Table 3 and Fig. 7. There was no statistical difference between the two groups of each item (P > .05).
Fig. 6. 3D comparison between the impressions made by diagnostic denture and complete denture. (A) upper jaw, (B) lower jaw.
Table 3. VAS scores of dentist and patients.
| Items | Chief physician group | Postgraduate group | |
|---|---|---|---|
| Score of dentist | Tissue surface adaptation | 9.2 ± 0.9 | 9.1 ± 1.0 |
| Retention (upper) | 9.6 ± 0.7 | 9.5 ± 1.1 | |
| Retention (lower) | 8.6 ± 1.4 | 7.7 ± 1.0 | |
| Stability (upper) | 9.6 ± 0.6 | 9.4 ± 0.9 | |
| Stability (lower) | 8.5 ± 1.4 | 8.4 ± 1.2 | |
| Border extension | 9.5 ± 1.0 | 9.1 ± 1.4 | |
| Score of patients | Overall satisfaction | 9.0 ± 0.9 | 8.9 ± 0.7 |
| Masticatory efficiency | 8.7 ± 1.2 | 8.3 ± 1.1 | |
| Stability (upper) | 9.6 ± 0.6 | 9.5 ± 0.7 | |
| Stability (lower) | 8.9 ± 1.3 | 8.4 ± 1.4 | |
| Comfort | 9.0 ± 1.1 | 8.7 ± 1.0 | |
| Pronunciation | 9.5 ± 1.1 | 9.4 ± 1.1 | |
| Esthetics | 9.6 ± 1.0 | 9.5 ± 0.7 | |
Fig. 7. VAS scores of dentist and patients. (A) score of patients, (B) score of dentist.
DISCUSSION
The core of FSD is a diagnostic denture that replaces the custom trays, occlusion rims and try-in dentures of conventional restoration process. All information used to design diagnostic dentures including the primary impression, jaw relation, and esthetic information can be obtained only by using the conventional edentulous tray without redundant tools. The software used for designing diagnostic denture and complete denture was co-developed by the research group and company. Hundreds of denture templates are built in, which can automatically match the most appropriate dentition during design. In order to make the diagnostic dentures with the function of making impressions, the relevant functions of the tray design were added to the software, such as the automatic return of the edge line, the offset of the intaglio surface to form the space of impression materials, and the addition of the tissue stops. When using diagnostic dentures to record jaw relations, good retention between the impression and the mucosa renders the recording of the jaw relation more stable and reliable compared with conventional occlusion rim records, and it is easier for dentists to judge whether jaw relations are correct and stable by observing the position of dentition. Closed-mouth impressions have shown good clinical performance across many studies.10 Rignon-Bret et al.11 have found that the thickness of the closed-mouth impression was more uniform compared with that of the open-mouth impression made by appropriate complete denture using different manipulation, and the force of closed-mouth impression was concentrated on the back 1/3 of the arch that was consistent with the masticatory force direction. Therefore, the author proposed that the patient’s occlusal force should be used whenever the trays are adapted to the occlusion. Jung et al.12 showed that the 3D comparisons between the impression made by self-designed closed-mouth custom trays and conventional open-mouth custom trays were 0.03 - 0.34 mm, and there was no significant difference between the two impressions. In our study, the final adjusted dentures were relieved at the incisive papilla, palatal suture and obvious bulge of bone, so the intaglio surfaces were not suitable for direct comparison with the impressions. Therefore, the final dentures were used as trays to make impressions, which is considered to be an accurate impression making method in clinic. The impression was made one week after the denture was adjusted properly and the mucosa was completely restored to a healthy state. The RMS values of 3D comparison between the impression made by final denture and diagnostic denture were all within 0.2 mm in this study, which is within the clinically acceptable range of 0.3 mm.13 Sources of impression accuracy error include impression error, scanner error, and the scope of selected impression area for software deviation assessment. To reduce the error noted above and ensure consistency in the experimental results, all impressions made via diagnostic dentures and final dentures in the present study were completed by one dentist. The scanning accuracy of the scanner used in this experiment is less than 20 µm that can be considered negligible. The margin area was not selected for deviation analysis, and the border extension was evaluated using the VAS.
Previous studies have shown that shorter clinic and laboratory time was needed in digital complete denture protocol compared with conventional restoration,14,15,16 and the digital denture process was preferred by predoctoral dental students.15 The main purpose of this study was to preliminarily evaluate whether FSD is feasible in clinic and whether it can achieve good restoration for dentists with different experience. Therefore, the chief physician and postgraduate student, representing two groups of dentists with more and less clinic experience, were selected to verify the feasibility of the technology. The average number of visits for patients in the two groups from the first appointment to denture delivery was 3.1 (chief physician group) and 3.3 (postgraduate group), respectively, and the average return visits were 1.2 and 1.6 in two groups. For beginners, some patients with high esthetic requirements or unstable jaw relationship required an additional appointment for denture try-in to reduce the probability of rework. Although one visit was added, the number of visits was still less than that of conventional treatment. It can be seen from the VASs questionnaire, the scores for border extension were all above 9, indicating that border extension of the impression made by this method achieved satisfied outcomes. For patients, masticatory efficiency earned the lowest score, and esthetics and stability of upper denture got higher score. Relatively, for dentists, the upper jaw achieved good retention and stability in almost all patients, and the lower denture retention earned the lowest score. Major possibilities are related to the patient’s own alveolar ridge condition, especially the patients with alveolar ridge class III and IV absorption. Previous studies have shown that the satisfaction of digital complete denture restoration can reach 80%,17,18 and our result was higher than this, which may be related to many subjective factors such as no fees charged. There was no statistical difference in scores between the two groups indicating that even students with little experience could use FSD technology to accomplish complete denture restoration. However, it still can be seen that the score of the postgraduate group is significantly lower than that of the chief physician group; this indicates that the impression making, jaw relation record, and esthetic conformation still relies on traditional skills although the digital method can reduce the clinical time. These suggest that if we can get rid of the use of physical entities to get the impression and jaw relationship, dentists’ experience dependence will be further reduced. In this way, intraoral scanners seem to be a viable option. However, due to the flatness of the mucosal surface and lack of landmarks that can be recognized by software in edentulous patients, significant errors or even split layers in calculating edentulous mucosa data when using an intraoral scanner may occur, and the accuracy of various intraoral scanners in scanning edentulous jaws exceeds the clinically acceptable range of 0.3 mm.12 Besides, it is difficult to determine the proper and stable morphology of the vestibule extension area in edentulous patients, and removing the extension area of the edentulous intraoral impression can significantly improve the accuracy, but its integrity will be greatly affected.19 Although some dentists have used intraoral scanners in complete denture restoration, relining the denture is still needed for the lower jaw.20,21,22 Some dentists also use intraoral scanning of the edentulous jaw data to fabricate custom trays.23 Intraoral scanning technology needs further development, however, and may soon rival impressions in accuracy and precision, though the margin extension is still an intractable problem.
Considering the cost and efficiency of technology application, FDM printing technique was used in FSD protocol. The printing materials polylactic acid (PLA) is a biodegradable material with good biocompatibility, which finally produces carbon dioxide and water after degradation.24 In dentistry, it is often used to print models, mold, custom trays, occlusion rims, and try-in dentures.25,26,27 In this protocol, FDM printer was used to print diagnostic denture and complete denture patterns as a mold for fabrication of dentures using conventional laboratory techniques like pack&press or injection molding. This technique can guarantee the proper position of teeth and is also suitable for the patient with short vertical dimension because the base of artificial teeth can be grinded before inserting into teeth sockets. In addition, if the patient requires metal framework or baseplate in the denture to improve the suitability and strength, this metal reinforcing structure can be added during the semi-digital denture fabrication. However, the polymerization shrinkage and monomer residuals cannot be avoided, so the dentures should be ground on an articulator by a technician to decrease the error generated during the denture fabrication. Our results demonstrated that dentures fabricated using this technique had earned good scores on retention and suitability. Therefore, a semi-digital denture fabrication with cheap 3D printer and materials was used in our protocol, which could be more economical for use in the areas where milling protocol is much more expensive than conventional technique.
There are still some improvements to be made to FSD. The final denture fabrication was not fully digitized and the denture base was still made using conventional methods. Previous researches have showed that dentures with a volumetric shrinkage of approximately 7% and linear shrinkage of 0.9% could be produced with compression molding technique.28,29 Besides, a fused deposition modeling (FDM) printer was used to print the denture pattern, which may not be as accurate as SLA/DLP printer, but the machines and materials are cheaper and may allow more people to use this technology to fabricate complete denture. Additionally, if there was a large deviation in the primary jaw relation during the first visit, inappropriate occlusion could occur in the diagnostic denture, and it will take more time to adjust the jaw position, which brings difficulty to the operation. Considering the small sample size of our study, further clinical effects remain to be confirmed by larger clinical trials, and more comparisons will be included, such as conventional technology and other digital technologies.
There is still a long way to fully digitize the complete denture restoration, including clinical and laboratory processes. In clinical operation, impression and jaw relation record are still needed. Intraoral scanning and mandibular movement device are a feasible method, but it still needs the maturity of technology and the exploration of process. In the laboratory process, compared with conventional denture processing or subtractive processing, 3D printing technology has been valued and carried out in many related researches because it is not limited by size, is suitable for complex shapes, and does not waste materials. However, it is currently mostly used for auxiliary restoration or temporary restoration, and its advantages are not recognized due to its limited strength, wear resistance, esthetics, etc. If 3D printers are manufactured at a lower price and higher strength than those produced by milling systems, the application of 3D printing can be further expanded.26,30 In the future, an integrated, printed, multi-color complete denture that meets the requirement of strength, abrasion resistance, esthetics, and biosafety is expected which, if realized, might allow chair-side creation of dentures that patients could receive upon their first visit.
CONCLUSION
FSD is a digital complete denture technique that can reduce two visits. The impressions made by diagnostic dentures were within clinically acceptable range. Primary clinical evaluations revealed that FSD dentures achieved good fitness, stable retention, and suitable border extension. The scores of chief physician were higher than those of postgraduate student, but there was no statistical difference, indicating that FSD technology is also very friendly to novices, but there is still a certain degree of experience reliance. Less experience-dependent digital technology for complete denture restoration needs to be studied in the future.
Footnotes
This study was supported by the National Key R&D Program of China (2018YFB1106900); Beijing Training Project for the Leading Talents in S & T (Z191100006119022); PKU-Baidu Fund (2019BD021).
References
- 1.Basker RM, Davenport JC, Thomason JM. Prosthetic treatment of the edentulous patient. 5th ed. Wiley-Blackwell; 2011. pp. 130–219. [Google Scholar]
- 2.Bidra AS, Taylor TD, Agar JR. Computer-aided technology for fabricating complete dentures: systematic review of historical background, current status, and future perspectives. J Prosthet Dent. 2013;109:361–366. doi: 10.1016/S0022-3913(13)60318-2. [DOI] [PubMed] [Google Scholar]
- 3.Schweiger J, Stumbaum J, Edelhoff D, Güth JF. Systematics and concepts for the digital production of complete dentures: risks and opportunities. Int J Comput Dent. 2018;21:41–56. [PubMed] [Google Scholar]
- 4.Baba NZ, Goodacre BJ, Goodacre CJ, Müller F, Wagner S. CAD/CAM complete denture systems and physical properties: a review of the literature. J Prosthodont. 2021;30:113–124. doi: 10.1111/jopr.13243. [DOI] [PubMed] [Google Scholar]
- 5.Baba NZ, AlRumaih HS, Goodacre BJ, Goodacre CJ. Current techniques in CAD/CAM denture fabrication. Gen Dent. 2016;64:23–28. [PubMed] [Google Scholar]
- 6.Baba NZ. Materials and processes for CAD/CAM complete denture fabrication. Current Oral Health Rep. 2016;3:203–208. [Google Scholar]
- 7.Steinmassl PA, Klaunzer F, Steinmassl O, Dumfahrt H, Grunert I. Evaluation of currently available CAD/CAM denture systems. Int J Prosthodont. 2017;30:116–122. doi: 10.11607/ijp.5031. [DOI] [PubMed] [Google Scholar]
- 8.Bonnet G, Batisse C, Bessadet M, Nicolas E, Veyrune JL. A new digital denture procedure: a first practitioners appraisal. BMC Oral Health. 2017;17:155. doi: 10.1186/s12903-017-0440-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maragliano-Muniz P, Kukucka ED. Incorporating digital dentures into clinical practice: flexible workflows and improved clinical outcomes. J Prosthodont. 2021;30:125–132. doi: 10.1111/jopr.13277. [DOI] [PubMed] [Google Scholar]
- 10.Felton DA, Cooper LF, Scurria MS. Predictable impression procedures for complete dentures. Dent Clin North Am. 1996;40:39–51. [PubMed] [Google Scholar]
- 11.Rignon-Bret C, Mushegyan V, Naveau A. On comparing two different tray-holding techniques for edentulous maxillary impressions. Int J Prosthodont. 2016;29:169–172. doi: 10.11607/ijp.4347. [DOI] [PubMed] [Google Scholar]
- 12.Jung S, Park C, Yang HS, Lim HP, Yun KD, Ying Z, Park SW. Comparison of different impression techniques for edentulous jaws using three-dimensional analysis. J Adv Prosthodont. 2019;11:179–186. doi: 10.4047/jap.2019.11.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ishinabe S. Mucosal thickness of the denture foundation under occlusal force. J Japan Prosthodont Soc. 1991;35:111–124. [Google Scholar]
- 14.Smith PB, Perry J, Elza W. Economic and clinical impact of digitally produced dentures. J Prosthodont. 2021;30:108–112. doi: 10.1111/jopr.13283. [DOI] [PubMed] [Google Scholar]
- 15.Kattadiyil MT, Jekki R, Goodacre CJ, Baba NZ. Comparison of treatment outcomes in digital and conventional complete removable dental prosthesis fabrications in a predoctoral setting. J Prosthet Dent. 2015;114:818–825. doi: 10.1016/j.prosdent.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Srinivasan M, Schimmel M, Naharro M, O’Neill C, McKenna G, Müller F. CAD/CAM milled removable complete dentures: time and cost estimation study. J Dent. 2019;80:75–79. doi: 10.1016/j.jdent.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Bidra AS, Farrell K, Burnham D, Dhingra A, Taylor TD, Kuo CL. Prospective cohort pilot study of 2-visit CAD/CAM monolithic complete dentures and implant-retained overdentures: Clinical and patient-centered outcomes. J Prosthet Dent. 2016;115:578–586.e1. doi: 10.1016/j.prosdent.2015.10.023. [DOI] [PubMed] [Google Scholar]
- 18.Kattadiyil MT, Jekki R, Goodacre CJ, Baba NZ. Comparison of treatment outcomes in digital and conventional complete removable dental prosthesis fabrications in a predoctoral setting. J Prosthet Dent. 2015;114:818–825. doi: 10.1016/j.prosdent.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 19.Lo Russo L, Caradonna G, Troiano G, Salamini A, Guida L, Ciavarella D. Three-dimensional differences between intraoral scans and conventional impressions of edentulous jaws: A clinical study. J Prosthet Dent. 2020;123:264–268. doi: 10.1016/j.prosdent.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 20.Fang JH, An X, Jeong SM, Choi BH. Digital immediate denture: A clinical report. J Prosthet Dent. 2018;119:698–701. doi: 10.1016/j.prosdent.2017.06.004. [DOI] [PubMed] [Google Scholar]
- 21.Goodacre BJ, Goodacre CJ, Baba NZ. Using intraoral scanning to capture complete denture impressions, tooth positions, and centric relation records. Int J Prosthodont. 2018;31:377–381. doi: 10.11607/ijp.5741. [DOI] [PubMed] [Google Scholar]
- 22.Unkovskiy A, Wahl E, Zander AT, Huettig F, Spintzyk S. Intraoral scanning to fabricate complete dentures with functional borders: a proof-of-concept case report. BMC Oral Health. 2019;19:46. doi: 10.1186/s12903-019-0733-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kanazawa M, Iwaki M, Arakida T, Minakuchi S. Digital impression and jaw relation record for the fabrication of CAD/CAM custom tray. J Prosthodont Res. 2018;62:509–513. doi: 10.1016/j.jpor.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 24.Dawood A, Marti Marti B, Sauret-Jackson V, Darwood A. 3D printing in dentistry. Br Dent J. 2015;219:521–529. doi: 10.1038/sj.bdj.2015.914. [DOI] [PubMed] [Google Scholar]
- 25.Chen H, Yang X, Chen L, Wang Y, Sun Y. Application of FDM three-dimensional printing technology in the digital manufacture of custom edentulous mandible trays. Sci Rep. 2016;6:19207. doi: 10.1038/srep19207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kihara H, Sugawara S, Yokota J, Takafuji K, Fukazawa S, Tamada A, Hatakeyama W, Kondo H. Applications of three-dimensional printers in prosthetic dentistry. J Oral Sci. 2021;63:212–216. doi: 10.2334/josnusd.21-0072. [DOI] [PubMed] [Google Scholar]
- 27.Wagner SA, Kreyer R. Digitally fabricated removable complete denture clinical workflows using additive manufacturing techniques. J Prosthodont. 2021;30:133–138. doi: 10.1111/jopr.13318. [DOI] [PubMed] [Google Scholar]
- 28.Jovanović M, Živić M, Milosavljević M. A potential application of materials based on a polymer and CAD/CAM composite resins in prosthetic dentistry. J Prosthodont Res. 2021;65:137–147. doi: 10.2186/jpr.JPOR_2019_404. [DOI] [PubMed] [Google Scholar]
- 29.Parvizi A, Lindquist T, Schneider R, Williamson D, Boyer D, Dawson DV. Comparison of the dimensional accuracy of injection-molded denture base materials to that of conventional pressure-pack acrylic resin. J Prosthodont. 2004;13:83–89. doi: 10.1111/j.1532-849X.2004.04014.x. [DOI] [PubMed] [Google Scholar]
- 30.Schweiger J, Edelhoff D, Güth JF. 3D printing in digital prosthetic dentistry: an overview of recent developments in additive manufacturing. J Clin Med. 2021;10:2010. doi: 10.3390/jcm10092010. [DOI] [PMC free article] [PubMed] [Google Scholar]