Abstract
Purpose
To evaluate the effectiveness of Janus kinase (JAK) inhibitors for the treatment of patients with autoimmune disease and associated inflammatory ocular diseases.
Methods
We identified relevant literature by screening the MEDLINE, PubMed, and Cochrane databases for randomized controlled trials, cohort studies, case controls, and case reports.
Results
Seven studies, including 11 patients, were included in the final systematic analysis. Of the 11 patients, there were 5 cases of juvenile idiopathic arthritis- (JIA-) associated uveitis, 1 case of rheumatoid arthritis- (RA-) associated keratitis, 1 case of RA-associated scleritis, 1 case of psoriasis-associated conjunctivitis, 2 cases of noninfectious scleritis, and 1 case of uveitis with suspected autoimmune disease. None of these 11 patients responded adequately to conventional treatments, including biological agents; these were all refractory cases and switched to JAK inhibitor therapy. Irrespective of whether they were suffering from uveitis, scleritis, or other types of ocular inflammation, all 11 patients showed an improvement to JAK inhibitors without significant side effects. Different types of JAK inhibitors might be associated with different responses when used to treat ocular inflammation.
Conclusions
JAK inhibitors may represent an alternative treatment option for patients with autoimmune ocular inflammation.
1. Introduction
Noninfectious inflammatory ocular diseases can occur in isolation or in the context of systemic autoimmune diseases, such as rheumatoid arthritis (RA), juvenile idiopathic arthritis (JIA), ankylosing spondylitis (AS), and systemic vasculitis (SV). Ocular inflammation includes a diverse group of ocular inflammatory diseases that frequently present in the form of scleritis, keratitis, uveitis, conjunctivitis, and retinitis; these conditions can lead to a number of other vision-threatening ocular complications.
Currently, the traditional treatments for such ocular complications are nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and conventional disease-modifying antirheumatic drugs (cDMARDs) [1]. However, some patients are nonresponsive to such therapies. Several classes of biological agents have been reported to control ocular inflammation, including TNF-alpha blockers, tocilizumab, and rituximab [2–5]. However, the literature also reports that some severe cases were refractory and failed to reach remission [2, 3].
The Janus kinase (JAK) pathway plays a key role in inflammatory cell regulation, cytokine production, and proinflammatory signal transduction [6, 7]. Dysregulation of the JAK pathway is associated with the pathogenesis of various inflammatory and autoimmune disorders. Therefore, JAK inhibitors have the potential to alleviate the inflammatory process. However, the applications of JAK inhibitors are relatively new in terms of clinical therapy, particularly for autoimmune diseases. Study data is not abundantly available for this particularly field-of-interest. In this study, we aimed to summarize and analyze existing evidence related to the efficacy of different JAK inhibitors with regard to controlling ocular inflammation.
2. Methods
2.1. Inclusion and Exclusion Criteria
We conducted a retrospective and systematic evaluation of patients with noninfectious inflammatory ocular diseases who were treated with JAK inhibitors. We examined a range of literature types, including randomized controlled trials, cohort studies, and case reports. These articles involved a range of inflammatory ocular diseases, including uveitis, scleritis, keratitis, conjunctivitis, and retinitis. During our literature searches, we defined JAK inhibitors as tofacitinib, baricitinib, jakinib, ruxolitinib, and filgotinib.
Articles were excluded if any infectious pathogen was involved. We also excluded research involving animal experiments and literature that had been duplicated, was incomplete, or contained obvious errors.
2.2. Search Strategy
Literature searches were carried out by two independent investigators. The investigators screened the MEDLINE, PubMed, and Cochrane databases for relevant articles that were published from inception to March 2021. The search algorithm included several keywords connected by Boolean operator reported to control ocular inflammation. First, the keywords “Janus Kinase inhibitor”, “JAK inhibitor”, “tofacitinib”, “baricitinib”, “jakinib”, “ruxolitinib” and “filgotinib” were connected by the Boolean operator “OR”. Next, the keywords “ocular inflammation”, “episcleritis”, “scleritis”, “uveitis”, “keratitis”, “conjunctivitis”, “retinal vasculitis”, and “retinitis” were connected by the Boolean operator “OR”. Finally, these search results were connected by the Boolean operator “AND”. Two investigators independently searched and assessed the published studies. Any disagreement was resolved by consensus.
2.3. Statistical Analysis
We retrospectively collated a range of demographic, clinical, and therapeutic data, including authors, publication date, country of origin, gender, age, disease duration, diagnoses, complications, previous therapy history, and treatment outcomes. Data were analyzed using IBM SPSS Statistics for Windows, version 24. For quantitative variables, we calculated the mean and standard deviation.
3. Results
3.1. Study Selection and Features
A total of 63 articles were separately identified from MEDLINE, PubMed, and Cochrane databases. Figure 1 provides flow diagram showing the process used to review the literature. All the identified articles were case reports; our literature searches did not identify any relevant randomized controlled trials, cohort studies, or cross-sectional surveys. The earliest case report was published in 2014. A total of 7 articles reported the therapeutic effects of JAK inhibitors when used to treat ocular inflammation; 11 patients were included [8–14]. The basic features of all included articles are summarized in Table 1.
Figure 1.
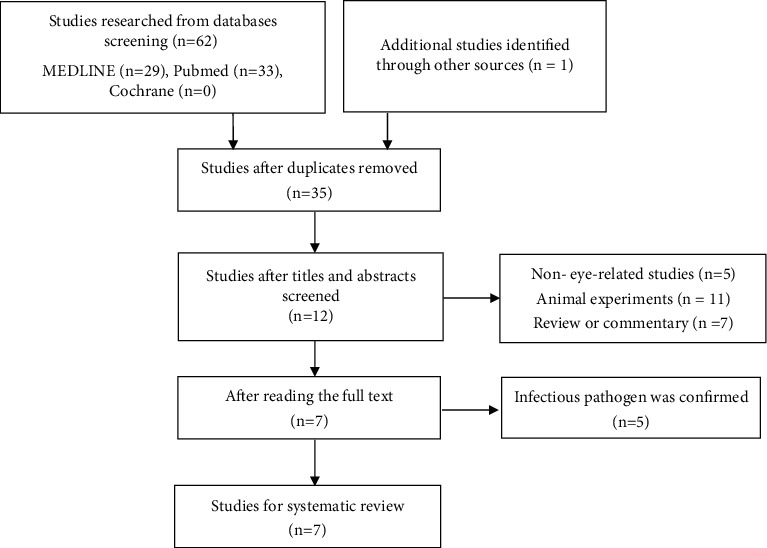
The flow diagram of the reviewed literature.
Table 1.
Features of the case reports included in the analysis.
| Author | Year | Country | Type | Number | Systemic disease | Eye involvement | Intervation |
|---|---|---|---|---|---|---|---|
| Philip B Meadow [8] | 2014 | America | Case report | 1 | RA | Keratitis | Tofacitinib |
| Stephanie Sarny [9] | 2018 | Austria | Case report | 1 | Psoriasis, MMP | Conjunctivitis | Baricitinib |
| Michael A. Paley [10] | 2019 | America | Case report | 2 | NA | Uveitis scleritis | Tofacitinib |
| P. Bauermann [11] | 2019 | Germany | Case report | 1 | JIA | Uveitis | Tofacitinib |
| Elisabetta Miserocchi [12] | 2020 | Italy | Case series | 4 | JIA | Uveitis | Baricitinib Tofacitinib |
| Richa Pyare [13] | 2020 | India | Case report | 1 | NA | Scleritis | Tofacitinib |
| Claudia Fabiani [14] | 2020 | Italy | Case report | 1 | RA | Scleritis | Tofacitinib |
JIA: juvenile idiopathic arthritis; RA: rheumatoid arthritis; MMP: mucous membrane pemphigoid; PsA: psoriatic arthritis; NA: not available.
3.2. Demographic and Clinical Features of Patients
We identified 11 patients who previously presented with ocular inflammation and received therapeutic management involving JAK inhibitors. Of the 11 patients, 5 (45.45%) had JIA-associated uveitis [11, 12], 1 (9.09%) had RA-associated keratitis [8], 1 (9.09%) had RA-associated scleritis [14], 1 (9.09%) had psoriasis-associated conjunctivitis [9], 2 (18.18%) had noninfectious scleritis, and 1 (9.09%) had uveitis with suspected autoimmune disease [10, 13] (Table 1). According to the classification proposed by the Standardization of Uveitis Nomenclature (SUN) Working Group [15], there were 6 patients with uveitis including 2 cases of anterior uveitis (33.33%), 3 cases of panuveitis (50.00%), and 1 case of anterior uveitis and intermediate uveitis (16.67%). These patients suffered from the abovementioned inflammations of ocular tissue and even had complications including macular edema, retinal detachment, cataract, band keratopathy, and glaucoma. In these articles, there were 3 males and 8 females whose mean age and mean disease duration were, respectively, 39.82 ± 14.94 years (range: 18-65 years) and 16.13 ± 12.18 years (range: 2-34 years) (Table 2).
Table 2.
Demographic and clinical features of patients.
| Patient | Author | Gender | Age | Ocular inflammation | Detail of ocluar inflammation | Systematic disease | Disease duration |
|---|---|---|---|---|---|---|---|
| 1 | Philip B. meadow | Female | 59 | Keratitis | Unilateral ulcerative keratitis (right eye), injection of the conjunctiva, pericentral ulceration of the cornea,stromal thinning, pannus, punctate epithelial erosion | RA | 9 years |
| 2 | Michael A. | Female | 45 | Anterior and intermediate uveitis | Bilateral anterior uveitis with hypopyon, Vitritis, cystoid macular edema | Undefined | NA |
| 3 | Michael A. | Female | 40 | Scleritis | Bilateral scleritis | NA | NA |
| 4 | P. Bauermann | Female | 22 | Anterior uveitis | Bilateral anterior uveitis with macular edema | JIA(oligo-extended) | 20years |
| 5 | Claudia Fabiani | Female | 45 | Scleritis | Bilateral anterior scleritis | RA | NA |
| 6 | Elisabetta Miserocchi | Female | 43 | Panuveitis | Bilateral aggressive anterior uveitis; cataract, band keratopathy, macular edema and retinal vasculitis, retinal detachment and phthisis bulbi; finally bilateral, chronic panuveitis | JIA(oligo-extended) | 33year |
| 7 | Elisabetta Miserocchi | Female | 18 | Panuveitis | Bilateral anterior uveitis at first; bilateral chronic panuveitis during follow-up cataract, band keratopathy, glaucoma | JIA(polyarticular) | 17years |
| 8 | Elisabetta Miserocchi | Female | 37 | Anterior uveitis | Bilateral anterior uveitis, cataract, band keratopathy | JIA(oligo-extended) | 34years |
| 9 | Elisabetta Miserocchi | Male | 21 | Panuveitis | Unilateral anterior uveitis(right eye), chronic panuveitis cataract, band keratopathy, macular edema | JIA(polyarticular) | 6years |
| 10 | Richa Pyare | Male | 65 | Scleritis | Deep episcleral congestion, active necrotizing scleritis with immature senile cataract | NA | 2years |
| 11 | Stephanie Sarny | Male | 43 | Conjunctivitis | Bilateral conjunctivitis, subconjunctival fibrosis, symblepharon, corneal neovascularization | Psoriasis, mucous membrane pemphigoid | 8years |
Note: NA: not available.
3.3. Previous Therapeutic Histories
Some of the identified patients received therapies involving conventional DMARDs. All patients had a long-term history of ocular inflammation, received complicated therapies, and were unable to achieve a long-term and stable resolution. Monotherapy involving conventional DMARDs was commonly reported to be ineffective. Even in combined therapeutic approaches, most of the identified patients failed to show adequate improvement; some even presented with obvious side effects (Table 3).
Table 3.
Previous therapy history of conventional DMARDs.
| Patient | Gender | Age | Ocular inflammation | MTX | CTX | CsA | MMF | LEF | AZA |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 59 | Keratitis | + | NA | NA | NA | NA | NA |
| 2 | Female | 45 | Anterior and intermediate uveitis | + | NA | NA | + | + | + |
| 3 | Female | 40 | Scleritis | + | + | NA | + | NA | + |
| 4 | Female | 22 | Anterior uveitis | + | NA | + | + | NA | NA |
| 5 | Female | 45 | Scleritis | NA | NA | NA | NA | NA | NA |
| 6 | Female | 43 | Panuveitis | NA | NA | NA | NA | + | NA |
| 7 | Female | 18 | Panuveitis | + | NA | NA | NA | NA | NA |
| 8 | Female | 37 | Anterior uveitis | + | NA | NA | NA | NA | + |
| 9 | Male | 21 | Panuveitis | + | NA | + | NA | NA | NA |
| 10 | Male | 65 | Scleritis | NA | NA | NA | + | NA | NA |
| 11 | Male | 43 | Conjunctivitis | + | + | NA | + | NA | NA |
Notes: MTX: methotrexate; CTX: cyclophosphamide; CsA: cyclosporine A; MMF: mycophenolate mofetil; LEF: leflunomide; AZA: azathioprine; NA: not available.
Our literature search revealed that biological inhibitors only provided temporary relief (Table 4). These patients experienced frequent flares of systemic symptoms and ocular symptoms. Most of the patients were treated with combined therapeutic approach involving multiple forms of steroids including 6 patients treated with prednisone, 1 patient treated with methylprednisolone, and 1 patient treated with dexamethasone. Three of them completely received the local injection and the topical and oral administration of steroids; six of them were treated in one or two ways. Ocular inflammations were refractory to topical steroid drops. Local steroid injections often led to transient relief. Oral prednisone was often effective but was difficult to taper without inducing flares (Table 5).
Table 4.
Previous therapy history of biological DMARDs.
| Patient | Gender | Age | Ocular inflammation | ADA | IFX | ETN | RTX | GOL | CER | ABA | TCZ |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 59 | Keratitis | NA | NA | NA | NA | NA | NA | + | NA |
| 2 | Female | 45 | Anterior and intermediate uveitis | + | + | NA | NA | NA | + | NA | NA |
| 3 | Female | 40 | Scleritis | NA | NA | NA | NA | NA | NA | NA | NA |
| 4 | Female | 22 | Anterior uveitis | + | + | NA | + | + | NA | NA | + |
| 5 | Female | 45 | Scleritis | + | NA | + | + | NA | NA | NA | + |
| 6 | Female | 43 | Panuveitis | + | + | NA | + | NA | NA | + | + |
| 7 | Female | 18 | Panuveitis | + | + | NA | + | NA | NA | + | NA |
| 8 | Female | 37 | Anterior uveitis | + | + | NA | NA | + | NA | NA | + |
| 9 | Male | 21 | Panuveitis | + | + | + | + | NA | NA | + | + |
| 10 | Male | 65 | Scleritis | NA | NA | NA | NA | NA | NA | NA | NA |
| 11 | Male | 43 | Conjunctivitis | + | NA | NA | + | NA | NA | NA | NA |
Notes: ADA: adalimumab; IFX: infliximab; ETN: etanercept; RTX: rituximab; GOL: golimumab; CER, certolizumab pegol; ABA: abatacept; TCZ: tocilizumab; NA: not available.
Table 5.
Previous therapy history of corticosteroids.
| Patient | Gender | Age | Ocular inflammation | Corticosteroid | Dosage | Topical | Local Injection |
Oral |
|---|---|---|---|---|---|---|---|---|
| 1 | Female | 59 | Keratitis | Methylprednisolone Prednisoneacetate |
Prednisoneacetate 1% 1 drop tid | + | NA | NA |
| 2 | Female | 45 | Anterior and intermediate uveitis | Prednisone | 80 mg bid | + | + | + |
| 3 | Female | 40 | Scleritis | Prednisone | 12 mg qd | + | + | + |
| 4 | Female | 22 | Anterior uveitis | Dexamethasone | 700ug | NA | + | NA |
| 5 | Female | 45 | Scleritis | NA | NA | NA | NA | NA |
| 6 | Female | 43 | Panuveitis | NA | NA | NA | NA | NA |
| 7 | Female | 18 | Panuveitis | Prednisone | 12.5 mg qd | + | + | + |
| 8 | Female | 37 | Anterior uveitis | NA | NA | NA | + | NA |
| 9 | Male | 21 | Panuveitis | Steroids | NA | NA | + | + |
| 10 | Male | 65 | Scleritis | Prednisolone | 1 mg/kg qd | + | NA | + |
| 11 | Male | 43 | Conjunctivitis | Prednisone | NA | NA | NA | + |
Note: NA: not available.
Due to serious complications, some of the patients underwent surgery. Patient number 1 underwent a corneal gluing procedure of the right eye [8]. Patient number 2 received bilateral implantation of fluocinolone acetonide intravitreal implants [10]. Patient number 4 received cataract surgery with intraocular lens (IOL) implantation in both eyes and vitrectomy in her right eye [11]. Patient number 6 underwent cataract extraction [12]. Finally, patient number 9 underwent cataract extraction with IOL implantation [12].
3.4. JAK Inhibitor Treatment
No matter which type of JAK inhibitor was used, all of the case reports, except for patient number 8 [12], showed good efficacy with regard to ocular symptoms. Irrespective of whether a patient received monotherapy or combined treatment, almost all gained some form of control over their condition. With regard to systemic symptoms, the combination of baricitinib with MTX and prednisone still showed an incomplete treatment response with relapsing episodes of active joint inflammation. While taking tofacitinib, none of the reported systemic symptoms were active. The available literature suggests that it might be easier to control systemic symptoms. In some case reports, the response to tofacitinib treatment was rapid; inflammation was usually resolved within one or two weeks (Table 6).
Table 6.
Characteristics of JAK inhibitor treatment.
| Patient | Gender | Age | Ocular inflammation | Inhibitor | Dosage | Treatment duration | Combined therapy | Side effects | Systematic symptoms | Ocular symptoms |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 59 | Keratitis | Tofacitinib | 5 mg bid | 1 month; Improved after 2 weeks |
NA | No | Inactive | Inactive |
| 2 | Female | 45 | Anterior and intermediate uveitis | Tofacitinib | 11 mg daily | 4months; Improved after 1 month |
MTX | No | Combination: Inactive Monotherapy: Active |
Inactive |
| 3 | Female | 40 | Scleritis | Tofacitinib | 11 mg daily | 9 months; Improved after 1 week |
MTX | No | No systematic symptoms | Inactive |
| 4 | Female | 22 | Anterior uveitis | Tofacitinib | 5 mg bid | 9 months | MTX 2.5 mg qod |
No | NA | Inactive |
| 5 | Female | 45 | Scleritis | Tofacitinib | 5 mg bid | 6 months | Prednisone 5 mg qd |
No | NA | Inactive |
| 6 | Female | 43 | Panuveitis | Tofacitinib | 5 mg bid | 7 months | NA | No | Inactive | Inactive |
| 7 | Female | 18 | Panuveitis | Baricitinib | 4 mg Qd |
5 months | MTX 15 mg qw Prednisone 12.5 mg qd |
No | Active | Inactive |
| 8 | Female | 37 | Anterior uveitis | Baricitinib | 4 mg qd | 13 months | NA | No | Inactive | Active |
| 9 | Male | 21 | Panuveitis | Baricitinib | 4 mg qd | 4 months | MTX 15 mg qw Prednisone 7.5 mg qd |
No | Active | Inactive |
| 10 | Male | 65 | Scleritis | Tofacitinib | 5 mg bid | Improvd after 1 month | MMF 500 mg bid Prednisone 2.5 mg qod |
No | No systematic symptoms | Inactive |
| 11 | Male | 43 | Conjunctivitis | Baricitinib | 4 mg qd | 6month; Improvd after 2 weeks |
MTX 25 mg qw Prednisolone 6 mg qd |
Yes | NA | Inactive |
Note: NA: not available.
Literature analysis showed that side effects were rare. Only patient number 11 experienced a low level of neutrophil granulocytes during treatment involving baricitinib and MTX [9]. This led to the discontinuation of baricitinib for 2 weeks; subsequently, the patient did not experience any adverse effects. However, we cannot rule out the potential adverse effects of MTX (Table 6).
Some of the literature described the use of JAK inhibitors to treat patients with uveitis and scleritis; the grading of the anterior chamber cells decreased from pretreatment to posttreatment. Other ocular indicators, including best corrected visual acuity and central foveal thickness, showed obvious improvements (Table 7).
Table 7.
Treatment response of ocular inflammation.
| Patient | Gender | Age | Ocular inflammation | BCVA | ACC | CFT |
|---|---|---|---|---|---|---|
| 1 | Female | 59 | Keratitis | Pre:RE:20/200 LE:20/20 Post:RE:20/30 |
Pre:RE0 | NA |
| 2 | Female | 45 | Anterior and intermediate uveitis | NA | Pre:RE2+ LE2+ Post: RE0.5+ LE0 |
NA |
| 3 | Female | 40 | Scleritis | NA | NA | NA |
| 4 | Female | 22 | Anterior uveitis | Pre:RE20/100 LE20/200 Post:RE20/25 LE20/32 |
Pre:RE3+ LE0+ Post:RE0 LE0 |
Pre: RE468 LE630 Post: RE252 LE254 |
| 5 | Female | 45 | Scleritis | NA | NA | NA |
| 6 | Female | 43 | Panuveitis | Pre:RE:20/40 LE:No light perception |
Pre:2+ Post:0 |
Pre:350 Post:270 |
| 7 | Female | 18 | Panuveitis | Post:RE:20/40 LE:20/200 | Pre:3+ Post:0.5+ |
Pre:320 Post:264 |
| 8 | Female | 37 | Anterior uveitis | Post:RE: 20/60 LE: 20/60 | Pre:2+ Post:0 |
Pre:450 Post:276 |
| 9 | Male | 21 | Panuveitis | Post:RE: 20/20 LE: 20/20 | Pre:3+ Post:0.5+ |
Pre:400 Post:280 |
| 10 | Male | 65 | Scleritis | Pre:RE6/ 6 LE 6/36 Post:LE6/24 |
Pre:1+ Post:0 |
NA |
| 11 | Male | 43 | Conjunctivitis | Pre:RE20/30 LE:Counting fingers | NA | NA |
Note: ACC: anterior chamber cell; BCVA: best corrected visual acuity; CFT: central foveal thickness: Pre: pretreatment; Post: posttreatment; RE: right eye; LE: left eye; NA: not available.
4. Discussion
The eyeball is composed of different layers and has a separated immune environment. Multiple mechanisms contribute to local immune tolerance, including the absence of vessels in the cornea and the anterior chamber, immunosuppressive factors, and inflammatory regulation via the anterior chamber [16]. The posterior segment of the eye is also a unique structure that contains photoreceptor cells and retinal pigment epithelium; this forms a physical barrier that separates the systemic immune system from the retinal space [17]. However, inflammatory rheumatic diseases can affect multilayer structures and have destructive effects on the ocular microenvironment. Therefore, inflammatory ophthalmic disorders are a group of heterogeneous inflammatory conditions that affect different anatomical ocular tissues, involving scleritis, keratitis, anterior uveitis, posterior uveitis, and retinal vasculitis; these occur in isolation or in the context of systemic autoimmune diseases. Systemic autoimmune diseases that include ocular involvement are also a group of diverse diseases, including rheumatoid arthritis, juvenile idiopathic arthritis, systemic vasculitis, systemic lupus erythematosus, Behçet's syndrome, and relapsing polychondritis [18].
In this article, we reviewed 5 cases of JIA-associated uveitis, 1 case of RA-associated keratitis, 1 case of RA-associated scleritis, 1 case of psoriasis-associated conjunctivitis, 2 cases of noninfectious scleritis, and 1 case of uveitis with suspected autoimmune disease.
Our results are consistent with other reports. JIA-associated uveitis is the most common rheumatic ocular involvement in pediatric patients [19]. The estimated prevalence of uveitis in patients with JIA ranges from 11.6% [20] to 30% [21]. The most common form was chronic anterior uveitis, as defined by the classification scheme published by the Standardization of Uveitis Nomenclature (SUN) Working Group [15, 22]. In a retrospective review, 68.3% of 1081 JIA cases were shown to have chronic anterior uveitis [23]. Acute anterior uveitis accounted for 16.2%, recurrent anterior uveitis reached 12%, and panuveitis was just 3.5% [23]. Of the multiple etiological factors responsible for noninfectious scleritis, RA represents a major cause [24]. The anterior segment is more commonly affected than the posterior segment in RA-related ocular complications. In a previous study of 243 patients with scleritis, the most frequent rheumatic disease was RA (15.2%) [25]. In other studies, RA-related scleritis accounted for approximately 25% of all cases [26]. RA-related keratitis is also common in patients with active scleritis [18]. However, compared with spondyloarthritis, RA is a rare cause of uveitis [27]. Ophthalmic manifestations are estimated to occur in 10% of patients with psoriasis and 31% of patients with psoriatic arthritis (PsA) [28]. Another study reported that the leading ocular disorder in PsA patients was conjunctivitis (19.6%), followed by iritis (7.1%) [29].
Our review of the literature revealed that most of these cases received treatments that included glucocorticoids, several conventional disease-modifying antirheumatic drugs, and multiple biological agents. However, patients did not show adequate improvements or achieve long-term resolutions; they even presented with obvious side effects and faced dilemmas as to whether to continue treatment or not. The statuses of the ocular and systematic inflammation in most of the patients reviewed were refractory and severe.
A range of JAK inhibitors have been or are being developed, for the treatment of refractory cases and those with various autoimmune diseases, including rheumatoid arthritis, psoriatic arthritis, ulcerative colitis, and ankylosing spondylitis [30–32]. Many of the cytokines involved in autoimmune and inflammatory diseases utilize JAKs and STATs to transduce intracellular signals. JAK inhibitors are less selective than biological inhibitors, can simultaneously block the signaling of multiple cytokine axis, and offer new therapeutic strategies [33]. Whether these inhibitors could simultaneously have therapeutic effects on ocular complications remains unclear. Unfortunately, the review of the literature failed to identify publications involving a large case series or randomized controlled trials. We only identified several case reports that indicated the anti-inflammatory effects of JAK inhibitors on the inflammation caused in a diverse range of ocular tissues by different rheumatic diseases.
It is important that we consider why JAK inhibitors exhibit the potential to play a role in autoimmune-related ocular inflammatory diseases. Dysregulation of the JAK-STAT pathway is known to be associated with the pathogenesis of various inflammatory and autoimmune disorders [33, 34]. The JAK-STAT pathway is known to be important for inflammatory cell regulation, cytokine production, and proinflammatory signal transduction [6, 7].
Although the etiology of ocular inflammation has yet to be fully elucidated, it is possible that the JAK/STAT pathway may participate in ocular pathology because this mechanism regulates the differentiation of pathogenic Th1 and Th17 cells. The Th1 and Th17 cell subsets require STAT1 and STAT3 during development and may be the etiological agents responsible for human uveitis and scleritis and experimental autoimmune uveoretinitis [35–37]. In the mouse model of uveitis, inhibition of the JAK/STAT signaling pathway by SOCS1-KIR, which binds to JAK2, could suppress and ameliorate experimental autoimmune uveitis (EAU) [38]. The mechanism that is responsible for this action involves downregulating the proliferation of pathogenic Th17 cells and inhibiting the migration of inflammatory cells into the neuroretina during EAU. However, some researchers have reported that the effect of tofacitinib on Th1/Th17 balance in the EAU model was different from the effects induced by SOCS1-KIR. Tofacitinib inhibited the development of EAU by reducing the proportion of Th1 cells instead of Th17 cells, and by suppressing the production of IFN-γ, did not exert effect on the expression of IL-17 and its transcription factor RORγt [39]. JAK inhibitors can control both intraocular inflammation and ocular surface inflammation. In an animal model of experimental dry eye, the application of a topical JAK inhibitor (tofacitinib) suppressed ocular surface inflammation and immunity in an experimental model of corneal thermocautery [40]. Even in the conjunctive structure of ocular tissue, tofacitinib has also been shown to prevent experimental allergic conjunctivitis in BALB/c mice by downregulating the phosphorylation of JAK3/STAT signaling [41].
This retrospective review had some limitations that need to be considered, including the lack of a control group, the small number of patients, and the lack of high-level evidence-based studies. However, we believe that all of these cases reported herein are valuable and can facilitate the future direction of our research. Future research may prove that JAK inhibitors can provide a novel treatment option for refractory autoimmune-related ocular inflammation.
5. Conclusion
JAK inhibitors may represent an alternative treatment option for patients with autoimmune-related ocular inflammation.
Acknowledgments
This project was supported by The Science and Technology Project Of The Health Planning Committee of Sichuan (Project no. 19PJ251) and by 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (Project nos. ZYGD18015 and ZYJC18003). The authors would like to express their gratitude to EditSprings (https://www.editsprings.com/) for the expert linguistic services provided.
Conflicts of Interest
None of the authors have any conflicts of interest to declare.
Authors' Contributions
Ji Wen, Huifang Hu, and Menglin Chen contributed equally to this work.
References
- 1.Wakefield D., di Girolamo N., Thurau S., Wildner G., McCluskey P. Scleritis: immunopathogenesis and molecular basis for therapy. Progress in Retinal and Eye Research . 2013;35:44–62. doi: 10.1016/j.preteyeres.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 2.Horton S., Jones A. P., Guly C. M., et al. Adalimumab in juvenile idiopathic arthritis-associated uveitis: 5-year follow-up of the bristol participants of the SYCAMORE trial. American Journal of Ophthalmology . 2019;207:170–174. doi: 10.1016/j.ajo.2019.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Suhler E. B., Lim L. L., Beardsley R. M., et al. Rituximab therapy for refractory scleritis: results of a phase I/II dose- ranging, randomized, clinical trial. Ophthalmology . 2014;121(10):1885–1891. doi: 10.1016/j.ophtha.2014.04.044. [DOI] [PubMed] [Google Scholar]
- 4.Dipasquale V., Atteritano M., Fresta J., Castagna I., Conti G. Tocilizumab for refractory uveitis associated with juvenile idiopathic arthritis: a report of two cases. Journal of Clinical Pharmacy and Therapeutics . 2019;44(3):482–485. doi: 10.1111/jcpt.12821. [DOI] [PubMed] [Google Scholar]
- 5.Ragam A., Kolomeyer A. M., Fang C., Xu Y., Chu D. S. Treatment of chronic, noninfectious, nonnecrotizing scleritis with tumor necrosis factor alpha inhibitors. Ocular Immunology and Inflammation . 2014;22(6):469–477. doi: 10.3109/09273948.2013.863944. [DOI] [PubMed] [Google Scholar]
- 6.Liew S. H., Nichols K. K., Klamerus K. J., Li J. Z., Zhang M., Foulks G. N. Tofacitinib (CP-690,550), a Janus kinase inhibitor for dry eye disease: results from a phase 1/2 trial. Ophthalmology . 2012;119(7):1328–1335. doi: 10.1016/j.ophtha.2012.01.028. [DOI] [PubMed] [Google Scholar]
- 7.Scott L. J. Tofacitinib: a review of its use in adult patients with rheumatoid arthritis. Drugs . 2013;73(8):857–874. doi: 10.1007/s40265-013-0065-8. [DOI] [PubMed] [Google Scholar]
- 8.Meadow P. B., Nguyen J., Kesavarapu K. Tofacitinib citrate for ulcerative keratitis in a patient with rheumatoid arthritis. Case reports in rheumatology . 2014;2014:3. doi: 10.1155/2014/403452.403452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarny S., Hucke M., el-Shabrawi Y. Treatment of mucous membrane pemphigoid with Janus kinase inhibitor baricitinib. JAMA ophthalmology . 2018;136(12):1420–1422. doi: 10.1001/jamaophthalmol.2018.3789. [DOI] [PubMed] [Google Scholar]
- 10.Paley M. A., Karacal H., Rao P. K., Margolis T. P., Miner J. J. Tofacitinib for refractory uveitis and scleritis. American journal of ophthalmology case reports . 2019;13:53–55. doi: 10.1016/j.ajoc.2018.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bauermann P., Heiligenhaus A., Heinz C. Effect of Janus kinase inhibitor treatment on anterior uveitis and associated macular edema in an adult patient with juvenile idiopathic arthritis. Ocular Immunology and Inflammation . 2019;27(8):1232–1234. doi: 10.1080/09273948.2019.1605453. [DOI] [PubMed] [Google Scholar]
- 12.Miserocchi E., Giuffrè C., Cornalba M., Pontikaki I., Cimaz R. JAK inhibitors in refractory juvenile idiopathic arthritis-associated uveitis. Clinical Rheumatology . 2020;39(3):847–851. doi: 10.1007/s10067-019-04875-w. [DOI] [PubMed] [Google Scholar]
- 13.Pyare R., Kaushik V., Dutta Majumder P., Biswas J. Tofacitinib in recalcitrant scleritis: first case report from India. Indian Journal of Ophthalmology . 2020;68(9):1988–1990. doi: 10.4103/ijo.IJO_534_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fabiani C., Sota J., Sainz-de-la-Maza M., et al. New potential weapons for refractory scleritis in the era of targeted therapy. Mediators of Inflammation . 2020;2020:6. doi: 10.1155/2020/8294560.8294560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jabs D. A., Nussenblatt R. B., Rosenbaum J. T. Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. American Journal of Ophthalmology . 2005;140(3):509–516. doi: 10.1016/j.ajo.2005.03.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Generali E., Cantarini L., Selmi C. Ocular involvement in systemic autoimmune diseases. Clinical Reviews in Allergy and Immunology . 2015;49(3):263–270. doi: 10.1007/s12016-015-8518-3. [DOI] [PubMed] [Google Scholar]
- 17.Perez V. L., Saeed A. M., Tan Y., Urbieta M., Cruz-Guilloty F. The eye: a window to the soul of the immune system. Journal of Autoimmunity . 2013;45:7–14. doi: 10.1016/j.jaut.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 18.McCluskey P., Powell R. J. The eye in systemic inflammatory diseases. Lancet . 2004;364(9451):2125–2133. doi: 10.1016/S0140-6736(04)17554-5. [DOI] [PubMed] [Google Scholar]
- 19.Smith J. A., Mackensen F., Sen H. N., et al. Epidemiology and course of disease in childhood uveitis. Ophthalmology . 2009;116(8):1544–1551.e1. doi: 10.1016/j.ophtha.2009.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Angeles-Han S. T., Pelajo C. F., Vogler L. B., et al. Risk markers of juvenile idiopathic arthritis-associated uveitis in the Childhood Arthritis and Rheumatology Research Alliance (CARRA) Registry. The Journal of Rheumatology . 2013;40(12):2088–2096. doi: 10.3899/jrheum.130302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moradi A., Amin R. M., Thorne J. E. The role of gender in juvenile idiopathic arthritis-associated uveitis. Journal of Ophthalmology . 2014;2014:7. doi: 10.1155/2014/461078.461078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sen E. S., Ramanan A. V. Juvenile idiopathic arthritis-associated uveitis. Clinical Immunology . 2020;211, article 108322 doi: 10.1016/j.clim.2019.108322. [DOI] [PubMed] [Google Scholar]
- 23.Sabri K., Saurenmann R. K., Silverman E. D., Levin A. V. Course, complications, and outcome of juvenile arthritis-related uveitis. Journal of AAPOS . 2008;12(6):539–545. doi: 10.1016/j.jaapos.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 24.Tong L., Thumboo J., Tan Y. K., Wong T. Y., Albani S. The eye: a window of opportunity in rheumatoid arthritis? Nature Reviews Rheumatology . 2014;10(9):552–560. doi: 10.1038/nrrheum.2014.85. [DOI] [PubMed] [Google Scholar]
- 25.Akpek E. K., Thorne J. E., Qazi F. A., Do D. V., Jabs D. A. Evaluation of patients with scleritis for systemic disease. Ophthalmology . 2004;111(3):501–506. doi: 10.1016/j.ophtha.2003.06.006. [DOI] [PubMed] [Google Scholar]
- 26.Artifoni M., Rothschild P. R., Brézin A., Guillevin L., Puéchal X. Ocular inflammatory diseases associated with rheumatoid arthritis. Nature Reviews Rheumatology . 2014;10(2):108–116. doi: 10.1038/nrrheum.2013.185. [DOI] [PubMed] [Google Scholar]
- 27.Sève P., Kodjikian L., Adélaïde L., Jamilloux Y. Uveitis in adults: what do rheumatologists need to know? Joint, Bone, Spine . 2015;82(5):308–314. doi: 10.1016/j.jbspin.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 28.Rehal B., Modjtahedi B. S., Morse L. S., Schwab I. R., Maibach H. I. Ocular psoriasis. Journal of the American Academy of Dermatology . 2011;65(6):1202–1212. doi: 10.1016/j.jaad.2010.10.032. [DOI] [PubMed] [Google Scholar]
- 29.Lambert J. R., Wright V. Eye inflammation in psoriatic arthritis. Annals of the Rheumatic Diseases . 1976;35(4):354–356. doi: 10.1136/ard.35.4.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.for the Pediatric Rheumatology International Trials Organization (PRINTO), the Pediatric Rheumatology Collaborative Study Group (PRCSG), Ruperto N., et al. Pharmacokinetic and safety profile of tofacitinib in children with polyarticular course juvenile idiopathic arthritis: results of a phase 1, open-label, multicenter study. Pediatric Rheumatology Online Journal . 2017;15(1):p. 86. doi: 10.1186/s12969-017-0212-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harigai M. Growing evidence of the safety of JAK inhibitors in patients with rheumatoid arthritis. Rheumatology (Oxford) . 2019;58(Supplement_1):i34–i42. doi: 10.1093/rheumatology/key287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abdulrahim H., Sharlala H., Adebajo A. O. An evaluation of tofacitinib for the treatment of psoriatic arthritis. Expert Opinion on Pharmacotherapy . 2019;20(16):1953–1960. doi: 10.1080/14656566.2019.1657404. [DOI] [PubMed] [Google Scholar]
- 33.You H., Xu D., Zhao J., et al. JAK inhibitors: prospects in connective tissue diseases. Clinical Reviews in Allergy and Immunology . 2020;59(3):334–351. doi: 10.1007/s12016-020-08786-6. [DOI] [PubMed] [Google Scholar]
- 34.Banerjee S., Biehl A., Gadina M., Hasni S., Schwartz D. M. JAK–STAT signaling as a target for inflammatory and autoimmune diseases: current and future prospects. Drugs . 2017;77(5):521–546. doi: 10.1007/s40265-017-0701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Luger D., Silver P. B., Tang J., et al. Either a Th17 or a Th1 effector response can drive autoimmunity: conditions of disease induction affect dominant effector category. The Journal of Experimental Medicine . 2008;205(4):799–810. doi: 10.1084/jem.20071258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Amadi-Obi A., Yu C. R., Liu X., et al. TH17 cells contribute to uveitis and scleritis and are expanded by IL-2 and inhibited by IL-27/STAT1. Nature Medicine . 2007;13(6):711–718. doi: 10.1038/nm1585. [DOI] [PubMed] [Google Scholar]
- 37.Liu X., Lee Y. S., Yu C. R., Egwuagu C. E. Loss of STAT3 in CD4+ T cells prevents development of experimental autoimmune diseases. Journal of Immunology . 2008;180(9):6070–6076. doi: 10.4049/jimmunol.180.9.6070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.He C., Yu C. R., Sun L., Mahdi R. M., Larkin J., III, Egwuagu C. E. Topical administration of a suppressor of cytokine signaling-1 (SOCS1) mimetic peptide inhibits ocular inflammation and mitigates ocular pathology during mouse uveitis. Journal of Autoimmunity . 2015;62:31–38. doi: 10.1016/j.jaut.2015.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bing S. J., Lyu C., Xu B., et al. Tofacitinib inhibits the development of experimental autoimmune uveitis and reduces the proportions of Th1 but not of Th17 cells. Molecular Vision . 2020;26:641–651. [PMC free article] [PubMed] [Google Scholar]
- 40.Stevenson W., Sadrai Z., Hua J., et al. Effects of topical Janus kinase inhibition on ocular surface inflammation and immunity. Cornea . 2014;33(2):177–183. doi: 10.1097/ICO.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 41.Li Y., Liu X., Yu J., et al. Tofacitinib suppresses mast cell degranulation and attenuates experimental allergic conjunctivitis. International Immunopharmacology . 2020;86, article 106737 doi: 10.1016/j.intimp.2020.106737. [DOI] [PubMed] [Google Scholar]


