Abstract
Background:
Lymphopenia contributes to the immune suppression observed in critical illness. However, its role in the immunologic response to trauma remains unclear. Herein, we assessed whether admission lymphopenia is associated with poor outcomes in patients with blunt chest wall trauma (BCWT).
Methods:
All adult patients with a Chest Abbreviated Injury Score (CAIS) ≥2 admitted to our Level I Trauma center between May 2009 and December 2018 were identified in our institution Trauma Registry. Patients with absolute lymphocyte counts (ALC) collected within 24 h of admission were included. Patients who died within 24 hours of admission, had bowel perforation on admission, penetrating trauma, and burns were excluded. Demographics, injury characteristics, comorbidities, ALC, complications, and outcomes were collected. Lymphopenia was defined as an ALC ≤1000/μL. Association between lymphopenia and clinical outcomes of BCWT was assessed using multivariate analyses. P < 0.05 was considered significant.
Results:
A total of 1394 patients were included; 69.7% were male; 44.3% were lymphopenic. On univariate analysis, lymphopenia was associated with longer in-hospital stay (11.6 ± 10.2 vs. 10.1 ± 11.4, p = 0.009), in-hospital death (9.7% vs. 5.8%, p = 0.006), and discharge to a healthcare facility (60.9% vs. 46.4%, p < 0.001). Controlling for Injury Severity Score, age, gender, and comorbidities, the association between lymphopenia and discharge to another facility (SNF/rehabilitation facility/ACH) (OR=1.380 [1.041–1.830], p = 0.025) remained significant.
Conclusions:
Lymphopenia on admission is associated with discharge requiring increased healthcare support. Routine lymphocyte count monitoring on admission may provide important prognostic information for BCWT patients
Keywords: Lymphopenia, Blunt chest wall trauma, discharge disposition, elderly
Graphical Abstract
INTRODUCTION
Trauma is the third highest cause of death for patients aged 18 years and above in United States and carries a significant financial burden on our healthcare system. Trauma care ranks as the second highest contributor to overall healthcare costs in the US, amounting to $671 billion in 2013.(1) Strikingly, costs associated with discharge to home health care (HHC) and skilled nursing care facilities (SNF) were estimated at $97 and $166.3 billion, respectively, in 2017.(2) Blunt chest wall injuries account for approximately 15% of all trauma admissions to emergency departments worldwide and approximately 90% of all chest wall traumas.(3) Blunt chest trauma patients represent a population of high acuity who require accurate diagnosis and early management to avoid serious complications and allow optimal recovery.(4) Early identification of populations vulnerable to complications, higher length of stay, and adverse discharge disposition play an important role in overall outcomes of trauma patients.(5–7) Lymphopenia following trauma and sepsis is a well-established phenomenon that is associated with poor outcomes.(8–11) In subsets of patients, admission lymphopenia that persists has been demonstrated as an independent predictor of infectious complications and mortality.(8, 9, 11–13) Current literature suggests lymphocytes undergo multiple functional disturbances, including increased apoptosis, reduced cell proliferation, and phenotypic changes in response to traumatic injury.(11, 14–16) These disturbances occur less than two hours following traumatic injury and persist for multiple days.(10, 16) While reduced lymphocyte number and function likely contributes to the immune suppression observed in critical illness, their precise role in the immunologic response to trauma has not been fully described in blunt chest wall trauma patients.(17, 18)
The goal of this study was to determine the relationship between absolute lymphocyte counts within 24-hours of admission and outcomes in chest wall trauma patients. We hypothesize that admission lymphopenia in patients with chest wall trauma was associated with infectious complications, in-hospital mortality, increased use of healthcare resources, and discharge disposition.
MATERIALS AND METHODS
Ethical Statement
Approval for this retrospective study was obtained from the University of Iowa Institutional Review Board (IRB # 201712728). A waiver of consent for all subjects was approved by the University of Iowa Institutional Review Board.
Study Design
The University of Iowa Trauma Registry was queried retrospectively to identify all adult patients with a Chest Abbreviated Injury Scale (CAIS) ≥2 admitted to our Level I Trauma center between May 2009 and December 2018. Patients with absolute lymphocyte counts (ALC) collected within 24 h of admission were included. Patients who died within 24 hours of admission, had bowel perforation on admission, penetrating trauma, and burns were excluded. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for cohort studies.(19, 20)
Data Collection
Demographics (age, gender, and race), comorbidities [Diabetes, obesity, chronic obstructive pulmonary disease, asthma, tobacco use, heart failure, coronary artery disease, chronic liver disease, chronic kidney disease, past or current history of cancer, undergoing chemotherapy, immunodeficiency, chronic steroid use, history of organ transplant], injury details, including time and date of injury, time and date of admission, and mechanism of injury, transfer status, Glasgow Coma Scale (GCS) at the time of admission, injury severity score (ISS), organ specific abbreviated injury scale (AIS), hospital length of stay (LOS), intensive care unit length of stay (ICU LOS), ventilator days, discharge disposition, absolute lymphocyte count (ALC), complications, and mortality were collected.
ALC collected within 24 h of admission as well as monocyte and neutrophil counts were recorded. Lymphopenia was defined as an ALC ≤1000/μL per NIH definition.(21)
Statistical Analysis
Patients were divided based on ALC counts using the cutoff of ALC ≤1000/μL into the lymphopenic and non-lymphopenic groups. Univariate analyses were performed to identify differences between groups. Normality was assessed using the Kolmogorov-Smirnov test for all continuous variables. All non-normally distributed continuous variables are presented as median and interquartile range. Chi square and Fisher exact-test were utilized for categorical variables, while Mann-Whitney U test was used for continuous variables. Multivariate logistic regression analyses were used to assess the association between lymphopenia and mortality and clinical outcomes in BCWT patients. Multivariate binary logistic regression, negative binomial multivariate analysis, and multinomial logistic regression were performed to identify variables associated with mortality, length of stay, and discharge disposition, respectively. Analyses were performed using SPSS 25.0 (IBM, Chicago, IL), and p < 0.05 was considered significant.
RESULTS
Patient selection
A total of 3,849 patients were admitted for chest wall trauma with a chest AIS ≥2 during our study period. After excluding patients admitted for penetrating or burn injuries, those with bowel perforation, those who died within 24 hours, and those for whom ALC within 24 hours of admission was unavailable, 1,394 patients were included in our study. Based on our registry information, 964 patients (69.2%) presented with rib fractures, 34 (2.4%) with sternal fractures, 116 (8.3%) with lung contusions not associated with rib or sternal fractures, 190 (13.6%) with other chest wall injuries including pneumothorax, hemothorax, and pleural effusion, and 90 (6.5%) presented with unspecified chest wall injuries. A total of 618 (44.3%) were lymphopenic on admission. (Figure 1)
Figure 1.
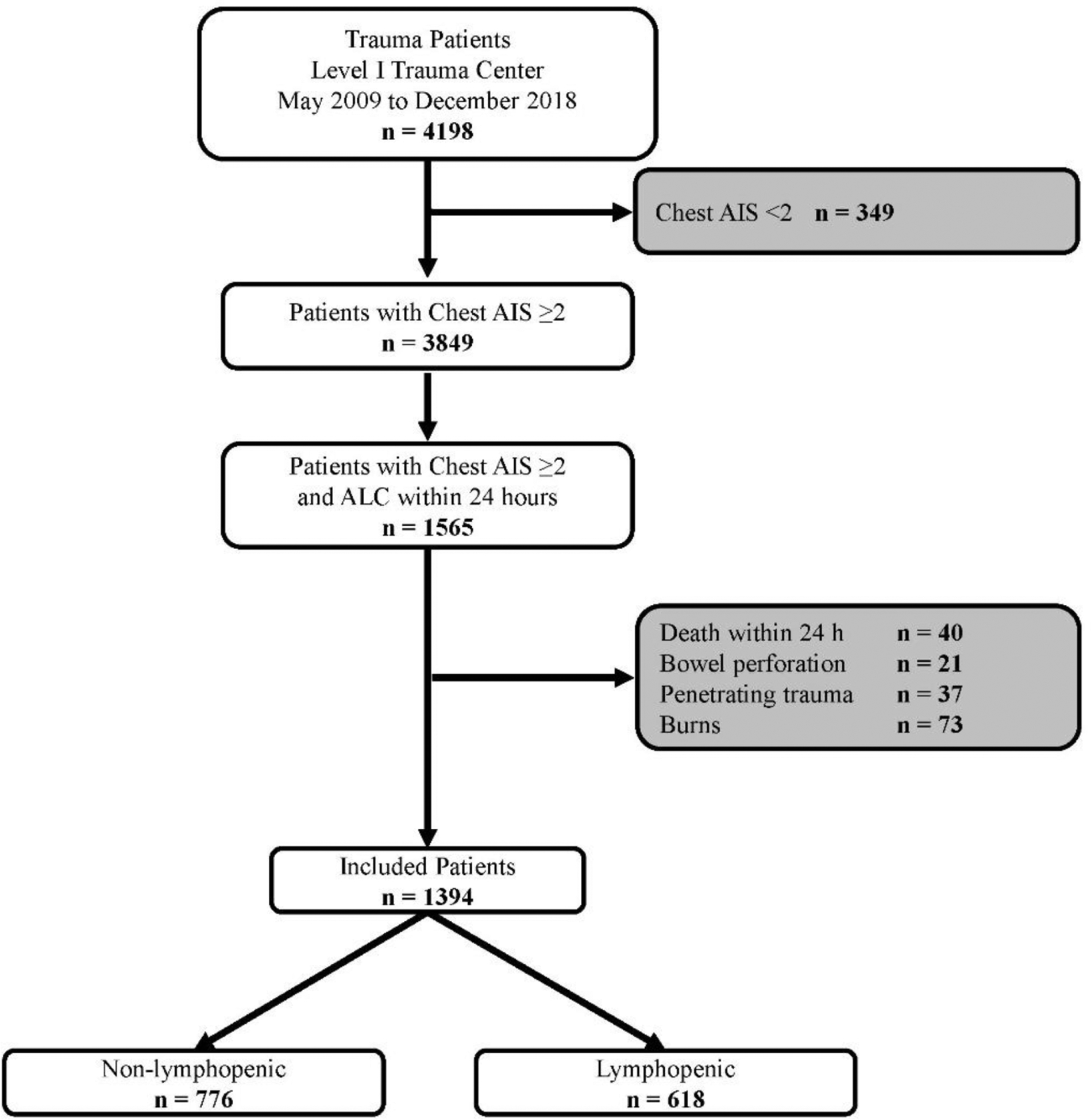
Patient selection flowchart.
Patient characteristics
As shown in Table 1, lymphopenic patients were older and presented a higher injury severity score (ISS). They were also more likely to suffer multiple injuries in addition to their chest injury. Lymphopenic patients were less likely to use tobacco, but more likely to have a history of heart failure, hypertension, chronic kidney disease, cancer, or transplant. No significant differences were observed in rates of diabetes, obesity, chronic obstructive pulmonary disease, asthma, coronary artery disease, or chronic liver disease. Similarly, there was no significant difference in the proportion of patients who were immunodeficient, on steroids, or undergoing chemotherapy between the groups.
Table 1.
Patient Characteristics
| Variables | Non Lymphopenic (n = 776) | Lymphopenic (n = 618) | p-value |
|---|---|---|---|
| Age (y), median [iQR] | 50 [32.3–66] | 56 [44–73] | <0.001 |
| Male, n (%) | 538 (69.3) | 433 (70.1) | 0.770 |
| White, n (%) | 717 (92.3) | 573 (92.7) | 0.907 |
| Injury severity score, median [IQR] | 19 [10–29] | 22 [13.8–22] | <0.001 |
| Lymphocyte count | 1470.0 [1202.3–1920.0] | 668.5 [480.0–820.0] | <0.001 |
| Injury | 0.032 | ||
| Isolated Chest | 128 (16.5) | 70 (11.3) | |
| Chest and Head Injury | 63 (8.1) | 56 (9.1) | |
| Chest and Facial Injury | 12 (1.6) | 9 (1.5) | |
| Chest and Abdomen | 31 (4.0) | 16 (2.6) | |
| Chest and Extremities | 69 (8.9) | 52 (8.4) | |
| Chest and External | 37 (4.8) | 21 (3.4) | |
| Chest and ≥ 2 Injuries | 434 (56.1) | 394 (63.8) | |
| Comorbidities, n (%) | |||
| Tobacco Use | 220 (28.4) | 132 (21.4) | 0.003 |
| Heart Failure | 26 (3.4) | 37 (6.0) | 0.019 |
| Hypertension | 249 (32.1) | 258 (41.7) | <0.001 |
| Chronic kidney disease | 18 (2.3) | 38 (6.1) | <0.001 |
| Cancer | 26 (3.4) | 50 (8.1) | <0.001 |
| Transplant | 1 (0.1) | 8 (1.3) | 0.013 |
Outcomes
On univariate analysis, lymphopenic patients were statistically significantly more likely to stay longer in hospital, more likely to die, and more likely to be discharged home with healthcare services or to a facility (Skilled nursing facility, rehabilitation facility, or long-term acute care hospital). No significant differences were observed in infectious complications between the groups (Table 2).
Table 2.
Outcomes
| Variables | Non-lymphopenic (n = 776) | Lymphopenic (n = 618) | p-value |
|---|---|---|---|
| Hospital Course | |||
| Length of stay (days), median [IQR] | 6 [3–13] | 9 [5–15] | <0.001 |
| ICU days, median [IQR] | 4 [2–10] | 4 [2–9] | 0.797 |
| Ventilator days, median [IQR] | 4 [1–10.3] 8 [3–12] | 4 [2–9] | 0.631 |
| Ventilator-free days, median [IQR] | 8 [4–13] | 0.376 | |
| Complications, n (%) | |||
| Pneumonia | 104 (13.4) | 95 (15.4) | 0.317 |
| Urinary Tract Infection | 66 (8.5) | 60 (9.7) | 0.453 |
| Wound Infection | 18 (2.3) | 14 (2.3) | 1.000 |
| Other Infection | 17 (2.2) | 16 (2.6) | 1.000 |
| In-hospital mortality, n (%) | 45 (5.8) | 60 (9.7) | 0.006 |
| Discharge Disposition, n (%) | < 0.001 | ||
| Home | 331 (45.3) | 169 (30.3) | |
| Home with Health Care | 35 (4.8) | 39 (7.0) | |
| SNF/Rehab/LTACH | 339 (46.4) | 340 (60.9) | |
| Other | 20 (2.7) | 6 (1.1) | |
| Hospice | 6 (0.8) | 4 (0.7) |
Multivariate analysis was performed to identify variables associated with hospital length of stay and discharge disposition while controlling for age, gender, and variables that were significantly different between the lymphopenic and non-lymphopenic groups on univariate analysis. As shown in Table 3, lymphopenia was associated with longer hospital stay and with discharge disposition to home with healthcare services or to another healthcare facility (Skilled nursing, rehabilitation or long-term acute care facilities) as compared to discharge to home without healthcare assistance. In our model, ISS was also significantly associated with longer hospital stay and with discharge to disposition to home with healthcare services or to another healthcare facility (Skilled nursing, rehabilitation or long-term acute care facilities) as compared to discharge home. Age was not associated with increased length of stay but was associated with discharge to home with healthcare services or to another healthcare facility (Skilled nursing, rehabilitation or long-term acute care facilities) as compared to discharge home. In this model, female patients were more likely to be discharged to home with healthcare services another healthcare facility (Skilled nursing, rehabilitation or long-term acute care facilities) than to home. When controlling for age, gender, ISS, comorbidities, ventilator free days, and injuries, the association between lymphopenia and mortality was no longer observed (OR = 1.140 [0.617–2.107], p = 0.676). Variables associated with mortality included age and ISS. (Table 4)
Table 3.
Multivariate analysis showing an association between lymphopenia and hospital length of stay, discharge to home with healthcare services or to another healthcare facility.
| Parameter | Hospital Length of Stay | Discharge disposition to home with healthcare | Discharge disposition to another healthcare facility | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | 95% CI | ||||||||||
| OR | Lower | Upper | p value | OR | Lower | Upper | p value | OR | Lower | Upper | p value | |
| (Intercept) | 2.933 | 1.343 | 6.404 | 0.007 | 0.051 | <0.001 | ||||||
| Age | 1.002 | 0.998 | 1.005 | 0.287 | 1.019 | 1.003 | 1.035 | 0.018 | 1.042 | 1.033 | 1.051 | <0.001 |
| Female | 1.001 | 0.885 | 1.132 | 0.985 | 1.846 | 1.083 | 3.146 | 0.024 | 1.698 | 1.258 | 2.292 | 0.001 |
| Tobacco use | 1.110 | 0.972 | 1.268 | 0.122 | 0.911 | 0.512 | 1.623 | 0.753 | 0.771 | 0.564 | 1.053 | 0.102 |
| Heart failure | 1.164 | 0.876 | 1.548 | 0.294 | 5.967 | 1.418 | 25.107 | 0.015 | 5.061 | 1.850 | 13.845 | 0.002 |
| Hypertension | 1.119 | 0.980 | 1.277 | 0.096 | 0.761 | 0.410 | 1.411 | 0.386 | 0.973 | 0.707 | 1.337 | 0.864 |
| Chronic kidney disease | 0.957 | 0.708 | 1.292 | 0.773 | 0.651 | 0.123 | 3.440 | 0.613 | 0.948 | 0.403 | 2.229 | 0.902 |
| Cancer | 1.115 | 0.867 | 1.433 | 0.395 | 0.544 | 0.195 | 1.516 | 0.244 | 0.898 | 0.466 | 1.731 | 0.747 |
| Transplant | 1.111 | 0.547 | 2.256 | 0.771 | 0.332 | 0.026 | 4.244 | 0.396 | 0.594 | 0.105 | 3.347 | 0.555 |
| ISS | 1.036 | 1.030 | 1.042 | <0.001 | 1.077 | 1.045 | 1.109 | <0.001 | 1.112 | 1.092 | 1.132 | <0.001 |
| Isolated chest injury | 0.993 | 0.811 | 1.216 | 0.946 | 1.320 | 0.556 | 3.134 | 0.529 | 1.008 | 0.633 | 1.604 | 0.974 |
| Chest and head injury | 0.896 | 0.729 | 1.103 | 0.301 | 0.946 | 0.367 | 2.442 | 0.909 | 0.852 | 0.515 | 1.407 | 0.531 |
| Chest and face injury | 0.933 | 0.581 | 1.497 | 0.773 | 3.901 | 0.920 | 16.538 | 0.065 | 1.123 | 0.369 | 3.419 | 0.838 |
| Chest and abdominal injury | 0.758 | 0.549 | 1.048 | 0.094 | 0.515 | 0.113 | 2.352 | 0.392 | 0.329 | 0.153 | 0.711 | 0.005 |
| Chest and extremity injury | 1.181 | 0.953 | 1.464 | 0.129 | 1.200 | 0.455 | 3.165 | 0.713 | 1.446 | 0.890 | 2.347 | 0.136 |
| Chest and external injury | 0.824 | 0.604 | 1.123 | 0.220 | 0.365 | 0.046 | 2.893 | 0.340 | 0.923 | 0.467 | 1.821 | 0.816 |
| Lymphopenia | 1.151 | 1.026 | 1.291 | 0.017 | 1.735 | 1.039 | 2.899 | 0.035 | 1.380 | 1.044 | 1.823 | 0.024 |
Note: Other healthcare facilities included skilled nursing, rehabilitation, or long-term acute care facilities.
Table 4.
Multivariate binary logistic regression showing no association between lymphopenia and mortality.
| Parameter | In-hospital mortality | |||
|---|---|---|---|---|
| OR | 95% CI | p value | ||
| Lower | Upper | |||
| (Intercept) | 0.999 | |||
| Age | 1.022 | 1.003 | 1.042 | 0.024 |
| Female | 1.177 | 0.558 | 2.486 | 0.668 |
| Tobacco use | 0.860 | 0.414 | 1.787 | 0.687 |
| heart failure | 3.854 | 1.004 | 14.796 | 0.049 |
| Hypertension | 0.869 | 0.418 | 1.804 | 0.706 |
| Chronic kidney disease | 3.813 | 1.005 | 14.468 | 0.049 |
| Cancer | 0.776 | 0.197 | 3.055 | 0.717 |
| Transplant | 49033948.142 | 0.000 | 0.999 | |
| ISS | 1.063 | 1.035 | 1.093 | <0.001 |
| Isolated chest injury | 1.869 | 0.534 | 6.539 | 0.327 |
| Chest and head injury | 1.681 | 0.654 | 4.321 | 0.281 |
| Chest and face injury | 0.922 | 0.058 | 14.767 | 0.954 |
| Chest and abdominal injury | 0.962 | 0.166 | 5.571 | 0.966 |
| Chest and extremity injury | 2.921 | 0.430 | 19.863 | 0.273 |
| Chest and external injury | 0.884 | 0.097 | 8.090 | 0.913 |
| Ventilator free days | 0.656 | 0.597 | 0.720 | <0.001 |
| Lymphopenia | 1.140 | 0.617 | 2.107 | 0.676 |
DISCUSSION
Herein, we show that admission lymphopenia in blunt chest wall trauma patient was associated with longer length of stay and need for increased health resources at discharge. These findings are indicative of prolonged recovery in these patients. Contrary to a previous study by Manson et al.,(11) no association was observed between admission lymphopenia and mortality when controlling for significantly different variables between our lymphopenic BCWT patients and non-lymphopenic BCWT patients.
Our study indicates that patients who experience BCWT and are lymphopenic within 24 hours of injury are more likely to have prolonged length of stay in the hospital. We confirm recent literature showing an association with higher ISS and prolonged length of stay.(4) Our data indicate that lymphopenia within 24 hours of injury is a slightly more potent predictor of prolonged hospitalization than ISS. These findings suggest an overall prolonged recovery in lymphopenic BCWT patients. Identifying a way to predict which patients are at increased risk for prolonged length of stay provides an opportunity to better address patient needs during the hospital stay as length of stay is one of the largest contributors to hospital cost.(22) Other studies have shown increased length of stay associated with increased age (Pressley, Crystal M. et al. 2012). Our data did not demonstrate a difference in length of stay at advanced age; however increased age was associated with discharge to facility. Providing trauma surgeons with an additional tool that can provide important prognostic information and help set expectations for patients and their families as it has been shown that effective physician-patient communication leads to overall improved patient outcomes. (23)
Our data also demonstrated that admission lymphopenia was associated with a higher likelihood of discharge to home with healthcare assistance or to SNF, rehabilitation facilities, or long-term acute care hospitals as compared to discharge to home without assistance. This finding shows added contribution to the overall cost of healthcare for lymphopenic BCWT patients beyond just longer length of hospital stay. Previous literature has shown ISS as a predictor of outcome in BCWT patients.(4) However, our data demonstrate a stronger association between lymphopenia and discharge disposition than that with ISS. In addition to the strength of the association, lymphocyte count proves superior to injury scoring systems in terms of simplicity. It is readily accessible at the patient’s bedside as part of a complete blood count (CBC) differential and requires no complicated reference materials or clinical calculators. Rapid access to this valuable tool can provide important prognostic information and help set expectations for patients and their families. This is an important prognostic tool to inform family discussions early on during the hospital stay, providing a rapidly accessible metric to help predict a more prolonged recovery.
This study presents some limitations. First, this is a retrospective study, which introduces a risk of selection bias and incomplete data capture from poor documentation or missing data. Secondly, this a single institution study and, therefore, our results may not be directly applicable in other settings. Additionally, our trauma order set was changed during our study period, removing the option for CBC with differential. This led to fewer patients with a differential drawn in the trauma bay, which limited our cohort to only 41% of the initial BCWT population. (Figure 1) While we aimed to look at the trend of lymphocyte counts over the hospital course, we were unable to do so as very few patients had serial CBC differentials ordered within the first week of admission, further limiting our potential for more definitive predictions about patient outcomes. However, our data demonstrate strong associations even with a single ALC. Lastly, our data is limited to in-hospital mortalities and outcomes, restricting our ability to analyze the impact that lymphopenia has on long-term outcomes. Despite these limitations, our study did demonstrate a strong association between lymphopenia on admission and discharge disposition in BCWT patients. Determining lymphopenia on admission by ordering a simple CBC differential for all trauma patients has the potential to easily identify patients at risk for poor outcomes.
CONCLUSIONS
Early and accurate identification of patients at risk for prolonged recovery is important for appropriate care of trauma patients beyond hospitalization. In our study population, we show an association between lymphopenia on admission and discharge requiring increased healthcare support. Our data suggest that lymphopenic patients following blunt chest wall trauma may have a longer recovery than their counterparts. Such information may be useful for providers when discussing patient care post-hospitalization, providing the patient and family with realistic expectations. Routine lymphocyte count monitoring on admission in BCWT patients may provide important prognostic information and help when discussing discharge planning. Further studies examining lymphocyte trends during hospitalization are warranted to evaluate the impact of quantitative and qualitative immune changes on patient recovery.
ACKNOWLEDGEMENTS
The authors wish to thank Michele Lilienthal, RN for her guidance and assistance extracting data from our institutional trauma registry.
FUNDING
K.E.K. was supported by the NIH grant T32CA148062. (P.I.: Ronald J. Weigel).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This work was presented as a virtual quick-shot presentation at the 16th Annual Academic Surgical Congress meeting in February 2021 (Abstract #: ASC20210926).
Declaration of Competing Interest
The authors declare no conflict of interests.
REFERENCES
- 1.Centers for Disease Control and Prevention. Ten Leading Causes of Death and Injury. Available at: http://www.cdc.gov/injury/wisqars/leadingcauses.html.
- 2.Centers for Disease Control and Prevention National health expenditures, average annual percent change, and percent distribution, by type of expenditure: United States, selected years 1960–2017. Available at: https://www.cdc.gov/nchs/hus/contents2018.htm#Table_043 Accessed April 27, 2020.
- 3.Agency on Aging https://acl.gov/aging-and-disability-in-america/data-and-research/projectedfuture-growth-older-population,.
- 4.Chrysou K, Halat G, Hoksch B, Schmid RA, Kocher GJ Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients—still a relevant problem? Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine 2017:25:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsia RY, Wang E, Saynina O, Wise P, Perez-Stable EJ, et al. Factors associated with trauma center use for elderly patients with trauma: a statewide analysis. Arch Surg 2011:146:585–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Joseph B, Pandit V, Zangbar B, Kulvatunyou N, Hashmi A, et al. Superiority of Frailty Over Age in Predicting Outcomes Among Geriatric Trauma Patients. JAMA Surgery 2014:149:766. [DOI] [PubMed] [Google Scholar]
- 7.Zafonte RD, Hammond FM, Mann NR, Wood DL, Black KL, et al. Relationship between Glasgow coma scale and functional outcome. Am J Phys Med Rehabil 1996:75:364–369. [DOI] [PubMed] [Google Scholar]
- 8.Vulliamy PE, Perkins ZB, Brohi K, Manson J Persistent lymphopenia is an independent predictor of mortality in critically ill emergency general surgical patients. Eur J Trauma Emerg Surg 2016:42:755–760. [DOI] [PubMed] [Google Scholar]
- 9.Morotti A, Marini S, Jessel MJ, Schwab K, Kourkoulis C, et al. Lymphopenia, Infectious Complications, and Outcome in Spontaneous Intracerebral Hemorrhage. Neurocrit Care 2017:26:160–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ritzel RM, Doran SJ, Barrett JP, Henry RJ, Ma EL, et al. Chronic Alterations in Systemic. Immune Function after Traumatic Brain Injury. J Neurotrauma 2018:35:1419–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Manson J, Cole E, De’Ath HD, Vulliamy P, Meier U, et al. Early changes within the lymphocyte population are associated with the development of multiple organ dysfunction syndrome in trauma patients. Critical Care 2016:20:176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heffernan DS, Monaghan SF, Thakkar RK, Machan JT, Cioffi WG, et al. Failure to normalize lymphopenia following trauma is associated with increased mortality, independent of the leukocytosis pattern. Crit Care 2012:16:R12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drewry AM, Samra N, Skrupky LP, Fuller BM, Compton SM, et al. Persistent lymphopenia after diagnosis of sepsis predicts mortality. Shock 2014:42:383–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Girardot T, Rimmele T, Venet F, Monneret G Apoptosis-induced lymphopenia in sepsis and other severe injuries. Apoptosis 2017:22:295–305. [DOI] [PubMed] [Google Scholar]
- 15.Venet F, Chung CS, Kherouf H, Geeraert A, Malcus C, et al. Increased circulating regulatory T cells (CD4(+)CD25 (+)CD127 (−)) contribute to lymphocyte anergy in septic shock patients. Intensive Care Med 2009:35:678–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Manson J, Hoffman R, Chen S, Ramadan MH, Billiar TR Innate-Like Lymphocytes Are Immediate Participants in the Hyper-Acute Immune Response to Trauma and Hemorrhagic Shock. Front Immunol 2019:10:1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eghbalzadeh K, Sabashnikov A, Zeriouh M, Choi YH, Bunck AC, et al. Blunt chest trauma: a clinical chameleon. Heart 2018:104:719–724. [DOI] [PubMed] [Google Scholar]
- 18.Ludwig C, Koryllos A Management of chest trauma. J Thorac Dis 2017:9:S172–s177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology 2007:18:805–835. [DOI] [PubMed] [Google Scholar]
- 20.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology 2007:18:800–804. [DOI] [PubMed] [Google Scholar]
- 21.NIH National Heart Lung, and Blood Institute Lymphocytopenia: https://www.nhlbi.nih.gov/health-topics/lymphocytopenia.
- 22.Geraerds AJLM, Haagsma JA, De Munter L, Kruithof N, De Jongh M, et al. Medical and productivity costs after trauma. PLOS ONE 2019:14:e0227131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stewart MA Effective physician-patient communication and health outcomes: a review. Cmaj 1995:152:1423–1433. [PMC free article] [PubMed] [Google Scholar]


