Abstract
The COVID-19 pandemic caused by highly-infectious virus namely severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has resulted in infection of millions of individuals and deaths across the world. The need of an hour is to find the innovative solution for diagnosis, prevention, and cure of the COVID-19 disease. Nanotechnology is emerging as one of the important tool for the same. In the present review we discuss the applications of nanotechnology-based approaches that are being implemented to speed up the development of diagnostic kits for SARS-CoV-2, development of personal protective equipments, and development of therapeutics of COVID-19 especially the vaccine development.
Keywords: COVID-19, SARS-CoV-2, nanotechnology, nanomaterials, nanostructures, vaccine, diagnostics
1. Introduction
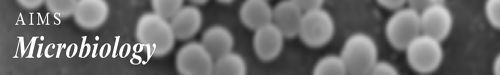
Coronavirus disease 2019 (COVID-19) is an infectious disease caused by virus namely severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This virus belongs to Coronaviridae family. SARS-CoV-2 is an enveloped virus with an average diameter of 60–140 nm and contains a single-stranded, positive-sense RNA [1]. The genome of SARS-CoV-2 is around 30 Kb, and it encodes for several accessory proteins and four structural proteins: spike (S), envelope (E), membrane (M), and nucleocapsid (N) (Figure 1) [2].
Figure 1. Structure of SARS-CoV-2.
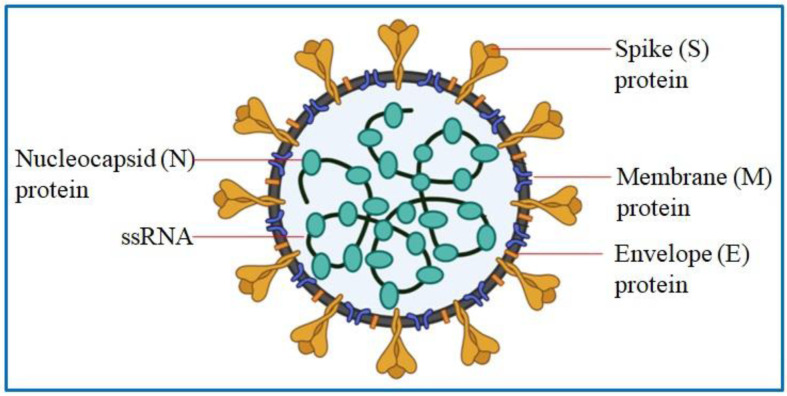
The virus, after being first discovered in Wuhan, China, has spread to all over the world and has caused over 1.2 million deaths and over 49.7 million total cases of infection as of 26 July 2021 [3]. Respiratory droplets released during coughing and sneezing and direct contact with infected individual transmit SARS-CoV-2 to healthy individual [4]. The virus mainly affects the respiratory system and can cause acute respiratory distress syndrome and multiple-organ failure, thus leading to patient's death [5]–[6]. COVID-19 affects many organs of the body, so people with COVID-19 may have a wide spectrum of symptoms. Symptoms and signs of the illness may be important to help them and the healthcare staffs they come into contact with know whether they have the disease. Most infected people with SARS-CoV-2 develop mild to moderate illness and recover without hospitalization and specialized treatment. The older people and those with medical complications such as chronic respiratory disease, cardiovascular disease, cancer, and diabetes are more vulnerable and more likely to develop serious illness. Most common symptoms, less common symptoms and serious symptoms associated with SARS-CoV-2 infection are represented in Figure 2.
Figure 2. Most common symptoms, less common symptoms and serious symptoms associated with SARS-CoV-2 infection.
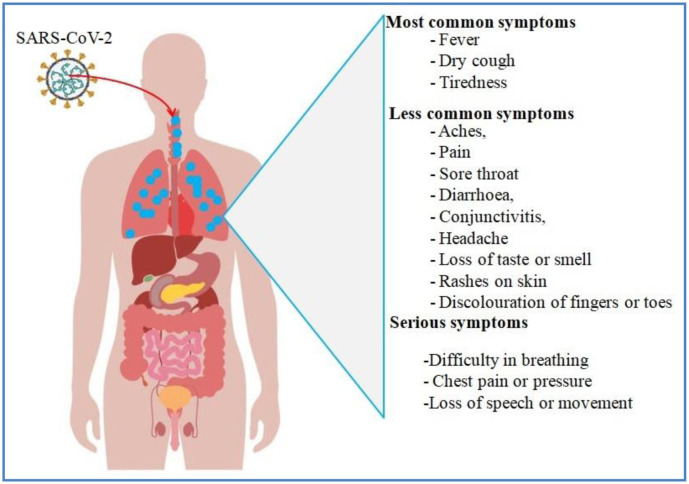
Mutations in the genome of SARS-CoV-2 have given rise to various new variants reported from many countries namely Brazil, India, South Africa, and the United Kingdom. These new variants are deadlier with higher transmission rate as compared to original strains. Moreover, these variants increase the chance of reinfection and have negative impact on the effectiveness of vaccines-induced immunity [7]. To prevent the spread of the COVID-19, the officials of the countries across the world, enforced various strategies such as suspension of traveling, prolonged lockdown, quarantine, and mandatory facial protection. Such measures indeed decreased the spread of the viral infection, but the limitations of these measures make the unsustainable in a long run due to the involvement of major socioeconomic cost [8]–[10]. Therefore, long-term innovative solution is need of an hour to fight the virus due to limited economic resources. Nanotechnology is one such innovative tool that has emerged with higher success rate in the field of therapeutics and diagnosis and imaging of various diseases [11]. Nanotechnology approaches normally utilizes nanoscale particles (i.e., nanostructures) falling under 1 to 100 nm range. But some authorities extend the definition of nanostructures to include molecules up to 1000 nm size [12]. Nanostructures' small size, large surface to volume ratio, surface charge, bioavailability, biodegradability, biocompatibility, and ability to be modified through surface modification impart nanomaterials unique physicochemical properties that made nanomaterials attractive for biomedical application [13]–[15]. Various types of nanostructures and nanomaterials including metal nanostructures, transition metal oxide nanostructures (emerging nanomaterials that have shown excellence in various fields),carbon-based nanostructures (carbon nanotubes, graphene and graphene oxide), lipid-based nanostructures (nanosized micelles/vesicles),quantum dots, and polymeric nanostructures are being used as theranostic (i.e., therapeutic and diagnostic) agents against viral infections [16]. The last few years have seen increasing use of nanostructures for the treatment of viral infections, such as HIV, hepatitis B virus, Hepatitis C virus, H1N1, herpes simplex virus, human papilloma virus, Zika virus, respiratory syncytial virus, and human norovirus [17]–[19]. During the start of COVID-19 pandemic biomedical researchers proposed that nanotechnology may play an important role in managing the COVID-19pandemic [20]–[24]. The prediction was surely found to be true as can be gauged from the related reports emerging across the globe. For example, scientists have taken advantage of nanotechnology to develop biosensors in order to detect SARS-CoV-2 in patient samples, and to develop antiviral products that can be implemented to prevent the transmission of SARS-CoV-2 [25]. Along with this, nanotechnologies have also been successfully used and are being used to develop therapeutic agents and vaccines against SARS-CoV-2 [25]. In the present review we discuss the nanotechnology-based approaches that are being utilized to mitigate COVID-19 disease. The first section the review summarizes recent studies that have implemented nanotechnology based approaches to speed up the development of diagnostic kits for SARS-CoV-2. The second section discuses the use of nanotechnology based approaches in the development of personal protective equipments such as face masks, sanitizers, surface coatings, etc. in order to prevent the spread of virus. Finally, the third section of the review discuses the application of nanotechnology in therapeutics of COVID-19 especially in the field of vaccine development against SARS-CoV-2.
Figure 3. Functional aspects of nanotechnology against COVID-19 pandemic.
2. Role of nanotechnology in the detection of SARS-CoV-2
Despite the development of new vaccines against COVID-19 (developed by the companies such as Pfizer, Moderna, Johnson & Johnson, Bharat Biotech International Limited, and Oxford-AstraZeneca), the importance of early rapid detection to control and prevent COVID-19 cannot be further emphasized due to the need to isolate the infected person from rest of the people living in the vicinity to prevent spread of the infection to the still unvaccinated population. There are mainly two types of approaches to detect the presence of SARS-CoV-2. One is the diagnostic approach that involves either detection of viral nucleic acid (i.e. molecular test/assay) or viral antigens (i.e. antigen test). The second one is serological approach that detects the presence of immunoglobulin G (IgG) and/or immunoglobulin M (IgM) or total antibodies produced in a person infected with SARS-CoV-2 [26]. World Health Organization (WHO) has mandated reverse transcription polymerase chain reaction (RT-PCR) as the standard test to diagnose SARS-CoV-2 in patient samples. But RT-PCR is not available everywhere due to economic constraints and the lack of infrastructure, and its results could take from few hours to many days due to insufficient human or lab capacities [27]. This time lag can lead to the spread of COVID-19 to a wider community and loss of precious life that could have been saved only if the person had been diagnosed earlier. In these circumstances, point-of-care testing that should be reliable, cheap, and fast and should provide results within short time window has become need of an hour for the prevention of COVID-19 pandemic. Because nanostructures are of similar size to that of SARS-CoV-2, nanostructures can bind to the virus and thus can be utilized for therapy and detection of COVID-19 infection [28]. The use of nanotechnology and nanostructures in order to develop diagnostic and serological tests for COVID-19 infection is increasing greatly [29]–[32]. Nanomaterials can be functionalized with biomolecules to detect and amplify signal in colorimetric detection of pathogens [33], and large surface area of nanostructures increases capture efficiency of, and thus sensitivity of a biosensor [34]. Similarly, the functionalization of nanostructures with antibodies against SARS-CoV-2 increases sensitivity and affinity of biosensor for the analyte and enhances signals (e.g. electrochemical, electrochemiluminescent, magnetic, or optical signals) thus making the detection of target molecule and of COVID-19 infection easier [35]. Table 1 lists the examples of nanomaterials that are being used to devise biosensor to detect SARS-CoV-2.
Table 1. Some recent studies using nanomaterials in the biosensor for detecting SARS-CoV-2.
| Nanomaterial/nanostructures | Detection of molecule | Limit of detection | Study |
| Gold nanostructures | Spike protein | 5 µg·mL–1 | [63] |
| Gold nanostructures | Spike protein | 80 copies mL−1 in contaminated water | [64] |
| Gold nanostructures | anti-SARS-CoV-2 IgG | Semi-quantitative | [37] |
| Gold nanostructures | RNA | 4 copies/µL | [65] |
| Gold nanostructures | N gene and E gene | 300 copies/µL of E gene; 225 copies/µL of N gene | [66] |
| Gold nanostructures | Viral proteins of SARS-CoV-2 trapped in surgical face masks | 3 ng mL−1 | [62] |
| Gold nanostructures | RNA | 50 RNA copies per reaction | [67] |
| Gold nanostructure | 16S rRNAs; N gene | (Not Reported) | [68] |
| Gold nanostructures | anti-SARS-CoV-2 IgG antibodies | 3.2 nM | [69] |
| Gold nanostructures | N gene | 0.18 ng/µL | [39] |
| Gold nanostructures | Viral particles | Viral loads corresponding to Ct = 36.5 | [38] |
| Gold nanostructures | RNA | 10 copies/µL | [70] |
| Gold nanostructures | anti-SARS-CoV-2 IgM | (Not reported) | [55] |
| Gold nanostructures | Highly conserved nucleoprotein | 250 pg/mL | [56] |
| Gold nanostructures | anti-SARS-CoV-2 IgG | (Not reported) | [57] |
| Gold nanostructures | Volatile organic compounds from breath | (Not reported) | [58] |
| Gold Nano star | Spike protein and the virus | 130 fg/mL for antigen and 8 particles/mL for virus | [71] |
| Gold nanoislands | RNA | 0.22 pM | [44] |
| Gold nanoisland films | RNA | 2.98 copies µL−1 | [72] |
| Gold nanostructures and spherical nucleic acid | RNA | (Not reported) | [73] |
| Gold nanostructures and spherical nucleic acid | RNA | Six copies of ssDNA per reaction | [36] |
| Gold nanostructures and graphite | Spike protein | 229 fg mL−1 | [74] |
| Gold and silver nanostructures | Spike protein | 0.77 fg mL−1 in PBS; 6.07 fg mL−1 in saliva; 7.60 fg mL−1 in serum; and 0.10 pg mL−1 in blood | [75] |
| (Not Reported) | SARS-CoV-2 total antibody | (Not Reported) | [76] |
| Gold-platinum core-shell nanostructures | Subunit S1 of spike protein (S) | 11 ng mL−1 | [77] |
| Gold nanostructure (AuNP)-decorated graphene field-effect transistor (G-FET) sensor | RNA | 0.37 fM in PBS; 2.29 fM in throat swab; and 3.99 fM in serum | [50] |
| Super paramagnetic nanostructures | anti-SARS-CoV-2 IgM and IgG | 10 ng/mL for IgM and 5 ng/mL for IgG | [78] |
| Lanthanide-doped nanostructures | anti-SARS-CoV-2 IgG | (Not Reported) | [79] |
| Selenium nanostructures | anti-SARS-CoV-2 IgM and IgG | 20 ng/mL for IgM and 5 ng/mL for IgG | [46] |
| Au/Ag coated carbon nanotubes | Live virus | (Not Reported) | [41] |
| Europium-chelate-based fluorescent nanostructures | RNA | 1,000 TU (transduction units) mL−1 | [80] |
| Ag shell on SiO2 core (SiO2@Ag) | anti-SARS-CoV-2 IgM/IgG | 1 pg/mL | [43] |
| (Not Reported) | Total antibody (IgA, IgM, and IgG) against SARS-CoV-2 | (Not Reported) | [81] |
| Cobalt functionalized-TiO2 nanotube | RBD domain of S protein | ~0.7 nM | [47] |
| Carbon black | Spike (S) protein or Nucleocapsid (N) protein | 19 ng/mL for S protein; 8 ng/mL for N protein | [60] |
| Carbon nanotubes | RNA | 6.4 copies/µL in PBS and 9.2 copies/µL in 50% human saliva | [48] |
| Graphene | Spike protein | 1.6 × 101 pfu/mL in culture medium; 2.42 × 102 copies/mL in clinical samples; 1 fg/mL in phosphate-buffered saline; 100 fg/mL in clinical transport medium | [49] |
| Graphene | Spike protein | ∼3.75 and ∼1 fg/mL in artificial saliva and phosphate-buffered saline, respectively | [82] |
| Reduced-graphene-oxide Nano flakes | Antibodies to spike S1 protein and its receptor-binding-domain (RBD) | 2.8 × 10−15 M for spike S1 protein and 16.9 × 10−15 M receptor-binding-domain | [51] |
| Quantum dot | Antibodies | 17.5 pM for nucleocapsid antibody and 24.4 pM for S1 antibody | [83] |
| Quantum dot Nano beads | SARS-CoV-2 total antibody | (Not Reported) | [84] |
| Enzyme-DNA hybrid Nano complexes | RNA | ~8 RNA copies/µL | [85] |
| Streptavidin coated polymer nanostructures | ORF1ab and N gene | 12 copies per reaction | [45] |
| Aggregation-induced emission (AIE) dye-loaded nanostructure | anti-SARS-CoV-2 IgM and IgG | 0.236 mL–1 for IgM; 0.125 µg mL–1 for IgG | [86] |
Many biosensing techniques for the detection of SARS-CoV-2 have utilized gold nanostructures (Table 1). Because these nanostructures are easier to synthesize, biocompatible, and physicochemically stable [36]. Karami and coworkers [37] devised a colorimetric detection technique for SARS-CoV-2 RNA by attaching spherical nucleic acids to the surface of gold nanostructures. The biosensing system included a 4-nucleotide palindromic linker to probe the E gene region of SARS-CoV-2 RNA. The assay was comparable in sensitivity to the real-time RT-PCR.
In an interesting approach, Sil and group [38] designed a type of qualitative immunoassay named as rapid flow-through dot-blot immunoassay. The group used gold nanostructures functionalized with antibodies to detect SARS-CoV-2 specific IgG in human serum, with sensitivity and specificity of 98.8% and 98%, respectively.
Ventura et al. [39] constructed gold nanostructures-based biosensor to detect SARS-CoV-2 in nasal and throat swabs. The researchers prepared three types of gold nanostructures, each functionalized with antibodies against spike, envelope, or membrane surface proteins of SARS-CoV-2. The three types of gold nanostructures were mixed in equal (1:1:1) ratio to make a colloidal solution, when interacted with virus particles, gave red color, which could be measured at 560 nm to quantify viral load. The detection method is a faster and better alternative to the RT-PCR method, because it does not require preparatory steps, such as RNA extraction and amplification. Further, the detection technique can quantify the viral load and severity of the viral infection, because the technique detects viral particles rather than SARS-CoV-2 RNA.
Moitra et al. [40] also utilized gold nanostructures and developed a colorimetric assay to detect SARS-CoV-2 in patient samples. The researchers functionalized gold nanostructures with thiol-modified antisense oligonucleotides specific for N-gene of SARS-CoV-2. In the presence of target RNA sequence of SARS-CoV-2, the functionalized gold nanostructures agglomerated, which could be detected by UV-Visible absorbance spectroscopy and other techniques including transmission electron microscopy, and hyper spectral microscopy. Further, when RNA samples with functionalized gold nanostructures were treated with enzyme RNase H at 65 °C for 5 min, the samples were precipitated that could easily be seen by naked-eye, thus avoiding the need for any sophisticated instrument to detect SARS-CoV-2. The bioassay was selective for SARS-CoV-2, because it did not produce any distinct change in absorbance in the presence of Middle East respiratory syndrome coronavirus (MERS-CoV) RNA; the limit of detection was 0.8 ng µL−1 for SARS-CoV-2.
Gold, silver and other nanostructures can show plasmonic effects that when combined with surface-enhanced Raman scattering (SERS) spectroscopy or surface-enhanced infrared absorption (SEIRA) spectroscopy can be used to detect small analyte at a very low concentration [41] and in the construction of point of care devices for virus detection [42],[43]. Jadhav and coworkers [44] exploited surface-enhanced Raman spectroscopy (SERS) by coupling it with a microfluidic platform that contained silver or gold nanostructures coated carbon nanotubes micro channels. Silver and gold nanostructures acted as plasmonic materials that could increase Raman intensity of even traces of SARS-CoV-2 in samples (eyes, nasal, throat, and saliva swabs) and helped in rapid of detection of the virus in the sample [44]. In another surface-enhanced Raman spectroscopy based lateral-flow immunoassay, Liu et al. [45] showed that using complete Ag shell on SiO2 core (i.e. core-shell nanostructures) resulted in 800 times increase in the sensitivity of biosensor for the detection of anti-SARS-CoV-2 IgM/IgG in comparison with that of standard gold nanostructures-based lateral-flow immunoassay method.
Recently, Qiu and coworkers [46] developed a dual-functional ultrasensitive biosensor based on plasmonic effects (plasmonic photo thermal effect and localized surface plasmon resonance) to detect SARS-CoV-2, with a detection limit of 0.22 × 10−12 M. The biosensor included two-dimensional gold nanoislands, a type of nanostructure, functionalized with complementary DNA, which when hybridized to RNA of SARS-CoV-2 could detect the presence of the virus.
Zhu et al. [47] devised a new diagnostic assay based on reverse transcription loop-mediated isothermal amplification method in combination with a nanostructure-based lateral flow biosensor to diagnose COVID-19 in patients. Zhu's group reported 100% sensitivity for the diagnostic assay, after analyzing 33 oropharynx swab samples from COVID-19 patients. The assay also showed very high specificity of 100% for COVID-19 negative samples. The assay was very fast and took only an hour to complete.
Wang's group [48] have recently exploited modified selenium nanostructures to prepare a lateral flow immunoassay kit that can detect anti-SARS-CoV-2 antibodies (IgG and IgM) in human serum, with naked-eye in only 10 minutes. The researchers tested the bioassay in 90 COVID-19-diagnosed patients and 263 non-infected controls and reported 93.33% sensitivity and 97.34% specificity.
Cobalt-functionalized TiO2 nanotubes (Co-TNTs) was used by Vadlamani et al. [49] to synthesize a non-expensive and highly sensitive electrochemical sensor that can detect the receptor-binding domain (RBD) domain of spike protein of SARS-CoV-2 in the concentration range of 14 to 1400 nM.
In the place of commonly used gold nanostructures in biosensor to detect SARS-CoV-2, some research groups used carbon nanotubes [41],[48], graphene [49],[50], and graphene-based (graphene oxide or reduced graphene oxide) [51] nanomaterials due to carbon nanotube's and graphene's high conductivity and biocompatibility [52],[53], and benefit of lower cost [29]. Further, the modification of graphene's surface with functional groups imparts the biosensor with very high sensitivity and ability to recognize biological molecule [54]. For example, Seo and colleagues [49] developed a graphene field-effect transistor (FET)-based biosensor device for the detection of SARS-CoV-2 in clinical samples. In this sensor, the researchers coated graphene sheets of field-effect transistor with a specific antibody against SARS-CoV-2 spike protein. The biosensor could detect the SARS-CoV-2 spike protein at concentration as low as of 1 fg/mL in phosphate-buffered saline (PBS) and of 100 fg/mL in clinical transport medium. The biosensor could further detect SARS-CoV-2 in clinical samples with the limit of detection of 2.42 × 102 copies/ml. The sensor can discriminate between SARS-CoV-2 antigen protein and MERS-CoV antigen protein, thus restricting any chance of cross-reactivity with MERS-CoV [49]. Li and collaborators [50] achieved amplification-free detection of SARS-CoV-2 RNA via a biosensor that included graphene field-effect transistor decorated with morpholino-modified gold nanostructure. The tests showed very low limit of detection of SARS-CoV-2 RNA in phosphate buffer saline (0.37 fM), throat swab (2.29 fM), and serum (3.99 fM); and the test took only 2 minutes to ascertain the SARS-CoV-2 infection in clinical throat swabs sample [50].
In another study, Huang et al. [55] developed lateral-flow assay based on colloidal gold nanostructures to detect IgM antibody against SARS-CoV-2 in serum samples of patients through immunochromatography. This assay can give results in only 15 minutes, and it needs only 20 µL of serum sample for each test in comparison with RT-PCR test that needs around 100 µL of the sample. The sensitivity and specificity of the nanostructures based lateral-flow assay were 100 and 93.3% respectively.
Similarly, Mertens and group [56] have prepared a diagnostic strip named as Ag Respi-Strip, which is based on the principles of immunochromatographic assay. The diagnostic strip utilized anti-SARS-CoV-2 (nucleocapsid protein) antibodies conjugated with colloidal gold nanostructures. The sensitivity and specificity of the test were 57.6% and 99.5%, respectively.
Wen et al. [57] reported a rapid point-of-care (POC) lateral-flow immunoassay based on colloidal gold nanostructures to diagnose SARS-CoV-2. The researcher's functionalized gold nanostructures to anti–human IgG, sprayed it onto the pre-treated conjugate pad that already contained SARS-CoV-2 nucleocapsid protein, and employed a change in color as a marker for the presence of viral protein in patient samples. The sensitivity and specificity of the assay were 69.1% and 100%, respectively.
Shan and coworkers [58] developed a novel biosensor that detects SARS-CoV-2 from exhaled breath. The sensor is based on the principle that during viral infection cells produce—due to interaction between host cells and virus—volatile organic compounds, which are present in the exhaled breath of a patient and thus can be used as a biomarker for the detection of a disease [59]. The sensor constructed by Shan's group (2020) [60] included a sensing layer composed of organic ligands and gold nanostructures. When exposed to volatile organic compounds present in exhaled breath, the sensing layer shrinks or swells and causes a volume change in the nanomaterial film that was captured by change in electric resistance. Although this technique needs to be validated in a larger cohort size, it can still be used for the rapid screening of COVID-19.
Fabiani et al. [54] have developed an electrochemical immunoassay for rapid detection of SARS-CoV-2 in saliva samples. Screen-printed electrodes used in the assay were based on carbon black nanomaterial, which due to its cost-effectiveness, electro catalytic properties, and biocompatibility is gaining popularity in the designing of electrochemical biosensors [61]. The assay could detect spike protein or nucleocapsid protein of the SARS-CoV-2. A detection limit of 100 fg/ml was found for nasopharyngeal swab samples from COVID-19 patients.
In a very interesting approach, Vaquer et al. [62] devised a non-invasive method for detecting SARS-CoV-2 proteins trapped in surgical face masks. The researchers used antibody-decorated gold nanostructures, which when comes in contact with SARS-CoV-2 antigens trapped in surgical face masks produce colorimetric signal; the whole assay takes only less than 10 minutes to complete.
3. Role of nanotechnology in preventing transmission of SARS-CoV-2
To prevent spread of COVID-19, social distancing, mask wearing, and hand sanitizing are being implemented. Similarly, products, such as face masks, face shields, disinfectants, and sanitizer are being used to minimize the spread of SARS-CoV-2 infection in the community. Although face masks protect the person from catching the virus, they do have certain limitations: (1) medical masks recommended for health workers are for single-use only; (2) face masks act only as a barrier to virus transmission, they do not inactivate virus; (3) N95 face masks provide only 95% filtration efficiency for particles more than 0.3 micron size [87], thus particles that are less than 200 nm, such as SARS-CoV-2 can pass through them. Nanotechnology-based solutions are being utilized to improve upon such limitations, because nanostructures can infiltrate viral coronae, can bind to the virus and prevent its attachment to the host cell surface during entry, and can inhibit viral replication thus preventing spread of infection [88],[89]. The embedding of nanomaterials can provide antiviral properties to (i.e., viral inactivation capability) and improve filtration ability of protective clothing [90]. Further, nanostructures can persist for longer duration and can be effective at a low concentration, which makes their use in disinfectants to sterilize air, physical surfaces, or skin beneficial [91]. Nanostructures can prevent spread of virus by various mechanisms: They can interact with the viral glycoproteins, thus prevent binding and penetration of viral glycoproteins to the host cell [91]; and on exposure to UV radiation, the nanostructures can generate reactive oxygen species that oxidize the viral membrane or envelope [91],[92]. Table 2 has listed some nanotechnology-based products that have claimed to prevent SARS-COV-2 transmission in community. The products are using various nanomaterials, including graphene, copper oxide, titanium dioxide, and silica, nanene (a type of graphene) in products, such as face masks, face shields, fabrics, packaging material, air filters, and coating (Table 2).
Table 2. Products based on nanotechnology to prevent SARS-CoV-2 transmission.
| Products | Nanostructures | Company/Organization | Country |
| Graphene Mask | Graphene | Flextrapower Inc | USA |
| Nano shield | CuO | Nanoveu Inc | Australia |
| Virucidal Graphene-Based Composite Ink | Graphene and Ag | ZEN Graphene Solutions Ltd | Canada |
| Guardian G-Volt respiratory mask | Graphene | LIGC Applications Ltd | USA |
| Co-Mask | Graphene | Directa Plus PLC | UK |
| Antiviral fabrics | Cu | Promethean Particles Ltd | UK |
| MVX Nano MaskTM | TiO2 | MVX Prime Ltd | UK |
| Nano Silver Sanitizer | Ag | Shepros Sdn. Bhd. | Malaysia |
| ReSpimask® VK (Virus Killer) | CuO | Respilon Group S. R. O. | Czech Republic |
| Diamond Face Mask | Diamond | Master Dynamic Limited | China |
| NANOHACK | CuO | Copper 3D Antibacterial Innovations | Chile |
| G1 Wonder Face Masks | Graphene | Nanomatrix Materials | India |
| Nanocoating | (Not reported) | Nanoksi Finland | Finland |
| Nanofense | Ag | Applied Nanoscience Inc. | USA |
| Transparent stretchable PVC film for use in packaging | Silver and silica | Alpes and Nanox | Brazil |
| Graphene Face Mask | Graphene | Medicevo | USA |
| Nanofiber Membranes | (Not reported) | BYU's College of Engineering with Nanos Foundation | USA |
| ZEN's Virucidal Ink | Graphene | ZEN Graphene Solutions Ltd. | Canada |
| Nano-coated air filters | (Not reported) | University of Houstan | USA |
| Graphene Enhanced Protective Face Mask | Nanene | Versarien | UK |
| Nano Textile Coating | (Not reported) | IIT Madras and Muse | India |
| Rubber, paint, coating, and cosmetics | ZnONPs | Brüggemann | Germany |
The nanostructures impregnated to the face masks can kill viral particles remained in the masks without altering filtering properties of face masks and thus can ensure further reduction in risk of viral infection due to incorrect handling and disposal of face masks [95]. Very recently, a research team from Korea Advanced Institute of Science and Technology (KAIST), Daejeon, South Korea has developed a nanotechnology-based filter that retains excellent filtering efficiency even after washing for more than 20 times [96]. The use of such filters can solve the problem of shortage of face masks. The researchers used orthogonal nanofibers and insulation block electrospinning process to create the face mask. According to the scientist, the nanofiber filter is water-resistant and shows 94% filtration efficiency after 20 repeated bactericidal tests with ethanol [96].
Similarly, Queensland University of Technology-based research team has constructed biodegradable face masks based on nanotechnology [97]. The face mask is made of cellulose nanofiber obtained from plant waste and agricultural waste. The breathable nanocellulose material can filter particles smaller than 100 nm, which is the size of several human viruses, including SARS-CoV-2.
Wakamono, which is a Vietnam based company working in field of nanotechnology, has announced that it has created the world's first anti-coronavirus surgical masks [98]. The mask is made of GECIDE fabric technology that utilizes organic nanostructures and can inactivate SARS-CoV-2 up to 99%. The mask is also effective against influenza A H1N1 and poliovirus I [98].
Tremiliosi et al. [99], in a recent study, functionalized polycotton fiber with silver nanostructures by the pad-dry-cure method. The composite fibers were found to inhibit the SARS-CoV-2 only after two minutes incubation. The fiber has the potential to be used in textile materials that can stop the transmission of SARS-CoV-2.
Jeremiah and group [100] have recently showed the antiviral effect of silver nanostructures on SARS-CoV-2 viral suspension. This study showed that silver nanostructures can be used as surface coating to deactivate SARS-CoV-2 and prevent their further transmission. The angiotensin-converting enzyme 2 (ACE2) receptor-expressed by various organs, such as liver, heart, kidney, lungs, etc. [101] plays an important role in the entry of SARS-CoV-2 into host cells [102]. But, the receptor can also play protective role in acute lung injury [103]; this fact prompted Aydemir and Ulusu [104] to propose that nanomaterials coated with ACE2 can be used to prepare clothes, mask, gloves, and other protective covers to sequester virus and block their entry into the host.
Products based on graphene and its derivatives (graphene oxide, reduced graphene oxide, and graphene quantum dots) as argued by Raghav and Mohanty [105], have the potential to be used against SARS-CoV-2 infection. The mono- or multi-layers graphene and its derivatives can be applied either as coating on fabrics to keep them dry to prevent aerosol transmission of SARS-CoV-2, or as a mist spray and cleaning solution to sanitize the infected surfaces of an object or human body [105]. The antiviral effect of graphene oxide and its Nano composite on feline coronavirus, an enveloped virus, has shown by Chen et al. [106]. Similar application of graphene oxide against SARS-CoV-2, also an enveloped virus, can be tried by using coatings of graphene oxide on clothes to make antiviral protective products.
De Maio and group [107] showed that polyurethane and cotton both used in personal protective equipment when functionalized with graphene nano platelets or graphene oxide can entrap SARS-CoV-2. When the SARS-CoV-2 culture was incubated with or filtered through the functionalized polyurethane and cotton material, the capacity of the virus to infect Vero cells (African green monkey kidney epithelial cell) decreased. However, the concentration range of graphene oxide (0.06–0.5 mg/mL) used in the experiment is not realistic for the purposes of therapeutics against SARS-CoV-2. Unal's group [112] in different experiment via molecular docking method and in vitro method showed that graphene oxide sheets could decrease infectivity of SARS-CoV-2 by interacting with its viral spike protein. The efficacy of graphene oxide sheets were also shown to be persisted when different mutations were present in the viral spike protein [112].
The Guardian G-Volt Respiratory mask by LIGC Applications employs a graphene filtration system [109]. This mask is 99% effective against particles over 0.3 micrometers, in comparison with N95 respirator mask that can only blocks 95 per cent of particles over 0.3 micrometers, thus having the potential to prevent SARS-CoV-2 transmission [113].
Coating of silver nanocluster/silica composite onto disposables facial FFP3 masks (3M™) have been shown to reduce the titer of SARS-CoV-2 to zero [114]. The application of the antiviral coating can be extended to other surfaces, such as ceramic, glass, and metallic to prevent the spread of the virus in public areas [115].
Kumar's group [96] has created a photoactive antiviral mask, which was coated with hybrid of copper nanostructures and shellac, a hydrophobic biopolymer. As per researchers, under the sunlight the temperature of the mask could reach >70 °C, which in turn give rise to free radicals that can disrupt the membrane of virus-like particles and give the mask self-sterilization capability. The mask can be a great asset against protection from SARS-CoV-2 and COVID-19 pandemic.
Although the COVID-19 pandemic is witnessing the emergence of many commercial products (e.g., face masks, coatings, etc.) that claim to be using nanostructures and be effective against SARS-CoV-2, such claims must be duly scrutinized to save consumer from any harm from potential exposure to the virus. For example, Blevens et al. [112] evaluated the claims of 40 cloth face masks that claimed to be using either silver or silver nanostructures and to have antiviral properties. The researchers concluded that the claims made by companies on using nanostructures in face masks are not always true, and further the filtration efficiency might not up to the standard certification requirement. The researchers proposed stricter regulation of products by governmental agencies to ensure efficacy of the face masks for safety of the consumer [112]. Similarly, there is a persisting concern among scientist due to the long-term effect of nanomaterial application in protective fabrics to the environment and to the person wearing the protective covering [86]. Further, the widespread uses of masks have inevitably accelerated the release of nanoplastics, micro plastics, and chemical pollutants from disposable masks to the environment [113],[114]. If the scientists could combine use of nanomaterials in masks with new nanotechnology that degrade micro plastics such as that shown by Kang's group [115], then it would be better for the environment and for people's health. Another approach to decrease the toxicity of metal nanostructures to the person using protective fabrics as suggested by Sportelli et al. [123] in a review article was to impregnate copper salt along with nanomaterials into the masks, personal protective clothing, and fabrics.
4. Role of nanotechnology in therapeutics development against SARS-CoV-2
Multiple research groups all over the world are working on therapeutic agents to prevent COVID-19. For example, as of 31 July 2021, more than 200 vaccines (including both in clinical and preclinical evaluation) against SARS-CoV-2 are in development [116]. Among these, seven (BNT162b2 or Comirnaty by Pfizer–BioNTech, mRNA-1273 by Moderna, AZD1222 by Oxford–AstraZeneca, Ad26.COV2.S by Janssen, Covishield by Serum Institute of India, BBIBP-CorV by Sinopharm-BBIBP, and CoronaVac by Sinovac) have been recognized by the World Health Organization for emergency use [117]. Recently, the U.S. Food and Drug Administration (FDA) has approved the Comirnaty. It is a vaccine for preventing coronavirus disease 2019 (COVID-19) in people aged 12 years and older. Comirnaty contains a molecule called messenger RNA (mRNA) with instructions for producing a protein from SARS-CoV-2, the virus that causes COVID-19. Comirnaty does not contain the virus itself and cannot cause COVID-19.Before the advent of any officially approved vaccine for use against COVID-19, the first approach of the scientists all over the world was to repurpose existing medicines including chloroquine, hydroxychloroquine, favipiravir, interferon, lopinavir, nitazoxanide, remdesivir, ribavirin, ritonavir, and umifenovir [118]. But interim results of the World Health Organization's SOLIDARITY trial found no significant effect for such drugs on COVID-19 patients [119]. In these circumstances, vaccines and other therapeutics agent that are being developed are only hope for protecting people from SARS-CoV-2. Many vaccines that are in pipeline against COVID-19 are exploiting nanotechnology, because nanostructures can increase the solubility of drugs, cross blood–brain barrier, increase half-life of drugs, decrease toxicity of drugs, and in some cases can deliver drug to the target organ and tissue inside the body, thus decreasing the toxicity of drugs [120]–[122]. Nanomaterials such as liposomes, micelles, polymeric nanostructures, lipid nanostructures (LNPs), and lipid-polymer hybrid nanostructures have also shown their importance for drug delivery [123]. Further, the surfaces of nanostructures can be modified by various molecule and functional group for desired biological properties.
Virus-like particles (VLPs) are a type of lipid-polymer hybrid nanostructures that are derived from self-assembly of viral capsid or envelope proteins and are non-infectious because they do not contain genetic material and ability to replicate [124],[125]. VLPs mimic virus particles and can be constructed via recombinant technology to present peptide antigen that could elicit immune response, and thus can be used in the development of vaccines [126]. The VLPs can be engineered to display antigen or epitope in highly ordered repeating manner, which gives VLPs high immunogenicity that can generate strong cellular and humoral immune responses with induction of high affinity antibodies [127],[128]. Further, VLPs due to its small size range (20–200 nm) [129] can also act as an efficient nanoacarrier for foreign (i.e. not related to VLPs itself) antigens that helps them in readily taken up by antigen presenting cells to stimulate the immune system [130],[131].
VLP-based vaccines have been successfully developed against many inflammatory or infectious diseases, such as human papillomavirus, hepatitis B virus, etc. [132]. Many companies are developing VLPs-based vaccines (some are in clinical phase, while others are in preclinical phase) against SARS-CoV-2 (Table 3).
Table 3. Virus-like particles (VLPs) Vaccine against SARS-CoV-2.
| VLPs-based COVID-19 vaccine in clinical development | ||
| Vaccine | Developer | Trial phase |
| CoVLP | Medicago; GSK; Dynavax | Phase 3 |
| SARS-CoV-2 VLP Vaccine | The Scientific and Technological Research Council of Turkey; Dr Abdurrahman Yurtaslan Ankara Oncology Training and Research Hospital; MonitorCRO; Nobel Pharmaceuticals | Phase 2 |
| IVX-411 | Icosavax, Inc.; Bill & Melinda Gates Foundation; Amgen; Seqirus | Phase 1/2 |
| VBI-2902a | VBI Vaccines Inc. | Phase 1/2 |
| ABNCoV2 | ExpreS2ion Biotech; Bavarian Nordic A/S | Phase 1/2 |
|
| ||
| VLPs-based COVID-19 vaccine in preclinical phase | ||
| Vaccine | Developer | Country |
|
| ||
| VLP | Max Planck Institute for Dynamics of Complex Technical Systems | Germany |
| Virus-like particle-based Dendritic Cell(DC)-targeting vaccine | University of Manitoba | Canada |
| VLP | Bezmialem Vakif University | Turkey |
| Enveloped Virus-Like Particle (eVLP) | VBI Vaccines Inc. | USA |
| S protein integrated in HIV VLPs | IrsiCaixa AIDS Research/IRTA-CReSA/Barcelona Supercomputing Centre/Grifols | Spain |
| VLP + Adjuvant | Mahidol University/ The Government Pharmaceutical Organization (GPO)/Siriraj Hospital | Thailand |
| Virus-like particles, lentivirus and baculovirus vehicles | Navarrabiomed, Oncoimmunology group | Spain |
| Virus-like particle, based on RBD displayed on virus-like particles | Saiba GmbH | Switzerland |
| ADDomer™ multiepitope display | Imophoron Ltd and Bristol University's Max Planck Centre | UK |
| VLP | OSIVAX | France |
| eVLP (enveloped VLP) | ARTES Biotechnology | Germany |
| VLPs-based COVID-19 vaccine in preclinical phase | ||
| Vaccine | Developer | Country |
| VLPs peptides/whole virus | University of Sao Paulo | Brazil |
| VLPs produced in baculovirus expression vector system or BEVS | Tampere University | Finland |
| Plant derived VLP | Shiraz University | Iran |
| Myxoma virus co-expressing S, M, N and E proteins | Arizona State University | USA |
| Plasmid driven production of VLPs containing S, M, N and E proteins of SARS-CoV-2 | Arizona State University | USA |
| Virus Like Particle with RCB | Berna Biotech Pharma | Switzerland |
| RBD-HBsAg VLPs or Receptor Binding Domain SARS-CoV-2 Hepatitis B surface antigen VLP Vaccine | SpyBiotech/Serum Institute of India | India |
| MVA encoded VLP | GeoVax/BravoVax | China |
| Drosophila S2 insect cell expression system VLPs | ExpreS2ion | Denmark |
| VLP-recombinant protein with adjuvant | Osaka University/ BIKEN/ National Institutes of Biomedical Innovation | Japan |
| Lipid nanostructures (LNP)-encapsulated mRNA cocktail encoding VLP | Fudan University/Shanghai JiaoTong University/RNACure Biopharma | China |
Medicago Inc, a Canadian company, has utilized plant-derived VLPs with vaccine adjuvants from GSK and Dynavax to develop a COVID-19 vaccine [116]. The CoVLP technology utilizes Nicotiana benthamiana plant as a bioreactor for the vaccine production by using Agrobacterium tumefaciens as disarmed vector that transfer episomal DNA containing SARS CoV-2 spike protein gene to the nucleus of the plant cells [133]. Similarly, ARTES Biotechnology is using two VLP-based technologies—enveloped VLP technology called METAVAX and capsid VLP technology called SplitCore—for the development of COVID-19 vaccines [134]. VBI Vaccines Inc. is also making COVID-19 vaccine named VBI-2902a using enveloped VLPs as platform, results of which recently have been published by Fluckiger and collaborators [135]. The researcher showed preliminary efficacy of the vaccine against SARS-CoV-2 in Syrian golden hamsters by suppressing clinical disease and lung inflammation [135].
Lipid nanostructures (LNPs) are another nanotechnology-based platform that is being used to develop vaccines against SARS-Co-2. Most of the mRNA-based COVID-19 vaccines are using lipid nanostructures to encapsulate mRNA for delivery into cells. Lipid nanostructures protect mRNA against enzymatic degradation, help mRNA in escaping from endosomes and allow release of the enclosed mRNA into the cytosol, and improve the cellular uptake and thus expression of mRNA by many-fold compared to naked mRNA inside the host cells [137]–[139]. Among the seven approved vaccine for COVID-19 by the World Health Organization [117], two are mRNA based and use lipid nanostructures as a nanocarrier for the delivery: Comirnaty (BNT162b2) by Pfizer, BioNTech and Fosun Pharma; and Moderna COVID-19 Vaccine (mRNA-1273) by Moderna, Biomedical Advanced Research and Development Authority (BARDA), and National Institute of Allergic and Infectious Diseases (NIAID). Along with these two, many other mRNA-based vaccines being developed against SARS-CoV-2 are using LNPs: ARCoV, CVnCoV, DS-5670a, MRT5500, PTX-COVID19-B, and ChulaCov19 (Table 4).
Table 4. mRNA-based vaccines using Lipid nanoparticles (LNPs) for the delivery of cargo.
| Vaccine | Developer | Trial phase |
| ARCoV | Walvax Biotechnology Co., Ltd.; Abogen Biosciences Co. Ltd.; Yuxi Walvax Biotechnology Co., Ltd. | Phase 3 |
| CVnCoV | CureVac; GSK | Phase 2b/3 |
| DS-5670a | Daiichi Sankyo Co., Ltd. | Phase 1/2 |
| MRT5500 | Sanofi, Translate Bio | Phase 1/2 |
| LUNAR-COV19 (ARCT-021) | Arcturus/Duke-NUS/Catalent | Phase 1/2 |
| LNP-nCoVsaRNA | Imperial College | Phase 1/2 |
| (Not named yet) | Shanghai Municipal Science and Technology Commission; Stemirna Therapeutics | Phase 1 |
| (Not named yet) | Gritstone Oncology, Inc.; National Institute of Allergic and Infectious diseases (NIAID) | Phase 1 |
| PTX-COVID19-B | Providence Therapeutics; Canadian government | Phase 1 |
| ChulaCov19 | Chulalongkorn University | Phase 1 |
| D614G variant LNP Encapsulated RNA (Bancovid, Banagavax) | Globe Biotech Ltd | Pre-clinical |
| LNP-encapsulated mRNA encoding S | Max-Planck-Institute of Colloids and Interfaces | Pre-clinical |
| Comirnaty (BNT162b2) | Pfizer, BioNTech; Fosun Pharma | Authorized or approved |
| Moderna COVID-19 Vaccine (mRNA-1273) | Moderna, Biomedical Advanced Research and Development Authority (BARDA), National Institute of Allergic and Infectious diseases (NIAID) | Authorized or approved |
Source: World Health Organization [116].
Pfizer, in collaboration with BioNTech, has developed the dual-dose vaccine Comirnaty®BNT162b2 against SARS-CoV-2 [140]. In Comirnaty®, nucleoside-modified mRNA—that encodes receptor binding domain (RBD) of the SARS-CoV-2 spike protein—has been encapsulated inside lipid nanostructures. In phase I/II trials in the USA and in Germany, the vaccine was found to induce robust immunogenic responses [140]. The UK was the first and Canada was second country to approve emergency use of Comirnaty against SARS-CoV-2. To see the efficacy of the vaccine among different population groups such as pregnant women over the age of 18, children under 12 years old, and adolescents between the age 12 and 15, the clinical trials have been started in different countries [140]. With an efficacy of 95%, Comirnaty® has been approved in 85 countries as of 16 May 2021 [141].
Similarly, Moderna has developed mRNA-1273 vaccine based on lipid nanostructures against SARS-CoV-2. The mRNA-1272 vaccine is also two-dosed like as that of Comirnaty® of Pfizer. The vaccine exploits lipid nanostructures to encapsulate nucleoside-modified mRNA that encodes SARS-CoV-2 spike glycoprotein stabilized in its prefusion conformation [142]. In the preliminary studies done in mice [142] and primates [143], the vaccine has been found to protect against SARS-CoV-2 infection. In The Coronavirus Efficacy (COVE) phase 3 randomized, observer-blinded, placebo-controlled, multicenter trial among 30,420 volunteers in the USA, the mRNA-1273 was found to be safe and efficacious for preventing SARS-CoV-2 infection [144]. The Moderna mRNA-1273 vaccine has an efficacy of 94.1% and has been approved for use in 46 countries as of 16 May 2021 [141].
The other example of COVID-19 vaccine that is using nanostructures platform is NVX-CoV2373 developed by Novavax. It is a recombinant nanostructure vaccine that displays trimeric full-length SARS-CoV-2 spike glycoproteins [145]. Novavax is using its own saponin-based Matrix-MTM adjuvant technology in the clinical trial for the NVX-CoV2373 vaccine [145]. In the phase 3 randomized, observer-blinded, placebo-controlled, multicenter trial in the UK, the two-dosed regimen of NVX-CoV2373 gave an efficacy of 89.7% against SARS-CoV-2 infection and also found to be highly effective against the B.1.1.7 variant [146]. In a recently published research articles, the combination of NVX-CoV2373 and recombinant hemagglutinin (HA) quadrivalent nanostructure influenza vaccine (qNIV) protected hamsters challenged with SARS-CoV-2 [147]. The combination vaccine can also protect against seasons influenza. He et al. [148] have reported a next generation vaccine strategy against SARS-CoV-2 using self-assembling protein nanostructures (SApNPs) technology. The researchers displayed receptor binding domain (RBD) and SARS-CoV-2 spike as vaccine antigens on SApNPs. The nanoparticle system elicited a potent immune response by T-cells in mouse model [148].
In a proof-of-concept study, Zeng's group [149] engineered endogenous untranslated regions (UTRs) of mRNAs termed as NASAR to enhance SARS-CoV-2 antigen production. The engineered mRNA when delivered using lipid-derived TT3 nanostructures induced improved antibody response in mice in comparison with formulation based on FDA-approved lipid nanostructure delivery system. The researchers argued for the further development of NASAR system into alternative COVID-19 vaccines.
Various research groups have utilized nanostructures such as liposomes, reconstituted lipoproteins, and cell-membrane-derived nanostructures that mimick cell membrane to counter SARS-Cov-2 infection. These are called nanodecoy or decoy nanostructures. Rao et al. [150] have engineered decoy nanostructures to counter SARS-CoV-2. The researchers constructed nanodecoys by fusing two types of cell membrane nanovesicles: (1) one derived from human embryonic kidney 293T cells that were genetically engineered to express SARS-CoV-2 receptor ACE2, and (2) another derived from human myeloid mononuclear THP-1 cells. The nanodecoys inhibited the replication and infection of SARS-CoV-2, and also suppressed immune disorder and lung injury in an acute pneumonia mouse model by neutralizing inflammatory cytokines, thus showing potential of nanotechnology against COVID-19 [150].
Li et al. [151] presented the anti-SARS-CoV-2 application of nanodecoys derived from human lung spheroid cells (LSCs). The study was done on SARS-CoV-2-infected cynomolgus macaque model, which when received nanodecoys via inhalation using a nebulizer showed a reduction of viral load and decrease in pulmonary fibrosis. Similarly, Zhang and coworkers [152] prepared two kinds of nanosponges (a type of lipid nanostructures) from cell membranes of either human lung epithelial type II cells or human macrophages. Because these nanosponges had on their surfaces protein receptors used by SARS-CoV-2 for cell entry, they could capture and neutralize SARS-CoV-2 and prevent the virus from infecting other host cells.
Recombinant S1 subunit protein from SARS-CoV-2 was encapsulated in cationic liposomes by Liu et al. [153] to prepare a nanovaccine. The vaccine elicited robust humoral responses in mice, and the serum from the vaccinated mice significantly inhibited SARS-CoV-2 infection in Vero cells. This lipid-based formulation technique presents an interesting approach that can be translated to clinical settings to tackle COVID-19.
Recently, nanobodies, which are highly stable small functional fragment of antibodies, are being used as therapeutic agents against many diseases. Canonical antibodies are comprise of two identical heavy and two identical light chains, both connected via interchain disulphide bonds and non-covalent interactions [154]. In comparison, nanobodies lack light chain and also the first constant domain (CH1) of the heavy chain, due to which nanobodies can attain compact structure and low dimensional size (4 × 2.5 × 3 nm) and low molecular weight (~15 kDa) than that of conventional antibodies [155],[156]. Nanobodies are naturally found in the camelid family (alpacas, camels, dromedaries, guanacos, and llamas) [157]. Nanobodies are highly stable and can easily be produced in large quantities in bacterial, yeast, or mammalian expression system [158]. Due to these reasons nanobodies are being utilized as therapeutic agents against SARS-CoV-2 infection (Table 5). Many studies in in vitro and in vivo conditions have showed strong neutralizing capability of nanobodies against SARS-CoV-2 even at nano molar and pico molar range of concentrations (Table 5). Nanobodies itself and their derived forms such as nanobody-coated nanostructures and nanobody-derived nanoprobes have successfully been utilized in imaging, target drug delivery and therapy, and diagnosis of diseases [159]. Therefore, nanobodies must be further explored for similar applications against SARS-CoV-2 to counter COVID-19 pandemic.
Table 5. Nanobodies against SARS-CoV-2.
| Study | Findings | Effective inhibitory concentration |
| Xu et al. [160] | anti-RBD nanobodies isolated from llamas and from engineered mice neutralized SARS-CoV-2 variants | In picomolar range |
| Güttler et al. [161] | The nanobodies bound the open and closed states of the Spike protein and interacted tightly with RBD domain. The nanobodies were found to be highly thermo stable at 95 °C | 17–50 pM |
| Sziemel et al. [162] | Recombinant alpaca antibodies neutralized live virus of B.1.351 variant of concern of SARS-CoV-2 | IC50< 3nM |
| Custódio et al. [163] | Nanobodies, Sb23, isolated from a synthetic library, sybodies (Sb), targeted the receptor-binding domain (RBD) of the SARS-CoV-2 spike protein and able to neutralized pseudoviruse | IC50 of 0.6µg/mL |
| Ye et al. [164] | The nanobody Nanosota-1 can bound to the receptor-binding domain (RBD) of SARS-CoV-2 spike protein thus blocking out ACE2 binding to the RBD. Single dose of Nanosota-1 showed therapeutic efficacy in a hamster model of SARS-CoV-2 infection. | Neutralization dose 50% (ND50) of 0.16 µg/mL |
| Pymm et al. [158] | Nanobody cocktails administered prophylactically reduced viral loads and infection in mice challenged with the N501Y D614G SARS-CoV-2 virus variant | half-maximal inhibitory concentration (IC50) = 0.1 nM |
| Hanke et al. [165] | The alpaca derived nanobody, Ty1, prevented binding of SARS-CoV-2 RBD to its host cell receptor ACE2. The Ty1 nanobody can easily be expressed in bacteria with very high yield (>30 mg/L culture) | IC50 of 0.77 µg/mL (54nM) |
| Nambulli et al. [166] | Pittsburgh inhalable Nanobody 21 (PiN-21), which can be delivered intranasally, prevented and treated SARS-CoV-2 infection in Syrian hamsters | 0.2 mg/kg |
| Esparza et al. [167] | NIH-CoVnb-112 nanobody blocked SARS-CoV-2 spike pseudotyped lentivirus infection of HEK293 cells expressing human ACE2 | EC50 of 0.3µg/mL |
| Xiang et al. [168] | The nanobodies showed very high affinity (~10 pM) with RBD of spike protein and able to neutralize pseudotyped SARS-CoV-2 | half-maximal inhibitory concentration as low as 0.058 ng/mL) |
| Koenig et al. [169] | Nanobodies able to neutralize SARS-CoV-2 and SARS-CoV-2–pseudotyped vesicular stomatitis virus | IC50 value of 60 nM |
| Lu et al. [170] | Nanobodies Nb91-hFc and Nb3-hFc against spike protein and its RBD domain neutralized spike pseudotyped viruses in vitro | IC50 of 1.54 nM |
5. Conclusions
The COVID-19 pandemic has created unprecedented challenges for humanity. Nanomaterials present interesting candidates that can be incorporated into therapy and diagnostics for SARS-CoV-2. Nanomaterials, such as metal nanostructures, graphene and graphene derivatives, nanocomposites, and lipid-derived nanomaterials have spawned novel detection methods for COVID-19. Similarly, to prevent spread of SARS-CoV-2 in public places and healthcare settings various new products (face masks and other personal protective clothings, surface coatings, etc.) based on nanotechnology have emerged. However, the claim of such products in controlling the spread of SARS-CoV-2 must be properly verified by the appropriate agencies of the respective countries to strengthen the fight against COVID-19. Similarly, if any such product is using metal nanostructures, then the toxicity analysis of metal nanostructures on human health must be properly assessed. All over the world, many research groups are also utilizing nanotechnology for designing vaccines and therapeutic agents against SARS-CoV-2. But these efforts have to keep pace with deadlier SARS-CoV-2 variants that are continuously emerging from different parts of the world. Further, the findings of research studies that used nanotechnology-based approaches against SARS-CoV-2 in lab settings need to be translated to clinical settings in humans. This present an attractive opportunity for the scientist working in the field of nanotechnology to use their expertise for fighting the COVID-19 pandemic by tooth and nail.
Acknowledgments
The authors acknowledge Almanac Life Science India Pvt. Ltd. for valuable inputs in the manuscript.
Footnotes
Conflict of interest: Author declares no conflict of interest.
References
- 1.Yang P, Wang X. COVID-19: a new challenge for human beings. Cell Mol Immunol. 2020;17:555–557. doi: 10.1038/s41423-020-0407-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finkel Y, Mizrahi O, Nachshon A, et al. The coding capacity of SARS-CoV-2. Nature. 2020;589:125–130. doi: 10.1038/s41586-020-2739-1. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Numbers at a glance. Retrieved July 26, 2021. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 4.Hussain A, Kaler J, Tabrez E, et al. Novel COVID-19: A comprehensive review of transmission, manifestation, and pathogenesis. Cureus. 2020;12:e8184. doi: 10.7759/cureus.8184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sultan A, Ali R, Sultan T, et al. Circadian clock modulating small molecules repurposing as inhibitors of SARS-CoV-2 Mpro for pharmacological interventions in COVID-19 pandemic. Chronobiol Int. 2021;38:971–985. doi: 10.1080/07420528.2021.1903027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang Y, Geng X, Tan Y, et al. New understanding of the damage of SARS-CoV-2 infection outside the respiratory system. Biomed Pharmacother. 2020;127:110195. doi: 10.1016/j.biopha.2020.110195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abdool Karim SS, Oliveira T. New SARS-CoV-2 variants—clinical public health, and vaccine implications. N Engl J Med. 2021;384:1866–1868. doi: 10.1056/NEJMc2100362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flaxman S, Mishra S, Gandy A, et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584:257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 9.Hsiang S, Allen D, Annan-Phan S, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature. 2020;584:262–267. doi: 10.1038/s41586-020-2404-8. [DOI] [PubMed] [Google Scholar]
- 10.Horton R. Offline: the second wave. Lancet. 2020;395:1960. doi: 10.1016/S0140-6736(20)31451-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flühmann B, Ntai I, Borchard G, et al. Nanomedicines: The magic bullets reaching their target? Eur J Pharm Sci. 2019;128:73–80. doi: 10.1016/j.ejps.2018.11.019. [DOI] [PubMed] [Google Scholar]
- 12.Hawthorne GH, Bernuci MP, Bortolanza M, et al. Clinical developments in antimicrobial nanomedicine: toward novel solutions. In: Ficai A, Grumezescu AM, editors. Nanostructures for antimicrobial therapy. Elsevier; 2017. pp. 653–668. [Google Scholar]
- 13.Szunerits S, Barras A, Khanal M, et al. Nanostructures for the inhibition of viral infections. Mol Basel Switz. 2015;20:14051–14081. doi: 10.3390/molecules200814051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sathish Sundar D, Gover Antoniraj M, Senthil Kumar C, et al. Recent trends of biocompatible and biodegradable nanoparticles in drug delivery: A review. Curr Med Chem. 2016;23:3730–3751. doi: 10.2174/0929867323666160607103854. [DOI] [PubMed] [Google Scholar]
- 15.Guntur SR, Kumar NS, Hegde MM, et al. In vitro studies of the antimicrobial and free-radical scavenging potentials of silver nanoparticles biosynthesized from the extract of Desmostachya bipinnata. Anal Chem Insights. 2018;13:1177390118782877. doi: 10.1177/1177390118782877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nasrollahzadeh M, Sajjadi M, Soufi GJ, et al. Nanomaterials and nanotechnology-associated innovations against viral infections with a focus on coronaviruses. Nanomater Basel Switz. 2020;10:1072. doi: 10.3390/nano10061072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh L, Kruger HG, Maguire GEM, et al. The role of nanotechnology in the treatment of viral infections. Ther Adv Infect Dis. 2017;4:105–131. doi: 10.1177/2049936117713593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang D. Application of nanotechnology in the COVID-19 pandemic. Int J Nanomedicine. 2021;16:623–649. doi: 10.2147/IJN.S296383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh L, Kruger HG, Maguire GE, et al. The role of nanotechnology in the treatment of viral infections. Ther Adv Infect Dis. 2017;4:105–131. doi: 10.1177/2049936117713593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bonam SR, Kotla NG, Bohara RA, et al. Potential immuno-nanomedicine strategies to fight COVID-19 like pulmonary infections. Nano Today. 2021;36:101051. doi: 10.1016/j.nantod.2020.101051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barar J. COVID-19 clinical implications: the significance of nanomedicine. Bioimpacts. 2020;10:137–138. doi: 10.34172/bi.2020.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sivaraman D, Pradeep PS, Manoharan SS, et al. Current Strategies and Approaches in Combating SARS-CoV-2 Virus that Causes COVID-19. Lett Drug Des Discov. 2020;17:672–674. [Google Scholar]
- 23.Sportelli MC, Izzi M, Kukushkina EA, et al. Can Nanotechnology and Materials Science Help the Fight against SARS-CoV-2? Nanomaterials. 2020;10:802. doi: 10.3390/nano10040802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang L, Rong Y, Pan Q, et al. SARS-CoV-2 vaccine research and development: Conventional vaccines and biomimetic nanotechnology strategies. Asian J Pharm Sci. 2021;16:136–146. doi: 10.1016/j.ajps.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yang D. Application of Nanotechnology in the COVID-19 Pandemic. Int J Nanomedicine. 2021;16:623–649. doi: 10.2147/IJN.S296383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheema R, Blumberg DA. Understanding laboratory testing for SARS-CoV-2. Children. 2021;8:355. doi: 10.3390/children8050355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization. COVID-19 target product profiles for priority diagnostics to support response to the COVID-19 pandemic v.0.1. 2020. Retrieved July 31, 2020, Available from: https://www.who.int/docs/default-source/blue-print/rd-blueprint-diagnostics-tpp-final-v31july2020.pdf?sfvrsn=2db5b31b_1&download=true.
- 28.Adhikari S, Adhikari U, Mishra A, et al. Nanomaterials for diagnostic, treatment and prevention of COVID-19. Appl Sci Technol Ann. 2020;1:155–164. [Google Scholar]
- 29.Balkourani G, Brouzgou A, Archonti M, et al. Emerging materials for the electrochemical detection of COVID-19. J Electroanal Chem. 2021;893:115289. doi: 10.1016/j.jelechem.2021.115289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Misra R, Acharya S, Sushmitha N. Nanobiosensor-based diagnostic tools in viral infections: Special emphasis on Covid-19. Rev Med Virol. 2021:e2267. doi: 10.1002/rmv.2267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shetti NP, Mishra A, Bukkitgar SD, et al. Conventional and nanotechnology-based sensing methods for SARS coronavirus (2019-nCoV) ACS Appl Bio Mater. 2021;4:1178–1190. doi: 10.1021/acsabm.0c01545. [DOI] [PubMed] [Google Scholar]
- 32.Suleman S, Shukla SK, Malhotra N, et al. Point of care detection of COVID-19: Advancement in biosensing and diagnostic methods. Chem Eng J. 2021;414:128759. doi: 10.1016/j.cej.2021.128759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Choi Y, Hwang JH, Lee SY. Recent trends in nanomaterials-based colorimetric detection of pathogenic bacteria and viruses. Small Methods. 2018;2:1700351. doi: 10.1002/smtd.201700351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen J, Andler SM, Goddard JM, et al. Integrating recognition elements with nanomaterials for bacteria sensing. Chem Soc Rev. 2017;46:1272–1283. doi: 10.1039/c6cs00313c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Saha K, Agasti SS, Kim C, et al. Gold nanoparticles in chemical and biological sensing. Chem Rev. 2012;112:2739–2779. doi: 10.1021/cr2001178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karami A, Hasani M, Azizi Jalilian F, et al. Hairpin-spherical nucleic acids for diagnosing COVID-19: A simple method to generalize the conventional PCR for molecular assays. Anal Chem. 2021;93:9250–9257. doi: 10.1021/acs.analchem.1c01515. [DOI] [PubMed] [Google Scholar]
- 37.Sil BK, Jamiruddin MR, Haq MA, et al. AuNP coupled rapid flow-through dot-blot immuno-assay for enhanced detection of SARS-CoV-2 specific nucleocapsid and receptor binding domain IgG. Int J Nanomedicine. 2021;16:4739–4753. doi: 10.2147/IJN.S313140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ventura BD, Cennamo M, Minopoli A, et al. Colorimetric test for fast detection of SARS-CoV-2 in nasal and throat swabs. ACS Sens. 2020;5:3043–3048. doi: 10.1021/acssensors.0c01742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moitra P, Alafeef M, Dighe K, et al. Selective naked-eye detection of SARS-CoV-2 mediated by N gene targeted antisense oligonucleotide capped plasmonic nanoparticles. ACS Nano. 2020;14:7617–7627. doi: 10.1021/acsnano.0c03822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mejía-Salazar JR, Oliveira ON. Plasmonic biosensing: Focus review. Chem Rev. 2018;118:10617–10625. doi: 10.1021/acs.chemrev.8b00359. [DOI] [PubMed] [Google Scholar]
- 41.Jadhav SA, Biji P, Panthalingal MK, et al. Development of integrated microfluidic platform coupled with Surface-enhanced Raman Spectroscopy for diagnosis of COVID-19. Med Hypotheses. 2021;146:110356. doi: 10.1016/j.mehy.2020.110356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shrivastav AM, Cvelbar U, Abdulhalim I. A comprehensive review on plasmonic-based biosensors used in viral diagnostics. Commun Biol. 2021;4:70. doi: 10.1038/s42003-020-01615-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu H, Dai E, Xiao R, et al. Development of a SERS-based lateral flow immunoassay for rapid and ultra-sensitive detection of anti-SARS-CoV-2 IgM/IgG in clinical samples. Sens Actuators B Chem. 2021;329:129196. doi: 10.1016/j.snb.2020.129196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Qiu G, Gai Z, Tao Y, et al. Dual-functional plasmonic photothermal biosensors for highly accurate severe acute respiratory syndrome coronavirus 2 detection. ACS Nano. 2020;14:5268–5277. doi: 10.1021/acsnano.0c02439. [DOI] [PubMed] [Google Scholar]
- 45.Zhu X, Wang X, Han L, et al. Multiplex reverse transcription loop-mediated isothermal amplification combined with nanoparticles-based lateral flow biosensor for the diagnosis of COVID-19. Biosens Bioelectron. 2020;166:112437. doi: 10.1016/j.bios.2020.112437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang Z, Zheng Z, Hu H, et al. A point-of-care selenium nanoparticles-based test for the combined detection of anti-SARS-CoV-2 IgM and IgG in human serum and blood. Lab Chip. 2020;20:4255–4261. doi: 10.1039/d0lc00828a. [DOI] [PubMed] [Google Scholar]
- 47.Vadlamani BS, Uppal T, Verma SC, et al. Functionalized TiO2 nanotube-based electrochemical biosensor for rapid detection of SARS-CoV-2. Sensors. 2020;20:5871. doi: 10.3390/s20205871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jeong S, González-Grandío E, Navarro N, et al. Extraction of viral nucleic acids with carbon nanotubes increases SARS-CoV-2 quantitative reverse transcription polymerase chain reaction detection sensitivity. ACS Nano. 2021;15:10309–10317. doi: 10.1021/acsnano.1c02494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Seo G, Lee G, Kim MJ, et al. Rapid detection of COVID-19 causative virus (SARS-CoV-2) in human nasopharyngeal swab specimens using field-effect transistor-based biosensor. ACS Nano. 2020;14:5135–5142. doi: 10.1021/acsnano.0c02823. [DOI] [PubMed] [Google Scholar]
- 50.Li J, Wu D, Yu Y, et al. Rapid and unamplified identification of COVID-19 with morpholino-modified graphene field-effect transistor nanosensor. Biosens Bioelectron. 2021;183:113206. doi: 10.1016/j.bios.2021.113206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ali MA, Hu C, Jahan S, et al. Sensing of COVID-19 antibodies in seconds via aerosol jet nanoprinted reduced-graphene-oxide-coated 3D electrodes. Adv Mater Deerfield Beach Fla. 2021;33:2006647. doi: 10.1002/adma.202006647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhu Z. An overview of carbon nanotubes and graphene for biosensing applications. Nano-Micro Lett. 2017;9:1–24. doi: 10.1007/s40820-017-0128-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vermisoglou E, Panáček D, Jayaramulu K, et al. Human virus detection with graphene-based materials. Biosens Bioelectron. 2020;166:112436. doi: 10.1016/j.bios.2020.112436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yang L, Xie X, Cai L, et al. p-sulfonated calix [8] arene functionalized graphene as a “turn on” fluorescent sensing platform for aconitine determination. Biosens Bioelectron. 2016;82:146–154. doi: 10.1016/j.bios.2016.04.005. [DOI] [PubMed] [Google Scholar]
- 55.Huang C, Wen T, Shi FJ, et al. Rapid detection of IgM antibodies against the SARS-CoV-2 virus via colloidal gold nanoparticle-based lateral-flow assay. ACS Omega. 2020;5:12550–12556. doi: 10.1021/acsomega.0c01554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mertens P, De Vos N, Martiny D, et al. Development and potential usefulness of the COVID-19 Ag Respi-Strip diagnostic assay in a pandemic context. Front Med. 2020;7:225. doi: 10.3389/fmed.2020.00225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wen T, Huang C, Shi FJ, et al. Development of a lateral flow immunoassay strip for rapid detection of IgG antibody against SARS-CoV-2 virus. Analyst. 2020;145:5345–5352. doi: 10.1039/d0an00629g. [DOI] [PubMed] [Google Scholar]
- 58.Shan B, Broza YY, Li W, et al. Multiplexed nanomaterial-based sensor array for detection of COVID-19 in exhaled breath. ACS Nano. 2020;14:12125–12132. doi: 10.1021/acsnano.0c05657. [DOI] [PubMed] [Google Scholar]
- 59.Lamote K, Janssens E, Schillebeeckx E, et al. The scent of COVID-19: viral (semi-)volatiles as fast diagnostic biomarkers? J Breath Res. 2020;14:042001. doi: 10.1088/1752-7163/aba105. [DOI] [PubMed] [Google Scholar]
- 60.Fabiani L, Saroglia M, Galatà G, et al. Magnetic beads combined with carbon black-based screen-printed electrodes for COVID-19: A reliable and miniaturized electrochemical immunosensor for SARS-CoV-2 detection in saliva. Biosens Bioelectron. 2020;171:112686. doi: 10.1016/j.bios.2020.112686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Arduini F, Cinti S, Mazzaracchio V, et al. Carbon black as an outstanding and affordable nanomaterial for electrochemical (bio)sensor design. Biosens Bioelectron. 2020;156:112033. doi: 10.1016/j.bios.2020.112033. [DOI] [PubMed] [Google Scholar]
- 62.Vaquer A, Alba-Patiño A, Adrover-Jaume C, et al. Nanoparticle transfer biosensors for the non-invasive detection of SARS-CoV-2 antigens trapped in surgical face masks. Sens Actuators B Chem. 2021;345:130347. doi: 10.1016/j.snb.2021.130347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Baker AN, Richards SJ, Guy CS, et al. The SARS-CoV-2 spike protein binds sialic acids and enables rapid detection in a lateral flow point of care diagnostic device. ACS Cent Sci. 2020;6:2046–2052. doi: 10.1021/acscentsci.0c00855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yang Y, Peng Y, Lin C, et al. Human ACE2-functionalized gold ‘virus-trap’ nanostructures for accurate capture of SARS-CoV-2 and single-virus SERS detection. Nano-Micro Lett. 2021;13:109. doi: 10.1007/s40820-021-00620-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang Y, Chen M, Liu C, et al. Sensitive and rapid on-site detection of SARS-CoV-2 using a gold nanoparticle-based high-throughput platform coupled with CRISPR/Cas12-assisted RT-LAMP. Sens Actuators B Chem. 2021;345:130411. doi: 10.1016/j.snb.2021.130411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cao Y, Wu J, Pang B, et al. CRISPR/Cas12a-mediated gold nanoparticle aggregation for colorimetric detection of SARS-CoV-2. Chem Commun Camb Engl. 2021;57:6871–6874. doi: 10.1039/d1cc02546e. [DOI] [PubMed] [Google Scholar]
- 67.Jiang Y, Hu M, Liu AA, et al. Detection of SARS-CoV-2 by CRISPR/Cas12a-enhanced colorimetry. ACS Sens. 2021;6:1086–1093. doi: 10.1021/acssensors.0c02365. [DOI] [PubMed] [Google Scholar]
- 68.Song F, Shen Y, Wei Y, et al. Botulinum toxin as an ultrasensitive reporter for bacterial and SARS-CoV-2 nucleic acid diagnostics. Biosens Bioelectron. 2021;176:112953. doi: 10.1016/j.bios.2020.112953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lew T, Aung K, Ow SY, et al. Epitope-functionalized gold nanoparticles for rapid and selective detection of SARS-CoV-2 IgG antibodies. ACS Nano. 2021 doi: 10.1021/acsnano.1c04091. Online ahead of print. [DOI] [PubMed] [Google Scholar]
- 70.Alafeef M, Moitra P, Dighe K, et al. RNA-extraction-free nano-amplified colorimetric test for point-of-care clinical diagnosis of COVID-19. Nat Protoc. 2021;16:3141–3162. doi: 10.1038/s41596-021-00546-w. [DOI] [PubMed] [Google Scholar]
- 71.Pramanik A, Gao Y, Patibandla S, et al. Aptamer conjugated gold nanostar-based distance-dependent nanoparticle surface energy transfer spectroscopy for ultrasensitive detection and inactivation of corona virus. J Phys Chem Lett. 2021;12:2166–2171. doi: 10.1021/acs.jpclett.0c03570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yao Z, Zhang Q, Zhu W, et al. Rapid detection of SARS-CoV-2 viral nucleic acids based on surface enhanced infrared absorption spectroscopy. Nanoscale. 2021;13:10133–10142. doi: 10.1039/d1nr01652k. [DOI] [PubMed] [Google Scholar]
- 73.Karami A, Hasani M, Azizi Jalilian F, et al. Conventional PCR assisted single-component assembly of spherical nucleic acids for simple colorimetric detection of SARS-CoV-2. Sens Actuators B Chem. 2021;328:128971. doi: 10.1016/j.snb.2020.128971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.de Lima LF, Ferreira AL, Torres MD, et al. Minute-scale detection of SARS-CoV-2 using a low-cost biosensor composed of pencil graphite electrodes. Proc Natl Acad Sci. 2021;118:e2106724118. doi: 10.1073/pnas.2106724118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zhang M, Li X, Pan J, et al. Ultrasensitive detection of SARS-CoV-2 spike protein in untreated saliva using SERS-based biosensor. Biosens Bioelectron. 2021;190:113421. doi: 10.1016/j.bios.2021.113421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sibai M, Solis D, Röltgen K, et al. Evaluation of SARS-CoV-2 total antibody detection via a lateral flow nanoparticles fluorescence immunoassay. J Clin Virol Off Publ Pan Am Soc Clin Virol. 2021;139:104818. doi: 10.1016/j.jcv.2021.104818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Fu Z, Zeng W, Cai S, et al. Porous Au@Pt nanoparticles with superior peroxidase-like activity for colorimetric detection of spike protein of SARS-CoV-2. J Colloid Interface Sci. 2021;604:113–121. doi: 10.1016/j.jcis.2021.06.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bayin Q, Huang L, Ren C, et al. Anti-SARS-CoV-2 IgG and IgM detection with a GMR based LFIA system. Talanta. 2021;227:122207. doi: 10.1016/j.talanta.2021.122207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chen Z, Zhang Z, Zhai X, et al. Rapid and sensitive detection of anti-SARS-CoV-2 IgG, using lanthanide-doped nanoparticles-based lateral flow immunoassay. Anal Chem. 2020;92:7226–7231. doi: 10.1021/acs.analchem.0c00784. [DOI] [PubMed] [Google Scholar]
- 80.Wang D, He S, Wang X, et al. Rapid lateral flow immunoassay for the fluorescence detection of SARS-CoV-2 RNA. Nat Biomed Eng. 2020;4:1150–1158. doi: 10.1038/s41551-020-00655-z. [DOI] [PubMed] [Google Scholar]
- 81.Stieber F, Howard J, Rao SN, et al. First performance report of QIAreach™ Anti-SARS-CoV-2 Total Test, an innovative nanoparticle fluorescence digital detection platform. J Clin Virol. 2020;133:104681. doi: 10.1016/j.jcv.2020.104681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nguyen N, Kim S, Lindemann G, et al. COVID-19 spike protein induced phononic modification in antibody-coupled graphene for viral detection application. ACS Nano. 2021;15:11743–11752. doi: 10.1021/acsnano.1c02549. [DOI] [PubMed] [Google Scholar]
- 83.Zhang Y, Malekjahani A, Udugama BN, et al. Surveilling and tracking COVID-19 patients using a portable quantum dot smartphone device. Nano Lett. 2021;21:5209–5216. doi: 10.1021/acs.nanolett.1c01280. [DOI] [PubMed] [Google Scholar]
- 84.Zhou Y, Chen Y, Liu W, et al. Development of a rapid and sensitive quantum dot nanobead-based double-antigen sandwich lateral flow immunoassay and its clinical performance for the detection of SARS-CoV-2 total antibodies. Sens Actuators B Chem. 2021;343:130139. doi: 10.1016/j.snb.2021.130139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sundah NR, Natalia A, Liu Y, et al. Catalytic amplification by transition-state molecular switches for direct and sensitive detection of SARS-CoV-2. Sci Adv. 2021;7:5940. doi: 10.1126/sciadv.abe5940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chen R, Ren C, Liu M, et al. Early Detection of SARS-CoV-2 seroconversion in humans with aggregation-induced near-infrared emission nanoparticle-labeled lateral flow immunoassay. ACS Nano. 2021;15:8996–9004. doi: 10.1021/acsnano.1c01932. [DOI] [PubMed] [Google Scholar]
- 87.Bałazy A, Toivola M, Reponen T, et al. Manikin-based performance evaluation of N95 filtering-facepiece respirators challenged with nanoparticles. Ann Occup Hyg. 2006;50:259–269. doi: 10.1093/annhyg/mei058. [DOI] [PubMed] [Google Scholar]
- 88.Chen L, Liang J. An overview of functional nanoparticles as novel emerging antiviral therapeutic agents. Mater Sci Eng C Mater Biol Appl. 2020;112:110924. doi: 10.1016/j.msec.2020.110924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Militky J, Novak O, Kremenakova D, et al. A review of impact of textile research on protective face masks. Material (Basel) 2021;14:1937. doi: 10.3390/ma14081937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Palmieri V, De Maio F, De Spirito M, et al. Face masks and nanotechnology: Keep the blue side up. Nano Today. 2021;37:101077. doi: 10.1016/j.nantod.2021.101077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Talebian S, Wallace GG, Schroeder A, et al. Nanotechnology-based disinfectants and sensors for SARS-CoV-2. Nat Nanotechnol. 2020;15:618–621. doi: 10.1038/s41565-020-0751-0. [DOI] [PubMed] [Google Scholar]
- 92.Kumar S, Karmacharya M, Joshi SR, et al. Photoactive Antiviral Face Mask with Self-Sterilization and Reusability. Nano Lett. 2021;21:337–343. doi: 10.1021/acs.nanolett.0c03725. [DOI] [PubMed] [Google Scholar]
- 93.Nanotechnology Products Database. 2021. Available from: https://product.statnano.com/search?keyword=COVID-19.
- 94.Nanotechnology in Battle Against Coronavirus. Retrieved July 31, 2021, Available from: https://statnano.com/nanotechnology-in-battle-against-coronavirus.
- 95.Borkow G, Zhou SS, Page T, et al. A novel anti-influenza copper oxide containing respiratory face mask. PloS One. 2010;5:e11295. doi: 10.1371/journal.pone.0011295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Korea Advanced Institute of Science and Technology, Recyclable nano-fiber filtered face masks a boon for supply fiasco, 2020. Available from: https://news.kaist.ac.kr/newsen/html/news/?mode=V&mng_no=6530.
- 97.Queensland University of Technology, New mask material can remove virus-size nanoparticles, 2020. Available from: https://www.qut.edu.au/news?id=161468.
- 98.The world's first anti-coronavirus surgical mask by Wakamono, 2020. Available from: https://wakamonobio.com/the-wakamono-mask-the-worlds-first-anti-coronavirus-surgical-mask-2/
- 99.Tremiliosi GC, Simoes LGP, Minozzi DT, et al. Ag nanoparticles-based antimicrobial polycotton fabrics to prevent the transmission and spread of SARS-CoV-2. 2020. Preprint.
- 100.Jeremiah SS, Miyakawa K, Morita T, et al. Potent antiviral effect of silver nanoparticles on SARS-CoV-2. Biochem Biophys Res Commun. 2020;533:195–200. doi: 10.1016/j.bbrc.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Gheblawi M, Wang K, Viveiros A, et al. Angiotensin-converting enzyme 2: SARS-CoV-2 receptor and regulator of the renin-angiotensin system: celebrating the 20th anniversary of the discovery of ACE2. Circ Res. 2020;126:1456–1474. doi: 10.1161/CIRCRESAHA.120.317015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ni W, Yang X, Yang D, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020;24:422. doi: 10.1186/s13054-020-03120-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Imai Y, Kuba K, Rao S, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436:112–116. doi: 10.1038/nature03712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Aydemir D, Ulusu NN. Correspondence: Angiotensin-converting enzyme 2 coated nanoparticles containing respiratory masks, chewing gums and nasal filters may be used for protection against COVID-19 infection. Travel Med Infect Dis. 2020;37:101697. doi: 10.1016/j.tmaid.2020.101697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Raghav PK, Mohanty S. Are graphene and graphene-derived products capable of preventing COVID-19 infection? Med Hypotheses. 2020;144:110031. doi: 10.1016/j.mehy.2020.110031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Chen YN, Hsueh YH, Hsieh CT, et al. Antiviral activity of graphene-silver nanocomposites against non-enveloped and enveloped viruses. Int J Environ Res Public Health. 2016;13:430. doi: 10.3390/ijerph13040430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.De Maio F, Palmieri V, Babini G, et al. Graphene nanoplatelet and graphene oxide functionalization of face mask materials inhibits infectivity of trapped SARS-CoV-2. iScience. 2021;24:102788. doi: 10.1016/j.isci.2021.102788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Unal MA, Bayrakdar F, Nazir H, et al. Graphene oxide nanosheets interact and interfere with SARS-CoV-2 surface proteins and cell receptors to inhibit infectivity. Small. 2021;17:2101483. doi: 10.1002/smll.202101483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Guardian G-Volt masks would use graphene and electrical charge to repel viruses and bacteria. 2020. Available from: https://www.dezeen.com/2020/03/06/guardian-g-volt-face-mask-graphene-coronavirus-bacteria/
- 110.Balagna C, Perero S, Percivalle E, et al. Virucidal effect against coronavirus SARS-CoV-2 of a silver nanocluster/silica composite sputtered coating. Open Ceram. 2020;100006 [Google Scholar]
- 111.Pastorino B, Touret F, Gilles M, et al. Prolonged infectivity of SARS-CoV-2 in fomites. Emerg Infect Dis. 2020;26:2256–2257. doi: 10.3201/eid2609.201788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Blevens MS, Pastrana HF, Mazzotta HC, et al. Cloth Face Masks Containing Silver: Evaluating the Status. J Chem Health Saf. 2021:1c00005. doi: 10.1021/acs.chas.1c00005. [DOI] [PubMed] [Google Scholar]
- 113.Chen X, Chen X, Liu Q, et al. Used disposable face masks are significant sources of microplastics to environment. Environ Pollut. 2021;285:117485. doi: 10.1016/j.envpol.2021.117485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Sullivan GL, Delgado-Gallardo J, Watson TM, et al. An investigation into the leaching of micro and nano particles and chemical pollutants from disposable face masks-linked to the COVID-19 pandemic. Water Res. 2021;196:117033. doi: 10.1016/j.watres.2021.117033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kang J, Zhou L, Duan X, et al. Degradation of Cosmetic microplastics via functionalized carbon nanosprings. Matter. 2019;1:745–758. [Google Scholar]
- 116.World Health Organization. COVID-19 vaccine tracker and landscape. Retrieved on July 31, 2021. Available from: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines.
- 117.World Health Organization. Status of COVID-19 Vaccines within WHO EUL/PQ evaluation process. Retrieved on May 18, 2021. Available from: https://extranet.who.int/pqweb/sites/default/files/documents/Status_COVID_VAX_18May2021.pdf.
- 118.Sanders JM, Monogue ML, Jodlowski TZ, et al. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): A review. JAMA. 2020;323:1824–1836. doi: 10.1001/jama.2020.6019. [DOI] [PubMed] [Google Scholar]
- 119.Pan H, Peto R, Abdool Karim Q, et al. Repurposed antiviral drugs for COVID-19 – interim WHO SOLIDARITY trial results. N Engl J Med. 2020;384:497–511. doi: 10.1056/NEJMoa2023184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tammam SN, Azzazy HM, Lamprecht A. Biodegradable particulate carrier formulation and tuning for targeted drug delivery. J Biomed Nanotechnol. 2015;11:555–577. doi: 10.1166/jbn.2015.2017. [DOI] [PubMed] [Google Scholar]
- 121.Patra JK, Das G, Fraceto LF, et al. Nano based drug delivery systems: recent developments and future prospects. J Nanobiotechnology. 2018;16:71. doi: 10.1186/s12951-018-0392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chakravarty M, Vora A. Nanotechnology-based antiviral therapeutics. Drug Deliv Transl Res. 2020;11:748–787. doi: 10.1007/s13346-020-00818-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Teixeira MC, Carbone C, Souto EB. Beyond liposomes: Recent advances on lipid based nanostructures for poorly soluble/poorly permeable drug delivery. Prog Lipid Res. 2017;68:1–11. doi: 10.1016/j.plipres.2017.07.001. [DOI] [PubMed] [Google Scholar]
- 124.Roldão A, Mellado MC, Castilho LR, et al. Virus-like particles in vaccine development. Expert Rev Vaccines. 2010;9:1149–1176. doi: 10.1586/erv.10.115. [DOI] [PubMed] [Google Scholar]
- 125.Schwarz B, Uchida M, Douglas T. Biomedical and catalytic opportunities of virus-like particles in nanotechnology. Adv Virus Res. 2017;60:1–60. doi: 10.1016/bs.aivir.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Syomin BV, Ilyin YV. Virus-like particles as an instrument of vaccine production. Mol Biol. 2019;53:323–334. doi: 10.1134/S0026893319030154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Bachmann M, Rohrer U, Kundig T, et al. The influence of antigen organization on B cell responsiveness. Science. 1993;262:1448–1451. doi: 10.1126/science.8248784. [DOI] [PubMed] [Google Scholar]
- 128.Zabel F, Kündig TM, Bachmann MF. Virus-induced humoral immunity: on how B cell responses are initiated. Curr Opin Virol. 2013;3:357–362. doi: 10.1016/j.coviro.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 129.Bachmann MF, Jennings GT. Vaccine delivery: a matter of size, geometry, kinetics and molecular patterns. Nat Rev Immunol. 2010;10:787–796. doi: 10.1038/nri2868. [DOI] [PubMed] [Google Scholar]
- 130.Bachmann MF, Dyer MR. Therapeutic vaccination for chronic diseases: a new class of drugs in sight. Nat Rev Drug Discov. 2004;3:81–88. doi: 10.1038/nrd1284. [DOI] [PubMed] [Google Scholar]
- 131.Zepeda-Cervantes J, Ramírez-Jarquín JO, Vaca L. Interaction between virus-like particles (VLPs) and pattern recognition receptors (PRRs) from dendritic cells (DCs): toward better engineering of VLPs. Front Immunol. 2020;11:1100. doi: 10.3389/fimmu.2020.01100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Mohsen MO, Zha L, Cabral-Miranda G, et al. Major findings and recent advances in virus–like particle (VLP)-based vaccines. Semin Immunol. 2017;34:123–132. doi: 10.1016/j.smim.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 133.Ward BJ, Gobeil P, Séguin A, et al. Phase 1 randomized trial of a plant-derived virus-like particle vaccine for COVID-19. Nat Med. 2021;27:1071–1078. doi: 10.1038/s41591-021-01370-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.ARTES Biotechnology. ARTES joins global combat against Corona, 2020. Available from: https://artes-biotechnology.biz/artes-joins-global-combat-against-corona/
- 135.Fluckiger AC, Ontsouka B, Bozic J, et al. An enveloped virus-like particle vaccine expressing a stabilized prefusion form of the SARS-CoV-2 spike protein elicits highly potent immunity. Vaccine. 2021;39:4988–5001. doi: 10.1016/j.vaccine.2021.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Milken Institute FasterCures. COVID-19 treatments and vaccine tracker. 2021. Retrieved July 31, 2021. Available from: https://covid-19tracker.milkeninstitute.org/
- 137.Reichmuth AM, Oberli MA, Jaklenec A, et al. mRNA vaccine delivery using lipid nanoparticles. Ther Deliv. 2016;7:319–334. doi: 10.4155/tde-2016-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Jackson N, Kester KE, Casimiro D, et al. The promise of mRNA vaccines: a biotech and industrial perspective. NPJ Vaccines. 2020;5:11. doi: 10.1038/s41541-020-0159-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Buschmann MD, Carrasco MJ, Alishetty S, et al. Nanomaterial Delivery Systems for mRNA Vaccines. Vaccines. 2021;9:65. doi: 10.3390/vaccines9010065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Khehra N, Padda I, Jaferi U, et al. Tozinameran (BNT162b2) vaccine: The journey from preclinical research to clinical trials and authorization. AAPS PharmSciTech. 2021;22:172. doi: 10.1208/s12249-021-02058-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Francis AI, Ghany S, Gilkes T, et al. Review of COVID-19 vaccine subtypes, efficacy and geographical distributions. Postgrad Med J. 2021;0:1–6. doi: 10.1136/postgradmedj-2021-140654. [DOI] [PubMed] [Google Scholar]
- 142.Corbett KS, Edwards DK, Leist SR, et al. SARS-CoV-2 mRNA vaccine design enabled by prototype pathogen preparedness. Nature. 2020;586:567–571. doi: 10.1038/s41586-020-2622-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Corbett KS, Flynn B, Foulds KE, et al. Evaluation of the mRNA-1273 vaccine against SARS-CoV-2 in nonhuman primates. N Engl J Med. 2020;383:1544–1555. doi: 10.1056/NEJMoa2024671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Baden LR, El Sahly HM, Essink B, et al. Efficacy and Safety of the mRNA-1273 SARS-CoV-2 Vaccine. N Engl J Med. 2021;384:403–416. doi: 10.1056/NEJMoa2035389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Keech C, Albert G, Cho I, et al. Phase 1-2 trial of a SARS-CoV-2 recombinant spike protein nanoparticles vaccine. N Engl J Med. 2020;383:2320–2332. doi: 10.1056/NEJMoa2026920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Heath PT, Galiza EP, Baxter DN, et al. Safety and efficacy of NVX-CoV2373 Covid-19 vaccine. N Engl J Med. 2021;385:1172–1183. doi: 10.1056/NEJMoa2107659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Massare MJ, Patel N, Zhou B, et al. Combination respiratory vaccine containing recombinant SARS-CoV-2 spike and quadrivalent seasonal influenza hemagglutinin nanoparticles with matrix-m adjuvant. 2021. Preprint.
- 148.He L, Lin X, Wang Y, et al. Self-assembling nanoparticles presenting receptor binding domain and stabilized spike as next-generation COVID-19 vaccines. 2020. Preprint. [DOI] [PMC free article] [PubMed]
- 149.Zeng C, Hou X, Yan J, et al. Leveraging mRNA sequences and nanoparticles to deliver SARS-CoV-2 antigens in vivo. Adv Mater. 2020;32:2004452. doi: 10.1002/adma.202004452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Rao L, Xia S, Xu W, et al. Decoy nanoparticles protect against COVID-19 by concurrently adsorbing viruses and inflammatory cytokines. Proc Natl Acad Sci. 2020;117:27141–27147. doi: 10.1073/pnas.2014352117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Li Z, Wang Z, Dinh PUC, et al. Cell-mimicking nanodecoys neutralize SARS-CoV-2 and mitigate lung injury in a non-human primate model of COVID-19. Nat Nanotechnol. 2021;16:942–951. doi: 10.1038/s41565-021-00923-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Zhang Q, Honko A, Zhou J, et al. Cellular nanosponges inhibit SARS-CoV-2 infectivity. Nano Lett. 2020;20:5570–5574. doi: 10.1021/acs.nanolett.0c02278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Liu L, Liu Z, Chen H, et al. A translatable subunit nanovaccine for COVID-19. 2020. Preprint.
- 154.Padlan EA. Anatomy of the antibody molecule. Mol Immunol. 1994;31:169–217. doi: 10.1016/0161-5890(94)90001-9. [DOI] [PubMed] [Google Scholar]
- 155.Huang L, Muyldermans S, Saerens D. Nanobodies®: proficient tools in diagnostics. Expert Rev Mol Diagn. 2010;10:777–785. doi: 10.1586/erm.10.62. [DOI] [PubMed] [Google Scholar]
- 156.Van Audenhove I, Gettemans J. Nanobodies as versatile tools to understand, diagnose, visualize and treat cancer. EBioMedicine. 2016;8:40–48. doi: 10.1016/j.ebiom.2016.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Bannas P, Hambach J, Koch-Nolte F. Nanobodies and nanobody-based human heavy chain antibodies as antitumor therapeutics. Front Immunol. 2017;8:1603. doi: 10.3389/fimmu.2017.01603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Pymm P, Adair A, Chan LJ, et al. Nanobody cocktails potently neutralize SARS-CoV-2 D614G N501Y variant and protect mice. Proc Natl Acad Sci. 2021;118:e2101918118. doi: 10.1073/pnas.2101918118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wang Y, Fan Z, Shao L, et al. Nanobody-derived nanobiotechnology tool kits for diverse biomedical and biotechnology applications. Int J Nanomedicine. 2016;11:3287–3303. doi: 10.2147/IJN.S107194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Xu J, Xu K, Jung S, et al. Nanobodies from camelid mice and llamas neutralize SARS-CoV-2 variants. Nature. 2021;595:278–282. doi: 10.1038/s41586-021-03676-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Güttler T, Aksu M, Dickmanns A, et al. Neutralization of SARS-CoV-2 by highly potent, hyperthermostable, and mutation-tolerant nanobodies. EMBO J. 2021;40:e107985. doi: 10.15252/embj.2021107985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Sziemel AM, Hwa SH, Sigal A, et al. Development of highly potent neutralising nanobodies against multiple SARS-CoV-2 variants including the variant of concern B.1.351. 2021. Preprint.
- 163.Custódio TF, Das H, Sheward DJ, et al. Selection, biophysical and structural analysis of synthetic nanobodies that effectively neutralize SARS-CoV-2. Nat Commun. 2020;11:5588. doi: 10.1038/s41467-020-19204-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Ye G, Gallant JP, Massey C, et al. The development of a novel nanobody therapeutic for SARS-CoV-2. 2020. Preprint.
- 165.Hanke L, Vidakovics Perez L, Sheward DJ, et al. An alpaca nanobody neutralizes SARS-CoV-2 by blocking receptor interaction. Nat Commun. 2020;11:4420. doi: 10.1038/s41467-020-18174-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Nambulli S, Xiang Y, Tilston-Lunel NL, et al. Inhalable Nanobody (PiN-21) prevents and treats SARS-CoV-2 infections in Syrian hamsters at ultra-low doses. Sci Adv. 2021;7:0319. doi: 10.1126/sciadv.abh0319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Esparza TJ, Martin NP, Anderson GP, et al. High affinity nanobodies block SARS-CoV-2 spike receptor binding domain interaction with human angiotensin converting enzyme. Sci Rep. 2020;10:1–13. doi: 10.1038/s41598-020-79036-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Xiang Y, Nambulli S, Xiao Z, et al. Versatile and multivalent nanobodies efficiently neutralize SARS-CoV-2. 2020;370:1479–1484. doi: 10.1126/science.abe4747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Koenig PA, Das H, Liu H, et al. Structure-guided multivalent nanobodies block SARS-CoV-2 infection and suppress mutational escape. 2021;371:6230. doi: 10.1126/science.abe6230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Lu Q, Zhang Z, Li H, et al. Development of multivalent nanobodies blocking SARS-CoV-2 infection by targeting RBD of spike protein. J Nanobiotechnology. 2021;19:33. doi: 10.1186/s12951-021-00768-w. [DOI] [PMC free article] [PubMed] [Google Scholar]