Abstract
The purpose of our work is to do an update of recent investigations about amblyopia treatment based on perceptual learning, dichoptic training and videogames. Therefore, we conducted a search of the studies published about this subject in the last six years. The review shows that the investigations during that period have used several kinds of treatments regarding their design (e.g., type of stimulus and context used, duration of the training), and in a wider range of age that also include adults. Most of the studies have found an improvement in some mono and binocular visual functions, such as visual acuity, contrast sensitivity and stereopsis, which for now, it seems advisable that these processes could be used, as an alternative or a complement of the traditional passive therapy. Nevertheless, it would be plausible to conduct additional, controlled and random, clinical trials in order to discover in a more deeply way which perceptive learning method of treatment is more effective for the improvement of visual functions and for how long the effects of the treatment could persist.
Keywords: Amblyopia, Perceptual learning, Dichoptic therapy, Videogames
Introduction
Amblyopia (from the greek word amblyos- weak, opia-vision), was defined by Burian in 1956 as a diminution in unilateral or bilateral vision, without any physical cause, detected in the eye exam.1 This type of dysfunction is the principal cause of preventable children blindness, with a prevalence between 1 and 5% and it is still considered one of the most common causes of unilateral visual impairment that persists in the adulthood.2 Amblyopia is considered as a neurodevelopmental disorder of the visual system due to an abnormal binocular vision experience in early childhood.3 Even though amblyopia causes a range of monocular deficit (e.g., visual acuity; VA from now on), it has been proved that one of amblyopia determining characteristics is the loss of binocularity.3 Nowadays, this has led to increased interest in the development of amblyopia treatments that directly address binocular dysfunction by promoting binocular vision and reducing inhibitory interactions within the visual cortex.3 Perceptual learning (PL from now on) refers to any rather stable change in the perception of a subject as a result of the experience with one or more stimulus.4 The repetitive training of a visual task looks forward to develop the perceptive capacity throught the knowledge and the control of the corporal sensations, and in that way, to estimulate the cortical area responsible of the trained function. PL, in some skills (Vernier acuity, position discrimination and contrast sensitivity) seems to transfer, al least partially, to visual acuity improvements and stereoacuity, althought is has been suggested that the transfer effect depends on the spatial frequency choice during the training and that the age (at least up to 30 years old) it does not seem to be an important limitation in PL efficacy.5 Nowadays it is believed that the alterations in neuronal responses in the visual cortex at a young age are the main cause of the visual disfunction in amblyopia, and the possibility to promote the plasticity of the visual cortex by a non-invasive method, such as PL, has opened a very promising field in amblyopia treatment.6 With the development of interactive tools, the PL based in visual stimulation is the new center of attention as a new treatment for amblyopia.
One of the approaches most commonly used to induce PL in amblyopia treatment is Dichoptic Therapy (DT from now on). The treatment for binocular vision using antisuppression dichoptic training is produced by the reduction of the supression in the visual cortex using stimulus presented simultaneouly which are perceived in a separately and different manner in each eye.7 Some computerized programs and videogames (VG from now on) have been thoroughly used in the visual cognition field to improve the selective visual attention and some visuospatial skills.8, 9, 10 In the optometry and ophthalmology field, for more than a decade they have been applied videogames of different types (falling blocks, action and adventure) for amblyopia treatment. The use of VG in the treatment of amblyopia is based in the idea that these can strengthen visual functions such as, VA and stereo acuity.
The conventional treatment for amblyopia is based on the increase of the visual stimulation of the amblyopic eye by oclussion, atropine or the optical penalization of the dominant eye. All of them have been shown effective in the visual improvement, specially in the monocular function. Nevertheless, the management of amblyopia is still a challenge due particularly to problems of compliance and suboptimal results. Recent studies have shown some evidence of different types of amblyopia treatments based in PL (monocular training with grating contrast detection tasks, monocular viewing of action movies and videogames, antisuppression DT, stereopsis training, etc), specially with the restoration of the binocular functions, although these are still under investigation. The main purpose of this article was to study the most recent investigations about amblyopia treatment based in PL and to try to establish the role that they have in these new kinds of treatment. In addition, the results obtained in last investigations that have compared classical occlusion therapy with new kinds of perceptive treatment were analyzed, in order to envisage if PL approach in amblyopia is necessary.
Material and methods
A bibliographic search was conducted using the data base of PubMED, using the following strategies:
- Strategy 1: "Amblyopia" [Mesh] AND "Perceptual Learning" [All Fields].
- Strategy 2: Amblyopia" [Mesh] AND "Dichoptic Therapy" OR "Dichoptic Training".
- Strategy 3: "Video Games" OR “Virtual Reality” [Mesh] AND "Amblyopia" [Mesh].
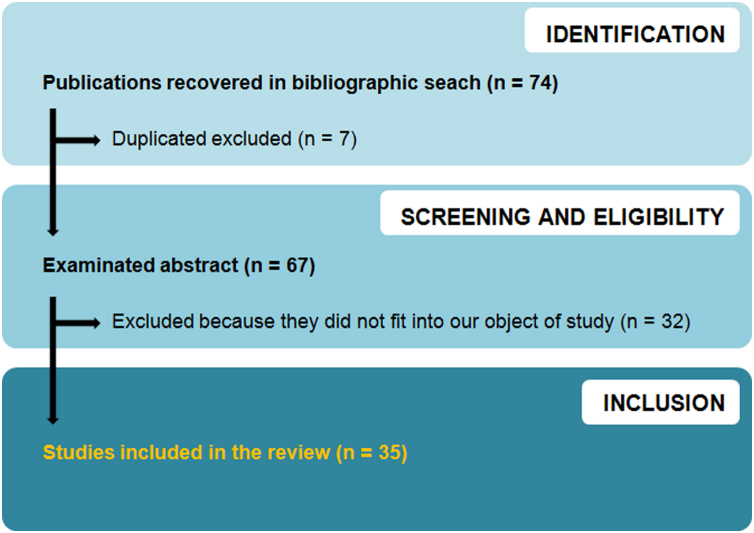
First documentary search was conducted on January 2019. In order to recover the most recent investigations, the publication date was limited to the last 5 years (from January 2014 to January 2019). The results were also limited to publications refering to humans and in English or Spanish. Databases were reviewed again on June 2020 in order to recover investigations published from February 2019 to June 2020, including 6 more studies. Article selection was conducted in different steps. Titles and abstracts were reviewed for excluding duplicates and those which were not relevant for this study because they did not fit into our study question. Following that, we proceeded to download the complete texts in order to review them, selecting those that fitted into our investigation, evaluating and extraction results. Fig. 1 shows schematically how the search and the systematic selection of the articles for this review took place.
Fig. 1.
Flow chart for article selection process.
Additionally, the GRADE system (Grading of Recommendations Assessment, Development, and Evaluation) was used, which is used to define the quality of the evidence in systematic reviews and to qualify the strengh of the recomendations in guidelines, based on a series of considerations.11
Results
In Table 1 the main methodological characteristics of studies in which our review is based are shown. In Table 2 the results, conclusions and limitations from the same studies as before are detailed.
Table 1.
Methodological characteristics of studies included in the review.
| Study | Sample type and size | Intervention | Characteristics of the PL group | Outcome measure |
|---|---|---|---|---|
| Hess et al., 201412 |
|
|
|
|
| Mansouri et al., 201413 |
|
|
|
|
| Xi et al., 201414 |
|
|
|
|
| Zhang et al., 201415 |
|
|
|
|
| Birch et al., 201516 |
|
|
|
|
| Khan et al., 201517 |
|
|
|
|
| Li SL et al., 201518 |
|
|
|
|
| Li J et al., 201519 |
|
|
|
|
| Verdamurthy et al., 2015a20 |
|
|
|
|
| Verdamurthy et al., 2015b21 |
|
|
|
|
| Chen et al., 201622 |
|
|
|
|
| Dadeya & Dangda, 201623 |
|
|
|
|
| Herbison et al., 201624 |
|
|
|
|
| Holmes et al., 201625 |
|
|
|
|
| Kelly et al., 201626 |
|
|
|
|
| Verdamurthy et al., 201627 |
|
|
|
|
| Barollo et al., 201728 |
|
|
|
|
| Bossi et al., 201729 |
|
|
|
|
| Singh et al., 201730 |
|
|
|
|
| Žiak et al., 201731 |
|
|
|
|
| Gambacorta et al., 201832 |
|
|
|
|
| Gao et al., 201833 |
|
|
|
|
| Jia et al., 201834 |
|
|
|
|
| Kelly et al., 201835 |
|
|
|
|
| Liu & Zhang, 201836 |
|
|
|
|
| Manh et al., 201837 |
|
|
|
|
| Mezad-Koursh et al., 201838 |
|
|
|
|
| Moret et al., 201839 |
|
|
|
|
| Portela et al., 201840 |
|
|
|
|
| Holmes et al., 201941 |
|
|
|
|
| Law & Backus 201942 |
|
|
|
|
| Liu & Zhang, 201943 |
|
|
|
|
| Sauvan et al., 201944 |
|
|
|
|
| Birch et al., 202045 |
|
|
|
|
| Gu et al., 202046 |
|
|
|
|
Note: A: anisometropic amblyopia; AE: amblyopic eye; BiT: binocular treatment; C: combined mechanism amblyopia (i.e., strabismic and anisometropic); cpd: cycles per degree; CS: contrast sensitivity; DT: dichoptic therapy; h: hour/ hours; hf-tRNS: high-frequency transcranial random noise stimulation; I: isometropic; IOR: interocular ratio; min: minutes; MT: monocular training; PL: perceptual learning; S: strabismic amblyopia; SSVEPs: Steady-state visually evoked potentials; tDCS: transcranial direct current stimulation; VA: visual acuity; VG: video game; VR: virtual reality. "Both" refers applied equally to both groups.
Table 2.
Most relevant results, conclusions and limitations of studies included in the review.
| Study | Results | Limitations / recomendations exposed by the authors | Compliance |
|---|---|---|---|
| Hess et al., 201412 |
|
|
|
| Mansouri et al., 201413 |
|
|
|
| Xi et al., 201414 |
|
|
|
| Zhang et al., 201415 |
|
|
|
| Birch et al., 201516 |
|
|
|
| Khan et al., 201517 |
|
|
|
| Li SL et al., 201518 |
|
|
|
| Li J et al., 201519 |
|
|
|
| Verdamurthy et al., 2015a20 |
|
|
|
| Verdamurthy et al., 2015b21 |
|
|
|
| Chen et al., 201622 |
|
|
|
| Dadeya & Dangda, 201623 |
|
|
|
| Herbison et al., 201624 |
|
|
|
| Holmes et al., 201625 |
|
|
|
| Kelly et al., 201626 |
|
|
|
| Verdamurthy et al., 201627 |
|
|
|
| Barollo et al., 201728 |
|
|
|
| Bossi et al., 201729 |
|
|
|
| Singh et al., 201730 |
Stereons, CSns |
|
|
| Žiak et al., 201731 |
|
|
|
| Gambacorta et al., 201832 |
|
|
|
| Gao et al., 201833 |
|
|
|
| Jia et al., 201834 |
|
|
|
| Kelly et al., 201835 |
|
Movie group: 100% prescribed treatment time |
|
| Liu & Zhang, 201836 |
|
|
|
| Manh et al., 201837 |
|
|
|
| Mezad-Koursh et al., 201838 |
|
|
|
| Moret et al., 201839 |
|
|
|
| Portela et al., 201840 |
|
|
|
| Holmes et al., 201941 |
|
|
|
| Law & Backus 201942 |
|
|
|
| Liu & Zhang, 201943 |
|
|
|
| Sauvan et al., 201944 |
|
|
|
| Birch et al., 202045 |
|
|
|
| Gu et al., 202046 |
|
|
Note: A: anisometropic amblyopia; BCVA: Best corrected visual acuity; BiT: binocular treatment; cpd: cycles per degree; CS: contrast sensitivity; DT: dichoptic therapy; h: hour/ hours; IOR: interocular ratio; min: minutes; MT: monocular training; ns: no significance; PL: perceptual learning; S: strabismic amblyopia; SSVEPs: Steady-state visually evoked potentials; VA: visual acuity; VG: video game.
Cohen's “d” effect size has been calculated when the p-value is not shown in the study, but means and SD are shown (d≥0.80 is considered a large effect size)."Both" refers applied equally to both groups. The average improvement in VA lines is always referred from the baseline.
p < 0.05;
p < .01;
p < .001.
Types of training based on PL for amblyopia
Over the last years several investigations have been conducted, in which the effect that different approaches have in amblyopia treatment through PL has been analyzed.12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46One of the approaches is monocular training (MT), which consists in making tasks while the dominant eye is occluded, the aim is that the amblyopic eye is stimulated. In some studies, MT has been conducted using grating contrast detection (Gabor patch)15, 22, 28, 30,34, 39, 46 while other studies have used monocular videogames viewing in order to stimulate the amblyopic eye.17, 23, 30 It has been seen that both types of treatment improve VA,15, 17, 22, 13,28, 30, 34, 39,46 while contrast sensitivity (CS, from now on) improves when grating patterns are used, more specifically those frequencies near the cutoff frequency.15, 34, 46 The studies which have analyzed the grade of improvement in stereoacuity with monocular training have positive results,15, 22, 23, 34,46 although it has not been like that when the treatment is used for children and using a similar time of treatment or, even higher, compared with those which have improved stereoscopic function.40
The other treatment approach for amblyopia through PL is the so called DT, which has been used over the last years in several investigations in order to reduce supression and to improve binocular function using the presentation of different information to each eye.12, 13, 16, 18, 19, 20, 21, 24, 25, 26, 27, 29, 31, 32, 33, 35–38, 41, 42, 43, 44, 45 The basis used in DT are different though different studies using anaglyphs,12, 16, 25, 26,33, 35, 37, 41,45stereoscopes,20, 21, 32, 36,42, 43, 44 lenticular screen,12, 19 virtual reality,27, 28 polarized lens,18 and other types of mechanisms used to improve binocular vision (e.g., video stereo-googles, liquid crystal shutter glasses).13, 19, 24, 29,38 In general, an improvement in VA has been noticed using this type of dichoptic procedures,12, 13, 16, 18,20, 21, 24, 25, 26, 29, 31, 32,35, 38, 43, 44, 45 though some studies conducted in children41 and in adult patients 27, 33, 36 have failed to show that evidence.
Regarding the improvement in stereopsis, the results are unalike, so some investigations12, 20, 21, 27,29, 31, 35, 36,42, 43 have shown an improvement of the binocular function, even though the intervention has been conducted in adult population,12, 20, 21, 27,31, 36, 42, 43 while other investigations have not proved this improvements even though the treatment has been conducted in children.16, 18, 24, 25,26, 44 In order to use suppression, which has not always been analyzed, different findings have been obtained, while some authors have obtained a reduction of supression in children35 and in adults,20, 27 other authors have not obtained these improvements.16, 18, 25, 26,44 CS is another function which can be improved using dichoptic therapy.19, 20, 21, 43
In other investigations they have explored if the two types of treatments mentioned (monocular and dichoptic) can have different effects over the improvement of the evaluated visual functions in amblyopic patients. For example, in one of the investigations21 it has been seen through an action video game in DT format, the improvements in VA are significantly better than monocular viewing of action movies, although both treatments are equally effective in the improvement of CS, stereoacuity and reading speed. In a similar way, in a different investigation32 it has been seen that antisupression DT produces better increments in VA, although not in stereopsis compared to MT. In other inversigation, with a crossover design,19 because improvements were small in the monocular group, this group was crossed over to DT for 10 days longer once the monocular training was completed in order to assess whether additional improvements would occur. Authors found out that DT was more effective at improving CS than monocular training, suggesting that this kind of DT modifies the sensitivity of the neural systems that underpin monocular CS. In other studies, they have compared the effects of occlussion clasical therapy with the ones produced by the use of VG with iPad in a DT format,25, 26, 37, 45 with the viewing of VG in monocular conditions,23, 30 or with grating contrast detection tasks.22, 46 While some authors have seen that DT produce higher improvements in VA than occlusion therapy,26, 45 other authours have not seen those differences.25, 37 Studies which have compared the effectivity obtained in VG viewing in monocular condition compared to the improvements obtained with patching therapy have demonstrated that PL in monocular conditions is more effective.23, 30 Meanwhile Chen et al.22 have not concluded if there are differences between both techniques (monocular task of detecting contrast patterns vs. patching) in terms of visual improvements. The gain produced using DT has also been compared to the gain obtained with a simple refractive grating with glasses, finding that increasements in VA after 4 weeks of treatment is similar between patients that only wear glasses and those who besides wearing glasses conduct dichoptic therapy using VG.51 Other investigations have been centered in analyze different effects in the improvements produced in VA, CS, stereopsis and suppression when DT is applied by itself or when combined with MT 43 or with patching,44 in other studies it has been seen that MT combined with a high-frequency transcranial random noise stimulation is more effective for VA improvement that MT by itself.39
As previously mentioned, there exists some divergence in the results obtained about the improvement that can be achieved in stereopsis in a training based in DT antisuppression. This fact has motivated, at least partially, that some authors have used the paradigm of directly training stereoscopic vision through PL in order to restore depth vision. And it has been suggested that training using stereograms can stimulate neurons that respond to disparity.47 For example, Xi et al.14 using different texture anaglyphs with different disparities found an improvement in disparity threshold, stereoacuity and VA. In a similar way, in another study27 that used DT with stereocopic cues in a virtual reality environment, that also found a significant reduction of the suppression and an improvement in stereoacuity, even though it is a trend to an improvement in VA. Portela et al.40 using VG in Random Dot stimuli format, and have found a significant improvement of stereoacuity in two levels on Wirt Circles and stereoacuity 140 s of arc or less, besides stereopsis remained stable after 6 months when it was measured with the Randot Preschool Stereoacuity Test.
Use of VG as a resource of PL in amblyopia
The investigation about the use of VG has increased over the last years, in an effort to improve the level of compliance of the patient and so the therapy for amblyopia will be more effective. Of the 35 studies gathered in this review, 18 of them (51.4%) use PL through several videogames of different contents, such as pieces and falling blocks12, 16, 19, 25,31, 33, 37 and VG based on action or adventure.20, 21, 23, 24,26, 30, 31, 32,35, 41, 45 It is rare that VG are used in a form of PL in a monocular way, but some authors have conducted this type of treatment in order to analysed the visual improvements produced.23, 30 In these studies with anisometropic amblyopes have compared the interaction with action VG monocularly and occlusion classical therapy, finding in both studies that the first method is more effective in order to improve VA. Nevertheless, the effects produced over stereopsis are not that clear. Dadeya and Dangda23 found stereopsis improvement in children from 4 to 7 years old, conducting a training with a duration of 6 h in clinic, so the children were supervised constantly and this ensured that the compliance rate was total. On the contrary, Singh et al.30 did not found improvement in depth perception in their group of children from 6 to 14 years old, in a training method conducted partially at home, even more (30 h in total) than the study of Dadeya & Dangda.
In most of VG, DT has been applied and improvements in VA have been found, even when compared with a control group or with a different group conducting a different strategy (e.g., patching).12, 16, 20, 21,24, 25, 26, 32 Several clinical trials have not found home training with VG more effective than a placebo training,33 occlusion therapy,37 or optical correction,41 although it should be pointed out that the rate of compliance of patients in this studies was <65%,33, 41 and even in the study of Manh and colleagues, compliance rate was really low (13%). On the contrary, other clinical trials have found VG at home as an useful tool used to improved VA35, 45 when compliance rate has been nearly or higher than 90% of the duration of the treatment prescribed. Regarding the improvements in stereoacuity, some unalike results have been found using this type of treatment consisting in DT in a gamified context of PL, so some authors have found improvements in this binocular function,12, 20 while others have not.16, 21, 32 DT in a virtual reality enviroment has aso been applied in a VG context.27, 31 In the investigation conducted by Verdamurthy et al.,27 a ‘bug squashing’ videogame was used in a VR environment and binocular functions improvements had been found (reduction of the suppression and stereopsis improvement). For their part, Žiak et al.31 used two types of VG (flying spaceship and block breaker games) in a DT with VR format, finding some improvements in VA and in stereoacuity.
In some investigations,40 as mentioned previously, specific VG have been used in order to improve stereoscopic vision, using tasks with random dot stimuli (RDS), finding satisfactory results in depth vision, even in strabismic amblyopes.
Inclusion of control group
The incorporation of control and/or placebo groups in investigations is an important aspect in order to know the real efficacy of a certain treatment, although this has not always been taking into account in different PL studies. While some investigations have only included an experimental group,13, 14, 15, 17, 18, 20,27, 29, 31, 34,36 other investigations have included two experimental groups which have subjected two different approaches of the treatment related to PL, but there were not a participants group without an intervention or with a different type of treatment which was not related to PL.12, 19, 21, 32,35, 43, 44 In other investigations a controlled or comparison group has been included, so the participants in this group have conducted a classical occlusion therapy22, 23, 25, 26,30, 37, 45, 46 or used the optical prescription by itself.41 In other studies, the control or comparison group has consisted in an ineffective type of treatment through stimulation strategies using the dominant eye –instead of the amblyopic eye–16, 33 or using both eyes equally24, 38, 42 when using DT, gross stimulation of stereopsis40 or the inclussion of non amblyopic patients.28
Durability and transfer of training
The durability of the effects produced by a treatment using PL has not always been a considered aspect. Just in 12 (34.2%) studies of this review a follow-up has been conducted in order to value if the improvements obtained after the training is completed are maintained through time. Nevertheless, this follow-up sessions are very variable through different studies which have analyzed this longitudinal aspect, varying from 6 weeks32 to 10 months.36 In general, it has been seen that the improvements in VA,13, 14, 21, 28,32, 36, 38, 39,44 in CS,28 in stereoacuity14, 21, 27, 32,36, 40 and in the reduction of the suppression27 can be maintained over time. It is worth it to say that in one study, the follow-up has been analyzed, like the one conducted by Xi et al.14 that found that visual improvements were maintained in two of the three patients re-evaluated after 5 months. Other authors have conducted a follow-up at 3 months after the cessation of game play but they have not informed about the obtained results.16
In general, it has been seen that training in amblyopic patients using specific skills that imply PL, transfers to an improvement in clinical trials such as VA and stereopsis as mentioned previously. Some investigations have proved the transfer effects that a monocular treatment may produce in binocular functions.15, 22, 23, 34,46 Aditionally, ii has been seen that the binocular training through DT,12, 13, 16, 18, 19, 20, 21, 24, 25, 26, 29, 31, 32,35, 38, 43, 44,45 or the specific training of stereopsis14 leads improvements in monocular functions. Nevertheless, it is not rare that PL produced a higher improvement in the trained skilled rather than VA or stereopsis as suggested by Liu and Zhang.36 Recently, Liu and Zhang43 have suggested that “transfer of learning with training plus exposure through an irrelevant task, is because an improvement in high-level brain processing, and that may strengthen top-down attention to fellow eyes to counter the impacts of attentional bias to fellow eye and/or physiological interocular suppression and improve stereoacuity”.
An essential point of a treatment whatever the method of training chosen, is the impact that the improvements can have in real-life. For example, Vedamurthy et al.27 found out that two of the eleven patients trained reported better distance judgement during driving, and one was able to appreciate depth from autostereograms for the first time. It would be plausible that the improvements produced in some activities in real –life were evaluated through questionaries or questions regarding the quality of life after the treatment.
Quality of evidence
In many investigations, the conclusions obtained are limited by the desing of the study (e.g. absence of a control group or the aplication of a method of masking [i.e., blinding] in order to reduce the risk of bias). The procedures used to organize the evidence hiearchically and to establish the recommendation are the basis for the development of the clinical practice guidelines. GRADE provides explicit criteria for rating the quality of evidence that include limitations in the study design (risk of bias), inconsistency of the results (inconsistency), uncertainty of the evidence being direct (indirectness), inaccuracy for wide confidence intervals (CI), small samples or small events (imprecision), bias of publication or notification (publication bias).11 Table 3 shows the GRADE evidence profile of the different studies included in this review.
Table 3.
GRADE evidence profile.
| Study | Design of study | Level of evidence† | A priori quality level | Detected criteria lowering and raising‡ “a priori quality level” | Quality of the evidence |
|---|---|---|---|---|---|
| Hess et al., 201412 | Case-series study | IV | low |
|
very low |
| Mansouri et al., 201413 | Case-series study | IV | low |
|
very low |
| Xi et al., 201414 | Case-series study | IV | low |
|
very low |
| Zhang et al., 201415 | Case-series study | IV | low |
|
very low |
| Birch et al., 201516 | Cohort study | III-2 | low |
|
low |
| Khan et al., 201517 | Case-series study | IV | low |
|
very low |
| Li SL et al., 201518 | Case-series study | IV | low |
|
very low |
| Li J et al., 201519 | Cohort study (crossover design) | III-2 | low |
|
very low |
| Verdamurthy et al., 2015a20 | Case-series study | IV | low |
|
very low |
| Verdamurthy et al., 2015b21 | Cohort study | III-2 | low |
|
low |
| Chen et al., 201622 | Cohort study | III-2 | low |
|
very low |
| Dadeya & Dangda, 201623 | Clinical trial (parallel, randomized, no masking) | II | high |
|
high |
| Herbison et al., 201624 | Clinical trial (parallel, randomized, simple-blind) | II | high | No highlights | high |
| Holmes et al., 201625 | Clinical trial (parallel, randomized, simple-blind) | II | high |
|
high |
| Kelly et al., 201626 | Clinical trial (cross-over, randomized, no masking) | II | high |
|
high |
| Verdamurthy et al., 201627 | Case-series study | IV | low |
|
very low |
| Barollo et al., 201728 | Cohort study | III-2 | low |
|
low |
| Bossi et al., 201729 | Cohort study | III-2 | low |
|
very low |
| Singh et al., 201730 | Clinical trial (parallel, randomized, no masking) | II | high |
|
high |
| Žiak et al., 201731 | Case-series study | IV | low |
|
very low |
| Gambacorta et al., 201832 | Clinical trial (parallel, randomized, no masking) | II | high |
|
moderate |
| Gao et al., 201833 | Clinical trial (parallel, randomized, double-blind) | II | high | No highlights | high |
| Jia et al., 201834 | Case-series study | IV | low | No highlights | low |
| Kelly et al., 201835 | Clinical trial (cross-over, randomized, no masking) | II | high |
|
moderate |
| Liu & Zhang, 201836 |
Case-series study | IV | low |
|
very low |
| Manh et al., 201837 |
Clinical trial (parallel, randomized, simple-blind) | II | high |
|
high |
| Mezad-Koursh et al., 201838 | Cohort study | III-2 | low |
|
very low |
| Moret et al., 201839 | Cohort study | III-2 | low |
|
low |
| Portela et al., 201840 |
Clinical trial (parallel, randomized, double-blind) | II | high |
|
high |
| Holmes et al., 201941 |
Clinical trial (parallel, randomized, simple-blind) | II | high | No highlights | high |
| Law & Backus 201942 | Cohort study | III-2 | low |
|
very low |
| Liu & Zhang, 201943 |
Cohort study | III-2 | low |
|
very low |
| Sauvan et al., 201944 | Cohort study | III-2 | low |
|
very low |
| Birch et al., 202045 | Clinical trial (cross-over, randomized, no masking) | II | high |
|
moderate |
| Gu et al., 202046 | Cohort study | III-2 | low |
|
very low |
Note: † National Health & Medical Research Council clinical evidence hierarchies.
Of the 35 studies included, 23 of them (65.7%) are of the observational type, and eleven of those (31.4%) are case-series study and twelve (34.3%) are cohort study. The other twelve (34.3%) remaining investigations are experimental or clinical trial, that vary in their design (see column “Design of the study in Table 3). After making a series of decisions based on the criteria for rating the quality of evidence11 (see “Discussion” section for a more thorough explanation), nine (25.7%) present “high” quality (a lot of confidence that the true effect is similar to the estimated effect), three (8.6%) in a “moderate”level (the true effect is probably close to the estimated effect), five (14.3%) in a “low” level (the true effect might be markedly different from the estimated effect) and 18 (51.4%) in a “very low”level (the true effect is probably markedly different from the estimated effect).
Discussion
Impact of PL in the visual improvement in amblyopes
As a result, the trials published in the last 6 years state some consistent aspects regarding the idea that amblyopia treatment might be aimed to restore visual functions (improvements in VA, CS or estereopsis and reduction in interocular suppression) using new active strategies such as perceptive learning taking advantage of technological resources that we now have, like videogames or virtual reality. Regarding the gain of one of the key visual functions, VA, different clinical trials23, 26, 30, 32,35, 45 have shown that a notorious increase can be achieved through an extent range of stimulus, tasks and duration of the training based in PL. The augmentation degree in VA varies from one study to another, but the increment found was from 1 and 2 lines in a logMAR chart. Even in a study conducted in 6 years old children it has been seen that the group who conducted a PL training for a small amount of time (6 h) gained an average of 4.2 lines.23 Also in some cohort studies19, 21, 22, 28,39, 43, 44, 46 conducted in adults it has been seen that the gain produced in VA breaks the theory that was established that the visual deficiency of amblyopic people, more concretely the VA, could just be recovered if the treatment was implemented before the end of the critical period. In some of these studies conducted in adult population, even the depth vision it is possible to restore.22, 42, 43, 46 This opens an encouraging path for this kind of population or group of age, for those whose treatment was reduced to surgery or, directly, those who were relegated to not being able to do any treatment.
Regarding the time employed in order to achieve some improvements, the results seem to be encouraging, due to the improvements found in a relatively small period of time. In some of the clinical trials of this review, training with PL took place that have varied from 6 to 30 h of training, in order to improve VA or stereopsis. In general, it is estimated that therapy with patching requires 120 h of training in order to achieve a 1-line gain in amblyopic children that were previously treated with glasses.48 In a recent investigation45 it has been seen that in just 2 weeks (10 h) of PL with a binocular adventure VG are enough to produce a gain in VA of 1.5 lines, a result which is a remarkably result when compared to previous findings in which 16 weeks of occlusion were needed (224 h in total) in order to produce improvements in VA of more than one line,25, 37 If the satisfactory results obtained in this controlled clinical trials are confirmed throughout other trials so the rate of gain of visual functions can be analyzed like stereopsis in adults with amblyopia, it could be confirmed that perceptual learning could be useful as a primary, complementary or maintenance treatment, obtaining improvement in a relatively brief period of time.
Empirical evidence of PL in amblyopia
Regarding the level and quality of evidence, it is important to point out that several investigations included in this review have a case-series study design, this fact makes a lower level of evidence. Even when cohort studies are conducted, where a control group inclusion is considered, it has been suggested that a randomized clinical trial is needed to evaluate the effectiveness of a potential amblyopia treatment in routine clinical practice16, 18 and to compare its effectiveness with the current standard of care.16 It seems that over the last few years, the number of experimental studies have increased (clinical trials) in the context of perceptual learning as a treatment for amblyopia.23, 24, 25, 26, 30, 32, 33,35, 37, 40, 41,45 This type of experimental investigations are characterized for the high level of evidence, because systematic mistakes or bias can be minimized considering the existence of a comparison or control group, that allows to prove if the intervention is better (or not) than the existing ones. Nevertheless, in the investigations there are presented some relative criteria for risk of bias (non making), imprecision (small sample size per group or per condition [i.e., stype of amblyopia]) and indirectness (wide age range, duration of exposure in both groups is different), and all of them lower the quality level of the study, and could affect negatively to their evidence rate. It is not usual in this kind of studies to inform about risk ratio (RR) or dose-response gradient, criteria that are used to improve the quality of the evidence. In fact, none of the studies provide RR, while the dose-response gradient was informed in two of the studies,30, 45 where it can be seen that the effects produced improve when the duration of the treatment is longer, In other cases,23, 26, 28, 39,40 we have considered the dose-response gradient when significant gain has been obtained with a training that has implied a substantial training with a duration and intensity (number of trials) enough to produce that gain. In this case, in order to have the certainty that the training effects were not related to a learning effect, we just consider the dose-gradient response in those studied that had a control group who did not conduct a therapy related to PL. Furthermore, this criteria was only considered when both treatment and control groups had the same dosage (duration and intensity) of treatment.
Of all of the studies included in this review, just the 34.3% are clinical trials, and the 25.7% of those have a “high” evidence quality, and the 8,6% have a “moderate” clinical evidence. In spite of that, it is interesting to remark that the investigation about PL (and the use of VG) is promising. Currently there are 15 clinical trials in process about this types of treatment for amblyopia and that are registered in ClinicalTrials.gov (http://www.clinicaltrials.gov), a database maintained by the National Library of Medicine (NLM) at the National Institutes of Health (NIH) where there are privately and publicly funded clinical studies conducted around the world.
Guidelines for home training and compliance rate of the patient
Some authors49 have proposed a protocol or a viable and detailed therapy guideline, based on the results of a clinical trial about PL using random-dot stimuli in a video game format to improve stereoacuity.40 This type of protocol can help the clinician in the decision making and the optimal management of the amblyopic patient who is treated with this type of training based on perceptual learning. In the first face-to-face session in the consult it is essential to provide to the patient/parents some guidelines such as the suitable distance to the monitor where the stimulus is presented, the correct position of the monitor in order to avoid light reflections, the previous configuration of the game or the appropriate position of the dissociative filters so the amblyopic eye is stimulated correctly. Evidently, it is not less important the realization of frequent follow-ups that serve to analyze the development and value if this type of treatment is being effective.40
Compliance or compromise rate that the patient has with the treatment will also determine the usefulness of the treatment. Most of the studies included in this review have been conducted in a laboratory or a clinic (see Table 1) using tasks that can be more or less tedious for the patient, but at the same time assures that the compliance rate of the patient increases because the clinician is keeping the patient under observation (in order to have a more detailed information about compliance rate, see Table 2). The use of serious VG, that have a series of qualities and mechanics of the game can help to benefit neuronal plasticity and a learning experience to the patient32 Moreover, the VG used have to be attractive in order to increase compliance rate of the patient, although it has been seen that is not always that way when training has been conducted at home,25, 37 In the study conducted by Holmes et al.25 compliance percentage was at first optimal according to the information provided by parents/patients (66.7%), but analyzing the database registered generated by iPad, the rate of compliance reported was significantly lower (22.2%). In a similar way, Manh et al.37 also found a poor adherence to the treatment with a VG using the iPad at home, so only 13% of participants completed more than 75% of the prescribed treatment. The use of VG at home as a way of amblyopia treatment could be an interesting resource, specially for those patients that have serious difficulties to go regularly to the consult, but in order to achieve that the program or the VG should allow the clinician to do a follow-up in a remotely and reliable manner about the duration and frequency of use by the patient.
Altogether, previous guidelines, compliance rate evaluation and frequent follow-ups to the patient, could be three important foundations so the success rate and the effectiveness of the treatment can be increased when using the VG method from home.
Limitations and future research
The PL studies reviewed show some limitations that sometimes their authors have acknowledge in the studies (see Table 2). Doubtlessly, one of the more important limitation is the small amount of subjects, so when analyzing by group segmentation (e.g., treatment groups, kind of amblyopia, group of age), the results could be spurious and inconclusive. Furthermore, some factors such as age of the patient, previous treatments (e.g., patching) in residual amblyopia, the modification or adaptation of the refraction using lenses during the training period, or the baseline of VA and stereopsis could have influence in the effects produced by the training. That is why, it would be plausible that in future investigations this differential factors are taken into account, something that has not been considered, or when considered dissimilar results have been obtained in different studies. Other limitation that affects to the quality of an investigation, as we have seen previously, could be the absence of a control group an aspect that is determining if you pretend to evaluate the truly effects of the training. The evaluation of the compliance rate of the patient regarding the training, short-medium term follow-ups in order to analyze the duration of the effects or the dose-response gradient (which has been thoroughly analyzed in occlusion therapy)48 are limitations that have been found in this review, and that are also key pieces in order to determine if therapy is effective or not.
Regarding the evident of PL using VG, some encouraging discoveries have been found, due to the fact that it seems to have obtained better and quicker results than with occlusion.26, 45 When VG have been combined with occlusion, it has been seen more benefits than occlusion by itself, that is why nowadays it could be recommended to use both types of treatments in a combined manner.23, 30 Some authors40 have suggested that a home treatment based in PL could provide compliance rates higher that other treatments, like occlusion. However additional studies are needed, because some investigations where has not been found that the use of VG is more effective than optical correction41 or than occlusion therapy,25, 37 a low compliance rate has been obtained. In this case, it could be encouraging to determine how to transform binocular games in an amblyopia treatment that could be comfortable and enjoyable in order to achieve a better adhesion. In this regard, it would be plausible to implement attractive VG, that have goals and rewards, in order to maintain the attention for longer periods of treatments maintaining an optimal compliance rate. Regarding that, Holmes y colleagues50 have proposed new studies with the goal of analyzing if the incorporation of longer periods of time with the game before increasing the contrast or carrying out shorter contrast steps in the fellow eye could generate better improvements in the visual functions. Regarding VG, nowadays some of the VG used in investigation, like Dig Rush, are in process of being authorized and commercialized, and other, like Tetris, are easily accessible in a simplified version for computer, smartphone and tablet. Another very useful PL tool (Gabor patches, DT and Random Dot stimuli for stereopsis) that is currently being commercialized is Visionary (https://www.visionarytool.com/). This tool has proven effective for working from home with amblyopic children.41
The limitations detailed until now are related to the ones found throughout the studies included in this review. But we also want to mention some limitations of the review itself. Although we think that the level of evidence showed in Table 3 could be precise, it needs to be said that we only have considered some criteria (risk of bias, indirectness, imprecision, publication bias) that low the “a priori quality level”. Regarding the criteria that could increase the “a priori quality level” these are more limited, considering that just the existence of the dose-response gradient, from the small studies which reflected this aspect. In the investigations in which this gradient has not been provided, we have applied this criteria in those studies when significant gain has been obtained using a training that has implied -to our judgement- a substantial training duration or intensity. Nevertheless, this criteria application should be considered cautiously. Another limitation of this study is that it has not considered doing a statistical analysis for the evaluation of the size of the medium effect throughout different studies about the improvements of visual functions (e.g., VA). This could be considered in future meta-analysis about this subject.
Conclusions
This systematic review of recent studies has found evidence of the new kind of amblyopia treatment, that pretends to stimulate the binocular system by perceptive training, using the dichoptic treatment with or without the use of videogames. In general, the studies conducted until now expose that this kind of treatment is effective, improving some visual functions such as VA even in adults that have exceeded the critical period. This could be, partially at least, due to the format used in this type of active therapy, and is that some authors have suggested that gamification has been used to enhance patient motivation and compliance.49 Nevertheless, it would be plausible to conduct additional controlled and random clinical trials in order to know more deeply in which visuals functions they are more efficient and how long the effects that this kind of treatment based in perceptual learning would persist over time. Based on the results obtained through different studies, for the moment, it seems reasonable to recommend this kind of active therapy as a complementary procedure to the different options of passive therapy like optic correction, occlusion or the penalization with atropine.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare that they have no conflict of interest.
Acknowledgements
The authors would like to thank Agustín Martínez Molina (Universidad Autónoma de Madrid) and Montaña Vivas Jiménez (Hospital San Pedro de Alcántara, Cáceres) for their methodological suggestions to improve this manuscript. Furthermore, thank the reviewers for all the corrections and advice they have given us throughout the process of drawing up.
References
- 1.Burian H.M. Thoughts on the nature of amblyopia ex anopsia. Am Orthopt J. 1956;6:5–12. doi: 10.1080/0065955x.1956.11981153. [DOI] [PubMed] [Google Scholar]
- 2.Papageorgiou E., Asproudis I., Maconachie G., Tsironi E.E., Gottlob I. The treatment of amblyopia: Current practice and emerging trends. Graefes Arch Clin Exp Ophthalmol. 2019;257(6):1061–1078. doi: 10.1007/s00417-019-04254-w. [DOI] [PubMed] [Google Scholar]
- 3.Hess R.F., Thompson B. Amblyopia and the binocular approach to its therapy. Vision Res. 2015;114:4–16. doi: 10.1016/j.visres.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 4.Gibson E.J. Perceptual learning. Ann Annu Rev Psychol. 1963;14(1):29–56. doi: 10.1146/annurev.ps.14.020163.000333. [DOI] [PubMed] [Google Scholar]
- 5.Levi D.M., Li R.W. Improving the performance of the amblyopic visual system. Philos Trans R Soc Lond B Biol Sci. 2009;364(1515):399–407. doi: 10.1098/rstb.2008.0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Polat U., Ma-Naim T., Spierer A. Treatment of children with amblyopia by perceptual learning. Vision Res. 2009;49(21):2599–2603. doi: 10.1016/j.visres.2009.07.008. [DOI] [PubMed] [Google Scholar]
- 7.Hess R.F., Thompson B., Baker D.H. Binocular vision in amblyopia: Structure, suppression and plasticity. Ophthalmic Physiol Opt. 2014;34(2):146–162. doi: 10.1111/opo.12123. [DOI] [PubMed] [Google Scholar]
- 8.Green C., Bavelier D. Action video game modifies visual selective attention. Nature. 2003;423:534–537. doi: 10.1038/nature01647. [DOI] [PubMed] [Google Scholar]
- 9.Rodán A., Contreras M.J., Elosúa M.R., Gimeno P. Experimental but not sex differences of a mental rotation training program on adolescents. Front Psychol. 2016;7:1050. doi: 10.3389/fpsyg.2016.01050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodán A., Gimeno P., Elosúa M.R., Montoro P.R., Contreras M.J. Boys and girls gain in spatial, but not in mathematical ability after mental rotation training in primary education. Learn Individ Differ. 2019;70:1–11. doi: 10.1016/j.lindif.2019.01.001. [DOI] [Google Scholar]
- 11.Balshem H., Helfand M., Schünemann H.J., et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–406. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 12.Hess R.F., Babu R.J., Clavagnier S., Black J., Bobier W., Thompson B. The iPod binocular home‐based treatment for amblyopia in adults: Efficacy and compliance. Clin Exp Optom. 2014;97(5):389–398. doi: 10.1111/cxo.12192. [DOI] [PubMed] [Google Scholar]
- 13.Mansouri B., Singh P., Globa A., Pearson P. Binocular training reduces amblyopic visual acuity impairment. Strabismus. 2014;22(1):1–6. doi: 10.3109/09273972.2013.877945. [DOI] [PubMed] [Google Scholar]
- 14.Xi J., Jia W.L., Feng L.X., Lu Z.L., Huang C.B. Perceptual learning improves stereoacuity in amblyopia. Invest Ophthalmol Vis Sci. 2014;55(4):2384–2391. doi: 10.1167/iovs.13-12627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang J.Y., Cong L.J., Klein S.A., Levi D.M., Yu C. Perceptual learning improves adult amblyopic vision through rule-based cognitive compensation. Invest Ophthalmol Vis Sci. 2014;55(4):2020–2030. doi: 10.1167/iovs.13-13739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Birch E.E., Li S.L., Jost R.M., Morale S.E., De La Cruz A., Stager D.R. Binocular iPad treatment for amblyopia in prescholl children. J AAPOS. 2015;19(1):6–11. doi: 10.1016/j.jaapos.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khan T. Is there a critical period for amblyopia therapy? Results of a study on older anisometropic amblyopes. J Clin Diagn Res. 2015;9(8) doi: 10.7860/JCDR/2015/13277.6288. NC01, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li S.L., Reynaud A., Hess R.F., et al. Dichoptic movie viewing treats childhood amblyopia. J AAPOS. 2015;19(5):401–405. doi: 10.1016/j.jaapos.2015.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li J., Spiegel D.P., Hess R.F., et al. Dichoptic training improves contrast sensitivity in adults with amblyopia. Vision Res. 2015;114:161–172. doi: 10.1016/j.visres.2015.01.017. [DOI] [PubMed] [Google Scholar]
- 20.Vedamurthy I., Nahum M., Bavelier D., Levi D.M. Mechanisms of recovery of visual function in adult amblyopia through a tailored action video game. Sci Rep. 2015;5:8482. doi: 10.1038/srep08482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vedamurthy I., Nahum M., Huang S.J., et al. A dichoptic custom-made action video game as a treatment for adult amblyopia. Vision Res. 2015;114:173–187. doi: 10.1016/j.visres.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen Z., Li J., Liu J., et al. Monocular perceptual learning of contrast detection facilitates binocular combination in adults with anisometropic amblyopia. Sci Rep. 2016;6:20187. doi: 10.1038/srep20187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dadeya S., Dangda S. Television video games in the treatment of amblyopia in children aged 4–7 years. Strabismus. 2016;24(4):146–152. doi: 10.1080/09273972.2016.1242637. [DOI] [PubMed] [Google Scholar]
- 24.Herbison N., MacKeith D., Vivian A., et al. Randomised controlled trial of video clips and interactive games to improve vision in children with amblyopia using the I-BiT system. Br J Ophthalmol. 2016;100(11):1511–1516. doi: 10.1136/bjophthalmol-2015-307798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holmes J.M., Manh V.M., Lazar E.L., et al. Effect of a binocular iPad game vs part-time patching in children aged 5 to 12 years with amblyopia: A randomized clinical trial. JAMA Ophthalmol. 2016;134(12):1391–1400. doi: 10.1001/jamaophthalmol.2016.4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kelly K.R., Jost R.M., Dao L., Beauchamp C.L., Leffler J.N., Birch E.E. Binocular iPad game vs patching for treatment of amblyopia in children: A randomized clinical trial. JAMA Ophthalmol. 2016;134(12):1402–1408. doi: 10.1001/jamaophthalmol.2016.4224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vedamurthy I., Knill D.C., Huang S.J., et al. Recovering stereo vision by squashing virtual bugs in a virtual reality environment. Philos Trans R Soc Lond B Biol Sci. 2016;371(1697):20150264. doi: 10.1098/rstb.2015.0264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barollo M., Contemori G., Battaglini L., Pavan A., Casco C. Perceptual learning improves contrast sensitivity, visual acuity, and foveal crowding in amblyopia. Restor Neurol Neurosci. 2017;35(5):483–496. doi: 10.3233/RNN-170731. [DOI] [PubMed] [Google Scholar]
- 29.Bossi M., Tailor V.K., Anderson E.J., et al. Binocular therapy for childhood amblyopia improves visión without breaking interocular suppression. Invest Ophthalmol Vis Sci. 2017;58:3031–3043. doi: 10.1167/iovs.16-20913. [DOI] [PubMed] [Google Scholar]
- 30.Singh A., Sharma P., Saxena R. Evaluation of the role of monocular video game play as an adjuvant to occlusion therapy in the management of anisometropic amblyopia. J Pediatr Ophthalmol Strabismus. 2017;54(4):244–249. doi: 10.3928/01913913-20170320-04. [DOI] [PubMed] [Google Scholar]
- 31.Žiak P., Holm A., Halička J., Mojžiš P., Piñero D.P. Amblyopia treatment of adults with dichoptic training using the virtual reality oculus rift head mounted display: Preliminary results. BMC Ophthalmol. 2017;17(1):1–8. doi: 10.1186/s12886-017-0501-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gambacorta C., Nahum M., Vedamurthy I., et al. An action video game for the treatment of amblyopia in children: A feasibility study. Vision Res. 2018;148:1–14. doi: 10.1016/j.visres.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gao T.Y., Guo C.X., Babu R.J., et al. Effectiveness of a binocular video game vs placebo video game for improving visual functions in older children, teenagers, and adults with amblyopia: A randomized clinical trial. JAMA Ophthalmol. 2018;136(2):172–181. doi: 10.1001/jamaophthalmol.2017.6090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jia W., Lan F., Zhao X., et al. The effects of monocular training on binocular functions in anisometropic amblyopia. Vision Res. 2018;152:74–83. doi: 10.1016/j.visres.2017.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kelly K.R., Jost R.M., Wang Y.-Z., et al. Improved binocular outcomes following binocular treatment for childhood amblyopia. Invest Ophthalmol Vis Sci. 2018;59:1221–1228. doi: 10.1167/iovs.17-23235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liu X.Y., Zhang J.Y. Dichoptic training in adults with amblyopia: Additional stereoacuity gains over monocular training. Vision Res. 2018;152:84–90. doi: 10.1016/j.visres.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 37.Manh V.M., Holmes J.M., Lazar E.L., et al. Pediatric Eye Disease Investigator Group. A randomized trial of a binocular iPad game versus part-time patching in children aged 13 to 16 years with amblyopia. Am J Ophthalmol. 2018;186:104–115. doi: 10.1016/j.ajo.2017.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mezad-Koursh D., Rosenblatt A., Newman H., Stolovitch C. Home use of binocular dichoptic video content device for treatment of amblyopia: A pilot study. J AAPOS. 2018;22(2):134–138. doi: 10.1016/j.jaapos.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 39.Moret B., Camilleri R., Pavan A., et al. Differential effects of high-frequency transcranial random noise stimulation (hf-tRNS) on contrast sensitivity and visual acuity when combined with a short perceptual training in adults with amblyopia. Neuropsychologia. 2018;114:125–133. doi: 10.1016/j.neuropsychologia.2018.04.017. [DOI] [PubMed] [Google Scholar]
- 40.Portela-Camino J.A., Martín-González S., Ruiz-Alcocer J., Illarramendi-Mendicute I., Garrido-Mercado R. A random dot computer video game improves stereopsis. Optom Vis Sci. 2018;95(6):523–535. doi: 10.1097/OPX.0000000000001222. [DOI] [PubMed] [Google Scholar]
- 41.Holmes J.M., Manny R.E., Lazar E.L., et al. A randomized trial of binocular dig rush game treatment for amblyopia in children aged 7 to 12 years. Ophthalmology. 2019;126(3):456–466. doi: 10.1016/j.ophtha.2018.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Law C.L., Backus B.T. Use of a new composite index to demonstrate improved stereoacuity after training on stimuli with dichoptically asymmetric contrast. Vision Res. 2019;171:73–83. doi: 10.1016/j.visres.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 43.Liu X.-Y., Zhang J.-Y. Dichoptic de-masking learning in adults with amblyopia and its mechanisms. Invest Ophthalmol Vis Sci. 2019;60:2968–2977. doi: 10.1167/iovs.18-26483. [DOI] [PubMed] [Google Scholar]
- 44.Sauvan L., Stolowy N., Denis D., et al. Contribution of short-time occlusion of the amblyopic eye to a passive dichoptic video treatment for amblyopia beyond the critical period. Neural Plast. 2019:6208414. doi: 10.1155/2019/6208414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Birch E.E., Jost R.M., Kelly K.R., Leffler J.N., Dao L., Beauchamp C.L. Baseline and clinical factors associated with response to amblyopia treatment in a randomized clinical trial. Optom Vis Sci. 2020;97(5):316–323. doi: 10.1097/OPX.0000000000001514. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gu L., Deng S., Feng L., et al. Effects of monocular perceptual learning on binocular visual processing in adolescent and adult amblyopia. Iscience. 2020;23(2):100875. doi: 10.1016/j.isci.2020.100875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gantz L., Bedell H.E. Transfer of perceptual learning of depth discrimination between local and global stereograms. Vision Res. 2010;50:1891–1899. doi: 10.1016/j.visres.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stewart C.E., Stephens D.A., Fielder A.R., Moseley M.J. Modeling dose-response in amblyopia: Toward a child-specific treatment plan. Invest Ophthalmol Vis Sci. 2007;48(6):2589–2594. doi: 10.1167/iovs.05-1243. [DOI] [PubMed] [Google Scholar]
- 49.Martín-González S., Portela-Camino J., Ruiz-Alcocer J., Illarramendi-Mendicute I., Garrido-Mercado R. Stereoacuity improvement using random-dot video games. JoVE. 2020;155 doi: 10.1016/0042-6989(77)90009-8. [DOI] [PubMed] [Google Scholar]
- 50.Holmes J.M. Lessons from recent randomized clinical trials of binocular treatment for amblyopia. JAMA Ophthalmol. 2018;136(2):181–183. doi: 10.1001/jamaophthalmol.2017.5938. [DOI] [PubMed] [Google Scholar]