Graphical abstract
Keywords: Echocardiography, Supraventricular arrhythmias, Cardiac magnetic resonance, Cardiac mass, Epidermoid cyst
Highlights
-
•
Cardiac heterotopia (noncardiac tissue in the heart) is a rare condition.
-
•
It is thought to be related to disrupted cell migration during development.
-
•
Cardiac heterotopia can give rises to masses that present with symptoms decades later.
Introduction
We present a case of an unusual right atrial mass found during a workup for palpitations in an otherwise healthy 31-year-old pregnant woman. Surgical pathology eventually revealed this to be a case of cardiac heterotopia, that is, noncardiac tissue located within the heart, presumably as a result of an error in cell migration during embryological development. This rarely observed type of mass provides a fascinating correlation among echo, cardiac magnetic resonance imaging, and histopathology.
Case Presentation
A 31-year-old woman presented with palpitations during her third pregnancy. She reported a feeling of racing heartbeat starting around 35 weeks’ gestation. She had no history of palpitations, documented arrhythmias, or other cardiovascular disease.
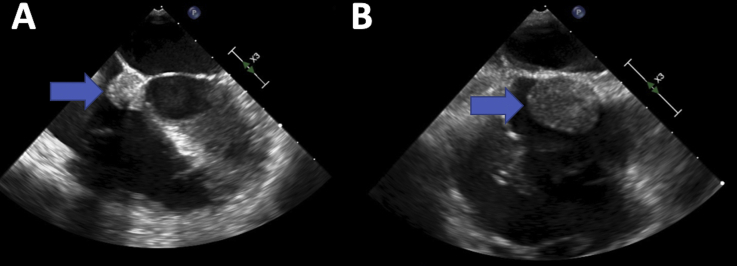
She presented to the emergency department after her Apple Watch reported a heart rate of 200 beats per minute (bpm). Initial electrocardiogram demonstrated a regular, narrow-complex tachycardia with a rate of approximately 200 bpm that terminated with intravenous adenosine, clinically suggestive of atrioventricular (AV) node reentry tachycardia (Figure 1). She was initiated on beta-blocker therapy. A transthoracic echocardiogram that was obtained to evaluate for structural heart disease demonstrated a 1.9 × 1.9 cm right atrial echodensity near the tricuspid valve annulus, without significant valvular dysfunction and with no other structural abnormalities (Figure 2A–B, Video 1). The patient was conservatively treated with metoprolol and subsequently underwent an uneventful labor without recurrence of the arrhythmia during the peripartum period.
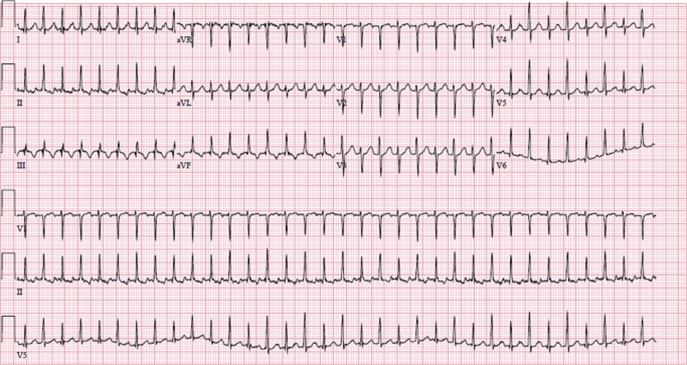
Figure 1.
Twelve-lead electrocardiogram showing presenting rhythm, SVT with rate ∼200 bpm.
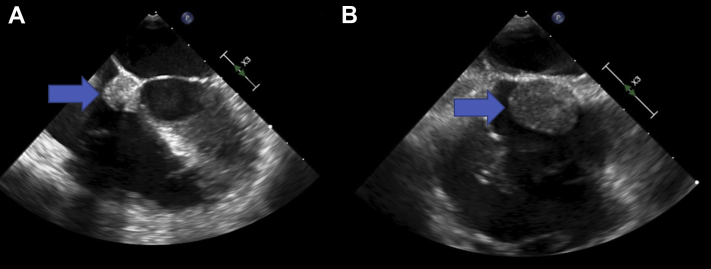
Figure 2.
Echocardiographic views of the mass (marked with arrows) from transthoracic echocardiography. (A) Transthoracic echocardiography apical four-chamber view showing the echo-dense mass arising from the apical portion of the interatrial septum near the tricuspid valve ring. (B) Transthoracic echocardiography parasternal short-axis view showing the right atrial mass attached to the anterior/superior interatrial septum adjacent to the aortic root, a few millimeters above the tricuspid valve annulus. This view better shows the mass's extension into the right atrial cavity.
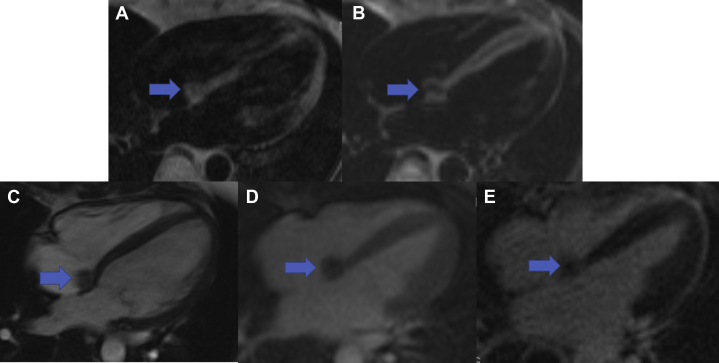
Postpartum, cardiac magnetic resonance imaging was performed for further tissue characterization and showed a 1.5 × 1.5 cm mass at the apical aspect of the interatrial septum (Figure 3A–E). The mass was predominantly isointense on precontrast T1 (Figure 3A) and T2 (Figure 3B) sequences with regions of hypointense signal. The mass was well delineated by steady-state free precession (Figure 3C). On first-pass perfusion imaging (Figure 3D), the mass was hypoperfused in comparison to the normal left ventricular myocardium and displayed no significant late gadolinium enhancement (Figure 3E). These findings were thought to be more consistent with a cystic tumor of the AV nodal region. She was referred to cardiac surgery for consideration of a resection, which is typically recommended promptly after diagnosis to prevent complications such as embolization or sudden cardiac death.1
Figure 3.
Horizontal long-axis cardiac magnetic resonance images characterizing the 1.5 × 1.5 cm mass (marked with arrows) using (A) precontrast T1 and (B) T2, (C) steady-state free precession, (D) first-pass perfusion, and (E) late gadolinium-enhanced sequences.
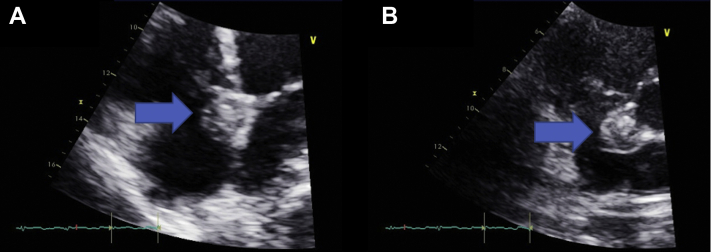
Intraoperative transesophageal echocardiography was utilized during the surgery and provided further views of the mass. These again showed a right atrial mass arising from the atrial septum near the tricuspid valve ring but without impingement on the valve (Figure 4A, Video 2). The mass appeared larger than appreciated on the transthoracic echocardiography in the midesophageal bicaval view (Figure 4B, Video 3) and seemed to be located in an anterior/superior position on the interatrial septum adjacent to the aortic root and anterior to the fossa ovalis. Three-dimensional echo visualization of the mass was also obtained in the midesophageal bicaval view showing its sessile attachment to the apical portion of the interatrial septum and the movement of the tricuspid valve below (Video 4).
Figure 4.
Echocardiographic views of the mass from intraoperative transesophageal echocardiography. (A) Transesophageal echocardiography midesophageal four-chamber view with a clearer view of the mass (marked with arrows) arising from the region of the anterior/superior portion of the interatrial septum. (B) Transesophageal echocardiography midesophageal bicaval view. The mass appears to be attached to the superior aspect of the interatrial septum, although the superior vena cava junction is not well seen in this view.
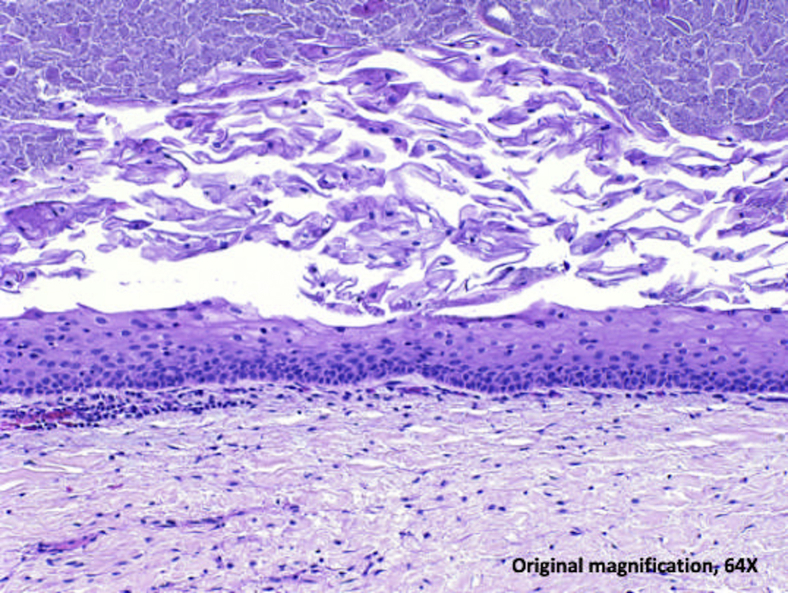
Surgical resection demonstrated a 2.3 cm tan-red cystic mass with focal defects and extruding tan-brown material (Figure 5). Resection of the mass caused a small atrial septal defect that was closed with a bovine pericardial patch. Histopathology of the mass showed a stratified squamous epithelial-lined cyst with abundant central keratinaceous debris and scant underlying fibrous tissue with minimal associated lymphocytic inflammation. The findings are consistent with an epidermoid cyst (Figure 6).
Figure 5.
Gross pathology image of the resected mass: ruler for scale.
Figure 6.
Hematoxylin and eosin–stained section from the resected mass showing a cyst lining of stratified squamous epithelium with abundant central keratinaceous debris and a rim of fibrous tissue.
Postoperatively, she developed transient intermittent complete AV block, likely as a consequence of surgical intervention in the region of the AV node. As her native junctional rate was 60-70 bpm, pacemaker was deferred and she had subsequent recovery of normal AV conduction. She had no further symptomatic arrhythmia after 6 months of follow-up and returned to her normal life. Given the benign nature of the mass, this should be a complete cure.
Discussion
Epidermoid cysts are rare findings within the chest, usually in the posterior mediastinum. Histologically they are lined with stratified squamous epithelial cells.2 They are benign but can causes symptoms due to mass effect. Within the heart itself is a highly unusual location for any type of ectopic tissue. Cardiac heterotopia, the presence of differentiated noncardiac tissue in the heart, has been described, although typically the tissue would be thyroid, thymus, mesothelium, endothelium, or respiratory epithelium3,4 rather than stratified squamous epithelium as in this case. The Pathology Department thought an esophageal cell origin for the cyst was most likely but not definite. Reported cases in the literature have been associated with cardiac or esophageal malformations,5, 6, 7, 8 but those did not seem to be present in this case. We favor the hypothesis that this was a congenital condition: a small patch of squamous epithelium was present in the atrium due to disrupted differentiated cell migration during congenital development and expanded over time.
The fact that the cyst was not associated with other significant anatomic abnormalities likely accounts for her delayed diagnosis, with this mass being found in adulthood. It is possible that the mass grew over time, due to desquamation leading to an accumulation of keratinaceous debris inside the mass. An electrophysiologic study was not clinically indicated, and surgical resection of the mass abolished the arrhythmia so we cannot definitively diagnose the mechanism of the arrhythmia; we hypothesize that the mass being present in the AV nodal region may have contributed an alteration of the AV nodal conduction properties resulting in the slow-fast pathway physiology that makes AV node reentry tachycardia possible and that surgical resection of the mass further altered the conduction properties and abolished the recurrence of the arrhythmia.
Interestingly, a prior similar case of a cystic AV nodal tumor with AV nodal conduction block was also diagnosed shortly after pregnancy and found to have strongly positive staining for estrogen receptors in the mass, with similar histology to this case.9 Estrogen receptor staining was not performed in this case, so we cannot confirm that this may have contributed in this case as well, but it is an interesting possibility.
Conclusion
Cardiac heterotopia (the presence of noncardiac tissue in the heart) is a rare condition but has been described in a few cases. These masses likely derive from disrupted cell migration during development. They are benign but can cause symptoms due to mass effect on cardiac structures. The treatment is surgical removal, which should be curative.
Footnotes
Conflicts of Interest: None.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.case.2021.08.005.
Supplementary Data
Transthoracic echocardiography apical four-chamber view showing the echodense mass arising from the apical portion of the interatrial septum.
Transesophageal echocardiography midesophageal four-chamber view with a clearer view of the origin of the mass from the anterior/superior the interatrial septum. At the end of the clip, the aortic root comes into view showing the mass arising from the interatrial septum adjacent to the aortic valve ring.
Transesophageal echocardiography midesophageal bicaval view showing the mass arising from the interatrial septum in a relatively superior position and anterior to the superior vena cava inflow.
Transesophageal echocardiography three-dimensional midesophageal bicaval view of the mass and its connection to the interatrial septum showing the movement of the tricuspid valve beneath.
References
- 1.Keeling I.M., Oberwalder P., Anelli-Monti M., Schuchlenz H., Demel U., Tilz G.P., et al. Cardiac myxomas: 24 years of experience in 49 patients. Eur J Cardiothoracic Surg. 2002;22:971. doi: 10.1016/s1010-7940(02)00592-4. [DOI] [PubMed] [Google Scholar]
- 2.Nalladaru Z., Mbahi M., Wessels A. Epidermoid cyst: a rare mediastinal mass. Indian J Surg. 2015;77:19–20. doi: 10.1007/s12262-014-1050-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Miller D.V., Edwards W.D. Cardiovascular tumor-like conditions. Semin Diagn Pathol. 2008;25:54–64. doi: 10.1053/j.semdp.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Luc J.G.Y., Phan K., Tchantchaleishvili V. Cystic tumor of the atrioventricular node: a review of the literature. J Thorac Dis. 2017;9:3313–3318. doi: 10.21037/jtd.2017.08.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scheimberg I., Rose S., Malone M. Intracardiac epithelial cyst associated with esophageal atresia. Pediatr Pathol Lab Med. 1996;17:945–949. [PubMed] [Google Scholar]
- 6.Paniagua J.R., Sadaba J.R., Davidson L.A., Munsch C.M. Cystic tumour of the AV nodal region: report of a case successfully treated with surgery. Heart. 2000;83:e6. doi: 10.1136/heart.83.4.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas R., Van Wesep R. Intracardiac epithelial cyst in association with an atrioventricular canal defect. Am J Cardiovasc Path. 1990;3:325–328. [PubMed] [Google Scholar]
- 8.Machens G., Vahl C.F., Hofmann R., Wolf D., Hagl D. Endodermal inclusion cyst of the tricuspid valve. Thorac Cardiovasc Surg. 1991;39:296–298. doi: 10.1055/s-2007-1019990. [DOI] [PubMed] [Google Scholar]
- 9.Tran T., Starnes V., Wang X., Getzen J., Ross B.D. Cardiovascular magnetic resonance diagnosis of cystic tumor of the AV node. J Cardiovasc Magn Res. 2009;11 doi: 10.1186/1532-429X-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Transthoracic echocardiography apical four-chamber view showing the echodense mass arising from the apical portion of the interatrial septum.
Transesophageal echocardiography midesophageal four-chamber view with a clearer view of the origin of the mass from the anterior/superior the interatrial septum. At the end of the clip, the aortic root comes into view showing the mass arising from the interatrial septum adjacent to the aortic valve ring.
Transesophageal echocardiography midesophageal bicaval view showing the mass arising from the interatrial septum in a relatively superior position and anterior to the superior vena cava inflow.
Transesophageal echocardiography three-dimensional midesophageal bicaval view of the mass and its connection to the interatrial septum showing the movement of the tricuspid valve beneath.