Abstract
Background
Aspirin is important for preventing thrombotic events but also increases bleeding complications. Minimizing bleeding while preventing thrombotic events remains challenging in patients undergoing coronary artery bypass grafting (CABG). Establishing the patient's preoperative aspirin response could distinguish patients at risk for perioperative blood loss.
Objective
Aim was to compare 12‐h blood loss after CABG between aspirin‐sensitive and aspirin‐resistant patients.
Patients/Methods
The primary analysis of this substudy of the POPular CABG trial (NCT02352402) included patients that used aspirin monotherapy preoperatively. A preoperative platelet function test by the VerifyNow aspirin assay was performed before CABG and patients were classified as aspirin‐sensitive or aspirin‐resistant based on an aspirin reaction units cutoff value of 550. The primary end point was 12‐hour blood loss after CABG. The secondary end point was, among others, clinical bleeding events after CABG.
Results
A total of 128 patients were included in the primary analysis. Of these, 116 patients were aspirin sensitive and 12 were aspirin resistant. Mean blood loss 12 hours after CABG was 555 ± 278 mL in aspirin‐sensitive patients and 406±110 mL in aspirin‐resistant patients (P = .04). All bleeding events (n = 15; 11.7%) occurred in aspirin‐sensitive patients.
Conclusions
In patients who are on aspirin preoperatively, aspirin sensitivity was associated with 12‐hour blood loss after CABG, suggesting that preoperative VerifyNow aspirin testing could identify patients undergoing CABG at high risk for perioperative bleeding.
Keywords: aspirin; cardiovascular surgical procedures; coronary artery bypass; platelet function tests; blood loss, surgical
Essentials.
Balancing thrombotic and bleeding complications is a challenge in coronary artery bypass grafting (CABG).
Our aim was to compare 12‐hour blood loss between aspirin‐sensitive and aspirin‐resistant patients.
Twelve‐hour blood loss did differ between aspirin‐sensitive and aspirin‐resistant patients.
VerifyNow aspirin testing could identify patients undergoing CABG at risk for perioperative bleeding.
1. INTRODUCTION
Relevant guidelines, including the 2018 European Society of Cardiology/European Association for Cardio‐Thoracic Surgery Guidelines on myocardial revascularization, recommend initiating or continuing aspirin throughout the perioperative period in both stable and unstable patients undergoing coronary artery bypass grafting (CABG), 1 , 2 , 3 as early postoperative use of aspirin is associated with a reduction in death and ischemic complications involving heart, brain, kidneys, and the gastrointestinal tract. 4 Nonetheless, the advantages of perioperative aspirin use are accompanied by a higher risk of perioperative and postoperative bleeding complications. 5 , 6 , 7 , 8
Not all patients display the same level of inhibitory response to aspirin. A proportion of patients, ranging from 10% to 90% (depending on the platelet function test used and timing of platelet function testing 9 ) demonstrate insufficiently suppressed platelets after CABG despite optimal perioperative aspirin administration. This phenomenon is known as aspirin resistance. 9 , 10 Although it is hypothesized that aspirin‐resistant patients are at increased risk of thrombotic events, 11 they might also have a lower bleeding risk, whereas aspirin‐sensitive patients might have lower risk of thrombotic events but increased bleeding risks. Quickly and correctly identifying the preoperative, baseline response to aspirin could be an important factor in distinguishing patients at risk for perioperative blood loss in cardiovascular surgical procedures.
Therefore, the aim of this study was to determine if aspirin responsiveness, determined by preoperative VerifyNow aspirin assay testing (Accumetrics, San Diego, CA, USA), is associated with blood loss within 12 hours after CABG.
2. METHODS
2.1. Study design
This was a post hoc substudy from the POPular CABG trial (Effect of Adding Ticagrelor to Standard Aspirin on Saphenous Vein Graft Patency in Patients Undergoing Coronary Bypass Grafting; NCT02352402). The study was designed in compliance with the Declaration of Helsinki and was approved by the relevant ethics committees and review boards. The POPular CABG was a randomized, double‐blind, placebo‐controlled trial that investigated the effect of ticagrelor in addition to standard aspirin on saphenous vein graft (SVG) patency 1 year after CABG. The rationale and design of the trial have been published, as well as the results of the primary end point. 12 , 13
2.2. Population
Patients who underwent planned CABG with one or more SVGs were eligible for participation. Major exclusion criteria were, among others, use of oral anticoagulation after CABG or a definite indication for use of a P2Y12 inhibitor or antithrombotic agent other than aspirin after CABG. All patients provided written informed consent for the POPular CABG trial, and patients who wanted to participate in this substudy also provided oral informed consent for the blood sampling. In the main study, patients were randomized in the two study groups after a second screening after CABG to ensure that patients did receive a SVG during surgery as planned. Patients who were not included in the POPular CABG trial because they did not meet the criteria of this second screening, but did consent to the trial and underwent blood sampling preoperatively, were included in this substudy. For this substudy, all patients who used a P2Y12 inhibitior within 48 hours before CABG were excluded, as P2Y12 inhibition before cardiac surgery is a well‐known risk factor for blood loss.
2.3. Platelet function testing by the VerifyNow assay
Blood was sampled using venipuncture with 21‐gauge needles before CABG. After a 5 mL discard tube, 1 Greiner Bio‐One partial fill Vacuette vacuum collection tube of whole blood (2 mL), anticoagulated with 3.2% sodium citrate, was withdrawn from each subject. The tubes were gently rotated at least 5 times to ensure complete mixing of the citrate with blood. The assay was performed according to manufacturer’s instructions. All platelet function analyses were performed between 30 minutes and 4 hours after blood sampling. Results of the preoperative VerifyNow assay remained unknown to all operation personnel. Based on the results of the preoperative VerifyNow assay, patients were classified as aspirin sensitive (aspirin reaction units [ARU] value <550) or aspirin resistant (ARU value ≥550). This cutoff value for aspirin‐responsiveness is set by the manufacturer 14 and has been accepted in the medical literature. 15 , 16 , 17
2.4. Blood loss
The primary end point of this study was blood loss 12 hours after CABG, defined as 12‐hour chest tube production. We also evaluated total drain production 12 hours after CABG (chest tube + leg drainage), as well as chest tube and total drain production at 1 hour and 6 hours after CABG and clinical bleeding events 12 hours after CABG. All bleeding events, except for chest tube output, were defined according to the universal definition of perioperative bleeding in cardiovascular surgical procedures 18 (Table S1). As packed red blood cell transfusions were often supplied during surgery to correct for a low baseline hemoglobin or induced hemodilution as a consequence of cardiopulmonary bypass (CPB) and not always for bleeding, it was decided to exclude class 1 bleeding events.
2.5. Statistical analysis
Continuous data are presented as mean ± standard deviation (SD) for normally distributed data, and median and interquartile range for nonnormally distributed data. Categorical data are presented as numbers and percentages. To compare independent continuous variables between groups for normally and nonnormally distributed variables, the Student’s t test and the Mann‐Whitney U test were used. For categorical data the chi‐squared test or Fisher’s exact test was used.
Statistical significance was assumed when the P value was <.05. All statistical analyses were performed using SPSS statistical software for Windows version 24 (IBM Corporation, Armonk, NY, USA).
3. RESULTS
3.1. Trial population
Table 1 shows baseline and procedural characteristics of patients and procedures, respectively. Of 128 patients included, 12 patients displayed a preoperative ARU value of ≥550 ARU and were classified as aspirin resistant. In the total population, the mean age was 69 years, and 87% were men. Indication for CABG was acute coronary syndrome in 24% of cases, and CABG was performed with CPB in 99% of cases. No significant differences in the baseline characteristics of aspirin‐resistant and aspirin‐sensitive patients were identified. Preoperative and direct postoperative hemoglobin, hematocrit, and platelet count were comparable in both groups (Table 1). All patients used aspirin preoperatively. None of the patients used preoperative anticoagulation therapy. Five patients used a P2Y12 inhibitor >48 hours before CABG. Four patients used ticagrelor, this was discontinued 5 days preoperatively in one patient, and 3 days preoperatively in three patients. One patient used clopidogrel; this was halted 5 days preoperatively. All five patients were aspirin sensitive and none of the patients used antithrombotic therapy other than aspirin or anticoagulation therapy within 12 hours after CABG (as this was an exclusion criterion for the trial).
TABLE 1.
Baseline and procedural characteristics
| Total population (N = 128) | Aspirin‐sensitive patients (N = 116) | Aspirin‐resistant patients (N = 12) | P value | |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age, y, mean ± SD | 69 ± 8 | 69 ± 8 | 67 ± 9 | .49 |
| Male sex, n (%) | 111 (86.7) | 100 (86.2) | 11 (91.7) | 1.0 |
| Body mass index, kg/m2, mean ± SD | 27.2 ± 3.9 | 27.2 ± 3.9 | 26.6 ± 4.2 | .61 |
| eGFR < 60, mL/min/1.37 m2, n (%) | 24 (18.8) | 22 (19.0) | 2 (16.7) | 1.0 |
| Current smoker, a n (%) | 19 (14.8) | 15 (13.0) | 4 (33.3) | .08 |
| Indication for CABG | ||||
| Acute coronary syndrome,n (%) | 31 (24.2) | 30 (28.3) | 1 (9.1) | .28 |
| Chronic coronary syndrome, n (%) | 86 (67.2) | 76 (71.7) | 10 (90.9) | |
| Medical history | ||||
| Diabetes mellitus, n (%) | 28 (21.9) | 25 (21.6) | 3 (25.0) | .72 |
| Hypertension, n (%) | 79 (61.7) | 74 (63.8) | 5 (41.7) | .21 |
| Hypercholesterolemia, b n (%) | 56 (43.8) | 48 (41.4) | 8 (66.7) | .09 |
| Prior PCI, n (%) | 28 (21.9) | 26 (22.4) | 2 (16.7) | 1.0 |
| Prior CABG, n (%) | 2 (1.6) | 2 (1.7) | 0 (0) | NA |
| Preoperative laboratory results | ||||
| Hemoglobin, mmol/L, mean ± SD | 9.0 ± 0.8 | 9.0 ± 0.8 | 9.0 ± 0.9 | .99 |
| Hematocrit, L/L, mean ± SD | 0.42 ± 0.04 | 0.42 ± 0.04 | 0.42 ± 0.04 | .71 |
| Platelet count, (×103 per mm3, mean ± SD | 241 ± 59 | 242 ± 59 | 231 ± 64 | .71 |
| Medication | ||||
| Start of aspirin <5 days preoperatively, n (%) | 11 (8.6) | 10 (8.6) | 1 (8.3) | 1.0 |
| Use of P2Y12 inhibitor >48 h before CABG | 5 (3.9) | 5 (4.3) | 0 (0) | 1.0 |
| Intraoperative characteristics | ||||
| On‐pump CABG, n (%) | 127 (99.2) | 115 (99.1) | 12 (100.0) | 1.0 |
| Time on cardiopulmonary bypass, hh:mm, mean ± SD | 01:28 ± 00:25 | 01:27 ± 00:23 | 01:35 ± 00:37 | .61 |
| Administering of tranexamic acid, n (%) | 183 (64.8) | 75 (64.7) | 8 (66.8) | 1.0 |
| Intraoperative RBC transfusion, c n (%) | 7 (5.5) | 7 (6.0) | 0 (0) | NA |
| Cellsaver transfusion, mL, –mean ± SD | 322 (269) | 321 (270) | 333 (268) | .89 |
| Direct postoperative laboratory results d | ||||
| Hemoglobin, mmol/L, mean ± SD | 6.6 ± 0.9 | 6.6 ± 0.8 | 7.0 ± 1.0 | .10 |
| Hematocrit, L/L, mean ± SD | 0.32 ± 0.07 | 0.31 ± 0.07 | 0.33 ± 0.05 | .11 |
| Platelet count, ×103 per mm3, mean ± SD | 153 ± 40 | 153 ± 39 | 156 ± 51 | .82 |
Plus‐minus values are means ± SD.
Abbreviations: CABG, coronary artery bypass grafting; eGFR, estimated glomerular filtration rate; NA, not available; PCI, percutaneous coronary intervention; RBC, red blood cell; SD, standard deviation.
Defined as current smoker or quit smoking < 3 months.
Defined as diagnosis in medical history or low‐density lipoprotein ≥ 2.5 mmol/L, high‐density lipoprotein < 1.1 mmol/L, total cholesterol > 6.5 mmol/L, and/or triglycerides ≥ 2.2 mmol/L.
Defined as administered intraoperatively or <1 h after operation.
Defined as first lab results after CABG, in 90% of cases within 1 h after CABG.
3.2. Primary outcome
Mean blood loss 12 hours after CABG was 555 ± 278 mL in the aspirin‐sensitive group and 406 ± 110 in the aspirin‐resistant group (P = .04; Table 2, Figure 1). Individual ARU values and 12‐hour blood loss are plotted in Figure 2.
TABLE 2.
Primary and secondary outcomes regarding chest tube and total drain production over time
| Total population (N = 128) | Aspirin‐sensitive patients (N = 116) | Aspirin‐resistant patients (N = 12) | P value | |
|---|---|---|---|---|
| Chest tube production at 1 h after CABG, mL, mean ± SD | 103 ± 76 | 105 ± 78 | 78 ± 40 | .36 |
| Total drain production 1 h after CABG, mL, mean ± SD | 159 ± 121 | 163 ± 124 | 122 ± 81 | .40 |
| Chest tube production at 6 h after CABG, mL, mean ± SD | 375 ± 220 | 386 ± 226 | 265 ± 88 | .05 |
| Total drain production 6 h after CABG, mL, mean ± SD | 438 ± 239 | 451 ± 245 | 316 ± 114 | .06 |
| Chest tube production 12 h after CABG, mL, mean ± SD | 541 ± 271 | 555 ± 278 | 406 ± 110 | .04 |
| Total drain production 12 h after CABG, mL, mean ± SD | 615 ± 294 | 631 ± 302 | 458 ± 128 | .04 |
Plus‐minus values are means ± SD.
Abbreviation: CABG, coronary artery bypass grafting.
FIGURE 1.
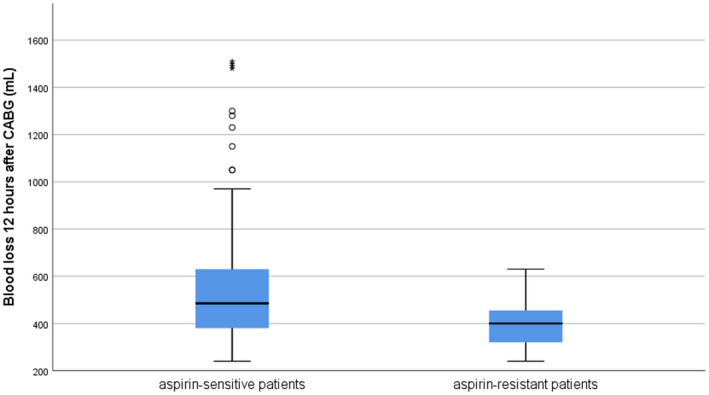
Boxplot of 12‐h blood loss after CABG by aspirin‐resistant or aspirin‐sensitive patients. The horizontal black line is the median value; boxes extend from the 25th to the 75th percentile of each group’s distribution of values; whiskers represent 1.5 times the interquartile range; dots denote outliers (observations outside the range of 1.5 times the interquartile range) and asterisks denote extremes (observations more than 3 times the interquartile range). CABG, coronary artery bypass grafting
FIGURE 2.
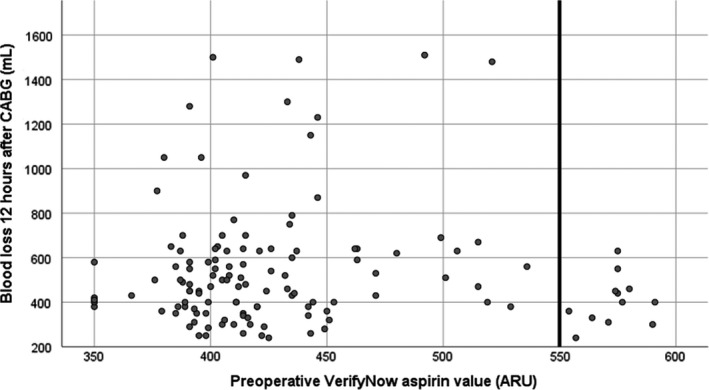
Scatterplot of 12‐h blood loss (mL) after CABG by individual ARU values. The vertical line at 550 ARU is the cutoff value for aspirin resistance. ARU, aspirin reaction units; CABG, coronary artery bypass grafting
3.3. Secondary outcomes
Total drain production at 12 hours was 631 ± 302 mL in the aspirin‐sensitive group and 458 ± 128 in the aspirin‐resistant group (P = .04). Results of chest tube and total drain production at 1 hour were comparable between aspirin‐resistant and aspirin‐sensitive groups. At 6 hours, both results of chest tube and total drain production differed between aspirin‐sensitive and aspirin‐resistant groups. All secondary outcomes rendered higher blood loss in the aspirin‐sensitive group (Table 2). In total, 15 patients (11.7%) experienced bleeding events during or up to 12 hours after CABG, 12 events were categorized as class 2 events and 3 events as class 3. All patients experiencing bleeding events were classified as aspirin sensitive.
4. DISCUSSION
This substudy of the POPular CABG randomized controlled trial investigated whether preoperative platelet function testing of aspirin responsiveness with the VerifyNow aspirin assay was associated with blood loss after CABG. We found a significant association between VerifyNow aspirin responsiveness and blood loss in patients who used aspirin preoperatively. In addition, all bleeding complications occurred in the aspirin‐sensitive group.
Some studies have investigated the relationship between aspirin responsiveness as measured with the VerifyNow aspirin assay and postoperative blood loss in cardiovascular surgical procedures. Takiuchi et al 19 enrolled 114 Japanese patients undergoing cardiac surgery, of which 30 underwent off‐pump CABG, of which 11 used only aspirin preoperatively (11 used aspirin + clopidogrel, 1 used aspirin + cilostazol, 1 used warfarin, 1 used aspirin + warfarin, and 4 used no antithrombotic medication). In these patients undergoing CABG, they established a weak inverse correlation (rS = −0.18), between preoperative ARU values and 24‐hour blood loss, but this was not significant, probably because of the small sample size. Welsh et al 20 retrospectively enrolled 88 patients that underwent cardiac surgery (12.5% CABG) and had VerifyNow aspirin testing. Of 88 patients in this study, 11 (12.5%) had significant bleeding during or after surgery. Five of these patients were aspirin sensitive (P = .32). VerifyNow ARU values for patients with significant bleeding did not significantly differ from patients without significant bleeding (546.5 ± 61.2 vs 519.1 ± 77.2). The study of Kim et al 21 prospectively included 220 aspirin‐taking patients undergoing elective off‐pump CABG. Patients who used other antiplatelet or anticoagulant medication were excluded from the study. The patients were divided in aspirin responders and aspirin nonresponders according to the VerifyNow aspirin assay. They identified 181 aspirin responders (82.3%) and 39 aspirin nonresponders (17.7%). Blood loss 12 hours after surgery, defined as the volume of the mediastinal and pleural chest tube drainage, did not differ between both groups (858 ± 530 mL in the aspirin‐responder group, 883 ± 474 mL in the aspirin‐nonresponder group, P = .52), nor did transfused packed red blood cells and the rate of reexploration for bleeding.
These results are not in line with the results of our study, as we can establish a significant difference when analyzing aspirin responders versus nonresponders. We can only speculate on the reasons why these studies do not demonstrate a relation between aspirin responsiveness and blood loss after cardiovascular surgical procedures.
First, the study of Takiuchi et al 19 is conducted in Japanese patients, and the study of Kim et al 21 is conducted in Korean patients, while our study population exists of European patients. These populations are not necessarily comparable. Vascular disease seems to manifest differently in Asians (higher stroke incidences but lower incidences of acute myocardial infarction). 22 Genetic differences may cause a dissimilar bleeding risk (and risk factors for bleeding) as well as changes in the aspirin metabolism, 23 as is the case with clopidogrel resistance. 24
Second, opposed to our study (>99% on‐pump surgery), the study population of Takiuchi et al 19 and Kim et al 21 consists of patients undergoing off‐pump CABG (the study of Welsh et al 20 does not comment on the type of CABG). Although the effect of off‐pump surgery on blood loss remains a topic for discussion, 25 , 26 the difference in thrombocyte (dys)function and (transient) aspirin resistance between on‐pump and off‐pump CABG might explain some of the discrepancies between the outcomes of our studies.
Finally, the study of Kim et al 21 is the only study that selected a similar study population with regard to preoperative antithrombotic and anticoagulation drugs (Welsh et al 20 do not mention preoperative medication use, and as mentioned the population of Takiuchi et al 1 differs in medication use). These other drugs might have influenced blood loss. Given our results, it could be proposed that preoperative testing of aspirin responsiveness might have value in predicting blood loss in patients undergoing cardiovascular surgical procedures who use aspirin preoperatively. Whether this difference in blood loss between aspirin‐sensitive and aspirin‐resistant patients is clinically meaningful can aid in determining the timing of surgery, 27 and whether classification according to aspirinresponsiveness with the preoperative VerifyNow aspirin assay can help identify patients undergoing CABG at risk for high blood loss and eventually could prevent bleeding events needs to be further investigated.
The following limitations should be considered. First, this is a relatively small study, with a small proportion of patients that were aspirin‐resistant. Second, no correction for the aforementioned other possible factors influencing blood loss was made. Therefore, it cannot be excluded that these factors influenced the results. Third, although results of the preoperative VerifyNow aspirin assay were unknown to all except the study team, blood transfusion management was left to the discretion of treating physicians, which could have influenced postoperative blood loss.
5. CONCLUSIONS
In patients who used aspirin preoperatively, aspirin responsiveness as classified by preoperative platelet function testing by the VerifyNow aspirin assay was associated with 12‐hour blood loss after CABG. Further investigation is needed to determine if and in which population preoperative VerifyNow aspirin testing can identify patients undergoing CABG at high risk for perioperative bleeding and whether this can prevent clinically relevant bleeding events.
AUTHOR CONTRIBUTIONS
LMW, PWAJ, E‐JvdD, CMH, and JMtB designed the study. LMW, EAV, and CDV collected study data. LMW, PWAJ drafted the manuscript. KZ and JCK supported the data analysis. PGN, PK, CMH, and JMtB supervised the study. All authors critically interpreted study data. All authors read and critically revised the manuscript and approved submission.
RELATIONSHIP DISCLOSURE
LMW was coordinating investigator of the POPular CABG trial, which was conducted with funding from AstraZeneca. PK declares consultancy and proctoring fees Edwards Lifesciences and BioVentrix Inc., and receiving a grant for conducting a clinical trial from Edwards Lifesciences, all unrelated to this work. JMtB reports institutional research grants from ZonMw (government institution) and AstraZeneca and being lecturer for AstraZeneca, Eli Lilly, Daiichi Sankyo, The Medicines Company, Accumetrics, Boehringer Ingelheim, BMS, Pfizer, Bayer, and Ferrer. EAV, PWAJ, CDV, KZ, JCK, PN, EJvdD, and CMH declare no conflicts of interest.
Supporting information
Supplementary Material
Willemsen LM, Vlot EA, Janssen PWA, et al. Blood loss after coronary artery bypass by aspirin responsiveness assessed with preoperative VerifyNow aspirin testing. Res Pract Thromb Haemost. 2021;5:e12623. doi: 10.1002/rth2.12623
Handling Editor: Dr Cihan Ay
Funding information
The POPular CABG trial was funded by AstraZeneca. AstraZeneca had no role in the study design, data collection, data analysis, data interpretation, or writing of the report of the trial or this substudy.
REFERENCES
- 1. Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2018;53(1):34‐78. [DOI] [PubMed] [Google Scholar]
- 2. Neumann F‐J, Sousa‐Uva M, Ahlsson A, et al. ESC/EACTS guidelines on myocardial revascularization. EuroIntervention. 2018;2019(14):1435‐1534. [DOI] [PubMed] [Google Scholar]
- 3. Hillis LD, Smith PK, Anderson JL, et al. 2011 ACCF/AHA guideline for coronary artery bypass graft surgery. J Am Coll Cardiol. 2011;58:e123‐e210. [DOI] [PubMed] [Google Scholar]
- 4. Mangano DT, Multicenter Study of Perioperative Ischemia Research Group . Aspirin and mortality from coronary bypass surgery. N Engl J Med. 2002;347:1309‐1317. [DOI] [PubMed] [Google Scholar]
- 5. Hastings S, Myles P, McIlroy D. Aspirin and coronary artery surgery: a systematic review and meta‐analysis. Br J Anaesth. 2015;115:376‐385. [DOI] [PubMed] [Google Scholar]
- 6. Ferraris VA, Ferraris SP, Joseph O, Wehner P, Mentzer RM. Aspirin and postoperative bleeding after coronary artery bypass grafting. Ann Surg Ann Surg. 2002;235:820‐827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ferraris VA, Ferraris SP, Lough FC, Berry WR. Preoperative aspirin ingestion increases operative blood loss after coronary artery bypass grafting. Ann Thorac Surg. 1988;45:71‐74. [DOI] [PubMed] [Google Scholar]
- 8. Sethi GK, Copeland JG, Goldman S, Moritz T, Zadina K, Henderson WG. Implications of preoperative administration of aspirin in patients undergoing coronary artery bypass grafting. Department of Veterans Affairs Cooperative Study on Antiplatelet Therapy. J Am Coll Cardiol United States. 1990;15:15‐20. [DOI] [PubMed] [Google Scholar]
- 9. Zimmermann N, Gams E, Hohlfeld T. Aspirin in coronary artery bypass surgery: new aspects of and alternatives for an old antithrombotic agent. Eur J Cardiothorac Surg. 2008;34:93‐108. [DOI] [PubMed] [Google Scholar]
- 10. Hovens MMC, Snoep JD, Eikenboom JCJ, van der Bom JG, Mertens BJA, Huisman MV. Prevalence of persistent platelet reactivity despite use of aspirin: a systematic review. Am Heart J. 2007;153:175‐181. [DOI] [PubMed] [Google Scholar]
- 11. Snoep JD, Hovens MMC, Eikenboom JCJ, van der Bom JG, Huisman MV. Association of laboratory‐defined aspirin resistance with a higher risk of recurrent cardiovascular events: a systematic review and meta‐analysis. Arch Intern Med. 2007;167:1593‐1599. [DOI] [PubMed] [Google Scholar]
- 12. Willemsen LM, Janssen PWA, Hackeng CM, et al. A randomized, double‐blind, placebo‐controlled trial investigating the effect of ticagrelor on saphenous vein graft patency in patients undergoing coronary artery bypass grafting surgery‐Rationale and design of the POPular CABG trial. Am Heart J. 2020;220:237‐245. [DOI] [PubMed] [Google Scholar]
- 13. Willemsen LM, Janssen PWA, Peper J, et al. Effect of adding ticagrelor to standard aspirin on saphenous vein graft patency in patients undergoing coronary artery bypass grafting (POPular CABG): a randomized, double‐blind, placebo‐controlled trial. Circulation. 2020;142:1799‐1807. [DOI] [PubMed] [Google Scholar]
- 14. San Diego CA . VerifyNow aspirin Test [package insert]. Revis April 2011.
- 15. Breet NJ, van Werkum JW, Bouman HJ, Kelder JC, Ten Berg JM, Hackeng CM. High on‐aspirin platelet reactivity as measured with aggregation‐based, cyclooxygenase‐1 inhibition sensitive platelet function tests is associated with the occurrence of atherothrombotic events. J Thromb Haemost. 2010;8:2140‐2148. [DOI] [PubMed] [Google Scholar]
- 16. Gurbel PA, Bliden KP, DiChiara J, et al. Evaluation of dose‐related effects of aspirin on platelet function: results from the Aspirin‐Induced Platelet Effect (ASPECT) study. Circulation. 2007;115:3156‐3164. [DOI] [PubMed] [Google Scholar]
- 17. Chen W‐H, Cheng X, Lee P‐Y, et al. Aspirin resistance and adverse clinical events in patients with coronary artery disease. Am J Med. 2007;120:631‐635. [DOI] [PubMed] [Google Scholar]
- 18. Dyke C, Aronson S, Dietrich W, et al. Universal definition of perioperative bleeding in adult cardiac surgery. J Thorac Cardiovasc Surg. 2014;147:1458‐1463.e1. [DOI] [PubMed] [Google Scholar]
- 19. Takiuchi H, Tanemoto K. Optimal timing of clopidogrel discontinuation in Japanese patients: platelet aggregation test using the VerifyNow® system. Gen Thorac Cardiovasc Surg. 2015;63:601‐606. [DOI] [PubMed] [Google Scholar]
- 20. Welsh KJ, Dasgupta A, Nguyen AND, Wahed A. Utility of VerifyNow for point‐of‐care identification of an aspirin effect prior to emergency cardiac surgery. Ann Clin Lab Sci. 2015;45:377‐381. [PubMed] [Google Scholar]
- 21. Kim HJ, Lee J‐M, Seo JH, et al. Preoperative aspirin resistance does not increase myocardial injury during off‐pump coronary artery bypass surgery. J Korean Med Sci. 2011;26:1041‐1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ueshima H, Sekikawa A, Miura K, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008;118:2702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Gao R, Li X. Risk assessment and aspirin use in Asian and Western populations. Vasc Health Risk Manag Dove Press. 2010;6:943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hasan MS, Basri HB, Hin LP, Stanislas J. Genetic polymorphisms and drug interactions leading to clopidogrel resistance: why the Asian population requires special attention. Int J Neurosci. 2013;123:143‐154. [DOI] [PubMed] [Google Scholar]
- 25. Johansson‐Synnergren M, Nilsson F, Bengtsson A, Jeppsson A, Wiklund L. Off‐pump CABG reduces complement activation but does not significantly affect peripheral endothelial function: a prospective randomized study. Scand Cardiovasc J. 2004;38:53‐58. [DOI] [PubMed] [Google Scholar]
- 26. Ascione R, Williams S, Lloyd CT, Sundaramoorthi T, Pitsis AA, Angelini GD. Reduced postoperative blood loss and transfusion requirement after beating‐heart coronary operations: a prospective randomized study. J Thorac Cardiovasc Surg. 2001;121:689‐696. [DOI] [PubMed] [Google Scholar]
- 27. Bolliger D, Lancé MD, Siegemund M. Point‐of‐care platelet function monitoring: implications for patients with platelet inhibitors in cardiac surgery. J Cardiothorac Vasc Anesth. 2021;35:1049‐1059. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


