Abstract
This narrative reviews the history and evolution of surgical training in Southwest Michigan, particularly Kalamazoo, over the past 100 years. During this time, the de novo growth of medical treatment and the gradual and progressive establishment of medical and surgical training, paralleled with innovation, have shaped the clinical practices in Southwest Michigan. The surgical expertise that exists in Kalamazoo has made it one of the most important headquarters for surgical innovation, not only in the United States, but in the world. The surgical training program in Kalamazoo began in the 1960s, and this accredited general surgery residency program has graduated numerous successful surgeons. Currently this program is one of several training programs at Western Michigan University Homer Stryker M.D. School of Medicine (WMed), the only medical school in Southwest Michigan. Under the leadership of Dean Surgeon Dr. Paula Termuhlen and Chair Dr. Robert Sawyer, a bright future in surgical education, research, and innovation is highly anticipated. Expectations of future growth in this program will provide a significant pipeline for graduating physicians and surgeons for decades to come.
Keywords: Surgery history, Surgical training in Kalamazoo, Stryker, History of medicine
1. The birth of medical treatment and innovation in Kalamazoo
Medical progress and innovation are an important part of the culture of Kalamazoo, Michigan. Starting in 1875, W.E. Upjohn ushered the pharmaceutical industry into the modern era here in Kalamazoo [1]. Homer Stryker, M.D., established his renowned medical device company in Kalamazoo in 1941 [2], revolutionizing many medical instruments and treatments. The Kellogg family pioneered new medical treatments, and, of course, Corn Flakes®, in nearby Battle Creek beginning in the 1860s [3]. Together the contributions of these entrepreneur-philanthropists have helped millions since.
Prior to the Civil War, medicine was largely provided in the home by family and neighbors. During the modern era of medicine dating from the end of the Civil War, Kalamazoo institutions had the commitment and vision to provide state-of-the-art medical care to the community. In addition to providing first-class medical care, Kalamazoo leaders demonstrate investment in patients of the present and future by facilitating the training of doctors, nurses, and a myriad of other healthcare providers.
2. Introducing specialties and surgical care to Kalamazoo
By the late 19th century, due to the advent of antiseptics, ether, anesthesia, and surgical innovation, medical care transitioned to become hospital based. In Kalamazoo, this trend was adopted with some trepidation at first. However, funding became available for the establishment of Borgess Hospital in 1889 and, soon after, Kalamazoo Hospital in 1900. Kalamazoo Hospital quickly became Bronson Hospital with the opening of its new facility in 1907 (Fig. 1A, Fig. 1BA and B, Fig. 2) [4,5].
Fig. 1A.
Kalamazoo Hospital 1905 (predecessor to Bronson Hospital) [Source: Local History collection, Kalamazoo Public Library, Michigan].
Fig. 1B.
Bronson Methodist Hospital 1949 [Source: Local History collection, Kalamazoo Public Library, Michigan].
Fig. 2.
Borgess Hospital, Gull Road, 1917 [Source: Local History collection, Kalamazoo Public Library, Michigan].
After the establishment of these two hospitals, newer techniques and services were quickly adopted in Kalamazoo. Dr. August Crane and others brought the budding specialty of radiology and radiotherapy to Kalamazoo, just 16 months after Dr. Roentgen described the technology and procedures. They formed what became the first radiology practice in the United States [[6], [7], [8]]. Dr. Homer Stryker, an MD graduate from the University of Michigan Medical School in 1925, began his medical practice in Kalamazoo, Michigan, and established offices in Borgess Hospital, where he was the only orthopedic surgeon in the region (Fig. 3). Dr. Stryker became an inventor, businessman, and subsequently the founder of the Stryker Corporation. Headquartered in Kalamazoo even today, Stryker remains one of the world's leading medical technology companies, offering innovative products and services in Orthopaedics, Medical and Surgical, as well as Neurotechnology and Spine that help improve patient and hospital outcomes [2,9].
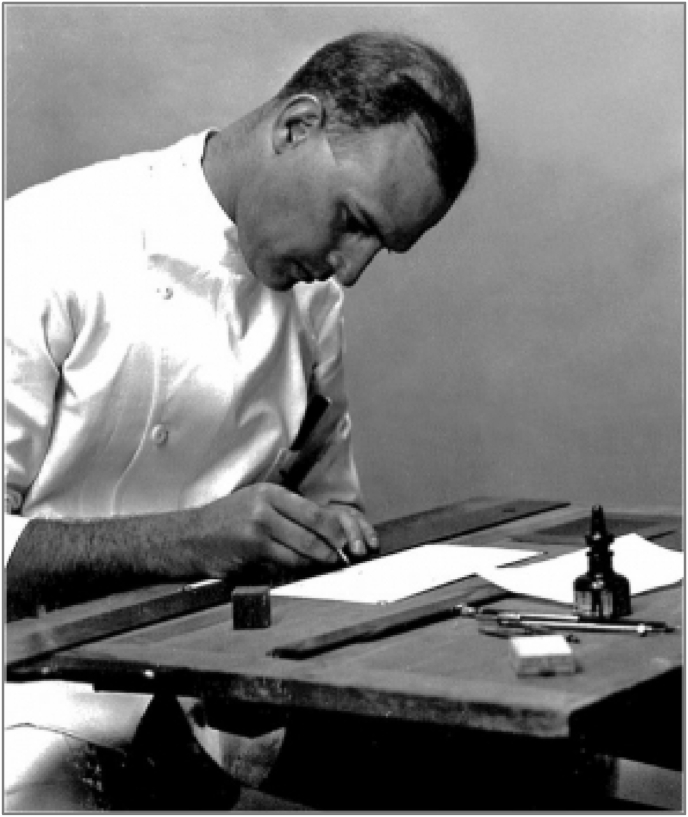
Fig. 3.
Dr. Stryker, orthopaedic surgeon and inventor works on research and development of surgical instruments [Source: Stryker Corporation].
The surgical services offered in Kalamazoo rapidly expanded with the recruitment of several pioneer surgeons. In the 1930s, Dr. Richard Upjohn Light established the first neurology/neurosurgery outpatient center at Borgess Hospital [4]. In 1956, Bronson opened a cardiac catheterization unit, and in 1968, the first cardiac intensive care unit (ICU) was opened at Borgess [4,5]. In 1966, Martin Verzi, a retired veteran, was employed by Borgess and championed dramatic changes in the hospital's philosophies. He recruited a neurosurgical specialist from Mayo Clinic. Additionally, Dr. William Behrje joined Dr. John Kostin, as the only general surgeons at Borgess at that time. Borgess established a kidney transplant program in 1971 and in November of that year performed their first kidney transplant operation. Shortly after, the first open cardiac surgery was performed at Borgess in January 1972 [4]. To facilitate the development of a trauma program, the first helicopter program in Michigan was designed by Borgess. This service was delayed due to a dispute with the University of Michigan but was later approved. Thus began the “helicopter wars” of Kalamazoo, as Bronson purchased Pumpkin Air and began flying throughout southwest Michigan to advance its cardiac and trauma programs.
3. Surgical residency programs in Kalamazoo
The initial medical trainees in Kalamazoo were fellows and residents who trained in an internal medicine internship and residency established at Bronson Methodist Hospital in 1946 followed in 1947 at Borgess with a rotating internship. Then in 1947 medical students from the University of Michigan began training at Bronson. These residency training and fellowship programs were funded via grants from the Upjohn and Kalamazoo Foundations [5]. Soon afterward, an orthopaedic surgery residency was established, leading to the first Kalamazoo-wide residency program as a collaboration between Bronson and Borgess in 1966 [10]. This quickly became a nationally renowned training program. Subsequently, Bronson established free-standing resident training programs in internal medicine, pediatrics, and general surgery in addition to the orthopedic program. The most notable graduate of the surgery program in that era was Dr. Konrads Lubavs, who settled in Kalamazoo and practiced surgery until his death in 2018 at the age of 86. Dr. Paul Fierke and Dr. James Hollinger were the last graduates of the program in 1974.
Armed with the success of the combined orthopaedic surgery program, Borgess and Bronson formed the Southwestern Michigan Area Health Education Center (SMAHEC) in 1973 [10]. The first interns of the combined 4-year program were Drs. James Heersink and Richard Jefson, under the directorship of Dr. James Kilway. They graduated in 1976, going on to serve the Kalamazoo community with quality surgical care for many years, in addition to their roles in resident education. Dr. Heersink died in 1996. The residency program honored him with an award in his name for “Excellence in Teaching” presented every year to a member of the faculty. Dr. Jefson retired in 2016, after more than 4 decades of surgical practice and dedication to teaching surgery residents in Kalamazoo.
The Medical Director of SMAHEC was Dr. Robert Nicholson, who strove to keep the program independent of any university affiliation, despite the fact that Michigan State University (MSU) had recently started a new medical school and sought collaboration for the training of its students in Kalamazoo. The independent surgery programs were incorporated into SMAHEC during the 1976-77 academic year. Dr. James Kilway was the Program Director from 1976 to 78, followed by Dr. Richard Schloemer from 1978 through 1984. The surgery program graduated two residents per year until the institution lost accreditation in 1989 [10].
In 1981, Dr. John Collins joined Borgess as a general and vascular surgeon, and Dr. Krishna Jain, a vascular surgeon who also served as the director of surgical research in Kalamazoo for SMAHEC and later for Michigan State University – Kalamazoo Center for Medical Studies between 1993 and 1998.
SMAHEC was an important step in the advancement of medical and surgical education in Kalamazoo. Unfortunately, it was born during an age of markedly increased scrutiny of medical training programs. In October of 1984, Libby Zion an 18-year-old college student was admitted to a New York hospital with flu-like symptoms. Her story was one of the most publicized cases of death due to medical error of the time, having received medication for treatment of her fever and rigors that interacted with another medication she was taking. Entire forests have been felled to provide the paper on which articles have been written about this case. Here is a brief quote (from the internet, no tree was harmed by quoting this article):
Sidney Zion, the father of Libby Zion, was a wealthy and powerful attorney. He was also a former writer for the New York Times. He insisted that his daughter had died due to overwork and a lack of supervision of these young doctors ….Zion indicted the entire medical training system for his daughter's death. [11].
This began a trying time for medical training and resulted in the critical examination and reshaping of residency programs across the United States.
4. University affiliation
The major upheaval in the rules regarding medical training, a site visit by an irascible representative of the surgery Residency Review Committee (RRC), and SMAHEC's steadfast resistance to an academic affiliation ultimately led to the loss of accreditation of the surgery program, along with the dissolution of the SMAHEC. The one remaining exception was the orthopaedic surgery residency which was never cited and remained viable throughout the transition. The senior residents in these no-longer-accredited programs were allowed to complete their training in Kalamazoo, but no new residents were accepted. Two notable contributors to the legacy of Kalamazoo surgery were junior residents at the time, Drs. Nancy Kalinowski and Daniel Stewart. Both started residency in 1985 under the guidance of Dr. Robert Hume (3rd PD) and eventually under Dr. James Babel. In 1988 when the surgery program lost its accreditation, these residents were forced to find other programs. Dr. Stewart completed his training at MSU's Flint program, while Dr. Kalinowski finished at MSU in Grand Rapids before both returned to Kalamazoo to start very successful careers.
A new consortium was formed in 1992 by Borgess, Bronson, and Michigan State University (MSU), leading to the development of the Michigan State University/Kalamazoo Center for Medical Studies (MSU/KCMS). MSU would provide the academic affiliation for all of the Kalamazoo residency programs with the chair of each program residing in East Lansing. Kalamazoo would serve as one of many sites available for medical students to train during their clerkship experiences. The residency programs in Kalamazoo were directed by Kevin Fickenscher, MD, of North Dakota, who was hired as the assistant dean and president/CEO of Michigan State University/Kalamazoo Center for Medical Studies, one of six campuses for the MSU College of Human Medicine. The facility that houses the residency offices and clinics was not completed until 1994. Dr. Luis Toledo, a transplant surgeon employed by Borgess until their transplant program was closed in 1996, was hired by MSU/KCMS and ran the research sciences and molecular biology program from 1998 until his retirement in 2016. The surgery program director was Dr. Duane Freier, a surgeon with strong ties to University of Michigan. He brought along a young, very accomplished University of Michigan graduate, Dr. Michael McLeod. Together they formed a strong residency program and graduated the first two residents of the program, Drs. Sean O'Brien and Jamal Mahdavvian, in 1997 (Fig. 4). Dr. O'Brien completed a vascular fellowship at Hahnemann University in 1999 and was recruited to join the general and vascular surgery practice at Borgess Medical Center, teaming up with Drs. John Collins and James McLaren. Today, he remains a very busy surgeon in the community.
Fig. 4.
MSU/KCMS General Surgery Residency graduation (1997 Class)
Left to Right: Willam Behrje, Richard Jefson, Dick Hodgman, Stuart Bussle (PGY2), Paul Albear (R4), Jamal Mahdavian (R5), Jim Kilway II (R2), Sean O'Brien (R5), Brian Anderson (R3), Doug Cummins (R3), Duane Frier, Jim Kilway, Karen Draper (R4), Michael McLeod, Chuck Black (R3), Gus Roty, John Kostin. (Source: Courtesy of Dr. Sean O'Brien).
The program was accredited to graduate two residents per year and staffed both Bronson and Borgess hospitals (approximately 800 certified beds), exposing its trainees to a tremendous breadth and depth of surgical procedures and experiences. Notable volunteer faculty were the aforementioned Drs. Collins and McLaren, along with Drs. James Babel, Harold D Friedl, Daniel Stewart, and Thomas Rohs who were physicians at Borgess. From Bronson, Drs. Scott Davidson, Mark Dittenbir, Mark Tagett, and Stephen Wysong generously gave their time.
5. New Era in 21st century
Before his retirement from MSU/KCMS in 2000, Dr. Freier served as the president of the Michigan Chapter of American College of Surgeon (1999–2000). Dr. McLeod was then appointed as the new program director. This was a challenging time due to the implementation of the new Accreditation Council on Graduate Medical Education (ACGME) duty-hour rules. These rules were implemented in July 2003 with the goal of reducing the risk of adverse events resulting from sleep deprivation and to enhance residents' well-being. Dr. McLeod, among all of the other program directors across the country, had to interpret and implement very stringent and seemingly arcane rules to maintain accreditation. Many programs were placed on probation during this time period, including MSU/KCMS's surgical residency. Dr. McLeod navigated these hurdles deftly while maintaining a very high level of surgical training for the graduating chief residents and ultimately transitioned the program into good standing with the ACGME. Dr. McLeod recruited Dr. Alan Saber as full-time faculty in 2002. Dr. Saber was the first surgeon in Southwest Michigan to establish a bariatric surgery program and performed the first Roux-en-Y gastric bypass here in 2004. As a chair of surgery department, Dr. McLeod also served as the president of the Michigan Chapter of the American College of Surgeon (2008–2009). He would continue to grow this program until his departure in 2010. In addition, Drs. James Kilway and August Roty were recruited from private practice to join the program in 1998. They provided much assistance to the program. Dr. Roty passed away in 2004 after a prolonged battle with cancer. Dr. Kilway retired from surgery in 2004. Dr. McLeod recruited Dr. Robert Osmer to join the program in 2004 from private practice and successfully recruited Dr. Earl Norman later that year. In 2008, Dr. Christian Ertl joined MSU/KCMS and initially served as the M4 clerkship director for MSU students rotating in Kalamazoo. Dr. Sheldon Maltz, a trauma surgeon at Bronson Methodist Hospital, served as the M3 clerkship director for MSU students in Kalamazoo between 2006 and 2014.
Dr. McLeod was recruited to lead the Michigan State surgical residency program in East Lansing in 2009, at which time Dr. Norman was appointed program director of the MSU/KCMS surgical residency. In 2010 Drs. Saad Shebrain, a surgeon trained in advanced laparoscopic and foregut surgery, and Lisa Miller, a general surgeon, joined the full-time faculty. Dr. Norman advanced the residency program further, and integrated the Surgical Council on Resident Education (SCORE®) curriculum into the educational didactics of the program. He also established a formal bioskills curriculum including dry lab, virtual reality (VR), cadaver and animal platforms, and established reciprocal operating room evaluations. In 2011, the program was granted a complement increase and became accredited to graduate three residents per year. Dr. Norman subsequently was named chair of the Department of Surgery, during which time he founded the surgical oncology program in Kalamazoo in collaboration with West Michigan Cancer Center (WMCC). In 2013, Dr. Shebrain was appointed to associate program director.
In 2007, John Dunn became the President of Western Michigan University (WMU). At that time, he set a goal to establish a medical school in Kalamazoo allied with WMU, a goal that initially seemed to be unattainable. However, with equal parts planning, cajoling, and generosity among many civic, medical, academic, and business leaders in Kalamazoo, the Western Michigan University Homer Stryker M.D. School of Medicine (WMed) was established in 2012, under the leadership of Founding Dean, Dr. Hal Jenson. WMed confers the Doctor of Medicine (MD) degree, as well as Master of Science in Biomedical Sciences and Medical Engineering. WMed is a collaboration between Western Michigan University and Kalamazoo's two teaching hospitals, Ascension Borgess (formerly Borgess Health) and Bronson Healthcare. The inaugural class of 54 students started in August 2014 [10]. This caused many changes in the structure and governance of the residency training programs. For example, all program directors were appointed as chairs of their respective departments. In 2015, Dr. Shebrain was appointed to program director, and Dr. Lisa Miller became the M3 clerkship director. With the ascent of the new medical school to support surgical training in Kalamazoo, MSU/KCMS was disbanded and the association with MSU's College of Human (allopathic) Medicine was diminished. Fig. 5 shows the general surgery residency program leadership over the last fifty years. Fig. 6 demonstrates the timeline of surgical practice and training in Kalamazoo over the last hundred years.
Fig. 5.
Surgery Program leadership (1973–2021)
From left to right: James Kilway, MD (1973–1978), Duane Freier, MD (1993–2000), Michael McLeod, MD (2000–2009), Earl Norman, MD (2009–2015), Saad Shebrain, MD (2015-current).
Fig. 6.
Evolution timeline of medicine and surgical practice and training in Kalamazoo, Michigan, U.S.A.
Simulation in medical education was introduced early into surgery training in Kalamazoo, more than 20 years ago. In 2007, the da Vinci Surgical System was brought to the Kalamazoo community by both Borgess Medical Center and Bronson Methodist Hospital. Since then, it has been widely implemented in many specialties, including urology, gynecology, general surgery, and thoracic surgery. Robotics has become standard in many residency programs. With the establishment of WMed, the development of a state-of-the-art simulation center has played a pivotal role in training hundreds of medical students, residents, and other healthcare providers. At WMed, surgical residents have access to the da Vinci technology in both the simulation center and the operating room. The most advanced Xi Robot with the dual console is currently available for training residents with a structured curriculum in place.
6. New leadership and empowering future surgical education
A new chair of surgery, Dr. Robert Sawyer, a professor of surgery and medical engineering, joined the department in 2017, after his distinguished service as professor of surgery and a pioneer in surgical infection research and nutrition at the University of Virginia from 2008 to 2017. Drs. Sawyer and Shebrain bring a high quality of training and a great deal of research experience to the department and the school. WMed is committed to diversity; the general surgery residency program currently has an equal number of male and female residents. Over the last four years, the general surgery residency program has expanded and currently is accredited by the ACGME for five residents per year, with one position designated for the rural track through the Michigan Doctors (MIDOCs),a program designed to recruit, train, and retain physicians serving in rural and underserved areas of Michigan [12].
Nearly all of the graduates interested in further fellowship training (65%–75%) matriculate to competitive fellowship opportunities of their choosing. The rest (25%–35%) go to private practice, with 15–30% of them returning to serve in Kalamazoo community.
In May 2021, Paula M. Termhulen, MD, FACS, became the new dean of WMed. Before coming to WMed, Dr. Termuhlen was a professor of surgery, surgical oncologist, and regional dean for the Duluth campus at the University of Minnesota Medical School. She previously served as a general surgery residency program director at Wright State University and the Medical College of Wisconsin. She was also vice-chair of the Department of Surgery at Wright State University. While at the Medical College of Wisconsin, Dr. Termhulen was president of the Association of Program Directors in Surgery and an inaugural member of the Academy of Master Surgeon Educators (Fig. 7A, Fig. 7B).
Fig. 7A.
New leadership in the department of Surgery
Robert sawyer, MD, department chair (2017-current).
Fig. 7B.
New leadership in the department of Surgery
Dean Paula Termuhlen, MD, Western Michigan University Homer stryker M.D. School of medicine.
On June 8, 2021, Western Michigan University was the recipient of the largest private gift to a public university ever in US history ($550 M), with $300 M allocated to Western Michigan University Homer Stryker M.D. School of Medicine. As our medical school progresses under the new leadership of Dr. Termuhlen, the Department of Surgery will continue to grow and invest in surgical education and research. However, our primary mission to graduate excellent, skilled surgeons will remain the focus, advancing in tandem with innovation and discovery in surgery for the foreseeable future.
Ethical approval
No patients were involved in this manuscript and therefore no need for ethical approval.
Source of funding
None.
Author contribution
Study conception and design: Shebrain, Swayer. Acquisition of data: Norman, Shebrain. Analysis and Interpretation of data: Shebrain, Norman. Drafting of Manuscript: Norman, Shebrain, Cookenmaster, Ferrin. Critical revision: Shebrain, Sawyer.
Consent
As stated in “Ethical Approval”: Informed consent was not necessary. No protected health information or other uniquely identifying information is included in this manuscript.
Registration of research studies
1. Name of the registry:
2. Unique Identifying number or registration ID:
3. Hyperlink to your specific registration (must be publicly accessible and will be checked):
Guarantor
Saad Shebrain, MBBCh, MMM, FACS.
Address:
Department of Surgery.
Western Michigan University Homer Stryker MD School of medicine.
1000 Oakland Drive, Kalamazoo, MI 49008.
Emil: saad.shebrain@med.wmich.edu.
Tel: 269-337-6260.
Provenance and peer review
Not commissioned, externally peer reviewed.
Declaration of competing interest
The authors have no conflicts of interest to disclose.
Acknowledgment
The authors would like to thank Drs. John Collins, Richard Jefson, Thomas Rohs, William Behrje, Sean O'Brien, Daniel Stewart, and Krishna Jain for their contribution to this article and for providing thoughtful feedback from their decades of surgical experience in the Kalamazoo community. The authors would like to thank Elizabeth Lorbeer and Ann Harris in the Department of Library at WMed, and Dr. Laura Bauler in the Department of Medical Education for their input during this manuscript preparation.
References
- 1.Funding Universe The Upjohn company history. http://www.fundinguniverse.com/company-histories/the-upjohn-company-history/
- 2.Stryker Corporation Our history. 2021. https://www.stryker.com/us/en/about/history.html
- 3.Kellogg’s Our history: from feeding the US Army to going to the moon to making everyday moments G-r-r-r-eat! 2021. https://www.kelloggs.com/en_US/who-we-are/our-history.html
- 4.Kalamazoo Public Library Borgess Hospital: Kalamazoo's first hospital. 2010. https://www.kpl.gov/local-history/kalamazoo-history/health/borgess/
- 5.Kalamazoo Public Library Bronson methodist hospital. 2009. https://www.kpl.gov/local-history/kalamazoo-history/health/bronson-methodist-hospital/
- 6.Western Michigan University Archives & Regional History Collections Caroline bartlett Crane collection, RH-A-92. https://aspace.library.wmich.edu/repositories/3/resources/118
- 7.Western Michigan University Libraries . Everyman's House; 2021. Caroline bartlett Crane collection.https://cdm16259.contentdm.oclc.org/digital/collection/p4022coll10 [Google Scholar]
- 8.Kalamazoo Area Medical Alliance History & mission. 2019. https://www.kalamazooama.org/history-mission
- 9.Stryker Corporation Our company. 2021. https://www.stryker.com/us/en/about.html
- 10.Wikipedia Western Michigan university homer stryker M.D. School of medicine. 2021. https://en.wikipedia.org/wiki/Western_Michigan_University_Homer_Stryker_M.D._School_of_Medicine [DOI] [PubMed]
- 11.The Knope Clinic October 4, 1984 & Libby Zion: the day medicine changed forever. 2019. https://conciergemedicinemd.com/october-4-1984-libby-zion-the-day-medicine-changed-forever/
- 12.MIDOCs https://www.michigandocs.org/