Abstract
Background
Hydrocolloid dressings (HCD) are helpful in chronic wound care, but research is limited in acute postoperative wounds. HCD can potentially be incorporated into a simplified wound care regimen after excisional surgeries.
Objective
To examine whether a one-time HCD application after dermatologic surgery results in greater patient satisfaction and improved postoperative outcomes compared with conventional daily dressings (CDD).
Methods
We examined patients who underwent Mohs or standard surgical excision with linear closure followed by HCD. The patients additionally had a history of excisional surgery with CDD in the past 5 years. A modified version of the validated Bluebelle Wound Healing Questionnaire was administered.
Results
The survey response rate was 74.4% (64/86). Compared with CDD, HCD rated higher in comfort, convenience, scar appearance, and simplicity of wound care instructions (P < .0001). Nearly all patients (96.8%) preferred HCD over CDD.
Limitations
Variability in time from prior dermatologic surgery may introduce recall bias. Prior surgeries involving CDD were sometimes performed by a different surgeon, which could introduce other confounding factors.
Conclusions
A simplified wound care regimen involving HCD can potentially lead to increased comfort, convenience, simplicity, and a subjective improvement in scar appearance, though additional studies are needed.
Key words: DuoDERM, excision, general dermatology, healing, hydrocolloid dressing, Mohs micrographic surgery, postoperative, surgery, wound care
Abbreviations used: CDD, conventional daily dressing; HCD, hydrocolloid dressing
Capsule Summary.
-
•
Hydrocolloid dressings are beneficial for healing chronic wounds, but research is limited for use in acute postoperative wounds in dermatology.
-
•
Hydrocolloid dressings may offer benefits beyond wound healing, including increased comfort, convenience, subjective improvement in scar appearance, and simplicity of wound care instructions, though further study is needed.
Introduction
Dermatologists performed nearly 14 million procedures in 2019 alone, a 78% increase from the year 2012.1 Between 2006 and 2012, the number of procedures for nonmelanoma skin cancer increased by an estimated 14% while procedures for melanoma increased by 77%.1,2 These numbers are likely to continue to rise with the aging population and increasing rates of skin cancers. The postoperative period plays an important role in overall patient satisfaction after dermatologic surgeries. The rising number of dermatologic procedures makes it more imperative for us to address the issue of postoperative wound care.
In terms of postoperative wound care, most of the prior research pertains to the postsurgical use of topical medications and oral antibiotics.3,4 There is a lack of evidence about wound care dressings after dermatologic surgery. Historically, conventional daily dressings (CDD) have consisted of layered ointments and nonadherent, absorbent, contouring, or compressive dressings.5 Many of these dressings require time-consuming daily changes and topical emollient reapplication. More recently, innovative dressings such as silicone gels, collagen films, and hydrocolloids have been suggested to be beneficial in wound healing because of their antimicrobial properties, insulation, and impermeability.5,6 In particular, hydrocolloid dressings (HCD) have been used for decades to assist in the healing of chronic wounds such as leg ulcers and pressure sores.6 A meta-analysis in 2003 found that 72% more ulcers healed completely with the use of HCD compared with CDD.6 Hydrocolloids have also demonstrated utility in the treatment of keloids and hypertrophic scars and have been shown to act as a barrier by maintaining skin integrity and preventing chronic irritation related to surgical and N95 face masks.7, 8, 9, 10
While the exact mechanism by which HCD facilitates wound healing remains under investigation, the prevailing hypothesis suggests a multifactorial effect involving the stimulation of fibroblasts, epidermal cell turnover, moist environment, and impermeability to bacteria.6 Despite this abundant data showing potential benefits of HCD in wound care, there is limited research documenting the use of HCD on surgical sites after dermatologic procedures.11, 12, 13
To the best of our knowledge, no study has ever assessed the benefit of HCD as a wound care dressing after excisional procedures in dermatology. To date, the use of HCD remains limited in our specialty. This study aims to evaluate whether using a simplified wound care regimen involving a one-time application of HCD after surgery shows superior or equivalent outcomes to CDD with regard to 4 primary outcome measures: comfort, convenience, scar appearance, and simplicity of wound care instructions. Any associations between wound care dressings and the 4 outcomes were controlled for possible confounders, including age, sex, surgical site, repair complexity, operating surgeon, and availability of assistance with wound care. The secondary aim is to determine the safety of HCD use compared with CDD.
Methods
Participants and study design
Inclusion criteria consisted of adult patients 18 years of age who underwent Mohs micrographic surgery or standard surgical excision with linear repair from January 2020 to January 2021, resulting in a one-time application of HCD for one week after the surgery. Eligible patients additionally had a history of at least one excisional surgery with CDD within the last 5 years. Finally, patients had a reliable and correct contact method, such as phone number or email address, located within their electronic medical record.
Exclusion criteria included non-English speaking patients or those who could not respond to the survey because of cognitive disability. Patients who received repairs consisting of grafts or flaps, repairs on acral or hair-bearing sites, and those with a history of allergy to adhesives were all excluded.
Each eligible participant had experience with both HCD and CDD and was therefore used as an internal control to compare patient satisfaction and patient-reported outcomes associated with the 2 types of wound care dressings.
The study was evaluated and granted institutional review board exemption by the Indiana University Human Research Protection Program office.
Objectives
The main objective of the study was to determine whether a wound care regimen involving a one-time application of HCD resulted in greater patient satisfaction in terms of comfort, convenience, scar appearance, and simplicity of wound care instructions compared with standard wound care with CDD. The secondary objective was to determine the safety of HCD compared with CDD.
Data collection and statistical analysis
Baseline sociodemographic data were collected, along with dermatologic surgery history, including surgical site, diagnosis, repair type, and wound dressing. If available, these data were also collected for previous excisions performed in the past 5 years. A modified version of the validated Bluebelle Wound Healing Questionnaire was used to evaluate patient-reported postoperative complications related to infection and wound dehiscence.14 Additional questions were created to assess patient-reported satisfaction and overall experience with HCD versus CDD. Survey data were stored in RedCap.
Generalized linear models using the Poisson distribution and a log-link function for analysis were performed to determine patient rating differences between HCD and CDD, controlling for sex, age, surgical site, repair complexity, operating surgeon, and availability of assistance with wound care. The results were then exponentiated back into their original scale. Unadjusted and multivariate models assessed the patient ratings associated with the 4 primary outcomes: (1) convenience, (2) comfort, (3) scar appearance, and (4) simplicity of wound care instructions. Any demographic or clinical variable with P < .20 was included in the multivariate model. Statistical significance for the final models was set at P < .05. Statistical analyses were performed using SAS v9.4 (SAS Institute).
Results
Study population
Demographics of the survey participants and characteristics of the surgeries preceding the use of wound dressings are depicted in Table I. In total, 64 (74.4%) of the 86 patients contacted completed the survey. The mean time from recent surgery to survey completion was 237.4 days (range, 95 to 462 days), and the meantime from current to previous surgery was 571.5 days (range, 12 to 2393 days). The mean age was 65 years (54.7% men). At the time of surgery, 28 (43.8%) participants were retired. Thirty-three (51.6%) patients had both the surgical procedures with HCD and CDD completed by the same surgeon (SKQ). Fifty-one (79.7%) patients performed wound care at home without assistance from a relative or other person. Mohs micrographic surgery preceded wound care in 49 (76.6%) cases, and a standard surgical excision was performed in 15 (23.4%) cases. Current and previous surgery type was matched in 31 (44.9%) cases. Forty-two (65.5%) surgeries involved the head and neck region. Current and previous surgeries were located on the same anatomical site in 25 (36.2%) patients. Intermediate repair was used in 45 (70.3%) cases.
Table I.
Demographics of survey participation (n = 64) and characteristics of surgeries preceding use of wound dressing
| No. of respondents (%) | |
|---|---|
| Age, mean (SD); range | 65.19 (13.93); 32-93 |
| Sex | |
| Female | 29 (45.3) |
| Male | 35 (54.7) |
| Job status at the time of surgery | |
| Working in an office | 22 (34.4) |
| Traveling for work | 3 (4.7) |
| Working from home | 10 (15.6) |
| Retired | 28 (43.8) |
| Family caregiver | 1 (1.6) |
| Wound care at home | |
| Performed without assistance | 51 (79.7) |
| Had assistance from another person | 13 (20.3) |
| Diagnosis of lesion | |
| Basal cell carcinoma | 37 (57.8) |
| Squamous cell carcinoma | 15 (23.4) |
| Other | 12 (18.8) |
| Surgical site | |
| Head/neck | 42 (65.6) |
| Other | 22 (34.4) |
| Type of surgery | |
| Mohs micrographic surgery | 49 (76.6%) |
| Standard excision | 15 (23.4%) |
| Repair type | |
| Intermediate | 45 (70.3) |
| Complex | 19 (29.7) |
| Surgeon for prior excisional surgery in the last 5 years | |
| SKQ | 33 (51.6) |
| Other | 31 (48.4) |
Patient satisfaction and safety of dressings
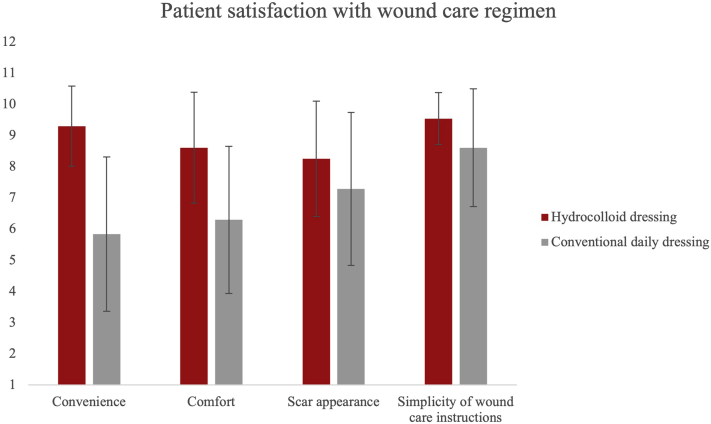
In the patients surveyed, HCD remained in place for 6.4 ± 3.1 days after application (compared with CDD, which was changed daily). Compared with CDD, HCD rated significantly higher in terms of comfort, convenience, scar appearance, and simplicity of wound care instructions (Table II and Fig 1).
Table II.
Patient satisfaction with a wound care regimen
| Outcome | Mean∗ (95% CI) |
P value† | |
|---|---|---|---|
| Hydrocolloid dressing (n = 64) | Conventional daily dressing (n = 64) | ||
| Convenience | 9.33 (9.02, 9.65) | 5.86 (5.28, 6.50) | <.0001 |
| Comfort | 8.69 (8.27, 9.13) | 6.25 (5.70, 6.85) | <.0001 |
| Scar appearance | 8.38 (7.97, 8.80) | 7.23 (6.65, 7.86) | .0025 |
| Simplicity of wound care instructions | 9.52 (9.31, 9.73) | 8.52 (8.08, 8.98) | <.0001 |
Scores are based on 10-point Likert scale questions, with a score of 10 being the best possible response for a given parameter and 1 being the worst rating for a given parameter.
P values were obtained using repeated measures Poisson regression models.
Fig 1.
Patient satisfaction with a wound care regimen. ∗, Scores are based on 10-point Likert scale questions, with a score of 10 being the best possible response for a given parameter and 1 being the worst rating for a given parameter.
When assessing convenience, there was a significantly higher rating for HCD over CDD (mean [95% CI]: 9.33 [9.02, 9.65] vs 5.86 [5.28, 6.50]; P < .0001). HCD also ranked higher than CDD with regards to comfort (mean [95% CI]: 8.69 [8.27, 9.13] vs 6.25 [5.70, 6.85]; P < .0001). While age was also significantly associated with comfort, with older patients more likely to rate wound care regimens with higher scores in general (P = .0077), comfort scores of HCD were higher than comfort scores of CDD even after controlling for age. In terms of scar appearance, there was a significantly higher rating with HCD versus CDD (mean [95% CI]: 8.38 [7.97, 8.80] vs 7.23 [6.65, 7.86]; P = .0025). Sex was also significantly associated with scar appearance, with men more likely to give higher scar appearance scores than women: respectively, 8.21 (7.80, 8.65) vs 7.31 (6.73, 7.94); P = .0194. Sex, when included in a multivariate model, did not affect the significantly higher scar appearance scores of HCD over CDD. Lastly, when evaluating for simplicity of wound care instructions, there was a significantly higher rating for HCD over CDD (mean [95% CI]: 9.52 [9.31, 9.73] vs 8.52 [8.08, 8.98]; P < .0001), even after controlling for the operating surgeon (SKQ vs other).
There was no statistically significant difference in erythema, edema, pain, report of associated fevers with either dressing (Table III). Patient-reported infections requiring antibiotics were higher with the use of CDD (7, 10.1%) than with HCD (1, 1.4%). Overall, 62 (96.8%) respondents responded that if given a choice between HCD and CDD, they would choose HCD as their wound care strategy after dermatologic excisional surgeries.
Table III.
Patient-reported complications associated with a wound care regimen∗
| n (%) |
P value† | ||
|---|---|---|---|
| Hydrocolloid dressing | Conventional daily dressing | ||
| Erythema | 20 (31.3) | 29 (45.3) | .145 |
| Warmth | 14 (21.9) | 16 (25.0) | .835 |
| Fluid leakage | 17 (26.6) | 14 (21.9) | .680 |
| Wound dehiscence | 6 (9.4) | 9 (14.1) | .584 |
| Edema | 24 (37.5) | 16 (25.0) | .182 |
| Malodorous smell | 6 (9.4) | 3 (4.7) | .492 |
| Pain | 26 (40.6) | 17 (26.6) | .134 |
| Infection requiring antibiotics | 1 (1.6) | 7 (10.9) | .062 |
| Fever | 0 (0) | 0 (0) |
Modified version of validated Bluebelle Wound Healing Questionnaire.14
2-sided Fisher's exact test value.
Discussion
Patient satisfaction is an important prognostic indicator for surgical outcomes, with satisfaction correlating with pain and ability to function physically.15,16 Postoperative wound care can pose a major source of anxiety and confusion for patients. Questions pertaining to wound care are responsible for more than half of patient calls received by dermatology offices following procedures.15 This confusion is amplified by the fact that wound care can differ between providers because of the lack of standardization among practices. These differences are numerous, including recommended lifestyle modifications, discussion of potential complications, and variation in topical medications.17 CDDs requiring frequent changes, cleansing, and topical emollient applications also places added burden on patients.
Results from our study suggest that the implementation of a simplified wound care regimen consisting of a one-time HCD application after dermatologic surgical procedures increases patient satisfaction and improves patient-reported outcomes. Participants rated HCD higher in convenience, comfort, scar appearance, and simplicity of wound care instructions compared with CDD, even after controlling for age, sex, surgical site, repair complexity, operating surgeon, and availability of assistance with wound care (Table II and Fig 1). On a 10-point Likert scale assessing convenience, HCD was rated as significantly more convenient at an average value of 9.30, compared with 5.84 for CDD. Studies in other disciplines support the idea that patients desire simpler wound management after surgery.18 Furthermore, patients subjectively rated the appearance of scars from wounds covered with HCD higher than those covered with CDD. HCD is suggested to have some intrinsic healing properties, which may help explain the perceived difference in scar appearance.19 There was no notable difference in postoperative complications when either dressing was used (Table III). Importantly, nearly all patients (96.8%) reported that they would choose HCD over CDD if given the choice of wound care dressing.
One limitation in this study is the variability in time from prior dermatologic surgery to survey completion leading to potential recall bias. In addition, some of these procedures were performed by different surgeons, and wound care instructions were provided by additional nursing staff when patients used CDD. In our study cohort, only 33 (51.6%) participants had both surgeries (HCD and CDD) performed by the same surgeon (SKQ). In our multivariate analysis, we were able to control for the operating surgeon as a potential confounder and showed that the statistically significant difference between HCD versus CDD scores was unattenuated by the surgeon who performed the surgery.
Conclusion
Postoperative wound care after dermatologic surgery can be tedious and confusing for patients. With the increasing age of patients and the number of surgical procedures performed in dermatology offices, there is an unmet need to improve postoperative wound care regimens. Our study suggests that a simplified wound care regimen—involving a one-time application of an HCD—results in greater comfort, convenience, scar appearance, and simplicity of wound care instructions compared with CDD changes.
Larger scale studies are needed to further elucidate the benefits of HCD over CDD with regard to postoperative complications. Objective scar assessment using validated scar rating scales can also more reliably measure any potential impact of HCD on scar appearance and cosmesis. Future investigations could also examine the cost-effectiveness of this wound care strategy, its use after less invasive dermatologic surgeries and cosmetic procedures, and its utility for surgeries involving more advanced closure techniques such as flaps and grafts.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: Dr Que receives research funding from the Indiana Clinical and Translational Sciences Institute.
IRB approval status: The study protocol, informed consent/assent form, participant recruitment materials, and other information provided to study participants were reviewed by the Indiana University Human Research Protection Program office and exempted from further review.
References
- 1.American Society for Dermatologic Surgery 2019 ASDS Survey on Dermatologic Procedures. https://www.asds.net/medical-professionals/practice-resources/asds-survey-on-dermatologic-procedures. 2021
- 2.Rogers H.W., Weinstock M.A., Feldman S.R., Coldiron B.M. Incidence estimate of nonmelanoma skin cancer (keratinocyte carcinomas) in the US population, 2012. JAMA Dermatol. 2015;151(10):1081–1086. doi: 10.1001/jamadermatol.2015.1187. [DOI] [PubMed] [Google Scholar]
- 3.Fathy R., Chu B., James W.D., Barbieri J.S. The frequency of topical antibiotic use after biopsy and excision procedures among dermatologists and nondermatologists: 2006 through 2015. J Am Acad Dermatol. 2020;82(5):1258–1261. doi: 10.1016/j.jaad.2019.12.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johnson-Jahangir H., Agrawal N. Perioperative antibiotic use in cutaneous surgery. Dermatol Clin. 2019;37(3):329–340. doi: 10.1016/j.det.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 5.Strickler A.G., Shah P., Bajaj S., et al. Preventing and managing complications in dermatologic surgery: procedural and postsurgical concerns. J Am Acad Dermatol. 2021;84(4):895–903. doi: 10.1016/j.jaad.2021.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh A., Halder S., Menon G.R., et al. Meta-analysis of randomized controlled trials on hydrocolloid occlusive dressing versus conventional gauze dressing in the healing of chronic wounds. Asian J Surg. 2004;27(4):326–332. doi: 10.1016/S1015-9584(09)60061-0. [DOI] [PubMed] [Google Scholar]
- 7.de Oliveira G.V., Gold M.H. Hydrocolloid dressings can be used to treat hypertrophic scars: an outpatient dermatology service devoted to treat keloids and challenging scars. J Cosmet Dermatol. 2020;19(12):3344–3348. doi: 10.1111/jocd.13792. [DOI] [PubMed] [Google Scholar]
- 8.Kamińska M.S., Cybulska A.M., Skonieczna-Żydecka K., Augustyniuk K., Grochans E., Karakiewicz B. Effectiveness of hydrocolloid dressings for treating pressure ulcers in adult patients: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(21):7881. doi: 10.3390/ijerph17217881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pacis M., Azor-Ocampo A., Burnett E., Tanasapphaisal C., Coleman B. Prophylactic dressings for maintaining skin integrity of healthcare workers when using N95 respirators while preventing contamination due to the novel coronavirus: a quality improvement project. J Wound Ostomy Continence Nurs. 2020;47(6):551–557. doi: 10.1097/WON.0000000000000713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang S., Hu S., Chen H., Jia X. Effectiveness of using hydrocolloid dressing combined with 3M Cavilon No-Sting Barrier Film to prevent facial pressure injury on medical staff in a COVID-19 designated hospital in China: a self-controlled study. Ann Palliat Med. 2021;10(1):3–9. doi: 10.21037/apm-20-1615. [DOI] [PubMed] [Google Scholar]
- 11.Norman G., Westby M.J., Rithalia A.D., Stubbs N., Soares M.O., Dumville J.C. Dressings and topical agents for treating venous leg ulcers. Cochrane Database Syst Rev. 2018;6(6):CD012583. doi: 10.1002/14651858.CD012583.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chamorro A.M., Vidal Thomas M.C., Mieras A.S., et al. Multicenter randomized controlled trial comparing the effectiveness and safety of hydrocellular and hydrocolloid dressings for treatment of category II pressure ulcers in patients at primary and long-term care institutions. Int J Nurs Stud. 2019;94:179–185. doi: 10.1016/j.ijnurstu.2019.03.021. [DOI] [PubMed] [Google Scholar]
- 13.Dumville J.C., Deshpande S., O'Meara S., Speak K. Hydrocolloid dressings for healing diabetic foot ulcers. Cochrane Database Syst Rev. 2013;2013(8):Cd009099. doi: 10.1002/14651858.CD009099.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bluebelle Study Group Validation of the Bluebelle Wound Healing Questionnaire for assessment of surgical-site infection in closed primary wounds after hospital discharge. Br J Surg. 2019;106(3):226–235. doi: 10.1002/bjs.11008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chitgopeker P., Sidey K., Aronson A., et al. Factors associated with patient-initiated communication after Mohs micrographic surgery. Dermatol Surg. 2019;45(2):234–243. doi: 10.1097/DSS.0000000000001750. [DOI] [PubMed] [Google Scholar]
- 16.Hamilton D.F., Lane J.V., Gaston P., et al. What determines patient satisfaction with surgery? A prospective cohort study of 4709 patients following total joint replacement. BMJ Open. 2013;3(4):e002525. doi: 10.1136/bmjopen-2012-002525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nguyen J.K., Huang A., Siegel D.M., Jagdeo J. Variability in wound care recommendations following dermatologic procedures. Dermatol Surg. 2020;46(2):186–191. doi: 10.1097/DSS.0000000000001952. [DOI] [PubMed] [Google Scholar]
- 18.Veiga D.F., Damasceno C.A., Veiga-Filho J., et al. Dressing wear time after breast reconstruction: a randomized clinical trial. PLoS One. 2016;11(12):e0166356. doi: 10.1371/journal.pone.0166356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mir M., Ali M.N., Barakullah A., et al. Synthetic polymeric biomaterials for wound healing: a review. Prog Biomater. 2018;7(1):1–21. doi: 10.1007/s40204-018-0083-4. [DOI] [PMC free article] [PubMed] [Google Scholar]