Abstract
Introduction: Acupuncture has demonstrated effectiveness for symptom management among breast cancer survivors. This meta-analysis aims to evaluate the effect of acupuncture on treatment-related symptoms among breast cancer survivors.
Methods: The authors searched PubMed, CINAHL, and EMBASE for relevant randomized clinical trials (RCTs) of acupuncture for managing treatment-related symptoms published in English through June 2021. They appraised the quality of each article using the Cochrane Collaboration Risk of Bias Criteria. The primary outcomes were pain, hot flashes, sleep disturbance, fatigue, depression, lymphedema, and neuropathy as individual symptoms. They also evaluated adverse events reported in acupuncture studies.
Results: Of 26 selected trials (2055 patients), 20 (1709 patients) were included in the meta-analysis. Acupuncture was more effective than control groups in improving pain intensity [standardized mean difference (SMD) = −0.60, 95% confidence intervals (CI) −1.06 to −0.15], fatigue [SMD = −0.62, 95% CI −1.03 to −0.20], and hot flash severity [SMD = −0.52, 95% CI −0.82 to −0.22]. The subgroup analysis indicated that acupuncture showed trends but not significant effects on all the treatment-related symptoms compared with the sham acupuncture groups. Compared with waitlist control and usual care groups, the acupuncture groups showed significant reductions in pain intensity, fatigue, depression, hot flash severity, and neuropathy. No serious adverse events were reported related to acupuncture intervention. Mild adverse events (i.e., bruising, pain, swelling, skin infection, hematoma, headache, menstrual bleeding) were reported in 11 studies.
Conclusion: This systematic review and meta-analysis suggest that acupuncture significantly reduces multiple treatment-related symptoms compared with the usual care or waitlist control group among breast cancer survivors. The safety of acupuncture was inadequately reported in the included studies. Based on the available data, acupuncture seems to be generally a safe treatment with some mild adverse events. These findings provide evidence-based recommendations for incorporating acupuncture into clinical breast cancer symptom management. Due to the high risk of bias and blinding issues in some RCTs, more rigorous trials are needed to confirm the efficacy of acupuncture in reducing multiple treatment-related symptoms among breast cancer survivors.
Keywords: acupuncture, breast cancer, meta-analysis, symptom, symptom cluster
Introduction
Breast cancer remains the most common cancer and the leading cause of cancer-related death among women worldwide.1 Breast cancer survivors are living longer with treatment-related symptoms.2 Women usually experience treatment-related fatigue, neuropathy, and lymphedema after chemotherapy and breast surgery.3 Women on endocrine therapy for 5 to 10 years after cancer treatment often experience joint pain, hot flashes, and sleep disturbance.4 Pain, fatigue, sleep disturbance, and depression can co-exist among breast cancer survivors during and years after cancer treatment.5 These symptoms have a detrimental impact on cognitive function and adherence to treatment, and compromise cancer survivors' quality of life, work functioning, and daily life.6,7 It is critical to understand the treatment-related symptoms experienced among breast cancer survivors and to maximize their management.
Symptoms experienced by breast cancer survivors can be managed with pharmacologic and nonpharmacologic treatments. Opioids and adjuvant analgesics have been used for cancer pain management, but are associated with intolerable side effects such as nausea, vomiting, and constipation.8 Hormonal replacement therapy can be used to treat menopausal symptoms. Due to increased risk of cancer recurrence and mortality, hormone replacement therapy is not recommended for the management of endocrine therapy treatment-related symptoms among breast cancer survivors.9 Moreover, some pharmacologic treatments such as the selective serotonin reuptake inhibitors (e.g., paroxetine, fluoxetine) can adversely interact with endocrine therapy drugs (e.g., tamoxifen).10 For these reasons, nonpharmacologic approaches such as acupuncture are increasingly used by breast cancer survivors to manage their symptoms.
Acupuncture is an integrative therapy that is a modality of Traditional Chinese Medicine (TCM). TCM addresses health issues based on the root and branch treatment principle.11 The root treatment focuses on correcting an underlying imbalance that affects the whole body as well as the presenting symptomatology. The branch treatment focuses on alleviating specific symptoms. Acupuncture stimulates pathways or meridians that conduct the body's vital energy, which produces a regulating and balancing effect on multiple organs and the whole body.12,13 Approximately 3.5 million adults in the United States receive acupuncture annually.14 Among them, 16% to 63% of breast cancer survivors have used acupuncture.15 More than 60% of the comprehensive National Cancer Institute-Designated Cancer Centers have used acupuncture for cancer symptom management.16 Previous literature has reported that acupuncture is safe, effective, and has few adverse effects.17 There is increasing evidence from randomized clinical trials (RCTs) that acupuncture can be used by breast cancer survivors to manage disease- and treatment-related symptoms, especially long-term treatment side effects.18,19
Most past RCTs and reviews have focused on the use of acupuncture for a single cancer-related symptom,20,21 not for multiple symptoms or overall health. Very few studies have summarized the effect of acupuncture on multiple common treatment-related symptoms experienced by breast cancer survivors. The primary aim of this systematic review and meta-analysis is to synthesize the evidence and assess the effect of acupuncture for managing each of the individual treatment-related symptoms experienced by breast cancer survivors.
Methods
This review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement. Please see supplemental files for PRISMA_2020_checklist.22 The primary outcomes of this review are treatment- related symptoms, which include pain, hot flashes, sleep disturbance, fatigue, depression, lymphedema, and neuropathy. The authors also evaluated adverse events reported in acupuncture RCTs.
Inclusion/exclusion criteria
A study was included if (1) it was a peer-reviewed prospective RCT published in the English language; (2) involved breast cancer survivors; (3) the treatment was acupuncture or electroacupuncture (various needle techniques were accepted); (4) the control group was sham acupuncture, waitlist control, usual care, or another intervention (e.g., medication, relaxation); and (5) it treated the chronic symptoms of interest (pain, hot flashes, sleep disturbance, fatigue, depression, lymphedema, and neuropathy). Studies were excluded if the intervention was (1) either acupressure or laser acupuncture without needles; (2) used to manage acute symptoms after surgery; (3) a retrospective chart review; or (4) a review article.
Search strategy
The authors searched PubMed, CINAHL, and Embase from 1974 through June 2021. The following terms were used in the search: (“breast cancer” [MeSH Terms] OR “breast cancer” [Title/Abstract] OR “breast neoplasm” [MeSH Terms] OR “breast neoplasm” [Title/Abstract] OR “breast tumor”[Title/Abstract] OR “breast tumor”[MeSH Terms]) AND “acupuncture” [MeSH Terms] OR “acupuncture”[Title/Abstract] OR “electro-acupuncture” [MeSH Terms] OR “electroacupuncture”[Title/Abstract]) AND (“joint pain” [Title/Abstract] OR “Arthralgia” [MeSH Terms] OR “pain” [Title/Abstract] OR “arthralgia”[Title/Abstract] OR “fatigue”[Title/Abstract] OR “Fatigue” [MeSH Terms] OR “sleep”[Title/Abstract] OR “insomnia”[Title/Abstract] OR “insomnia” [MeSH Terms] OR “depression”[Title/Abstract] OR “depression” [MeSH Terms] OR “depressive symptom”[Title/Abstract] OR “depressive symptom” [MeSH Terms] OR “neuropathy”[Title/Abstract] OR “lymphedema”[Title/Abstract] OR “lymphoedema”[Title/Abstract] OR “Lymphedema” [MeSH Terms] OR “hot flashes”[MeSH Terms] OR “hot flashes”[Title/Abstract] OR “hot flush”[Title/Abstract] OR “vasomotor symptoms”[Title/Abstract] OR “menopausal symptoms”[Title/Abstract]) AND (random* OR “Clinical Trials as Topic”[Mesh] OR “Clinical Trial”[Publication Type]).
Data extraction and quality assessment
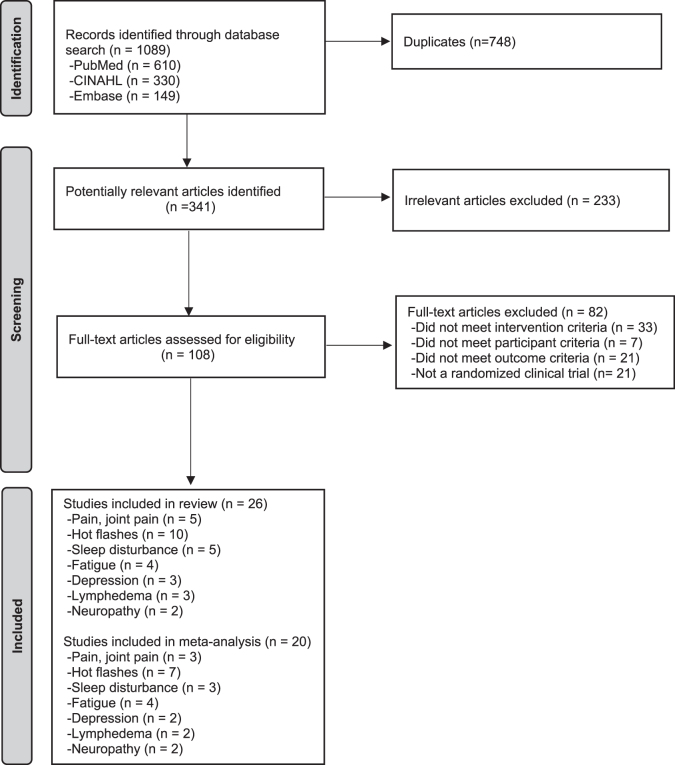
Data screening was managed using Endnote X9.2. Studies with duplicate titles were deleted. Two researchers (H.L. and T.L.) screened the titles and abstracts independently according to the inclusion and exclusion criteria. Any disagreements between two researchers were resolved by discussion with a third researcher. Details of the screening and selection process are shown in the PRISMA flowchart (Fig. 1).
FIG. 1.
PRISMA flowchart describing the selection process. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analysis.
Four authors (H.L., M.K.J., Y.L., and M.S.) extracted data independently, then appraised the quality of each article in pairs, rating it as having low, high, or unclear risk of bias (RoB) using the Cochrane Collaboration Risk of Bias Criteria, which is based on random sequence generation, allocation concealment, blinding, incomplete outcome data, selective outcome reporting, and other sources of bias.23 For each article, the authors extracted information about authors, country where the study was performed, symptoms, study design, sample size, treatment period, acupuncture protocol style, adverse effect, and significant results between the acupuncture and control groups on an Excel spreadsheet. Discrepancies noted during study selection and data extraction were discussed with another author and agreement was obtained.
Meta-analysis and synthesis of evidence
The meta-analysis and subgroup analysis were conducted using RevMan 5.3.24 First, the authors compared the acupuncture group versus all the control groups for each symptom. The effect sizes for each symptom were measured as standardized mean differences (SMDs) and the corresponding 95% confidence intervals (CI) were calculated. Then, a subgroup analysis was conducted according to different control groups: acupuncture versus sham acupuncture, acupuncture versus usual care or waitlist control, and acupuncture versus other interventions. Heterogeneity among trials was identified by the χ2 test and reported as I2; 0%–40% was considered to represent a low level of heterogeneity, 40%–75% was considered to represent moderate heterogeneity, whereas 75%–90% was considered to represent considerable heterogeneity. A random effects model was employed for pooled analyses. If the summary of statistics was missing or not reported in the original study, the authors (1) contacted the authors for additional data and (2) used the following formula to compute standard deviation (SD) for changes: .
Results
The database search yielded 1089 journal articles. After omitting 748 duplicates, 341 articles remained for screening, 26 RCTs that studied any of the 7 individual symptoms of interest were included for systematic review and evaluated for RoB, and 20 RCTs were found eligible for meta-analysis.
Characteristics of clinical studies and quality of evidence
Among the 26 studies (2055 patients) reviewed, the most commonly evaluated symptom was hot flashes (n = 10),25–34 followed by endocrine-therapy-induced joint pain (n = 5),35–39 fatigue (n = 4),40–43 sleep disturbance (n = 5),28,29,40,44,45 lymphedema (n = 3),46–48 depression (n = 3),29,34,40 and neuropathy (n = 2).49,50 Fourteen studies (54%) were conducted in the United States,26,29,30,33,35–37,39–41,44,47,49,50 4 in Sweden,31,32,34,45 3 in Australia,38,42,48 and 1 each in the United Kingdom,43 Italy,25 China,46 Norway,27 and Denmark.28 Sample size for the studies ranged from 29 to 302. The acupuncture interventions were conducted after the completion of chemotherapy and during endocrine therapy. Manual acupuncture was used in 17 studies and electroacupuncture in 9 studies. Study design and type of control groups differed, including acupuncture versus sham, acupuncture versus usual care, acupuncture versus waitlist control, acupuncture versus sham versus usual care, and acupuncture versus other interventions (i.e., applied relaxation, hormone replacement therapy, diosmin, gabapentin, or venlafaxine). Three types of acupuncture protocols were used across studies: standardized, semistandardized, and individualized. The semistandardized acupuncture protocol consists of a standardized acupuncture protocol plus additional acupuncture points that take interindividual variability and individual health conditions into account. Additional acupuncture points are then needled as the patient's condition dictates. The individualized acupuncture protocol is an acupuncture point prescription formulated by the acupuncturist after development of a patient-specific TCM pattern diagnosis. Seventeen out of 26 studies (65%) used a standardized acupuncture protocol.27–34,37,38,41,42,45–50 Among them, only five studies (29%) found significant effect in favor of acupuncture on treatment-related symptoms compared with control groups.27,28,31,46,50 Eight studies used the semistandardized acupuncture protocol and all of these studies found significant effect in favor of acupuncture compared with control groups.26,35,36,39,40,42–44 Only one study used an individualized acupuncture protocol and showed that acupuncture significantly managed hot flashes compared with the usual care group.25
Of the 26 RCTs included in this review, 12 (46%) were determined to have low RoB in the following five domains: random sequence generation, allocation concealment, blinding, incomplete outcome data, and selective outcome reporting. Other sources of bias were unclear in these studies. Twelve studies (46%) that did not include sham acupuncture were rated as high risk for blinding; five studies were unclear concerning allocation concealment; and five studies were unclear concerning random sequence generation. Three studies had selective outcome reporting and only reported a subset of the original outcomes. The authors did not assess blinding of personnel in the RoB assessment because the acupuncturist was not blinded in any of these studies. A summary of the included RCTs and details of domain-specific assessed RoB are provided in Table 1 and Supplementary Data.
Table 1.
Summary of Included Studies
| Author (year) | Country | Symptoms | Study design | Sample size | Period (weeks) | Protocol | Significant result | Included in meta-analysis | AEs |
|---|---|---|---|---|---|---|---|---|---|
| Pain | |||||||||
| Hershman (2018) | United States | Joint pain | VA vs. SA vs. WL | 110/59/27 | 6 | SS | Yes (VAa vs. SA); yes (VAa vs. WL) | Yes | No serious AE. Grade 1 AE (n = 61) and grade 2 AE (n = 16) were reported in VA group. Grade 1 AE (n = 22) and grade 2 AE (n = 10) were reported in SA group. |
| Mao (2014) | United States | Joint pain | VA (EA) vs. SA vs. WL | 22/22/23 | 8 | SS | Yes (EAa vs. WL); yes (SAa vs. WL) | Yes | No serious AE. The EA group had more AEs reported than the SA group (16 vs. 4). A major category of AEs reported in the EA group was related to the de qi sensation (n = 6) |
| Bao (2013) | United States | Joint pain | VA vs. SA | 23/24 | 8 | ST | No (VA vs. SA) | No | Not reported. |
| Oh (2013) | Australia | Joint pain | VA (EA) vs. SA | 15/14 | 6 | ST | No (EA vs. SA) | No | No serious AE. Only minor bruising on acupuncture points (n = 5). |
| Crew (2010) | United States | Joint pain | VA vs. SA | 20/18 | 6 | SS | Yes (VAa vs. SA) | Yes | No serious AE. Only 3 participants thought that acupuncture was moderately painful (TA, n_2; SA, n_1). |
| Hot flashes | |||||||||
| Lesi (2016) | Italy | Hot flashes | VA vs. UC | 85/105 | 12 | I | Yes (VAa vs. UC) | Yes | No serious AE. Twelve patients in the acupuncture arm experienced mild AEs (muscle pain, headache, and one menstrual bleed). |
| Mao (2015) | United States | Hot flashes | VA (EA) vs. SA vs. PP vs. gabapentin | 30/32/30/28 | 8 | SS | Yes (SAa vs. PP); yes (EAa vs. PP); no (gabapentin vs. PP) | Yes | No serious AE. Five mild AE (4 bruising, 1 increased pain) in VA group, 1 in SA group. |
| Bao (2014) | United States | Hot flashes; sleep; depression | VA vs. SA | 23/24 | 8 | ST | No (Hot flashes, sleep, mood: VA vs. SA) | No | Not reported. |
| Bokmand (2013) | Denmark | Hot flashes; sleep disturbance | VA vs. SA vs. UC | 60/62/34 | 5 | ST | Yes (Hot flashes, sleep: VAa vs. SA); yes (Hot flashes, sleep: VAa vs. UC); no (Hot flashes, sleep: SA vs. UC) | No | Not reported. |
| Liljegren (2012) | Sweden | Hot flashes | VA vs. SA | 42/42 | 5 | ST | No (VA vs. SA) | Yes | No serious AE. Two minor events, a slight bleeding and a bruise at the needle site were reported in the sham group. |
| Walker (2010) | United States | Hot flashes; depression | VA vs. venlafaxine | 25/25 | 12 | ST | No (Hot flashes, mood: VA vs. venlafaxine) | No | Not reported. |
| Hervik (2009) | Norway | Hot flashes | VA vs. SA | 30/29 | 10 | ST | Yes (VAa vs. SA) | Yes | Not reported. |
| Frisk (2008) | Sweden | Hot flashes | VA (EA) vs. HT | 23/18 | 12 | ST | Yes (EA vs. HTa) | Yes | No serious AE. |
| Deng (2007) | United States | Hot flashes | VA vs. SA | 42/30 | 4 | ST | No (VA vs. SA) | Yes | Only very minor adverse effects, such as slight bleeding or bruising at the needle site, were reported, and none required further medical intervention. A total of 14 grade 1 AEs (of about 560 acupuncture sessions) were recorded by 12 participants as definitely, probably, or likely due to a study intervention. |
| Nedstrand (2006) | Sweden | Hot flashes; depression | VA (EA) vs. applied relaxation | 19/19 | 12 | ST | No (hot flashes, mood: EA vs. applied relaxation) | Yes | Not reported. |
| Fatigue | |||||||||
| Mao (2014) | United States | Fatigue; sleep; depression | VA (EA) vs. SA vs. WL | 22/22/23 | 8 | SS | Yes (fatigue, depression, anxiety: EAa vs. WL); no (fatigue, sleep, anxiety: SA vs. WL) | Yes | Not reported. |
| Deng (2013) | United States | Fatigue; depression | VA vs. SA | 47/50 | 6 | ST | No (fatigue, depression: VA vs. SA) | Yes | A total of 11 serious AEs occurred during the study period, including bronchospasm (1), low blood counts (1), renal failure (2), secondary malignancy (1), nausea (1), vomiting (2), small bowel obstruction (1), dyspnea (1), and back pain (1). None of these events was deemed related to the study interventions because of the timing and characteristics of the symptoms, as well as the apparent alternative explanations for them. |
| Smith (2013) | Australia | Fatigue | VA vs. SA vs. WL | 10/10/10 | 6 | SS | No (VA vs. SA); yes (VAa vs. WL) | Yes | Not reported. |
| Molassiotis (2012) | United Kingdom | Fatigue; depression | VA vs. UC | 227/75 | 6 | SS | Yes (fatigue, depression: VAa vs. UC) | Yes | Not reported. |
| Sleep disturbance [also see Mao (2014); Bao (2014); Bokmand (2013)] | |||||||||
| Garland (2017) | United States | Sleep disturbance | VA (EA) vs. gabapentin | 30/28 | 8 | SS | Yes (EAa vs. gabapentin) | Yes | Not reported. |
| Frisk (2012) | Sweden | Sleep disturbance | VA (EA) vs. HT | 26/18 | 12 | ST | No (EA vs. HT) | Yes | No AE. |
| Depression [also see Mao (2014); Deng (2013); Bao (2013); Nedstrand (2006)] | |||||||||
| Neuropathy | |||||||||
| Lu (2020) | United States | Neuropathy | VA+EA vs. UC | 20/20 | 8 | ST | Yes (VA+EAa vs. UC) | Yes | No serious AE. 2 AEs in VA group (pruritis, joint pain) |
| Greenlee (2016) | United States | Neuropathy | VA (EA) vs. SA | 31/32 | 6 | ST | No (EA vs. SA) | Yes | No serious AE. 1 AE in VA group (grade 1 acupuncture needle site reaction with discomfort, minor swelling, and bruising after acupuncture needle withdrawal) |
| Lymphedema | |||||||||
| Bao (2018) | United States | Lymphedema | VA vs. WL | 36/37 | 6 | ST | No (VA vs. WL) | Yes | No serious AE. Grade 1 treatment-related AEs such as bruising (45), hematoma (2), pain (2), skin infection (1) were reported in patients who received at least one acupuncture (n = 77). |
| Yao (2016) | China | Lymphedema | VA+WA vs. diosmin | 15/15 | 4 | ST | Yes (VA+WAa vs. diosmin) | Yes | No serious AE. |
| Smith (2014) | Australia | Lymphedema | VA vs. UC | 9/8 | 8 | ST | No (VA vs. UC) | No | No serious AE. |
Has more favor for effect.
AE, adverse event; EA, electroacupuncture; HT, hormone replacement therapy; I, individualized acupuncture protocol; PP, placebo pills; SA, sham acupuncture; SS, semistandardized acupuncture protocol; ST, standardized acupuncture protocol; UC, usual care; VA, verum acupuncture; WA, warm acupuncture; WL, waitlist control.
Adverse event
Fifteen studies reported no serious adverse events.25,26,30–32,35,36,38–40,45,46,48–50 Only one study reported 11 serious adverse events during the study period.41 However, none of these events was related to the acupuncture intervention. Mild adverse events (i.e., bruising, pain, swelling, skin infection, hematoma, headache, menstrual bleeding) were reported in the verum acupuncture group in 11 studies.25,26,30,32,35,36,38–40,49,50 Ten studies did not report or mention adverse events.
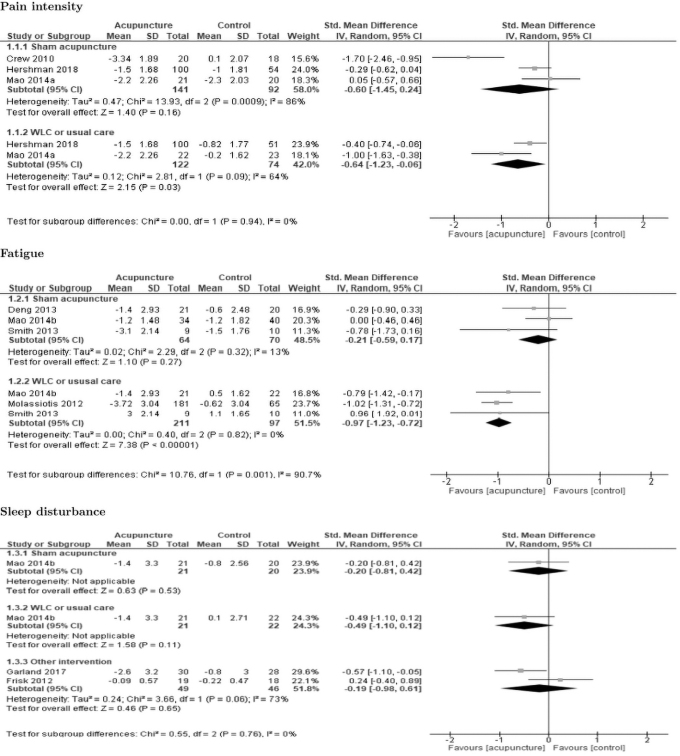
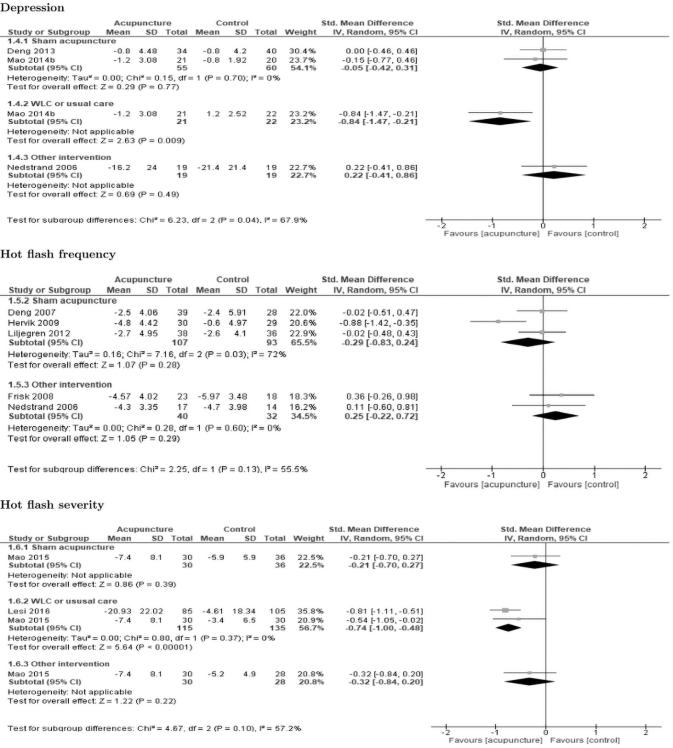
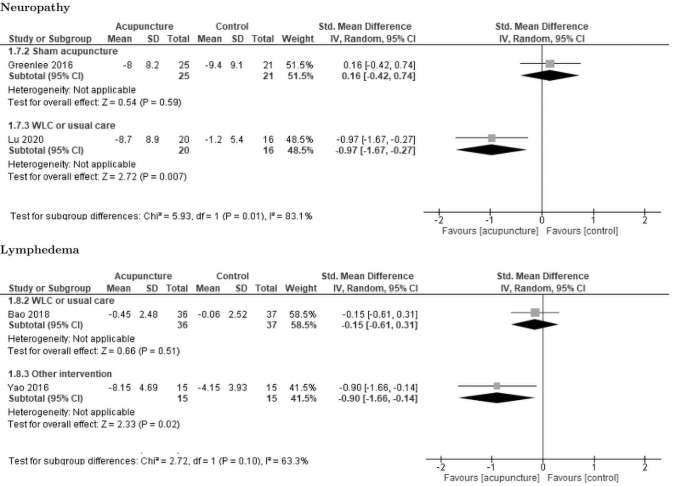
Meta-analysis results: verum acupuncture versus control
Forest plots for acupuncture compared with the control groups and the subgroup analysis for each symptom are shown in Figure 2. There was a statistically significant effect in favor of acupuncture on pain intensity [SMD = −0.60, 95% CI −1.06 to −0.15], fatigue [SMD = −0.62, 95% CI −1.03 to −0.20], and hot flash severity [SMD = −0.52, 95% CI −0.82 to −0.22], with statistical heterogeneity of 77%, 68%, and 45%, respectively. Verum acupuncture showed trends, but no significant differences between the control groups for hot flash frequency, sleep disturbance, depression, neuropathy, and lymphedema compared with the control groups.
FIG. 2.
Forest plots of the comparison of acupuncture with control groups for each symptom and subgroup analysis for sham, waitlist control or usual care, and other interventions.
Subgroup analysis: verum acupuncture versus sham acupuncture
Verum acupuncture showed trends but not significant effects on pain intensity [SMD = −0.60, 95% CI −1.45 to 0.24], sleep disturbance [SMD = −0.20, 95% CI −0.81 to 0.42], fatigue [SMD = −0.21, 95% CI −0.59 to 0.17], depression [SMD = −0.05, 95% CI −0.42 to 0.31], hot flash frequency [SMD = −0.29, 95% CI −0.83 to 0.24], and hot flash severity [SMD = −0.21, 95% CI −0.70 to 0.27] compared with the sham acupuncture groups at the end of acupuncture treatment.
Subgroup analysis: verum acupuncture versus waitlist control or usual care
The authors combined the waitlist control and usual care groups for this analysis. The results revealed a statistically significant effect in favor of acupuncture on the management of pain intensity [SMD = −0.64, 95% CI −1.23 to −0.06] with heterogeneity of 64%, fatigue [SMD = −0.97, 95% CI −1.23 to −0.72] with heterogeneity of 0%, depression [SMD = −0.84, 95% CI −1.47 to −0.21], hot flash severity [SMD = −0.74, 95% CI −1.00 to −0.48] with heterogeneity of 0%, and neuropathy [SMD = −0.97, 95% CI −1.67 to −0.27] compared with the waitlist control or usual care groups at the end of treatment. Verum acupuncture showed trends but not significant effects on sleep disturbance [SMD = −0.49, 95% CI −1.10 to 0.12] and lymphedema [SMD = −0.15, 95% CI −0.61 to 0.31] compared with waitlist control or usual care.
Subgroup analysis: verum acupuncture versus other interventions
The results revealed a statistically significant effect in favor of acupuncture compared with diosmin on the management of lymphedema [SMD = −0.90, 95% CI −1.66 to −0.14]. There were no significant differences in change scores for depression (compared with applied relaxation), sleep disturbance (compared with gabapentin, hormone therapy), hot flash frequency (applied relaxation, hormone therapy), and hot flash severity (gabapentin).
Discussion
The authors included 26 RCTs (2055 patients) in the systematic review and 20 RCTs (1709 patients) in the meta-analysis. Consistent with most meta-analyses, we found acupuncture reduced multiple treatment-related symptoms (pain intensity, hot flashes, fatigue, depression, and neuropathy) compared with the usual care or waitlist control group, it only showed trends but not significant effects compared with sham acupuncture control.19,51–53 The effect of acupuncture on study outcomes is sensitive to the type of control used,19 with larger effect sizes found in trials with waitlist control or usual care compared with sham acupuncture control groups.54 Rigorous RCTs are still needed to confirm these findings. Below are methodological challenges and research gaps that still need to be addressed.
Challenges to using sham acupuncture control groups
Using high-quality control groups in acupuncture research is challenging because it is hard to blind acupuncturists, and there is likely a therapeutic effect with sham acupuncture.36,55 Two types of sham acupuncture controls are commonly used. The first uses acupuncture needles that either penetrate the skin at nonacupuncture points or are inserted only shallowly into acupuncture points.55 Four studies in this review used penetrating needles at nonacupuncture points for the sham acupuncture group.27,28,35,39 However, sham acupuncture controls using penetrating needles at nonacupuncture points have been criticized because they may have therapeutic effect.54,56 More studies are needed to examine the validity of using this type of sham acupuncture control group.
The second type of sham acupuncture control uses a device with a nonpenetrating placebo needle (i.e., Streitberger or Park needles). Six studies in this review used the Streitberger needle,57 a single-blind device, for the sham control group, and none showed significance between the verum and the Streitberger needle groups.26,30,36,38,40,41 Five studies used the Park needle, which can be either be used as a single- or double-blind device; again, none showed significance between the verum and the Park needle groups.29,32,36,37,42 It is important to note that the acupuncturist was not blinded in any of these studies, including those using the Park needle. The major limitation of a single-blind device is that it may potentiate acupuncturist bias, which may result in participant bias and/or unblinding.58
The gold standard for acupuncture research is the double-blind RCT,55,59 which allows comparison of treatment with placebo.58 The Takakura double-blind needle consists of a set of one penetrating needle and one placebo skin touch needle and blinds both participants and acupuncturists.60 Neither participant nor acupuncturist can determine by sight or feel which needle (penetrating or placebo) is being used. The validity of the Takakura needle has been established,58,60–62 and this device should be considered for future double-blind acupuncture RCTs. None of the studies in this review used this double-blind device.
Different acupuncture protocols
Multiple studies in this review used a semistandardized acupuncture research protocol, and this review suggested that the semistandardized protocols were in general more effective than the standardized protocols in terms of ability to manage treatment-related symptoms. Semistandardized protocols consist of a standardized acupuncture protocol plus additional acupuncture points that take interindividual variability and individual health conditions into account. Mao et al.36 used a semistandardized protocol where each participant chose one most painful joint area for treatment and the acupuncturist selected an additional four acupuncture points based on the participant's complaints of depression, anxiety, or fatigue. Since each person's symptom experience is different, and most breast cancer survivors experience multiple symptoms, the authors recommend that future studies use semistandardized acupuncture protocols.
Only one study in this review (which addressed hot flashes) used individualized acupuncture points to treat participants based on individual TCM pattern diagnosis.25 Individualized protocols are highly influenced by acupuncturists' training, clinical judgment, preferences, and acumen. Meanwhile, there is insufficient evidence regarding whether individualized protocols are more effective than standardized or semistandardized protocols for symptom management. More studies are needed to evaluate the efficacy of individualized acupuncture protocols for symptom management.
Effects of acupuncture on multiple symptoms
This review found that acupuncture has a significant effect on multiple treatment-related symptoms. This finding supports another recent review finding that acupuncture improves overall health.13 This may be because acupuncture is often focused on enhancing overall health not just on individual symptoms. According to the principles of TCM, a patient is dually treated with a root and branch treatment. When an acupuncturist develops a specific TCM pattern diagnosis, both root and branch assessments and treatment plans are formulated. These treatments overlap and often potentiate one another, leading not only to symptom amelioration but also to improvement in overall health.13 Thus, acupuncture for hot flashes may also reduce sleep disturbance, fatigue, depression, and the psychoneurologic symptom cluster among people with breast cancer.29,63
Given the coexisting cluster of psychoneurologic symptoms (i.e., pain, fatigue, sleep disturbance, depression, anxiety) among breast cancer survivors,64 additional studies with additional measures are needed to evaluate the effect of acupuncture on symptom clusters and/or general health improvement. For example, a global well-being outcomes rating scale can be used to measure general health improvement,65 and a composite score that sums standardized scores for each symptom or produces a data-driven reduced rank regression score may be calculated.66
Limitations
This review had several limitations. First, due to language limitations and accessibility of databases in other languages, the authors only included studies published in English. This limits the scope of the review, since there are other acupuncture RCTs published in Chinese, Korean, and Japanese. Future reviews may include more studies that are written in these languages. Second, we did not perform a meta-analysis for the symptom cluster, even though two studies reported multiple outcomes. Future reviews can use robust methods to handle multiple outcomes (i.e., robust variance estimation, multilevel meta-analysis). The authors also encourage future investigators to measure multiple co-occurring symptoms using a comprehensive scale. When enough published studies have done so, more valid and efficient methods will be available for meta-analysis.67 Lastly, this meta-analysis included only one time point, at completion of the acupuncture intervention. Some studies reported long-term follow-up and suggested persistence of the acupuncture effect, and this should be included in future analyses.
Conclusion
Compared with a usual care or waitlist control group, verum acupuncture significantly reduces multiple treatment-related symptoms among breast cancer survivors. The safety of acupuncture was inadequately reported in the included studies. Based on the available data, acupuncture seems to be generally a safe treatment with some mild adverse events. Acupuncture can be recommended to breast cancer survivors who seek nonpharmacologic care for their distressing symptoms. Due to the high RoB and blinding issues in some RCTs, more rigorous trials are needed to confirm the efficacy of acupuncture in reducing multiple treatment-related symptoms among breast cancer survivors.
Supplementary Material
Acknowledgment
The authors thank Tandem Editing LLC for article editing.
Authors' Contributions
H.L, M.K.J, Y.L., and T.L. were responsible for acquisition, interpretation, and drafting the article. C.G.P. substantially contributed to the data analysis. J.M.S. and A.D. critically revised the work for important intellectual content. M.S. was included in the article drafting and also critically revised the work. All authors provided final approval of the version to be published and agree to be accountable for all aspects of the work.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
This work was supported by the National Institute of Nursing Research of the National Institutes of Health (award no. K24NR015340).
Supplementary Material
References
- 1. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. [DOI] [PubMed] [Google Scholar]
- 2. Kim JE, Dodd MJ, Aouizerat BE, et al. A review of the prevalence and impact of multiple symptoms in oncology patients. J Pain Symptom Manage 2009;37:715–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sullivan CW, Leutwyler H, Dunn LB, et al. Stability of symptom clusters in patients with breast cancer receiving chemotherapy. J Pain Symptom Manage 2018;55:39–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yoo TK, Jang MJ, Lee E, et al. Endocrine treatment-related symptoms and patient outcomes in breast cancer: A meta-analysis. J Breast Cancer 2018;21:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kim HJ, Barsevick AM, Tulman L, et al. Treatment-related symptom clusters in breast cancer: A secondary analysis. J Pain Symptom Manage 2008;36:468–479. [DOI] [PubMed] [Google Scholar]
- 6. Ng CG, Mohamed S, See MH, et al. Anxiety, depression, perceived social support and quality of life in Malaysian breast cancer patients: A 1-year prospective study. Health Qual Life Outcomes 2015;13:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Biglia N, Bounous VE, Malabaila A, et al. Objective and self-reported cognitive dysfunction in breast cancer women treated with chemotherapy: A prospective study. Eur J Cancer Care (Engl) 2012;21:485–492. [DOI] [PubMed] [Google Scholar]
- 8. Siotos C, Cheah MA, Karahalios A, et al. Interventions for reducing the use of opioids in breast reconstruction. Cochrane Database Syst Rev 2020:CD013568. [Google Scholar]
- 9. Lupo M, Dains JE, Madsen LT. Hormone replacement therapy: An increased risk of recurrence and mortality for breast cancer patients? J Adv Pract Oncol 2015;6:322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Haque R, Shi J, Schottinger JE, et al. Tamoxifen and antidepressant drug interaction among a cohort of 16 887 breast cancer survivors. J Natl Cancer Inst 2016;108:djv337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhuo L-S. Acupuncture based on the theory of Biao and Ben. Zhongguo Zhen Jiu 2011;31:75–78. [PubMed] [Google Scholar]
- 12. Zhou W, Benharash P. Effects and mechanisms of acupuncture based on the principle of meridians. J Acupunct Meridian Stud 2014;7:190–193. [DOI] [PubMed] [Google Scholar]
- 13. Birch S. Treating the patient not the symptoms: Acupuncture to improve overall health–Evidence, acceptance and strategies. Integr Med Res 2019;8:33–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. National Center for Complementary and Integrative Health (NCCIH). National Health Interview Survey (NHIS). Use of complementary health approaches: 2012. adult use report. Online document at: https://nccih.nih.gov/research/statistics/NHIS, accessed August 12, 2020.
- 15. Jia L. Cancer complementary and alternative medicine research at the US National Cancer Institute. Chin J Integr Med 2012;18:325–332. [DOI] [PubMed] [Google Scholar]
- 16. Brauer JA, El Sehamy A, Metz JM, et al. Complementary and alternative medicine and supportive care at leading cancer centers: A systematic analysis of websites. J Altern Complement Med 2010;16:183–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Paley CA, Johnson MI, Tashani OA, et al. Acupuncture for cancer pain in adults. Cochrane Database Syst Rev 2015:Cd007753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Salehi A, Marzban M, Zadeh AR. Acupuncture for treating hot flashes in breast cancer patients: An updated meta-analysis. Support Care Cancer 2016;24:4895–4899. [DOI] [PubMed] [Google Scholar]
- 19. Pan Y, Yang K, Shi X, et al. Clinical benefits of acupuncture for the reduction of hormone therapy-related side effects in breast cancer patients: A systematic review. Integr Cancer Ther 2018;17:602–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhang X, Wang X, Zhang B, et al. Effects of acupuncture on breast cancer-related lymphoedema: A systematic review and meta-analysis of randomised controlled trials. Acupunct Med 2019;37:16–24. [DOI] [PubMed] [Google Scholar]
- 21. Chen L, Lin C-C, Huang T-W, et al. Effect of acupuncture on aromatase inhibitor-induced arthralgia in patients with breast cancer: A meta-analysis of randomized controlled trials. Breast 2017;33:132–138. [DOI] [PubMed] [Google Scholar]
- 22. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. RevMan. Review Manager (Revman) [Computer Program]. Version 5.3. Denmark: The Nordic Cochrane Centre, The Cochrane Collaboration Copenhagen, 2014. [Google Scholar]
- 25. Lesi G, Razzini G, Musti MA, et al. Acupuncture as an integrative approach for the treatment of hot flashes in women with breast cancer: A prospective multicenter randomized controlled trial (AcCliMaT). J Clin Oncol 2016;34:1795–1802. [DOI] [PubMed] [Google Scholar]
- 26. Mao JJ, Bowman MA, Xie SX, et al. Electroacupuncture versus gabapentin for hot flashes among breast cancer survivors: A randomized placebo-controlled trial. J Clin Oncol 2015;33:3615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hervik J, Mjåland O. Acupuncture for the treatment of hot flashes in breast cancer patients, a randomized, controlled trial. Breast Cancer Res Treat 2009;116:311. [DOI] [PubMed] [Google Scholar]
- 28. Bokmand S, Flyger H. Acupuncture relieves menopausal discomfort in breast cancer patients: A prospective, double blinded, randomized study. Breast 2013;22:320–323. [DOI] [PubMed] [Google Scholar]
- 29. Bao T, Cai L, Snyder C, et al. Patient-reported outcomes in women with breast cancer enrolled in a dual-center, double-blind, randomized controlled trial assessing the effect of acupuncture in reducing aromatase inhibitor-induced musculoskeletal symptoms. Cancer 2014;120:381–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Deng G, Vickers A, Yeung S, et al. Randomized, controlled trial of acupuncture for the treatment of hot flashes in breast cancer patients. J Clin Oncol 2007;25:5584–5590. [DOI] [PubMed] [Google Scholar]
- 31. Frisk J, Carlhäll S, Källström A-C, et al. Long-term follow-up of acupuncture and hormone therapy on hot flushes in women with breast cancer: A prospective, randomized, controlled multicenter trial. Climacteric 2008;11:166–174. [DOI] [PubMed] [Google Scholar]
- 32. Liljegren A, Gunnarsson P, Landgren B-M, et al. Reducing vasomotor symptoms with acupuncture in breast cancer patients treated with adjuvant tamoxifen: A randomized controlled trial. Breast Cancer Res Treat 2012;135:791–798. [DOI] [PubMed] [Google Scholar]
- 33. Walker EM, Rodriguez AI, Kohn B, et al. Acupuncture versus venlafaxine for the management of vasomotor symptoms in patients with hormone receptor-positive breast cancer: A randomized controlled trial. J Clin Oncol 2010;28:634–640. [DOI] [PubMed] [Google Scholar]
- 34. Nedstrand E, Wyon Y, Hammar M, et al. Psychological well-being improves in women with breast cancer after treatment with applied relaxation or electro-acupuncture for vasomotor symptom. J Psychosom Obstet Gynaecol 2006;27:193–199. [DOI] [PubMed] [Google Scholar]
- 35. Hershman DL, Unger JM, Greenlee H, et al. Effect of acupuncture vs sham acupuncture or waitlist control on joint pain related to aromatase inhibitors among women with early-stage breast cancer: A randomized clinical trial. JAMA 2018;320:167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mao JJ, Xie SX, Farrar JT, et al. A randomised trial of electro-acupuncture for arthralgia related to aromatase inhibitor use. Eur J Cancer 2014;50:267–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bao T, Cai L, Giles JT, et al. A dual-center randomized controlled double blind trial assessing the effect of acupuncture in reducing musculoskeletal symptoms in breast cancer patients taking aromatase inhibitors. Breast Cancer Res Treat 2013;138:167–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Oh B, Kimble B, Costa D, et al. Acupuncture for treatment of arthralgia secondary to aromatase inhibitor therapy in women with early breast cancer: Pilot study. Acupunct Med 2013;31:264–271. [DOI] [PubMed] [Google Scholar]
- 39. Crew KD, Capodice JL, Greenlee H, et al. Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor–associated joint symptoms in women with early-stage breast cancer. J Clin Oncol 2010;28:1154–1160. [DOI] [PubMed] [Google Scholar]
- 40. Mao JJ, Farrar JT, Bruner D, et al. Electroacupuncture for fatigue, sleep, and psychological distress in breast cancer patients with aromatase inhibitor-related arthralgia: A randomized trial. Cancer 2014;120:3744–3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Deng G, Chan Y, Sjoberg D, et al. Acupuncture for the treatment of post-chemotherapy chronic fatigue: A randomized, blinded, sham-controlled trial. Support Care Cancer 2013;21:1735–1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Smith C, Carmady B, Thornton C, et al. The effect of acupuncture on post-cancer fatigue and well-being for women recovering from breast cancer: A pilot randomised controlled trial. Acupunct Med 2013;31:9–15. [DOI] [PubMed] [Google Scholar]
- 43. Molassiotis A, Bardy J, Finnegan-John J, et al. Acupuncture for cancer-related fatigue in patients with breast cancer: A pragmatic randomized controlled trial. J Clin Oncol 2012;30:4470–4476. [DOI] [PubMed] [Google Scholar]
- 44. Garland SN, Xie SX, Li Q, et al. Comparative effectiveness of electro-acupuncture vs. gabapentin for sleep disturbances in breast cancer survivors with hot flashes: A randomized trial. Menopause 2017;24:517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Frisk J, Källström A-C, Wall N, et al. Acupuncture improves health-related quality-of-life (HRQoL) and sleep in women with breast cancer and hot flushes. Support Care Cancer 2012;20:715–724. [DOI] [PubMed] [Google Scholar]
- 46. Yao C, Xu Y, Chen L, et al. Effects of warm acupuncture on breast cancer–related chronic lymphedema: A randomized controlled trial. Curr Oncol 2016;23:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Bao T, Zhi WI, Vertosick EA, et al. Acupuncture for breast cancer-related lymphedema: A randomized controlled trial. Breast Cancer Res Treat 2018;170:77–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Smith CA, Pirotta M, Kilbreath S. A feasibility study to examine the role of acupuncture to reduce symptoms of lymphoedema after breast cancer: A randomised controlled trial. Acupunct Med 2014;32:387–393. [DOI] [PubMed] [Google Scholar]
- 49. Greenlee H, Crew KD, Capodice J, et al. Randomized sham-controlled pilot trial of weekly electro-acupuncture for the prevention of taxane-induced peripheral neuropathy in women with early stage breast cancer. Breast Cancer Res Treat 2016;156:453–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lu W, Giobbie-Hurder A, Freedman RA, et al. Acupuncture for chemotherapy-induced peripheral neuropathy in breast cancer survivors: A randomized controlled pilot trial. Oncologist 2020;25:310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Chien T-J, Liu C-Y, Chang Y-F, et al. Acupuncture for treating aromatase inhibitor–related arthralgia in breast cancer: A systematic review and meta-analysis. J Altern Complement Med 2015;21:251–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. He Y, Guo X, May BH, et al. Clinical evidence for association of acupuncture and acupressure with improved cancer pain: A systematic review and meta-analysis. JAMA Oncol 2020;6:271–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Chien T-J, Hsu C-H, Liu C-Y, et al. Effect of acupuncture on hot flush and menopause symptoms in breast cancer—A systematic review and meta-analysis. PLoS One 2017;12: e0180918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Vickers AJ, Vertosick EA, Lewith G, et al. Acupuncture for chronic pain: Update of an individual patient data meta-analysis. J Pain 2018;19:455–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Zhu D, Gao Y, Chang J, et al. Placebo acupuncture devices: Considerations for acupuncture research. Evid Based Complement Alternat Med 2013;2013:628907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Birch S, Alraek T, Kim KH, et al. Placebo-controlled trials in acupuncture: Problems and solutions. Evid Based Res Methods Chin Med 2016:55–64. [Google Scholar]
- 57. Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet 1998;352:364–365. [DOI] [PubMed] [Google Scholar]
- 58. Takakura N, Takayama M, Yajima H. Double-blind and single-blind retractable placebo needles. Anaesthesia 2018;73:258–260. [DOI] [PubMed] [Google Scholar]
- 59. Tavel ME. The placebo effect: The good, the bad, and the ugly. Am J Med 2014;127:484–488. [DOI] [PubMed] [Google Scholar]
- 60. Takakura N, Yajima H. A double-blind placebo needle for acupuncture research. BMC Complement Altern Med 2007;7:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Takakura N, Takayama M, Kawase A, et al. Double blinding with a new placebo needle: A validation study on participant blinding. Acupunct Med 2011;29:203–207. [DOI] [PubMed] [Google Scholar]
- 62. Takakura N, Takayama M, Kawase A, et al. Double-blind acupuncture needle: A potential tool to investigate the nature of pain and pleasure. ISRN Pain 2013:825751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Otte JL, Carpenter JS, Zhong X, et al. Feasibility study of acupuncture for reducing sleep disturbances and hot flashes in post-menopausal breast cancer survivors. Clin Nurse Spec 2011;25:228–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Li H, Sereika SM, Marsland AL, et al. Symptom clusters in women with breast cancer during the first 18 months of adjuvant therapy. J Pain Symptom Manage 2020;59:233–241. [DOI] [PubMed] [Google Scholar]
- 65. Bell IR, Cunningham V, Caspi O, et al. Development and validation of a new global well-being outcomes rating scale for integrative medicine research. BMC Complement Altern Med 2004;4:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Salomon RE, Crandell J, Muscatell KA, et al. Two methods for calculating symptom cluster scores. Nurs Res 2020;69:133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Moeyaert M, Ugille M, Natasha Beretvas S, et al. Methods for dealing with multiple outcomes in meta-analysis: A comparison between averaging effect sizes, robust variance estimation and multilevel meta-analysis. Int J Soc Res Methodol 2017;20:559–572. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.