Abstract
The digestive system is one of the most common sites of malignancies in humans. Since gastrointestinal tumors represent a massive global health burden both in terms of morbidity and health care expenditures, scientists continuously develop novel diagnostic and therapeutic methods to ameliorate the detrimental effects of this group of diseases. Apart from the well-established role of the endoscopic ultrasound (EUS) in the diagnostic course of gastrointestinal and hepatobiliary malignancies, we have recently become acquainted with a vast array of its therapeutic possibilities. A multitude of previously established, evidence-based methods that might now be guided by the EUS emerged: Radiofrequency ablation, brachytherapy, fine needle injection, celiac plexus neurolysis, and endoscopic submucosal dissection. In this review we endeavored to provide a comprehensive overview of the role of these methods in different malignancies of the digestive system, primarily in the treatment and symptom control in pancreatic cancer, and additionally in the management of hepatic, gastrointestinal tumors, and pancreatic cysts.
Keywords: Pancreatic cancer, Endoscopic ultrasound, Endoscopic ultrasound-guided fine needle injection, Pancreatic cyst, Gastrointestinal tumor, Portal vein
Core Tip: Apart from the well-established role of the endoscopic ultrasound (EUS) along the diagnostic path of gastrointestinal and hepatobiliary malignancies, the EUS recently emerged as a carrier of various therapeutic modalities. In this review we sought to give a comprehensive overview of the role of various established methods that might now be guided by the EUS in different malignancies of the digestive system, primarily regarding the treatment and symptom control in pancreatic cancer, and additionally in the management of hepatic, gastrointestinal tumors, and pancreatic cysts.
INTRODUCTION
Endoscopic ultrasound (EUS) is one of the principal tools in cancer screening and staging. Apart from its use in the diagnostic course of gastrointestinal and hepatobiliary malignancies, it has an entire range of other therapeutic possibilities (Figure 1). The ability of the EUS to obtain tissue samples using either fine needle aspiration (FNA) or fine needle biopsy makes it a unique method in the screening of pancreatic cystic lesions, as well as in the assessment of regional lymph node involvement in esophageal, gastric, and rectal cancer (Figures 2-4). The EUS is therefore essential in the concurrent pancreatic cancer diagnosis[1]. Over the last few years, the implementation of the EUS has expanded from the diagnostic into the therapeutic field. Endoscopic ultrasound-guided fine needle injection (EUS-FNI) of chemotherapeutics, immunotherapy and gene therapy, tissue ablation, stereotactic radiation therapy, brachytherapy and celiac plexus neurolysis have been thoroughly investigated and steadily introduced into the clinical practice[1,2]. Multiple studies suggest that some of these methods might be crucial in overcoming the problem of drug distribution to tumorous tissue in patients with pancreatic cancer, whereas other methods could be of aid in pain management of the same population. In this review we endeavored to give a comprehensive overview of the role of the EUS in anticancer therapy: primarily in the treatment and symptom control in pancreatic cancer, and, additionally, in the management of hepatic and gastrointestinal tumors.
Figure 1.
Overview of endoscopic ultrasound-guided methods. EUS-FNI: Endoscopic ultrasound-fine needle injection; HCC: Hepatocellular carcinoma; GI: Gastrointestinal; Nd:YAG: Neodymium-doped yttrium aluminum garnet; SBRT: Stereotactic body radiotherapy.
Figure 2.
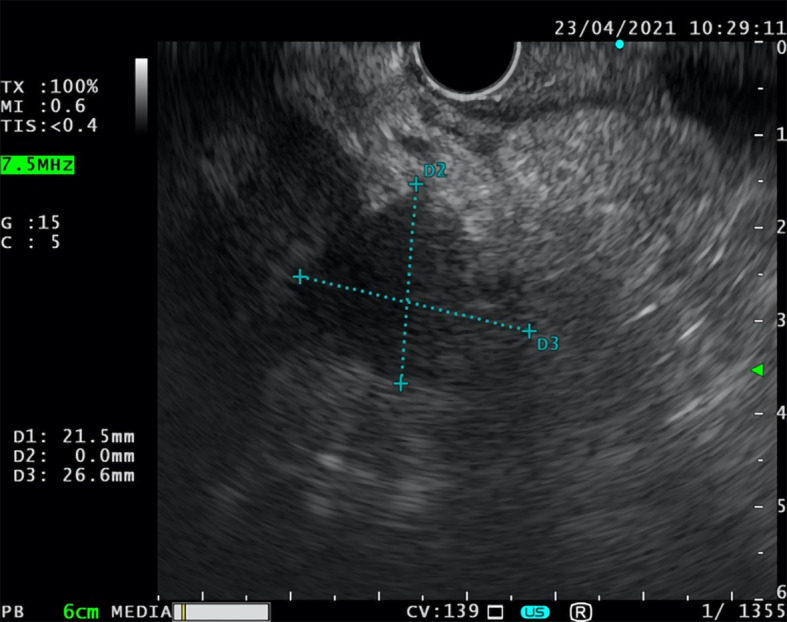
Endoscopic ultrasound-fine needle aspiration. Fine needle aspiration of inhomogeneous oval lesion located on the border between head and corpus of the pancreas (26.6 mm × 21.5 mm).
Figure 4.

Endoscopic ultrasound-fine needle biopsy. Fine needle biopsy of the focal lesion in the pancreatic head (42 mm × 38 mm).
Figure 3.
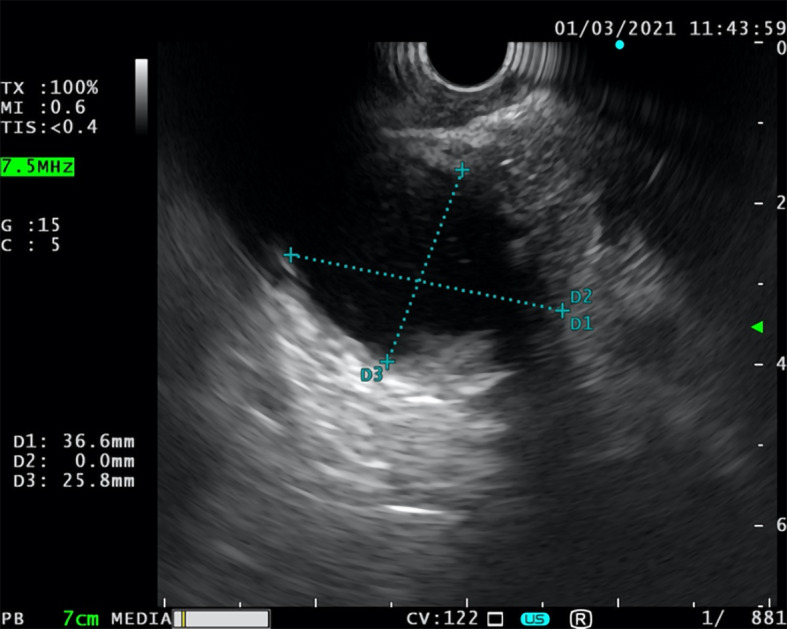
Unsuccessful endoscopic ultrasound-fine needle aspiration. Unsuccessful attempt of fine needle aspiration of the cystic lesion with thick, calcified border (37 mm × 26 mm) located in the head of the pancreas.
THE EUS IN TREATMENT OF PANCREATIC CANCER
As hypovascularity and abundant desmoplasia are landmarks of pancreatic cancer, delivery of chemotherapeutic medications to the tumor-affected area is insufficient[3]. Consequently, effects of chemotherapeutics on pancreatic cancer are mitigated, resulting in higher required therapeutic doses which increases the incidence of adverse effects[4]. Therefore, several local strategies that could possibly overcome these issues were developed. Among a number of EUS-based therapeutic interventions, radiofrequency ablation (RFA), brachytherapy, EUS-FNI, and EUS-guided celiac plexus neurolysis (EUS-CPN) emerged as viable strategies for improvement of poor outcomes regarding the pancreatic cancer.
RFA
RFA is an invasive antitumor method which works by generating heat from high-frequency alternating current that induces frictional heating, leading to thermal coagulative necrosis of the target tissue[5]. In addition, several authors demonstrated that RFA may trigger immunomodulatory activity, and in this way, further dampening the cancer development[6-9]. RFA is already a well-established therapeutic modality in management of other cancers, particularly for patients with hepatocellular carcinoma, and has been included in the latest guidelines for management of hepatocellular carcinoma by a major European organization[10].
Owing to the anatomical positioning of the pancreas, suitable approaches for the inclusion of the RFA in pancreatic cancer are multiple, including open surgery, laparoscopic approach, percutaneous approach, and an EUS-guided approach. Initially, safety and effectiveness of EUS-guided RFA of the pancreatic tissue were evaluated in porcine models[11-14]. Although results of the animal studies were promising, clinicians were doubtful, as thermal-induced pancreatitis and thermal injuries of the adjoining structures emerged as adverse effects in the animal studies and in early intraoperative studies[11,15-17]. Early on, surgeons observed that detrimental effects of intraoperative RFA could be reduced by using lower temperatures, maintaining a margin from the major adjacent vessels, and by using stepwise approach in bigger, poorly demarcated lesions[18,19]. Intraoperative studies have also provided an insight into the effectiveness of the RFA. Multiple studies have demonstrated that intraoperative RFA leads to tumor necrosis and a decrease of tumor volume, as well as reduction in CA 19-9 plasma levels, the main pancreatic cancer marker[16,20-25]. Unfortunately, in all of the aforementioned studies, all patients that underwent RFA eventually developed disease progression[16,20-25]. Of note, in a small sample (n = 25) study by Spiliotis et al[16], authors have shown a significant prolongation in survival in patients treated with both palliative care and RFA in opposition to patients that received palliative care exclusively, an observation that Matsui et al[25] failed to demonstrate. In addition, Cantore et al[26] argue that combined multiple-treatment followed by RFA can prolong survival in patients with unresectable pancreatic cancer.
Together, these findings paved the way for the investigation of the EUS-guided RFA. In a pilot study by Song et al[27], 6 patients with unresectable pancreatic cancer underwent EUS-guided RFA. Two out of six patients suffered abdominal pain, whereas other patients reported no adverse, effects implying the safety of the procedure. However, as the purpose of the study was to assess the technical feasibility and safety of the procedure, long-term survival of the patients was not studied. Multiple similar studies were performed following this study, and their results with regard to effectiveness and adverse events were summarized in a recent meta-analysis by Dhaliwal et al[28]. Meta-analysis showed that technical success, defined as the successful placement of the needle within the pancreatic lesions with safe margins from the surrounding vital structure, and clinical success, defined as decrease in lesion size and presence of necrosis on CT scan after the procedure, were 100% and 91.5%, respectively. Adverse events were observed in 15% of the patients, with abdominal pain being the most common (10%) and only 2 cases of pancreatitis and 1 perforation in total. Overall, the EUS-guided RFA appears to be safe, but multicenter, randomized control trials are needed in order to clearly define the utility of this method.
EUS-FNI
EUS-FNI is an antitumor agent delivery method in which the EUS serves as a guide for needle placement into target lesions. Aside from injection of various therapeutic agents, EUS-FNI is also suitable for implantation of fiducial markers that enables targeted radiation therapy and for injection of dyes to tattoo the tumor[29,30]. The first human clinical trial (phase I) using the EUS-FNI was performed by Chang et al[31] in 2000. Authors used EUS-FNI to deliver allogeneic mixed lymphocyte culture (cytoimplant) into the tumor tissue. The median survival of the 8 patients enrolled in the study was 13.2 mo, with 3 partial responses and no adverse events reported. Since then, the largest conducted trial of this sort was a phase III trial in which effects of TNFeradeTM biologic, in combination with fluorouracil and radiotherapy, were assessed on 304 patients with advanced pancreatic cancer[32]. Unfortunately, Herman et al[32] failed to demonstrate better progression-free survival or overall survival in comparison to controls. Recently Lee et al[33] conducted a phase I trial in which authors combined adenovirus-mediated double-suicide gene therapy with gemcitabine in patients with locally advanced pancreatic cancer. Nonetheless, despite the fact that the trial proved the safety of the procedure, pioneers of EUS-FNI argued in a recent paper that a lot of hurdles have to be overcome in order to develop a clinically functional EUS-FNI method, especially in terms of oncolytic viruses[34]. Among recently conducted trials, we have highlighted the following two: (1) Nishimura et al[35] injected a double-stranded RNA oligonucleotide that repressed tumor growth in 6 patients with unresectable pancreatic cancer and reported no adverse effects, as well as reduction in plasma levels of the target molecule and tumor size reduction; and (2) A prospective study by Levy et al[36] tested the use of EUS-FNI for the guided delivery of gemcitabine, a chemotherapeutic whose role in treatment of pancreatic cancer has been well-established. Authors administered gemcitabine in 36 patients with various stages of pancreatic cancer (II-IV), and no adverse events were reported. Overall survival of the patients was 10.4 mo, and more importantly, 20% of patients with stage III unresectable disease were down-staged and underwent an R0 resection. In conclusion, as pancreatic cancer is a systemic disease, it is practically impossible to assume that EUS-FNI will fully replace current therapeutic modalities of pancreatic cancer, but, given the safety and feasibility of the method, as well as expansion of translational medicine, it could emerge as a viable adjuvant method in the future.
Brachytherapy
EUS-guided brachytherapy involves implantation of radioactive seeds directly into or adjacent to the tumor-affected tissue. The target tissue is then exposed to the emission of low-energy gamma, X-rays, or beta particles, leading to localized tissue injury and tumor ablation. The main advantage of brachytherapy is its ability to deliver a markedly higher dose of radiation to the tumor mass in comparison to external beam radiation therapy. In the latter, radiation beams pass through other non-tumorous tissues in reaching the target mass, thus resulting in collateral toxicity and more damage to healthy tissue. Although there is abundant evidence to suggest that brachytherapy can deliver a higher dose of radiation and provide local control as well as palliative benefits, currently no brachytherapy device is approved for the treatment of patients with pancreatic cancer[37-42]. There are multiple approaches for implantation of radioactive seeds, one of which is the EUS-guided brachytherapy, and a variety of chemical elements that could be used in this manner (phosphorus-32 (P-32), iodine, gold, iridium, etc.)[43,44]. Two pilot trials that tested the potential of EUS-guided brachytherapy in patients with pancreatic cancer had rather disappointing results with no benefits with regard to overall survival rate (27%) and partial response rate (13.6%), respectively[45,46]. Nonetheless, authors of one of the trials argued that such results might be due to an insufficient radiation dose to local lesions[47]. They performed another study in which they implemented a novel computer-aided treatment-planning system (TPS). Under the support of the new TPS, partial remission rate was 80% and expected median survival time of the 42 patients was 9.0 mo (24 patients were in stage IV). At present, there is an ongoing open-label, single-arm pilot study of EUS-guided brachytherapy with P-32 microparticles in combination with gemcitabine and/or nab-paclitaxel in unresectable locally advanced pancreatic cancer (OncoPaC-1 study)[48]. However, the role of the EUS-guided brachytherapy in pancreatic cancer is yet to be determined. Hopefully, conjunction of brachytherapy and chemotherapeutics will increase the share of patients with pancreatic cancer that convert to resectable and provide us with more durable, local control in comparison to conventional treatments.
EUS-guided celiac plexus neurolysis
Among a multitude of options, the EUS has also found its place in the palliative treatment of patients with pancreatic cancer. Given the fact that most patients present in the advanced stages of the disease, palliative care is often the primary goal of care. Pain, the most significant and most common complication of pancreatic cancer, has traditionally been managed by nonsteroidal and opioid analgesic, often with numerous side effects, including constipation, sedation, nausea, vomiting, and delirium[49,50]. In order to overcome these issues and while trying to improve quality of life, endoscopic ultrasound-guided celiac plexus neurolysis (EUS-CPN) was introduced by Wierseme and Wierseme in 1996 (Table 1)[51].
Table 1.
Overview of the endoscopic ultrasound-guided celiac plexus neurolysis characteristics
|
Procedure
|
Chemical ablation of the celiac plexus
|
| Indications | Chronic abdominal pain caused by: Pancreatic cancer; Chronic pancreatitis; Gallbladder carcinoma1 |
| Contraindications[57] | Coagulation disorders; INR > 1.5; Platelet count < 50000/µL; Retroperitoneal abscess; Disturbed anatomy (difficulties in visualizing the celiac trunk and ganglia); Malformations of the celiac or superior mesenteric artery |
| Serious complications (observed in 0.2% of the patients[63]) | Paraplegia; Retroperitoneal abscess; Ischemia with visceral injury |
| Supporting evidence | Kaufman et al[50]; Wiersema et al[51]; Puli et al[54]; Wyse et al[55]; Arcidiacono et al[58] |
Only pivotal studies were so far conducted. INR: International normalized ratio.
EUS-CPN is a minimally invasive method for the treatment of pain through the chemical ablation of the celiac plexus under the control of the EUS. The current National Comprehensive Cancer Network guidelines recommend EUS-CPN for treatment of severe pancreatic cancer-associated pain in the case of failure of achieving adequate analgesia and/or intolerable adverse effects[52].
The EUS-guided neurolysis is indicated for patients with chronic abdominal pain caused by an upper GI tract malignancy, mostly pancreatic cancer. Patients with unresectable disease whose pain affects their quality of life are considered good candidates for this approach. Furthermore, there are pivotal studies of the EUS-CPN efficacy in patients with gallbladder carcinoma[53]. However, besides pancreatic carcinoma, the main indication for EUS-CPN still remains chronic pancreatitis[50,54].
The optimal timing in which the EUS neurolysis should be applied is still unclear. However, in randomized, double-blind, controlled trial, Wyse et al[55] found that early EUS-CPN, performed during the diagnostic EUS, provided better pain management and prevented an increase in morphine consumption than EUS-CPN later in the course of the disease. However, further studies are needed to define the optimal timing for CPN. CPN consists of injecting a neurolytic agent (absolute alcohol or phenol) into the area around the celiac plexus monitored by an echo endoscope with prior administration of a local anesthetic (bupivacaine or lidocaine). Application of the neurolytic agent can be unilateral (just above the celiac trunk) or bilateral (on both sides of the celiac trunk)[56-58].
Several studies have shown pain improvement after CPN[50,51,54,55]. In the initial study, pain improvement was achieved at 2, 4, 8, and 12 wk after CPN in 79%-88% patients[51]. Additionally, a Cochrane Review of six studies (358 patients), that showed that the EUS-CPN was superior at 4 and 8 wk compared to drug-based management, with significant drug consumption reduction[5]. Whether the application of the EUS-CPN affects survival remains unclear. A study by Fujii-Lau et al[59] indicates that the EUS-guided neurolysis is associated with longer survival than the non-EUS guided approach. However, further studies are needed to assess the potential impact of the neurolysis on survival. In order to improve the efficiency of pain treatment, the following EUS-CPN modifications have been presented: EUS-guided direct celiac ganglia neurolysis (EUS-CGN); and EUS-guided broad plexus neurolysis[60-62]. In a randomized study by Doi et al[60], authors indicated better pain improvement in CGN over CPN. Levy et al[61] have successfully demonstrated the modification of the neurolysis of the celiac plexus in the form of direct injection of the agent into the celiac ganglion, requiring prior visualization of the ganglia itself. Sakamoto et al[62] in 2010 described the injection of a neurolytic agent in the area around the origin of the superior mesenteric artery, introducing a method of broad plexus neurolysis, which demonstrated better pain relief compared to the CPN.
A recent review of 20 studies comprising 1142 patients, revealed that complications of EUS-CPN occurred in 21% of 661 EUS-guided CPN interventions[63]. The most frequent complications included diarrhea, transient pain exacerbation, and hypotension. Most of the complications seem to be a consequence of a sympatholytic reaction and are self-limited (< 48 h). However, in 0.2% of cases, major complications were observed, including paraplegia, retroperitoneal abscess, and ischemia with visceral injury[63].
Given the unequivocal beneficial effects of EUS-CPN in the palliative care of the patients with advance pancreatic cancer, we can expect further increase of its usage in routine clinical practice.
EUS IN PANCREATIC CYSTIC NEOPLASMS
Pancreatic cystic neoplasms (PCN) represent a heterogeneous group of pancreatic cysts with significant differences in their pathological and clinical features, the most important one being the difference in malignant potential among subtypes. These differences are important as they determine the approach for both the treatment and the surveillance of PCN[64-66]. A prevalence of all PCN varies from 2%-45% in general population)[67-70], with constant increase in the PCN detection rate. The explanation for the observed increase lies in the improved modalities of non-invasive (computed tomography (CT) scan, magnetic resonance imaging- cholangiopancreatography (MRI-MRCP)) and minimally invasive (endoscopic ultrasound-fine needle aspiration (EUS-FNA)) imaging methods, and their broader use in preventive check-ups, as well as an awareness of true nature of PCN and the necessity for their close follow-up. According to different studies, abdominal ultrasonography detects PCN in 0.21% of individuals[71], CT in 2.6%[72], and MRI-MRCP in 2.4% to 49.1% of tested individuals[65,72-74]. The management of PCN may be quite challenging, with identification of specific PCN type being a crucial step since malignant potential varies significantly between different types of PCN. Timely and correct management of PCN is vital, as it may prevent progression to pancreatic cancer and decrease the need for lifelong follow-up[71].
Due to the challenges in differentiation between the various types of PCN and its implications on therapeutic approach, guidelines on the management of PCN were proposed by expert groups, most notably by the Association of Pancreatology, the American Gastroenterological Association, and by the European Study Group on Cystic Tumors of the Pancreas[65,66,73,75]. Various approaches, including surgical resection, endoscopic techniques, and surveillance, are covered in all of the above-noted guidelines. Surgical resection is the golden standard for management of premalignant and malignant cystic lesions. Indications for resection depend on the presence of symptoms, probability of malignancy, location of the lesion, and surgical risk of the patient. On the other hand, surgery carries a considerable risk, with perioperative complication rates from 20% to 40%, and mortality rates up to 2%[76-79]. Therefore, endoscopic techniques represent an important alternative to surgery, especially in patients with significant comorbidities or in cases of indeterminate cystic lesions.
The main advantage of the EUS in this setting is the fact that EUS-guided pancreatic cyst ablation using ethanol and/or paclitaxel enables organ preservation, leaving endocrine and exocrine function intact[80-83]. However, there is concern about the use of ethanol, as the rate of reported complications was as high as 2%–10%[84]. Another disadvantage of this method is the inability to obtain a sample for histopathological analysis. The long-term effects of ablation and prevention of malignant alteration are yet to be evaluated in future studies[84-87]. The current diagnostic workup of PCN includes CT or MRI with the addition of MRCP and EUS when appropriate[64-67,88]. EUS is indicated in addition to other imaging modalities if there are worrisome clinical or radiological features present (nodules, dilated pancreatic duct, thickened wall), or if there is a need for obtaining the cystic fluid for cytological and/or biochemical analysis.
The reported accuracy of EUS imaging for differentiating mucinous from non-mucinous PCN is relatively low (48%-94%), with sensitivity of 36%-91%, and specificity of 45%-81%[89-93]. Cytopathological analysis of cystic fluid may reveal dysplasia or clear malignancy. Although cytology is highly specific (83%-100%), it is relatively insensitive (27%-48%), resulting in relatively low diagnostic accuracy of this procedure (8%-59%)[89-92,94]. However, sensitivity could be increased by an additional puncture of the cystic wall. Additional biochemical markers, including carcinoembryonic antigen (CEA), which has been proved to be useful in distinction between mucinous and non-mucinous PCN, and amylase, which strongly suggests a connection between the cyst and the pancreatic ductal system, may also be obtained from cystic fluid[95,96]. Combination of multiple EUS-guided methods, such as EUS morphology, cytology, and cyst fluid CEA, provide us with greater accuracy in detecting malignant PCN than any of the methods individually[97,98]. Recently, DNA testing of pancreatic cyst fluid emerged as a promising additional tool for the differentiation between mucinous and non-mucinous PCN, between mucinous PCN subtypes, and between premalignant PCN and advanced neoplasia[99].
According to the latest recommendations, surgically fit patients with asymptomatic cysts that are presumed to be premalignant (intraductal papillary mucinous neoplasms (IPMN) or mucinous cystic neoplasms(MCN)), but which possess no concerning features, should be monitored, preferably using MRI-MRCP or EUS if MRCP is not available[100,101]. In cases in which any of the worrisome features emerges, the EUS-FNA should be used in the cyst follow-up. For both IPMN and MCN, surveillance should continue as long as the patient is fit for surgery[102]. On the other hand, current guidelines do not address the need for surveillance in asymptomatic patients with serous cystic neoplasms (SCN), since malignant progression of SCN is very rare[102-104].
EUS-GUIDED PORTAL VEIN INTERVENTIONS
The portal vein (PV) can be accessed via trans-gastric or trans-duodenal access under the EUS guidance using an 18G-25G needle with low risk of complications. Multiple studies have demonstrated that EUS is successful in sampling of the PV to reveal circulating tumor cells, as well as obtaining the portal vein thrombus specimen[105], which has an utmost significance in the staging of hepatocellular liver cancer (HCC)[106-108]. The diagnostic yield of the EUS is confirmed by the reported cases of HCC detection using the EUS-FNA of radiologically suspected malignant thrombi without an evident liver mass[108,109].
As a significant step forward, Park et al[110] have even demonstrated the technical feasibility of the EUS guided transhepatic PV stenting in porcine models, without any immediate or late complications[110]. However, patients who undergo PV stenting due to malignant thrombosis or stenosis may bear certain procedural risk factors, such as coagulopathy and risk of rapid clinical deterioration if biliary leak or bacteremia occurs.
The EUS-guided PV injection of chemotherapy (EPIC) is another novel therapeutic possibility with a few significant advantages in comparison to the current methods[106]. EPIC uses drug eluting microbeads that eventually lodges in hepatic sinusoids and results in the prolonged hepatic drug exposure[111]. Studies suggest that EPIC achieves appropriate intrahepatic drug levels, while simultaneously bypassing the systemic side effects and avoiding the ischemic bile duct injury that occurs during the transarterial approach[106]. Faigel et al[111] compared the EPIC administration of irinotecan loaded liquid chromatography beads with the systemic unloaded irinotecan application in animal models and revealed EPIC-associated higher irinotecan intrahepatic concentration, as well as lower plasma, bone marrow, and skeletal muscle drug concentrations. Two years later, the same group confirmed their findings on a greater number of animal models using irinotecan, doxorubicin, and albumin-bound paclitaxel nanoparticles[112].
Preoperative selective embolization of the PV branch that feeds the tumor-affected liver lobe has been utilized in clinical practice since 1986 using the percutaneous transhepatic approach[106,113]. Embolization leads to the atrophy of the involved liver segment and hypertrophy of the remnant liver parenchyma, thus preventing the postoperative liver failure[113]. Recently, Park et al[113] used nine porcine models to successfully prove the efficacy and safety of the EUS guided embolization of the PV using coil and cyanoacrylate. Furthermore, Matthes et al[114] demonstrated efficient selective PV embolization using ethylene-vinyl alcohol copolymer, known as EVAL (Enteryx), in an animal model. Unfortunately, to our knowledge, studies including PV interventions in anticancer treatment have been so far limited to animal models. Still, exciting advances in the field are revealed, and prospective studies involving humans are eagerly awaited.
ROLE OF THE EUS IN LIVER TUMOR MANAGEMENT
EUS-guided tumor ablation is a safe and effective treatment modality for tumor lesions of the caudate and left liver lobe. Multiple studies have successfully demonstrated the benefits of ethanol administration via EUS-FNI in the treatment of both HCC and liver metastases[115]. Carrara et al[116] described the EUS guided trans-gastric bipolar hybrid cryotherm ablation on a porcine model without complications. Varadarajulu et al[117] reported RFA in animal models with effective coagulation necrosis of large areas and without damage to the surrounding liver parenchyma. Multiple studies have also demonstrated success of the EUS-guided neodymium-doped yttrium aluminum garnet (Nd:YAG) laser ablation in patients with HCC and colorectal cancer metastases[118,119]. In addition, several other methods, including injection of sclerosants and chemotherapeutics, represent viable future therapeutic options[115].
In the management of the HCC-related complications, one of the most common and disastrous is the variceal bleeding incident. With respect to secondary prevention of this complication in patients with inoperable HCC, Tang et al[120] used EUS guided cyanoacrilate injection, which led to reduced rebleeding rates, as well as improved variceal bleeding free survival.
ROLE OF EUS IN ENDOSCOPIC SUBMUCOSAL DISSECTION
The development of gastrointestinal endoscopic tissue resection techniques demands precise diagnostic tools in the preoperative evaluation. Accurate information about the depth of tumor invasion of the gastrointestinal wall and the nodal involvement are necessary for determining the appropriate intervention.
Endoscopic submucosal dissection (ESD), the newest and most invasive method, has become standard of care of precancerous and some early cancer lesions in gastrointestinal tract, allowing curative resection of the lesions[121]. Depending on the proximity of the GI tract wall during the procedure, the EUS enables clear image of the lesion depth and vital surrounding structures, especially of the lymph nodes[121].
Endoscopic resection is indicated in early esophageal cancer with minimal or no lymph node invasion[122]. According to the latest guidelines for the treatment of esophageal cancer of the Japan Esophageal Society, the absolute indication for endoscopic resection is defined as flat lesion (Paris 0-II), with m1 (intraepithelial) - m2 (invading lamina propria) invasion, and circumferential extent of ≤ 2/3[123]. A systematic review and meta-analysis has demonstrated that sensitivity and specificity for T1a staging were 85% and 87%, respectively, and 86% for both sensitivity and specificity for T1b staging[124]. However, the ability of the EUS to predict endoscopic resectability by discrimination between T1 and T2 lesions is still intensively studied. Available data suggests that 15%-25% of cases are under-staged compared with endoscopic mucosal resection staging, while about 4%-12% of cases are over-staged[125,126].
Conventional EUS has limited accuracy in the detection of submucosal invasion in early esophageal cancer[127,128]. It remains questionable whether the EUS should be routinely performed prior to ESD of esophageal superficial lesions. European Society of Gastrointestinal Endoscopy (ESGE) suggests that EUS should be considered in esophageal superficial carcinomas with suspicious features for submucosal invasion or lymph node metastasis[122].
Esophageal submucosal tumors are becoming more common indication for ESD. EUS allows for the evaluation of size, echo pattern, layer of origin, and eventual surrounding nodal involvement[121,129]. The biggest setback in EUS evaluation is still interobserver variation. Notwithstanding, endoscopic ultrasonography has become the most valuable tool in diagnostics of esophageal submucosal tumors[129].
The role of EUS in establishing the feasibility of endoscopic resection of superficial gastric lesions is still controversial. ESD is indicated as the treatment of choice for most gastric superficial neoplastic lesions, including low- or high-grade non-invasive neoplasia and adenocarcinoma with no evidence of deep submucosal invasion[130-133]. Although EUS is considered a reliable method for locoregional staging, endoscopic evaluation is still favored over EUS for predicting endoscopic resectability[134]. We should also highlight different approaches in the use of EUS before intervention. Although favored in the prior planning of endoscopic resection in Western countries, in the Eastern countries (in which the incidence of gastric cancer is notably higher), it is not considered necessary to perform EUS in the preoperative evaluation prior to the planned intervention[131,135,136].
Since ESD has been achieving similar results compared with surgery in treatment of gastric submucosal tumors (< 50 mm in size), the role of the EUS in preoperative management has recently evolved[137]. Today, it is the main tool in preoperative assessment, including evaluation of size, layer of origin, and echo pattern. Furthermore, the use of EUS has extended to marking the lesion with EUS-assisted injection into the muscularis propria, providing a deeper safety cushion for submucosal dissection procedure[138].
A randomized study by Fernandez-Esparrach et al[139] concluded that EUS and MRI have similar accuracy in T and N staging for rectal cancer. The ESGE recommends using one of these methods for staging of rectal cancer, but not for colon cancer[122]. However, the role of EUS and MRI for superficial lesions has been undefined.
A prospective study comparing high frequency EUS vs magnifying chromoendoscopy in early colorectal neoplasia showed that high frequency EUS was superior to chromoendoscopy in determining the depth of invasion, showing an accuracy of 93% vs 59%[140]. Nevertheless, endoscopic resection will probably remain the best staging tool for superficial rectal lesions, and if the endoscopist feels the lesion is endoscopically resectable, it will probably not require preoperative EUS[122]. On the other hand, according to the ESGE recommendations, the use of EUS or MRI should be considered for rectal lesions with endoscopic features suspected for submucosal invasion, since the finding of suspicious lymph nodes could be an indication for neoadjuvant treatment[122].
To summarize, the role of EUS in ESD is still evolving. The main goal of the endoscopic ultrasonography remains to evaluate a potential submucosal invasion and locoregional staging of the disease. Future research on the role of EUS in ESD should be concentrated in reduction of interobserver variations and alleviating possible complications.
CONCLUSION
Even though recent technological advancements in endoscopic approaches led to an improvement of outcomes of tumors in the abdominal cavity, as indicated by reduced mortality, morbidity, and palliative care, we are still far from having an optimal treatment, particularly for pancreatic cancer. Nonetheless, the novel EUS-guided approaches (RFA, brachytherapy, FNI, etc.) for pancreatic cancer might be crucial in overcoming the problem of drug distribution to tumorous tissue and reducing the required therapeutic doses and incidence of adverse effects. In addition, alleviating extreme pain that many patients with pancreatic cancer endure seems to be achievable through celiac plexus neurolysis. Furthermore, EUS is already a part of the algorithm in management of PCN, where EUS-FNA is the method of choice in case of appearance of certain alarming features of cysts.
The utility of EUS in PV interventions is most prominent in relation to the staging of HCC. The role of EUS in ESD with respect to management of precancerous and some early cancer lesions in GI tract, as well as EUS-guided treatment of various hepatic cancers, is yet to be determined, as current data is insufficient to recommend these techniques as standards of care.
Footnotes
Conflict-of-interest statement: The authors declare no conflicts of interest.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review started: February 21, 2021
First decision: May 8, 2021
Article in press: August 27, 2021
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Croatia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jagielski M S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
Contributor Information
Andre Bratanic, Department of Gastroenterology and Hepatology, University Hospital of Split, Split 21000, Croatia.
Dorotea Bozic, Department of Gastroenterology and Hepatology, University Hospital of Split, Split 21000, Croatia.
Antonio Mestrovic, Department of Gastroenterology and Hepatology, University Hospital of Split, Split 21000, Croatia.
Dinko Martinovic, Department of Pathophysiology, University of Split School of Medicine, Split 21000, Croatia.
Marko Kumric, Department of Pathophysiology, University of Split School of Medicine, Split 21000, Croatia.
Tina Ticinovic Kurir, Department of Pathophysiology, University of Split School of Medicine, Split 21000, Croatia; Department of Endocrinology, University Hospital of Split, Split 21000, Croatia.
Josko Bozic, Department of Pathophysiology, University of Split School of Medicine, Split 21000, Croatia. josko.bozic@mefst.hr.
References
- 1.Yan BM, Van Dam J. Endoscopic ultrasound-guided intratumoral therapy for pancreatic cancer. Can J Gastroenterol. 2008;22:405–410. doi: 10.1155/2008/104398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cazacu IM, Singh BS, Saftoiu A, Bhutani MS. Endoscopic Ultrasound-Guided Treatment of Pancreatic Cancer. Curr Gastroenterol Rep. 2020;22:27. doi: 10.1007/s11894-020-00767-1. [DOI] [PubMed] [Google Scholar]
- 3.Aguirre AJ, Collisson EA. Advances in the Genetics and Biology of Pancreatic Cancer. Cancer J. 2017;23:315–320. doi: 10.1097/PPO.0000000000000286. [DOI] [PubMed] [Google Scholar]
- 4.Hajatdoost L, Sedaghat K, Walker EJ, Thomas J, Kosari S. Chemotherapy in Pancreatic Cancer: A Systematic Review. Medicina (Kaunas) 2018;54 doi: 10.3390/medicina54030048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.LeVeen R. Laser hyperthermia and radiofrequency ablation of hepatic lesions. Semin Interv Radiol. 1997;205:313–324. [Google Scholar]
- 6.Haen SP, Pereira PL, Salih HR, Rammensee HG, Gouttefangeas C. More than just tumor destruction: immunomodulation by thermal ablation of cancer. Clin Dev Immunol. 2011;2011:160250. doi: 10.1155/2011/160250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Waitz R, Solomon SB. Can local radiofrequency ablation of tumors generate systemic immunity against metastatic disease? Radiology. 2009;251:1–2. doi: 10.1148/radiol.2511082215. [DOI] [PubMed] [Google Scholar]
- 8.Teng LS, Jin KT, Han N, Cao J. Radiofrequency ablation, heat shock protein 70 and potential anti-tumor immunity in hepatic and pancreatic cancers: a minireview. Hepatobiliary Pancreat Dis Int. 2010;9:361–365. [PubMed] [Google Scholar]
- 9.Giardino A, Innamorati G, Ugel S, Perbellini O, Girelli R, Frigerio I, Regi P, Scopelliti F, Butturini G, Paiella S, Bacchion M, Bassi C. Immunomodulation after radiofrequency ablation of locally advanced pancreatic cancer by monitoring the immune response in 10 patients. Pancreatology. 2017;17:962–966. doi: 10.1016/j.pan.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 10.European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182–236. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 11.Goldberg SN, Mallery S, Gazelle GS, Brugge WR. EUS-guided radiofrequency ablation in the pancreas: results in a porcine model. Gastrointest Endosc. 1999;50:392–401. doi: 10.1053/ge.1999.v50.98847. [DOI] [PubMed] [Google Scholar]
- 12.Kim HJ, Seo DW, Hassanuddin A, Kim SH, Chae HJ, Jang JW, Park DH, Lee SS, Lee SK, Kim MH. EUS-guided radiofrequency ablation of the porcine pancreas. Gastrointest Endosc. 2012;76:1039–1043. doi: 10.1016/j.gie.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 13.Lee JM, Han JK, Kim HC, Choi YH, Kim SH, Choi JY, Choi BI. Switching monopolar radiofrequency ablation technique using multiple, internally cooled electrodes and a multichannel generator: ex vivo and in vivo pilot study. Invest Radiol. 2007;42:163–171. doi: 10.1097/01.rli.0000252495.44818.b3. [DOI] [PubMed] [Google Scholar]
- 14.Gaidhane M, Smith I, Ellen K, Gatesman J, Habib N, Foley P, Moskaluk C, Kahaleh M. Endoscopic Ultrasound-Guided Radiofrequency Ablation (EUS-RFA) of the Pancreas in a Porcine Model. Gastroenterol Res Pract. 2012;2012:431451. doi: 10.1155/2012/431451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu Y, Tang Z, Fang H, Gao S, Chen J, Wang Y, Yan H. High operative risk of cool-tip radiofrequency ablation for unresectable pancreatic head cancer. J Surg Oncol. 2006;94:392–395. doi: 10.1002/jso.20580. [DOI] [PubMed] [Google Scholar]
- 16.Spiliotis JD, Datsis AC, Michalopoulos NV, Kekelos SP, Vaxevanidou A, Rogdakis AG, Christopoulou AN. Radiofrequency ablation combined with palliative surgery may prolong survival of patients with advanced cancer of the pancreas. Langenbecks Arch Surg. 2007;392:55–60. doi: 10.1007/s00423-006-0098-5. [DOI] [PubMed] [Google Scholar]
- 17.Elias D, Baton O, Sideris L, Lasser P, Pocard M. Necrotizing pancreatitis after radiofrequency destruction of pancreatic tumors. Eur J Surg Oncol. 2004;30:85–87. doi: 10.1016/j.ejso.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 18.Girelli R, Frigerio I, Giardino A, Regi P, Gobbo S, Malleo G, Salvia R, Bassi C. Results of 100 pancreatic radiofrequency ablations in the context of a multimodal strategy for stage III ductal adenocarcinoma. Langenbecks Arch Surg. 2013;398:63–69. doi: 10.1007/s00423-012-1011-z. [DOI] [PubMed] [Google Scholar]
- 19.Paiella S, Salvia R, Ramera M, Girelli R, Frigerio I, Giardino A, Allegrini V, Bassi C. Local Ablative Strategies for Ductal Pancreatic Cancer (Radiofrequency Ablation, Irreversible Electroporation): A Review. Gastroenterol Res Pract. 2016;2016:4508376. doi: 10.1155/2016/4508376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Varshney S, Sewkani A, Sharma S, Kapoor S, Naik S, Sharma A, Patel K. Radiofrequency ablation of unresectable pancreatic carcinoma: feasibility, efficacy and safety. JOP. 2006;7:74–78. [PubMed] [Google Scholar]
- 21.Siriwardena AK. Radiofrequency ablation for locally advanced cancer of the pancreas. JOP. 2006;7:1–4. [PubMed] [Google Scholar]
- 22.Casadei R, Ricci C, Pezzilli R, Serra C, Calculli L, Morselli-Labate AM, Santini D, Minni F. A prospective study on radiofrequency ablation locally advanced pancreatic cancer. Hepatobiliary Pancreat Dis Int. 2010;9:306–311. [PubMed] [Google Scholar]
- 23.Giardino A, Girelli R, Frigerio I, Regi P, Cantore M, Alessandra A, Lusenti A, Salvia R, Bassi C, Pederzoli P. Triple approach strategy for patients with locally advanced pancreatic carcinoma. HPB (Oxford) 2013;15:623–627. doi: 10.1111/hpb.12027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tang Z, Wu YL, Fang HQ, Xu J, Mo GQ, Chen XM, Gao SL, Li JT, Liu YB, Wang Y. [Treatment of unresectable pancreatic carcinoma by radiofrequency ablation with 'cool-tip needle': report of 18 cases] Zhonghua Yi Xue Za Zhi. 2008;88:391–394. [PubMed] [Google Scholar]
- 25.Matsui Y, Nakagawa A, Kamiyama Y, Yamamoto K, Kubo N, Nakase Y. Selective thermocoagulation of unresectable pancreatic cancers by using radiofrequency capacitive heating. Pancreas. 2000;20:14–20. doi: 10.1097/00006676-200001000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Cantore M, Girelli R, Mambrini A, Frigerio I, Boz G, Salvia R, Giardino A, Orlandi M, Auriemma A, Bassi C. Combined modality treatment for patients with locally advanced pancreatic adenocarcinoma. Br J Surg. 2012;99:1083–1088. doi: 10.1002/bjs.8789. [DOI] [PubMed] [Google Scholar]
- 27.Song TJ, Seo DW, Lakhtakia S, Reddy N, Oh DW, Park DH, Lee SS, Lee SK, Kim MH. Initial experience of EUS-guided radiofrequency ablation of unresectable pancreatic cancer. Gastrointest Endosc. 2016;83:440–443. doi: 10.1016/j.gie.2015.08.048. [DOI] [PubMed] [Google Scholar]
- 28.Dhaliwal A, Kolli S, Dhindsa BS, Choa J, Mashiana HS, Ramai D, Chandan S, Bhogal N, Sayles H, Bhat I, Singh S, Adler DG. Efficacy of EUS-RFA in pancreatic tumors: Is it ready for prime time? Endosc Int Open. 2020;8:E1243–E1251. doi: 10.1055/a-1221-5012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DiMaio CJ, Nagula S, Goodman KA, Ho AY, Markowitz AJ, Schattner MA, Gerdes H. EUS-guided fiducial placement for image-guided radiation therapy in GI malignancies by using a 22-gauge needle (with videos) Gastrointest Endosc. 2010;71:1204–1210. doi: 10.1016/j.gie.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 30.Lennon AM, Newman N, Makary MA, Edil BH, Shin EJ, Khashab MA, Hruban RH, Wolfgang CL, Schulick RD, Giday S, Canto MI. EUS-guided tattooing before laparoscopic distal pancreatic resection (with video) Gastrointest Endosc. 2010;72:1089–1094. doi: 10.1016/j.gie.2010.07.023. [DOI] [PubMed] [Google Scholar]
- 31.Chang KJ, Nguyen PT, Thompson JA, Kurosaki TT, Casey LR, Leung EC, Granger GA. Phase I clinical trial of allogeneic mixed lymphocyte culture (cytoimplant) delivered by endoscopic ultrasound-guided fine-needle injection in patients with advanced pancreatic carcinoma. Cancer. 2000;88:1325–1335. doi: 10.1002/(sici)1097-0142(20000315)88:6<1325::aid-cncr8>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 32.Herman JM, Wild AT, Wang H, Tran PT, Chang KJ, Taylor GE, Donehower RC, Pawlik TM, Ziegler MA, Cai H, Savage DT, Canto MI, Klapman J, Reid T, Shah RJ, Hoffe SE, Rosemurgy A, Wolfgang CL, Laheru DA. Randomized phase III multi-institutional study of TNFerade biologic with fluorouracil and radiotherapy for locally advanced pancreatic cancer: final results. J Clin Oncol. 2013;31:886–894. doi: 10.1200/JCO.2012.44.7516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee JC, Shin DW, Park H, Kim J, Youn Y, Kim JH, Hwang JH. Tolerability and safety of EUS-injected adenovirus-mediated double-suicide gene therapy with chemotherapy in locally advanced pancreatic cancer: a phase 1 trial. Gastrointest Endosc. 2020;92:1044–1052.e1. doi: 10.1016/j.gie.2020.02.012. [DOI] [PubMed] [Google Scholar]
- 34.Nakai Y, Chang KJ. EUS-guided fine-needle injection for pancreatic cancer: back to the future. Gastrointest Endosc. 2020;92:1053–1054. doi: 10.1016/j.gie.2020.06.025. [DOI] [PubMed] [Google Scholar]
- 35.Nishimura M, Matsukawa M, Fujii Y, Matsuda Y, Arai T, Ochiai Y, Itoi T, Yahagi N. Effects of EUS-guided intratumoral injection of oligonucleotide STNM01 on tumor growth, histology, and overall survival in patients with unresectable pancreatic cancer. Gastrointest Endosc. 2018;87:1126–1131. doi: 10.1016/j.gie.2017.10.030. [DOI] [PubMed] [Google Scholar]
- 36.Levy MJ, Alberts SR, Bamlet WR, Burch PA, Farnell MB, Gleeson FC, Haddock MG, Kendrick ML, Oberg AL, Petersen GM, Takahashi N, Chari ST. EUS-guided fine-needle injection of gemcitabine for locally advanced and metastatic pancreatic cancer. Gastrointest Endosc. 2017;86:161–169. doi: 10.1016/j.gie.2016.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Handley WS. PANCREATIC CANCER AND ITS TREATMENT BY IMPLANTED RADIUM. Ann Surg. 1934;100:215–223. doi: 10.1097/00000658-193407000-00021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shipley WU, Nardi GL, Cohen AM, Ling CC. Iodine-125 implant and external beam irradiation in patients with localized pancreatic carcinoma: a comparative study to surgical resection. Cancer. 1980;45:709–714. doi: 10.1002/1097-0142(19800215)45:4<709::aid-cncr2820450416>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 39.Westlin JE, Andersson-Forsman C, Garske U, Linné T, Aas M, Glimelius B, Lindgren PG, Order SE, Nilsson S. Objective responses after fractionated infusional brachytherapy of unresectable pancreatic adenocarcinomas. Cancer. 1997;80:2743–2748. doi: 10.1002/(sici)1097-0142(19971215)80:12+<2743::aid-cncr54>3.3.co;2-4. [DOI] [PubMed] [Google Scholar]
- 40.DeNittis AS, Stambaugh MD, Lang P, Wallner PE, Lustig RA, Dillman RO, Order SE. Complete remission of nonresectable pancreatic cancer after infusional colloidal phosphorus-32 brachytherapy, external beam radiation therapy, and 5-fluorouracil: a preliminary report. Am J Clin Oncol. 1999;22:355–360. doi: 10.1097/00000421-199908000-00006. [DOI] [PubMed] [Google Scholar]
- 41.Mutignani M, Shah SK, Morganti AG, Perri V, Macchia G, Costamagna G. Treatment of unresectable pancreatic carcinoma by intraluminal brachytherapy in the duct of Wirsung. Endoscopy. 2002;34:555–559. doi: 10.1055/s-2002-33214. [DOI] [PubMed] [Google Scholar]
- 42.Peretz T, Nori D, Hilaris B, Manolatos S, Linares L, Harrison L, Anderson LL, Fuks Z, Brennan MF. Treatment of primary unresectable carcinoma of the pancreas with I-125 implantation. Int J Radiat Oncol Biol Phys. 1989;17:931–935. doi: 10.1016/0360-3016(89)90138-7. [DOI] [PubMed] [Google Scholar]
- 43.Rosemurgy A, Luzardo G, Cooper J, Bowers C, Zervos E, Bloomston M, Al-Saadi S, Carroll R, Chheda H, Carey L, Goldin S, Grundy S, Kudryk B, Zwiebel B, Black T, Briggs J, Chervenick P. 32P as an adjunct to standard therapy for locally advanced unresectable pancreatic cancer: a randomized trial. J Gastrointest Surg. 2008;12:682–688. doi: 10.1007/s11605-007-0430-6. [DOI] [PubMed] [Google Scholar]
- 44.Goertz SR, Ali MM, Parker GA. Local management of pancreatic carcinoma: iodine-125 implantation. Clin Oncol (R Coll Radiol) 1990;2:22–26. doi: 10.1016/s0936-6555(05)80214-6. [DOI] [PubMed] [Google Scholar]
- 45.Sun S, Xu H, Xin J, Liu J, Guo Q, Li S. Endoscopic ultrasound-guided interstitial brachytherapy of unresectable pancreatic cancer: results of a pilot trial. Endoscopy. 2006;38:399–403. doi: 10.1055/s-2006-925253. [DOI] [PubMed] [Google Scholar]
- 46.Jin Z, Du Y, Li Z, Jiang Y, Chen J, Liu Y. Endoscopic ultrasonography-guided interstitial implantation of iodine 125-seeds combined with chemotherapy in the treatment of unresectable pancreatic carcinoma: a prospective pilot study. Endoscopy. 2008;40:314–320. doi: 10.1055/s-2007-995476. [DOI] [PubMed] [Google Scholar]
- 47.Sun X, Lu Z, Wu Y, Min M, Bi Y, Shen W, Xu Y, Li Z, Jin Z, Liu Y. An endoscopic ultrasonography-guided interstitial brachytherapy based special treatment-planning system for unresectable pancreatic cancer. Oncotarget. 2017;8:79099–79110. doi: 10.18632/oncotarget.15763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bhutani MS, Klapman JB, Tuli R, El-Haddad G, Hoffe S, Wong FCL, Chasen B, Fogelman DR, Lo SK, Nissen NN, Hendifar AE, Varadhachary G, Katz MHG, Erwin WD, Koay EJ, Tamm EP, Singh BS, Mehta R, Wolff RA, Soman A, Cazacu IM, Herman JM. An open-label, single-arm pilot study of EUS-guided brachytherapy with phosphorus-32 microparticles in combination with gemcitabine +/- nab-paclitaxel in unresectable locally advanced pancreatic cancer (OncoPaC-1): Technical details and study protocol. Endosc Ultrasound. 2020;9:24–30. doi: 10.4103/eus.eus_44_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.World Health Organization. Cancer Pain Relief, 2nd ed. WHO: Geneva, Switzerland, 2006. [Google Scholar]
- 50.Kaufman M, Singh G, Das S, Concha-Parra R, Erber J, Micames C, Gress F. Efficacy of endoscopic ultrasound-guided celiac plexus block and celiac plexus neurolysis for managing abdominal pain associated with chronic pancreatitis and pancreatic cancer. J Clin Gastroenterol. 2010;44:127–134. doi: 10.1097/MCG.0b013e3181bb854d. [DOI] [PubMed] [Google Scholar]
- 51.Wiersema MJ, Wiersema LM. Endosonography-guided celiac plexus neurolysis. Gastrointest Endosc. 1996;44:656–662. doi: 10.1016/s0016-5107(96)70047-0. [DOI] [PubMed] [Google Scholar]
- 52. NCCN Guidelines for Adult Cancer Pain. Version 1. 2020. [cited 10 February 2021] Available from: https://www.nccn.org/professionals/physician_gls/pdf/pain.pdf .
- 53.Rai P, Cr L, Kc H. Endoscopic ultrasound-guided celiac plexus neurolysis improves pain in gallbladder cancer. Indian J Gastroenterol. 2020;39:171–175. doi: 10.1007/s12664-019-01003-z. [DOI] [PubMed] [Google Scholar]
- 54.Puli SR, Reddy JB, Bechtold ML, Antillon MR, Brugge WR. EUS-guided celiac plexus neurolysis for pain due to chronic pancreatitis or pancreatic cancer pain: a meta-analysis and systematic review. Dig Dis Sci. 2009;54:2330–2337. doi: 10.1007/s10620-008-0651-x. [DOI] [PubMed] [Google Scholar]
- 55.Wyse JM, Carone M, Paquin SC, Usatii M, Sahai AV. Randomized, double-blind, controlled trial of early endoscopic ultrasound-guided celiac plexus neurolysis to prevent pain progression in patients with newly diagnosed, painful, inoperable pancreatic cancer. J Clin Oncol. 2011;29:3541–3546. doi: 10.1200/JCO.2010.32.2750. [DOI] [PubMed] [Google Scholar]
- 56.Sahai AV, Lemelin V, Lam E, Paquin SC. Central vs. bilateral endoscopic ultrasound-guided celiac plexus block or neurolysis: a comparative study of short-term effectiveness. Am J Gastroenterol. 2009;104:326–329. doi: 10.1038/ajg.2008.64. [DOI] [PubMed] [Google Scholar]
- 57.Penman ID. State of the art: putting EUS-guided block/neurolysis into perspective. Gastrointest Endosc. 2009;69:S174–S175. doi: 10.1016/j.gie.2008.12.023. [DOI] [PubMed] [Google Scholar]
- 58.Arcidiacono PG, Calori G, Carrara S, McNicol ED, Testoni PA. Celiac plexus block for pancreatic cancer pain in adults. Cochrane Database Syst Rev. 2011:CD007519. doi: 10.1002/14651858.CD007519.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fujii-Lau LL, Bamlet WR, Eldrige JS, Chari ST, Gleeson FC, Abu Dayyeh BK, Clain JE, Pearson RK, Petersen BT, Rajan E, Topazian MD, Vege SS, Wang KK, Wiersema MJ, Levy MJ. Impact of celiac neurolysis on survival in patients with pancreatic cancer. Gastrointest Endosc. 2015;82:46–56.e2. doi: 10.1016/j.gie.2014.12.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Doi S, Yasuda I, Kawakami H, Hayashi T, Hisai H, Irisawa A, Mukai T, Katanuma A, Kubota K, Ohnishi T, Ryozawa S, Hara K, Itoi T, Hanada K, Yamao K. Endoscopic ultrasound-guided celiac ganglia neurolysis vs. celiac plexus neurolysis: a randomized multicenter trial. Endoscopy. 2013;45:362–369. doi: 10.1055/s-0032-1326225. [DOI] [PubMed] [Google Scholar]
- 61.Levy MJ, Topazian MD, Wiersema MJ, Clain JE, Rajan E, Wang KK, de la Mora JG, Gleeson FC, Pearson RK, Pelaez MC, Petersen BT, Vege SS, Chari ST. Initial evaluation of the efficacy and safety of endoscopic ultrasound-guided direct Ganglia neurolysis and block. Am J Gastroenterol. 2008;103:98–103. doi: 10.1111/j.1572-0241.2007.01607.x. [DOI] [PubMed] [Google Scholar]
- 62.Sakamoto H, Kitano M, Kamata K, Komaki T, Imai H, Chikugo T, Takeyama Y, Kudo M. EUS-guided broad plexus neurolysis over the superior mesenteric artery using a 25-gauge needle. Am J Gastroenterol. 2010;105:2599–2606. doi: 10.1038/ajg.2010.339. [DOI] [PubMed] [Google Scholar]
- 63.Alvarez-Sánchez MV, Jenssen C, Faiss S, Napoléon B. Interventional endoscopic ultrasonography: an overview of safety and complications. Surg Endosc. 2014;28:712–734. doi: 10.1007/s00464-013-3260-5. [DOI] [PubMed] [Google Scholar]
- 64.Del Chiaro M, Verbeke C, Salvia R, Klöppel G, Werner J, McKay C, Friess H, Manfredi R, Van Cutsem E, Löhr M, Segersvärd R European Study Group on Cystic Tumors of the Pancreas. European experts consensus statement on cystic tumors of the pancreas. Dig Liver Dis. 2013;45:703–711. doi: 10.1016/j.dld.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 65.Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, Salvia R, Shimizu Y, Tada M, Wolfgang CL. Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology. 2017;17:738–753. doi: 10.1016/j.pan.2017.07.007. [DOI] [PubMed] [Google Scholar]
- 66.European Study Group on Cystic Tumors of the Pancreas. European evidence-based guidelines on pancreatic cystic neoplasms. Gut. 2018;67:789–804. doi: 10.1136/gutjnl-2018-316027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ip IK, Mortele KJ, Prevedello LM, Khorasani R. Focal cystic pancreatic lesions: assessing variation in radiologists' management recommendations. Radiology. 2011;259:136–141. doi: 10.1148/radiol.10100970. [DOI] [PubMed] [Google Scholar]
- 68.Girometti R, Intini S, Brondani G, Como G, Londero F, Bresadola F, Zuiani C, Bazzocchi M. Incidental pancreatic cysts on 3D turbo spin echo magnetic resonance cholangiopancreatography: prevalence and relation with clinical and imaging features. Abdom Imaging. 2011;36:196–205. doi: 10.1007/s00261-010-9618-4. [DOI] [PubMed] [Google Scholar]
- 69.Chang YR, Park JK, Jang JY, Kwon W, Yoon JH, Kim SW. Incidental pancreatic cystic neoplasms in an asymptomatic healthy population of 21,745 individuals: Large-scale, single-center cohort study. Medicine (Baltimore) 2016;95:e5535. doi: 10.1097/MD.0000000000005535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.de Jong K, Nio CY, Hermans JJ, Dijkgraaf MG, Gouma DJ, van Eijck CH, van Heel E, Klass G, Fockens P, Bruno MJ. High prevalence of pancreatic cysts detected by screening magnetic resonance imaging examinations. Clin Gastroenterol Hepatol. 2010;8:806–811. doi: 10.1016/j.cgh.2010.05.017. [DOI] [PubMed] [Google Scholar]
- 71.Del Chiaro M, Segersvärd R, Lohr M, Verbeke C. Early detection and prevention of pancreatic cancer: is it really possible today? World J Gastroenterol. 2014;20:12118–12131. doi: 10.3748/wjg.v20.i34.12118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Del Chiaro M, Segersvärd R, Pozzi Mucelli R, Rangelova E, Kartalis N, Ansorge C, Arnelo U, Blomberg J, Löhr M, Verbeke C. Comparison of preoperative conference-based diagnosis with histology of cystic tumors of the pancreas. Ann Surg Oncol. 2014;21:1539–1544. doi: 10.1245/s10434-013-3465-9. [DOI] [PubMed] [Google Scholar]
- 73.Vege SS, Ziring B, Jain R, Moayyedi P Clinical Guidelines Committee; American Gastroenterology Association. American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology. 2015;148:819–22; quiz e12. doi: 10.1053/j.gastro.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 74.Jaeschke R, Guyatt GH, Dellinger P, Schünemann H, Levy MM, Kunz R, Norris S, Bion J GRADE Working Group. Use of GRADE grid to reach decisions on clinical practice guidelines when consensus is elusive. BMJ. 2008;337:a744. doi: 10.1136/bmj.a744. [DOI] [PubMed] [Google Scholar]
- 75.van Huijgevoort NCM, Del Chiaro M, Wolfgang CL, van Hooft JE, Besselink MG. Diagnosis and management of pancreatic cystic neoplasms: current evidence and guidelines. Nat Rev Gastroenterol Hepatol. 2019;16:676–689. doi: 10.1038/s41575-019-0195-x. [DOI] [PubMed] [Google Scholar]
- 76.Allen PJ, D'Angelica M, Gonen M, Jaques DP, Coit DG, Jarnagin WR, DeMatteo R, Fong Y, Blumgart LH, Brennan MF. A selective approach to the resection of cystic lesions of the pancreas: results from 539 consecutive patients. Ann Surg. 2006;244:572–582. doi: 10.1097/01.sla.0000237652.84466.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kiely JM, Nakeeb A, Komorowski RA, Wilson SD, Pitt HA. Cystic pancreatic neoplasms: enucleate or resect? J Gastrointest Surg. 2003;7:890–897. doi: 10.1007/s11605-003-0035-7. [DOI] [PubMed] [Google Scholar]
- 78.Horvath KD, Chabot JA. An aggressive resectional approach to cystic neoplasms of the pancreas. Am J Surg. 1999;178:269–274. doi: 10.1016/s0002-9610(99)00186-5. [DOI] [PubMed] [Google Scholar]
- 79.Goh BK, Tan YM, Cheow PC, Chung YF, Chow PK, Wong WK, Ooi LL. Cystic lesions of the pancreas: an appraisal of an aggressive resectional policy adopted at a single institution during 15 years. Am J Surg. 2006;192:148–154. doi: 10.1016/j.amjsurg.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 80.Oh HC, Seo DW, Song TJ, Moon SH, Park DH, Soo Lee S, Lee SK, Kim MH, Kim J. Endoscopic ultrasonography-guided ethanol lavage with paclitaxel injection treats patients with pancreatic cysts. Gastroenterology. 2011;140:172–179. doi: 10.1053/j.gastro.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 81.DeWitt J, McGreevy K, Schmidt CM, Brugge WR. EUS-guided ethanol vs saline solution lavage for pancreatic cysts: a randomized, double-blind study. Gastrointest Endosc. 2009;70:710–723. doi: 10.1016/j.gie.2009.03.1173. [DOI] [PubMed] [Google Scholar]
- 82.Moyer MT, Sharzehi S, Mathew A, Levenick JM, Headlee BD, Blandford JT, Heisey HD, Birkholz JH, Ancrile BB, Maranki JL, Gusani NJ, McGarrity TJ, Dye CE. The Safety and Efficacy of an Alcohol-Free Pancreatic Cyst Ablation Protocol. Gastroenterology. 2017;153:1295–1303. doi: 10.1053/j.gastro.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 83.Choi JH, Seo DW, Song TJ, Park DH, Lee SS, Lee SK, Kim MH. Long-term outcomes after endoscopic ultrasound-guided ablation of pancreatic cysts. Endoscopy. 2017;49:866–873. doi: 10.1055/s-0043-110030. [DOI] [PubMed] [Google Scholar]
- 84.Oh HC, Seo DW. Endoscopic ultrasonography-guided pancreatic cyst ablation (with video) J Hepatobiliary Pancreat Sci. 2015;22:16–19. doi: 10.1002/jhbp.179. [DOI] [PubMed] [Google Scholar]
- 85.Ho KY, Brugge WR EUS 2008 Working Group. EUS 2008 Working Group document: evaluation of EUS-guided pancreatic-cyst ablation. Gastrointest Endosc. 2009;69:S22–S27. doi: 10.1016/j.gie.2008.10.059. [DOI] [PubMed] [Google Scholar]
- 86.Gómez V, Takahashi N, Levy MJ, McGee KP, Jones A, Huang Y, Chari ST, Clain JE, Gleeson FC, Pearson RK, Petersen BT, Rajan E, Vege SS, Topazian MD. EUS-guided ethanol lavage does not reliably ablate pancreatic cystic neoplasms (with video) Gastrointest Endosc. 2016;83:914–920. doi: 10.1016/j.gie.2015.08.069. [DOI] [PubMed] [Google Scholar]
- 87.DeWitt J, DiMaio CJ, Brugge WR. Long-term follow-up of pancreatic cysts that resolve radiologically after EUS-guided ethanol ablation. Gastrointest Endosc. 2010;72:862–866. doi: 10.1016/j.gie.2010.02.039. [DOI] [PubMed] [Google Scholar]
- 88.Tanaka M, Fernández-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, Kimura W, Levy P, Pitman MB, Schmidt CM, Shimizu M, Wolfgang CL, Yamaguchi K, Yamao K International Association of Pancreatology. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology. 2012;12:183–197. doi: 10.1016/j.pan.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 89.de Jong K, van Hooft JE, Nio CY, Gouma DJ, Dijkgraaf MG, Bruno MJ, Fockens P. Accuracy of preoperative workup in a prospective series of surgically resected cystic pancreatic lesions. Scand J Gastroenterol. 2012;47:1056–1063. doi: 10.3109/00365521.2012.674970. [DOI] [PubMed] [Google Scholar]
- 90.Brugge WR, Lewandrowski K, Lee-Lewandrowski E, Centeno BA, Szydlo T, Regan S, del Castillo CF, Warshaw AL. Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology. 2004;126:1330–1336. doi: 10.1053/j.gastro.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 91.Cizginer S, Turner BG, Bilge AR, Karaca C, Pitman MB, Brugge WR. Cyst fluid carcinoembryonic antigen is an accurate diagnostic marker of pancreatic mucinous cysts. Pancreas. 2011;40:1024–1028. doi: 10.1097/MPA.0b013e31821bd62f. [DOI] [PubMed] [Google Scholar]
- 92.Sedlack R, Affi A, Vazquez-Sequeiros E, Norton ID, Clain JE, Wiersema MJ. Utility of EUS in the evaluation of cystic pancreatic lesions. Gastrointest Endosc. 2002;56:543–547. doi: 10.1067/mge.2002.128106. [DOI] [PubMed] [Google Scholar]
- 93.Koito K, Namieno T, Nagakawa T, Shyonai T, Hirokawa N, Morita K. Solitary cystic tumor of the pancreas: EUS-pathologic correlation. Gastrointest Endosc. 1997;45:268–276. doi: 10.1016/s0016-5107(97)70269-4. [DOI] [PubMed] [Google Scholar]
- 94.Morris-Stiff G, Lentz G, Chalikonda S, Johnson M, Biscotti C, Stevens T, Matthew Walsh R. Pancreatic cyst aspiration analysis for cystic neoplasms: mucin or carcinoembryonic antigen--which is better? Surgery. 2010;148:638–644; discussion 644. doi: 10.1016/j.surg.2010.07.023. [DOI] [PubMed] [Google Scholar]
- 95.Thornton GD, McPhail MJ, Nayagam S, Hewitt MJ, Vlavianos P, Monahan KJ. Endoscopic ultrasound guided fine needle aspiration for the diagnosis of pancreatic cystic neoplasms: a meta-analysis. Pancreatology. 2013;13:48–57. doi: 10.1016/j.pan.2012.11.313. [DOI] [PubMed] [Google Scholar]
- 96.Dumonceau JM, Deprez PH, Jenssen C, Iglesias-Garcia J, Larghi A, Vanbiervliet G, Aithal GP, Arcidiacono PG, Bastos P, Carrara S, Czakó L, Fernández-Esparrach G, Fockens P, Ginès À, Havre RF, Hassan C, Vilmann P, van Hooft JE, Polkowski M. Indications, results, and clinical impact of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline - Updated January 2017. Endoscopy. 2017;49:695–714. doi: 10.1055/s-0043-109021. [DOI] [PubMed] [Google Scholar]
- 97.Ohno E, Hirooka Y, Itoh A, Ishigami M, Katano Y, Ohmiya N, Niwa Y, Goto H. Intraductal papillary mucinous neoplasms of the pancreas: differentiation of malignant and benign tumors by endoscopic ultrasound findings of mural nodules. Ann Surg. 2009;249:628–634. doi: 10.1097/SLA.0b013e3181a189a8. [DOI] [PubMed] [Google Scholar]
- 98.Nara S, Onaya H, Hiraoka N, Shimada K, Sano T, Sakamoto Y, Esaki M, Kosuge T. Preoperative evaluation of invasive and noninvasive intraductal papillary-mucinous neoplasms of the pancreas: clinical, radiological, and pathological analysis of 123 cases. Pancreas. 2009;38:8–16. doi: 10.1097/MPA.0b013e318181b90d. [DOI] [PubMed] [Google Scholar]
- 99.Wu J, Jiao Y, Dal Molin M, Maitra A, de Wilde RF, Wood LD, Eshleman JR, Goggins MG, Wolfgang CL, Canto MI, Schulick RD, Edil BH, Choti MA, Adsay V, Klimstra DS, Offerhaus GJ, Klein AP, Kopelovich L, Carter H, Karchin R, Allen PJ, Schmidt CM, Naito Y, Diaz LA Jr, Kinzler KW, Papadopoulos N, Hruban RH, Vogelstein B. Whole-exome sequencing of neoplastic cysts of the pancreas reveals recurrent mutations in components of ubiquitin-dependent pathways. Proc Natl Acad Sci U S A. 2011;108:21188–21193. doi: 10.1073/pnas.1118046108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Canto MI, Hruban RH. Managing pancreatic cysts: less is more? Gastroenterology. 2015;148:688–691. doi: 10.1053/j.gastro.2015.02.033. [DOI] [PubMed] [Google Scholar]
- 101.Fernández-Del Castillo C, Tanaka M. Management of pancreatic cysts: the evidence is not here yet. Gastroenterology. 2015;148:685–687. doi: 10.1053/j.gastro.2015.02.034. [DOI] [PubMed] [Google Scholar]
- 102.Crippa S, Pezzilli R, Bissolati M, Capurso G, Romano L, Brunori MP, Calculli L, Tamburrino D, Piccioli A, Ruffo G, Fave GD, Falconi M. Active Surveillance Beyond 5 Years Is Required for Presumed Branch-Duct Intraductal Papillary Mucinous Neoplasms Undergoing Non-Operative Management. Am J Gastroenterol. 2017;112:1153–1161. doi: 10.1038/ajg.2017.43. [DOI] [PubMed] [Google Scholar]
- 103.Lawrence SA, Attiyeh MA, Seier K, Gönen M, Schattner M, Haviland DL, Balachandran VP, Kingham TP, D'Angelica MI, DeMatteo RP, Brennan MF, Jarnagin WR, Allen PJ. Should Patients With Cystic Lesions of the Pancreas Undergo Long-term Radiographic Surveillance? Ann Surg. 2017;266:536–544. doi: 10.1097/SLA.0000000000002371. [DOI] [PubMed] [Google Scholar]
- 104.Jais B, Rebours V, Malleo G, Salvia R, Fontana M, Maggino L, Bassi C, Manfredi R, Moran R, Lennon AM, Zaheer A, Wolfgang C, Hruban R, Marchegiani G, Fernández Del Castillo C, Brugge W, Ha Y, Kim MH, Oh D, Hirai I, Kimura W, Jang JY, Kim SW, Jung W, Kang H, Song SY, Kang CM, Lee WJ, Crippa S, Falconi M, Gomatos I, Neoptolemos J, Milanetto AC, Sperti C, Ricci C, Casadei R, Bissolati M, Balzano G, Frigerio I, Girelli R, Delhaye M, Bernier B, Wang H, Jang KT, Song DH, Huggett MT, Oppong KW, Pererva L, Kopchak KV, Del Chiaro M, Segersvard R, Lee LS, Conwell D, Osvaldt A, Campos V, Aguero Garcete G, Napoleon B, Matsumoto I, Shinzeki M, Bolado F, Fernandez JM, Keane MG, Pereira SP, Acuna IA, Vaquero EC, Angiolini MR, Zerbi A, Tang J, Leong RW, Faccinetto A, Morana G, Petrone MC, Arcidiacono PG, Moon JH, Choi HJ, Gill RS, Pavey D, Ouaïssi M, Sastre B, Spandre M, De Angelis CG, Rios-Vives MA, Concepcion-Martin M, Ikeura T, Okazaki K, Frulloni L, Messina O, Lévy P. Serous cystic neoplasm of the pancreas: a multinational study of 2622 patients under the auspices of the International Association of Pancreatology and European Pancreatic Club (European Study Group on Cystic Tumors of the Pancreas) Gut. 2016;65:305–312. doi: 10.1136/gutjnl-2015-309638. [DOI] [PubMed] [Google Scholar]
- 105.Chapman CG, Waxman I. EUS-guided portal vein sampling. Endosc Ultrasound. 2018;7:240–245. doi: 10.4103/eus.eus_28_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kayar Y, Turkdogan KA, Baysal B, Unver N, Danalioglu A, Senturk H. EUS-guided FNA of a portal vein thrombus in hepatocellular carcinoma. Pan Afr Med J. 2015;21:86. doi: 10.11604/pamj.2015.21.86.6991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Garg R, Rustagi T. Endoscopic Ultrasound-guided Portal Venous Access: Diagnostic and Therapeutic Implications. J Clin Gastroenterol. 2017;51:677–682. doi: 10.1097/MCG.0000000000000897. [DOI] [PubMed] [Google Scholar]
- 108.Moreno M, Gimeno-García AZ, Corriente MM, Nicolás-Pérez D, Brito-García A, García-Castro C, Quintero E. EUS-FNA of a portal vein thrombosis in a patient with a hidden hepatocellular carcinoma: confirmation technique after contrast-enhanced ultrasound. Endoscopy. 2014;46 Suppl 1 UCTN:E590–E591. doi: 10.1055/s-0034-1390734. [DOI] [PubMed] [Google Scholar]
- 109.Gimeno Garcia AZ, Aparicio JR, Barturen A, Moreno M, Nicolas-Perez D, Quintero E. Short article: Endoscopic ultrasound-guided fine-needle aspiration of portal vein thrombosis in patients with chronic liver disease and suspicion of hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2018;30:418–423. doi: 10.1097/MEG.0000000000001094. [DOI] [PubMed] [Google Scholar]
- 110.Park TY, Seo DW, Kang HJ, Cho MK, Song TJ, Park DH, Lee SS, Lee SK, Kim MH. Endoscopic ultrasonography-guided placement of a transhepatic portal vein stent in a live porcine model. Endosc Ultrasound. 2016;5:315–319. doi: 10.4103/2303-9027.191611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Faigel D, Lake D, Landreth T, Kelman C, Marler R. Endoscopic ultrasonography-guided portal injection chemotherapy for hepatic metastases. Endosc Ultrasound. 2014;3:S1. [PMC free article] [PubMed] [Google Scholar]
- 112.Faigel DO, Lake DF, Landreth TL, Kelman CC, Marler RJ. EUS-guided portal injection chemotherapy for treatment of hepatic metastases: feasibility in the acute porcine model. Gastrointest Endosc. 2016;83:444–446. doi: 10.1016/j.gie.2015.08.064. [DOI] [PubMed] [Google Scholar]
- 113.Park TY, Seo DW, Kang HJ, Song TJ, Park DH, Lee SS, Lee SK, Kim MH. Feasibility and safety of EUS-guided selective portal vein embolization with a coil and cyanoacrylate in a live porcine model. Endosc Ultrasound. 2018;7:389–394. doi: 10.4103/eus.eus_18_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Matthes K, Sahani D, Holalkere NS, Mino-Kenudson M, Brugge WR. Feasibility of endoscopic ultrasound-guided portal vein embolization with Enteryx. Acta Gastroenterol Belg. 2005;68:412–415. [PubMed] [Google Scholar]
- 115.Chua T, Faigel DO. Endoscopic Ultrasound-Guided Ablation of Liver Tumors. Gastrointest Endosc Clin N Am. 2019;29:369–379. doi: 10.1016/j.giec.2018.11.007. [DOI] [PubMed] [Google Scholar]
- 116.Carrara S, Arcidiacono PG, Albarello L, Addis A, Enderle MD, Boemo C, Neugebauer A, Campagnol M, Doglioni C, Testoni PA. Endoscopic ultrasound-guided application of a new internally gas-cooled radiofrequency ablation probe in the liver and spleen of an animal model: a preliminary study. Endoscopy. 2008;40:759–763. doi: 10.1055/s-2008-1077520. [DOI] [PubMed] [Google Scholar]
- 117.Varadarajulu S, Jhala NC, Drelichman ER. EUS-guided radiofrequency ablation with a prototype electrode array system in an animal model (with video) Gastrointest Endosc. 2009;70:372–376. doi: 10.1016/j.gie.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 118.Jiang T, Tian G, Bao H, Chen F, Deng Z, Li J, Chai W. EUS dating with laser ablation against the caudate lobe or left liver tumors: a win-win proposition? Cancer Biol Ther. 2018;19:145–152. doi: 10.1080/15384047.2017.1414760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Di Matteo F, Grasso R, Pacella CM, Martino M, Pandolfi M, Rea R, Luppi G, Silvestri S, Zardi E, Costamagna G. EUS-guided Nd:YAG laser ablation of a hepatocellular carcinoma in the caudate lobe. Gastrointest Endosc. 2011;73:632–636. doi: 10.1016/j.gie.2010.08.019. [DOI] [PubMed] [Google Scholar]
- 120.Tang RSY, Kyaw MH, Teoh AYB, Lui RNS, Tse YK, Lam TYT, Chan SL, Wong VWS, Wu JCY, Lau JYW, Sung JJY. Endoscopic ultrasound-guided cyanoacrylate injection to prevent rebleeding in hepatocellular carcinoma patients with variceal hemorrhage. J Gastroenterol Hepatol. 2020;35:2192–2201. doi: 10.1111/jgh.15168. [DOI] [PubMed] [Google Scholar]
- 121.Han Y, Sun S, Guo J, Ge N, Wang S, Liu X, Wang G, Hu J. Is endoscopic ultrasonography useful for endoscopic submucosal dissection? Endosc Ultrasound. 2016;5:284–290. doi: 10.4103/2303-9027.191606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Pimentel-Nunes P, Dinis-Ribeiro M, Ponchon T, Repici A, Vieth M, De Ceglie A, Amato A, Berr F, Bhandari P, Bialek A, Conio M, Haringsma J, Langner C, Meisner S, Messmann H, Morino M, Neuhaus H, Piessevaux H, Rugge M, Saunders BP, Robaszkiewicz M, Seewald S, Kashin S, Dumonceau JM, Hassan C, Deprez PH. Endoscopic submucosal dissection: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy. 2015;47:829–854. doi: 10.1055/s-0034-1392882. [DOI] [PubMed] [Google Scholar]
- 123.Japan Esophageal Society. Japanese Classification of Esophageal Cancer, 11th Edition: part I. Esophagus. 2017;14:1–36. doi: 10.1007/s10388-016-0551-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Thosani N, Singh H, Kapadia A, Ochi N, Lee JH, Ajani J, Swisher SG, Hofstetter WL, Guha S, Bhutani MS. Diagnostic accuracy of EUS in differentiating mucosal vs submucosal invasion of superficial esophageal cancers: a systematic review and meta-analysis. Gastrointest Endosc. 2012;75:242–253. doi: 10.1016/j.gie.2011.09.016. [DOI] [PubMed] [Google Scholar]
- 125.May A, Günter E, Roth F, Gossner L, Stolte M, Vieth M, Ell C. Accuracy of staging in early oesophageal cancer using high resolution endoscopy and high resolution endosonography: a comparative, prospective, and blinded trial. Gut. 2004;53:634–640. doi: 10.1136/gut.2003.029421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Larghi A, Lightdale CJ, Memeo L, Bhagat G, Okpara N, Rotterdam H. EUS followed by EMR for staging of high-grade dysplasia and early cancer in Barrett's esophagus. Gastrointest Endosc. 2005;62:16–23. doi: 10.1016/s0016-5107(05)00319-6. [DOI] [PubMed] [Google Scholar]
- 127.Pech O, Günter E, Dusemund F, Ell C. Value of high-frequency miniprobes and conventional radial endoscopic ultrasound in the staging of early Barrett's carcinoma. Endoscopy. 2010;42:98–103. doi: 10.1055/s-0029-1243839. [DOI] [PubMed] [Google Scholar]
- 128.Pech O, May A, Günter E, Gossner L, Ell C. The impact of endoscopic ultrasound and computed tomography on the TNM staging of early cancer in Barrett's esophagus. Am J Gastroenterol. 2006;101:2223–2229. doi: 10.1111/j.1572-0241.2006.00718.x. [DOI] [PubMed] [Google Scholar]
- 129.Ko WJ, Song GW, Cho JY. Evaluation and Endoscopic Management of Esophageal Submucosal Tumor. Clin Endosc. 2017;50:250–253. doi: 10.5946/ce.2016.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Chung IK, Lee JH, Lee SH, Kim SJ, Cho JY, Cho WY, Hwangbo Y, Keum BR, Park JJ, Chun HJ, Kim HJ, Kim JJ, Ji SR, Seol SY. Therapeutic outcomes in 1000 cases of endoscopic submucosal dissection for early gastric neoplasms: Korean ESD Study Group multicenter study. Gastrointest Endosc. 2009;69:1228–1235. doi: 10.1016/j.gie.2008.09.027. [DOI] [PubMed] [Google Scholar]
- 131.Gotoda T, Jung HY. Endoscopic resection (endoscopic mucosal resection/ endoscopic submucosal dissection) for early gastric cancer. Dig Endosc. 2013;25 Suppl 1:55–63. doi: 10.1111/den.12003. [DOI] [PubMed] [Google Scholar]
- 132.Lian J, Chen S, Zhang Y, Qiu F. A meta-analysis of endoscopic submucosal dissection and EMR for early gastric cancer. Gastrointest Endosc. 2012;76:763–770. doi: 10.1016/j.gie.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 133.Park YM, Cho E, Kang HY, Kim JM. The effectiveness and safety of endoscopic submucosal dissection compared with endoscopic mucosal resection for early gastric cancer: a systematic review and metaanalysis. Surg Endosc. 2011;25:2666–2677. doi: 10.1007/s00464-011-1627-z. [DOI] [PubMed] [Google Scholar]
- 134.Choi J, Kim SG, Im JP, Kim JS, Jung HC, Song IS. Comparison of endoscopic ultrasonography and conventional endoscopy for prediction of depth of tumor invasion in early gastric cancer. Endoscopy. 2010;42:705–713. doi: 10.1055/s-0030-1255617. [DOI] [PubMed] [Google Scholar]
- 135.Gotoda T, Yamamoto H, Soetikno RM. Endoscopic submucosal dissection of early gastric cancer. J Gastroenterol. 2006;41:929–942. doi: 10.1007/s00535-006-1954-3. [DOI] [PubMed] [Google Scholar]
- 136.Ajani JA, Bentrem DJ, Besh S, D'Amico TA, Das P, Denlinger C, Fakih MG, Fuchs CS, Gerdes H, Glasgow RE, Hayman JA, Hofstetter WL, Ilson DH, Keswani RN, Kleinberg LR, Korn WM, Lockhart AC, Meredith K, Mulcahy MF, Orringer MB, Posey JA, Sasson AR, Scott WJ, Strong VE, Varghese TK Jr, Warren G, Washington MK, Willett C, Wright CD, McMillian NR, Sundar H National Comprehensive Cancer Network. Gastric cancer, version 2.2013: featured updates to the NCCN Guidelines. J Natl Compr Canc Netw. 2013;11:531–546. doi: 10.6004/jnccn.2013.0070. [DOI] [PubMed] [Google Scholar]
- 137.Meng FS, Zhang ZH, Hong YY, Li DJ, Lin JQ, Chen X, Ji F. Comparison of endoscopic submucosal dissection and surgery for the treatment of gastric submucosal tumors originating from the muscularis propria layer: a single-center study (with video) Surg Endosc. 2016;30:5099–5107. doi: 10.1007/s00464-016-4860-7. [DOI] [PubMed] [Google Scholar]
- 138.Fujii LL, Gomez V, Song LM, Levy MJ. Endoscopic ultrasound-assisted endoscopic submucosal dissection of a gastric subepithelial tumor. Endoscopy. 2013;45 Suppl 2 UCTN:E225–E226. doi: 10.1055/s-0033-1344157. [DOI] [PubMed] [Google Scholar]
- 139.Fernández-Esparrach G, Ayuso-Colella JR, Sendino O, Pagés M, Cuatrecasas M, Pellisé M, Maurel J, Ayuso-Colella C, González-Suárez B, Llach J, Castells A, Ginès A. EUS and magnetic resonance imaging in the staging of rectal cancer: a prospective and comparative study. Gastrointest Endosc. 2011;74:347–354. doi: 10.1016/j.gie.2011.03.1257. [DOI] [PubMed] [Google Scholar]
- 140.Hurlstone DP, Brown S, Cross SS, Shorthouse AJ, Sanders DS. High magnification chromoscopic colonoscopy or high frequency 20 MHz mini probe endoscopic ultrasound staging for early colorectal neoplasia: a comparative prospective analysis. Gut. 2005;54:1585–1589. doi: 10.1136/gut.2005.069849. [DOI] [PMC free article] [PubMed] [Google Scholar]



