Abstract
Background
The COVID-19 pandemic and associated policy responses, such as physical distancing interventions, pose risks to mental health that could be mitigated by social support systems. We examine associations between changes in mental health in the population aged 50 years and older in Europe and stringency of pandemic responses and social protection.
Methods
We analysed data from the Survey of Health, Ageing and Retirement in Europe: n = 50,278 individuals aged 50 years and older in 26 European countries between June and August 2020. Linear multivariable regression models were used to evaluate potential risk factors for deterioration in self-reported mental health and investigate whether social protection systems mitigate it.
Results
Across the European Union, 28.1% (95% CI:27.1–29.2) of participants reported worsening mental health since the beginning of the pandemic, ranging from 16.1% in Slovakia to 54.8% in Portugal. Factors associated with increased risk of deterioration included: being female (12.7 percentage points (ppt), 95%CI:9.2–16.2); experiencing unmet healthcare needs during the pandemic (14.6 ppt, 95%CI:11.2–18.1); job loss during the pandemic (6.2 ppt, 95%CI:1.1–11.8); and financial hardship (5.1 ppt, 95%CI:2.9–7.2). Greater stringency of physical distancing measures in countries was associated with worsening mental health (0.2 ppt per each one point increase on a stringency index, 95% CI:0.09–0.4); however, country-level pre-pandemic expenditures on various social protection packages was associated with decreased probability of worsening mental health (−1.3 ppt, 95%CI: 0.3 to −2.3 per €1,000 increase in health care expenditures per capita and, among the unemployed, −3.8 ppt, 95%CI: 1.6 to −2.4 per €100 increase in unemployment expenditure per capita).
Conclusions
The COVID-19 pandemic has been associated with substantial mental health deterioration exhibiting social inequalities. Adverse mental health has been exacerbated by policy responses to the pandemic regulating physical distancing, but social protection expenditure might have helped mitigate the impact. Strengthening social protection systems might render the mental health of the population more resilient to the consequences of crises such as the COVID-19 pandemic.
Keywords: COVID-19, Mental health, Older adults, Europe, Socioeconomic inequalities, Containment measures, Physical distancing, Social protection
Highlights
-
•
Multi-country study on mental health in the population aged 50 years and older in Europe during the COVID-19 pandemic.
-
•
Mental health decline among older adults varies by socioeconomic group.
-
•
More stringent physical distancing increases mental health decline in older adults.
-
•
Stronger social protection might have mitigated risk of worse mental health in older adults.
1. Introduction
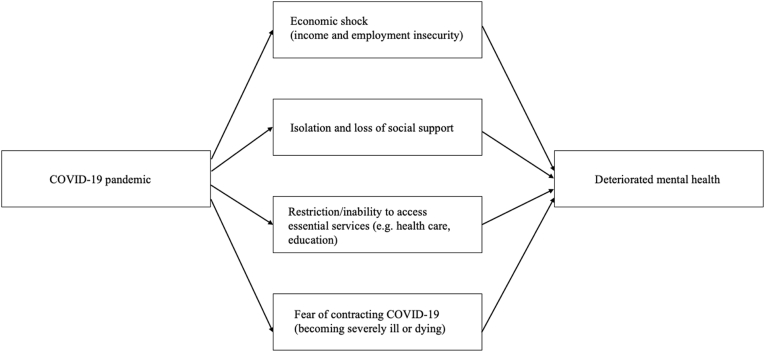
The COVID-19 pandemic and corresponding responses have massively disrupted daily life in many countries, with profound consequences for mental health and wellbeing, especially those whose lives were already precarious. In response, the United Nations has called for mental health protection to be made a policy priority (United Nations Secretary-General Policy Brief, 2020). Mental health is threatened by multiple pandemic-related stressors, including insecurity of income and employment, isolation, and loss of social support, inability to access essential services such as health and education, and fear of contracting COVID-19 and becoming severely ill or dying.
A review of the evidence on the psychological impact of quarantine found that most studies reported negative psychological effects (Brooks et al., 2020), and systematic reviews on the specific impact of the COVID-19 pandemic on mental health found a deterioration of mental health in the general population, but with significant differences among socioeconomic groups (Vindegaard & Benros, 2020; Wang et al., 2020; Xiong et al., 2020). Several more recent studies have also found similar findings (Ettman et al., 2020; Fancourt et al., 2021; González-Sanguino et al., 2020; Pan et al., 2021; M. Pierce, Hope, et al., 2020). Although some of these studies have used data representative of populations, many use non-representative samples, such as those recruited using the internet, which can introduce bias as those who experience digital exclusion, including many older or poorer people or those with mental illness, and who are at increased risk from both COVID-19 and policy responses, may be excluded (Sounderajah et al., 2021). As a consequence, there have been calls for greater use of high-quality representative data that can provide more robust evidence on the impact of the pandemic on mental health (Holmes et al., 2020; Matthias Pierce, McManus, et al., 2020b).
Underrepresentation of older people is especially problematic. The World Health Organization has viewed the mental health of older adults as a particular concern in the COVID-19 pandemic, especially those who are isolated or experience cognitive decline (World Health Organization, 2020c), as older population have been at highest risk of complications and death from COVID-19 (Lloyd-Sherlock et al., 2020). On the other hand, there is some evidence that older adults may be more resilient, at least in the short-term, to some of the harms arising from the COVID-19 pandemic (Vahia et al., 2020). However, depression outcomes among older populations are, as in all population groups, characterized by sociodemographic inequalities (Richardson et al., 2020). Additionally, the pattern of sociodemographic inequalities varies substantially across countries (Richardson et al., 2020). The apparent mental health resilience of older adults to the effects of the COVID-19 pandemic may also vary across countries, as will the exposure of older adults to risk and protective factors (World Health Organization, 2020a), plausibly because of differences in policy responses that offer protection.
Countries have adopted different responses to control of the pandemic. They entered it with different social support systems, with implications for their resilience to adversity, shocks, and crises. Social protection policies can provide a safety net to protect against the negative consequences of adverse life events and conditions, while promoting social and health equity. A study from the United States found that people living in states with more supportive social policies experienced less impact on mental health when exposed to COVID-19-related household income shocks (Donnelly & Farina, 2021). Given the often more generous welfare regimes in European countries, we might expect to see at least the same effect, but the greater diversity in Europe may offer additional insights. Thus, different social protection systems might be expected to offer differing levels of protection.
Here we seek a broad understanding of how older people in Europe have experienced the effects of the pandemic on mental health, looking first at socioeconomic inequalities and stressors placed upon the population, such as income and employment insecurity and potential isolation resulting from physical and social distancing measures. Second, measures that might mitigate these effects, in the form of existing social protection measures. We thus use harmonised cross-national, nationally representative survey data to provide estimates of the prevalence of self-reported decline in mental health during the COVID-19 pandemic. We describe differences within the population aged 50 years or older and among 26 European countries, with a focus on socioeconomic characteristics of participants before and during the pandemic, assessing whether the stringency of policy responses to the pandemic in Europe, in terms of containment and closure measures, affected the mental health of older populations. Finally, we test whether and to what extent social protection expenditures influence their mental health.
2. Methods
2.1. Sources of data
We used data from the Survey of Health, Ageing and Retirement in Europe (SHARE) COVID-19 survey. Details of the dataset have been describe elsewhere (Börsch-Supan et al., 2013). Briefly, SHARE COVID-19 is a cross-sectional dataset with information on health, social and environmental characteristics of adults aged 50 years or older in 27 European countries and Israel, with samples that are nationally representative. The SHARE COVID-19 data were collected via computer-assisted telephone interviews between June and August 2020 using a survey harmonised ex-ante and translated into the national languages (Börsch-Supan, 2020).
The SHARE COVID-19 cross-sectional dataset contains data on 50,278 individuals (representing, when weighted, a population of 180,358,661 individuals) aged 50 years or older who reported whether their mental health status had worsened from before the pandemic. Information on survey non-response is currently not available. Respondents are from the 26 European countries for which there are publicly available data (25 European Union countries (which excludes Austria and Ireland because data were not available) and Switzerland. The countries included are Belgium, Bulgaria, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Italy, Lithuania, Luxembourg, Latvia, Malta, Netherlands, Poland, Portugal, Romania, Slovakia, Slovenia, Spain, Sweden, and Switzerland. Israel was not included in this study.
SHARE is a multinational survey using probability-based sampling. Because data are collected by national agencies, differences in sampling methods and resources between countries exist, particularly in access to official person registries covering the population of interest including information on age. SHARE sampling details for each country can be found elsewhere (Bergmann et al., 2019; Börsch-Supan, 2020; Börsch-Supan et al., 2013). All respondents provided informed consent.
Data on social protection system expenditures were taken from Eurostat for the latest available year (2018) (Eurostat, 2021). Data on country-level COVID-19 incidence as of 1st June of 2020 and data on the stringency of government policy measures were taken from Our World in Data database, which are sourced, respectively, from Johns Hopkins University (Dong et al., 2020) and the Oxford Coronavirus Government Response Tracker (OxCGRT) (Hale et al., 2021).
2.2. Outcome measure
Worsened mental health was measured as self-reported decline in mental health between the inception of the pandemic and the month prior to responding to the survey. Specifically, it combined data collected in response to four questions asking: “In the last month, have you been sad or depressed?” and “In the last month, have you felt nervous, anxious or on edge?“, both questions followed by “Has that been more so, less so, or about the same as before the outbreak of Corona?“. For the first two questions, the possible answers were either positive or negative. Those who responded affirmatively were asked the last question, with possible answers “More so”, “Less so” or “About the same”. We classified individuals who responded “More so” to either the question referring to sadness and/or depression or the question about having felt nervous, anxious, and/or on edge as having experienced worsened mental health during the outbreak; all other responses were classified as not having experienced worsened mental health.
2.3. Individual-level socio-economic and health measures
To capture the socioeconomic impact of the pandemic on mental health, we included a series of variables on demographic and socioeconomic characteristics before and during the pandemic that measured income insecurity, unemployment, and socialization. We also capture the impact of health-related variables during the pandemic on worsened mental health, including the impact of personally experiencing COVID-19 or having someone close experience it, as well as the effect of foregone healthcare. Fig. 1 illustrates the pathways of pandemic-related stressors on mental health deterioration.
Fig. 1.
DAG of the pathways of pandemic-related stressors on mental health deterioration.
The included variables are age, an ordinal variable categorized in the following three groups: 50–64 years old, 65–79 years old, and 80 years old and older; gender, a dichotomous variable with the categories male and female; self-rated health before the pandemic is an ordinal variable measuring the self-reported health status of the respondent before the pandemic including the categories excellent, very good, good, fair, and poor; COVID-19 positive is a dichotomous variables measuring whether the responded had tested positive for the virus; anyone known with a COVID-19 positive test is a dichotomous variable measuring whether someone close to the respondent tested positive for the virus; foregone healthcare during the pandemic is a dichotomous variables that measures whether the respondent had impeded healthcare service access during the pandemic; household size is a dichotomous variable measuring whether the respondent lives alone or in a household of two people or more; working before the pandemic is a dichotomous variable capturing whether the respondent was working before the pandemic or was unemployed or retired; became unemployed during the pandemic is a dichotomous variable measuring whether among those working, the respondent became unemployed during the pandemic; and make ends meet is an ordinal variable measuring the ability of the household to live on their available economic resources during the pandemic and includes the categories with great difficulty, with some difficulty, fairly easily, and easily.
2.4. Lockdown measures
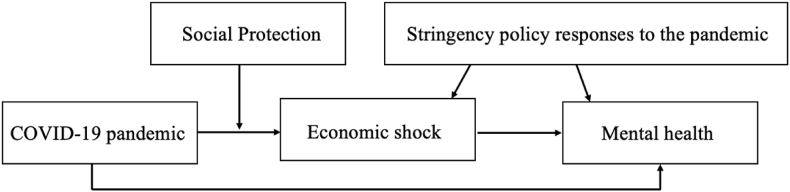
The severity of lockdown measures was captured using the Oxford Stringency Index of government policy responses to the coronavirus pandemic. Details on how OxCGRT constructs the Stringency Index are available elsewhere (Hale et al., 2021). Briefly, the Stringency Index aggregates various measures of governments’ responses to the pandemic capturing variations across countries in measures to increase physical distancing, such as school and work closures, stay-at-home orders, cancelling public events and restrictions on gathering sizes, public transport closures, and restrictions on internal and international travel. The Stringency Index measures policy responses per day since the January 1, 2020, taking a value between 1 and 100, where a higher score indicates a stricter government response. To capture the stringency of lockdown measures over time, we used the average of the daily values for the period between the day after the declaration of the outbreak as public health emergency of international concern by the World Health Organization (January 31, 2020) (World Health Organization, 2020b) and the initiation of the SHARE COVID-19 fieldwork (June 1, 2020) (Börsch-Supan, 2020). Fig. 2 illustrates the pathways of impact of lockdown measures directly on mental health deterioration (see pandemic-related stressor in Fig. 1) and through the economic shock associated to physical distancing measures.
Fig. 2.
DAG of the pathways of country-level determinants of mental health deterioration.
2.5. Social protection measures
To assess the role of each country's social protection system on the change in mental health during the pandemic, we incorporated a series of ecologic variables measuring national expenditure on social protection systems pre-pandemic, using data for 2018, the latest available year. These variables included spending on a full package of social protection benefits as well as on the categories of healthcare/sickness, old-age/pensions, and unemployment. The full package of social protection benefits comprises expenditures on disability, sickness/healthcare, old age, survivors, family/children, unemployment, housing, and social exclusion not covered elsewhere. Healthcare expenditures include current expenditures on healthcare goods and services. Pension expenditures include disability pension, early retirement due to reduced capacity to work, old-age pension, anticipated old-age pension, partial pension, survivors' pension, and early retirement due to labour market factors. Unemployment expenditures include spending on benefits for unemployed persons such as cash benefits, vocational training allowances, redundancy compensations, placement services and job search assistance. Data are measured as expenditures per inhabitant in Euros adjusted for purchasing power parities. Fig. 2 illustrates the pathway by which social protection expenditures might impact mental health, where social protection moderates the economic shock resulting from the pandemic-related physical distancing measures.
2.6. Statistical analyses
First, we report estimates of the prevalence of worsened mental health overall and disaggregated by mental health condition: depression and/or sadness, and feeling anxious, nervous, and/or on edge. We estimated prevalence as the proportion of individuals reporting having experienced an adverse mental health outcome. We also report the prevalence of worsened mental health by age, sex, COVID-19 infection status, ability of the individual's household to make ends meet, and by country. Chi-square tests for proportions and linear trend were performed to explore unadjusted statistical differences between groups. We used calibrated individual weights to adjust the prevalence estimates for the different selection probabilities and non-response rates.
Second, country fixed-effects multivariable linear probability models were used to evaluate individual-level determinants of change in the probability of worsened mental health (equation (1)), as follows:
| Worsened mental health i,c = α + β + βSocDemi,c + βHealth i,c + βCOVID-19 positive i,c + βForegone care i,c + βHousehold size i,c + βMake ends meet i,c +βEmployment i,c + μc + ε i,c | (1) |
where i is individual and c is country. Worsened mental health measures self-reported worsened mental health since the beginning of the pandemic. SocDem is a vector of sociodemographic variables, including age and gender. Health measures self-rated health before the pandemic and serves as an adjustment to limit the effect of confounding due to previous poor health. COVID-19 positive is a vector of two variables indicating whether the respondent tested positive for COVID-19 or someone close to them did. Employment is a vector of two variables measuring, first, whether the respondent was working before the pandemic, and, second, whether among those working, the respondent became unemployed during the pandemic. The other terms in the equation correspond to the definitions provided above. μ was used to capture unobserved country characteristics; ε is the error term. We report robust standard errors clustered by country to account for within country correlation and used calibrated individual weights.
Next, we used multivariable linear probability models to evaluate country-level determinants of worsened mental health. First, we test whether, in countries with a greater toll of the pandemic on population health measured as total cases per million inhabitant, mental health had further deteriorated. Second, we test whether in countries with more stringent lockdown response measures to the pandemic, individuals had worsened metal health. We evaluate this association with the overall stringency index as well as each of its components. Third, we test whether more generous social protection systems, measured as higher social protection expenditures, may mitigate mental health deterioration, for which we perform analyses for the overall sample or affected population subgroups. Calibrated individual weights were used in all models. Missing data were handled with pairwise deletion. Analyses were performed using Stata 16.1 (StataCorp, 2019).
3. Results
3.1. Prevalence of worsened mental health during the COVID-19 pandemic
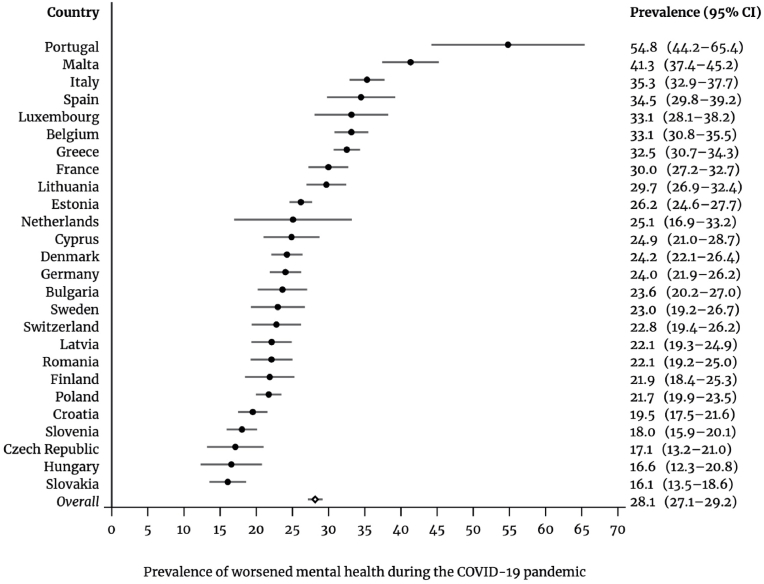
Across all countries, the prevalence of worsened mental health during the COVID-19 pandemic, compared to before, was 28.1% (95% CI: 27.1–29.2), ranging from 16.1% in Slovakia to 54.8% in Portugal (Fig. 3). Looking at each mental health condition, 18.1% of the respondents reported experiencing worsened depression and/or sadness, 22.1% worsened feelings of being anxious, nervous and/or on edge, and 12.0% reported experiencing both (Table 1).
Fig. 3.
Prevalence of worsened mental health due to the COVID-19 pandemic in 26 European countries, June–August 2020.
Table 1.
Descriptive statistics of study population, June–August 2020.
| N | Unweighted proportion or mean (SD) | Weighted proportion or mean (SD) | |
|---|---|---|---|
| Total sample | 50,278 | 100.0 | 100.0 |
| Total population | 180,358,661 | 100.0 | 100.0 |
| Sociodemographic variables | |||
| Age groups; 50–64 | 14,793 | 29.23 | 48.43 |
| 65-79 | 26,550 | 52.46 | 35.58 |
| 80+ | 9,266 | 18.31 | 15.99 |
| Gender; Female | 29,422 | 57.86 | 54.03 |
| Health-related variables | |||
| Worsened mental health; Yes | 13,504 | 26.69 | 28.14 |
| Worsened depression; Yes | 8,299 | 16.41 | 18.05 |
| Worsened anxiety; Yes | 10,820 | 21.39 | 22.13 |
| Worsened depression and anxiety; Yes | 5,615 | 11.04 | 11.97 |
| Self-rated health before pandemic; Excellent | 3,377 | 6.68 | 7.18 |
| Very good | 7,986 | 15.79 | 17.83 |
| Good | 22,455 | 44.39 | 47.01 |
| Fair | 13,155 | 26.01 | 22.06 |
| Poor | 3,608 | 7.13 | 5.93 |
| COVID-19 positive test; Yes | 238 | 0.47 | 0.77 |
| Anyone known COVID-19 positive test; Yes | 3,363 | 6.69 | 8.86 |
| Forgone healthcare during pandemic; Yes | 5,991 | 11.85 | 11.57 |
| Socioeconomic variables | |||
| Living alone; Yes | 12,301 | 24.19 | 27.07 |
| Working before pandemic; Yes | 10,744 | 21.25 | 32.88 |
| Became unemployed during pandemic; Yes | 1,949 | 3.85 | 6.67 |
| Make ends meet during pandemic; With great difficulty | 4,683 | 9.51 | 8.49 |
| With some difficulty | 12,993 | 26.38 | 23.79 |
| Fairly easily | 17,233 | 34.99 | 36.18 |
| Easily | 14,346 | 29.13 | 31.55 |
| Country-level variables | |||
| Total COVID-19 cases per million inhabitants | 26 countries | 2,090.89 (1,690.31) | 2,640.67 (1,468.72) |
| Stringency index of policy responses to the pandemic | 26 countries | 56.41 (7.39) | 61.15 (5.43) |
| Social protection expenditures per capita in Euros, PPS | 26 countries | 6,972.92 (3,001.77) | 8,161.31 (2,760.94) |
| Healthcare expenditures per capita in Euros, PPS | 26 countries | 1,936.97 (908.18) | 2,385.93 (1,072.76) |
| Unemployment expenditures per capita in Euros, PPS | 26 countries | 291.17 (208.32) | 359.77 (187.26) |
| Old age expenditures per capita in Euros, PPS | 26 countries | 2,935.51 (1,116.10) | 3,312.86 (923.18) |
SD: Standard deviation.
PPS: Purchasing parity standard.
The prevalence was higher for women, of whom 34.4% (95% CI: 33.1–35.7) reported worsened mental health during the pandemic, which is 13.7 percentage points (ppt) above the 20.7% (95% CI: 19.2–22.3) prevalence among men (Table 2). People aged 80 years or older reported slightly worsened mental health (30.6%, 95% CI: 29.0–32.2) compared to the age group 65–79 years old (27.1%, 95% CI: 26.1–27.9) but no different from the age group 50–64 years old (28.1%, 95% CI: 26.2–30.1). There was no trend in the reported prevalence estimates across age groups (p-value = 0.261). Individuals who had been infected with COVID-19 had a prevalence of worsened mental health of 41.7% (95% CI: 29.2–54.2), which was 13.7 ppt above the prevalence among those who had not contracted the virus (28.0%, 95% CI: 27.0–29.1). The prevalence of worsened mental health was also higher for people who had someone close to them who had been infected (33.5%, 95% CI: 28.7–38.4, vs. 27.6, 95% CI: 26.6–28.6). Looking at economic status, individuals with greater capacity to make ends meet were less likely to report worsened mental health (p-value <0.0001). Individuals who faced great difficulty making ends meet reported a 13.9 ppt higher prevalence than individuals who easily made ends meet (25.0%, 95% CI: 23.2–26.9 and 38.9%, 95% CI: 35.6–42.4, respectively). The prevalence of worsened mental health for those facing some difficulty making ends meet was 31.9% (95% CI: 29.6–34.1) and in those finding it fairly easy to make ends meet was 26.2% (95% CI: 24.5–27.8).
Table 2.
Prevalence of worsened mental health during the COVID-19 pandemic in 26 European countries by sociodemographic characteristics and COVID-19 infection status, June–August 2020.
| % | 95%CI | p-value | N | |
|---|---|---|---|---|
| Gender | ||||
| Male | 20.7 | 19.2–22.3 | P < 0.0001 a | 4,278 |
| Female | 34.4 | 33.1–35.7 | 9,133 | |
| Age group | ||||
| 50-64 | 28.1 | 26.2–30.1 | p = 0.279 ° | 3,956 |
| 65-79 | 27.1 | 26.1–27.9 | 6,821 | |
| 80+ | 30.6 | 29.0–32.2 | 2,634 | |
| Respondent had a COVID-19 positive test | ||||
| Yes | 41.7 | 29.2–54.2 | p = 0.021 a | 95 |
| No | 28.0 | 27.0–29.1 | 13,314 | |
| Someone close to respondent had a COVID-19 positive test | ||||
| Yes | 33.5 | 28.7–38.4 | p = 0.014 a | 1,118 |
| No | 27.6 | 26.6–28.6 | 12,204 | |
| Make ends meet during pandemic | ||||
| With great difficulty | 38.9 | 35.6–42.4 | P < 0.0001 ° | 1,742 |
| With some difficulty | 31.9 | 29.6–34.1 | 3,763 | |
| Fairly easily | 26.2 | 24.5–27.8 | 4,330 | |
| Easily | 25.0 | 23.2–26.9 | 3,276 | |
Chi-square test for proportions; °Chi-square test for trend.
Thus, we found that the greatest prevalence of worsened mental health occurred among individuals who had tested positive for COVID-19 (41.7%, 95% CI: 29.2–54.2), those with great difficulty to make ends meet (38.9%, 95% CI: 35.6–42.4), women (34.4%, 95% CI: 33.1–35.7), individuals who had someone close to them test positive for COVID-19 (33.5%, 95% CI: 28.7–38.4), individuals with some difficulty to make ends meet (31.9%, 95% CI: 29.6–34.1), and individuals aged 80 years old and older vs those aged 65–79 years old (30.6%, 95% CI: 29.0–32.2).
3.2. Risk factors for worsening mental health during the COVID-19 pandemic
Table 3 shows estimates of the change in the probability of reporting worsened mental health during the COVID-19 pandemic according to multiple individual-level determinants. Estimates from the fully adjusted regression model show that women had a 12.7 ppt higher probability than men of reporting worsened mental health (95% CI: 9.2–16.2). The probability of reporting worsened mental health was lower for individuals aged 80+, compared with those aged 50–65 (80+ vs 50–64 years old: 4.1 ppt, 95% CI: 0.7 to −7.5; 65–79 years old vs 50–64: 2.9 ppt, 95% CI: 7.2–1.4).
Table 3.
Individual-level determinants of change in the probability of worsened mental health during the COVID-19 pandemic in 26 European countries, June–August 2020.
| Worsened mental health during the COVID-19 pandemic |
|||
|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |
| Age group | |||
| 50-64 | reference | reference | reference |
| 65-79 | −0.00947 | −0.0308* | −0.0292 |
| (-0.0481–0.0292) | (-0.0615 to −0.0000496) | (-0.0721–0.0138) | |
| 80+ | 0.00418 | −0.0469*** | −0.0411* |
| (-0.0247–0.0330) | (-0.0664 to −0.0273) | (-0.0750 to −0.00719) | |
| Gender | |||
| Male | reference | reference | reference |
| Female | 0.137*** | 0.129*** | 0.127*** |
| (0.106–0.169) | (0.0964–0.162) | (0.0922–0.162) | |
| Self-rated health before pandemic | |||
| Excellent | reference | reference | |
| Very good | 0.0176 | 0.0134 | |
| (-0.0103–0.0454) | (-0.0185–0.0453) | ||
| Good | 0.0661*** | 0.0579** | |
| (0.0313–0.101) | (0.0221–0.0938) | ||
| Fair | 0.161*** | 0.146*** | |
| (0.129–0.193) | (0.112–0.181) | ||
| Poor | 0.232*** | 0.213*** | |
| (0.198–0.266) | (0.176–0.250) | ||
| Respondent COVID-19 positive | |||
| Not positive | reference | reference | |
| Positive | 0.112 | 0.125* | |
| (-0.00427–0.229) | (0.00706–0.243) | ||
| Anyone known COVID-19 positive | |||
| No | reference | reference | |
| Yes | 0.0260 | 0.0288 | |
| (-0.0224–0.0743) | (-0.0193–0.0769) | ||
| Forgone healthcare during pandemic | |||
| No | reference | reference | |
| Yes | 0.145*** | 0.142*** | |
| (0.122–0.168) | (0.120–0.165) | ||
| Living alone | |||
| 2 or more in household | reference | ||
| 1 person in household (living alone) | 0.0162* | ||
| (0.00128–0.0312) | |||
| Make ends meet during pandemic | |||
| Easily/Fairly easily | reference | ||
| With some/great difficulty | 0.0508*** | ||
| (0.0293–0.0724) | |||
| Working before pandemic | |||
| No or Retired | reference | ||
| Yes | −0.0141 | ||
| (-0.0370–0.00878) | |||
| Became unemployed during pandemic | |||
| No or Retired | reference | ||
| Yes | 0.0646* | ||
| (0.0110–0.118) | |||
| Number of individuals | 50278 | 49856 | 48566 |
| R2 | 0.048 | 0.079 | 0.083 |
95% confidence intervals in brackets.
*p < 0.05, **p < 0.01, ***p < 0.001.
Robust standard errors clustered by country; constant calculated but not shown; all models adjusted by country indicator variables.
Turning to direct experience of COVID-19, those who had tested positive were 12.5 ppt (95% CI: 0.7–24.3) more likely to report worsened mental health than those who had not but having someone close test positive had no effect (2.9 ppt, 95% CI: 1.9–7.7). Self-rated health before the pandemic showed a dose-response relationship with worsened mental health. Those whose general health had been worse were more likely to report worsening mental health (poor vs excellent health: 21.3 ppt, 95% CI: 17.6–25.0; fair vs excellent health: 14.6 ppt, 95% CI: 11.2–18.1; good vs excellent health: 5.8 ppt, 95% CI: 2.2–9.4; and very good vs excellent health: 1.3 ppt, 95% CI: 1.9–4.5). Individuals foregoing healthcare had a higher probability of reporting worsened mental health, by 14.2 ppt (95% CI: 12.0–16.5).
Living alone was associated with an increased probability of reporting mental health deterioration compared to living in a household with two or more people (1.6 ppt, 95% CI: 0.1–3.1).
Turning to economic risk factors, we observed that job loss and financial difficulty were associated with worsening mental health. We estimated that those who lost their job were 6.5 ppt (95% CI: 1.1–11.8) more likely to report worsened mental health compared with those who did not become unemployed or were already retired. We did not find that having being working or not before the pandemic had an effect on worsening mental health (−1.4 ppt, 95% CI: 3.7–0.9). Finally, those who reported some or great difficulty making ends meet had 5.1 ppt higher risk of worsening mental health (95% CI: 2.9–7.2) compared with those who did not have problems in this regard.
Thus, we found that the risk factors for worsened mental health with the greatest effect sizes were poor and fair self-rated health before the pandemic (21.3 ppt, 95% CI: 17.6–25.0; and 14.6 ppt, 95% CI: 11.2–18.1, respectively), foregone healthcare during the pandemic (14.2 ppt, 95% CI: 12.0–16.5), being female (12.7 ppt, 95% CI: 9.2–16.2), having tested positive for COVID-19 (12.5 ppt, 95% CI: 0.7–24.3), job loss (6.5 ppt, 95% CI: 1.1–11.8), good self-rated health before the pandemic (5.8 ppt, 95% CI: 2.2–9.4), some/great difficulty to make ends meet (5.1 ppt, 95% CI: 2.9–7.2), and living alone (1.6 ppt, 95% CI: 0.1–3.1). After adjusting for other risk factors, we found being aged 80 years old and older vs 50–64 years old (−4.1 ppt, 95% CI: 0.7 to −7.5) had a protective effect.
3.3. Country-level determinants of worsened mental health during the COVID-19 pandemic
Table 4 shows estimates of the impact on worsened mental health of the national toll of COVID-19 cases and of the stringency of policy responses to the pandemic. Countries with a higher number of COVID-19 cases had a greater risk of mental health deterioration (3.1 ppt, 95% CI: 2.3–3.9 per 1,000 cases increase). Next, we found that a higher overall stringency index was associated with a 0.2 ppt (95% CI: 0.1–0.3) increase in the probability of worsened mental health. Several components of the index had specific impacts on mental health deterioration, including workplace closures (6.6 ppt, 95% CI: 2.2–10.9), restrictions on gatherings (3.9 ppt, 95% CI: 0.8–6.9), public transportation closures (6.3 ppt; 95% CI: 2.3–10.2), and stay-at-home requirements (3.1 ppt, 95% CI: 0.6–5.7). We found that greater restrictions on international travel had a protective effect on mental health (−5.1 ppt, 95% CI: 1.7–8.5). No effect on mental health was found for components measuring the cancellation of public events (2.7 ppt, 95% CI: 2.4–3.1), the level of restrictions on national travel (−0.2 ppt, 95% CI: 2.5–2.0) and school closures (0.1 ppt, 95% CI: 2.9–3.1).
Table 4.
Impact of stringency of policy responses to the pandemic on the change in the probability of worsened mental health during the COVID-19 pandemic in 26 European countries, June–August 2020.
| Worsened mental health during the COVID-19 pandemic |
||
|---|---|---|
| Model 1 | Models 2-9 | |
| Total COVID-19 cases per million inhabitants | 0.0000313*** | |
| (0.0000234–0.0000392) | ||
| Stringency index of policy responses to the pandemic | 0.00237** | |
| (0.000895–0.00384) | ||
| Stringency index components: | ||
| C1 School closing | 0.000541 | |
| (-0.0294–0.0305) | ||
| C2 Workplace closing | 0.0655** | |
| (0.0222–0.109) | ||
| C3 Cancel public events | 0.0268 | |
| (-0.0237–0.0773) | ||
| C4 Restrictions on gathering size | 0.0387* | |
| (0.00830–0.0690) | ||
| C5 Close public transport | 0.0626** | |
| (0.0232–0.102) | ||
| C6 Stay at home requirements | 0.0311* | |
| (0.00560–0.0567) | ||
| C7 Restrictions on internal movement | −0.00248 | |
| (-0.0250–0.0200) | ||
| C8 Restrictions on international travel | −0.0514** | |
| (-0.0854–0.0174) | ||
| Number of individuals | 48566 | 48566 |
| Number of countries | 26 | 26 |
| R2 | 0.077 | – |
95% confidence intervals in brackets.
*p < 0.05, **p < 0.01, ***p < 0.001.
Constant calculated but not shown.
Models 1–9 are adjusted for all variables included in Model 3, Table 2.
Models 2–9 are adjusted for total COVID-19 cases per million inhabitants.
C: component.
Table 5 shows estimates of the association between a series of variables measuring expenditures on social protection benefits and worsened mental health, adjusting for the total number of COVID-19 cases and stringency of policy responses. For each additional €1,000 increase in expenditures on overall social protection benefits, reporting of worsened mental health decreased among those who became unemployed during the pandemic (−2.3 ppt, 95% CI: 0.6–4.1), individuals with poor/fair health (−0.8 ppt, 95% CI: 0.01–1.5), and among individuals aged ≥65 years (−0.5 ppt, 95% CI: 0.2–0.8). No effect of overall social protection spending was observed the population in general (−0.3 ppt, 95% CI: 0.7–0.1) and those facing difficulties making ends meet (0.2 ppt, 95% CI: 0.7–1.2). The same increase in spending on healthcare was associated with a protective effect on the mental health of the general population (−1.3 ppt, 95% CI: 0.3–2.3) and a stronger effect among those who reported poor health (−2.2 ppt, 95% CI: 0.3–4.0). In countries with higher spending on unemployment benefits, worsened mental health among the unemployed was ameliorated (−3.8 ppt, 95% CI: 0.5–7.1 per €100 increased spending; here, as opposed to Table 5, we report changes per €100 instead of €1,000 because the range of amounts paid in unemployment benefits among countries is substantially lower than for other social protection payments, as shown in Table 1). Differences in pension spending were not associated with the probability of reporting adverse mental health among people aged ≥65 (0.4 ppt, 95% CI: 0.6–1.4 per €1,000 increase in spending).
Table 5.
Impact of social protection expenditures on the change in the probability of worsened mental health during the COVID-19 pandemic in 26 European countries, June–August 2020.
| Worsened mental health during the COVID-19 pandemic |
||
|---|---|---|
| Models 1-9 | ||
| Sample | ||
| Per 1,000 € increase in social protection expenditures per capita | All | −0.00339 |
| (n = 49880) | (-0.00760–0.000829) | |
| Poor/fair health | −0.00787* | |
| (n = 16523) | (-0.0155 to −0.000261) | |
| Unemployed | −0.0233** | |
| (n = 1888) | (-0.0407 to −0.00592) | |
| ≥65 years old | −0.00499** | |
| (n = 35292) | (-0.00826 to −0.00172) | |
| Difficulty make ends meet | 0.00198 | |
| (n = 17423) | (-0.00767–0.0116) | |
| Per 1,000 € increase in health care/sickness expenditures per capita | All | −0.0130* |
| (n = 49880) | (-0.0230 to −0.00311) | |
| Poor/fair health | −0.0219* | |
| (n = 16523) | (-0.0404 to −0.00340) | |
| Per 1,000 € increase in unemployment benefits expenditures per capita | Unemployed | −0.380* |
| (n = 1888) | (-0.711 to −0.0504) | |
| Per 1,000 € increase in pensions/old age expenditures per capita | ≥65 years old | 0.00375 |
| (n = 35292) | (-0.00598–0.0135) | |
95% confidence intervals in brackets.
*p < 0.05, **p < 0.01, ***p < 0.001.
Constant calculated but not shown.
All models adjusted by age, gender, health status before the pandemic, tested positive for COVID-19 oneself or someone close, household size, total COVID-19 cases per million inhabitants, and stringency index of policy responses to the pandemic.
3.4. Sensitivity tests
We ran a series of sensitivity tests using the two components of the main outcome as outcome variables: worsened depression and worsened anxiety since the inception of the COVID-19 pandemic, observing that the findings did not substantially change, although in some instances the estimates’ effect sizes were smaller or greater than with the combined outcome (Online supplementary material).
4. Discussion
We found a substantial deterioration in mental health in persons aged 50 years and older between the beginning of the pandemic and June to August 2020. This was strongly associated with greater severity of physical distancing measures and exhibited substantial social inequalities, with people with poor and fair health, foregoing healthcare, women, and persons who experienced job loss and financial hardship during the pandemic suffering the most. Importantly, however, stronger social protection systems, as measured by greater spending, appeared to mitigate the risk of worsened mental health.
We observed great differences across countries in the prevalence of worsened mental health, again consistent with previous research (Wang et al., 2020). However, a consistent finding is that people in lower socioeconomic groups and women have been hardest hit. Individuals with worse overall health status before the pandemic were substantially more likely to experience mental health deterioration, as were individuals with unmet healthcare needs since the inception of the pandemic. This might suggest a relationship between COVID-19 comorbidities and deteriorating mental health. Also, those with a diagnosis of COVID-19 were more likely to experience further declines in mental health, which is aligned with findings from previous research (Taquet et al., 2021a, 2021b). This could be due to, or exacerbated by, fear of becoming severely ill or dying as well as disrupted health services provision (World Health Organization, 2020a), including reduced access to mental health services, either for ongoing conditions or for new ones arising since the inception of the pandemic.
Individuals who reported good overall health status during the pandemic also experienced declines in mental health, which may be due not only to COVID-19, but also the physical distancing measures and closure policies having impacted mental health, particularly through job loss and difficulties to make ends meet. In this context, greater social protection expenditures may have increased resilience during the pandemic as our social protection variable was measured pre-pandemic. That the expenditures measures are pre-pandemic might also explain why we found greater expenditures in a full package of social protection protected the mental health for some population subgroups (those with poor health, unemployed, and those aged 65 and older, all of who may have benefited from a stronger public health system, unemployment benefits, and old age pensions); however, greater expenditures in a full package of social protection did not protect the mental health of the whole population aged 50 years old and older as many may have not been directly benefiting from the social protection programmes until after the crisis began.
Our analysis has several limitations. First, we were unable to attribute worsened mental health with certainty to the pandemic and policy responses or some other event during this time frame. However, the outcome variable is based on a question inquiring whether mental health had worsened since the onset of the pandemic, which is likely to anchor it to the pandemic. While SHARE is a panel dataset, the timing of the wave, in summer 2020, means that we have no absolute measure of mental health just prior and subsequent to the onset of the pandemic but the additional question in the cross-sectional data, asking whether symptoms had worsened since the inception of the pandemic partially circumvents this limitation. Nonetheless, other studies using longitudinal designs have produced similar findings to ours (Ettman et al., 2020; González-Sanguino et al., 2020; Pan et al., 2021; M.; Pierce, Hope, et al., 2020). Although we were not able to adjust for previous mental health status specifically, we could adjust for prior self-reported general health status.
A second limitation is the ecologic nature of the social protection measures used in the analysis. Thus, we could not include individual level data on social protection benefits although we could identify those potentially eligible for pensions or unemployment benefits. Third, we did not include data on other socioeconomic determinants of mental health, such as experience of racism among migrants and minority ethnic groups. Also, while almost everyone in Europe is affected by the pandemic, we were not able to capture aspects that may have made individual exposure to it more or less intense. Fourth, mental health can be complex to measure. We used self-reported data where response bias could have over or underestimated the strength of the associations. However, self-reporting is common in mental health research. Telephone interviewing could have also made respondents hesitant to accurately report information, particularly mental health and financial status information. Measurement of social protection systems is difficult, and our measurement approach is just an approximation. While the Oxford COVID-19 government response tracker aims to capture how many measures a government has adopted and to what degree, the index cannot say whether each has been effectively implemented and whether it is adhered to. Differences in policy implementation and adherence could have biased our estimates, over or under-estimating the strength of the reported associations. Fifth, the findings herein refer to the first few months of the pandemic, as the data were collected between June and August 2020 but the relationship between social protection and mental health may change over time, particularly when assessing social protection measures introduced during the pandemic as opposed to assessing previously established social protection systems as we have done. Finally, our study only included the population aged 50 and above, so the findings cannot be extrapolated to the rest of the population. Most other studies have focused on younger populations (adolescents, university students) and healthcare workers. Thus, our study fills an important gap, capturing experiences of those hardest hit by COVID-19 illness. Although we would expect similar findings, further research could explore the impact of the COVID-19 pandemic on mental health among older populations in low- and middle-income countries.
Our study has implications for policy. It reveals how the adverse impacts of physical distancing and closures are not inevitable. Increased spending on various social protection benefits, including healthcare, unemployment, and a package of social protection benefits seems to ameliorate the risk of mental health deterioration. A recent study found that governments in many countries were perceived to have responded poorly to the burden of mental health suffering associated with COVID-19 (Lazarus et al., 2020). Greater expenditure on social protection may have enabled more support and acted as a safety net for those at risk of mental health problems during what was a health and economic crisis. These findings are consistent with the aforementioned study from the United States which found that stronger social support policies helped mitigate the mental health consequences of household income shocks during the COVID-19 pandemic (Donnelly & Farina, 2021). We also found that individuals living alone had a higher risk of mental health deterioration, which may be explained by feelings of isolation and lack of social support, particularly among older people who may have less access to digital communications. This highlights the importance of considering emotional and social support as part of government and civil society responses to the COVID-19 pandemic, bearing in mind that many of those worst affected risk being further excluded from the increasingly digital delivery of services (Seifert et al., 2021). Faced with a continuing COVID-19 pandemic, with more time spent under physical distancing and other containment measures and further economic downturn, there is a risk of further harm to mental health. It is imperative that countries build strong social protection systems and resilient health systems that can protect their populations from the mental health consequences of crises (Hanefeld et al., 2018; Tediosi et al., 2020; Thomas et al., 2020; World Health Organization, 2020a).
Author statement
AML conceived the study, analysed the data, and prepared the first draft. AML and DS designed the study. All authors provided critical revisions and contributed to the interpretation of the data and writing of the manuscript. All authors read and approved the submitted manuscript.
Data sharing
SHARE data is available upon registration on their website. Data from Eurostat and from the Oxford COVID-19 Government Response Tracker are publicly available on their websites.
Financial disclosure
Progetto: Rif. 2018- 0863 “Pension reforms and spatial-temporal patterns in healthy ageing in Lombardy: quasinatural experimental analysis of linked health and pension data in comparative Italian and European perspective” finanziato da Fondazione Cariplo nell’ambito del bando “Ricerca sociale sull’invecchiamento: persone, luoghi e relazioni”.
Ethical statement
Hereby, I, Ana Méndez López, consciously assure that for the manuscript submitted the following is fulfilled:
-
1)
This material is the authors' own original work, which has not been previously published elsewhere.
-
2)
The paper is not currently being considered for publication elsewhere.
-
3)
The paper reflects the authors' own research and analysis in a truthful and complete manner.
-
4)
The paper properly credits the meaningful contributions of co-authors and co-researchers.
-
5)
The results are appropriately placed in the context of prior and existing research.
-
6)
All sources used are properly disclosed (correct citation). Literally copying of text must be indicated as such by using quotation marks and giving proper reference.
-
7)
All authors have been personally and actively involved in substantial work leading to the paper, and will take public responsibility for its content.
Declaration of competing interest
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.101017.
Contributor Information
Ana Mendez-Lopez, Email: ana.mendezl@estudiante.uam.es.
David Stuckler, Email: david.stuckler@unibocconi.it.
Martin McKee, Email: Martin.McKee@lshtm.ac.uk.
Jan C. Semenza, Email: jan.semenza@lateralphc.com.
Jeffrey V. Lazarus, Email: Jeffrey.lazarus@isglobal.org.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Bergmann M., Kneip T., De Luca G., Scherpenzeel A. SHARE-ERIC; 2019. Survey participation in the survey of health, ageing and retirement in Europe (SHARE), wave 1-7. Based on release 7.0.0. [Google Scholar]
- Börsch-Supan A. SHARE-ERIC; 2020. Survey of health, ageing and retirement in Europe (SHARE) wave 8. COVID-19 survey 1. Release version: 0.0.1. Beta. [Google Scholar]
- Börsch-Supan A., Brandt M., Hunkler C., Kneip T., Korbmacher J., Malter F., et al. Data resource profile: The survey of health, ageing and retirement in Europe (SHARE) International Journal of Epidemiology. 2013;42:992–1001. doi: 10.1093/ije/dyt088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. The Lancet Infectious Diseases. 2020;20:533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly R., Farina M.P. How do state policies shape experiences of household income shocks and mental health during the COVID-19 pandemic? Social Science & Medicine. 2021;269 doi: 10.1016/j.socscimed.2020.113557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eurostat . 2021. European system of integrated social PROtection statistics (ESSPROS) [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in england: A longitudinal observational study. The Lancet Psychiatry. 2021;8:141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M., Saiz J., López-Gómez A., Ugidos C., et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale T., Angrist N., Goldszmidt R., Kira B., Petherick A., Phillips T., et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker) Nature Human Behaviour. 2021;5:529–538. doi: 10.1038/s41562-021-01079-8. [DOI] [PubMed] [Google Scholar]
- Hanefeld J., Mayhew S., Legido-Quigley H., Martineau F., Karanikolos M., Blanchet K., et al. Towards an understanding of resilience: Responding to health systems shocks. Health Policy and Planning. 2018;33:355–367. doi: 10.1093/heapol/czx183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarus J.V., Ratzan S., Palayew A., Billari F.C., Binagwaho A., Kimball S., et al. COVID-SCORE: A global survey to assess public perceptions of government responses to COVID-19 (COVID-SCORE-10) PLoS One. 2020;15 doi: 10.1371/journal.pone.0240011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Sherlock P., Ebrahim S., Geffen L., McKee M. Bearing the brunt of covid-19: Older people in low and middle income countries. BMJ. 2020;368:m1052. doi: 10.1136/bmj.m1052. [DOI] [PubMed] [Google Scholar]
- Pan K.-Y., Kok A.A.L., Eikelenboom M., Horsfall M., Jörg F., Luteijn R.A., et al. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: A longitudinal study of three Dutch case-control cohorts. The Lancet Psychiatry. 2021;8:121–129. doi: 10.1016/S2215-0366(20)30491-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7:883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., McManus S., Jessop C., John A., Hotopf M., Ford T., et al. Says who? The significance of sampling in mental health surveys during COVID-19. The Lancet Psychiatry. 2020;7:567–568. doi: 10.1016/S2215-0366(20)30237-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson R.A., Keyes K.M., Medina J.T., Calvo E. Sociodemographic inequalities in depression among older adults: Cross-sectional evidence from 18 countries. The Lancet Psychiatry. 2020;7:673–681. doi: 10.1016/S2215-0366(20)30151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seifert A., Cotten S.R., Xie B. A double burden of exclusion? Digital and social exclusion of older adults in times of COVID-19. Journal of Gerontology: Serie Bibliographique. 2021;76:e99–e103. doi: 10.1093/geronb/gbaa098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sounderajah V., Clarke J., Yalamanchili S., Acharya A., Markar S.R., Ashrafian H., et al. A national survey assessing public readiness for digital health strategies against COVID-19 within the United Kingdom. Scientific Reports. 2021;11:5958. doi: 10.1038/s41598-021-85514-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . StataCorp LP; College Station, TX: 2019. Stata statistical software: Release 16. [Google Scholar]
- Taquet M., Geddes J.R., Husain M., Luciano S., Harrison P.J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: A retrospective cohort study using electronic health records. The Lancet Psychiatry. 2021 doi: 10.1016/S2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62354 COVID-19 cases in the USA. The Lancet Psychiatry. 2021;8:130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tediosi F., Lönnroth K., Pablos-Méndez A., Raviglione M. Build back stronger universal health coverage systems after the COVID-19 pandemic: The need for better governance and linkage with universal social protection. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-004020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas S., Sagan A., Larkin J., Cylus J., Figueras J., Karanikolos M. European Observatory Policy Briefs Copenhagen (Denmark): European Observatory on Health Systems and Policies, World Health Organization 2020 (acting as the host organization for, and secretariat of, the European Observatory on Health Systems and Policies); 2020. Strengthening health systems resilience: Key concepts and strategies. [PubMed] [Google Scholar]
- United Nations Secretary-General Policy Brief . United Nations; New York, NY, USA: 2020. United Nations policy Brief: COVID-19 and the need for action on mental health. [Google Scholar]
- Vahia I.V., Jeste D.V., Reynolds C.F., 3rd Older adults and the mental health effects of COVID-19. JAMA. 2020;324:2253–2254. doi: 10.1001/jama.2020.21753. [DOI] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain, Behavior, and Immunity. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Kala M.P., Jafar T.H. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLoS One. 2020;15 doi: 10.1371/journal.pone.0244630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . World Health Organization. Regional Office for Europe; 2020. Health inequity and the effects of COVID-19: Assessing, responding to and mitigating the socioeconomic impact on health to build a better future. [Google Scholar]
- World Health Organization . 2020. Listings of WHO's response to COVID-19. [Google Scholar]
- World Health Organization . World Health Organization; 2020. Mental health and psychosocial considerations during the COVID-19 outbreak, 18 March 2020. [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.