Abstract
Objectives. To determine the effect of heat waves on emergency department (ED) visits for individuals experiencing homelessness and explore vulnerability factors.
Methods. We used a unique highly detailed data set on sociodemographics of ED visits in San Diego, California, 2012 to 2019. We applied a time-stratified case–crossover design to study the association between various heat wave definitions and ED visits. We compared associations with a similar population not experiencing homelessness using coarsened exact matching.
Results. Of the 24 688 individuals identified as experiencing homelessness who visited an ED, most were younger than 65 years (94%) and of non-Hispanic ethnicity (84%), and 14% indicated the need for a psychiatric consultation. Results indicated a positive association, with the strongest risk of ED visits during daytime (e.g., 99th percentile, 2 days) heat waves (odds ratio = 1.29; 95% confidence interval = 1.02, 1.64). Patients experiencing homelessness who were younger or elderly and who required a psychiatric consultation were particularly vulnerable to heat waves. Odds of ED visits were higher for individuals experiencing homelessness after matching to nonhomeless individuals based on age, gender, and race/ethnicity.
Conclusions. It is important to prioritize individuals experiencing homelessness in heat action plans and consider vulnerability factors to reduce their burden. (Am J Public Health. 2022;112(1):98–106. https://doi.org/10.2105/AJPH.2021.306557)
Heat waves increase the risk of a wide range of health conditions, including cardiovascular- and respiratory-related outcomes.1,2 Heat waves can trigger highly morbid physiological responses through various pathways, such as inflammation, heat cytotoxicity, ischemia, disseminated intravascular coagulation, and rhabdomyolysis, which can lead to significant end-organ damage and even death.3 In California alone, heat waves have been shown to cause 11 000 excess hospitalizations in 20 years.4 Targeted research can inform policies to protect vulnerable populations from the adverse health impacts of increasingly prevalent heat waves, as the frequency, intensity, and severity of heat waves have been increasing and are projected to increase further in California owing to climate change.5
Certain populations are commonly thought to be particularly vulnerable to the health effects of heat waves, including people who experience homelessness. In this context, we define increased vulnerability as having characteristics that modify the effect of heat waves on morbidity; this is measured by the differential health risks from heat waves across subgroups.6 Although there are varying classifications of individuals experiencing homelessness, people are commonly considered homeless when they are without a physical shelter or are in physical shelters that do not meet basic standards of health and safety.7 People that experience homelessness are considered to be among the most vulnerable to extreme weather impacts because of their exposure to the elements and high rates of preexisting health conditions, such as mental illness, as well as higher rates of smoking and drug and alcohol use.8,9 It is estimated that approximately 30% of persons experiencing homelessness suffer from serious mental illness, and they have twice the odds of having unmet medical care needs as people living in homes.10 Underresourcing of homelessness-related measures may further increase their vulnerability to harmful exposures.9 Accessibility to air conditioning or a cool location during a heat wave is a strong indicator of heat-related health disparities.11,12 As a population with no consistent access to reliable shelter, it is presumed that individuals experiencing homelessness should be a targeted population in heat action plans to mitigate the health burden they experience during heat waves.
The majority of evidence concerning heat impacts on the health of populations that experience homelessness has been based on qualitative findings or conceptual studies.9,13–15 Research into the perceptions and experiences of these individuals and service providers indicates that heat waves adversely affect people experiencing homelessness. However, limited epidemiological studies exist to provide evidence of the association between heat waves and the health of persons experiencing homelessness. The factors that make them particularly vulnerable are still obscure.
According to a 2020 US Department of Housing and Urban Development assessment, California is particularly affected when it comes to homelessness. Partly because of the warmer climate16 and the increasingly expensive housing market in California,17 the state accounts for 51% of all unsheltered individuals in the entire country.18 Not only is California the state with the highest number of people experiencing homelessness, but it also has one of the highest rates of homelessness at 41 people per 10 000.18 The urban centers of San Diego City and County in California, in particular, had the fifth largest number of people experiencing homelessness in the United States in 2019.18 Therefore, San Diego County is a fitting context to study vulnerability factors in this population.
We aimed to quantify the effects of heat waves on emergency department (ED) visits among patients experiencing homelessness. The results of this study can be used to provide evidence on the importance of prioritizing people who experience homelessness in heat warning systems and action plans and limit the harmful impacts of heat waves on vulnerable populations.
METHODS
We obtained ED utilization data from 2012 through 2019 for patients admitted to 1 of 2 hospitals in San Diego County in a single health system with a shared patient population and electronic medical record. One hospital is an urban academic teaching hospital (level 1 trauma center), whereas the second hospital is a suburban community hospital.
Patient and Exposure Data
We queried patient data from the electronic health record EPIC (Epic, Verona, WI) and included demographics and visit characteristics. Demographics included homelessness, age, ethnicity (Hispanic or not non-Hispanic), and race (American Indian/Alaska Native, Asian, Black/African American, Native Hawaiian/Pacific Islander, other race, or mixed race, White, or unknown). The homeless status of a patient was determined by registration staff or triage nurses upon arrival to the ED and based on their housing status at that time. Visit characteristics included whether the patient had a psychiatric consult (yes or no), time of day of ED arrival (day: 7:00 am to 6:59 pm or night: 7:00 pm to 6:59 am), and method of transportation to the hospital.
We used gridded observed data from the PRISM Climate Group of Oregon State University to derive daily maximum and minimum temperatures, averaged at the zip code level.19 We restricted our analysis to the warm season, from May to September, consistent with previous literature studying heat and health in California.1,4 As persons experiencing homelessness do not have a stable residence by definition, we used a weighted measure of point-in-time counts of individuals experiencing homelessness in San Diego County to characterize exposure by weighting daily maximum and minimum temperatures based on the number of individuals experiencing homelessness in that zip code.20 Point-in-time counts are an annual count of people experiencing homelessness on a single night in January collected by the US Department of Housing and Urban Development.18,20 To capture the potential range in effects based on heat wave measurements, we considered multiple heat wave definitions, including where the weighted temperature exceeded the 99th, 97.5th, and 95th percentiles of the total temperature distribution of the study period for 1 or 2 days. For 1-day events, we defined any daily temperature exceeding the percentile of interest as a heat wave day, whereas we defined 2-day heat wave temperature as exceeding the threshold for 2 consecutive days. When applying these definitions to both maximum and minimum (to capture nighttime heat waves) temperatures, we considered 12 definitions for analysis. Nighttime heat waves defined using minimum temperature thresholds can also be associated with hot daytime temperatures and are commonly expressed with increased humidity in the California climate.5
Statistical Analysis
We categorized age as 18 to 44 years, 45 to 64 years, and 65 years or older, as the elderly (older than 65 years) have been shown particularly vulnerable to heat.21 We categorized method of transportation as ambulance transportation (paramedic unit, basic life support, critical care transportation, private ambulance), personal transportation (automobile, public transportation, taxi, walk-in), and other (helicopter, military, police custody, special transportation, unknown). We conducted descriptive analyses of patient and visit characteristics.
We used a time-stratified case–crossover design to study the association between each heat wave definition and ED visit in the population experiencing homelessness. The methodology resembles the design and analysis of a case–control study, but we identified control days for each case in the study population. We selected control days based on the same day of the week of the ED visit in the same month and year that the case occurred, and we compared exposure to a heat wave for these case and control days. Each case day had 3 to 4 control days. The benefit of this methodology is that, as we treated each ED visit as its own control, all potential time-fixed confounding is adjusted for by design. We employed a conditional logistic regression model to study the association between heat waves and ED visits for each heat wave measure. We stratified the study population by age group, race, ethnicity, psychiatric consultation, means of arrival, and time of day of the ED visit. We ran independent regressions for each subgroup and heat wave definition. We applied the Cochran Q test to understand heterogeneity between subgroups.
We used coarsened exact matching to match the distribution of ED visits among individuals experiencing homelessness to the nonhomeless patients based on age (18–24, 25–34, 35–44, 45–54, 55–64, or ≥ 65 years), gender (female, male, or unknown), and race/ethnicity (categories described in Patient and Exposure Data). We then conducted stratified analyses in the matched data set, comparing the ED visits of individuals experiencing homelessness with those of nonhomeless individuals.
Sensitivity Analysis
As some patients visited the ED multiple times, we applied a sensitivity analysis by restricting the study to patients experiencing homelessness who visited the ED only 1 time in the study period. This was to ensure that any results were not driven by multiple ED visits from the same individuals. We also conducted a sensitivity analysis with heat waves based on apparent temperature, using estimates accounting for relative humidity, consistent with previous work.22
RESULTS
A total of 24 688 ED visits were by patients who were identified as homeless in the 2 hospitals during May to September from 2012 to 2019 out of 242 262 total visits over the study period. Among ED visits by individuals experiencing homelessness, the majority (94%) were younger than 65 years, of non-Hispanic ethnicity (84%), and White (60%; Table 1). Of the 12 heat wave definitions considered in the analysis, the number of events that exceeded the threshold ranged from 4 (99th percentile, 2 days, maximum temperature) to 62 (95th percentile, 1 day, minimum temperature). The temperature thresholds for heat wave events ranged from 20.4°C for the minimum temperature in the least stringent definition to 34.5°C for the maximum temperature in the most stringent definition (Table 2). Heat waves were generally well distributed across the study years, with the majority of events occurring in the later months (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). The thresholds we used for heat wave definitions varied spatially across San Diego, with higher temperature thresholds in the inland region and lower temperature thresholds in the coastal areas (Figure B, available as a supplement to the online version of this article at http://www.ajph.org). The daily mean number of ED visits was generally higher on heat wave days, with an average of 22.83 cases on heat wave days and an average of 20.71 visits on non–heat wave days (Table 2).
TABLE 1—
Description of Patients Experiencing Homelessness Who Visited an Emergency Department: San Diego, CA, May–September 2012–2019
| Characteristic | No. (%) |
| Age, y | |
| 18–44 | 9 666 (39.15) |
| 45–64 | 13 437 (54.43) |
| ≥ 65 | 1 585 (6.42) |
| Ethnicity | |
| Hispanic | 3 448 (13.97) |
| Non-Hispanic | 20 729 (83.96) |
| Unknown | 511 (2.07) |
| Race | |
| American Indian/Alaska Native | 68 (0.28) |
| Asian | 117 (0.47) |
| Black/African American | 4 829 (19.56) |
| Native Hawaiian/Pacific Islander | 35 (0.14) |
| Other race/mixed race | 4 298 (17.41) |
| Unknown | 539 (2.18) |
| White | 14 802 (59.96) |
| Psychiatric consultation | |
| No | 21 202 (85.88) |
| Yes | 3 486 (14.12) |
| Time of admission | |
| Day (7:00 am to 6:59 pm) | 15 381 (62.30) |
| Night (7:00 pm to 6:59 am) | 9 307 (37.70) |
| Method of transportation to ED | |
| Emergency | 12 703 (51.46) |
| Personal | 10 436 (42.28) |
| Other | 1 545 (6.26) |
Note. ED = emergency department. The population size was n = 24 688.
TABLE 2—
Environmental Description and Number of Daily Emergency Department Visits by Heat Wave Definition: San Diego, CA, May–September 2012–2019
| Heat Wave Definition (HWD) | Temp Metric | Percentile (Temperature, °C) | Duration, Days | No. Days (%) | Mean Cases Non-HW (SD) | Mean Cases During HWa (SD) |
| HWD1 | Maximum | 95 (31.52) | 1 | 61 (4.98) | 20.69 (6.02) | 21.85 (6.64) |
| HWD2 | Maximum | 95 (31.52) | 2 | 34 (2.78) | 20.68 (6.03) | 22.71 (6.66) |
| HWD3 | Maximum | 97.5 (32.92) | 1 | 31 (2.53) | 20.74 (6.04) | 20.84 (6.74) |
| HWD4 | Maximum | 97.5 (32.92) | 2 | 16 (1.31) | 20.73 (6.05) | 22.25 (6.49) |
| HWD5 | Maximum | 99 (34.54) | 1 | 13 (1.06) | 20.73 (6.05) | 22.08 (6.96) |
| HWD6 | Maximum | 99 (34.54) | 2 | 4 (0.33) | 20.74 (6.04) | 23.5 (11.27) |
| HWD7 | Minimum | 95 (20.42) | 1 | 62 (5.07) | 20.67 (6.05) | 22.05 (6.17) |
| HWD8 | Minimum | 95 (20.42) | 2 | 39 (3.19) | 20.71 (6.04) | 22.92 (6.61) |
| HWD9 | Minimum | 97.5 (20.99) | 1 | 30 (2.45) | 20.70 (6.03) | 22.53 (7.02) |
| HWD10 | Minimum | 97.5 (20.99) | 2 | 14 (1.14) | 20.69 (6.03) | 25.21 (6.80) |
| HWD11 | Minimum | 99 (21.63) | 1 | 13 (1.06) | 20.70 (6.04) | 24.77 (6.46) |
| HWD12 | Minimum | 99 (21.63) | 2 | 7 (0.57) | 20.73 (6.05) | 23.29 (7.41) |
Note. The population size was n = 24 688.
On the second day for 2-day heat waves.
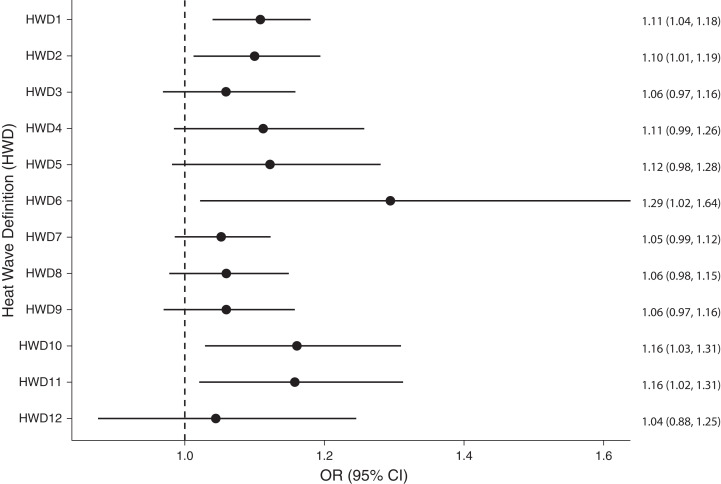
We found a consistent positive signal between heat waves and the risk of ED visits of people experiencing homelessness for the majority of heat wave definitions considered (Figure A). The strongest precise signal detected was 2-day heat waves defined at the 99th percentile using maximum temperature, which increased odds of an ED visit by 1.29 (95% confidence interval [CI] = 1.02, 1.64). Results also indicated effects for heat wave definitions based on minimum temperature, although we no longer observed this when considering heat waves based on apparent temperature (Figure C, available as a supplement to the online version of this article at http://www.ajph.org). Generally, odds of an ED visit increased with longer heat waves at more extreme temperature thresholds, particularly on the second day of 2-day heat waves (Figure 1).
FIGURE 1—
Odds Ratios (ORs) and 95% Confidence Intervals (CIs) of Heat Wave Impacts on Emergency Department Visits Among Patients Experiencing Homelessness: San Diego, CA, May–September 2012–2019
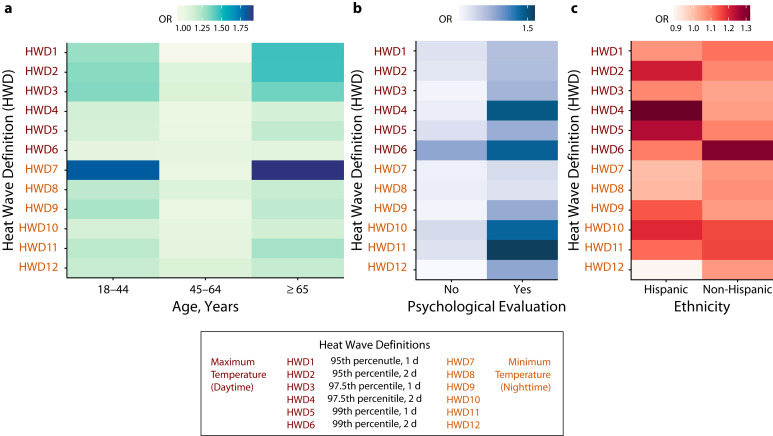
We also identified vulnerability characteristics among patients experiencing homelessness. In the stratification by age group, we observed a stronger effect in the youngest population (aged 18–44 years) and the oldest population (aged ≥ 65 years) than in the middle-aged group (aged 45–65 years) (Figure 2; Table C, available as a supplement to the online version of this article at http://www.ajph.org). There was also a consistently stronger effect for patients requiring a psychiatric consultation than for those who did not (Figure 2). When we considered the method of transportation to the ED, we found that individuals who arrived by personal transportation appeared to be more affected by daytime heat wave events, whereas those arriving with an emergency vehicle appeared to be more affected by nighttime heat waves (Figure D; Table D, available as a supplement to the online version of this article at http://www.ajph.org). When stratifying the population by time of admission to the hospital, daytime ED visits were slightly higher and had more precise effects (Figure C).
FIGURE 2—
Odds Ratios (ORs) of Heat Wave Impacts on Emergency Department Visits Among Patients Experiencing Homelessness by (a) Age Group, (b) Encounter With a Psychiatric Consultation, and (c) Hispanic Ethnicity: San Diego, CA, May–September 2012–2019
Stratification by race/ethnicity led to imprecise estimates attributable to small sample sizes, and we could not draw any differences from these results (Table A, available as a supplement to the online version of this article at http://www.ajph.org). When considering ethnicity, we observed an effect for both Hispanic and non-Hispanic groups, although precision increased for non-Hispanic patients (Figure 2). The heat wave definition that drives the greatest health burden for Hispanic patients is the 97.5th percentile threshold for 2 consecutive days using maximum temperature, which increased the odds of an ED visit by 1.32 (95% CI = 0.95, 1.83), although the effect is imprecise. When stratifying by time of admission and ethnicity, estimates are even more imprecise (Figure E, available as a supplement to the online version of this article at http://www.ajph.org).
Overall, persons experiencing homelessness were more vulnerable to heat waves than were nonhomeless persons (Figure F; Table B, available as a supplement to the online version of this article at http://www.ajph.org). The results of the sensitivity analysis restricting patients that have visited the ED only once in San Diego County are consistent with the other findings and show that multiple ED visits by the same individual are not driving the observed effects (Figure G available as a supplement to the online version of this article at http://www.ajph.org). The Cochran Q heterogeneity test indicated a difference between subgroups at the 10% significance level for some heat wave definitions, although this was not consistent across all comparisons (Table B).
DISCUSSION
Capitalizing on a unique data set with detailed information on the sociodemographics of ED visits, this study provides evidence that persons who are experiencing homelessness have increased odds of visiting an ED during a heat wave event compared with the nonhomeless population (Figure F). Although individuals experiencing homelessness have been targeted by heat action plans aimed at limiting the health effects of heat waves,14,23 these results provide the first epidemiological evidence, to our knowledge, to substantiate this effort and evaluate which characteristics contribute to this presumed vulnerability. By using a range of metrics to define heat wave events and patient-level demographic information, this study denotes that certain subgroups are particularly at risk and illustrates that the association can vary by metric used to define heat wave events.
Various early warning systems and heat action plans have considered populations that experience homelessness to be a particularly vulnerable group.23 For example, action plans in Phoenix, Arizona, provided cooling stations and distributed water in areas where people who were experiencing homelessness congregated and included a psychiatrist on outreach teams for triaging mental health needs.23 In a qualitative study on Montreal, Canada’s heat action plan evaluating the perceptions of vulnerable populations, some of whom were individuals experiencing homelessness, participants indicated that messaging to lessen the negative impacts of heat waves was not effective. For example, some of the recommendations of the heat action plan included spending time in a cooled public area; however, some participants mentioned being asked to leave by guards when seeking refuge in these areas.14 Although populations experiencing homelessness are recognized as a priority in many early warning system or heat action plans, the most appropriate actions to protect these individuals may be more challenging to identify than the measures indicated for other high-risk groups.
These results are valuable for understanding the implications of an increasingly prevalent exposure for the health of people experiencing homelessness and can be used to inform targeted actions to provide appropriate resources to this highly vulnerable population. Using thresholds based on past climatic data to define heat waves is useful in providing an evidence-based structure for activating interventions to protect vulnerable populations during heat waves and can be effective in decreasing heat-related illnesses.24 The evidence can also be useful for health care systems to better identify heat-related stress and be prepared to care for this vulnerable population during heat waves.
Our result that the younger adult age group had increased vulnerability differs from the existing literature on heat waves and morbidity in the general population. A literature review on heat waves and morbidity indicates that children and the elderly are at increased risk for morbidity during heat wave events,25 but no study to our knowledge has identified the adult population younger than 45 years to be a vulnerable group. The increased vulnerability of this group may be driven by the higher proportion of persons in that age group (23.8%) that required a psychiatric consultation, as compared with 13.6% and 13.4% in the middle-aged and elderly age groups, respectively. A meta-analysis on heat-related deaths showed that preexisting psychiatric illness triples the risk of heat wave–related mortality; this is thought to be related to the impaired ability of these individuals to recognize symptoms of heat exposure, seek access to a cool space, and rehydrate during a heat wave.26 The higher vulnerability in the elderly population is consistent with previous work on heat-related impacts21,27; weakened physiological responses, higher prevalence of underlying health risks, and vulnerability caused by social isolation are risk factors that are associated with older age.27
The results indicating increased vulnerability for patients who required a psychiatric consultation is consistent with previous literature. A systematic review on the health effects of high ambient temperatures and heat waves on mental health found an increased risk of mental health–related ED visits during heat waves.28 The review also indicated that the risk of mortality attributable to substance and alcohol misuse increased during a heat wave.28 These results indicate that targeting persons who are experiencing homelessness and have psychiatric conditions during extreme heat may be an effective strategy; including a psychiatrist on outreach teams, as has been done in Phoenix, Arizona, could be very beneficial to this specific population.23
A difference in vulnerability by ethnicity is not apparent, consistent with the existing literature on ethnic disparities in heat wave impacts in the general population. For example, Guirguis et al. did not find a greater impact of temperature on hospitalizations for Hispanic individuals, despite this population having lower access to air conditioning than do non-Hispanic White residents in San Diego County.11 The effects we observed for nighttime heat waves throughout the main and stratified analyses are noteworthy. A study assessing the effect of heat waves on individual exposure by using wearable sensors indicated that nighttime heat waves are associated with increased heat inequality, as income, employment type, and housing type were found to be strongly associated with heat exposure during the night.29 Also, nighttime heat waves are associated with increased humidity,5 which may be a driver of this increased effect. Interestingly, we no longer observed the effect when we considered nighttime heat waves based on apparent temperature, indicating the need to further explore the role of humidity in driving the health impacts of nighttime heat waves.
This study is one of the first to highlight the vulnerability of persons experiencing homelessness to the health effects of heat waves and explore underlying factors that contribute to this association. We exploited a data set that has detailed information about ED visits to understand vulnerability factors in a county with one of the highest rates of individuals experiencing homelessness in the United States.18 Although we were able to detect heterogeneous effects across some subgroups (Table B), other heterogeneity test results did not show differences between subgroups. This is mostly because of the relatively small sample size of our study, and future studies may replicate such analyses in different contexts and larger samples. This first assessment is critical to understanding the specific vulnerability of persons experiencing homelessness to increasingly frequent and intense heat wave events.5
Limitations
This study has some limitations that are important to acknowledge. First, we did not consider the role of humidity in our main analysis, which may play an important role in the experience and effects of heat; nevertheless, a sensitivity analysis considering apparent temperature showed similar results for daytime heat waves. We focused on ED visits in 1 hospital system. The effect of heat waves on this population may also drive impacts in other hospital systems and health measures. Although these findings are not generalizable to the entire population of people experiencing homelessness in San Diego, we believe these findings can serve as a first demonstration of the vulnerability of this group and will pave the way for future work on this topic. Also, homeless status of the patient is determined upon arrival to the ED; this categorization may only include populations that have no access to housing and exclude populations that have inadequate or insecure housing. Lastly, the point-in-time counts of individuals experiencing homelessness in San Diego we used for the exposure assessment are determined annually on 1 night in January20; this may vary from what would be observed in the summer months. However, as San Diego has a moderate year-round climate, the difference may not be as important as it would be in other regions.
Public Health Implications
There are many other important areas for future work on the topic of individuals experiencing homelessness and heat-related health impacts. First, the susceptibility of persons who are homeless in San Diego County may differ greatly from that of other cities; therefore, it would be important to study this question across different contexts. Additionally, there are many ways to define homelessness, and examining different measures of homelessness or housing exclusion would be important in future work.30 Also, although we were unable to study differential susceptibility of this homeless population by race because of the limited sample size, we hope to be able to explore potential racial disparities in future work; minority populations are hugely overrepresented in the homeless population compared with the general population of San Diego.20 However, this assessment is important to demonstrate the first evidence of the susceptibility of this population and can be expanded to explore differential vulnerability across populations and contexts.
Homelessness is rapidly becoming a major social challenge in the United States. Structural inequalities,31 housing crises,32 high rental costs,33 and natural disasters34 have all contributed to the increasing number of persons experiencing homelessness in recent years.18 The nation has seen increases in homelessness for the past 3 years, particularly during the COVID-19 pandemic; the number of people who became homeless for the first time more than doubled in San Diego County in 2020 compared with 2019.18,20 As the threat of increasingly frequent and more intense heat waves continues to rise in the United States,34 particularly in California,5 understanding and prioritizing the needs of this rapidly growing vulnerable population will be a critical action in developing and deploying effective mitigation strategies. As the first study, to our knowledge, to quantify the effect of heat waves on the health burden of persons experiencing homelessness by using reproducible heat wave definitions, we hope to pave the way for additional studies to provide evidence on how to best protect this population in the context of climate and social change.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose.
HUMAN PARTICIPANT PROTECTION
No protocol approval was necessary because data analysis in this study was de-identified.
Footnotes
See also Levy and Hernández, p. 48.
REFERENCES
- 1.Basu R, Pearson D, Malig B, Broadwin R, Green R. The effect of high ambient temperature on emergency room visits. Epidemiology. 2012;23(6):813–820. doi: 10.1097/EDE.0b013e31826b7f97. [DOI] [PubMed] [Google Scholar]
- 2.Cheng J, Xu Z, Bambrick H, et al. Cardiorespiratory effects of heatwaves: a systematic review and meta-analysis of global epidemiological evidence. Environ Res. 2019;177:108610. doi: 10.1016/j.envres.2019.108610. [DOI] [PubMed] [Google Scholar]
- 3.Mora C, Counsell CW, Bielecki CR, Louis LV. Twenty-seven ways a heat wave can kill you: deadly heat in the era of climate change. Circ Cardiovasc Qual Outcomes. 2017;10(11):e004233. doi: 10.1161/CIRCOUTCOMES.117.004233. [DOI] [PubMed] [Google Scholar]
- 4.Guirguis K, Gershunov A, Tardy A, Basu R. The impact of recent heat waves on human health in California. J Appl Meteorol Climatol. 2014;53(1):3–19. doi: 10.1175/JAMC-D-13-0130.1. [DOI] [Google Scholar]
- 5.Gershunov A, Guirguis K. California heat waves in the present and future. Geophys Res Lett. 2012;39(18) doi: 10.1029/2012GL052979. [DOI] [Google Scholar]
- 6.Benmarhnia T, Deguen S, Kaufman JS, Smargiassi A. Vulnerability to heat-related mortality: a systematic review, meta-analysis, and meta-regression analysis. Epidemiology. 2015;26(6):781–793. doi: 10.1097/EDE.0000000000000375. [DOI] [PubMed] [Google Scholar]
- 7.Hwang SW. Homelessness and health. CMAJ. 2001;164(2):229–233. [PMC free article] [PubMed] [Google Scholar]
- 8.Ramin B, Svoboda T. Health of the homeless and climate change. J Urban Health. 2009;86(4):654–664. doi: 10.1007/s11524-009-9354-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pendrey CG, Carey M, Stanley J. Impacts of extreme weather on the health and well-being of people who are homeless. Aust J Prim Health. 2014;20(1):2–3. doi: 10.1071/PY13136. [DOI] [PubMed] [Google Scholar]
- 10.Lebrun‐Harris LA, Baggett TP, Jenkins DM, et al. Health status and health care experiences among homeless patients in federally supported health centers: findings from the 2009 patient survey. Health Serv Res. 2013;48(3):992–1017. doi: 10.1111/1475-6773.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guirguis K, Basu R, Al‐Delaimy WK, et al. Heat, disparities, and health outcomes in San Diego County’s diverse climate zones. Geohealth. 2018;2(7):212–223. doi: 10.1029/2017GH000127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Neill MS, Zanobetti A, Schwartz J. Disparities by race in heat-related mortality in four US cities: the role of air conditioning prevalence. J Urban Health. 2005;82(2):191–197. doi: 10.1093/jurban/jti043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cusack L, van Loon A, Kralik D, Arbon P, Gilbert S. Extreme weather-related health needs of people who are homeless. Aust J Prim Health. 2013;19(3):250–255. doi: 10.1071/PY12048. [DOI] [PubMed] [Google Scholar]
- 14.Benmarhnia T, Alexander S, Price K, Smargiassi A, King N, Kaufman JS. The heterogeneity of vulnerability in public health: a heat wave action plan as a case study. Crit Public Health. 2018;28(5):619–625. doi: 10.1080/09581596.2017.1322176. [DOI] [Google Scholar]
- 15.Walters V, Gaillard JC. Disaster risk at the margins: homelessness, vulnerability and hazards. Habitat Int. 2014;44:211–219. doi: 10.1016/j.habitatint.2014.06.006. [DOI] [Google Scholar]
- 16.Corinth K, Lucas DS.2017. https://www.aei.org/research-products/working-paper/on-the-relationship-between-climate-and-homelessness
- 17.Quigley JM, Raphael S, Smolensky E. Homeless in America, homeless in California. Rev Econ Stat. 2001;83(1):37–51. doi: 10.1162/003465301750160027. [DOI] [Google Scholar]
- 18.Henry M, de Sousa T, Roddey C, Gayen S, Bednar TJ.2021. https://www.huduser.gov/portal/sites/default/files/pdf/2020-AHAR-Part-1.pdf
- 19.PRISM Climate Group. PRISM climate data. 2021. https://prism.oregonstate.edu
- 20.San Diego Regional Task Force on Homelessness. WeAllCount. 2021. https://www.rtfhsd.org/about-coc/weallcount-pitc/2020
- 21.Gronlund CJ, Zanobetti A, Schwartz JD, Wellenius GA, O’Neill MS. Heat, heat waves, and hospital admissions among the elderly in the United States, 1992–2006. Environ Health Perspect. 2014;122(11):1187–1192. doi: 10.1289/ehp.1206132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ilango SD, Weaver M, Sheridan P, et al. Extreme heat episodes and risk of preterm birth in California, 2005–2013. Environ Int. 2020;137:105541. doi: 10.1016/j.envint.2020.105541. [DOI] [PubMed] [Google Scholar]
- 23.White-Newsome JL, McCormick S, Sampson N, et al. Strategies to reduce the harmful effects of extreme heat events: a four-city study. Int J Environ Res Public Health. 2014;11(2):1960–1988. doi: 10.3390/ijerph110201960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benmarhnia T, Schwarz L, Nori-Sarma A, Bell ML. Quantifying the impact of changing the threshold of New York City Heat Emergency Plan in reducing heat-related illnesses. Environ Res Lett. 2019;14(11):114006. doi: 10.1088/1748-9326/ab402e. [DOI] [Google Scholar]
- 25.Li M, Gu S, Bi P, Yang J, Liu Q. Heat waves and morbidity: current knowledge and further direction—a comprehensive literature review. Int J Environ Res Public Health. 2015;12(5):5256–5283. doi: 10.3390/ijerph120505256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bouchama A, Dehbi M, Mohamed G, Matthies F, Shoukri M, Menne B. Prognostic factors in heat wave–related deaths: a meta-analysis. Arch Intern Med. 2007;167(20):2170–2176. doi: 10.1001/archinte.167.20.ira70009. [DOI] [PubMed] [Google Scholar]
- 27.Åström DO, Bertil F, Joacim R. Heat wave impact on morbidity and mortality in the elderly population: a review of recent studies. Maturitas. 2011;69(2):99–105. doi: 10.1016/j.maturitas.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 28.Thompson R, Hornigold R, Page L, Waite T. Associations between high ambient temperatures and heat waves with mental health outcomes: a systematic review. Public Health. 2018;161:171–191. doi: 10.1016/j.puhe.2018.06.008. [DOI] [PubMed] [Google Scholar]
- 29.Hass AL, Ellis KN. Using wearable sensors to assess how a heatwave affects individual heat exposure, perceptions, and adaption methods. Int J Biometeorol. 2019;63(12):1585–1595. doi: 10.1007/s00484-019-01770-6. [DOI] [PubMed] [Google Scholar]
- 30.Busch-Geertsema V. Defining and measuring homelessness. In: Busch-Geertsema V, Quilgars D, Pleace N., editors. Homelessness Research in Europe: Festschrift for Bill Edgar and Joe Doherty. Brussels, Belgium: FEANTSA; 2010. pp. 19–39. [Google Scholar]
- 31.Olivet J, Dones M, Richard M. The intersection of homelessness, racism, and mental illness. In: Racism and Psychiatry. New York, NY: Springer; 2019 10.1007/978-3-319-90197-8_4 [DOI]
- 32.Timmer DA, Eitzen DS, Talley KD. Paths to Homelessness: Extreme Poverty and the Urban Housing Crisis. New York, NY: Routledge; 2019. [DOI] [Google Scholar]
- 33.Glynn C, Fox EB. Dynamics of homelessness in urban America. Ann Appl Stat. 2019;13(1):573–605. doi: 10.1214/18-AOAS1200. [DOI] [Google Scholar]
- 34.Habeeb D, Vargo J, Stone B. Rising heat wave trends in large US cities. Nat Hazards. 2015;76(3):1651–1665. doi: 10.1007/s11069-014-1563-z. [DOI] [Google Scholar]