Abstract
The LGBTQ+ (lesbian, gay, bisexual, transgender/-sexual, queer or questioning, intersex, asexual, and all subsects) population has been the target of federal and state discriminatory policies leading to high levels of institutional discrimination in the housing, employment, and health sectors. Social determinants of health such as housing conditions, economic opportunities, and access to health care may negatively and disproportionately affect the LGBTQ+ population and reduce their capacity to respond to environmental harm (e.g., obtaining necessary medical care).
Social determinants of health have been shown to be associated with unequal harmful environmental exposure, primarily along lines of race/ethnicity and socioeconomic status. However, chronic diseases, such as respiratory diseases, cardiovascular disease, and cancer, associated with environmental exposure have been shown to occur in higher rates in the LGBTQ+ population than in the cisgender, heterosexual population.
We explore how environmental exposures may disproportionately affect the LGBTQ+ population through examples of environmental exposures, health risks that have been linked to environmental exposures, and social institutions that could affect resilience to environmental stressors for this population. We provide recommendations for policymakers, public health officials, and researchers. (Am J Public Health. 2022;112(1):79–87. https://doi.org/10.2105/AJPH.2021.306406)
The LGBTQ+ (lesbian, gay, bisexual, transgender/-sexual, queer or questioning, intersex, asexual, and all subsects) community is a diverse population of at least 14 million individuals in the United States alone.1 Evidence indicates that sexual and gender minorities, as with other marginalized populations, experience health inequalities stemming from social determinants of health. LGBTQ+ persons have higher levels of homelessness, unemployment, lack of health care, and identity-based violence than do cisgender, heterosexual populations.2 Discrimination faced by LGBTQ+ persons is part of the more encompassing environmental health inequities of race/ethnicity, socioeconomic position, disability, rurality, and more. Although intersectionality is increasingly recognized, most research to date has focused on the cisheteronormative White experience, particularly the male experience.3 Intersectionality is not fully incorporated into research or discussions on environmental justice in public health,4 yet LGBTQ+ persons who are also members of other marginalized groups are particularly vulnerable.
Environmental justice studies focus on intersections between environmental exposure, marginalized subpopulations, and health disparities. Scholars in this field have validated the experiences of racial minorities by demonstrating links between environmental exposures, geography, race, and socioeconomic status.5 Toxic industries and sources of air pollution have consistently been located in communities of color.6 Although the study of environmental justice has expanded to include women, indigeneity, citizenship, and more, far less attention has been paid to sexual orientation and gender identity, including in the context of intersectionality. For example, LGBTQ+ people of color may experience environmental injustices related to race/ethnicity, as would their cisgender and heterosexual counterparts, in addition to any disproportionate burden of the LGBTQ+ population.7
There is insufficient research on associations between environment and health inequalities in LGBTQ+ populations, despite higher rates of chronic physical and mental illnesses.8 Only a few studies have been conducted on LGBTQ+ populations and environmental exposures such as air pollution, secondhand smoke, and environmental disasters.
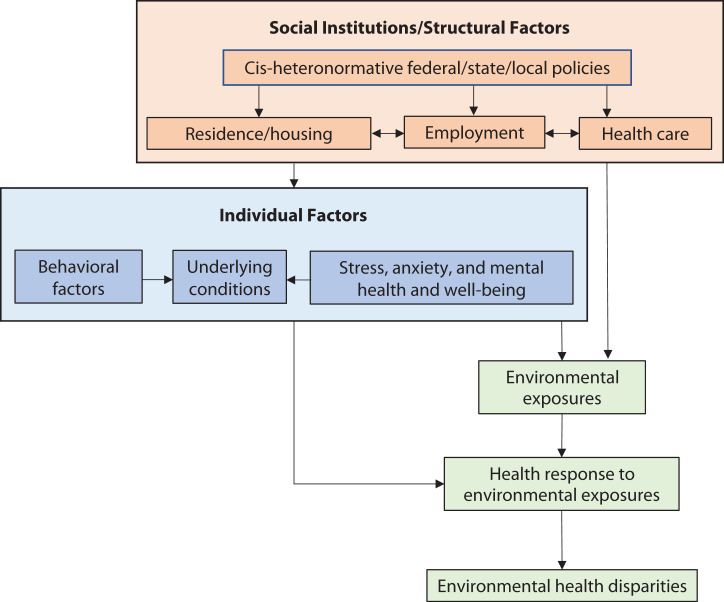
There are many ways that LGBTQ+ persons face disproportionate environmental health burdens. Figure 1 depicts an environmental justice LGBTQ+ framework loosely based on the environmental justice race/ethnicity framework proposed by Gee and Payne-Sturges.9 This figure depicts several pathways through which LGBTQ+ persons could face environmental health disparities. Social institutional and structural factors include discrimination affecting community of residence and housing options, employment, and access to appropriate health care formed through cisheteronormative federal, state, and local policies. Employment affects options for housing, health care, and mental health and well-being.
FIGURE 1—
Conceptual Framework for Environmental Health Disparities for the LGBTQ+ Population
Note. LGBTQ+ = lesbian, gay, bisexual, transgender/-sexual, queer or questioning, intersex, asexual, and all subsects. This schematic depicts the social institution and structural factors and individual factors that relate to pathways through which LGBTQ+ populations could suffer disproportionate public health burden from environmental stressors. The figure is not intended to show all pathways or links between these factors.
Individual factors include behavior, such as proximity to secondhand smoke, and underlying health conditions, including HIV, respiratory distress owing to chest binding, and mental factors. All of these could affect environmental exposures, for example, from occupational exposures, community-based exposures (e.g., ambient air pollution), and exposure to environmental disasters in relation to discriminatory disaster relief programs.
In addition to differential exposures, LGBTQ+ populations may have a different health response to those exposures (referred to as effect modification in epidemiology), for example, because of underlying health conditions or inability to mitigate adverse health effects through medical services. Collectively, these factors could lead to environmental health disparities for LGBTQ+ persons. This conceptual framework does not capture all factors and interconnections among these factors. For example, underlying health conditions could contribute to stress, as would discrimination and violence. Housing practices may affect employment opportunities. Intersectionality with other marginalized groups would further contribute to environmental health disparities.
We explore several examples of these pathways with respect to social institutions, environmental exposures, and health outcomes. Despite little relevant research, we conclude that there are multiple pathways through which environmental exposures and associated health impacts may disproportionately affect LGBTQ+ persons. We provide recommendations for policy, practice, and research.
SOCIAL INSTITUTIONS
Discrimination through social institutions may lead to disproportionate environmental health outcomes for the LGBTQ+ community. Here we describe 2 examples: health care and employment, although many other cases exist, such as discriminatory housing policies and responses to environmental disasters, which we discuss in a later section.
Health Care
LGBTQ+ persons often face disadvantages in receiving health care. They are less likely to seek medical care until they have a serious health issue because of fear of discrimination or cost, are less likely to have health insurance, and experience extensive mistreatment or discrimination from health professionals.10 One study found that 1 in 6 LGBTQ+ adults avoided seeking health care because of anticipated discrimination.11 In 2015, 33% of transgender individuals were either verbally harassed or refused medical care.12 These stark realities may place the LGBTQ+ population in a more vulnerable position when subjected to the health outcomes from environmental exposures if they are less willing or able to find or receive comprehensive care from health care providers.
Employment
The LGBTQ+ population is more susceptible to unemployment than is the non-LGBTQ+ population and are more likely to work in certain occupations. Unemployment can place individuals in poverty, which is associated with exposure to environmental pollution and injustice. One study found that 9% of LGBTQ+ individuals are unemployed in the US compared with 5% of cisgender, heterosexuals.13 The unemployment rate for transgender individuals is 15%, corresponding to nearly one third of transgender individuals living in poverty compared with 14% of the general population.12
LGBTQ+ individuals also work in industries disproportionately affected by occupational hazards that are associated with respiratory illnesses. Forty percent of LGBTQ+ individuals work in 5 industries (restaurant and food services, retail, hospitals, K–12 education, and colleges and universities) compared with 22% of cisgender, heterosexual individuals.14 Although this issue is understudied, the different distribution of occupational hazards and higher unemployment for the LGBTQ+ community, which relates to lack of access to health care and housing and other health stressors, plausibly relates to different health consequences for environmental exposures.
ENVIRONMENTAL EXPOSURE
We explore 3 examples of environmental exposures that may disproportionately affect LGBTQ+ persons: ambient air pollution, environmental disasters, and secondhand smoke. These issues relate to different levels of exposures, as well as the impacts and discrimination encountered by the LGBTQ+ population during environmental disasters.
Air Pollution
Ambient air pollution varies among and in communities. Where LGBTQ+ people live, just as any other population, affects their exposures. After World War II, “heteronormative NIMBYism,” where locally unwanted land uses such as gay bars and businesses were excluded from heterosexual spaces, was common.15 This may have led to other locally unwanted land uses being located in LGBTQ+ spaces, as occurred for racial/ethnic minority communities. Around this time, the Federal Housing Administration prioritized housing loans for married couples that proved they were in a “fit” marriage, preventing accumulation of generational wealth for LGBTQ+ persons and thus affecting their ability to afford housing.
Exclusive policies in urban planning also pushed LGBTQ+ individuals into low-income, declining neighborhoods.16 “Gayborhoods” often have few LGBTQ+ residents because high property values create the illusion that the LGBTQ+ population is primarily White, cisgender, affluent, gay men. This renders others in the community invisible to possible exposure and impact. Currently, 29 states have no antidiscrimination housing policies, and the Federal Housing Act and Equal Credit Opportunity Act does not explicitly prohibit discrimination against sexual orientation and gender identity.2 The Department of Housing and Urban Development has antidiscrimination policies for LGBTQ+ individuals, but as of 2019 male same-sex couples still experienced discrimination when seeking mortgages from the Federal Housing Administration.
These differences and this discrimination could lead to different environmental exposures that vary by community. LGBTQ+ persons may have higher health impacts from air pollution because of where they live, although this exposure also presents a large public health burden for the general population. More than a 100 000 000 people live in areas exceeding the US Environmental Protection Agency’s health-based standards for ozone and fine particulate matter.17
Evidence on disproportionate exposure from air pollution is limited—another example of a research gap in identifying residences of LGBTQ+ populations—but the existing research suggests potential disparities. Two studies, conducted by the same research team, used census data on same-sex couples and hazardous air pollution (HAPs) data from the National Air Toxics Assessment. These studies examined same-sex enclaves for census tracts with a high proportion of same-sex couples using a K-means cluster analysis. Such enclaves were defined as census tracts in the highest fifth percentile for households where 2 people of the same sex lived together in a domestic partnership. In one such study, the authors proposed that heterosexist urban planning may explain the presence of same-sex couple enclaves and their unequal exposure to areas with high HAPs.15 In that work, based in Greater Houston, Texas, census tracts with same-sex enclaves had a higher estimated risk of cumulative cancer from HAPs. Another study found that the HAPs levels were higher in areas where same-sex couples lived than in areas where opposite-sex couples lived.18 Based on different models, same-sex enclaves were associated with a 9.8% to 13.3% higher risk of respiratory illnesses and cancer. Results indicated that sexual orientation, even when accounting for other confounders such as race, is a strong indicator of living in an area with high levels of HAPs.15
There are other pathways through which the LGBTQ+ population may be vulnerable to the health impacts of air pollution. It is lifesaving and gender affirming for some transgender and nonbinary individuals to chest bind to make their chests appear flatter. Doing so helps prevent mental anguish in the form of anxiety, depression, and suicidal ideation; however, chest binding can also cause abnormal lung function.19 Although researchers have not yet investigated this issue, detrimental lung function from chest binding for transgender and nonbinary individuals may increase the risk of respiratory impacts of environmental exposures, such as air pollution.
Environmental Disasters
Environmental disasters such as hurricanes and wildfires also may disproportionately affect LGBTQ+ health; this is owing to hindered access to resources and inclusion in disaster response policies and protocol. Although this is understudied, the existing evidence suggests a higher burden. For example, environmental disasters were associated with increased physical violence against LGBTQ+ individuals.20
One report describes the unique marginalization and vulnerabilities of LGBTQ+ populations during Hurricane Katrina: LGBTQ+ persons were blamed by some religious leaders for the disaster and excluded from disaster response policies; additionally, they lacked benefits given to married heterosexual couples, did not receive adequate health care particularly if HIV positive, and faced stigma and discrimination.21 Two Black transgender women were arrested for using the bathroom of their gender at an emergency temporary shelter, which highlights the added layer of intersectionality. Other transgender individuals were denied aid from faith-based organizations for not possessing identification that matched their name or gender. Federal Emergency Management Agency’s lack of recognition of LGBTQ+ families led to unequal distribution of resources, often to the detriment of their children.22
Section 308 of the Robert T. Stafford Disaster Relief and Emergency Assistance Act currently does not protect sexual orientation or gender identity. The US Department of Department of Housing and Urban Development update to the Equal Access Rule, announced July 1, 2020, prohibits discrimination to Department of Housing and Urban Development–funded housing services, such as temporary emergency shelters during disasters, based on sexual orientation or gender identity, but specifically allows shelters to “voluntary establish a policy,” leaving these persons open to discrimination.
Research on this issue has been limited and primarily not based in the United States. Sexuality and gender identity are very different in cultures and countries that do not subscribe to Western ideas of sex and gender.23 Therefore, we refer to these non-US populations as sexual and gender minorities rather than LGBTQ+. A study synthesizing 12 articles found that gender minorities worldwide faced physical, sexual, and emotional violence from environmental disasters and lacked support from governmental agencies.23 During the 2020 Haitian earthquake, sexual and gender minorities were denied access to emergency housing and disaster relief services, as occurred during Hurricane Katrina, leaving them more vulnerable to the disaster.21 During the 2011 Queensland, Australia, floods, 43% of LGBTQ+ individuals felt afraid in places such as streets, parks, and evacuation centers during the disaster and recovery.24 More research on the LGBTQ+ population in the United States may show similar occurrences.
Secondhand Smoke
Smoking is an environmental justice concern for LGBTQ+ populations because of their higher exposure to respiratory pollutants and secondhand smoke, both of which exacerbate respiratory illnesses. A study based in California found that homosexual women, bisexual women, and homosexual men were much more likely to smoke cigarettes than were heterosexual individuals.25 The smoking rate of homosexual women was 70% more than the rate of heterosexual women. Other studies have shown that the transgender population also has higher rates of cigarette use than does the cisgender population. Transgender men have the highest past 30-day use rate of cigarette, e-cigarette, and cigar use among transgender populations. Transgender men are twice as likely as cisgender men and 3 times as likely as cisgender women to use cigarettes or e-cigarettes.26
Minority stress, targeted advertising by tobacco companies, and gender stereotypes may contribute to health disparities related to cigarette smoking.27 A systematic review of risk factors of smoking in the lesbian, gay, and bisexual population found that different smoking rates may relate to factors unique to this population: internalized homophobia, negative reactions to disclosure of sexual orientation, and identity within the sexual minority community.28 Factors that are not unique to, but occur at higher rates in, the lesbian, gay, and bisexual population and could lead to higher smoking rates include stress, depression, alcohol use, victimization, lack of support networks, and low socioeconomic status.
These higher rates of smoking among the LGBTQ+ community mean higher exposure to secondhand smoke where they live, work, and socialize. A study using the California Health Survey found that sexual minority men and women are twice as likely to be exposed in their own household to secondhand smoke.29 Another study found that homosexual women are more exposed to secondhand smoke in the workplace and bisexual women are more exposed in their home than women in different-sex relationships.30 Patrons of LGBTQ+ bars and venues had 38% higher odds of being exposed to secondhand smoke than did visitors of non-LGBTQ+ bars and venues.31
HEALTH OUTCOMES
We explore 3 examples of health outcomes that disproportionately affect LGBTQ+ populations and have links to environmental stressors: HIV, respiratory illness, and mental health. These health outcomes may also be exacerbated or stigmatized in response to environmental conditions.
HIV
HIV is one of the most studied health outcomes that disproportionately affect LGBTQ+ persons, and environmental conditions have been shown to exacerbate HIV. Cisgender gay men, cisgender bisexual men, and transgender individuals are more likely to develop HIV. Gay and bisexual men comprise 55% of HIV cases but comprise only 2% of the US population.32 Having an intersectional racial minority identity is associated with higher rates of HIV. Half of Black gay and bisexual men have HIV. Transgender women are greatly affected, particularly if they are Black.33
Several studies investigated how environmental exposures may exacerbate HIV. Air pollution can cause and worsen conditions such as pneumocystis pneumonia and tuberculosis (TB), leading to complications in HIV-positive individuals. For example, exposure to PM10 (particulate matter with a diameter of ≤ 10 micrometers), nitrogen dioxide, and ozone has been associated with an increased risk of pneumocystis pneumonia hospitalization in people with HIV.34
In 2014, 33% of people with HIV had TB—one of the deadliest communicable diseases.34 A study in Spain of HIV patients using combined antiretroviral therapy between 1997 and 2012 found that nitrogen dioxide and sulfur dioxide exposure were associated with a risk of hospital admission related to TB.34 A study in Northern California found a positive association between carbon monoxide and nitrogen dioxide exposure and contracting TB.35 Thus, populations with high rates of HIV are particularly susceptible to poor health consequences from exposure to air pollution.
Respiratory Illnesses
The LGBTQ+ population is at higher risk for respiratory illnesses such as asthma and chronic obstruction pulmonary disease, which are diseases related to environmental exposures such as air pollution and smoking. Same-sex couples had higher rates of lifetime and current asthma than did heterosexual couples; these higher rates are related to higher rates of obesity among homosexual women as well as higher rates of smoking, stress, and victimization.28 However, environmental conditions, such as air pollution, also can cause asthma and related complications by increasing lung inflammation.36 Some other health outcomes related to the environment are higher in LGBTQ+ populations; one study found that the risk of chronic obstruction pulmonary disease was significantly higher for the LGBTQ+ population except for transgender men. The authors attributed sleep deprivation as 1 of the chronic obstruction pulmonary disease risk factors,37 although disproportionate burden from air pollution has not been studied.
Mental Health
Mental health issues have been linked with multiple environmental conditions, which may put the LGBTQ+ population at higher risk or exacerbate existing inequalities. LGBTQ+ persons experience higher levels of mental illnesses than do the cisgender, heterosexual population. Institutional and social-based discrimination and stigma contribute to unique internalized anguish that affects LGBTQ+ populations.38 The LGBTQ+ population struggles with expectation of rejection because of their identity, concealment of their identity, and internalized homophobia, factors leading to higher levels of mental illnesses. In the LGBTQ+ population, transgender individuals of all sexualities face more mental health burden than do cisgender lesbian, gay, and bisexual individuals, with 40% of the transgender population experiencing psychological distress.16
Mental health conditions can be aggravated by environmental conditions, including air pollution, weather, environmental disasters, and noise. For example, air pollution can exacerbate mental illness in populations with high rates of psychological distress attributable to minority stress. Long-term exposure to air pollution was found to increase the odds of depression.39 Although this issue remains unstudied, environmental stressors contributing to mental health may be particularly harmful for the LGBTQ+ population, which already face higher levels of mental health burdens.
ADDITIONAL PATHWAYS
Despite limited research, there exist multiple pathways through which the LGBTQ+ population could face disproportionate health burdens from environmental conditions. The examples provided here for social institutions (i.e., health care and employment), exposures (i.e., air pollution, environmental disasters, and secondhand smoke), and health outcomes (i.e., HIV, respiratory illness, and mental health) are meant to be illustrative, not an exhaustive discussion of the potential harm. As an example of another potential link, cardiovascular disease (CVD) risks are higher for some LGBTQ+ subgroups and are linked to environmental conditions. One study found higher CVD risk for bisexual men than heterosexual men.40 Another study found that same-sex women living together have higher risk of CVD mortality than do women living with opposite-sex partners.41 CVD is the leading disease-specific cause of death for transgender and nonbinary individuals receiving gender-affirming treatment.42 Transgender women are more likely to suffer CVD mortality than are transgender men and cisgender men and women.42 Although CVD has been linked to many environmental contaminants, such as air pollution, the potential effect of environmental exposures on CVD outcomes for the LGBTQ+ population is unknown.
INTERSECTIONALITY
The examples of societal institutions, environmental exposures, and health outcomes discussed here do not act in isolation (Figure 1). For instance, many chronic illnesses and conditions, such as HIV and poor mental health and well-being, that disproportionately affect LGBTQ+ populations may synergistically interact with HAPs.10 As another example, bacterial or fungal infestation of housing materials after a flood could affect people with HIV, causing respiratory illnesses such as pneumonia, asthma, and fevers.43 One study recommends that after a hurricane or a major flood, people who are immunocompromised should only go near a moldy building with respiratory protection and avoid handling any of their contaminated belongings.44
Another environmental disaster, wildfires, release fungi from soils that cause the disease coccidioidomycosis (valley fever), which can affect the immunocompromised and cause pneumonia and tissue destruction.45 Furthermore, given their compromised immunity, people with HIV are particularly affected by poor quality air and water and during environmental disasters can suffer disproportionately from lack of lifesaving medications and lack of access to health centers.46 LGBTQ+ individuals who do not have access to lifesaving medications for HIV or hormone replacement therapy during environmental disasters may not seek aid for fear of discrimination.47 During Hurricane Maria, many pharmacies were destroyed or did not have electricity. Working with limited telecommunications, pharmacists were unable to reach providers to update prescription refills or reach those needing medication.48 During Hurricane Katrina, LGBTQ+ individuals with HIV were reluctant to disclose their status and deal with emergency relief doctors who were unfamiliar with treating patients with HIV.22 There is a lack of inclusive and thoughtful disaster response policies for the LGBTQ+ population.
LGBTQ+ persons of color may be at particular risk because of environmental justice concerns overlapping with race/ethnicity concerns, as minorities face well-established higher environmental health burdens. A US Department of Agriculture report concluded that LGBTTQ (lesbian, gay, bisexual, transgender, 2-spirit, and queer) communities have added layers of trauma, discrimination, and stigma from colonization, but also gender and sexuality can place them in a vulnerable position in environmental disasters.49 Intersectionality of environmental justice risk factors cause some portions of the LGBTQ+ population to be particularly vulnerable.
RESEARCH AND DATA GAPS
Lack of research on where LGBTQ+ individuals live challenges the investigation of their potentially disproportionate exposure to spatially heterogenous environmental contaminants, such as air pollution (e.g., proximity to traffic-related pollutants). To date, data on LGBTQ+ residence is limited. The largest survey of where people live in the United States is the US Census and the American Community Survey. These surveys collect demographic information such as race/ethnicity, income, and limited gender information, but they have not explicitly collected data on sexual orientation or gender identity. The only information on sexual orientation that can be gathered from these data are same-sex partnerships. Same-sex households are calculated by pairing households in which 2 people of the same-sex live together and have documented that they are in a domestic partnership. This omits LGBTQ+ partners that do not live together, single LGBTQ+ people, bisexual individuals in opposite-sex partnerships, and many transgender individuals.
There are additional barriers to acquiring LGBTQ+ population data. Institutional discrimination can lead to LGBTQ+ individuals concealing their identity. Sexual orientation and gender identity can be fluid and change over time. Individuals figuring out their sexual orientation or gender identity may switch how they identify over time, and there are transgender individuals who are gender fluid or variant. To fully understand sexual orientation, researchers need to understand identity, attraction, and behavior. Most federal surveys ask only for identity. Including attraction and behavior in surveys can help identify individuals who may not identify as lesbian, gay, or bisexual but may be attracted to or have sexual intercourse with the same sex. This is especially true for many subcultures in which one may not identify as lesbian, gay, or bisexual depending on sexual position.
PUBLIC HEALTH IMPLICATIONS
To further understand and address the potential disproportionate health burden of environmental exposure on the LGBTQ+ population, we recommend both further research and actions to address the underlying discrimination. The following are some specific recommendations for policy, practice, and research:
-
1.
Implement LGBTQ+ antidiscriminatory policies in health care facilities and provide cultural competency for health care workers and mental health professionals. This should include training on LGBTQ+ issues and care.
-
2.
Implement policies to aid the ability of transgender and nonbinary individuals to obtain appropriate identification documents such as driver’s licenses and passports with their name and gender identity.
-
3.
Implement federal, state, and local nondiscrimination policies in sectors such as housing, employment, and health.
-
4.
Target the LGBTQ+ communities in tobacco cessation ads and campaigns.
-
5.
Develop partnerships between government agencies at all levels (municipal, state, and federal) and LGBTQ+ organizations for disasters response and relief to address access and discrimination.
-
6.
Incorporate LGBTQ+ issues into environmental justice research and organizations.
-
7.
Develop and implement a system of collecting sexual orientation and gender identity data that is consistent and addresses the complex nature of the LGBTQ+ population. Such a data set needs to include variables that would help researchers assess environmental exposures (e.g., exact residence or area of residence, such as zip code) and intersectionality of risk (e.g., low income, race/ethnicity). This would provide the means to research environmental injustice and health in the LGBTQ+ population and compare them with other populations, especially for spatially based environmental hazards (e.g., air pollution).
In summary, there exist multiple, interconnected pathways through which LGBTQ+ persons may suffer disproportionate health burdens from environmental stressors, including differences in exposures and health responses, with links to social institutions and entrenched discrimination that affect many aspects of LGBTQ+ lives, such as education, health care, and access to resources during an environmental disaster. Further research and response are needed to better protect the LGBTQ+ population to address potential environmental inequities as well as the underlying discrimination and stigma that contributes to such inequities.
ACKNOWLEDGMENTS
This work was supported by the Environmental Justice Initiative at the Yale University School of the Environment.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to report.
HUMAN PARTICIPANT PROTECTION
No protocol approval was necessary because no human participants were involved in the study.
Footnotes
REFERENCES
- 1.Newport F.2018. https://news.gallup.com/poll/234863/estimate-lgbt-population-rises.aspx
- 2.Romero AP, Goldberg SK, Vasquez LA.2020. https://williamsinstitute.law.ucla.edu/publications/lgbt-housing-instability
- 3.Bowleg L, del Rio-Gonzalez AM, Holt SL, et al. Intersectional epistemologies of ignorance: how behavioral and social science research shapes what we know, think we know, and don’t know about U.S. Black men’s sexualities. J Sex Res. 2017;54(4–5):577–603. doi: 10.1080/00224499.2017.1295300. [DOI] [PubMed] [Google Scholar]
- 4.Zota AR, VanNoy BN. Integrating intersectionality into the exposure paradigm: a novel approach to racial inequities in uterine fibroids. Am J Public Health. 2021;111(1):104–109. doi: 10.2105/AJPH.2020.305979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith A, Laribi O.. J Racial Ethn Health Disparities. [Online ahead of print January 8, 2021 10.1007/s40615-020-00949-7 [DOI]
- 6.Mohai P, Saha R. Which came first, people or pollution? Assessing the disparate siting and post-siting demographic change hypotheses of environmental justice. Environ Res. 2015;10(11):115008. doi: 10.1088/1748-9326/10/11/115008. [DOI] [Google Scholar]
- 7.Hsieh N, Ruther M. Sexual minority health and health risk factors: intersection effects of gender, race, and sexual identity. Am J Prev Med. 2016;50(6):746–755. doi: 10.1016/j.amepre.2015.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sly PD, Carpenter DO, Van den Berg M, et al. Health consequences of environmental exposures: causal thinking in global environmental epidemiology. Ann Glob Health. 2016;82(1):3–9. doi: 10.1016/j.aogh.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 9.Gee GC, Payne-Sturges DC. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect. 2004;112(17):1645–1653. doi: 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quinn GP, Sutton SK, Winfield B, et al. Lesbian, gay, bisexual, transgender, queer/questioning (LGBTQ) perceptions and health care experiences. J Gay Lesbian Soc Serv. 2015;27(2):246– 261. doi: 10.1080/10538720.2015.1022273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Casey LS, Reisner SL, Finding MG, et al. Discrimination in the United States: experiences of lesbian, gay, bisexual, transgender, and queer Americans. Health Serv Res. 2019;54(suppl 2):1454–1466. doi: 10.1111/1475-6773.13229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.James SE, Herman JL, Rankin S, Keisling M, Mottet L, Anafi M. The Report of the 2015 US Transgender Survey. Washington, DC: National Center for Transgender Equality; 2016. [Google Scholar]
- 13.Williams Institute. 2019. https://williamsinstitute.law.ucla.edu/visualization/lgbt-stats/?topic=LGBT#density
- 14.Human Rights Campaign Foundation. The lives and livelihoods of many in the LGBTQ community are at risk amidst COVID-19 crisis. 2020. https://www.hrc.org/resources/the-lives-and-livelihoods-of-many-in-the-lgbtq-community-are-at-risk-amidst-covid-19-crisis
- 15.Collins TW, Grineski SE, Morales DX. Sexual orientation, gender, and environmental injustice: unequal carcinogenic air pollution risks in Greater Houston. Ann Am Assoc Geogr. 2017;107(1):72–92. doi: 10.1080/24694452.2016.1218270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kattari SK, Whitfield DI, Walls NE, Langenderfer-Magruder L, Ramos D. Policing gender through housing and employment discrimination: comparison of discrimination experiences of transgender and cisgender LGBQ individuals. J Soc Social Work Res. 2016;7(3):427–447. doi: 10.1086/686920. [DOI] [Google Scholar]
- 17.US Environmental Protection Agency. https://www.epa.gov/green-book [PubMed]
- 18.Collins TW, Grineski SE, Morales DX. Environmental injustice and sexual minority health disparities: a national study of inequitable health risks from air pollution among same-sex partners. Soc Sci Med. 2017;191:38–47. doi: 10.1016/j.socscimed.2017.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cumming R, Sylvester K, Fuld J. Understanding the effects on lung function of chest binder use in the transgender population. Thorax. 2016;71(suppl 3):A227–A227. doi: 10.1136/thoraxjnl-2016-209333.400. [DOI] [Google Scholar]
- 20.McKinnon S, Gorman-Murray A, Dominey-Howes D. Disasters, queer narratives, and the news: how are LGBTI disaster experiences reported by the mainstream and LGBTI media? J Homosex. 2017;64(1):122–144. doi: 10.1080/00918369.2016.1172901. [DOI] [PubMed] [Google Scholar]
- 21.Dominey-Howes D, Gorman-Murray A, McKinnon S. Queering disasters: on the need to account for LGBTI experiences in natural disaster contexts. Gend Place Cult. 2014;21(7):905–918. doi: 10.1080/0966369X.2013.802673. [DOI] [Google Scholar]
- 22.Haskell B.2021. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2513650
- 23.Rushton A, Gray L, Canty J, Blanchard K. Beyond binary: (re)defining “gender” for 21st century disaster risk reduction research, policy, and practice. Int J Environ Res Public Health. 2019; 16(20):3984. doi: 10.3390/ijerph16203984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gorman-Murray A, Morris S, Keppel J, McKinnon S, Dominey-Howes D. Problems and possibilities on the margins: LGBT experiences in the 2011 Queensland floods. Gend Place Cult. 2017;24(1):37–51. doi: 10.1080/0966369X.2015.1136806. [DOI] [Google Scholar]
- 25.Tang H, Greenwood GL, Cowling DW, Lloyd JC, Roeseler AG, Bal DG. Cigarette smoking among lesbians, gays, and bisexuals: how serious a problem? (United States) Cancer Causes Control. 2004;15(8):797–803. doi: 10.1023/B:CACO.0000043430.32410.69. [DOI] [PubMed] [Google Scholar]
- 26.Buchting FO, Emory KT. Transgender use of cigarettes, cigars, and e-cigarettes in a national study. Am J Prev Med. 2017;53(1):e1–e7. doi: 10.1016/j.amepre.2016.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Delahanty J, Ganz O, Hoffman L, Guillory J, Crankshaw E, Farrelly M. Tobacco use among lesbian, gay, bisexual and transgender young adults varies by sexual and gender identity. Drug Alcohol Depend. 2019;201:161–170. doi: 10.1016/j.drugalcdep.2019.04.013. [DOI] [PubMed] [Google Scholar]
- 28.Blosnich J, Lee JGL, Horn K. A systematic review of the aetiology of tobacco disparities for sexual minorities. Tob Control. 2013;22(2):66–73. doi: 10.1136/tobaccocontrol-2011-050181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Max WB, Stark B, Sung HY, Offen N. Sexual identity disparities in smoking and secondhand smoke exposure in California: 2003–2013. Am J Public Health. 2016;106(6):1136–1142. doi: 10.2105/AJPH.2016.303071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cochran SD, Bandiera FC, Mays VM. Sexual orientation-related differences in tobacco use and secondhand smoke exposure among US adults aged 20 to 59 years: 2003–2010 National Health and Nutrition Examination Surveys. Am J Public Health. 2013;103(10):1837–1844. doi: 10.2105/AJPH.2013.301423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fallin A, Neilands TB, Jordan JW, Ling PM. Secondhand smoke exposure among young adult sexual minority bar and nightclub patrons. Am J Public Health. 2014;104(2):e148–e153. doi: 10.2105/AJPH.2013.301657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Human Rights Campaign. How HIV impacts LGBTQ people. 2020. https://www.hrc.org/resources/hrc-issue-brief-hiv-aids-and-the-lgbt-community
- 33.Herbst JH, Jacobs ED, Finlayson TJ, McKleroy VS, Neumann MS, Crepaz N. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- 34.Alvaro-Meca A, Sancho IP, Diaz A, Resino R, Gil-de-Miguel A, Resino S. Pneumocystis pneumonia in HIV-positive patients in Spain: epidemiology and environmental risk factors. J Int AIDS Soc. 2015;18(1):19906. doi: 10.7448/IAS.18.1.19906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith GS, Van Den Eeden SK, Garcia C, et al. Air pollution and pulmonary tuberculosis: a nested case-control study among members of a Northern California health plan. Environ Health Perspect. 2016;124(6):761–768. doi: 10.1289/ehp.1408166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383(9928):1581–1592. doi: 10.1016/S0140-6736(14)60617-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dai H, Hao J. Sleep deprivation and chronic health conditions among sexual minority adults. Behav Sleep Med. 2019;17(3):254–268. doi: 10.1080/15402002.2017.1342166. [DOI] [PubMed] [Google Scholar]
- 38.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vert C, Sánchez-Benavides G, Martínez D, et al. Effect of long-term exposure to air pollution on anxiety and depression in adults: a cross-sectional study. Int J Hyg Environ Health. 2017;220(6):1074–1080. doi: 10.1016/j.ijheh.2017.06.009. [DOI] [PubMed] [Google Scholar]
- 40.Caceres BA, Brody AA, Halkitis PN, Dorsen C, Yu G, Chyun DA. Sexual orientation differences in modifiable risk factors for cardiovascular disease and cardiovascular disease diagnoses in men. LGBT Health. 2018;5(5):284–294. doi: 10.1089/lgbt.2017.0220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meads C, Martin A, Grierson J, Varney J. Systematic review and meta-analysis of diabetes mellitus, cardiovascular and respiratory condition epidemiology in sexual minority women. BMJ Open. 2018;8(4):e020776. doi: 10.1136/bmjopen-2017-020776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dutra E, Lee J, Torbati T, Garcia M, Merz CNB, Shufelt C. Cardiovascular implications of gender-affirming hormone treatment in the transgender population. Maturitas. 2019;129:45–49. doi: 10.1016/j.maturitas.2019.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Johanning E, Auger P, Morey PR, Yang CS, Olmsted E. Review of health hazards and prevention measures for response and recovery workers and volunteers after natural disasters, flooding, and water damage: mold and dampness. Environ Health Prev Med. 2013;19(2):93–99. doi: 10.1007/s12199-013-0368-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Centers for Disease Control and Prevention. Mold prevention strategies and possible health effects in the aftermath of hurricanes and major floods MMWR Recomm Rep. 200655RR-81–27. [PubMed] [Google Scholar]
- 45.Pearson D, Ebisu K, Wu X, Basu R. A review of coccidioidomycosis in California: exploring the intersection of land use, population movement, and climate change. Epidemiol Rev. 2019;41(1):145–157. doi: 10.1093/epirev/mxz004. [DOI] [PubMed] [Google Scholar]
- 46.Gomez M.2012. https://www.hiv.gov/blog/natural-disasters-and-people-living-with-hiv-and-aids-2
- 47.Yamashita A, Gomez C, Dombroski K. Segregation, exclusion and LGBT people in disaster impacted areas: experiences from the Higashinihon Dai-Shinsai (Great East-Japan Disaster. Gend Place Cult. 2017;24(1):64–71. doi: 10.1080/0966369X.2016.1276887. [DOI] [Google Scholar]
- 48.Melin K, Maldonado WT. López-Candales A. Lessons learned from Hurricane Maria: pharmacists’ perspective. Ann Pharmacother. 2018;52(5):493–494. doi: 10.1177/1060028017751691. [DOI] [PubMed] [Google Scholar]
- 49.Vinyeta K, Whyte KP, Lynn K.2015. https://www.fs.fed.us/pnw/pubs/pnw_gtr923.pdf