Abstract
We conducted a second nationwide severe acute respiratory syndrome coronavirus 2 seroprevalence study in the Faroe Islands during November 2020. We found crude seroprevalence was 0.3% and prevalence was 0.4% after adjusting for test sensitivity and specificity. This low seroprevalence supports the prevention strategies used in the Faroe Islands.
Keywords: COVID-19, respiratory infections, severe acute respiratory syndrome coronavirus 2, SARS-CoV-2, SARS, coronavirus disease, zoonoses, viruses, coronavirus, seroprevalence, Faroe Islands
Early in the coronavirus disease (COVID-19) pandemic, the World Health Organization recommended close surveillance and abundant testing at the regional level (1). In the Faroe Islands, extensive testing capacity, easily accessible testing, and intensive contact tracing helped eliminate COVID-19 after the first (2) and second epidemic waves and further contained outbreaks later in 2020 (3). A population-based seroprevalence study of 1,075 persons in the Faroe Islands during May 2020 reported few undetected cases (4). However, prevalence studies from Spain, Greece, and Denmark measured severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibody seroprevalences of 0.36%–34.6% (5–7).
During the first COVID-19 wave in the Faroe Islands, societal lockdown and border closings helped contain the contagion. After the first wave, rather than reinstating lockdown, the country implemented testing, tracing, and quarantine, combined with entry restrictions for travelers, including a negative SARS-CoV-2 test upon entry and recommended self-quarantine until retesting 6 days after arrival (3). Despite society returning to near prepandemic normal, subsequent outbreaks in the Faroe Islands were contained efficiently. However, the reopening strategy might have led to undetected cases. We conducted a seroprevalence survey to estimate the number of undetected COVID-19 cases in the Faroe Islands.
We randomly selected 1,500 persons from the Faroese Population Registry (https://www.us.fo/Default.aspx?ID=13792). After excluding 2 newborns, we invited 1,498 persons by letter to provide blood samples at 1 of 6 study sites around the islands during November 21–30, 2020. We offered home visits to those unable to attend. Nonresponders received a follow-up phone call. All participants provided oral and written informed consent. The study was approved by the Faroese Ethical Committee and Data Protection Agency and is methodologically aligned with the World Health Organization generic protocol for population-based seroepidemiologic COVID-19 studies (1).
We conducted total antibody analyses by using the SARS-CoV-2 Ab ELISA Kit (Beijing Wantai Biologic Pharmacy Enterprise, https://www.ystwt.cn), which has a sensitivity of 94.4% (95% CI 90.9%–96.8%) and specificity of 100% (95% CI 98.8%–100.0%). We estimated 95% CI for crude seroprevalence by using exact binomial models and used bootstrap methods to adjust seroprevalence for test performance (8).
In all, 960 (64.1%) persons participated in the serosurvey (Figure); mean age was 48 years (SD 21.0, range 1–98 years), 52.2% were female, and 47.8% were male (Table). We excluded 12 persons with a previous positive reverse transcription PCR (RT-PCR) result from the seroprevalence study but included them in the total number of cases.
Figure.
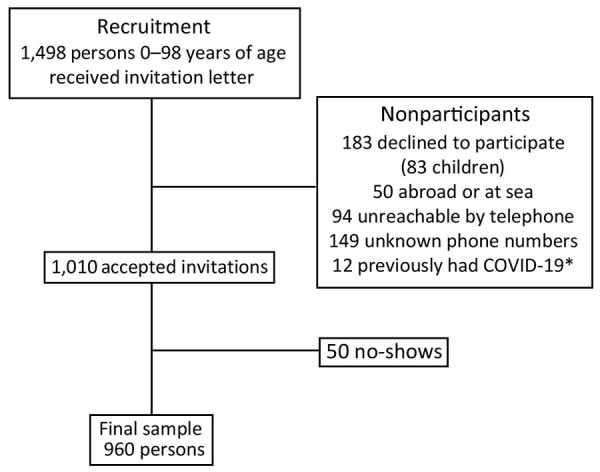
Flowchart of participant recruitment for severe acute respiratory syndrome coronavirus 2 seroprevalence study, Faroe Islands, November 2020. *Persons previously diagnosed with COVID-19 were excluded from serosurvey but included in the total number of cases. COVID-19, coronavirus disease.
Table. Characteristics of study participants compared with entire population and crude prevalence for severe acute respiratory syndrome coronavirus 2–specific antibodies, Faroe Islands, November 2020.
| Characteristics | No. (%) sampled | Total population (%) | p value | No. positive | Crude seroprevalence, % (95% CI)* |
|---|---|---|---|---|---|
| Total |
960 (100) |
52,854 (100) |
|
3 |
0.3 (0.06–0.9) |
| Sex | |||||
| M | 459 (47.8) | 27,380 (51.8) | 0.014 | 1 | 0.2 (0.01–1.2) |
| F |
501 (52.2) |
25,474 (48.2) |
0.014 |
2 |
0.4 (0.05–1.4) |
| Age, y | |||||
| 0–9 | 33 (3.4) | 7,259 (13.7) | <0.0001 | 1 | 3.0 (0.08–15.8) |
| 10–19 | 76 (7.9) | 7,357 (13.9) | <0.0001 | 0 | 0 |
| 20–29 | 88 (9.2) | 5,983 (11.3) | 0.0414 | 0 | 0 |
| 30–39 | 134 (14.0) | 6,534 (12.4) | 0.1364 | 0 | 0 |
| 40–49 | 135 (14.1) | 6,554 (12.4) | 0.1136 | 0 | 0 |
| 50–59 | 191 (19.9) | 6,780 (12.8) | <0.0001 | 0 | 0 |
| 60–69 | 157 (16.4) | 5,685 (10.8) | <0.0001 | 2 | 1.3 (0.2–4.5) |
| 70–79 | 103 (10.7) | 4,337 (8.2) | 0.0053 | 0 | 0 |
| 80–89 | 36 (3.8) | 1,875 (3.5) | 0.6165 | 0 | 0 |
|
>90 |
7 (0.7) |
490 (0.9) |
0.5147 |
0 |
0 |
| Geographic area | |||||
| Streymoy | 473 (49.3) | 25,288 (47.8) | 0.3565 | 2 | 0.4 (0.05–1.5) |
| Eysturoy | 216 (22.5) | 11,966 (22.6) | 0.9415 | 0 | 0 |
| Norðoyggjar | 114 (11.9) | 6,278 (11.9) | 1 | 0 | 0 |
| Vágar | 49 (5.1) | 3,361 (6.4) | 0.1023 | 0 | 0 |
| Sandoy og Suðuroy | 108 (11.2) | 5,961 (11.3) | 0.9227 | 1 | 0.9 (0.02–5.1) |
*Exact 95% CI calculated by binomial regression.
The study sample was geographically representative of the population but had minor differences in sex and age distribution. More men and younger persons comprised nonparticipants than participants: 41.3 (SD +23.4) years of age for nonparticipants versus 48.1 (SD +20.5) years of age for participants (p<0.0001). Persons 0–29 years of age were underrepresented and persons 50–79 years of age overrepresented.
Among participants, 3 tested positive for SARS-CoV-2–specific antibodies, resulting in a crude seroprevalence of 0.3% (exact binomial 95% CI 0.06%–0.9%). After adjusting for test sensitivity and specificity, we estimated a seroprevalence of 0.4% (bootstrap 95% CI 0.1%–1.0%). Including cases previously confirmed by RT-PCR, seroprevalence in the sample was 1.5%.
We found only a few undetected cases, underpinning the effectiveness of the prevention strategies in the Faroe Islands. Among the 3 seropositive cases, 1 was a child who had experienced symptoms at the beginning of the epidemic. Subsequent serologic analyses revealed that both parents and the child’s siblings were seropositive. The other 2 seropositive cases were in adults who did not recall any symptoms.
Our study’s strengths include the sample size, ≈2% of the country’s population, and the high participation rate of 64%, which increases to 77% when we exclude 243 persons who were not reachable. A study of 82 seroprevalence estimates from 51 different locations and >500 participants noted infection rates ranging from 0.02% to 53.4% by September 9, 2020, but reported large variations in sampling, clustering, and adjustment for test performance (9). A serosurvey of 4,000 persons in Switzerland during November–December 2020 reported regional seroprevalence of 21.2% after the second pandemic peak (10), >10 times higher than that observed in the Faroe Islands. The differences in seroprevalence might reflect differences in COVID-19 management strategies and geography because, unlike Switzerland, the Faroe Islands do not share borders with other countries. Furthermore, participation rates in the study from Switzerland varied substantially across age groups, from 17% for persons 0–18 years of age to 69% for persons >65 years of age.
In May 2020, we estimated 0.6% seroprevalence in the Faroe Islands (4), resulting in slightly higher number of cases than official confirmed cases. Applying the 1.5% seroprevalence we found in this study to the overall population corresponds to 793 cases, whereas 663 RT-PCR–confirmed cases were officially reported (https://www.corona.fo). Nonetheless, our results show that prevention strategies effectively managed the COVID-19 epidemic in the Faroe Islands and that the country effectively reacted to timely information of the contagion.
Acknowledgments
We thank all the study subjects for participating and the technicians around the islands for drawing blood samples. We thank Durita Djurhuus, Marjun Danielsen, Elsa Helmsdal, and Marita Hansen for assistance in contacting the participants. We also thank to the Faroese COVID-19 Research Group for support.
This project was funded by the Association of Pelagic Fishing Vessels, Felagnum Nótaskip.
Biography
Dr. Petersen is an associate professor at the University of the Faroe Islands, a senior researcher at the Faroese Hospital System, and head of the Centre of Health Sciences, Tórshavn, Faroe Islands. Her primary research interests include epidemiological research, and she has initiated and conducted multiple COVID-19 health science research projects in the Faroe Islands.
Footnotes
Suggested citation for this article: Petersen MS, Strøm M, Fjallsbak JP, Hansen JL, Larsen S, Eliasen EH, et al. Low seroprevalence among undetected COVID-19 cases, Faroe Islands, November 2020. Emerg Infect Dis. 2022 Jan [date cited]. https://doi.org/10.3201/eid2801.210917
References
- 1.World Health Organization. Population-based age-stratified seroepidemiological investigation protocol for coronavirus 2019. (COVID-19) infection, 2020 May 26 [cited 2020 Apr 1]. https://www.who.int/publications/i/item/WHO-2019-nCoV-Seroepidemiology-2020.2
- 2.Kristiansen MF, Heimustovu BH, Borg SA, Mohr TH, Gislason H, Møller LF, et al. Epidemiology and clinical course of first wave coronavirus disease cases, Faroe Islands. Emerg Infect Dis. 2021;27:749–58. 10.3201/eid2703.202589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strøm M, Kristiansen MF, Christiansen DH, Weihe P, Petersen MS. Elimination of COVID-19 in the Faroe Islands: Effectiveness of massive testing and intensive case and contact tracing. Lancet Reg Health Eur. 2021;1:100011. 10.1016/j.lanepe.2020.100011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petersen MS, Strøm M, Christiansen DH, Fjallsbak JP, Eliasen EH, Johansen M, et al. Seroprevalence of SARS-CoV-2–specific antibodies, Faroe Islands. Emerg Infect Dis. 2020;26:2761–3. 10.3201/eid2611.202736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pollán M, Pérez-Gómez B, Pastor-Barriuso R, Oteo J, Hernán MA, Pérez-Olmeda M, et al. ; ENE-COVID Study Group. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet. 2020;396:535–44. 10.1016/S0140-6736(20)31483-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bogogiannidou Z, Vontas A, Dadouli K, Kyritsi MA, Soteriades S, Nikoulis DJ, et al. Repeated leftover serosurvey of SARS-CoV-2 IgG antibodies, Greece, March and April 2020. Euro Surveill. 2020;25:25. 10.2807/1560-7917.ES.2020.25.31.2001369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iversen K, Bundgaard H, Hasselbalch RB, Kristensen JH, Nielsen PB, Pries-Heje M, et al. Risk of COVID-19 in health-care workers in Denmark: an observational cohort study. Lancet Infect Dis. 2020;20:1401–8. 10.1016/S1473-3099(20)30589-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Speybroeck N, Devleesschauwer B, Joseph L, Berkvens D. Misclassification errors in prevalence estimation: Bayesian handling with care. Int J Public Health. 2013;58:791–5. 10.1007/s00038-012-0439-9 [DOI] [PubMed] [Google Scholar]
- 9.Ioannidis JPA. Infection fatality rate of COVID-19 inferred from seroprevalence data. Bull World Health Organ. 2021;99:19–33F. 10.2471/BLT.20.265892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stringhini S, Zaballa ME, Perez-Saez J, Pullen N, de Mestral C, Picazio A, et al. ; Specchio-COVID19 Study Group. Seroprevalence of anti-SARS-CoV-2 antibodies after the second pandemic peak. Lancet Infect Dis. 2021;21:600–1. 10.1016/S1473-3099(21)00054-2 [DOI] [PMC free article] [PubMed] [Google Scholar]


