Abstract
Background
The impact of striae gravidarum (SG), or stretch marks of pregnancy, on quality of life (QoL) is unclear.
Objective
The purpose of this study was to investigate how SG affect QoL in pregnant women.
Methods
In this cross-sectional survey study of healthy pregnant women who developed SG during their current pregnancy, we asked about the impact of lesions on emotional, psychological, and life-quality facets. Spearman product-moment correlation coefficients were generated to determine the strength of relationships between variables.
Results
We analyzed 116 valid surveys. Participants reported permanency of SG as the top physical concern (n = 87; 75%). With regard to severity, nearly three-quarters of participants rated their lesions as very prominent (n = 24; 21%) or moderate (n = 57; 49%). Among the life-quality facets queried, embarrassment/self-consciousness was the most frequently associated with SG, with over one-third of participants reporting “a lot” (n = 19; 16%) or a “moderate” (n = 26; 22%) amount of embarrassment/self-consciousness related to having SG. Lesion severity significantly correlated with the degree of embarrassment/self-consciousness (r = .543), as well as the impact of SG on other life-quality facets, including overall QoL (r = .428), clothing choice (r = .423), self-image/self-esteem (r = .417), feelings of anxiety/depression (r = .415), and social activities (r = .313; all p ≤ .001). Nearly one-quarter of participants believed that emotional distress related to SG was similar or greater than that caused by other skin problems, such as acne, psoriasis, or eczema.
Conclusion
SG can be associated with a host of negative reactions reflecting increased psychological and emotional distress, including embarrassment and decreased QoL. These consequences may compound the emotional stress of pregnancy, potentially warranting psychological support and adjustment strategies.
Keywords: stretch marks, striae distensae, striae gravidarum, perceptions, emotional impact, pregnancy
What is known about this subject in regard to women and their families?
-
•
The impact of stretch marks of pregnancy, or striae gravidarum (SG), on women’s quality of life is unclear.
-
•
There are few studies investigating the effects of SG on the psychological and emotional health of pregnant women.
-
•
Prior observations suggest that SG cause concern for many women.
What is new from this article as messages for women and their families?
-
•
Among the life-quality facets that we queried, embarrassment/self-consciousness was the most frequently associated with striae gravidarum (SG).
-
•
Severity of SG was correlated with the degree of embarrassment/self-consciousness, as well as the impact of lesions on other life-quality facets, including overall quality of life, clothing choice, self-image/self-esteem, feelings of anxiety/depression, and social activities.
-
•
Some women feel that emotional distress related to SG is similar to that caused by other skin problems, such as acne, psoriasis, or eczema.
-
•
SG are associated with a constellation of negative reactions reflecting increased emotional/psychological distress, which potentially compounds the stress inherent to pregnancy.
Alt-text: Unlabelled box
Introduction
Striae distensae (SD), or stretch marks, develop as a result of obesity, growth spurts, rapid weight gain, corticosteroid therapy, or pregnancy. Stretch marks resulting from pregnancy, or striae gravidarum (SG), affect as many as 50% to 90% of women and usually develop on the abdomen and breasts during the second or third trimester (Chang et al., 2004). Lesions begin as erythematous to violaceous itchy streaks (striae rubra) that mature over months to years into shiny, hypopigmented, atrophic, permanent, scar-like bands (striae alba).
Although little is known about the molecular pathogenesis of SG (Korgavkar and Wang, 2015; Mitts et al., 2005; Salter and Kimball, 2006; Wang et al., 2015; 2018), numerous risk factors predispose women to developing lesions, such as a family history of SG, personal history of SD on the breasts or thighs, and young maternal age (Al-Himdani et al., 2014; Atwal et al., 2006; Chang et al., 2004; Osman et al., 2007). Interestingly, there are conflicting reports regarding the role of skin stretching as a risk factor (Arem and Kischer, 1980; Mitts et al., 2005; Poidevin, 1959; Wang et al., 2015), as increased maternal baseline weight, maternal weight gain during pregnancy, abdominal and hip girth of the mother during pregnancy, and neonatal weight have inconsistently been associated with the emergence of lesions (Al-Himdani et al., 2014; Atwal et al., 2006; Chang et al., 2004; Davey, 1972; Elsaie et al., 2009; Osman et al., 2007; Picard et al., 2015; Poidevin, 1959).
Although SG are not physically detrimental, lesions can be undesirable and, in severe cases, cosmetically disfiguring (Salter and Kimball, 2006; Yamaguchi et al., 2012). Despite the expense and lack of efficacy of various therapies for SG, many women report trying oils, emollients, massage, prescription and over-the-counter topical remedies, vitamins, lasers, and more recently microneedling to prevent lesions or improve their appearance (Al-Himdani et al., 2014; Korgavkar and Wang, 2015; Park et al., 2012; Salter and Kimball, 2006). These observations suggest that SG cause concern for many women and are associated with increased self-consciousness.
There are few studies investigating the effects of SG on the psychological and emotional health of women (Yamaguchi et al., 2012). However, studies have found that other skin disorders, such as acne, eczema, and psoriasis, cause psychosocial impairment, including poor self-image, depression/anxiety, and decreased quality of life (QoL; Dowlatshahi et al., 2014; Dunn et al., 2011; Fox et al., 2007; Gupta and Gupta, 2003; Holm et al., 2016; Koo, 1995; Lewis-Jones, 2006; Mulder et al., 2001; Skevington et al., 2006; Yazici et al., 2004). In the present study, we hypothesized that SG negatively affect the psychological and emotional wellbeing of pregnant women. To investigate this hypothesis, we conducted a cross-sectional survey study of healthy, pregnant women with SG. We evaluated participants’ general views and specific concerns about SG, as well as the impact of lesions on various facets of life quality. We found that SG can be associated with a host of negative reactions reflecting increased psychological and emotional distress.
Methods
Subjects
The study was approved by the institutional review board at the University of Michigan Medical School and conducted in accordance with the Declaration of Helsinki principles. Participants were recruited from outpatient clinics at the Departments of Obstetrics/Gynecology and Dermatology and during tours of the Labor and Delivery Unit at the Von Voigtlander Women's Hospital at the University of Michigan in Ann Arbor, Michigan. After providing written informed consent, participants were administered a one-time written survey or directed to an online version of the survey available at UMClinicalStudies.org, powered by www.surveymonkey.com. The inclusion criteria included pregnancy, good general health (i.e., absence of acute physical, mental, or social distress), and age ≥18 years. The exclusion criteria included physical or mental health conditions that would impair the ability to complete a questionnaire.
Survey
The survey was adapted from the Dermatology Life Quality Index, a validated survey instrument, and specifically designed based on the authors’ experiences with patients who had SG. In particular, the content and format of the survey were modeled on questions from the Dermatology Life Quality Index that asked about the impact of skin disease on embarrassment/self-consciousness, clothing choice, leisure activities, and interpersonal problems. The content of the questions was also devised from direct discussions with pregnant women attending clinic appointments or participating in other research studies on SG at our institution (Wang et al., 2015; 2018) and discussions with expert colleagues in obstetrics and dermatology.
The survey consisted of 35 questions, 32 of which had 2 to 6 categorical answer choices (Supplemental File). Questions captured the following: demographic information (age, race, and income), pregnancy characteristics (gestational age, medical complications, and self-perceived weight gain), history of SG from prior pregnancies, family history of SD, specific physical concerns about SG, impact of SG on view of pregnancy, and willingness to prevent SG or seek treatment. Additional questions included the following: self-evaluation of SG severity based on a scale (“barely visible,” “moderate,” or “very prominent”), impact of SG on specific life-quality facets (embarrassment, social activities, clothing choice, interpersonal problems, anxiety/depression, and overall QoL), and location of lesions.
A total of 218 surveys were received. Ninety-three surveys were excluded from the analysis because responders did not report SG related to the current pregnancy. The remaining 125 surveys were from participants reporting the presence of SG related to their current pregnancy. Nine of these surveys were excluded due to consent violation (n = 1), conflicting information (n = 1), or participants not being pregnant (n = 7), resulting in a total of 116 valid surveys.
Power and statistics
To find significant Spearman correlation coefficients with 80% power at a two-sided 5% significance level, a minimum number of 85 valid surveys from participants reporting the presence of SG was needed, as determined by an a priori power analysis assuming Cohen's medium effect size rules. The 116 surveys that were analyzed resulted in 90% power.
All categorical variables were summarized by frequency and/or percentage for each category. Differences were statistically assessed using Pearson's x2 test for categorical variables. Spearman product-moment correlation coefficients were generated to determine the strength of the relationships between the response variables. Correlations of moderate and strong value (defined as r ≥ 0.3 and r ≥ 0.7, respectively) were considered relevant and are presented. An overall alpha level of 0.05 was used to determine statistical significance, and tests were two-sided. All data were analyzed using SAS software, version 9.3 (SAS Institute, Cary, NC).
Results
Demographic and clinical characteristics of participants
Survey data from 116 women who developed SG during their current pregnancy are presented. Demographic and clinical information are summarized in Table 1. Nearly 72% of participants were age 26 to 35 years. More than two-thirds of the participants were white, with the remainder identifying themselves as Asian, Black or African-American, Native American, or other. There was a wide distribution of annual household incomes, although some women preferred not to answer this question.
Table 1.
Demographic information, pregnancy characteristics, and medical history of participants.
| Pregnant women with striae gravidarum (n = 116), n (%) | ||
|---|---|---|
| Age, years | <20 | 3 (2) |
| 20–25 | 19 (16) | |
| 26–30 | 46 (40) | |
| 31–35 | 37 (32) | |
| 36–40 | 9 (8) | |
| >40 | 2 (2) | |
| Race | Caucasian | 80 (69) |
| Asian | 17 (15) | |
| Black or African-American | 13 (11) | |
| Native American | 1 (1) | |
| Other | 5 (4) | |
| Income | <$24,999 | 25 (22) |
| $25,000–$49,999 | 21 (18) | |
| $50,000–$74,999 | 14 (12) | |
| $75,000–$99,999 | 18 (16) | |
| >$100,000 | 19 (16) | |
| Prefer not to answer | 19 (16) | |
| First pregnancy | Yes | 54 (47) |
| No | 62 (53) | |
| Gestational age | First trimester | 2 (2) |
| Second trimester | 12 (10) | |
| Third trimester | 102 (88) | |
| Gestation | Single | 109 (95) |
| Multiple | 4 (3) | |
| Not sure | 2 (2) | |
| Planned pregnancy | Yes | 83 (72) |
| No | 33 (28) | |
| Major medical complications with current pregnancy | Yes | 15 (13) |
| No | 98 (87) | |
| Weight gain | Below average | 9 (8) |
| Average | 87 (76) | |
| Above average | 19 (16) | |
| Diagnosis of mental health condition | Yes | 18 (16) |
| No | 96 (84) | |
| Past stretch marks | Yes, from previous pregnancy | 51 (45) |
| Yes, not pregnancy-related | 38 (33) | |
| No | 25 (22) | |
| Family history of stretch marks | Yes | 76 (65) |
| No | 10 (9) | |
| Not sure | 30 (26) | |
Nearly half of participants were pregnant for the first time, and most participants were in the third trimester with a single-gestation, planned pregnancy. Most reported no major medical complications and had “average” weight gain during the current pregnancy. The majority of participants had no history of a mental health condition. Almost half of participants (45%) had a history of SG from prior pregnancies, 33% had SD from other causes, and 65% reported a family history of SD.
Characteristics and perception of striae gravidarum
When asked where SG from the current pregnancy were located, participants reported that the most frequently affected area was the abdomen (n = 87; 75%), followed by the breasts (n = 50; 43%), hips (n = 50; 43%), thighs (n = 42; 36%), buttocks (n = 22; 19%), or other areas (n = 7, 6%). Addition of these percentages was >100% because participants could choose multiple answers. The number of locations affected by SG was moderately correlated with a history of prior SD from any cause (r = .30; p = .001), but not primigravid status or self-reported weight gain (data not shown).
Participants were next asked questions about physical concerns related to SG (Table 2). Permanency of lesions was the top physical concern about SG (n = 87; 75%). Discoloration (n = 43; 37%) and discomfort (n = 26; 22%), such as itching or pain, were less frequently reported concerns. Individual physical concerns did not correlate significantly with demographic characteristics, including age and income (data not shown).
Table 2.
Concerns regarding SG and interest in prevention or treatment
| Pregnant women with SG (n = 116), n (%) | ||
|---|---|---|
| Specific physical concerns regarding SG* | Permanency | 87 (75) |
| Discoloration | 43 (37) | |
| Discomfort (pain/itching) | 26 (22) | |
| Other | 4 (3) | |
| Used creams/oils to prevent SG | Yes | 58 (51) |
| No | 57 (49) | |
| Interest in treatment | Yes | 23 (20) |
| Maybe | 63 (54) | |
| Unsure | 16 (14) | |
| No | 14 (12) | |
| Interest in treatment if not covered by insurance | Yes | 9 (8) |
| Maybe | 29 (25) | |
| Unsure | 13 (11) | |
| No | 65 (56) | |
SG = striae gravidarum
Addition of percentages is greater than 100% because participants could choose multiple answers for this question.
We then asked participants about attempts at prevention, as well as the general desire to treat SG. Approximately half of participants (n = 58; 51%) reported attempting to prevent SG, typically with topical agents (e.g., creams or oils). When asked about willingness to seek treatment for SG if readily available, most participants reported “yes” or “maybe” (total n = 86; 74%). If treatment was not covered by insurance, the number of participants reporting these answers decreased significantly (total n = 38; 33%; p = .008; Table 2).
Correlation of severity of striae gravidarum with life-quality facets
With regard to the severity of lesions, nearly half of participants rated their lesions as “moderate” (n = 57; 49%). Others said that their lesions were either “barely visible” (n = 35; 30%) or “very prominent” (n = 24; 21%).
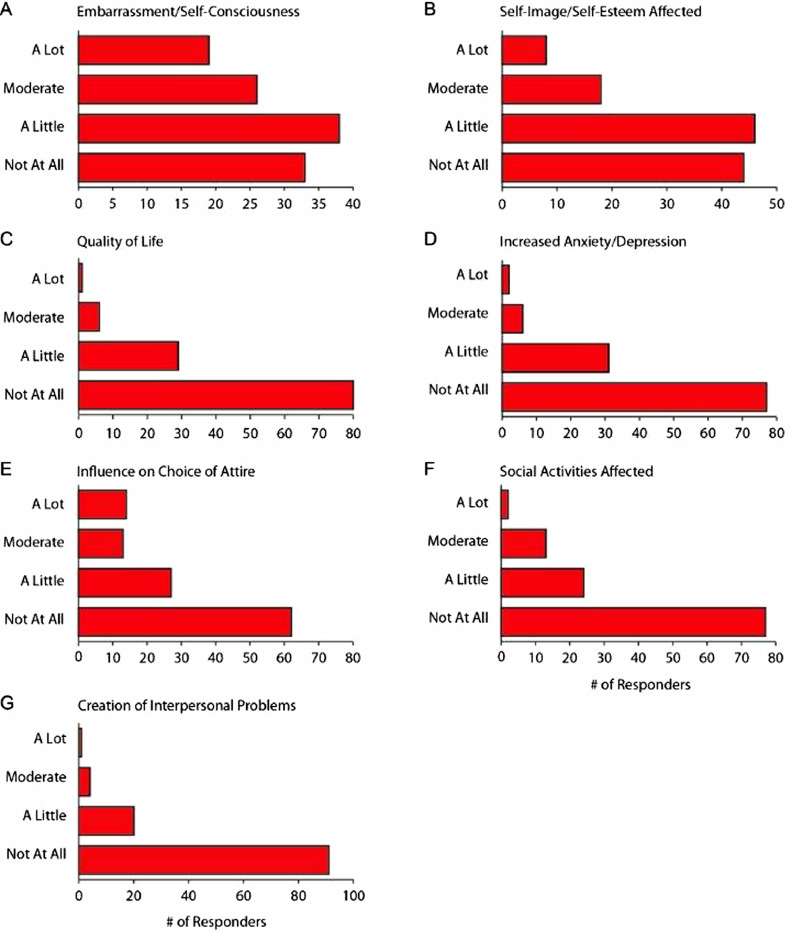
Participants were then asked questions about the impact of lesions on specific emotional, psychological, and life-quality facets, including embarrassment/self-consciousness, self-image/self-esteem, overall QoL, feelings of anxiety/depression, choice of attire, and social activities (Fig. 1). Overall, the parameter that was affected the most was embarrassment/self-consciousness, with more than one-third of women reporting either “a lot” (n = 19; 16%) or a “moderate” (n = 26; 22%) amount of embarrassment related to having SG.
Fig. 1.
Striae gravidarum: Impact of lesions on specific emotional, psychological, and life-quality facets in pregnant women. Participants with striae gravidarum (n = 116) were asked questions about the impact of lesions on various life-quality facets, as indicated. The x-axis for each bar graph indicates the number of responses for each answer.
Next, we performed correlative statistics to examine the degree to which specific life-quality facets were correlated with lesion severity (Table 3). Embarrassment/self-consciousness displayed the strongest correlation with lesion severity (r = .543; p < .001). In order of descending correlation, the following life-quality facets were also correlated with lesion severity: impact of SG on general QoL (r = .428; p < .001), impact of SG on choice of attire (r = .423; p < .001), impact of SG on self-image/self-esteem (r = .417; p < .001); feelings of anxiety/depression related to SG (r = .415; p < .001), alteration of social/leisure activities related to SG (r = .313; p = .001), and creation of interpersonal problems related to SG to SG (r = .221; p = .017).
Table 3.
Correlation between lesion severity and psychological/emotional distress related to striae gravidarum
| Correlation with lesion severity, r (p-value) | ||
|---|---|---|
| Embarrassment/self-consciousness | .543 (<.001) | |
| General quality of life | .428 (<.001) | |
| Choice of attire | .423 (<.001) | |
| Self-image/self-esteem | .417 (<.001) | |
| Anxiety/depression | .415 (<.001) | |
| Social activities affected | .313 (.001) | |
| Creation of interpersonal problems | .221 (.017) |
Impact of striae gravidarum on life-quality and association with younger age and weight gain
When evaluating how specific life-quality facets (originally displayed in Fig. 1) were correlated with demographic/clinical characteristics, we found that increased impact of SG on self-image/self-esteem was moderately associated with younger age (r = – .31; p < .001) and that increased embarrassment related to SG was moderately associated with weight gain during pregnancy (r = .30; p < .001).
There were no substantial correlations between life-quality facets and other demographic/clinical characteristics, such as income, personal history of SG, family history of SG, gravidity of women, or planned pregnancy (data not shown).
Impact of striae gravidarum on multiple life-quality facets in correlated fashion
Next, we analyzed correlations between each of the life-quality facets, as originally displayed in Figure 1. Table 4 displays these correlations. We found that the more SG caused embarrassment/self-consciousness, the greater the impact of lesions on self-image/self-esteem (r = .751; p < .001), clothing choice r = .706; p < .001), or social/leisure activities (r = .688; p < .001). Additionally, we observed strong correlations between anxiety/depression related to SG and impact on self-image/self-esteem (r = .634; p < .001) and between impact of SG on social/leisure activities and influence on clothing choice (r = .716; p < .001).
Table 4.
Correlation between psychological/emotional parameters in women affected by striae gravidarum
| Self-image/ self-esteem affected | Type of clothing influenced | Social activities affected | Quality of life | Anxiety/ depression | Willingness to seek treatment | creation of interpersonal problems | Negative view of pregnancy | |
|---|---|---|---|---|---|---|---|---|
| Embarrassment/self-consciousness, r (p-value) | .751 (<.001)* | .706 (<.001)* | .688 (<.001)* | .620 (<.001) | .562 (<.001) | .436 (<.001) | .343 (<.001) | .327 (< .001) |
| Negative view of pregnancy, r (p-value) | .442 (<.001) | .241 (.009) | .272 (.003) | .382 (<.001) | .393 (<.001) | .253 (0.011) | .327 (<.001) | |
| Creation of interpersonal problems, r (p-value) | .427 (<.001) | .292 (.002) | .345 (<.001) | .522 (<.001) | .503 (<.001) | .243 (.015) | ||
| Willingness to seek treatment, r (p-value) | .509 (<.001) | .389 (<.001) | .359 (<.001) | .370 (<.001) | .378 (<.001) | |||
| Anxiety/depression, r (p-value) | .634 (<.001)* | .370 (<.001) | .392 (<.001) | .625 (<.001) | ||||
| Quality of life, r (p-value) | .633 (<.001) | .527 (<.001) | .572 (<.001) | |||||
| Social activities affected, r (p-value) | .559 (<.001) | .716 (<.001)* | ||||||
| Type of clothing influenced, r (p-value) | .616 (<.001) |
The five strongest correlations among measures of psychological distress due to striae gravidarum
Emotional impact of striae gravidarum compared with other skin diseases
Finally, we asked participants to compare the emotional distress caused by SG to that caused by other skin problems. Seventy-eight participants reported current or previous skin problems, such as acne, psoriasis, or eczema. Of these participants, 23% (n = 18) indicated that SG caused “much greater,” “greater,” or the “same” amount of distress as these other skin conditions. The same group was more likely to report greater severity of SG (r = .42; p < .0 0 1) and expressed a greater desire to seek treatment for SG (r = .53; p < .0 01). The same women were also more likely to indicate that SG affected the following life-quality facets (in order of descending correlation): embarrassment/self-consciousness (r = .57), clothing choice (r = .57), self-image/self-esteem (r = .59), social/leisure activities (r = .54), anxiety/depression (r = .44), general QoL (r = .43; all p < .0 01), and general perception of pregnancy (r = .28; p = .01).
Discussion
We undertook this study of pregnant women with SG to gain insight into general views of SG, the desire to prevent or treat lesions, and the impact of SG on various life-quality facets. We sought to better understand the impact of SG on the emotional and psychological health of pregnant women, with the idea that our findings would have implications for supporting the wellbeing of affected patients and developing effective therapeutic strategies.
We found that the permanency of SG represented the most pressing physical concern for the participants. Discoloration and discomfort were less disconcerting physical concerns, which may be because these features improve with time or emollients. Concern over permanency likely stems from general awareness or apprehension among women that SG pose a therapeutic challenge. Indeed, most topical and surgical modalities demonstrate minimal or inconsistent efficacy in preventing or improving SG (Korgavkar and Wang, 2015). Even currently available sophisticated surgical options, such as ablative fractional laser resurfacing, nonablative fractional lasers, radiofrequency, microneedling, platelet-rich plasma, and pulsed dye laser, may benefit some patients but not others (Wang et al., 2021). Yet, most of our participants reported attempting topical products to prevent SG and expressed willingness to seek treatment, if readily available. Thus, despite a lack of reliable therapeutic modalities, the desire to prevent or treat SG is common (Yamaguchi et al., 2012).
Many participants perceived their lesions to be moderate or prominent in severity. The severity of SG correlated with distress in multiple facets of life. For instance, greater severity of lesions was associated with increased embarrassment/self-consciousness from SG, as well as increased impact of SG on general QoL, choice of attire, self-image/self-esteem, feelings of anxiety/depression, and social/leisure activities. Unlike previous reports, we did not observe a correlation between lesion severity and demographic or medical characteristics, such as younger age or family history of SG (Osman et al., 2007). However, when examining the correlation between demographic characteristics and life-quality facets, we found that younger age was associated with decreased self-image/self-esteem related to SG. As such, medical providers may consider asking patients, particularly younger women, about the impact of SG on emotional wellbeing.
When investigating the associations between individual emotional, psychological, and life-quality facets affected by SG, we found numerous correlations, as shown in Table 4. For instance, increased embarrassment/self-consciousness attributed to SG was correlated with increased impact of SG on self-image and clothing choice. Based on these findings, patients who believe that SG negatively influence one aspect of their life-quality or emotional health are likely vulnerable to additional negative emotional consequences related to SG. Similarly, other dermatologic disorders, such as acne, appear to affect multiple psychological and emotional factors in a correlated manner (Dunn et al., 2011).
Finally, we found that, for a proportion of participants, the distress associated with SG may be comparable to that of other dermatologic disorders, such as acne, psoriasis, or eczema (Dowlatshahi et al., 2014; Dunn et al., 2011; Fox et al., 2007; Gupta and Gupta, 2003; Holm et al., 2016; Koo, 1995; Lewis-Jones, 2006; Mulder et al., 2001; Skevington et al., 2006; Yazici et al., 2004). This subgroup is more likely to perceive their SG lesions to be severe and is more likely to feel that SG affect multiple life-quality facets. As such, we suggest that health care providers avoid thinking of SG as merely a cosmetic nuisance. Instead, providers should approach SG like other dermatologic concerns and consider asking patients whether SG cause emotional distress and whether prevention or treatment strategies should be attempted, even if not completely effective and potentially costly. Providers might also consider whether patients could benefit from psychological support and adjustment strategies.
Compared with a prior study, which used a general dermatologic survey to study the impact of SG on QoL (Yamaguchi et al., 2012), our study involved the use of survey questions specifically designed for pregnant women with SG, such as the influence of lesions on clothing choice. Additionally, we related pregnancy-specific characteristics to the impact of SG on specific life-quality facets and assessed the correlations between these life-quality parameters to provide insight into the impact of one facet on another and highlight the complexity of the emotional impact of SG on pregnant women.
There are limitations to this study. First, some data, such as lesion severity, were obtained through self-report rather than assessments by health care providers. However, patients’ self-perception of severity and/or disfigurement is an important driver of embarrassment, self-consciousness, and desire to seek treatment (Koo, 1995; Mulder et al., 2001; Russo et al., 2004; Yazici et al., 2004). In addition, survey data were obtained from healthy women who had not experienced major pregnancy complications and were attending well-pregnancy visits at a tertiary care referral institution. It is not clear whether attitudes toward SG are similar among women with high-risk or medically complicated pregnancies.
Level of education was not assessed in participants but may influence attitudes toward SG and be of interest to investigate in the future. Likewise, it may be intriguing to investigate whether pregnant women's attitudes toward SG change after delivery. Finally, the nature of our correlative data (as displayed in Table 4) highlights associations but does not necessarily establish causality between the various life-quality facets.
Conclusion
Pregnancy is a joyful yet stressful life-changing event. Our study suggests that SG may compound this stress for some women, negatively affecting their psychological and emotional wellness, much like psoriasis, eczema, or acne often does for many patients. As such, patients who are affected by SG may benefit from psychological and emotional support. Our findings highlight the need for further epidemiologic, clinical, and basic science research, with the goal of better understanding the pathophysiology of SG (and SD in general) and translating these findings into effective prevention and treatment modalities.
Declaration of Competing Interest
None.
Acknowledgments
Acknowledgments
The authors thank the study participants; Jennifer Bell, our research coordinator; Debbie Smith, who assisted with the recruitment of the participants; Laura VanGoor, BFA, for assistance with the graphic material; and Erin Wal, for administrative assistance.
Funding
None.
Study approval
The author(s) confirm that any aspect of the work covered in this manuscript that has involved human patients has been conducted with the ethical approval of all relevant bodies.
Footnotes
Preliminary data were presented at the 71st Annual Meeting of the Society for Investigative Dermatology, held in Phoenix, Arizona in 2011, and the 6th International Congress on Dermato-Epidemiology, held in Malmö, Sweden in 2012.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijwd.2021.10.015.
Appendix. Supplementary materials
References
- Al-Himdani S, Ud-Din S, Gilmore S, Bayat A. Striae distensae: A comprehensive review and evidence-based evaluation of prophylaxis and treatment. Br J Dermatol. 2014;170:527–547. doi: 10.1111/bjd.12681. [DOI] [PubMed] [Google Scholar]
- Arem AJ, Kischer CW. Analysis of striae. Plast Reconstr Surg. 1980;65:22–29. doi: 10.1097/00006534-198001000-00005. [DOI] [PubMed] [Google Scholar]
- Atwal GS, Manku LK, Griffiths CE, Polson DW. Striae gravidarum in primiparae. Br J Dermatol. 2006;155:965–969. doi: 10.1111/j.1365-2133.2006.07427.x. [DOI] [PubMed] [Google Scholar]
- Chang AL, Agredano YZ, Kimball AB. Risk factors associated with striae gravidarum. J Am Acad Dermatol. 2004;51:881–885. doi: 10.1016/j.jaad.2004.05.030. [DOI] [PubMed] [Google Scholar]
- Davey CM. Factors associated with the occurrence of striae gravidarum. J Obstet Gynaecol Br Commonw. 1972;79:1113–1114. doi: 10.1111/j.1471-0528.1972.tb11896.x. [DOI] [PubMed] [Google Scholar]
- Dowlatshahi EA, Wakkee M, Arends LR, Nijsten T. The prevalence and odds of depressive symptoms and clinical depression in psoriasis patients: A systematic review and meta-analysis. J Invest Dermatol. 2014;134:1542–1551. doi: 10.1038/jid.2013.508. [DOI] [PubMed] [Google Scholar]
- Dunn LK, O'Neill JL, Feldman SR. Acne in adolescents: Quality of life, self-esteem, mood, and psychological disorders. Dermatol Online J. 2011;17:1. [PubMed] [Google Scholar]
- Elsaie ML, Baumann LS, Elsaaiee LT. Striae distensae (stretch marks) and different modalities of therapy: An update. Dermatol Surg. 2009;35:563–573. doi: 10.1111/j.1524-4725.2009.01094.x. [DOI] [PubMed] [Google Scholar]
- Fox FE, Rumsey N, Morris M. Ur skin is the thing that everyone sees and you can't change it!": Exploring the appearance-related concerns of young people with psoriasis. Dev Neurorehabil. 2007;10:133–141. doi: 10.1080/13638490701217594. [DOI] [PubMed] [Google Scholar]
- Gupta MA, Gupta AK. Psychiatric and psychological co-morbidity in patients with dermatologic disorders: epidemiology and management. Am J Clin Dermatol. 2003;4:833–842. doi: 10.2165/00128071-200304120-00003. [DOI] [PubMed] [Google Scholar]
- Holm JG, Agner T, Clausen ML, Thomsen SF. Quality of life and disease severity in patients with atopic dermatitis. J Eur Acad Dermatol Venereol. 2016;30(10):1760–1767. doi: 10.1111/jdv.13689. [DOI] [PubMed] [Google Scholar]
- Koo J. The psychosocial impact of acne: Patients' perceptions. J Am Acad Dermatol. 1995;32:S26–S30. doi: 10.1016/0190-9622(95)90417-4. [DOI] [PubMed] [Google Scholar]
- Korgavkar K, Wang F. Stretch marks during pregnancy: A review of topical prevention. Br J Dermatol. 2015;172:606–615. doi: 10.1111/bjd.13426. [DOI] [PubMed] [Google Scholar]
- Lewis-Jones S. Quality of life and childhood atopic dermatitis: The misery of living with childhood eczema. Int J Clin Pract. 2006;60:984–992. doi: 10.1111/j.1742-1241.2006.01047.x. [DOI] [PubMed] [Google Scholar]
- Mitts TF, Jimenez F, Hinek A. Skin biopsy analysis reveals predisposition to stretch mark formation. Aesthet Surg J. 2005;25:593–600. doi: 10.1016/j.asj.2005.09.004. [DOI] [PubMed] [Google Scholar]
- Mulder MM, Sigurdsson V, van Zuuren EJ, Klaassen EJ, Faber JA, de Wit JB, et al. Psychosocial impact of acne vulgaris. evaluation of the relation between a change in clinical acne severity and psychosocial state. Dermatology. 2001;203:124–130. doi: 10.1159/000051726. [DOI] [PubMed] [Google Scholar]
- Osman H, Rubeiz N, Tamim H, Nassar AH. Risk factors for the development of striae gravidarum. Am J Obstet Gynecol. 2007;196 doi: 10.1016/j.ajog.2006.08.044. 62.e1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park KY, Kim HK, Kim SE, Kim BJ, Kim MN. Treatment of striae distensae using needling therapy: A pilot study. Dermatol Surg. 2012;38:1823–1828. doi: 10.1111/j.1524-4725.2012.02552.x. [DOI] [PubMed] [Google Scholar]
- Picard D, Sellier S, Houivet E, Marpeau L, Fournet P, Thobois B, et al. Incidence and risk factors for striae gravidarum. J Am Acad Dermatol. 2015;73:699–700. doi: 10.1016/j.jaad.2015.06.037. [DOI] [PubMed] [Google Scholar]
- Poidevin LO. Striae gravidarum. Their relation to adrenal cortical hyperfunction. Lancet. 1959;2:436–439. doi: 10.1016/s0140-6736(59)90421-0. [DOI] [PubMed] [Google Scholar]
- Russo PA, Ilchef R, Cooper AJ. Psychiatric morbidity in psoriasis: A review. Australas J Dermatol. 2004;45:155–159. doi: 10.1111/j.1440-0960.2004.00078.x. quiz 60–1. [DOI] [PubMed] [Google Scholar]
- Salter SA, Kimball AB. Striae gravidarum. Clin Dermatol. 2006;24:97–100. doi: 10.1016/j.clindermatol.2005.10.008. [DOI] [PubMed] [Google Scholar]
- Skevington SM, Bradshaw J, Hepplewhite A, Dawkes K, Lovell CR. How does psoriasis affect quality of life? Assessing an Ingram-regimen outpatient programme and validating the WHOQOL-100. Br J Dermatol. 2006;154:680–691. doi: 10.1111/j.1365-2133.2005.07045.x. [DOI] [PubMed] [Google Scholar]
- Wang F, Calderone K, Do TT, Smith NR, Helfrich YR, Johnson TRB, et al. Severe disruption and disorganization of dermal collagen fibrils in early striae gravidarum. Br J Dermatol. 2018;178(3):749–760. doi: 10.1111/bjd.15895. [DOI] [PubMed] [Google Scholar]
- Wang F, Calderone K, Smith NR, Do TT, Helfrich YR, Johnson TR, et al. Marked disruption and aberrant regulation of elastic fibres in early striae gravidarum. Br J Dermatol. 2015;173:1420–1430. doi: 10.1111/bjd.14027. [DOI] [PubMed] [Google Scholar]
- Wang JV, Kream EJ, Munavalli GS, Geronemus RG. Experiences and perspectives of patients with striae: A survey with treatment implications. Dermatol Surg. 2021;47(10):1408–1410. doi: 10.1097/DSS.0000000000003167. [DOI] [PubMed] [Google Scholar]
- Yamaguchi K, Suganuma N, Ohashi K. Quality of life evaluation in Japanese pregnant women with striae gravidarum: A cross-sectional study. BMC Res Notes. 2012;5:450. doi: 10.1186/1756-0500-5-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yazici K, Baz K, Yazici AE, Kokturk A, Tot S, Demirseren D, et al. Disease-specific quality of life is associated with anxiety and depression in patients with acne. J Eur Acad Dermatol Venereol. 2004;18:435–439. doi: 10.1111/j.1468-3083.2004.00946.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.