Abstract
There has been exponential growth in research on emotion regulation and substance use in the past decade. The current meta-analysis evaluated variability in the magnitude of the relation between aspects of emotion regulation and substance use. A search of PsycINFO, Embase, PubMed, CINAHL Plus, and PILOTS in December 2020 resulted in 6,642 initial studies, of which 95 met inclusion criteria (association between emotion regulation and substance use was reported, participants were > 18 years old, article was in English). A total of 445 effects were obtained (N = 156,025 participants; weighted Mage = 29.31; 59.5% female; 66.1% White; 76.6% non-clinical). Emotion regulation and substance use were significantly related (r = 0.19; p < .001; 95%CI [0.17, 0.20]). Emotion regulation abilities were generally more strongly related to substance use than emotion regulation strategies; this pattern was stronger for behavioral vs. cognitive abilities and extended to both negative and positive emotions. Relations were stronger for older and clinical samples; mixed effects were found for sex and no conclusive effects were found for race. Despite limitations of the existing literature (e.g., cross-sectional, self-reports), results indicated that the magnitude of the relation between emotion regulation and substance use varied considerably as a function of emotion regulation and substance use constructs and sample characteristics.
Keywords: emotion regulation, DERS, ERQ, substance use, alcohol, drugs, tobacco
In recent years, there has been a surge of research on emotion regulation and substance use (see Weiss, Sullivan, et al., 2015; Weiss, Tull, et al., 2015). Emotion regulation predicts proximal intensity of emotion state (MacIntyre et al., 2018), which demonstrates a well-established and robust influence on substance use (for reviews, see O’Donnell et al., 2019; Shiffman, 2009; Wray et al., 2014). Individuals who exhibit emotion regulation difficulties may be more likely to engage in substance use as a means of alleviating or distracting themselves from emotional states perceived as aversive, consistent with negative reinforcement models (e.g., Baker et al., 2004). Alternatively, positive reinforcement models (e.g., Cooper et al., 2016) suggest that the immediate and short-term gratification associated with substance use may counter or distract from unpleasant emotional states that such individuals may be unwilling to approach, tolerate, or accept. Additionally, according to the resource model of self-control (Inzlicht & Schmeichel, 2012), deficits in emotion regulation promote substance use by reducing individuals’ ability to inhibit behaviors in emotionally salient contexts. The down-regulation of emotions is an effortful, and not necessarily immediately rewarding, process. As the need for regulation persists, individuals experience a shift in motivation from the regulation of emotion toward the acquisition of rewarding experiences. In turn, there is increased allocation of attention toward cues that signal immediate reward, thereby increasing substance use.
Empirical evidence supports an association between emotion regulation and substance use. First, individuals with vs. without alcohol (Fox et al., 2008) and drug (Fox et al., 2007) use disorders have been shown to exhibit greater deficits in emotion regulation. Second, cross-sectional correlational studies have found that greater deficits in emotion regulation relate to worse substance use (Dvorak et al., 2014; Weiss et al., 2018). Finally, clinical research provides evidence for impacts of emotion regulation on substance use treatment outcomes (Gratz et al., 2015). For instance, deficits in emotion regulation predict alcohol use during and after cognitive behavioral treatment for alcohol use (Berking et al., 2011), and treatments targeting an improvement in emotion regulation reduce substance use (Axelrod et al., 2011; Rodriguez et al., 2019). In sum, research on emotion regulation and substance use converges to underscore the key role of emotion regulation in the etiology, maintenance, and treatment of substance use.
Importantly, however, emotion regulation has varied definitions in the literature (Tull & Aldao, 2015), and research on its relation to substance use has relied on these diverse conceptualizations (Weiss, Sullivan, et al., 2015). In their review of the emotion regulation literature, Tull and Aldao (2015) distinguished between emotion regulation abilities and strategies. Emotion regulation abilities (or potential) refer to the typical or dispositional ways in which individuals understand, regard, and respond to their emotional experiences (see Gratz & Roemer, 2004; Thompson, 1994; Weiss, Gratz, et al., 2015). Emotion regulation ability models are multi-faceted, emphasizing ones’ awareness, understanding, and acceptance of emotions; ability to control behaviors when experiencing emotional distress; access to emotion regulation strategies that are perceived as effective and flexibly applied to modulate the duration and/or intensity of aversive emotional experiences; and willingness to experience emotional distress as part of pursing meaningful activities in life. Alternatively, the extended process model of emotion regulation (Gross, 2015) highlights the role of type and timing of emotion regulation strategies at different points in the emotion-generative process. Emotion regulation strategy models focus on the specific strategies individuals use (e.g., reappraisal, suppression) to influence the experience and expression of their emotions (see also Cole et al., 1994; Koole, 2009). Notably, ability and strategy models capture distinct and important aspects of the larger construct of emotion regulation, and thus their complementary examination provides valuable and comprehensive data on the relation of emotion regulation and substance use.
Advancing existing research, the current meta-analysis examined the nature and magnitude of the relations between emotion regulation (overall and across the specific aspects) and substance use (i.e., alcohol use only, drug use only, tobacco use only, use of multiple substances); as well as moderators of obtained associations. To our knowledge, only one meta-analytic review (Aldao et al., 2010) has examined the relation of emotion regulation and substance use (as part of a larger study on psychopathology). This study’s focus on substance use was considerably limited: (1) it was conducted in 2010 and almost all of the investigations in this area were published after this date; (2) it focused only on emotion regulation strategies, at the exclusion of abilities; and (3) only 10 effect sizes were available across two studies. Results from the current study will identify aspects of emotion regulation paramount to substance use, underscoring avenues for future research and targets for substance use interventions.
Of note, several constructs that are similar to emotion regulation have been studied in relation to substance use, such as mindfulness (Bodenlos et al., 2013; Fernandez et al., 2010), distress tolerance (Gorka et al., 2012; Marshall-Berenz et al., 2011), and anxiety sensitivity (Howell et al., 2010; Schmidt et al., 2008). Critically, literature shows that these constructs are distinct from emotion regulation (Bernstein et al., 2009; Brandt et al., 2012; Gratz & Tull, 2010; McHugh et al., 2013). Likewise, the focus of this review was on substance use; as such, papers that examined other substance-related constructs (e.g., coping, motives, expectancies) were excluded. Finally, experimental laboratory paradigms such as cue reactivity that intended to tap into emotion regulation processes and substance use but did not explicitly measure both emotion regulation and substance use were excluded from the current review (Tull, Berghoff, et al., 2016; Tull, Gratz, et al., 2016; Tull et al., 2018; Tull et al., 2019).
Method
Search Strategy
This review was registered with PROSPERO (CRD42021225363) and followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis guidelines (Moher et al., 2009). On December 9, 2020, a literature search was conducted in the following databases to identify articles that reported on relations between emotion regulation and substance use: PsycINFO (n = 2,540), Embase (n = 2,331), PubMed (n = 1,388), CINAHL Plus (n = 225), and PILOTS (n = 158). Search terms were: (emotion* regulation OR emotion* dysfunction OR emotion* dysregulation OR affect* regulation OR affect* dysfunction OR affect* dysregulation OR difficult* regulat*) AND (substance OR alcohol OR drug* OR addit* OR drink* OR marijuana OR cannabis OR cocaine OR opioid OR opiate OR prescription med* OR prescription pain* OR heroin OR *amphetamine* OR MDMA OR LSD OR stimulant OR sedative OR hallucinogen OR tobacco OR nicotine OR smok* OR cigarette* OR vape OR vaping OR crack OR illicit OR meth OR polydrug OR polysubstance OR PCP OR inhalant*).
Inclusion and Exclusion Criteria
Of the 6,642 titles that resulted from the literature search, 3,276 were retained for abstract review after removal of duplicates. Following the abstract review, 140 articles were selected for full-text review, based on the following criteria: (1) association between emotion regulation and substance use reported, (2) study participants were > 18 years old, and (3) article was written in English. In the 16 cases where sufficient information for calculating effect sizes was not reported, but all other inclusion criteria were met, we contacted study authors via email to request this information. Seven of these authors provided sufficient information for calculating effect sizes. Of the articles selected for full-text review, 15 were conference poster abstracts. These authors were contacted to inquire whether a manuscript was written from their data. Of the ten authors who responded, two provided manuscripts while the remaining eight stated that their project had not become a manuscript. Thus, 127 manuscripts (i.e., journal articles, theses, dissertations) were included in the final full-text review. Of these, 95 articles were deemed eligible for inclusion in this study. See Figure 1 for a flow chart of study selection.
Figure 1.
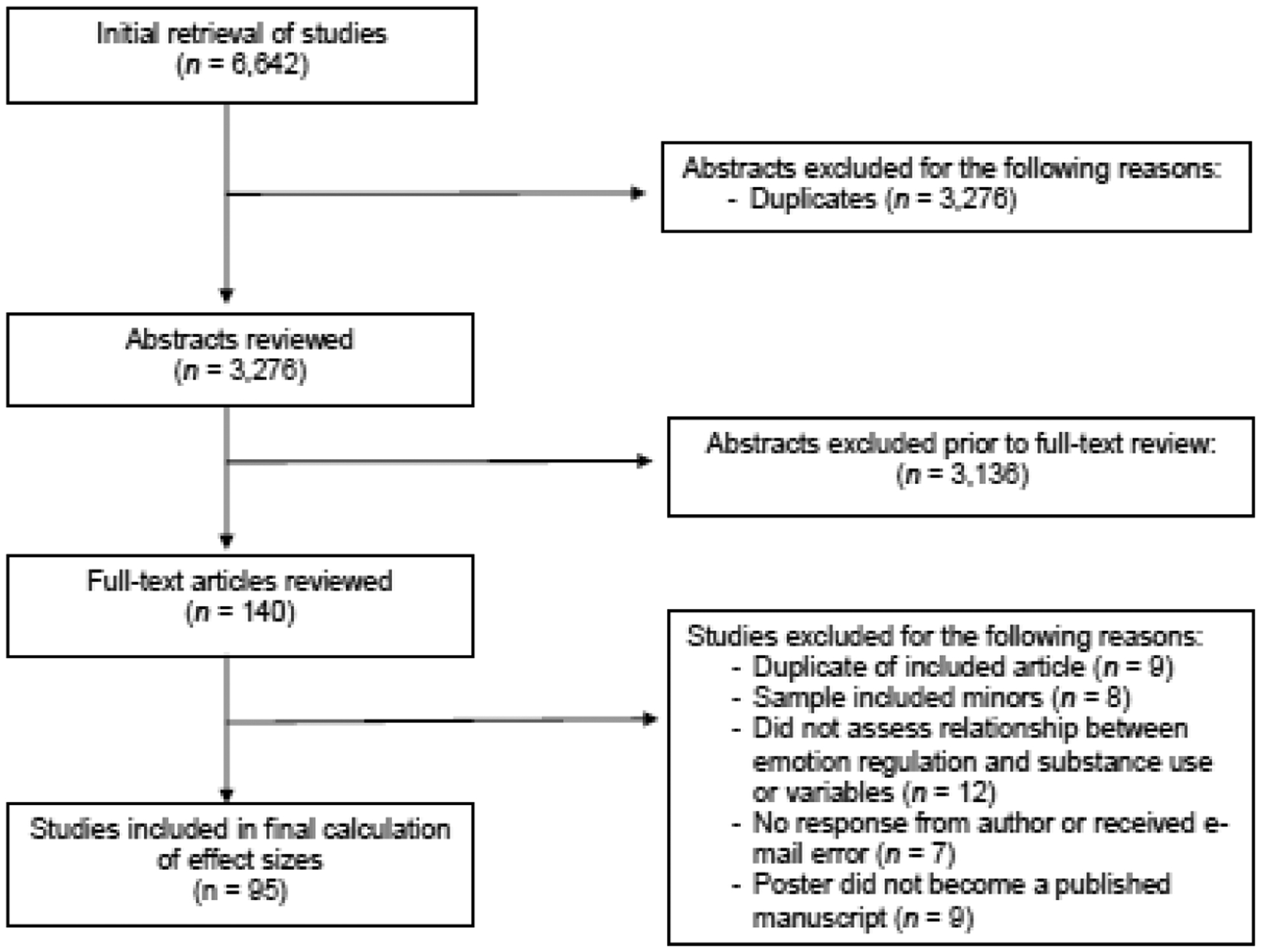
Flow chart for the selection of studies used in the meta-analysis.
Coding
The 3,276 abstracts were independently double coded by undergraduate research assistants, graduate research assistants, and the first author. All discrepancies in double coding were resolved by an additional round of independent coding and through discussions with the first author. Full-text coding decisions were made collaboratively by the study authors. The following information was extracted from each article: (1) author name(s) and publication year; (2) study type (i.e., journal article, thesis, or dissertation); (3) study design (e.g., correlational, group comparison, longitudinal); (4) sample size; (5) mean, standard deviation, and range of sample age; (6) sex (i.e., percent female); (7) race as a series of continuous variables (i.e., percent White, Black or African American, American Indian or Alaskan Native, Asian, Native Hawaiian or Other Pacific Islander, Hispanic or Latino/a, Multiracial, or Other); (8) sample type (i.e., clinical, college, and/or community); (9) sample diagnoses (when clinical); (10) emotion regulation type(s); (11) emotion regulation measure(s); (12) mean, standard deviation, and range of emotion regulation variable(s); (13) substance type(s); (14) substance measure(s); (15) mean, standard deviation, and range of substance use variable(s); and (16) effect size(s).
Emotion Regulation Types
Consistent with Tull and Aldao (2015a), coding of emotion regulation distinguished between abilities and strategies (see Supplemental Table 1). Overall emotion regulation abilities and three aspects of emotion regulation abilities – i.e., non-acceptance of emotions (non-acceptance), inability to engage in goal-directed behaviors when experiencing emotions (goals), and difficulties controlling impulsive behaviors when experiencing emotions (impulse) – were coded in relation to both negative and positive emotions. Another aspect of emotion regulation abilities was only coded for negative emotions: limited access to emotion regulation strategies perceived as effective (strategies). Finally, two aspects of emotion regulation abilities that were coded did not specify emotion valence: lack of emotional awareness (awareness) and lack of emotional clarity (clarity). For emotion regulation strategies, maladaptive and adaptive tactics broadly were coded. Further, one maladaptive tactic (suppression; attempts to hide, inhibit or reduce ongoing emotion-expressive behavior) and one adaptive tactic (reappraisal; attempts to reinterpret an emotion-eliciting situation to alter its meaning) were coded. Papers that examined constructs that were similar to emotion regulation, but fell outside of this conceptualization of emotion regulation (e.g., mindfulness, distress tolerance, anxiety sensitivity), were excluded.
Substance Use
Four types of substance use were coded (see Supplemental Table 2): alcohol use only, drug use only, tobacco use only, and use of multiple substances (e.g., alcohol and drugs). Papers that examined other substance use constructs (e.g., coping, motives, expectancies) were excluded.
Analytic Plan
Descriptive analyses and frequencies were conducted using SPSS Version 26.0.0.1. All other analyses were conducted using the metaphor package in RStudio Version 1.2.1335. Random effects models were employed to account for both within- and between-study error, providing conservative estimates of effects (Field, 2003; Lipsey & Wilson, 2001). Analyses were conducted separately for each emotion regulation construct to ensure independence of effect sizes by not including multiple effects from any given study. In order to determine the amount of heterogeneity among studies (i.e., how much variability in the models was not accounted for by sampling error), Q statistics were examined for each observed association between emotion regulation and substance use to determine how much variability in the models was not accounted for by sampling error (Hedges & Olkin, 1985). Consistent with Cohen’s (1988) guidelines regarding r-type effect sizes, effects around 0.10 were considered small, 0.25 were considered medium, and 0.40 were considered large. According to Hedges and Vevea (1998), using less than five effect sizes might result in random-effect tests that can only be regarded as approximate. However, for many combinations of emotion regulation and substance use, less than five effect sizes were found in the literature, thus, we ran these models with two, three, and four effect sizes. We suggest caution in the interpretation of these effect sizes.
Following examination of the random effects models, we used meta-regression to examine the ability of potential moderators, including mean age, sex (i.e., % female), race (i.e., % White), and sample type (i.e., clinical adults vs. college students, clinical adults vs. community members, and clinical adults seeking treatment for a substance use disorder vs. adults without a substance use disorder), to predict the effect size magnitude for each aspect of emotion regulation and overall substance use (collapsed across substance use types to accommodate the number of analyses while maintaining adequate power).
Lastly, to examine the potential for publication bias in the present study, we used several methods. First, we created a funnel plot and ran follow-up regression and rank correlation tests for funnel plot asymmetry. Second, we computed Rosenthal’s (1979) fail-safe N-test for each significant relationship to estimate the number of studies with null findings that would cause the effect sizes found in a meta-analysis to drop to nonsignificant levels (Lipsey & Wilson, 2001).
Results
Study Sample
Sample demographics and study characteristics are summarized in Table 1. The final sample included 156,025 participants represented across 95 studies. Sample sizes ranged from 27 (Axelrod et al., 2011) to 2,080 (Bakhshaie et al., 2019), and the mean sample size was 350.62 (SD = 326.75). The weighted mean age of the sample was 29.31 (SD = 8.59) and participants ranged in age from 18 to 80. Of the 156,025 total participants, 76.6% were non-clinical adults (43.7% [n = 68,251] college students; 32.9% [n = 51,289] community members), 17.3% were clinical adults (14.8% [n = 23,020] substance use treatment seeking; 2.5% [n = 13,465] other treatment seeking), and the remaining 6.1% were mixed samples. The majority of the samples were comprised of mostly female (59.5%) and White (66.1%) adults.
Table 1.
Sample Demographics and Study Characteristics.
| Citation | Sample Characteristics | ER Aspect/Measure | Substance Type/Measure | ||
|---|---|---|---|---|---|
| Aase et al. (2018) | 71 post-9/11 U.S. military veterans seeking treatment at a VA hospital (Mage= 33.1, 16.9% Female, 63.7% White) | REAP, SUPP | ERQ | Alcohol | AUDIT |
| Adams et al. (2012) | 125 smokers in residential substance abuse treatment (Mage= 35.0, 40.3% Female, 26.8% White) | NER, NNA | DERS | Tobacco | Cigarettes smoked in past hour |
| Axelrod et al, (2011) | 27 adults with DSM-IV borderline personality disorder and substance dependence seeking treatment at a primary substance use clinic (Mage= 38.0, 100.0% Female, 92.0% White) | NER | DERS | Substances | Items assessing past month substance use frequency |
| Bakhshaie et al. (2019) | 2,080 college students (Mage= 21.9, 78.7% Female, 22.7% White) | NER | DERS | Alcohol, Drugs | PDUQ, CADS |
| Berking et al. (2011) | 232 inpatients with ICD-10 alcohol dependence (Mage= 43.1, 14.2% Female) | NNA, NS, CL, AW | ERSQ | Alcohol | Items assessing average grams of alcohol per day |
| Blanchard et al. (2019) | 643 college students (64.0% Female, 67.0% White) | REAP, SUPP | ERQ | Alcohol, Drugs | Items assessing frequency of past two-week binge drinking episodes, past-month cannabis use, and AUD/CUD criteria |
| Boden et al. (2013) | 153 medical cannabis users seeking treatment for physical or mental health conditions (Mage= 42.7, 21.6% Female, 68.7% White) | REAP, CL | ERQ, CL | Drugs | CUDIT-R |
| Brem et al. (2019) | 578 college students (Mage= 19.0, 85.1% Female, 84.5% White) | NER | DERS | Alcohol | AUDIT |
| Buckholdt et al. (2015) | 82 patients in a residential substance abuse treatment facility (Mage= 36.6, 48.0% Female, 54.0% White) | NER, NNA, NG, NI, NS, CL, AW | DERS | Substances | DUQ |
| Carr (2020) | 427 community adults (Mage= 37.3, 60.7% Female, 62.8% White) | NER, NNA, NG, NI, NS, CL, AW | DERS | Alcohol, Drugs, Substances | RAD |
| Castaños-Cervantes & Domíngu (2020) | 104 college students (Mage= 19.7, 64.4% Female) | NER | DERS | Alcohol | CAGE |
| Cavicchioli et al. (2019)a | 193 treatment-seeking adults with DSM-IV-TR AUD (Mage= 46.8, 40.4% Female) | NER | DERS | Drugs, Substances | Unstructured Clinical Interview based on DSM-IV-TR |
| Cavicchioli et al. (2019)b | 244 treatment-seeking adults with DSM-IV-TR AUD (Mage= 47.1, 38.9% Female) | NER | DERS | Alcohol, Drugs | SPQ |
| Cavicchioli et al. (2019)c | 108 treatment-seeking adults with DSM-5 AUD (Mage= 48.4, 40.7% Female) | NER | DERS | Alcohol, Drugs | SPQ |
| Chandley et al. (2014) | 223 college students (Mage= 20.4, 100.0% Female, 93.2% White) | NER | DERS | Alcohol | DDQ-R RAPI |
| Chavarria et al. (2020) | 508 community adults (Mage= 33.7, 59.6 % Female, 81.1% White) | NER, NNA, NG, NI, NS, CL, AW | DERS | Alcohol | Items assessing frequency and quantity in the past year |
| Clarke et al. (2020) | 179 adults enrolled in SUD treatment (Mage= 40.0, 42.5% White) | NER, REAP, SUPP | DERS, ERQ | Substances | Number of relapse days since beginning of treatment |
| Claudat et al. (2020)a | 98 partial hospital patients with an ED or comorbid ED-SUD (Mage= 24.6, 86.7% Female, 82.7% White) | NER, NNA, NG, NI, NS, CL, AW | DERS | Substances | SCID-5 |
| Collado et al. (2020) | 241 community adults (Mage= 50.6, 49.8% Female, 20.3% White) | NER | DERS | Substances | DUDIT-11 |
| Dragan (2015) | 502 community adults (Mage= 21.8, 100% Female) | NER, NNA, NG, NI, NS, CL, AW | DERS | Alcohol | AUDIT |
| Dutcher et al. (2017) | 111 psychiatric inpatients with DSM-5 trauma (Mage= 33.5, 45.0% Female, 45.0% White) | NER | DERS | Alcohol, Drugs | ASI-SR |
| Dvorak et al. (2014) | 1,758 college students (Mage= 20.5, 59.7% Female, 90.6% White) | NER, NNA, NG, NI, NS, CL, AW | DERS | Alcohol | DDQ-M, YAACQ |
| Espeleta et al. (2018) | 668 college students (Mage= 20.0, 83.0% Female, 76.3% White) | NER | DERS | Alcohol | BYAACQ |
| Fairholme et al. (2012) | 220 adults in a residential substance abuse treatment facility with probable PTSD (Mage= 33.7, 47.7% Female, 77.7% White) | NER | DERS | Alcohol | ADS |
| Fillo et al. (2019) | 73 pregnant smokers (Mage= 24.8, 100% Female, 30.1% White) | NER | DERS | Tobacco | FTND, Items assessing frequency and quantity in past 6 months |
| Fitzpatrick et al. (2019) | 962 community adults (Mage= 20.0, 100% Female, 67.8% White) | NER | DERS | Alcohol | YAACQ |
| Forkus et al. (2020) | 515 community adults (Mage= 37.5, 28.7% Female, 70.5% White) | NER, NNA, NG, NI, NS, CL, AW, PER, PNA, PG, PI | DERS, DERS-P | Alcohol | AUDIT |
| Fucito et al. (2010) | 121 community adults (Mage= 33.8, 49.6% Female, 45.0% White) | REAP, SUPP | ERQ | Tobacco | SHQ |
| Garey et al. (2015) | 94 adults seeking treatment for HIV/AIDS (Mage= 48.6, 11.7% Female, 42.6% White) | NER | DERS | Alcohol | AUDIT |
| Garofalo & Velotti (2015) | 437 psychiatric inpatients and healthy controls (Mage= 41.1, 40.7% Female) | NER | DERS | Alcohol | MCMI-III |
| Goldstein et al. (2017) | 437 adults seeking treatment for physical health concerns (Mage= 39.8, 100% Female, 1.1% White) | NER, NNA, NG, NI, NS, CL, AW | DERS | Alcohol | MINI |
| Goldstein et al. (2019) | 203 community adults (Mage= 21.2, 64.7% Female, 50.0% White) | NER | DERS | Alcohol | YAACQ, Items assessing standard drinks per day |
| Goncharenko et al. (2019) | 475 community adults (Mage= 35.6, 55.4% Female, 77.0% White) | NER, PER | DERS, DERS-P | Alcohol | AUDIT |
| Gonzalez et al. (2008) | 189 community adults (Mage= 25.0, 46.0% Female, 96.0% White) | NER | DERS | Alcohol, Drugs, Tobacco | FTQ, AUDIT, MSHQ |
| Gonzalez et al. (2009) | 174 community adults (Mage= 25.3, 46.0% Female, 95.0% White) | NER | DERS | Alcohol, Drugs, Tobacco | FTQ, AUDIT, MSHQ |
| Grigorian et al. (2019a) | 71 adults arrested for domestic violence and court-referred to a Batterer Intervention Program (Mage= 30.4, 100% Female, 73.2% White) | NER | DERS | Alcohol, Drugs | AUDIT, DUDIT-14 |
| Grigorian et al. (2019b) | 391 adults arrested for domestic violence and court-referred to a Batterer Intervention Program (Mage= 33.4, 60.4% White) | NER | DERS | Alcohol | AUDIT |
| Han (2010) | 381 college students (Mage= 25.3, 58.0% Female, 67.2% White) | NNA, NG, NI, NS, CL, AW | DERS | Alcohol | DSQ |
| Hartmann & McLeish (2020) | 378 college students (Mage= 19.9, 72.6% Female, 86.0% White) | NNA, NG, NI, NS, CL, AW | DERS | Alcohol | AUDIT |
| Hasking & Claes (2019) | 951 college students (Mage= 21.9, 79.4 % Female) | NER | DERS | Alcohol | AUDIT |
| Hasking et al. (2020) | 733 college students (Mage= 21.5, 76.6% Female) | NER | DERS | Alcohol | AUDIT |
| Heads et al. (2020) | 266 college students (Mage= 19.9, 71.8% Female, 0% White) | REAP, SUPP | ERQ | Alcohol, Drugs | AUDIT, YRBSS |
| Hebard (2015) | 189 college students (Mage= 19.7, 73.0% Female, 71.4% White) | NER | DERS | Alcohol | AUDIT-C, BYAACQ |
| Horvath et al. (2020) | 417 college students (Mage= 19.3, 51.8% Female, 87.0% White) | NER | DERS | Alcohol | AUDIT |
| Jakubczyk et al. (2020) | 165 adults with DSM-5 AUD (Mage= 44.0) | NER, NNA, NG, NI, NS, CL, AW | DERS | Alcohol | MINI |
| Jauregui et al. (2016) | 167 pathological gamblers (Mage= 37.0, 0% Female) | NER, NNA, NG, NI, NS, CL, AW | DERS | Alcohol, Drugs | MULTICAGE CAD-4 |
| Johnson et al. (2008) | 202 community adults (Mage= 23.8, 44.6% Female, 96.0% White) | NER | DERS | Tobacco, Alcohol, Drugs | FTQ, AUDIT, MSHQ |
| Khosravani et al. (2018) | 205 adults seeking treatment for alcohol dependence (Mage= 33.4, 24.9% Female) | REAP, SUPP | ERQ | Alcohol | AUDIT |
| Khosravani et al. (2019) | 329 adults seeking treatment for a principal diagnosis of alcohol dependence (Mage= 33.5, 0% Female) | AS, MS | CERQ-S | Alcohol | ADS, OCDS |
| Kim & Kwon (2020) | 647 college students (Mage= 20.9, 68.8% Female, 0% White) | REAP, SUPP | ERQ | Alcohol | AUDIT |
| Kirwan et al. (2019) | 101 college students (Mage= 21.0, 0% Female, 78.2% White) | NER | DERS | Alcohol | Items assessing frequency in the past year |
| Klanecky et al. (2015) | 200 college students (Mage= 19.5, 62.0% Female, 72.2% White) | NER | DERS | Alcohol | AUDIT |
| Liese et al. (2020) | 712 college students (68% Female) | NER, NNA, NG, NI, NS, CL, AW | DERS | Alcohol | Items assessing AUD criteria |
| Lilly & London (2015) | 205 community adults with interpersonal trauma (Mage= 31.5, 100% Female, 44.4% White) | NER | DERS | Alcohol | MAST |
| Lutz et al. (2019) | 205 adults seeking treatment for chronic pain (Mage= 54.0, 59.0% Female) | NER | DERS | Drugs | SOAPP-R |
| Mandavia et al. (2016) | 2,014 adults seeking treatment for physical health concerns (Mage= 39.8, 71.9% Female, 6.1% White) | NER | EDS | Alcohol | AUDIT |
| Manning et al. (2019) | 525 community adults (Mage= 35.3, 51.8% Female) | NER | DERS | Tobacco | EC-SHQ |
| Messman-Moore & Ward (2014) | 424 community adults (Mage= 19.8, 100% Female, 81.9% White) | NNA, NG, NI, NS | DERS | Alcohol | AUDIT-C |
| Miller & Racine (2020) | 238 college students (Mage= 19.4, 69.0% Female, 89.9% White) | NNA, NG, NI, NS, CL, AW | DERS | Alcohol, Drugs | AUDIT, CARE-R |
| Nauser et al. (2020) | 212 adults seeking treatment for chronic pain (Mage= 53.6, 52.8% Female) | NER | DERS | Drugs | SOAPP-R |
| Nikamanesh et al. (2015) | 452 college students | NER | DERS | Substances | DAI |
| Orr et al. (2019) | 431 community adults (Mage= 39.0, 74.6% Female, 77.8% White) | NER | DERS | Drugs | Alcohol, Smoking, and Substance Involvement Screening Test |
| Oshri et al. (2015) | 361 college students (Mage= 19.1, 62.3% Female, 87.3% White) | NNA, NG, NI, NS, CL, AW | DERS | Alcohol, Substances | CAB |
| Paulus et al. (2019)a | 94 adults seeking treatment for primary health care concerns (Mage= 38.5, 86.6% Female) | NER | DERS | Alcohol | AUDIT |
| Paulus et al. (2016)a | 126 adults seeking treatment for HIV/AIDS (Mage= 48.3, 34.1% Female, 28.6% White) | NER | DERS | Alcohol | AUDIT, TLBF, Item assessing for heavy episodic drinking |
| Paulus et al. (2016)b | 119 psychiatric inpatients (Mage= 33.2, 43.7% Female, 46.2% White) | NER | DERS | Drugs, Tobacco, Alcohol | ASI-SR |
| Paulus et al. (2017) | 264 adults seeking treatment for primary health care concerns (Mage= 38.7, 86.4% Female) | NER | DERS | Alcohol | AUDIT |
| Paulus et al. (2018) | 145 community adults (Mage= 38.4, 31.0 % Female, 23.4% White) | NER | DERS | Alcohol, Drugs | AUDIT, MPS, CUPIT, CUD-CSR |
| Paulus et al. (2019)b | 238 community adults (Mage= 38.0, 88.7% Female, 0% White) | NNA, NG, NI, NS, CL, AW | DERS | Alcohol | AUDIT |
| Preonas (2018) | 480 college students (Mage= 20.4, 65.4% Female, 40.4% White) | NER | DERS | Alcohol | DDQ, YAACQ |
| Radomski & Read (2014) | 466 college students (Mage= 19.5, 53.0% Female, 72.0% White) | NER, NNA, NG, NI, NS, CL, AW | DERS | Alcohol | Items assessing past six-month alcohol use |
| Reffi et al. (2019) | 306 college students (Mage= 19.3, 100% Female, 58.8% White) | NER | DERS | Drugs | NIDA Quick Screer |
| Rellini et al. (2010) | 43 community adults (Mage= 20.2, 39.5% Female, 93.0% White) | NER | DERS | Tobacco | SHQ |
| Richmond et al. (2020) | 194 patients with alcohol and/or cocaine dependence in residential substance abuse treatment (Mage= 34.2, 49.5% Female, 59.3% White) | NER | DERS | Drugs | DUQ |
| Rivera-Perez (2018) | 144 community adults (Mage= 47.1, 0% Female, 72.9% White) | NER | DERS | Alcohol, Drugs | MAST, DAST |
| Rodgers et al. (2017) | 305 community adults (Mage= 28.7, 38.4% Female, 83.9% White) | NER | DERS | Alcohol, Drugs | SMAST, DAST |
| Roeser et al. (2019) | 437 college students (Mage= 19.7, 64.2% Female, 50.2% White) | NER | DERS | Alcohol, Drugs | CARE-R |
| Rogers et al. (2018) | 469 treatment-seeking smokers (Mage= 36.6, 48.2% Female, 85.3% White) | NER, NNA, NG, NI, NS, CL, AW | DERS | Tobacco, Alcohol | FTCD, SHQ, AUDIT |
| Rogers et al. (2020) | 431 community adults (Mage= 38.3, 74.0% Female, 72.6% White) | NER | DERS | Drugs | COMM, SDS |
| Schatz (2014) | 117 adults enrolled in substance abuse treatment (52.1% White) | NER, NNA, NG, NI, NS, CL, AW | DERS | Substances | CAGE, MAST |
| Schick et al. (2020) | 373 community adults (Mage= 35.7, 57.1% Female, 75.9% White) | PER | DERS-P | Alcohol, Drugs | AUDIT-C, DAST |
| Schick et al. (2019) | 395 community adults (Mage= 35.6, 56.2% Female, 76.7% White) | PER, PNA, PG, PI | DERS-P | Alcohol | AUDIT-C |
| Stappenbeck et al. (2015) | 158 college students (Mage= 20.2, 42.0% White) | NNA, NG, NI, NS, CL, AW | DERS | Alcohol | Recommended Alcohol Questions from the NIAAA |
| Traylor (2013) | 102 college students (78.4% Female, 78.4% White) | REAP, SUPP | ERQ | Alcohol | AUDIT |
| Vilhena-Churchill & Goldstein (2014) | 125 community adults (Mage= 22.5, 66.9% Female) | NER | DERS | Drugs | MPS, Items assessing marijuana use frequency in past 3 months |
| Watkins et al. (2015) | 490 community adults (Mage= 21.7, 100% Female, 61.0% White) | NI | DERS | Alcohol | AUDIT |
| Weiss et al. (2019)a | 229 college students (Mage= 19.4, 66.8% Female, 67.2% White) | NER, PER, PNA, PG, PI | DERS, DERS-P | Alcohol, Drugs | AUDIT, DAST |
| Weiss et al. (2019)b | 353 community adults (Mage= 35.8, 57.8% Female, 71.2% White) | NER, PER, PNA, PG, PI | DERS, DERS-P | Alcohol, Drugs | AUDIT, DAST |
| Weiss et al. (2019)c | 463 community adults (Mage= 35.7, 55.7% Female, 76.6% White) | PER | DERS-P | Alcohol, Drugs | AUDIT, DAST |
| Weiss et al. (2020)a | 298 community adults (Mage= 36.5, 100% Female, 31.5% White) | PER, PNA, PG, PI | DERS-P | Alcohol, Drugs | AUDIT, DAST |
| Weiss et al. (2020)b | 373 community adults (Mage= 35.7, 57.1% Female, 75.9% White) | NER, PER | DERS, DERS-P | Alcohol, Drugs | AUDIT, DAST |
| Williams & Hasking (2010) | 289 community adults (Mage= 22.5, 73.0% Female) | REAP, SUPP | ERQ | Alcohol | AUDIT |
| Wolff et al. (2016) | 159 adults with or without childhood trauma and alcohol or dependence (Mage= 37.9, 47.2% Female) | NNA, NG, NI, NS, CL | DERS | Substances | SCID-IV |
| Wong et al. (2019) | 98 adults seeking treatment for HIV/AIDS (Mage= 48.4, 39.8% Female, 33.7% White) | NER | DERS | Alcohol | AUDIT |
| Zareban et al. (2017) | 286 adults with or without drug dependence (Mage= 28.2, 38.1% Female) | NNA, NG, NI, NS, CL, AW | DERS | Alcohol | Items assessing alcohol use in the past 4 months |
| Zvolensky et al. (2019) | 363 community adults (Mage= 33.3, 58.7% Female, 0% White) | NER | DERS | Alcohol, Drugs, Tobacco | AUDIT, Drug Abuse/Dependence Screener, FTCD |
Note. ADS = Alcohol Dependence Scale. AS = Adaptive Strategies. ASI-SR = Addition Severity Index Self-Report. AUD = Alcohol Use Disorder. AUDIT = Alcohol Use Disorder Identification Test. AUDIT-C = Alcohol Use Disorder Identification Test – Consumption. AW = Awareness. BYAACQ = Brief Young Adult Alcohol Consequences Questionnaire. CAB = Crime and Analogous Behavior. CADS = Core Alcohol and Drug Survey. CARE-R = Cognitive Appraisal of Risky Activities – Revised. CERQ-S = Cognitive Emotion Regulation Questionnaire - Short. CL = Clarity. COMM = Current Opioid Misuse Measure. CUD = Cannabis Use Disorder. CUD-CSR = Cannabis Use Disorder – Clinician Severity Rating. CUDIT-R = Cannabis Use Disorders Identification Test – Revised. CUPIT = Cannabis Use Problems Identification Test. DAST = Drug Abuse Screening Test. DDQ = Daily Drinking Questionnaire. DERS = Difficulties in Emotion Regulation Scale. DSQ = Drinking Style Questionnaire. DUDIT = Drug Use Disorders Identification Test. DUQ = Drug Use Questionnaire. EC-SHQ = Electronic Cigarette Smoking History Questionnaire. ED = eating disorder. ERSQ = Emotion Regulation Skills Questionnaire. FTCD = Fagerström Test for Cigarette Dependence. FTND = Fagerström Test for Nicotine Dependence. MAST = Michigan Alcohol Screening Test. MINI = Mini-International Neuropsychiatric Interview. MS = Maladaptive Strategies. MPS = Marijuana Problems Scale. MSHQ = Marijuana Smoking History Questionnaire. NER = Negative Emotion Regulation. NG = Negative Goals. NI = Negative Impulse. NIAAA = National Institute on Alcohol Abuse and Alcoholism. NIDA = National Institute of Drug Abuse. NNA = Negative Non-Accept. NS = Negative Strategies. OCDS = Obsessive Compulsive Drinking Scale. PER = Positive Emotion Regulation. PG = Positive Goals. PI = Positive Impulse. PNA = Positive Non-Accept. RAD = Recognizing Addictive Disorders. RAPI = Rutgers Alcohol Problem Index. REAP = Reappraisal. SCID = Structured Clinical Interview for DSM. SDS = Severity of Dependence Scale. SOAPP-R = Screener and Opioid Assessment for Patients with Pain – Revised. SPQ = Shorter PROMIS Questionnaire. SUD = substance use disorder. SUPP = Suppression. TLFB = Timeline Follow Back. YAACQ = Young Adult Alcohol Consequences Questionnaire. YRBSS = Youth Risk Behavior Surveillance Survey.
Meta-Analytic Findings
Table 2 presents the mean effect sizes, confidence intervals, z-test, standard error, number of studies, total sample size, Q-test, and fail-safe N results for associations between aspects emotion regulation and types of substance use.
Table 2.
Mean Effect Sizes and Q-test of Homogeneity for Each Association.
| ER Construct | Substance | K | N | ES | 95 % CI | z | p | SE | Q(df) | Fail-safe N |
|---|---|---|---|---|---|---|---|---|---|---|
| All | All | 445 | 156,025 | 0.19 | 0.17 to 0.20 | 22.51 | <.001 | 0.01 | 4,148 (444)c | 743,765 |
| Negative Overall | Alcohol | 79 | 26,025 | 0.23 | 0.19 to 0.26 | 12.39 | <.001 | 0.02 | 644.95 (78)c | 30,647 |
| Drugs | 38 | 12,456 | 0.27 | 0.19 to 0.35 | 6.82 | <.001 | 0.04 | 640.67 (37)c | 9,622 | |
| Tobacco | 14 | 3,324 | 0.19 | 0.11 to 0.28 | 4.45 | <.001 | 0.04 | 74.61 (13)c | 533 | |
| Substances | 9 | 1,816 | 0.25 | 0.15 to 0.35 | 4.99 | <.001 | 0.05 | 41.39 (8)c | 331 | |
| Negative Non-Accept | Alcohol | 26 | 11,460 | 0.14 | 0.09 to 0.18 | 6.41 | <.001 | 0.02 | 118.21 (25)c | 1,725 |
| Drugs | 5 | 1,140 | 0.15 | 0.04 to 0.26 | 2.68 | .01 | 0.06 | 12.89 (4)a | 41 | |
| Tobacco | 4 | 1,490 | 0.24 | 0.10 to 0.29 | 3.27 | .001 | 0.07 | 20.63 (3)c | 106 | |
| Substances | 7 | 1,530 | 0.28 | 0.16 to 0.40 | 4.68 | <.001 | 0.06 | 31.05 (6)c | 278 | |
| Negative Goals | Alcohol | 25 | 11,228 | 0.15 | 0.11 to 0.20 | 6.29 | <.001 | 0.02 | 140.90 (24)c | 1,995 |
| Drugs | 5 | 1,140 | 0.16 | 0.10 to 0.21 | 5.21 | <.001 | 0.03 | 4.07 (4) | 41 | |
| Tobacco | 3 | 1,365 | 0.13 | −0.06 to 0.33 | 1.35 | .177 | 0.10 | 27.06 (2)c | 0 | |
| Substances | 7 | 1,530 | 0.25 | 0.15 to 0.35 | 4.83 | <.001 | 0.05 | 22.71 (6)c | 206 | |
| Negative Impulse | Alcohol | 28 | 11,747 | 0.19 | 0.14 to 0.24 | 7.46 | <.001 | 0.03 | 171.26 (27)c | 3,835 |
| Drugs | 4 | 866 | 0.26 | 0.11 to 0.41 | 3.33 | <.001 | 0.08 | 14.60 (3)b | 76 | |
| Tobacco | 3 | 1,365 | 0.21 | 0.04 to 0.37 | 2.40 | .02 | 0.09 | 19.81 (2)c | 61 | |
| Substances | 7 | 1,530 | 0.38 | 0.25 to 0.50 | 5.88 | <.001 | 0.06 | 31.38 (6)c | 524 | |
| Negative Strategies | Alcohol | 25 | 11,186 | 0.18 | 0.13 to 0.23 | 6.93 | <.001 | 0.03 | 148.87 (24)c | 2,673 |
| Drugs | 4 | 866 | 0.18 | 0.03 to 0.34 | 2.27 | .02 | 0.08 | 12.37 (3)b | 35 | |
| Tobacco | 3 | 1,365 | 0.22 | 0.03 to 0.41 | 2.24 | .03 | 0.10 | 26.25 (2)c | 69 | |
| Substances | 7 | 1,530 | 0.41 | 0.22 to 0.59 | 4.33 | <.001 | 0.09 | 82.79 (6)c | 621 | |
| Clarity | Alcohol | 25 | 11,036 | 0.18 | 0.12 to 0.23 | 5.83 | <.001 | 0.03 | 191.27 (24)c | 2,651 |
| Drugs | 6 | 1,293 | 0.12 | −0.01 to 0.25 | 1.85 | .06 | 0.07 | 21.06 (5)c | 0 | |
| Tobacco | 3 | 1,365 | 0.12 | 0.03 to 0.22 | 2.60 | .01 | 0.05 | 6.18 (2)a | 21 | |
| Substances | 7 | 1,530 | 0.17 | −0.01 to 0.36 | 1.89 | .06 | 0.09 | 52.87 (6)c | 0 | |
| Awareness | Alcohol | 19 | 9,142 | 0.09 | 0.07 to 0.11 | 8.83 | <.001 | 0.01 | 30.84 (18)a | 471 |
| Drugs | 4 | 713 | 0.07 | −0.01 to 0.14 | 1.72 | .08 | 0.04 | 1.19 (3) | 0 | |
| Tobacco | 2 | 938 | 0.08 | 0.01 to 0.14 | 2.33 | .02 | 0.03 | 0.91 (1) | 3 | |
| Substances | 5 | 944 | 0.10 | 0.04 to 0.17 | 3.17 | .002 | 0.03 | 3.67 (4) | 13 | |
| Positive Overall | Alcohol | 8 | 3,079 | 0.24 | 0.15 to 0.32 | 5.47 | <.001 | 0.04 | 45.45 (7)c | 533 |
| Drugs | 6 | 2,089 | 0.28 | 0.23 to 0.33 | 10.64 | <.001 | 0.03 | 7.42 (5) | 356 | |
| Tobacco | - | - | - | - | - | - | - | - | - | |
| Substances | - | - | - | - | - | - | - | - | - | |
| Positive Non-Accept | Alcohol | 5 | 1,790 | 0.20 | 0.04 to 0.36 | 2.45 | .01 | 0.08 | 48.46 (4)c | 148 |
| Drugs | 3 | 880 | 0.19 | 0.01 to 0.37 | 2.06 | .04 | 0.09 | 15.67 (2)c | 34 | |
| Tobacco | - | - | - | - | - | - | - | - | - | |
| Substances | - | - | - | - | - | - | - | - | - | |
| Positive Goals | Alcohol | 5 | 1,790 | 0.24 | 0.10 to 0.38 | 3.35 | <.001 | 0.07 | 43.52 (4)c | 195 |
| Drugs | 3 | 880 | 0.24 | 0.17 to 0.30 | 6.99 | <.001 | 0.03 | 0.27 (2) | 52 | |
| Tobacco | - | - | - | - | - | - | - | - | - | |
| Substances | - | - | - | - | - | - | - | - | - | |
| Positive Impulse | Alcohol | 5 | 1,790 | 0.25 | 0.11 to 0.39 | 3.60 | <.001 | 0.07 | 38.03 (4)c | 222 |
| Drugs | 3 | 880 | 0.23 | 0.10 to 0.36 | 3.53 | <.001 | 0.07 | 7.92 (2)a | 51 | |
| Tobacco | - | - | - | - | - | - | - | - | - | |
| Substances | - | - | - | - | - | - | - | - | - | |
| Adaptive Strategies | Alcohol | 12 | 3,801 | −0.20 | −0.27 to −0.13 | −5.52 | <.001 | 0.04 | 46.38 (11)c | 603 |
| Drugs | 3 | 1,439 | −0.04 | −0.12 to 0.02 | −1.32 | .19 | 0.03 | 3.10 (2) | 0 | |
| Tobacco | - | - | - | - | - | - | - | - | - | |
| Substances | - | - | - | - | - | - | - | - | - | |
| Reappraisal | Alcohol | 8 | 2,485 | −0.17 | −0.27 to −0.06 | −3.16 | .002 | 0.05 | 33.38 (7)c | 159 |
| Drugs | 3 | 1,439 | −0.04 | −0.11 to 0.02 | −1.32 | .19 | 0.03 | 3.10 (2) | 0 | |
| Tobacco | - | - | - | - | - | - | - | - | - | |
| Substances | - | - | - | - | - | - | - | - | - | |
| Maladaptive Strategies | Alcohol | 12 | 3,801 | 0.18 | 0.06 to 0.30 | 3.01 | .003 | 0.06 | 160.76 (11)c | 442 |
| Drugs | 2 | 1,286 | −0.01 | −0.09 to 0.07 | −0.25 | .80 | 0.04 | 2.05 (1) | 0 | |
| Tobacco | - | - | - | - | - | - | - | - | - | |
| Substances | ||||||||||
| Suppression | Alcohol | 8 | 2,485 | 0.07 | −0.04 to 0.18 | 1.18 | .24 | 0.06 | 44.31 (7)c | 0 |
| Drugs | 2 | 1,286 | −0.01 | −0.09 to 0.07 | −0.25 | .80 | 0.04 | 2.05 (1) | 0 | |
| Tobacco | - | - | - | - | - | - | - | - | - | |
| Substances | - | - | - | - | - | - | - | - | - |
Note. - denotes that fewer than two studies examined this association and thus no statistics could be calculated.
p < .05;
p < .01;
p < .001
Emotion Regulation and Substance Use.
The effect size for the relation between all aspects of emotion regulation and all substance use was significant and small-to-medium, r = 0.19 (SE = 0.01; 95% CI [0.17, 0.20], based on 445 effect sizes from 95 studies). This effect size was significantly different from zero (z = 22.51, p < .001) and varied significantly across effects (Q = 4,148, df = 444, p < .001). Rosenthal’s (1979) fail-safe N-test for the overall emotion regulation and substance use association revealed that it would take 743,765 studies with null effects to reduce this effect to a nonsignificant level.
Emotion Regulation Abilities and Substance Use.
The effect sizes for the relations between overall negative emotion regulation abilities and each type of substance use were significant and ranged from small-to-medium to medium for alcohol use (r = 0.23, p < .001), drug use (r = 0.27, p < .001), tobacco use (r = 0.19, p < .001), and use of multiple substances (r = 0.25, p < .001). The effect sizes for the relations between overall positive emotion regulation abilities and each type of substance use were significant and medium for alcohol use (r = 0.24, p < .001) and drug use (r = 0.28, p < .001).
Regarding relations between aspects of negative emotion regulation abilities and types of substance use, large effects were observed between negative strategies and use of multiple substances (r = 0.41, p < .001) and between negative impulse and use of multiple substances (r = 0.38, p < .001). Medium effects were observed for the relations between negative non-acceptance and use of multiple substances (r = 0.28, p < .001), negative impulse and drugs (r = 0.26, p < .001), negative goals and use of multiple substances (r = 0.25, p < .001), and negative non-acceptance and tobacco use (r = 0.24, p = .001). Small-to-medium to small effects were observed for the relations between negative strategies and tobacco use (r = 0.22, p = .03), negative impulse and tobacco use (r = 0.21, p = .02), negative impulse and alcohol use (r = 0.19, p < .001), negative strategies and alcohol use (r = 0.18, p < .001), negative strategies and drug use (r = 0.18, p = .02), negative goals and drug use (r = 0.16, p < .001), negative non-acceptance and drug use (r = 0.15, p = .01), negative goals and alcohol use (r = 0.15, p < .001), and negative non-acceptance and alcohol use (r = 0.14, p < .001). A small effect was also found for negative goals and tobacco, although this was nonsignificant.
In term of the relations between aspects of positive emotion regulation abilities and types of substance use, medium effects were observed between positive impulse and alcohol use (r = 0.25, p < .001), positive goals and alcohol use (r = 0.24, p < .001), positive goals and drug use (r = 0.24, p < .001), and positive impulse and drug use (r = 0.23, p < .001). Small-to-medium effects were observed for the relations between positive non-acceptance and alcohol use (r = 0.20, p = .01) and positive non-acceptance and drug use (r = 0.19, p = .04).
Finally, regarding emotion regulation abilities that did not reference emotion valence, small-to-medium to small effects were observed for the relations between clarity and alcohol use (r = 0.18, p < .001), clarity and tobacco use (r = 0.12, p = .01), awareness and use of multiple substances (r = 0.10, p = .002), awareness and alcohol use (r = 0.09, p < .001), and awareness and tobacco use (r = 0.08, p = .02). Small effects were also observed for the relations between clarity and use of multiple substances, clarity and drug use, and awareness and drug use, although these were nonsignificant.
Emotion Regulation Strategies and Substance Use.
The effect sizes for the relations between all aspects of emotion regulation strategies and alcohol use were significant and small-to-medium (r = −0.20, p < .001 for adaptive strategies and alcohol use; r = −0.17, p < .001 for cognitive reappraisal and alcohol use; r = 0.18, p = .001 for maladaptive strategies and alcohol use), with the exception of expressive suppression for which the association to alcohol use was nonsignificant. Although small effects were observed for the relations between all aspects of emotion regulation strategies and drug use, these effects were nonsignificant.
Moderation Analyses.
Age.
Analyses (see Table 3) revealed significant differences in effect sizes for relations between all aspects of emotion regulation (B = 0.01, p < .001), overall negative emotion regulation abilities (B = 0.01, p < .001), negative non-acceptance (B = 0.01, p < .001), negative goals (B = 0.01, p < .001), negative impulse (B = 0.01, p = .01), and negative strategies (B = 0.01, p = .006), and overall substance use. These relations were stronger among studies with older samples.
Table 3.
Moderating Role of Demographic Factors.
| ER Construct | K | B | 95% CI | Q(df) | p |
|---|---|---|---|---|---|
| Age | |||||
| All | 413 | 0.01 | .006 to .01 | 76.93(1) | < .001 |
| Negative Overall | 136 | 0.01 | .006 to .01 | 40.60(1) | < .001 |
| Negative Non-Accept | 39 | 0.01 | .004 to .01 | 14.10(1) | < .001 |
| Negative Goals | 35 | 0.01 | .005 to .01 | 19.80(1) | < .001 |
| Negative Impulse | 39 | 0.01 | .002 to .01 | 6.28(1) | .012 |
| Negative Strategies | 36 | 0.01 | .003 to .015 | 7.46(1) | .006 |
| Clarity | 38 | 0.004 | −.002 to .01 | 1.49(1) | .22 |
| Awareness | 27 | 0.001 | −.002 to .003 | 0.19(1) | .67 |
| Positive Overall | 14 | 0.005 | −.005 to .01 | 0.91(1) | .34 |
| Positive Non-Accept | 8 | 0.01 | −.01 to .02 | 1.20(1) | .27 |
| Positive Goals | 8 | 0.002 | −.01 to .01 | 0.08(1) | .78 |
| Positive Impulse | 8 | 0.007 | −.01 to .02 | 1.19(1) | .28 |
| Adaptive Strategies | 12 | 0.002 | −.01 to .02 | 0.05(1) | .83 |
| Maladaptive Strategies | 11 | 0.01 | −.004 to .03 | 2.23(1) | .14 |
| Reappraisal | 8 | 0.004 | −0.01 to 0.02 | 0.22(1) | .64 |
| Suppression | 7 | 0.005 | −.01 to .02 | 0.35(1) | .55 |
| Sex (% Female) | |||||
| All | 427 | −0.0002 | −.001 to .0005 | 0.27(1) | .60 |
| Negative Overall | 136 | 0.0001 | −.001 to .001 | 0.01(1) | .91 |
| Negative Non-Accept | 40 | −0.001 | −.003 to .0003 | 2.38(1) | .12 |
| Negative Goals | 38 | −0.001 | −.002 to .001 | 0.47(1) | .49 |
| Negative Impulse | 40 | −0.001 | −.002 to .001 | 0.45(1) | .50 |
| Negative Strategies | 37 | −0.002 | −.004 to .001 | 1.73(1) | .19 |
| Clarity | 39 | 0.0004 | −.001 to .002 | 0.17(1) | .68 |
| Awareness | 28 | 0.001 | .001 to .002 | 8.81(1) | .003 |
| Positive Overall | 14 | −0.004 | −.004 to −.002 | 11.95(1) | < .001 |
| Positive Non-Accept | 8 | −0.01 | −.01 to −.003 | 13.82(1) | < .001 |
| Positive Goals | 8 | −0.003 | −.01 to .001 | 2.07(1) | .15 |
| Positive Impulse | 8 | −0.004 | −.01 to −.001 | 7.72(1) | .006 |
| Adaptive Strategies | 16 | 0.002 | .001 to .004 | 6.39(1) | .01 |
| Maladaptive Strategies | 15 | −0.005 | −.01 to −.003 | 25.88(1) | < .001 |
| Reappraisal | 12 | 0.002 | −.002 to .006 | 0.72(1) | .40 |
| Suppression | 11 | −0.002 | −.01 to .002 | 0.97(1) | .33 |
| Race (% White) | |||||
| All | 353 | 0.0000 | −.001 to .001 | 0.004(1) | .95 |
| Negative Overall | 107 | −0.001 | −.002 to .001 | 1.43(1) | .23 |
| Negative Non-Accept | 33 | −0.0004 | −.002 to .001 | 0.21(1) | .65 |
| Negative Goals | 32 | −0.001 | −.002 to .001 | 1.02(1) | .31 |
| Negative Impulse | 36 | 0.001 | −.001 to .002 | 0.63(1) | .43 |
| Negative Strategies | 32 | −0.0002 | −.002 to .001 | 0.06(1) | .80 |
| Clarity | 32 | 0.001 | −.001 to .003 | 1.23(1) | .27 |
| Awareness | 22 | −0.001 | −.002 to .001 | 1.14(1) | .29 |
| Positive Overall | 14 | 0.002 | −.001 to .006 | 1.73(1) | .19 |
| Positive Non-Accept | 8 | 0.01 | −.001 to .01 | 2.94(1) | .09 |
| Positive Goals | 8 | 0.001 | −.005 to .006 | 0.04(1) | .84 |
| Positive Impulse | 8 | 0.003 | −.002 to .008 | 1.15(1) | .28 |
| Adaptive Strategies | 11 | 0.001 | −.001 to .002 | 0.74(1) | .39 |
| Maladaptive Strategies | 10 | −0.001 | −.004 to .001 | 1.22(1) | .27 |
| Reappraisal | 11 | 0.001 | −.001 to .002 | 0.74(1) | .39 |
| Suppression | 10 | −0.001 | −.004 to .001 | 1.22(1) | .27 |
Note. ER = emotion regulation.
Sex.
Analyses (see Table 3) revealed significant differences in effect sizes for the relations between overall positive emotion regulation abilities (B = −0.004, p < .001), positive non-acceptance (B = −0.01, p < .001), positive impulse (B = −0.004, p = .006), and maladaptive strategies (B = −0.005, p < .001), and overall substance use, with these relations being stronger among samples with fewer female participants. For awareness (B = 0.001, p = .003) and adaptive strategies (B = 0.002, p = .01), analyses revealed significant differences in effect sizes, with relations to overall substance use being stronger in studies with more female participants.
Race.
Analyses (see Table 3) revealed no significant differences in effect sizes for the relations between any aspect of emotion regulation and overall substance use.
Sample Type.
Comparing clinical adults (majority who were in treatment for a SUD; see Table 1) vs. college students (see Table 4), analyses revealed significant differences in effect sizes for the relations between all aspects of emotion regulation (B = 0.13, p < .001), overall negative emotion regulation abilities (B = 0.17, p < .001), negative non-acceptance (B = 0.15, p < .001), negative goals (B = 0.16, p < .001), negative impulse (B = 0.15, p = .004), negative strategies (B = 0.21, p = .002), and maladaptive strategies (B = 0.28, p < .001), and overall substance use. These relations were stronger among studies comprised of clinical adults vs. college students. Comparing clinical adults vs. community members (see Table 4), analyses revealed a significant difference in effect size for the relation between overall negative emotion regulation abilities and overall substance use (B = 0.08, p = .03), with this relation being stronger among studies of clinical adults vs. community members. Comparing clinical adults seeking treatment for a substance use disorder vs. adults without a substance use disorder (majority who were in general psychiatric treatment; see Table 1), analyses revealed significant differences in effect sizes for the relations between all aspects of emotion regulation (B = 0.04, p = .03), negative non-acceptance (B = 0.12, p = .01), negative goals (B = 0.13, p = .01), negative strategies (B = 0.19, p = .002), maladaptive strategies (B = 0.31, p < .001), and expressive suppression (B = 0.20, p = .04), and overall substance use, with these relations being stronger among studies comprised of clinical adults seeking treatment for a substance use disorder vs. adults without a substance use disorder (see Table 4). There was also a significant difference in effect size for the relation of adaptive strategies to overall substance use (B = −0.17, p < .001), with this relation being stronger among studies comprised of adults without a substance use disorder vs. clinical adults seeking treatment for a substance use disorder.
Table 4.
Sample Type as a Moderator
| ER Construct | K | B | 95% CI | Q(df) | p |
|---|---|---|---|---|---|
| Clinical Adults vs. College Students | |||||
| All | 303 | 0.13 | .09 to .17 | 44.96(1) | < .001 |
| Negative Overall | 96 | 0.17 | .11 to .24 | 26.76(1) | < .001 |
| Negative Non-Accept | 30 | 0.15 | .06 to .23 | 12.26(1) | < .001 |
| Negative Goals | 28 | 0.16 | .07 to .24 | 11.84(1) | < .001 |
| Negative Impulse | 29 | 0.15 | .05 to .25 | 8.15(1) | .004 |
| Negative Strategies | 27 | 0.21 | .08 to .34 | 9.58(1) | .002 |
| Clarity | 29 | 0.05 | −.08 to .17 | 0.57(1) | .45 |
| Awareness | 27 | 0.01 | −.03 to .05 | 0.28(1) | .60 |
| Adaptive Strategies | 15 | −0.11 | −.24 to .03 | 2.33(1) | .13 |
| Maladaptive Strategies | 14 | 0.28 | .14 to .42 | 15.70(1) | < .001 |
| Reappraisal | 11 | −0.03 | −.23 to .17 | 0.10(1) | .75 |
| Suppression | 10 | 0.13 | −.06 to .32 | 1.74(1) | .19 |
| Clinical Adults vs. Community Individuals | |||||
| All | 304 | 0.02 | −.02 to .06 | 1.22(1) | .27 |
| Negative Overall | 106 | 0.08 | .01 to .15 | 4.68(1) | .03 |
| Negative Non-Accept | 28 | 0.02 | −.06 to .11 | 0.32(1) | .57 |
| Negative Goals | 26 | 0.06 | −.03 to .15 | 2.11(1) | .15 |
| Negative Impulse | 25 | 0.07 | −.06 to .20 | 1.23(1) | .27 |
| Negative Strategies | 25 | 0.10 | −.04 to .24 | 1.96(1) | .16 |
| Clarity | 28 | −0.01 | −.14 to .13 | 0.02(1) | .90 |
| Awareness | 17 | 0.03 | −.05 to .10 | 0.55(1) | .46 |
| Adaptive Strategies | 10 | −0.09 | −.37 to .19 | 0.36(1) | .55 |
| Maladaptive Strategies | 9 | 0.18 | −.10 to .45 | 1.53(1) | .22 |
| Reappraisal | 6 | −0.01 | −.42 to .40 | 0.003(1) | .96 |
| Suppression | 5 | 0.01 | −.37 to .40 | 0.01(1) | .94 |
| Clinical Adults Seeking Treatment for a Substance Use Disorder vs. Adults without a Substance Use Disorder | |||||
| All | 445 | 0.04 | .004 to .09 | 4.70(1) | .03 |
| Negative Overall | 140 | 0.02 | −.07 to .10 | 0.15(1) | .70 |
| Negative Non-Accept | 42 | 0.12 | .03 to .20 | 6.93(1) | .01 |
| Negative Goals | 40 | 0.13 | .04 to .22 | 7.45(1) | .01 |
| Negative Impulse | 42 | 0.11 | −.002 to .22 | 3.71(1) | .054 |
| Negative Strategies | 39 | 0.19 | .07 to .30 | 9.84(1) | .002 |
| Clarity | 41 | 0.04 | −.08 to .15 | 0.40(1) | .52 |
| Awareness | 30 | 0.01 | −.03 to .06 | 0.41(1) | .52 |
| Adaptive Strategies | 17 | −0.17 | −.27 to −.07 | 10.23(1) | .001 |
| Maladaptive Strategies | 16 | 0.31 | .20 to .43 | 30.45(1) | < .001 |
| Reappraisal | 13 | −0.16 | −.36 to .04 | 2.47(1) | .12 |
| Suppression | 12 | 0.20 | .01 to .39 | 4.13(1) | .04 |
Note. Positive emotion dysregulation variables are not included in this table because no clinical samples were utilized in these studies; ER = emotion regulation.
Publication Bias Findings
To examine publication bias in the current study, a funnel plot of all effect sizes plotted by the standard error was created (see Figure 2). The funnel plot was visually symmetrical, with nonsignificant regression and rank correlation tests for funnel plot asymmetry (p = .07 and p = .14, respectively). These findings indicate that publication bias is likely not present. To further investigate publication bias, Rosenthal’s (1979) fail-safe N was calculated for each significant relationship (see Table 2), revealing that for the majority of the relations between aspects of emotion regulation and types of substance use, the number of studies with null findings that would cause the effect sizes found in a meta-analysis to drop to non-significant levels was well above the cutoff values identified by Fragkos et al. (2014). Fail-safe N values for the relations between negative non-acceptance and drug use (fail-safe N = 41), negative goals and drugs (fail-safe N = 41), negative strategies and drug use (fail-safe N = 35), clarity and tobacco use (fail-safe N = 21), awareness and use of multiple substances (fail-safe N = 13), awareness and tobacco use (fail-safe N = 3), and positive non-acceptance and drug use (fail-safe N = 35) were below cutoff values. Thus, these effect sizes should be interpreted with caution.
Figure 2.
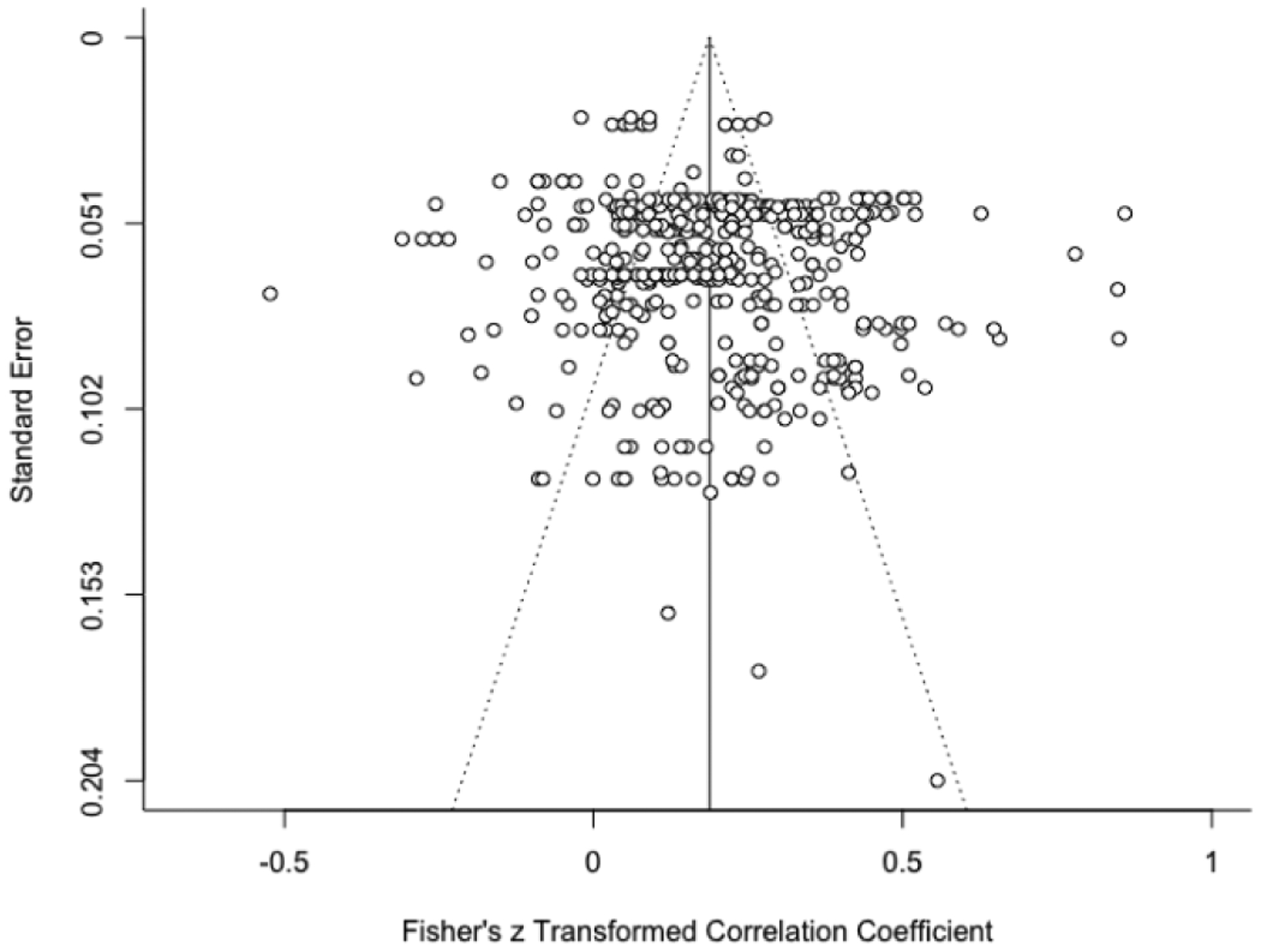
Funnel Plot Representing All Effect Sizes Plotted by Standard Error.
Discussion
In the present meta-analytic review, we evaluated associations between emotion regulation (overall and across 15 specific aspects) and substance use (overall and for alcohol use only, drug use only, tobacco use only, and use of multiple substances). A total of 461 effect sizes (N = 156,025 participants) were extracted from 95 eligible studies. Emotion regulation and substance use were significantly related (r = 0.19; p < .001); however, this effect size varied considerably across studies (from −0.01 to 0.41 for aspects of emotion regulation characterized as maladaptive and −0.20 to −0.07 for aspects of emotion regulation characterized as adaptive). Several clinically significant interpretations can be extrapolated from the findings that advance our understanding of the relation between emotion regulation and substance use.
Varying Magnitude of Effects
Aspects of emotion regulation were significantly related – and in the expected direction – to substance use with only a few exceptions. However, a key finding of this study is that there was a range in the magnitude of the effects between aspects of emotion regulation and types of substance use. Indeed, inspection of the data showed that the overall effect size for emotion regulation and substance use misrepresented this relation. To specify, the overall results for emotion regulation and substance use indicated a small-to-medium effect; however, examination of the relations between aspects of emotion regulation and types of substance use revealed a wide range of magnitudes, with some representing large effects, while others were quite small. Thus, when averaged, it was not surprising that a small-to-medium effect size was found for the overall results, as large effects for some associations were likely masked or reduced by small and/or nonsignificant effects for other relations. Overall, these findings suggest problems with aggregating across aspects of emotion regulation and types of substance use. As such, our results indicate that future research in this area would benefit from examining these factors separately versus collapsing. As one example, researchers conducting work in this area should consider using the subscales of the Difficulties in Emotion regulation Scale (Gratz & Roemer, 2004)—as opposed to the total score alone—as well as assessing distinct types of substance use (e.g., alcohol, marijuana) vs. any substance use.
Emotion Regulation Abilities versus Strategies
The size of the effects between emotion regulation abilities and substance use was generally larger than those between emotion regulation strategies and substance use. The contextually dependent nature of emotion regulation strategies may provide one explanation for this finding. Specifically, researchers have postulated that the adaptiveness of emotion regulation strategies requires consideration of the individual’s goals, as well as situational demands (Aldao, 2013; Gross, 2015); thus, studies that assess individuals’ typical strategies across contexts may have limited utility. For instance, although suppression is generally considered to be a maladaptive emotion regulation strategy (Aldao et al., 2010), it may confer benefits in certain situations (Aldao, 2013), such as when the down-regulation of emotion—resultant from suppression (Dunn et al., 2009)—aligns with an individuals’ goals or the situational demands. Moreover, the benefits of purportedly adaptive emotion regulation strategies, such as cognitive reappraisal (Aldao et al., 2010), may depend on co-occurring maladaptive emotion regulation strategies, with one study showing that individuals who used more adaptive and maladaptive emotion regulation strategies had more psychopathology than those who used adaptive emotion regulation strategies alone (Dixon-Gordon et al., 2015). These latter findings suggest that adaptive emotion regulation strategies may lose their protective value in the context of co-occurring maladaptive emotion regulation strategies, perhaps because use of multiple strategies reflects greater distress. Considering the context-dependent nature of emotion regulation strategies, our findings of nonsignificant and/or small effects for emotion regulation strategies and substance use should be interpreted with caution. It is possible that dispositional measures of emotion regulation strategies have less utility in predicting substance use. Research utilizing study designs that speak to the influence of context may be better suited to assess the association between emotion regulation and substance use. For instance, experimental or daily monitoring studies may address how emotion regulation and substance use relate to one another over time and across contexts, enhancing the ecological validity of study findings and capturing the dynamic, fluctuating nature of this association.
Behavioral versus Cognitive Aspects of Emotion Regulation Abilities
There was considerable variability in the strength of effects across aspects of emotion regulation abilities in relation to types of substance use. For example, the observed effects were generally larger for behavioral aspects of emotion regulation abilities characterized by impulsivity and access to strategies and weaker for cognitive aspects of emotion regulation abilities characterized by awareness and clarity. These findings can be understood in the context of the existing literature. Regarding the relation of emotion-driven impulsivity to substance use, there is a robust body of literature linking impulsivity—including in the context of intense emotions—to substance use (for meta-analytic reviews, see Coskunpinar et al., 2013; Kale et al., 2018; VanderVeen et al., 2016). Indeed, affect is a strong proximal trigger of substance use (for meta-analytic reviews, see Bresin et al., 2018; Serre et al., 2015) and contemporary models of substance use highlight internally-driven negative reinforcement as a prominent motivation underlying substance use (for a review, see Cooper et al., 2016). In terms of the aspect of emotion regulation abilities characterized by flexible use of strategies, individuals who perceive themselves as having limited access to effective emotion regulation strategies may be more likely to use substances to modulate emotional experiences. This is consistent with the purported emotion-regulating function of substance use (Weiss et al., 2012).
Also noteworthy were findings of weaker effects for deficits in the understanding (i.e., clarity) and recognition (i.e., awareness) of emotional experiences in relation to substance use. Individuals with these deficits may pay less attention to their emotions, which may result in fewer intense emotions, thereby reducing the likelihood that such emotions will serve as an antecedent to substance use (for meta-analytic reviews, see Bresin et al., 2018; Serre et al., 2015). However, two considerations are worthy of attention when interpreting these latter findings. Emotional clarity and awareness have been proposed to be foundational to the enactment of other aspects of emotion regulation (Vine & Aldao, 2014). As such, it is possible that deficits in these areas may be indirectly related to substance use through other aspects of emotion regulation. For example, lack of emotional clarity and awareness may exacerbate other deficits in emotion regulation abilities and skills, which, in turn, may increase substance use. Future research that speaks to potential cascading effects among aspects of emotion regulation in relation to substance use is necessary. Also, some evidence suggests that the awareness aspect of emotion regulation shows divergent relations with criterion variables (Salters-Pedneault et al., 2006; Tull et al., 2007) and does not represent a higher-order construct (Bardeen et al., 2012; Fowler et al., 2014). As such, some researchers have argued for removal of the awareness aspect (Bardeen et al., 2012; Fowler et al., 2014). Additional research is needed to examine the optimal latent structure of the construct of emotion regulation, including whether the awareness dimension represents the higher-order construct of emotion regulation.
Single versus Multiple Substance Use
The strength of associations between emotion regulation abilities and type of substance use also varied, with the largest effects being found for any substance versus alcohol use or drug use alone. These results may indicate greater emotion regulation difficulties among individuals with polysubstance use. The decision to use multiple substances may serve to attenuate the effects of each substance alone, for instance in the case of opioids and benzodiazepines (for a review, see Jones et al., 2012), and thus may be functionally tied to emotion regulation. Specifically, in the context of intense emotions, individuals with greater deficits in emotion regulation may be more motivated to use multiple substances to down-regulate emotional experiences. This suggestion aligns with research indicating that emotion regulation difficulties increase in relation to severity and frequency of substance use (Garke et al., in press). Given the high prevalence and clinically significant correlates of polysubstance use (for a review, see Connor et al., 2014), research is needed to further mechanisms underlying relations of emotion regulation to polysubstance use. For instance, individuals who exhibit deficits in emotion regulation may experience distress from a wider range of sources (e.g., psychiatric, interpersonal), and may use different substances to modulate the psychological pain associated with these unique experiences.
Regulation of Negative versus Positive Emotions
Another important interpretation is related to the distinction between negative and positive emotion regulation in relation to substance use. Specifically, findings showed medium effects for aspects of regulation of positive emotions, akin to aspects of regulation of negative emotions. Indeed, the evidence that some individuals experience positive emotions as aversive (Weiss, Gratz, et al., 2015) may explain the relation of positive emotion regulation to substance use (for a review, see Weiss, Sullivan, et al., 2015). For instance, heightened physiological responding to positive emotions (Litz et al., 2000) may elicit distress through stimulus generalization (i.e., arousal paired with negative emotions may expand to arousal paired with positive emotions; Roemer et al., 2001). Alternatively, some individuals may experience competing negative cognitions in the context of positive emotions, such as the belief that they do not deserve to experience positive emotions or that positive emotions are a sign of weakness (Lawrence & Lee, 2014). The resultant negative affect interference (Frewen et al., 2012) may lead to attempts to suppress positive emotional experiences (Beblo et al., 2013; Beblo et al., 2012; Roemer et al., 2001), including through substance use (Weiss et al., 2020; Weiss, Goncharenko, et al., in press). Notably, however, few studies reviewed here examined associations among positive emotion dysregulation and substance use. Further, all of these studies utilized non-clinical samples. Thus, while early findings are promising, additional research is needed, including with clinical populations. For instance, future investigations would benefit from examining the unique and amplifying effects of positive emotion dysregulation in the association between negative emotion dysregulation and substance use.
Relatedly, evidence for a robust relation between positive emotion dysregulation and substance use may point to the role of reward functioning, including reward motivation (i.e., “wanting”), marked by anticipation and approach of reward and related to the desire or motivation to pursue reward; consummatory reward (i.e., “liking”), or being able to enjoy a reward and related to feelings of pleasure and future pursuit of behaviors that elicit rewards; and reward learning, or changing one’s behavior based on reward history (Berridge et al., 2009). Deficits in each of these areas have been linked to elevated substance use (Hommer et al., 2011; Lubman et al., 2009; Park et al., 2010) and may be exacerbated by positive emotion dysregulation. As such, additional research is needed to explore the role of reward functioning in the relation between positive emotion regulation and substance use.
Moderators of Age, Sex, Race, and Sample Type
Findings for age indicated that most aspects of negative emotion regulation abilities were more strongly related to substance use for samples characterized by older adults. Perhaps, younger adults may be motivated to use substances for reasons other than those related to emotion regulation, such as those that serve social/affiliative or approval/conformity functions (Cooper et al., 2016). Notably, literature suggests fewer deficits in emotion regulation in older age resultant from (1) smaller/more transient increases in negative affect, (2) increased well-being and positive affect, and (3) enhanced emotion regulation (for a review, see Urry & Gross, 2010). As most of the studies reviewed here were comprised of young- to middle-aged adults, research on emotion regulation and substance use among samples of older adults is warranted. Such investigations may highlight a U-shaped function of age in relation to emotion regulation and substance use, with other motives for substances being more prominent in younger and older adults compared to middle-aged adults.
In terms of sex, most aspects of positive emotion regulation strategies and maladaptive strategies were more strongly related to overall substance use for samples comprised of fewer females, whereas awareness of negative emotions and adaptive strategies were more strongly related to overall substance use for samples characterized by more females. Greater fear of positive emotions has been shown to be associated with more masculine gender role stress (Jakupcak et al., 2003). Thus, males, who typically identify with more masculine gender roles, may take a more judgmental and evaluative stance toward positive emotion states (Weiss et al., 2019), which, in turn, may motivate their substance use (Weiss et al., 2018). The stronger link between maladaptive strategies and substance use among samples comprised of fewer females is consistent with existing research (for a review, see Nolen-Hoeksema, 2004); moreover, this link has been tied to an increased likelihood to use alcohol for the purpose of denying or avoiding emotions among males compared to females (Cooper et al., 1992). Our findings regarding the awareness aspect of emotion regulation suggest that females who pay less attention to their emotions are more likely to use substances compared to males. For females, allocating minimal attention to emotions may be more indicative of a tendency towards emotional avoidance—a central mechanism known to underlie substance use (Baker et al., 2004). Finally, our review results suggest that the use of more adaptive emotion regulation strategies may be linked to less substance use for females as compared to males. There is evidence that females generate more positive affect than males when using adaptive strategies (McRae et al., 2008); this may protect against substance use (Wills et al., 1999).
Regarding race, percent of White individuals across studies was not found to influence the relations among aspects of emotion regulation and overall substance use. This finding should be considered in the context of relevant limitations of the reviewed studies: specifically, the vast majority of investigations were conducted in the United States and were comprised of predominantly White individuals. Examining relations of emotion regulation to substance use within international and racially diverse samples would better speak to the potential racial differences in this association. Indeed, racial groups hold different guidelines for the regulation of emotional expression (Matsumoto, 1993). These culturally sanctioned norms and rules result in divergent conditions under which emotional responses are sanctioned (Butler et al., 2007). For example, racial groups characterized by collectivist values generally prioritize in-group (vs. individual) goals; as such, members are encouraged to modify their emotions to meet the needs of the group (Hofstede, 2001). Cultural values of conformity, obedience, and in-group cohesion among such racial groups may motivate individuals to simultaneously express emotions that maintain in-group harmony and down-regulate emotions (e.g., via substances; Weiss et al., 2020; Weiss, Goncharenko, et al., in press) that threaten in-group harmony. In line with this theory, studies suggest racial differences in the relation of emotion regulation to substance use (Richman et al., 2011; Weiss, Schick, et al., in press).
Finally, sample type was found to be a moderator; samples characterized by clinical participants (vs. college or community participants) generally showed stronger relations between aspects of emotion regulation and overall substance use. Stronger relations were also generally found among samples comprised of clinical participants seeking treatment for a substance use disorder (vs. participants without a substance use disorder). Thus, the strength of the relations between aspects of emotion regulation and substance use may vary as a function of clinical or substance use severity; these findings are consistent with research showing that emotion regulation plays a key role in the etiology and maintenance of clinical levels of psychopathology (Chaplin & Cole, 2005; Jazaieri et al., 2013; Kring & Sloan, 2009) and substance use disorder specifically (Fox et al., 2007; Fox et al., 2008). Our results highlight the importance of studying and comparing analogue and clinical populations when conducting research on emotion regulation and substance use. Comparisons between analogue and clinical populations may delineate how and when aspects of emotion regulation increase risk for substance use. For instance, the relation between suppression and substance use was stronger in clinical samples with substance use disorder compared to non-clinical samples, a notable finding given the small/non-significant effects between suppression and substance use in the overall sample. Paradoxical effects of suppression—at least in terms of substance use—may be more likely among individuals with substance use disorders, perhaps because they rigidly apply suppression to regulate distress (Kober & Bolling, 2014). In particular, more frequent use of suppression among individuals with substance use disorders may exacerbate distressing emotions, increasing motivations to use substances. It also warrants mention that the strength of the relations among aspects of emotion regulation and substance use between samples of clinical and community individuals were comparable. Although not identified by clinically significant levels of psychopathology or substance use specifically, it is likely that many individuals in the community also experience these concerns.
Additional Limitations
Other limitations warrant consideration when interpreting review findings. First, although results of the funnel plot indicated that publication bias was unlikely, and the fail-safe N analyses generally suggested robust effects for many relations, the file drawer problem remains a concern and could have contributed to inflated effect sizes (Rosenthal, 1979). Second, data from the reviewed studies were cross-sectional; thus, we cannot speculate on the directionality of the examined relations. Nonetheless, convergence across multiple cross-sectional studies does increase the confidence in the current findings. Third, most studies used retrospective and self-report measures of emotion regulation and substance use. Thus, we were not able to examine the influence of self-report vs. diagnostic interview for substance use, and readers should be sensitive to potential reporting bias that may be more salient to populations described by substance use. Use of prospective longitudinal designs, including experience sampling methodology, as well as the examination of objective metrics of emotion regulation (e.g., physiological [high frequency heart rate variability; Weiss et al., 2021], behavioral [Paced Auditory Serial Addition Task—Computerized; Gratz et al., 2006]) may reduce biases related to social desirability, selective recall, or deficient awareness (Althubaiti, 2016). Fourth, we excluded papers that examined constructs that were similar to emotion regulation but fell outside the conceptualization of emotion regulation described by Tull and Aldao (2015a; e.g., mindfulness, distress tolerance, anxiety sensitivity). Similarly, the focus of this review was on substance use; as such, papers that examined other substance use constructs (e.g., coping, motives, expectancies) were excluded. Synthesis of research examining constructs that are similar to, but distinct from, emotion regulation and substance use is an important avenue for future research. Relatedly, although outside the scope of the current study, research would benefit from examination of the latent structure of the emotion regulation construct. Fifth, there were not a sufficient number of studies to disaggregate substance use constructs as much as we would have liked (e.g., by specific drug, such as opioids and marijuana). It is likely that differences in the substance use constructs could affect the calculated effect sizes. This is an important avenue for future research given that individuals use certain substances for their differential emotion-regulating effects (Tull et al., 2010). Finally, while this review examined the impact of clinical vs. non-clinical sample type in the relations between emotion regulation and substance use, we did not evaluate the moderating influence of specific psychiatric comorbidity in these associations. The presence of psychiatric comorbidity (e.g., mood, anxiety, trauma-related disorders) is relevant to both emotion regulation (Roemer et al., 2009; Tull & Gratz, 2008; Weiss et al., 2013) and substance use (Grant et al., 2015; Grant et al., 2016), and as such should be empirically examined in studies examining their association. Relatedly, clinical samples reviewed here were predominantly composed of adults in substance use or general psychiatric treatments. Investigations of the relation between emotion regulation and substance use are needed in other clinical populations at elevated risk for substance use disorder (e.g., individuals with psychotic or personality disorders; Blanchard et al., 2000; Trull et al., 2000).
Conclusions
Despite these limitations, the current meta-analytic review advances the existing literature on emotion regulation and substance use. Specifically, our findings suggest that the strength of this association varies considerably in relation to both the aspect of emotion regulation and type of substance use. Moreover, findings indicated that the relations between aspect of emotion regulation and substance use were generally stronger for samples that were older and clinical; mixed effects were found for sex and no conclusive effects for race. These results underscore the potential utility of targeting emotion regulation in the prevention and treatment of substance use (Gratz et al., 2015), and of targeting abilities (vs. strategies) in particular, inclusive of the regulation of both negative and positive emotions.
Supplementary Material
Highlights.
The emotion regulation and substance use relation was significant and small-to-medium
Emotion regulation abilities vs. strategies were more strongly related to substance use
Behavioral vs. cognitive abilities were more strongly related to substance use
Both negative and positive emotion regulation abilities were related to substance use
Relations were stronger for older and clinical samples; mixed effects were found for sex
Acknowledgements
The authors would like to thank Joseph Mammay and Savannah Hill for their help with abstract coding.
Role of Funding Sources
Work on this paper by the first author (NHW) was supported by National Institutes of Health Grant K23 DA039327. NHW also acknowledges the support from the Center for Biomedical Research and Excellence (COBRE) on Opioids and Overdose funded by the National Institute on General Medical Sciences (P20 GM125507). Work on this paper by the fifth author (SRF) was supported by National Institute on Drug Abuse Grant F31 DA051167.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors declare that they have no conflicts of interest.
References
- Aldao A (2013). The future of emotion regulation research capturing context. Perspectives on Psychological Science, 8(2), 155–172. 10.1177/1745691612459518 [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- Althubaiti A (2016). Information bias in health research: definition, pitfalls, and adjustment methods. Journal of Multidisciplinary Healthcare, 9, 211–217. 10.2147/JMDH.S104807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelrod SR, Perepletchikova F, Holtzman K, & Sinha R (2011). Emotion regulation and substance use frequency in women with substance dependence and borderline personality disorder receiving dialectical behavior therapy. The American Journal of Drug and Alcohol Abuse, 37(1), 37–42. 10.3109/00952990.2010.535582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111(1), 33–51. 10.1037/0033-295X.111.1.33 [DOI] [PubMed] [Google Scholar]
- Bakhshaie J, Rogers AH, Kauffman BY, Tran N, Buckner JD, Ditre JW, & Zvolensky MJ (2019). Emotion dysregulation as an explanatory factor in the relation between negative affectivity and non-medical use of opioid in a diverse young adult sample. Addictive Behaviors, 95, 103–109. 10.1016/j.addbeh.2019.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardeen JR, Fergus TA, & Orcutt HK (2012). An examination of the latent structure of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 34, 382–392. 10.1007/s10862-012-9280-y [DOI] [Google Scholar]
- Beblo T, Fernando S, Kamper P, Griepenstroh J, Aschenbrenner S, Pastuszak A, Schlosser N, & Driessen M (2013). Increased attempts to suppress negative and positive emotions in borderline personality disorder. Psychiatry Research, 210(2), 505–509. 10.1016/j.psychres.2013.06.036 [DOI] [PubMed] [Google Scholar]
- Beblo T, Fernando S, Klocke S, Griepenstroh J, Aschenbrenner S, & Driessen M (2012). Increased suppression of negative and positive emotions in major depression. Journal of Affective Disorders, 141(2–3), 474–479. 10.1016/j.jad.2012.03.019 [DOI] [PubMed] [Google Scholar]
- Berking M, Margraf M, Ebert D, Wupperman P, Hofmann SG, & Junghanns K (2011). Deficits in emotion-regulation skills predict alcohol use during and after cognitive–behavioral therapy for alcohol dependence. Journal of Consulting and Clinical Psychology, 79(3), 307–318. 10.1037/a0023421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein A, Zvolensky MJ, Vujanovic AA, & Moos R (2009). Integrating anxiety sensitivity, distress tolerance, and discomfort intolerance: A hierarchical model of affect sensitivity and tolerance. Behavior Therapy, 40(3), 291–301. 10.1016/j.beth.2008.08.001 [DOI] [PubMed] [Google Scholar]
- Blanchard JJ, Brown SA, Horan WP, & Sherwood AR (2000). Substance use disorders in schizophrenia: Review, integration, and a proposed model. Clinical Psychology Review, 20(2), 207–234. 10.1016/s0272-7358(99)00033-1 [DOI] [PubMed] [Google Scholar]
- Bodenlos JS, Noonan M, & Wells SY (2013). Mindfulness and alcohol problems in college students: The mediating effects of stress. Journal of American College Health, 61(6), 371–378. 10.1080/07448481.2013.805714 [DOI] [PubMed] [Google Scholar]
- Brandt CP, Johnson KA, Schmidt NB, & Zvolensky MJ (2012). Main and interactive effects of emotion dysregulation and breath holding duration in relation to panic-relevant fear and expectancies about anxiety-related sensations among adult daily smokers. Journal of Anxiety Disorders, 26(1), 173–181. 10.1016/j.janxdis.2011.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bresin K, Mekawi Y, & Verona E (2018). The effect of laboratory manipulations of negative affect on alcohol craving and use: A meta-analysis. Psychology of Addictive Behaviors, 32(6), 617–627. 10.1037/adb0000383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler EA, Lee TL, & Gross JJ (2007). Emotion regulation and culture: Are the social consequences of emotion suppression culture-specific? Emotion, 7(1), 30–48. 10.1037/1528-3542.7.1.30 [DOI] [PubMed] [Google Scholar]
- Chaplin TM, & Cole PM (2005). The role of emotion regulation in the development of psychopathology. In Hankin BL & Abela JRZ (Eds.), Development of psychopathology: A vulnerability-stress perspective (p. 49–74). Sage Publications, Inc. 10.4135/9781452231655.n3 [DOI] [Google Scholar]
- Cohen J (1988). The effect size. Statistical power analysis for the behavioral sciences, 77–83. [Google Scholar]
- Cole PM, Michel MK, & Teti LO (1994). The development of emotion regulation and dysregulation: A clinical perspective. Monographs of the Society for Research in Child Development, 59, 73–102. 10.1111/j.1540-5834.1994.tb01278.x [DOI] [PubMed] [Google Scholar]
- Connor JP, Gullo MJ, White A, & Kelly AB (2014). Polysubstance use: Diagnostic challenges, patterns of use and health. Current Opinion in Psychiatry, 27(4), 269–275. 10.1097/YCO.0000000000000069 [DOI] [PubMed] [Google Scholar]
- Cooper ML, Kuntsche E, Levitt A, Barber LL, & Wolf S (2016). Motivational models of substance use: A review of theory and research on motives for using alcohol, marijuana, and tobacco. In Sher KJ (Ed.), The Oxford handbook of substance use and substance use disorders (p. 375–421). Oxford University Press. 10.1093/oxfordhb/9780199381678.013.017 [DOI] [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Frone MR, & Mudar P (1992). Stress and alcohol use: Moderating effects of gender, coping, and alcohol expectancies. Journal of Abnormal Psychology, 101(1), 139–152. 10.1037/0021-843X.101.1.139 [DOI] [PubMed] [Google Scholar]
- Coskunpinar A, Dir AL, & Cyders MA (2013). Multidimensionality in impulsivity and alcohol use: A meta-analysis using the UPPS model of impulsivity. Alcoholism: Clinical and Experimental Research, 37(9), 1441–1450. 10.1111/acer.12131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon-Gordon KL, Aldao A, & De Los Reyes A (2015). Repertoires of emotion regulation: A person-centered approach to assessing emotion regulation strategies and links to psychopathology. Cognition and Emotion, 29(7), 1314–1325. 10.1080/02699931.2014.983046 [DOI] [PubMed] [Google Scholar]
- Dunn BD, Billotti D, Murphy V, & Dalgleish T (2009). The consequences of effortful emotion regulation when processing distressing material: A comparison of suppression and acceptance. Behaviour Research and Therapy, 47(9), 761–773. 10.1016/j.brat.2009.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvorak RD, Sargent EM, Kilwein TM, Stevenson BL, Kuvaas NJ, & Williams TJ (2014). Alcohol use and alcohol-related consequences: Associations with emotion regulation difficulties. The American Journal of Drug and Alcohol Abuse, 40(2), 125–130. 10.3109/00952990.2013.877920 [DOI] [PubMed] [Google Scholar]
- Fernandez AC, Wood MD, Stein LAR, & Rossi JS (2010). Measuring mindfulness and examining its relationship with alcohol use and negative consequences. Psychology of Addictive Behaviors, 24(4), 608–616. 10.1037/a0021742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field AP (2003). The problems in using fixed-effects models of meta-analysis on real-world data. Understanding Statistics: Statistical Issues in Psychology, Education, and the Social Sciences, 2(2), 105–124. 10.1207/S15328031US0202_02 [DOI] [Google Scholar]
- Fowler JC, Charak R, Elhai JD, Allen JG, Frueh BC, & Oldham JM (2014). Construct validity and factor structure of the difficulties in emotion regulation scale among adults with severe mental illness. Journal of Psychiatric Research, 58, 175–180. 10.1016/j.psychires.2014.07.029 [DOI] [PubMed] [Google Scholar]
- Fox HC, Axelrod SR, Paliwal P, Sleeper J, & Sinha R (2007). Difficulties in emotion regulation and impulse control during cocaine abstinence. Drug and Alcohol Dependence, 89(2–3), 298–301. 10.1016/j.drugalcdep.2006.12.026 [DOI] [PubMed] [Google Scholar]
- Fox HC, Hong KA, & Sinha R (2008). Difficulties in emotion regulation and impulse control in recently abstinent alcoholics compared with social drinkers. Addictive Behaviors, 33(2), 388–394. 10.1016/j.addbeh.2007.10.002 [DOI] [PubMed] [Google Scholar]
- Fragkos KC, Tsagris M, & Frangos CC (2014). Publication bias in meta-analysis: Confidence intervals for Rosenthal’s fail-safe number. International Scholarly Research Notices, 2014, 1–17. 10.1155/2014/825383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen PA, Dean JA, & Lanius RA (2012). Assessment of anhedonia in psychological trauma: Development of the Hedonic Deficit and Interference Scale. European Journal of Psychotraumatology, 3(1), 8585–8596. 10.3402/ejpt.v3i0.8585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garke MA, Isacsson NH, Sörman K, Bjureberg J, Hellner C, Gratz KL, Berghoff CR, Sinha R, Tull MT, & Jayaram-Lindström N (2021). Emotion dysregulation across levels of substance use. Psychiatry Research, 296, 113662. 10.1016/j.psychres.2020.113662 [DOI] [PubMed] [Google Scholar]
- Gorka SM, Ali B, & Daughters SB (2012). The role of distress tolerance in the relationship between depressive symptoms and problematic alcohol use. Psychology of Addictive Behaviors, 26(3), 621–626. 10.1037/a0026386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, … & Hasin DS (2015). Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry, 72(8), 757–766. 10.1001/jamapsychiatry.2015.0584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Saha TD, Ruan WJ, Goldstein RB, Chou SP, Jung J, … & Hasin DS (2016). Epidemiology of DSM-5 drug use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions–III. JAMA Psychiatry, 73(1), 39–47. 10.1001/jamapsychiatry.2015.2132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. 10.1023/B:JOBA.0000007455.08539.94 [DOI] [Google Scholar]
- Gratz KL, & Tull MT (2010). Emotion regulation as a mechanism of change in acceptance- and mindfulness-based treatments. In Baer RA (Ed.), Assessing Mindfulness and Acceptance: Illuminating the Theory and Practice of Change (pp. 105–133). New Harbinger Publications. [Google Scholar]
- Gratz KL, Weiss NH, & Tull MT (2015). Examining emotion regulation as an outcome, mechanism, or target of psychological treatments. Current Opinion in Psychology, 3, 85–90. 10.1016/j.copsyc.2015.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross JJ (2015). Emotion regulation: Current status and future prospects. Psychological Inquiry, 26(1), 1–26. 10.1080/1047840X.2014.940781 [DOI] [Google Scholar]
- Hedges LV, & Olkin I (1985). Statistical methods for meta-analysis. Orlando, FL: Academic Press. [Google Scholar]
- Hedges LV, & Vevea JL (1998). Fixed- and random-effects models in meta-analysis. Psychological Methods, 3(4), 486–504. 10.1037/1082-989X.3.4.486 [DOI] [Google Scholar]
- Hofstede G (2001). Culture’s consequences: Comparing values, behaviors, institutions and organizations across nations. Sage. [Google Scholar]
- Hommer DW, Bjork JM, & Gilman JM (2011). Imaging brain response to reward in addictive disorders. Annals of the New York Academy of Sciences, 1216(1), 50–61. 10.1111/j.1749-6632.2010.05898.x [DOI] [PubMed] [Google Scholar]
- Howell AN, Leyro TM, Hogan J, Buckner JD, & Zvolensky MJ (2010). Anxiety sensitivity, distress tolerance, and discomfort intolerance in relation to coping and conformity motives for alcohol use and alcohol use problems among young adult drinkers. Addictive Behaviors, 35(12), 1144–1147. 10.1016/j.addbeh.2010.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inzlicht M, & Schmeichel BJ (2012). What is ego depletion? Toward a mechanistic revision of the resource model of self-control. Perspectives on Psychological Science, 7(5), 450–463. 10.1177/1745691612454134 [DOI] [PubMed] [Google Scholar]
- Jakupcak M, Salters K, Gratz KL, & Roemer L (2003). Masculinity and emotionality: An investigation of men’s primary and secondary emotional responding. Sex Roles, 49(3–4), 111–120. 10.1023/A:1024452728902 [DOI] [Google Scholar]
- Jazaieri H, Urry HL, & Gross JJ (2013). Affective disturbance and psychopathology: An emotion regulation perspective. Journal of Experimental Psychopathology, 4(5), 584–599. 10.5127/jep.030312 [DOI] [Google Scholar]
- Jones JD, Mogali S, & Comer SD (2012). Polydrug abuse: A review of opioid and benzodiazepine combination use. Drug and Alcohol Dependence, 125(1–2), 8–18. 10.1016/j.drugalcdep.2012.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kale D, Stautz K, & Cooper A (2018). Impulsivity related personality traits and cigarette smoking in adults: A meta-analysis using the UPPS-P model of impulsivity and reward sensitivity. Drug and Alcohol Dependence, 185(1), 149–167. 10.1016/j.drugalcdep.2018.01.003 [DOI] [PubMed] [Google Scholar]
- Kober H, & Bolling D (2014). Emotion regulation in substance use disorders (Vol. 2nd). Guilford Press. [Google Scholar]
- Koole SL (2009). The psychology of emotion regulation: An integrative review. Cognition and Emotion, 23(1), 4–41. 10.1080/02699930802619031 [DOI] [Google Scholar]
- Kring AM, & Sloan DM (2009). Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment. Guilford Press. [Google Scholar]
- Lawrence VA, & Lee D (2014). An exploration of people’s experiences of compassion-focused therapy for trauma, using interpretative phenomenological analysis. Clinical Psychology & Psychotherapy, 21(6), 495–507. 10.1002/cpp.1854 [DOI] [PubMed] [Google Scholar]
- Lipsey MW, & Wilson DB (2001). Practical meta-analysis. SAGE publications, Inc. [Google Scholar]
- Litz BT, Orsillo SM, Kaloupek D, & Weathers F (2000). Emotional processing in posttraumatic stress disorder. Journal of Abnormal Psychology, 109(1), 26–39. 10.1037/0021-843X.109.1.26 [DOI] [PubMed] [Google Scholar]
- Lubman DI, Yücel M, Kettle JW, Scaffidi A, MacKenzie T, Simmons JG, & Allen NB (2009). Responsiveness to drug cues and natural rewards in opiate addiction: Associations with later heroin use. Archives of General Psychiatry, 66(2), 205–212. 10.1001/archgenpsychiatry.2008.522 [DOI] [PubMed] [Google Scholar]
- MacIntyre JM, Ruscio AC, Brede E, & Waters AJ (2018). Emotion dysregulation and negative affect: Laboratory and EMA investigations in smokers. Addictive Behaviors Reports, 7, 65–70. 10.1016/j.abrep.2018.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall-Berenz EC, Vujanovic AA, & MacPherson L (2011). Impulsivity and alcohol use coping motives in a trauma-exposed sample: The mediating role of distress tolerance. Personality and Individual Differences, 50(5), 588–592. 10.1016/j.paid.2010.11.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsumoto D (1993). Ethnic differences in affect intensity, emotion judgments, display rule attitudes, and self-reported emotional expression in an American sample. Motivation and Emotion, 17(2), 107–123. [Google Scholar]
- McHugh RK, Reynolds EK, Leyro TM, & Otto MW (2013). An examination of the association of distress intolerance and emotion regulation with avoidance. Cognitive Therapy and Research, 37(2), 363–367. 10.1007/s10608-012-9463-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McRae K, Ochsner KN, Mauss IB, Gabrieli JJ, & Gross JJ (2008). Gender differences in emotion regulation: An fMRI study of cognitive reappraisal. Group Processes & Intergroup Relations, 11(2), 143–162. 10.1177/1368430207088035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S (2004). Gender differences in risk factors and consequences for alcohol use and problems. Clinical Psychology Review, 24(8), 981–1010. 10.1016/j.cpr.2004.08.003 [DOI] [PubMed] [Google Scholar]
- Park SQ, Kahnt T, Beck A, Cohen MX, Dolan RJ, Wrase J, & Heinz A (2010). Prefrontal cortex fails to learn from reward prediction errors in alcohol dependence. Journal of Neuroscience, 30(22), 7749–7753. 10.1523/JNEUROSCI.5587-09.2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richman JA, Sohmer D, Rospenda KM, & Shannon CA (2011). Race/ethnicity, coping, and drinking outcomes. Journal of Drug Issues, 41, 401–418. 10.1177/002204261104100305 [DOI] [Google Scholar]
- Rodriguez LM, Dell JB, Lee KD, & Onufrak J (2019). Effects of a brief cognitive reappraisal intervention on reductions in alcohol consumption and related problems. Psychology of Addictive Behaviors, 33(7), 637. 10.1037/adb0000509 [DOI] [PubMed] [Google Scholar]
- Roemer L, Lee JK, Salters-Pedneault K, Erisman SM, Orsillo SM, & Mennin DS (2009). Mindfulness and emotion regulation difficulties in generalized anxiety disorder: Preliminary evidence for independent and overlapping contributions. Behavior Therapy, 40(2), 142–154. 10.1016/j.beth.2008.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Litz BT, Orsillo SM, & Wagner AW (2001). A preliminary investigation of the role of strategic withholding of emotions in PTSD. Journal of Traumatic Stress, 14(1), 149–156. [Google Scholar]
- Rosenthal R (1979). The file drawer problem and tolerance for null results. Psychological Bulletin, 86(3), 638–641. 10.1037/0033-2909.86.3.638 [DOI] [Google Scholar]
- Rothstein HR (2007). Publication bias as a threat to the validity of meta-analytic results. Journal of Experimental Criminology, 4, 61–81. doi: 10.1007/s11292-007-9046-9 [DOI] [Google Scholar]
- Rothstein HR, Sutton AJ, & Borenstein M (Eds.). (2006). Publication bias in meta-analysis: Prevention, assessment and adjustments. West Sussex: Wiley. [Google Scholar]
- Salters-Pedneault K, Roemer L, Tull MT, Rucker L, & Mennin DS (2006). Evidence of broad deficits in emotion regulation associated with chronic worry and generalized anxiety disorder. Cognitive Therapy and Research, 30, 469–480. 10.1007/s10608-006-9055-4 [DOI] [Google Scholar]
- Schmidt NB, Buckner JD, & Keough ME (2007). Anxiety sensitivity as a prospective predictor of alcohol use disorders. Behavior Modification, 31(2), 202–219. 10.1177/0145445506297019 [DOI] [PubMed] [Google Scholar]
- Shiffman S (2009). Ecological momentary assessment (EMA) in studies of substance use. Psychological Assessment, 21(4), 486–497. 10.1037/a0017074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RA (1994). Emotion regulation: A theme in search of definition. Monographs of the Society for Research in Child Development, 59(2–3), 25–52. 10.1111/j.1540-5834.1994.tb01276.x [DOI] [PubMed] [Google Scholar]
- Trull TJ, Sher KJ, Minks-Brown C, Durbin J, & Burr R (2000). Borderline personality disorder and substance use disorders: A review and integration. Clinical Psychology Review, 20(2), 235–253. 10.1016/s0272-7358(99)00028-8 [DOI] [PubMed] [Google Scholar]
- Tull MT, & Aldao A (2015). Editorial overview: New directions in the science of emotion regulation. Current Opinion in Psychology, 3, 4–10. [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, & Roemer L (2007). A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy, 38(3), 303–313. 10.1016/j.beth.2006.10.001 [DOI] [PubMed] [Google Scholar]
- Tull MT, Berghoff CR, Wheeless LE, Cohen RT, & Gratz KL (2018). PTSD symptom severity and emotion regulation strategy use during trauma cue exposure among patients with substance use disorders: Associations with negative affect, craving, and cortisol reactivity. Behavior Therapy, 49(1), 57–70. 10.1016/j.beth.2017.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Forbes CN, Weiss NH, & Gratz KL (2019). An investigation of the effect of trauma script exposure on risk-taking among patients with substance use disorders and posttraumatic stress disorder. Journal of Anxiety Disorders, 62, 77–85. 10.1016/j.janxdis.2019.01.002 [DOI] [PubMed] [Google Scholar]
- Tull MT, & Gratz KL (2008). Further examination of the relationship between anxiety sensitivity and depression: The mediating role of experiential avoidance and difficulties engaging in goal-directed behavior when distressed. Journal of Anxiety Disorders, 22(2), 199–210. 10.1016/j.janxdis.2007.03.005 [DOI] [PubMed] [Google Scholar]
- Tull MT, Gratz KL, Aklin WM, & Lejuez CW (2010). A preliminary examination of the relationships between posttraumatic stress symptoms and crack/cocaine, heroin, and alcohol dependence. Journal of Anxiety Disorders, 24(1), 55–62. 10.1016/j.janxdis.2009.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Gratz KL, McDermott MJ, Bordieri MJ, Daughters SB, & Lejuez CW (2016). The role of emotion regulation difficulties in the relation between PTSD symptoms and the learned association between trauma-related and cocaine cues. Substance Use & Misuse, 51(10), 1318–1329. 10.3109/10826084.2016.1168445 [DOI] [PubMed] [Google Scholar]
- Tull MT, McDermott MJ, & Gratz KL (2016). Marijuana dependence moderates the effect of posttraumatic stress disorder on trauma cue reactivity in substance dependent patients. Drug and Alcohol Dependence, 159, 219–226. 10.1016/j.drugalcdep.2015.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urry HL, & Gross JJ (2010). Emotion regulation in older age. Current Directions in Psychological Science, 19(6), 352–357. 10.1177/0963721410388395 [DOI] [Google Scholar]
- VanderVeen JD, Hershberger AR, & Cyders MA (2016). UPPS-P model impulsivity and marijuana use behaviors in adolescents: A meta-analysis. Drug and Alcohol Dependence, 168, 181–190. 10.1016/j.drugalcdep.2016.09.016 [DOI] [PubMed] [Google Scholar]
- Vine V, & Aldao A (2014). Impaired emotional clarity and psychopathology: A transdiagnostic deficit with symptom-specific pathways through emotion regulation. Journal of Social and Clinical Psychology, 33(4), 319–342. 10.1521/jscp.2014.33.4.319 [DOI] [Google Scholar]
- Weiss NH, Darosh A, Contractor A, Schick MR, & Dixon-Gordon KL (2019). Confirmatory validation of the factor structure and psychometric properties of the Difficulties in Emotion Regulation Scale – Positive. Journal of Clinical Psychology, 75(7), 1267–1287. 10.1002/jclp.22768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Forkus SR, Contractor AA, & Schick MR (2018). Difficulties regulating positive emotions and alcohol and drug misuse: A path analysis. Addictive Behaviors, 84, 45–52. 10.1016/j.addbeh.2018.03.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Forkus SR, Raudales AM, Schick MR, & Contractor AA (2020). Alcohol misuse to down-regulate positive emotions: A cross-sectional multiple mediator analysis among US military veterans. Addictive Behaviors, 105, 106322. 10.1016/j.addbeh.2020.106322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Goncharenko S, Raudales AM, Forkus SR, & Contractor AA (in press). PTSD symptoms are assoicated with alcohol misuse through alcohol use to down-regulate positive emotions. Addictive Behaviors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Gratz KL, & Lavender J (2015). Factor structure and initial validation of a multidimensional measure of difficulties in the regulation of positive emotions: The DERS-Positive. Behavior Modification, 39(3), 431–453. 10.1177/0145445514566504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Schick MR, Contractor AA, Reyes ME, Suazo NC, & Sullivan TP (in press). Racial/ethnic differences in alcohol and drug misuse among IPV-victimized women: Exploring the role of difficulties regulating positive emotions. Journal of Interpersonal Violence. 10.1177/0886260520943735 [DOI] [PubMed] [Google Scholar]
- Weiss NH, Schick MR, Waite EE, Haliczer LA, & Dixon-Gordon KL (2021). Association of positive emotion dysregulation to resting heart rate variability: The influence of positive affect intensity. Personality and Individual Differences, 173, 110607. 10.1016/j.paid.2020.110607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Sullivan TP, & Tull MT (2015). Explicating the role of emotion dysregulation in risky behaviors: A review and synthesis of the literature with directions for future research and clinical practice. Current Opinion in Psychology, 3, 22–29. 10.1016/j.copsyc.2015.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Anestis MD, & Gratz KL (2013). The relative and unique contributions of emotion dysregulation and impulsivity to posttraumatic stress disorder among substance dependent inpatients. Drug and Alcohol Dependence, 128(1–2), 45–51. 10.1016/j.drugalcdep.2012.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, & Sullivan TP (2015). Emotion dysregulation and risky, self-destructive, and health compromising behaviors: A review of the literature. Nova Science Publishers. [Google Scholar]
- Weiss NH, Tull MT, Viana AG, Anestis MD, & Gratz KL (2012). Impulsive behaviors as an emotion regulation strategy: Examining associations between PTSD, emotion dysregulation, and impulsive behaviors among substance dependent inpatients. Journal of Anxiety Disorders, 26(3), 453–458. 10.1016/j.janxdis.2012.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wray TB, Merrill JE, & Monti PM (2014). Using ecological momentary assessment (EMA) to assess situation-level predictors of alcohol use and alcohol-related consequences. Alcohol Research: Current Reviews, 36(1), 19–27. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


