Abstract
Background
Adverse parenting is consistently associated with increased sleep problems among adolescents. Shelter-in-Place restrictions and the uncertainty linked to the Covid-19 pandemic have introduced new stressors on parents and families, adding to the risk for youth's sleep problems.
Objective
Using multidimensional assessments of child maltreatment (CM; threat vs. deprivation), the present study examined whether parent-report and child-report of Covid-19 related stress potentiated the effect of CM on sleep problems among boys and girls.
Participants and setting
The study focused on a sample of 124 dyads of adolescents (Mage = 12.89, SD = 0.79; 52% female) and their primary caregivers (93% mothers) assessed before and during the pandemic (May to October 2020).
Method
Data were obtained from both youth and their parents. Structural equation modeling (SEM) was used to test all study hypotheses. Simple slopes and Johnson-Neyman plots were generated to probe significant interaction effects.
Results
Deprivation, but not threat, directly predicted increased sleep problems among boys during the pandemic. Additionally, elevation in Covid-19 stress (both parent and child report) intensified the link between CM (threat and deprivation) and sleep problems among boys.
Conclusion
Our findings inform prevention and intervention efforts that aim to reduce sleep problems among boys during stressful contexts, such as the Covid-19 pandemic.
Keywords: Covid-19 related stress, Child maltreatment, Multidimensional approach, Sleep problems, Gender differences
1. Introduction
Sleep is a bio-regulatory behavior linked to essential restorative cognitive and emotional functioning in adolescence (Dahl & Lewin, 2002). Extant research suggests that parenting behaviors significantly influence adolescents' sleep quality (El-Sheikh & Kelly, 2017; Tsai et al., 2018). In particular, adverse parenting (e.g., child maltreatment) is a significant stressor that is robustly linked to youth sleep problems (McPhie, Weiss, & Wekerle, 2014; Turner et al., 2020). In 2019, the Coronavirus pandemic (Covid-19) introduced a new form of stress for families and adolescents worldwide and within the United States (Dalton, Rapa, & Stein, 2020). With over 2 million positive cases and 500,000 deaths in the U.S. since the widespread transmission of the virus (Honein et al., 2020), youth are experiencing abrupt changes in their daily routines (e.g., home quarantine, social isolation), increased rates of stress and anxiety, insecurity about health, and worries about the future (Altena et al., 2020). During this time of increased uncertainty and strain within families (Liu & Fisher, in press), we expect that the impact of adverse parenting on youth's sleep will be intensified. Specifically, Covid-19 related stressors might be particularly harmful to sleep patterns among youth who are already experiencing stress within the home environment. Using a multidimensional assessment of child maltreatment (CM, i.e., threat vs. deprivation), multiple reports of Covid-19 related stress, and a two-wave design (before and during the pandemic), the present study aimed to examine whether Covid-19 related stressors on families intensified the effect of adverse parenting on youth's sleep problems.
1.1. Child maltreatment and sleep: a dimensional approach
The negative impact of CM on adolescents is evident across multiple bio-regulatory outcomes (Mills et al., 2013; Oshri, Kogan, Liu, Sweet and Mackillop, 2017, Oshri, Sutton, Clay-Warner and Miller, 2015), including sleep problems (Xiao et al., 2020; Sasser, Oshri, Duprey, Doane and Peltz, 2021). Previous research demonstrated that CM severity in adolescence predicted sleep disturbances after one year (e.g., sleep latency, waking episodes, daytime sleepiness; McPhie et al., 2014). Emerging research has also identified a dose-response association between maltreatment and sleep, such that youth who experienced a greater frequency of CM were at increased risk for sleep problems (Turner et al., 2020; Xiao et al., 2020). Although the associations between CM and adolescents' sleep problems are well documented, most research has either examined maltreatment using single types of adversity (e.g., physical abuse or neglect) or cumulative approaches (e.g., combining multiple types of maltreatment).
Recent conceptualization of adverse parenting suggests that attention to maltreatment dimensions provides a more precise operationalization of the subjective experience of different maltreatment types (McLaughlin & Sheridan, 2016; McLaughlin, Sheridan, & Lambert, 2014). Accordingly, adverse parenting experiences are grouped into two main dimensions — omission versus commission, or more recently referred to in the literature as “threat versus deprivation” (McLaughlin et al., 2014). The threat dimension includes physical, emotional, and sexual abuse because these parenting behaviors constitute acts of commission that often exert significant danger to the child (Humphreys & Salo, 2020; McLaughlin & Sheridan, 2016). Physical and emotional neglect are types of CM that constitute the deprivation dimension (McLaughlin et al., 2014) and involve acts of omission that deprive youth of primary care and fundamental physical and emotional needs (Manly, 2005). Studying the dimensions of CM informs preventive intervention efforts as it recognizes the high co-occurrence of CM types and provides insights into developmental mechanisms specific to aspects of adversity (Miller et al., 2018).
Growing evidence shows that the CM dimensions are differentially linked with youth's psychopathology and adjustment (Busso, McLaughlin, & Sheridan, 2017; McLaughlin, Weissman, & Bitrán, 2019; Miller et al., 2018). However, the relative impact of threat versus deprivation on youth's sleep is yet examined. Among studies using adult samples, the long-term effects of CM dimensions on sleep problems yield inconsistent results (Poon & Knight, 2011; Bader, Schäfer, Schenkel, Nissen, & Schwander, 2007). Experiences of threat are linked to hypersensitivity to stimuli, unsafe feelings, hypervigilance, and restless behaviors, leading to sleep disruptions (Dahl & Lewin, 2002; Sadeh & Gruber, 2002). Consequently, adults who experienced threat (e.g., abuse) showed reduced sleep quality compared to adults who reported neglect (Poon & Knight, 2011; Tinajero et al., 2020). Some adult research shows that deprivation (i.e., emotional and physical neglect) may have a worse negative influence on sleep (e.g., insomnia) than measures of threat (i.e., physical, sexual, and emotional abuse; Bader et al., 2007). In addition, a recent study by Semsar, Mousavi, Tran, and Kuhlman (2021) found that both threat and deprivation dimensions were associated with equivalent clinical levels of sleep disturbance in adulthood. Thus, the documented relations between CM dimensions and sleep problems among adults do not provide a basis for forming directional hypotheses on the impact of threat versus deprivation on sleep behaviors in adolescence.
1.2. Covid-19 related stress
Stress among children and adolescents has been hard to avoid during the Covid-19 pandemic (Dalton et al., 2020). The rapid increase in the number of infected cases and deaths, disruption of daily routines, home quarantine, worries of becoming infected, reduced in-person social interactions with peers and friends, and lack of access to educational resources have introduced uncertainty and anxiety among children and adolescents (Dalton et al., 2020; Ellis, Dumas, & Forbes, 2020; Golberstein, Wen, & Miller, 2020). Indeed, growing reports show the detrimental impact of stress related to the pandemic on adolescents' health and adjustment, including sleep behaviors (Imran, Zeshan, & Pervaiz, 2020). For example, a recent study found that higher Covid-19 stress was significantly associated with poorer sleep quality and more frequent insomnia in adolescents (Zhou et al., 2020). Further, families' sleep schedules may shift later during Covid-19, with adolescents reporting more delayed sleep/wake behaviors (Becker et al., 2021).
In addition to adolescents' stress, the Covid-19 pandemic has had negative repercussions for parents and families. For example, home lockdowns in response to the Covid-19 pandemic have been found to induce stress and adverse outcomes (e.g., mental health conditions) within families (Singh et al., 2020). Similarly, home quarantine significantly increases family members' anxiety, depression (Guessoum et al., 2020), and feelings of social isolation (Imran et al., 2020). The inability to access supportive and educational services, visit friends and/or relatives, and participate in outdoor activities may worsen existing family vulnerabilities (Altena et al., 2020). These effects are particularly relevant to rural contexts. Rural families and adolescents may be especially susceptible to the negative effects of Covid-19 due to less restricted precautions, fewer physicians, and a lack of local community resources (Peters, 2020). In addition, for many families residing in rural communities, the pandemic has hindered access to mental health services to mitigate the emotional and financial stress caused by Covid-19 (Peters, 2020).
At-home confinement due to the pandemic can be particularly deleterious in situations where there is pre-existing family strain and stress. Multiple studies have reported a significant increase in intrafamilial violence during the Covid-19 pandemic, including child abuse and neglect (Guessoum et al., 2020; Humphreys & Salo, 2020). Specifically, challenges related to the pandemic can contribute to parental burnout, and parents who experience burnout are more likely to engage in harsh, violent, and neglectful parenting behaviors (Griffith, 2020). The Covid-19 pandemic has also created substantial economic hardship on many families, which has been shown to lead to increased incidents of CM (Rodriguez, Lee, Ward, & Pu, 2020; Sedlak et al., 2010). In addition, parents may experience less social support due to the Covid-19 pandemic, which is a significant risk factor for physical abuse and neglect (Freisthler, Holmes, & Wolf, 2014; Rodriguez & Tucker, 2015). Taken together, youth who were already experiencing adverse parenting and undergoing additional stress related to the Covid-19 pandemic may be at increased risk for sleep problems.
1.3. Gender differences in adolescents' sleep research
The psychological, health and socioemotional effects of psychosocial stress on youth often vary by gender (Campbell, Bann, & Patalay, 2021; Conley & Rudolph, 2009). In the literature on resilience, where positive psychological development is examined in the context of maltreatment, adolescent boys showed heightened vulnerability (Oshri, Duprey, Kogan, Carlson, & Liu, 2018), whereas maltreated girls were more likely to follow resilient trajectories (e.g., no psychiatric diagnosis, socially active, higher employment rate; DuMont, Widom, & Czaja, 2007; McGloin & Widom, 2001; Oshri et al., 2018). Nevertheless, research on gender differences in sleep outcomes shows divergent findings. For example, one study showed that the link between weekday sleep duration and risk behaviors was more robust for boys (Pasch, Laska, Lytle, & Moe, 2010). A large population-based study on sleep in adolescence reported that, compared to girls, boys exhibited significantly stronger associations between depressive symptoms and sleep problems (Sivertsen, Harvey, Lundervold, & Hysing, 2014). In contrast, a study examining over 153,000 Chinese adolescents found that maltreated girls were particularly at risk for sleep problems (Xiao et al., 2020). Another study did not find a significant gender difference in adolescents' sleep patterns (Schneiderman, Ji, Susman, & Negriff, 2018), such that maltreatment was positively correlated with longer sleep duration among both male and female adolescents (Schneiderman et al., 2018). Further, in the context of Covid-19 stress, a recent study by Zhou et al. (2020) found that females were at enhanced risk for sleep problems (e.g., insomnia) during the Covid-19 pandemic. These studies provide mixed evidence for gender differences in the effect of psychosocial stress on sleep problems among youth. However, to the best of our knowledge, no empirical longitudinal study has examined gender differences in the impact of adverse parenting on youth's sleep problems during the Covid-19 pandemic.
1.4. Present study
In this prospective investigation of rural families and adolescents, we examined the direct effects of two main dimensions of adverse parenting (threat and deprivation) on sleep problems among youth assessed before and during the Covid-19 pandemic. In line with previous research (McPhie et al., 2014; Turner et al., 2020; Xiao et al., 2020), we hypothesized that youth with elevated experiences of adverse parenting (both threat and deprivation) would exhibit increased sleep problems compared to non-maltreated youth. Due to limited literature investigating the effects of dimensional CM (threat and deprivation) on adolescents' sleep problems, we did not hypothesize which dimension would be more harmful to adolescents' sleep patterns. Second, we aimed to test whether Covid-19 related stress, as reported by children and parents, would significantly moderate the associations between CM (threat versus deprivation) and sleep problems among adolescents. We expected that increases in Covid-19 related stress would intensify the links between threatening and depriving parenting behaviors and youth's sleep problems. Additionally, we sought to investigate if there were significant gender differences in the effect of Covid-19 related stress on the links between CM dimensions and adolescents' sleep problems. Given the mixed findings in existing literature surrounding gender differences in sleep problems, we did not specify a directional hypothesis for this aim.
2. Methods
2.1. Sample
The present study used data from a longitudinal study composed of 124 dyads of adolescents (M age = 12.89, SD = 0.79; 52% female) and their primary caregivers (93% mothers) from a catchment area of rural communities in the Southeastern of the United States. The first wave of the study took place before the emergence of the Covid-19 pandemic (January 2018 to early March 2020), and the second wave of data was collected during the Covid-19 pandemic (from May to October 2020), which was explicitly designed to capture participants' experiences of Covid-19 related stress. The sample's racial-ethnic composition was 78.8% European American, 11.5% African American, 3.8% Latino(a), 1.0% Asian/Pacific Islander, and 4.8% Other. Potential participants were excluded if they were not fluent in English or if the child had a significant developmental delay.
2.2. Procedure
The Institutional Review Board approved the present research study at the authors' primary institution. The first wave of data was collected during a visit to participants' homes by the study team members. Primary caregivers and youth were instructed to answer a series of survey questions about their past traumatic experiences, demographics, and sleep behaviors. Due to risks associated with Covid-19, participants completed the second wave of the study online, which consisted of a series of surveys about their experiences, psychological symptoms, and sleep patterns during the pandemic. All members of the research team are mandatory reporters of suspected child abuse and neglect. Primary caregivers gave informed consent, and the youth provided informed assent to participate in the study.
2.3. Measures
2.3.1. Child maltreatment (CM)
The Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998) is a psychometrically validated 28-item self-report inventory used to assess participants' accounts of their experiences of childhood maltreatment (Scher, Stein, Asmundson, McCreary, & Forde, 2001). Participants answered questions using a 5-point Likert scale ranging from “never true” (1) to “very often true” (5) about their experiences across five domains: emotional abuse, emotional neglect, physical abuse, physical neglect, and sexual abuse. A sample question is “I got hit so hard by someone in my family that I had to see a doctor or go to the hospital.” The CTQ scores for all maltreatment subtypes fall into four categories: none to minimal exposure, low to moderate exposure, moderate to severe exposure, and severe to extreme exposure. In the present study, the percentages of low to severe exposure to maltreatment were 11.8% for physical abuse, 18.5% for emotional abuse, 14.2% for emotional neglect, and 13.4% for physical neglect. Sexual abuse (2.4%) was eliminated due to extremely low prevalence. We defined threat and deprivation according to existing literature (McLaughlin et al., 2014). Threat was operationalized as experiences of abusive parenting behaviors that pose a significant risk to a child's physical integrity. Deprivation was defined by experiences of neglect that reflect a child's lack of fundamental physical and emotional care from a caregiver. Therefore, we measured threat using a total score of the emotional and physical abuse subscales (α = 0.70) and deprivation using a total score of emotional and physical neglect subscales (α = 0.70).
2.3.2. Adolescents' sleep problems
Youth's sleep problems (αT1 = 0.72; αT2 = 0.75) were assessed using the Pittsburgh Sleep Quality Index (PSQI, Buysse, Reynolds III, Monk, Berman, & Kupfer, 1989), a widely used self-report instrument that produces a global (i.e., total) sleep quality score consisting of seven component scores (i.e., subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleeping medications, and daytime dysfunction). Scores range from 0 to 21, and a higher global sleep score represents worse sleep quality. Participants with scores of 5 or higher are defined as poor sleepers and refer to those who had severe or moderate sleep problems in at least two or three areas (e.g., sleep quality, sleep duration; Buysse et al., 1989). A sample question is “During the past month, how many hours of actually sleep did you get at night?”
2.3.3. Covid-19 stress
Youth-reported Covid-19 related stress was measured using the Covid-19 Adolescent Symptom & Psychological Experience Questionnaire (Ladouceur, 2020). Three questions assessing youth's negative affect, uncertainty about the future, and stress associated with routine disruptions were used. A sample item includes, “Overall, how much has the Covid-19 outbreak, and the resulting changes to daily life, affected your life in a negative way?” Adolescents rated each item on a 5-point Likert scale (1 = “very slightly or not at all” to 5 = “extremely”). A higher sum score indicated higher Covid-19 related stress. The reliability of these three items was 0.70.
Parent-reported stress during the pandemic outbreak was assessed using the Parent Perceived Stress scale (PSS; Cohen, Kamarck, & Mermelstein, 1983). Three questions that ask parents about their negative affect, levels of stress, and a sense of losing control over important life events during the pandemic were used. A sample item is “In the last month of the Covid-19 outbreak, how often have you felt that you were unable to control the important things in your life?” Parents rated each item on a 5-point Likert scale (0 = “Never” to 5 = “Very Often”). Higher scores indicated higher levels of stress. Reliability for this scale was good (α = 0.79).
2.3.4. Covariates
Youth's gender (0 = male, 1 = female), minority status (European American = 0, ethnic minority = 1), family socioeconomic status (SES), puberty status, and negative affect at T1 were controlled for all analyses. Family annual household income (e.g., 1 ≤ $5000, 2 = $5000 - $10,000) was used as a proxy for family SES. Pubertal status was included as a covariate due to previous evidence suggesting that pubertal maturation may explain gender differences in adolescents' sleep (e.g., Laberge et al., 2001; Zhang et al., 2016). Puberty status was measured using Peterson's Pubertal Development scale (Petersen, Crockett, Richards, & Boxer, 1988). Adolescents rated each item on a 4-point Likert scale (0 = “not yet started”, to 4 = “seems completed”). Lastly, due to the possibility that depressive symptoms may systematically influence the association between stress and sleep quality, Time 1 negative affect was included as a covariate using the Positive Affect and Negative Affect Schedule (Watson, Clark, & Tellegen, 1988).
2.4. Analytic plan
Analyses were performed in Mplus 7.4 (Muthén & Muthén, 2009). Structural equation modeling (SEM) using maximum likelihood estimation was used in all of the modeling procedures. Missing data ranged from 1.6% to 33.1% on all study variables. The missing data pattern was determined as Missing Completely at Random (MCAR) per Little's MCAR test (χ2(127) = 142.27, p = .17). Therefore, a full information maximum likelihood (FIML) model estimator was deemed appropriate for modeling data under MCAR conditions as it produces unbiased parameter estimates (Enders & Bandalos, 2001). Criteria for evaluating model fit were as follows: a maximum value of 0.06 for the root mean square error of approximation (RMSEA) and 0.08 for the standardized root mean squared (SRMR), and a minimum value of 0.90 for the comparative fit index (CFI; Hu & Bentler, 1999).
First, multigroup SEM models were used to test gender difference in the direct effects of threat and deprivation on the change in sleep problems prior to and during the pandemic, which was examined using Latent Change Score Modeling (McArdle & Hamagami, 2001). Next, we examined whether Covid-19 related stress differentially moderated the associations between CM dimensions and sleep problems among boys and girls in separate multigroup models. Due to our limited sample size, we did not apply the Latent Change Score Modeling on sleep problems in the multigroup interaction models (i.e., three-way interaction). Control variables included minority status, family SES, puberty status, negative affect, and sleep problems at T1. Non-significant covariates were trimmed from the analyses. Last, simple slopes (Aiken, West, & Reno, 1991; Dawson, 2014) and Johnson-Neyman plots were generated to probe significant interaction effects (Johnson & Neyman, 1936).
3. Results
3.1. Preliminary analyses
Descriptive statistics and bivariate correlations among study variables are presented in Table 1 . Poor sleep was reported by 32% of youth at T1 and 39.8% of youth at T2 (PSQI global score ≥ 5). Threat was positively associated with sleep problems at T1 (r = 0.23, p < .05), but not at T2. Deprivation was positively linked to sleep problems at both T1 (r = 0.31, p < .01) and T2 (r = 0.23, p < .05). (See Table 2.)
Table 1.
Descriptive statistics and bivariate correlations among study variables (N = 124).
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1.Threat T1 | – | ||||||||||
| 2. Deprivation T1 | 0.47⁎⁎ | – | |||||||||
| 3. Sleep problems T1 | 0.23⁎ | 0.32⁎⁎ | – | ||||||||
| 4. Sleep problems T2 | 0.07 | 0.23⁎ | 0.48⁎⁎ | – | |||||||
| 5. Child report Covid stress T2 | −0.02 | 0.01 | 0.20 | 0.44⁎⁎ | – | ||||||
| 6. Parent report Covid stress T2 | 0.12 | 0.23⁎ | 0.08 | 0.22⁎ | −0.02 | – | |||||
| 7. Negative affect T1 | 0.32⁎⁎ | 0.21⁎ | 0.54⁎⁎ | 0.32⁎⁎ | 0.21 | 0.09 | – | ||||
| 8. Puberty status T1 | 0.06 | 0.19⁎ | 0.24⁎ | −0.08 | 0.02 | −0.10 | 0.18 | – | |||
| 9. Age | 0.11 | 0.23⁎ | 0.11 | −0.11 | 0.04 | −0.04 | 0.01 | 0.37⁎⁎ | – | ||
| 10. Minority status | −0.18⁎ | −0.16 | −0.05 | 0.00 | 0.01 | −0.12 | −0.09 | −0.05 | −0.12 | – | |
| 11. Family income | −0.02 | −0.05 | −0.27⁎ | −0.07 | −0.01 | 0.15 | 0.03 | 0.05 | 0.03 | −0.43⁎⁎ | – |
| M | 12.66 | 13.14 | 5.16 | 5.07 | 7.02 | 5.52 | 17.36 | 8.20 | 12.90 | 0.24 | 65.69 |
| SD | 3.27 | 3.89 | 3.32 | 3.46 | 2.08 | 2.48 | 6.65 | 1.70 | 0.80 | 0.43 | 30.70 |
Notes. Minority status coded as 0 = European American, 1 = race-ethnic minority; gender coded as 0 = male, 1 = female. T1 = Time-point 1; T2 = Time-point 2; Threat = physical abuse + emotional abuse; Deprivation = physical neglect + emotional neglect.
p < .05.
p < .01.
Table 2.
SEM models of the associations between child maltreatment, Covid-19 Stress, and sleep problems (N = 124).
| Structural equation models | B (SE) | β | B [95% CI] | R2 |
|---|---|---|---|---|
| Direct effects (boys) | ||||
| Threat→sleep problemsa | −0.09(0.09) | −0.08 | [−0.27, 0.10] | 0.28 |
| Deprivation→sleep problemsa | 0.32(0.12) | 0.27 | [0.08, 0.56]⁎⁎ | 0.22 |
| Boys interaction effects (INT) | ||||
| INT(threat×Covid-C) → sleep problemsb | 0.21(0.05) | 0.49 | [0.13, 0.28]⁎⁎⁎ | 0.52⁎⁎ |
| INT(deprivation×Covid-C) → sleep problemsc | 0.15(0.04) | 0.38 | [0.25, 0.68]⁎⁎⁎ | 0.54⁎⁎⁎ |
| INT(threat×Covid-P) → sleep problemsd | 0.21(0.09) | 0.41 | [0.07, 0.35]⁎ | 0.42⁎⁎⁎ |
| INT(deprivation×Covid-P) → sleep problemse | 0.15(0.07) | 0.39 | [0.04, 0.25]⁎ | 0.43⁎⁎⁎ |
| Direct effects (girls) | ||||
| Threat→sleep problemsa | 0.05(0.09) | 0.05 | [−0.14, 0.23] | 0.28 |
| Deprivation→sleep problemsa | −0.10(0.08) | −0.13 | [−0.26, 0.07] | 0.22 |
| Girls interaction effects (INT) | ||||
| INT(threat×Covid-C) → sleep problemsb | 0.02(0.10) | 0.03 | [−0.14, 0.18] | 0.31⁎⁎ |
| INT(deprivation×Covid-C) → sleep problemsc | 0.44(0.27) | 0.03 | [−0.11, 0.14] | 0.36⁎⁎ |
| INT(threat×Covid-P) → sleep problemsd | −0.09(0.05) | −0.34 | [−0.16, −0.01] | 0.34⁎ |
| INT(deprivation×Covid-P) → sleep problemse | −0.06(0.05) | −0.21 | [−0.13, 0.02] | 0.34⁎ |
Notes.a χ2(2) = 1.75, p = .42, CFI = 1.00, RMSEA = 0.00, SRMR = 0.04; Models b, c, d, e were all saturated. Covid-C = Child report of Covid-19 related stress; Covid-P = Parent report of Covid-19 related stress; INT = interaction.
p < .05.
p < .01.
p < .001.
3.2. Structural equation modeling
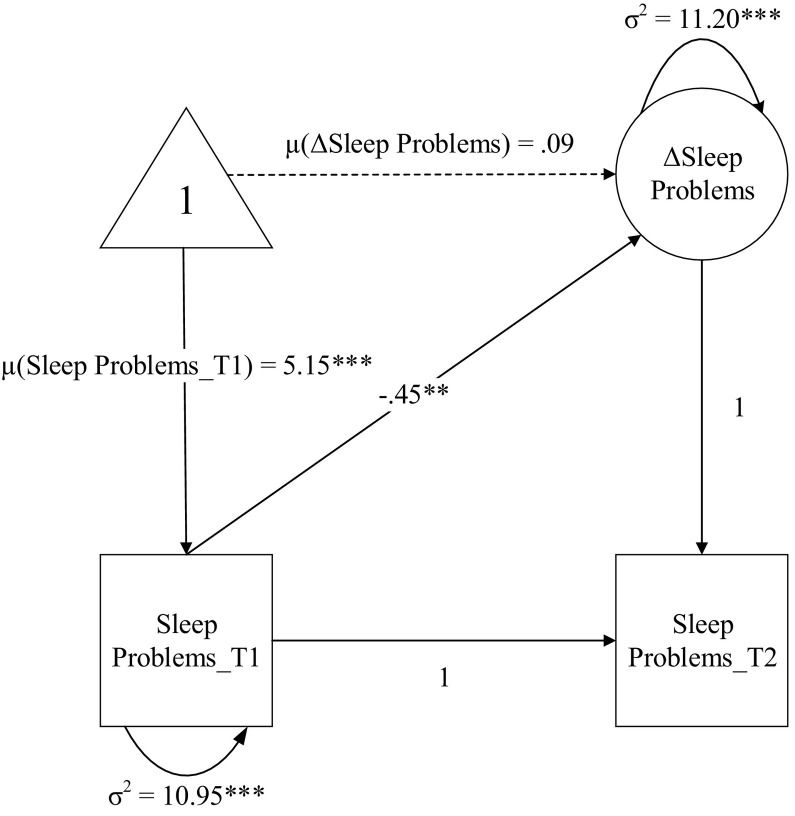
The latent change score model showed that youth's sleep problems increased from baseline (T1) to follow-up (T2) data collected during the pandemic, though this increase was not statistically significant (mean of ΔSleep Problems = 0.09; See Fig. 1 ). Multigroup analyses showed that gender significantly moderated the direct effects of deprivation on youth's sleep problems (Δχ2(1) = 17.23, p < .001), such that deprivation was significantly associated with increased sleep problems at T2 among boys (β = 0.27, p < .01), but not among girls (β = −0.13, p = .29). Threat was not directly associated with sleep problems among boys (β = −0.08, p = .38) or girls (β = 0.05, p = .64).
Fig. 1.
Univariate latent change score model of youth's sleep problems.
Notes. Unstandardized parameters are presented. T1 = Time 1, T2 = Time 2.
Next, we investigated whether child and parent reports of Covid-19 related stress significantly moderated the associations between CM (threat vs. deprivation) and sleep problems and whether the moderating effects differed significantly for boys and girls. Multigroup analyses using Chi-square tests showed that child report of Covid-19 related stress differentially moderated the effects of threat (Δχ 2(1) = 12.34, p < .001) and deprivation (Δχ2(1) = 7.37, p < .01) on sleep problems across gender groups. For boys, Covid-19 related stress significantly intensified the link between threat and sleep problems (β =0.49, p < .001) as well as the link between deprivation and sleep problems (β =0.38, p < .001) at T2. However, among girls, Covid-19 related stress did not significantly impact the links between threat (β = 0.03, p = .86) or deprivation (β =0.03, p = .85) on sleep problems at T2.
Similarly, chi-square tests showed that parents' perception of Covid-19 associated stress moderated the effects of threat (Δχ2(1) = 8.73, p < .05) and deprivation (Δχ 2(1) = 6.23, p < .05) on youth's sleep problems differently across gender groups. For boys, parents' experience of Covid-19 related stress significantly exacerbated the links between threat and sleep problems (β = 0.41, p < .05) as well as between deprivation and sleep problems (β = 0.39, p < .05) at T2. However, parents' experience of Covid-19 related stress did not significantly moderate the effects of threat (β = −0.34, p = .06) or deprivation (β = −0.21, p = .21) on sleep problems at T2 for girls.
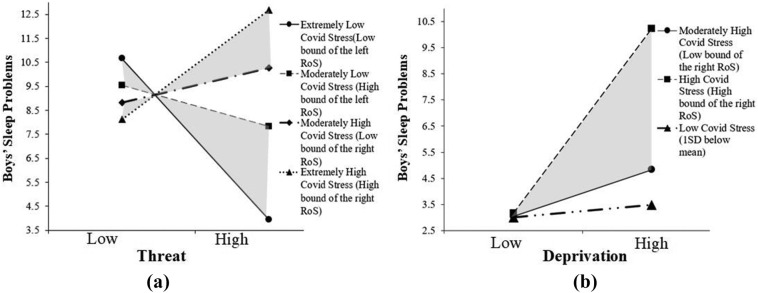
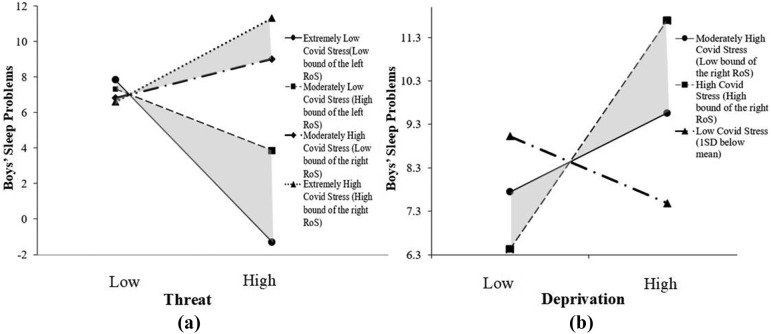
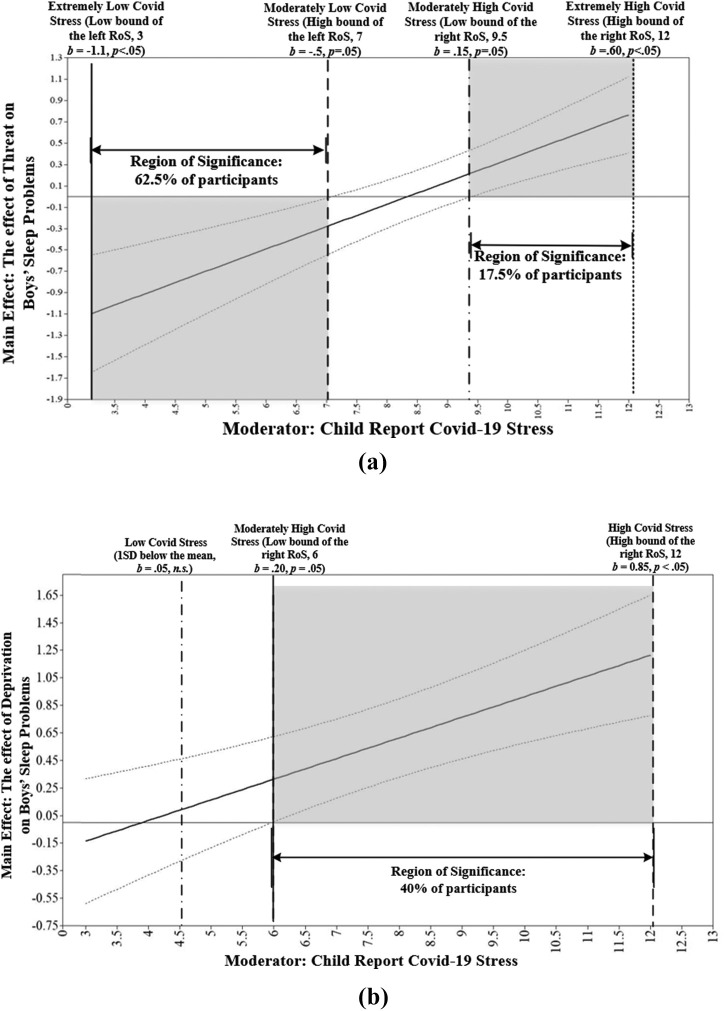
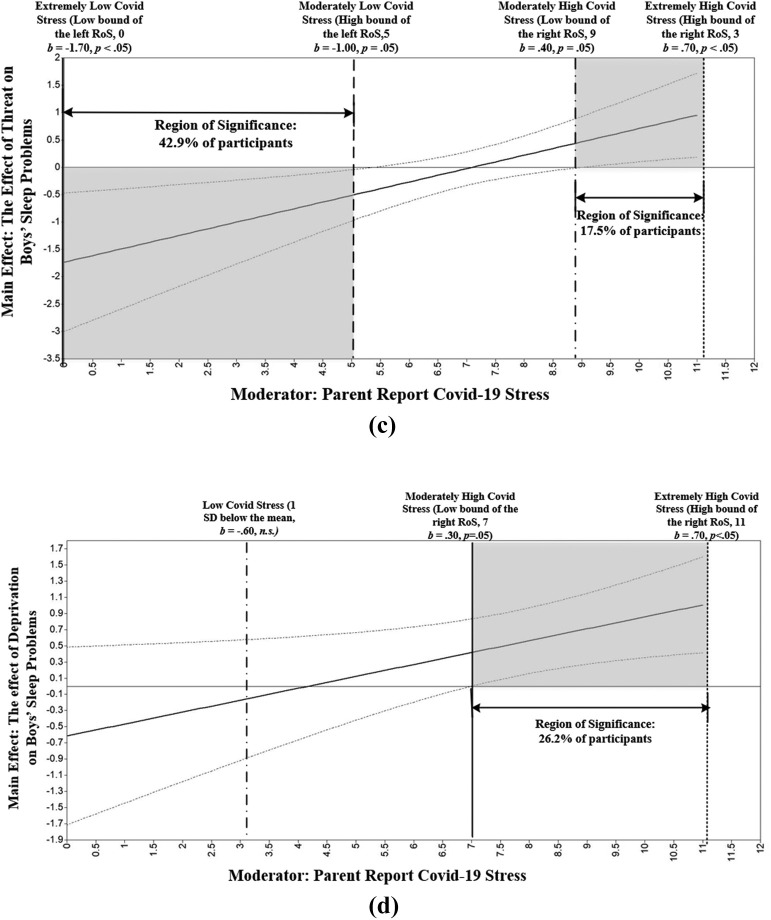
To probe the interaction effects, we used the simple slope method (see Fig. 2, Fig. 3 ; Dawson, 2014) and the Johnson-Neyman technique (Johnson & Neyman, 1936). Fig. 2a & b illustrate that, in the context of increased CM (threat and deprivation), boys who experienced higher levels of Covid-19 related stress (1SD above the mean) exhibited more sleep problems than those who experienced low levels of Covid-19 related stress (1SD below the mean). We identified comparable patterns of interactions in Fig. 3a & b (parent report of perceived Covid-19 stress). Accordingly, when experiencing increased threat and deprivation, boys with parents who had higher levels of Covid-19 stress (1SD above the mean) exhibited more sleep problems.
Fig. 2.
Moderation effect of Covid-19 related stress (child report) on the association between child maltreatment (threat vs deprivation) and boys' sleep problems.
Fig. 3.
Moderation effect of Covid-19 related stress (parent report) on the association between child maltreatment (threat vs deprivation) and boys' sleep problems.
In Johnson-Neyman plots (see Fig. 4a–d), the x-axis represents child and parent report of Covid-19 stress. The y-axis represents the unstandardized coefficient of the effects of CM (threat and deprivation) on youth's sleep problems. The shaded areas reflect regions of significance (RoS) for the moderating effects. According to Fig. 4a, with the increase in child report of Covid-19 stress, the left RoS (62.5% participants) indicated that the negative associations between threat and boys' sleep problems decreased and the right RoS (17.5% participants) showed that the effect of threat on boys' sleep problems increased. In Fig. 4b, with increases in child report of Covid-19 stress, the RoS (40.0% of participants) showed that the effect of deprivation on change in boys' sleep problems increased. Similarly, according to Fig. 4c, with the increase in parent report of Covid-19 stress, the left RoS (42.9% participants) showed that the negative association between threat and boys' sleep problems decreased, and the right RoS (17.5% participants) indicated that the effect of threat on boys' sleep problems increased. Lastly, in Fig. 4d, as Covid-19 stress, reported by the parents increased, the RoS (26.2% of participants) showed that the effect of deprivation on boys' sleep problems increased. Overall, our analyses suggested that Covid-19 related stress, as reported by parents and youth, exacerbated the links between both threat and deprivation types of CM on sleep problems for boys.
Fig. 4.
The exacerbating effect of child and parent report of Covid-19 stress on the links between child maltreatment (threat vs deprivation) and boys' sleep problems.
4. Discussion
The Covid-19 pandemic has disrupted the lives of millions of adolescents and their families (Altena et al., 2020; Magson et al., 2021). Shelter-in-Place orders restricted families and youth to staying home to reduce social gathering and contact. Youth who are socially isolated (Magson et al., 2021), stressed about changes in daily routines, and uncertain about the future (Altena et al., 2020) are consequently at an increased risk for psychological disorders and sleep problems (Imran et al., 2020; Zhao, Lan, Li, & Yang, 2020). However, little is known regarding the impact of pandemic-related stress on sleep patterns among adolescents with experiences of adverse parenting. Based on a longitudinal design, the present study documented the effects of multidimensional CM (threat and deprivation) on youth's sleep problems measured before and during the pandemic context. Our findings demonstrated that, among boys, deprivation but not threat, directly predicted increases in sleep problems during the pandemic. Further, Covid-19 related stress (both parent and child report) significantly intensified the links between threat and deprivation on sleep problems for boys. In contrast, among girls, we did not observe significant direct effects of dimensional CM on sleep problems nor interaction effects of CM and Covid-19 related stress on sleep problems.
In the present investigation, we first sought to expand upon the existing body of knowledge by modeling the effect of CM on sleep using a dimensional approach (i.e., threat and deprivation; McLaughlin et al., 2014). Extant research suggests that adverse parenting, including CM, is linked to sleep problems (Turner et al., 2020; Xiao et al., 2020). However, scarce research examined the relative effects of threat versus deprivation on adolescents' sleep problems over time (Bader et al., 2007). Past research has predominately focused on linking components of threat (e.g., physical abuse, sexual abuse) and sleep patterns in adolescents and adults (Dahl & Lewin, 2002; Noll, Trickett, Susman, & Putnam, 2006; Tashjian & Galván, 2020). Considering the prevalence of child neglect (i.e., most frequent form of maltreatment; Child Trends, 2019), the paucity of data on the effect of depriving types of parenting on sleep problems is a substantial gap in the literature. By modeling threat and deprivation concurrently, our study showed that deprivation, but not threat, was directly linked to an elevation in adolescent boys' sleep problems. Given such a dearth of research on the dimensional effects of CM on adolescents' sleep problems, it would be speculative to determine in this study why depriving parenting was associated with more sleep problems than parenting characterized by threat. Nonetheless, these findings are consistent with research on the negative effects of adverse parenting characterized by deprivation on youth well-being and mental health. A large body of research suggests that depriving parenting is associated with a wide range of bio-regulatory risks (Doom et al., 2020; Reilly & Gunnar, 2019; White et al., 2017). Similarly, in support of the present findings, some studies suggest that depriving parenting is developmentally more detrimental for youth development (Dubowitz, Papas, Black, & Starr, 2002; Eckenrode, Laird, & Doris, 1993). Nevertheless, future research needs to explore the differential effects of threat and deprivation and their underlying psychosocial and biological mechanisms leading to sleep disturbances among adolescents.
Our findings partially corroborated the second hypothesis that elevated stress during the pandemic amplified the harmful effects of threat and deprivation on boys' sleep quality. These results are consistent with recent research showing that youth's stress and worries about the pandemic were significantly linked to decreased sleep quality (Zhao et al., 2020) and delayed sleep/wake behaviors (Becker et al., 2021). Exacerbated sleep problems in the context of pandemic stress might result from an accumulation of multiple stressors, leading to toxic and potentially chronic stress. Indeed, the allostatic load model suggests that exposure to repeated and multiple types of stress bears adverse effects on bio-regulatory and psychological functioning (McEwen, 1998). For adolescents already experiencing adversity, the addition of pandemic stress could further tax an already burdened stress-response system, potentiating increased sleep problems.
Further, parental stress during the pandemic was also found to intensify the association between adverse parenting and adolescent boys' sleep problems. This finding is consistent with emerging research that documents linkages between parents' stress and adolescents' sleep problems (El-Sheikh & Kelly, 2017; Hale, Emanuele, & James, 2015). Ecological research on family stress shows that families are embedded in and influenced by cultural and societal stressors, including stress related to Covid-19 (Conger, 2005). Home quarantine considerably increases space density at home, resulting in more time for family members to interact and engage in family conflicts (Rodriguez et al., 2020). In addition, this added stress may have further compromised parents' abilities to provide sufficient care to their children when children need it the most (Masten & Narayan, 2012; Salmon & Bryant, 2002). Overall, findings from our study suggest that elevated stress related to the pandemic, as reported by both parents and youth, are critical contexts to consider when investigating sleep behaviors among adolescents.
The moderating effects of Covid-19 stress on the relations between threat and sleep quality yielded a subtle pattern. Interestingly, in the context of low Covid-19 stress, boys experiencing higher threat levels had fewer sleep problems than those experiencing lower threat levels (see Figs. 2a & 3a). Adolescents' use of sleep to cope with harsh parenting may explain this result (Sadeh & Gruber, 2002; Sadeh, Keinan, & Daon, 2004). For individuals exposed to low levels of pandemic stress, it is possible that those who also experienced harsh parenting were motivated to retreat and withdraw from the stress of interacting with their parents by resorting to prolonged and deepened sleep (Sadeh & Gruber, 2002). Such avoidant coping strategies may be less available in the presence of the pandemic, during which personal space is scarcer in families. Moreover, new forms of stress introduced by the Covid-19 pandemic may overwhelm adolescents' existing coping mechanisms. Our overall results suggest that the pandemic stress exacerbated the negative effect of threat on sleep problems.
Gender differences in the effect of adverse parenting on sleep were consistently observed across the examined models. Specifically, boys' sleep quality was impacted by both dimensions of CM in the context of Covid-19 stress, while no significant associations between parenting and sleep were found for girls. The literature on gender differences in the effects of adversity on sleep quality is not uniform. One study did not find a significant gender difference in maltreated adolescents' sleep patterns (Schneiderman et al., 2018). Other studies show that maltreated girls experience more sleep problems than maltreated boys (Agargun et al., 2003; Xiao et al., 2020). Moreover, Ramsawh, Ancoli-Israel, Sullivan, Hitchcock, and Stein (2011) found a stronger association between CM and subjective sleep quality among adult men. Nonetheless, our results corroborate resilience literature in which, compared to girls, maltreated adolescent boys are more likely to manifest a wide range of mental health and socioemotional vulnerabilities (DuMont et al., 2007; McGloin & Widom, 2001; Oshri et al., 2018). It is possible that the observed gender differences in sleep problems in the present study stem from the unique constellation of pandemic-related stressors on families. Further, research has shown that boys are more reluctant than girls to seek help from friends or professionals due to the stigma associated with mental health issues (Chandra & Minkovitz, 2007). Therefore, the negative consequences of reduced psychosocial support might be amplified by the experience of additional stress during the pandemic among boys. Our results highlight the urgency to develop prevention and intervention programs to provide coping strategies/resources that mitigate family and adolescent stress and attendant sleep problems while considering how this stress might influence boys and girls differently. Future research should also aim to extend these findings by investigating the role of gender in the associations between Covid-19 stress and adolescents' sleep problems.
4.1. Limitations
The current study has several limitations. Although the study obtained valuable data on pandemic-related stress and youth's sleep quality before and during the pandemic, the study's sample size and demographic backgrounds (e.g., 78.8% European American and predominately rural southern United States families) limit our ability to generalize findings to other demographic groups. A larger, more diverse adolescent sample is needed for future research to thoroughly examine the impact of Covid-19 related stress on the association between adverse parenting and sleep problems. Second, despite considerable investigations into the impacts of the Covid-19 pandemic on urbanized areas, less research has examined its impact on rural families in the United States (Mueller et al., 2021). Our research provides preliminary results on how pandemic stress exacerbates the association between CM and rural adolescents' sleep problems. However, further research that considers the unique challenges that rural families face in the context of the pandemic and their impact on youth's sleep patterns is warranted. Third, the use of a retrospective and self-reported measure of CM (CTQ) may have led to underreported maltreatment and recall bias (Martin, Viljoen, Kidd, & Seedat, 2014). Therefore, the actual percentage of CM that participants experienced may be higher than what was reported in the present study. As expected from a low-risk community sample, relatively low rates of severe CM were reported. Despite the low prevalence, we still found significant cross-sectional and longitudinal associations between CM dimensions and sleep problems among youth. This may suggest the susceptibility of sleep behaviors to adverse rearing environments and the profound impact of CM on bio-regulatory outcomes. Future research should continuously investigate the negative impact of CM on sleep among community samples of adolescents.
Fourth, the assessment of adolescents' sleep problems was based on a subjective sleep questionnaire instead of objective measurements of sleep (e.g., actigraphy), which has been shown to capture more comprehensive and reliable sleep patterns (Sadeh, 2011). However, research has shown that the PSQI, used in the present study, has strong reliability and validity (Mollayeva et al., 2016) and is a widely adopted measure in adolescent sleep research (Schneiderman et al., 2018). Fifth, our analysis showed that youth's sleep problems increased from T1 to T2 (proportion of poor sleepers increasing from 32% to 40%); however, this increase was not statistically significant (p = .82). This non-significant change might be due to a large amount of heterogeneity in youth's changes in sleep patterns from T1 to T2 (i.e., some youth might have increased sleep problems, while others might have experienced a decrease in sleep problems), which may undermine the statistical power to detect significant effects. In addition, T2 data were collected at a relatively early stage of the pandemic (May to October 2020); it could be that there was not enough time between T1 and T2 for significant changes in youth's sleep to occur. Therefore, future research should investigate how Covid-19 related stress impacts youth's sleep patterns over more extended time periods. It is plausible that these studies would observe a significant increase in youth's sleep problems as the pandemic continues to influence families. On the other hand, as communities return to pre-pandemic routines, we may see some recovery in sleep qualities (e.g., as restrictions are lifted). However, children most affected by the pandemic and those with continued exposure to CM may not return to normal sleep patterns as readily. Despite the several limitations above, the present study used a longitudinal design with multiple sources of reports and provided crucial preliminary results on adolescents' sleep during the pandemic.
Footnotes
Funding: Support for this work was provided through Award K01DA045219 (PI: Assaf Oshri) by the National Institute on Drug Abuse.
References
- Agargun M.Y., Kara H., Özer Ö.A., Selvi Y., Kiran Ü., Kiran S. Nightmares and dissociative experiences: The key role of childhood traumatic events. Psychiatry and Clinical Neurosciences. 2003;57(2):139–145. doi: 10.1046/j.1440-1819.2003.01093.x. [DOI] [PubMed] [Google Scholar]
- Aiken L.S., West S.G., Reno R.R. Sage; New York: 1991. Multiple regression: Testing and interpreting interactions. [Google Scholar]
- Altena E., Baglioni C., Espie C.A., Ellis J., Gavriloff D., Holzinger B.…Riemann D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. Journal of Sleep Research. 2020;29(4) doi: 10.1111/jsr.13052. [DOI] [PubMed] [Google Scholar]
- Bader K., Schäfer V., Schenkel M., Nissen L., Schwander J. Adverse childhood experiences associated with sleep in primary insomnia. Journal of Sleep Research. 2007;16(3):285–296. doi: 10.1111/j.1365-2869.2007.00608.x. [DOI] [PubMed] [Google Scholar]
- Becker S.P., Dvorsky M.R., Breaux R., Cusick C.N., Taylor K.P., Langberg J.M. Prospective examination of adolescent sleep patterns and behaviors before and during COVID-19. Sleep. 2021;44(8) doi: 10.1093/sleep/zsab054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein D.P., Fink L. The Psychological Cooperation; San Antonio, TX: 1998. Childhood trauma questionnaire: A retrospective self-report. Manual. [Google Scholar]
- Busso D.S., McLaughlin K.A., Sheridan M.A. Dimensions of adversity, physiological reactivity, and externalizing psychopathology in adolescence: Deprivation and threat. Psychosomatic Medicine. 2017;79(2):162–171. doi: 10.1097/PSY.0000000000000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buysse D.J., Reynolds C.F., III, Monk T.H., Berman S.R., Kupfer D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Campbell O.L.K., Bann D., Patalay P. The gender gap in adolescent mental health: A cross-national investigation of 566,829 adolescents across 73 countries. SSM - Population Health. 2021;13:100742. doi: 10.1016/j.ssmph.2021.100742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra A., Minkovitz C.S. Factors that influence mental health stigma among 8th grade adolescents. Journal of Youth and Adolescence. 2007;36(6):763–774. doi: 10.1007/s10964-006-9091-0. [DOI] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- Conger R.D. Center for Public Policy Research, University of California, Davis; Davis: 2005. The effects of poverty and economic hardship across generations. [Google Scholar]
- Conley C.S., Rudolph K.D. The emerging sex difference in adolescent depression: Interacting contributions of puberty and peer stress. Development and Psychopathology. 2009;21(2):593–620. doi: 10.1017/S0954579409000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahl R.E., Lewin D.S. Pathways to adolescent health sleep regulation and behavior. Journal of Adolescent Health. 2002;31(6):175–184. doi: 10.1016/S1054-139X(02)00506-2. [DOI] [PubMed] [Google Scholar]
- Dalton L., Rapa E., Stein A. Protecting the psychological health of children through effective communication about COVID-19. The Lancet Child & Adolescent Health. 2020;4(5):346–347. doi: 10.1016/S2352-4642(20)30097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson J.F. Moderation in management research: What, why, when, and how. Journal of Business and Psychology. 2014;29(1):1–19. doi: 10.1007/s10869-013-9308-7. [DOI] [Google Scholar]
- Doom J.R., Peckins M.K., Hein T.C., Dotterer H.L., Mitchell C., Lopez-Duran N.L.…Abelson J.L. Differential associations of parental harshness and parental disengagement with overall cortisol output at 15 years: Implications for adolescent mental health. Development and Psychopathology. 2020;19:1–8. doi: 10.1017/S0954579420000954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dubowitz H., Papas M.A., Black M.M., Starr R.H. Child neglect: Outcomes in high-risk urban preschoolers. Pediatrics. 2002;109(6):1100–1107. doi: 10.1542/peds.109.6.1100. [DOI] [PubMed] [Google Scholar]
- DuMont K.A., Widom C.S., Czaja S.J. Predictors of resilience in abused and neglected children grown-up: The role of individual and neighborhood characteristics. Child Abuse & Neglect. 2007;31(3):255–274. doi: 10.1016/j.chiabu.2005.11.015. [DOI] [PubMed] [Google Scholar]
- Eckenrode J., Laird M., Doris J. School performance and disciplinary problems among abused and neglected children. Developmental Psychology. 1993;29(1):53–62. doi: 10.1037/0012-1649.29.1.53. [DOI] [Google Scholar]
- Ellis W.E., Dumas T.M., Forbes L.M. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioural Science. 2020;52(3):177–187. doi: 10.1037/cbs0000215. [DOI] [Google Scholar]
- El-Sheikh M., Kelly R.J. Family functioning and children’s sleep. Child Development Perspectives. 2017;11(4):264–269. doi: 10.1111/cdep.12243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enders C.K., Bandalos D.L. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8:430–457. [PubMed] [Google Scholar]
- Freisthler B., Holmes M.R., Wolf J.P. The dark side of social support: Understanding the role of social support, drinking behaviors and alcohol outlets for child physical abuse. Child Abuse & Neglect. 2014;38(6):1106–1119. doi: 10.1016/j.chiabu.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golberstein E., Wen H., Miller B.F. Coronavirus disease 2019 (COVID-19) and mental health for children and adolescents. JAMA Pediatrics. 2020;174(9):819–820. doi: 10.1001/jamapediatrics.2020.1456. [DOI] [PubMed] [Google Scholar]
- Griffith A.K. Parental burnout and child maltreatment during the COVID-19 pandemic. Journal of Family Violence. 2020:1–7. doi: 10.1007/s10896-020-00172-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guessoum S.B., Lachal J., Radjack R., Carretier E., Minassian S., Benoit L., Moro M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Research. 2020;291:113264. doi: 10.1016/j.psychres.2020.113264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L., Emanuele E., James S. Recent updates in the social and environmental determinants of sleep health. Current Sleep Medicine Reports. 2015;1(4):212–217. doi: 10.1007/s40675-015-0023-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honein M.A., Christie A., Rose D.A., Brooks J.T., Meaney-Delman D., Cohn A., Sauber-Schatz E.K., Walker A., McDonald L.C., Liburd L.C., Hall J.E., Fry A.M., Hall A.J., Gupta N., Kuhnert W.L., Yoon P.W., Gundlapalli A.V., Beach M.J., Walke H.T., CDC COVID-19 Response Team Summary of Guidance for Public Health Strategies to Address High Levels of Community Transmission of SARS-CoV-2 and Related Deaths, December 2020. MMWR. Morbidity and mortality weekly report. 2020;69(49):1860–1867. doi: 10.15585/mmwr.mm6949e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L.t., Bentler P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Humphreys K.L., Salo V.C. Expectable environments in early life. Current Opinion in Behavioral Sciences. 2020;36:115–119. doi: 10.1016/j.cobeha.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imran N., Zeshan M., Pervaiz Z. Mental health considerations for children & adolescents in COVID-19 pandemic. Pakistan Journal of Medical Sciences. 2020;36 doi: 10.12669/pjms.36.COVID19-S4.2759. S-1-S-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson P.O., Neyman J. Tests of certain linear hypotheses and their application to some educational problems. Statistical research memoirs. 1936;1:57–93. [Google Scholar]
- Laberge L., Petit D., Simard C., Vitaro F., Tremblay R.E., Montplaisir J. Development of sleep patterns in early adolescence. Journal of Sleep Research. 2001;10(1):59–67. doi: 10.1046/j.1365-2869.2001.00242.x. [DOI] [PubMed] [Google Scholar]
- Ladouceur C. Author; Pittsburgh, PA: 2020. COVID-19 adolescent symptom and psychological experience questionnaire (CASPE) [Google Scholar]
- Liu S., Fisher P.A. Early experience unpredictability in child development as a model for understanding the impact of the COVID-19 pandemic: A translational neuroscience perspective. Developmental Cognitive Neuroscience. 2021 doi: 10.1016/j.dcn.2022.101091. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson N.R., Freeman J.Y.A., Rapee R.M., Richardson C.E., Oar E.L., Fardouly J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. Journal of Youth and Adolescence. 2021;50(1):44–57. doi: 10.1007/s10964-020-01332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manly J.T. Advances in research definitions of child maltreatment. Child Abuse & Neglect. 2005;29(5):425–439. doi: 10.1016/j.chiabu.2005.04.001. [DOI] [PubMed] [Google Scholar]
- Martin L., Viljoen M., Kidd M., Seedat S. Are childhood trauma exposures predictive of anxiety sensitivity in school attending youth? Journal of Affective Disorders. 2014;168:5–12. doi: 10.1016/j.jad.2014.06.035. [DOI] [PubMed] [Google Scholar]
- Masten A.S., Narayan A.J. Child development in the context of disaster, war, and terrorism: Pathways of risk and resilience. Annual Review of Psychology. 2012;63:227–257. doi: 10.1146/annurev-psych-120710-100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle J.J., Hamagami F. In: New methods for the analysis of change (pp. 139–175) Collins L.M., Sayer A.G., editors. American Psychological Association; 2001. Latent difference score structural models for linear dynamic analyses with incomplete longitudinal data. [DOI] [Google Scholar]
- McEwen B.S. Stress, adaptation, and disease: Allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840(1):33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McGloin J.M., Widom C.S. Resilience among abused and neglected children grown up. Development and Psychopathology. 2001;13(4):1021–1038. doi: 10.1017/S095457940100414X. [DOI] [PubMed] [Google Scholar]
- McLaughlin K.A., Sheridan M.A. Beyond cumulative risk: A dimensional approach to childhood adversity. Current Directions in Psychological Science. 2016;25(4):239–245. doi: 10.1177/0963721416655883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin K.A., Sheridan M.A., Lambert H.K. Childhood adversity and neural development: Deprivation and threat as distinct dimensions of early experience. Neuroscience and Biobehavioral Reviews. 2014;47:578–591. doi: 10.1016/j.neubiorev.2014.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin K.A., Weissman D., Bitrán D. Childhood adversity and neural development: A systematic review. Annual Review of Developmental Psychology. 2019;1:277–312. doi: 10.1146/annurev-devpsych-121318-084950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPhie M.L., Weiss J.A., Wekerle C. Psychological distress as a mediator of the relationship between childhood maltreatment and sleep quality in adolescence: Results from the Maltreatment and Adolescent Pathways (MAP) Longitudinal Study. Child Abuse & Neglect. 2014;38(12):2044–2052. doi: 10.1016/j.chiabu.2014.07.009. [DOI] [PubMed] [Google Scholar]
- Miller A.B., Sheridan M.A., Hanson J.L., McLaughlin K.A., Bates J.E., Lansford J.E.…Dodge K.A. Dimensions of deprivation and threat, psychopathology, and potential mediators: A multi-year longitudinal analysis. Journal of Abnormal Psychology. 2018;127(2):160–170. doi: 10.1037/abn0000331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills R., Scott J., Alati R., O’Callaghan M., Najman J.M., Strathearn L. Child maltreatment and adolescent mental health problems in a large birth cohort. Child Abuse & Neglect. 2013;37(5):292–302. doi: 10.1016/j.chiabu.2012.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollayeva T., Thurairajah P., Burton K., Mollayeva S., Shapiro C.M., Colantonio A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Medicine Reviews. 2016;25:52–73. doi: 10.1016/j.smrv.2015.01.009. [DOI] [PubMed] [Google Scholar]
- Mueller J.T., McConnell K., Burow P.B., Pofahl K., Merdjanoff A.A., Farrell J. Impacts of the COVID-19 pandemic on rural America. Proceedings of the National Academy of Sciences. 2021;118(1) doi: 10.1073/pnas.2019378118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L., Muthén B. Muthén & Muthén; Los Angeles, CA: 2009. Mplus. Statistical analysis with latent variables. User's guide, 7. [Google Scholar]
- Noll J.G., Trickett P.K., Susman E.J., Putnam F.W. Sleep disturbances and childhood sexual abuse. Journal of Pediatric Psychology. 2006;31(5):469–480. doi: 10.1093/jpepsy/jsj040. [DOI] [PubMed] [Google Scholar]
- Oshri A., Duprey E.B., Kogan S.M., Carlson M.W., Liu S. Growth patterns of future orientation among maltreated youth: A prospective examination of the emergence of resilience. Developmental Psychology. 2018;54(8):1456–1471. doi: 10.1037/dev0000528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshri A., Kogan S., Liu S., Sweet L., Mackillop J. Pathways linking adverse childhood experiences to cigarette smoking among young black men: A prospective analysis of the role of sleep problems and delayed reward discounting. Annals of Behavioral Medicine. 2017;51(6):890–898. doi: 10.1007/s12160-017-9914-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshri A., Sutton T.E., Clay-Warner J., Miller J.D. Child maltreatment types and risk behaviors: Associations with attachment style and emotion regulation dimensions. Personality and Individual Differences. 2015;73:127–133. doi: 10.1016/j.paid.2014.09.015. [DOI] [Google Scholar]
- Pasch K.E., Laska M.N., Lytle L.A., Moe S.G. Adolescent sleep, risk behaviors, and depressive symptoms: Are they linked? American Journal of Health Behavior. 2010;34(2):237–248. doi: 10.5993/AJHB.34.2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters D.J. Community susceptibility and resiliency to COVID-19 across the rural-urban continuum in the United States. The Journal of Rural Health. 2020;36(3):446–456. doi: 10.1111/jrh.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen A.C., Crockett L., Richards M., Boxer A. A self-report measure of pubertal status: Reliability, validity, and initial norms. Journal of Youth and Adolescence. 1988;17(2):117–133. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Poon C.Y., Knight B.G. Impact of childhood parental abuse and neglect on sleep problems in old age. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2011;66(3):307–310. doi: 10.1093/geronb/gbr003. [DOI] [PubMed] [Google Scholar]
- Ramsawh H.J., Ancoli-Israel S., Sullivan S.G., Hitchcock C.A., Stein M.B. Neuroticism mediates the relationship between childhood adversity and adult sleep quality. Behavioral Sleep Medicine. 2011;9(3):130–143. doi: 10.1080/15402002.2011.583895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly E.B., Gunnar M.R. Neglect, HPA axis reactivity, and development. International Journal of Developmental Neuroscience. 2019;78:100–108. doi: 10.1016/j.ijdevneu.2019.07.010. [DOI] [PubMed] [Google Scholar]
- Rodriguez C.M., Lee S.J., Ward K.P., Pu D.F. The perfect storm: Hidden risk of child maltreatment during the Covid-19 pandemic. Child Maltreatment. 2020;26(2):139–151. doi: 10.1177/1077559520982066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez C.M., Tucker M.C. Predicting maternal physical child abuse risk beyond distress and social support: Additive role of cognitive processes. Journal of Child and Family Studies. 2015;24(6):1780–1790. doi: 10.1007/s10826-014-9981-9. [DOI] [Google Scholar]
- Sadeh A. The role and validity of actigraphy in sleep medicine: An update. Sleep Medicine Reviews. 2011;15(4):259–267. doi: 10.1016/j.smrv.2010.10.001. [DOI] [PubMed] [Google Scholar]
- Sadeh A., Gruber R. In: Adolescent sleep patterns: Biological, social, and psychological influences. (pp. 236–253) Carskadon M.A., editor. Cambridge University Press; 2002. Stress and sleep in adolescence: A clinical-developmental perspective. [DOI] [Google Scholar]
- Sadeh A., Keinan G., Daon K. Effects of stress on sleep: The moderating role of coping style. Health Psychology. 2004;23(5):542–545. doi: 10.1037/0278-6133.23.5.542. [DOI] [PubMed] [Google Scholar]
- Salmon K., Bryant R.A. Posttraumatic stress disorder in children: The influence of developmental factors. Clinical Psychology Review. 2002;22(2):163–188. doi: 10.1016/S0272-7358(01)00086-1. [DOI] [PubMed] [Google Scholar]
- Sasser J., Oshri A., Duprey E.B., Doane L.D., Peltz J.S. Daytime sleepiness underlies the link between adverse parenting and youth psychopathology among adolescent girls. Journal of Adolescence. 2021;90:32–44. doi: 10.1016/j.adolescence.2021.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scher C.D., Stein M.B., Asmundson G.J., McCreary D.R., Forde D.R. The childhood trauma questionnaire in a community sample: Psychometric properties and normative data. Journal of Traumatic Stress. 2001;14(4):843–857. doi: 10.1023/A:1013058625719. [DOI] [PubMed] [Google Scholar]
- Schneiderman J.U., Ji J., Susman E.J., Negriff S. Longitudinal relationship between mental health symptoms and sleep disturbances and duration in maltreated and comparison adolescents. Journal of Adolescent Health. 2018;63(1):74–80. doi: 10.1016/j.jadohealth.2018.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedlak A.J., Mettenburg J., Basena M., Peta I., McPherson K., Greene A. Fourth national incidence study of child abuse and neglect (NIS-4) Washington, DC: US Department of Health and Human Services. 2010;9:2010. [Google Scholar]
- Semsar N., Mousavi Z., Tran M.-L.M., Kuhlman K.R. Dysregulated arousal as a pathway linking childhood neglect and clinical sleep disturbances in adulthood. Child Abuse & Neglect. 2021;122:105306. doi: 10.1016/j.chiabu.2021.105306. [DOI] [PubMed] [Google Scholar]
- Singh S., Roy M.D., Sinha C.P.T.M.K., Parveen C.P.T.M.S., Sharma C.P.T.G., Joshi C.P.T.G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Research. 2020;293:113429. doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sivertsen B., Harvey A.G., Lundervold A.J., Hysing M. Sleep problems and depression in adolescence: Results from a large population-based study of Norwegian adolescents aged 16–18 years. European Child & Adolescent Psychiatry. 2014;23(8):681–689. doi: 10.1007/s00787-013-0502-y. [DOI] [PubMed] [Google Scholar]
- Tashjian S.M., Galván A. Neural recruitment related to threat perception differs as a function of adolescent sleep. Developmental Science. 2020;23(5) doi: 10.1111/desc.12933. [DOI] [PubMed] [Google Scholar]
- Tinajero R., Williams P.G., Cribbet M.R., Rau H.K., Silver M.A., Bride D.L., Suchy Y. Reported history of childhood trauma and stress-related vulnerability: Associations with emotion regulation, executive functioning, daily hassles and pre-sleep arousal. Stress and Health. 2020;36(4):405–418. doi: 10.1002/smi.2938. [DOI] [PubMed] [Google Scholar]
- Trends C. 2019. Child maltreatment.https://www.childtrends.org/indicators/childmaltreatment Avaiable from: [Google Scholar]
- Tsai K.M., Dahl R.E., Irwin M.R., Bower J.E., McCreath H., Seeman T.E.…Fuligni A.J. The roles of parental support and family stress in adolescent sleep. Child Development. 2018;89(5):1577–1588. doi: 10.1111/cdev.12917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner S., Menzies C., Fortier J., Garces I., Struck S., Taillieu T.…Afifi T.O. Child maltreatment and sleep problems among adolescents in Ontario: A cross sectional study. Child Abuse & Neglect. 2020;99:104309. doi: 10.1016/j.chiabu.2019.104309. [DOI] [PubMed] [Google Scholar]
- Watson D., Clark L.A., Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- White L.O., Ising M., von Klitzing K., Sierau S., Michel A., Klein A.M.…Müller-Myhsok B. Reduced hair cortisol after maltreatment mediates externalizing symptoms in middle childhood and adolescence. Journal of Child Psychology and Psychiatry. 2017;58(9):998–1007. doi: 10.1111/jcpp.12700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao D., Wang T., Huang Y., Wang W., Zhao M., Zhang W.-H.…Lu C. Gender differences in the associations between types of childhood maltreatment and sleep disturbance among Chinese adolescents. Journal of Affective Disorders. 2020;265:595–602. doi: 10.1016/j.jad.2019.11.099. [DOI] [PubMed] [Google Scholar]
- Zhang J., Chan N.Y., Lam S.P., Li S.X., Liu Y., Chan J.W.Y.…Wing Y.-K. Emergence of sex differences in insomnia symptoms in adolescents: A large-scale school-based study. Sleep: Journal of Sleep and Sleep Disorders Research. 2016;39(8):1563–1570. doi: 10.5665/sleep.6022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X., Lan M., Li H., Yang J. Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: A moderated mediation model. Sleep Medicine. 2020;77:339–345. doi: 10.1016/j.sleep.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou S.-J., Wang L.-L., Yang R., Yang X.-J., Zhang L.-G., Guo Z.-C., Chen J.-C., Wang J.-Q., Chen J.-X. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Medicine. 2020;74:39–47. doi: 10.1016/j.sleep.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]