Abstract
Introduction.
Subjective ratings of cannabis effects are important predictors of use-related consequences. However, psychometric research is fairly limited, particularly for measures to capture variability in daily life when diverse modes of cannabis administration and co-substance use are common.
Methods.
This study evaluated the predictive utility of a revised item to assess perceived cannabis effects and examined modes of cannabis administration and alcohol and nicotine co-use as moderators. Participants were 106 young adults (18–25 years; 51% female) who completed up to 14 consecutive daily reports of substance use (n = 1,405 person-days). Two measures of subjective effects were examined: a standard item (0–100 rating of “how high do you feel?”) and a revised item that uses four crowd-sourced anchor points ranging from relaxed (0), calm/chill (33), high (67), and stoned/baked (100). The items shared substantial variance (Pseudo-R2 = 59.5%), however, the revised item showed greater within-person variability (77.0% vs. 68.8%) and stronger day-level associations with consumption levels (Pseudo-R2 = 25.0% vs. 16.7%).
Results.
The cannabis consumption-subjective effects link was weaker on blunt-only days compared to vape-only days. Subjective cannabis effects were higher on nicotine co-use days after controlling for cannabis consumption; neither alcohol nor nicotine co-use moderated the cannabis consumption-subjective effects link.
Discussion.
The revised subjective cannabis effects item is a viable alternative to the standard item among young adults who engage in simultaneous alcohol and cannabis use.
Conclusions.
Future research focused on characterizing the variability in cannabis effects is needed.
Keywords: Cannabis, Marijuana, Subjective Intoxication, Subjective Effects, Daily Diary, Mode of Administration
1.0. Introduction
After alcohol, cannabis is the most widely used regulated substance in the US; 39% of young adults report cannabis use in the past year and 24% in the past 30 days (Schulenberg et al., 2019; Substance Abuse and Mental Health Services Administration, 2019). As cannabis becomes legalized and decriminalized, cannabis and related products (e.g., vape pens) are becoming more accessible and potent, with increasing tetrahydrocannabinol (THC) concentrations (Borodovsky, 2016; Prince and Conner, 2019; Russell et al., 2018; Spindle et al., 2019a). Characterizing individuals’ perceived effects of cannabis in daily life is particularly important to inform interventions (Nahum-Shani et al., 2018), but psychometric research in this area is limited.
Subjective cannabis effects include intoxication (e.g., degree of impairment) and other states, such as feeling “relaxed” and “calm.” Subjective effects are critical for assessing and intervening on cannabis use behaviours. First, young adults predominately use cannabis to achieve a specific psychoactive effect or subjective experience such as relaxing or enhancing the effects of other substances (Brackenbury et al., 2016; Patrick et al., 2019). Second, young adults’ subjective experiences predict subsequent risk behaviour (e.g., co-use, intoxicated driving) more accurately than plasma THC levels and form the basis for interventions increasing self-awareness and decision-making (Aston et al., 2019; Ronen et al., 2010). Capturing variability in subjective cannabis effects in daily life could facilitate development of individualized targets for intervention.
Studies examining subjective feelings of intoxication or impairment after using cannabis have typically used one-item Likert-type sliders, such as, “How high do you feel?” (Bravo, 2017; Cloutier et al., 2021; Hughes et al., 2014; Quinn and Fromme, 2011). While these items are widely used to assess cannabis use and related disorders in the laboratory and in diary and longitudinal studies (Cloutier et al., 2021; Cooper and Haney, 2009; Fischman and Foltin, 1991; Haney et al., 1999), there are a wide range of effects beyond how “high” someone feels, and using more common language may be important among young adults (Linden-Carmichael et al., 2020a; Patrick and Lee, 2018; Watkins et al., 2021). In Linden-Carmichael, Masters et al. (2020), young adult cannabis users across the US were asked to describe how they feel after low, moderate, and heavy cannabis use. A second sample ranked the most commonly used words in order of impairment. Few participants self-generated terms commonly included in research such as “intoxication” or “impairment,” suggesting a disconnect between the language used in daily life and research contexts to describe cannabis use. The term “high” was endorsed by many of the participants (49%), but ranked at moderate impairment levels. This suggested that using “high” as the upper anchor may create a ceiling effect inhibiting distinguishing between moderate and extreme intoxication. To address this, Linden-Carmichael, Masters et al. (2020) constructed a single slider asking participants to rate how they felt after using cannabis, with four evenly spaced anchors from 0 to 100: “relaxed,” “calm/chill,” “high,” and “stoned/baked.” This item appeared to capture greater variability in the cross-sectional, retrospective self-report survey, but examining applications in daily life is key for capturing subtle fluctuations that occur on a shorter timescale (e.g., across use episodes).
Conducting assessments in daily life also enables identification of use-episode characteristics that may moderate the link between cannabis consumption and subjective effects (e.g., mode of cannabis administration; co-using other substances). For example, cross-sectional studies and retrospective surveys suggest that vaporizers may produce stronger, more efficient subjective intoxication and THC blood plasma levels than smoking (Aston et al., 2019; Borodovsky, 2016; Budney et al., 2015; Spindle et al., 2018). This has led to speculation that vaping may increase risk for longer-term problems (Budney et al., 2015; Solowij, 2018). However, a recent daily diary study revealed similar or lower cannabis consumption and intoxication levels on days young adults vaped cannabis relative using pipes, bongs, blunts, or joints (Cloutier et al., 2021). Likewise, when nicotine or alcohol are administered within 20 minutes to 4 hours of administering cannabis in the laboratory (i.e., so the effects of each substance overlaps with the others), plasma THC and subjective cannabis intoxication/effects ratings increase, suggesting simultaneous use increases subjective cannabis effects by enhancing THC absorption (Downey et al., 2013; Lukas and Orozco, 2001; Penetar et al., 2005). Daily diary studies indicate that using alcohol and cannabis on the same day increases overall consequences and subjective intoxication, even when they were not necessarily used simultaneously such that the effects of the substances overlapped, highlighting any co-use as a key risk factor, not just simultaneous use (Sokolovsky et al., 2020). Yet, when assessing substance-specific effects of co-use of cannabis with alcohol or nicotine in daily life, young adults report more alcohol- and nicotine-related effects, but no change in cannabis effects (Linden-Carmichael et al., 2020b; Lipperman-Kreda et al., 2017; Thrul et al., 2021). Extant research suggests that certain modes of cannabis administration and alcohol or nicotine co-use may increase the effects of consumption on subjective cannabis effects in laboratory contexts. Nonetheless, it is unclear whether these moderation effects operate within individuals, where on any given day young adults choose what substances they consume as well as how and how much they consume.
The current study aimed to expand upon initial analysis of the revised, four-anchored (“relaxed,” “calm/chill,” “high,” and “stoned/baked”) cannabis effects item. Building upon results from a cross-sectional study (Linden-Carmichael, Masters, et al., 2020) we conducted a secondary data analysis of a 14-day diary study of young adults who used cannabis (Linden-Carmichael, Van Doren et al., 2020). This study evaluates the validity of the revised item versus a standard assessment of subjective effects (0–100 scale) used to assess subjective cannabis effects in daily life (Aim 1). This study then tests key potential moderators of the association between cannabis consumption and subjective effects, including mode of cannabis administration (Aim 2) and cannabis-alcohol co-use and cannabis-nicotine co-use (Aim 3). Based on prior research, subjective cannabis effects were hypothesized to be highest on days participants reported greater levels of consumption, indicating validity of the revised item. The effects of cannabis consumption level were expected to be moderated by vaporizer use (relative to all other cannabis smoking modes) as well as any alcohol or nicotine co-use (relative to no co-use).
2.0. Material and Methods
2.1. Participants and Procedures
Participants in the original study were 161 young adults recruited for a 14-day daily diary study on simultaneous alcohol and cannabis use (Linden-Carmichael et al., 2020b). Participants were recruited via flyers at the local campus and in the community and postings on the university’s StudyFinder website that advertises research opportunities to local community members. Eligible participants (1) were 18–25 years old, (2) reported past-month simultaneous alcohol and cannabis use, and (3) reported past two-week heavy episodic drinking (4+/5+ drinks in one occasion for females/males). After a brief online screening, eligible participants completed an online survey assessing demographics and baseline substance use, then given instructions for completing daily surveys and were emailed/texted reminders at 9 and 11:30 am to report the prior day’s behaviours. Participants received up to $48 in compensation. Of eligible participants, 95% completed at least one daily survey (Mean=13.13; SD=1.95) surveys (see Linden-Carmichael, Van-Doren et al., 2020). Study procedures were approved by the university’s Institutional Review Board. Data were collected from October 2018 to March 2019 in a state where recreational cannabis use had not been legalized or decriminalized. The analytic sample for this study included 105 participants (47.6% female; Mage=20.30, SDage=1.44, 607 use days) who endorsed at least one cannabis use event during the assessment period. See Table 1 for descriptive statistics.
Table 1.
Participant Demographics and Summary of Alcohol and Cannabis Use
| Variable | |
|---|---|
| Sex (% female) | 47.60 |
| M (SD) Age | 20.30 (1.44) |
| Race/Ethnicity | |
| % NHL White | 69.50 |
| % NHL Asian | 12.20 |
| % NHL Black | 4.61 |
| % NHL Multiracial | 2.80 |
| % Hispanic Only/Hispanic White | 10.82 |
| Cannabis Use | |
| M (SD) Number of Days (out of possible 14) | 5.78 (4.32) |
| M (SD) Number of Hits Per Day | 8.56 (8.10) |
| M (SD) Subjective Intoxication Scale | 42.40 (18.90) |
| M (SD) Subjective Cannabis Effects Scale | 50.10 (21.40) |
| % Vape-Only Days | 24.10 |
| % Bong-Only Days | 30.30 |
| % Blunt-Only Days | 5.77 |
| % Joint-Only Days | 11.20 |
| % Pipe-Only Days | 7.58 |
| % Multimode Days | 21.1 |
| % Cannabis Days with Other Substance Use | |
| % of Alcohol Co-Use Days | 42.20 |
| % of Nicotine Co-Use Days | 27.70 |
| % of Cigarette Co-Use Days | 5.60 |
| % of Vaping Co-Use Days | 24.50 |
Note. N = 607 cannabis use days from 102 participants. NHL = Non-Hispanic/Latinx.
2.2. Daily Measures
2.2.1. Cannabis Use
Participants were asked to check all substances used during the prior day from a comprehensive list. If cannabis use was endorsed, participants indicated all modes used (e.g., bongs, edibles) and the number of hits taken from each. Mode of cannabis administration was recoded to reflect bong only, vape only, joint only, pipe only, blunt only, edible only, other only, and multimode days. The quantity of cannabis consumed (cannabis use) was calculated by summing the number of hits for each mode, with half hits rounded up (e.g., 0.5 was recoded as 1).
2.2.2. Subjective Cannabis Intoxication and Effects
On days when participants endorsed cannabis use, they were asked to rate their subjective intoxication after using cannabis using a standard item (e.g., Bravo et al., 2017; Quinn & Fromme, 2011) and the revised four-anchored item (Linden-Carmichael, Van Doren et al., 2020). For the standard item, participants were asked, “How high did you feel yesterday?” with a visual analog scale slider ranging from 0 (not at all) to 100 (highest I have ever felt). For the four-anchored item, participants were prompted, “Please indicate how you felt after using marijuana yesterday” with another visual analog scale slider with anchors at 0 (Relaxed), 33 (Calm/Chill), 67 (High), and 100 (Stoned/Baked). To ameliorate test-retest effects, participants were asked other questions between these items. Figure S1 shows the sliders participants viewed.
2.2.3. Other Substance Use
Alcohol use days were coded 1 (any use) or 0 (no use). Nicotine use days were coded as 1 (any blunts, combustible cigarettes, hookah, vaping nicotine) and 0 (no use)1. Indicators of specific nicotine products (e.g., combustible cigarettes) were coded as 1 (any use) or 0 (no use).
2.3. Data Analysis
One extreme outlier for number of cannabis hits was winsorized to match the next-highest value. Missing data were minimal (<2% across all person-days) and addressed via pairwise deletion. Edible-only (n=18) and other-only (n=17) days were excluded because they were rarely endorsed and the metric of consumption (number of hits) was not meaningful. In analyses testing the effects of mode of cannabis administration on subjective effects, multimode days (n=128) were excluded because heterogeneity of modes used (26 unique combinations, <20 days per combination) limited meaningful interpretation. Blunts contain nicotine even when tobacco is removed; therefore, days in which cannabis was consumed via blunts (n=73) were also coded as nicotine use days. There was one hookah use person-day; it was included in tests of any nicotine use but not in specific tests of nicotine products.
Multilevel models (MLMs) with random intercepts using restricted maximum likelihood estimation were specified to model subjective cannabis effects as a function of day (Level-1) and person (Level-2). All models were estimated using the lmer() function in the lme4 package (Bates, Mächler, Bolker, & Walker, 2015) in R 4.0.2. All Level-1 variables except the cannabis mode indicator were person-mean centered and all Level-2 variables were grand-mean centered. Aims were addressed by testing the main and interaction effects of day-level cannabis consumption, mode of cannabis administration, and co-substance use on subjective cannabis effects. Specifically, Aim 1 compared the main effects of day- and person- level cannabis consumption on the standard intoxication item and the revised subjective cannabis effects item. Aims 2 and 3 tested whether day-level mode of cannabis administration and co-use moderated the association between cannabis consumption and subjective cannabis effects, assessed with the revised item.
3.0. Results
3.1. Descriptive Statistics and Item Comparisons
Across the 607 person-days on which cannabis was used, participants reported an average of 8.56 hits (SD=8.10). The majority of cannabis use days involved a single mode of administration (n=479; 78.9% of person-days). The mean on the standard intoxication item was 42.36 (SD=18.93) and on the revised item was 50.15 (SD=21.45). As shown in Table 1, participants reported consuming cannabis via bongs only on the greatest proportion of use days (30.3%), followed by vaping only, joints only, pipes only, and blunts only. Alcohol was co-used most often (n=256 days; 42.2% of cannabis use days), followed by nicotine (n=214 days; 35.26% of cannabis use days). On nicotine co-use days, participants primarily reported vaporizing nicotine (n=149 days), followed by smoking blunts (n=73), combustible cigarettes (n=34 days), and hookah (n=1 day). All types of nicotine use days were coded as 1 (any use) or 0 (no nicotine use). Use of specific nicotine products were coded as 1 (any use) or 0 (no use) for the following: blunt use days, combustible cigarette use days, and nicotine vaping days..2
The intra-class correlations for each subjective cannabis effects item indicated slightly greater within-person variability for the four-anchored item (76.5%) versus the standard item (68.3%). Figure 1 presents a scatterplot of the two item scores as a function of day-level consumption; darker markers correspond to more raw hits. This plot shows a modest, positive association between the items (b=0.88, SE=0.04, p<.001, Pseudo-R2=33.7%, p<.001). The overall MLMs with day- and person- level number of hits predicting subjective effects accounted for 9.9% of the variance in the standard, and 14.9% in the revised, items. For the standard item, the intercept (b=41.74, SE=1.34, p<.001) and day-level hits variable (b=2.35, SE=0.23, p<.001), but not the person-level hits variable (b=0.37, SE=0.27, p=.170), were statistically significant. For the revised item, the intercept (b=49.76, SE=1.39, p<.001), day-level hits (b=2.35, SE=0.23, p<.001), and person-level hits (b=0.55, SE=0.27, p=.046) were all statistically significant.
Figure 1.
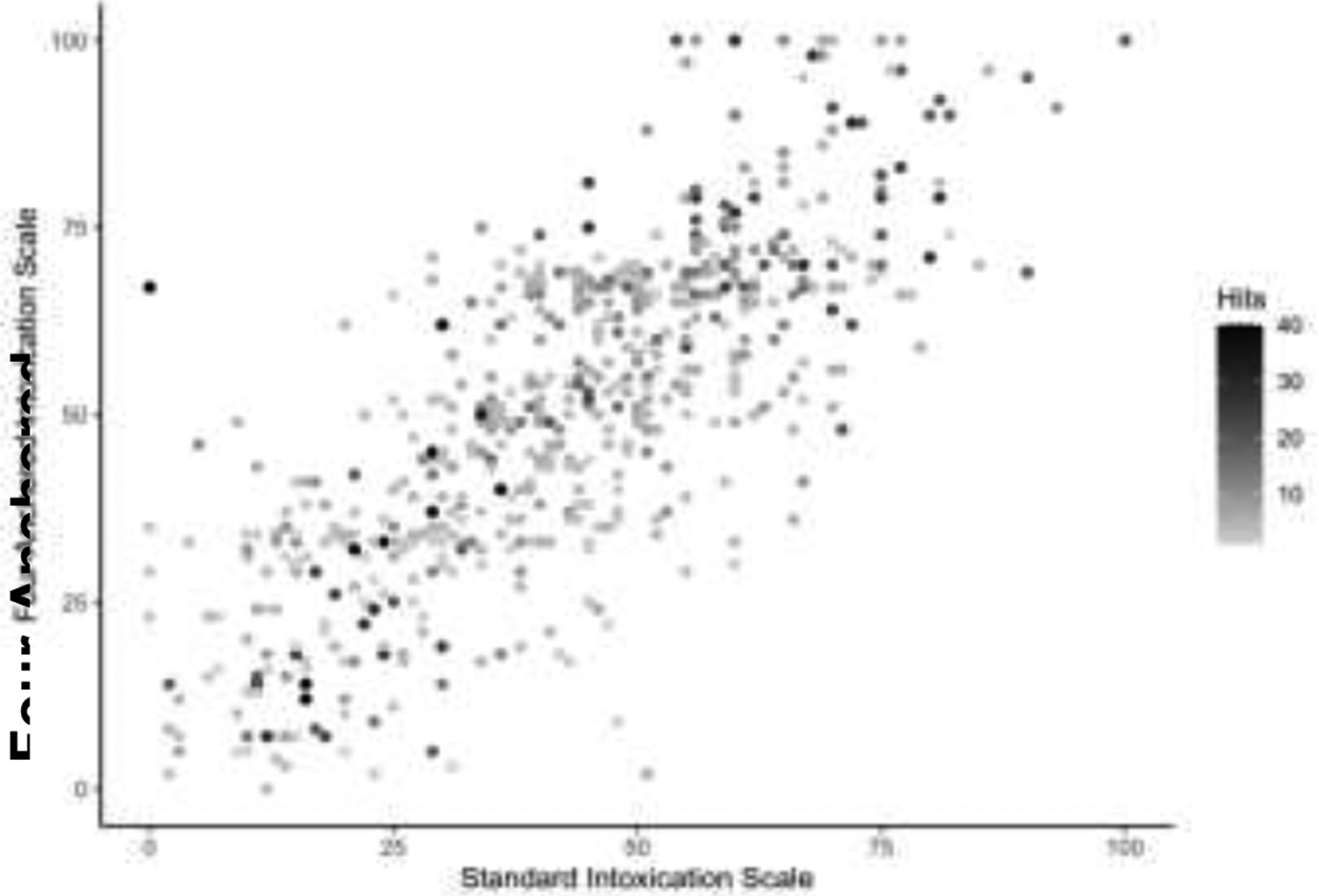
Scatterplot of Scores on the Standard Subjective Cannabis Intoxication Scale and the Four-Anchored Subjective Cannabis Effects Scale, Conditioned by the Number of Hits
3.2. Mode of Administration as a Moderator of Cannabis Use and Subjective Effects
On single-mode days there was minimal variability in the overall mean number of daily hits across modes of administration, ranging from 5.6 (bong) to 9.1 (blunts); corresponding mean subjective cannabis effects ranged from 43.8 (pipe) to 57.6 (blunts). Table 2 presents results from models testing whether cannabis mode of administration moderated the association between number of cannabis hits and subjective effects assessed with the revised item. Significant main effects in Table 2 indicate participants reported higher subjective effects levels on bong-only days than vape-only days. Subjective cannabis effects levels on joint-only and pipe-only days did not differ from vape-only days. Blunt use was the only mode of administration that moderated the association between cannabis consumption levels and subjective effects. As shown in Figure 2, the strength of the association between number of hits and subjective effects was significantly weaker on blunt-only days compared to vape-only days. Subjective effects increased by 2.87 for each cannabis hit on vape-only days (b=2.87, p<.001), but the change in subjective effects on blunt-only days was not significantly different from 0 (b=1.04, p=.157).
Table 2.
Multilevel Models of Mode Type Predicting Subjective Cannabis Effects
| Hits Only | Main Effects Only | Interaction | ||||
|---|---|---|---|---|---|---|
| Fixed Effects | b | SE | b | SE | b | SE |
| Intercept | 49.76*** | 1.39 | 45.52*** | 2.13 | 45.96*** | 2.10 |
| Level 1: Main Effects | ||||||
| Number of Hits | 2.35*** | 0.23 | 2.50*** | 0.23 | 2.88*** | 0.40 |
| Vape-Only (Reference) | ||||||
| Bong-Only | - | - | 9.77*** | 2.59 | 9.48*** | 2.63 |
| Blunt-Only | - | - | 8.70* | 4.00 | 8.47* | 3.98 |
| Joint-Only | - | - | 2.13 | 3.31 | 2.57 | 3.32 |
| Pipe-Only | - | - | −2.55 | 3.61 | −2.58 | 3.60 |
| Level 1: Interactions | ||||||
| HitsXBong | - | - | - | - | −0.31 | 0.54 |
| HitsXBlunt | - | - | - | - | −1.84* | 0.83 |
| HitsXJoint | - | - | - | - | 0.54 | 0.85 |
| HitsXPipe | - | - | - | - | −1.23 | 0.80 |
| Level 2 | ||||||
| Mean Number of Hits | 0.55* | 0.27 | 0.51 | 0.27 | 0.58* | 0.27 |
| Pseudo-R 2 | 14.9% | 19.6% | 20.7% | |||
Note.n = 472 days nested within 102 individuals.
p < .05;
p <.01;
p <.001
Figure 2.

Associations Between Mode of Cannabis Administration and Subjective Cannabis Effects
3.3. Co-Use as a Moderator of Cannabis Use and Subjective Effects
Table 3 Model Set A shows models testing associations of the main effects of co-use of alcohol or nicotine and cannabis with increased subjective cannabis effects, as well as whether use of each substance moderated the association between cannabis consumption and subjective effects. In main effects models, participants reported stronger subjective effects from cannabis on days when they co-used with nicotine, suggesting a within-person enhancement effect of nicotine use after controlling for the number of cannabis hits. There were no significant moderation effects and no significant association between daily alcohol use and subjective cannabis effects.
Table 3.
Multilevel Models of Co-Use Predicting Subjective Cannabis Effects on the Revised Scale
| Fixed Effects | Main Effects | All Interactions | ||
|---|---|---|---|---|
| Model Set A | b | SE | b | SE |
| Intercept | 49.90*** | 1.35 | 49.93*** | 1.36 |
| Level 1 | ||||
| Number of Hits | 2.11*** | 0.16 | 2.11*** | 0.16 |
| aAlcohol | −0.48 | 1.56 | −0.44 | 1.57 |
| bNicotine | 5.24* | 2.15 | 5.18* | 2.17 |
| Hits X Alcohol | - | - | 0.23 | 0.40 |
| Hits X Nicotine | - | - | −0.11 | 0.57 |
| Level 2 | ||||
| Mean Number of Hits | 0.24 | 0.22 | 0.24 | 0.23 |
| Model Set B | ||||
| Intercept | 49.84*** | 1.36 | 49.84*** | 1.36 |
| Level 1 | ||||
| Number of Hits | 2.03*** | 0.15 | 2.04*** | 0.15 |
| cBlunts | 6.47** | 2.05 | 6.41** | 2.06 |
| dCigarettes | −5.16 | 3.94 | −5.17 | 3.96 |
| eNicotine Vaping | 7.23** | 2.53 | 7.30** | 2.54 |
| Hits X Blunts | −0.10 | 0.56 | ||
| Hits X Cigarettes | 0.68 | 0.80 | ||
| Hits X Nicotine Vaping | 0.13 | 0.67 | ||
| Level 2 | ||||
| Mean Number of Hits | 0.24 | 0.22 | 0.24 | 0.22 |
Note. n = 597 days nested within 105 individuals.
p < .05;
p <.01;
p <.001
Alcohol: 1 = Any alcohol used; 0 = No alcohol used;
Nicotine: 1 = Any blunts, cigarettes, cigars, cigarillos, hookah, or e-cigarettes used; 0 = No cigarettes, cigars, cigarillos, hookah, or e-cigarettes used;
Blunts: 1 = Blunt only day; 0 = Other Mode of Administration Day;
Cigarettes: 1 = Any cigarettes used; 0 = No cigarettes used;
Nicotine Vaping: 1 = Any e-cigarettes/nicotine vaping used; 0 = No e-cigarettes/nicotine vaping used
Table 3 Model Set B presents results from models testing the main effects of co-use of smoking blunts, combustible cigarettes, and vaping nicotine on subjective cannabis effects, as well as whether either type of nicotine use moderated the association between number of cannabis hits and subjective effects. In the main-effects models, participants reported greater subjective effects of cannabis on days when they co-used nicotine by vaping. Co-using combustible cigarettes was not associated with subjective cannabis effects. There were no statistically significant moderation effects.
4.0. Discussion
As cannabis is increasingly legalized, daily cannabis use has increased, particularly among adults. Therefore, there is an increased need to understand cannabis use outcomes. Characterizing subjective cannabis effects in daily life is critical for understanding how and why young adults use cannabis, to inform prevention and intervention efforts. This study aimed to validate a new four-anchored item that uses contemporary young adult language to assess subjective cannabis effects in daily life and the extent to which the association between cannabis consumption and subjective effects were moderated by mode of cannabis administration and co-use of alcohol or nicotine. As expected, cannabis consumption levels were positively associated with the revised subjective cannabis effects slider and this association was moderated by mode of administration. In other words, the cannabis consumption-subjective effects link was stronger on vape-only days relative to blunt-only days. Unexpectedly, there was a main effect of bong-only days relative to vape-only days on subjective cannabis effects and there was not a statistically significant moderation of vape-only days relative to any other mode of administration. While nicotine co-use was associated with greater subjective cannabis effects, neither alcohol nor nicotine co-use moderated the effect of cannabis consumption on subjective cannabis effects.
As expected, the revised item was highly correlated with the standard item. Cannabis consumption levels accounted for 5% more variance on the revised item, indicating that the increased variability is substantively meaningful. Similar to findings from a four-anchored item assessing subjective alcohol effects in daily life (Linden-Carmichael & Calhoun, 2021), the revised item had a larger standard deviation than the standard item, suggesting that the anchors encouraged use of the full scale. Including a top anchor of “very high” or “the highest I have ever felt” may not adequately capture the full spectrum of cannabis effects, as the word “high” was associated with only moderate effects (Linden-Carmichael, Masters et al., 2020). Anchoring a scale using contemporary young adult language may help participants differentiate subjective experiences.
Several key findings emerged when testing moderation effects of mode of administration and co-use on the cannabis consumption-subjective effects link. Concerning mode of administration, associations between level of cannabis use and subjective effects were weaker on blunt-only days than vape-only days, suggesting that the number of hits differentially predicts subjective effects by mode of administration. Combined with laboratory-based and recent daily diary studies, blunts may be relatively “inefficient” compared to vaporizers at producing the desired subjective cannabis effects when consuming the same cannabis levels (Cloutier et al., 2021; Mariani et al., 2011; Streck et al., 2019). Unlike vaporizers, pipes, and bongs, users prepare blunts themselves which may produce weaker seals than other modes of administration. An alternative explanation is that young adults smoking cannabis via blunts are consuming plant products, whereas those using vaporizers are consuming concentrates. While this interpretation aligns with emerging data on vaporizer use (Aston et al., 2019), it does not explain why a similar pattern did not emerge for all smoking modes (i.e., pipes, bongs, joints) that are typically associated with plant consumption. The present study did not capture how each mode was prepared, the types of products consumed with each mode, nor the potency of the products; these factors should be considered in future research.
The effects of co-use on subjective cannabis effects were mixed. Alcohol use did not associate with subjective cannabis use effects nor moderate the association between use and subjective effects. Emerging literature on the role of alcohol and cannabis co-use on subjective effects is mixed. Some studies suggest higher subjective intoxication and negative consequences relative to alcohol or cannabis-only days (Sokolovsky et al., 2020); others suggest higher alcohol intoxication and lower cannabis intoxication (Lee et al., 2017). Still others, including the parent study (Linden-Carmichael et al., 2020b), suggest similar subjective effects across alcohol-only, cannabis-only, and co-use days. It is unlikely that the effects were not observed in the present study because of how co-use was assessed and defined. Large studies testing the effects of competing operationalizations of simultaneous and co- alcohol and cannabis use based on how closely each substance was consumed (within 1–240 minutes in 1 min increments), found no differences in day level consequences or subjective intoxication (Sokolovsky et al., 2020). Mixed findings may be related to the assessment of subjective effects. Prior laboratory work has found that THC can increase certain subjective states when also using alcohol. It is possible that individuals experience specific subjective effects that may not be captured on a slider of “how high do you feel?” (Lukas and Orozco, 2001). Future work assessing these effects in real-world settings may be informative.
Days on which young adults co-used nicotine with cannabis were associated with greater subjective cannabis effects, but nicotine co-use did not moderate the association between consumption and effects. In other words, participants reported feeling higher on days they also used nicotine, but nicotine co-use did not necessarily exaggerate the effect of cannabis consumption on subjective cannabis effects. When nicotine days were specified further by mode of administration, the association with subjective cannabis effects were specific to blunt use and nicotine vaping. Consistent with prior work demonstrating that using nicotine increases the odds of using cannabis (Wilhelm et al., 2020), findings suggest certain nicotine products may predict greater subjective cannabis effects, independent of cannabis consumption. Clinically, these results may be relevant to individuals who regularly co-use cannabis and nicotine by serving as an etiological mechanism explaining higher rates of comorbid use and use-related disorders (Leventhal et al., 2020). By extension, efforts to reduce using one substance, may trigger an increase in the other, making quit or reduction attempts more challenging. Because the current study did not directly test this, such patterns will need to be directly explored in future diary research.
4.1. Future Directions and Limitations
Several limitations should be noted. First, subjective cannabis effects were assessed the day after a cannabis use event with a single item broadly referring to how participants felt. There is a large body of work indicating that the effects young adults experience after using cannabis are nuanced, multidimensional, and variable across age and gender (Ewusi Boisvert et al., 2020; Green et al., 2003; Linden-Carmichael et al., 2020a; Spindle et al., 2019b). Future research should seek to capture this variability with multiple items and more specific instructions (e.g., asking about peak intoxication/effects) with larger samples. Second, in the present study participants completed a daily diary about their prior day cannabis use; participants may have had difficulty accurately rating subjective effects on days involving multiple cannabis use events and modes of administration. More intensive assessments to capture nuanced changes throughout a day would be useful.
Third, given the inclusion criteria and sampling population, findings may be limited to white young adults who regularly use both cannabis and alcohol (Linden-Carmichael et al., 2020b). Approximately 75% of young adults in the US who report cannabis use also report regular alcohol use, and the current findings likely generalize to this majority (Terry-McElrath and Patrick, 2018). Nevertheless, as cannabis is decriminalized/legalized and products become more accessible, the prevalence of individuals who regularly use only cannabis is likely to increase (Budney et al., 2019; Budney and Borodovsky, 2017). Because access and consequences are not equally distributed across racial groups (Matsuzaka and Knapp, 2020), research with diverse samples should consider how these changing populations differ in their experiences with cannabis and how they describe their experiences with cannabis vs. alcohol. Importantly, both the preliminary study used crowdsource current terms describing cannabis use intoxication/effects (Linden-Carmichael et al., 2020a) and the present study explicitly sampled young adults aged 18–25 years as a population engaging in the highest rates of cannabis use relative to other age groups and whom describe the subjective effects of cannabis differently from older generations. Given a growing population of older adults engaging in regular cannabis use and co-use (Han et al., 2017), future research with middle-aged and elderly adults explicitly designed to characterize shifts in language to describe subjective cannabis effects well as replicate the pattern of effects in the present study is needed.
4.2. Conclusions
Several organizations have called for research to characterize the effects of cannabis use (National Academies of Sciences, Engineering, and Medicine, 2017; World Health Organization, 2016). This study tested the psychometric properties of a revised, single-item scale of cannabis effects in daily life and explored key day-level moderators. The revised item, which incorporates contemporary young adult language, has strengths relative to standard assessments of subjective intoxication, including greater within-person variability that encourages use of the full range of the scale. As cannabis use becomes legalized or decriminalized across the United States and increases access to a range of cannabis products, findings reinforce the need to update and expand our assessments of cannabis predictors to include modes of administration as well as cannabis effects to align with the language used by young adults, rather than focusing narrowly on ‘degrees of impairment’ or ‘intoxication’. Future policy and interventions focused on co-use behaviors will need to carefully define outcomes based on conceptual relevance (e.g., broader subjective effects vs. impairment/intoxication) and target substances (e.g., cannabis vs. alcohol vs. nicotine).
Supplementary Material
Highlights.
A revised four-anchored sliding item using contemporary young adult language to assess subjective cannabis effects is a viable alternative to the standard subjective intoxication sliding item.
Subjective cannabis effects were rated higher on days participants took more hits; this effect was weakened on days cannabis was smoked via blunts or joints relative to vaping.
Subjective cannabis effects were higher on days cannabis was co-used with nicotine, but not alcohol.
As cannabis use becomes decriminalized across the United States, findings reinforce the need to update our assessments of cannabis effects to align with the language used by young adults.
Role of Funding Source
Funding for this study was provided by NIDA Grant P50 DA039838, NIAAA Grant K01 AA026854, and NIDA Grant T32 DA017629. NIDA and NIAAA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Blunt use was coded as an indicator of nicotine use based on research demonstrating that even when tobacco is removed from blunt wraps, trace nicotine levels remain which may impact the subjective cannabis effects experienced by young adults (Peters et al., 2016). This categorization also permitted more nuanced ad hoc analyses in Table 3, Model Set B which explores the extent to which specific nicotine products are associated with subjective cannabis effects with blunt use as a specified variable. Importantly, the substantive interpretation of the findings does not change when blunt use is not treated as a separate indicator of nicotine use.
There were 12 days where participants vaporized nicotine and smoked combustible cigarettes, 20 days where participants smoked blunts and vaporized nicotine, and 3 days where participants smoked blunts, combustible cigarettes, and vaporized nicotine. These occasions followed the same coding system as described.
Conflict of Interest
None of the authors have financial disclosures or other conflicts of interest to disclose.
References
- Aston ER, Farris SG, Metrik J, Rosen RK, 2019. Vaporization of marijuana among recreational users: A qualitative study. J. Stud. Alcohol Drugs 80, 56–62. 10.15288/jsad.2019.80.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borodovsky JT, 2016. Smoking, vaping, eating: Is legalization impacting the way people use cannabis? Int. J. Drug Policy 7. 10.1016/j.drugpo.2016.02.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brackenbury LM, Ladd BO, Anderson KG, 2016. Marijuana use/cessation expectancies and marijuana use in college students. Am. J. Drug Alcohol Abuse 42, 8. 10.3109/00952990.2015.1105242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo AJ, 2017. Is 4/20 an event-specific marijuana holiday? A daily diary investigation of marijuana use and consequences among college students. J. Stud. Alcohol Drugs 6. 10.15288/jsad.2017.78.134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney AJ, Borodovsky JT, 2017. The potential impact of cannabis legalization on the development of cannabis use disorders. Prev. Med 104, 31–36. 10.1016/j.ypmed.2017.06.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney AJ, Sargent JD, Lee DC, 2015. Vaping cannabis (marijuana): parallel concerns to e- cigs? Addiction 110, 1699–1704. 10.1111/add.13036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney AJ, Sofis MJ, Borodovsky JT, 2019. An update on cannabis use disorder with comment on the impact of policy related to therapeutic and recreational cannabis use. Eur. Arch. Psychiatry Clin. Neurosci 269, 73–86. 10.1007/s00406-018-0976-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloutier RM, Calhoun Brian H., Linden-Carmichael AN, 2021. Associations of mode of administration on cannabis consumption and subjective intoxication in daily life. Psychol. Addict. Behav 10.1037/adb0000726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper ZD, Haney M, 2009. Comparison of subjective, pharmacokinetic, and physiological effects of marijuana smoked as joints and blunts. Drug Alcohol Depend. 103, 107–113. 10.1016/j.drugalcdep.2009.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downey LA, King R, Papafotiou K, Swann P, Ogden E, Boorman M, Stough C, 2013. The effects of cannabis and alcohol on simulated driving: Influences of dose and experience. Accid. Anal. Prev 50, 879–886. 10.1016/j.aap.2012.07.016 [DOI] [PubMed] [Google Scholar]
- Ewusi Boisvert E, Bae D, Pang RD, Davis JP, Kelley-Quon LI, Barrington-Trimis JL, Kirkpatrick MG, Chai SH, Leventhal AM, 2020. Subjective effects of combustible, vaporized, and edible cannabis: Results from a survey of adolescent cannabis users. Drug Alcohol Depend. 206, 107716. 10.1016/j.drugalcdep.2019.107716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fischman MW, Foltin RW, 1991. Utility of subjective-effects measurements in assessing abuse liability of drugs in humans. Br. J. Addict 86, 1563–1570. 10.1111/j.1360-0443.1991.tb01749.x [DOI] [PubMed] [Google Scholar]
- Green B, Kavanagh D, Young R, 2003. Being stoned: a review of self-reported cannabis effects. Drug Alcohol Rev. 22, 453–460. 10.1080/09595230310001613976 [DOI] [PubMed] [Google Scholar]
- Han BH, Sherman S, Mauro PM, Martins SS, Rotenberg J, Palamar JJ, 2017. Demographic trends among older cannabis users in the United States, 2006–13. Addiction 112, 516–525. 10.1111/add.13670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haney M, Ward AS, Comer SD, Foltin RW, Fischman MW, 1999. Abstinence symptoms following smoked marijuana in humans. Psychopharmacology (Berl.) 141, 395–404. 10.1007/s002130050849 [DOI] [PubMed] [Google Scholar]
- Hughes JR, Fingar JR, Budney AJ, Naud S, Helzer JE, Callas PW, 2014. Marijuana use and intoxication among daily users: An intensive longitudinal study. Addict. Behav 39, 1464–1470. 10.1016/j.addbeh.2014.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CM, Cadigan JM, Patrick ME, 2017. Differences in reporting of perceived acute effects of alcohol use, marijuana use, and simultaneous alcohol and marijuana use. Drug Alcohol Depend. 180, 391–394. 10.1016/j.drugalcdep.2017.08.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Bae D, Kechter A, Barrington-Trimis JL, 2020. Psychiatric comorbidity in adolescent use and poly-use of combustible, vaporized, and edible cannabis products. J. Psychiatr. Res 124, 91–98. 10.1016/j.jpsychires.2020.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Masters LD, Lanza ST, 2020a. “Buzzwords”: Crowd-sourcing and quantifying U.S. young adult terminology for subjective effects of alcohol and marijuana use. Exp. Clin. Psychopharmacol 28, 632–637. 10.1037/pha0000344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linden-Carmichael AN, Van Doren N, Masters LD, Lanza ST, 2020b. Simultaneous alcohol and marijuana use in daily life: Implications for level of use, subjective intoxication, and positive and negative consequences. Psychol. Addict. Behav 34, 447–453. 10.1037/adb0000556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipperman-Kreda S, Gruenewald PJ, Grube JW, Bersamin M, 2017. Adolescents, alcohol, and marijuana: Context characteristics and problems associated with simultaneous use. Drug Alcohol Depend. 179, 55–60. 10.1016/j.drugalcdep.2017.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukas SE, Orozco S, 2001. Ethanol increases plasma Δ9-tetrahydrocannabinol (THC) levels and subjective effects after marihuana smoking in human volunteers. Drug Alcohol Depend. 64, 143–149. 10.1016/S0376-8716(01)00118-1 [DOI] [PubMed] [Google Scholar]
- Mariani JJ, Brooks D, Haney M, Levin FR, 2011. Quantification and comparison of marijuana smoking practices: Blunts, joints, and pipes. Drug Alcohol Depend. 113, 249–251. 10.1016/j.drugalcdep.2010.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuzaka S, Knapp M, 2020. Anti-racism and substance use treatment: Addiction does not discriminate, but do we? J. Ethn. Subst. Abuse 19, 567–593. 10.1080/15332640.2018.1548323 [DOI] [PubMed] [Google Scholar]
- Nahum-Shani I, Smith SN, Spring BJ, Collins LM, Witkiewitz K, Tewari A, Murphy SA, 2018. Just-in-time adaptive interventions (JITAIs) in mobile health: Key components and design principles for ongoing health behavior support. Ann. Behav. Med 52, 446–462. 10.1007/s12160-016-9830-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine, 2017. The health effects of cannabis and cannabinoids: The current state of evidence and recommendations for research. The National Academies Press, Washington, DC. [PubMed] [Google Scholar]
- Patrick ME, Fairlie AM, Cadigan JM, Abdallah DA, Larimer ME, Lee CM, 2019. Daily motives for alcohol and marijuana use as predictors of simultaneous use among young adults. J. Stud. Alcohol Drugs 80, 454–461. 10.15288/jsad.2019.80.454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Lee CM, 2018. Cross-faded: Young adults’ language of being simultaneously drunk and high. Cannabis Res. Soc. Marijuana 1, 60–65. 10.26828/cannabis.2018.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penetar DM, Kouri EM, Gross MM, McCarthy EM, Rhee CK, Peters EN, Lukas SE, 2005. Transdermal nicotine alters some of marihuana’s effects in male and female volunteers. Drug Alcohol Depend. 79, 211–223. 10.1016/j.drugalcdep.2005.01.008 [DOI] [PubMed] [Google Scholar]
- Peters EN, Schauer GL, Rosenberry ZR, Pickworth WB, 2016. Does marijuana “blunt” smoking contribute to nicotine exposure?: Preliminary product testing of nicotine content in wrappers of cigars commonly used for blunt smoking. Drug Alcohol Depend. 168, 119–122. 10.1016/j.drugalcdep.2016.09.007 [DOI] [PubMed] [Google Scholar]
- Prince MA, Conner BT, 2019. Examining links between cannabis potency and mental and physical health outcomes. Behav. Res. Ther 115, 111–120. 10.1016/j.brat.2018.11.008 [DOI] [PubMed] [Google Scholar]
- Quinn PD, Fromme K, 2011. Predictors and outcomes of variability in subjective alcohol intoxication among college students: An event-level analysis across 4 years. Alcohol. Clin. Exp. Res 35, 484–495. 10.1111/j.1530-0277.2010.01365.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronen A, Chassidim HS, Gershon P, Parmet Y, Rabinovich A, Bar-Hamburger R, Cassuto Y, Shinar D, 2010. The effect of alcohol, THC and their combination on perceived effects, willingness to drive and performance of driving and non-driving tasks. Accid. Anal. Prev 42, 1855–1865. 10.1016/j.aap.2010.05.006 [DOI] [PubMed] [Google Scholar]
- Russell C, Rueda S, Room R, Tyndall M, Fischer B, 2018. Routes of administration for cannabis use – basic prevalence and related health outcomes: A scoping review and synthesis. Int. J. Drug Policy 52, 87–96. 10.1016/j.drugpo.2017.11.008 [DOI] [PubMed] [Google Scholar]
- Schulenberg J, Johnston L, O’Malley P, Bachman P, Miech R, Patrick M, 2019. Monitoring the Future national survey results on drug use, 1975–2018 Volume II, college students and adults.
- Sokolovsky AW, Gunn RL, Micalizzi L, White HR, Jackson KM, 2020. Alcohol and marijuana co-use: Consequences, subjective intoxication, and the operationalization of simultaneous use. Drug Alcohol Depend. 212, 107986. 10.1016/j.drugalcdep.2020.107986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solowij N, 2018. Peering through the haze of smoked vs vaporized cannabis—to vape or not to vape? JAMA Netw. Open 1, e184838. 10.1001/jamanetworkopen.2018.4838 [DOI] [PubMed] [Google Scholar]
- Spindle TR, Bonn-Miller MO, Vandrey R, 2019a. Changing landscape of cannabis: novel products, formulations, and methods of administration. Curr. Opin. Psychol 30, 98–102. 10.1016/j.copsyc.2019.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spindle TR, Cone EJ, Schlienz NJ, Mitchell JM, Bigelow GE, Flegel R, Hayes E, Vandrey R, 2019b. Acute pharmacokinetic profile of smoked and vaporized cannabis in human blood and oral fluid. J. Anal. Toxicol 43, 233–258. 10.1093/jat/bky104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spindle TR, Cone EJ, Schlienz NJ, Mitchell JM, Bigelow GE, Flegel R, Hayes E, Vandrey R, 2018. Acute effects of smoked and vaporized cannabis in healthy adults who infrequently use cannabis: A crossover trial. JAMA Netw. Open 1, e184841. 10.1001/jamanetworkopen.2018.4841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streck JM, Hughes JR, Klemperer EM, Howard AB, Budney AJ, 2019. Modes of cannabis use: A secondary analysis of an intensive longitudinal natural history study. Addict. Behav 98, 106033. 10.1016/j.addbeh.2019.106033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2019. Key substance use and mental health indicators in the United States: Results from the 2018 National Survey on Drug Use and Health (No. (HHSPublication No. PEP19–5068, NSDUH Series H-54)) Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Terry-McElrath YM, Patrick ME, 2018. Simultaneous Alcohol and Marijuana Use Among Young Adult Drinkers: Age-Specific Changes in Prevalence from 1977 to 2016. Alcohol. Clin. Exp. Res 42, 2224–2233. 10.1111/acer.13879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thrul J, Gubner NR, Nguyen N, Nguyen C, Goodell EA, Holmes LM, Vandrey RG, Ling PM, 2021. Perceived reward from using cigarettes with alcohol or cannabis and concurrent use: A smartphone-based daily diary study. Addict. Behav 114, 106747. 10.1016/j.addbeh.2020.106747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins SL, Karliner-Li P, Lee YO, Koester KA, Ling PM, 2021. A mixed-methods study to inform the clarity and accuracy of cannabis-use and cannabis-tobacco co-use survey measures. Drug Alcohol Depend. 224, 108697. 10.1016/j.drugalcdep.2021.108697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhelm J, Abudayyeh H, Perreras L, Taylor R, Peters EN, Vandrey R, Hedeker D, Mermelstein R, Cohn A, 2020. Measuring the temporal association between cannabis and tobacco use among Co-using young adults using ecological momentary assessment. Addict. Behav 104, 106250. 10.1016/j.addbeh.2019.106250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2016. The health and social effects of nonmedical cannabis use. Retrieved from https://www.who.int/substance_abuse/publications/msbcannabis.pdf. Accessed on 10/18/2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


