Abstract
Background:
Naloxone is a prescription medication that reverses opioid overdoses. Allowing naloxone to be dispensed directly by a pharmacist without an individual prescription under a naloxone standing order (NSO) can expand access. The community-level factors associated with naloxone dispensed under NSO are unknown.
Methods:
Using a dataset comprised of pharmacy reports of naloxone dispensed under NSO from 70% of Massachusetts retail pharmacies, we examined relationships between community-level demographics, rurality, measures of treatment for opioid use disorder, and overdose deaths with naloxone dispensed under NSO per ZIP Code-quarter from 2014 until 2018. We used a multi-variable zero-inflated negative binomial model, assessing odds of any naloxone dispensed under NSO, as well as a multi-variable negative binomial model assessing quantities of naloxone dispensed under NSO.
Results:
From 2014–2018, quantities of naloxone dispensed under NSO and the number of pharmacies dispensing any naloxone under NSO increased over time. However, communities with greater percentages of people with Hispanic ethnicity (aOR 0.91, 95% CI 0.86–0.96 per 5% increase), and rural communities compared to urban communities (aOR 0.81, 95% CI 0.73–0.90) were less likely to dispense any naloxone by NSO. Communities with more individuals treated with buprenorphine dispensed more naloxone under NSO, as did communities with more opioid-related overdose deaths.
Conclusion:
Naloxone dispensing has substantially increased, in part driven by standing orders. A lower likelihood of naloxone being dispensed under NSO in communities with larger Hispanic populations and in more rural communities suggests the need for more equitable access to, and uptake of, lifesaving medications like naloxone.
Keywords: naloxone, pharmacy, standing orders, harm reduction, analgesics, opioid
1. Introduction
Overdose deaths, primarily due to opioids, have continued to increase in the United States in recent years (Wilson et al., 2020). From 2010–2018, the state of Massachusetts reported an increase in the rate of fatal opioid overdoses from 8.0 to 28.5 overdose deaths per 100,000 population (Data Brief: Opioid-Related Overdose Deaths among Massachusetts Residents, 2019). In Massachusetts, this drastic increase was primarily driven by the rise of illicitly manufactured fentanyl in the drug supply (Somerville et al., 2017). In response to the growth of fatal overdose events in Massachusetts, the state sought to increase naloxone access, namely through community and pharmacy-based naloxone distribution. Naloxone is an opioid antagonist that “reverses” opioid overdoses (Wermeling, 2015). Increased naloxone distribution has been associated with reduced opioid overdose mortality (Bird et al., 2016; Walley et al., 2013); however, naloxone is a prescription drug, which has historically limited opportunities to expand access to it.
In addition to naloxone prescribed to an individual, an additional important source of naloxone is naloxone distributed by community overdose education and naloxone distribution (OEND) programs. In Massachusetts, OEND programs—coordinated by the Massachusetts Department of Public Health—have been educating individuals about signs of opioid overdose and distributing naloxone since 2006. While they are an important source of naloxone, not all communities have OEND programs (Walley et al., 2013).
A third important source of naloxone is naloxone dispensed by a pharmacy under a standing order. Pharmacy standing orders, which allow dispensing of a medication or treatment without an individual prescription, have historically been a strategy used to improve access to and uptake of important public health interventions. For example, standing orders for vaccinations, including influenza vaccinations, have been used to facilitate access, since pharmacies often have longer hours, more locations, and fewer or no requirements for appointments (Shen and Peterson, 2020). Pharmacy standing orders have also been a strategy for facilitating expedited partner treatment for individuals with sexually transmitted infections, bypassing the delay and cost associated with clinician evaluation (“Legal Status of Expedited Partner Therapy (EPT),” 2020).
In March 2014, the Massachusetts governor declared a public health emergency and promoted naloxone distribution to people at risk of opioid overdose, as well as their friends and family, via naloxone standing orders at community pharmacies (MacQuarrie, 2014; Queensland, 2017). The Massachusetts Department of Public Health (MDPH) issued guidance to pharmacies on creating a standing order, so that people could obtain a naloxone rescue kit from the pharmacy without a prescription. Under the standing order, pharmacies dispense naloxone to individuals at risk of having, or witnessing, an opioid overdose. The standing order removed the need to have a prescription for naloxone written by an individual’s medical provider. Massachusetts is one of the first states to implement a pharmacy-based naloxone distribution program. On December 1, 2017, MDPH mandated that all retail pharmacies have a standing order and on October 4, 2018, MDPH issued a statewide standing order that applied to all pharmacies (“2018–04: Naloxone Dispensing via Standing Order,” 2020).
Certain pharmacy-level factors are known to be associated with dispensing naloxone by standing order (NSO). A study that telephone surveyed 78% of Massachusetts pharmacies in 2015 found that chain pharmacies and staff training was associated with increased distribution under NSO (Stopka et al., 2017). Specifically, in multivariable logistic regression analyses chain pharmacies, pharmacy staff awareness and interest in participating in distribution under a standing order, pharmacy staff training in overdose prevention, and pharmacy technician respondents were all independently and positively associated with reported sales naloxone under NSO (Stopka et al., 2017).
Certain neighborhood characteristics are associated with differential pharmacy naloxone dispensing, though not specifically dispensing under NSO. Younger age distribution in a community has been associated with greater quantities of naloxone distributed (Green et al., 2019). Data on the relationship between racial/ethnic makeup of a community and naloxone availability and distribution have been mixed. In a national study of naloxone dispensing by county, high naloxone-dispensing counties were more likely to have lower percentages of non-Hispanic White residents (Guy et al., 2019). In contrast, in a “mystery caller” study in North Carolina, pharmacies in census tracts with larger racial and ethnic minority populations were less likely to have naloxone available (Egan et al., 2020). With regard to rurality, In the abovementioned Guy study, rural counties were less likely to be high-dispensing counties than urban ones (Guy et al., 2019). With regard to socioeconomic status, census tracts with higher rates of public health insurance coverage (a proxy for lower socioeconomic status) were associated with greater likelihood of naloxone availability (Egan et al., 2020).” Higher buprenorphine prescription fills and greater nonprescription syringe sales in a geographic area are also associated with more naloxone dispensing (Green et al., 2019).
Knowing how much naloxone has been distributed by pharmacies through a standing order and exploring community-level sociodemographic associations with dispensing under NSO could help better target community naloxone distribution efforts through pharmacies and through community OEND programs. In this study using pharmacy-dispensing data, we aimed to describe naloxone rescue kit dispensing at the Massachusetts ZIP Code level via pharmacy standing orders from 2014 to 2018. We aimed to examine the associations of ZIP Code level sociodemographic exposures with dispensing events under NSO in Massachusetts. Based on the aforementioned findings from prior pharmacy-based naloxone studies, we hypothesized that communities with younger population distributions, lower percentages of individuals from racial and ethnic minority groups, urban classifications, and lower income distributions would be more likely to dispense naloxone under NSO and dispense more of it. We also examined whether higher buprenorphine and methadone treatment admissions and community opioid overdose fatality rates were associated with quantities of naloxone dispensed under NSO.
2. Methods
2.1. Population, Setting, and Primary Data Source
We used two sources for retail pharmacy data of naloxone distributed between April, 2014 and October, 2018 in Massachusetts. One of this study’s authors (AYW) was the standing order writer for many independent pharmacies and large chain pharmacies. These pharmacies reported quantities of NSO naloxone dispensed directly to AYW. The pharmacies dispensing naloxone under this standing order represent 34% of the 1042 (after deduplication) retail pharmacies on a list of pharmacies made available from a previous study in Massachusetts (Stopka et al., 2017). Independently, a large retail pharmacy business in Massachusetts dispensed and documented quantities of naloxone under NSO over the same 2014–2018 study period under a single standing order prescriber. The locations of this large retail pharmacy business represented another 36% of 1042 retail pharmacies registered in Massachusetts. The naloxone dispensing data from the retail pharmacy business have been described and analyzed in prior studies (Green et al., 2020, 2019). For this analysis, we combined the AYW dataset and the retail pharmacy business dataset to produce a merged dataset covering an estimated 70% of retail pharmacies in the state.
2.2. Data
2.2.1. Outcome
Our primary outcome was the number of naloxone dispensing events (NDEs). We defined an NDE as a dispensing event documented by the pharmacy. We made the assumption that each dispensing event represented one naloxone kit containing two doses. While a dispensing event might actually represent more than one kit, we believe that such events were rare, and thus consider NDEs and kits as interchangeable units.
We included NDEs recorded under the standing order in Massachusetts, per ZIP Code and quarter, between 2014 and 2018. This analysis used aggregated pharmacy ZIP Code-quarterly reports of NDEs from the first quarter of 2014 to the third quarter of 2018 in the combined dataset.
2.2.1. ZIP Code level exposure characteristics
We used the American Community Survey (ACS) 5-year estimates (2014–2018) (ACS) to define ZIP Code level demographic characteristics, some of which have been previously examined in pharmacy naloxone studies, including age, gender (Green et al., 2019), race (population percentage White vs. non-White) (Guy et al., 2019; Madden and Qeadan, 2019), ethnicity (population percentage Hispanic vs. non-Hispanic), and income (Egan et al., 2020; Guy et al., 2019). We dichotomized the race category to White vs. non-White (where the category non-White included people who identified as Black/African-American, American Indian and Alaska Native, Asian, Native Hawaiian and Other Pacific Islander, some other race or two or more races) because the other race categories were not large enough to analyze individually. For ethnicity, the ACS only provides the categories Hispanic vs. non-Hispanic.
We additionally examined rurality because a 2019 study revealed that rural counties were three times more likely to be low-dispensing for prescription naloxone than metropolitan counties (Guy et al., 2019). To define rurality, we used the Isolation Scale Score, a continuous variable measuring distance from health care resources—with higher scores indicating greater geographic isolation—to capture rurality in a nuanced, relevant way (Doogan et al., 2018). The scale was constructed with 2010 US Census Bureau data—including from the Bureau’s OpenStreetMaps to assess distances—and data from the US Department of Health and Services, the US Department of Agriculture, and the Federal Communications Commission for inclusion of relevant health care resources (hospitals and physicians, though not pharmacies) (Doogan et al., 2018). The Isolation Scale Score was initially calculated for census tracts then recalculated by the original study authors for ZIP Code areas.
Increased buprenorphine treatment capacity has been associated with increased pharmacy naloxone distribution in a geographic area (Guy et al., 2019), so we additionally examined associations with community-level buprenorphine and methadone treatment admissions. Data for community-level treatment utilization were obtained from the MDPH Bureau of Substance Addiction Services and were defined as the number of methadone and buprenorphine treatment admissions per 100,000 population, a variable used in previous community-level analyses (Walley et al., 2013).
Because communities that have been more affected by overdose mortality may be more likely to make naloxone accessible, we assessed overdose mortality per ZIP Code and quarter. We included data from the Massachusetts Registry of Vital Records and Statistics to determine the count and rate of opioid overdose fatalities that occurred from 2014–2018 per resident ZIP Code. We measured fatal overdoses when the decedent’s primary cause of death was reported with the ICD-10 codes for unintentional or undetermined intentional poisoning (X40-X44, Y10-Y14) in the underlying cause field and an opioid-specific T code (T40.0–T40.4) and/or narcotic T40.6 code in any associated cause of death field.
To assess the relative contribution of naloxone from sources other than standing order, we included a measure of naloxone distributed from another major source—MDPH-funded OEND sites. MDPH gathers information on naloxone distributed at the 23 MDPH-funded OEND programs. We measured OEND naloxone distribution as the total naloxone kits distributed (enrollment and refill) per reported recipient ZIP Code from 2014 to 2018. OEND naloxone is reported as kits, which we compared to NDEs, the vast majority of which are single kits.
Additionally, we assessed the relative contribution of individually prescribed naloxone to overall quantities of dispensed naloxone. Quantities of naloxone dispensed under individual prescriptions were reported by 84% of pharmacies in our dataset.
2.3. Data Analysis and Statistical Methods
We reported quantities of naloxone distributed under NSO per ZIP Code and quarter in Massachusetts during the study period. Of the 538 ZIP codes in Massachusetts, we eliminated ZIP codes that did not contain a retail pharmacy in our dataset, resulting in a list of 281 ZIP codes we used for the primary analysis. We used a deduplicated list of 1042 pharmacies obtained from the Massachusetts State Board of Pharmacy in 2015 for a prior study (Stopka et al., 2017).
In order to determine which variables would be included in our multivariate model, our first step was to assess collinearity between the ZIP Code level factors using a correlation matrix of covariates measuring age, gender, racial/ethnic composition, rurality, income, buprenorphine admissions, methadone admissions, and overdose death rates (see Supplemental Table 1 for a full list of initial covariates). For highly correlated variables that measured similar concepts (for example, proportion of the population with income greater than $75,000, and proportion of the population on public health insurance were highly negatively correlated with a correlation coefficient of −0.763) we retained the fewest number of variables in order to keep the model parsimonious.
For the remaining variables, we computed the variance inflation factor (VIF), a measure of multicollinearity (Lewis-Beck et al., 2012). We pre-specified that we would use a VIF in excess of 5 as an indicator of inflated variance (Lewis-Beck et al., 2012). None of the co-variates had a VIF in excess of 5, therefore no predictors were excluded in this step. Final covariates included percentage of people younger than 25, percentage of people older than 65, percentage of female residents, percentage of individuals who do not identify as White, percentage of residents who identify as Hispanic, Isolation Scale Score, percentage of individuals with income greater than $75,000, buprenorphine admissions per 100,000, methadone admissions per 100,000, quantities of OEND naloxone per ZIP Code-quarter, and overdose deaths per 100,000. We also included calendar year as a term in the adjusted models in order to control for secular trends. In some cases for the multivariate regression model described below, we re-scaled the predictor variable in order to report more clinically relevant effect estimates. For example, rather than reporting change in quantity dispensed under NSO per additional one buprenorphine admission, we re-scaled the change in quantity of naloxone dispensed for every 100 additional buprenorphine admissions.
Due to a high number of zero-count NDEs by ZIP Code-quarters (in 672 out of 3346, or 20.1%, of ZIP Code-quarters, zero NDEs under NSO were reported), we compared model goodness of fit based on a standard negative binomial model or a zero-inflated negative binomial model. We performed a Vuong test of these two models and determined that a zero-inflated negative binomial model provided a better-fitted model over a standard negative binomial model. We employed a generalized estimating equations approach in the regression analysis to account for the clustering of repeated measures of NSO rates by ZIP Code.
We conducted a sensitivity analysis including conventionally prescribed naloxone in the model, though did not include this in the main analysis due to a large proportion of pharmacies (16%) not reporting NDEs under conventional prescriptions. The correlation coefficient between NDEs under NSO and by individual prescriptions was 0.27, and VIF for conventionally prescribed naloxone was also less than 5.
All data cleaning and regression analyses were conducted using R software, version 3.6.3 (R Core Team, 2020).
The project was determined to not be human subjects research by the Boston University Medical Center Institutional Review Board (H-39270).
3. Results
In Figure 1 we depict the geographic distribution of NDEs dispensed by year from 2014 to 2018, revealing a pattern of increasing dispensing under NSO over time. A total of 672 (20.1%) ZIP Code-quarters in our study sample had no naloxone dispensed under NSO, though many of those ZIP Codes did not have a pharmacy as of 2015 (Figure 1). The sociodemographic characteristics of the Massachusetts ZIP Codes included in this analysis are listed in Table 1. The quantity of naloxone kits dispensed via standing order, prescription, and community OEND programs are reported in Table 2 and displayed in Figure 2. Amounts of community OEND dispensed naloxone over the study period are substantial and stay relatively stable over time. In contrast, both pharmacy-dispensed individually prescribed naloxone, and naloxone dispensed under NSO start at very low levels but increase comparably over time (Figure 2).
Figure 1:
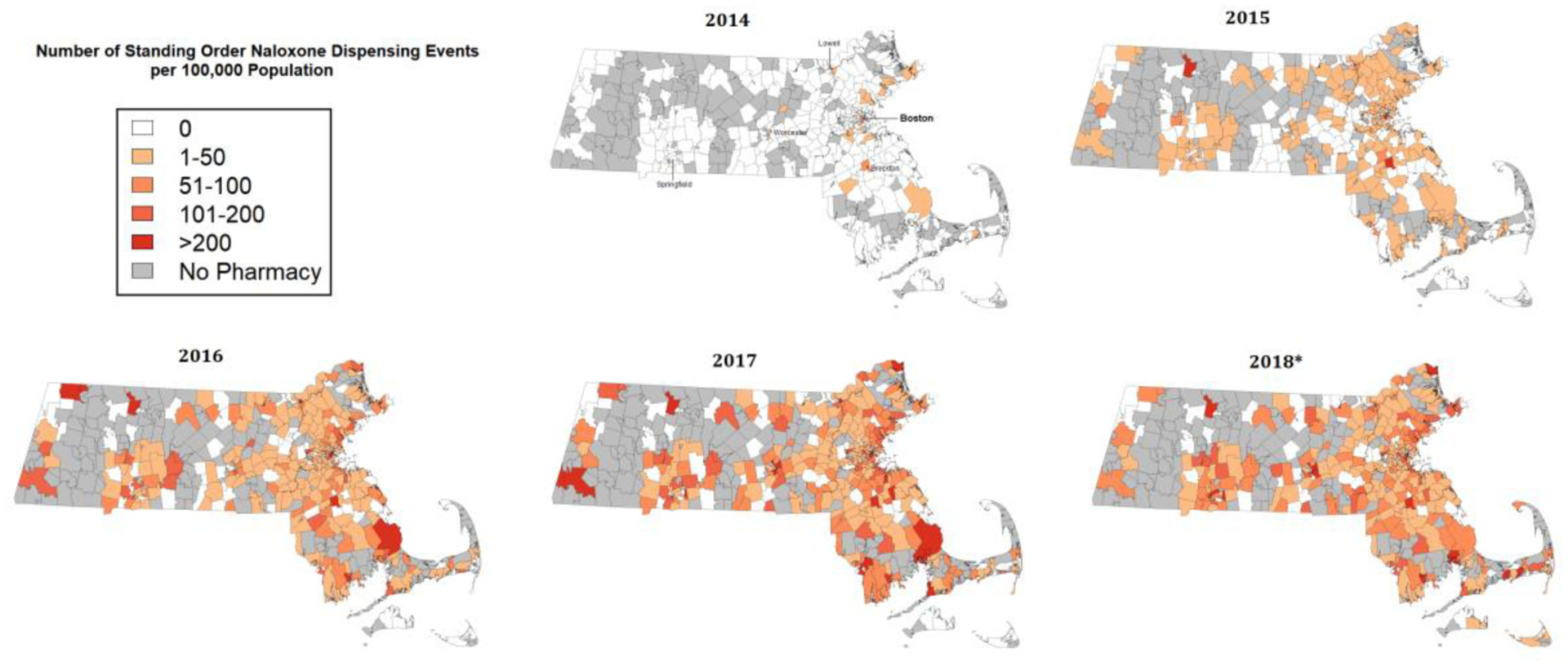
Number of standing order naloxone dispensing events per 100,000 population in Massachusetts ZIP Codes (n=538) by year between 2014 and 2018 in a large sample (70%) of retail pharmacies. ZIP Codes in gray did not have any retail pharmacies in 2015.(Stopka et al., 2017)
* 2018 totals include only three quarters of naloxone dispensing events
Table 1.
Sociodemographic characteristics of residents in Massachusetts ZIP Codes in which retail pharmacies from a large sample (70% of known pharmacies) distributed standing order naloxone between 2014 and 2018 (n=281 of 538 Massachusetts ZIP codes).
| Variables | ZIP Code mean ± SD |
|---|---|
| Age (%) | |
| Less than 25 years old | 30.2 ± 6.4 |
| More than 65 years old | 15.7 ± 5.1 |
| Gender (%) | |
| Female | 51.6 ± 2.3 |
| Race (%) | |
| Nonwhite population | 20.0 ± 17.4 |
| Ethnicity (%) | |
| Hispanic population | 10.5 ± 13.5 |
| Rurality | |
| Isolation score | 4.2 ± 1.4 |
| Income (%) | |
| Annual income greater than 75,000 | 18.7 ± 9.7 |
| Buprenorphine admission (number of admission per 100,000 population) | 29.1 ± 30.2 |
| Methadone admission (number of admission per 100,000 population) | 30.3 ± 35.3 |
| OEND naloxone distribution (dispensing events per 100,000 population) | 104.0 ± 191.9 |
| Distribution under NSO (dispensing events per 100,000 population per quarter) | 21.4 ± 47.7 |
| Overdose related deaths (number of deaths per 100,000 population) | 55.5 ± 177.5 |
SD=Standard Deviation
Isolation=Isolation Scale Score (see Doogan NJ, Roberts ME, Wewers ME, Tanenbaum ER, Mumford EA, Stillman FA. Validation of a new continuous geographic isolation scale: A tool for rural health disparities research. Soc Sci Med. 2018.)
OEND=Overdose Education and Naloxone Distribution
NSO=Naloxone Standing Order
Table 2:
Quantity of naloxone—from a large sample (70%) of retail pharmacies via standing order and non-standing order, and from statewide Overdose Education and Naloxone Distribution Programs—dispensed in Massachusetts between 2014 and the third quarter of 2018,
| Year | Pharmacy, standing order | Pharmacy, non-standing order | Community OEND programs | Total |
|---|---|---|---|---|
| 2014 | 132 | 142 | 15772 | 16046 |
| 2015 | 1679 | 872 | 17491 | 20042 |
| 2016 | 3883 | 2497 | 24894 | 31274 |
| 2017 | 5624 | 4799 | 27667 | 38090 |
| 2018 | 4912 | 4366 | 22006 | 31284 |
Figure 2:
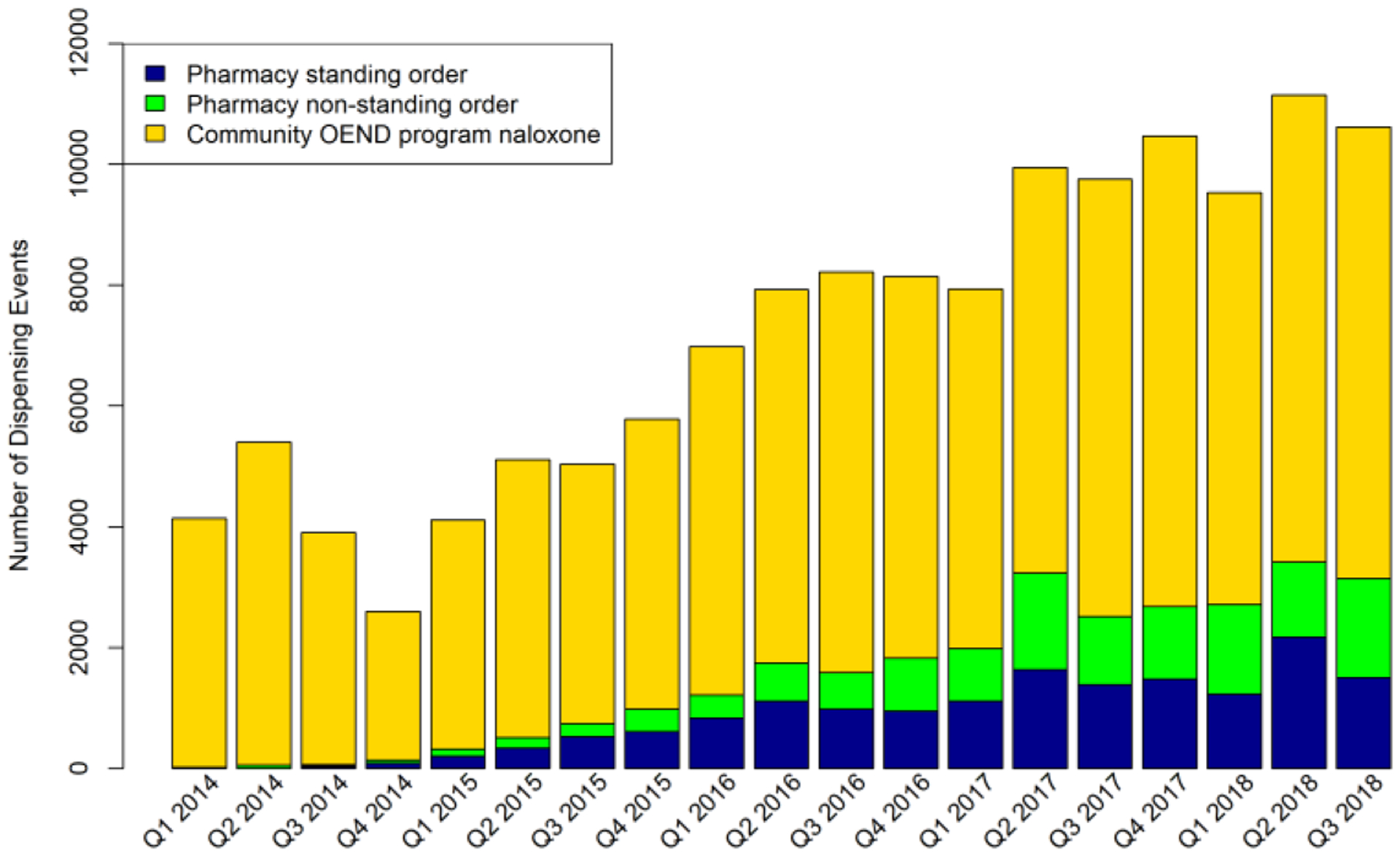
Number of naloxone dispensing events in Massachusetts between 2014 quarter 1 and 2018 quarter 3 from three sources: pharmacy standing order (blue) and prescription naloxone (green) both from a sample of 70% of retail pharmacies in Massachusetts; and naloxone from statewide overdose education and naloxone distribution (OEND) programs from Massachusetts Department of Public Health data (gold).
Compared to 2014, each subsequent year showed a strong positive relationship with the odds of any standing order naloxone dispensed, and the quantity dispensed. In adjusted models there was no relationship between age categories and standing order naloxone dispensed, though there was a relationship between proportion of individuals of female gender and whether or not standing order naloxone was dispensed in a ZIP Code-quarter (adjusted Odds Ratio [aOR] 0.94, 95% CI 0.89–0.98). There was no association between proportion of non-White individuals in a community and standing order naloxone dispensed, however, communities with a higher proportion of individuals with Hispanic ethnicity had a lower odds of any standing order naloxone dispensed at all (aOR 0.91, 95% CI 0.86–0.96). In adjusted models, more rural communities had decreased odds of dispensing any naloxone under standing order (aOR 0.81, 95% CI 0.73–0.90). Additionally, communities with higher percentages of people with income greater than $75,000 were less likely to have any naloxone dispensed under NSO at all (aOR 0.88, 95% CI 0.82–0.95), and lower quantities when it was dispensed (adjusted Rate Ratio [aRR] 0.91, 95% CI 0.87–0.96). Higher numbers of buprenorphine admissions were associated with higher odds of any standing order naloxone (aOR 2.26, 95% CI 1.27–4.03), and a greater quantity of standing order naloxone dispensed (aRR 1.30, 95% CI 1.10–1.53), though this was not true for methadone admissions after adjustment. While there was no association between overdose deaths and whether any standing order naloxone was dispensed (aOR 0.95, 95% CI 0.90–1.00 per 100 overdose deaths), communities with more overdose deaths had more dispensed (aRR 1.12, 95% CI 1.08–1.17 per 100 overdose deaths). Quantity of naloxone distribution by OEND programs was not associated with whether or not standing order naloxone was dispensed, or quantity of standing order naloxone (Table 3).
Table 3.
Unadjusted and adjusted relationships between ZIP Code characteristics, whether standing order naloxone was dispensed, and quantity of standing order naloxone dispensing events from a large sample (70%) of retail pharmacies in Massachusetts, 2014–2018.
| Variables | Zero-inflated model, OR (95% CI) | Negative binomial model, IRR (95% CI) | ||
|---|---|---|---|---|
| Dichotomous odds ratio (OR) outcome of whether any standing order naloxone was dispensed | Incidence rate ratio (IRR) outcome of the quantity of standing order naloxone in zip codes that dispense standing order naloxone | |||
| Unadjusted | Adjusted | Unadjusted | Adjusted | |
| Year | ||||
| 2014 | Ref | Ref | Ref | Ref |
| 2015 | 2.86 (1.61, 5.08) ** | 3.83 (2.13, 6.91) ** | 2.25 (1.64, 3.09) ** | 2.18 (1.59, 2.98) * |
| 2016 | 5.43 (3.09, 9.55) ** | 7.85 (4.38, 14.10) ** | 4.14 (3.03, 5.65) ** | 3.83 (2.80, 5.24) ** |
| 2017 | 7.93 (4.49, 14.02) ** | 11.50 (6.30, 20.88) ** | 5.34 (3.91, 7.29) ** | 4.80 (3.50, 6.59) ** |
| 2018 | 10.92 (6.11, 19.50) ** | 15.91 (8.56, 29.58) ** | 5.58 (4.09, 7.62) ** | 4.96 (3.60, 6.84) ** |
| Age | ||||
| Less than 25 years old (5)◆ | 1.01 (0.94, 1.09) | 1.03 (0.91, 1.15) | 0.84 (0.79, 0.90) ** | 0.96 (0.89, 1.03) |
| More than 65 years old (5)◆ | 0.97 (0.89, 1.05) | 0.99 (0.87, 1.14) | 1.29 (1.19, 1.40) ** | 1.09 (0.99, 1.20) |
| Gender | ||||
| Female (1)◆ | 0.97 (0.93, 1.01) | 0.94 (0.89, 0.98) ** | 1.00 (0.97, 1.03) | 0.98 (0.95, 1.00) |
| Race | ||||
| Nonwhite population (5)◆ | 1.05 (1.02, 1.08) ** | 1.03 (0.97, 1.09) | 1.02 (0.99, 1.05) | 0.99 (0.96, 1.03) |
| Ethnicity | ||||
| Hispanic population (5)◆ | 1.02 (0.99, 1.06) | 0.91 (0.86, 0.96) ** | 1.05 (1.01, 1.08) ** | 0.99 (0.95, 1.02) |
| Rurality | ||||
| Isolation score (1)◆ | 0.94 (0.88, 1.00) | 0.81 (0.73, 0.90) ** | 1.04 (0.97, 1.11) | 1.04 (0.96, 1.12) |
| Income | ||||
| Annual income greater than 75,000 (5)◆ | 0.94 (0.90, 0.99) * | 0.88 (0.82, 0.95) ** | 1.02 (0.97, 1.07) | 0.91 (0.87, 0.96) ** |
| Buprenorphine admission (100)◆ | 4.81 (3.16, 7.31) ** | 2.26 (1.27, 4.03) ** | 2.46 (2.13, 2.83) ** | 1.30 (1.10, 1.53) ** |
| Methadone admission (100)◆ | 2.97 (2.00, 4.41) ** | 1.02 (0.63, 1.64) | 1.98 (1.73, 2.27) ** | 1.12 (0.96, 1.29) |
| Overdose death (100) ◆ | 1.00 (0.95, 1.06) | 0.95 (0.90, 1.00) | 1.14 (1.10, 1.19) ** | 1.12 (1.08, 1.17) ** |
| OEND naloxone distribution (100) ◆ | 1.12 (1.04, 1.22) ** | 1.02 (0.96, 1.09) | 1.12 (1.09, 1.16) ** | 1.02 (0.99, 1.05) |
The zero-inflated model has a dichotomous outcome of whether or not any standing order naloxone was dispensed, while the negative binomial model has an outcome of the quantity of standing order naloxone in ZIP Codes that do dispense standing order naloxone.
The numbers in parentheses indicate the unit of analysis for the regression. For example, for every 5 percentage point increase in proportion of people younger than 25, the odds ratio is 1.04 (0.94, 1.16) in the unadjusted, zero-inflated model.
=p<0.05
=p<0.01
Results from the sensitivity analysis including individually prescribed naloxone were very similar, with individual prescriptions having a minimal association with standing order naloxone (Supplemental Table 1).
4. Discussion
Pharmacy locations where standing order naloxone was dispensed and the quantity of naloxone dispensed under NSO steadily increased after the initiation of the Massachusetts naloxone standing order in 2014, rising steeply starting in 2016 when fentanyl entered the drug supply (Somerville et al., 2017). This rapid and substantial uptake, which occurred in parallel with community OEND expansion, indicates rapid logistical integration and normalization of a standing order of this life-saving medication into existing systems of care. ZIP Codes with higher proportions of Hispanic individuals were less likely to dispense under NSO. Rural ZIP Codes had fewer pharmacies, and thus less likely to have pharmacies that dispensed under NSO. Finally, communities with more buprenorphine admissions and with more overdose deaths had more naloxone dispensed under NSO.
A statewide standing order greatly expanded naloxone dispensing to people and places that may not otherwise have access to naloxone via an OEND program. NSO likely complements OEND program distribution, engages pharmacies in harm reduction activities, is sustainable (in that it is charged to insurance) and appears to be easily integrated into existing health care systems. For states pursuing means of expanding access to naloxone to address increasing numbers of overdose deaths, facilitation of NSO implementation is an important policy option. Whether prescribed or standing order naloxone goes to people at high risk who are likely to use the naloxone to rescue someone overdosing warrants further study to understand how community OEND and pharmacy naloxone distribution complement each other.
Our analysis raises potential issues around equitable distribution of naloxone. The racialization of the opioid epidemic in the United States is well-documented, with criminalization being more likely when addiction affects communities of color, and treatment emphasized when addiction impacts White communities (Mendoza et al., 2019; Netherland and Hansen, 2016). In light of this racialization, previous work has shown that Black people who inject drugs are less likely to use harm reduction services such as syringe services programs and syringes from pharmacies (Rudolph et al., 2010). This analysis revealed mixed results with regard to naloxone dispensed under NSO in ZIP Codes with greater proportions of individuals of non-White race and Hispanic ethnicity. Communities with larger proportions of non-White individuals had the same likelihood and quantity of standing order naloxone dispensed. In contrast, community-level proportion of individuals of Hispanic ethnicity stood out as a factor associated with lower odds of dispensing standing order naloxone. This is concerning because of relatively high and increasing rates of overdose death among Hispanic men in Massachusetts (“Opioid-Related Overdose Deaths, All Intents, MA Residents – Demographic Data Highlights,” 2019), though this finding is consistent with other reports that individuals of Hispanic and Latinx individuals are less likely to be engaged in existing harm reduction services (RACK: Trends in Hispanic and LatinX Communities, 2020). Particularly for individuals of Hispanic or Latinx identity, language barriers, insurance status, lack of culturally appropriate care (Guerrero et al., 2013), and immigration enforcement activities (Hacker et al., 2011) might be factors that play a role in patients asking for naloxone under a standing order and warrant addressing as part of efforts to increase naloxone uptake. A caveat of this analysis is that we examined community-level race and ethnicity variables, so we are unable to assess standing order naloxone dispensing to non-White and Hispanic or Latinx people at the individual level.
Rurality seems to play a complex role with regard to standing order naloxone dispensing. While pharmacies in more isolated ZIP Codes were less likely to dispense under NSO at all, when they did, they dispensed similar quantities of compared to less-isolated communities. Of note, since the definition of rurality in the isolation scale did include distance to hospitals and physicians but not pharmacies, this relationship was not a consequence of the definition itself. In a prior study of retail pharmacy chain dispensed naloxone (individually prescribed and standing order) in Massachusetts and Rhode Island between 2013 and 2017, pharmacies in more rural areas were more likely to dispense naloxone, and dispensed more of it when they did (Green et al., 2019). This difference suggests that rural areas may see more naloxone dispensed in pharmacies through prescription rather than standing order models. Further exploration of barriers to and facilitators of standing order naloxone dispensing in rural communities is warranted, and in particular, what makes a pharmacy willing or able to dispense under a standing order at all. Interestingly, areas with a greater proportion of higher-income individuals were less likely to dispense standing order naloxone and dispensed less of it. This could be a reflection of successful efforts distribute life-saving intervention in higher-poverty communities, which have been shown to have higher overdose rates (Altekruse et al., 2020).
Community-level buprenorphine, but not methadone, admissions as well as overdose death rates were associated with higher likelihood of any NSO dispensed, and greater quantities of NSO dispensed. We expect that in communities where there were more people receiving OUD treatment, that there would be greater awareness, demand, and supply of naloxone, including NSO. Co-prescription (Sohn et al., 2019) of naloxone with buprenorphine for OUD and other opioids prescribed for pain are recommended by the US Department of Health and Human Services since December of 2018 (Naloxone: The Opioid Reversal Drug that Saves Lives, 2018) and the FDA since July of 2020 (“FDA Requiring Labeling Changes for Opioid Pain Medicines, Opioid Use Disorder Medicines Regarding Naloxone,” 2020). Even prior to these national recommendations, based on clinical experience and early research in Massachusetts and Rhode Island, several coauthors on this paper created the program PrescribeToPrevent in order to encourage prescription naloxone dispensing, which included advocating for co-prescription with buprenorphine (Lim et al., 2016).
In our analysis, a similar relationship for methadone went away after adjustment for other factors, including year. We hypothesize that this may be due to some year-to-year fluctuation in missingness in methadone data, or due to adjustment for known racial segregation in methadone treatment (Goedel et al., 2020) and differential geographic locations of pharmacies and methadone programs attenuating the relationship. Still, patients on methadone should also be receiving naloxone, and exploring whether they receive it via other sources (i.e., OEND or prescription naloxone) will be important. In communities where there are higher overdose death rates, we analogously expect greater awareness, demand, and, thus, supply of standing order naloxone. In this analysis, higher overdose death rates were associated with more standing order naloxone dispensed. We believe this association represents appropriate increased access to a life-saving tool in the face of the worsening impact of the opioid crisis. Future studies using causal inference methods that control for confounding by indication should examine how standing order naloxone can reduce overdose deaths.
Our data support policies that lower barriers to naloxone distribution in the community. Studies have shown an association between statewide standing orders giving pharmacists direct authority to dispense naloxone (Abouk et al., 2019), as well as between a broader set of policies expanding naloxone access, and decreased overdose mortality (McClellan et al., 2018). Our data suggest that naloxone distribution under NSO is happening in high-need areas with high growth in distribution over time. Encouraging expansion of NSO implementation, particularly in areas not already receiving naloxone through these programs, is indicated. Further work understanding the reasons for disparities in dispensing under NSO, particularly with regard to Hispanic/Latinx ethnicity and rurality, is vital. Large parts of western Massachusetts, a relatively rural part of the state, do not have a pharmacy at all, and if they do, are less likely to prescribe naloxone. Learning from pharmacies and communities how to promote naloxone dispensing to match community overdose rates—and community outreach to encourage vulnerable individuals to ask for it—will be important. Finally, efforts to coordinate community OEND, individually prescribed, and standing order naloxone across the state will be important to address the current high rates of overdose deaths across communities in Massachusetts.
4.1. Limitations
This was an exploratory analysis and while it can help generate hypotheses for future studies, the associational nature of these findings is limited in determining the causal relationships between community-level factors and dispensing under NSO. The pharmacy data used in this study represent a substantial proportion of Massachusetts pharmacies, but lacks the remaining approximately 30% of pharmacies and their naloxone dispensing data. If pharmacies that were not included serve more rural or more ethnically diverse populations, there may be differential measurement of the exposure and outcome, which could bias the results away from the null. We used a list of pharmacies from 2015, because a more time-varying list was not available, however, we acknowledge that the number and locations of pharmacies may have been more dynamic. Additionally, we assumed that each dispensing event involved one naloxone kit and two doses, however, there may have been variability across communities and prescribers in what a dispensing event entailed. The ZIP Code level characteristics did not indicate who within communities actually received standing order naloxone, and it is possible that residents in ZIP Codes of close proximity may purchase naloxone kit from pharmacies in neighboring ZIP Codes. Data sets with individual-level data with geospatial clustering structure are needed to further describe naloxone distribution equity at the individual level. Finally, the data in this analysis pertained to the period before the state-wide standing order was updated in 2018. The updated standing order named a single statewide standing order writer (as opposed to requiring each pharmacy to name one) and mandated stocking of naloxone (“Policy 2020–07: Naloxone Dispensing,” 2020), which may have further improved standing order naloxone dispensing. However, we were not able to assess the impact of this updated standing order on naloxone dispensing in this analysis.
5. Conclusions
Policies promoting naloxone distribution under a standing order have increased access to this life-saving medication in Massachusetts over time, particularly in areas with high rates of overdose, but distribution from any source may be uneven across the state. Observed disparities in quantities dispensed by community proportion of Hispanic individuals raise questions about the potential structural factors shaping medication access and uptake. Buprenorphine and naloxone seem to be being dispensed together, which should be considered a success, though further exploration of how to make sure that individuals receiving methadone also receive naloxone will be important. Further work elucidating barriers to dispensing under a standing order, especially in rural areas, and strategies to increase standing order naloxone dispensing are necessary.
Supplementary Material
Highlights.
Naloxone by standing order (NSO) in Massachusetts increased from 2014–2018
There are inequities in dispensing NSO based on ethnicity and rurality
More NSO is dispensed in communities with more people receiving buprenorphine
More NSO is dispensed in communities with more opioid-related overdose deaths
NSO has expanded naloxone access but more equitable approaches may be necessary
Acknowledgements
Mary Tomanovich, Jenny Ozga-Hess, Nathan J. Doogan
Role of Funding Source
This work was supported by the National Institute on Drug Abuse [grant numbers R01DA040807, R01DA046527, P30DA040500, R01DA045745]; the National Institute of General Medical Sciences [grant number P20GM125507-01]; and the National Center for Injury Prevention and Control [grant number R01CE002999].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
The authors declare no conflict of interest.
References
- 2018–04: Naloxone Dispensing via Standing Order [WWW Document], 2020. . Mass.gov Website. URL https://www.mass.gov/policy-statement/2018-04-naloxone-dispensing-via-standing-order (accessed 4.23.20).
- Altekruse SF, Cosgrove CM, Altekruse WC, Jenkins RA, Blanco C, 2020. Socioeconomic risk factors for fatal opioid overdoses in the United States: Findings from the Mortality Disparities in American Communities Study (MDAC). PLoS One. 10.1371/journal.pone.0227966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird SM, Mcauley A, Perry S, Hunter C, 2016. Effectiveness of Scotland’s National Naloxone Programme for reducing opioid-related deaths: A before (2006–10) versus after (2011–13) comparison. Addiction. 10.1111/add.13265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Data Brief: Opioid-Related Overdose Deaths among Massachusetts Residents, 2019. . Boston. [Google Scholar]
- Doogan NJ, Roberts ME, Wewers ME, Tanenbaum ER, Mumford EA, Stillman FA, 2018. Validation of a new continuous geographic isolation scale: A tool for rural health disparities research. Soc. Sci. Med 10.1016/j.socscimed.2018.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan KL, Foster SE, Knudsen AN, Lee JGL, 2020. Naloxone Availability in Retail Pharmacies and Neighborhood Inequities in Access. Am. J. Prev. Med 10.1016/j.amepre.2019.11.009 [DOI] [PubMed] [Google Scholar]
- FDA Requiring Labeling Changes for Opioid Pain Medicines, Opioid Use Disorder Medicines Regarding Naloxone, 2020. . USFDA Website. [Google Scholar]
- Goedel WC, Shapiro A, Cerdá M, Tsai JW, Hadland SE, Marshall BDL, 2020. Association of Racial/Ethnic Segregation With Treatment Capacity for Opioid Use Disorder in Counties in the United States. JAMA Netw. open 10.1001/jamanetworkopen.2020.3711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green TC, Bratberg J, Baird J, Burstein D, Lenz K, Case P, Walley AY, Xuan Z, 2019. Rurality and differences in pharmacy characteristics and community factors associated with provision of naloxone in the pharmacy. Int. J. Drug Policy 10.1016/j.drugpo.2019.11.010 [DOI] [PubMed] [Google Scholar]
- Green TC, Davis C, Xuan Z, Walley AY, Bratberg J, 2020. Laws mandating coprescription of naloxone and their impact on naloxone prescription in five US states, 2014–2018. Am. J. Public Health 10.2105/AJPH.2020.305620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerrero EG, Marsh JC, Khachikian T, Amaro H, Vega WA, 2013. Disparities in Latino substance use, service use, and treatment: Implications for culturally and evidence-based interventions under health care reform. Drug Alcohol Depend. 10.1016/j.drugalcdep.2013.07.027 [DOI] [PubMed] [Google Scholar]
- Guy GP, Haegerich TM, Evans ME, Losby JL, Young R, Jones CM, 2019. Vital Signs: Pharmacy-Based Naloxone Dispensing - United States, 2012–2018. MMWR. Morb. Mortal. Wkly. Rep 10.15585/mmwr.mm6831e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hacker K, Chu J, Leung C, Marra R, Pirie A, Brahimi M, English M, Beckmann J, Acevedo-Garcia D, Marlin RP, 2011. The impact of Immigration and Customs Enforcement on immigrant health: Perceptions of immigrants in Everett, Massachusetts, USA. Soc. Sci. Med 10.1016/j.socscimed.2011.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legal Status of Expedited Partner Therapy (EPT) [WWW Document], 2020. . CDC Website. URL https://www.cdc.gov/std/ept/legal/default.htm (accessed 1.23.21).
- Lewis-Beck M, Bryman A, Futing Liao T, 2012. Variance Inflation Factors, in: The SAGE Encyclopedia of Social Science Research Methods. 10.4135/9781412950589.n1067 [DOI] [Google Scholar]
- Lim JK, Bratberg JP, Davis CS, Green TC, Walley AY, 2016. Prescribe to prevent: Overdose prevention and naloxone rescue kits for prescribers and pharmacists. J. Addict. Med 10.1097/ADM.0000000000000223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacQuarrie B, 2014. Governer Declares an Emergency on Opiate Abuse. Boston Globe. [Google Scholar]
- Madden EF, Qeadan F, 2019. Racial inequities in U.S. naloxone prescriptions. Subst. Abus 10.1080/08897077.2019.1686721 [DOI] [PubMed] [Google Scholar]
- Mendoza S, Rivera AS, Hansen HB, 2019. Re-racialization of Addiction and the Redistribution of Blame in the White Opioid Epidemic. Med. Anthropol. Q 10.1111/maq.12449 [DOI] [PubMed] [Google Scholar]
- Naloxone: The Opioid Reversal Drug that Saves Lives, 2018.
- Netherland J, Hansen HB, 2016. The War on Drugs That Wasn’t: Wasted Whiteness, “Dirty Doctors,” and Race in Media Coverage of Prescription Opioid Misuse. Cult. Med. Psychiatry 10.1007/s11013-016-9496-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opioid-Related Overdose Deaths, All Intents, MA Residents – Demographic Data Highlights [WWW Document], 2019. . Massachusetts Dep. Public Heal. Website. URL https://www.mass.gov/doc/opioid-related-overdose-deaths-demographics-february-2019/download (accessed 11.5.20). [Google Scholar]
- Queensland R, 2017. DECLARED STATES OF EMERGENCY – OPIOID CRISIS.
- R Core Team (2020), 2020. R: A language and environment for statistical computing. R A Lang. Environ. Stat. Comput. R Found. Stat. Comput. Vienna, Austria. [Google Scholar]
- RACK: Trends in Hispanic and Latinx Communities, 2020. . Boston. [Google Scholar]
- Rudolph AE, Crawford ND, Ompad DC, Benjamin EO, Stern RJ, Fuller CM, 2010. Comparison of injection drug users accessing syringes from pharmacies, syringe exchange programs, and other syringe sources to inform targeted HIV prevention and intervention strategies. J. Am. Pharm. Assoc 10.1331/JAPhA.2010.09193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen AK, Peterson A, 2020. The pharmacist and pharmacy have evolved to become more than the corner drugstore: a win for vaccinations and public health. Hum. Vaccines Immunother 10.1080/21645515.2019.1660119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohn M, Talbert JC, Huang Z, Lofwall MR, Freeman PR, 2019. Association of Naloxone Coprescription Laws with Naloxone Prescription Dispensing in the United States. JAMA Netw. Open 10.1001/jamanetworkopen.2019.6215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somerville NJ, O’Donnell J, Gladden RM, Zibbell JE, Green TC, Younkin M, Ruiz S, Babakhanlou-Chase H, Chan M, Callis BP, Kuramoto-Crawford J, Nields HM, Walley AY, 2017. Characteristics of Fentanyl Overdose — Massachusetts, 2014–2016. MMWR. Morb. Mortal. Wkly. Rep 66, 382–386. 10.15585/mmwr.mm6614a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stopka TJ, Donahue A, Hutcheson M, Green TC, 2017. Nonprescription naloxone and syringe sales in the midst of opioid overdose and hepatitis C virus epidemics: Massachusetts, 2015. J. Am. Pharm. Assoc 10.1016/j.japh.2016.12.077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, Ruiz S, Ozonoff A, 2013. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: Interrupted time series analysis. BMJ. 10.1136/bmj.f174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wermeling DP, 2015. Review of naloxone safety for opioid overdose: Practical considerations for new technology and expanded public access. Ther. Adv. Drug Saf 10.1177/2042098614564776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson N, Kariisa M, Seth P, Smith H, Davis NL, 2020. Drug and Opioid-Involved Overdose Deaths — United States, 2017–2018. MMWR. Morb. Mortal [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


